
Prepared by
Department of Mental Health Law & Policy
Louis de la Parte Florida Mental Health Institute
College of Behavioral and Community Sciences
University of South Florida
The Florida Mental Health Act
User Reference Guide
2014
Baker Act

Recommended Citation:
Mental Health Program Oce & Department of Mental Health Law & Policy
(2014). 2014 Baker Act User Reference Guide: e Florida Mental Health Act.
Tallahassee, FL: Department of Children and Families, Mental Health Program
Oce; Tampa, FL: University of South Florida, Louis de la Parte Florida Mental
Health Institute.
Louis de la Parte Florida Mental Health Institute Publication, Baker Act Series #253-5
For more information
Baker Act Reporting Center Website:
http://bakeract.fmhi.usf.edu/
FMHI Baker Act Training Website:
http://www.bakeracttraining.org/
Florida Department of Children and Families Baker Act Site:
http://www.dcf.state..us/programs/samh/MentalHealth/laws/index.shtml
Copies of this Manual
is manual is available in electronic form at the Florida Department of Children and
Families Baker Act Website (http://www.dcf.state..us/programs/samh/MentalHealth/
laws/index.shtml).
Additional hard copies of this manual are available at cost through a partnership of
the de la Parte Florida Mental Health Institute at the University of South Florida
and ProCopy. ProCopy will produce bound copies and ship them to your location
throughout the United States and Canada. Orders will typically be processed and
shipped within 3 days. Shipping and handling will be gured individually on orders of
more than one book and communicated to the customer.
Instructions for how to download the manual and order hard copies of manuals can be
found at our Baker Act Reporting Center Website: http://bakeract.fmhi.usf.edu/
is document may be reproduced in whole or part without restriction with proper
attribution to the State of Florida Mental Health Program Oce and the Louis de la Parte
Florida Mental Health Institute at the University of South Florida.

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
i
Introduction
2014 Baker Act —Table of Contents
Introduction
Appendices
Development and Use of Baker Act Handbook v
Use of Handbook .............................................................................. v
Statutes Not Included in Handbook ................................................. v
Baker Act Reporting Center .............................................................. v
Baker Act Website ............................................................................. v
Baker Act Training Online ................................................................ v
Baker Act Technical Assistance vi
Florida’s Judicial Circutes and DCF Regions Map ..........................vi
Managing Entities ...........................................................................vii
DCF Regions and Managing Entities..............................................vii
Baker Act History & Overview ix
Continuity of Care - Relationships xix
Baker Act Flow Chart xx
Statutes and Rules
Short title .................................................................................................1
Legislative intent ......................................................................................1
Denitions...............................................................................................2
Operation and administration .................................................................7
Screening of mental health personnel ....................................................11
Continuity of care management system .................................................12
Assisted living facility.............................................................................18
Introduction or removal of certain articles .............................................20
Rights of patients...................................................................................21
Sexual misconduct ................................................................................58
Florida statewide and local advocacy councils ........................................60
Guardian advocate .................................................................................62
Notice ....................................................................................................65
Rights of professionals ...........................................................................67
Designation of receiving and treatment facilities....................................67
Integrated adult mental health receiving facilities ..................................76
Clinical records; condentiality.............................................................. 77
Transportation .......................................................................................80
Voluntary admissions .............................................................................85
Involuntary examination........................................................................89
Involuntary outpatient placement..........................................................95
Involuntary inpatient placement .........................................................107
Rulemaking authority ..........................................................................113
Procedure for placement of veteran with federal agency.......................113
Admission and discharge procedures....................................................115
Transfer of patients among facilities .....................................................115
Discharge of involuntary patients ........................................................117
Attorney’s fee; expert witness fee ..........................................................117
Involuntary placement from out-of-state mental health authorities .....118
Minors access to outpatient crisis intervention services ........................119
Children admission and placement in mental facilities ........................120
Military veterans and service members court programs .......................121
A Baker Act and Related Laws A1
Marchman Act .............................................................................. A1
Developmental Disabilities ............................................................ A1
Emergency Examination and Treatment of Incapacitated Persons.. A1
EMTALA ....................................................................................... A2
Access to Emergency Services and Care.......................................... A2
Adult Abuse, Neglect, and Exploitation ......................................... A3
Advance Directives ......................................................................... A3
Guardianship.................................................................................. A4
Quick Reference Guide to Related Statutes.................................... A5
B Voluntary Admissions B1
Selected Denitions........................................................................ B1
Criteria ........................................................................................... B1
Exclusions....................................................................................... B1
Right to Discharge ......................................................................... B2
Transfer from Involuntary to Voluntary Status ............................... B2
Transfer from Voluntary to Involuntary Status ............................... B2
Discharge of Persons on Voluntary Status ...................................... B2
Elopement of a Person on Voluntary Status.................................... B3
FORM: Voluntary Admissions Quick Reference Guide for
Receiving and Treatment Facilities ................................................. B4
FIGURE: Adult Seeking Voluntary Admission .............................. B6
FIGURE: Request for Discharge of Person on Voluntary Status ... B7
C Express and Informed Consent C1
Documentation of Competence to Provide Express and Informed
Consent.......................................................................................... C1
Persons Determined Incompetent to Consent to Treatment .......... C2
Persons Adjudicated Incapacitated ................................................. C2
Persons with Health Care Surrogates / Proxies ............................... C3
Summary of Consent Issues ........................................................... C3
TABLE: Summary Reference on Substitute Decision Making ....... C4
FORM: Mental Health Advance Directive .................................... C6
D Consent for Admission and Treatment for Minors D1
Minority/Non-Age .........................................................................D1
Consent to Mental Health Admission ...........................................D3
Admission ................................................................................D3
Hospitals..................................................................................D3
Children’s Crisis Stabilization Units .........................................D3
Consent to Psychiatric Treatment ...................................................D3
Inpatient Treatment .................................................................D3
Residential Treatment Centers .................................................D3
Outpatient Crisis Intervention Services ...................................D4
Substance Abuse (Marchman Act) Admission and Treatment ........D4
Criteria ....................................................................................D4
Initiation .................................................................................D4
Disposition ..............................................................................D5
Parental Participation in Treatment..........................................D5
Release of Information .............................................................D5
Parental Participation/Payment ...............................................D5
Consent for General Medical Care & Treatment............................D5
Power to Consent ...................................................................D5
Emergency Care.......................................................................D5
Emergency Care of Youth in DCF or DJJ Custody .................D6

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Delinquent Youth ..........................................................................D6
Medical, psychiatric, psychological, substance abuse, and
educational examination and treatment ..................................D6
Dependent Youth ..........................................................................D7
Medical, psychiatric, and psychological examination and
treatment of child in DCF Custody.........................................D7
Psychotropic Medications...............................................................D7
Examination, Treatment, & Placement....................................D9
E Baker Act and Long-Term Care Facilities Licensed Under
Chapter 400 and 429 E1
Introduction ................................................................................... E1
Voluntary Admissions .................................................................... E1
Involuntary Examinations .............................................................. E2
Transportation................................................................................ E2
Florida Health Care Association Recommendations ...................... E3
Nursing Homes ............................................................................. E5
Psychotropic Medication Usage Issues............................................ E5
FIGURE: Person Seeking Voluntary Admission............................. E6
Quality First Credentialing Program Best Practices Tools............... E7
F Involuntary Examination F1
Criteria ............................................................................................F1
Initiation .........................................................................................F1
Denitions of Professionals .............................................................F2
Selected Procedures .........................................................................F2
Examination ....................................................................................F2
Release.............................................................................................F3
Escape or Elopement of a Person from a Receiving
or Treatment Facility .......................................................................F3
Notice of Discharge or Release ........................................................F3
FORM: Baker Act Involuntary Examination
Quick Reference Guide for Receiving Facilities ...............................F4
FIGURE: Involuntary Examination................................................F7
G Law Enforcement and the Baker Act G1
Introduction ...................................................................................G1
Voluntary Admission ......................................................................G1
Involuntary Examination ...............................................................G1
Behaviors to Look For ....................................................................G1
Transportation for Medical Emergencies .................................G5
Designation of Transportation Responsibility ..........................G5
Nearest Receiving Facility ........................................................G5
Criminal Charges ...........................................................................G5
Use of Restraining Devices....................................................... G5
Procedures................................................................................G6
Escape or Elopement of Persons from a Baker Act Receiving
Facility .....................................................................................G6
Condentiality of Clinical Records.......................................... G7
Crisis Intervention Teams ........................................................G7
FIGURE: Law Enforcement Ocer (LEO)................................... G9
e Baker Act – A Quick Reference Guide for Law Enforcement
Ocers.........................................................................................G10
Family Interaction with Law Enforcement ...................................G11
H Baker Act and Emergency Medical Conditions H1
Introduction .................................................................................. H1
Voluntary Admission ..................................................................... H1
Criteria for Involuntary Examination ............................................ H1
Initiation of Involuntary Examination .......................................... H2
Certicate of a Professional ..................................................... H2
Baker Act Involuntary Examination .............................................. H3
Emergency Medical Conditions (EMC)........................................ H3
Duties of all Hospitals............................................................. H4
EMTALA and the Baker Act Emergency Medical Treatment and
Active Labor Act............................................................................ H4
Medical & Psychiatric Screening............................................. H5
Medical Clearance .................................................................. H5
Baker Act Exam/Release.......................................................... H6
Transfers.................................................................................. H6
CSU’s...................................................................................... H8
Law Enforcement.................................................................... H8
Safety/Stabilization ................................................................. H8
Informed Consent for Transfer ............................................... H9
Funding .................................................................................. H9
EMTALA Ceases .................................................................. H10
Summary .............................................................................. H10
FIGURE: Emergency Medical Treatment of Persons for Whom
Involuntary Examination has been or will be Initiated ................ H11
I Orders for Emergency Treatment Including Restraints and
Seclusion I1
Introduction .................................................................................... I1
General Management of the Treatment Environment ..................... I2
Individual Behavior Management Programs ................................... I2
Emergency Treatment Orders.......................................................... I2
Restraint and Seclusion .................................................................. I3
Sta Training ................................................................................... I4
Prior to the Implementation of Seclusion or Restraint ................... I4
Implementation of Seclusion or Restraint ....................................... I4
During Seclusion or Restraint......................................................... I6
Release from Seclusion or Restraint and Post-Release Activities ...... I7
Oversight......................................................................................... I7
Reporting ........................................................................................ I7
Emergency Orders for Psychiatric Medications ............................... I8
Initiation of an Emergency Treatment Order For Psychiatric
Medications..................................................................................... I9
Health Care Surrogate and Proxy .................................................. I10
Quick Reference Guide to Restraint and Seclusion ....................... I12
J Involuntary Inpatient Placement J1
Criteria ............................................................................................ J1
Initiation of Involuntary Inpatient Placement ................................. J1
Petition for Involuntary Inpatient Placement .................................. J1
Appointment of Counsel................................................................. J2
Continuance of Hearing.................................................................. J2
Independent Expert Examination ................................................... J2
Hearing on Involuntary Inpatient Placement .................................. J2
Admission to a Treatment Facility ................................................... J3
Release of Persons ............................................................................ J3
Return of Persons ............................................................................ J3
Procedure for Continued Involuntary Inpatient Placement ............ J4
FORM: Quick Reference Guide for Receiving and Treatment
Facilities Involuntary Inpatient Placement ...................................... J5
FIGURE: Involuntary Inpatient Placement .................................... J7
ii

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
iii
Introduction
L
K Involuntary Outpatient Placement K1 O Baker Act/Marchman Act Comparison O1
Introduction ................................................................................... K1
Rights of Persons ............................................................................ K1
Criteria ........................................................................................... K1
Petition........................................................................................... K2
Service Provider .............................................................................. K2
Treatment Plan .............................................................................. K3
County of Filing............................................................................. K3
Notice of Petition ........................................................................... K3
Hearing .......................................................................................... K4
Testimony....................................................................................... K4
Court Order ................................................................................... K5
Continued Involuntary Outpatient Placement............................... K5
Notice of Petition for Continued Involuntary Outpatient Placement.. K5
Hearing on Continued Involuntary Outpatient Placement............ K6
Order for Continued Involuntary Outpatient Placement .............. K6
Modication to Court Order for Involuntary Outpatient Placement.. K6
Change of Service Provider............................................................. K7
Non-Compliance with Court Order .............................................. K7
Discharge from Involuntary Outpatient Placement ....................... K7
FIGURE: Involuntary Outpatient Placement ................................ K8
FIGURE: Non-Compliance with Treatment Order ..................... K10
FIGURE: Modication to Treatment Plans ................................. K10
Qualifications of Professionals & Others to Perform
Baker Act Related Functions L1
Denitions ..................................................................................... L1
Credentials ..................................................................................... L2
FIGURE: Quick Reference Guide to Decision-Making
by Mental Health Professionals and Others.................................... L3
M Baker Act Notices M1
Voluntary Admission .................................................................... M1
Involuntary Examination ............................................................. M1
CHART: Notices/Copies Quick Reference Guide Facilities .......... M3
N Marchman Act History and Overview N1
History ...........................................................................................N1
Related Legislation .........................................................................N1
Legislative Intent ............................................................................N2
Selected Denitions........................................................................N2
Client Rights ..................................................................................N3
Voluntary Admission ......................................................................N4
Involuntary Admissions..................................................................N4
Criteria ...........................................................................................N4
Protective Custody .........................................................................N5
Emergency Admission ....................................................................N5
Alternative Involuntary Assessment for Minors ..............................N5
Involuntary Assessment & Stabilization .........................................N5
Involuntary Treatment....................................................................N5
Provider Responsibilities.................................................................N5
Oversight........................................................................................N6
Quick Reference Guide to Involuntary Admissions under the
Marchman Act ...............................................................................N7
Introduction and History .............................................................. O1
Denitions .................................................................................... O1
Service Providers............................................................................ O3
Voluntary Admissions ................................................................... O3
Involuntary Examination/ Admission Criteria .............................. O4
Procedure for Involuntary Examination/Assessments .................... O5
Transportation Requirements for Involuntary
Examination / Admission .............................................................. O9
Examination or Assessment ......................................................... O12
Release or Discharge.................................................................... O13
Notice of Release from Involuntary Examination / Involuntary
Admission ................................................................................... O14
Involuntary Placement / Involuntary Treatment —
Procedure for Filing Petitions ...................................................... O15
Appointment of Counsel............................................................. O17
Hearings for Involuntary Placement / Treatment ........................ O17
Initial Order ................................................................................ O17
Hearings on Continued Involuntary Placement / Treatment....... O17
Release from Involuntary Placement / Treatment & Notices....... O19
Responsibilities of Providers ........................................................ O20
Rights: General........................................................................... O21
Rights: Individual Dignity.......................................................... O21
Rights: Treatment ....................................................................... O21
Rights: Express and Informed Consent ...................................... O22
Rights: Quality Treatment / Services ........................................... O24
Rights: Condentiality ............................................................... O25
Rights: Communication, Abuse Reporting & Visitation............. O26
Rights: Care & Custody of Personal Eects ................................ O26
Rights: Non-Discrimination ...................................................... O27
Rights: Voting in Public Elections .............................................. O27
Rights: Right to Counsel ............................................................ O27
Rights: Habeas Corpus............................................................... O27
Rights: Separation of Children from Adults ............................... O28
Rights: Education of Minors ...................................................... O28
Special Issues ............................................................................... O28
P Resources P1
Department of Children & Family Services ................................... P1
Managing Entities .......................................................................... P1
Baker Act Website .......................................................................... P1
Receiving Facility List..................................................................... P1
Baker Act Training Online ............................................................. P1
Florida Abuse Registry.................................................................... P1
Agency for Health Care Administration ......................................... P1
Professional Regulation .................................................................. P1
Other State Agencies ...................................................................... P2
Federal Agencies ............................................................................. P2
Advocacy Organizations ................................................................. P3
Family Support............................................................................... P3
Elders ............................................................................................. P4
Addictions ...................................................................................... P4
Other Resources ............................................................................. P5
Baker Act Online Training ............................................................. P5

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Q Military Service Members and Veterans Q1
DD-214 ........................................................................................ Q1
Identifying Veterans....................................................................... Q1
Organizations ................................................................................ Q1
Specic Populations....................................................................... Q2
Veterans Health Initiative .............................................................. Q3
Veterans’ Crisis Line ...................................................................... Q4
Key Phone Numbers ..................................................................... Q4
Veteran’s Issues and the Baker Act ................................................. Q4
R Frequently Asked Baker Act Questions R1
Baker Act Forms
iv

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
v
Introduction
Development and Use of Baker Act Handbook
Use of Handbook
is Handbook is intended to be used for informational
purposes only. e information presented herein is not
legally binding and does not have any legal authority. Only
Chapters 394, F.S. and 65E-5, F.A.C. have legal authority,
as well as Chapter 65E-12, F.A.C. which governs crisis
stabilization units and short-term residential treatment
facilities. Information is provided for purposes of
orientation on how the Baker Act interacts with other laws.
e information is not authoritative in these related areas.
e creation of administrative rules to implement and
clarify the statute is governed by Chapter 120, F.S. e
state law prohibits the repetition of statute in administrative
rules. erefore, individuals must be familiar with and
routinely reference both the statutes and the corresponding
rules to ensure correct implementation of the Baker Act law.
For training purposes, the statute and the corresponding
administrative rules concerning the same subjects have been
displayed side-by-side; statutes are sequentially displayed
in the left column of each page in numerical order. e
corresponding administrative rules are sequentially
displayed in the right column. However, ve rules are
intentionally listed out of numerical sequence to display
them next to the statute to which they refer. ese ve
rules are those governing rights of persons in and operation
of state mental health treatment facilities (Chapters 65E-
5.601 and 65E-5.602), training (Chapter 65E-5.330,
F.A.C.), designation of facilities (Chapter 65E-5.350,
F.A.C.) and funded Baker Act services (Chapter 65E-5.400,
F.A.C.).
To the extent possible, the word “individual” or “person”
is used (rather than “patient”) throughout this Handbook,
except for direct quotes from the statutes and for the
purpose of clarity. Person-rst language works to reduce
stigma and increases professional sensitivity to the dignity
of persons served. Following the display of statutes and
corresponding administrative rules are appendices. ese
appendices contain useful material on select complex
subjects derived from the Baker Act law, administrative
rules, forms, practices and other statutes/case law. All
current Baker Act forms are located in the back of the
handbook.
Statutes Not Included in Handbook
Plan and Report 394.4674; Residential care for psychotic
and emotionally disturbed children 394.4781; Intent
394.4786; South Florida State Hospital Privatization
394.47865; Denitions 394.4787; Use of certain
Public Medical Assistance Trust Fund (PMATF) funds
for the purchase of acute care mental health services
394.4788; Establishment of referral process and eligibility
determination 394.4789.
Baker Act Reporting Center
e Louis de la Parte Florida Mental Health Institute
is designated by the Florida Agency for Health Care
Administration to be the Baker Act Reporting Center. e
purpose of the BA Reporting Center is to receive the Baker
Act involuntary examination initiation forms, orders for
involuntary inpatient/outpatient placement, and cover
sheets submitted by every receiving facility to the Agency for
Health Care Administration (as required by Florida Statutes
Chapter 394), organize and enter the data from the forms
into an electronic database, and provide reports on the data
collected. It is the ocial repository for the Baker Act data.
For more information on Baker Act Reports, please contact
Dr. Annette Christy by email at [email protected] or by
telephone at (813) 279-1923.
e address of the Reporting Center is:
BA Reporting Center
FMHI
13301 Bruce B. Downs Blvd. MHC 2637
Tampa, FL 33612-3807
Baker Act Website
e state’s Baker Act internet site is located at http://www.
dcf.state.fl.us/programs/samh/mentalhealth/laws/index.
shtml. Updated information about the Baker Act can also
be found at the Baker Act Reporting Center website (http://
bakeract.fmhi.usf.edu).
BAKER ACT TRAINING ONLINE
http://www.bakeracttraining.org
Free online courses are available. ey are approved
for Continuing Education Credits (CEs) for a
varienty of professionals. ere is a charge for the
processing of the CEs

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Florida’s Judicial Circuits and DCF Regions
CIRCUT
CIRCUT
14
CIRCUT
CIRCUT
1
CIRCUT
2
3
4
Florida’s 20 Judicial Circuits
e numbers on this map show Florida’s 20 Judicial
Circuits.
DCF Regions
Information about the Department of Children and
Families (DCF) Regions can be found at
http://www.myfamilies.com/contact-us
DCF Headquarters (850) 487-1111
DCF Central Region (407) 317-7000
DCF Northeast Region (904) 723-2000
DCF Northwest Region (850) 872-7648
DCF Southeast Region (561) 837-5078
DCF Southern Region (305) 377-5055
DCF SunCoast Region (813) 558-5500
Managing Entities
e Department of Children and Families contracts
for behavioral health services through regional
systems of care called Managing Entities (MEs).
ese entities do not provide direct services; rather,
they allow the department’s funding to be tailored
to the specic behavioral health needs in the various
regions of the State.
List of and links to web pages of Managing Entities
(MEs) can be found at http://www.myfamilies.com/
service-programs/substance-abuse/managing-entities
CIRCUT
8
CIRCUT
6
CIRCUT
5
CIRCUT
13
CIRCUT
12
CIRCUT
7
CIRCUT
10
Osceola
CIRCUT
9
CIRCUT
18
CIRCUT
19
CIRCUT
20
CIRCUT
CIRCUT
17
CIRCUT
15
11
CIRCUT
Southern
16
Two colorful maps that help clarify the DCF
regions and Managing Entities can be found
online at http://bakeract.fmhi.usf.edu/
vi

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
DCF Regions and Managing Entities
Managing Entities
County
DCF
Region
Managing
Entity
Judicial
Circuit
Alachua Northeast Lutheran Services Florida 8th
Baker Northeast Lutheran Services Florida 8th
Bay Northwest Big Bend Community Based Care 14th
Bradford Northeast Lutheran Services Florida 8th
Brevard Central Central Florida Health System 18th
Broward Southeast Broward Behavioral Health Coalition 17th
Calhoun Northwest Big Bend Community Based Care 14th
Charlotte SunCoast Central Florida Behavioral Health Network 20th
Citrus Central Lutheran Services Florida 5th
Clay Northeast Lutheran Services Florida 4th
Collier SunCoast Central Florida Behavioral Health Network 20th
Columbia Northeast Lutheran Services Florida 3rd
Desoto SunCoast Central Florida Behavioral Health Network 12th
Dixie Northeast Lutheran Services Florida 3rd
Duval Northeast Lutheran Services Florida 4th
Escambia Northwest Big Bend Community Based Care 1st
Flagler Northeast Lutheran Services Florida 7th
Franklin Northwest Big Bend Community Based Care 2nd
Gadsden Northwest Big Bend Community Based Care 2nd
Gilchrist Northeast Lutheran Services Florida 8th
Glades SunCoast Central Florida Behavioral Health Network 20th
Gulf Northwest Big Bend Community Based Care 14th
Hamilton Northeast Lutheran Services Florida 3rd
Hardee Central Central Florida Behavioral Health Network 10th
Hendry SunCoast Central Florida Behavioral Health Network 20th
Hernando Central Lutheran Services Florida 5th
Highlands Central Central Florida Behavioral Health Network 10th
Hillsborough SunCoast Central Florida Behavioral Health Network 13th
Holmes Northwest Big Bend Community Based Care 14th
Indian River Southeast Southeast Florida Behavioral Health Network 19th
Jackson Northwest Big Bend Community Based Care 14th
Jefferson Northwest Big Bend Community Based Care 2nd
Lafayette Northeast Lutheran Services Florida 3rd
Lake Central Lutheran Services Florida 5th
Lee SunCoast Central Florida Behavioral Health Network 20th
Leon Northwest Big Bend Community Based Care 2nd
Levy Northeast Lutheran Services Florida 8th
Liberty Northwest Big Bend Community Based Care 2nd
Madison Northeast Big Bend Community Based Care 3rd
Big Bend Community Based Care
525 North Martin Luther King Jr. Blvd.
Tallahassee, FL 32301
(850) 410-1020
http://www.bigbendcbc.org
Broward Behavioral Health Coalition
1715 SE 4th Avenue
Ft. Lauderdale, FL 33316
(954) 622-8121
http://www.bbhcorida.org
Central Florida Behavioral Health Network
719 US Highway 301 South
Tampa, FL 33619
(813) 740-4811
http://www.cfbhn.org
Central Florida Cares Health System
707 Mendham Blvd., Suite 104
Orlando, FL 32825
(407) 985-3560
http://centraloridacares.org/
Lutheran Services Florida
10450 San Jose Blvd., Unit A
Jacksonville, FL 33257
(904) 900-1075
http://www.lsfnet.org
Southeast Florida Behavioral Health Network
140 Intracoastal Point Drive, Suite 211
Jupiter, FL 33477
(561) 203-2485
http://web.sefbhn.org
South Florida Behavioral Health Network
7205 Corporate Center Drive, Suite 200
Miami, FL 33126
(305) 858-3335
http://sfbhn.org
vii

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
DCF Regions and Managing Entities (Continued)
Two colorful maps that help clarify
the DCF regions and Managing
Entities can be found online at
http://bakeract.fmhi.usf.edu/
DCF Regions
Northeast Region
ME: Lutheran Service Florida
Jacksonville
Northwest Region
ME Big Bend Community BasedCare
Tallahassee
Central Region
ME: Central Florid Cares
Health System
Fern Park
SunCoas Region
ME Centra Florida Behavioral Healt Network
Tampa
Southern Region
ME: Sout Florida Behavioral Healt Network
Miami
Broward County
ME: Broward Behavioral
Health CoaliDon
Broward
Florida Department of Children and Families
Substance Abuse and Mental Health
Region and Circuit Map
Detailing
Regions as indicated by a geographic break in the map,
Circuits as indicated by numbered circles,
DCF Headquarter Offices (HQ),
Managing Entities (ME), and
State Mental Health Treatment Facilities
=
=
DCF Managing Entities Map
Southeast Region
ME Southeas Florida
Behavioral Health
Network
County
DCF
Region
Managing
Entity
Judicial
Circuit
Manatee SunCoast Central Florida Behavioral Health Network 12th
Marion Central Lutheran Services Florida 5th
Martin Southeast Southeast Florida Behavioral Health Network 19th
Miami-Dade Southern South Florida Behavioral Health Network 11th
Monroe Southern South Florida Behavioral Health Network 16th
Nassau Northeast Lutheran Services Florida 4th
Okaloosa Northwest Big Bend Community Based Care 1st
Okeechobee Southeast Southeast Florida Behavioral Health Network 19th
Orange Central Central Florida Health System 9th
Osceola Central Central Florida Health System 9th
Palm Beach Southeast Southeast Florida Behavioral Health Network 15th
Pasco SunCoast Central Florida Behavioral Health Network 6th
Pinellas SunCoast Central Florida Behavioral Health Network 6th
Polk Central Central Florida Behavioral Health Network 10th
Putnam Northeast Lutheran Services Florida 7th
Saint Johns Northeast Lutheran Services Florida 7th
Saint Lucie Southeast Southeast Florida Behavioral Health Network 19th
Santa Rosa Northwest Big Bend Community Based Care 1st
Sarasota SunCoast Central Florida Behavioral Health Network 12th
Seminole Central Central Florida Health System 18th
Sumter Central Lutheran Services Florida 5th
Suwannee Northeast Lutheran Services Florida 3rd
Taylor Northeast Big Bend Community Based Care 3rd
Union Northeast Lutheran Services Florida 8th
Volusia Northeast Lutheran Services Florida 7th
Wakulla Northwest Big Bend Community Based Care 2nd
Walton Northwest Big Bend Community Based Care 1st
Washington Northwest Big Bend Community Based Care 14th
viii

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
ix
Introduction
Baker Act
History & Overview
Statutes governing the treatment of mental illness in Florida
date back to 1874. Amendments to the law were passed
many times over the years but in 1971 the Legislature
enacted the Florida Mental Health Act. is Act brought
about a dramatic and comprehensive revision of Florida’s 97-
year old laws. It substantially strengthened the due process
and civil rights of persons in mental heath facilities.
e Act, usually referred to as the “Baker Act,” was named
after Maxine Baker, former State representative from
Miami who sponsored the Act, while serving as chairperson
of the House Committee on Mental Health. Referring to
the treatment of persons with mental illness before the
passage of her bill, Representative Baker stated “In the
name of mental health, we deprive them of their most
precious possession – liberty.”
Since the Baker Act became eective in 1972, a number of
legislative amendments have been enacted to protect persons’
civil and due process rights. e most recent major revision
was when Involuntary Outpatient Placement was added by
the Legislature eective January 2005.
It is important that the Baker Act only be used in situations
where the person has a mental illness and meets all remaining
criteria for voluntary or involuntary admission. e Baker
Act is the Florida Mental Health Act. It does not substitute
for any other law that may permit the provision of medical
or substance abuse care to persons who lack the capacity to
request such care. For many persons, the use of other statutes
may be more appropriate. Alternatives may include:
Developmental Disabilities, Chapter 393, F.S.
Marchman Act, (Substance Abuse Impairment),
Chapter 397, F.S.
Emergency Examination and Treatment of Incapacitated
Persons, Chapter 401.445, F.S.
Federal Emergency Medical Treatment and Active Labor
Act (EMTALA) hospital “Anti-Dumping” law, 42 USC
1395dd.
Hospital Access to Emergency Services and Care,
Chapter 395.1041, F.S.
Adult Abuse, Neglect, and Exploitation, Chapter
415.1051, F.S.
Advance Directive, Chapter 765, F.S.
Guardianship, Chapter 744, F.S.
Expedited Judicial Intervention for Medical Procedures,
Probate Rule 5.900
Rights of Persons with Mental Illnesses
s. 394.459, F.S. Ch. 65E-5.140, FAC
e Baker Act ensures many rights to persons who have
mental illnesses. Some of these rights are as follows:
Individual Dignity: Ensures all constitutional rights and
requires that persons be treated in a humane way while
being transported or treated for mental illness.
Treatment: Prohibits the delay or denial of treatment
due to a person’s inability to pay and requires prompt
physical examination after arrival; requires treatment
planning to involve the person; and requires the least
restrictive appropriate available treatment be based on
the individual needs of each person.
Express and Informed Consent: Encourages people to
voluntarily apply for mental health services when they
are competent to do so, to choose their own treatment,
and to decide when they want to stop treatment. e
law requires that consent be voluntarily given in writing
by a competent person after sucient explanation to
enable the person to make well-reasoned, willful and
knowing decisions without any coercion.
Quality of Treatment: Requires medical, vocational,
social, educational, and rehabilitative services suited to
each person’s needs to be administered skillfully, safely,
and humanely. Use of restraint, seclusion, isolation,
emergency treatment orders, physical management
techniques, and elevated levels of supervision are
regulated. Grievance procedures and complaint
resolution is required.
Communication, Abuse Reporting, and Visits:
Guarantees persons in mental health facilities the right
to communicate freely and privately with persons
outside the facilities by phone, mail, or visitation. If
communication is restricted, written notice must be
provided. No restriction of calls to the Abuse Registry
or to the person’s attorney is permitted under any
circumstances.
Care and Custody of Personal Effects: Ensures that
persons may keep their own clothing and personal
eects, unless they are removed for safety or medical
reasons. If removed, a witnessed inventory is required.
Voting in Public Elections: Persons are guaranteed the
right to register and to vote in any elections for which
they are qualied voters.
Habeas Corpus: Guarantees the right to ask the
court to review the cause and legality of the person’s
detention or unjust denial of a legal right or privilege
or an authorized procedure.
Treatment and Discharge Planning: Guarantees the
opportunity to participate in treatment and discharge

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
planning and to seek treatment from the professional or
agency of person’s choice upon discharge.
Sexual Misconduct Prohibited: Any sta who engages
in sexual activity with a person served by a receiving/
treatment facility is guilty of a felony. Failure to report
such misconduct is a misdemeanor.
Right to a Representative: Selected by persons (or by
facility when person can’t/won’t select their own) when
admitted on an involuntary basis or transferred from
voluntary to involuntary status. e representative
must be promptly notied of the person’s admission
and all proceedings and restrictions of rights, receives
copy of the inventory of the person’s personal eects,
has immediate access to the person, and is authorized
to le a petition for a writ of habeas corpus on behalf of
the person. e representative can’t make any treatment
decisions, can’t access or release the person’s clinical
record without the person’s consent, and can’t request the
transfer of the person to another facility.
Confidentiality: Ensures that all information about
a person in a mental health facility is maintained as
condential and only released with the consent of the
person or a legally authorized representative. However,
certain information may be released without consent to
the person’s attorney, in response to a court order (after
a good cause hearing), after a threat of harm to others
or other very limited circumstances. Persons in mental
health facilities have the right to access their clinical
records.
Violation of Rights: Anyone who violates or abuses any
rights or privileges of persons provided in the Baker Act
is liable for damages as determined by law.
Voluntary Admissions
s. 394.4625, F.S. Chapter 65E-5.270, F.A.C.
e Baker Act encourages the voluntary admission of
persons for psychiatric care, but only when they are able to
understand the decision and its consequences and are able
to fully exercise their rights for themselves. When this is not
possible due to the severity of the person’s condition, the
law requires that the person be extended the due process
rights assured for those under involuntary status.
Selected Definitions
s. 394.455, F.S.
Several denitions are important to understanding the
criteria for voluntary admissions and consent to treatment.
Mental illness means an impairment of the mental or
emotional processes that exercise conscious control of one’s
actions or of the ability to perceive or understand reality,
which impairment substantially interferes with a person’s
ability to meet the ordinary demands of living, regardless
of etiology. For the purposes of this part, the term does not
include a developmental disability as dened in Chapter
393, intoxication, or conditions manifested only by
antisocial behavior or substance abuse impairment. (18)
Express and informed consent means consent voluntarily
given in writing, by a competent person, after sucient
explanation and disclosure of the subject matter involved to
enable the person to make a knowing and willful decision
without any element of force, fraud, deceit, duress, or other
form of constraint or coercion. (9)
Incompetent to consent to treatment means that a person’s
judgment is so aected by his or her mental illness that the
person lacks the capacity to make a well-reasoned, willful,
and knowing decision concerning his or her medical or
mental health treatment. (15)
Criteria for Voluntary Admissions
s. 394.4625(1)(a), F.S. s. 394.459(3)(a), F.S.
A facility may receive for observation, diagnosis, or
treatment any person 18 years of age or older making
application by express and informed consent for admission
or any person age 17 or under for whom such application
is made by his or her legal guardian. A person age 17 or
under can be admitted only after a hearing to verify the
voluntariness of the consent.
If found to show evidence of mental illness, to be
competent to provide express and informed consent, and
to be suitable for treatment, such person 18 years of age or
older may be admitted to the facility. Each person entering
a facility, regardless of age, must be asked to give express
and informed consent for admission and treatment. If
the person is a minor, express and informed consent for
admission and treatment must also be requested from
the person’s guardian. Express and informed consent for
admission and treatment of a person under 18 years of age
is required from the minor’s guardian.
x

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
xi
Introduction
Voluntary Admission Exclusions
s. 394.4625(1), F.S.
A minor can only be admitted on a voluntary basis if
willing and upon application by his/her legal guardian
and after a judicial hearing to verify the voluntariness of
the consent.
A facility may not admit a person on a voluntary basis
who has been adjudicated by a court as incapacitated.
e health care surrogate or proxy of a person on
voluntary status may not consent to mental health
treatment for the person. erefore, such a person would
be discharged from the facility or involuntary procedures
initiated.
Certain individuals residing in or served by long-
term facilities licensed under Chapter 400 and 429,
F.S., may not be removed from their residence for
voluntary examination unless previously screened by
an independent authorized professional and found to
be able to provide express and informed consent to
treatment.
A person on voluntary status who is unwilling or unable
to provide express and informed consent to mental
health treatment must either be discharged or transferred
to involuntary status.
Consent to Admission/Treatment
Before giving consent to admission or treatment, the
following information must be given to the person or his/
her legally authorized substitute decision-maker:
Reason for admission
Proposed treatment, including proposed psychotropic
medications
Purpose of treatment
Alternative treatments
Specic dosage range for medications
Frequency and method of administration
Common risks, benets and common short-term and
long-term side eects
Any contraindications which may exist
Clinically signicant interactive eects with other
medications
Similar information on alternative medication which
may have less severe or serious side eects
Potential eects of stopping treatment
Approximate length of care
How treatment will be monitored
Disclosure that any consent for treatment may be
revoked orally or in writing before or during the
treatment period if the person legally authorized to make
health care decisions on behalf of the person.
Within 24 hours after a voluntary admission of an adult,
the admitting physician must document in the person’s
clinical record that the person is able to give express and
informed consent for admission and treatment. If the adult
is not able to give express and informed consent, the facility
must either discharge the adult or transfer the person to
involuntary status.
Transfer to Voluntary Status
s. 394.4625(4), F.S.
A person on involuntary status who applies to be
transferred to voluntary status must be transferred unless
the person has been charged with a crime or has been
involuntarily placed for treatment by a court and continues
to meet the criteria for involuntary placement.
Before the transfer to voluntary status is processed, the
mandatory initial involuntary examination must be
performed by a physician or clinical psychologist and a
certication of the person’s competence to consent must
be completed by a physician. In addition, the competent
person must have formally applied for voluntary admission.
Transfer to Involuntary Status
s. 394.4625(5), F.S.
At any time a person on voluntary status is determined not
to have the capacity to make well-reasoned, willful, and
knowing decisions about mental health or medical care, he/
she must be transferred to involuntary status.
When a person on voluntary status, or an authorized
individual acting on the person’s behalf, makes a request
for his/her discharge, the request for discharge, unless
freely and voluntarily rescinded, must be communicated
to a physician, clinical psychologist, or psychiatrist as
quickly as possible, but not later than 12 hours after the
request is made.
If the person meets the criteria for involuntary placement,
the administrator of the facility must le a petition for
involuntary placement with the court within two court
working days after the request for discharge is made. If the
petition is not led within two court working days, the
person must be discharged.

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Discharge of Persons on Voluntary Status
s.394.4625(2), F.S.
A facility must discharge a person on voluntary status:
1. Who has sufficiently improved so that retention in the
facility is no longer clinically appropriate. A person may
also be discharged to the care of a community facility.
2. Who requests discharge. A person on voluntary status
or a relative, friend, or attorney of the person may
request discharge either orally or in writing at any time
following admission to the facility.
e person must be discharged within 24 hours of the
request, unless the request is rescinded or the person
is transferred to involuntary status. e 24-hour
time period may be extended by a treatment facility
(which generally is a state hospital) when necessary for
adequate discharge planning, but must not exceed three
days exclusive of weekends and holidays.
3. A person on voluntary status who has been admitted
to a facility and who refuses to consent to or revokes
consent to treatment must be discharged within 24
hours after such refusal or revocation unless transferred
to involuntary status or unless the refusal or revocation
is freely and voluntarily rescinded by the person.
Involuntary Examination
s. 394.463, F.S. Chapter 65E-5.280, F.A.C.
Criteria
s. 394.463(1), F.S.
A person may be taken to a receiving facility for involuntary
examination if there is reason to believe that he or she has a
mental illness (as dened in the Baker Act) and because of
his or her mental illness:
1. e person has refused voluntary examination after
conscientious explanation and disclosure of the
purpose of the examination; or the person is unable to
determine whether examination is necessary; and
2a) Without care or treatment, the person is likely to suer
from neglect or refuse to care for himself or herself;
such neglect or refusal poses a real and present threat
of substantial harm to his or her well-being; and it is
not apparent that such harm may be avoided through
the help of willing family members or friends or the
provision of other services; or
b) ere is a substantial likelihood that without care or
treatment the person will cause serious bodily harm to
self or others in the near future, as evidenced by recent
behavior.
Initiation of Involuntary Examination
s. 394.463(2), F.S.
An involuntary examination may be initiated by any one of
the three following means:
1. A court may enter an ex parte order stating that a
person appears to meet the criteria for involuntary
examination, giving the ndings on which that
conclusion is based. e ex parte order for involuntary
examination must be based on sworn testimony,
written or oral. No fee can be charged for the ling of a
petition for an order for involuntary examination.
A law enforcement ocer, or other designated agent
of the court, must take the person into custody and
deliver him or her to the nearest receiving facility for
involuntary examination. A law enforcement ocer
acting in accordance with an ex parte order may serve
and execute such order on any day of the week, at any
time of the day or night. A law enforcement ocer
acting in accordance with an ex parte order may use
such reasonable physical force as is necessary to gain
entry to the premises, and any dwellings, buildings, or
other structures located on the premises, and to take
custody of the person who is the subject of the ex parte
order.
e ocer must execute a written report entitled
“Transportation to a Receiving Facility” detailing the
circumstances under which the person was taken into
custody, and the report must be made a part of the
person’s clinical record. [65E-5.260, FAC]
e ex parte order is valid only until executed or, if not
executed, for the period specied in the order itself. If
no time limit is specied in the order, the order is valid
for seven days after the date that the order was signed.
Once a person is picked up on the order and taken to
a receiving facility for involuntary examination and
released, the same order cannot be used again during
the time period. e order of the court must be made a
part of the person’s clinical record.
2. A law enforcement officer must take a person who
appears to meet the criteria for involuntary examination
into custody and deliver the person or have him
or her delivered to the nearest receiving facility for
examination. e ocer must execute a written
report detailing the circumstances (doesn’t require
observations) under which the person was taken into
custody, and the report must be made a part of the
person’s clinical record.
3. A physician, clinical psychologist, clinical social worker,
mental health counselor, marriage and family therapist,
or psychiatric nurse (each as dened in the Baker Act)
may execute a certicate (CF-MH 3052b) stating that
xii

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
xiii
Introduction
he or she has examined the person within the preceding
48 hours and nds that the person appears to meet
the criteria for involuntary examination and stating
the observations of the authorized professional upon
which that conclusion is based. A law enforcement
ocer must take the person named in the certicate
into custody and deliver him or her to the nearest
receiving facility for involuntary examination. e
law enforcement ocer must execute a written report
detailing the circumstances under which the person was
taken into custody. e report and certicate must be
made a part of the person’s clinical record. (While not
authorized by statute, Florida's Attorney General wrote
on May 28, 2008 that physician assistants could under
specic circumstances initiate Baker Act involuntary
examinations.)
Definitions of Professionals
s. 394.455, F.S.
Physician means a medical practitioner licensed under
Chapter 458 or Chapter 459 who has experience in the
diagnosis and treatment of mental and nervous disorders or
a physician employed by a facility operated by the United
States Department of Veterans Aairs which qualies as a
receiving or treatment facility under this part. (21)
Psychiatrist means a medical practitioner licensed under
Chapter 458 or Chapter 459 who has primarily diagnosed
and treated mental and nervous disorders for a period of
not less than three years, inclusive of psychiatric residency.
(24)
Clinical psychologist means a psychologist as dened in s.
490.003(3) with 3 years of postdoctoral experience in the
practice of clinical psychology, inclusive of the experience
required for licensure, or a psychologist employed by
a facility operated by the United States Department of
Veterans Aairs that qualies as a receiving or treatment
facility under this part. (2)
Clinical social worker means a person licensed as a clinical
social worker under Chapter 491. (4)
Mental health counselor means a person licensed as a
mental health counselor under Chapter 491. (37)
Marriage and family therapist means a person licensed as a
marriage and family therapist under Chapter 491 (36)
Psychiatric nurse means a registered nurse licensed under
Chapter 464 who has a master’s degree or a doctorate in
psychiatric nursing and two years of post-master’s clinical
experience under the supervision of a physician. (23)
Selected Procedures
s. 394.463(2), F.S.
Any receiving facility accepting a person based on a
court’s ex parte order, law enforcement ocer’s report or a
professional’s certicate must send a copy of the document
with the required cover sheet to the Agency for Health Care
Administration (via the Baker Act Reporting Center) on the
next working day.
BA Reporting Center, FMHI
13301 Bruce B. Downs Blvd. MHC 2637
Tampa, FL 33612-3807
A person can’t be removed from any long-term care
program or residential placement licensed under Chapter
400/429, F.S. and transported to a receiving facility for
involuntary examination unless an ex parte order, a Law
Enforcement Ocer’s report, or a Professional’s Certicate
is rst prepared. If the condition of the person is such that
preparation of a law enforcement ocer’s report is not
practicable before removal, the report must be completed
as soon as possible after removal, but in any case before
the person is transported to a receiving facility. A receiving
facility admitting a person for involuntary examination
who is not accompanied by the required ex parte order,
professional certicate, or law enforcement ocer’s report
must notify AHCA of the admission by certied mail no
later than the next working day.
Involuntary Examination
s. 394.463(2)(f ), F.S. Chapter 65E-5.2801, F.A.C.
A person must receive an initial mandatory examination
by a physician or clinical psychologist at a receiving
facility without unnecessary delay. is initial mandatory
involuntary examination must include:
1. A thorough review of any observations of the person’s
recent behavior;
2. A review of the document initiating the involuntary
examination and the transportation form;
3. A brief psychiatric history; and
4. A face-to-face examination of the person in a timely
manner to determine if the person meets criteria for
release.
e person can’t be released by a receiving facility without
the documented approval of a psychiatrist, clinical
psychologist, or physician in the hospital’s emergency
department. However, a person may not be held in a
receiving facility for involuntary examination longer than
72 hours. e person must be given prompt opportunity to
notify others of his or her whereabouts.

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Release
s. 394.463(2)(i), F.S.
Within the 72-hour examination period, one of the
following three actions must be taken based on the
individual needs of the person:
1. e person must be released unless he or she is
charged with a crime, in which case the person must be
returned to the custody of a law enforcement ocer; or
2. e person, unless he or she is charged with a crime,
must be asked to give express and informed consent to
placement on voluntary status, and, if such consent is
given, the person must be voluntarily admitted. Such
transfer from involuntary to voluntary status must be
conditioned on the certication by a physician that
the person has the capacity to make well-reasoned,
willful, and knowing decisions about mental health and
medical issues; or
3. A petition for involuntary placement must be
completed within 72 hours and be led with the circuit
court within the 72 hours. If the 72 hours ends on a
weekend or holiday, the ling must be no later than the
next working day thereafter.
Notice of Discharge or Release
s. 394.463(3), F.S. s. 394.469(2), F.S.
Notice of discharge or transfer of a person must be given as
provided in s. 394.4599, F.S. Notice of the release must be
given to the person’s guardian or representative, to any person
who executed a certicate admitting the person to the receiving
facility, and to any court that ordered the person’s evaluation.
Reporting to AHCA
394.463(2)(a)
Any receiving facility accepting a person for involuntary
examination must send the BA Reporting Center cover
sheet (3118) and copy of completed initiating form:
Ex Parte Petition/Order, or
Report of Law Enforcement Ocer, or
Certicate of a Professional
All court orders for Involuntary Placement must also be
sent to the BA Reporting Center within 1 day, including:
Involuntary Inpatient Placement Order
Involuntary Outpatient Placement Order
Continued Involuntary Outpatient Order
Receiving facilities must report directly to AHCA by
certied mail within one working day any long-term care
facility licensed under chapter 400/429, F.S. that does not
fully comply with Baker Act provisions governing voluntary
admissions, involuntary examinations, or transportation.
Transportation of Persons for
Involuntary Examination
394.462, F.S. 65E-5.260, FAC
Law enforcement has no responsibility to transport persons
for voluntary admission. Neither is law enforcement
responsible for transferring persons from a hospital ER
where they may have been medically examined or treated
to a Baker Act receiving facility. In the latter case, the
person’s transfer is the responsibility of the sending hospital,
pursuant to the Federal EMTALA law.
Regardless of whether the involuntary examination is
initiated by the courts, law enforcement, or an authorized
mental health professional, law enforcement is responsible
for transporting the person to the nearest receiving facility
for the examination.
A law enforcement agency may decline to transport a
person to a receiving facility only if:
1. e county has contracted for transportation at the
sole cost to the county, and the law enforcement
ocer and medical transport service agree that the
continued presence of law enforcement personnel is
not expected to be necessary for the safety of the person
to be transported or others. is statute requires the
law enforcement ocer to report to the scene, assess
the risk circumstances, and, if appropriate, to “consign”
the person to the care of the transport company. is
includes nursing homes and ALF’s, but not hospitals.
When a jurisdiction has entered into a county-funded
contract with a transport service for transportation
of persons to receiving facilities, such service must be
given preference for transportation of persons from
nursing homes, assisted living facilities, adult day
care centers, or adult family care homes, unless the
behavior of the person being transported is such that
transportation by a law enforcement ocer is necessary.
2. When a law enforcement ocer takes custody of a
person under the Baker Act, the ocer may request
assistance from emergency medical personnel if such
assistance is needed for the safety of the ocer or the
person in custody.
If the law enforcement ocer believes that a person has
an emergency medical condition, the person may be
rst transported to a hospital for emergency medical
treatment, regardless of whether the hospital is a
designated receiving facility.
An emergency medical condition is dened in Chapter
395, F.S. as a medical condition manifesting itself
by acute symptoms of sucient severity, which may
include severe pain, such that absence of immediate
medical attention could reasonably be expected to
xiv

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
xv
Introduction
result in serious jeopardy to patient health (including
pregnant women and their fetus), serious impairment
to bodily functions, or serious dysfunction of any
bodily organ or part.
Once the person is delivered by law enforcement to
a hospital for emergency medical examination or
treatment and the person is placed in the hospital’s
care, the ocer’s responsibility for the person is over,
assuming no criminal charges are pending.
Eventual transfer of the person from the hospital
oering emergency medical treatment to the designated
receiving facility for an involuntary examination under
the Baker Act is the responsibility of the referring
hospital, unless other appropriate arrangements have
been made.
Other than when an emergency medical condition
exists, the person must be delivered to the nearest
designated receiving facility – not to an emergency
room that might be more convenient to the law
enforcement ocer, unless a Transportation Exception
Plan has been approved by the Board of County
Commissioners and the Secretary of DCF. If the person
requires transfer to a dierent facility for specialized
care, the sending facility is responsible for arranging
safe and appropriate transportation.
3. When a mental health professional member of a state
funded mental health overlay program or mobile
crisis response service (as dened in the statute)
evaluates a person and determines that transportation
to a receiving facility is needed, the service, at its
discretion, may transport the person to the facility or
may call law enforcement or make other transportation
arrangements best suited to the needs of the person.
4. When a transportation exception plan meeting the
criteria set out in s. 394.462 (4), F.S. has been approved
by Board of County Commissioners and the Secretary
of the Department of Children and Families.
e nearest receiving facility must accept persons brought
by law enforcement ocers for involuntary examination.
[s. 394.462(1)(j), F.S.] is means that the law enforcement
ocer will never be legally obligated to further transport a
person once presented to the nearest receiving facility or a
hospital.
Persons with Criminal Charges
394.462, F.S. 65E-5.260, FAC
When an ocer has custody of a person based on either
non-criminal or minor criminal behavior that meets the
statutory guidelines for involuntary examination under the
Baker Act, the law enforcement ocer must transport the
person to the nearest receiving facility for examination.
When any law enforcement ocer has arrested a person for
a felony and it appears that the person meets the statutory
guidelines for involuntary examination or placement under
the Baker Act, such person must rst be processed in the
same manner as any other criminal suspect.
A receiving facility is not required to admit a person charged
with felony charges for whom the facility determines and
documents that it is unable to provide adequate security, but
must provide mental health examination and treatment to
the person where he or she is held. No person brought to a
receiving facility on involuntary status who is charged with
a crime can be released except back to the custody of a law
enforcement ocer.
e costs of transportation, evaluation, hospitalization, and
treatment incurred by persons who have been arrested for
violations of any state law or county or municipal ordinance
may be recovered as provided in s. 901.35, F.S.
Weapons Prohibited on the Grounds of a
Hospital Providing Mental Health Services
394.458, F.S.
Except as authorized by law or hospital administrator,
rearms or deadly weapons cannot be brought into a
hospital providing mental health services. Law enforcement
ocers may choose to lock their rearms in their vehicle
prior to entering such a hospital or may place the rearms
in a lock-box at the hospital, if one exists.
Paperwork Required by the Baker Act
394.462, F.S. 394.463, F.S. 65E-5.280, FAC
A law enforcement ocer must execute a written report
detailing the circumstances under which the person was
taken into custody and the report must be made a part
of the person’s clinical record. A mandatory form entitled
“Transportation to Receiving Facility” (form CF-MH
3100) has been developed to serve this purpose. An ocer
should not simply transport a person and leave him or
her at a receiving facility for involuntary examination
under the Baker Act unless the examination has been
previously initiated by a court, an authorized mental health
professional, or a law enforcement ocer.

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
If the ocer takes an individual to an ED due to a medical
emergency after initiating the involuntary examination, the
“Report of Law Enforcement Ocer Initiating Involuntary
Examination” must be submitted to hospital personnel to
accompany the person to a receiving facility as well as the
transport form.
If the ocer was only transporting a person whose
involuntary examination was initiated by a court or mental
health professional, the ocer must submit the court’s Ex
Parte Order or the Certicate of Professional Initiating
Involuntary Examination, along with the “Transportation
to a Receiving Facility” form completed by the law
enforcement ocer which will be made a part of the
person’s clinical record.
Involuntary Placement
s. 394.467 & .4655, F.S. s. 65E-5.290 & .285, FAC
A person may be ordered for Involuntary Inpatient
Placement upon a nding of the court by clear and
convincing evidence that he or she has a mental illness and
because of his or her mental illness:
1. She/he has refused voluntary placement or is unable to
determine whether placement is necessary; and
2. She/he is incapable of surviving alone or with the
help of others and without treatment is likely to suer
from neglect which poses a real and present threat of
substantial harm to his or her well-being; or
3. ere is substantial likelihood that in the near future
she/he will inict serious bodily harm on self or other
person, as evidenced by recent behavior causing,
attempting, or threatening such harm; and
4. All available less restrictive treatment alternatives which
would oer an opportunity for improvement of his or
her condition have been judged to be inappropriate.
An adult may be involuntarily ordered for Involuntary
Outpatient Placement upon a nding of the court by clear
and convincing evidence that he or she has a mental illness
and because of his or her mental illness:
1. e person is unlikely to survive safely in the
community without supervision, based on a clinical
determination;
2. e person has a history of lack of compliance with
treatment for mental illness;
3. e person has:
a. At least twice within the immediately preceding 36
months been involuntarily admitted to a receiving
or treatment facility as dened in s. 394.455, or
has received mental health services in a forensic or
correctional facility. e 36-month period does not
include any period during which the person was
admitted or incarcerated; or
b. Engaged in one or more acts of serious violent
behavior toward self or others, or attempts at serious
bodily harm to himself or herself or others, within
the preceding 36 months;
4. e person is, as a result of his or her mental illness,
unlikely to voluntarily participate in the recommended
treatment plan and either he or she has refused
voluntary placement for treatment after sucient and
conscientious explanation and disclosure of the purpose
of placement for treatment or he or she is unable to
determine for himself or herself whether placement is
necessary;
5. In view of the person’s treatment history and current
behavior, the person is in need of involuntary
outpatient placement in order to prevent a relapse or
deterioration that would be likely to result in serious
bodily harm to himself or herself or others, or a
substantial harm to his or her well-being as set forth in
s. 394.463(1);
6. It is likely that the person will benet from involuntary
outpatient placement; and
7. All available, less restrictive alternatives that would oer
an opportunity for improvement of his or her condition
have been judged to be inappropriate or unavailable.
Within 72 hours of arrival at facility, or if the 72 hours ends
on a weekend or holiday, no later than the next working day
thereafter, a petition for involuntary inpatient placement
must be led by the receiving facility administrator (or
petition for involuntary outpatient placement may be
led) and supported by the opinion of a psychiatrist and
the second opinion of a clinical psychologist or another
psychiatrist, both of whom have personally examined the
person within the preceding 72 hours, that the criteria for
involuntary placement are met (in certain rural counties
the second opinion may be provided by a physician or
psychiatric nurse, both with special training and experience
as dened in the statute). e second opinion may be done
by electronic means.
e public defender will be appointed by the court to
represent the person unless otherwise represented by
private counsel. e state attorney represents the state,
rather than the petitioning facility administrator, as the real
party in interest in the proceeding. e court will order an
independent expert examination if requested by the person.
xvi

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
xvii
Introduction
e court is required to hold the involuntary placement
hearing within ve (5) court working days unless a
continuance is requested by the person with concurrence
of counsel and granted by the court. e court may
appoint a magistrate to preside at the hearing. One of
the two professionals who executed the involuntary
placement petition must testify at the hearing. e person’s
attendance at the hearing may be waived and the person
may refuse to testify. All testimony must be given under
oath and recorded. At the hearing, the court must consider
testimony and evidence regarding the person’s competence
to consent to treatment. If the court nds that the person
is incompetent to consent to treatment, it must appoint a
guardian advocate.
If the court concludes that the person, by clear and
convincing evidence, meets the criteria for involuntary
inpatient placement, it must order the person to be retained
at or transferred to, or be treated at or by an appropriate
receiving or treatment facility on an involuntary basis, for
a period of up to 6 months. e Florida Supreme Court
has dened “clear and convincing evidence” as that which
is precise, explicit, lacking in confusion, and of such
weight that it produces a rm belief or conviction, without
hesitation, about the matter at issue.
A petition for involuntary outpatient placement can only
be led by an administrator of a receiving or treatment
facility -- if by a receiving facility it must be led in the
county where the facility is located – if by a state hospital
administrator, it must be led in the county where the
person will be living. In either case, a service provider
must be designated to develop with the person a proposed
treatment plan (that meets specic criteria) for the court’s
consideration and attach the proposed plan to the petition.
e service provider cannot propose nor can the court
order services unless they are readily available for the person
in the community, funded, determined by an authorized
mental health professional to be clinically appropriate, and
for which the service provider agrees to deliver.
A person can be held at a receiving facility pending the
court hearing on involuntary outpatient placement
unless stabilized in which case the person must be released
pending the hearing.
If material modications later need to be made to the
involuntary outpatient placement order or approved
treatment plan and there are no objections, the court must
be notied. If there are objections to proposed material
changes, the court must consider whether or not to approve
those changes.
If in the clinical judgment of a physician, the person has
failed or refused to comply with involuntary outpatient
treatment ordered by the court and eorts were made
to solicit compliance, and the person meets criteria for
involuntary examination, the person may be brought to
a receiving facility. If the person doesn’t meet the criteria
for involuntary inpatient placement, the person must be
discharged from the receiving facility. e service provider
must then determine if modications should be made to
the existing treatment plan and try to continue to engage
the person in treatment.
Continued Involuntary Placement
s. 394.4655(7), F.S. Ch. 65E-5.285(4), FAC
If a person continues to meet the criteria for involuntary
placement, the administrator is required, prior to the
expiration of the period during which the treatment facility
is authorized to retain the person or a service provider is
authorized to treat the person, to le a petition requesting
authorization for continued involuntary placement.
e request must be accompanied by a statement from
the person’s physician or clinical psychologist justifying
the request, a brief description of the person’s treatment
during the time he/she was involuntarily placed, and an
individualized plan of continued treatment.
Hearings on petitions for continued involuntary inpatient
placement are administrative rather than judicial hearings
and are conducted by an administrative law judge.
Hearings on petitions for continued involuntary outpatient
placement are judicial and are conducted by the circuit
court. Unless the person is otherwise represented by private
counsel, he/she will be represented at the hearing by the
public defender. If at a hearing it is shown that the person
continues to meet the criteria for involuntary placement,
the judge will sign the order for continued involuntary
placement for a period not to exceed 6 months. e same
procedure can be repeated prior to the expiration of each
additional period the person is retained.
e 5DCA ruled that within the six month maximum
period of an order for involuntary inpatient placement
that the circuit court has concurrent jurisdiction over
commitment proceedings. After the six month period
expires, all placements must be handled through
administrative hearings.

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Discharge of Persons on Involuntary
Status
s. 394.469, F.S. Ch. 65E-5.320, FAC
Receiving and treatment facilities, as well as service
providers, are required to discharge a person at any time
the person no longer meets the criteria for involuntary
placement, unless the person has transferred, by express
and informed consent, to voluntary status. If the person
being discharged is under a criminal charge, he or she
must be transferred to the custody of the appropriate law
enforcement agency at the time of release.
Transfers
s. 394.4685, F.S. Ch. 65E-5.310, FAC
Transfers of persons with emergency medical conditions
(including psychiatric and substance abuse emergencies)
from hospital emergency departments are governed by the
federal EMTALA “anti-dumping” law and Florida’s hospital
licensing law. If a person requires transfer from a hospital
emergency department that has provided the person
evaluation or treatment for an emergency medical condition
to a Baker Act receiving facility, the transfer must take
place within 12 hours after the condition has stabilized.
Otherwise, under provisions of the Baker Act governing
transfers between designated receiving and treatment
facilities, transfers may occur:
Between public facilities, upon the request of the
person or specied others or upon the discretion of
the department to meet the medical or mental health
treatment needs of the person or the availability of
appropriate facility resources.
From public to private facilities, upon request of the
person, guardian or guardian advocate and upon
acceptance of the person by the private facility.
From private to public facilities upon request of the
person, guardian, guardian advocate, or private facility,
and upon acceptance of the person by the public
facility. e public facility must respond to a request for
the transfer within 2 working days after receiving the
request. e cost of such transfer requested by a private
facility is the responsibility of the sending facility.
Between private facilities upon request of the person,
guardian, or guardian advocate, and upon acceptance of
the person by the facility to which transfer is sought.
Oversight
s. 394.457, F.S.
e Department of Children and Family Services
(DCF) is designated the “Mental Health Authority” of
Florida. e Department and the Agency for Health
Care Administration (AHCA) exercise executive and
administrative supervision over all mental health facilities,
programs, and services.
DCF is required to report to AHCA any violation of the
rights or privileges of persons, or of any procedure provided
by any facility or professional licensed or regulated by
AHCA.
DCF is required to adopt rules establishing forms and
procedures relating to the rights and privileges of persons
seeking mental health treatment from designated receiving and
treatment facilities. Unless designated by DCF, facilities are not
permitted to hold or treat persons on involuntary status.
Disability Rights Florida (formerly known as the Advocacy
Center for Persons with Disabilities) is a private nonprot
organization that receives federal funding to protect and
advocate for the rights of persons who have disabilities.
Disability Rights Florida prioritizes services to people
with psychiatric disabilities in institutional inpatient and
residential treatment settings. Some services are provided
to those living independently as resources allow. Services to
individuals include information and referrals, self advocacy
support, technical assistance, investigations into complaints
of abuse, neglect and rights violations, support in dispute
resolution, negotiation and mediation, as well as advocacy
services. Statewide initiatives include workshops and
trainings, education of policymakers, systemic and legal
advocacy, collaborative work on disability rights issues and
the monitoring of public programs and facilities. Disability
Rights Florida has oces in Tallahassee, Tampa, and Ft.
Lauderdale, from which it serves the entire state of Florida
Contact can be made through www.disabilityrightsorida.org
or 1-800-342-0823. (1-800-346-4127 TDD).
Immunity
394.459(10), F.S.
Any person who acts in good faith in compliance with
the provisions of the Baker Act is immune from civil or
criminal liability for his or her actions in connection with
the admission, diagnosis, treatment, or discharge of a
person to or from a facility. However, this section does not
relieve any person from liability if such person commits
negligence.
xviii
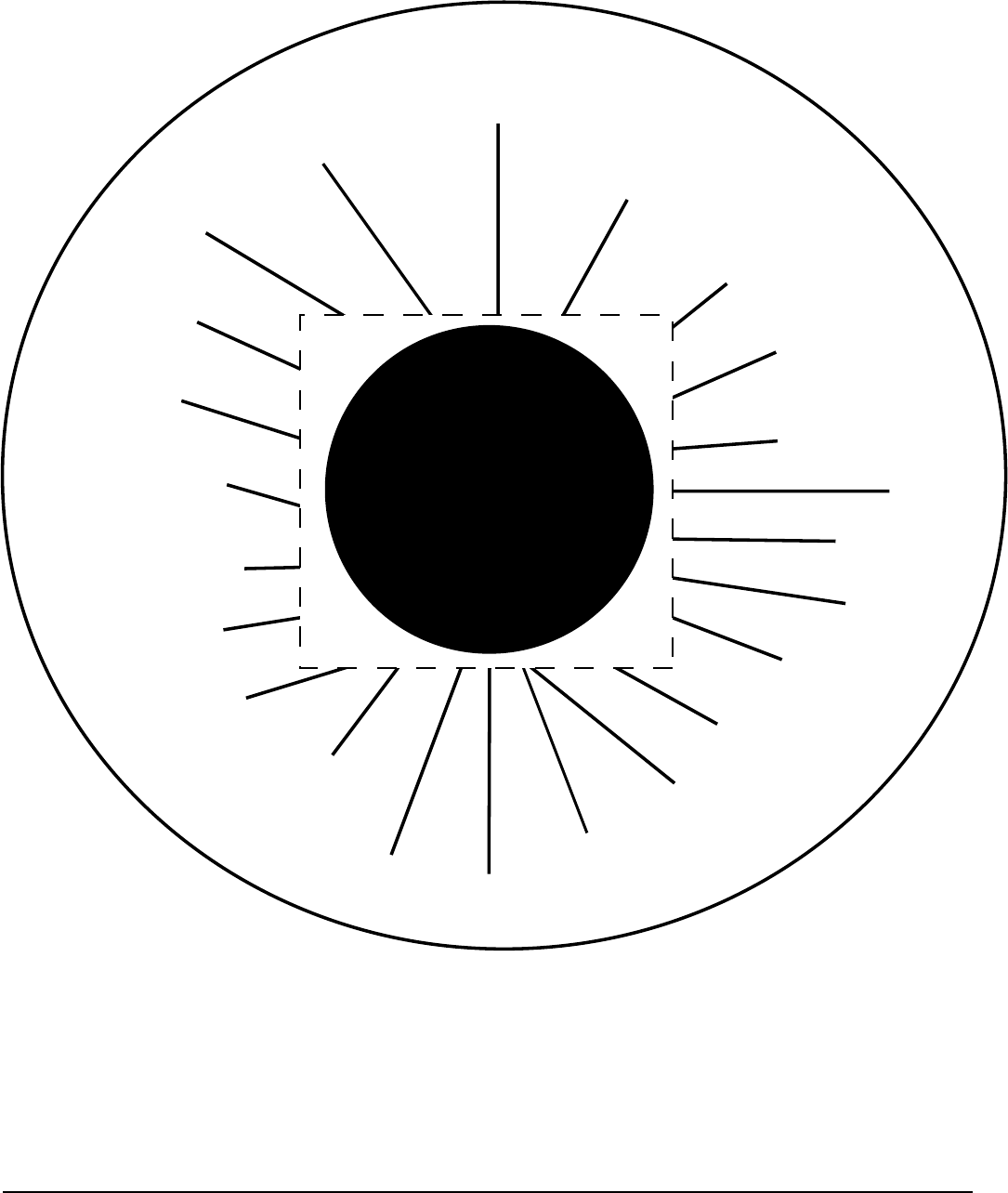
Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
xix
Introduction
Continuity of Care - Relationships
Agency for Health
Care Administration
(AHCA) Licensing
(Hospitals/CSU’s)
Designated Receiving
Facilities
Law Enforcement
Department of
Children & Families
(DCF) Receiving
Facility Designation
County Government
Matching Funds
Jails
Clerks of Court
Circuit Courts
State Attorneys
Public Defenders
Persons with
Mental Illnesses
Homeless Coalitions
State Mental
Health Facilities
Emergency
Departments
Community
Hospitals
Assisted Living
Facilities
Nursing Homes
Children’s Residential
Treatment Centers
Public School Systems
Substance Abuse
Baker Act
Acute Care System
Advocates
Families
Mental Health
Professionals
Baker Act
Acute Care System

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Baker Act Flow Chart
Person receives
physical exam within
24 hours of arrival
Person presents self at receiving
facility for psychiatric exam
and treatment
Person is examined by physician for
competence to consent to
admission/treatment within 24 hours
of arrival
(found to be able to make well-reasoned
willful, knowing medical and mental
health decisions)
Voluntary
Admission
Baker Act Flow Chart
Involuntary
u
Examination
Initiated by:
-ex parte order of court
-law enforcement officer
-professional's certificate
Taken into custody by law en-
forcement officer (few exceptions
available in law) and transported
to nearest receiving facility for
examination
Person receives physical
exam within 24 hours
after arrival
Appears to meet criteria
for involuntary
inpatient/outpatient
placement
Does not meet criteria
for involuntary
inpatient/outpatient
placement
Transferred to volun-
tary status if criteria
is met
Discharged
Appears to meet
criteria for involuntary
placement
Discharged
Transferred to volun-
tary status if criteria
is met
Petition signed by receiving
treatment facility administrator and
filed with court within 72 hours of
arrival at receiving facility
(sooner if delayed at ER).
Guardian advocate
appointed
May consent or refuse
consent to own treatment
unless IOP order states
otherwise
Involuntarily placed
inpatient/outpatient for
up to 6 months
Determined by court to be
competent to consent to own
treatment
Determined by court to be
incompetent to consent to
own treatment
Person improved so that
one or more criteria for
involuntary inpatient/out-
patient placement is not
met
Prior to end of order, if
person continues to meet all
criteria for involuntary inpa-
tient/outpatient placement
Does not meet
involuntary placement
criteria
Person examined by
psychologist or 2nd psychiatrist
(or other authorized professional in rural locale)
u
u
u
u
u
u
u
u
u
u
u
xx

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
Discharged
Permitted to consent or refuse consent to treatment
Treatment continued until person is sufciently improved, or
refuses/revokes consent to treatment, or requests discharge
Person is discharged or transferred to
involuntary status
Incompetent
to consent
Competent
to consent
Incompetent
to consent
Competent
to consent
Petition for adjudication of incompetence to consent to treatment
and appointment of a guardian advocate filed with court - health care
surrogate/proxy, if available, notified
Appears to meet
criteria for involuntary
inpatient/outpatient-
placement
Does not meet
criteria for involuntary
inpatient/outpatient
placement
Transferred to voluntary
status if above criteria
is met and no criminal
charges.
Discharged
Court appoints PD and notifies
person of right to an independent
expert examination
Clerk immediately notifies PD of ap-
pointment and the SAO to represent
the state. Clerk provides copy of
petition to required parties
Does not meet one or more
criteria for involuntary inpatient/
outpatient placement
Hearing conducted within 5 work-
ing days by judge or magistrate
Person discharged
Meets all criteria for involuntary
inpatient/outpatient placement
Meets Marchman Act criteria
Ordered for 5 day involuntary
assessment
Person is discharged
Person is transferred to voluntary
status if criteria is met
Petition for continued involun-
tary inpatient placement filed by
administrator with State Division
of Administrative Hearings
Petition for continued involuntary
outpatient placement filed with
clerk of court
Person is transferred
to voluntary status if
criteria is met
Person is discharged
Determined by administrative
law judge or circuit court
to meet all criteria for
involuntary inpatient/
outpatient placement
Determined by
administrative law judge
or circuit court to not
meet one or more criteria
for involuntary inpatient/
outpatient placement
Initial mandatory examination performed without
unnecessary delay by clinical psychologist or physician
u
Person examined by physician
for competence to consent
to treatment within 24 hours
of arrival
Order is signed for subsequent
period of involuntary
inpatient/outpatient
placement for up to
6 months
q
Person examined by
a psychiatrist (1st
opinion) if initial
mandatory exam was
performed by other
than a psychiatrist
u
u
u
u
u
u
u
u
u
u
u
u
u
u
xxi

Baker Act Handbook and User Reference Guide 2014
State of Florida Department of Children & Families
Introduction
xxii

i Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute & Rule Matrix — Florida Mental Health Act (Baker Act)
Statute Contents
Corresponding Rule Section
Page
394.451 Short title
N/A
1
394.453 Legislative intent
N/A
1
394.455 Denitions
65E-5.100 Definitions
2
394.457 Operation and administration
65E-5.110 Delegation of Authority
7
65E-5.120 Forms
8
394.4572 Screening of mental health personnel
N/A
11
394.4573 Continuity of care management system; measures
of performance; reports
65E-5.130 Continuity of Care Management System
12
65E-5.1301 Transfer Evaluations for Admission to State
Mental Health Treatment Facilities from
Receiving Facilities
13
65E-5.1302 Admissions to State Treatment Facilities
15
65E-5.1303 Discharge from Receiving and Treatment
Facilities
15
394.4574 Department responsibilities for a mental health
resident who resides in an assisted living facility
that holds a limited mental health license
N/A
18
394.458 Introduction or removal of certain articles
unlawful; penalty
N/A
20
394.459 Rights of patients
65E-5.140 Rights of Persons.
21
65E-5.150 Person’s Right to Individual Dignity
22
65E-5.160 Right to Treatment
23
65E-5.1601 General Management of the Treatment
Environment
24
65E-5.1602 Individual Behavioral Management Programs
25
65E-5.170 Right to Express and Informed Consent
26
65E-5.1703 Emergency Treatment Orders
32
65E-5.180 Right to Quality Treatment
35
65E-5.1802 Maintenance of the Facility
50
65E-5.190 Right to Communication and Visits
51
65E-5.200 Right to Care and Custody of Personal Effects
53
65E-5.210 Right to Vote in Public Elections
53
65E-5.220 Right to Habeas Corpus
54
65E-5.601 Operation and Administration of State Mental
Health Treatment Facilities
54
65E-5.602 Rights of Residents of State Mental Health
Treatment Facilities
55
394.4593 Sexual misconduct prohibited; reporting required;
penalties
N/A
58
394.4595 Florida statewide and local advocacy councils;
access to patients and records (Defunded by 2010
Legislature)
N/A
60
394.4597 Persons to be notied; patient’s representative 61
394.4598 Guardian advocate
65E-5.230 Guardian Advocate
62
65E-5.2301 Health Care Surrogate or Proxy
64

ii
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute Contents
Corresponding Rule Section
Page
394.4599 Notice
N/A
65
394.460 Rights of professionals
N/A
67
394.461 Designation of receiving and treatment facilities
65E-5.350 Eligibility Criteria and Procedures for
Designation of Baker Act Receiving Facilities
67
65E-5.351 Minimum Standards for Designated Receiving
Facilities
73
65E-5.352 Procedures for Complaints and Investigations
in Receiving Facilities
74
65E-5.353 Criteria and Procedures for Suspension or
Withdrawal of Designation of Receiving
Facilities
75
394.4612 Integrated adult mental health crisis stabilization
and addictions receiving facilities
N/A
76
394.4615 Clinical records; condentiality
65E-5.250 Clinical Records; Confidentiality
77
394.462 Transportation
65E-5.260 Transportation
80
65E-5.2601 Transportation Exception Plan
84
394.4625 Voluntary admissions
65E-5.270 Voluntary Admission
85
394.463 Involuntary examination
65E-5.280 Involuntary Examination
89
65E-5.2801 Minimum Standards for Involuntary
Examination Pursuant to Section 394.463, F.S
91
394.4655 Involuntary outpatient placement
65E-5.285 Involuntary Outpatient Placement
95
394.467 Involuntary inpatient placement
65E-5.290 Involuntary Inpatient Placement
107
65E-5.300 Continued Involuntary Inpatient Placement at
Treatment Facilities
111
394.46715 Rulemaking authority
N/A
113
394.4672 Procedure for placement of veteran with federal
agency
N/A
113
394.468 Admission and discharge procedures
N/A
115
394.4685 Transfer of patients among facilities
65E-5.310 Transfer of Persons Among Facilities
116
394.469 Discharge of involuntary patients
65E-5.320 Discharge of Persons on Involuntary Status
118
394.473 Attorney’s fee; expert witness fee
N/A
117
394.475 Acceptance, examination, and involuntary
placement of Florida residents from out-of-state
mental health authorities
N/A
118
394.4784 Minors; access to outpatient crisis intervention
services and treatment
N/A
119
394.4785 Children and adolescents; admission and
placement in mental facilities
N/A
120
394.47891 Military veterans and service members court
programs
N/A
121
65E-5.330 Training
122
65E-5.400 Baker Act Funded Services Standards
123
*e following sections of Chapter 394,FS (Baker Act) have been intentionally omitted from this matrix and the sections that follow: 394.4674 –
Plan and report; 394.4781 – Residential care for psychotic and emotionally disturbed children; 394.4786 – Intent; 394.47865 – South Florida State
Hospital; privatization; 394.4787 – Denitions; ss. 394.4786, 394.4787, 394.4788, and 394.4789; 394.4788 – Use of certain PMATF funds for the
purchase of acute care mental health services; and 394.4789 – Establishment of referral process and eligibility determination.

1 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.453 F.S.)
65E-5 F.A.C.
394.451 Short title.
is part shall be known as “e Florida Mental
Health Act” or “e Baker Act.”
394.453 Legislative intent.
It is the intent of the Legislature to authorize
and direct the Department of Children and
Family Services to evaluate, research, plan, and
recommend to the Governor and the Legislature
programs designed to reduce the occurrence,
severity, duration, and disabling aspects of mental,
emotional, and behavioral disorders. It is the intent
of the Legislature that treatment programs for
such disorders shall include, but not be limited
to, comprehensive health, social, educational, and
rehabilitative services to persons requiring intensive
short-term and continued treatment in order to
encourage them to assume responsibility for their
treatment and recovery. It is intended that such
persons be provided with emergency service and
temporary detention for evaluation when required;
that they be admitted to treatment facilities on a
voluntary basis when extended or continuing care
is needed and unavailable in the community; that
involuntary placement be provided only when
expert evaluation determines that it is necessary;
that any involuntary treatment or examination
be accomplished in a setting which is clinically
appropriate and most likely to facilitate the person’s
return to the community as soon as possible;
and that individual dignity and human rights be
guaranteed to all persons who are admitted to
mental health facilities or who are being held under
s. 394.463. It is the further intent of the Legislature
that the least restrictive means of intervention be
employed based on the individual needs of each
person, within the scope of available services. It
is the policy of this state that the use of restraint
and seclusion on clients is justied only as an
emergency safety measure to be used in response
to imminent danger to the client or others. It is,
therefore, the intent of the Legislature to achieve
an ongoing reduction in the use of restraint and
seclusion in programs and facilities serving persons
with mental illness.
N/A
N/A
Crisis Stabilization
Units (CSU) and short-term
residential treatment (SRT)
facilities licensed under Chapter
394, Part IV, FS are also
governed by
65E-12, F.A.C.
Receiving facilities
are governed by other federal
and state laws or accreditation
standards as well as their own policies
and procedures. When in conict,
whichever applies to a facility and
is most stringent and/or protective
of the person's rights should be
followed.
Legislative Intent

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
2
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.455 F.S.)
65E-5.100 F.A.C.
394.455 Denitions.
As used in this part, unless the context clearly
requires otherwise, the term:
(1) “Administrator” means the chief administrative
ocer of a receiving or treatment facility or his
or her designee.
(2) “Clinical psychologist” means a psychologist
as dened in s. 490.003(7) with 3 years of
postdoctoral experience in the practice of clinical
psychology, inclusive of the experience required
for licensure, or a psychologist employed
by a facility operated by the United States
Department of Veterans Aairs that qualies as a
receiving or treatment facility under this part.
(3) “Clinical record” means all parts of the record
required to be maintained and includes all
medical records, progress notes, charts, and
admission and discharge data, and all other
information recorded by a facility which pertains
to the patient’s hospitalization or treatment.
(4) “Clinical social worker” means a person licensed
as a clinical social worker under chapter 491.
(5) “Community facility” means any community
service provider contracting with the department
to furnish substance abuse or mental health
services under part IV of this chapter.
(6) “Community mental health center or clinic”
means a publicly funded, not-for-prot center
which contracts with the department for
the provision of inpatient, outpatient, day
treatment, or emergency services.
(7) “Court,” unless otherwise specied, means the
circuit court.
(8) “Department” means the Department of
Children and Family Services.
(9) “Express and informed consent” means consent
voluntarily given in writing, by a competent
person, after sucient explanation and disclosure
of the subject matter involved to enable the
person to make a knowing and willful decision
without any element of force, fraud, deceit,
duress, or other form of constraint or coercion.
(10) “Facility” means any hospital, community
facility, public or private facility, or receiving or
65E-5.100 Definitions.
As used in this chapter the following words and phrases
have the following definitions:
(1) Advance directive means a witnessed written
document described in Section 765.101, F.S.
(2) Assessment means the systematic collection and
integrated review of individual-specific data. It is
the process by which individual-specific information
such as examinations and evaluations are gathered,
analyzed, monitored and documented to develop
the person’s individualized plan of treatment
and to monitor recovery. Assessment specifically
includes efforts to identify the person’s key medical
and psychological needs, competency to consent
to treatment, patterns of a co-occurring mental
illness and substance abuse, as well as clinically
significant neurological deficits, traumatic brain
injury, organicity, physical disability, developmental
disability, need for assistive devices, and physical or
sexual abuse or trauma.
(3) Certified recovery specialist means an individual
credentialed by the Florida Certification Board as a
Certified Recovery Peer Specialist, Certified Recovery
Peer Specialist – Adult, Certified Recovery Peer
Specialist – Family, Certified Recovery Peer Specialist
– Veteran, or Certified Recovery Support Specialist.
(4) Discharge plan means the plan developed
with and by the person which sets forth how
the person will meet his or her needs, including
living arrangements, transportation, aftercare,
physical health, and securing needed psychotropic
medications for the post-discharge period of up to
21 days.
(5) Emergency treatment order (ETO) means
a written emergency order for psychotropic
medications, as described in Rule 65E-5.1703,
F.A.C.; or a written emergency order for seclusion or
restraint, as described in subsection (7) of Rule 65E-
5.180, F.A.C.
(6) Examination means the integration of the physical
examination required under Section 394.459(2),
F.S., with other diagnostic activities to determine
if the person is medically stable and to rule out
abnormalities of thought, mood, or behavior
that mimic psychiatric symptoms but are due to
non-psychiatric medical causes such as disease,
infection, injury, toxicity, or metabolic disturbances.
Examination includes the identification of person-
Definitions

3 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.455 F.S.)
65E-5.100 F.A.C.
treatment facility providing for the evaluation,
diagnosis, care, treatment, training, or
hospitalization of persons who appear to have a
mental illness or have been diagnosed as having
a mental illness. “Facility” does not include any
program or entity licensed pursuant to chapter
400 or chapter 429.
(11) “Guardian” means the natural guardian of a
minor, or a person appointed by a court to act
on behalf of a ward’s person if the ward is a
minor or has been adjudicated incapacitated.
(12) “Guardian advocate” means a person appointed
by a court to make decisions regarding mental
health treatment on behalf of a patient who
has been found incompetent to consent to
treatment pursuant to this part. e guardian
advocate may be granted specic additional
powers by written order of the court, as
provided in this part.
(13) “Hospital” means a facility as dened in s.
395.002 and licensed under chapter 395 and
part II of chapter 408.
(14) “Incapacitated” means that a person has been
adjudicated incapacitated pursuant to part V of
chapter 744 and a guardian of the person has
been appointed.
(15) “Incompetent to consent to treatment” means
that a person’s judgment is so aected by his
or her mental illness that the person lacks the
capacity to make a well-reasoned, willful, and
knowing decision concerning his or her medical
or mental health treatment.
(16) “Law enforcement officer” means a law
enforcement ocer as dened in s. 943.10.
(17) “Mental health overlay program” means a
mobile service which provides an independent
examination for voluntary admissions and a
range of supplemental onsite services to persons
with a mental illness in a residential setting such
as a nursing home, assisted living facility, adult
family-care home, or nonresidential setting
such as an adult day care center. Independent
examinations provided pursuant to this part
through a mental health overlay program
must only be provided under contract with
Definitions
specific risk factors for treatment such as elevated
blood pressure, organ dysfunction, substance abuse,
or trauma.
(7) Health care proxy means a competent adult who
has not been expressly designated by an advance
directive to make health care decisions for a
particular incapacitated individual, but is authorized
pursuant to Section 765.401, F.S., to make health
care decisions for such individual.
(8) Health care surrogate means any competent
adult expressly designated by a principal’s advance
directive to make health care decisions on behalf of
the principal upon the principal’s incapacity.
(9) Person means an individual of any age, unless
statutorily restricted, with a mental illness served in
or by a mental health facility or service provider.
(10) Personal Safety Plan is a form used to document
information regarding calming strategies that the
person identifies as being helpful in avoiding a crisis.
The plan also lists triggers that are identified that
may signal or lead to agitation or distress.
(11) Pro re nata (PRN) means an individualized order
for the care of an individual person which is written
after the person has been seen by the practitioner,
which order sets parameters for attending staff to
implement according to the circumstances set out
in the order. A PRN order shall not be used as an
emergency treatment order.
(12) Protective medical devices mean a specific
category of medical restraint that includes devices,
or combinations of devices, to restrict movement for
purposes of protection from falls or complications
of physical care, such as geri-chairs, posey vests,
mittens, belted wheelchairs, sheeting, and bed rails.
The requirements for the use and documentation
of use of these devices are for specific medical
purposes rather than for behavioral control.
(13) Recovery Plan may also be referred to as a
“service plan” or “treatment plan.” A recovery plan
is a written plan developed by the person and his
or her recovery team to facilitate achievement of
the person's recovery goals. This plan is based on
assessment data, identifying the person’s clinical,
rehabilitative and activity service needs, the strategy
for meeting those needs, documented treatment
goals and objectives, and documented progress in
meeting specified goals and objectives.
(14) Recovery Team may also be referred to as “service
team” or “treatment team.” A recovery team is

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
4
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.455 F.S.)
65E-5.100 F.A.C.
the department for this service or be attached
to a public receiving facility that is also a
community mental health center.
(18) “Mental illness” means an impairment of the
mental or emotional processes that exercise
conscious control of one’s actions or of the
ability to perceive or understand reality, which
impairment substantially interferes with the
person’s ability to meet the ordinary demands
of living. For the purposes of this part, the term
does not include a developmental disability
as dened in chapter 393, intoxication, or
conditions manifested only by antisocial
behavior or substance abuse impairment.
(19) “Mobile crisis response service” means a
nonresidential crisis service attached to a public
receiving facility and available 24 hours a day,
7 days a week, through which immediate
intensive assessments and interventions,
including screening for admission into a
receiving facility, take place for the purpose of
identifying appropriate treatment services.
(20) “Patient” means any person who is held or
accepted for mental health treatment.
(21) “Physician” means a medical practitioner
licensed under chapter 458 or chapter 459 who
has experience in the diagnosis and treatment
of mental and nervous disorders or a physician
employed by a facility operated by the United
States Department of Veterans Aairs which
qualies as a receiving or treatment facility
under this part.
(22) “Private facility” means any hospital or facility
operated by a for-prot or not-for-prot
corporation or association that provides mental
health services and is not a public facility.
(23) “Psychiatric nurse” means a registered nurse
licensed under part I of chapter 464 who has
a master’s degree or a doctorate in psychiatric
nursing and 2 years of post-master’s clinical
experience under the supervision of a physician.
(24) “Psychiatrist” means a medical practitioner
licensed under chapter 458 or chapter 459 who
has primarily diagnosed and treated mental and
nervous disorders for a period of not less than 3
an assigned group of individuals with specific
responsibilities identified on the recovery plan who
support and facilitate a person’s recovery process.
Team members may include the person, psychiatrist,
guardian/guardian advocate, community case
manager, family member, peer specialist and
others as determined by the person’s needs and
preferences.
(15) Seclusion and Restraint Oversight Committee
is a group of staff members or volunteers that
monitors the use of seclusion and restraint in a
facility in order to assist in safely reducing the use
of these practices. Members are selected by the
administrator and include, but are not limited to,
the administrator or designee, medical director
or a physician designated by the medical director,
quality assurance staff, and a certified recovery
specialist, if available. If no certified recovery
specialist is employed by the facility, a volunteer
certified recovery specialist may be selected by the
administrator.
(16) Standing order means a broad protocol or
delegation of medical authority that is generally
applicable to a group of persons, hence not
individualized. As limited by this chapter, it prohibits
improper delegations of authority to staff that are
not authorized by the facility, or not permitted by
practice licensing laws, to independently make
such medical decisions; such as decisions involving
determination of need, medication, routes, dosages
for psychotropic medication, or use of restraints or
seclusion upon a person.
Definitions
5 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
years, inclusive of psychiatric residency.
(25) “Public facility” means any facility that has
contracted with the department to provide
mental health services to all persons, regardless
of their ability to pay, and is receiving state
funds for such purpose.
(26) “Receiving facility” means any public or private
facility designated by the department to receive
and hold involuntary patients under emergency
conditions or for psychiatric evaluation and to
provide short-term treatment. e term does
not include a county jail.
(27) “Representative” means a person selected to
receive notice of proceedings during the time a
patient is held in or admitted to a receiving or
treatment facility.
(28)(a) “Restraint” means a physical device, method,
or drug used to control behavior. A physical
restraint is any manual method or physical
or mechanical device, material, or equipment
attached or adjacent to the individual’s body
so that he or she cannot easily remove the
restraint and which restricts freedom of
movement or normal access to one’s body.
(b) A drug used as a restraint is a medication
used to control the person’s behavior or to
restrict his or her freedom of movement and
is not part of the standard treatment regimen
of a person with a diagnosed mental illness
who is a client of the department. Physically
holding a person during a procedure to
forcibly administer psychotropic medication
is a physical restraint.
(c) Restraint does not include physical devices,
such as orthopedically prescribed appliances,
surgical dressings and bandages, supportive
body bands, or other physical holding when
necessary for routine physical examinations
and tests; or for purposes of orthopedic,
surgical, or other similar medical treatment;
when used to provide support for the
achievement of functional body position or
proper balance; or when used to protect a
person from falling out of bed.
Definitions
(Chapter 394.455 F.S.)
65E-5 F.A.C.
Online Baker Act Training
http://www.bakeracttraining.org
FREE!
On demand!
CEC's offered at low cost!

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
6
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.455 F.S.)
65E-5 F.A.C.
(29) “Seclusion” means the physical segregation of
a person in any fashion or involuntary isolation
of a person in a room or area from which the
person is prevented from leaving. e prevention
may be by physical barrier or by a sta member
who is acting in a manner, or who is physically
situated, so as to prevent the person from leaving
the room or area. For purposes of this chapter,
the term does not mean isolation due to a per-
son’s medical condition or symptoms.
(30) “Secretary” means the Secretary of Children
and Family Services.
(31) “Transfer evaluation” means the process, as
approved by the appropriate district oce of
the department, whereby a person who is being
considered for placement in a state treatment
facility is rst evaluated for appropriateness of
admission to the facility by a community-based
public receiving facility or by a community
mental health center or clinic if the public
receiving facility is not a community mental
health center or clinic.
(32) “Treatment facility” means any state-owned,
state-operated, or state-supported hospital,
center, or clinic designated by the department
for extended treatment and hospitalization,
beyond that provided for by a receiving facility,
of persons who have a mental illness, including
facilities of the United States Government,
and any private facility designated by the
department when rendering such services to
a person pursuant to the provisions of this
part. Patients treated in facilities of the United
States Government shall be solely those whose
care is the responsibility of the United States
Department of Veterans Aairs.
(33) “Service provider” means any public or private
receiving facility, an entity under contract with
the Department of Children and Family Services
to provide mental health services, a clinical
psychologist, a clinical social worker, a marriage
and family therapist, a mental health counselor,
a physician, a psychiatric nurse as dened in
subsection (23), or a community mental health
center or clinic as dened in this part.
Definitions
7 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(34) “Involuntary examination” means an
examination performed under s. 394.463
to determine if an individual qualies for
involuntary inpatient treatment under s.
394.467(1) or involuntary outpatient treatment
under s. 394.4655(1).
(35) “Involuntary placement” means either
involuntary outpatient treatment pursuant to
s. 394.4655 or involuntary inpatient treatment
pursuant to s. 394.467.
(36) “Marriage and family therapist” means a person
licensed as a marriage and family therapist under
chapter 491.
(37) “Mental health counselor” means a person
licensed as a mental health counselor under
chapter 491.
(38) “Electronic means” means a form of
telecommunication that requires all
parties to maintain visual as well as audio
communication.
394.457 Operation and administration.
(1) ADMINISTRATION. e Department of
Children and Family Services is designated
the “Mental Health Authority” of Florida.
e department and the Agency for Health
Care Administration shall exercise executive
and administrative supervision over all mental
health facilities, programs, and services.
(2) RESPONSIBILITIES OF THE
DEPARTMENT.
e department is responsible for:
(a) e planning, evaluation, and
implementation of a complete and
comprehensive statewide program of
mental health, including community
services, receiving and treatment facilities,
child services, research, and training as
authorized and approved by the Legislature,
based on the annual program budget of
the department. e department is also
responsible for the coordination of eorts
65E-5.110 Delegation of Authority.
In order to protect the health and safety of persons
treated in or served by any receiving or treatment
facility or any service provider, any delegation of an
administrator’s authority pursuant to Chapter 394, F.S.,
or these rules shall be documented in writing prior to
exercising the delegated authority. Routine delegations
of authority shall be incorporated in the facility’s written
policies.
Operation and Administration
(Chapter 394.457 F.S.)
65E-5.110 F.A.C.
Telepsychiatry

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
8
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.457 F.S.)
65E-5.120 F.A.C.
with other departments and divisions
of the state government, county and
municipal governments, and private
agencies concerned with and providing
mental health services. It is responsible for
establishing standards, providing technical
assistance, and exercising supervision
of mental health programs of, and the
treatment of patients at, community
facilities, other facilities for persons who
have a mental illness, and any agency
or facility providing services to patients
pursuant to this part.
(b)e publication and distribution of
an information handbook to facilitate
understanding of this part, the policies and
procedures involved in the implementation
of this part, and the responsibilities of the
various providers of services under this
part. It shall stimulate research by public
and private agencies, institutions of higher
learning, and hospitals in the interest of
the elimination and amelioration of mental
illness.
(3) POWER TO CONTRACT. e department
may contract to provide, and be provided with,
services and facilities in order to carry out its re-
sponsibilities under this part with the following
agencies: public and private hospitals; receiving
and treatment facilities; clinics; laboratories;
departments, divisions, and other units of state
government; the state colleges and universi-
ties; the community colleges; private colleges
and universities; counties, municipalities, and
any other governmental unit, including facili-
ties of the United States Government; and any
other public or private entity which provides
or needs facilities or services. Baker Act funds
for community inpatient, crisis stabilization,
short-term residential treatment, and screen-
ing services must be allocated to each county
pursuant to the department’s funding allocation
methodology. Notwithstanding s. 287.057(3)
(e), contracts for community-based Baker
Act services for inpatient, crisis stabilization,
Operation and Administration

9 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.457 F.S.)
65E-5 F.A.C.
short-term residential treatment, and screening
provided under this part, other than those with
other units of government, to be provided for
the department must be awarded using competi-
tive sealed bids if the county commission of the
county receiving the services makes a request to
the department’s district oce by January 15 of
the contracting year. e district may not enter
into a competitively bid contract under this
provision if such action will result in increases of
state or local expenditures for Baker Act services
within the district. Contracts for these Baker
Act services using competitive sealed bids are
eective for 3 years. e department shall adopt
rules establishing minimum standards for such
contracted services and facilities and shall make
periodic audits and inspections to assure that the
contracted services are provided and meet the
standards of the department.
(4) APPLICATION FOR AND ACCEPTANCE
OF GIFTS AND GRANTS. e department
may apply for and accept any funds, grants, gifts,
or services made available to it by any agency or
department of the Federal Government or any
other public or private agency or individual in aid
of mental health programs. All such moneys shall
be deposited in the State Treasury and shall be
disbursed as provided by law.
(5) RULES.
(a) e department shall adopt rules
establishing forms and procedures relating
to the rights and privileges of patients
seeking mental health treatment from
facilities under this part.
(b)e department shall adopt rules necessary
for the implementation and administration
of the provisions of this part, and a program
subject to the provisions of this part shall
not be permitted to operate unless rules
designed to ensure the protection of the
health, safety, and welfare of the patients
treated through such program have been
adopted. Rules adopted under this subsec-
tion must include provisions governing
the use of restraint and seclusion which are
Operation and Administration
65E-5.120 Forms.
All forms referred to in this chapter are available from
the department’s website, http://www.dcf.state.fl.us/
mentalhealth/laws/ index.shtml, by scrolling down
to and clicking on “Baker Act Forms” under “Baker Act
Handbook,” or may be obtained from the department’s
district or regional mental health program offices. Single
copies of all the forms or a disk containing electronic
copies of all the forms are also available from district or
regional offices. Recommended forms are those which
are incorporated by reference because they provide a list
of the information necessary to comply with the statutory
and rule requirements. Mandatory forms are incorporated
by reference and the specific form is required and may
not be altered.
Links to the DCF website, including forms, can also be
found at the Baker Act Reporting Center website:
http://bakeract.fmhi.usf.edu/

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
10
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.457 F.S.)
65E-5 F.A.C.
consistent with recognized best practices
and professional judgment; prohibit inher-
ently dangerous restraint or seclusion pro-
cedures; establish limitations on the use and
duration of restraint and seclusion; establish
measures to ensure the safety of program
participants and sta during an incident of
restraint or seclusion; establish procedures
for sta to follow before, during, and after
incidents of restraint or seclusion; establish
professional qualications of and training
for sta who may order or be engaged in
the use of restraint or seclusion; and estab-
lish mandatory reporting, data collection,
and data dissemination procedures and
requirements. Rules adopted under this
subsection must require that each instance
of the use of restraint or seclusion be docu-
mented in the record of the patient.
(c) e department shall adopt rules
establishing minimum standards for
services provided by a mental health overlay
program or a mobile crisis response service.
(6) PERSONNEL.
(a) e department shall, by rule, establish
minimum standards of education and
experience for professional and technical
personnel employed in mental health
programs, including members of a mobile
crisis response service.
(b)e department shall design and distribute
appropriate materials for the orientation
and training of persons actively engaged in
implementing the provisions of this part
relating to the involuntary examination and
placement of persons who are believed to
have a mental illness.
(7) PAYMENT FOR CARE OF PATIENTS.
Fees and fee collections for patients in state-
owned, state-operated, or state-supported
treatment facilities shall be according to s.
402.33.
Operation and Administration

11 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
394.4572 Screening of mental health
personnel.
(1) (a) e department and the Agency for
Health Care Administration shall require
level 2 background screening pursuant to
chapter 435 for mental health personnel.
“Mental health personnel” includes all
program directors, professional clinicians,
sta members, and volunteers working in
public or private mental health programs
and facilities who have direct contact with
individuals held for examination or admitted
for mental health treatment. For purposes
of this chapter, employment screening of
mental health personnel also includes, but
is not limited to, employment screening as
provided under chapter 435 and s. 408.809.
(b) Students in the health care professions who
are interning in a mental health facility
licensed under chapter 395, where the
primary purpose of the facility is not the
treatment of minors, are exempt from the
ngerprinting and screening requirements
if they are under direct supervision in the
actual physical presence of a licensed health
care professional.
(c) A volunteer who assists on an intermittent
basis for less than 10 hours per month
is exempt from the ngerprinting and
screening requirements if a person who
meets the screening requirement of
paragraph (a) is always present and has the
volunteer within his or her line of sight.
(d) Mental health personnel working in a facil-
ity licensed under chapter 395 who work on
an intermittent basis for less than 15 hours
per week of direct, face-to-face contact
with patients, and who are not listed on the
Department of Law Enforcement Career
Oender Search or the Dru Sjodin National
Sex Oender Public Website, are exempt
from the ngerprinting and screening re-
quirements, except that persons working in
a mental health facility where the primary
N/A
Screening of mental health personnel
(Chapter 394.4572 F.S.)
65E-5 F.A.C.
Level 2 screening
for mental health personnel.
Required

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
12
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4573 F.S.)
65E-5.130 F.A.C.
purpose of the facility is the mental health
treatment of minors must be ngerprinted
and meet screening requirements.
(2) e department or the Agency for Health Care
Administration may grant exemptions from
disqualication as provided in chapter 435.
394.4573 Continuity of care
management system; measures of
performance; reports.
(1) For the purposes of this section:
(a) “Case management” means those activities
aimed at assessing client needs, planning
services, linking the service system to a
client, coordinating the various system
components, monitoring service delivery,
and evaluating the eect of service delivery.
(b)“Case manager” means an individual
who works with clients, and their families
and signicant others, to provide case
management.
(c) “Client manager” means an employee of
the department who is assigned to specic
provider agencies and geographic areas to
ensure that the full range of needed services
is available to clients.
(d)“Continuity of care management system”
means a system that assures, within
available resources, that clients have access
to the full array of services within the
mental health services delivery system.
(2) e department is directed to implement a
continuity of care management system for
the provision of mental health care, through
the provision of client and case management,
including clients referred from state treatment
facilities to community mental health facilities.
Such system shall include a network of client
managers and case managers throughout the
state designed to:
(a) Reduce the possibility of a client’s
admission or readmission to a state
treatment facility.
65E-5.130 Continuity of Care Management
System.
Persons receiving case management services.
(1) At the time of admission receiving facilities shall
inquire of the person or significant others as to
the existence of any advance directives and as
to the identity of the person’s case manager. If
a case manager for the person is identified, the
administrator or designee shall request the person’s
authorization to notify the person’s case manager
or the case management agency of the person’s
admission to the facility.
If authorized, such notification shall be made within
12 hours to the published 24-hour
telephone listing for the case manager or case
management agency. This inquiry, notification,
and the identity of the case manager or case
management agency, if any, shall be
documented on the face sheet or other
prominent location in the person’s clinical record.
(2) A department funded mental health case manager,
when notified by a receiving facility that a client
has been admitted, shall visit that person as soon
as possible but no later than two working days after
notification to assist with discharge and aftercare
planning to the least restrictive, appropriate and
available
placement. If the person is located in a receiving
facility outside of the case manager’s district or
region of residence, the department funded mental
health case manager may substitute a telephone
contact for a face-to-face visit which shall be
documented in the case management record and in
the person’s clinical record at the receiving facility.
Continuity of Care

13 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4573 F.S.)
65E-5.1301F.A.C.
(b)Provide for the creation or designation of
an agency in each county to provide single
intake services for each person seeking
mental health services. Such agency shall
provide information and referral services
necessary to ensure that clients receive the
most appropriate and least restrictive form
of care, based on the individual needs of the
person seeking treatment. Such agency shall
have a single telephone number, operating
24 hours per day, 7 days per week, where
practicable, at a central location, where each
client will have a central record.
(c) Advocate on behalf of the client to ensure
that all appropriate services are aorded to
the client in a timely and dignied manner.
(d)Require that any public receiving facility
initiating a patient transfer to a licensed
hospital for acute care mental health services
not accessible through the public receiving
facility shall notify the hospital of such
transfer and send all records relating to the
emergency psychiatric or medical condition.
(3) e department is directed to develop and
include in contracts with service providers
measures of performance with regard to goals
and objectives as specied in the state plan.
Such measures shall use, to the extent practical,
existing data collection methods and reports
and shall not require, as a result of this subsec-
tion, additional reports on the part of service
providers. e department shall plan monitor-
ing visits of community mental health facilities
with other state, federal, and local governmen-
tal and private agencies charged with monitor-
ing such facilities.
65E-5.1301 Transfer Evaluations for
Admission to State Mental Health
Treatment Facilities from Receiving
Facilities.
(1) A person in a receiving facility shall not be
transferred to a state treatment facility
without the completion of a transfer
evaluation, in accordance with Section 394.461(2),
F.S., using mandatory form CF-MH 3089, Feb. 05,
“Transfer Evaluation,” which is hereby incorporated
by reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter. The process
for conducting such transfer evaluations shall be
developed by the community mental health center
or clinic and be approved by the district or regional
office of the department where the center or clinic is
located and shall include:
(a) Designation of the contracted mental health
centers or clinics that are responsible for
conducting the transfer evaluations,
including the receiving facilities or persons for
which each center or clinic is
responsible;
(b) Establishment of the time within which
a mandatory form CF-MH 3089, “Transfer
Evaluation,” as referenced in subsection 65E-
5.1301(1), F.A.C., shall be completed. This
form shall be completed by the designated
community mental health center and
submitted to the court for all persons for whom
involuntary placement in a state treatment
facility is sought, and directly to the state
treatment facility for all persons for whom
voluntary admission is sought; and
(c) Specification of the minimum training and
education of the persons qualified to conduct
the transfer evaluations and the training and
educational qualifications of the evaluators’
immediate supervisor.
Unless otherwise established in writing by the
district or region, the evaluator shall have at
least a bachelor’s degree and the immediate
supervisor a master’s degree in a clinical or
human services area of study.
(2) A community mental health center or clinic shall
evaluate each person seeking voluntary admission
to a state treatment facility and each person for
whom involuntary placement in a state treatment
Continuity of Care

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
14
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.1301 F.A.C.
(3)
facility is sought, to determine and document:
(a) Whether the person meets the statutory criteria
for admission to a state treatment facility; and
(b) Whether there are appropriate more
integrated and less restrictive mental health
treatment resources available to meet the
person’s needs.
Following an evaluation of the person, the
executive director of the community mental health
center or clinic shall recommend the
admission to a state treatment facility or, if
criteria for involuntary placement are not met, to
alternative treatment programs and shall document
that recommendation by completing
and signing the form CF-MH 3089, “Transfer
Evaluation,” as referenced in subsection
65E-5.1301(1), F.A.C.
(a) The executive director’s responsibility for
completing and signing mandatory form CF-MH
3089, “Transfer Evaluation,” as
referenced in subsection 65E-5.1301(1), F.A.C.,
may be delegated in writing to the chief clinical
officer of the center or clinic.
(b) An original signature on the mandatory form
CF-MH 3089, “Transfer Evaluation,” as referenced
in subsection 65E-5.1301(1), F.A.C., is required.
(c) A copy of the mandatory form CF-MH 3089,
“Transfer Evaluation,” as referenced in
subsection 65E-5.1301(1), F.A.C., shall be
retained in the files of the community
mental health center or clinic.
(d) The completed and signed mandatory form
CF-MH 3089, “Transfer Evaluation,” as referenced
in subsection 65E-5.1301(1), F.A.C., shall be
forwarded to the court before the hearing at
which a person’s involuntary placement in a
state treatment facility will be considered. The
evaluator, or in the
absence of the evaluator, another
knowledgeable staff person employed by the
community mental health center or clinic,
shall be present at any hearing on involuntary
placement in a state treatment facility to provide
testimony as desired by the court.
Continuity of Care

15 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
65E-5.1302 Admissions to State Treatment
Facilities.
(1) Receiving facilities must obtain approval from the
state treatment facility prior to the transfer of a
person. A state treatment facility shall be permitted
to accept persons for transfer from a receiving
facility if the administrator of the receiving facility
has provided the following documentation, which
documentation shall be retained in the person’s
clinical record:
(a) Recommended form CF-MH 7000, Jan. 98,
“State Mental Health Facility Admission Form,”
with all required attachments, which is hereby
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter;
(b) Recommended forms CF-MH 3040, Feb. 05,
“Application for Voluntary Admission,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, or CF-MH 3008, Feb. 05, “Order for
Involuntary Inpatient Placement,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter; and
(c) Mandatory form CF-MH 3089, “Transfer
Evaluation” as referenced in subsection 65E-
5.1301(1), F.A.C.
(2) Use of recommended form CF-MH 7002, Feb.
05, “Physician to Physician Transfer,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used for documentation when
completed by the referring physician or in the
absence of the referring physician the physician’s
designee within state law and approved facility
protocols and practice guidelines, at the time of
transfer. The form shall accompany the person to
the state treatment facility and upon arrival shall be
presented to admitting staff.
65E-5.1303 Discharge from Receiving and
Treatment Facilities.
(1) Before discharging a person who has been admitted
to a facility, the person shall be encouraged to
actively participate in treatment and discharge
planning activities and shall be notified in writing
of his or her right to seek treatment from the
Continuity of Care
(Chapter 394 F.S.)
65E-5.1302 F.A.C.
Admission to State Treatment
Facilities.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
16
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
professional or agency of the person’s choice and
the person shall be assisted in making appropriate
discharge plans. The person shall be advised that,
pursuant to Section 394.460, F.S., no professional is
required to accept persons for psychiatric treatment.
(2) Discharge planning shall include and document
consideration of the following:
(a) The person’s transportation resources;
(b) The person’s access to stable living arrangements;
(c) How assistance in securing needed living
arrangements or shelter will be provided to
individuals who are at risk of re-admission
within the next 3 weeks due to homelessness
or transient status and prior to discharge shall
request a commitment from a shelter provider
that assistance will be rendered;
(d) Assistance in obtaining a timely aftercare
appointment for needed services, including
continuation of prescribed psychotropic
medications. Aftercare appointments for
psychotropic medication and case management
shall be requested to occur not later than 7
days after the expected date of discharge; if the
discharge is delayed, the facility will notify the
aftercare provider. The facility shall coordinate
with the aftercare service provider and shall
document the aftercare planning;
(e) To ensure a person’s safety and provide
continuity of essential psychotropic medications,
such prescribed psychotropic medications,
prescriptions, or multiple partial prescriptions
for psychotropic medications, or a combination
thereof, shall be provided to a person when
discharged to cover the intervening days until
the first scheduled psychotropic medication
aftercare appointment, or for a period of up to 21
calendar days, whichever occurs first. Discharge
planning shall address the availability of and
access to prescribed psychotropic medications in
the community;
(f ) The person shall be provided education and
written information about his or her illness
and psychotropic medications including other
prescribed and over-the-counter medications,
the common side-effects of any medications
prescribed and any adverse clinically significant
drug-to-drug interactions common between
that medication and other commonly available
prescribed and over-the-counter medications;
Continuity of Care
Aftercare appointment required.
Access to psychotropic
medications following discharge
required.
(Chapter 394 F.S.)
65E-5.1303 F.A.C.

17 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(g) The person shall be provided contact and
program information about and referral to any
community-based peer support services in the
community;
(h) The person shall be provided contact and
program information about and referral to any
needed community resources;
(i) Referral to substance abuse treatment programs,
trauma or abuse recovery focused programs,
or other self-help groups, if indicated by
assessments; and
( j) The person shall be provided information about
advance directives, including how to prepare and
use the advance directives.
(3) Should a person in a receiving or treatment
facility meet the criteria for involuntary outpatient
placement rather than involuntary inpatient
placement, the facility administrator may initiate
such involuntary outpatient placement, pursuant to
Section 394.4655, F.S., and Rule 65E-5.285, F.A.C., of
this rule chapter.
(4) Receiving and treatment facilities shall have written
discharge policies and procedures which shall
contain:
(a) Agreements or protocols for transfer and
transportation arrangements between facilities;
(b) Protocols for assuring that current medical
and legal information, including medication
administered on the day of discharge, is
transferred before or with the person to another
facility; and
(c) Policy and procedures which address continuity
of services and access to necessary psychotropic
medications.
(5) When a state mental health treatment facility
has established an anticipated discharge date
for discharge to the community which is more
than seven days in advance of the person’s
actual discharge, at least 7 days notice must be
given to the community agency which has been
assigned case management responsibility for the
implementation of the person’s discharge plan.
When an impending discharge is known 7 days
or less prior to the discharge, the staff of the state
mental health treatment facility shall give verbal
and written notice of the impending discharge to
the community case management agency within
1 working day after the decision to discharge is
Continuity of Care
(Chapter 394 F.S.)
65E-5.1303 F.A.C.
Referral to needed
services required.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
18
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
394.4574 Department responsibilities
for a mental health resident who resides
in an assisted living facility that holds a
limited mental health license.
(1) e term “mental health resident,” for pur-
poses of this section, means an individual
who receives social security disability income
due to a mental disorder as determined by
the Social Security Administration or receives
supplemental security income due to a mental
disorder as determined by the Social Security
Administration and receives optional state
supplementation.
(2) e department must ensure that:
(a) A mental health resident has been assessed
by a psychiatrist, clinical psychologist,
clinical social worker, or psychiatric nurse,
or an individual who is supervised by one
of these professionals, and determined
to be appropriate to reside in an assisted
living facility. e documentation must be
provided to the administrator of the facility
within 30 days after the mental health
resident has been admitted to the facility.
N/A
Assisted living facility
made. Recommended form CF-MH 7001, Jan. 98,
“State Mental Health Facility Discharge Form,”
which is incorporated by reference, may be used
for this purpose, and may be obtained online
at https://www.flrules.org/Gateway/reference.
asp?No=Ref-02361, http://www.myflfamilies.com/
service-programs/mental-health/baker-act-forms.
(6) On the day of discharge from a state mental
health treatment facility, the referring physician,
or his or her designee, within the requirements
of Section 394.4615, F.S., and the policies and
procedures required by subsection (4) of this rule,
shall immediately notify the community aftercare
provider or entity responsible for dispensing or
administering medications. Recommended form
CF-MH 7002, Feb. 05, “Physician to Physician
Transfer,” as referenced in subsection 65E-5.1302(2),
F.A.C., may be used for this purpose, and may
be obtained online at https://www.flrules.org/
Gateway/reference.asp?No=Ref-02362, http://www.
myflfamilies.com/service-programs/mental-health/
baker-act-forms.
(Chapter 394.4574 F.S.)
65E-5.1303 F.A.C.
ALF with Limited Mental Health
License.

19 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4574 F.S.)
65E-5 F.A.C.
An evaluation completed upon discharge
from a state mental hospital meets the
requirements of this subsection related to
appropriateness for placement as a mental
health resident if it was completed within
90 days prior to admission to the facility.
(b)A cooperative agreement, as required in s.
429.075, is developed between the mental
health care services provider that serves a
mental health resident and the administrator
of the assisted living facility with a limited
mental health license in which the mental
health resident is living. Any entity that
provides Medicaid prepaid health plan
services shall ensure the appropriate
coordination of health care services with
an assisted living facility in cases where a
Medicaid recipient is both a member of the
entity’s prepaid health plan and a resident of
the assisted living facility. If the entity is at
risk for Medicaid targeted case management
and behavioral health services, the entity
shall inform the assisted living facility of the
procedures to follow should an emergent
condition arise.
(c) e community living support plan, as
dened in s. 429.02, has been prepared
by a mental health resident and a mental
health case manager of that resident in
consultation with the administrator of the
facility or the administrator’s designee. e
plan must be provided to the administrator
of the assisted living facility with a limited
mental health license in which the mental
health resident lives. e support plan and
the agreement may be in one document.
(d)e assisted living facility with a limited
mental health license is provided with
documentation that the individual meets
the denition of a mental health resident.
(e) e mental health services provider assigns a
case manager to each mental health resident
who lives in an assisted living facility with
a limited mental health license. e case
manager is responsible for coordinating the
Assisted living facility

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
20
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
N/A
Firearms and deadly weapons
in hospitals providing mental
health services.
development of and implementation of the
community living support plan dened
in s. 429.02. e plan must be updated at
least annually.
(3) e Secretary of Children and Family Services,
in consultation with the Agency for Health
Care Administration, shall annually require
each district administrator to develop, with
community input, detailed plans that demon-
strate how the district will ensure the provision
of state-funded mental health and substance
abuse treatment services to residents of assisted
living facilities that hold a limited mental
health license. ese plans must be consistent
with the substance abuse and mental health
district plan developed pursuant to s. 394.75
and must address case management services;
access to consumer-operated drop-in centers;
access to services during evenings, weekends,
and holidays; supervision of the clinical needs
of the residents; and access to emergency psy-
chiatric care.
394.458 Introduction or removal of
certain articles unlawful; penalty.
(1)(a) Except as authorized by law or as speci-
cally authorized by the person in charge
of each hospital providing mental health
services under this part, it is unlawful to
introduce into or upon the grounds of
such hospital, or to take or attempt to take
or send therefrom, any of the following
articles, which are hereby declared to be
contraband for the purposes of this section:
1. Any intoxicating beverage or beverage
which causes or may cause an intoxicat-
ing eect;
2. Any controlled substance as dened in
chapter 893; or
3. Any rearms or deadly weapon.
(b) It is unlawful to transmit to, or attempt to
transmit to, or cause or attempt to cause to
Assisted living facility
(Chapter 394.458 F.S.)
65E-5 F.A.C.

21 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
be transmitted to, or received by, any patient
of any hospital providing mental health
services under this part any article or thing
declared by this section to be contraband,
at any place which is outside of the grounds
of such hospital, except as authorized by law
or as specically authorized by the person in
charge of such hospital.
(2) A person who violates any provision of this sec-
tion commits a felony of the third degree, pun-
ishable as provided in s. 775.082, s. 775.083,
or s. 775.084.
394.459 Rights of patients.
Rights of patients
Federal conditions of
participation and other federal/
state laws/regulation and
accreditation standards may
also apply
See bakeracttraining.org for
course on Rights of Persons in
Mental Health Facilities
(Chapter 394.459 F.S.)
65E-5.140 F.A.C.
65E-5.140 Rights of Persons.
(1) Every person admitted to a designated receiving
or treatment facility or ordered to treatment at a
service provider shall be provided with a written
description of his or her rights at the time of
admission. Recommended form CF-MH 3103, Feb.
05, “Rights of Persons in Mental Health Facilities and
Programs,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose. A
copy of the rights statement, signed by the person
evidencing receipt of the copy, shall be placed in the
person’s clinical record and shall also be provided
to the person’s guardian, guardian advocate,
representative, and health care surrogate or proxy.
(2) To assure that persons have current information as
to their rights, a copy of the Florida Mental Health
Act (Chapter 394, Part I, F.S.) and Mental Health Act
Regulations (Chapter 65E-5, F.A.C.) shall be available,
and provided upon request, in every psychiatric
unit of each receiving and treatment facility and by
each service provider and, upon request shall be
made available for review by any person, guardian,
guardian advocate, representative, or health care
surrogate or proxy. The administrator or designee of
the facility or service provider shall make physicians,
nurses, and all other direct service staff aware of
the location of these documents so they are able to
promptly access them upon request.
(3) Posters delineating rights of persons served in
mental health facilities and by service providers,
including those with telephone numbers for the

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
22
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(1) RIGHT TO INDIVIDUAL DIGNITY.
It is the policy of this state that the individual
dignity of the patient shall be respected at all
times and upon all occasions, including any
occasion when the patient is taken into cus-
tody, held, or transported. Procedures, facili-
ties, vehicles, and restraining devices utilized
for criminals or those accused of crime shall
not be used in connection with persons who
have a mental illness, except for the protection
of the patient or others. Persons who have a
mental illness but who are not charged with a
criminal oense shall not be detained or incar-
cerated in the jails of this state. A person who
is receiving treatment for mental illness shall
not be deprived of any constitutional rights.
However, if such a person is adjudicated inca-
pacitated, his or her rights may be limited to
the same extent the rights of any incapacitated
person are limited by law.
Rights of patients
(Chapter 394.459 F.S.)
65E-5.150 F.A.C.
Florida Abuse Hotline, Florida Local Advocacy
Council, and the Advocacy Center for Persons with
Disabilities, shall be legible, a minimum of 14 point
font size, and shall be posted immediately next to
telephones which are available for persons served
by the facility or provider.
(4) Each person shall be afforded the opportunity to
exercise his or her rights in a manner consistent with
Section 394.459(1), F.S. The imposition of individual
or unit restrictions and the development of unit
policies and procedures shall address observance of
protecting rights of persons served in developing
criteria or processes to provide for care and safety
65E-5.150 Person’s Right to Individual
Dignity.
(1) Freedom of movement is a right of persons in
mental health receiving and treatment facilities.
Any restriction of this right requires a physician’s
order based upon risk factors. Each receiving and
treatment facility shall have policies that describe
freedom of movement and access to grounds. When
a suitable area is immediately adjacent to the unit,
the staff shall afford each person an opportunity
to spend at least one half hour per day in an
open, out of doors, fresh air activity area, unless
there is a physician’s order prohibiting this, with
documentation in the person’s clinical record of the
clinical reasons that access to fresh air will not be
accommodated.
(2) Use of special clothing for identification purposes
such as surgical scrubs or hospital gowns to identify
persons who are in need of specific precautions
or behavior modification restrictions is prohibited
as a violation of individual dignity. Prison or jail
attire shall not be permitted for persons admitted
or retained in a receiving facility except while
accompanied by a uniformed law enforcement
officer, for purposes of security. Under non-
psychiatric medical circumstances, use of special
clothing may be ordered by the person’s physician
on an individual basis. Documentation of the
circumstances shall be included in the person’s
clinical record.
Florida statewide and local advocacy
councils no longer exist because they
were de-funded by the 2010 Florida
Legislature.

23 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.160 F.A.C.
(2) RIGHT TO TREATMENT.
(a) A person shall not be denied treatment
for mental illness and services shall not be
delayed at a receiving or treatment facility
because of inability to pay. However, every
reasonable eort to collect appropriate
reimbursement for the cost of providing
mental health services to persons able to pay
for services, including insurance or third-
party payments, shall be made by facilities
providing services pursuant to this part.
(b)It is further the policy of the state that
the least restrictive appropriate available
treatment be utilized based on the
individual needs and best interests of the
patient and consistent with optimum
improvement of the patient’s condition.
(c) Each person who remains at a receiving or
treatment facility for more than 12 hours
shall be given a physical examination by a
health practitioner authorized by law to give
such examinations, within 24 hours after
arrival at such facility.
(d)Every patient in a facility shall be aorded
the opportunity to participate in activities
designed to enhance self-image and the
benecial eects of other treatments, as
determined by the facility.
(e) Not more than 5 days after admission to a
facility, each patient shall have and receive
an individualized treatment plan in writing
which the patient has had an opportunity
to assist in preparing and to review prior to
its implementation. e plan shall include a
space for the patient’s comments.
65E-5.160 Right to Treatment.
(1) Patients shall have the opportunity to participate in
the preparation of their own treatment and discharge
plans at receiving and treatment facilities and by
service providers. In instances when the person
refuses or is unable to participate in such planning,
such refusal or inability shall be documented in the
person’s clinical record.
(2) Comprehensive service assessment and treatment
planning, including discharge planning, shall begin the
day of admission and shall also include the person’s
case manager if any, the person’s friends, family,
significant others, or guardian, as desired by the person.
If the person has a court appointed guardian, the
guardian shall be included in the service assessment
and treatment planning. Obtaining legal consent for
treatment, assessment and planning protocols shall also
include the following:
(a) How any advance directives will be obtained and
their provisions addressed and how consent for
treatment will be expeditiously obtained for any
person unable to provide consent;
(b) Completion of necessary diagnostic testing and
the integration of the results and interpretations
from those tests. The results and interpretation of
the results shall be reviewed with the person;
(c) The development of treatment goals specifying the
factors and symptomology precipitating admission
and addressing their resolution or mitigation;
(d) The development of a goal within an
individualized treatment plan, including
the individual’s strengths and weaknesses,
that addresses each of the following: living
arrangements, social supports, financial supports,
and health, including mental health. Goals shall be
inclusive of the person’s choices and preferences
and utilize available natural social supports such as
family, friends, and peer support group meetings
and social activities;
(e) Objectives for implementing each goal shall list
the actions needed to obtain the goal, and shall be
stated in terms of outcomes that are observable,
measurable, and time-limited;
(f) Progress notes shall be dated and shall address
each objective in relation to the goal, describing
the corresponding progress, or lack of progress
being made. Progress note entries and the name
and title of writer must be clearly legible;
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
24
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(g) Periodic reviews shall be comprehensive,
include the person, and shall be the basis for
major adjustments to goals and objectives.
Frequency of periodic reviews shall be
determined considering the degree to which the
care provided is acute care and the projected
length of stay of the person;
(h) Progress note observations, participation by the
person, rehabilitative and social services, and
medication changes shall reflect an integrated
approach to treatment;
(i) Facilities shall update the treatment plan,
including the physician summary, at least
every 30 days during the time a person is in
a receiving or treatment facility except that
persons retained for longer than 24 months
shall have updates at least every 60 days;
( j) The clinical record shall comprehensively
document the person’s care and treatment,
including injuries sustained and all uses of
emergency treatment orders; and
(k) Persons who will have a continued involuntary
outpatient placement hearing pursuant to
Section 394.4655(7), F.S., or continued involuntary
inpatient placement hearing pursuant to
Section 394.467(7), F.S., shall be provided with
comprehensive re-assessments, the results of
which shall be available at the hearing.
3) The physical examination required to be provided to
each person who remains at a receiving or treatment
facility for more than 12 hours must include:
(a) A determination of whether the person is
medically stable; and
(b) A determination that abnormalities of thought,
mood, or behavior due to non-psychiatric causes
have been ruled out.
65E-5.1601 General Management of the
Treatment Environment.
(1) Management and personnel of the facility’s
treatment environment shall use positive incentives
in assisting persons to acquire and maintain socially
positive behaviors as determined by the person’s
age and developmental level.
Rights of patients
(Chapter 394.459 F.S.)
65E-5.1601 F.A.C.
Treatment Planning.

25 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.1602 F.A.C.
(2) Each designated receiving and treatment facility
shall develop a schedule of daily activities listing the
times for specific events, which shall be posted in a
common area and provided to all persons.
(3) Interventions such as the loss of personal freedoms,
loss of earned privileges or denial of activities
otherwise available to other persons shall be
minimized and utilized only after the documented
failure of the unit’s positive incentives for the
individuals involved.
(4) Facilities shall ensure that any verbal or written
information provided to persons must be accessible
in the language and terminology the person
understands.
65E-5.1602 Individual Behavioral
Management Programs.
When an individualized treatment plan requires
interventions beyond the existing unit rules of conduct,
the person shall be included, and the person’s treatment
plan shall reflect:
(1) Documentation, signed by the physician that the
person’s medical condition does not exclude the
proposed interventions;
(2) Consent for the treatment to be provided;
(3) A general description of the behaviors requiring
the intervention, which may include previous
emergency interventions;
(4) Antecedents of that behavior;
(5) The events immediately following the behavior;
(6) Objective definition of the target behaviors, such as
specific acts, level of aggression, encroachment on
others’ space, self-injurious behavior or excessive
withdrawal;
(7) Arrangements for the consistent collection and
recording of data;
(8) Analysis of data;
(9) Based on data analysis, development of intervention
strategies, if necessary;
(10) Development of a written intervention strategy that
includes criteria for starting and stopping specific
staff interventions and the process by which they
are to occur;
(11) Continued data collection, if interventions are
implemented; and
(12) Periodic review and revision of the plan based upon
data collected and analyzed.
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
26
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.
(3) RIGHT TO EXPRESS AND INFORMED
PATIENT CONSENT.
(a) 1. Each patient entering treatment shall
be asked to give express and informed
consent for admission or treatment. If
the patient has been adjudicated inca-
pacitated or found to be incompetent
to consent to treatment, express and
informed consent to treatment shall be
sought instead from the patient’s guard-
ian or guardian advocate. If the patient
is a minor, express and informed consent
for admission or treatment shall also be
requested from the patient’s guardian.
Express and informed consent for ad-
mission or treatment of a patient under
18 years of age shall be required from
the patient’s guardian, unless the minor
is seeking outpatient crisis intervention
services under s. 394.4784. Express and
informed consent for admission or treat-
ment given by a patient who is under 18
years of age shall not be a condition of
admission when the patient’s guardian
gives express and informed consent for
the patient’s admission pursuant to s.
394.463 or s. 394.467.
2. Before giving express and informed
consent, the following information shall
be provided and explained in plain lan-
guage to the patient, or to the patient’s
guardian if the patient is 18 years of age
or older and has been adjudicated inca-
pacitated, or to the patient’s guardian
advocate if the patient has been found to
be incompetent to consent to treatment,
or to both the patient and the guardian
if the patient is a minor: the reason for
admission or treatment; the proposed
treatment; the purpose of the treatment
to be provided; the common risks, ben-
ets, and side eects thereof; the specic
dosage range for the medication, when
applicable; alternative treatment modali-
ties; the approximate length of care; the
65E-5.170 Right to Express and Informed
Consent.
(1) Establishment of Consent.
(a) Receiving Facilities. As soon as possible, but
in no event longer than 24 hours from entering
a designated receiving facility on a voluntary
or involuntary basis, each person shall be
examined by the admitting physician to assess
the person’s ability to provide express and
informed consent to admission and treatment.
The examination of a minor for this purpose may
be limited to the documentation of the minor’s
age. The examination of a person alleged to be
incapacitated for this purpose may be limited to
the documentation of letters of guardianship.
Documentation of the assessment results shall
be placed in the person’s clinical record. The
facility shall determine whether a person has
been adjudicated as incapacitated and whether
a guardian has been appointed by the court. If a
guardian has been appointed by the court, the
limits of the authority of the guardian shall be
determined prior to allowing the guardian to
authorize treatment. A copy of any court order
delineating a guardian’s authority to consent
to mental health or medical treatment shall
be obtained by the facility and included in the
person’s clinical record prior to allowing the
guardian to give express and informed consent
to treatment for the person.
(b) Treatment Facilities. Upon entering a
designated treatment facility on a voluntary or
involuntary basis, each person shall be examined
by the admitting physician to assess the person’s
ability to provide express and informed consent
to admission and treatment, which shall be
documented in the person’s clinical record.
The examination of a person alleged to be
incapacitated or incompetent to consent to
treatment, for this purpose, may be limited to
documenting the letters of guardianship or order
of the court. If a person has been adjudicated
as incapacitated and a guardian appointed by
the court or if a person has been found to be
incompetent to consent to treatment and a
guardian advocate has been appointed by the
court, the limits of authority of the guardian or
guardian advocate shall be determined prior to
Rights of patients

27 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.
potential eects of stopping treatment;
how treatment will be monitored; and
that any consent given for treatment
may be revoked orally or in writing
before or during the treatment period by
the patient or by a person who is legally
authorized to make health care decisions
on behalf of the patient.
(b)In the case of medical procedures requiring
the use of a general anesthetic or electrocon-
vulsive treatment, and prior to performing
the procedure, express and informed con-
sent shall be obtained from the patient if the
patient is legally competent, from the guard-
ian of a minor patient, from the guardian of
a patient who has been adjudicated incapac-
itated, or from the guardian advocate of the
patient if the guardian advocate has been
given express court authority to consent
to medical procedures or electroconvulsive
treatment as provided under s. 394.4598.
(c) When the department is the legal guardian
of a patient, or is the custodian of a
patient whose physician is unwilling to
perform a medical procedure, including
an electroconvulsive treatment, based
solely on the patient’s consent and whose
guardian or guardian advocate is unknown
or unlocatable, the court shall hold a
hearing to determine the medical necessity
of the medical procedure. e patient shall
be physically present, unless the patient’s
medical condition precludes such presence,
represented by counsel, and provided the
right and opportunity to be confronted
with, and to cross-examine, all witnesses
alleging the medical necessity of such
procedure. In such proceedings, the burden
of proof by clear and convincing evidence
shall be on the party alleging the medical
necessity of the procedure.
(d)e administrator of a receiving or
treatment facility may, upon the
recommendation of the patient’s attending
physician, authorize emergency medical
Rights of patients
allowing the guardian or guardian advocate to
authorize treatment for the person. A copy of any
court order delineating a guardian’s authority to
consent to mental health or medical treatment
shall be obtained by the facility and included in
the person’s clinical record prior to allowing the
guardian to give express and informed consent
to treatment for the person.
(c) If the admission is voluntary, the person’s
competence to provide express and informed
consent for admission shall be documented
by the admitting physician. Recommended
form CF-MH 3104, Feb. 05, “Certification of
Person’s Competence to Provide Express and
Informed Consent,” which is incorporated by
reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter may
be used for this purpose. The completed form
or other documentation shall be retained in the
person’s clinical record. Facility staff monitoring
the person’s condition shall document any
observations which suggest that a person may
no longer be competent to provide express and
informed consent to his or her treatment. In such
circumstances, staff shall notify the physician and
document in the person’s clinical record that the
physician was notified of this apparent change in
clinical condition.
(d) In the event there is a change in the ability of a
person on voluntary status to provide express
and informed consent to treatment, the change
shall be immediately documented in the person’s
clinical record. A person’s refusal to consent
to treatment is not, in itself, an indication of
incompetence to consent to treatment.
1. If the person is assessed to be competent
to consent to treatment and meets the
criteria for involuntary inpatient placement,
the facility administrator shall file with the
court a petition for involuntary placement.
Recommended form CF-MH 3032, Feb.
05, “Petition for Involuntary Inpatient
Placement,” which is incorporated by
reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter
may be used for this purpose.
2. If the person is assessed to be incompetent
to consent to treatment, and meets
the criteria for involuntary inpatient or

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
28
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
treatment, including a surgical procedure, if
such treatment is deemed lifesaving, or if the
situation threatens serious bodily harm to
the patient, and permission of the patient or
the patient’s guardian or guardian advocate
cannot be obtained.
involuntary outpatient placement, the
facility administrator shall expeditiously
file with the court both a petition for
the adjudication of incompetence to
consent to treatment and appointment
of a guardian advocate, and a petition
for involuntary inpatient or involuntary
outpatient placement. Upon determination
that a person is incompetent to consent to
treatment the facility shall expeditiously
pursue the appointment of a duly authorized
substitute decision-maker that can make
legally required decisions concerning
treatment options or refusal of treatments
for the person. Recommended forms CF-MH
3106, Feb. 05, “Petition for Adjudication
of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate,”
which is incorporated by reference may
be obtained pursuant to Rule 65E-5.120,
F.A.C., of this rule chapter, and CF-MH
3032, “Petition for Involuntary Inpatient
Placement,” as referenced in subparagraph
65E-5.170(1)(d)1., F.A.C., or CF-MH 3130,
“Petition for Involuntary Outpatient
Placement,” which is incorporated by
reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter
may be used for this purpose.
(e) Competence to provide express and informed
consent shall be established and documented
in the person’s clinical record prior to the
approval of a person’s transfer from involuntary
to voluntary status or prior to permitting a
person to consent to his or her own treatment
if that person had been previously determined
to be incompetent to consent to treatment.
Recommended form CF-MH 3104, “Certification
of Person’s Competence to Provide Express and
Informed Consent,” as referenced in paragraph
65E-5.170(1)(c), F.A.C., properly completed by a
physician may be used for this purpose.
(f ) Any guardian advocate appointed by a court
to provide express and informed consent to
treatment for the person shall be discharged and
a notice of such guardian advocate discharge
provided to the court upon the establishment and
documentation that the person is competent to
provide express and informed consent.
Rights of patients
Other state statutes governing
substitute decision-makers, such
as guardians (744 FS) and health
care surrogates and proxies (765
FS) may apply.
See Appendix C for summary
reference on substitute
decision making
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.

29 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(g) If a person entering a designated receiving
or treatment facility has been adjudicated
incapacitated under Chapter 744, F.S., as
described in Section 394.455(14), F.S., express
and informed consent to treatment shall be
sought from the person’s guardian.
(h) If a person entering a designated receiving
or treatment facility has been determined by
the attending physician to be incompetent
to consent to treatment as defined in Section
394.455(15), F.S., express and informed consent
to treatment shall be expeditiously sought by the
facility from the person’s guardian advocate or
health care surrogate or proxy.
(i) A copy of the letter of guardianship, court order,
or advance directive shall be reviewed by facility
staff to ensure that the substitute decision-
maker has the authority to provide consent to
the recommended treatment on behalf of the
person. If the facility relies upon the expression
of express and informed consent for person’s
treatment from a substitute decision-maker,
a copy of this documentation shall be placed
in the person’s clinical record and shall serve
as documentation of the substitute decision-
maker’s authority to give such consent. With
respect to a health care proxy, where no advance
directive has been prepared by the person,
facility staff shall document in the person’s
clinical record that the substituted decision-
maker was selected in accordance with the list of
persons and using the priority set out in Section
765.401, F.S. When a health care surrogate or
proxy is used, the facility shall immediately file
a petition for the appointment of a guardian
advocate.
(2) Authorization for Treatment.
(a) Express and informed consent, including the
right to ask questions about the proposed
treatment, to receive complete and accurate
answers to those questions, and to negotiate
treatment options, shall be obtained from
a person who is competent to consent to
treatment. If the person is incompetent to
consent to treatment, such express and informed
consent shall be obtained from the duly
authorized substitute decision-maker for the
person before any treatment is rendered, except
where emergency treatment is ordered by a
Rights of patients
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.
Authorization for Treatment

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
30
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.
physician for the safety of the person or others.
Chapter 394, Part I, F.S., and this rule chapter
govern mental health treatment. Medical
treatment for persons served in receiving
and treatment facilities and by other service
providers are governed by other statutes and
rules.
(b) A copy of information disclosed while
attempting to obtain express and informed
consent shall be given to the person and to any
substitute decision-maker authorized to act on
behalf of the person.
(c) When presented with an event or an alternative
which requires express and informed consent,
a competent person or, if the person is
incompetent to consent to treatment, the
duly authorized substitute decision-maker
shall provide consent to treatment, refuse
consent to treatment, negotiate treatment
alternatives, or revoke consent to treatment.
Recommended forms CF-MH 3042a, Feb. 05,
“General Authorization for Treatment Except
Psychotropic Medications,” which is incorporated
by reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter, and
CF-MH 3042b, Feb. 05, “Specific Authorization for
Psychotropic Medications,” which is incorporated
by reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter may be
used as documentation of express and informed
consent and any decisions made pursuant to
that consent. If used, recommended form CF-MH
3042a, “General Authorization for Treatment
Except Psychotropic Medications,” as referenced
in paragraph 65E-5.170(2)(c), F.A.C., shall be
completed at the time of admission to permit
routine medical care, psychiatric assessment,
and other assessment and treatment except
psychotropic medications. The more specific
recommended form CF-MH 3042b, “Specific
Authorization for Psychotropic Medications,” as
referenced in paragraph 65E-5.170(2)(c), F.A.C.,
or its equivalent, shall be completed prior to the
administration of any psychotropic medications,
except under an emergency treatment order. The
completed forms, or equivalent documentation,
shall be retained in the person’s clinical record.
(d) No facility or service provider shall initiate any
mental health treatment, including psychotropic
Rights of patients

31 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.170 F.A.C.
(3)
(4)
(5)
(6)
(7)
medication, until express and informed consent
for psychiatric treatment is sought from a person
legally qualified to give it, except in instances
where emergency treatment is ordered by a
physician to preserve the immediate safety of
the person or others.
Receiving and treatment facilities shall request
copies of any advance directives completed by
persons admitted to the facilities, from the person
or the person’s family or representative.
In addition to any other requirements, at least
the following must be given to the person before
express and informed consent will be valid:
(a) Identification of the proposed psychotropic
medication, together with a plain language
explanation of the proposed dosage range,
the frequency and method of administration,
the recognized short-term and long-term side
effects, any contraindications which may exist,
clinically significant interactive effects with
other medications, and similar information on
alternative medications which may have less
severe or serious side effects.
(b) A plain language explanation of all other
treatments or treatment alternatives
recommended for the person.
If a change in psychotropic medication is
recommended which is not included in the previously
signed CF-MH 3042b, “Specific Authorization for
Psychotropic Medications” form, as referenced in
paragraph 65E-5.170(2)(c), F.A.C., after an explanation
and disclosure of the altered treatment plan is
provided by the physician express and informed
consent must be obtained from the person
authorized to provide consent and be documented in
the person’s clinical record prior to the administration
of the treatment or psychotropic medication.
The facility or service provider staff shall explain
to a guardian, guardian advocate, or health care
surrogate or proxy, the duty of the substitute
decision-maker to provide information to the
facility or service provider on how the substitute
decision-maker may be reached at any time during
the person’s hospitalization or treatment to provide
express and informed consent for changes of
treatment from that previously approved.
Electroconvulsive treatment may be recommended
to the person or the person’s substitute decision-
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
32
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
Electroconvulsive Treatment
(ECT) Also see
Section 458.325, F.S.
maker by the attending physician. Such
recommendation must also be concurrently
recommended by at least one other physician
not directly involved with the person’s care who
has reviewed the person’s clinical record. Such
recommendation shall be documented in the
person’s clinical record and shall be signed by both
physicians. Recommended form CF-MH 3057, Feb.
05, “Authorization for Electroconvulsive Treatment,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of
this rule chapter may be used for this purpose. If
used, this form shall also be signed by the person,
if competent, or by the guardian advocate, if
previous court approval has been given, or by the
guardian where the person has been found by the
court to be incapacitated, or by the health care
surrogate if the person had expressly delegated
such authority to the surrogate in the advance
directive. Express and informed consent from the
person or his or her substitute decision-maker, as
required by Section 394.459(3), F.S., including an
opportunity to ask questions and receive answers
about the procedure, shall be noted on or attached
to recommended form CF-MH 3057, “Authorization
for Electroconvulsive Treatment,” as referenced in
subsection 65E-5.170(7), F.A.C., or its equivalent,
as documentation of the required disclosures and
of the consent. Each signed authorization form
is permission for the person to receive a series of
up to, but not more than, the stated number of
electroconvulsive treatments identified on the
form. Additional electroconvulsive treatments
require additional written authorization. The signed
authorization form shall be retained in the person’s
clinical record and shall comply with the provisions
of Section 458.325, F.S.
65E-5.1703 Emergency Treatment Orders
for the Administration of Psychotropic
Medications.
(1) An emergency treatment order shall be consistent
with the least restrictive treatment interventions,
including the emergency administration of
psychotropic medications or the emergency
use of restraints or seclusion. Use of seclusion or
restraint in an emergency situation is addressed in
subparagraph 65E-5.180(7)(a)3., F.A.C., and is not
addressed in this rule. This rule pertains only to the
use of psychotropic medication in an emergency
situation.
Rights of patients
(Chapter 394.459 F.S.)
65E-5.1703 F.A.C.
Federal and JCAHO
requirements governing chemical
restraints may apply. Emergency
Treatment Orders (ETOs)
are not the same as chemical
restraints.

33 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.1703 F.A.C.
(a) The issuance of an emergency treatment order
requires a physician’s review of the person’s
condition for causal medical factors, such as
insufficiency of psychotropic medication blood
levels, as determined by drawing a blood sample;
medication interactions with psychotropic
or other medications; side effects or adverse
reactions to medications; organic, disease or
medication based metabolic imbalances or
toxicity; or other biologically based or influenced
symptoms.
(b) All emergency treatment orders may only
be issued by a physician licensed under the
authority of Chapter 458 or 459, F.S.
(c) The physician must review, integrate and address
such metabolic imbalances in the issuance of an
emergency treatment order.
(d) The use of an emergency treatment order must
be consistent with the least restrictive treatment
requirements, and, absent more appropriate
interventions, an emergency treatment order
is for immediate administration of rapid
response psychotropic medications to a person
to expeditiously treat symptoms, that if left
untreated, present an immediate danger to the
safety of the person or others.
(2) An emergency treatment order for psychotropic
medication supersedes the person’s right to
refuse psychotropic medication if based upon
the physician’s assessment that the individual is
not capable of exercising voluntary control over
his or her own symptomatic behavior and that
these uncontrolled symptoms and behavior are
an imminent danger to the person or to others
in the facility. When emergency treatment with
psychotropic medication is ordered for a minor
or an incapacitated or incompetent adult, facility
staff shall document attempts to promptly contact
the guardian, guardian advocate, or health
care surrogate or proxy to obtain express and
informed consent for the treatment in advance of
administration where possible and if not possible, as
soon thereafter as practical.
(3) The physician’s initial order for emergency
treatment may be by telephone but such a verbal
order must be reduced to writing upon receipt and
signed by a physician within 24 hours.
(4) Each emergency treatment order shall only be valid
and shall be authority for emergency treatment only
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
34
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.1703 F.A.C.
(5)
(6)
(7)
(8)
(9)
for a period not to exceed 24 hours.
The need for each emergency treatment order
must be documented in the person’s clinical record
in the progress notes and in the section used for
physician’s orders and must describe the specific
behavior which constitutes a danger to the person
or to others in the facility, and the nature and extent
of the danger posed.
Upon the initiation of an emergency treatment
order the facility shall, within two court working
days, petition the court for the appointment of
a guardian advocate pursuant to the provisions
of Section 394.4598, F.S., to provide express and
informed consent, unless the person voluntarily
withdraws a revocation of consent or requires only
a single emergency treatment order for emergency
treatment.
If a second emergency treatment order is issued
for the same person within any 7 day period, the
petition for the appointment of a guardian advocate
pursuant to the provisions of Section 394.4598, F.S.,
to provide express and informed consent shall be
filed with the court within 1 court working day.
While awaiting court action, treatment may be
continued without the consent of the person, but
only upon the daily written emergency treatment
order of a physician who has determined that the
person’s behavior each day during the wait for court
action continues to present an immediate danger
to the safety of the person or others and who
documents the nature and extent of the emergency
each day of the specific danger posed. Such orders
may not be written in advance of the demonstrated
need for same.
To assure the safety and rights of the person, and
since emergency treatment orders by a physician
absent express and informed consent are permitted
only in an emergency, any use of psychotropic
medications other than rapid response psychotropic
medications requires a detailed and complete
justification for the use of such medication. Both the
nature and extent of the imminent emergency and
any orders for the continuation of that medication
must be clearly documented daily as required
above.
Rights of patients

35 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
(4) QUALITY OF TREATMENT.
(a) Each patient shall receive services,
including, for a patient placed under s.
394.4655, those services included in the
court order which are suited to his or her
needs, and which shall be administered
skillfully, safely, and humanely with full
respect for the patient’s dignity and personal
integrity. Each patient shall receive such
medical, vocational, social, educational, and
rehabilitative services as his or her condition
requires in order to live successfully in the
community. In order to achieve this goal,
the department is directed to coordinate
its mental health programs with all other
programs of the department and other state
agencies.
(b)Facilities shall develop and maintain,
in a form accessible to and readily
understandable by patients and consistent
with rules adopted by the department, the
following:
1. Criteria, procedures, and required sta
training for any use of close or elevated
levels of supervision, of restraint, seclu-
sion, or isolation, or of emergency treat-
ment orders, and for the use of bodily
control and physical management
techniques.
2. Procedures for documenting, monitor-
ing, and requiring clinical review of
all uses of the procedures described in
subparagraph 1. and for documenting
and requiring review of any incidents
resulting in injury to patients.
3. A system for investigating, tracking,
managing, and responding to com-
plaints by persons receiving services or
individuals acting on their behalf.
(c) A facility may not use seclusion or restraint
for punishment, to compensate for
inadequate stang, or for the convenience
of sta. Facilities shall ensure that all sta
are made aware of these restrictions on
65E-5.180 Right to Quality Treatment.
The following standards shall be required in the provision
of quality mental health treatment:
(1) Each receiving and treatment facility and service
provider shall, using nationally accepted accrediting
standards for guidance, develop written policies
and procedures for planned program activities
designed to enhance the person’s self image, as
required by Section 394.459(2)(d), F.S. These policies
and procedures shall include curriculum, specific
content, and performance objectives and shall be
delivered by staff with content expertise. Medical,
rehabilitative, and social services shall be integrated
and provided in the least restrictive manner
consistent with the safety of the persons served.
(2) Each facility and service provider, using nationally
accepted accrediting standards for guidance, shall
adopt written professional standards of quality,
accuracy, completeness, and timeliness for all
diagnostic reports, evaluations, assessments,
examinations, and other procedures provided to
persons under the authority of Chapter 394, Part
I, F.S. Facilities shall monitor the implementation
of those standards to assure the quality of all
diagnostic products. Standards shall include and
specify provisions addressing:
(a) The minimum qualifications to assure
competence and performance of staff who
administer and interpret diagnostic procedures
and tests;
(b) The inclusion and updating of pertinent
information from previous reports, including
admission history and key demographic, social,
economic, and medical factors;
(c) The dating, accuracy and the completeness of
reports;
(d) The timely availability of all reports to users;
(e) Reports shall be legible and understandable;
(f) The documentation of facts supporting each
conclusion or finding in a report;
(g) Requirements for the direct correlation of identified
problems with problem resolutions that consider
the immediacy of the problem or time frames for
resolution and which include recommendations for
further diagnostic work-ups;
(h) Requirement that the completed report be signed
and dated by the administering staff ; and
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
the use of seclusion and restraint and
(i) Consistency of information across various
shall make and maintain records which
reports and integration of information and
demonstrate that this information has been
approaches across reports.
conveyed to individual sta members.
(3) Psychiatric Examination. Psychiatric examinations
shall include:
(a) Medical history, including psychiatric history,
developmental abnormalies, physical or sexual
abuse or trauma, and substance abuse;
Psychiatric Examinations
(b) Examination, evaluative or laboratory results,
including mental status examination;
(c) Working diagnosis, ruling out non-psychiatric
causes of presenting symptoms of abnormal
thought, mood or behaviors;
(d) Course of psychiatric interventions including:
1. Medication history, trials and results;
2. Current medications and dosages;
3. Other psychiatric interventions in response
to identified problems;
(e) Course of other non-psychiatric medical
problems and interventions;
(f) Identification of prominent risk factors including
physical health, psychiatric and co-occurring
substance abuse; and
(g) Discharge or transfer diagnoses.
(4) So that care will not be delayed upon arrival,
procedures for the transfer of the physical custody of
persons shall specify and require that documentation
necessary for legal custody and medical status,
including the person’s medication administration
record for that day, shall either precede or
accompany the person to his or her destination.
(5) Mental health services provided shall comply with
the following standards:
(a) In designated receiving facilities, the on-site
provision of emergency psychiatric reception
and treatment services shall be available
24-hours-a-day, seven-days-a-week, without
regard to the person’s financial situation.
(b) Assessment standards shall include provision
for determining the presence of a co-occurring
mental illness and substance abuse, and
clinically significant physical and sexual abuse or
trauma.
(c) A clinical safety assessment shall be
accomplished at admission to determine the
person’s need for, and the facility’s capability to
provide, an environment and treatment setting
that meets the person’s need for a secure facility
or close levels of staff observation.
Rights of patients
36

37 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
(d) The development and implementation of
protocols or procedures for conducting
and documenting the following shall be
accomplished by each facility:
1. Determination of a person’s competency to
consent to treatment within 24 hours after
admission;
2. Identification of a duly authorized decision-
maker for the person upon any person being
determined not to be competent to consent
to treatment;
3. Obtaining express and informed consent
for treatment and medications before
administration, except in an emergency; and
4. Required involvement of the person and
guardian, guardian advocate, or health
care surrogate or proxy, in treatment and
discharge planning.
(e) Use of age sensitive interventions in the
implementation of seclusion or in the use
of physical force as well as the authorization
and training of staff to implement restraints,
including the safe positioning of persons in
restraints. Policies, procedures and services
shall incorporate specific provisions regarding
the restraining of minors, elders, and persons
who are frail or with medical problems such as
potential problems with respiration.
(f ) Plain language documentation in the person’s
clinical record of all uses of “as needed” or
emergency applications of psychotropic
medications, and all uses of physical force,
restraints, seclusion, or “time-out” procedures upon
persons, and the explicit reasons for their use.
(g) The prohibition of standing orders or similar
protocols for the emergency use of psychotropic
medication, restraint, or seclusion.
(h) Provision of required training for guardian
advocates including activities and available
resources designed to assist family members
and guardian advocates in understanding
applicable treatment issues and in identifying
and contacting local self-help organizations.
(6) Each facility shall develop a written policy and
procedure for receiving, investigating, tracking,
managing and responding to formal and informal
complaints by a person receiving services or by an
individual acting on his or her behalf.
(a) The complaint process shall be verbally
Complaint investigation procedure
required. See 65E-5.352 for
additional complaint investigation
procedures.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
38
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
Florida statewide and local advocacy
councils no longer exist because they
were de-funded by the 2010 Florida
Legislature.
explained during the orientation process
and provided in writing in language and
terminology that the person receiving services
can understand. It will explain how individuals
may address complaints informally through the
facility staff and treatment team, and formally
through the staff person assigned to handle
formal complaints, as well as the administrator
or designee of the facility. The person receiving
services shall also be advised that he or she
may contact the Local Advocacy Council, the
Florida Abuse Registry, the Advocacy Center for
Persons with Disabilities, or any other individual
or agency at anytime during the complaint
process to request assistance. The complaint
process, including telephone numbers for the
above named entities, shall be posted in plain
view in common areas and next to telephones
used by individuals receiving services. Any
complaint may be verbal or written. Any
staff person receiving an informal or formal
complaint dealing with life-safety issues will take
immediate action to resolve the matter.
(b) Informal complaints are initial complaints that
are usually made verbally by a person receiving
services or by an individual acting on his or her
behalf. If resolution cannot be mutually agreed
upon, a formal written complaint may be initiated.
(c) When the person receiving services, or a person
acting upon that person’s behalf, makes a formal
complaint a staff person not named in the
complaint shall assist the person in initiating the
complaint. The complaint shall include the date
and time of the complaint and detail the issue
and the remedy sought. All formal complaints
shall be forwarded to the staff person, or
designee, who is assigned to track and monitor
formal complaints. All formal complaints shall be
tracked and monitored for compliance and shall
contain the following information:
1. The date and time the formal complaint was
originally received by staff ;
2. The date and time the formal complaint was
received by the staff assigned to track formal
complaints;
3. The nature of the complaint;
4. The name of the person receiving services;
5. The name of the person making the
complaint;
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.

39 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
6. The name of the individual assigned to
investigate the complaint;
7. The date the individual making the
complaint was notified of the individual
assigned to investigate the complaint;
8. The due date for the written response; and
9. At closure, the written disposition of the
formal complaint.
(d) The investigation shall be completed within 7
days from the date of entry into the system for
tracking complaints.
(e) A written response must be given or mailed to
the person receiving services within 24 hours of
disposition. The individual acting on behalf of
the person receiving services shall be notified of
the completion of the investigation but will not
be given specific details of the disposition unless
they have a legal right to the information or a
signed release of information is in place.
(f ) The disposition of a complaint may be appealed
to the administrator of the facility. If appealed,
the facility administrator or designee shall
review the written complaint and the initial
disposition. Within five working days, the
facility administrator or designee will make a
final decision concerning the outcome of the
complaint and will provide a written response
within 24 hours to the person receiving
services. A copy of the written response shall
also be given to the staff member assigned to
track complaints.
(7) Seclusion and Restraint for Behavior
Management Purposes. All facilities, as defined in
Section 394.455(10), F.S., are required to adhere to
the standards and requirements of subsection (7).
(a) General Standards.
1. Each facility will provide a therapeutic
milieu that supports a culture of recovery
and individual empowerment and
responsibility. Each person will have a voice
in determining his or her treatment options.
Treatment will foster trusting relationships
and partnerships for safety between staff
and individuals. Facility practices will be
particularly sensitive to persons with a
history of trauma.
2. The health and safety of the person shall be
the primary concern at all times.
3. Seclusion or restraint shall be employed only
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
Seclusion and Restraint also governed
by federal conditions of participation,
accreditation organizations, and
facility policies and procedures.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
40
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
in emergency situations when necessary
to prevent a person from seriously injuring
self or others, and less restrictive techniques
have been tried and failed, or if it has been
clinically determined that the danger is
of such immediacy that less restrictive
techniques cannot be safely applied.
4. There is a high prevalence of past traumatic
experience among persons who receive
mental health services. The response
to trauma can include intense fear and
helplessness, a reduced ability to cope,
and an increased risk to exacerbate or
develop a range of mental health and other
medical conditions. The experience of being
placed in seclusion or being restrained is
potentially traumatizing. Seclusion and
restraint practices shall be guided by the
following principles of trauma-informed
care: assessment of traumatic histories
and symptoms; recognition of culture and
practices that are re-traumatizing; processing
the impact of a seclusion or restraint with the
person; and addressing staff training needs to
improve knowledge and sensitivity.
5. When a person demonstrates a need for
immediate medical attention in the course
of an episode of seclusion or restraint, the
seclusion or restraint shall be discontinued,
and immediate medical attention shall be
obtained.
6. Persons will not be restrained in a prone
position. Prone containment will be used
only when required by the immediate
situation to prevent imminent serious harm
to the person or others. To reduce the risk of
positional asphyxiation, the person will be
repositioned as quickly as possible.
7. Responders will pay close attention to
respiratory function of the person during
containment and restraint. All staff involved
will observe the person’s respiration,
coloring, and other possible signs of distress
and immediately respond if the person
appears to be in distress. Responding to the
person's distress may include repositioning
the person, discontinuing the seclusion or
restraint, or summoning medical attention,
as necessary.
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
Trauma Informed Care.

41 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
8. Objects that impair respiration shall not be
placed over a person’s face. In situations
where precautions need to be taken to
protect staff, staff may wear protective gear.
9. Unless necessary to prevent serious injury, a
person's hands shall not be secured behind
the back during containment or restraint.
10. The use of walking restraints is prohibited
except for purposes of off-unit transportation
and may only be used under direct
observation of trained staff. In this instance,
direct observation means that staff maintains
continual visual contact of the person and is
within close physical proximity to the person
at all times.
11. The person shall be released from seclusion
or restraint as soon as he or she is no longer
an imminent danger to self or others.
12. Seclusion or restraint use shall not be based
on the person’s seclusion or restraint use
history or solely on a history of dangerous
behavior. Dangerous behaviors include those
behaviors that jeopardize the physical safety
of oneself or others.
13. Seclusion and restraint may not be used
simultaneously for children less than 18 years
of age.
14. A person who is restrained must not be
located in areas, whenever possible, subject
to view by persons other than involved staff
or where exposed to potential injury by other
persons. This does not apply to the use of
walking restraints.
15. Each facility utilizing seclusion or restraint
procedures shall establish and utilize a
Seclusion and Restraint Oversight Committee.
(b) Staff training.
Staff must be trained as part of orientation
and subsequently on at least an annual basis.
Staff responsible for the following actions
will demonstrate relevant competency in the
following areas before participating in a seclusion
or restraint event or related assessment, or before
monitoring or providing care during an event:
1. Strategies designed to reduce confrontation
and to calm and comfort people, including
the development and use of a personal safety
plan,
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
Training required for all
direct service staff. See
also 65E-5.330, F.A.C.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
42
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
2. Use of nonphysical intervention skills as well
as bodily control and physical management
techniques, based on a team approach, to
ensure safety,
3. Observing for and responding to signs of
physical and psychological distress during
the seclusion or restraint event,
4. Safe application of restraint devices,
5. Monitoring the physical and psychological
well-being of the person who is restrained
or secluded, including but not limited
to: respiratory and circulatory status,
skin integrity, vital signs, and any special
requirements specified by facility policy
associated with the one hour face-to-face
evaluation,
6. Clinical identification of specific behavioral
changes that indicate restraint or seclusion is
no longer necessary,
7. The use of first aid techniques, and
8. Certification in the use of cardiopulmonary
resuscitation, including required periodic
recertification. The frequency of training
for cardiopulmonary resuscitation will be in
accordance with certification requirements,
notwithstanding provision subparagraph
(7)(b).
(c) Prior to the Implementation of Seclusion or
Restraint.
1. Prior intervention shall include
individualized therapeutic actions such as
those identified in a personal safety plan
that address individual triggers leading
to psychiatric crisis. Recommended form
CF-MH 3124, Feb. 05, “Personal Safety Plan,”
which is incorporated by reference and may
be obtained pursuant to Rule 65E-5.120,
F.A.C., of this rule chapter may be used
for the purpose of guiding individualized
techniques. Prior interventions may also
include verbal de-escalation and calming
strategies. Non physical interventions shall
be the first choice unless safety issues
require the use of physical intervention.
2. A personal safety plan shall be completed or
updated as soon as possible after admission
and filed in the person’s medical record.
a. This form shall be reviewed by the
recovery team, and updated if necessary,
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
Prior to Seclusion and Restraint.

43 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
after each incident of seclusion or
restraint.
b. Specific intervention techniques from
the personal safety plan that are offered
or used prior to a seclusion or restraint
event shall be documented in the per-
son's medical record after each use of
seclusion or restraint.
c. All staff shall be aware of and have
ready access to each person’s personal
safety plan.
(d) Implementation of Seclusion or Restraint.
1. A registered nurse or highest level staff
member, as specified by written facility
Federal conditions of
policy, who is immediately available and
participation and JCAHO/
who is trained in seclusion and restraint
CARF requirements governing
procedures may initiate seclusion or restraint
seclusion/restraints may also
in an emergency when danger to oneself or
apply. The most stringent
others is imminent. An order for seclusion
standard applying to each facility
or restraint must be obtained from the
must be followed.
physician, Advanced Registered Nurse
Practitioner (ARNP), or Physician's Assistant
(PA), if permitted by the facility to order
seclusion and restraint and stated within
their professional protocol. The treating
physician must be consulted as soon as
possible if the seclusion or restraint was not
ordered by the person's treating physician.
2. An examination of the person will be
conducted within one hour by the physician
or may be delegated to an Advanced
Registered Nurse Practitioner, Physician's
Assistant, or Registered Nurse (RN), if
authorized by the facility and trained
in seclusion and restraint procedures
as described in paragraph (7)(b). This
examination shall include a face-to face
assessment of the person’s medical and
behavioral condition, a review of the
clinical record for any pre-existing medical
diagnosis or physical condition which
may contraindicate the use of seclusion or
restraint, a review of the person’s medication
orders including an assessment of the need
to modify such orders during the period of
seclusion or restraint, and an assessment
of the need or lack of need to elevate the
person’s head and torso during restraint.
The comprehensive examination must
Rights of patients
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
44
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
3.
4.
5.
determine that the risks associated with the
use of seclusion or restraint are significantly
less than not using seclusion or restraint
and whether to continue or terminate the
intervention. A licensed psychologist may
conduct only the behavioral assessment
portion of the comprehensive assessment
if authorized by the facility and trained
in seclusion and restraint procedures as
described in paragraph (7)(b). Documentation
of the comprehensive examination, including
the time and date completed, shall be
included in the person’s medical record. If
the face-to-face evaluation is conducted by
a trained Registered Nurse, the attending
physician who is responsible for the care of
the person must be consulted as soon as
possible after the evaluation is completed.
Each written order for seclusion or restraint
is limited to four hours for adults, age 18 and
over; two hours for children and adolescents
age nine through 17; or one hour for children
under age nine. A seclusion or restraint
order may be renewed in accordance with
these limits for up to a total of 24 hours,
after consultation and review by a physician,
ARNP, or PA in person, or by telephone with a
Registered Nurse who has physically observed
and evaluated the person. When the order
has expired after 24 hours, a physician,
ARNP, or PA must see and assess the person
before seclusion or restraint can be re-
ordered. The results of this assessment must
be documented. Seclusion or restraint use
exceeding 24 hours requires the notification
of the Facility Administrator or designee.
All orders must be signed within 24 hours of
the initiation of seclusion or restraint.
The order shall include the specific behavior
prompting the use of seclusion or restraint,
the time limit for seclusion or restraint, and
the behavior necessary for the person's
release. Additionally, for restraint, the
order shall contain the type of restraint
ordered and the positioning of the person,
including possibly elevating the person’s
head for respiratory and other medical
safety considerations. Consideration shall be
Rights of patients

45 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
given to age, physical fragility, and physical
disability when ordering restraint type.
6. An order for seclusion or restraint shall not
be issued as a standing order or on an as-
needed basis.
7. In order to protect the safety of each
person served by a facility, each person
shall be searched for contraband before
or immediately after being placed into
seclusion or restraints.
8. The person shall be clothed appropriately for
temperature and at no time shall a person
be placed in seclusion or restraint in a nude
or semi-nude state.
9. Every secluded or restrained person shall be
immediately informed of the behavior that
resulted in the seclusion or restraint and the
behavior and the criteria reflecting absence
of imminent danger that are necessary for
release.
10.For persons under the age of 18, the facility
must notify the parent(s) or legal guardian(s)
of the person who has been restrained or
placed in seclusion as soon as possible, but
no later than 24 hours, after the initiation
of each seclusion or restraint event. This
notification must be documented in the
person's medical record, including the date
and time of notification and the name of the
staff person providing the notification.
11.For each use of seclusion or restraint, the
following information shall be documented
in the person's medical record: the
emergency situation resulting in the
seclusion or restraint event; alternatives
or other less restrictive interventions
attempted, as applicable, or the clinical
determination that less restrictive
techniques could not be safely applied;
the name and title of the staff member
initiating the seclusion or restraint; the
date/time of initiation and release; the
person’s response to seclusion or restraint,
including the rationale for continued use of
the intervention; and that the person was
informed of the behavior that resulted in
the seclusion or restraint and the criteria
necessary for release.
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
During seclusion and restraint.
Federal and JCAHO
requirements governing seclusion
and restraints may apply.
(e) During Seclusion or Restraint Use.
1. When restraint is initiated, nursing staff
shall see and assess the person as soon as
possible but no later than 15 minutes after
initiation and at least every hour thereafter.
The assessment shall include checking
the person's circulation and respiration,
including necessary vital signs (pulse and
respiratory rate at a minimum).
2. The person over age 12 who is secluded
shall be observed by trained staff every 15
minutes. At least one observation an hour
will be conducted by a nurse. Restrained
persons must have continuous observation
by trained staff. Secluded children age 12
and under must be monitored continuously
by face-to-face observation or by direct
observation through the seclusion window
for the first hour and then at least every 15
minutes thereafter.
3. Monitoring the physical and psychological
well-being of the person who is secluded
or restrained shall include but is not
limited to: respirator y and circulator y
status; signs of injur y; vital signs; skin
integrity; and any special requirements
specified by facility policies. This
monitoring shall be conduc ted by trained
staff as required in paragraph (7)(b).
4. During each period of seclusion or restraint,
the person must be offered reasonable
opportunities to drink and toilet as
requested. In addition, the person who is
restrained must be offered opportunities
to have range of motion at least every two
hours to promote comfort. Each facility
shall have written policies and procedures
specifying the frequency of providing drink,
toileting, and check of bodily positioning to
avoid traumatizing a person and retaining
the person’s maximum degree of dignity and
comfort during the use of bodily control and
physical management techniques.
5. Documentation of the observations and the
staff person’s name shall be recorded at the
time the observation takes place.
(f) Release from Seclusion or Restraint and
Post-Release Activities.
1. Release from seclusion or restraint shall
Rights of patients
46
47Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
(Chapter 394.459 F.S.)
Current and accurate as of date of printing September 2013
occur as soon as the person no longer
appears to present an imminent danger
to themselves or others. Upon release
from seclusion or restraint, the person’s
physical condition shall be observed,
evaluated, and documented by trained staff.
Documentation shall also include: the name
and title of the staff releasing the person;
and the date and time of release.
2. After a seclusion or restraint event, a
debriefing process shall take place to
decrease the likelihood of a future seclusion
or restraint event for the person and to
provide support.
a. Each facility shall develop policies to ad-
dress:
(I) A review of the incident with the person
who was secluded or restrained. The
person shall be given the opportunity to
process the seclusion or restraint event
as soon as possible but no longer than
within 24 hours of release. This debrief-
ing discussion shall take place between
the person and either the recovery team
or another preferred staff member. This
review shall seek to understand the
incident within the framework of the
person's life history and mental health
issues. It should assess the impact of
the event on the person and help the
person identify and expand coping
mechanisms to avoid the use of seclu-
sion or restraint in the future. The discus-
sion will include constructive coping
techniques for the future. A summary
of this review should be documented in
the person’s medical record.
(II) A review of the incident with all staff
involved in the event and supervisors
or administrators. This review shall be
conducted as soon as possible after the
event and shall address: the circum-
stances leading to the event, the nature
of de-escalation efforts and alternatives
to seclusion and restraint attempted,
staff response to the incident, and ways
to effectively support the person's con-
structive coping in the future and avoid
the need for future seclusion or restraint.
Rights of patients
65E-5.180 F.A.C.
Release and Post-Release from
seclusion and restraint.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
48
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
The outcomes of this review should be
documented by the facility for purposes
of continuous performance improve-
ment and monitoring. The review find-
ings will be forwarded to the Seclusion
and Restraint Oversight Committee, and
(III) Support for other persons served and
staff, as needed, to return the unit to a
therapeutic milieu.
b. Within 2 working days after any use of
seclusion or restraint, the recovery team
shall meet and review the circumstances
preceding its initiation and review the
person's recovery plan and personal
safety plan to determine whether any
changes are needed in order to prevent
the further use of seclusion or restraint.
The recovery team shall also assess the
impact the event had on the person and
provide any counseling, services, or treat-
ment that may be necessary as a result.
The recovery team shall analyze the
person’s clinical record for trends or pat-
terns relating to conditions, events, or the
presence of other persons immediately
before or upon the onset of the behavior
warranting the seclusion or restraint, and
upon the person’s release from seclusion.
The recovery team shall review the effec-
tiveness of the emergency intervention
and develop more appropriate thera-
peutic interventions. Documentation of
this review shall be placed in the person’s
clinical record.
c. The Seclusion and Restraint Oversight
Committee shall conduct timely reviews
of each use of seclusion and restraints
and monitor patterns of use, for the
purpose of assuring least restrictive ap-
proaches are utilized to prevent or reduce
the frequency and duration of use.
(g) Reporting.
1. All facilities, as defined in Section
394.455(10), Florida Statutes, are required
to report each seclusion and restraint
event to the Department of Children and
Families. This reporting shall be done
electronically using the Department’s
web-based application either directly via
Rights of patients
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
Reporting events of seclusion
and restraint.

49 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.180 F.A.C.
2.
3.
the data input screens or indirectly via the
File Transfer Protocol batch process. The
required reporting elements are: Provider
tax identification number; Person's social
security number and identification number;
date and time the seclusion or restraint
event was initiated; discipline of the person
ordering the seclusion or restraint; discipline
of the person implementing the seclusion or
restraint; reason seclusion or restraint was
initiated; type of restraint used; whether
significant injuries were sustained by the
person; and date and time seclusion or
restraint was terminated. Facilities shall
report seclusion and restraint events on a
monthly basis. Events that result in death or
significant injury either to a staff member or
person shall be reported to the department’s
web based system in accordance with
department operating procedures.
All facilities that are subject to the
Conditions of Participation for Hospitals,
42 Code of Federal Regulations, part
482, under the Centers for Medicare and
Medicaid Services (CMS), must report to
CMS any death that occurs in the following
circumstances:
a. While a person is restrained or secluded;
b. Within 24 hours after release from seclu-
sion or restraint; or
c. Within one week after seclusion or re-
straint, where it is reasonable to assume
that use of the seclusion or restraint
contributed directly or indirectly to the
person’s death.
Each death described in this section shall be
reported to CMS by telephone no later than
the close of business the next business day
following knowledge of the persons’ death.
A report shall simultaneously be submitted
to the Director of Mental Health/Designee
in the Mental Health Program Office
headquarters in Tallahassee, FL. The address
is: 1317 Winewood Blvd., Tallahassee, Fl,
32399-0700.
The Department shall collect and review
the data on a monthly basis. The Director
of Mental Health shall be informed of any
deaths or significant injuries related to
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
50
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
Rights of patients
seclusion or restraint and significant trends
regarding seclusion and restraint use.
(h) Nothing herein shall affect the ability of
emergency medical technicians, paramedics or
physicians or any person acting under the direct
medical supervision of a physician to provide
examination or treatment of incapacitated
persons in accordance with Section 401.445, F.S.
(8) Use of Protective Medical Devices with Frail or
Mobility Impaired Persons.
(a) When ordering safety or protective devices such
as posey vests, geri-chairs, mittens, and bed rails
which also restrain, facility staff shall consider
alternative means of providing such safety so
that the person’s need for regular exercise is
accommodated to the greatest extent possible.
(b) Where frequent or prolonged use of safety
or protective devices is required, the person’s
treatment plan shall address debilitating
effects due to decreased exercise levels such
as circulation, skin, and muscle tone and the
person’s need for maintaining or restoring bowel
and bladder continence.
(c) The treatment plan shall include scheduled
activities to lessen deterioration due to the usage
of such protective medical devices.
(9) Elevated Levels of Supervision. Receiving and
treatment facilities shall ensure that where one-
on-one supervision is ordered by a physician, it
shall be continuous and shall not be interrupted as
a result of shift changes or due to conflicting staff
assignments. Such supervision shall be continuous
until documented as no longer medically necessary
by a physician.
65E-5.1802 Maintenance of the Facility.
The facility shall ensure the proper functioning and
maintenance of the facility structure, finishes, fixtures,
furnishings, and equipment. The facility shall ensure the
ready availability of necessary medical equipment or
devices for the populations served, including restraint
equipment that is suitable to the safety and medical
needs of the persons being served.
(Chapter 394.459 F.S.)
65E-5.1802 F.A.C.
Protective Medical Devices.

51 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(5) COMMUNICATION, ABUSE
REPORTING, AND VISITS.
(a) Each person receiving services in a facility
providing mental health services under this
part has the right to communicate freely
and privately with persons outside the
facility unless it is determined that such
communication is likely to be harmful
to the person or others. Each facility
shall make available as soon as reasonably
possible to persons receiving services a
telephone that allows for free local calls and
access to a long-distance service. A facility
is not required to pay the costs of a patient’s
long-distance calls. e telephone shall be
readily accessible to the patient and shall
be placed so that the patient may use it to
communicate privately and condentially.
e facility may establish reasonable rules
for the use of this telephone, provided that
the rules do not interfere with a patient’s
access to a telephone to report abuse
pursuant to paragraph (e).
(b) Each patient admitted to a facility under
the provisions of this part shall be allowed
to receive, send, and mail sealed, unopened
correspondence; and no patient’s incoming
or outgoing correspondence shall be
opened, delayed, held, or censored by the
facility unless there is reason to believe
that it contains items or substances which
may be harmful to the patient or others,
in which case the administrator may direct
reasonable examination of such mail and
may regulate the disposition of such items
or substances.
(c) Each facility must permit immediate access
to any patient, subject to the patient’s right
to deny or withdraw consent at any time,
by the patient’s family members, guardian,
guardian advocate, representative, Florida
statewide or local advocacy council, or
attorney, unless such access would be
detrimental to the patient. If a patient’s
Rights of patients
(Chapter 394.459 F.S.)
65E-5.190 F.A.C.
65E-5.190 Right to Communication and
Visits.
(1) If the treatment team imposes any restrictions
on whom a person in a receiving or treatment
facility may communicate, such restrictions and
justification shall be recorded in the person’s
clinical record. Recommended form CF-MH 3049,
Feb. 05, “Restriction of Communication or Visitors,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
rule chapter may be used for this purpose. Facility
staff shall make competent adults aware that they
have the ability to waive the confidentiality of their
presence in a receiving or treatment facility and
allowing all or specified individuals the person
selects access to private and open communication
with the person. Recommended form CF-MH 3048,
Feb. 05, “Confidentiality Agreement,” incorporated
by reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter may be used for
this purpose.
(2) Immediate access to a telephone shall be provided
to each person requesting to call his or her legal
counsel, Florida Abuse Registry, Florida Local
Advocacy Council, or the Advocacy Center for
Persons with Disabilities.
Florida statewide and local
advocacy councils no longer exist
because they were de-funded by
the 2010 Florida Legislature.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
52
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.190 F.A.C.
right to communicate or to receive visitors
is restricted by the facility, written notice
of such restriction and the reasons for
the restriction shall be served on the
patient, the patient’s attorney, and the
patient’s guardian, guardian advocate, or
representative; and such restriction shall
be recorded on the patient’s clinical record
with the reasons therefor. e restriction
of a patient’s right to communicate or to
receive visitors shall be reviewed at least
every 7 days. e right to communicate
or receive visitors shall not be restricted as
a means of punishment. Nothing in this
paragraph shall be construed to limit the
provisions of paragraph (d).
(d)Each facility shall establish reasonable rules
governing visitors, visiting hours, and the
use of telephones by patients in the least
restrictive possible manner. Patients shall
have the right to contact and to receive
communication from their attorneys at any
reasonable time.
(e) Each patient receiving mental health
treatment in any facility shall have ready
access to a telephone in order to report an
alleged abuse. e facility sta shall orally
and in writing inform each patient of the
procedure for reporting abuse and shall
make every reasonable eort to present
the information in a language the patient
understands. A written copy of that
procedure, including the telephone number
of the central abuse hotline and reporting
forms, shall be posted in plain view.
(f) e department shall adopt rules providing
a procedure for reporting abuse. Facility
sta shall be required, as a condition of
employment, to become familiar with
the requirements and procedures for the
reporting of abuse.
Rights of patients
53 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.210 F.A.C.
(6) CARE AND CUSTODY OF PERSONAL
EFFECTS OF PATIENTS.
A patient’s right to the possession of his or her
clothing and personal eects shall be respected.
e facility may take temporary custody of such
eects when required for medical and safety rea-
sons. A patient’s clothing and personal eects shall
be inventoried upon their removal into temporary
custody. Copies of this inventory shall be given to
the patient and to the patient’s guardian, guardian
advocate, or representative and shall be recorded
in the patient’s clinical record. is inventory
may be amended upon the request of the patient
or the patient’s guardian, guardian advocate, or
representative. e inventory and any amend-
ments to it must be witnessed by two members of
the facility sta and by the patient, if able. All of a
patient’s clothing and personal eects held by the
facility shall be returned to the patient immedi-
ately upon the discharge or transfer of the patient
from the facility, unless such return would be
detrimental to the patient. If personal eects are
not returned to the patient, the reason must be
documented in the clinical record along with the
disposition of the clothing and personal eects,
which may be given instead to the patient’s guard-
ian, guardian advocate, or representative. As soon
as practicable after an emergency transfer of a
patient, the patient’s clothing and personal eects
shall be transferred to the patient’s new location,
together with a copy of the inventory and any
amendments, unless an alternate plan is approved
by the patient, if able, and by the patient’s guard-
ian, guardian advocate, or representative.
(7) VOTING IN PUBLIC ELECTIONS.
A patient who is eligible to vote according to
the laws of the state has the right to vote in the
primary and general elections. e department
shall establish rules to enable patients to obtain
voter registration forms, applications for absen-
tee ballots, and absentee ballots.
65E-5.200 Right to Care and Custody of
Personal Effects.
Each designated receiving and treatment facility shall
develop policies and procedures governing what
personal effects will be removed from persons for
reasons of personal or unit safety, how they will be safely
retained by the facility, and how and when they will be
returned to the person or other authorized individual.
Policies and procedures shall specify how contraband
and other personal effects determined to be detrimental
to the person will be addressed when not returned to
the person or other authorized individual. An inventory
of personal effects shall be witnessed by two staff and by
the person, if able, at the time of admission, at any time
the inventory is amended, and at the time the personal
effects are returned or transferred. Recommended form
CF-MH 3043, Feb. 05, “Inventory of Personal Effects,”
which is incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule chapter
may be used for this purpose.
65E-5.210 Right to Vote in Public Elections.
The facility shall have voter registration forms and
applications for absentee ballots readily available at the
facility or in accordance with the procedures established
by the supervisor of elections, and shall assure that
each person who is eligible to vote and wishes to do
so, may exercise his or her franchise. Each designated
receiving and treatment facility shall develop policies and
procedures governing how persons will be assisted in
exercising their right to vote.
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
54
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.601 F.A.C.
(8) HABEAS CORPUS.
(a) At any time, and without notice, a person
held in a receiving or treatment facility,
or a relative, friend, guardian, guardian
advocate, representative, or attorney, or
the department, on behalf of such person,
may petition for a writ of habeas corpus
to question the cause and legality of such
detention and request that the court order
a return to the writ in accordance with
chapter 79. Each patient held in a facility
shall receive a written notice of the right to
petition for a writ of habeas corpus.
(b) At any time, and without notice, a person
who is a patient in a receiving or treatment
facility, or a relative, friend, guardian,
guardian advocate, representative, or
attorney, or the department, on behalf of
such person, may le a petition in the circuit
court in the county where the patient is
being held alleging that the patient is being
unjustly denied a right or privilege granted
herein or that a procedure authorized herein
is being abused. Upon the ling of such a
petition, the court shall have the authority
to conduct a judicial inquiry and to issue
any order needed to correct an abuse of the
provisions of this part.
(c) e administrator of any receiving or
treatment facility receiving a petition under
this subsection shall le the petition with
the clerk of the court on the next court
working day.
(d)No fee shall be charged for the ling of a
petition under this subsection.
(9) VIOLATIONS.
e department shall report to the Agency for
Health Care Administration any violation of
the rights or privileges of patients, or of any
procedures provided under this part, by any
facility or professional licensed or regulated by
the agency. e agency is authorized to im-
pose any sanction authorized for violation of
this part, based solely on the investigation and
ndings of the department.
65E-5.220 Right to Habeas Corpus.
(1) Upon admission to a receiving or treatment facility,
each person shall be given notice of his or her
right to petition for a writ of habeas corpus and for
redress of grievances. Recommended form CF-MH
3036, Feb. 05, “Notice of Right to Petition for Writ
of Habeas Corpus or for Redress of Grievances,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
rule chapter may be used for this purpose. A copy
of the notice shall be provided to the guardian,
guardian advocate, representative, or the health care
surrogate or proxy, and the person’s clinical record
shall contain documentation that the notice was
provided. A petition form shall be promptly provided
by staff to any person making a request for such a
petition. Recommended form CF-MH 3090, Feb. 05,
“Petition for Writ of Habeas Corpus or for Redress of
Grievances,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose.
(2) Receiving and treatment facilities shall accept and
forward to the appropriate court of competent
jurisdiction a petition submitted by the person or
others in any form in which it is presented.
65E-5.601 Operation and Administration of
State Mental Health Treatment Facilities.
(1) In order to protect the welfare of the individuals
residing in state civil mental health facilities, the
department shall establish the following grievance
process for residents of all state civil mental health
treatment facilities. The process shall be explained
during the orientation process and in written
orientation materials.
Rights of patients

55 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Rights of patients
(Chapter 394.459 F.S.)
65E-5.602 F.A.C.
(10) LIABILITY FOR VIOLATIONS.
Any person who violates or abuses any rights
or privileges of patients provided by this part
is liable for damages as determined by law.
Any person who acts in good faith in compli-
ance with the provisions of this part is immune
from civil or criminal liability for his or her
actions in connection with the admission, diag-
nosis, treatment, or discharge of a patient to or
from a facility. However, this section does not
relieve any person from liability if such person
commits negligence.
(11) RIGHT TO PARTICIPATE IN TREAT-
MENT AND DISCHARGE PLANNING.
e patient shall have the opportunity to par-
ticipate in treatment and discharge planning
and shall be notied in writing of his or her
right, upon discharge from the facility, to seek
treatment from the professional or agency of
the patient’s choice.
(12) POSTING OF NOTICE OF RIGHTS OF
PATIENTS.
Each facility shall post a notice listing and
describing, in the language and terminology
that the persons to whom the notice is ad-
dressed can understand, the rights provided in
this section. is notice shall include a state-
ment that provisions of the federal Americans
with Disabilities Act apply and the name and
telephone number of a person to contact for
further information. is notice shall be posted
in a place readily accessible to patients and in a
format easily seen by patients. is notice shall
include the telephone numbers of the Florida
local advocacy council and Advocacy Center
for Persons with Disabilities, Inc.
Florida Local Advocacy
Council is no longer in existance.
Advocacy Center for Persons
with Disabilities is now known as
Disability Rights Florida, Inc.
(2) Any grievance may be verbal or written. When the
grievance is verbal, the facility will provide a party
not named in the dispute to assist the resident in
writing the grievance. The grievance shall detail the
issue and the remedy sought. All resident grievances
shall be addressed to the resident advocate and the
unit director or treatment team leader. The Resident
Advocacy Office shall monitor all grievances.
(3) The grievance shall be date-stamped upon receipt
by the unit director or treatment team leader. At
a minimum, the resident shall receive a written
response to the grievance within 14 calendar days
from date of receipt. The resident or the resident’s
representative may appeal the disposition of a
grievance to the facility administrator.
(4) The steps for filing a grievance as stated in this rule
shall be conspicuously posted in the living areas
where the residents can read the steps.
65E-5.602 Rights of Residents of State
Mental Health Treatment Facilities.
(1) Each state civil mental health treatment facility
shall make telephones available for residents. Any
restriction on telephone usage shall be documented
in the clinical record. Such documentation shall
specify the reason for the restriction, its duration,
and the treatment goals and interventions aimed
at lifting the restriction. At no time, shall there
be a restriction of telephone access to his or her
legal counsel, the Florida Abuse Registry, Local
or Statewide Advocacy Councils, or the Advocacy
Center for Persons with Disabilities.
(2) The Department shall protect the confidentiality of
records within the facility and in transport to other
facilities and other therapeutic services.
(3) Each state civil mental health treatment facility shall
post instructions conspicuously in living areas and
visiting areas where residents and visitors can read
the instructions on how to report a complaint.
(4) Each state civil mental health treatment facility shall
establish visiting hours for each of its residential
units. The visiting hours shall be based on the needs
of residents and their visitors and shall minimize
interruption of the individual’s treatment program

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
56
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.210 & 65E-5.602 F.A.C.
(5)
(6)
(7)
schedules. Each state civil mental health treatment
facility shall post its visiting hours in places where
residents and visitors frequent. Visiting hours
shall be provided to the resident, family, and
representatives at the time of admission. Visitors
may request exceptions to posted visiting hours
with the Unit Director or treatment team leader.
Each state civil mental health treatment facility
shall establish with the local county supervisor of
elections, a process for allowing eligible residents to
register and to vote in public elections. The process
shall be published and provided to each resident
and conspicuously posted in living areas where
residents can read it. The resident’s representative
shall also be informed of the process. The facility
shall make available voter registration forms,
applications for absentee ballots, and absentee
ballots.
No state civil mental health treatment facility shall
initiate any mental health treatment, including
psychotropic medication, until express and
informed consent for psychiatric treatment is
obtained from a person legally qualified to give it,
except in the following situations:
(a) Where emergency psychotropic medication
treatment is ordered by a physician, as defined
in Section 394.455(21), F.S., to preserve the
immediate safety of the resident or others in the
facility;
(b) When a person is admitted to a state mental
health treatment facility and has a current
prescription for psychotropic medication(s), is
unable to provide express and informed consent,
is determined by the admitting physician to be
in need of the medication prescribed prior to
admission and an alternative decision maker is
being pursued through the court; or
(c) When a Court Order is obtained after adequate
notice and hearing.
(a) Any limitation or restriction of a resident’s access
to the grounds or treatment program shall be
based on clearly documented evidence of risks to
self or others.
(b) The time span during which residents are
allowed access to the grounds shall be specified
conspicuously and posted in living areas. Access
to grounds may be limited during the hours
a resident is scheduled to attend prescribed
programming. Access to grounds status shall
Rights of patients

57 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.459 F.S.)
65E-5.602 F.A.C.
be established and documented in the clinical
record for all newly admitted persons within 72
hours of admission.
(c) An individualized plan shall be developed and
documented in the clinical record for residents
who have been identified by the treatment team
as experiencing significant loss of independent
access to grounds.
(d) Those residents certified by the facility as
experiencing long-term loss of independent
access to grounds based on physical health
issues or adaptive deficits shall be provided
opportunities to go outside unless medically
contraindicated.
(e) Any change to access to the grounds status shall
be based on the treatment team’s assessment.
An assessment of risk shall consider, at a
minimum, the following categories of risk:
1. Suicide attempts or threats,
2. Intentional self-injury,
3. Homicide,
4. Assault,
5. Elopement,
6. Substance abuse,
7. Physically vulnerable,
8. Psychotropic medication issues, and
9. Other potentially harmful behaviors.
(f) Decisions about changes in access to grounds
status shall be based in part on an assessment
of risk, with criteria influencing access changes
being documented and filed in the person-
centered record.
(g) Teams shall show progressive actions taken
to manage significant, recurring issues for
residents in the least restrictive manner possible.
The exception shall be those changes where a
resident’s access to the grounds is limited due to
serious, acute health/safety matters. Interventions
must be documented in order to show the use of
the least intrusive, most positive methods for the
restoration of freedom of movement and follow
through with treatment before the use of more
restrictive options.
(h) Residents who disagree with limitations to
grounds access shall have a right to a review of
those limitations. Each treatment facility shall
publish procedures to insure the limitations
are reviewed. The resident or the resident’s
representative may appeal the restriction to
Rights of patients

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
58
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4593 F.S.)
65E-5.602 F.A.C.
the facility administrator through the grievance
process.
(i) Residents shall retain their access to grounds
status when transferred from one residential
area to another, unless their psychological or
physical condition has changed, based on a
comprehensive risk assessment.
(j) Residents who do not have full access to the
grounds shall be provided the opportunity to
exit the building for outside time and physical
exercise on a daily basis, excluding severe
weather conditions, for at least a half-hour per
day. Residents have the right to decline to go
outside, if they so choose.
(k) All residents with full or prescribed access to
grounds (as indicated in their individualized
service plan) shall be provided with an
orientation to grounds and boundaries of the
facility.
394.4593 Sexual misconduct prohibited;
N/A
reporting required; penalties.
(1) As used in this section, the term:
(a) “Employee” includes any paid sta member,
volunteer, or intern of the department; any
person under contract with the department; and
any person providing care or support to a client
on behalf of the department or its providers.
(b)“Sexual activity” means:
1. Fondling the genital area, groin, inner
thighs, buttocks, or breasts of a person.
2. e oral, anal, or vaginal penetration by
or union with the sexual organ of another
or the anal or vaginal penetration of an-
other by any other object.
3. Intentionally touching in a lewd or lascivi-
ous manner the breasts, genitals, the genital
area, or buttocks, or the clothing covering
them, of a person, or forcing or enticing a
person to touch the perpetrator.
4. Intentionally masturbating in the pres-
ence of another person.
5. Intentionally exposing the genitals in a
lewd or lascivious manner in the presence
of another person.
Sexual misconduct

59 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4593 F.S.)
65E-5 F.A.C.
6. Intentionally committing any other
sexual act that does not involve actual
physical or sexual contact with the
victim, including, but not limited to,
sadomasochistic abuse, sexual bestial-
ity, or the simulation of any act involv-
ing sexual activity in the presence of a
victim.
(c) “Sexual misconduct” means any sexual
activity between an employee and a patient,
regardless of the consent of the patient.
e term does not include an act done for
a bona de medical purpose or an internal
search conducted in the lawful performance
of duty by an employee.
(2) An employee who engages in sexual miscon-
duct with a patient who:
(a) Is in the custody of the department; or
(b)Resides in a receiving facility or a treatment
facility, as those terms are dened in s.
394.455, commits a felony of the second
degree, punishable as provided in s.
775.082, s. 775.083, or s. 775.084. An
employee may be found guilty of violating
this subsection without having committed
the crime of sexual battery.
(3) e consent of the patient to sexual activity is
not a defense to prosecution under this section.
(4) is section does not apply to an employee who:
(a) Is legally married to the patient; or
(b)Has no reason to believe that the person
with whom the employee engaged in sexual
misconduct is a patient receiving services as
described in subsection (2).
(5) An employee who witnesses sexual misconduct,
or who otherwise knows or has reasonable
cause to suspect that a person has engaged in
sexual misconduct, shall immediately report
the incident to the department’s central abuse
hotline and to the appropriate local law en-
forcement agency. Such employee shall also
prepare, date, and sign an independent report
that specically describes the nature of the
sexual misconduct, the location and time of
the incident, and the persons involved. e
Sexual misconduct

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
60
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
employee shall deliver the report to the su-
pervisor or program director, who is respon-
sible for providing copies to the department’s
inspector general. e inspector general shall
immediately conduct an appropriate adminis-
trative investigation, and, if there is probable
cause to believe that sexual misconduct has
occurred, the inspector general shall notify
the state attorney in the circuit in which the
incident occurred.
(6) (a) Any person who is required to make a re-
port under this section and who knowingly
or willfully fails to do so, or who knowingly
or willfully prevents another person from
doing so, commits a misdemeanor of the
rst degree, punishable as provided in s.
775.082 or s. 775.083.
(b) Any person who knowingly or willfully
submits inaccurate, incomplete, or
untruthful information with respect to a
report required under this section commits a
misdemeanor of the rst degree, punishable
as provided in s. 775.082 or s. 775.083.
(c) Any person who knowingly or willfully
coerces or threatens any other person
with the intent to alter testimony or a
written report regarding an incident of
sexual misconduct commits a felony of the
third degree, punishable as provided in s.
775.082, s. 775.083, or s. 775.084.
(7) e provisions and penalties set forth in this
section are in addition to any other civil, ad-
ministrative, or criminal action provided by law
which may be applied against an employee.
394.4595 Florida statewide and local
advocacy councils; access to patients and
records.
Any facility designated by the department as a
receiving or treatment facility must allow access to
any patient and the clinical and legal records of any
patient admitted pursuant to the provisions of this
act by members of the Florida statewide and local
advocacy councils.
Local advocacy council
(Chapter 394.4595 F.S.)
65E-5 F.A.C.
N/A
Florida statewide and local
advocacy councils no longer exist
because they were de-funded by
the 2010 Florida Legislature.

61 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
394.4597 Persons to be notied; patient’s
representative.
(1) VOLUNTARY PATIENTS. At the time a
patient is voluntarily admitted to a receiving or
treatment facility, the identity and contact in-
formation of a person to be notied in case of
an emergency shall be entered in the patient’s
clinical record.
(2) INVOLUNTARY PATIENTS.
(a) At the time a patient is admitted to a facility
for involuntary examination or placement,
or when a petition for involuntary
placement is led, the names, addresses, and
telephone numbers of the patient’s guardian
or guardian advocate, or representative if the
patient has no guardian, and the patient’s
attorney shall be entered in the patient’s
clinical record.
(b) If the patient has no guardian, the patient
shall be asked to designate a representative.
If the patient is unable or unwilling to
designate a representative, the facility shall
select a representative.
(c) e patient shall be consulted with regard
to the selection of a representative by the
receiving or treatment facility and shall
have authority to request that any such
representative be replaced.
(d) When the receiving or treatment facility
selects a representative, rst preference shall
be given to a health care surrogate, if one
has been previously selected by the patient.
If the patient has not previously selected a
health care surrogate, the selection, except
for good cause documented in the patient’s
clinical record, shall be made from the
following list in the order of listing:
1. e patient’s spouse.
2. An adult child of the patient.
3. A parent of the patient.
4. e adult next of kin of the patient.
5. An adult friend of the patient.
6. e appropriate Florida local advocacy
council as provided in s. 402.166.
Persons to be notified
(Chapter 394.4597 F.S.)
65E-5 F.A.C.
N/A
All adults on involuntary status
must have a representative
designated unless a guardian has
been appointed by the court.
This list is not part of this section of the rule. It is
taken from multiple sections of the statute/rule and
compiled here as one list because it is relevant to the
content of this part of the statutes/rules.
Role of Designated Representative
• Receive notice of individual's admission
• Have immediate access to the individual unless
documented to be detrimental
• Receive notice of any restriction of right to
communicate or receive visitors
• Receive written notice of any restriction of the
individual's right to inspect his or her clinical
record
• Petition on behalf of the individual for a writ of
habeas corpus
• Receive copy of the inventory of personal
effects
• Receive notice of proceedings
• Receive copy of petition for the individual's
involuntary placement filed with the court
• Apply for change of venue for the involuntary
placement hearing for the convenience of the
parties or the individual's condition
• Be informed by the court of the individual's
right to an independent expert evaluation
• Receive notice of individual's release from a
receiving facility
• Receive disposition of the individual's clothing
and personal effects, if not returned to the
individual

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
62
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4598 F.S.)
65E-5.230 F.A.C.
(e) A licensed professional providing
services to the patient under this part, an
employee of a facility providing direct
services to the patient under this part, a
department employee, a person providing
other substantial services to the patient
in a professional or business capacity,
or a creditor of the patient shall not be
appointed as the patient’s representative.
394.4598 Guardian advocate.
(1) e administrator may petition the court for
the appointment of a guardian advocate based
upon the opinion of a psychiatrist that the pa-
tient is incompetent to consent to treatment.
If the court nds that a patient is incompetent
to consent to treatment and has not been adju-
dicated incapacitated and a guardian with the
authority to consent to mental health treat-
ment appointed, it shall appoint a guardian
advocate. e patient has the right to have an
attorney represent him or her at the hearing. If
the person is indigent, the court shall appoint
the oce of the public defender to represent
him or her at the hearing. e patient has the
right to testify, cross-examine witnesses, and
present witnesses. e proceeding shall be
recorded either electronically or stenographi-
cally, and testimony shall be provided under
oath. One of the professionals authorized
to give an opinion in support of a petition
for involuntary placement, as described in s.
394.4655 or s. 394.467, must testify. A guard-
ian advocate must meet the qualications of
a guardian contained in part IV of chapter
744, except that a professional referred to in
this part, an employee of the facility providing
direct services to the patient under this part, a
departmental employee, a facility administra-
tor, or member of the Florida local advocacy
council shall not be appointed. A person who
is appointed as a guardian advocate must agree
to the appointment.
65E-5.230 Guardian Advocate.
(1) A copy of the completed recommended form CF-MH
3106, “Petition for Adjudication of Incompetence
to Consent to Treatment and Appointment of a
Guardian Advocate,” as referenced in subparagraph
65E-5.170(1)(d)2., F.A.C., or its equivalent, shall be
given to the person, the person’s representative if
any, and to the prospective guardian advocate with a
copy retained in the person’s clinical record.
(2) The person’s clinical record shall reflect that the
guardian advocate has been appointed by the
court and has completed the training required
by Section 394.4598(4), F.S., and further training
required pursuant to a court order, prior to being
asked to provide express and informed consent to
treatment. Recommended form CF-MH 3120, Feb.
05, “Certification of Guardian Advocate Training
Completion,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose.
(3) When a guardian advocate previously appointed
by the court cannot or will not continue to serve in
that capacity, and the person remains incompetent
to consent to treatment, the facility administrator
shall petition the court for a replacement guardian
advocate. A copy of the completed petition shall
be given to the person, the current guardian
advocate, the prospective replacement guardian
advocate, person’s attorney, and representative,
with a copy retained in the person’s clinical record.
Recommended form CF-MH 3106, “Petition for
Adjudication of Incompetence to Consent to
Treatment and Appointment of a Guardian Advocate,”
as referenced in subparagraph 65E-5.170(1)(d)2.,
F.A.C., may be used for this documentation if Parts I
and III are completed.
Gardian advocate

63 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4598 F.S.)
65E-5.230 F.A.C.
(2) A facility requesting appointment of a guard-
ian advocate must, prior to the appointment,
provide the prospective guardian advocate with
information about the duties and responsi-
bilities of guardian advocates, including the
information about the ethics of medical deci-
sionmaking. Before asking a guardian advocate
to give consent to treatment for a patient, the
facility shall provide to the guardian advocate
sucient information so that the guardian ad-
vocate can decide whether to give express and
informed consent to the treatment, including
information that the treatment is essential to
the care of the patient, and that the treatment
does not present an unreasonable risk of seri-
ous, hazardous, or irreversible side eects. Be-
fore giving consent to treatment, the guardian
advocate must meet and talk with the patient
and the patient’s physician in person, if at all
possible, and by telephone, if not. e decision
of the guardian advocate may be reviewed by
the court, upon petition of the patient’s attor-
ney, the patient’s family, or the facility adminis-
trator.
(3) Prior to a guardian advocate exercising his or
her authority, the guardian advocate shall at-
tend a training course approved by the court.
is training course, of not less than 4 hours,
must include, at minimum, information about
the patient rights, psychotropic medications,
diagnosis of mental illness, the ethics of medi-
cal decisionmaking, and duties of guardian
advocates. is training course shall take the
place of the training required for guardians ap-
pointed pursuant to chapter 744.
(4) e information to be supplied to prospective
guardian advocates prior to their appointment
and the training course for guardian advocates
must be developed and completed through a
course developed by the department and ap-
proved by the chief judge of the circuit court
and taught by a court-approved organization.
Court-approved organizations may include, but
are not limited to, community or junior col-
leges, guardianship organizations, and the local
Gardian advocate
(4) If the court finds the person incompetent to
consent to treatment a guardian advocate shall be
appointed. Recommended form CF-MH 3107, Feb.
05, “Order Appointing Guardian Advocate,” which
is incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, or other order used by the court, may be
used for documentation of this finding. The order
shall be provided to the person, guardian advocate,
representative, and to the facility administrator for
retention in the person’s clinical record.
(5) If a guardian advocate is required by Section
394.4598, F.S., or otherwise to petition the court for
authority to consent to extraordinary treatment, a
copy of the completed petition form shall be given
to the person, a copy to the attorney representing
the person, and a copy retained in the person’s
clinical record. Recommended form CF-MH 3108,
Feb. 05, “Petition Requesting Court Approval for
Guardian Advocate to Consent to Extraordinary
Treatment,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose.
Any order issued by the court in response to such
a petition shall be given to the person, attorney
representing the person, guardian advocate, and
to the facility administrator, with a copy retained
in the person’s clinical record. Recommended form
CF-MH 3109, Feb. 05, “Order Authorizing Guardian
Advocate to Consent to Extraordinary Treatment,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
rule chapter, or other order used by the court may
be used for such documentation.
(6) At any time a person, who has previously been
determined to be incompetent to consent to
treatment and had a guardian advocate appointed
by the court, has been found by the attending
physician to have regained competency to consent
to treatment, the facility shall notify the court that
appointed the guardian advocate of the patient’s
competence and the discharge of the guardian
advocate. Recommended form CF-MH 3121, Feb.
05, “Notification to Court of Person’s Competence
to Consent to Treatment and Discharge of Guardian
Advocate,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
64
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4598 F.S.)
65E-5.2301 F.A.C.
bar association or e Florida Bar. e court
may, in its discretion, waive some or all of the
training requirements for guardian advocates or
impose additional requirements. e court shall
make its decision on a case-by-case basis and, in
making its decision, shall consider the experi-
ence and education of the guardian advocate,
the duties assigned to the guardian advocate,
and the needs of the patient.
(5) In selecting a guardian advocate, the court
shall give preference to a health care surrogate,
if one has already been designated by the pa-
tient. If the patient has not previously selected
a health care surrogate, except for good cause
documented in the court record, the selection
shall be made from the following list in the
order of listing:
(a) e patient’s spouse.
(b)An adult child of the patient.
(c) A parent of the patient.
(d)e adult next of kin of the patient.
(e) An adult friend of the patient.
(f) An adult trained and willing to serve as
guardian advocate for the patient.
(6) If a guardian with the authority to consent
to medical treatment has not already been
appointed or if the patient has not already
designated a health care surrogate, the court
may authorize the guardian advocate to con-
sent to medical treatment, as well as mental
health treatment. Unless otherwise limited by
the court, a guardian advocate with authority
to consent to medical treatment shall have the
same authority to make health care decisions
and be subject to the same restrictions as a
proxy appointed under part IV of chapter 765.
Unless the guardian advocate has sought and
received express court approval in proceeding
separate from the proceeding to determine the
competence of the patient to consent to medi-
cal treatment, the guardian advocate may not
consent to:
(a) Abortion.
(b)Sterilization.
(c) Electroconvulsive treatment.
65E-5.2301 Health Care Surrogate or Proxy.
(1) During the interim period between the time a
person is determined to be incompetent to consent
to treatment by one or more physicians, pursuant
to Section 765.204, F.S., and the time a guardian
advocate is appointed by a court to provide express
and informed consent to the person’s treatment,
a health care surrogate designated by the person,
pursuant to Chapter 765, Part II, F.S., may provide
such consent to treatment.
(2) In the absence of an advance directive or when
the health care surrogate named in the advance
directive is no longer able or willing to serve, a
health care proxy, pursuant to Chapter 765, Part IV,
F.S., may also provide interim consent to treatment.
(3) Upon the documented determination that a
patient is incompetent to make health care
decisions for himself or herself by one or more
physicians, pursuant to Section 765.204, F.S.,
the facility shall notify the surrogate or proxy in
writing that the conditions under which he or she
can exercise his or her authority under the law
have occurred. Recommended form CF-MH 3122,
Feb. 05, “Certification of Person’s Incompetence to
Consent to Treatment and Notification of Health
Care Surrogate/Proxy,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter may be used
for this purpose.
(4) If the surrogate selected by the person is not
available or is unable to serve or if no advance
directive had been prepared by the person, a
proxy may be designated as provided by law.
Recommended form CF-MH 3123, Feb. 05, “Affidavit
of Proxy,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this purpose.
(5) A petition for adjudication of incompetence
to consent to treatment and appointment of a
guardian advocate shall be filed with the court
within 2 court working days of the determination
of the patient’s incompetence to consent to
treatment by one or more physicians, pursuant to
Section 765.204, F.S. Recommended form CF-MH
3106, “Petition for Adjudication of Incompetence
to Consent to Treatment and Appointment of a
Guardian Advocate,” as referenced in subparagraph
65E-5.170(1)(d)2., F.A.C., may be used for this
purpose.
Gardian advocate

65 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(d) Psychosurgery.
(e) Experimental treatments that have not been
approved by a federally approved institutional
review board in accordance with 45 C.F.R.
part 46 or 21 C.F.R. part 56.
e court must base its decision on evidence
that the treatment or procedure is essential to
the care of the patient and that the treatment
does not present an unreasonable risk of seri-
ous, hazardous, or irreversible side eects. e
court shall follow the procedures set forth in
subsection (1) of this section.
(7) e guardian advocate shall be discharged
when the patient is discharged from an or-
der for involuntary outpatient placement or
involuntary inpatient placement or when
the patient is transferred from involuntary to
voluntary status. e court or a hearing ocer
shall consider the competence of the patient
pursuant to subsection (1) and may consider
an involuntarily placed patient’s competence to
consent to treatment at any hearing. Upon suf-
cient evidence, the court may restore, or the
hearing ocer may recommend that the court
restore, the patient’s competence. A copy of the
order restoring competence or the certicate of
discharge containing the restoration of compe-
tence shall be provided to the patient and the
guardian advocate.
394.4599 Notice.
(1) VOLUNTARY PATIENTS.
Notice of a voluntary patient’s admission shall
only be given at the request of the patient, ex-
cept that in an emergency, notice shall be given
as determined by the facility.
(2) INVOLUNTARY PATIENTS.
(a) Whenever notice is required to be given
under this part, such notice shall be
given to the patient and the patient’s
guardian, guardian advocate, attorney, and
representative.
Notice
(Chapter 394.4599 F.S.)
65E-5.2301 F.A.C.
See Appendix C-4 for summary
reference on Substitute
Decision-making including
surrogates and proxies
(6) The facility shall immediately provide to the health
care surrogate or proxy the same information
required by statute to be provided to the guardian
advocate. In order to protect the safety of the
person, the facility shall make available to the health
care surrogate or proxy the training required of
guardian advocates and ensure that the surrogate
or proxy communicate with the person and person’s
physician prior to giving express and informed
consent to treatment.
(7) Each designated receiving and treatment facility
shall adopt policies and procedures specifying how
its direct care and assessment staff will be trained on
how to honor each person’s treatment preferences
as detailed in his or her advance directives. The
person being served shall be provided information
about advance directives and offered assistance in
completing an advance directive, if willing and able
to do so.
N/A

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
66
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
1. When notice is required to be given to a
patient, it shall be given both orally and
in writing, in the language and termi-
nology that the patient can understand,
and, if needed, the facility shall provide
an interpreter for the patient.
2. Notice to a patient’s guardian, guardian
advocate, attorney, and representative
shall be given by United States mail and
by registered or certied mail with the
receipts attached to the patient’s clini-
cal record. Hand delivery by a facility
employee may be used as an alternative,
with delivery documented in the clini-
cal record. If notice is given by a state
attorney or an attorney for the depart-
ment, a certicate of service shall be
sucient to document service.
(b) A receiving facility shall give prompt notice
of the whereabouts of a patient who is
being involuntarily held for examination,
by telephone or in person within 24 hours
after the patient’s arrival at the facility, unless
the patient requests that no notication
be made. Contact attempts shall be
documented in the patient’s clinical record
and shall begin as soon as reasonably possible
after the patient’s arrival. Notice that a
patient is being admitted as an involuntary
patient shall be given to the Florida local
advocacy council no later than the next
working day after the patient is admitted.
(c) e written notice of the ling of the
petition for involuntary placement must
contain the following:
1. Notice that the petition has been led
with the circuit court in the county in
which the patient is hospitalized and
the address of such court.
2. Notice that the oce of the public
defender has been appointed to
represent the patient in the proceeding,
if the patient is not otherwise
represented by counsel.
Notice
(Chapter 394.4598 F.S.)
65E-5 F.A.C.
Representatives must be
notied of involuntary admissions
unless person objects. No other
notices to representatives
can be waived.
Guardian must be notied
of all involuntary admissions -
cannot be waived.
Florida statewide and local
advocacy councils no longer exist
because they were de-funded by
the 2010 Florida Legislature.

67 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
3. e date, time, and place of the hearing
and the name of each examining expert
and every other person expected to tes-
tify in support of continued detention.
4. Notice that the patient, the patient’s
guardian or representative, or the ad-
ministrator may apply for a change of
venue for the convenience of the parties
or witnesses or because of the condition
of the patient.
5. Notice that the patient is entitled to an
independent expert examination and,
if the patient cannot aord such an
examination, that the court will provide
for one.
(d)A treatment facility shall provide notice of
a patient’s involuntary admission on the
next regular working day after the patient’s
arrival at the facility.
(e) When a patient is to be transferred from
one facility to another, notice shall be given
by the facility where the patient is located
prior to the transfer.
394.460 Rights of professionals.
No professional referred to in this part shall
be required to accept patients for treatment of
mental, emotional, or behavioral disorders. Such
participation shall be voluntary.
394.461 Designation of receiving and
treatment facilities.
e department is authorized to designate and
monitor receiving facilities and treatment facilities
and may suspend or withdraw such designation
for failure to comply with this part and rules
adopted under this part. Unless designated by the
department, facilities are not permitted to hold or
treat involuntary patients under this part.
(1) RECEIVING FACILITY. e department
may designate any community facility as a
receiving facility. Any other facility within the
Designation of facilities
Professionals employed by,
under contract with, or having privileges
at any hospital or receiving facility must
comply with any state/federal laws and
rules governing those facilities.
N/A
65E-5.350 Eligibility Criteria and
Procedures for Designation of Baker Act
Receiving Facilities.
(1) General Provisions. Pursuant to Sections
394.455(26) and 394.461, F.S., only facilities
designated by the department are permitted to
involuntarily hold and treat persons for a mental
illness, except as required by 42 USC 1395 for all
hospitals providing emergency services for access,
assessment, stabilization and transfer.
(2) Designation as a private receiving or treatment
facility shall not entitle the facility to receive any

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
68
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
state, including a private facility or a federal fa-
cility, may be so designated by the department,
provided that such designation is agreed to by
the governing body or authority of the facility.
(2) TREATMENT FACILITY. e department may
designate any state-owned, state-operated, or
state-supported facility as a state treatment facil-
ity. A civil patient shall not be admitted to a state
treatment facility without previously undergoing
a transfer evaluation. Before a court hearing for
involuntary placement in a state treatment facility,
the court shall receive and consider the informa-
tion documented in the transfer evaluation. Any
other facility, including a private facility or a feder-
al facility, may be designated as a treatment facility
by the department, provided that such designation
is agreed to by the appropriate governing body or
authority of the facility.
(3) PRIVATE FACILITIES. Private facilities des-
ignated as receiving and treatment facilities by
the department may provide examination and
treatment of involuntary patients, as well as vol-
untary patients, and are subject to all the provi-
sions of this part.
(4) (a) A facility designated as a public receiving
or treatment facility under this section shall
report to the department on an annual basis
the following data, unless these data are
currently being submitted to the Agency for
Health Care Administration:
1. Number of licensed beds.
2. Number of contract days.
3. Number of admissions by payor class and
diagnoses.
4. Number of bed days by payor class.
5. Average length of stay by payor class.
6. Total revenues by payor class.
(b) For the purposes of this subsection, “payor
class” means Medicare, Medicare HMO,
Medicaid, Medicaid HMO, private-pay health
insurance, private-pay health maintenance
organization, private preferred provider
organization, the Department of Children and
Family Services, other government programs,
self-pay patients, and charity care.
funding appropriated for the Baker Act. Such
funding is based solely on a contract between the
department and the facility, specifically for this
purpose.
(3) Two types of licensed civil facilities are authorized to
provide acute psychiatric treatment and are eligible
to apply for designation as receiving facilities. Since
designation to receive persons under Chapter
394, Part I, F.S., does not distinguish between the
capacity to serve adults and minors, all designated
facilities are required to provide emergency services,
consistent with their facility’s licensure to persons
regardless of age, except as provided for under
subsection (4) of this rule.
(a) Hospitals licensed under the authority of Chapter
395, F.S., to provide psychiatric care may be
designated as either public or private receiving
facilities.
(b) Facilities licensed under the provisions of
Chapter 394, Part IV, F.S., shall only be designated
as public receiving facilities and may include
only crisis stabilization units (CSU) and children’s
crisis stabilization units (CCSU). Short-term
residential treatment facilities (SRT ) are not free-
standing emergency care units and may only be
designated collectively with a CSU or CCSU as
part of a public receiving facility.
(4) Specific Circumstances for Designation.
Pursuant to the exceptions authorized under
Section 394.462(3), F.S., for transportation purposes,
and at the discretion of the department’s district
or regional office with the approval of the mental
health and substance abuse program supervisor, a
facility designation may be modified or restricted
to specify services for just adults or for just children,
consistent with its license and subject to inclusion
and subsequent approval by required parties as part
of an approved transportation exemption plan.
(5) Application and Supporting Documentation
for Designation. In order to apply for designation
as a receiving facility, an applicant must complete
and submit mandatory form CF-MH 3125, Feb. 05,
“Application for Designation as a Receiving Facility,”
which is hereby incorporated by reference and may
be obtained in accordance with Rule 65E-5.120,
F.A.C., of this rule chapter. Required application
information includes:
(a) A copy of the facility’s license issued pursuant to
Chapter 394 or 395, F.S., evidencing its eligibility
Designation of facilities

69 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
(c) e data required under this subsection
shall be submitted to the department no
later than 90 days following the end of the
facility’s scal year. A facility designated as
a public receiving or treatment facility shall
submit its initial report for the 6-month
period ending June 30, 2008.
(d)e department shall issue an annual report
based on the data required pursuant to
this subsection. e report shall include
individual facilities’ data, as well as statewide
totals. e report shall be submitted to the
Governor, the President of the Senate, and
the Speaker of the House of Representatives.
(5) RULES. e department shall adopt rules
relating to:
(a) Procedures and criteria for receiving
and evaluating facility applications for
designation, which may include onsite
facility inspection and evaluation of an
applicant’s licensing status and performance
history, as well as consideration of local
service needs.
(b)Minimum standards consistent with this
part that a facility must meet and maintain
in order to be designated as a receiving
or treatment facility and procedures for
monitoring continued adherence to such
standards.
(c) Procedures for receiving complaints against
a designated facility and for initiating
inspections and investigations of facilities
alleged to have violated the provisions of
this part or rules adopted under this part.
(d)Procedures and criteria for the suspension or
withdrawal of designation.
Designation of facilities
to apply for designation;
(b) A current certificate of good standing for the
applicant organization issued by the Florida
Secretary of State;
(c) Documentation of the applicant’s governing
authority action authorizing the application for
designation;
(d) Description of proposed psychiatric services
including any distinct programs to be provided
to each of the following consumer age groups,
and the projected numbers of persons to be
served in each following group:
1. Minors below 10 years of age;
2. Minors between the ages of 10 to 17 years;
3. Adults;
4. Persons 60 or more years of age; and
5. Other specific populations.
(e) The corresponding street address for each
reception and treatment location for the above
services must be provided. Designation is limited
to only the locations specified in the application
and approved by the department; and
(f) Documentation of community need for
maintaining or expanding the present level of
designated facilities’ services to meet the existing
need, and why the applicant is best suited to
meet this need.
1. The information may address the public’s
need for specific services for minors, aged,
blind or hearing-impaired persons. Evidence
of such need may include: Certificate
of Need data and other information
published by the Agency for Health
Care Administration, the organization’s
or community’s utilization of available
or licensed bed capacity, geographical
accessibility information, input from local
governmental agencies, or information on
the specific needs of persons if the particular
specialty services offered are accredited or
certified by a nationally recognized body for
that specific population or service.
2. The applicant shall describe local need
and accommodation of that need for
indigent and low income individuals and
families receiving the facility’s services.
The applicant shall describe how it shall
protect economically vulnerable persons
received for involuntary examination or

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
70
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
(6)
treatment from exorbitant charges and
billings for services. A statement comparing
representative facility charges and billings
for individuals who are uninsured or without
a third party payer who are held under the
provisions of the Baker Act to otherwise
similar representative charges and billings
for group health care members and insurers
shall be included.
3. The applicant shall describe local need and
accommodation of that need for indigent
and low income individuals and families
being discharged from the facility in need
of continuing psychotropic medications.
The applicant shall describe how it shall
directly provide, or otherwise assist the
person in ensuring continuity of availability
of necessary psychotropic medications
until a scheduled aftercare psychotropic
medication appointment.
(g) Documentation of key facility protocols to
assure all involved practitioners and staff are
knowledgeable of, and implement, person’s
legal rights, key psychiatric care, records
standards, complaint reporting, investigation
and reviews to maintain a consistently high level
of compliance with applicable Baker Act laws,
ethical principles, and rights protections;
(h) Description of how the facility’s physical
structure, staffing and policies offers frequent,
if not daily, opportunity for persons to have
exercise, fresh air and sunshine, except as
individually restricted and documented in the
person’s clinical record and within the physical
limitations of the facility;
(i) Description of how the facility’s discharge
planning policies provide for continuity of
psychotropic medication availability until post-
discharge follow-up services are scheduled; and
(j) For general hospitals, a description of the means
utilized to create or approximate a distinct
psychiatric emergency reception and triage area
that minimizes individual’s exposure to undue
and exacerbating environmental stresses while
awaiting or receiving services.
Application Process for Designation. All
facilities desiring to obtain, or to retain, designation
as a receiving facility must complete and submit
mandatory form CF-MH 3125, “Application for
Designation of facilities

71 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Designation of facilities
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
Designation as a Receiving Facility,” as referenced
in subsection 65E-5.350(5), F.A.C., for departmental
review. All receiving facility designations shall be
subject to departmental review and authorization
in accordance with the provisions of Chapter 394,
Part I, F.S., and this chapter after receipt of the
application.
(a) The department’s district or regional office
is responsible for receipt of the application,
reviewing the application, requesting additional
information as needed, verifying essential
information, and forwarding the information
along with the recommendation of the mental
health and substance abuse program supervisor
to the Secretary for final action. Applications
received that are incomplete will be returned
by certified mail with a letter informing the
applicant of missing items. The district or region
will seek and review pertinent information from
any source such as:
1. Accreditation status and submission of
the latest survey report of any applicable
accrediting bodies;
2. Relevant history of compliance with the
Baker Act and other related protection laws
protecting persons served by mental health
facilities;
3. Agency for Health Care Administration
(AHCA) licensure reports and complaint
investigation findings against the facility or
professionals associated with the facility;
4. Actions, findings or reports of the Florida
Local Advocacy Council, and other district or
regional consumer complaint offices;
5. Florida Abuse Hotline receipt, or lack or
receipt, of complaints and actions;
6. Actions initiated by any state enforcement
authority including the Florida Attorney
General’s Office, the Florida Department of
Law Enforcement, the Florida Department
of Insurance, and statewide or local State’s
Attorneys Offices; and
7. Actions initiated by any federal law
enforcement or investigative authority
including the federal Department of Health
and Human Services, the federal Centers for
Medicare and Medicaid Services, and the
Federal Bureau of Investigation against the
facility, its employees, privileged personnel
Florida statewide and local
advocacy councils no longer exist
because they were de-funded by
the 2010 Florida Legislature.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
72
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.350 F.A.C.
(7)
or contractors, subcontractors, or operators
relating to services, billings or operations.
(b) The district or region, upon receipt of a properly
completed application, shall schedule and
advertise a public meeting for purposes of
obtaining public input and information on the
initial designation of the applicant.
(c) In meeting the local need for designated
facilities, priority shall be given to facilities with
management that consistently exhibits high
levels of compliance with Chapter 394, Part I,
F.S., this rule chapter, and related protection
laws in Chapters 395, 415, 458, and 817, F.S., as
documented in state agencies’ files.
(d) The submission of the district or region’s
recommendation to the Secretary must
include a listing of the key information sources
and pertinent factors relied upon in making
the recommendation and a summary of the
comments and information received at the
public meeting.
(e) Within 60 days of receiving the recommendation
from the district or region, the Secretary, or the
Secretary’s designee, will review the district
or region recommendation and supporting
documentation and will issue final departmental
action with regard to the application which
may be approved, denied, or returned to the
district or region for additional information or
processing.
(f) The designation shall be for 3 years.
Re-Applications for Renewal of Designation.
(a) A re-application must be submitted for re-
designation every 3 calendar years, after
approval of initial applications or 90 days in
advance of the relocation of a facility to a new
address. The designation is valid only for the
address to which it was issued.
(b) A renewal application shall be forwarded to
the department at least 90 days prior to the
expiration of its existing designation.
(c) A re-application must be submitted by a facility
upon a change of controlling ownership of
the facility or of the contractual management
entity for the psychiatric service. Failure to
submit notification to the department of
changes of controlling ownership or a change
in the management entity within 30 days
Designation of facilities

73 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.461 F.S.)
65E-5.351 F.A.C.
after the change will terminate the facility’s
designation 60 days after the effective date of
the action changing the control of ownership or
management.
(d) Any change in the name of a facility, that remains
under the same ownership and management,
must be reported in writing to the department’s
district or regional office within 30 days after
the effective date of the change. Upon receipt
of the notification, the department will issue
a letter confirming receipt of the notification
and extending designation until a replacement
certificate of designation showing the correct
facility name is received by the facility. Failure
to provide such notification to the district or
region within 30 days of the change will result
in the withdrawal of the designation upon the
expiration of the 60th day following the facility
name change.
(8) Certificate of Designation.
(a) Upon approval by the Secretary or his or her
designee, the department shall issue a certificate
of designation which shall include the following
information on the face of the Certificate of
Designation:
1. Effective commencement date and
expiration date;
2. Name of the owner and licensee as stated on
the facility license issued by the Agency for
Health Care Administration; and
3. Street address of where services are
provided.
(b) The certificate shall be prominently displayed to
the general public at the service site. Designation
provided by this certificate is invalid if the
information on the certificate is not correct
or the information provided in the submitted
application is false or misleading.
65E-5.351 Minimum Standards for
Designated Receiving Facilities.
(1) Any facility designated as a receiving facility
failing to comply with this chapter may have such
designation suspended or withdrawn.
(2) Each receiving facility shall have policies and
procedures that prescribe, monitor and enforce all
requirements specified in Chapter 65E-5, F.A.C.
Designation of facilities

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
74
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
Designation of facilities
(3) Each receiving facility shall assure that its reception,
screening, and inpatient services are fully
operational 24-hours-per-day, 7-days-per-week.
(4) Each receiving facility shall have a compliance
program that monitors facility and professional
compliance with Chapter 394, Part I, F.S., and this
chapter. Every such program shall specifically
monitor the adequacy of and the timeframes
involved in the facility procedures utilized to
expedite obtaining informed consent for treatment.
This program may be integrated with other
activities.
(5) A public receiving facility that is affiliated with
a publicly funded community mental health
center shall ensure the centralized provision and
coordination of acute care services for eligible
individuals with an acute mental illness.
65E-5.352 Procedures for Complaints and
Investigations in Receiving Facilities.
Complaints with regard to the provisions of this chapter
shall be filed with the district or region mental health
and substance abuse program supervisor, or designee,
of the district or region in which the violation is alleged
to have occurred. The district or region mental health
and substance abuse program supervisor shall appoint
one or more employees to determine if an investigation
is warranted. If warranted, the investigation may include
the assistance of other agencies having jurisdiction over
the facility. If the district or region mental health and
substance abuse program supervisor determines that a
violation of this chapter has occurred:
(1) Corrective action shall be required and a reasonable
time in which to correct the violation shall be
accorded to the facility; or
(2) If the corrective action is not sufficient, or the
district or region mental health and substance
abuse program supervisor determines that the
violation warrants suspension or removal of
designation, such action shall be considered
pursuant to Rule 65E-5.353, F.A.C.
(Chapter 394 F.S.)
65E-5.352 F.A.C.
Public Receiving Facilities must
ensure centralized coordination of
acute care services.
See 65E-5.180(6), FAC
for additional complaint
investigation procedures.

75 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Designation of facilities
65E-5.353 Criteria and Procedures for
Suspension or Withdrawal of Designation
of Receiving Facilities.
(1) The district or regional offices of the department
shall continuously collect and monitor information
relative to complaints or allegations against
designated facilities from sources such as
individuals, local advocacy or self-help groups,
local organizations including law enforcement, the
Agency for Health Care Administration, and the
Florida Local Advocacy Council. When a district or
region mental health and substance abuse program
supervisor recommends to the Secretary, or the
Secretary’s designee, withdrawal or suspension of
designation, at least the following information must
be submitted with the recommendation:
(a) Description of violations such as extent of
violations of Chapter 394, F.S., and this rule
chapter, and the extent and seriousness of
known injuries or injury including the severity
and number of violations, severity and chronic
violation of rights, and any pattern of inadequate
supervision, injury or harm to individuals; and
(b) Mitigating circumstances including the
responsiveness and extent of any actions taken
by the facility to remediate, compensate, or
correct the situation, as well as the facility’s
recent history of charitable public service to
persons with psychiatric disabilities in the
community, and compliance and responsiveness
to any prior violations or complaints.
(2) Suspension of Designation. When the district
or region determines that it is more likely than not
that a facility, or its related entities, has failed to
consistently meet one or more of the standards for
designation or maintenance of designation under
this chapter, it may suspend designation pending
corrective action plan implementation. During the
suspension period, no persons on involuntary status
may be admitted to the facility. No re-application
for designation as a receiving facility is required for
reinstatement of designation.
(3) Withdrawal of Designation.
(a) Designation may be withdrawn upon approval
of the Secretary, or the Secretary’s designee,
when the district or region determines that
it is more likely than not that any pattern of
violations, or combination of violations, of
(Chapter 394 F.S.)
65E-5.353 F.A.C.
Florida statewide and local
advocacy councils no longer exist
because they were de-funded by
the 2010 Florida Legislature.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
76
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4612 F.S.)
65E-5.353 F.A.C.
394.4612 Integrated adult mental
health crisis stabilization and addictions
receiving facilities.
(1) e Agency for Health Care Administration, in
consultation with the Department of Children
and Family Services, may license facilities that
integrate services provided in an adult men-
tal health crisis stabilization unit with services
provided in an adult addictions receiving facility.
Such a facility shall be licensed by the agency as
an adult crisis stabilization unit under part IV
and must meet all licensure requirements for
crisis stabilization units providing integrated
services.
(2) An integrated mental health crisis stabilization
unit and addictions receiving facility may pro-
vide services under this section to adults who
are 18 years of age or older and who fall into
one or more of the following categories:
(a) An adult meeting the requirements for
voluntary admission for mental health
treatment under s. 394.4625.
Chapter 394, F.S., this rule chapter, and Chapter
65E-12, F.A.C., exists such as deficient admission,
transfer or care practices, deficient observation
or documentation of rights abuses, deficient
discharge practices, deceptive or misleading
practices in marketing, admission recruitment
or referral practices; fraudulent clinical or
billing practices; or patient brokering is evident.
Examples of such offenses include violations
by the facility, or parties acting on behalf of
or in concert with the facility, or acting under
its supervision, having engaged in deceptive,
fraudulent, exploitative, abusive, or neglect type
violations of Florida law, including Chapters 394
and 415, F.S., Sections 817.505 and 458.331, F.S.
(b) Upon re-application after withdrawal of
designation, the department must have clear
and convincing evidence that the problems
with the facility, or its practitioners, leading to
withdrawal of designation have been corrected
and will not reoccur. This may include required
internal and external monitoring to document
continued satisfactory performance.
N/A
Designation of facilities

77 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4615 F.S.)
65E-5.250 F.A.C.
(b)An adult meeting the criteria for
involuntary examination for mental illness
under s. 394.463.
(c) An adult qualifying for voluntary admission
for substance abuse treatment under s.
397.601.
(d)An adult meeting the criteria for
involuntary admission for substance abuse
impairment under s. 397.675.
(3) e department, in consultation with the agen-
cy, shall adopt by rule standards that address
eligibility criteria; clinical procedures; stang
requirements; operational, administrative, and
nancing requirements; and the investigation
of complaints.
394.4615 Clinical records; condentiality.
(1) A clinical record shall be maintained for each
patient. e record shall include data pertain-
ing to admission and such other information as
may be required under rules of the department.
A clinical record is condential and exempt
from the provisions of s. 119.07(1). Unless
waived by express and informed consent, by
the patient or the patient’s guardian or guard-
ian advocate or, if the patient is deceased, by
the patient’s personal representative or the
family member who stands next in line of
intestate succession, the condential status of
the clinical record shall not be lost by either
authorized or unauthorized disclosure to any
person, organization, or agency.
(2) e clinical record shall be released when:
(a) e patient or the patient’s guardian authorizes
the release. e guardian or guardian advocate
shall be provided access to the appropriate
clinical records of the patient. e patient or
the patient’s guardian or guardian advocate
may authorize the release of information and
clinical records to appropriate persons to
ensure the continuity of the patient’s health
care or mental health care.
Clinical records; confidentiality
65E-5.250 Clinical Records; Confidentiality.
(1) Except as otherwise provided by law, verbal or
written information about a person shall only be
released when the competent person, or a duly
authorized legal decision-maker such as guardian,
guardian advocate, or health care surrogate or
proxy provides consent to such release. When
such information is released, a copy of a signed
authorization form shall be retained in the person’s
clinical record. Recommended form CF-MH 3044,
Feb. 05, “Authorization for Release of Information,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of
this rule chapter may be used as documentation.
Consent or authorization forms may not be altered
in any way after signature by the person or other
authorized decision-maker nor may a person or
other authorized decision-maker be allowed to sign
a blank form.
(2) Facility staff shall inform each person that he
or she has the right to waive, in writing, the
confidentiality of his or her presence in a receiving
or treatment facility and to communicate with
all or a group of individuals as specified by the
person. Recommended form CF-MH 3048, Feb.
05, “Confidentiality Agreement,” as referenced in
subsection 65E-5.190(1), F.A.C., may be used for
this purpose.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
78
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4615 F.S.)
65E-5.250 F.A.C.
(b)e patient is represented by counsel and
the records are needed by the patient’s
counsel for adequate representation.
(c) e court orders such release. In
determining whether there is good cause for
disclosure, the court shall weigh the need
for the information to be disclosed against
the possible harm of disclosure to the
person to whom such information pertains.
(d)e patient is committed to, or is to be
returned to, the Department of Corrections
from the Department of Children and
Family Services, and the Department of
Corrections requests such records. ese
records shall be furnished without charge to
the Department of Corrections.
(3) Information from the clinical record may be
released in the following circumstances:
(a) When a patient has declared an intention to
harm other persons. When such declaration
has been made, the administrator may
authorize the release of sucient information
to provide adequate warning to the person
threatened with harm by the patient.
(b)When the administrator of the facility or
secretary of the department deems release
to a qualied researcher as dened in
administrative rule, an aftercare treatment
provider, or an employee or agent of the
department is necessary for treatment of the
patient, maintenance of adequate records,
compilation of treatment data, aftercare
planning, or evaluation of programs.
For the purpose of determining whether a
person meets the criteria for involuntary
outpatient placement or for preparing the
proposed treatment plan pursuant to s.
394.4655, the clinical record may be released
to the state attorney, the public defender
or the patient’s private legal counsel, the
court, and to the appropriate mental
health professionals, including the service
provider identied in s. 394.4655(6)(b)2., in
accordance with state and federal law.
(3) For purposes of Section 394.4615(3)(b), F.S., a
“qualified researcher” is one who after making
application to review confidential data and who,
after documenting his or her bona fide academic,
scientific or medical credentials and describing the
particular research which gives rise to the request,
is determined by the administrator of a receiving
or treatment facility or by the Secretary of the
department, to be eligible to review such data. In
making that determination the administrator or the
Secretary shall weigh the person’s right to privacy
against the benefit of disclosure and shall determine
whether the disclosure is in the best interest of
the state. Person identifying information obtained
by such a qualified researcher shall not be further
disclosed without the express and informed consent
of the person or individual authorized to provide
consent for him or her.
(4) When a person’s access to his or her clinical record
or any part of his or her record is restricted by
written order of the attending physician such
restriction shall be documented in the person’s
clinical record. If the request is denied or such access
is restricted, a written response shall be provided to
the person. Recommended form CF-MH 3110, Feb.
05, “Restriction of Person’s Access to Own Record,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
rule chapter may be used for such documentation.
(5) Each receiving facility shall develop detailed policies
and procedures governing release of records to
each person requesting release, including criteria
for determining what type of information may be
harmful to the person, establishing a reasonable
time for responding to requests for access, and
identifying methods of providing access that ensure
clinical support to the person while securing the
integrity of the record.
Clinical records; confidentiality

79 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Clinical records; confidentiality
(4) Information from clinical records may be used
for statistical and research purposes if the infor-
mation is abstracted in such a way as to protect
the identity of individuals.
(5) Information from clinical records may be used
by the Agency for Health Care Administra-
tion, the department, and the Florida advocacy
councils for the purpose of monitoring facility
activity and complaints concerning facilities.
(6) Clinical records relating to a Medicaid recipi-
ent shall be furnished to the Medicaid Fraud
Control Unit in the Department of Legal Af-
fairs, upon request.
(7) Any person, agency, or entity receiving infor-
mation pursuant to this section shall maintain
such information as condential and exempt
from the provisions of s. 119.07(1).
(8) Any facility or private mental health practitio-
ner who acts in good faith in releasing infor-
mation pursuant to this section is not subject
to civil or criminal liability for such release.
(9) Nothing in this section is intended to prohibit
the parent or next of kin of a person who is
held in or treated under a mental health facil-
ity or program from requesting and receiving
information limited to a summary of that per-
son’s treatment plan and current physical and
mental condition. Release of such information
shall be in accordance with the code of ethics
of the profession involved.
(10) Patients shall have reasonable access to their
clinical records, unless such access is deter-
mined by the patient’s physician to be harmful
to the patient. If the patient’s right to inspect
his or her clinical record is restricted by the fa-
cility, written notice of such restriction shall be
given to the patient and the patient’s guardian,
guardian advocate, attorney, and representative.
In addition, the restriction shall be recorded in
the clinical record, together with the reasons
for it. e restriction of a patient’s right to
inspect his or her clinical record shall expire
after 7 days but may be renewed, after review,
for subsequent 7-day periods.
(Chapter 394.4615 F.S.)
65E-5 F.A.C.
Other federal
and state laws governing
condentiality may
also apply.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
80
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.462 F.S.)
65E-5.260 F.A.C.
(11) Any person who fraudulently alters, defaces,
or falsies the clinical record of any person
receiving mental health services in a facility
subject to this part, or causes or procures any
of these oenses to be committed, commits a
misdemeanor of the second degree, punishable
as provided in s. 775.082 or s. 775.083.
394.462 Transportation.
(1) TRANSPORTATION TO A RECEIVING
FACILITY.
(a) Each county shall designate a single law
enforcement agency within the county,
or portions thereof, to take a person into
custody upon the entry of an ex parte
order or the execution of a certicate
for involuntary examination by an
authorized professional and to transport
that person to the nearest receiving
facility for examination. e designated
law enforcement agency may decline to
transport the person to a receiving facility
only if:
1. e jurisdiction designated by the
county has contracted on an annual ba-
sis with an emergency medical transport
service or private transport company for
transportation of persons to receiving
facilities pursuant to this section at the
sole cost of the county; and
2. e law enforcement agency and the
emergency medical transport service or
private transport company agree that
the continued presence of law enforce-
ment personnel is not necessary for the
safety of the person or others.
3. e jurisdiction designated by the county
may seek reimbursement for transporta-
tion expenses. e party responsible for
payment for such transportation is the
person receiving the transportation. e
county shall seek reimbursement from the
following sources in the following order:
65E-5.260 Transportation.
(1) Each law enforcement officer who takes a person
into custody upon the entry of recommended form
CF-MH 3001, Feb. 05, “Ex Parte Order for Involuntary
Examination,” which is incorporated by reference
and may be obtained pursuant to Rule 65E-5.120,
F.A.C., of this rule chapter, or other form provided
by the court, or the execution of mandatory form
CF-MH 3052b, Sept. 06, “Certificate of Professional
Initiating Involuntary Examination,” which is hereby
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule chapter
or completion of mandatory form CF-MH 3052a, Sept.
06, “Report of a Law Enforcement Officer Initiating
Involuntary Examination,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter shall ensure that
such forms accompany the person to the receiving
facility for inclusion in the person’s clinical record.
(2) The designated law enforcement agency shall
transport the person to the nearest receiving facility
as required by statute, documenting this transport on
mandatory form CF-MH 3100, Feb. 05, “Transportation
to Receiving Facility,” which is hereby incorporated
by reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter. The designated
law enforcement agency may decline to transport the
person to a receiving facility only if the provisions of
Section 394.462(1), F.S., apply. When the designated
law enforcement agency and the medical transport
company agree that the continued presence of law
enforcement personnel is not necessary for the safety
of the person or others. Part II of mandatory form
CF-MH 3100, “Transportation to Receiving Facility,” as
referenced in subsection 65E-5.260(2), F.A.C., reflecting
the agreement between law enforcement and the
transport service shall accompany the person to the
receiving facility. The completed form shall be retained
in the person’s clinical record.
Transportation

81 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
a. From an insurance company, health
care corporation, or other source, if
the person receiving the transporta-
tion is covered by an insurance policy
or subscribes to a health care corpora-
tion or other source for payment of
such expenses.
b. From the person receiving the trans-
portation.
c. From a nancial settlement for medi-
cal care, treatment, hospitalization, or
transportation payable or accruing to
the injured party.
(b) Any company that transports a patient
pursuant to this subsection is considered an
independent contractor and is solely liable
for the safe and dignied transportation
of the patient. Such company must be
insured and provide no less than $100,000
in liability insurance with respect to the
transportation of patients.
(c) Any company that contracts with a
governing board of a county to transport
patients shall comply with the applicable
rules of the department to ensure the safety
and dignity of the patients.
(d) When a law enforcement ocer takes
custody of a person pursuant to this part,
the ocer may request assistance from
emergency medical personnel if such
assistance is needed for the safety of the
ocer or the person in custody.
(e) When a member of a mental health overlay
program or a mobile crisis response service
is a professional authorized to initiate an
involuntary examination pursuant to s.
394.463 and that professional evaluates a
person and determines that transportation
to a receiving facility is needed, the service,
at its discretion, may transport the person
to the facility or may call on the law
enforcement agency or other transportation
arrangement best suited to the needs of the
patient.
Transportation
(Chapter 394.462 F.S.)
65E-5 F.A.C.
Law enforcement mandated to
transport people on involuntary
status to receiving facilities—Not to
treatment facilities.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
82
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(f ) When any law enforcement ocer has
custody of a person based on either
noncriminal or minor criminal behavior
that meets the statutory guidelines for
involuntary examination under this part,
the law enforcement ocer shall transport
the person to the nearest receiving facility
for examination.
(g) When any law enforcement ocer has
arrested a person for a felony and it
appears that the person meets the statutory
guidelines for involuntary examination or
placement under this part, such person shall
rst be processed in the same manner as any
other criminal suspect. e law enforcement
agency shall thereafter immediately notify
the nearest public receiving facility, which
shall be responsible for promptly arranging
for the examination and treatment of the
person. A receiving facility is not required
to admit a person charged with a crime
for whom the facility determines and
documents that it is unable to provide
adequate security, but shall provide mental
health examination and treatment to the
person where he or she is held.
(h) If the appropriate law enforcement ocer
believes that a person has an emergency
medical condition as dened in s. 395.002,
the person may be rst transported to a
hospital for emergency medical treatment,
regardless of whether the hospital is a
designated receiving facility.
(i) e costs of transportation, evaluation,
hospitalization, and treatment incurred
under this subsection by persons who have
been arrested for violations of any state law
or county or municipal ordinance may be
recovered as provided in s. 901.35.
(j) e nearest receiving facility must accept
persons brought by law enforcement ocers
for involuntary examination.
(k) Each law enforcement agency shall develop
a memorandum of understanding with each
receiving facility within the law enforcement
Transportation
(Chapter 394.462 F.S.)
65E-5. F.A.C.
FELONY CHARGES
MISDEMEANOR CHARGES
Nearest Receiving Facility
must accept any person brought by
law enforcement for involuntary
examination.

FELONY CHARGES
MISDEMEANOR CHARGES
83 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
agency’s jurisdiction which reects a single
set of protocols for the safe and secure
transportation of the person and transfer of
custody of the person. ese protocols must
also address crisis intervention measures.
(l) When a jurisdiction has entered into
a contract with an emergency medical
transport service or a private transport
company for transportation of persons to
receiving facilities, such service or company
shall be given preference for transportation
of persons from nursing homes, assisted
living facilities, adult day care centers, or
adult family-care homes, unless the behavior
of the person being transported is such that
transportation by a law enforcement ocer
is necessary.
(m)
Nothing in this section shall be construed
to limit emergency examination and
treatment of incapacitated persons provided
in accordance with the provisions of s.
401.445.
(2) TRANSPORTATION TO A TREATMENT
FACILITY.
(a) If neither the patient nor any person
legally obligated or responsible for the
patient is able to pay for the expense of
transporting a voluntary or involuntary
patient to a treatment facility, the governing
board of the county in which the patient is
hospitalized shall arrange for such required
transportation and shall ensure the safe
and dignied transportation of the patient.
e governing board of each county is
authorized to contract with private transport
companies for the transportation of such
patients to and from a treatment facility.
(b) Any company that transports a patient
pursuant to this subsection is considered an
independent contractor and is solely liable
for the safe and dignied transportation
of the patient. Such company must be
insured and provide no less than $100,000
in liability insurance with respect to the
transportation of patients.
Transportation
(Chapter 394.462 F.S.)
65E-5. F.A.C.
Treatment facilities are
different from receiving
facilities.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
84
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.462 F.S.)
65E-5.2601 F.A.C.
(c) Any company that contracts with the
governing board of a county to transport
patients shall comply with the applicable
rules of the department to ensure the safety
and dignity of the patients.
(d)County or municipal law enforcement
and correctional personnel and equipment
shall not be used to transport patients
adjudicated incapacitated or found by the
court to meet the criteria for involuntary
placement pursuant to s. 394.467, except in
small rural counties where there are no cost-
ecient alternatives.
(3) TRANSFER OF CUSTODY. Custody of a
person who is transported pursuant to this
part, along with related documentation, shall
be relinquished to a responsible individual at
the appropriate receiving or treatment facility.
(4) EXCEPTIONS.
An exception to the requirements of this sec-
tion may be granted by the secretary of the
department for the purposes of improving
service coordination or better meeting the
special needs of individuals. A proposal for an
exception must be submitted by the district
administrator after being approved by the gov-
erning boards of any aected counties, prior to
submission to the secretary.
(a) A proposal for an exception must identify
the specic provision from which an
exception is requested; describe how
the proposal will be implemented by
participating law enforcement agencies and
transportation authorities; and provide a
plan for the coordination of services such as
case management.
(b)e exception may be granted only for:
1. An arrangement centralizing and im-
proving the provision of services within
a district, which may include an excep-
tion to the requirement for transporta-
tion to the nearest receiving facility;
2. An arrangement by which a facility may
provide, in addition to required psychi-
atric services, an environment and ser-
65E-5.2601 Transportation Exception Plan.
(1) In determining whether to approve a proposal for
an exception or exceptions to the transportation
requirements of Section 394.462(3), F.S., the
following shall be considered by the department:
(a) The specific provision from which an exception is
requested;
(b) Evidence presented by the department’s district
or region of community need and support for
the request;
(c) Whether the proposal is presented in a
format that is clear, simple, and can be readily
implemented by all parties and the public;
(d) How the proposed plan will improve services
to the public and persons needing Baker Act
services; and
(e) Whether the geographic boundaries identified in
the proposal are distinct and unambiguous.
(2) The proposal must include provisions which
address:
(a) Accountability for delays or confusion when
transportation fails to respond appropriately;
(b) How disputes which may arise over
implementation of the plan will be resolved;
(c) Identification of the public official whose
position is responsible for the continuing
oversight and monitoring of the service in
compliance with the terms of the approved
proposal;
Transportation

85 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4625 F.S.)
65E-5.270 F.A.C.
vices which are uniquely tailored to the
needs of an identied group of persons
with special needs, such as persons with
hearing impairments or visual impair-
ments, or elderly persons with physical
frailties; or
3. A specialized transportation system that
provides an ecient and humane meth-
od of transporting patients to receiving
facilities, among receiving facilities, and
to treatment facilities.
(c) Any exception approved pursuant to this
subsection shall be reviewed and approved
every 5 years by the secretary.
394.4625 Voluntary admissions.
(1) AUTHORITY TO RECEIVE PATIENTS.
(a) A facility may receive for observation,
diagnosis, or treatment any person 18
years of age or older making application by
express and informed consent for admission
or any person age 17 or under for whom
such application is made by his or her
guardian. If found to show evidence of
mental illness, to be competent to provide
express and informed consent, and to be
suitable for treatment, such person 18 years
of age or older may be admitted to the
facility. A person age 17 or under may be
admitted only after a hearing to verify the
voluntariness of the consent.
(b)A mental health overlay program or a
mobile crisis response service or a licensed
professional who is authorized to initiate
an involuntary examination pursuant to s.
394.463 and is employed by a community
mental health center or clinic must,
pursuant to district procedure approved
by the respective district administrator,
conduct an initial assessment of the ability
of the following persons to give express and
(d) The plan for periodically monitoring compliance
with the proposal, public satisfaction with the
service provided, and assurance of rights of each
person served by the facility;
(e) The method complaints and grievances are to be
received and resolved; and
(f) Community support and involvement including
a description of the participation of designated
public and private receiving facilities, law
enforcement, transportation officials, consumers,
families, and advocacy groups.
(3) The approval by the governing boards of any
affected counties, shall be certified in writing by
the district or region’s mental health and substance
abuse program supervisor, prior to the plan’s
submission to the Secretary of the Department.
65E-5.270 Voluntary Admission.
(1) Recommended form CF-MH 3040, “Application for
Voluntary Admission,” as referenced in paragraph
65E-5.1302(1)(b), F.A.C., may be used to document
an application of a competent adult for admission
to a receiving facility. Recommended form CF-MH
3097, Feb. 05, “Application for Voluntary Admission
– Minors,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter, may be used to document a
guardian’s application for admission of a minor to
a receiving facility. Recommended form CF-MH
3098, Feb. 05, “Application for Voluntary Admission
– State Treatment Facility,” which is incorporated
by reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter, may be
used to document an application of a competent
adult for admission to a state treatment facility. Any
application for voluntary admission shall be based
on the person’s express and informed consent.
(a) Recommended form CF-MH 3104, “Certification
of Person’s Competence to Provide Express and
Informed Consent,” as referenced in paragraph
65E-5.170(1)(c), F.A.C., may be used to document
the competence of a person to give express and
informed consent to be on voluntary status. The
original of the completed form shall be retained
in the person’s clinical record.
Voluntary admissions

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
86
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4625 F.S.)
65E-5.270 F.A.C.
informed consent to treatment before such
persons may be admitted voluntarily:
1. A person 60 years of age or older for
whom transfer is being sought from a
nursing home, assisted living facility,
adult day care center, or adult family-
care home, when such person has been
diagnosed as suering from dementia.
2. A person 60 years of age or older
for whom transfer is being sought
from a nursing home pursuant to s.
400.0255(12).
3. A person for whom all decisions con-
cerning medical treatment are currently
being lawfully made by the health care
surrogate or proxy designated under
chapter 765.
(c) When an initial assessment of the ability of a
person to give express and informed consent
to treatment is required under this section,
and a mobile crisis response service does not
respond to the request for an assessment
within 2 hours after the request is made
or informs the requesting facility that it
will not be able to respond within 2 hours
after the request is made, the requesting
facility may arrange for assessment by any
licensed professional authorized to initiate
an involuntary examination pursuant to s.
394.463 who is not employed by or under
contract with, and does not have a nancial
interest in, either the facility initiating the
transfer or the receiving facility to which the
transfer may be made.
(d)A facility may not admit as a voluntary
patient a person who has been adjudicated
incapacitated, unless the condition of
incapacity has been judicially removed.
If a facility admits as a voluntary patient
a person who is later determined to have
been adjudicated incapacitated, and the
condition of incapacity had not been
removed by the time of the admission, the
facility must either discharge the patient or
transfer the patient to involuntary status.
(b) Recommended form CF-MH 3104, “Certification
of Person’s Competence to Provide Express and
Informed Consent,” as referenced in paragraph 65E-
5.170(1)(c), F.A.C., may be used to document a person
applying for transfer from involuntary to voluntary
status is competent to provide express and informed
consent. The original of the completed form shall be
filed in the person’s clinical record. A change in legal
status must be followed by notice sent to individuals
pursuant to Section 394.4599, F.S.
(2) Persons on voluntary status shall be advised of their
right to request discharge. Recommended forms
CF-MH 3051a, Feb. 05, “Notice of Right of Person
on Voluntary Status to Request Discharge from a
Receiving Facility,” which is incorporated by reference
and may be obtained pursuant to Rule 65E-5.120,
F.A.C., of this rule chapter, or CF-MH 3051b, Feb. 05,
“Notice of Right of Person on Voluntary Status to
Request Discharge from a Treatment Facility,” which
is incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule chapter
and used to document the giving of such advice. A
copy of the notice or its equivalent shall be given to
the person and to the person’s parent if a minor, with
the original of each completed application and notice
retained in the person’s clinical record.
(3) Documenting the assessment of each person pursuant
to Section 394.4615(1)(b), F.S., shall be done prior
to moving the person from his or her residence to a
receiving facility for voluntary admission. Recommended
form CF-MH 3099, Feb. 05, “Certification of Ability to
Provide Express and Informed Consent for Voluntary
Admission and Treatment of Selected Persons from
Facilities Licensed under Chapter 400, F.S.,” which
is incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule chapter
and used for this purpose.
(4) If a competent adult or the guardian of a minor
refuses to consent to mental health treatment,
the person shall not be eligible for admission on
a voluntary status. A person on voluntary status
who refuses to consent to or revokes consent to
treatment shall be discharged from a designated
receiving or treatment facility within 24 hours after
such refusal or revocation, unless the person is
transferred to involuntary status or unless the refusal
or revocation is freely and voluntarily rescinded
by the person. When a person refuses or revokes
consent to treatment, facility staff shall document
Voluntary admissions

87 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4625 F.S.)
65E-5.270 F.A.C.
(e) e health care surrogate or proxy of a
voluntary patient may not consent to the
provision of mental health treatment for
the patient. A voluntary patient who is
unwilling or unable to provide express and
informed consent to mental health treatment
must either be discharged or transferred to
involuntary status.
(f) Within 24 hours after admission of a voluntary
patient, the admitting physician shall
document in the patient’s clinical record that
the patient is able to give express and informed
consent for admission. If the patient is not
able to give express and informed consent for
admission, the facility shall either discharge the
patient or transfer the patient to involuntary
status pursuant to subsection (5).
(2) DISCHARGE OF VOLUNTARY PATIENTS.
(a) A facility shall discharge a voluntary patient:
1. Who has suciently improved so that
retention in the facility is no longer desir-
able. A patient may also be discharged to
the care of a community facility.
2. Who revokes consent to admission or
requests discharge. A voluntary patient or
a relative, friend, or attorney of the patient
may request discharge either orally or in
writing at any time following admission to
the facility. e patient must be discharged
within 24 hours of the request, unless the
request is rescinded or the patient is trans-
ferred to involuntary status pursuant to
this section. e 24-hour time period may
be extended by a treatment facility when
necessary for adequate discharge planning,
but shall not exceed 3 days exclusive of
weekends and holidays. If the patient, or
another on the patient’s behalf, makes an
oral request for discharge to a sta member,
such request shall be immediately entered
in the patient’s clinical record. If the request
for discharge is made by a person other
than the patient, the discharge may be con-
ditioned upon the express and informed
consent of the patient.
Voluntary admissions
this immediately in the person’s clinical record.
Recommended form CF-MH 3105, Feb. 05, “Refusal
or Revocation of Consent to Treatment,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used for this purpose. Should a
competent person withdraw his or her refusal or
revocation of consent to treatment, the person shall
be asked to complete Part II of recommended form
CF-MH 3105, “Refusal or Revocation of Consent
to Treatment,” as referenced in subsection 65E-
5.270(4), F.A.C., or similar documentation, and the
original shall be retained in the person’s clinical
record.
(5) An oral or written request for discharge made by
any person following admission to the facility shall
be immediately documented in the person’s clinical
record. Recommended forms CF-MH 3051a, “Notice
of Right of Person on Voluntary Status to Request
Discharge from a Receiving Facility,” as referenced
in subsection 65E-5.270(2), F.A.C., or CF-MH 3051b,
“Notice of Right of Person on Voluntary Status to
Request Discharge from a Treatment Facility,” as
referenced in subsection 65E-5.270(2), F.A.C., may
be used for this purpose. This form may also be
completed by a relative, adult friend, or attorney of
the person.
(6) When a person on voluntary status refuses
treatment or requests discharge and the facility
administrator makes the determination that the
person will not be discharged within 24 hours
from a designated receiving or treatment facility,
a petition for involuntary inpatient placement
or involuntary outpatient placement shall be
filed with the court by the facility administrator.
Recommended form CF-MH 3032, “Petition for
Involuntary Inpatient Placement,” as referenced
in subparagraph 65E-5.170(1)(d)1., F.A.C., or
recommended form CF-MH 3130, “Petition for
Involuntary Outpatient Placement”, as referenced
in subparagraph 65E-5.170(1)(d)2., F.A.C., may be
used for this purpose. The first expert opinion by
a psychiatrist shall be obtained on the petition
form within 24 hours of the request for discharge
or refusal of treatment to justify the continued
detention of the person and the petition shall be
filed with the court within 2 court working days
after the request for discharge or refusal to consent
to treatment was made.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
88
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(b) A voluntary patient who has been admitted
to a facility and who refuses to consent
to or revokes consent to treatment shall
be discharged within 24 hours after such
refusal or revocation, unless transferred to
involuntary status pursuant to this section
or unless the refusal or revocation is freely
and voluntarily rescinded by the patient.
(3) NOTICE OF RIGHT TO DISCHARGE.
At the time of admission and at least every 6
months thereafter, a voluntary patient shall be
notied in writing of his or her right to apply
for a discharge.
(4) TRANSFER TO VOLUNTARY STATUS.
An involuntary patient who applies to be
transferred to voluntary status shall be trans-
ferred to voluntary status immediately, unless
the patient has been charged with a crime, or
has been involuntarily placed for treatment by
a court pursuant to s. 394.467 and continues
to meet the criteria for involuntary placement.
When transfer to voluntary status occurs, no-
tice shall be given as provided in s. 394.4599.
(5) TRANSFER TO INVOLUNTARY STATUS.
When a voluntary patient, or an authorized
person on the patient’s behalf, makes a request
for discharge, the request for discharge, unless
freely and voluntarily rescinded, must be com-
municated to a physician, clinical psychologist,
or psychiatrist as quickly as possible, but not
later than 12 hours after the request is made.
If the patient meets the criteria for involuntary
placement, the administrator of the facility
must le with the court a petition for involun-
tary placement, within 2 court working days
after the request for discharge is made. If the
petition is not led within 2 court working
days, the patient shall be discharged. Pend-
ing the ling of the petition, the patient may
be held and emergency treatment rendered in
the least restrictive manner, upon the written
order of a physician, if it is determined that
such treatment is necessary for the safety of the
patient or others.
Voluntary admissions
(Chapter 394.4625 F.S.)
65E-5.270 F.A.C.
(7) If a person is delivered to a receiving facility
for voluntary examination from any program or
residential placement licensed under the provisions
of Chapter 400, F.S., without first arranging
an independent evaluation of the resident’s
competence to provide express and informed
consent to admission and treatment, as required in
Sections 394.4625(1)(b) and (c), F.S., the receiving
facility shall notify the Agency for Health Care
Administration by using recommended form CF-MH
3119, Feb. 05, “Notification of Non-Compliance
with Required Certificate,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter.
Transfers between legal statuses
See Appendix B for extensive
information on voluntary
admission.

89 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
65E-5.280 F.A.C.
394.463 Involuntary examination.
(1) CRITERIA. A person may be taken to a re-
ceiving facility for involuntary examination if
there is reason to believe that the person has a
mental illness and because of his or her mental
illness:
(a) 1. e person has refused voluntary
examination after conscientious
explanation and disclosure of the
purpose of the examination; or
2. e person is unable to determine for
himself or herself whether examination
is necessary; and
(b) 1. Without care or treatment, the person is
likely to suer from neglect or refuse to
care for himself or herself; such neglect
or refusal poses a real and present threat
of substantial harm to his or her well-
being; and it is not apparent that such
harm may be avoided through the help
of willing family members or friends or
the provision of other services; or
2. ere is a substantial likelihood that
without care or treatment the person
will cause serious bodily harm to himself
or herself or others in the near future, as
evidenced by recent behavior.
(2) INVOLUNTARY EXAMINATION.
(a) An involuntary examination may be
initiated by any one of the following means:
1. A court may enter an ex parte order stat-
ing that a person appears to meet the cri-
teria for involuntary examination, giving
the ndings on which that conclusion is
based. e ex parte order for involuntary
examination must be based on sworn
testimony, written or oral. If other less
restrictive means are not available, such
as voluntary appearance for outpatient
evaluation, a law enforcement ocer, or
other designated agent of the court, shall
take the person into custody and de-
liver him or her to the nearest receiving
facility for involuntary examination. e
Involuntary examination
65E-5.280 Involuntary Examination.
(1) Court Order. Sworn testimony shall be documented
by using recommended form CF-MH 3002, Feb. 05,
“Petition and Affidavit Seeking Ex Parte Order Requiring
Involuntary Examination,” which is incorporated by
reference and may be obtained pursuant to Rule 65E-
5.120, F.A.C., of this rule chapter, or other form used
by the court. Documentation of the findings of the
court on recommended form CF-MH 3001, “Ex Parte
Order for Involuntary Examination,” as referenced in
subsection 65E-5.260(1), F.A.C., or other order used
by the court, shall be used when there is reason to
believe the criteria for involuntary examination are met.
The ex parte order for involuntary examination shall
accompany the person to the receiving facility and be
retained in the person’s clinical record.
(2) Law Enforcement.
(a) If a law enforcement officer, in the course of his
or her official duties, initiates an involuntary
examination, the officer shall complete the
mandatory form CF-MH 3052a, “Report of Law
Enforcement Officer Initiating Involuntary
Examination,” as referenced in subsection 65E-
5.260(1), F.A.C.
(b) Mandatory form CF-MH 3052a, “Report of Law
Enforcement Officer Initiating Involuntary
Examination,” as referenced in subsection 65E-
5.260(1), F.A.C., shall accompany the person to
the nearest receiving facility for retention in the
person’s clinical record.
(3) Professional Certificate.
(a) A professional authorized by Section 394.463(2)
(a)3., F.S., who determines, after personally
examining a person believed to meet the
involuntary examination criteria within the
preceding 48 hours, verifies that the criteria are
met, is authorized to execute the mandatory
form CF-MH 3052b, “Certificate of Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C.
(b) Mandatory form CF-MH 3052b, “Certificate of
Professional Initiating Involuntary Examination,”
as referenced in subsection 65E-5.260(1), F.A.C.,
shall be executed immediately upon its initiation
and is valid throughout the state. The completed
certificate shall accompany the person to a
receiving facility and be retained in the person’s
clinical record.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
90
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
65E-5.280 F.A.C.
order of the court shall be made a part
of the patient’s clinical record. No fee
shall be charged for the ling of an order
under this subsection. Any receiving fa-
cility accepting the patient based on this
order must send a copy of the order to
the Agency for Health Care Administra-
tion on the next working day. e order
shall be valid only until executed or, if
not executed, for the period specied in
the order itself. If no time limit is speci-
ed in the order, the order shall be valid
for 7 days after the date that the order
was signed.
2. A law enforcement ocer shall take a
person who appears to meet the criteria
for involuntary examination into cus-
tody and deliver the person or have him
or her delivered to the nearest receiv-
ing facility for examination. e ocer
shall execute a written report detailing
the circumstances under which the per-
son was taken into custody, and the re-
port shall be made a part of the patient’s
clinical record. Any receiving facility ac-
cepting the patient based on this report
must send a copy of the report to the
Agency for Health Care Administration
on the next working day.
3. A physician, clinical psychologist, psy-
chiatric nurse, mental health counselor,
marriage and family therapist, or clinical
social worker may execute a certicate
stating that he or she has examined a
person within the preceding 48 hours
and nds that the person appears to
meet the criteria for involuntary ex-
amination and stating the observations
upon which that conclusion is based.
If other less restrictive means are not
available, such as voluntary appearance
for outpatient evaluation, a law enforce-
ment ocer shall take the person named
in the certicate into custody and de-
liver him or her to the nearest receiving
(4) Emergency Medical Conditions.
(a) Recommended form CF-MH 3101, Feb. 05,
“Hospital Determination that Person Does Not
Meet Involuntary Placement Criteria,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used to document the results of
the examination prescribed in Section 394.463(2)
(g), F.S.
(b) Receiving facilities shall develop policies and
procedures that expedite the transfer of persons
referred from non-designated hospitals after
examination or treatment of an emergency
medical condition, within the 12 hours permitted
by Section 394.463(2)(h), F.S.
(c) The 72-hour involuntary examination period
set out in Section 394.463(2)(f ), F.S., shall not
be exceeded. In order to document the 72-hour
period has not been exceeded, recommended
form CF-MH 3102, Feb. 05, “Request for
Involuntary Examination After Stabilization
of Emergency Medical Condition,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used for this purpose. The form
may be sent by fax, or otherwise, to promptly
communicate its contents to a designated
receiving facility at which appropriate medical
treatment is available.
(5) In order for the department to implement
the provisions of Section 394.463(2)(e), F.S.,
and to ensure that the Agency for Health Care
Administration will be able to analyze the data
it receives pursuant to that section, designated
receiving facilities shall forward copies of each
recommended form CF-MH 3001, “Ex Parte Order
for Involuntary Examination,” as referenced in
subsection 65E-5.260(1), F.A.C., or other order
provided by the court, mandatory form CF-
MH 3052a, “Report of Law Enforcement Officer
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., mandatory
form CF-MH 3052b, “Certificate of Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., accompanied by
mandatory form CF-MH 3118, Sept. 06, “Cover Sheet
to Agency for Health Care Administration,” which
is hereby incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
Involuntary examination

91 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
facility for involuntary examination. e
law enforcement ocer shall execute a
written report detailing the circumstanc-
es under which the person was taken
into custody. e report and certicate
shall be made a part of the patient’s clini-
cal record. Any receiving facility accept-
ing the patient based on this certicate
must send a copy of the certicate to the
Agency for Health Care Administration
on the next working day.
(b)A person shall not be removed from any
program or residential placement licensed
under chapter 400 or chapter 429 and
transported to a receiving facility for
involuntary examination unless an ex parte
order, a professional certicate, or a law
enforcement ocer’s report is rst prepared.
If the condition of the person is such that
preparation of a law enforcement ocer’s
report is not practicable before removal, the
report shall be completed as soon as possible
after removal, but in any case before the
person is transported to a receiving facility.
A receiving facility admitting a person
for involuntary examination who is not
accompanied by the required ex parte order,
professional certicate, or law enforcement
ocer’s report shall notify the Agency
for Health Care Administration of such
admission by certied mail no later than
the next working day. e provisions of this
paragraph do not apply when transportation
is provided by the patient’s family or
guardian.
(c) A law enforcement ocer acting in
accordance with an ex parte order issued
pursuant to this subsection may serve and
execute such order on any day of the week,
at any time of the day or night.
(d)A law enforcement ocer acting in
accordance with an ex parte order issued
pursuant to this subsection may use such
reasonable physical force as is necessary
to gain entry to the premises, and any
Involuntary examination
65E-5.2801 F.A.C.
rule chapter to: BA Reporting Center, FMHI-MHC
2737, 13301 Bruce B. Downs Boulevard, Tampa,
Florida 33612-3807.
(6) If a person is delivered to a receiving facility for
an involuntary examination from any program or
residential placement licensed under the provisions
of Chapter 400, F.S., without an ex parte order,
the mandatory form CF-MH 3052a, “Report of
Law Enforcement Officer Initiating Involuntary
Examination,” as referenced in subsection 65E-
5.260(1), F.A.C., or mandatory form CF-MH 3052b,
“Certificate of Professional Initiating Involuntary
Examination,” as referenced in subsection 65E-
5.260(1), F.A.C., the receiving facility shall notify
the Agency for Health Care Administration by
the method and timeframe required by Section
394.463(2)(b), F.S. The receiving facility may
use recommended form CF-MH 3119, Feb. 05,
“Notification of Non-Compliance with Required
Certificate,” as referenced in subsection 65E-
5.270(7), F.A.C., for this purpose.
(7) Documentation that each completed form was
submitted in a timely way shall be retained in the
person’s clinical record.
(8) Recommended form CF-MH 3045, Feb. 05, “Notice
of Person’s Admission for Involuntary Examination,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of this
rule chapter may be used when notifying authorized
individuals of a person’s involuntary admission to a
receiving facility.
65E-5.2801 Minimum Standards for
Involuntary Examination Pursuant to
Section 394.463, F.S.
The involuntary examination is also known as the initial
mandatory involuntary examination.
(1) Whenever an involuntary examination is initiated
by a circuit court, a law enforcement officer, or a
mental health professional as provided in Section
394.463(2), F.S., an examination by a physician
or clinical psychologist must be conducted and
documented in the person’s clinical record. The
examination, conducted at a facility licensed under
Chapter 394 or 395, F.S., must contain:
(a) A thorough review of any observations of the
person’s recent behavior;
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
92
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
65E-5.2801 F.A.C.
dwellings, buildings, or other structures
located on the premises, and to take custody
of the person who is the subject of the ex
parte order.
(e) e Agency for Health Care Administration
shall receive and maintain the copies of
ex parte orders, involuntary outpatient
placement orders issued pursuant to
s. 394.4655, involuntary inpatient
placement orders issued pursuant to s.
394.467, professional certicates, and
law enforcement ocers’ reports. ese
documents shall be considered part of the
clinical record, governed by the provisions
of s. 394.4615. e agency shall prepare
annual reports analyzing the data obtained
from these documents, without information
identifying patients, and shall provide
copies of reports to the department, the
President of the Senate, the Speaker of the
House of Representatives, and the minority
leaders of the Senate and the House of
Representatives.
(f) A patient shall be examined by a physician
or clinical psychologist at a receiving
facility without unnecessary delay and may,
upon the order of a physician, be given
emergency treatment if it is determined
that such treatment is necessary for the
safety of the patient or others. e patient
may not be released by the receiving
facility or its contractor without the
documented approval of a psychiatrist, a
clinical psychologist, or, if the receiving
facility is a hospital, the release may also
be approved by an attending emergency
department physician with experience in
the diagnosis and treatment of mental and
nervous disorders and after completion of
an involuntary examination pursuant to this
subsection. However, a patient may not be
held in a receiving facility for involuntary
examination longer than 72 hours.
(g) A person for whom an involuntary
examination has been initiated who is being
(b) A review of mandatory form CF-MH 3100,
“Transportation to Receiving Facility,” as
referenced in subsection 65E-5.260(2), F.A.C.,
and recommended form CF-MH 3001, “Ex Parte
Order for Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., or other form
provided by the court, or mandatory form CF-
MH 3052a, “Report of Law Enforcement Officer
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., or mandatory
form CF-MH 3052b, “Certificate of Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C.
(c) A brief psychiatric history; and
(d) A face-to-face examination of the person in a
timely manner to determine if the person meets
criteria for release.
(2) If the physician or clinical psychologist conducting
the initial mandatory involuntary examination
determines that the person does not meet the
criteria for involuntary inpatient placement or
involuntary outpatient placement, the person can
be offered voluntary placement, if the person meets
criteria for voluntary admission, or released directly
from the hospital providing emergency medical
services. Such determination must be documented
in the person’s clinical record.
(3) If not released, recommended form CF-MH
3040, “Application for Voluntary Admission,” as
referenced in paragraph 65E-5.1302(1)(b), F.A.C.,
or recommended form CF-MH 3097, “Application
for Voluntary Admission – Minors,” as referenced in
subsection 65E-5.270(1), F.A.C., may be used if the
person wishes to apply for voluntary admission.
(4) If not released and the person wishes to transfer
from involuntary to voluntary status, recommended
form CF-MH 3104, “Certification of Person’s
Competence to Provide Express and Informed
Consent,” as referenced in paragraph 65E-5.170(1)
(c), F.A.C., documenting the person is competent to
provide express and informed consent, may be used
for this purpose.
(5) All results and documentation of all elements of the
initial mandatory involuntary examination shall be
retained in the person’s clinical record.
(6) If the person is not released or does not become
voluntary as a result of giving express and informed
consent to admission and treatment in the first
part of the involuntary examination, the person
Involuntary examination

93 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
65E-5.2801 F.A.C.
evaluated or treated at a hospital for an
emergency medical condition specied in s.
395.002 must be examined by a receiving
facility within 72 hours. e 72-hour
period begins when the patient arrives at
the hospital and ceases when the attending
physician documents that the patient has
an emergency medical condition. If the
patient is examined at a hospital providing
emergency medical services by a professional
qualied to perform an involuntary
examination and is found as a result of that
examination not to meet the criteria for
involuntary outpatient placement pursuant
to s. 394.4655(1) or involuntary inpatient
placement pursuant to s. 394.467(1), the
patient may be oered voluntary placement,
if appropriate, or released directly from
the hospital providing emergency medical
services. e nding by the professional
that the patient has been examined and
does not meet the criteria for involuntary
inpatient placement or involuntary
outpatient placement must be entered into
the patient’s clinical record. Nothing in this
paragraph is intended to prevent a hospital
providing emergency medical services
from appropriately transferring a patient
to another hospital prior to stabilization,
provided the requirements of s. 395.1041(3)
(c) have been met.
(h) One of the following must occur within 12
hours after the patient’s attending physician
documents that the patient’s medical
condition has stabilized or that an emergency
medical condition does not exist:
1. e patient must be examined by a desig-
nated receiving facility and released; or
2. e patient must be transferred to a des-
ignated receiving facility in which ap-
propriate medical treatment is available.
However, the receiving facility must be
notied of the transfer within 2 hours
after the patient’s condition has been
stabilized or after determination that an
Involuntary examination
shall be examined by a psychiatrist to determine if
the criteria for involuntary inpatient or involuntary
outpatient placement are met.
(7) After the initial mandatory involuntary examination,
the person’s clinical record shall include:
(a) An intake interview;
(b) The mandatory form CF-MH 3100,
“Transportation to Receiving Facility,” as
referenced in subsection 65E-5.260(1), F.A.C.,
and recommended form CF-MH 3001, “Ex Parte
Order for Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., or other form
provided by the court, or mandatory form CF-
MH 3052a, “Report of Law Enforcement Officer
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., or mandatory
form CF-MH 3052b, “Certificate of Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C.; and
(c) The psychiatric evaluation, including the mental
status examination or the psychological status
report.
(8) Disposition Upon Initial Mandatory Involuntary
Examination.
(a) The release of a person from a receiving
facility requires the documented approval of
a psychiatrist, clinical psychologist, or if the
receiving facility is a hospital, the release may
also be approved by an attending emergency
department physician after the completion of
an initial mandatory involuntary examination.
Recommended form CF-MH 3111, Feb. 05,
“Approval for Release of Person on Involuntary
Status from a Receiving Facility,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used for this purpose. A copy of
the form used shall be retained in the person’s
clinical record.
(b) In order to document a person’s transfer from
involuntary to voluntary status, recommended
form CF-MH 3040, “Application for Voluntary
Admission,” as referenced in paragraph 65E-
5.1302(1)(b), F.A.C., or recommended form CF-
MH 3097, “Application for Voluntary Admission –
Minors,” as referenced in subsection 65E-5.270(1),
F.A.C., completed prior to transfer, may be used.
(c) A person for whom an involuntary examination
has been initiated shall not be permitted to

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
94
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.463 F.S.)
emergency medical condition does not
exist.
(i) Within the 72-hour examination period
or, if the 72 hours ends on a weekend or
holiday, no later than the next working day
thereafter, one of the following actions must
be taken, based on the individual needs of
the patient:
1. e patient shall be released, unless he
or she is charged with a crime, in which
case the patient shall be returned to the
custody of a law enforcement ocer;
2. e patient shall be released, subject to
the provisions of subparagraph 1., for
voluntary outpatient treatment;
3. e patient, unless he or she is charged
with a crime, shall be asked to give
express and informed consent to place-
ment as a voluntary patient, and, if
such consent is given, the patient shall
be admitted as a voluntary patient; or
4. A petition for involuntary placement
shall be led in the circuit court when
outpatient or inpatient treatment is
deemed necessary. When inpatient
treatment is deemed necessary, the least
restrictive treatment consistent with the
optimum improvement of the patient’s
condition shall be made available.
When a petition is to be led for invol-
untary outpatient placement, it shall be
led by one of the petitioners specied
in s. 394.4655(3)(a). A petition for
involuntary inpatient placement shall
be led by the facility administrator.
(3) NOTICE OF RELEASE. Notice of the re-
lease shall be given to the patient’s guardian or
representative, to any person who executed a
certicate admitting the patient to the receiv-
ing facility, and to any court which ordered
the patient’s evaluation.
65E-5.2801 F.A.C.
consent to voluntary admission until after
examination by a physician to confirm his or her
ability to provide express and informed consent
to treatment. Recommended form CF-MH 3104,
“Certification of Person’s Competence to Provide
Express and Informed Consent,” as referenced in
paragraph 65E-5.170(1)(c), F.A.C., may be used
for documentation.
(d) If the facility administrator, based on facts and
expert opinions, believes the person meets the
criteria for involuntary inpatient or involuntary
outpatient placement or is incompetent to
consent to treatment, the facility shall initiate
involuntary placement within 72 hours of the
person’s arrival by filing a petition for involuntary
placement. Recommended form CF-MH 3032,
“Petition for Involuntary Inpatient Placement,”
as referenced in subparagraph 65E-5.170(1)
(d)1., F.A.C., or CF-MH 3130, “Petition for
Involuntary Outpatient Placement” as referenced
in subparagraph 65E-5.170(1)(d)2., F.A.C., may
be used for this purpose. Such petition shall be
signed by the facility administrator or designee
within the 72-hour examination period. The
petition shall be filed with the court within the
72-hour examination period or, if the 72 hours
ends on a weekend or legal holiday, no later than
the next court working day thereafter. A copy
of the completed petition shall be retained in
the person’s clinical record and a copy given to
the person and his or her duly authorized legal
decision-maker or representatives.
(e) When a person on involuntary status is released,
notice shall be given to the person’s guardian or
representative, to any individual who executed
a certificate for involuntary examination,
and to any court which ordered the person’s
examination with a copy retained in the person’s
clinical record. Recommended form CF-MH 3038,
Feb. 05, “Notice of Release or Discharge,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used for this purpose.
Involuntary examination

95 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
394.4655 Involuntary outpatient
placement.
(1) CRITERIA FOR INVOLUNTARY
OUTPATIENT PLACEMENT.
A person may be ordered to involuntary out-
patient placement upon a nding of the court
that by clear and convincing evidence:
(a) e person is 18 years of age or older;
(b)e person has a mental illness;
(c) e person is unlikely to survive safely in
the community without supervision, based
on a clinical determination;
(d)e person has a history of lack of
compliance with treatment for mental
illness;
(e) e person has:
1. At least twice within the immediately
preceding 36 months been involuntarily
admitted to a receiving or treatment
facility as dened in s. 394.455, or
has received mental health services in
a forensic or correctional facility. e
36-month period does not include any
period during which the person was
admitted or incarcerated; or
2. Engaged in one or more acts of serious
violent behavior toward self or others,
or attempts at serious bodily harm to
himself or herself or others, within the
preceding 36 months;
(f) e person is, as a result of his or her mental
illness, unlikely to voluntarily participate
in the recommended treatment plan and
either he or she has refused voluntary
placement for treatment after sucient and
conscientious explanation and disclosure of
the purpose of placement for treatment or
he or she is unable to determine for himself
or herself whether placement is necessary;
(g) In view of the person’s treatment history and
current behavior, the person is in need of
involuntary outpatient placement in order
to prevent a relapse or deterioration that
would be likely to result in serious bodily
Involuntary outpatient placement
65E-5.285 Involuntary Outpatient
Placement.
(1) Petition for Involuntary Outpatient
Placement.
(a) Each criterion alleged must be substantiated by
evidence, as follows:
1. Evidence of age must be substantiated,
whenever there is any question as to
whether the person may be age 18 or older.
2. A diagnosis of mental illness shall be
substantiated by 2 professionals as
provided in Section 394.4655(2)(a), F.S.,
who have recently examined the person
and whose observations of the person’s
condition are consistent with the statutory
definition of mental illness, pursuant to
Section 394.455(18), F.S., and the clinical
description of that diagnosis as described
in the Diagnostic and Statistical Manual
of Mental Disorders, Fourth Edition, Text
Revision, American Psychiatric Association,
which is incorporated by reference and may
be obtained from the American Psychiatric
Association, 1000 Wilson Boulevard,
Arlington, VA 22209-3901.
3. The clinical determination that a person is
unlikely to survive safely in the community
without supervision must be substantiated
by evidence of current or past behaviors.
4. The person’s history of lack of compliance
with treatment for mental illness must be
substantiated by evidence showing specific
previous incidents in which the person was
non-compliant with treatment, including
time periods in which the person was non-
compliant with treatment.
5. The person’s involuntarily admission to a
receiving or treatment facility or the mental
health services in a forensic or correctional
facility at least twice in the preceding 36
months, or the person’s acts of serious
violent behavior toward self or others or
attempted serious bodily harm to self or
others at least once during the preceding
36 months, shall be substantiated by
evidence.
6. Evidence of the unlikelihood of the
person to voluntarily participate in the

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
96
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
harm to himself or herself or others, or a
substantial harm to his or her well-being as
set forth in s. 394.463(1);
(h)It is likely that the person will benet from
involuntary outpatient placement; and
(i) All available, less restrictive alternatives
that would oer an opportunity for
improvement of his or her condition
have been judged to be inappropriate or
unavailable.
(2) INVOLUNTARY OUTPATIENT
PLACEMENT.
(a)1. A patient who is being recommended
for involuntary outpatient placement by
the administrator of the receiving facility
where the patient has been examined may
be retained by the facility after adherence
to the notice procedures provided in s.
394.4599. e recommendation must be
supported by the opinion of a psychiatrist
and the second opinion of a clinical
psychologist or another psychiatrist, both
of whom have personally examined the
patient within the preceding 72 hours,
that the criteria for involuntary outpatient
placement are met. However, in a county
having a population of fewer than
50,000, if the administrator certies that a
psychiatrist or clinical psychologist is not
available to provide the second opinion,
the second opinion may be provided by a
licensed physician who has postgraduate
training and experience in diagnosis and
treatment of mental and nervous disorders
or by a psychiatric nurse. Any second
opinion authorized in this subparagraph
may be conducted through a face-to-face
examination, in person or by electronic
means. Such recommendation must be
entered on an involuntary outpatient
placement certicate that authorizes the
receiving facility to retain the patient
pending completion of a hearing. e
certicate shall be made a part of the
patient’s clinical record.
recommended treatment plan, and either
his or her refusal of voluntary placement or
inability to determine whether placement
is necessary must be substantiated by
behaviors, events, and statements by the
person supporting this finding.
7. Evidence of the person’s treatment history
and current behavior must be presented,
including time periods of such treatment to
substantiate the conclusion that the person
needs involuntary placement in order to
prevent a relapse or deterioration that would
be likely to result in serious bodily harm to
self or others or a substantial harm to his or
her well-being.
8. Evidence must be presented to substantiate
the likelihood of how the person will benefit
from involuntary outpatient placement.
9. Evidence must be presented to substantiate
each less restrictive alternative that was
examined that would have offered an
opportunity for the improvement of the
person’s condition.
(b) Petition Filed by Receiving Facility
Administrator.
1. If a person is retained involuntarily in a
receiving facility, a petition for involuntary
outpatient placement must be filed with
the circuit court by the facility administrator
within the 72-hour examination period, or
if the 72 hours ends on a weekend or legal
holiday, the petition shall be filed no later
than the next court working day thereafter.
Recommended form CF-MH 3130, Feb.
05, “Petition for Involuntary Outpatient
Placement,” as referenced in subparagraph
65E-5.170(1)(d)2., F.A.C., may be used for this
purpose. A copy of the completed petition
shall be retained in the person’s clinical
record.
2. A petition filed by a receiving facility
administrator shall be filed in the county
where the facility is located.
3. The administrator of the receiving facility
or a designated department representative
shall identify the service provider that will
have the responsibility of developing a
treatment plan and primary responsibility
for service provision under an order for
Involuntary outpatient placement

97 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
2. If the patient has been stabilized and no
longer meets the criteria for involuntary
examination pursuant to s. 394.463(1),
the patient must be released from the
receiving facility while awaiting the
hearing for involuntary outpatient
placement. Before ling a petition for
involuntary outpatient treatment, the
administrator of a receiving facility or
a designated department representa-
tive must identify the service provider
that will have primary responsibility for
service provision under an order for in-
voluntary outpatient placement, unless
the person is otherwise participating in
outpatient psychiatric treatment and is
not in need of public nancing for that
treatment, in which case the individual,
if eligible, may be ordered to involun-
tary treatment pursuant to the existing
psychiatric treatment relationship.
3. e service provider shall prepare a writ-
ten proposed treatment plan in consul-
tation with the patient or the patient’s
guardian advocate, if appointed, for the
court’s consideration for inclusion in the
involuntary outpatient placement order.
e service provider shall also provide
a copy of the proposed treatment plan
to the patient and the administrator of
the receiving facility. e treatment plan
must specify the nature and extent of
the patient’s mental illness, address the
reduction of symptoms that necessitate
involuntary outpatient placement, and
include measurable goals and objectives
for the services and treatment that are
provided to treat the person’s mental
illness and assist the person in living and
functioning in the community or to pre-
vent a relapse or deterioration. Service
providers may select and supervise other
individuals to implement specic as-
pects of the treatment plan. e services
in the treatment plan must be deemed
Involuntary outpatient placement
involuntary outpatient placement, unless
the person is otherwise participating in
outpatient psychiatric treatment and is
not in need of public financing for that
treatment. Recommended form CF-MH 3140,
Sept. 06, “Designation of Service Provider for
Involuntary Outpatient Placement,” which
is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter may be used for this
purpose.
4. A treatment plan, complying with the
requirements of Section 394.4655, F.S., and
this rule, shall be attached to the petition,
along with a certification from the service
provider that:
a. The proposed services are available in
the person’s local community;
b. There is space available in the pro-
gram or service for the person;
c. Funding is available for the program
or service;
d. The service provider agrees to provide
those services; and
e. Proposed services have been deemed
to be clinically appropriate by a physi-
cian, clinical psychologist, clinical
social worker, mental health coun-
selor, marriage and family therapist,
or psychiatric nurse, as defined in Sec-
tion 394.455, F.S., who consults with,
is employed by, or has a contract with
the service provider.
5. Recommended form CF-MH 3145, Sept.
06, “Proposed Individualized Treatment
Plan for Involuntary Outpatient Placement
and Continued Involuntary Outpatient
Placement”, which is incorporated by
reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter
may be used for the development of a
treatment plan.
6. If the service provider developing a
treatment plan, pursuant to involuntary
outpatient placement determines the
person is in need of services that cannot be
proposed due to non-availability of services,
funding, a willing provider, or other reason,
it shall submit a completed recommended

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
98
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
clinically appropriate by a physician,
clinical psychologist, psychiatric nurse,
mental health counselor, marriage and
family therapist, or clinical social work-
er who consults with, or is employed
or contracted by, the service provider.
e service provider must certify to the
court in the proposed treatment plan
whether sucient services for improve-
ment and stabilization are currently
available and whether the service pro-
vider agrees to provide those services.
If the service provider certies that the
services in the proposed treatment plan
are not available, the petitioner may not
le the petition.
(b)If a patient in involuntary inpatient
placement meets the criteria for involuntary
outpatient placement, the administrator
of the treatment facility may, before the
expiration of the period during which the
treatment facility is authorized to retain the
patient, recommend involuntary outpatient
placement. e recommendation must be
supported by the opinion of a psychiatrist
and the second opinion of a clinical
psychologist or another psychiatrist, both
of whom have personally examined the
patient within the preceding 72 hours,
that the criteria for involuntary outpatient
placement are met. However, in a county
having a population of fewer than 50,000,
if the administrator certies that a
psychiatrist or clinical psychologist is not
available to provide the second opinion,
the second opinion may be provided by a
licensed physician who has postgraduate
training and experience in diagnosis and
treatment of mental and nervous disorders
or by a psychiatric nurse. Any second
opinion authorized in this subparagraph
may be conducted through a face-to-face
examination, in person or by electronic
means. Such recommendation must be
entered on an involuntary outpatient
form CF-MH 3150, Feb. 05, “Notice to
Department of Children and Families of Non-
Filing of Petition for Involuntary Outpatient
Placement or Diminished Treatment Plan
Due to Non-Availability of Services or
Funding,” which is incorporated by reference
and may be obtained pursuant to Rule 65E-
5.120, F.A.C., of this rule chapter.
7. A copy of the petition for involuntary
outpatient placement and the proposed
treatment plan shall be provided within
1 working day after filing by the clerk of
the court to the respondent, department,
guardian or representative, state attorney,
and counsel for the respondent. A notice
of filing of the petition shall be provided
by the clerk of court using recommended
form CF-MH 3021, Feb. 05, “Notice of
Petition for Involuntary Placement,” which
is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter, or other form adopted
by the court.
(c) Petition Filed by Treatment Facility
Administrator.
1. A petition for involuntary outpatient
placement filed by a treatment facility
administrator shall be filed prior to the
expiration of the involuntary inpatient
placement order in the county where the
person will be living after discharge from the
treatment facility.
2. A copy of form CF-MH 7001, Jan. 98, “State
Mental Health Facility Discharge Form,” as
referenced in subsection 65E-5.1305(1),
F.A.C., shall be attached to the petition.
3. The service provider designated by
the department that will have primary
responsibility for service provision shall
provide a certification to the court,
attached to the petition, that the services
recommended in the discharge plan are
available in the local community and
that the provider agrees to provide those
services.
4. The petition shall have attached an
individualized treatment or service plan
that addresses the needs identified in the
discharge plan developed by the treatment
Involuntary outpatient placement

99 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
placement certicate, and the certicate
must be made a part of the patient’s clinical
record.
(c) 1. e administrator of the treatment
facility shall provide a copy of the
involuntary outpatient placement
certicate and a copy of the state mental
health discharge form to a department
representative in the county where the
patient will be residing. For persons
who are leaving a state mental health
treatment facility, the petition for
involuntary outpatient placement must
be led in the county where the patient
will be residing.
2. e service provider that will have primary
responsibility for service provision shall be
identied by the designated department
representative prior to the order for invol-
untary outpatient placement and must,
prior to ling a petition for involuntary
outpatient placement, certify to the court
whether the services recommended in the
patient’s discharge plan are available in the
local community and whether the service
provider agrees to provide those services.
e service provider must develop with
the patient, or the patient’s guardian advo-
cate, if appointed, a treatment or service
plan that addresses the needs identied
in the discharge plan. e plan must be
deemed to be clinically appropriate by a
physician, clinical psychologist, psychiatric
nurse, mental health counselor, marriage
and family therapist, or clinical social
worker, as dened in this chapter, who
consults with, or is employed or contract-
ed by, the service provider.
3. If the service provider certies that
the services in the proposed treatment
or service plan are not available, the
petitioner may not le the petition.
(3) PETITION FOR INVOLUNTARY
OUTPATIENT PLACEMENT.
(a) A petition for involuntary outpatient
Involuntary outpatient placement
facility as represented by form CF-MH
3145, “Proposed Individualized Treatment
Plan for Involuntary Outpatient Placement
and Continued Involuntary Outpatient
Placement,” as referenced in subparagraph
65E-5.285(1)(b)5., F.A.C. The plan must have
been deemed to be clinically appropriate by
a physician, clinical psychologist, psychiatric
nurse, mental health counselor, marriage
and family therapist, or clinical social worker,
as defined in Section 394.455, F.S.
5. A copy of the petition for involuntary
outpatient placement and the proposed
treatment plan shall be provided within
1 working day after filing by the clerk of
the court to the respondent, department,
guardian or representative, state attorney,
and counsel for the respondent. A notice of
filing of the petition shall be provided by
the clerk of court using recommended form
CF-MH 3021, Feb. 05, “Notice of Petition for
Involuntary Placement,” as referenced in
subparagraph 65E-5.285(1)(b)7., F.A.C., or
other equivalent form adopted by the court.
(2) Hearing on Petition for Involuntary Outpatient
Placement.
(a) The clerk of court shall provide notice of the
hearing, using recommended form CF-MH
3021, Feb. 05, “Notice of Petition for Involuntary
Placement”, as referenced in subparagraph 65E-
5.285(1)(b)7., F.A.C., or other form used by the
court.
(b) A hearing on the petition for involuntary
outpatient placement shall be conducted within
5 working days after the filing of the petition
in the county in which the petition is filed. The
person is entitled, with the concurrence of
counsel, to at least 1 continuance of the hearing,
for a period of up to 4 weeks. Recommended
form CF-MH 3113, Feb. 05, “Notice to Court
– Request for Continuance of Involuntary
Placement Hearing,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter may be
used for this purpose.
(c) The person and his representative or guardian
shall be informed by the court of the right to
an independent expert examination and that if
the person cannot afford such an examination,

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
100
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
placement may be led by:
1. e administrator of a receiving facility; or
2. e administrator of a treatment facility.
(b) Each required criterion for involuntary
outpatient placement must be alleged and
substantiated in the petition for involuntary
outpatient placement. A copy of the
certicate recommending involuntary
outpatient placement completed by a
qualied professional specied in subsection
(2) must be attached to the petition. A copy
of the proposed treatment plan must be
attached to the petition. Before the petition
is led, the service provider shall certify that
the services in the proposed treatment plan
are available. If the necessary services are not
available in the patient’s local community to
respond to the person’s individual needs, the
petition may not be led.
(c) e petition for involuntary outpatient
placement must be led in the county
where the patient is located, unless the
patient is being placed from a state
treatment facility, in which case the
petition must be led in the county where
the patient will reside. When the petition
has been led, the clerk of the court shall
provide copies of the petition and the
proposed treatment plan to the department,
the patient, the patient’s guardian or
representative, the state attorney, and the
public defender or the patient’s private
counsel. A fee may not be charged for ling
a petition under this subsection.
(4) APPOINTMENT OF COUNSEL.
Within 1 court working day after the l-
ing of a petition for involuntary outpatient
placement, the court shall appoint the public
defender to represent the person who is the
subject of the petition, unless the person is
otherwise represented by counsel. e clerk of
the court shall provide for one. Recommended
form CF-MH 3022, Feb. 05, “Application for
Appointment of Independent Expert Examiner,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of
this rule chapter may be used for this purpose.
(d) Recommended form CF-MH 3033, Feb. 05,
“Notification to Court of Withdrawal of Petition
on Involuntary Inpatient or Involuntary
Outpatient Placement,” which is incorporated
by reference and may be obtained pursuant to
Rule 65E-5.120, F.A.C., of this rule chapter may
be used if the facility administrator seeks to
withdraw the petition for involuntary outpatient
placement prior to the hearing. The facility will
retain a copy in the person’s clinical record. When
a facility withdraws a petition for involuntary
placement, it shall notify the court, state
attorney, public defender or other attorney for
the person, and guardian or representative by
telephone within 1 business day of its decision
to withdraw the petition, unless such decision
is made within 24 hours prior to the hearing.
In such cases, the notification must be made
immediately.
(e) If the court determines the person does not meet
the criteria for involuntary outpatient placement,
but instead meets the criteria for involuntary
inpatient placement use of recommended
form CF-MH 3001, Feb. 05, “Ex Parte Order for
Involuntary Inpatient Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., or other order
used by the court, may be used.
(f) If the court determines the person meets the
criteria for involuntary assessment, protective
custody, or involuntary admission pursuant to
Section 397.675, F.S., and issues an order for one
of the same, recommended form CF-MH 3114,
Feb. 05, “Order Requiring Involuntary Assessment
and Stabilization for Substance Abuse and
for Baker Act Discharge of Person,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, or other order entered by the court, may
be used.
the court shall immediately notify the pub-
lic defender of the appointment. e public
defender shall represent the person until the
petition is dismissed, the court order expires,
(3) Court Order.
(a) If the court concludes that the person meets the
criteria for involuntary outpatient placement
pursuant to Section 394.4655, F.S., it shall
Involuntary outpatient placement

101 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
or the patient is discharged from involun-
tary outpatient placement. An attorney who
represents the patient shall have access to the
patient, witnesses, and records relevant to the
presentation of the patient’s case and shall rep-
resent the interests of the patient, regardless of
the source of payment to the attorney.
(5) CONTINUANCE OF HEARING.
e patient is entitled, with the concurrence of
the patient’s counsel, to at least one continu-
ance of the hearing. e continuance shall be
for a period of up to 4 weeks.
(6) HEARING ON INVOLUNTARY
OUTPATIENT PLACEMENT.
(a)1. e court shall hold the hearing on
involuntary outpatient placement
within 5 working days after the ling
of the petition, unless a continuance is
granted. e hearing shall be held in the
county where the petition is led, shall
be as convenient to the patient as is
consistent with orderly procedure, and
shall be conducted in physical settings
not likely to be injurious to the patient’s
condition. If the court nds that the
patient’s attendance at the hearing is
not consistent with the best interests of
the patient and if the patient’s counsel
does not object, the court may waive
the presence of the patient from all or
any portion of the hearing. e state
attorney for the circuit in which the
patient is located shall represent the
state, rather than the petitioner, as the
real party in interest in the proceeding.
2. e court may appoint a master to
preside at the hearing. One of the pro-
fessionals who executed the involuntary
outpatient placement certicate shall be
a witness. e patient and the patient’s
guardian or representative shall be in-
formed by the court of the right to an
independent expert examination. If the
patient cannot aord such an examina-
tion, the court shall provide for one. e
Involuntary outpatient placement
prepare an order. Recommended form CF-MH
3155, Feb. 05, “Order for Involuntary Outpatient
Placement or Continued Involuntary Outpatient
Placement,” which is incorporated by reference
and may be obtained pursuant to Rule 65E-
5.120, F.A.C., of this rule chapter, or other order
entered by the court, may be used for this
purpose. This signed order shall be given to
the person, guardian, guardian advocate or
representative, counsel for the person, state
attorney, and administrator of the receiving
or treatment facility, with a copy of the order
retained in the person’s clinical record.
(b) Upon receipt of the court order for involuntary
outpatient placement, the administrator of a
treatment facility will provide a copy of the court
order and adequate documentation of a person’s
mental illness to the service provider, including
any advance directives, a psychiatric evaluation
of the person, and any evaluations of the person
performed by a clinical psychologist, mental
health counselor, marriage and family therapist,
or clinical social worker.
(c) In order for the department to implement
the provisions of Section 394.463(2)(e), F.S.,
and to ensure that the Agency for Health
Care Administration will be able to analyze
the data it receives pursuant to that section,
service providers shall forward copies of each
recommended form CF-MH 3155, “Order for
Involuntary Outpatient Placement or Continued
Involuntary Outpatient Placement,” as referenced
in paragraph 65E-5.285(3)(a), F.A.C., or other
order provided by the court, accompanied by
mandatory form CF-MH 3118, “Cover Sheet
to Agency for Health Care Administration,” as
referenced in subsection 65E-5.280(5), F.A.C., to:
BA Reporting Center, FMHI-MHC 2637, 13301
Bruce B. Downs Boulevard, Tampa, Florida 33612-
3807.
(d) At any time material modifications are proposed
to the court ordered treatment plan for which
the person and his or her substitute decision-
maker if any, agree, the service provider shall
submit recommended form CF-MH 3160, Feb.
05, “Notice to Court of Modification to Treatment
Plan for Involuntary Outpatient Placement and/
or Petition Requesting Approval of Material
Modifications to Plan,” which is incorporated

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
102
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
independent expert’s report shall be con-
dential and not discoverable, unless the
expert is to be called as a witness for the
patient at the hearing. e court shall al-
low testimony from individuals, including
family members, deemed by the court to
be relevant under state law, regarding the
person’s prior history and how that prior
history relates to the person’s current con-
dition. e testimony in the hearing must
be given under oath, and the proceedings
must be recorded. e patient may refuse
to testify at the hearing.
(b)1. If the court concludes that the patient
meets the criteria for involuntary
outpatient placement pursuant to
subsection (1), the court shall issue
an order for involuntary outpatient
placement. e court order shall be for
a period of up to 6 months. e order
must specify the nature and extent of
the patient’s mental illness. e order of
the court and the treatment plan shall
be made part of the patient’s clinical
record. e service provider shall
discharge a patient from involuntary
outpatient placement when the order
expires or any time the patient no
longer meets the criteria for involuntary
placement. Upon discharge, the service
provider shall send a certicate of
discharge to the court.
2. e court may not order the depart-
ment or the service provider to provide
services if the program or service is not
available in the patient’s local commu-
nity, if there is no space available in the
program or service for the patient, or if
funding is not available for the program
or service. A copy of the order must
be sent to the Agency for Health Care
Administration by the service provider
within 1 working day after it is received
from the court. After the placement
order is issued, the service provider and
by reference and may be obtained pursuant
to Rule 65E-5.120, F.A.C., of this rule chapter or
other form adopted by the court. Each person
undergoing involuntary outpatient placement
and his or her substitute decision-maker if
any, must be given a copy of this form by the
service provider, and if requested, the service
provider shall assist the person or substitute
decision-maker in its completion. If the person
or his substitute decision-maker object to
the modifications proposed by the service
provider or wish to propose modifications not
proposed by the service provider, recommended
form CF-MH 3160, Feb. 05, “Notice to Court of
Modification to Treatment Plan for Involuntary
Outpatient Placement and/or Petition
Requesting Approval of Material Modifications
to Plan,” as referenced in this subsection, or other
form adopted by the court may be used.
(e) If a physician has determined the person
who is subject to a court order for involuntary
outpatient placement has failed or has refused
to comply with the treatment ordered by the
court, and in his or her clinical judgment, efforts
were made to solicit compliance and the person
meets the criteria for involuntary examination,
the person may be brought to a receiving facility
pursuant to Section 394.463, F.S. Mandatory
form CF-MH 3052b, “Certificate of a Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., shall be used.
(4) Continued Involuntary Outpatient Placement.
(a) A request for continued involuntary outpatient
placement by the service provider administrator
shall be filed prior to the expiration of the
period for which the treatment was ordered.
Recommended form CF-MH 3180, Feb. 05,
“Petition Requesting Authorization for Continued
Involuntary Outpatient Placement,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, may be used as documentation of that
request. The petition shall be filed with the clerk
of the circuit court in the county where the
person who is the subject of the petition resides.
(b) The petition requesting authorization for
continued involuntary outpatient placement
shall contain the signed statement of the
person’s physician or clinical psychologist
Involuntary outpatient placement

103 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
the patient may modify provisions of
the treatment plan. For any material
modication of the treatment plan to
which the patient or the patient’s guard-
ian advocate, if appointed, does agree,
the service provider shall send notice
of the modication to the court. Any
material modications of the treatment
plan which are contested by the patient
or the patient’s guardian advocate, if
appointed, must be approved or disap-
proved by the court consistent with
subsection (2).
3. If, in the clinical judgment of a physi-
cian, the patient has failed or has refused
to comply with the treatment ordered
by the court, and, in the clinical judg-
ment of the physician, eorts were made
to solicit compliance and the patient
may meet the criteria for involuntary
examination, a person may be brought
to a receiving facility pursuant to s.
394.463. If, after examination, the
patient does not meet the criteria for in-
voluntary inpatient placement pursuant
to s. 394.467, the patient must be dis-
charged from the receiving facility. e
involuntary outpatient placement order
shall remain in eect unless the service
provider determines that the patient no
longer meets the criteria for involuntary
outpatient placement or until the order
expires. e service provider must deter-
mine whether modications should be
made to the existing treatment plan and
must attempt to continue to engage the
patient in treatment. For any material
modication of the treatment plan to
which the patient or the patient’s guard-
ian advocate, if appointed, does agree,
the service provider shall send notice
of the modication to the court. Any
material modications of the treatment
plan which are contested by the patient
or the patient’s guardian advocate, if
Involuntary outpatient placement
justifying the request and shall be accompanied
by the following additional documentation:
1. Evidence justifying the request by
the physician or clinical psychologist
for continued involuntary outpatient
placement, including how the person meets
each of the statutorily required criteria;
2. A brief summary of the person’s treatment
during the time he or she was subject to
involuntary outpatient placement; and
3. An individualized plan of continued
treatment.
(c) If the service provider developing a treatment
plan pursuant to involuntary outpatient
placement determines the person is in need
of services that cannot be proposed due to
non-availability of services, funding, a willing
provider, or other reason, it shall submit
completed recommended form CF-MH 3150,
Feb. 05, “Notice to Department of Children and
Families of Non-Filing of Petition for Involuntary
Outpatient Placement or Diminished Treatment
Plan Due to Non-Availability of Services or
Funding,” as referenced in subparagraph 65E-
5.285(1)(b)6., F.A.C. This completed form shall be
submitted to the BA Reporting Center, FMHI-
MHC 2637, 13301 Bruce B. Downs Boulevard,
Tampa, Florida 33612-3807.
(d) Each criterion alleged must be substantiated by
evidence.
(e) The clerk of court shall provide notice of the
hearing, using recommended form CF-MH
3021, Feb. 05, “Notice of Petition for Involuntary
Placement,” as referenced in subparagraph 65E-
5.285(1)(b)7., F.A.C., or other form approved by
the court.
(f ) The person and his or her attorney may agree
to a period of continued outpatient placement
without a court hearing. Should such a hearing
be waived, recommended form CF-MH 3185,
Feb. 05, “Notice to Court of Waiver of Continued
Involuntary Outpatient Placement Hearing and
Request for Order,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter may be
used for this purpose.
(g) Use of recommended form CF-MH 3033, Feb.
05, “Notification to Court of Withdrawal of
Petition on Involuntary Inpatient or Involuntary

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
104
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
appointed, must be approved or disap-
proved by the court consistent with
subsection (2).
(c) If, at any time before the conclusion of the
initial hearing on involuntary outpatient
placement, it appears to the court that
the person does not meet the criteria for
involuntary outpatient placement under
this section but, instead, meets the criteria
for involuntary inpatient placement, the
court may order the person admitted for
involuntary inpatient examination under
s. 394.463. If the person instead meets
the criteria for involuntary assessment,
protective custody, or involuntary admission
pursuant to s. 397.675, the court may order
the person to be admitted for involuntary
assessment for a period of 5 days pursuant to
s. 397.6811. ereafter, all proceedings shall
be governed by chapter 397.
(d)At the hearing on involuntary outpatient
placement, the court shall consider
testimony and evidence regarding the
patient’s competence to consent to
treatment. If the court nds that the patient
is incompetent to consent to treatment,
it shall appoint a guardian advocate as
provided in s. 394.4598. e guardian
advocate shall be appointed or discharged
in accordance with s. 394.4598.
(e) e administrator of the receiving facility
or the designated department representative
shall provide a copy of the court order and
adequate documentation of a patient’s mental
illness to the service provider for involuntary
outpatient placement. Such documentation
must include any advance directives made
by the patient, a psychiatric evaluation of the
patient, and any evaluations of the patient
performed by a clinical psychologist or a
clinical social worker.
Outpatient Placement,” as referenced in
paragraph 65E-5.285(2)(d), F.A.C., if the facility
administrator seeks to withdraw the petition for
continued involuntary outpatient placement
prior to the hearing. The facility will retain a copy
in the person’s clinical record. When a facility
withdraws a petition for continued involuntary
outpatient placement, it shall notify the court,
state attorney, public defender or other attorney
for the person, and guardian or representative by
telephone within 1 business day of its decision
to withdraw the petition, unless such decision
is made within 24 hours prior to the hearing.
In such cases, the notification must be made
immediately.
(h) Based on the findings at the hearing, the court
may extend the period of involuntary outpatient
placement, release the person from involuntary
outpatient placement, or find the person eligible
for voluntary status. Recommended form CF-MH
3155, Feb. 05, “Order for Involuntary Outpatient
Placement or Continued Involuntary Outpatient
Placement,” as referenced in paragraph 65E-
5.285(3)(a), F.A.C., or other equivalent form
adopted by the court may be used. A copy of the
completed order shall be filed in the person’s
clinical record and a copy shall be provided to
the person, attorney, facility administrator, and
guardian, guardian advocate or representative.
(i) IIn order for the department to implement
the provisions of Section 394.463(2)(e), F.S.,
and to ensure that the Agency for Health
Care Administration will be able to analyze
the data it receives pursuant to that section,
service providers shall forward copies of each
recommended form CF-MH 3155, “Order for
Involuntary Outpatient Placement or Continued
Involuntary Outpatient Placement,” as referenced
in paragraph 65E-5.285(3)(a), F.A.C., or other
order provided by the court, accompanied by
mandatory form CF-MH 3118, “Cover Sheet
to Agency for Health Care Administration,” as
referenced in subsection 65E-5.280(5), F.A.C., to:
BA Reporting Center, FMHI-MHC 2637, 13301
Bruce B. Downs Boulevard, Tampa, Florida 33612-
3807.
(j) If at any time material modifications are
proposed to the court ordered treatment plan
to which the person and his or her substitute
Involuntary outpatient placement

105 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
(7) PROCEDURE FOR CONTINUED
INVOLUNTARY OUTPATIENT
PLACEMENT.
(a)1. If the person continues to meet the
criteria for involuntary outpatient
placement, the service provider shall,
before the expiration of the period
during which the treatment is ordered
for the person, le in the circuit court
a petition for continued involuntary
outpatient placement.
2. e existing involuntary outpatient
placement order remains in eect until
disposition on the petition for contin-
ued involuntary outpatient placement.
3. A certicate shall be attached to the pe-
tition which includes a statement from
the person’s physician or clinical psy-
chologist justifying the request, a brief
description of the patient’s treatment
during the time he or she was involun-
tarily placed, and an individualized plan
of continued treatment.
4. e service provider shall develop the
individualized plan of continued treat-
ment in consultation with the patient
or the patient’s guardian advocate, if
appointed. When the petition has been
led, the clerk of the court shall pro-
vide copies of the certicate and the
individualized plan of continued treat-
ment to the department, the patient, the
patient’s guardian advocate, the state at-
torney, and the patient’s private counsel
or the public defender.
(b)Within 1 court working day after the ling
of a petition for continued involuntary
outpatient placement, the court shall
appoint the public defender to represent the
person who is the subject of the petition,
unless the person is otherwise represented
by counsel. e clerk of the court shall
immediately notify the public defender of
such appointment. e public defender
shall represent the person until the petition
Involuntary outpatient placement
decision-maker, if any, agree, the service provider
shall submit recommended form CF-MH 3160,
Feb. 05, “Notice to Court of Modification to
Treatment Plan for Involuntary Outpatient
Placement and/or Petition Requesting Approval
of Material Modifications to Plan,” as referenced
in paragraph 65E-5.285(3)(d), F.A.C., or other
form adopted by the court. If the person or
his substitute decision-maker object to the
modifications proposed by the service provider
or wish to propose modifications not proposed
by the service provider, recommended form
CF-MH 3160, Feb. 05, “Notice to Court of
Modification to Treatment Plan for Involuntary
Outpatient Placement and/or Petition
Requesting Approval of Material Modifications to
Plan,” as referenced in paragraph 65E-5.285(3)(d),
F.A.C., or other form adopted by the court may
be used.
(k) If a physician has determined the person
who is subject to a court order for involuntary
outpatient placement has failed or has refused
to comply with the treatment ordered by the
court, and in his or her clinical judgment, efforts
were made to solicit compliance and the person
meets the criteria for involuntary examination,
the person may be brought to a receiving facility
pursuant to Section 394.463, F.S. Mandatory
form CF-MH 3052b, “Certificate of a Professional
Initiating Involuntary Examination,” as referenced
in subsection 65E-5.260(1), F.A.C., shall be used.
(5) Discharge from Involuntary Outpatient
Placement.
(a) At any time a person no longer meets each of
the criteria for involuntary outpatient placement,
the administrator of the service provider shall
discharge the person from treatment or transfer
the person, if the person is able and willing
to provide express and informed consent, to
voluntary status.
(b) The administrator of the service provider will
provide notification to the person, guardian,
guardian advocate, representative, attorney
for the person, and the court that ordered such
treatment, with a copy placed in the person’s
clinical record. Recommended form CF-MH
3038, Feb. 05, “Notice of Release or Discharge,” as
referenced in paragraph 65E-5.2801(8)(e), F.A.C.,
may be used for this purpose.

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
106
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
Involuntary outpatient placement
is dismissed or the court order expires or
the patient is discharged from involuntary
outpatient placement. Any attorney
representing the patient shall have access to
the patient, witnesses, and records relevant
to the presentation of the patient’s case and
shall represent the interests of the patient,
regardless of the source of payment to the
attorney.
(c) Hearings on petitions for continued
involuntary outpatient placement shall
be before the circuit court. e court
may appoint a master to preside at the
hearing. e procedures for obtaining an
order pursuant to this paragraph shall be
in accordance with subsection (6), except
that the time period included in paragraph
(1)(e) is not applicable in determining the
appropriateness of additional periods of
involuntary outpatient placement.
(d) Notice of the hearing shall be provided as
set forth in s. 394.4599. e patient and
the patient’s attorney may agree to a period
of continued outpatient placement without
a court hearing.
(e) e same procedure shall be repeated before
the expiration of each additional period the
patient is placed in treatment.
(f ) If the patient has previously been found
incompetent to consent to treatment, the
court shall consider testimony and evidence
regarding the patient’s competence.
Section 394.4598 governs the discharge
of the guardian advocate if the patient’s
competency to consent to treatment has
been restored.
(c) At any time a person who is subject to an
order for involuntary outpatient placement or
continued involuntary outpatient placement,
or the guardian, guardian advocate, health care
surrogate or proxy, or attorney representing
the person, believes any one of the criteria
for involuntary outpatient placement are
no longer met, a petition for termination of
an involuntary outpatient placement order
may be filed with the circuit court having
jurisdiction. Recommended form CF-MH 3170,
Feb. 05, “Petition for Termination of Involuntary
Outpatient Placement Order,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, or other form adopted by the court may
be used for this purpose. If the court determines
to conduct a hearing on the petition, notice of
the hearing shall be provided by the clerk of
court, pursuant to Section 394.4599, F.S.
(Chapter 394.4655 F.S.)
65E-5.285 F.A.C.
See Appendix K for extensive
information on Involuntary
Outpatient Placement

107 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5.290 F.A.C.
394.467 Involuntary inpatient
placement.
(1) CRITERIA. A person may be placed in invol-
untary inpatient placement for treatment upon
a nding of the court by clear and convincing
evidence that:
(a) He or she is mentally ill and because of his
or her mental illness:
1. a. He or she has refused voluntary
placement for treatment after suf-
cient and conscientious explana-
tion and disclosure of the purpose of
placement for treatment; or
b. He or she is unable to determine for
himself or herself whether placement
is necessary; and
2. a. He or she is manifestly incapable
of surviving alone or with the help
of willing and responsible family or
friends, including available alterna-
tive services, and, without treatment,
is likely to suer from neglect or
refuse to care for himself or herself,
and such neglect or refusal poses a
real and present threat of substantial
harm to his or her well-being; or
b. ere is substantial likelihood that
in the near future he or she will
inict serious bodily harm on him-
self or herself or another person, as
evidenced by recent behavior caus-
ing, attempting, or threatening such
harm; and
(b)All available less restrictive treatment
alternatives which would oer an
opportunity for improvement of his or
her condition have been judged to be
inappropriate.
(2) ADMISSION TO A TREATMENT
FACILITY. A patient may be retained by a
receiving facility or involuntarily placed in a
treatment facility upon the recommendation
of the administrator of the receiving facility
where the patient has been examined and after
65E-5.290 Involuntary Inpatient Placement.
(1) If a person is retained involuntarily after an
involuntary examination is conducted, a petition
for involuntary inpatient placement or involuntary
outpatient placement shall be filed with the court
by the facility administrator within the 72-hour
examination period, or if the 72 hours ends on
a weekend or legal holiday, the petition shall be
filed no later than the next court working day
thereafter. Recommended form CF-MH 3032,
“Petition for Involuntary Inpatient Placement,” as
referenced in subparagraph 65E-5.170(1)(d)1., F.A.C.,
or recommended form CF-MH 3130, “Petition for
Involuntary Outpatient Placement,” as referenced
in subparagraph 65E-5.170(1)(d)2., F.A.C., or other
forms adopted by the court may be used for this
purpose. A copy of the completed petition shall be
retained in the person’s clinical record.
(2) Each criterion alleged must be substantiated by
evidence.
(3) Use of recommended form CF-MH 3021, Feb. 05,
“Notice of Petition for Involuntary Placement,” as
referenced in subparagraph 65E-5.285(1)(b)7., F.A.C.,
or other form used by the court, when properly
completed, will satisfy the requirements of Section
394.4599, F.S. A copy of that completed form, or its
equivalent, shall be retained in the person’s clinical
record. Whenever potential involuntary inpatient
placement in a state treatment facility is proposed,
a copy of the completed notice form shall also be
provided to the designated community mental
health center or clinic for purposes of conducting a
transfer evaluation.
(4) Recommended form CF-MH 3113, Feb. 05, “Notice
to Court – Request for Continuance of Involuntary
Placement Hearing,” as referenced in paragraph
65E-5.285(2)(b), F.A.C., may be used by the counsel
representing a person in requesting a continuance.
A completed copy of the form used shall be
provided to the facility administrator for retention in
the person’s clinical record.
(5) Recommended form CF-MH 3022, Feb. 05,
“Application for Appointment of Independent
Expert Examiner,” as referenced in paragraph 65E-
5.285(2)(c), F.A.C., may be used to request the expert
examiner.
(6) Recommended form CF-MH 3033, Feb. 05,
“Notification to Court of Withdrawal of Petition on
Involuntary inpatient placement

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
108
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5.290 F.A.C.
adherence to the notice and hearing procedures
provided in s. 394.4599. e recommendation
must be supported by the opinion of a
psychiatrist and the second opinion of a clinical
psychologist or another psychiatrist, both of
whom have personally examined the patient
within the preceding 72 hours, that the criteria
for involuntary inpatient placement are met.
However, in a county that has a population of
fewer than 50,000, if the administrator certies
that a psychiatrist or clinical psychologist is
not available to provide the second opinion,
the second opinion may be provided by a
licensed physician who has postgraduate
training and experience in diagnosis and
treatment of mental and nervous disorders or
by a psychiatric nurse. Any second opinion
authorized in this subsection may be conducted
through a face-to-face examination, in person
or by electronic means. Such recommendation
shall be entered on an involuntary inpatient
placement certicate that authorizes the
receiving facility to retain the patient pending
transfer to a treatment facility or completion of
a hearing.
(3) PETITION FOR INVOLUNTARY INPA-
TIENT PLACEMENT. e administrator of
the facility shall le a petition for involuntary
inpatient placement in the court in the county
where the patient is located. Upon ling, the
clerk of the court shall provide copies to the
department, the patient, the patient’s guardian
or representative, and the state attorney and
public defender of the judicial circuit in which
the patient is located. No fee shall be charged for
the ling of a petition under this subsection.
(4) APPOINTMENT OF COUNSEL. Within 1
court working day after the ling of a petition
for involuntary inpatient placement, the court
shall appoint the public defender to represent
the person who is the subject of the petition,
unless the person is otherwise represented
by counsel. e clerk of the court shall im-
mediately notify the public defender of such
appointment. Any attorney representing the
Involuntary Inpatient or Outpatient Placement,”
as referenced in paragraph 65E-5.285(2)(d),
F.A.C., may be used if the facility administrator
seeks to withdraw the petition for involuntary
placement prior to the hearing. The facility shall
retain a copy in the person’s clinical record. When
a facility withdraws a petition for involuntary
inpatient placement, it shall notify the court, state
attorney, attorney for the person, and guardian
or representative by telephone within 1 business
day of its decision to withdraw the petition, unless
such decision is made within 24 hours prior to the
hearing. In such cases, the notification must be
made immediately. In all cases involving potential
involuntary inpatient placement in a state treatment
facility, a copy of the notification form shall also
be provided to the designated community mental
health center or clinic responsible for conducting a
transfer evaluation.
(7) If the court determines the person meets the
criteria for involuntary assessment, protective
custody, or involuntary admission pursuant
to Section 397.675, F.S., and issues an order,
recommended form CF-MH 3114, Feb. 05, “Order
Requiring Involuntary Assessment and Stabilization
for Substance Abuse and for Baker Act Discharge of
Person,” as referenced in paragraph 65E-5.285(2)(g),
F.A.C., or other order used by the court, may be used
for this purpose.
(8) If at any time prior to the conclusion of the hearing
on involuntary inpatient placement, the person
instead meets the criteria for involuntary outpatient
placement, the court may order the person
evaluated for involuntary outpatient placement.
Recommended form CF-MH 3115, Feb. 05, “Order
Requiring Evaluation for Involuntary Outpatient
Placement,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter, or other order adopted by the
court, may be used.
(9) If the court concludes that the person meets
the criteria for involuntary inpatient placement
pursuant to Section 394.467, F.S., it shall prepare an
order. Recommended form CF-MH 3008, “Order for
Involuntary Inpatient Placement,” as referenced in
paragraph 65E-5.1302(1)(b), F.A.C., or other order
used by the court, may be used for this purpose. This
signed order shall be given to the person, guardian,
guardian advocate or representative, counsel for
Involuntary inpatient placement

Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5.290 F.A.C.
patient shall have access to the patient, wit-
nesses, and records relevant to the presentation
of the patient’s case and shall represent the
interests of the patient, regardless of the source
of payment to the attorney.
(5) CONTINUANCE OF HEARING.
e patient is entitled, with the concurrence of
the patient’s counsel, to at least one continu-
ance of the hearing. e continuance shall be
for a period of up to 4 weeks.
(6) HEARING ON INVOLUNTARY
INPATIENT PLACEMENT.
(a) 1. e court shall hold the hearing on
involuntary inpatient placement within
5 days, unless a continuance is granted.
e hearing shall be held in the county
where the patient is located and shall be
as convenient to the patient as may be
consistent with orderly procedure and
shall be conducted in physical settings
not likely to be injurious to the patient’s
condition. If the court nds that the
patient’s attendance at the hearing is
not consistent with the best interests of
the patient, and the patient’s counsel
does not object, the court may waive
the presence of the patient from all or
any portion of the hearing. e state
attorney for the circuit in which the
patient is located shall represent the
state, rather than the petitioning facility
administrator, as the real party in
interest in the proceeding.
2. e court may appoint a general or spe-
cial magistrate to preside at the hearing.
One of the professionals who executed
the involuntary inpatient placement
certicate shall be a witness. e patient
and the patient’s guardian or representa-
tive shall be informed by the court of the
right to an independent expert examina-
tion. If the patient cannot aord such
an examination, the court shall provide
for one. e independent expert’s report
shall be condential and not discover-
Involuntary inpatient placement
the person, state attorney, and administrator of the
receiving or treatment facility, with a copy of the
order retained in the person’s clinical record.
(10) In order for the department to implement the
provisions of Section 394.463(2)(e), F.S., and
to ensure that the Agency for Health Care
Administration will be able to analyze the data
it receives pursuant to that section, designated
receiving facilities and treatment facilities shall
forward copies of each recommended form CF-MH
3008, “Order for Involuntary Inpatient Placement,”
as referenced in paragraph 65E-5.1302(1)(b), F.A.C.,
or other order provided by the court, accompanied
by mandatory form CF-MH 3118, “Cover Sheet
to Agency for Health Care Administration,” as
referenced in subsection 65E-5.280(5), F.A.C., to: BA
Reporting Center, FMHI-MHC 2637, 13301 Bruce B.
Downs Boulevard, Tampa, Florida 33612-3807.
See Appendix J for extensive
information on Involuntary
Inpatient Placement
109
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
110
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5. F.A.C.
able, unless the expert is to be called as a
witness for the patient at the hearing. e
testimony in the hearing must be given
under oath, and the proceedings must
be recorded. e patient may refuse to
testify at the hearing.
(b) If the court concludes that the patient
meets the criteria for involuntary inpatient
placement, it shall order that the patient be
transferred to a treatment facility or, if the
patient is at a treatment facility, that the
patient be retained there or be treated at any
other appropriate receiving or treatment
facility, or that the patient receive services
from a receiving or treatment facility, on an
involuntary basis, for a period of up to 6
months. e order shall specify the nature
and extent of the patient’s mental illness.
e facility shall discharge a patient any time
the patient no longer meets the criteria for
involuntary inpatient placement, unless the
patient has transferred to voluntary status.
(c) If at any time prior to the conclusion of the
hearing on involuntary inpatient placement
it appears to the court that the person
does not meet the criteria for involuntary
inpatient placement under this section, but
instead meets the criteria for involuntary
outpatient placement, the court may order the
person evaluated for involuntary outpatient
placement pursuant to s. 394.4655. e
petition and hearing procedures set forth
in s. 394.4655 shall apply. If the person
instead meets the criteria for involuntary
assessment, protective custody, or involuntary
admission pursuant to s. 397.675, then the
court may order the person to be admitted
for involuntary assessment for a period of 5
days pursuant to s. 397.6811. ereafter, all
proceedings shall be governed by chapter 397.
(d)At the hearing on involuntary inpatient
placement, the court shall consider
testimony and evidence regarding the
patient’s competence to consent to
treatment. If the court nds that the patient
Involuntary inpatient placement

111 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5.300 F.A.C.
is incompetent to consent to treatment,
it shall appoint a guardian advocate as
provided in s. 394.4598.
(e) e administrator of the receiving facility
shall provide a copy of the court order and
adequate documentation of a patient’s mental
illness to the administrator of a treatment
facility whenever a patient is ordered for
involuntary inpatient placement, whether by
civil or criminal court. e documentation
shall include any advance directives made
by the patient, a psychiatric evaluation
of the patient, and any evaluations of the
patient performed by a clinical psychologist,
a marriage and family therapist, a mental
health counselor, or a clinical social worker.
e administrator of a treatment facility may
refuse admission to any patient directed to
its facilities on an involuntary basis, whether
by civil or criminal court order, who is not
accompanied at the same time by adequate
orders and documentation.
(7) PROCEDURE FOR CONTINUED
INVOLUNTARY INPATIENT
PLACEMENT.
(a) Hearings on petitions for continued
involuntary inpatient placement shall
be administrative hearings and shall be
conducted in accordance with the provisions
of s. 120.57(1), except that any order entered
by the administrative law judge shall be nal
and subject to judicial review in accordance
with s. 120.68. Orders concerning patients
committed after successfully pleading not
guilty by reason of insanity shall be governed
by the provisions of s. 916.15.
(b)If the patient continues to meet the criteria
for involuntary inpatient placement, the
administrator shall, prior to the expiration
of the period during which the treatment
facility is authorized to retain the patient,
le a petition requesting authorization for
continued involuntary inpatient placement.
e request shall be accompanied by a
statement from the patient’s physician or
Involuntary inpatient placement
65E-5.300 Continued Involuntary Inpatient
Placement at Treatment Facilities.
(1) In order to request continued involuntary inpatient
placement, the treatment facility administrator
shall, prior to the expiration of the period during
which the treatment facility is authorized to
retain the person, file a request for continued
placement. Recommended form CF-MH 3035,
Feb. 05, “Petition Requesting Authorization for
Continued Involuntary Inpatient Placement,” which
is incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter may be used as documentation of that
request. The petition shall be filed with the Division
of Administrative Hearings within 20 days prior to
the expiration date of a person’s authorized period
of placement or, in the case of a minor, the date
when the minor will reach the age of majority. The
petition shall contain the signed statement of the
person’s physician or clinical psychologist justifying
the request and shall be accompanied by the
following additional documentation:
(a) Evidence justifying the request by the physician
or clinical psychologist for involuntary inpatient

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
112
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.467 F.S.)
65E-5.300 F.A.C.
clinical psychologist justifying the request,
a brief description of the patient’s treatment
during the time he or she was involuntarily
placed, and an individualized plan of
continued treatment. Notice of the hearing
shall be provided as set forth in s. 394.4599.
If at the hearing the administrative law
judge nds that attendance at the hearing
is not consistent with the best interests of
the patient, the administrative law judge
may waive the presence of the patient from
all or any portion of the hearing, unless
the patient, through counsel, objects to
the waiver of presence. e testimony in
the hearing must be under oath, and the
proceedings must be recorded.
(c) Unless the patient is otherwise represented
or is ineligible, he or she shall be represented
at the hearing on the petition for continued
involuntary inpatient placement by the
public defender of the circuit in which the
facility is located.
(d)If at a hearing it is shown that the
patient continues to meet the criteria
for involuntary inpatient placement, the
administrative law judge shall sign the
order for continued involuntary inpatient
placement for a period not to exceed 6
months. e same procedure shall be
repeated prior to the expiration of each
additional period the patient is retained.
(e) If continued involuntary inpatient
placement is necessary for a patient
admitted while serving a criminal sentence,
but whose sentence is about to expire, or
for a patient involuntarily placed while a
minor but who is about to reach the age
of 18, the administrator shall petition
the administrative law judge for an order
authorizing continued involuntary inpatient
placement.
(f) If the patient has been previously found
incompetent to consent to treatment, the
administrative law judge shall consider
testimony and evidence regarding the
placement, including how the person meets
each of the statutorily required criteria;
(b) A brief summary of the person’s treatment
during the time he or she was placed; and
(c) An individualized treatment plan.
(2) Each criterion alleged must be substantiated by
evidence.
(3) The administrative law judge shall provide notice of
the hearing. Recommended form CF-MH 3024, Feb.
05, “Notice of Petition for Continued Involuntary
Placement,” which is incorporated by reference and
may be obtained pursuant to Rule 65E-5.120, F.A.C.,
of this rule chapter, may be used for this purpose.
Copies shall be provided to the person, attorney,
and guardian, guardian advocate or representative,
with a copy of the notice filed in the person’s clinical
record.
(4) If the administrative law judge finds evidence that
the person has regained his or her competency to
consent to treatment, the administrative law judge
shall notify the court appointing the guardian
advocate. Recommended form CF-MH 3116, Feb.
05, “Findings and Recommended Order Restoring
Person’s Competence to Consent to Treatment and
Discharging the Guardian Advocate,” which is
incorporated by reference and may be obtained
pursuant to Rule 65E-5.120, F.A.C., of this rule
chapter, may be used for this purpose.
(5) Based on the findings of the hearing, the
administrative law judge may return the person to
involuntary placement pending the next statutorily
required periodic hearing, release the person from
placement, or find the person eligible for voluntary
status. Recommended form CF-MH 3031, Feb.
05, “Order for Continued Involuntary Inpatient
Placement or for Release,” which is incorporated by
reference and may be obtained pursuant to Rule
65E-5.120, F.A.C., of this rule chapter, may be used
for this purpose. A copy of the completed order shall
be filed in the person’s clinical record and a copy
shall be provided to the person, attorney, facility
administrator, and guardian, guardian advocate or
representative.
(6) In order for the department to implement
the provisions of Section 394.463(2)(e), F.S.,
and to ensure that the Agency for Health Care
Administration will be able to analyze the data
it receives pursuant to that section, designated
receiving facilities and treatment facilities shall
Involuntary inpatient placement

113 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
patient’s competence. If the administrative
law judge nds evidence that the patient
is now competent to consent to treatment,
the administrative law judge may issue
a recommended order to the court that
found the patient incompetent to consent
to treatment that the patient’s competence
be restored and that any guardian advocate
previously appointed be discharged.
(8) RETURN OF PATIENTS. When a patient at
a treatment facility leaves the facility without
authorization, the administrator may authorize
a search for the patient and the return of the
patient to the facility. e administrator may
request the assistance of a law enforcement
agency in the search for and return of the
patient.
394.46715 Rulemaking authority.
e Department of Children and Family Services
shall have rulemaking authority to implement the
provisions of ss. 394.455, 394.4598, 394.4615,
394.463, 394.4655, and 394.467 as amended
or created by this act. ese rules shall be for the
purpose of protecting the health, safety, and well-
being of persons examined, treated, or placed under
this act.
394.4672 Procedure for placement of
veteran with federal agency.
(1) Whenever it is determined by the court that a
person meets the criteria for involuntary place-
ment and it appears that such person is eligible
for care or treatment by the United States De-
partment of Veterans Aairs or other agency
of the United States Government, the court,
upon receipt of a certicate from the United
States Department of Veterans Aairs or such
other agency showing that facilities are avail-
able and that the person is eligible for care or
treatment therein, may place that person with
Placement of veteran
(Chapter 394.4672 F.S.)
65E-5.300 F.A.C.
forward copies of each recommended form CF-MH
3031, “Order for Continued Involuntary Inpatient
Placement or Release,” as referenced in subsection
65E-5.300(5), F.A.C., accompanied by mandatory
form CF-MH 3118, “Cover Sheet to Agency for Health
Care Administration,” as referenced in subsection
65E-5.280(5), F.A.C., to: BA Reporting Center, FMHI-
MHC 2637, 13301 Bruce B. Downs Boulevard, Tampa,
Florida 33612-3807.
N/A
N/A
VETERANS

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
114
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4672 F.S.)
65E-5. F.A.C.
the United States Department of Veterans Af-
fairs or other federal agency. e person whose
placement is sought shall be personally served
with notice of the pending placement proceed-
ing in the manner as provided in this part, and
nothing in this section shall aect his or her
right to appear and be heard in the proceeding.
Upon placement, the person shall be subject to
the rules and regulations of the United States
Department of Veterans Aairs or other federal
agency.
(2) e judgment or order of placement by a court
of competent jurisdiction of another state or
of the District of Columbia, placing a person
with the United States Department of Veterans
Aairs or other federal agency for care or treat-
ment, shall have the same force and eect in
this state as in the jurisdiction of the court en-
tering the judgment or making the order; and
the courts of the placing state or of the District
of Columbia shall be deemed to have retained
jurisdiction of the person so placed. Consent
is hereby given to the application of the law
of the placing state or district with respect to
the authority of the chief ocer of any facility
of the United States Department of Veterans
Aairs or other federal agency operated in this
state to retain custody or to transfer, parole, or
discharge the person.
(3) Upon receipt of a certicate of the United States
Department of Veterans Aairs or such other
federal agency that facilities are available for
the care or treatment of mentally ill persons
and that the person is eligible for care or
treatment, the administrator of the receiving
or treatment facility may cause the transfer of
that person to the United States Department of
Veterans Aairs or other federal agency. Upon
eecting such transfer, the committing court
shall be notied by the transferring agency. No
person shall be transferred to the United States
Department of Veterans Aairs or other federal
agency if he or she is conned pursuant to the
conviction of any felony or misdemeanor or
if he or she has been acquitted of the charge
Placement of veteran
115 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4685 F.S.)
65E-5 F.A.C.
solely on the ground of insanity, unless prior to
transfer the court placing such person enters an
order for the transfer after appropriate motion
and hearing and without objection by the
United States Department of Veterans Aairs.
(4) Any person transferred as provided in this
section shall be deemed to be placed with
the United States Department of Veterans
Aairs or other federal agency pursuant to the
original placement.
394.468 Admission and discharge
procedures.
Admission and discharge procedures and treatment
policies of the department are governed solely by
this part. Such procedures and policies shall not
be subject to control by court procedure rules. e
matters within the purview of this part are deemed
to be substantive, not procedural.
394.4685 Transfer of patients among
facilities.
(1) TRANSFER BETWEEN PUBLIC
FACILITIES.
(a) A patient who has been admitted to a
public receiving facility, or the family
member, guardian, or guardian advocate
of such patient, may request the transfer
of the patient to another public receiving
facility. A patient who has been admitted
to a public treatment facility, or the family
member, guardian, or guardian advocate of
such patient, may request the transfer of the
patient to another public treatment facility.
Depending on the medical treatment or
mental health treatment needs of the patient
and the availability of appropriate facility
resources, the patient may be transferred
at the discretion of the department. If the
department approves the transfer of an
involuntary patient, notice according to the
Transfer of patients
N/A
65E-5.310 Transfer of Persons Among
Facilities.
(1) Recommended form CF-MH 3046, Feb. 05,
“Application for and Notice of Transfer to Another
Facility,” which is incorporated by reference and may
be obtained pursuant to Rule 65E-5.120, F.A.C., of
this rule chapter may be used to request the transfer
of a person to another receiving or treatment
facility. This application, or its equivalent, shall be
completed and filed with the facility administrator
or designee. A copy of the completed application
shall be retained in the person’s clinical record.
(2) The administrator of the facility or designee
at which the person resides shall, without
delay, submit an application for transfer to the
administrator of the facility to which a person has
requested transfer. Upon acceptance of the person
by the facility to which the transfer is sought, the
administrator of the transferring facility or his or her
designee shall mail the statutorily required notices
to the person, the person’s attorney, guardian,
guardian advocate or representative, retaining a
copy in the person’s clinical record. Recommended

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
116
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
provisions of s. 394.4599 shall be given prior
to the transfer by the transferring facility. e
department shall respond to the request for
transfer within 2 working days after receipt of
the request by the facility administrator.
(b) When required by the medical treatment
or mental health treatment needs of the
patient or the ecient utilization of a
public receiving or public treatment
facility, a patient may be transferred
from one receiving facility to another, or
one treatment facility to another, at the
department’s discretion, or, with the express
and informed consent of the patient or the
patient’s guardian or guardian advocate, to a
facility in another state. Notice according to
the provisions of s. 394.4599 shall be given
prior to the transfer by the transferring
facility. If prior notice is not possible, notice
of the transfer shall be provided as soon as
practicable after the transfer.
(2) TRANSFER FROM PUBLIC TO PRIVATE
FACILITIES.
A patient who has been admitted to a public
receiving or public treatment facility and has
requested, either personally or through his or
her guardian or guardian advocate, and is able
to pay for treatment in a private facility shall be
transferred at the patient’s expense to a private
facility upon acceptance of the patient by the
private facility.
(3) TRANSFER FROM PRIVATE TO PUBLIC
FACILITIES.
(a) A patient or the patient’s guardian or
guardian advocate may request the
transfer of the patient from a private to a
public facility, and the patient may be so
transferred upon acceptance of the patient
by the public facility.
(b) A private facility may request the transfer of
a patient from the facility to a public facility,
and the patient may be so transferred upon
acceptance of the patient by the public
facility. e cost of such transfer shall be the
responsibility of the transferring facility.
Transfer of patients
(Chapter 394.4685 F.S.)
65E-5.310 F.A.C.
form CF-MH 3046, “Application for and Notice
of Transfer to Another Facility,” as referenced in
subsection 65E-5.310(1), F.A.C., may be used for this
documentation.
(3) If the proposed transfer of a person originates
with the administrator of the facility or his or her
designee or with the treating physician a notice of
transfer is required. The notice shall be completed
by the administrator or designee of the transferring
facility, after acceptance of the person by the
facility to which he or she will be transferred, with
copies provided prior to the transfer to those
required by law, with a copy retained in the person’s
clinical record. Recommended form CF-MH 3046,
“Application for and Notice of Transfer to Another
Facility,” as referenced in subsection 65E-5.310(1),
F.A.C., may be used for this purpose.
(4) All relevant documents including a copy of the
person’s clinical record, shall be transferred prior to
or concurrent with the person to the new facility.
(5) Each facility shall develop and implement policies
and procedures for transfer that provide for safety
and care during transportation.
Transfers from hospitals must
comply with federal EMTALA law.

117 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.473 F.S.)
65E-5.310 F.A.C.
(c) A public facility must respond to a request
for the transfer of a patient within 2
working days after receipt of the request.
(4) TRANSFER BETWEEN PRIVATE
FACILITIES. A patient in a private facility
or the patient’s guardian or guardian advocate
may request the transfer of the patient to
another private facility at any time, and the
patient shall be transferred upon acceptance of
the patient by the facility to which transfer is
sought.
394.469 Discharge of involuntary
patients.
(1) POWER TO DISCHARGE. At any time a
patient is found to no longer meet the criteria
for involuntary placement, the administrator
shall:
(a) Discharge the patient, unless the patient is
under a criminal charge, in which case the
patient shall be transferred to the custody of
the appropriate law enforcement ocer;
(b)Transfer the patient to voluntary status on
his or her own authority or at the patient’s
request, unless the patient is under criminal
charge or adjudicated incapacitated; or
(c) Place an improved patient, except a patient
under a criminal charge, on convalescent
status in the care of a community facility.
(2) NOTICE.—Notice of discharge or transfer
of a patient shall be given as provided in s.
394.4599.
394.473 Attorney’s fee; expert witness fee.
(1) In the case of an indigent person for whom an
attorney is appointed pursuant to the provi-
sions of this part, the attorney shall be compen-
sated by the state pursuant to s. 27.5304. In
the case of an indigent person, the court may
appoint a public defender. e public defender
Attorney's and expert witness fees
65E-5.320 Discharge of Persons on
Involuntary Status.
A receiving or treatment facility administrator shall
provide prompt written notice of the discharge of a
person on involuntary status to the person, guardian,
guardian advocate, representative, initiating professional,
and circuit court, with a copy retained in the person’s
clinical record. Recommended form CF-MH 3038, “Notice
of Release or Discharge,” as referenced in paragraph
65E-5.280(7)(e), F.A.C., may be used as documentation of
such notice. If the discharge occurs while a court hearing
for involuntary placement or continued involuntary
placement is pending, all parties including the state
attorney and attorney representing the person, shall be
given telephonic notice of the discharge by the facility
administrator or his or her designee.
N/A

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
118
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.475 F.S.)
65E-5.320 F.A.C.
shall receive no additional compensation other
than that usually paid his or her oce.
(2) In the case of an indigent person for whom expert
testimony is required in a court hearing pursuant
to the provisions of this act, the expert, except
one who is classied as a full-time employee of
the state or who is receiving remuneration from
the state for his or her time in attendance at
the hearing, shall be compensated by the state
pursuant to s. 27.5304.
394.475 Acceptance, examination,
and involuntary placement of Florida
residents from out-of-state mental health
authorities.
(1) Upon the request of the state mental health
authority of another state, the department is
authorized to accept as a patient, for a period
of not more than 15 days, a person who is and
has been a bona de resident of this state for a
period of not less than 1 year.
(2) Any person received pursuant to subsection
(1) shall be examined by the sta of the state
facility where such patient has been accepted,
which examination shall be completed during
the 15-day period.
(3) If upon examination such a person requires
continued involuntary placement, a petition
for a hearing regarding involuntary placement
shall be led with the court of the county
wherein the treatment facility receiving the
patient is located or the county where the
patient is a resident.
(4) During the pendency of the examination
period and the pendency of the involuntary
placement proceedings, such person may
continue to be held in the treatment facility
unless the court having jurisdiction enters an
order to the contrary.
N/A
Acceptance, examination, and involuntary placement

Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394.4784 F.S.)
65E-5 F.A.C.
394.4784 Minors; access to outpatient
N/A
crisis intervention services and treatment.
For the purposes of this section, the disability of
nonage is removed for any minor age 13 years
or older to access services under the following
circumstances:
(1) OUTPATIENT DIAGNOSTIC AND
EVALUATION SERVICES.
When any minor age 13 years or older experi-
ences an emotional crisis to such degree that he
or she perceives the need for professional assis-
tance, he or she shall have the right to request,
consent to, and receive mental health diagnostic
and evaluative services provided by a licensed
mental health professional, as dened by Florida
Statutes, or in a mental health facility licensed
by the state. e purpose of such services shall
be to determine the severity of the problem and
the potential for harm to the person or others
if further professional services are not provided.
Outpatient diagnostic and evaluative services
shall not include medication and other somatic
methods, aversive stimuli, or substantial depri-
vation. Such services shall not exceed two visits
during any 1-week period in response to a crisis
situation before parental consent is required for
further services, and may include parental partici-
pation when determined to be appropriate by the
mental health professional or facility.
(2) OUTPATIENT CRISIS INTERVENTION,
THERAPY AND COUNSELING SERVICES
When any minor age 13 years or older
experiences an emotional crisis to such
degree that he or she perceives the need
for professional assistance, he or she shall
have the right to request, consent to, and
receive outpatient crisis intervention services
including individual psychotherapy, group
therapy, counseling, or other forms of verbal
therapy provided by a licensed mental health
professional, as dened by Florida Statutes, or
in a mental health facility licensed by the state.
Such services shall not include medication and
other somatic treatments, aversive stimuli, or
Minors access to services and treatment
Outpatient Services for
Minors.
See Appendix D for
issues addressing consent
for admission and
treatment for minors
119

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
120
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
substantial deprivation. Such services shall not
exceed two visits during any 1-week period in
response to a crisis situation before parental
consent is required for further services, and
may include parental participation when
determined to be appropriate by the mental
health professional or facility.
(3) LIABILITY FOR PAYMENT.
e parent, parents, or legal guardian of a
minor shall not be liable for payment for any
such outpatient diagnostic and evaluation
services or outpatient therapy and counseling
services, as provided in this section, unless such
parent, parents, or legal guardian participates
in the outpatient diagnostic and evaluation
services or outpatient therapy and counseling
services and then only for the services rendered
with such participation.
(4) PROVISION OF SERVICES.
No licensed mental health professional shall be
obligated to provide services to minors accorded
the right to receive services under this section.
Provision of such services shall be on a voluntary
basis. 394.4785 Children and adolescents;
admission and placement in mental
394.4785 Children and adolescents;
admission and placement in mental
facilities.
(1) A child or adolescent as dened in s. 394.492
may not be admitted to a state-owned or state-
operated mental health treatment facility. A
child may be admitted pursuant to s. 394.4625
or s. 394.467 to a crisis stabilization unit or a
residential treatment center licensed under this
chapter or a hospital licensed under chapter
395. e treatment center, unit, or hospital
must provide the least restrictive available
treatment that is appropriate to the individual
needs of the child or adolescent and must ad-
here to the guiding principles, system of care,
and service planning provisions contained in
part III of this chapter.
Children and adolescents; admission and placement
(Chapter 394.4785 F.S.)
65E-5. F.A.C.
N/A
Inpatient Services for
Minors.

121 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
Veterans and service members court programs
(Chapter 394.47891 F.S.)
65E-5. F.A.C.
(2) A person under the age of 14 who is admitted
to any hospital licensed pursuant to chapter 395
may not be admitted to a bed in a room or ward
with an adult patient in a mental health unit or
share common areas with an adult patient in a
mental health unit. However, a person 14 years
of age or older may be admitted to a bed in a
room or ward in the mental health unit with
an adult if the admitting physician documents
in the case record that such placement is
medically indicated or for reasons of safety. Such
placement shall be reviewed by the attending
physician or a designee or on-call physician each
day and documented in the case record.
394.47891 Military veterans and service
members court programs.
e chief judge of each judicial circuit may establish
a Military Veterans and Servicemembers Court
Program under which veterans, as dened in s. 1.01,
and servicemembers, as dened in s. 250.01, who
are convicted of a criminal oense and who suer
from a military-related mental illness, traumatic brain
injury, substance abuse disorder, or psychological
problem can be sentenced in accordance with chapter
921 in a manner that appropriately addresses the
severity of the mental illness, traumatic brain injury,
substance abuse disorder, or psychological problem
through services tailored to the individual needs of
the participant. Entry into any Military Veterans and
Service members Court Program must be based upon
the sentencing court’s assessment of the defendant’s
criminal history, military service, substance abuse
treatment needs, mental health treatment needs,
amenability to the services of the program, the
recommendation of the state attorney and the victim,
if any, and the defendant’s agreement to enter the
program.
N/A
New!!
Veterans and service
members court programs

N/A
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
122
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.330 F.A.C.
Also see 65E-5.180(7)(b)
FAC for additional training
required regarding restraint
and seclusion
65E-5.330 Training.
(1) In order to ensure the protection of the health,
safety, and welfare of persons treated in receiving
and treatment facilities, required by Section
394.457(5)(b), F.S., the following is required:
(a) Each designated receiving and treatment facility
shall develop policies and procedures for abuse
reporting and shall conduct training which shall
be documented in each employee’s personnel
record or in a training log.
(b) All staff who have contact with persons served
shall receive training in verbal de-escalation
techniques and the use of bodily control and
physical management techniques based on
a team approach. Less restrictive verbal de-
escalation interventions shall be employed
before physical interventions, whenever safety
conditions permit.
(c) All staff who have contact with persons served
shall receive training in cardiopulmonary
resuscitation within the first six months of
employment if not already certified when
employed and shall maintain current certification
as long as duties require direct contact with
persons served by the facility.
(d) A personnel training plan that prescribes and
assures that direct care staff, consistent with
their assigned duties, shall receive and complete
before providing direct care or assessment
services, 14 hours of basic orientation training,
documented in the employee’s personnel record,
in the following:
1. Rights of persons served by the facility and
facility procedures required under Chapter
394, Part I, F.S., and Chapter 65E-5, F.A.C.;
2. Confidentiality laws including psychiatric,
substance abuse, HIV and AIDS;
3. Facility incident reporting;
4. Restrictions on the use of seclusion and
restraints, consistent with unit policies and
procedures, and this chapter;
5. Abuse reporting required by Chapter 415,
F.S.;
6. Assessment for past or current sexual,
psychological, or physical abuse or trauma;
7. Cross-training for identification of, and
working with, individuals recently engaging
in substance abuse;
Online Baker Act Training
http://www.bakeracttraining.org
FREE!
On demand!
CEC's offered at low cost!
Training

123 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
8. Clinical risk and competency assessment;
9. Universal or standard practices for infection
control;
10. Crisis prevention, crisis intervention and
crisis duration services;
11. Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition, Text Revision, as
referenced in subparagraph 65E-5.285(1)
(a)2., F.A.C.; and
12. Honoring preferences contained in advance
directives prepared by persons served by the
facility.
(2) In addition to the training required in this rule,
procedures must assure that mental health services
staff shall annually receive 12 hours continuing
training in the skills and knowledge employed
in performing their respective responsibilities.
Employees during their first year of employment
shall undergo no less than the 14 hours of
orientation, as described in paragraph (1)(c) above,
and 12 hours of in-service training.
(3) Procedures shall require that individuals who deliver
the staff training curriculum for mental health
services shall be qualified by their experience and
training in the content presented.
(4) A plan shall be developed and implemented
providing for the mandatory training for employees,
emergency room personnel and physicians in
the Baker Act, relative to their positions and
responsibilities, and any implementing local
coordination agreements or protocols.
65E-5.400 Baker Act Funded Services
Standards.
(1) Applicability. Designation as a public receiving
facility is required for any facility licensed under
the authority of Chapter 395 or 394, F.S., to be
eligible for payment from Baker Act appropriations.
Designation does not in and of itself represent
any agreement to pay for any services rendered
pursuant to Chapter 394, Part I, F.S., or this chapter.
Public receiving facilities, under contract with the
department, serve as a local focal point for district
or region public information dissemination and
educational activities with other local Baker Act
involved entities and public agencies.
Chapter 65E-14, FAC also
governs funding.
Baker Act funded services

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
124
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
(2) Baker Act Funding.
(a) Only public receiving facilities, pursuant to
Section 394.455(25), F.S., and only the costs
of eligible Baker Act services provided to
diagnostically and financially eligible persons
may be paid with Baker Act appropriations.
(b) Baker Act services shall first be provided to
acutely ill persons who are most in need of
mental health services and are least able to pay.
(c) Persons receiving Baker Act funded services must
meet financial eligibility criteria as established
by the federal poverty guidelines. Public
receiving facilities may provide Baker Act funded
services to acutely ill persons who are financially
ineligible if the total number of days of service
paid for with Baker Act funds for financially
ineligible persons does not exceed 20 percent of
the total number of days paid for with Baker Act
funds.
(d) An individual’s diagnostic and financial eligibility
shall be documented on mandatory form CF-
MH 3084, Feb. 05, “Baker Act Service Eligibility,”
which is incorporated by reference and may be
obtained pursuant to Rule 65E-5.120, F.A.C., of
this rule chapter.
(3) This section applies to all Baker Act funded
providers. All services including hospital inpatient
facilities, crisis stabilization units, short-term
residential treatment programs, and children’s crisis
stabilization units providing services purchased
by the department under this chapter shall be
consistent with licensure requirements and must
comply with written facility policies and procedures.
(4) Training. The training required in Rule 65E-5.330,
F.A.C., is required for all direct service staff employed
by publicly funded Baker Act service providers.
(5) Emergency Reception and Screening.
(a) Providers authorized by the department
shall have a policy and procedure manual
for the specific service being provided. The
administration of the provider organization shall
ensure the completeness and accuracy of the
manual and that organizational operations are in
accordance with the manual. The manual must
be approved by the respective departmental
district or regional office for completeness and
consistency in implementing this chapter and
Chapter 394, Part I, F.S. The manual shall be
consistent with the provisions of Chapter 394,
Emergency Screening.
Baker Act funded services
125 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
Part I, F.S., and with Chapter 65E-5, F.A.C., and
must include the following:
1. Procedures for responding to requests for
services that specify a prompt screening
to determine the person’s immediacy of
need, and for prioritizing access to services
with limited availability. Staff skills shall be
specific to the unique needs of the persons
to be served;
2. A description of the services offered,
recipient eligibility criteria, how eligible
recipient facilities or individuals are
informed of service availability, service
locations, costs, criteria for response, hours
of operation, staffing with staff qualifications
and supervision, and organizational line of
authority to the operating entity;
3. Procedures to be utilized to implement
and document staff training in accord with
Rule 65E-5.330, F.A.C., staff proficiency or
competency including the performance of
any subcontractors employed to provide
services, and how training will be used to
effect remediable identified deficiencies;
4. Procedures for a complaint and grievance
system that provide a prompt response to
the individuals served, and mechanisms to
monitor and evaluate service quality, and
the outcomes attained by individuals served.
Facility personnel shall provide each person
served with a listing of his or her rights and a
telephone number to which complaints may
be directed;
5. Procedures to determine if the individual
has a case manager from a mental health
center or clinic, as well as notification and
coordination of activities with the case
manager;
6. Procedures to maintain a clinical record for
each individual served and its safeguarding
in accordance with Section 394.4615, F.S.;
and
7. Procedures to inform the public of the
availability of services.
(b) Procedures must assure that a psychiatrist
or a physician shall be available on-call for
consultation at all times and hours during which
emergency reception and screening services are
operated.
Baker Act funded services

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
126
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
(6) Mobile Crisis Response Service and Mental
Health Overlay Program Requirements.
(a) The criteria and operational requirements for a
mobile crisis response service and a mental health
overlay program is defined in Sections 394.455(19)
and 394.455(17), F.S., respectively. The operation of
these services is expressly limited to the program’s
contract with the department.
(b) Providers authorized by the department to provide
mobile crisis response services and mental health
overlay programs shall have a policy and procedure
manual for the specific service being provided.
The administration of the provider organization
shall ensure the completeness and accuracy of the
manual and that organizational operations are in
accordance with the manual. The manual must be
approved by the departmental district or regional
office in which the facility is located. The manual
shall be consistent with the provisions of Chapter
394, Part I, F.S., and these rules, and shall include:
1. A description of the services offered, eligibility
criteria, how eligible recipient facilities or
individuals are informed of service availability,
criteria for response, hours of operation, staffing
with staff qualifications and supervision, and
organizational line of authority to the operating
entity;
2. Procedures to be utilized to implement the
provisions of Section 394.4625, F.S., including
staff training, proficiency or competency
assessment instruments to be administered,
credentialing, and distribution of results
obtained;
3. A description of on-site evaluation, educational,
assistance or supportive services, if provided,
to be rendered by mental health overlay
programs. The extent and frequency of services
offered must be described. Staff skills shall be
specific to unique needs of the persons to be
served;
4. Procedures for the provision of a complaint and
grievance procedure to be used by individuals
served, and mechanisms to monitor and
evaluate the service’s quality and the outcomes
attained by individuals served. Personnel shall
provide each person served with a listing of his
or her rights and a telephone number to which
complaints may be directed;
Mobile Crisis Response &
Mental Health Overlay dened
in 394.455 (17) & (19) F.S.
Baker Act funded services

127 Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
5. Procedures that require the provider’s issuance
of, and the employees wearing of identification
badges including a photograph of employee,
organization’s name, and employees name and
identification number, if full name is not used,
for all employees responding to, or working in,
off-site situations;
6. Procedures that assure determination of
whether the individual has a case manager from
a mental health center or clinic, and require
notification and coordination of activities with
the case manager; and
7. Procedures that require the maintenance of a
clinical record for each individual served and
safeguarding it in accordance with Section
394.4615, F.S.
(c) Procedures must require employee’s clinical
activities and performance, as opposed to primarily
administrative functions, are supervised by one
of the following: a psychiatrist, physician, clinical
psychologist, clinical social worker, mental health
counselor, marriage and family therapist, or
psychiatric nurse, as defined in Section 394.455, F.S.
(d) Procedures must assure that a physician or
psychiatrist shall be available on-call for consultation
at all times and hours during which mental health
overlay programs and mobile crisis response services
are operated.
(e) Procedures must be consistent with Section 394.462,
F.S., and these rules, and must limit transportation
of an involuntary person by the mental health
overlay program or mobile crisis response service
to only directly transporting individuals to the
nearest designated receiving facility. In addition, the
following provisions shall be met and described in
the manual:
1. Liability insurance of no less than $100,000 per
person shall be provided.
2. The vehicle shall be equipped with a Type
2A10BC fire extinguisher, seat belts, 2-way
communication radio or cellular telephone with
accompanying emergency telephone numbers,
and a functioning air conditioner and heater.
3. Staff having the responsibility for transporting
people shall be trained and experienced in
transporting people with mental illness and
substance abuse who may become confused,
volatile, or combative.
Baker Act funded services

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
128
Baker Act Handbook and User Reference Guide • 2014
State of Florida Department of Children & Families
Statute
Rule
Current and accurate as of date of printing September 2013
(Chapter 394 F.S.)
65E-5.400 F.A.C.
(7)
4. At least 2 members shall be present to transport
an individual. The total number of people in the
vehicle at any time shall not exceed the legal
seating capacity.
5. Firearms shall not be worn or carried in the
vehicle.
6. Physical restraints, such as canvas cuffs, shall
not be used except by personnel trained in
their use, and only when necessary to protect
the person being transported from injury
to themselves or others. Any use of physical
or mechanical restraints shall be fully and
completely documented in the person’s clinical
record.
7. The vehicle used to transport people shall
be unmarked, maintained and operated in
accordance with Chapter 316, F.S., and in a
manner that protects the individual’s rights,
dignity and physical safety.
8. Procedures must require the immediate
reporting of any unusual incidents or injuries,
upon arrival at the intended destination.
Requirements for Mental Health Overlay
Programs in Nursing Homes, Assisted Living
Facilities, Adult Day Care Centers, and Adult
Family Care Homes.
(a) All plans, contracts and activities shall recognize
that the primary responsibility for the care and
treatment of individuals rests with the nursing
home, assisted living facility, adult day care center,
or adult family care home.
(b) Activities representative of those services
appropriate to be provided by a mental health
overlay program include:
1. Assisting in the development or
implementation of individual care plans;
2. Assessing and making recommendations for
needed physical or psychiatric services to the
facility administrator; and
3. Providing training to facility staff or residents
in various mental health skills or knowledge,
such as anger management, psychotropic
medications, depression, loss, physical and
sexual trauma, and competency to consent
determinations.
(c) Personnel shall provide each person served with a
list of his or her rights pursuant to Chapter 394, Part
I, F.S.
Baker Act funded services

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix A - 1
Related Laws
Appendix A
A
Baker Act and Related Laws
Statutes governing the treatment of mental illness in Florida
date back to 1874. Amendments to the law were passed
many times over the years but in 1971 the Legislature
enacted the Florida Mental Health Act. is Act brought
about a dramatic and comprehensive revision of Florida’s
97-year old mental health law. It substantially strengthened
the due process and civil rights of persons in mental heath
facilities.
e Florida Mental Health Act, usually referred to as the
“Baker Act,” was named after Maxine Baker, former State
representative from Miami who sponsored the Act, after
serving as chairperson of the House Committee on Mental
Health. Referring to the treatment of persons with mental
illness before the passage of her bill, Representative Baker
stated “ In the name of mental health, we deprive them of
their most precious possession – liberty.”
It is important that the Baker Act only be used in situations
where the person has a mental illness as dened in the Baker
Act and meets all remaining statutory criteria for voluntary
or involuntary admission. e Baker Act does not authorize
provision of medical examination or medical treatment.
Further, the legal denition of mental illness excludes
intoxication, substance abuse impairment, any form of
developmental disability, and antisocial behavior. For many
persons, the use of other statutes may be more appropriate.
Some alternative statutes may include:
Marchman Act
Chapter 397, F.S.
A person may voluntarily enter substance abuse treatment
or undergo involuntary admission into a licensed substance
abuse facility if found to be substance abuse impaired and
meeting certain other criteria. is means a condition
involving the use of alcoholic beverages or any psychoactive
or mood-altering substance in such a manner as to induce
mental, emotional, or physical problems and cause socially
dysfunctional behavior.
e involuntary assessment and treatment criteria under
the Marchman Act requires a good faith reason to believe
the person is substance abuse impaired and because of such
impairment, has lost the power of self-control with respect
to substance use and either has inflicted, or threatened or
attempted to inflict, or unless admitted is likely to inflict,
physical harm on self or others or is in need of substance
abuse services and, by reason of substance abuse impairment,
his judgment has been so impaired that he is incapable
of appreciating his need for such services and of making
a rational decision in regard thereto (mere refusal is
insucient).
Involuntary admission can be initiated in a number of ways:
Protective Custody by a law enforcement ocer
Emergency Admission, requiring a physician’s certicate
Alternative Assessments for Minors by parent or legal
guardian to a Juvenile Addiction Receiving Facility
Assessment and Stabilization ordered by a Circuit Court
Judge.
If the assessment conducted by a qualied professional
under one of the above conrms criteria is met, a petition
can be led with the court and the judge can order up to
60 days of treatment if the person is accepted by a licensed
treatment provider.
Developmental Disabilities
Chapter 393, F.S.
is statute governs disorders or syndromes that are
attributable to intellectual disability, cerebral palsy, autism,
spina bifida or Prader-Wili Syndrome that occur before the
age of 18 and that constitute a substantial handicap that can
reasonably be expected to continue indenitely.
A person may be court ordered to undergo involuntary
admission to residential services under Chapter 393.11,
F.S. if he or she has intellectual disability, in order that the
person may receive the care, treatment, habilitation, and
rehabilitation which the person needs.
Emergency Examination and
Treatment of Incapacitated Persons
s. 401.445, F.S.
is statute provides insulation from liability in cases where
the person’s emergency medical condition is a life-threatening
one and treatment is provided without consent. A person
is generally incapable of providing informed consent if he
cannot understand the procedure, the medically acceptable
alternatives, and the substantial risks and hazards inherent in
the proposed treatment or procedures.
ese conditions include when:
(a) e patient at the time of examination or
treatment is intoxicated, under the inuence

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
Appendix A - 2
A
of drugs, or otherwise incapable of providing
informed consent;
(b) e patient at the time of examination or
treatment is experiencing an emergency medical
condition; and
(c) e patient would reasonably, under all the
surrounding circumstances, undergo such
examination, treatment, or procedure if he or she
were advised by the emergency medical technician,
paramedic, physician, advanced registered nurse
practitioner, or physician assistant.
Examination and treatment is limited to reasonable
examination of the patient to determine the medical
condition of the patient and treatment reasonably necessary
to alleviate the emergency medical condition or to stabilize
the patient.
When examining or treating a person who is apparently
intoxicated, under the inuence of drugs, or otherwise
incapable of providing informed consent, an authorized
professional acting under the direct medical supervision
of a physician, shall proceed wherever possible with
the consent of the person. If the person appears to be
incapacitated and refuses his or her consent, the person
may be examined, treated, or taken to a hospital or other
appropriate treatment resource if he or she is in need of
emergency attention, without his or her consent, but
unreasonable force cannot be used. is doesn’t limit
medical treatment provided pursuant to a court order or
treatment provided in accordance with the Baker Act or
Marchman Act.
EMTALA
42 USC 1395dd
is federal statute titled Emergency Medical Treatment
and Active Labor Act prohibits the delay and/or denial
of emergency medical services, including psychiatric and
substance abuse emergencies due to inability to pay for
care. is law applies to all hospitals having emergency
service capability, including freestanding psychiatric
hospitals.
EMTALA governs access to emergency care, transfers
between facilities, and penalties for violation by physicians
and hospitals. Where the state Baker Act law conicts with
the federal EMTALA law, the federal law prevails. If the
laws are not in conict, both must be followed.
Access to Emergency Services and Care
s.395.1041, F.S.
is state statute is the equivalent of the federal EMTALA
law. It prohibits the delay or denial of emergency services
and care by hospitals and physicians and enforces the ability
of persons to get all necessary and appropriate emergency
care within the capability and capacity of each hospital. is
statute governs access to care, transfers from one hospital
to other facilities, and establishes penalties for violations by
physicians and hospitals.
395.1041 Access to emergency services and care
(3)(e)Except as otherwise provided by law, all medically
necessary transfers shall be made to the geographically
closest hospital with the service capability, unless another
prior arrangement is in place or the geographically closest
hospital is at service capacity. When the condition of a
medically necessary transferred patient improves so that
the service capability of the receiving hospital is no longer
required, the receiving hospital may transfer the patient
back to the transferring hospital and the transferring
hospital shall receive the patient within its service
capability.
(h)A hospital may request and collect insurance
information and other nancial information from a
patient, in accordance with federal law, if emergency
services and care are not delayed. No hospital to which
another hospital is transferring a person in need of
emergency services and care may require the transferring
hospital or any person or entity to guarantee payment
for the person as a condition of receiving the transfer.
In addition, a hospital may not require any contractual
agreement, any type of preplanned transfer agreement, or
any other arrangement to be made prior to or at the time
of transfer as a condition of receiving an individual patient
being transferred...
is statute also requires that a hospital providing emergency
services and care to a person who is being involuntarily
examined under the Baker Act must adhere to all rights of
patients and involuntary examination procedures provided by
the Baker Act, regardless of whether the hospital, or any part
thereof, is designated as a receiving or treatment facility, and
regardless of whether the person is admitted to the hospital.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix A - 3
Related Laws
Appendix A
A
Adult Abuse, Neglect, and Exploitation
s. 415.1051, F.S.
is statute may be appropriate when a vulnerable adult
is alleged to be a victim of abuse, neglect, or exploitation
and lacks the capacity to consent to needed services and
care. is means a mental impairment that causes a person
to lack sucient understanding or capacity to make or
communicate responsible decisions concerning his person
or property, including whether or not to accept protective
services from the Department of Children and Families
(DCF).
A vulnerable adult is dened in Chapter 415 as one whose
ability to perform the normal activities of daily living or to
provide for his/her own care or protection is impaired due to
a mental, emotional, long-term physical or developmental
disability, dysfunction, brain damage, or the inrmities of
aging.
Where the person’s condition is not a life-threatening
emergency and no health care surrogate or proxy is available
to consent, a report to the Department of Children and
Families of the need for non-emergency protective service
intervention is required. If the Department has reasonable
cause to believe that a vulnerable adult is in need of
protective services but lacks the capacity to consent to
protective services, the Department must petition the court
for an order authorizing the provision of protective services.
e Department of Children and Families and a law
enforcement ocer may forcibly enter and may remove
a vulnerable adult who is likely to incur a risk of death or
serious physical injury.
Emergency medical treatment (that doesn’t violate an
advance directive) may be provided without consent for a
vulnerable adult after admission to a medical facility. Further
treatment without informed consent is subject to a DCF
petition and a court order.
Advance Directives
Chapter 765, F.S.
If a competent person has previously executed an advance
directive designating a health care surrogate and a
physician has now found the person to be incompetent
or incapacitated to consent to his/her own treatment, the
surrogate may instead be asked to provide such consent.
Incapacity or incompetent means the person is physically
or mentally unable to communicate a willful and knowing
health care decision.
In the absence of an advance directive, a health care
proxy may be notied, if a person meeting the degree of
relationship specied in Chapter 765, Part IV, F.S. is available
to serve. A proxy can be:
1. A judicially appointed guardian of the person
or the guardian advocate of the person having a
developmental disability (totally dierent than
under the Baker Act) who has been authorized to
consent to medical treatment, if such guardian has
previously been appointed;
2. e spouse;
3. An adult child, or if the patient has more than one
adult child, a majority of the adult children who are
reasonably available for consultation;
4. A parent;
5. e adult sibling or, if the patient has more than
one sibling, a majority of the adult siblings who are
reasonably available for consultation;
6. An adult relative of the patient who has exhibited
special care and concern for the patient and who has
maintained regular contact with the patient and who
is familiar with the patient’s activities, health, and
religious or moral beliefs; or
7. A close adult friend of the patient who has exhibited
special care and concern for the patient, and who
presents an adavit to the health care facility or to
the attending or treating physician stating that he or
she is a friend of the patient; is willing and able to
become involved in the patient’s health care; and has
maintained such regular contact with the patient so
as to be familiar with the patient’s activities, health,
and religious or moral beliefs.
8. A clinical social worker licensed pursuant to chapter
491, or who is a graduate of a court-approved
guardianship program. Such a proxy must be
selected by the provider’s bioethics committee
and must not be employed by the provider. If the
provider does not have a bioethics committee, then
such a proxy may be chosen through an arrangement
with the bioethics committee of another provider.
Any health care decision made must be based on informed
consent and on the decision the surrogate or proxy reasonably
believes the person would have made under the circumstances
(substitute judgement). If there is no indication what the
patient would have chosen, the surrogate or proxy may
consider the patient’s best interest in deciding that proposed
treatments are to be withheld or that treatments currently in
eect are to be withdrawn.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
Appendix A - 4
A
e Baker Act requires that any person who has a health care
surrogate or proxy making his/her treatment decisions be on
involuntary status.
A health care facility must notify the surrogate or proxy in
writing that his or her authority has begun. e surrogate or
proxy has the authority to:
Make written consent to health care decisions the
principal would have made if capable of making such
decisions (substitute judgement);
Have access to clinical records;
Authorize release of records for continuity of care;
Authorize transfer of principal to or from a health
care facility; and
Apply for public benets.
A sample mental health advance directive can be found
in Appendix C of this handbook. However, any advance
directive designating a health care surrogate which is prepared
in accord with Florida law is acceptable.
Guardianship
Chapter 744, F.S.
Some persons, due to their incapacity, require either a limited
or a plenary guardian to make many life decisions.
An incapacitated person is one who has been judicially
determined to lack the capacity to manage at least some of
his/her property or to meet at least some of the essential
health and safety requirements of such person.
Both plenary and limited guardianship is initiated by a
petition to the court. Any order of a circuit judge must state
the nature of the guardianship as either plenary, where the
guardian exercises all delegable rights, or limited where the
guardian exercises only those removed from the ward in the
order.
e Baker Act prohibits the voluntary admission of any
person who has been adjudicated incapacitated. However, a
plenary guardian or guardian of person may provide express
and informed consent for the person’s treatment while held
under involuntary status.
*See chart comparing related statutes.
**Laws governing minors, including those who
are dependent or delinquent, are addressed in Appendix D.
Specialized on-line Baker Act courses can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
Appendix A
A
Quick Reference Guide to Related Statutes (Does not substitute for consulting the statutes)
Baker Act - The
Florida Mental
Health Act
Developmental
Disabilities
Marchman Act Emergency
Medical Services
& Transportation
Adult Abuse,
Neglect, and
Exploitation
Guardianship Health Care
Surrogate &
Proxy
Chapter 394.455
(18), Part 1, F.S.
s. 393.063(9), s.
393.0641(1), F.S.
Chapter 397, Part
V, F.S.
s. 401.445, F.S. s. 415.1051, F.S. Chapter 744, F.S. Chapter 765, F.S.
Definitions Mental illness
means an
impairment
of the mental
or emotional
processes
that exercise
conscious control
of one's actions
or of the ability
to perceive or
understand
reality, which
impairment
substantially
interferes with a
person's ability to
meet the ordinary
demands of
living, regardless
of etiology. For
the purposes of
this part, the term
does not include
a developmental
disability as
defined in chapter
393, intoxication,
or conditions
manifested only
by antisocial
behavior or
substance abuse
impairment.
Developmental
disability is
a disorder or
syndrome that is
attributable to
intellectual
disability, cerebral
palsy, autism,
spina bifida,
or Prader-Willi
syndrome; that
manifests before
the age of 18; and
that constitutes
a substantial
handicap that
can reasonably
be expected
to continue
indefinitely.
Self Injurious
behavior is any
chronic behavior
that results in
injury to the
person’s own
body, including,
but not limited to,
self-hitting, head
banging, self-
biting, scratching,
and the ingestion
of harmful or
potentially
harmful nutritive
or nonnutritive
substances.
Substance
abuse Impaired:
condition
involving the
use of alcoholic
beverages or any
psychoactive or
mood-altering
substance in such
a manner as to
induce mental,
emotional, or
physical problems
and cause socially
dysfunctional
behavior.
EMS means
the activities
or services to
prevent or treat
a sudden critical
illness or injury
and to provide
emergency
medical care
and pre-hospital
emergency
medical
transportation
to sick, injured,
or otherwise
incapacitated
persons.
A person is
incapable
of providing
informed
consent if he
cannot generally
understand
the procedure,
the medically
acceptable
alternatives, and
the substantial
risks and hazards
inherent in
the proposed
treatment or
procedures.
A vulnerable
adult is one
whose ability
to perform the
normal activities
of daily living or
to provide for
his/her own care
or protection is
impaired due
to a mental,
emotional, long-
term physical or
developmental
disability,
dysfunctional,
brain damage, or
the infirmities of
aging.
Neglect by
caregiver or
vulnerable adult
to provide care,
supervision, food,
clothing, shelter
and medical
services essential
for well being.
An incapacitated
person is
one who has
been judicially
determined to
lack the capacity
to manage at
least some of
his/her property
or to meet at
least some of
the essential
health and safety
requirements of
such person.
Incapacity or
incompetent
means the person
is physically or
mentally unable
to communicate
a willful and
knowing health
care decision.
A health care
surrogate is
any competent
adult expressly
designated by
a person to
make health
care decisions
on behalf of the
person upon
the principal’s
incapacity.
A health care
proxy is a
competent adult
who has not
been expressly
designated to
make health
care decisions
for a particular
incapacitated
person, but
who, is one of
the designated
authorized
persons eligible
to make health
care decision for
the individual.
Appendix A - 5
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
A
Baker Act - The
Florida Mental
Health Act
Developmental
Disabilities
Marchman Act Emergency
Medical Services
& Transportation
Adult Abuse,
Neglect, and
Exploitation
Guardianship Health Care
Surrogate &
Proxy
Chapter 394, Part
1, F.S.
s. 393,.11, F.S. Chapter 397, Part
V, F.S.
s. 401.445, F.S. s. 415.1051, F.S. Chapter 744, F.S. Chapter 765, F.S.
Involuntary
Criteria
A person may
be taken to a
receiving facility
for involuntary
examination if
there is reason to
believe that he or
she has a mental
illness and because
of his or her mental
illness the person
has refused or is
unable to consent
to voluntary
examination and
without care or
treatment, the
person is likely to
suff er from neglect
or refuse to care
for self ; such
neglect or refusal
poses a real and
present threat of
substantial harm to
his well-being; and
it is not apparent
that such harm may
be avoided through
the help of willing
family members
or friends or the
provision of other
services; or there
is a substantial
likelihood that
without care or
treatment the
person will cause
serious bodily harm
to self or others in
the near future, as
evidenced by recent
behavior.
Suff ers from
intellectual
disabilities, in
need of residential
services, lacks
the capacity to
give express and
informed consent
to voluntary
admission, and
either lacks the
basic survival and
self-care skills to
provide for one’s
well-being or is
likely to physically
injure others if
allowed to remain
at liberty.
Good faith reason
to believe the
person is substance
abuse impaired,
and, because of
such impairment
has lost the power
of self-control
with respect to
substance use and
either has inflicted,
or threatened or
attempted to inflict,
or unless admitted
is likely to inflict,
physical harm on
self or others or is in
need of substance
abuse services
and, by reason of
substance abuse
impairment, his
judgment has been
so impaired that
he is incapable
of appreciating
his need for such
services and of
making a rational
decision in regard
thereto (mere
refusal insufficient).
Presence of
an emergency
medical condition
in a person who
is intoxicated,
under influence or
drugs or otherwise
incapable of
providing informed
consent.
Emergency
personnel may
take with or
without consent
if incapacitated
to a hospital or
other appropriate
treatment
resources, but
unreasonable force
shall not be used.
Vulnerable adult
alleged to be a
victim of abuse,
neglect, or
exploitation, who
lacks capacity
to consent. This
means a mental
impairment that
causes a person
to lack sufficient
understanding or
capacity to make
or communicate
responsible
decisions
concerning his
person or property,
including whether
or not to accept
protective services
from DCF.
If risk of death or
serious physical
injury, DCF with law
enforcement may
forcibly enter and
may remove person
to a medical or
protective services
facility.
Criteria diff ers
for various types
of guardians,
including:
Natural
Guardians
Guardians of
minors
Emergency
Temporary
Guardians
Standby
Guardians
Pre-Need
Guardians
Foreign
Guardians
Resident
Guardians
Guardian
Advocates
Determination
of incapacity or
incompetence of
a person needing
medical treatment.
Appendix A - 6

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
Appendix A
A
Baker Act - The
Florida Mental
Health Act
Developmental
Disabilities
Marchman Act Emergency
Medical Services
& Transportation
Adult Abuse,
Neglect, and
Exploitation
Guardianship Health Care
Surrogate &
Proxy
Chapter 394, Part
1, F.S.
s. 393. 11, F.S. Chapter 397, Part
V, F.S.
s. 401.445, F.S. s. 415.1051, F.S. Chapter 744, F.S. Chapter 765, F.S.
Initiation
Ex parte order
of a circuit
judge
State
Certified law
enforcement
officer acting
in his or her
official capacity
Specified
professional
(MD, DO,
clinical
psychologist,
LCSW, LMHC,
LMFT or
psychiatric
nurse – all as
defined in 394).
Petitioning
Commission of 3
persons, one must
be a physician,
file petition with
circuit court.
2 forms of
court involved
initiation and 3
forms of non-
court. Protective
custody by LEO
or emergency
admission with
physician’s
certificate, or
petition to circuit
court.
See Appendix N for
details
EMS personnel
may treat without
informed consent
if the patient at
the time of exam
or treatment has
an emergency
medical condition
and is intoxicated,
under the
influence of drugs,
or otherwise
incapable
of providing
informed
consent.
Court order upon
petition by DCF in
non-emergency
cases.
DCF and LEO
may forcibly enter
and may remove
incapacitated
person who is
likely to incur a risk
of death or serious
physical injury.
Petition to the
court to determine
incapacity filed by
an adult.
Order of a circuit
judge stating
the nature of the
guardianship as
either plenary or
limited. If limited,
order states the
rights that have
been removed and
delegated to the
guardian.
Determination
by attending
physician, that
the principal
lacks capacity
to make health
care decisions for
himself.
Health care facility
notifies surrogate
or proxy in writing
that his or her
authority under
the advance
directive has
begun.
Authority
of
Substitute
Decision
Maker
Guardian Advocate
may be appointed
by the court for
any person found
to be incompetent
to consent to
treatment. This
means that a
person’s judgment
is so aff ected
by his or her
mental illness
that he lacks the
capacity to make
a well-reasoned,
willful, and
knowing decision
concerning his
or her medical
or mental health
treatment.
Guardian Advocate
is a person
appointed by the
Circuit Court for
a person with
developmental
disabilities in
any proceedings
brought pursuant
to 393.12 and
excludes the use
of the same term
as applied to a
guardian advocate
for persons with
a mental illness in
Chapter 394.
Guardian Advocate
can be appointed
for the person
during the court
hearing if person
cannot attend.
Otherwise,
no substitute
decision-maker
provided in 397
other than the
parent of a minor.
A Guardian
ad litem must
be appointed
for a minor
unrepresented
by an attorney
in an involuntary
hearing.
Emergency
medical treatment
(that doesn’t
violate an advance
directive) without
consent for
incapacitated
person, after
admission to a
medical facility.
Further treatment
without informed
consent is subject
to a DCF petition
and a court order.
Limited to
authority granted
by Circuit Court:
in Letters of
Guardianship.
Plenary Guardian
shall exercise all
delegable rights
while Limited
Guardian exercises
only those
removed from the
ward in the order.
Must file reports,
plans, inventory,
and accounting.
Make written
consent to health
care decisions the
principal would
have made if
capable of making
such decisions.
(Substitute
Judgement)
Have access to
clinical records,
authorize release
of records for
continuity of care,
authorize transfer
of principal to
or from a health
care facility, and
apply for public
benefits.
Appendix A - 7
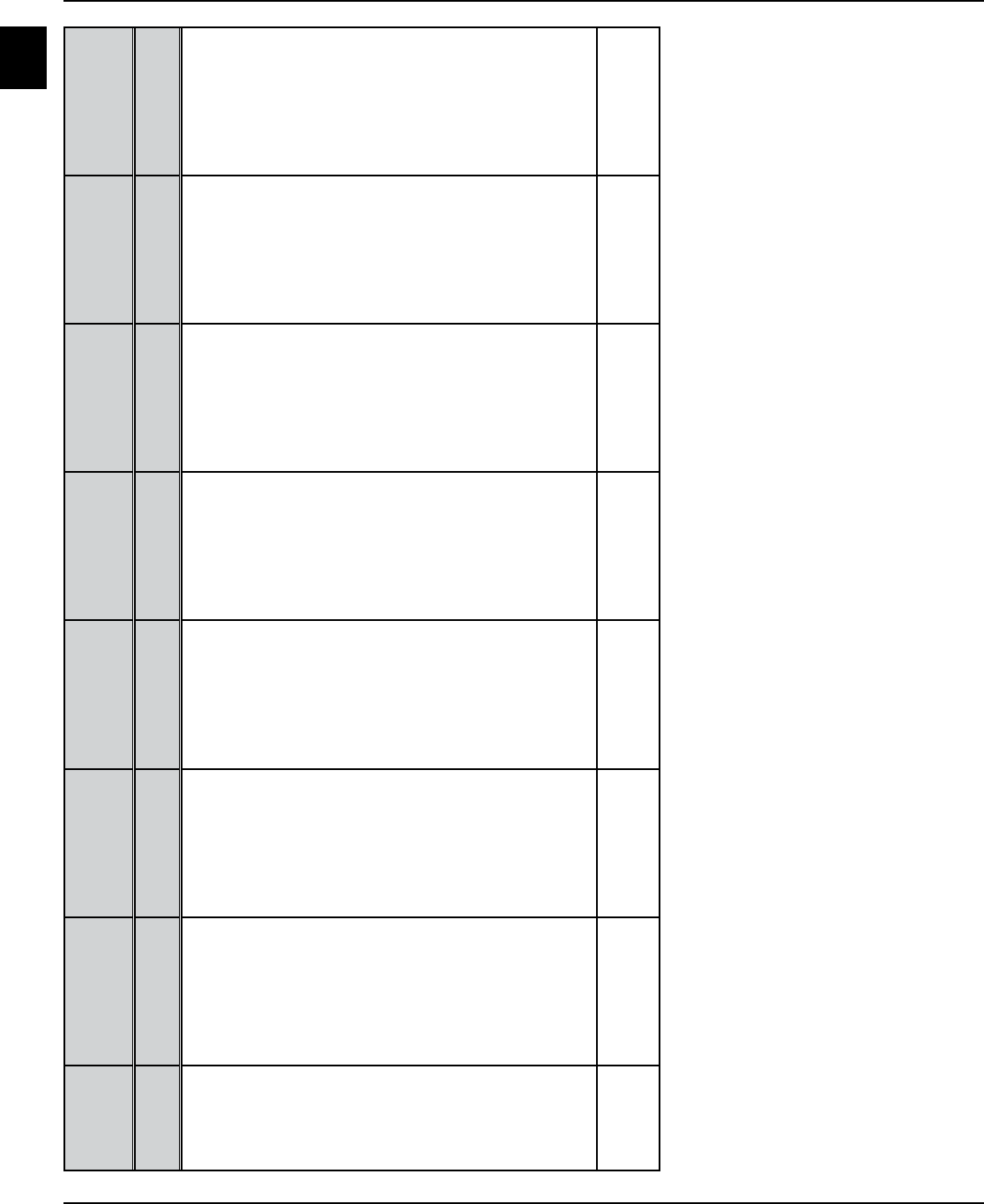
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Related Laws
A
Baker Act - The
Florida Mental
Health Act
Developmental
Disabilities
Marchman Act Emergency
Medical Services
& Transportation
Adult Abuse,
Neglect, and
Exploitation
Guardianship Health Care
Surrogate &
Proxy
Authorizing
Statute
Chapter 394, Part
1, F.S.
s. 393.11, F.S. Chapter 397, Part
V, F.S.
s. 401.445, F.S. s. 415.1051, F.S. Chapter 744, F.S. Chapter 765, F.S.
Limitations
of
Authority
of
Substitute
Decision
Makers
Guardian
Advocate cannot
authorize
voluntary
admission or
consent to
treatment for a
voluntary person.
Cannot consent
to medical
treatment unless
authorized by the
court.
Cannot consent
to ECT and
certain other
extraordinary
procedures
without authority
given by the
court.
Guardian is
prohibited from
having ward
placed voluntarily
in psychiatric
facility but
may consent
to treatment
for a ward on
involuntary
status.
Guardians may
consent to
treatment but not
to admission.
May not consent
to voluntary
admission
of person to
psychiatric
facility or to
the psychiatric
treatment
of a person
on voluntary
status. May not
provide consent
for abortion,
sterilization, ECT,
psychosurgery,
experimental
treatment
without Court
approval or
express authority
in an advance
directive.
See Also 65E-5, FAC
65E-12, FAC
65E-30, FAC
395.1041, F.S.
42USC 1395dd.
Chapter 825, F.S. s. 394.4625 (1)(e),
F.S.
s. 394.4625 (1)
(e), F.S. and 65E-
5.2301
Appendix A - 8

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix B - 1
Voluntary Admissions
Appendix B
B
Voluntary Admissions
s. 394.4625, F.S. Chapter 65E-5.270, F.A.C.
e Baker Act encourages the voluntary admission of persons
for psychiatric care, but only when they are able to fully
understand the decision and its consequences and are able
to fully exercise their rights for themselves. When this is not
possible due to the severity of the person’s condition, the law
requires that the person be extended the due process rights
assured for those under involuntary status. is is further
supported by the U.S. Supreme court case of Zinermon v.
Burch (1990).
Selected Definitions
s. 394.455, F.S.
“Mental illness” means an impairment of the mental or emo-
tional processes that exercise conscious control of one’s actions or
of the ability to perceive or understand reality, which impairment
substantially interferes with a person’s ability to meet the ordi-
nary demands of living, regardless of etiology. For the purposes of
this part, the term does not include a developmental disability as
dened in Chapter 393, intoxication, or conditions manifested
only by antisocial behavior or substance abuse impairment. (18)
“Express and informed consent” means consent voluntarily
given in writing, by a competent person, after sucient
explanation and disclosure of the subject matter involved to
enable the person to make a knowing and willful decision
without any element of force, fraud, deceit, duress, or other
form of constraint or coercion. (9)
“Incompetent to consent to treatment” means that a person’s
judgment is so aected by his or her mental illness that the
person lacks the capacity to make a well-reasoned, willful, and
knowing decision concerning his or her medical or mental
health treatment. (15)
Criteria
s. 394.4625(1)(a), F.S. s. 394.459(3)(a), F.S.
A facility may receive for observation, diagnosis, or treatment
any person 18 years of age or older making application by
express and informed consent for admission or any person age
17 or under for whom such application is made by his or her
guardian. A person age 17 or under can be admitted only after
a hearing to verify the voluntariness of the consent.
If found to show evidence of mental illness, to be competent
to provide express and informed consent, and to be suitable
for treatment, such person 18 years of age or older may be
admitted to the facility.
Each person entering a facility, regardless of age, must be
asked to give express and informed consent for admission
and treatment. If the person is a minor, express and
informed consent for admission and treatment must also be
requested from the person’s guardian. Express and informed
consent for admission and treatment of a person under
18 years of age is required from the person’s guardian. See
Appendix D for extensive information about consent for
admission and treatment of minors.
Exclusions
s. 394.4625(1), F.S.
A facility may not admit a person on a voluntary basis
who has been adjudicated incapacitated and has a
guardian appointed by the court.
e health care surrogate or proxy of a person on
voluntary status may not consent to mental health
treatment for the person. erefore, such a person
must be discharged from the facility or involuntary
placement procedures initiated.
Certain individuals residing in or served by long-
term care facilities such as nursing homes and assisted
living facilities (licensed under Chapter 400 and 429,
F.S.), may not be removed from their residence for
voluntary examination unless previously screened by
an authorized independent mental health professional
and found to be able to provide express and informed
consent to treatment (able to make well-reasoned,
willful, and knowing decisions about their medical
or mental health treatment) (CF-MH 3099). See
Appendix E for additional information about long-term
care facilities
A person on voluntary status who is unwilling or unable
to provide express and informed consent to mental health
treatment must either be discharged from a receiving/
treatment facility or transferred to involuntary status.
Within 24 hours after a voluntary admission, the admitting
physician must document in the person’s clinical record that
the person is able to give express and informed consent for
admission and treatment (CF-MH 3104). If the person is
not able to give express and informed consent, the facility
must either discharge the person or transfer the person to
involuntary status.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Voluntary Admissions
Appendix B - 2
B
Right to Discharge
s. 394.4625(3), F.S.
At the time of admission and at least every six months
thereafter, a person on voluntary status must be notied
in writing of his or her right to apply for a discharge. (CF-
MH 3051)
Transfer from Involuntary
to Voluntary Status
s. 394.4625(4), F.S.
A person on involuntary status who applies to be
transferred to voluntary status must be transferred to
voluntary status, unless the person has been charged with
a crime, or has been involuntarily placed for treatment by
a court and continues to meet the criteria for involuntary
placement.
Before the transfer to voluntary status is processed, the
mandatory initial involuntary examination must be
performed by a physician or clinical psychologist and a
certification of the person’s competence to provide express
and informed consent to treatment must be completed
by a physician. In addition, the competent person must
have formally applied for voluntary admission, without any
coersion.
Such a transfer is contingent on the person meeting the
criteria for voluntary status found above which should be
documented by an Application for Voluntary Admission
(CF-MH 3040, 3097, or 3098) and a Certication of
Person’s Competence to Provide Express and Informed
Consent (CF-MH-3104).
When transfer to voluntary status occurs, notice must be
provided to the person and the person’s guardian advocate,
attorney, and representative.
If a physician has determined the individual transferring
from involuntary to voluntary status is of imminent
danger to self or others, notication to the Clerk of Court
regarding prohibition of rearm purchase or to obtain/
retain a concealed weapon permit may be required (See
Appendix S).
Transfer from Voluntary
to Involuntary Status
s. 394.4625(5), F.S.
At any time a person on voluntary status is determined not to
have the capacity to make well-reasoned, willful, and knowing
decisions about his or her mental health or medical care, he/she
must be transferred to involuntary status.
When a person on voluntary status, or an authorized
individual acting on the person’s behalf, makes a request
for his/her discharge, the request for discharge, unless freely
and voluntarily rescinded, must be communicated to a
physician, clinical psychologist, or psychiatrist as quickly
as possible, but not later than 12 hours after the request is
made.
If the person meets the criteria for involuntary inpatient
placement, the administrator of the facility must le a
petition for involuntary placement (CF-MH 3032) or may
le a petition for involuntary outpatient placement (CF-
MH 3130), with the court within two court working days
after the request for discharge is made. If the petition is not
led within two court working days, the person must be
discharged.
Discharge of Persons
on Voluntary Status
s.394.4625(2), F.S.
A facility must discharge a person on voluntary status:
1. Who has suciently improved so that retention in the
facility is no longer clinically appropriate. A person may
also be discharged to the care of a community facility.
2. Who requests discharge. A person on voluntary status or
a relative, friend, or attorney of the person may request
discharge either orally or in writing at any time following
admission to the facility. (CF-MH 3051)
If the person, or another acting on the person’s behalf,
makes an oral request for discharge to a sta member,
such request must be immediately entered in the person’s
clinical record. If the request for discharge is made by
a person other than the patient, the discharge may be
conditioned upon the express and informed consent of
the person.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix B - 3
Voluntary Admissions
Appendix B
Specialized on-line Baker Act courses can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.
B
e person must be discharged within 24 hours of the
request, unless the request is rescinded or the person
is transferred to involuntary status. e 24-hour time
period may be extended by a treatment facility (which
generally is a state hospital) when necessary for adequate
discharge planning, but must not exceed three days
exclusive of weekends and holidays.
3. A person on voluntary status who has been admitted to a
facility and who refuses to consent to or revokes consent
to treatment (CF-MH 3105) must be discharged
within 24 hours after such refusal or revocation unless
transferred to involuntary status or unless the refusal
or revocation is freely and voluntarily rescinded by the
person.
Elopement of a Person
on Voluntary Status
If a person on voluntary status elopes or leaves the facility
against medical advice, law enforcement should only be
notied to return the person to the receiving facility if the
person is under a criminal charge or it appears the person
meets the criteria for involuntary examination or placement.
A minor’s guardian must be notied as soon as possible that
the minor has eloped or left against advice. e notication
must be documented in the person’s record.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Voluntary Admissions
Appendix B - 4
B
Voluntary Admissions
Quick Reference Guide for Receiving and Treatment Facilities
The person being admitted must:
Have a mental illness, as defined in the law, and
Be suitable for treatment, and
Be competent to provide express and informed consent to the voluntary admission and to treatment as well as being
willing and able to sign an Application for Voluntary Admission (CF-MH 3040 for adults at receiving facilities, CF-MH
3097 for minors, and CF-MH 3098 for State Treatment Facilities)
Prior to admission of a person meeting certain criteria from a long-term care facility licensed under Chapter 400 or 429, F.S.
he or she has been assessed by an authorized service or independent professional as able to provide express and informed
consent to admission and treatment (CF-MH 3099). _____ yes _____ no _____ not applicable
At the time of admission, the facility must open a clinical record containing the following information and may include the
following completed recommended forms:
____ Application for Voluntary Admission (CF-MH 3040, or 3097 or 3098)
____ Notice of Right to Release (CF-MH 3051a for receiving facility and CF-MH 3051b for treatment facility) completed
and given to the person at the time of admission and every 6 months thereafter.
____ General Authorization for Treatment Except Psychotropic Medications (CF-MH 3042a)
____ Inventory of Personal Effects (CF-MH 3043) documenting property brought by the person to the facility, signed by
the person, if able, and witnessed by two staff members.
____ Notice of Right to Petition for Writ of Habeas Corpus or for Redress of Grievances (CF-MH 3036)
_____ Documentation of providing explanation and copy of Rights of Persons in Mental Health Facilities or Programs
(CF-MH 3103)
_____ Intake Interview
_____ Baker Act Service Eligibility Form (CF-MH 3084) for an indigent person at a CSU or other public receiving facility.
Subsequent to the person’s admission, the following should be completed:
____ Documentation by the admitting physician that the person is able to give express and informed consent for
admission. (CF-MH 3104) If not, the person must be discharged or transferred to involuntary status.
____ Documentation of a physical examination by an authorized health practitioner within 24 hours of arrival.
_____ Personal Safety Plan (CF-MH 3124)
____ Completion of a “Specific Authorization for Psychotropic Medications” (CF-MH 3042b) prior to the administration
of any psychotropic medications, after a complete disclosure to the person and to the guardian of a minor of the
following:
____ An individualized treatment plan completed within five days of the person’s admission in which the person has
had the opportunity to assist in preparing, including space for the person’s comments and a copy of which has
been provided to the person and to a minor’s guardian.
Reason for Admission Specific dosage range for medications
Proposed treatment, including proposed Frequency and method of administration
psychotropic medications
Common risks, benefits and common short-term and
Purpose of treatment long-term side effects
Alternative treatments Any contraindications which may exist

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix B - 5
Voluntary Admissions
Appendix B
B
Clinically significant interactive effects with other
medications
Similar information on alternative medication
which may have less severe or serious side effects
Potential effects of stopping treatment
Approximate length of care
The following forms shall be included only if applicable:
How treatment will be monitored, and that
Any consent for treatment may be revoked orally or
in writing before or during the treatment period if
the person legally authorized to make health care
decisions on behalf of the person.
____ Authorization for Release of Information (CF-MH 3044) completed and signed only when such release is to take place.
____ Authorization for Electroconvulsive Treatment (CF-MH 3057)
____ Refusal or Revocation of Consent to Treatment (CF-MH 3105)
____ Restriction of Communication or Visitors (CF-MH 3049)
____ Restriction of Person's Access to Own Record (CF-MH 3110)
____ Petition for Writ of Habeas Corpus or for Redress of Grievances (CF-MH 3090)
____ Application for and Notice of Transfer to Another Facility (CF-MH 3046)
____ Packet of forms to Clerk of Court on firearms prohibition if of imminent danger to self/others
Request for Discharge: If the person, or an authorized person acting on his/her behalf, makes an oral or written request for
discharge, facility staff must:
____ Immediately enter the oral or written request for release in the person’s clinical record.
____ Notify the physician, psychiatrist, or clinical psychologist within 12 hours of the request for discharge.
____ Discharge the person within 24 hours of the request unless a petition for involuntary placement (CF-MH
3032 or 3130) has been initiated. (State hospitals have 3 working days in which to discharge such persons)
If a person requesting discharge meets criteria for involuntary inpatient placement, the facility must (Or in cases of
involuntary outpatient placement, the facility may):
____ Initiate proceedings for involuntary placement within 24 hours by having the first expert opinion
documented on the petition form.
____ File the Petition for Involuntary Placement (CF-MH 3032 or 3130) with the circuit court within two court working days
of the request for discharge.
State Mental Health Facility: If voluntary placement in a state mental health facility is sought for the person, the following
must be completed:
____ Transfer Evaluation (CF-MH 3089)
____ State Mental Health Facilities Admission Form (CF-MH 7000)
____ Physician to Physician Transfer Form (CF-MH 7002)
Recommended forms are those which are not required by the department, but which have been determined to satisfy the
specific requirements for which the form has been developed. Alteration of recommended forms may jeopardize this status.
Mandatory forms may not be altered. No blank forms should be signed by staff, the person, or substitute decision-maker.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Voluntary Admissions
Appendix B - 6
B
Physician assessment of person's ability to provide
express and informed consent conducted within 24
hours after admission
Person not able to give express and
informed consent to treatment
Person is able to give express and
informed consent to treatment
Transfer person to
involuntary status
Discharge person
File a Petition for Involuntary Inpatient
or Involuntary Outpatient Placement
with court within two court working
days
May be treated until discharged
unless ability to provide express and
informed consent is in doubt
Adult Seeking Voluntary Admission
(other than from a facility licensed under Chapter 400/429, F.S.)
Criteria:
18 years of age or older
Shows evidence of mental illness
Suitable for treatment
Competent to provide express and informed consent to treatment
(Can make well-reasoned, willful, and knowing decisions regarding medical or
mental health treatment)

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix B - 7
Voluntary Admissions
Appendix B
B
Request for Discharge of Person on Voluntary Status
By competent adult
By other authorized person acting on
person's behalf
Notify attending physician or
psychologist within 12 hours
Consultation with person
Petition for involuntary
Inpatient/Outpatient
placement initiated by
at least one psychiatrist
within 24 hours
Document in clinical
record-person
remains in facility
until hearing
Person discharged within
24 hours of request
from receiving facility
or 3 working days from
treatment facility
Second opinion by
a psychologist or 2
nd
psychiatrist and petition
signed by administrator
and filed with circuit
court within 2 working
days of the request for
discharge
Court hearing
within 5 working
days unless person
requests and court
grants a continuance
Person does not
concur with request
for discharge
Person
concurs with
request for
discharge

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Voluntary Admissions
Appendix B - 8
B

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix C - 1
Express and Informed Consent
Appendix C
C
Express and Informed Consent
s. 394.459(3), F.S. Chapter 65E-5.170, F.A.C.
Consent in the mental health treatment context is simply the
Reason for admission or treatment
agreement of one person to accept the actions or decisions
of another as his/her own. Consent must be voluntary,
by a person who is competent to choose, and who is fully
informed and understands the consequences of that choice.
Individuals competent to consent to treatment are also
competent to refuse or revoke consent to treatment. When
a person is not competent to choose, he or she must be
transferred to involuntary status. ere are legally prescribed
methods for obtaining substitute decision-making in such
circumstances.
Express and Informed Consent is dened in the
Baker Act as consent voluntarily given in writing, by
a competent person, after sucient explanation and
disclosure of the subject matter involved to enable the
person to make a knowing and willful decision without
any element of force, fraud, deceit, duress, or other form
of constraint or coercion.
A person is incompetent to consent to treatment, as
dened in the Baker Act, as one whose judgment is so
aected by mental illness that he or she lacks the capacity
to make a well-reasoned, willful, and knowing decision
concerning medical or mental health treatment.
Each person entering a facility, other than those who are
incapacitated or incompetent to consent to treatment, must
be asked to give express and informed consent for admission
and treatment. If the person is a minor, express and
informed consent for admission and treatment is required
from the guardian.
No person can be administered treatment in a receiving or
treatment facility without express and informed consent to
the treatment having rst been provided by a person legally
authorized to give that consent, except in documented cases
of imminent danger when a physician orders emergency
treatment.
Prior to seeking such consent, the person and/or guardian
(if incapacitated or a minor), or guardian advocate or health
care surrogate/proxy must be given at least the following
information and the clinical record should reect that the
person or substitute decision-maker clearly understood
the information, had an opportunity to ask questions /
get answers about the information, and understood the
consequences of providing or withholding consent:
Proposed treatment, including proposed psychotropic
medications
Purpose of treatment to be provided
Alternative treatments
Specic dosage range for medication
Frequency and method of administration
Common risks, benets and common short-term and
long-term side eects
Any contraindications which may exist
Clinically signicant interactive eects with other
medications
Similar information on alternative medication which
may have less severe or serious side eects
Potential eects of stopping treatment
Approximate length of care
How treatment will be monitored, and that
Notication that any consent for treatment may be
revoked orally or in writing before or during the
treatment period by the person legally authorized to
make health care decisions on behalf of the person.
Documentation of Competence to
Provide Express and Informed Consent
e admitting physician must determine whether a person
being admitted to a receiving or treatment facility is
competent to provide express and informed consent to his/
her admission and treatment.
An adult admitted on a voluntary basis or transferred
from involuntary to voluntary status must be
competent to provide his or her own consent. e
guardian of a minor must be willing to provide express
and informed consent for the minor.
A person admitted on an involuntary status may or
may not be competent to provide express and informed
consent for his/her own treatment.
In any case, when an adult is permitted to provide consent
for his/her own treatment, the physician must document
in the clinical record the adult’s competence to make
well-reasoned, willful, and knowing mental health and

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
Appendix C - 2
C
medical decisions. If not competent to consent, as dened
above, the facility administrator must release the person
or petition the court for appointment of a guardian
advocate, unless the person already has a court-appointed
guardian. Only when the safety of the person or others is
in imminent danger, may the physician order emergency
treatment.
Emergency psychiatric treatment (ETO) may be
rendered in the least restrictive manner upon the written
order of a physician, if it is determined that such treatment
is necessary for the safety of the person or others and
express and informed consent from an authorized person
is unavailable. If the person has not had a guardian
appointed by the court, a petition for a guardian advocate
must be initiated within 24 hours and submitted to the
court within two court working days (unless only one ETO
is ordered within a two day period).
Drugs used as a restraint are medications used to control
behavior or to restrict the person’s freedom of movement
and are not a standard treatment for the person’s medical or
psychiatric condition. Chemical restraints are also regulated
by federal conditions of participation and accrediting
organizations.
e administrator of a receiving or treatment facility
may, upon the recommendation of the person’s attending
physician, authorize emergency medical treatment,
including a surgical procedure, if such treatment is deemed
lifesaving, or if the situation threatens serious bodily harm
to the person, and informed consent of the person or the
person’s guardian or guardian advocate cannot be obtained.
See Appendix I for more information about emergency
treatment orders.
Electroconvulsive treatment (ECT) may be authorized
by a competent person, or by a guardian, or by a guardian
advocate who has been given express court authority to
consent to electroconvulsive treatment. [s. 394.459(3)(b),
F.S.] Section 458.325, F.S. requires that electroconvulsive
treatment be agreed to by a second physician not directly
involved with the responsibility for the person’s care. Such
agreement must be documented in the person’s treatment
record and must be signed by both physicians.
Persons Determined Incompetent to
Consent to Treatment
s. 394.4598, F.S. Chapter 65E-5.230, F.A.C.
e administrator of a receiving or treatment facility may
petition the court for the appointment of a guardian advocate
based upon the opinion of a psychiatrist that the person is
incompetent - unable to make well-reasoned, willful and
knowing decisions about his or her medical or mental health
treatment.
Before giving consent to treatment, the guardian advocate
must meet and talk with the individual and the individual’s
physician in person, if at all possible, and by telephone, if not.
e guardian advocate must certify that such communication
with the individual and physician has taken place before
authorizing treatment. e guardian advocate must also
complete court-ordered training. See the Guardian Advocate
Training & Resource Manual for extensive information about
the duties of a guardian advocate. e Manual can be found
on the DCF website http://www.dcf.state..us/ . A specialized
web-based training course for Guardian Advocates can be
found at http://guardianadvocate.org/.
Persons Adjudicated Incapacitated
Chapter 394.4625(1)(d) F.S.
e Baker Act prohibits the voluntary admission of any
person who has been adjudicated by a court as incapacitated
even though the guardianship law [744.3725, FS] denes
specic steps the court must follow before granting a
guardian the authority to do so. e rst District Court
of Appeals has ruled that where the Baker Act and the
guardianship law conict on least restrictive alternatives, the
Baker Act prevails (Hanley v. Dennis).
e court order adjudicating the person as incapacitated will
designate who is the guardian. Letters of guardianship are
issued to the guardian and specify whether the guardianship
pertains to the person, or to the property, or both, of the
ward. e letters will state whether the guardianship is
plenary or limited, and, if limited, the letters must state
the powers and duties of the guardian. [s. 744.345, F.S.]
e guardian can only be permitted to perform those
responsibilities that have been expressly removed from the
ward and delegated to the guardian.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix C - 3
Express and Informed Consent
Appendix C
C
Persons with Health Care
Surrogates / Proxies
Chapter 765, F.S. Chapter 65E-5.2301, F.A.C.
Any competent adult may execute an advance directive
designating any other adult to make his/her health-related
decisions should he/she ever become incompetent to make
these decisions. If the person has not executed an advance
directive or the surrogate selected by the person is not
available, health care decisions may be made by a proxy
chosen from a statutorily authorized prioritized list of
persons: guardian, spouse, adult child, parent, adult sibling,
adult relative, close friend, or independent licensed clinical
social worker.
If a person’s capacity to make health care decisions for
oneself or provide express and informed consent is in
question, the attending physician should evaluate the
person’s capacity. If the attending physician concludes that
the person lacks such capacity to make mental health care
decisions, the facility must enter the physician’s evaluation
in the person’s clinical record and notify the surrogate
or proxy in writing that his/her authority to act has
commenced (recommended form “Certication of Person’s
Incompetence to Consent to Treatment and Notication
of Health Care Surrogate/Proxy” CF-MH 3122 may be
used). e authority thus activated remains in eect until a
determination that the person has regained his/her capacity.
When a healthcare proxy is designated, the proxy should also
complete an adavit (CF-MH 3123).
A specialized Mental Health Advance Directive has been
developed for optional use and can be found at the end of
this appendix.
During the interim period between the time a person is
determined by a physician to be incompetent to consent to
treatment and the time a guardian advocate is appointed
by a court to provide express and informed consent to the
person’s treatment, the health care surrogate or proxy may
provide such consent to treatment.
A petition for adjudication of incompetence to consent to
treatment and appointment of a guardian advocate must be
led with the court within two court working days of the
determination by the physician of the person’s incompetence
to consent to treatment. Recommended form “Petition for
Adjudication of Incompetence to Consent to Treatment and
Appointment of a Guardian Advocate,” (CF-MH 3106)
may be used.
e facility must immediately provide to the health care
surrogate or proxy the same information required by statute
to be provided to the guardian advocate. In order to protect
the safety of the person, the facility must make available to
the health care surrogate or proxy the same training required
of guardian advocates and ensure that the surrogate or proxy
communicates with the person and person’s physician prior
to giving express and informed consent to treatment.
e surrogate or proxy may only provide consent for
treatment for persons on involuntary status. e surrogate or
proxy has the authority to:
Make any and all health care decisions, but must make
those decisions based upon what he or she believes
the principal would have decided if that principal was
capable of making such decisions, (substitute judgment).
Only if the surrogate/proxy doesn’t know what the
person would have wanted can a “best interest” standard
be used;
Access the person’s clinical record;
Authorize the release of information and clinical records
to appropriate persons to ensure the continuity of the
person’s health care;
Apply for private, public, governmental, or veteran’s
benets to defray the cost of health care and to have
access to nancial information of the principal and;
Authorize transfers to and from other facilities.
Summary of Consent Issues
A person who is competent to provide express and informed
consent to admission or to treatment is competent to refuse
or revoke such consent. A mere refusal or revocation of
consent does not justify a transfer to involuntary status
without clear documentation of other behaviors by the
person that satisfy the involuntary placement criteria.
However, a person who has been adjudicated incapacitated or
found to be incompetent to consent to treatment by a court
is incapable of refusing treatment that has been authorized,
by express and informed consent, by a legally authorized
substitute decision-maker.
Specialized on-line Baker Act courses can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
C
Summary Reference on Substitute Decision Making
(Does not substitute for Statutes or Legal Advice)
Guardian Guardian Advocate Representative
Health Care
Surrogate (HCS)
Health Care Proxy
(HCP)
Statutory
Citation
Chapter 744, F.S. s. 394.4598, F.S. s. 394.4597, F.S. Chapter 765, Part
II, F.S.
Chapter 765, Part IV, F.S.
Initiation Petition to determine
incapacity filed by an
adult.
Determination by a
psychiatrist that the
person is incompetent
to provide express and
informed consent to
treatment.
Conversion from
voluntary to
involuntary status
or admission to a
receiving or treatment
facility on involuntary
status.
Determination by
attending physician,
that principal lacks
capacity to make
health care decisions
for him/her self.
Same as Health Care
Surrogate
Appointment Order of a Circuit Judge
stating the nature of the
guardianship as either
plenary or limited. If
limited, order states the
rights which have been
removed and delegated
to the guardian.
Circuit judge upon
petition of Receiving
or Treatment Facility
Administrator
and adjudication
of incompetence to
consent to treatment.
Selected by the
person if possible;
if not, designated
by the facility from
a prioritized list
specified in law.
Healthcare facility
notifies Surrogate
in writing that
authority under the
advance directive has
commenced.
Health care facility
notifies Proxy in writing
that authority has
commenced.
Qualifications Competent adult; if
non-resident, must
be related by blood or
adoption. Preference
given to wishes of ward,
to a relative, and to a
person with ability to
perform. Prohibits a
felon, an incapacitated
person, creditor, or other
unsuitable person, or
one with a conflict of
interest. If providing any
professional or business
services, must be a close
relative. Prohibits a
judge unless related to
ward. See law for other
limitations.
Same as guardian
but gives preference
to HCS followed by
spouse, adult child,
parent, adult next of
kin, adult friend, or
trained adult. Prohibits
MH professional, facility
employee, or DCF, from
serving.
Any competent
adult selected by the
person. Otherwise
preference given to
HCS, followed by
spouse, adult child,
parent, adult next of
kin or adult friend.
Prohibits licensed
professional, facility
employee, DCF staff,
creditor, or other
person providing
substantial services
from serving.
Any competent
adult selected by the
principal through an
advance directive.
Designated by law
from a prioritized list
of persons including
guardian, spouse, adult
child, parent, adult
sibling, adult relative,
close friend*, or clinical
social worker*.
*Friend is defined in
law and LCSW limits
provided in law.
Requirements 40 hours training on
duties, rights of ward,
local resources, and
plans/reports within 1
year of appointment.
Professional and public
guardian must take oath
and file a bond (unless
waived).
Agreement to serve,
undergo 4 hour training
course, meet with
person and physician
prior to providing
consent.
No prerequisites or
training required.
No prerequisites or
training required
by law. 65E-5.2301
FAC requires HCS
to be given same
information required
to be given to gardian
advocate.
Same as Health Care
Surrogate
Appendix C - 4

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
Appendix C
C
Guardian Guardian Advocate Representative
Health Care
Surrogate (HCS)
Health Care Proxy
(HCP)
Tenure While person is
incapacitated.
While person is
incompetent to consent
to treatment.
While person is on
involuntary status in a
receiving or treatment
facility.
While principal
is physically or
mentally unable to
communicate a willful
and knowing health
care decision.
Same authority
as a Health Care
Surrogate.
Authority Limited to authority
granted by Circuit
Court in Letters of
Guardianship. Plenary
Guardian shall exercise
all delegable rights
while Limited Guardian
exercises only those
removed from the ward
in the order. Must file
reports, plans, inventory,
and accounting.
Consent to psychiatric
treatment, access
client record, and
release of information
for continuity of
care. Consent to
medical care, ECT,
abortion, sterilization,
psychosurgery, and
experimental treatment
only upon Court
approval. Receives all
notices and may file
Habeas petition.
Receives notices of
proceedings and any
restrictions during the
time a person is held
in or admitted to a
receiving or treatment
facility. Has standing
to file a Petition for
Habeas Corpus if it is
believed the person
is being held illegally
or to file a petition
if person is unjustly
denied a right or
privilege.
Make written consent
to health care
decisions the principal
would have made if
capable of making
such decisions. Have
access to clinical
records, authorize
release of records for
continuity of care,
authorize transfer of
principal to or from
a health care facility,
and apply for public
benefits.
Same as Health Care
Surrogate.
Limitations Prohibited from having
ward admitted on a
voluntary basis for
psychiatric examination
or treatment. May only
consent to treatment of
ward if on involuntary
status.
Medical, ECT, and
other extraordinary
interventions are
prohibited without
Court approval.
Has no authority
other than described
above.
May not consent to
psychiatric treatment
for a person on a
voluntary status.
May not provide
consent for abortion,
sterilization, ECT,
psychosurgery,
or experimental
treatment without
Court approval or
express authority in
an advance directive.
Same authority
as a Health Care
Surrogate.
Termination Upon resignation
of guardian and
appointment of
successor guardian;
upon restoration of
capacity; or removal of
guardian by the Court.
Persons' restoration of
competency, discharge
from involuntary
inpatient/outpatient
placement, or transfer
to voluntary status.
Transfer to voluntary
status or discharge
from receiving or
treatment facility.
Upon revocation of
the advance directive
by a competent
principal, upon the
principal’s gaining
capacity to consent,
or removal by court.
Same as Health Care
Surrogate.
Appendix C - 5

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
Appendix C - 6
C
Mental Health Advance Directive
If you believe you may be hospitalized for mental health care in the future and that your doctor may think you
aren’t able to make good decisions about your treatment, then completing a mental health advance directive will
ensure that your treatment choices are known. It is important that you decide NOW what types of treatment you
do or do not want and to appoint a friend or family member to make the mental health care decisions that you
want carried out. You may always change your preferences or surrogate later.
You can use the following Advance Directive form to direct your future care.
Read each section of the form carefully and talk about your choices with someone you trust.
The person you choose to be your health care surrogate and alternate must be a competent adult whose
civil rights have not been taken away. The person you choose should not be a mental health professional, an
employee of a facility that might provide services to you, or an employee of the Department of Children &
Family Services.
You should sign the form in front of two witnesses.
Make sure your surrogate understands your wishes and is willing to accept the responsibility. Your surrogate
(and a back-up alternate surrogate if you wish) should sign this form now or at a later time to show they are
aware you have chosen them to be your surrogate.
Have copies made and give them to your surrogate, your case manager, your doctor, the hospital or crisis unit at
which you are most likely be treated, your family and anyone else who might be involved in your care. Discuss
your choices with each of them.
The document should be available quickly if you need it. If you travel, be sure to take a copy with you.
Your advance directive will not take effect unless a physician decides that you are not competent to make your
own treatment decisions. If you are in a psychiatric facility on an involuntary basis, you will have an attorney
appointed to represent your interests and a hearing will be conducted in front of a judge or magistrate. A health
care surrogate is not authorized to consent to treatment for a person on voluntary status.
I, ____________________________________________, being of sound mind, willfully and voluntarily execute this
mental health advance directive to assure that if I should be found incompetent to consent to my own mental
health treatment, my choices regarding my treatment will be carried out despite my inability to make informed
decisions for myself.
If a guardian, guardian advocate or other decision maker is appointed by a court to make health care or mental
health decisions for me, I intend this document to take precedence over all other means of determining my intent
while competent. This document represents my wishes, and it should be given the greatest possible legal weight
and respect. If the surrogate(s) named in this directive are not available, my wishes shall be binding on whoever is
appointed to make such decisions.
If I become incompetent to make decisions about my own mental health treatment, I have authorized a mental
health care surrogate to make certain treatment decisions for me. My surrogate is also authorized to apply for
public benefits to defray the cost of my health care, to release information to appropriate persons and to authorize
my transfer from a health care facility.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix C - 7
Express and Informed Consent
Appendix C
C
My mental health care surrogate is:
Name: _____________________________________________________________________________
Address: ___________________________________________________________________________
Day Telephone: ________________________ Evening Telephone: ____________________________
If the person named above is unable or unavailable to serve as my mental health care surrogate, I hereby
appoint and request immediate notification of my alternate mental health care surrogate as follows:
Name of Alternate: ___________________________________________________________________
Address: ___________________________________________________________________________
Day Telephone: ________________________ Evening Telephone: ____________________________
Complete the following or Initial in the blank marked yes or no:
A. If I become incompetent to give consent to mental health treatment, I give my mental health care surrogate
full power and authority to make mental health care decisions for me. This includes the right to consent,
refuse consent or withdraw consent to any mental health care, treatment, service or procedure consistent with
any instructions and/or limitations I have stated in this advance directive. If I have not expressed a choice in
this advance directive, I authorize my surrogate to make the decision that (s)he determines is the decision I
would make if I were competent to do so. _____Yes ____No
B. My choices of treatment facilities are as follows:
1. In the event my psychiatric condition is serious enough to require 24-hour care, I would prefer to receive this care in
this/these facilities:
Facility: _________________________ Facility: ___________________________________
2. I do not wish to be admitted to the following facilities for psychiatric care (optional):
Facility: __________________________ Facility: ___________________________________
C. My choice of a treating physician is:
First choice of physician: ____________________ Second choice of physician: _______________
I do not wish to be treated by the following physicians: (optional)
Name of physician: ______________________ Name of Physician: _______________________
D. My wishes about confidentiality of my admission to a facility and my treatment while there are as follows:
1. My representative may be notified of my involuntary admission ___ Yes ___ No
2. Any person who seeks to contact me while I am in a facility may be told I am there. __ Yes __ No
3. I consent to release of information about my condition and treatment plan ___ Yes ___ No
To the following persons: _________________________ _______________________________
_________________________ _______________________________
_________________________ _______________________________
4. If I am incompetent to give consent, I want staff to immediately notify the following persons that I have been
admitted to a psychiatric facility.
Name: _______________________________________ Relationship: ___________________________
Address: _____________________________________________________________________________
Day Phone: _____________________________ ______Evening Phone: _________________________
Name: _______________________________________ Relationship: ___________________________
Address: _____________________________________________________________________________
Day Phone: __________________________________ Evening Phone: __________________________

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
Appendix C - 8
C
______________________________________________________________________________________________
__________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
_______________________________________________________________________________________
______________________________________________________________________________________________
____________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
E. If I am not competent to consent to my own treatment or to refuse medications relating to my mental
health treatment, I have initialed one of the following, which represents my wishes:
1. _____I wish to take the medications that Dr. ________________________________ recommends.
2. _____I wish to take the medications agreed to by my mental health care surrogate after consulting with my
treating physician and any other individuals my surrogate deems appropriate, with the exceptions found in #3
below.
3. _____I specifically do not wish to take and I do not authorize my mental health care surrogate to consent to the
administration of the following medications or their respective brand name, trade name or generic equivalents:
(list name of drug):______________________________________________________________________________
4. _____I am willing to take the medications excluded in #3 above if my only reason for excluding them is their side
effects and the dosage can be adjusted to eliminate those side effects.
5. I have the following other preferences about psychiatric treatment and medications: ________________________
F. Florida law prohibits a mental health care surrogate from consenting to experimental treatments that have
not been approved by a federally approved institutional review board without my prior written consent or
the express approval of the court.
_____ I wish to participate in experimental drug studies or drug trials
_____ I do not wish to participate in experimental drug studies or drug trials
G. My wishes regarding Electroconvulsive Therapy (ECT) are as follows:
1 _____My surrogate may not consent to ECT without express court approval.
2. _____I authorize my surrogate to consent to ECT, but only (initial one of the following):
a. _____ with the number of treatments the attending psychiatrist thinks is appropriate; OR
b. _____ with the number of treatments that Dr. ____________ thinks is appropriate; OR
c. _____for no more than the following number of ECT treatments: ________.
3. Other instructions and wishes regarding ECT are as follows: ____________________________ ________________
H. I ____have / ____ have not attached to this advance directive a Personal Safety Plan, regarding my
preferences.
I. Other instructions I wish to make about my mental health care are (use additional pages if needed): _______
______________________Check here ( ) if other pages are used

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix C - 9
Express and Informed Consent
Appendix C
C
_________________________________ ____________________________________
_________________________________ _____________________________________
_________________________________ _____________________________________
_________________________________ _____________________________________
_____________________________________________________________________________________________
_____________________________________________ __________________________
_____________________________________________ _________________________
Signature
By signing here I indicate that I fully understand that this advance directive will permit my mental health care
surrogate to make decisions and to provide, withhold or withdraw consent for my mental health treatment.
Printed Name (Declarant): ________________________________________________________
Signature: ____________________________________________Date: _____________________
Witnesses
This advance directive was signed by _____________________________ in our presence. At his/her request, we
have signed our names below as witnesses. We declare that, at the time this advance directive was signed, the
Declarant, according to our best knowledge and belief, was of sound mind and under no constraint or undue
influence. We further declare that we are both adults, are not designated in this advance directive as the mental
health care surrogate, and at least one of us is neither the person’s spouse nor blood relative.
Dated at _______________________ This __________day of _____________, _________.
(County & State) (Day) (Month) (Year)
Witness 1: Witness 2:
Signature of witness 1 Signature of witness 2
Printed name of witness 1 Printed name of witness 2
Address of witness 1 Address of witness 2
City, State, Zip Code of witness 1 City, State, Zip Code of witness 2
Acknowledgement of Health Care Surrogate/Alternate
I, __________________________________________, mental health care surrogate designated by ________
____________________________________________, hereby accept the designation.
(Signature of Mental Health Care Surrogate) (Date)
I, __________________________________________, alternate mental health care surrogate designated by
__________________________________________, hereby accept the designation.
(Signature of Alternate Mental Health Care Surrogate) (Date)

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Express and Informed Consent
Appendix C - 10
C

Appendix D - 1 Consent for Minors
Appendix D
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
D
Consent for Admission and Treatment for Minors
(Baker Act, Marchman Act/Substance Abuse, and Medical-related Statutes)
Cautionary Note:
Many statutes, case law, and rules govern how minors are to be treated in Florida. Some of these legal requirements regarding
mental health differ, based on whether the minor lives with his/her own family or is in the custody of the Department of Children
& Families or Department of Juvenile Justice, whether the minor is on voluntary or involuntary status, whether the issue relates to
admission or to treatment, and whether the issue relates to inpatient, residential or outpatient settings. Mental health requirements
applying to minors are different than those applying to substance abuse and general medical examination/treatment. Consult with
an attorney for legal advice.
e Baker Act makes only a few distinctions between adults
and minors. Where distinctions are not made, adults and
minors have the same rights and are to be treated the same.
Specic reference to the admission and treatment of minors
in the Baker Act and other statutes are summarized here, with
the corresponding statutory references.
Since the Baker Act contains so few specic references to
minors, and since this law must be carried out in the context
of other coexisting statutes and case law, it is important for
each professional and mental health agency to involve legal
counsel in reviewing policies and procedures for properly
carrying out one’s responsibilities. Legal consultation on an
on-going basis is necessary to assure responsible and lawful
conduct. In each circumstance in which consent to admission
and/or treatment is sought for a minor, it is essential that the
professional consider the nature and context of the consent in
determining whether the consent is legally sucient.
A specialized on-line Baker Act course for persons
dealing with minors can be found at
www.bakeracttraining.org.
Minority/Non-Age
e Baker Act considers all persons under the age of 18 to be
minors. However, for other purposes, the following may apply:
“Minor” means a person under 18 years of age whose
disabilities have not been removed by marriage or otherwise.
[s. 744.102(13), F.S.]
Removal of Disabilities of Non-Age:
Married minors. e disability of nonage of a minor
who is married or has been married or subsequently
becomes married, including one whose marriage is
dissolved, or who is widowed, or widowered, is removed.
e minor may assume the management of his or her
estate, contract and be contracted with, sue and be sued,
and perform all acts that he or she could do if not a
minor. [s.743.01, F.S.]
Unwed Pregnant Minors or Minor Mothers. An
unwed pregnant minor may consent to the performance
of medical or surgical care or services relating to her
pregnancy by a hospital or clinic or by a physician licensed
under chapter 458 or chapter 459, and such consent is
valid and binding as if she had achieved her majority. She
may consent to the performance of medical or surgical
care or services for her child by a hospital or clinic or by a
physician licensed under chapter 458 or chapter 459, and
such consent is valid and binding as if she had achieved
her majority. However, this doesn’t aect the provisions
of s. 390.0111 which governs Termination of Pregnancy.
[s.743.065, F.S.]
Circuit Court. A circuit court has jurisdiction to
remove the disabilities of nonage of a minor age 16 or
older residing in this state upon a petition led by the
minor’s natural or legal guardian or, if there is none, by a
guardian ad litem. e court shall consider the petition
and, if satised that the removal of the disabilities is in
the minor’s best interest, shall remove the disabilities of
nonage; and shall authorize the minor to perform all acts
that the minor could do if he or she were 18 years of age.
[s.743.015, F.S.]
Minors adjudicated as adults. e disability of nonage
of a minor adjudicated as an adult and in the custody or
under the supervision of the Department of Corrections
is removed, as such disability relates to health care
services, except in regard to medical services relating to
abortion and sterilization. [s.743.066, F.S.]

Consent for Minors
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix D - 2
D
Rights, privileges, and obligations of persons 18 years of
age or older [s.743.07, F.S.]
e disability of nonage is hereby removed for all
persons in this state who are 18 years of age or older,
and they shall enjoy and suer the rights, privileges,
and obligations of all persons 21 years of age or older
except as otherwise excluded by the State Constitution
immediately preceding the eective date of this section
and except as otherwise provided in the Beverage Law.
is section shall not prohibit any court of
competent jurisdiction from requiring support for a
dependent person beyond the age of 18 years when
such dependency is because of a mental or physical
incapacity which began prior to such person reaching
majority or if the person is dependent in fact, is
between the ages of 18 and 19, and is still in high
school, performing in good faith with a reasonable
expectation of graduation before the age of 19.
Consent to Treatment
Generally, persons under the age of 18 cannot consent
to their own treatment because they are presumed to be
legally incompetent as a result of their age or presumed
immaturity of judgment. When needed, parents usually
provide consent on their children’s behalf, except where
parental consent is not required. e mother and father
jointly are natural guardians of their own biological
children and of their adopted children during minority.
[s.744.301, (1) F.S.] However:
If one parent dies, the natural guardianship passes to
the surviving parent, and the right continues even
though the surviving parent remarries.
If the marriage between the parents is dissolved, the
natural guardianship belongs to the parent to whom
the responsibility of the child is given. (See Chapter
61, F.S., governing dissolution of marriage.)
If the parents share parental responsibility, then both
continue as natural guardians.
If the marriage is dissolved and neither the father nor
the mother is given parental responsibility of the child,
neither can act as natural guardian of the child.
e mother of a child born out of wedlock is the
natural guardian of the child and is entitled to primary
residential care and custody of the child unless a court
enters an order stating otherwise.
Upon petition of a parent, brother, sister, next of
kin, or other person interested in the welfare of a
minor, a guardian for a minor may be appointed by
the court without appointing an examining committee
or adjudicating the child incapacitated. A guardian
appointed for a minor, whether of the person or
property, has the authority of a plenary guardian. [s.
744.3021(1) and s.744.342. F.S.] e court must
consider the preference of a minor who is age 14 or over
as to who should be appointed guardian. [s. 744.312(3)
(b), F.S.]
“Legal custody” means a legal status created by a court which
vests in a custodian of the person or guardian, whether an
agency or an individual, the right to have physical custody of
the child and the right and duty to protect, nurture, guide,
and discipline the child and to provide him or her with food,
shelter, education, and ordinary medical, dental, psychiatric,
and psychological care. [s. 39.01(35), F.S.]
A guardian appointed by the court does not have the power
to admit the minor to a facility, institution, or licensed service
provider without formal placement proceeding, pursuant
to Chapter 393, Chapter 394, or Chapter 397 without first
obtaining specific authority from the court, as described in s.
744.3725. [s. 744.3215(4)(a), F.S.]
e 2008 Florida Legislature extensively rewrote state laws
(chapter 61, F.S.) governing the dissolution of marriage
(SB2532). is action substantially changed terms used
as well as the relationship among the parties of a divorce
as it pertained to children. It removed the term “divorce,”
exchanged the term “custody” with “parental responsibility”
and changed the term “visitation” for “time sharing.” Some of
these terms are as follows:
Parenting Plan. Governs all circumstances among the
parties including decision-making and time sharing.
Shared Parental Responsibility. Court-ordered
relationship in which both parents retain full parental
rights/responsibilities and shared decision-making.
Certain decisions may be assigned to one parent.
Sole Parental Responsibility. Court-ordered relationship
in which one parent makes decisions (with or without
visitation).
Time Sharing Schedule. A time table included in
Parenting Plan that specied the time the child will
spend with each parent.
Access to Information. Treatment records are available
to either parent unless the court specically revokes this
right.

Appendix D - 3 Consent for Minors
Appendix D
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
D
Consent to Mental Health Admission
Admission
A facility may receive for observation, diagnosis or treatment
any person age 17 or under and for whom such application
is made by his or her guardian, only after a hearing to verify
the voluntariness of the consent. [s. 394.4625(1), F.S.]
A facility is dened in the Baker Act as:
Any hospital, community facility under contract with
the department, public or private facility, or receiving
or treatment facility providing for the evaluation,
diagnosis, care, treatment, training, or hospitalization of
persons who appear to have a mental illness or have been
diagnosed as having a mental illness.
Each person, regardless of age, who enters treatment must
be asked to give express and informed consent for admission
and for treatment. If the person is a minor, express and
informed consent for admission and treatment must also be
requested from the guardian, but such consent is required
from the guardian. [394.459(3)(a) F.S.]
Hospitals
A minor under the age of 14 who is admitted to any hospital
licensed pursuant to Chapter 395, F.S. may not be admitted
to a bed in a room or ward with an adult in a mental health
unit or share common areas with an adult in a mental health
unit. However, a minor 14 years of age or older may be
admitted to a bed in a room or ward in the mental health
unit with an adult if the admitting physician documents in
the case record that such placement is medically indicated
or for reasons of safety. Such placement must be reviewed
by the attending physician or a designee or on-call
physician each day and documented in the case record. [s.
394.4785(2), F.S.]
In addition, all hospitals are required to ensure full compliance
with the Baker Act as a condition of licensure, as follows:
395.003(5)(a), F.S. governing licensure of all hospitals
states “Adherence to patient rights, standards of care,
and examination and placement procedures provided
under part I of chapter 394 shall be a condition
of licensure for hospitals providing voluntary or
involuntary medical or psychiatric observation,
evaluation, diagnosis, or treatment.”
395.003(5)(b), F.S. states that “any hospital that
provides psychiatric treatment to persons under 18 years
of age who have emotional disturbances shall comply
with the procedures pertaining to the rights
of patients prescribed in part I of chapter 394.”
395.1041(6), F.S. governing Rights Of Persons Being
Treated states that “A hospital providing emergency
services and care to a person who is being involuntarily
examined under the provisions of s. 394.463 shall adhere
to the rights of patients specied in part I of chapter 394
and the involuntary examination procedures provided
in s. 394.463, regardless of whether the hospital, or any
part thereof, is designated as a receiving or treatment
facility under part I of chapter 394 and regardless of
whether the person is admitted to the hospital.”
395.1055(5), F.S. governing rules and enforcement
states “e agency shall enforce the provisions of part
I of chapter 394, and rules adopted thereunder, with
respect to the rights, standards of care, and examination
and placement procedures applicable to patients
voluntarily or involuntarily admitted to hospitals
providing psychiatric observation, evaluation, diagnosis,
or treatment.”
Children’s Crisis Stabilization Units
Minors under the age of 14 years cannot be admitted to
a bed in a room or ward with an adult. ey may share
common areas with an adult only when under direct visual
observation by unit sta. Minors who are 14 years of age
and older may be admitted to a bed in a room or ward in
the mental health unit with an adult, if the clinical record
contains documentation by a physician that such placement
is medically indicated or for reasons of safety. is must be
reviewed and documented by the physician on a daily basis.
[Chapter 65E-12.106(22), F.A.C.]
Consent to Psychiatric Treatment
Inpatient Treatment
Each person entering a facility must be asked to give express
and informed consent for admission and treatment. If
the person is a minor, express and informed consent for
admission and treatment must also be requested from
the person’s guardian. Express and informed consent for
admission and treatment of a person under 18 years of age
is required from the person’s guardian, unless the minor is
seeking outpatient crisis intervention services (see below).
[s. 394.459(3)(a), F.S.]
Residential Treatment Centers
All rights, specied in s. 394.459, F.S., must be safeguarded
for minors in residential treatment centers as well as receiving
facilities. Children must be informed of their legal and
civil rights, including the right to legal counsel and all
other requirements of due process. erefore, the Baker

Consent for Minors
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix D - 4
D
Act describes the rights of children in residential treatment
centers. [Chapter 65E-10.021(3(e), F.A.C]
Outpatient Crisis Intervention Services
e disability of nonage is removed for any minor age
13 years or older to access services under the following
circumstances (s. 394.4784, F.S.):
Outpatient Diagnostic and Evaluation Services
When any minor age 13 years or older experiences an
emotional crisis to such degree that he or she perceives
the need for professional assistance, he or she shall have
the right to request, consent to, and receive mental health
diagnostic and evaluative services provided by a licensed
mental health professional, as dened by Florida Statutes,
or in a mental health facility licensed by the state. e
purpose of such services shall be to determine the severity
of the problem and the potential for harm to the person
or others if further professional services are not provided.
Outpatient diagnostic and evaluative services shall not
include medication and other somatic methods, aversive
stimuli, or substantial deprivation. Such services shall not
exceed two visits during any 1-week period in response
to a crisis situation before parental consent is required for
further services, and may include parental participation
when determined to be appropriate by the mental health
professional or facility.
Outpatient Crisis Intervention, erapy and
Counseling Services
When any minor age 13 years or older experiences an
emotional crisis to such degree that he or she perceives the
need for professional assistance, he or she shall have the
right to request, consent to, and receive outpatient crisis
intervention services including individual psychotherapy,
group therapy, counseling, or other forms of verbal
therapy provided by a licensed mental health professional,
as dened by Florida Statutes, or in a mental health
facility licensed by the state. Such services shall not
include medication and other somatic treatments, aversive
stimuli, or substantial deprivation. Such services shall not
exceed two visits during any 1-week period in response
to a crisis situation before parental consent is required for
further services, and may include parental participation
when determined to be appropriate by the mental health
professional or facility.
Liability for Payment
e parent, parents, or legal guardian of a minor shall
not be liable for payment for any such outpatient
diagnostic and evaluation services or outpatient therapy
and counseling services, as provided in this section, unless
such parent, parents, or legal guardian participates in the
outpatient diagnostic and evaluation services or outpatient
therapy and counseling services and then only for the
services rendered with such participation.
Provision of Services
No licensed mental health professional shall be obligated
to provide services to minors accorded the right to receive
services under this section. Provision of such services shall
be on a voluntary basis.
Substance Abuse (Marchman Act)
Admission and Treatment
e disability of minority for persons under 18 years of age
is removed solely for the purpose of obtaining voluntary
substance abuse impairment services from a licensed service
provider, and consent to such services by a minor has the
same force and eect as if executed by an individual who has
reached the age of majority. Such consent is not subject to
later disarmance based on minority. [s. 397.601(4)(a), F.S.]
Criteria
A minor may be taken to a detox facility, hospital or an
addictions receiving facility (ARF) for involuntary admission
if there is a good faith reason to believe the minor suers
from a condition involving the use of alcoholic beverages
or any psychoactive or mood-altering substance in such a
manner as to induce mental, emotional, or physical problems
and cause socially dysfunctional behavior, and who, because
of such condition [s. 397.311(14) and s. 397.675, F.S.]:
1. Has lost the power of self-control with respect to
substance use; and either:
2. Inicted, or threatened or attempted to inict, or unless
admitted is likely to inict, physical harm on himself or
herself or another; or
3. Is in need of substance abuse services and, by reason
of substance abuse impairment, his or her judgment
has been so impaired that the person is incapable of
appreciating his or her need for such services and of
making a rational decision in regard thereto; however,
mere refusal to receive such services does not constitute
evidence of lack of judgment with respect to his or her
need for such services.
Initiation
Protective custody may be initiated through law enforcement
[s. 397.677, F.S.]. A parent/guardian may apply for a minor’s
emergency admission if a physician’s certicate has been

Appendix D - 5 Consent for Minors
Appendix D
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
D
obtained [397.6791(2) F.S.], as well as for admission to a
Juvenile Addiction Receiving Facility [397.6798, F.S.]. A
parent/guardian or a licensed service provider can also petition
the court for an involuntary assessment and stabilization order.
[(397.6811, F.S.]
Disposition
Release of the minor from protective custody, emergency
admission, involuntary assessment, involuntary treatment, and
alternative involuntary assessment of a minor, upon approval
of a qualied professional in a hospital, a detoxication facility,
addictions receiving facility, or any less restrictive treatment
component must be to the minor’s parent, legal guardian, or
legal custodian or the authorized designee thereof or to the
department. [s. 397.6758, F.S.]
Parental Participation in Treatment
A parent, legal guardian, or legal custodian who seeks
involuntary admission of a minor is required to participate
in all aspects of treatment as determined appropriate by the
director of the licensed service provider. [397.6759, F.S.]
Release of Information
Since a minor acting alone has the legal capacity to voluntarily
apply for and obtain substance abuse treatment, any written
consent for disclosure may be given only by the minor. is
restriction includes, but is not limited to, any disclosure of
identifying information to the parent, legal guardian, or
custodian of a minor for the purpose of obtaining nancial
reimbursement. When the consent of a parent, legal guardian,
or custodian is required under this chapter in order for a minor
to obtain substance abuse treatment, any written consent for
disclosure must be given by both the minor and the parent,
legal guardian, or custodian. [ss. 397.501(7)(e) 1 and 2, F.S.]
Parental Participation/Payment
A parent or legal guardian of a minor is required to contribute
toward the cost of substance abuse services in accordance with
his ability to pay, unless otherwise provided by law. e parent,
legal guardian or legal custodian of a minor is not liable for
payment for any voluntary substance abuse services provided
to the minor without parental consent, unless the parent,
legal guardian, or legal custodian participates or is ordered to
participate in the services, and only for the substance abuse
services rendered. If the minor is receiving services as a juvenile
oender, the obligation to pay is governed by the law relating to
juvenile oenders. [s. 397.431(2)(3), F.S.]
See Appendix N for more information on Florida’s Marchman Act.
Consent for General
Medical Care & Treatment
Power to Consent
Persons who have the power to consent for a minor’s medical
care and treatment includes a natural or adoptive parent, legal
custodian, or legal guardian.
ere must be maintained in treatment provider’s records
of the minor documentation that a reasonable attempt was
made to contact the person who has the power to consent.
Any of the following persons, in order of priority listed, may
consent to the “medical care or treatment” of a minor who is
not committed to the Department of Children and Families
or the Department of Juvenile Justice when, after a reasonable
attempt, a person who has the power to consent as otherwise
provided by law cannot be contacted by the treatment
provider and actual notice to the contrary has not been given
to the provider by that person [ss. 743.0645(1) and (2), F.S.]:
1. A person who possesses a power of attorney to provide
medical consent for the minor
2. e stepparent
3. e grandparent
4. An adult brother or sister
5. An adult aunt or uncle
“Medical care or treatment” includes ordinary and necessary
medical and dental examinations and treatment, but does not
include surgery, general anesthesia, provision of psychotropic
medication or other extraordinary procedures for which a
separate court order, power of attorney, or informed consent
as provided by law is required. [743.0645(1)(b), F.S.]
Emergency Care
e absence of parental consent notwithstanding, a physician
licensed under chapter 458 or an osteopathic physician
licensed under chapter 459 may render emergency medical
care or treatment to any minor who has been injured in an
accident or who is suering from an acute illness, disease, or
condition if, within a reasonable degree of medical certainty,
delay in initiation or provision of emergency medical care or
treatment would endanger the health or physical wellbeing
of the minor, and provided such emergency medical care
or treatment is administered in a hospital licensed by the
state under chapter 395 or in a college health service.
Emergency medical care or treatment may also be rendered
in the prehospital setting by paramedics, emergency medical
technicians, and other emergency medical services personnel,

Consent for Minors
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
D
provided such care is rendered consistent with the provisions
of chapter 401.
is section applies only when parental consent cannot be
immediately obtained for one of the following reasons [ss.
743.064(1) and (2), F.S.]:
e minor’s condition has rendered him or her unable
to reveal the identity of his or her parents, guardian, or
legal custodian, and such information is unknown to any
person who accompanied the minor to the hospital.
e parents, guardian, or legal custodian cannot be
immediately located by telephone at their place of
residence or business.
Notication shall be accomplished as soon as possible
after the emergency medical care or treatment is
administered.
e hospital records shall reect the reason such consent was not
initially obtained and shall contain a statement by the attending
physician that immediate emergency medical care or treatment
was necessary for the patient’s health or physical wellbeing.
e hospital records shall be open for inspection by the person
legally responsible for the minor. [s. 743.064(3), F.S.]
Emergency Care of Youth in DCF or DJJ Custody
e Department of Children and Family Services or
the Department of Juvenile Justice caseworker, juvenile
probation ocer, or person primarily responsible for the case
management of the child, the administrator of any facility
licensed by the department under s. 393.067,
s. 394.875, or s. 409.175, or the administrator of any
state-operated or state-contracted delinquency residential
treatment facility may consent to the medical care or
treatment of any minor committed to it or in its custody
under chapter 39, chapter 984, or chapter 985, when the
person who has the power to consent as otherwise provided
by law cannot be contacted and such person has not expressly
objected to such consent. ere shall be maintained in
the records of the minor documentation that a reasonable
attempt was made to contact the person who has the power
to consent as otherwise provided by law. [s.743.0645(3), F.S.]
e medical provider shall notify the parent or other person
who has the power to consent as otherwise provided by law
as soon as possible after the medical care or treatment is
administered pursuant to consent given under this section.
e medical records shall reect the reason consent as
otherwise provided by law was not initially obtained and
shall be open for inspection by the parent or other person
who has the power to consent as otherwise provided by law.
[s.743.0645(4), F.S.]
e person who gives consent; a physician, dentist, nurse,
or other health care professional licensed to practice in this
state; or a hospital or medical facility, including, but not
limited to, county health departments, shall not incur civil
liability by reason of the giving of consent, examination,
or rendering of treatment, provided that such consent,
examination, or treatment was given or rendered as a
reasonable prudent person or similar health care professional
would give or render it under the same or similar
circumstances. [s.743.0645(5), F.S.]
Delinquent Youth
(Chapter 985, F.S.)
Medical, psychiatric, psychological, substance
abuse, and educational examination and
treatment
After a detention petition or a petition for delinquency
has been led, the court may order the child named in the
petition to be examined by a physician. e court may
also order the child to be evaluated by a psychiatrist or a
psychologist. If it is necessary to place a child in a residential
facility for such evaluation, the criteria and procedures
established in chapter 393, chapter 394, or chapter 397,
whichever is applicable, shall be used. [s.985.18(1), F.S.]
Whenever a child has been found to have committed a
delinquent act, or before such nding with the consent of
any parent or legal custodian of the child, the court may
order the child to be treated by a physician. e court may
also order the child to receive mental health, substance
abuse services for intellectual disabilities from a psychiatrist,
psychologist, or other appropriate service provider. If it is
necessary to place the child in a residential facility for such
services, the procedures and criteria established in chapter
393, chapter 394, or chapter 397, whichever is applicable,
shall be used. [s.985.18(2), F.S.]
A physician shall be immediately notied by the person
taking the child into custody or the person having custody if
there are indications of physical injury or illness, or the child
shall be taken to the nearest available hospital for emergency
care. A child may be provided mental health, substance
abuse, or intellectual disabilities services, in emergency
situations, pursuant to chapter 393, chapter 394, or chapter
397, whichever is applicable. After a hearing, the court may
order the custodial parent or parents, guardian, or other
custodian, if found able to do so, to reimburse the county or
state for the expense involved in such emergency treatment
or care. [s.985.18(6), F.S.]
Appendix D - 6

Appendix D - 7 Consent for Minors
Appendix D
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
D
Nothing eliminates the right of the parents or the child to
consent to examination or treatment for the child, except
that consent of a parent shall not be required if the physician
determines there is an injury or illness requiring immediate
treatment and the child consents to such treatment or an
ex parte court order is obtained authorizing treatment.
[985.18(7), F.S.]
Dependent Youth
(Chapter 39, F.S.) (Chapter 65C-35, F.A.C.)
Medical, psychiatric, and psychological
examination and treatment of child in DCF Custody
Parents or legal guardians retain the right to consent to or
decline the administration of psychotropic medications for
children taken into state care until such time as their parental
rights, or court ordered guardianship or custodial rights, have
been terminated.
If the parents’ or guardians’ legal rights have been terminated;
their identity or location is unknown; or they decline to
approve administration of psychotropic medications, and
any party believes that administration of the medication is
in the best interest of the child and medically necessary, then
authorization to treat with psychotropic medication must be
pursued through a court order via Children’s Legal Services.
In no case may the dependency case manager, child
protective investigator, the child’s caregiver, representatives
from DJJ, or sta from residential treatment centers
provide express and informed consent for a child in out-of-
home care to be prescribed a psychotropic medication.
When any child is removed from the home and maintained
in an out-of-home placement, the department is authorized
to have a medical screening performed on the child without
authorization from the court and without consent from a
parent or legal custodian. Such medical screening shall be
performed by a licensed health care professional and shall be
to examine the child for injury, illness, and communicable
diseases and to determine the need for immunization.
e department shall by rule establish the invasiveness of
the medical procedures authorized to be performed under
this subsection. In no case does this subsection authorize
the department to consent to medical treatment for such
children. [s.39.407(1), F.S.]
When DCF has performed the medical screening or
when it is otherwise determined by a licensed health
care professional that a child who is in an out-of-
home placement, but who has not been committed
to the department, is in need of medical treatment,
including the need for immunization, consent for
medical treatment shall be obtained from a parent or
legal custodian of the child, or a court order for such
treatment shall be obtained (2).
If a parent or legal custodian of the child is unavailable
and his or her whereabouts can’t be reasonably
ascertained, and it is after normal working hours so
that a court order cannot reasonably be obtained, an
authorized agent of the department has the authority to
consent to necessary medical treatment, for the child.
DCF authority to consent to medical treatment in this
circumstance is limited to the time reasonably necessary
to obtain court authorization (2)(b).
If a parent or legal custodian of the child is available but
refuses to consent to the necessary treatment, a court
order is required unless the situation meets the denition
of an emergency in s. 743.064 or the treatment
needed is related to suspected abuse, abandonment,
or neglect of the child by a parent, caregiver, or legal
custodian. In such case, DCF can consent to necessary
medical treatment. is authority is limited to the time
reasonably necessary to obtain court authorization (2)(c).
Psychotropic Medications
(Chapter 65C-35, F.A.C.)
Before DCF provides psychotropic medications to a child in
its custody, the prescribing physician must attempt to obtain
express and informed consent from the child’s parent or legal
guardian. DCF must take steps necessary to facilitate the
inclusion of the parent in the child’s consultation with the
physician. However, if the parental rights of the parent have
been terminated, the parent’s location or identity is unknown
or cannot reasonably be ascertained, or the parent declines
to give express and informed consent, the department may,
after consultation with the prescribing physician, seek court
authorization to provide the psychotropic medications to
the child. Unless parental rights have been terminated and
if it is possible to do so, the department shall continue to
involve the parent in the decision-making process regarding
the provision of psychotropic medications. If, at any time,
a parent whose parental rights have not been terminated
provides express and informed consent to the provision of
a psychotropic medication, the requirements of this section
that DCF seek court authorization do not apply to that
medication until such time as the parent no longer consents.
Any time DCF seeks a medical evaluation to determine
the need to initiate or continue a psychotropic
medication for a child, DCF must provide to the
evaluating physician all pertinent medical information

Consent for Minors
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix D - 8
known to the department concerning that child.
If a child who is removed from the home under s.
39.401 is receiving prescribed psychotropic medication
at the time of removal and parental authorization
to continue providing the medication cannot be
obtained, the department may take possession of the
remaining medication and may continue to provide the
medication as prescribed until the shelter hearing, if it is
determined that the medication is a current prescription
for that child and the medication is in its original
container.
If DCF continues to provide the psychotropic
medication to a child when parental authorization
cannot be obtained, the department shall notify the
parent or legal guardian as soon as possible that the
medication is being provided to the child. e child’s
ocial departmental record must include the reason
parental authorization was not initially obtained and an
explanation of why the medication is necessary for the
child’s well-being.
If DCF is advised by a licensed physician that the child
should continue the psychotropic medication and
parental authorization has not been obtained, DCF
must request court authorization at the shelter hearing
to continue to provide the psychotropic medication
and must provide to the court any information in its
possession in support of the request. Any authorization
granted at the shelter hearing may extend only until the
arraignment hearing on the petition for adjudication of
dependency or 28 days following the date of removal,
whichever occurs sooner.
Before ling the dependency petition, DCF must
ensure that the child is evaluated by a licensed physician
to determine whether it is appropriate to continue
the psychotropic medication. If, as a result of the
evaluation, DCF seeks court authorization to continue
the psychotropic medication, a motion for such
continued authorization shall be led at the same time
as the dependency petition, within 21 days after the
shelter hearing.
DCF must le a motion seeking the court’s authorization
to initially provide or continue to provide psychotropic
medication to a child in its legal custody. e motion
must be supported by a written report prepared by the
department which describes the eorts made to enable
the prescribing physician to obtain express and informed
consent for providing the medication to the child and other
treatments considered or recommended for the child. In
addition, the motion must be supported by the prescribing
physician’s signed medical report providing:
1. e name of the child, the name and range of the
dosage of the psychotropic medication, and that there
is a need to prescribe psychotropic medication to the
child based upon a diagnosed condition for which such
medication is being prescribed.
2. A statement indicating that the physician has reviewed
all medical information concerning the child which has
been provided.
3. A statement indicating that the psychotropic
medication, at its prescribed dosage, is appropriate for
treating the child’s diagnosed medical condition, as well
as the behaviors and symptoms the medication, at its
prescribed dosage, is expected to address.
4. An explanation of the nature and purpose of the
treatment; the recognized side eects, risks, and
contra indications of the medication; drug-interaction
precautions; the possible eects of stopping the
medication; and how the treatment will be monitored,
followed by a statement indicating that this explanation
was provided to the child if age appropriate and to the
child’s caregiver.
5. Documentation addressing whether the psychotropic
medication will replace or supplement any other
currently prescribed medications or treatments; the
length of time the child is expected to be taking the
medication; and any additional medical, mental health,
behavioral, counseling, or other services that the
prescribing physician recommends.
Chapter 65C-35, F.A.C., ADOPTED on March 17, 2010,
governs Psychotropic Medications for Children in Out of
home Care. Several of the many Denitions included in this
rule include:
Assent means a process by which a provider of medical
services helps the patient achieve a developmentally
appropriate awareness of the nature of his or her
condition; informs the patient of what can be expected
with tests and treatment; makes a clinical assessment
of the patient’s understanding of the situation and the
factors inuencing how he or she is responding; and
solicits an expression of the patient’s willingness to accept
the proposed care.
Express and Informed Consent means voluntary
written consent from a competent person who has
received full, accurate, and sucient information
and explanation about a child’s medical condition,
medication and treatment to enable the person to make
a knowledgeable decision without being subjected to
D

Appendix D - 9 Consent for Minors
Appendix D
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
any deceit or coercion. Express and informed consent
for the administration of psychotropic medications may
only be given by a parent whose rights have not been
terminated, or a legal guardian of the child. Sucient
explanation includes but is not limited to the following
information, provided and explained in plain language
by the prescribing physician to the consent giver: the
medication, reason for prescribing it, and its purpose
or intended result; side eects,, risks, and contra
indications, including eects of stopping the medication;
method for administering the medication, and dosage
range when applicable; potential drug interactions;
alternative treatments; and the behavioral health or other
services used to complement the use of medication,
when applicable.
Legal guardian means a permanent guardian as described
in Section 39.6221, F.S., or a “guardian” as dened in
Section 744.102, F.S., or a relative with a court order of
temporary custody under Chapter 751, F.S. Dependency
case managers and Guardians ad Litem do not meet the
denition of legal guardian.
Medical report means a report prepared by the prescribing
physician that includes information required by Section
39.407(3)(c), F.S. e form for the medical report is
“Medical Report” (form CF-FSP 5339 dated January
2010) which is hereby incorporated by reference and
is available by contacting the Family Safety Program
Oce at 1317 Winewood Boulevard, Tallahassee, Florida
32399-0700, or at http://www.dcf.state..us/DCFForms/
Search/DCFFormSearch.aspx.
Psychotropic medications means, for the purpose of this
rule, any chemical substance prescribed with the intent
to treat psychiatric disorders; and those substances, which
though prescribed with the intent to treat other medical
conditions, have the eect of altering brain chemistry
or involve any of the medications in the categories listed
below. e medications include, without limitation, the
following major categories:
Antipsychotics
Antidepressants
Sedative Hypnotics
Lithium
Stimulants
Non-stimulant Attention Decit Hyperactivity
Disorder medications
Anti-dementia medications and cognition enhancers
Anticonvulsants and alpha-2 agonists
Any other medication used to stabilize or improve
mood, mental status, behavior, or mental illness
Psychotropic medications may be administered in
advance of a court order or parental authorization under
two circumstances including:
If the prescribing physician certies in writing on
the Medical Report form that delay in providing
the prescribed psychotropic medication would more
likely than not cause signicant harm to the child, or
In hospitals, crisis stabilization units, and in
psychiatric Residential Treatment programs.
In the above two circumstances, the dependency case
manager or child protective investigator must assist the
prescribing physician in obtaining express and informed
consent and must take steps to include the parent or legal
guardian in the child’s consultation with the prescribing
physician. If express and informed consent hasn’t been
obtained, the dependency case manager or child protective
investigator must obtain a completed/signed copy of the
Medical Report and provide it to Children’s Legal Services in
time for a motion to be led within 3 business days after the
medication is begun.
Examination, Treatment, & Placement
A judge may order a child in an out-of-home placement
to be examined by a licensed health care professional.
e judge may also order such child to be evaluated by
a psychiatrist or a psychologist or, if a developmental
disability is suspected or alleged, by the developmental
disability diagnostic and evaluation team of the
department. If it is necessary to place a child in a
residential facility for such evaluation, the criteria and
procedure established in s. 394.463(2) or chapter 393
shall be used, whichever is applicable. [s. 39.407 (4), F.S.]
A judge may order a child in an out-of-home placement
to be treated by a licensed health care professional based
on evidence that the child should receive treatment.
e judge may also order such child to receive mental
health or developmental disabilities services from a
psychiatrist, psychologist, or other appropriate service
provider. If it is necessary to place the child in a
residential facility for such services, the procedures and
criteria established in s. 394.467 shall be used. A child
may be provided mental health services in emergency
situations, pursuant to the procedures and criteria
contained in s. 394.463(1). [s. 39.407(5), F.S.]
Children who are in the legal custody of the department
D

Consent for Minors
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix D - 10
may be placed by DCF, without prior approval of the
court, in a residential treatment center licensed under
s. 394.875 or a hospital licensed under chapter 395 for
residential mental health treatment or may be placed
by the court in accordance with an order of involuntary
examination or involuntary placement entered pursuant
to s. 394.463 or s. 394.467. All children placed in a
residential treatment program under this subsection must
have a guardian ad litem appointed. [s.39.407 (6), F.S.]
D
A specialized on-line Baker Act course for persons dealing with
minors can be found at www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix E - 1 Chapter 400 and 429 Facilities
Appendix E
E
Baker Act and Long-Term Care Facilities
Licensed Under Chapter 400 and 429
Introduction
e 1996 legislative reform of the Baker Act has had a
signicant impact on long-term care facilities and programs
licensed by the Agency for Health Care Administration
under the authority of Chapter 400/429, F.S. such as nursing
homes, assisted living facilities, adult day care centers,
and adult family care homes. Failure to follow the criteria
and procedures provided under the Baker Act relating to
the transportation, voluntary admission, and involuntary
examination of a resident by a facility or its employee
are grounds for action by the Agency for Health Care
Administration against a licensed long-term care facility or
program.
Before referring any resident or client to a Baker Act receiving
facility on a voluntary or involuntary basis, the sta of the
long-term care facility must make every eort to provide
appropriate psychiatric interventions to avoid such referrals.
However, if all appropriate on-site interventions prove
ineective and are fully documented in a resident’s record,
a referral to a Baker Act receiving facility may be necessary.
In such cases, the resident may be sent for either a voluntary
admission or for an involuntary examination, following the
provisions in the Baker Act. A person may not be sent for
“assessment” at a Baker Act receiving facility, without rst
making the on-site determination through legal means of
either voluntary or involuntary status. Referral of the resident
to an emergency room or other site for this psychiatric
assessment is contrary to the law.
e role of a Baker Act receiving facility is to provide
psychiatric evaluations and short-term psychiatric treatment
for persons in acute mental health emergencies. If the resident
requires something dierent than psychiatric examination or
short-term psychiatric treatment, he/she should not be sent
to a receiving facility simply because of behavioral problems
or to evade federal and state discharge/transfer requirements.
Instead, the resident should be directly transferred to a more
appropriate type of facility.
Voluntary Admissions
s. 394.4625, F.S. Chapter 65E-5.270, F.A.C.
A person may go to a Baker Act receiving facility for
voluntary psychiatric examination from a facility licensed
under Chapter 400/429, F.S. only if the person is:
Over the age of 18,
Has a mental illness, as dened in the statute,
Competent to provide express and informed consent to
his or her own treatment, and
Suitable for treatment.
Express and informed consent requires that a person on
voluntary status be competent to make well-reasoned, willful,
and knowing decisions concerning his or her medical or
mental health treatment.
Consent must be voluntarily given in writing after sucient
explanation of the need for admission so that the person can
make a knowing and willful decision without any element of
force or deceit.
If residents cannot meet these criteria, they cannot be on
voluntary status in a Baker Act receiving facility, and instead,
must be handled under the involuntary provisions of the law
if they meet the involuntary criteria.
e Baker Act specically states that the following persons
cannot be sent on a voluntary basis to a receiving facility
until after an initial assessment of the resident’s ability to give
express and informed consent is conducted at the sending
facility by an authorized independent professional. ese
residents include:
1. A person 60 years of age or older for whom an emergency
transfer is being sought from a nursing home pursuant to
s. 400.0255, F.S.
2. A person 60 years of age or older with a diagnosis of
dementia for whom transfer is being sought from a:
Nursing home,
Assisted-living facility,
Adult day care center, or
A specialized on-line Baker Act course
Adult family care home.
for staff of long-term care facilities can be found at:
3. A person for whom all decisions concerning medical
http://www.bakeracttraining.org
treatment are currently being lawfully made by a health care
surrogate or proxy designated under Chapter 765, F.S.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Chapter 400 and 429 FacilitiesAppendix E - 2
E
e initial assessment, documented on recommended
form CF-MH 3099, can only be performed by one of the
following [see denition of each of the following in
s 394.455(6), (17), and (19), F.S.] as specied by the circuit
oce of the Department of Children and Families:
1. A mental health overlay program,
2. A mobile crisis response team, or
3. A licensed professional who is authorized to initiate an
involuntary examination and is employed by a publicly
funded community mental health center.
If none of the above services exist in the locale, or if the
service cannot respond within two hours of being called,
the facility may contact a licensed professional authorized
to initiate an involuntary examination who is not employed
by or under contract with, and does not have a nancial
interest in, either the facility initiating the transfer or the
Baker Act receiving facility to which the transfer may be
made to conduct and document this assessment.
Involuntary Examinations
s. 394.463, F.S. Chapter 65E-5.280, F.A.C.
A person may be taken to a Baker Act receiving facility for
involuntary examination if there is reason to believe that
he or she has a mental illness, as dened in the law, and
because of his or her mental illness:
e person has refused examination or is unable to
determine whether examination is necessary; and
Without care or treatment, the person is likely to suer
from neglect or refuse to care for himself or herself,
such neglect or refusal poses a real and present threat of
substantial harm to his or her well-being, and it is not
apparent that such harm may be avoided through the help
of willing family members or friends or the provision of
other services; or
ere is a substantial likelihood that without care or
treatment the person will cause serious bodily harm to
himself or others in the near future, as evidenced by recent
behavior.
ere are only three methods to initiate an involuntary
examination. ey are:
1. A physician, clinical psychologist, psychiatric nurse,
clinical social worker, licensed mental health
counselor or licensed marriage and family therapist.
(See denitions in Baker Act) may execute a certicate
stating that he or she has examined a person within the
preceding 48 hours and nds that the person appears
to meet the criteria for involuntary examination and
stating the professional’s observations upon which that
conclusion is based. ese observations and conclusions
should be those of the professional signing the certicate,
rather than those of persons who are not legally authorized
to initiate the involuntary examination. e professional
should complete the form entitled “Certicate of
Professional Initiating Involuntary Examination” (CF-
MH 3052b). e professional’s observations should focus
on the resident’s overt behavior supporting the ndings
rather than just a diagnosis and specically relate to the
statutory criteria for involuntary examination.
2. If no legally authorized mental health professional is
available to personally conduct an examination and
complete the professional’s certicate, a court may issue
an Ex Parte Order for Involuntary Examination of the
resident. To obtain such an order, one or more persons
including facility sta, guardian or family members who
have personally observed the resident’s behavior must go
the oce of the Clerk of the Circuit Court (usually the
Probate Division) at the Courthouse to le a petition(s).
e petition must contain a sworn statement of the facts
and circumstances that the petitioner(s) believe justify
an involuntary examination of the person. e petition
must be signed under oath by those who have personal
knowledge of the person’s behavior.
3. In an emergency, law enforcement may be called to
complete the “Report of a Law Enforcement Ocer
Initiating an Involuntary Examination,” (CF-MH 3052a).
Transportation
s. 394.462, F.S. Chapter 65E-5.260, F.A.C.
Regardless of which of these three methods is used to initiate
the involuntary examination, law enforcement is responsible
for transporting the person to the nearest receiving facility for
the examination. A law enforcement agency may decline to
transport the person to a receiving facility only if:
1. e county has contracted for transportation, at the
sole cost to the county, and the law enforcement ocer
and medical transport service agree that the continued
presence of law enforcement personnel is not necessary for
the safety of the person or others.
2. In cases where the ocer requests assistance from
emergency medical personnel for the safety of the ocer
or the person in custody or the ocer believes the person
has an emergency medical condition.
3. When a transportation exception plan has been approved
by the Board of County Commissioners and the Secretary
of the Department of Children and Families.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix E - 3 Chapter 400 and 429 Facilities
Appendix E
E
e law enforcement ocer must complete the form
entitled “Transportation to Receiving Facility,” (CF-MH
3100) describing the circumstances under which the person
was taken into custody.
e Baker Act forbids the removal of a person from any
program or residential placement licensed under Chapter
400/429, F.S. and transport to a receiving facility for
involuntary examination unless a Professional’s Certicate,
a court’s Ex Parte Order, or a Law Enforcement Ocer’s
Report is rst prepared. If the client’s condition is such that
preparation of a Law Enforcement Ocer’s Report is not
practical before removal, the Report must be completed as
soon as possible after removal, but in any case before the
person is transported to a Baker Act receiving facility. If
the sending facility fails to properly initiate an involuntary
examination, the Baker Act receiving facility must report
such failure to the Agency for Health Care Administration
by certied mail on the next working day.
Florida Health Care Association
Recommendations
e Florida Health Care Association has developed through
its Quality First Credentialing Program a Best Practice
Tool for Behavior Management, Aggression Control, and
Baker Act Guidelines. is tool was developed to provide
guidelines for redirecting a resident who exhibits aggressive
behavior that may present as a risk to self or others. e tool
recommends:
1. Attempt to identify triggers for the adverse behavior such as:
Being touched
Noise
Yelling
Contact with person that is unfamiliar or upsetting
Restraint
Isolation
Perception of threat
2. rough the facility assessment and care planning process
attempt to identify triggers as well as calming strategies.
Integrate them, as appropriate, into the resident plan of
care. Suggestions could include:
Identify preferences regarding daily routine and
caregivers as possible: Male, female, language,
ethnicity, culture, of a particular religion, etc.
Music, reading a book or being read to
Wrapping in a blanket
Watching TV or movies of preference
Quiet room, soft lighting
Talk with trusted person/sta
Go for a supervised walk
Outdoor activity, (supervised)
Take a bath or shower, (do not force care)
Massage, imagery, relaxation techniques, aroma
therapy
Drink/snack
Stued animal or comfort article
Artwork
Diversion to preferred activity
Other as noted through assessment
3. Attempt to identify signals of distress as part of the MDS/
RAI/Care plan process and daily systems of care before
behavior accelerates such as: Sweating, crying, breathing
hard, yelling, screaming or resisting care, accelerated
pacing, injuring self, clenching teeth, running, clenching
sts, swearing, not eating, potential self neglect, threats,
other as noted.
4. If a resident in a nursing home demonstrates aggressive
behavior, (verbal or physical) and a potential for being an
imminent threat to themselves or others, the nursing sta
are to notify the Director of Nursing or designee or the
Unit Manager and/or RN of record for assistance with
further assessment of the situation and the current health
status of the resident.
5. Be certain that the Administrator/designee is aware of the
possibility of an involuntary admission for psychiatric
examination (Baker Act). Keep the primary physician
and responsible party (RP) notied and kept informed
throughout the course of the treatment, and until the
situation has resolved.
6. Notify Social Services for therapeutic intervention, and
direct involvement of the behavioral management plan for
the resident.
7. Provide for the safety of all other facility residents. Provide
1: 1 sta oversight as possible. Enlist the help of sta
that are familiar with the resident, and have successfully
redirected behavior(s) in the past.
8. Gather and re-evaluate behavioral data to include
behavioral ow records and documentation of the
behavior within the clinical record.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Chapter 400 and 429 FacilitiesAppendix E - 4
E
9. Verbally redirect and assist the resident to a quiet area of
the facility that is free from all stimuli, and is away from
other residents. Time outs are utilized for behaviors,
which place others in potential danger due to the negative
behavior of the resident. As such, these are specic timed
activities, followed with appropriate praise for compliance.
10. Review/revise the current plan of care as indicated. Notify
the RP, and if they are available, suggest their assistance in
calming the resident. Oer comfort measures that might
include: toileting, oering food and uids, providing
warmth, repositioning, rest, music, reminiscence therapy,
aroma therapy, supervised activity outdoors in a safe
secure area, or known diversions that may have worked
with the resident in the past. Document the eectiveness
of all interventions.
11. Interact with the resident in a calm, non-threatening way.
Assure the resident has the use of adaptive devices such as
hearing aids and/or glasses so that communication eorts
are maximized.
12. Be kind and direct when addressing the resident. Do not
force care. If the resident escalates, do not proceed. Back
away and notify the nurse immediately.
13. Review the resident history and diagnoses. Identify
medical conditions, disabilities, and related medical
problems. Review the record for identication of recent
falls, lab work, or tests that will be helpful information for
the assessment.
14. Assess for signs and symptoms of an acute onset of
infection. Monitor vital signs every shift or as warranted
by nursing assessment. Do not proceed if the resident
is resistant. Notify the physician if attempts to monitor
clinical symptoms are unsuccessful due to resident’s
behavior/resistance.
15. Assess for signs of acute pain. Notify the physician as
warranted for tests, treatments, or alterations to the
current pain management plan. Medicate for pain as
indicated after checking to be certain there are no drug
allergies. Document the eectiveness of the intervention.
16. Review the medication prole. Check for recent
medication changes, e.g. omission, additions, or dosing
adjustments. If time allows, request that the Pharmacist
provide a review of the medication plan as warranted.
17. Medicate the resident with a sedative if required, as
ordered by the physician. Document the reasons for the
medication, frequency and method of administration,
and monitor for any side eects or contraindications that
may exist. Be sure that the legally authorized substitute
decision maker has been notied.
18. Discuss with the physician the possibility of lab work
to rule out physiological causes. Consider asking for a
chemical prole, CBC, UA, yroid prole, and pertinent
medication levels e.g. Digoxin, Dilantin, etc. If labs are
ordered, request a STAT report to the facility as warranted
per resident assessment.
19. Keep the physician/RP notied of the status of the
resident and the need for further interventions/orders.
20. Inform the physician and RP, (responsible party), that
the goal of the facility is to keep the resident within their
known home environment as long as it remains a medically
safe option for the resident, sta, and other residents.
21. e primary role of a Baker Act receiving facility is to
perform psychiatric evaluations and provide short term
psychiatric treatment. If a person has behavioral conditions
that may have resulted from non-psychiatric conditions, the
person should not be sent to a psychiatric facility.
22. Residents cannot be sent out for psychiatric examinations
unless the voluntary or involuntary provisions of the
Baker Act are followed. Residents should never be sent
out to ER’s for “altered mental status” if sta believes the
person’s symptoms are related to a mental illness.
23. If the above noted interventions are not successful,
notify the primary physician and implement one of the
following options:
As authorized by s394.463(2)(a)3, F.S., the physician
may elect to personally evaluate the resident on site
to determine if the resident meets the criteria for
involuntary examination, and will complete the form
CF-MH3052b.
As authorized by s394.463(2)(a)3, F.S., the physician
may elect to have the involuntary examination
(Baker Act), coordinated through the services of a
clinical psychologist, licensed clinical social worker
or licensed psychiatric nurse. e requirements
specify that the clinical social worker be licensed, or
psychiatric nurse have a Masters or doctorate degree
in psychiatric nursing with two years experience
under the supervision of a physician, as dened in
the Baker Act. A licensed mental health counselor
and licensed marriage and family therapist are also
authorized by law to initiate an involuntary Baker Act
examination. In any case, the licensed professional
initiating the examination must base the conclusion
that the person meets criteria on his/her own
evaluation and observations.
A person may not be removed from any program or
residential placement under Chapter 400/429, FS,
and transported for involuntary examination unless
an ex parte order (CF-MH 3001), a law enforcement
ocer’s report, (CF-MH 3052a), or a Professional’s
Certicate, (CF-MH 3052b) is rst prepared.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix E - 5 Chapter 400 and 429 Facilities
Appendix E
E
In an emergency situation the police may be called for
Document your actions in the resident record.
on-site evaluation, but a law enforcement ocer should
e facility is responsible for assuring that
not be expected to initiate an involuntary examination
appropriate notice of transfer is issued at the time of
in a nursing home except in cases of imminent
transfer.
danger. Instead, the facility’s physician, or other legally
It is expected that the resident will be accepted back
authorized professionals as noted above should be called
to the facility after the provision of examination and
to initiate the examination.
treatment at a receiving facility. e facility should
A police ocer must be notied for coordination of
re-evaluate the resident prior to making a
transport to the receiving facility. e ocer must
determination that it is no longer able to meet
execute a written report detailing the circumstances
the individual needs of the resident.
under which the person is taken into custody (CF-MH
3100). e report and a copy of the certicate should
Nursing Homes
be copied and made to be part of the resident’s clinical
Psychotropic Medication Usage Issues
record.
e use of psychotropic medications in nursing homes,
Law enforcement transportation is required for any
particularly anti-psychotic medications, is under close review
person for whom an involuntary examination has
due to potential adverse eects.
been initiated, whether by the court, mental health
professional, or law enforcement ocer. e ocer can
Nursing home sta and related medical personnel must
make the determination to consign a person to medical
follow the federal regulations governing use of psychotropic
transportation at any time that the ocer determines
medications to protect the health and safety of residents
that emergency medical personnel are needed or for the
e following are some, but not all, of the federal regulations
safety of the ocer or others. is consignment can take
governing this issue:
place once the ocer and EMS have agreed that the
continued presence of law enforcement personnel is not
Federal Regulation FO329, FO320, FO425, and
necessary for the safety of the person or others. In this
FO428 regulate anti psychotic medications.
case, the decision needs to be reected within the clinical
Federal Regulation FO386 governs physicians’ active
record.
role including medication regime (see also FO425 and
A law enforcement ocer may decline to transport a
FO428).
resident if the county has contracted for transportation
Federal Regulation FO319 regulates assessment and
at the sole cost to the county and the law enforcement
adjustment.
ocer and medical transport service agree that the
Federal Regulation FO425 requires routine
continued presence of law enforcement personnel is not
and emergency drugs and biological and other
expected to be necessary for the safety of the person to
pharmaceutical services including accurate acquiring,
be transported or others. e statute requires that the
receiving, dispensing, and administering of all drugs to
law enforcement ocer report to the scene, assess the
meet the needs of residents.
risk circumstances, and if appropriate, to “consign” the
person to the care of the transport company.
All facility and medical sta should refer to the most current
regulations for appropriate use of medications in a nursing
If law ocers refuse to respond to a facility’s request
home setting.
for transporting a resident for whom an involuntary
examination has been initiated, it is recommended
that the facility administrator contact the supervisor
of the ocer refusing to transport. If that fails, it is
A specialized on-line Baker Act course for long-term care
recommended that the facility ask to speak to the
facility personnel can be found at
attorney for the law enforcement agency. If that
http://www.bakeracttraining.org.
intervention fails, contact the local DCF mental health
***
program oce and/or the local AHCA eld oce.
For further assistance visit: http://www.dcf.state.fl.us/
If it is at night or on a weekend, and none of the above is
available and the need for transport is urgent, the facility
programs/samh/MentalHealth/laws/index.shtml to
should seek EMS assistance to transport the resident to
view DCF’s most Frequently Asked Questions list.
the nearest receiving facility. On the next working day,
contact DCF and AHCA to seek long-term resolution.
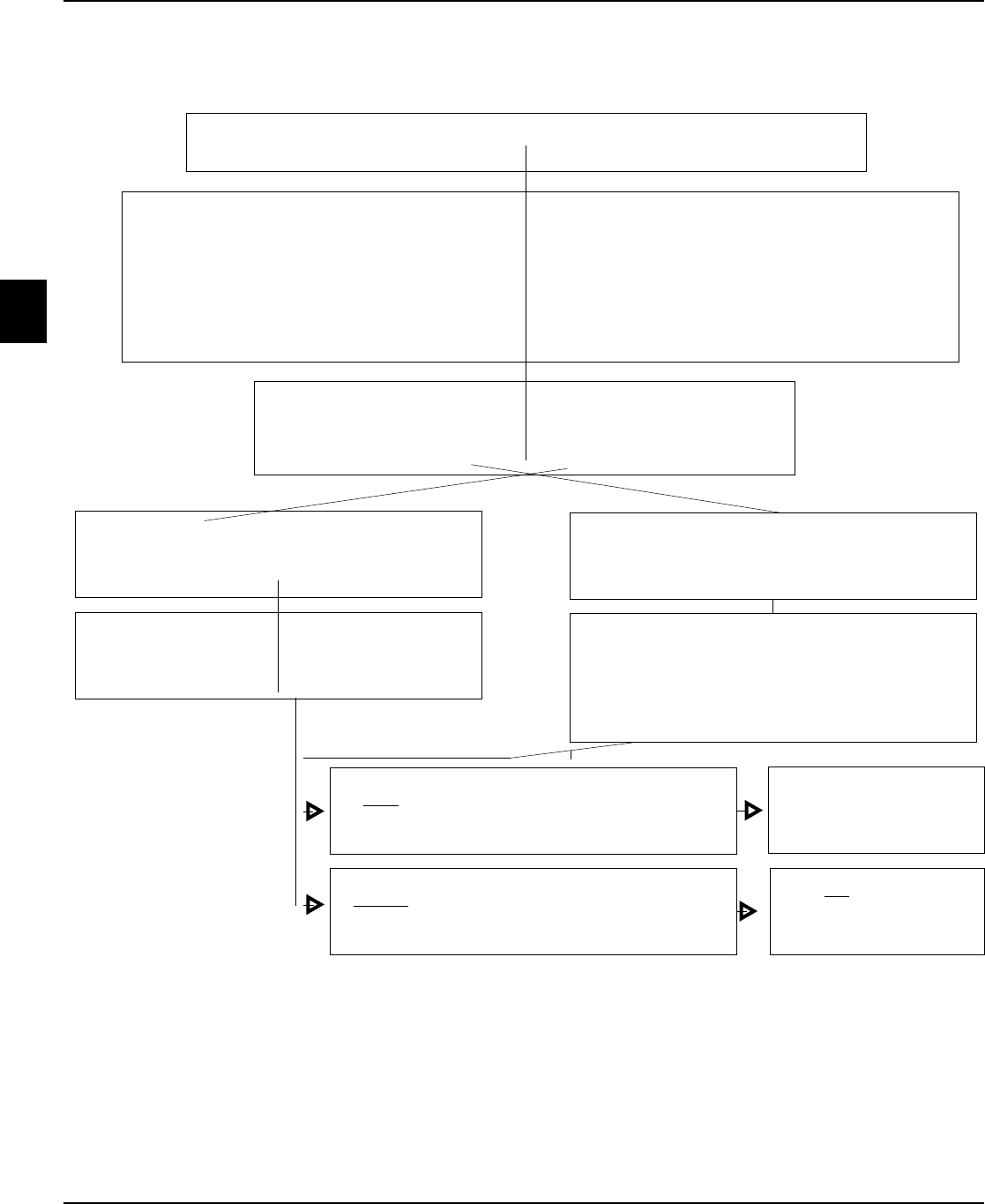
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Chapter 400 and 429 Facilities
Appendix E - 6
E
Person Seeking Voluntary Admission
(from a facility licensed under Chapter 400/429, F.S.)
All possible interventions have been tried, documented, and found to be ineffective (See
model policy and procedures developed by the Florida Health Care Association)
Determined by referring facility to meet voluntary admission criteria:
These extraordinary protections apply to persons:
60 years of age or older for whom an emergency transfer is being sought from a nursing home, or
60 years of age or older with a diagnosis of dementia for whom transfer is being sought from a nursing
home, assisted-living facility, adult day care center, or adult family care home.
For whom all decisions concerning medical treatment are currently being lawfully made by the health
care surrogate or proxy.
Publicly funded service responds within 2 hours
Publicly funded service does not exist or informs
facility it will be unable to respond within 2 hours
Able to give express and informed consent to
treatment
Unable to give express and informed consent to
treatment
May be transported by any
safe method to facility of
patient’s choice
May not be transported
except after involuntary
examination is initiated
Contacts independent authorized licensed
professional to perform assessment of ability to
provide express and informed consent to treatment
who is not employed by, under contact with, or has
no financial interest in the sending or receiving facility
Assessed by service for ability to provide express
and informed consent to treatment
If the person does not meet the criteria for voluntary admission, see flow chart for "Involuntary Examination" in Appendix F. A
person may not be removed from any program or residential placement licensed under Chapter 400/429, F.S. and transported
to a receiving facility for involuntary examination unless an ex parte order, a professional’s certificate, or a law enforcement
officer’s report is first prepared. A receiving facility admitting a person for involuntary examination who is not accompanied by
such documentation shall notify AHCA of such admission by certified mail no later than the next working day.
q
q
q
q
Notified publicly funded mobile crisis response service, mental health
overlay program or authorized professional employed by Community
Mental Health Center

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix E - 7 Chapter 400 and 429 Facilities
Appendix E
E
Quality First Credentialing Program Best Practices Tools
Title: Behavior Management/Aggression Control /Involuntary Baker Act Guidelines
Latest Revision: 3-27-07 Regulatory: # of Pages: 4
Approved By: Quality First Credentialing Foundation Board/Subcommittee
The Quality First Credentialing Foundation disclaims responsibility for any adverse
effects resulting directly or indirectly from the use of the sample Best Practices Tools
from any undetected errors, And from the reader’s misunderstanding of the text. The
Quality First Credentialing Foundation exerted every effort to ensure that any Tools set
forth in this text were in accord with current regulations, recommendations, and practice
at the time of publication.
MISSION: This protocol is intended to comply with Federal and State statutes.
PURPOSE: To provide guidelines pertaining to the redirection of a resident exhibiting aggressive
behavior that may present as a risk to self or others.
1. Attempt to identify triggers for the adverse behavior such as:
• Being touched
• Noise
• Yelling
• Contact with person that is unfamiliar or
upsetting
• Restraint
• Isolation
• Perception of threat
2. Through the facility assessment and care planning process attempt to identify triggers as well as
calming strategies. Integrate them, as appropriate, into the resident plan of care.
3. Suggestions could include:
• Identify preferences regarding daily
routine and caregivers as possible: Male,
female, language, ethnicity, culture, of a
particular religion, etc.
• Music, reading a book or being read to
• Wrapping in a blanket
• Watching TV or movies of preference
• Quiet room, soft lighting
• Talk with trusted person/sta
• Go for a supervised walk
• Outdoor activity, (supervised)
• Take a bath or shower, (do not force care)
• Massage, imagery, relaxation techniques, aroma
therapy
• Drink/snack
• Quiet room
• Stued animal or comfort article
• Artwork
• Diversion to preferred activity
• Other as noted through assessment
4. Attempt to identify signals of distress as part of the MDS/RAI/Care plan process and daily systems
of care before behavior accelerates such as: Sweating, crying, breathing hard, yelling, screaming or
resisting care, accelerated pacing, injuring self, clenching teeth, running, clenching fists, swearing, not
eating, potential self neglect, threats, other as noted.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Chapter 400 and 429 FacilitiesAppendix E - 8
E
Quality First Credentialing Program Best Practices Tools (continued)
5. If a resident in a nursing home demonstrates aggressive behavior, (verbal or physical) and a potential
for being an imminent threat to themselves or others, the nursing staff are to:
a. Notify the Director of Nurses or designee, the Unit Manager and/or RN of record for assistance
with further assessment of the situation and the current health status of the resident.
b. Be certain that the Administrator/designee is aware of the possibility of an involuntary
admission for psychiatric examination, (Baker Act). Keep the primary physician and RP,
(responsible party) notified and kept informed throughout the course of the treatment, and
until the situation has resolved.
c. Notify Social Services for therapeutic intervention, and direct involvement of the behavioral
management plan for the resident.
d. Provide for the safety of all other facility residents. Provide 1: 1 staff oversight as possible. Enlist
the help of staff that are familiar with the resident, and have successfully redirected behavior(s)
in the past.
e. Gather and re-evaluate behavioral data to include behavioral flow records and documentation
of the behavior within the clinical record.
f. Verbally redirect and assist the resident to a quiet area of the facility that is free from all stimuli,
and is away from other residents. Time outs are utilized for behaviors, which place others in
potential danger due the negative behavior of the resident. As such these are specific timed
activities, followed with appropriate praise for compliance.
g. Review/revise the current plan of care as indicated. Notify the RP, and if they are available,
suggest their assistance in calming the resident. Offer comfort measures that might include:
Toileting, offering food and fluids, providing warmth, repositioning, rest, music, reminiscence
therapy, aroma therapy, supervised activity outdoors in a safe secure area, or known diversions
that may have worked with the resident in the past. Document the effectiveness of all
interventions.
h. Interact with the resident in a calm, non-threatening way. Assure the resident has the use
of adaptive devices such as hearing aides and/or glasses so that communication efforts are
maximized.
i. Be kind and direct when addressing the resident. Do not force care. If the resident accelerates,
do not proceed. Back away and notify the nurse immediately.
j. Review the resident history and diagnoses. Identify medical conditions, disabilities, and related
medical problems. Review the record for identification of recent falls, lab work, or tests that will
be helpful information for the assessment?
k. Assess for signs and symptoms of an acute onset of infection. Monitor vital signs every shift
or as warranted by nursing assessment. Do not proceed if the resident is resistant. Notify the
physician if attempts to monitor clinical symptoms are unsuccessful due to resident’s behavior/
resistance.
l. Assess for signs of acute pain. Notify the physician as warranted for tests, treatments, or
alterations to the current pain management plan. Medicate for pain as indicated after checking
to be certain there are no drug allergies. Document the effectiveness of the intervention.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix E - 9 Chapter 400 and 429 Facilities
Appendix E
E
Quality First Credentialing Program Best Practices Tools (continued)
m. Review the medication profile. Check for recent medication changes, e.g. omission, additions,
or dosing adjustments. If time allows, request that the Pharmacist provide a review of the
medication plan as warranted.
n. Medicate the resident with a sedative if required, as ordered by the physician. Document the
reasons for the medication, frequency and method of administration, and monitor for any side
effects or contraindications that ma exist. Be sure that the legally authorized substitute decision
maker has been notified.
o. Discuss with the physician the possibility of lab work to rule out physiological causes. Consider
asking for a chemical profile, CBC, UA, Thyroid profile, and pertinent medication levels e.g.
Digoxin, Dilantin, etc. If labs are ordered, request a STAT report to the facility as warranted per
resident assessment.
p. Keep the physician/RP notified of the status of the resident and the need for further
interventions/orders.
q. Inform the physician and RP, (responsible party), that the goal of the facility is to keep the
resident within their known home environment as long as it remains a medically safe option for
the resident, staff, and other residents.
r. The primary role of a Baker Act receiving facility is to perform psychiatric evaluations and provide
short term psychiatric treatment. If a person has behavioral conditions that are not psychiatric in
nature they should not be sent to a psychiatric facility.
s. Residents cannot be sent out for psychiatric examinations unless the voluntary or involuntary
provisions of the Baker Act are followed. Residents should never be sent out to ER’s for “altered
mental status.”
t. If the above noted interventions are not successful, notify the primary physician and implement
one of the following options:
i. As authorized by s394.463 (2)(a)3, F.S., the physician may elect to personally evaluate the
resident on site to determine if the resident meets the criteria for involuntary examination,
and will complete the form CF-MH3052b.
ii. As authorized by s394.463 (2)(a)3, F.S., the physician may elect to have the involuntary
examination (Baker Act), coordinated through the services of a clinical Psychologist, clinical
social worker or psychiatric nurse. The requirements specify that the clinical social worker be
licensed, or psychiatric nurse have a Masters degree or doctorate in psychiatric nursing with
two years experience under the supervision of a physician as defined in the Baker Act.
iii. A person may not be removed from any program or residential placement under Chapter
400, FS, and transported for involuntary examination unless an ex parte order (CF-MH 3001),
a law enforcement officer’s report, (CF-MH 3052a), or a Professional’s Certificate, (CF-MH
3052b) is first prepared.
iv. In an emergency situation the police may be called for on site evaluation, but a law
enforcement officer should not be expected to initiate an involuntary examination in a
nursing home except in cases of imminent danger. Instead, the facility’s physician, or other
authorized parties as noted in ii. should be called to initiate the examination.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Chapter 400 and 429 FacilitiesAppendix E - 10
E
Quality First Credentialing Program Best Practices Tools (continued)
v. A police officer must be notified for coordination of transport to the receiving facility. The officer
shall execute a written report detailing the circumstances under which the person is taken into
custody. The report and a copy of the certificate should be copied and made to be part of the
resident’s clinical record.
vi. Law enforcement transportation is required for any person for whom an involuntary examination
has been initiated, whether by the court, mental health professional, or law enforcement officer. The
officer can make the determination to consign a person to medical transportation at any time that
the officer determines that emergency medical personnel are needed or for the safety of the officer
or others. This consignment can take place once the officer and EMS have agreed that the continued
presence of law enforcement personnel is not necessary for the safety of the person or others. In
this case, the decision needs to be reflected within the clinical record.
vii. A law enforcement officer may decline to transport a resident if the county has contracted for
transportation at the sole cost to the county and the law enforcement officer and medical transport
service agree that the continued presence of law enforcement personnel is not expected to be
necessary for the safety of the person to be transported or others. The statute requires that the
law enforcement officer report to the scene, assess the risk circumstances, and if appropriate, to
“consign” the person to the care of the transport company.
viii. If law officers refuse to respond to a facility’s request for transporting a resident for whom an
involuntary examination has been initiated, it is recommended that the facility administrator
contact the supervisor of the office refusing to transport. If that fails it is recommended that the
facility ask to speak to the attorney for the law enforcement agency. If that intervention fails, contact
the local DCF mental health program office and/or the local AHCA field office. If it is at night or on a
weekend, and none of the above is available and the need for transport is urgent, the facility should
seek EMS assistance to transport the resident to the nearest receiving facility. On the next working
day, contact DCF and AHCA to seek long term resolution. Document your actions in the resident
record.
ix. The facility is responsible for assuring that appropriate notice of transfer is issued at the time of
transfer. It is expected that the resident will be accepted back to the facility after the provision
of treatment at a receiving facility. The facility should re-evaluate the resident prior to making a
determination that they are no longer able to meet the individual needs of the resident.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix F - 1
Involuntary Examination
Appendix F
F
Involuntary Examination
s. 394.463, F.S.
e Baker Act encourages the voluntary admission of
persons for psychiatric care, but only when they are able to
understand the decision and its consequences and are able
to fully exercise their rights for themselves. When this is not
possible due to the severity of the person’s condition, the law
requires that the person be extended the due process rights
assured under the Baker Act’s involuntary provisions.
e denition of “mental illness” is not a part of this section
of the statute. However, because it is relevant to the content
of this part of the statute it is being included on this page.
“Mental illness” means an impairment of the mental or
emotional processes that exercise conscious control of
one’s actions or of the ability to perceive or understand
reality, which impairment substantially interferes with a
person’s ability to meet the ordinary demands of living,
regardless of etiology. For the purposes of this part,
the term does not include a developmental disability
as dened in chapter 393, intoxication, or conditions
manifested only by antisocial behavior or substance
abuse impairment.[(F.S. 394.455 (18)]
Criteria
s. 394.463(1), F.S.
A person may be taken to a receiving facility for involuntary
examination if there is reason to believe that he or she has a
mental illness (as dened in the Baker Act) and because of
his or her mental illness:
1. e person has refused voluntary examination after
conscientious explanation and disclosure of the purpose
of the examination; or the person is unable to determine
whether examination is necessary; and
a. Without care or treatment, the person is likely to
suer from neglect or refuse to care for himself
or herself; such neglect or refusal poses a real and
present threat of substantial harm to his or her
well-being; and it is not apparent that such harm
may be avoided through the help of willing family
members or friends or the provision of other
services; or
b. ere is a substantial likelihood that without care or
treatment the person will cause serious bodily harm
to self or others in the near future, as evidenced by
recent behavior.
Chapter 65E-5.280, F.A.C.
Initiation
s. 394.463(2), F.S. 65E-5.280(1)(2)(3)F.A.C.
An involuntary examination may be initiated by any one of
the three following means:
1. A court may enter an ex parte order (CF-MH 3001 or other
order developed by the court) stating that a person appears
to meet the criteria for involuntary examination, giving the
ndings on which that conclusion is based. e ex parte
order for involuntary examination must be based on sworn
testimony, written or oral (CF-MH 3002 or other form
developed by the court). No fee can be charged for the ling
of a petition for an order for involuntary examination.
A law enforcement ocer, or other designated agent
of the court, must take the person into custody and
deliver him or her to the nearest receiving facility for an
involuntary examination. A law enforcement ocer acting
in accordance with an ex parte order may serve and execute
such order on any day of the week, at any time of the day
or night. A law enforcement ocer acting in accordance
with an ex parte order may use such reasonable physical
force as is necessary to gain entry to the premises, and any
dwellings, buildings, or other structures located on the
premises, and to take custody of the person who is the
subject of the ex parte order.
e ocer must execute a written report entitled
“Transportation to a Receiving Facility” (CF-MH 3100)
detailing the circumstances under which the person was
taken into custody, and the report must be made a part of
the person’s clinical record.
e ex parte order is valid only until executed or, if not
executed, for the period specied in the order itself. If no
time limit is specied in the order, the order is valid for
seven days after the date that the order was signed. Once a
person is picked up on the order and taken to a receiving
facility for involuntary examination and released, the same
order cannot be used again during the time period. e
order of the court must be made a part of the person’s
clinical record.
2. A law enforcement ocer shall take a person who
appears to meet the criteria for involuntary examination
into custody and deliver the person or have him or her
delivered to the nearest receiving facility for examination.
(CF-MH 3052a) e ocer must execute a written report
(CF-MH 3100) detailing the circumstances under which
the person was taken into custody, and the report must be
made a part of the person’s clinical record.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Examination
Appendix F - 2
F
3. A physician, clinical psychologist, clinical social worker,
mental health counselor, marriage and family therapist
or psychiatric nurse (each as dened in the Baker Act)
may execute a certicate (CF-MH 3052b) stating that
he or she has examined a person within the preceding
48 hours and nds that the person appears to meet the
criteria for involuntary examination and stating the
professional’s observations upon which that conclusion
is based. A law enforcement ocer must take the person
named in the certicate into custody and deliver him
or her to the nearest receiving facility for involuntary
examination. e law enforcement ocer must execute a
written report detailing the circumstances (CF-MH 3100)
under which the person was taken into custody. e
report and certicate shall be made a part of the person’s
clinical record.
Definitions of Professionals
s. 394.455, F.S.
Physician means a medical practitioner licensed under
Chapter 458 or Chapter 459 who has experience in the
diagnosis and treatment of mental and nervous disorders or
a physician employed by a facility operated by the United
States Department of Veterans Aairs which qualies as a
receiving or treatment facility under this part. (21)
Psychiatrist means a medical practitioner licensed under
Chapter 458 or Chapter 459 who has primarily diagnosed and
treated mental and nervous disorders for a period of not less
than three years, inclusive of psychiatric residency. (24)
Clinical Psychologist means a psychologist as dened in s.
490.003(3) with 3 years of postdoctoral experience in the
practice of clinical psychology, inclusive of the experience
required for licensure, or a psychologist employed by a
facility operated by the United States Department of Veterans
Aairs that qualies as a receiving or treatment facility under
this part. (2)
Clinical Social Worker means a person licensed as a clinical
social worker under Chapter 491. (4)
Marriage and Family erapist means a person licensed as a
marriage and family therapist under Chapter 491. (36)
Mental Health Counselor means an individual who is licensed
as a mental health counselor under Chapter 491, F.S. (37)
Psychiatric Nurse means a registered nurse licensed under
Chapter 464 who has a master’s degree or a doctorate in
psychiatric nursing and two years of post-master’s clinical
experience under the supervision of a physician. (23)
e Florida Attorney General determined in May 2008 that
Physician Assistants can, under certain conditions, initiate
an involuntary examination. e ruling did not extend any other
authority granted to physicians.
Selected Procedures
Any receiving facility accepting a person based on a court’s ex
parte order, law enforcement ocer’s report or a professional’s
certicate must send a copy of the initiating document with
the required cover sheet (3118) to the Agency for Health Care
Administration on the next working day.
is must be mailed to:
Baker Act Reporting Center
FMHI
13301 Bruce B. Downs Blvd., MHC 2637
Tampa, Florida 33612-3807
A person cannot be removed from any long-term care program
or residential placement licensed under Chapter 400 or 429,
F.S. and transported to a receiving facility for involuntary
examination unless an ex parte order (CF-MH 3001), a
Law Enforcement Ocer’s report (CF-MH 3052a), or a
Professional’s Certicate (CF-MH 3052b), is rst prepared. If
the condition of the person is such that preparation of a law
enforcement ocer’s report is not practical before removal, the
report must be completed as soon as possible after removal,
but in any case before the person is transported to a receiving
facility. A receiving facility admitting a person for involuntary
examination who is not accompanied by the required ex parte
order, professional certicate, or law enforcement ocer’s report
must notify AHCA of such admission by certied mail no later
than the next working day. [CF-MH3119]
Examination
s. 394.463(2)(f ), F.S. Chapter 65E-5.2801, F.A.C.
A person must receive a mandatory initial mandatory involuntary
examination by a physician or clinical psychologist at a receiving
facility without unnecessary delay and may, upon the order of a
physician, be given emergency treatment if it is determined that
such treatment is necessary for the safety of the person or others.
is initial mandatory involuntary examination must include:
1. A thorough review of any observations of the person’s recent
behavior;
2. A review of the document initiating the involuntary
examination and transportation form;
3. A brief psychiatric history; and
4. A face-to-face examination of the person in a timely manner to
determine if the person meets criteria for release.
A physical examination, which must be conducted within 24 hours
of a person’s arrival at the facility, is intended to rule out mock

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix F - 3
Involuntary Examination
Appendix F
F
psychiatric symptoms caused by non-psychiatric medical illness,
injury, metabolic disorders, and drug toxicity.
e person cannot be released by the receiving facility
without the documented approval of a psychiatrist, clinical
psychologist, or physician in the hospital’s emergency
department. However, a person may not be held in a receiving
facility for involuntary examination longer than 72 hours. e
person must be given prompt opportunity to notify others of
his whereabouts. See Appendix H for circumstances involving
persons having an emergency medical condition for whom an
involuntary examination has been initiated.
Release
s. 394.463(2)(i), F.S.
Within the 72-hour examination period, one of the following
actions must be taken, based on the individual needs of the person:
1. e person must be released, unless he or she is charged
with a crime, in which case the person must be returned to
the custody of a law enforcement ocer;
2. e person must be released for outpatient treatment;
3. e person, unless he or she is charged with a crime, must
be asked to give express and informed consent to placement
on voluntary status, and, if such consent is given, the person
shall be voluntarily admitted. Such transfer from involuntary
to voluntary status must be conditioned on the certication
by a physician that the person has the capacity to make
well-reasoned, willful, and knowing decisions about mental
health and medical issues; or
4. A petition for involuntary inpatient placement CF-MH
3032) shall be led or a petition for involuntary outpatient
placement (CF/MH 3130) may be led in the appropriate
court by the facility administrator when treatment is
deemed necessary within the 72 hours or, if the 72 hours
ends on a weekend or holiday, no later than the next
working day thereafter.
If converted to voluntary status in lieu of seeking involuntary
placement, it may be necessary under some circumstances to
le documents with the Clerk of Court to prohibit rearm
purchase (see appendix S).
Escape or Elopement of a Person
from a Receiving or Treatment Facility
If a person being involuntarily examined or treated at a
receiving or treatment facility elopes from the facility, the
following procedures are recommended:
1. If the person is an adult on voluntary status and does
not meet the criteria for involuntary placement, law
enforcement will not be notied by the facility.
2. If the person is on voluntary status and does meet the criteria
for involuntary placement, a certicate (Form CF-MH
3052b) may be initiated by an authorized professional at the
facility and the appropriate law enforcement agency may be
requested to take the person named in the certicate into
custody and deliver him or her to the nearest receiving facility.
A transfer of the person, if appropriate, will then be arranged
using the procedure for transporting persons from facility to
facility.
3. If the person is on involuntary examination status and
within 72 hours of arrival at the facility appears to meet the
criteria for involuntary placement, but prior to the Petition
for Involuntary Placement being led with the court, the
appropriate law enforcement agency should be provided
a copy of the original ex parte order, Law Enforcement
Ocer’s Report (CF-MH 3052a), or Certicate of a
Professional (CF-MH 3052b) and requested to take the
person into custody and deliver him or her to the nearest
receiving facility. A transfer of the person, if appropriate, will
then be arranged from facility to facility.
4. If the person is on involuntary examination status and a
Petition for Involuntary Inpatient Placement has already
been led with the court, the appropriate law enforcement
agency will be provided a copy of the petition form (CF-
MH 3032) and requested to return the person to the
facility from which the petition was led.
5. If a person is under a court’s Order for Involuntary
Inpatient Placement (CF-MH 3008) at a treatment facility
leaves the facility without authorization, the administrator
may authorize a search for the person and the return of
the person to the facility. While the statute is silent with
regard to receiving facilities, it is presumed that the court
order itself would provide the required authority. e
administrator of the facility may request the assistance of
a law enforcement agency in the search for and return of
the person and may provide a copy of the order (CF-MH
3008) to law enforcement.
6. If a person escapes/elopes from a hospital Emergency
Department, he/she should be returned to the ED for an
appropriate transfer as required by EMTALA.
Notice of Discharge or Release
s. 394.463(3), F.S. s. 394.469(2), F.S.
Notice of discharge or transfer of a person shall be given as
provided in s. 394.4599, F.S. Notice of the release (CF-MH
3038) shall be given to the person’s guardian or representative,
to any person who executed a certicate admitting the person
to the receiving facility, and to any court that ordered the
person’s evaluation.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Examination
Appendix F - 4
F
Baker Act Involuntary Examination
Quick Reference Guide for Receiving Facilities
The person:
____ Has a mental illness, as defined in the Baker Act, and because of his or her mental illness:
____ Either ____refused or is ____unable to determine the need for voluntary examination, and either:
Without care or treatment, the person is likely to suffer from neglect or refuse to care for himself or
herself; or
There is a substantial likelihood that without care or treatment the person will cause serious bodily harm
to himself or herself or others in the near future, as evidenced by recent behavior.
The facility must open a clinical record on the person containing the following information/mandatory forms and
may include the recommended completed forms:
Documentation initiating involuntary examination and any accompanying affidavits, which shall be one
of the following three:
____Ex Parte Order for Involuntary Examination (CF-MH 3001) with the Petition and Affidavit Seeking Ex
Parte Order Requiring Involuntary Examination (CF-MH 3002), or
____Report of Law Enforcement Officer Initiating Involuntary Examination (CF-MH 3052a); or
____Certificate of Professional Initiating Involuntary Examination (CF-MH 3052b) by one of the
authorized professionals.
Transportation to Receiving Facility (CF-MH 3100) if the involuntary examination was initiated at a
location other than the receiving facility or hospital.
Notification of person’s representative or guardian of admission for involuntary examination by
telephone or in person within 24 hours. Opportunity for the person to notify others of whereabouts is
documented.
General Authorization for Treatment Except Psychotropic Medications (CF-MH 3042a) for those persons
appearing to be competent to consent to treatment or by their guardian or health care surrogate/proxy.
Inventory of Personal Effects (CF-MH 3043) documenting property brought by the person to the facility
signed by the person, if able, and witnessed by two staff members.
Authorization for Release of Information (CF-MH 3044) completed and signed only when such release is
to take place. No blank forms should be signed by the person or decision-maker.
Notice of Right to Petition for Writ of Habeas Corpus or for Redress of Grievances (CF-MH 3036)
Explanation and copy of Rights of Persons in Mental Health Facilities and Programs (CF-MH 3103)
Intake Interview
Baker Act Service Eligibility Form (CF-MH 3084) for persons admitted to public receiving facilities.
Subsequent to the person’s admission, the following forms or documentation must be completed:
Cover Sheet to Agency for Health Care Administration (CF-MH 3118) documenting the submission of the
court order, law enforcement officer’s report, or professional’s certificate to AHCA (BA Reporting Center
in Tampa).

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix F - 5
Involuntary Examination
Appendix F
F
Documentation of a physical examination by an authorized health practitioner within 24 hours of arrival
(medical stability and rule out non-psychiatric medical causes of symptoms]
Documentation of the Initial Mandatory Involuntary Examination by a physician or clinical psychologist,
including:
1. A thorough review of any observations of the person's recent behavior;
2. A review of the document initiating the involuntary examination and transportation form;
3. A brief psychiatric history; and
4. A face-to-face examination of the person in a timely manner to determine if the person meets
criteria for release.
Certification of Person's Competence to Provide Express and Informed Consent (CF-MH 3104) if
the person was permitted to sign a General Authorization for Treatment Except for Psychotropic
Medications (CF-MH 3042a) at the time of admission or if the person is to be permitted to sign a Specific
Authorization for Psychotropic Medications (CF-MH 3042b).
Completion of a Specific Authorization for Psychotropic Medications (CF-MH 3042b) by a qualified
health care practitioner prior to the administration of any psychotropic medications, and only after a
complete disclosure is made to the person, the guardian, guardian advocate, health care surrogate/
proxy, and to the guardian of a minor as to the:
_____ Reason for admission or treatment _____ Similar information on alternative
medication which may have less severe or
_____ Proposed treatment, including proposed
serious side effects
psychotropic medications
_____ Potential effects of stopping treatment
_____ Purpose of treatment to be provided
_____ Approximate length of care
_____ Alternative treatments
_____ How treatment will be monitored
_____ Specific dosage range of medications
_____ Any consent for treatment may be revoked
_____ Frequency and method of administration
orally or in writing before or during the
_____ Common risks, benefits and common
treatment period by the person legally
short-term and long-term side effects
authorized to make health care decisions
_____ Any contraindications which may exist
on behalf of the person
_____ Clinically significant interactive effects with
other medications
Personal Safety Plan (CF-MH 3124)
An individualized treatment plan completed within 5 days of the person’s admission in which the person
has had the opportunity to assist in preparing, including space for the person’s comments and a copy of
which has been provided to the person, guardian, guardian advocate, and a minor’s guardian
The following forms shall be included only if applicable:
If the person has been determined to be incompetent to consent to his or her own treatment, the
following forms may be used:
____Certification of Person's Incompetence to Consent to Treatment and Notification of Health Care
Surrogate/Proxy (CF-MH 3122)
____Affidavit of Health Care Proxy (CF-MH 3123)
____Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a
Guardian Advocate (CF-MH 3106)
____Order Appointing Guardian Advocate (CF-MH 3107)
____Certification of Guardian Advocate Training Completion (CF-MH 3120)

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Examination
Appendix F - 6
F
____Petition Requesting Court Approval for Guardian Advocate to Consent to Extraordinary Treatment
(CF-MH 3108)
____Order Authorizing Guardian Advocate to Consent to Extraordinary Treatment (CF-MH 3109)
Request for Involuntary Examination after Emergency Medical Services (CF-MH 3102)
Notification of a facility's Non-Compliance (CF-MH 3119)
Authorization for Electroconvulsive Treatment (CF-MH 3057)
Refusal or Revocation of Consent to Treatment (CF-MH 3105)
Restriction of Communication or Visitors (CF-MH 3049)
Restriction of Person's Access to Own Record (CF-MH 3110)
Petition for Writ of Habeas Corpus or for Redress of Grievance (CF-MH 3090)
Application for and Notice of Transfer to Another Facility (CF-MH 3046)
If it is determined that the person does not meet the criteria for involuntary inpatient or outpatient placement
and the person refuses voluntary admission, the facility must:
Release the person within 72 hours with the documented approval of a psychiatrist, clinical psychologist,
or emergency department physician using “Approval for Release of Person on Involuntary Status from a
Receiving Facility” (CF-MH 3111)
Send copies of “Notice of Release or Discharge” (CF-MH 3038) by first class mail to:
____Person’s guardian or representative
____Any person executing certificate admitting person to a receiving facility
____Any court which ordered person’s involuntary examination
If it is determined that the person meets the criteria for involuntary inpatient/outpatient placement and either
refuses voluntary placement or is unable to determine that such placement is needed, the facility must (see Quick
Reference Guide for Receiving and Treatment Facilities for Involuntary Inpatient Placement- Appendix J):
File a Petition for Involuntary Inpatient Placement (CF-MH 3032) with the circuit court.
Facility may file a petition for involuntary outpatient placement (CF-MH 3130) with the circuit court
(Appendix K)
If involuntary inpatient placement in a state mental health facility is sought for the person:
Transfer Evaluation (CF-MH 3089)
State Mental Health Facilities Admission Form (CF-MH 7000)
Physician to Physician Transfer Form (CF-MH 7002)
If at any time prior to the court hearing on involuntary inpatient placement, the facility determines that the person
will be discharged, transferred to another facility, or transferred to voluntary status, it will immediately:
Telephone, then submit in writing, a Notification to Court of Withdrawal of Petition for Hearing on Involuntary
Placement (CF-MH 3033) and notify any persons expected to attend the hearing.
File packet of forms for Firearm Prohibition with the Clerk of Court within 24 hours if person is found to be of
imminent danger by a physician (per 790.065, F.S.)
Recommended forms are those which are not required by the department, but which have been determined to satisfy the
specific requirements for which the form has been developed. Alteration of recommended forms may jeopardize this status.
Mandatory forms may not be altered. No blank forms should be signed by staff, the person, or substitute decision-maker.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix F - 7
Involuntary Examination
Appendix F
F
Criteria: Reason to believe person has a mental illness and because of the
mental illness
Person refuses or is unable to determine examination is necessary; and
Likely to suffer from self-neglect or harm to self or others
Law enforcement
Authorized mental
health professional
Transportation to Receiving Facility
Law enforcement takes person into custody and delivers person to
nearest receiving facility for involuntary examination
Exceptions to law enforcement transport only in accord with
transportation exception plan, county-funded transport contract, or
emergency medical transport
Within 72 hours of examination period
Petition for involuntary inpatient/outpatient
placement completed by two experts and facility
administrator
If 72 hour period ends on weekend or holiday,
petition filed by next working day
Transferred to voluntary status if
all criteria are met
Notices to guardian or representative
Initiating document and cover sheet sent to BA Reporting Center within 1 working day
Initial mandatory examination by a physician or clinical psychologist without necessary delay
Physical examination by an authorized health practitioner within 24 hours after arrival
Determination of adult’s competence to give express and informed consent to treatment
Involuntary Examination
s. 394.463, F.S. Chapter 65E-5.280, F.A.C.
Released from receiving
facility after "approval"
by psychiatrist, clinical
psychologist, or ER physician,
with required notices sent
q
q
q
q
q
Initiation by
Circuit court
Competent
to consent
3040a
3040b
Petition for adjudication of
incompetence to consent
and appointment of
guardian advocate
Incompetent to
consent to treatment
If person is determined by physician
to be of imminent danger, packet of
forms on firearm prohibition filed
within 24 hours with Clerk of Court

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Examination
Appendix F - 8
F
Specialized on-line Baker Act courses can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 1
Law Enforcement
Appendix G
G
Law Enforcement and the Baker Act
Initiation: s. 394.463, F.S. and s. 65E-5.280, F.A.C.
Transportation: s. 394.462, F.S and 65E-5.260, F.A.C.
Introduction
Law enforcement ocers often serve as the front line for
many social and health problems of our communities.
Although mental illness is a health problem, it is often a
personal and a public safety issue as well. e Legislature in
Florida has granted law enforcement certain authority and
responsibilities under the Baker Act.
e authority to initiate an involuntary examination of
persons when they meet certain criteria and are unable
or unwilling to consent to the examination themselves.
e responsibility, with few exceptions, to transport
persons to the nearest receiving facility for involuntary
examination.
e Baker Act is Florida’s Mental Health Act and cannot be
used interchangeably with other statutes. Other related but
dierent statutes include:
Marchman Act, Chapter 397, F.S., which governs
all issues related to intoxication or substance abuse
impairment.
Chapter 393, F.S., which governs all issues related to
intellectual disability, autism, and other developmental
disabilities.
Chapter 401, F.S., which is the emergency medical
services law containing provisions for the Emergency
Examination & Treatment of Incapacitated Persons who
cannot provide consent to Emergency Medical Services
(EMS) personnel.
Florida’s hospital licensing statute, Chapter 395.1041,
F.S., which governs Access to Emergency Services and
Care in hospital emergency departments.
e federal Emergency Medical Treatment and Active
Labor Law, or EMTALA, that requires all licensed
hospitals to accept persons for medical screening and
stabilization, and makes those hospitals responsible for
arranging safe and appropriate secondary transfers to
other facilities.
Chapter 415, F.S., the Adult Protective Services law that
protects vulnerable adults (persons age of 60 or older and
disabled adults) from abuse, neglect and exploitation.
Voluntary Admission
Adults can only be admitted to a facility on a voluntary
basis if they have a mental illness as dened in the Baker
Act, are willing to be admitted without any coersion, are
competent to provide express and informed consent, and are
suitable for treatment. A minor must meet the same criteria,
including willingness to be admitted, but the application
for admission must be made by his or her parent or legal
guardian following a judicial hearing.
Law enforcement ocers have no legal duty to transport any
person for voluntary admission to a psychiatric facility.
Involuntary Examination
A person may be taken to a receiving facility for involuntary
examination if there is reason to believe that he or she has a
mental illness and because of his or her mental illness:
1. e person has either refused a voluntary examination or
is unable to determine for himself or herself whether an
examination is necessary; and
2. Either:
» e person is likely to suer from neglect which
poses a real and present threat of substantial harm to
his or her well-being that can’t be avoided through
the help of willing family members or friends or the
provision of other services; or
» ere is substantial likelihood that without care or
treatment the person will cause serious bodily harm
to himself or herself or others in the near future, as
evidenced by recent behavior.
Behaviors to Look For
Individuals with mental illness who may need further
evaluation typically exhibit some combination of the
following behaviors, or characteristics:
Behaviors: rapid speech, ight of thought, no eye contact,
quick movements, disconnected speech patterns, constant
movement, can’t concentrate, swift and frequent mood
changes, disorganized thoughts, disoriented to time and
place, acts of violence, cutting self, combative/aggressive
behavior, inappropriate dress or nudity.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
Appendix G - 2
G
Hallucinations: sees people who aren’t there, hears voices
telling them to hurt themselves or others, reports that the
television is suggesting harm to others, turning the head as
if listening to an unseen person.
Self-Care Issues: insomnia or increased sleep, has not eaten
for days, not taking prescribed medications, home is in
disarray, neglects household, property, or personal hygiene
to the point of putting self/others at risk.
Feelings: low self-esteem with feelings of hopelessness or
helplessness, at aect, or not reacting with much feeling
or interest.
Suicidal Risks: has weapons or access to weapons, speaks
about previous attempts, makes direct comments about
dying or hurting self, evidence of previous attempts such as
scars on the wrists.
Elderly Issues: wandering at night, leaving things on stove
unattended, not eating or sleeping or caring for personal
needs, unrealistic fears, uncontrollable anxiety, confusion,
quantity and age of unused foods in the home.
Substance Abuse: abuse of prescribed medications, use
of alcohol or illegal substances while taking medications.
(If substance abuse appears to be the only issue, the
Marchman Act may be more appropriate.)
Initiation of Involuntary Examination
An involuntary examination under the Baker Act can
be initiated by a circuit court judge, an authorized
mental health professional or by a Florida certied law
enforcement ocer. e criteria is the same, regardless of
which of the three methods is used to initiate.
A “law enforcement ocer” is specically dened in the
Baker Act as a law enforcement ocer as dened in s.
943.10, F.S. erefore, as Chapter 943 is revised in future
legislative sessions, the Baker Act will not have to be revised
further. [s.394.455, F.S.] is denition includes a wide
array of state certied law enforcement ocers, but doesn’t
include probation ocers who are licensed under chapter
943, but not as law enforcement ocers.
943.10(1) “Law enforcement ocer” means any person
who is elected, appointed, or employed full time by any
municipality or the state or any political subdivision
thereof; who is vested with authority to bear arms and
make arrests; and whose primary responsibility is the
prevention and detection of crime or the enforcement
of the penal, criminal, trac, or highway laws of the
state. is denition includes all certied supervisory
and command personnel whose duties include, in whole
or in part, the supervision, training, guidance, and
management responsibilities of full-time law enforcement
ocers, part-time law enforcement ocers, or auxiliary
law enforcement ocers but does not include support
personnel employed by the employing agency.
e Florida Attorney General has determined that “Federal
law enforcement ocers do not constitute law enforcement
ocers for purposes of Florida’s Baker Act, and thus possess
no authority under the act to initiate the involuntary
examination of a person or to transport such person as law
enforcement ocers.”
ere are three important key points to remember for
ocers:
1. Your role is not to diagnose. However, if you have
reason to believe that someone has a mental illness, you
can decide whether or not that person may be putting
himself/herself or others in active danger or self neglect,
and therefore meet the criteria for a complete evaluation.
2. You do not need to witness all of the behaviors
personally. You can consider credible eyewitness accounts
from others as you determine the need for further
assessment.
3. Law enforcement officers must complete two state
forms when initiating a Baker Act. e two forms are
Report of Law Enforcement Ocer Initiating Involuntary
Examination (CF-MH 3052a), and Transportation to
a Receiving Facility-Part 1 (CF-MH 3100). Generally,
ocers also must complete their own department’s
Oense/Incident report.
While a circuit court judge or mental health professional may
initiate an involuntary examination if they believe the criteria
are met, the Baker Act requires a law enforcement ocer to
take a person who appears to meet the criteria for involuntary
examination into custody.
e statute is silent as to whether the ocer must personally
see the person’s behavior, but there is no expectation that the
ocer should be able to clinically diagnose mental illness or
predict dangerousness. Evidence of likelihood of harm to self
or others is dened solely by the person’s “recent behavior.”
e law requires that the law enforcement ocer’s report
detail the “circumstances” under which the person was taken
into custody, not personal observations. As the Baker Act is a
civil law, not a criminal one, “probable cause” is not required.
Since the ocer is rarely on site when the event prompting
the Baker Act call occurs, his or her judgment may often be
based upon the statements by the person or the credibility
of the witnesses to the event. For example, one can usually
presume a relative contacting law enforcement about a

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 3
Law Enforcement
Appendix G
G
family member has their loved one’s best interest in mind,
unless the ocer believes that the call to law enforcement
may be a retaliatory act. It is not the ocer’s job to conduct
an examination, only to initiate the examination when
the criteria appears to be met by taking the person to a
designated receiving facility where an expert must perform
the involuntary examination.
e Baker Act states that “any person who acts in good faith
in compliance with the provisions of this part is immune
from civil or criminal liability for his or her actions in
connection with the admission, diagnosis, treatment, or
discharge of a patient to or from a facility. However, this
section does not relieve any person from liability if such
person commits negligence.” Law enforcement ocers
should consult with their department’s legal counsel in
determining whether there is greater liability in:
Acting to protect a person even though a skilled
clinician may ultimately determine that the person
does not meet the more stringent statutory criteria for
involuntary placement, or
Failing to act when credible witnesses allege passive or
active danger and the person ultimately suers harm or
commits an act of violence.
Most attorneys would gauge the seriousness of the
consequences of the above decisions and suggest that the
examination be initiated by law enforcement, leaving it to
mental health experts to conrm whether the criteria have
been met. While common sense should always prevail,
each law enforcement department needs to develop explicit
policies and procedures to reect the actions which should
be taken in such circumstances.
Initiation of Involuntary
Examination by Others
If the involuntary examination has been initiated by
the circuit court, a court order will be given to the law
enforcement ocer to deliver with the person to the nearest
receiving facility where it will be made a part of the person’s
clinical record.
A law enforcement ocer acting in accordance with an ex
parte order may serve and execute such order on any day of
the week, at any time of the day or night, and may use such
reasonable physical force as is necessary to gain entry to the
premises and any dwellings, buildings, or other structures
located on the premises and to take custody of the person
who is the subject of the ex parte order.
e court order for involuntary examination, along with
the petition(s) seeking the order, will be delivered by the
law enforcement ocer to the facility to be placed in the
person’s clinical record along with the “Transportation to a
Receiving Facility” form (CF-MH 3100) completed by the
law enforcement ocer. [ss. 394.463(2)(a), (c) and (d), F.S.]
If the involuntary examination has been initiated by a
physician, clinical psychologist, psychiatric nurse, clinical
social worker, licensed mental health counselor or licensed
marriage and family therapist, a certicate must be
completed by the professional stating that he or she has
examined a person within the preceding 48 hours and nds
that the person appears to meet the criteria for involuntary
examination and stating the professional’s observations upon
which that conclusion is based.
e professional, if not already located at a receiving facility
or hospital emergency room, will call the law enforcement
agency designated by the Board of County Commissioners
to execute such certicates to transport the person to the
nearest receiving facility for examination. e mental
health professional’s certicate (CF-MH 3052b) and the
“Transportation to a Receiving Facility” form (CF-MH 3100)
completed by the law enforcement ocer will be made a part
of the person’s clinical record.
Transportation of Persons
for Involuntary Examination
e Baker Act requires law enforcement ocers to transport
any person for whom an involuntary examination has been
initiated to the nearest receiving facility. Law enforcement
ocers have the responsibility to transport persons under
involuntary examination status, instead of health or social
service personnel, because the involuntary criteria requires
that the person be refusing examination or be unable to
determine that the examination is necessary. For anyone other
than those authorized by statute to take a person against his
or her will or without informed consent could be a criminal
oense such as battery, false imprisonment, kidnapping, etc.
In addition, law enforcement is specically trained in the
transportation of persons who are either violent, resisting
transportation, or are otherwise unwilling to comply with
directions. Others without that training are much more likely
to either injure or be injured by the person.
Two appellate cases and a Florida Attorney General Opinion
apply to law enforcement duty to transport:
Administrator, Retreat Hospital v. Honorable W.
Clayton Johnson of the Seventeenth Judicial Circuit In
and For Broward County, FL, Alan Schreiber, Broward
County Public Defender, and Fredrick A. Goldstein,
Special Assistant Public Defender, Respondents, 660
So. 2d 333 (Fla. 4th DCA 1995). Individuals were

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
Appendix G - 4
G
transported by private entities to a receiving facility for
involuntary placement under the Baker Act. e Circuit
Court Judge found that this did not comport with the
requirements of section, 394.463(2), F.S. which requires
that only law enforcement ocer may transport persons
on involuntary status to a receiving facility. e Fourth
District Court of Appeals armed that only a law
enforcement ocer may transport a Baker Act patient to
a receiving facility.
Donald Pruessman v. Dr. John T. MacDonald
Foundation, 589 So. 2d 948 (Fla. 3d DCA 1991). e
3rd DCA held that where a patient was discharged
from a hospital and the patient refused to leave, and the
hospital administrator contacted an outside doctor to
evaluate the patient regarding Baker Acting the patient,
the hospital was not legally responsible for any action
taken by the outside doctor involved in Baker Acting
the patient. e 3rd DCA also held that the actions of
the city police ocers who were called to the hospital to
take the patient into custody, remove the patient from
the hospital, and transport the patient to a Baker Act
receiving facility based on a doctor’s certication were
not discretionary under the Baker Act and the city was
not liable for the actions of the city police ocers in
transporting the patient to a receiving facility.
AGO 2001-73 Regarding the responsibility for
Transportation of Mentally Ill Person to Treatment
Facility. If a person is the subject of an ex parte order
or certicate requiring involuntary examination and
treatment under Florida’s Baker Act, the single law
enforcement agency designated by the county for this
purpose is responsible for transporting that person to
the nearest receiving facility. If a person is taken into
custody by a law enforcement ocer for minor criminal
behavior or non-criminal behavior that meets the
statutory guidelines for involuntary examination under
the Act, the law enforcement ocer taking the person
into custody is responsible for transporting the person
to the nearest treatment facility. If a law enforcement
ocer arrests a person for commission of a felony
and believes that the person meets the guidelines for
involuntary examination or placement, the person shall
be processed through the criminal justice system like any
other criminal suspect and is entitled to examination and
treatment in the facility where he or she is held.
While a law enforcement ocer is responsible for
transporting all persons for involuntary examination, there
is no responsibility for an ocer to transport persons for
voluntary examinations since persons on voluntary status
are by denition both willing and able to provide consent
to the examination. However, there is nothing to prohibit
such transportation if an ocer and their law enforcement
department (including legal counsel) concur.
Memorandum of Understanding (MOU) Required
(394.462 (1),(K) F.S.) Each law enforcement agency is
required by law to develop a MOU with each receiving
facility within it’s jurisdiction reecting a single set of
protocols for the safe and secure transport, crisis intervention,
and transfer of custody of a responsible individual at the
facility. DCF has made available a template for the MOU
to incorporate the requirements, but modications to the
format are allowed.
ere are circumstances under which a law enforcement
ocer can delegate the responsibility to someone else
to perform the transport. e Baker Act states that the
designated law enforcement agency may decline to
transport the person to a receiving facility only if:
1. e jurisdiction designated by the county has contracted
with an emergency medical transport service or private
transport company for transportation of persons to Baker
Act receiving facilities at the sole cost of the county; and the
law enforcement agency and the transport service agree that
the continued presence of law enforcement personnel is
not necessary for the safety of the person or others.
2. When a law enforcement ocer takes custody of a person
under the Baker Act, the ocer can request assistance
from emergency medical personnel if such assistance
is needed for the safety of the ocer or the person in
custody (person may be too frail, heavy, non-ambulatory,
or medically involved to be placed in a cruiser). Further,
if the ocer believes that a person has an emergency
medical condition, the person can be rst transported to
a hospital for emergency medical treatment, regardless
of whether the hospital is a designated receiving facility.
Once taken to a hospital for examination or treatment of
an emergency medical condition, transportation of the
patient to a Baker Act receiving facility is the responsibility
of the sending hospital.
3. When a mental health overlay program or a mobile crisis
response service evaluates a person and determines that
transportation to a receiving facility is needed, it may
transport the person to the facility or may call on the
law enforcement agency or make other transportation
arrangements best suited to the needs of the patient.
4. When a transportation exception plan has been approved
by the Board of County Commissioners and the Secretary
of the Department of Children and Family Services [s.
394.462(3), F.S.] permitting use of a “more humane
method of transport.
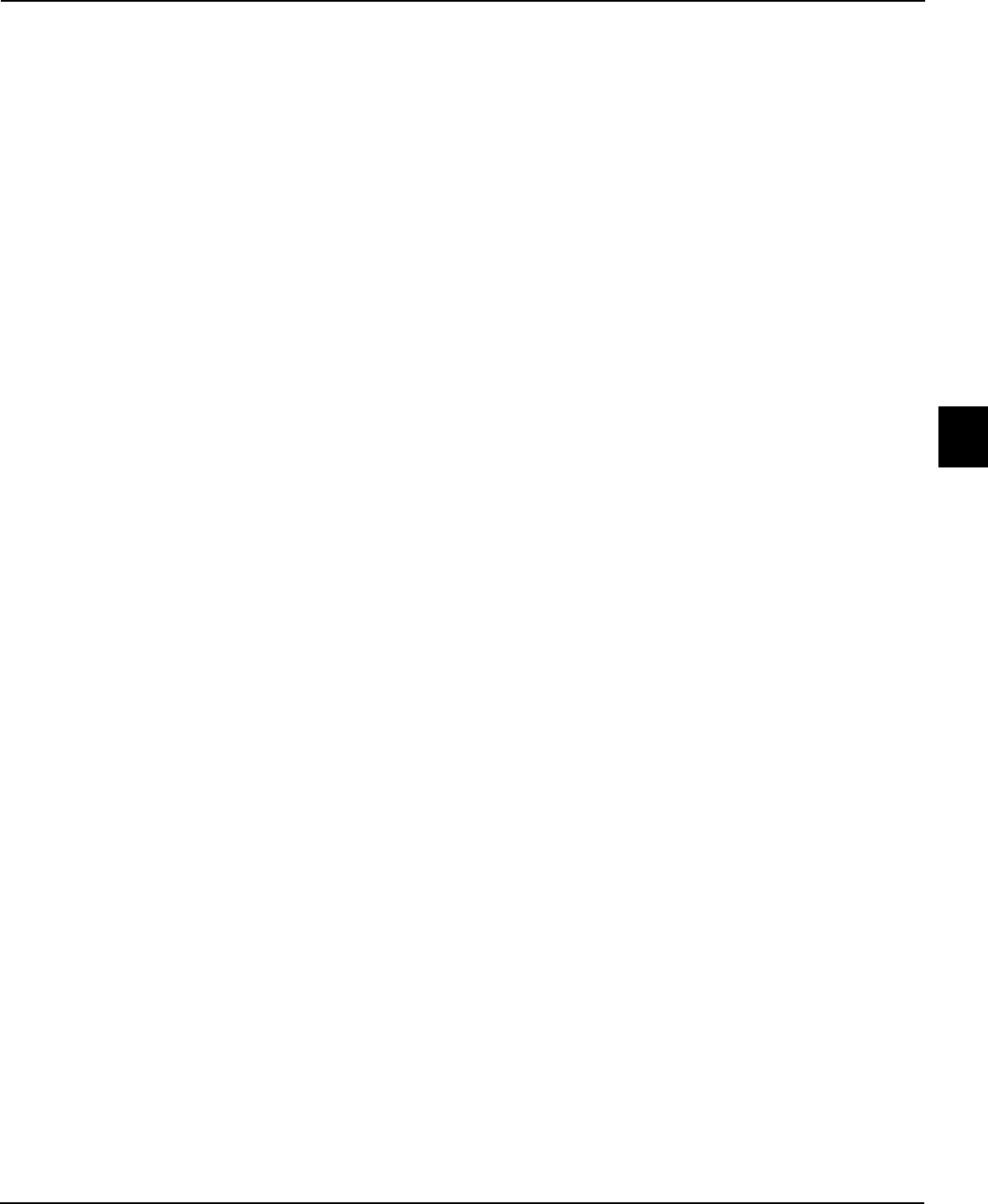
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 5
Law Enforcement
Appendix G
G
Transportation for Medical Emergencies
Law enforcement ocers are statutorily required to take
persons to the nearest receiving facility for involuntary
examinations. It is not appropriate to have law enforcement
take individuals to a non-receiving facility for “medical
clearance” rst unless the ocer believes the individual was
in an emergency medical condition. An emergency medical
condition is dened in Chapter 395, F.S. as a medical
condition manifesting itself by acute symptoms of sucient
severity, which may include severe pain, such that absence of
immediate medical attention could reasonably be expected
to result in serious jeopardy to patient health, serious
impairment to bodily functions, or serious dysfunction of any
bodily organ or part.
Once a person is delivered by law enforcement to a
hospital for emergency medical examination or treatment
and the person is placed in the hospital’s care, the ocer’s
responsibility to the person is over, assuming there are no
criminal charges pending.
Eventual safe and appropriate transfer of the person from
the hospital oering emergency medical treatment to the
designated receiving facility for an involuntary examination
under the Baker Act is the responsibility of the referring
hospital, unless other appropriate arrangements have been
made.
Designation of Transportation Responsibility
e law enforcement agency responsible for transporting
people for involuntary examinations under the Baker
Act is determined by each county’s Board of County
Commissioners. e 1984 Florida Legislature required
that each county designate a single law enforcement agency
within the county, or portions thereof, to take persons into
custody upon entry of an ex parte order or the execution of
a certicate for involuntary examination by an authorized
professional and to transport that person to the nearest
receiving facility for examination. is might result in the
Sheri’s Oce being responsible for certain transportation
and municipal police responsible for others. A copy of the
formal action taken by the Board of County Commissioners
should be available through the County Attorney’s oce.
Nearest Receiving Facility
Law enforcement ocers have to take persons to the nearest
Baker Act receiving facility, regardless of whether the facility
is public or private and regardless of whether a person has
the ability to pay for care. Further, it cannot be to a dierent
facility where the person, their caregiver, or mental health
professional has asked they be taken. e only alternative
to this is when a Transportation Exception Plan has been
approved by the Board of County Commissioners and the
DCF Secretary that provides persons be taken to a central
receiving facility or to facility that has specialized care for
certain persons such as minors or elders. If a person is at a
hospital or other receiving facility that can’t meet his/her
medical or psychiatric needs or if the person’s age or nancial
status requires transfer, the federal EMTALA law and state
Baker Act transfer provisions place responsibility on the
sending hospital, not on law enforcement personnel.
e Baker Act requires that the person be taken to the
nearest receiving facility, making no reference to remaining
in an ocer’s jurisdiction. However, if a transportation
exception plan is approved by a Board of County
Commissioners and the Secretary of the Department of
Children and Families for a given county, the plan may
result in jurisdictional boundaries.
Criminal Charges
e Baker Act requires a law enforcement ocer who has
custody of a person based on either non-criminal or minor
criminal behavior that meets the statutory guidelines for
involuntary examination to transport the person to the
nearest receiving facility for examination, instead of to jail. [s.
394.462(1)(f ), F.S.]
However, the transportation provisions of the Baker Act
state that if the person meets the criteria for involuntary
examination and has been arrested for a felony, the person
must rst be processed in the same manner as any other
criminal suspect. [s. 394.462(1)(g)m F.S.] Law enforcement
ocials must then contact the nearest public receiving
facility which is then responsible for promptly arranging for
the examination and treatment of the person. If the receiving
facility can document that it cannot provide adequate
security of a person with felony charges, it is required to
provide the mental health examination and treatment to the
person where he or she is held. e costs of transportation,
evaluation, hospitalization, and treatment incurred by
persons who have been arrested for violations of any state,
county, or municipal law/ordinance can be recovered by the
receiving facility as provided in s.901.35, F.S.
Use of Restraining Devices
e Baker Act states that the individual dignity of the
person must be respected at all times, including any
occasion when the person is taken into custody, held or
transported. Procedures, facilities, vehicles, and restraining
devices utilized for criminals or those accused of crime

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
Appendix G - 6
G
may not be used in connection with persons who have a
mental illness, except for the protection of the person or
others. When the ocer documents in his or her report
that circumstances require such protection, restraints may
be used in accordance with the law enforcement agency’s
written policies [s. 394.459(1), F.S.].
Procedures
1. Facilities Must Accept. e Baker Act states that
the nearest receiving facility must accept persons
brought by law enforcement ocers for involuntary
examination. If the receiving facility believes the person
should be “medically cleared,” the facility must arrange
appropriate medical transport for this purpose. It would
be inappropriate for a law enforcement ocer to place
a person at medical risk back into the cruiser. If the
receiving facility is at capacity or otherwise cannot meet
the person’s needs due to age or nancial need, it should
accept the person and arrange an appropriate transfer to
another receiving facility.
2. Weapons. e Baker Act prohibits rearms or deadly
weapons from being brought onto the grounds of a
hospital providing mental health services, including by
law enforcement ocers, unless specically authorized by
law or by the hospital administrator. Law enforcement
ocers may choose to lock their rearms in their vehicle
prior to entering a facility or may place the weapons in a
lock-box at the facility, if one exists. [s. 394.458(1), F.S.]
3. Hospital Security. A law enforcement ocer does not
have to wait at a hospital or other receiving facility for
the person to be medically screened, treated, or to have
their insurance veried. e ocer’s only duties are to
present the person and the required completed paperwork
and make a responsible hando to the appropriate sta
member. However, if the person is acting in a dangerous
manner, beyond the ability of the facility sta to manage,
the ocer should stay to assist for a temporary period
until hospital clinical or security sta can arrive. If the
person has criminal charges, the ocer’s Department
Policy should be followed.
4. Transfers. A law enforcement ocer does not have to
return to a hospital to transfer the person to another
facility following medical clearance. Once the person
is taken to the hospital, the state’s Baker Act and the
federal EMTALA law require the hospital to arrange for
appropriate transfer, when necessary.
e federal Emergency Medical Treatment and Active
Labor Act (EMTALA) preempts any state law with which
it is in conict. EMTALA requires that a hospital accept
any person who presents or is brought to the emergency
room for the purpose of performing a medical screening.
If the ED sta determine the person has an emergency
medical condition (including psychiatric and substance
abuse emergencies), the hospital is then responsible for the
person until the emergency has been stabilized, including
the person’s discharge or transfer from the hospital to
another facility that has the capability and capacity to
manage the person’s condition. is includes, among other
responsibilities, the duty to arrange a safe and appropriate
method of transportation to the destination facility.
5. Paperwork. A law enforcement ocer has to present
certain completed forms to the Baker Act receiving facility
sta. e Baker Act form entitled “Transportation to a
Receiving Facility” (CF-MH 3100) must be presented
each time a law enforcement ocer takes a person to a
receiving facility for involuntary examination, regardless
of whether the examination is initiated by a judge, a
mental health professional, or by the ocer. In addition,
the Baker Act form entitled “Report of Law Enforcement
Ocer Initiating Involuntary Examination” (CF-MH
3052a) must be completed when the ocer, as opposed
to the judge or mental health professional, initiates the
examination. ese forms, as well as all other Baker
Act forms can be obtained from the circuit oce of
the Department of Children and Families or can be
downloaded from the DCF website. [Chapter 65E-5.280,
F.A.C.]
e Mental Health Professional’s Certicate form should go
with the law enforcement ocer to deliver with the person
to the receiving facility. Many receiving facilities want the
original, although they are required to accept the person from
law enforcement regardless of whether the form is an original
or a copy. e initiating professional should retain a copy of
the initiation form in the person’s record.
Law enforcement ocers are required to complete the front
side of the transportation form (CF-MH 3100). In addition,
they should complete and sign the back of the form when
delegating the transportation to medical transport. en the
transport form as well as the initiation form (BA 52a, BA
52b, or ex parte order) must be sent with the person to the
receiving facility.
e Baker Act is very clear. e nearest receiving facility must
accept any person brought by law enforcement ocers for
involuntary examination. [s.394.462(1)(j), F.S.]

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 7
Law Enforcement
Appendix G
G
Escape or Elopement of Persons from a Baker Act
Receiving Facility
It is the responsibility of each Baker Act receiving facility and
hospital emergency departments to retain persons safely and
not allow them to elope or to depart against medical advice if
they meet criteria for involuntary examination.
If a person being examined or treated at a receiving facility
or ER elopes from the facility, the following procedures are
recommended:
1. If an adult is on voluntary status and does not meet the
criteria for involuntary placement, law enforcement
should not be notied by the facility.
2. If the person is on voluntary status and does appear to
meet the criteria for involuntary placement, a certicate of
a professional should be initiated by an authorized person
at the facility and the appropriate law enforcement agency
should be requested to take the person named in the
certicate into custody for delivery to the nearest receiving
facility. A transfer of the person, if appropriate, will then
be arranged between facilities.
3. If the person elopes while on involuntary examination
status within 72 hours of arrival at the facility, but prior
to the Petition for Involuntary Placement being led with
the court, the appropriate law enforcement agency will be
provided a copy of the original CF-MH 3052a or 3052b
and requested to take the person into custody for delivery
to the nearest receiving facility. A transfer of the person, if
appropriate, will then be arranged from facility to facility.
4. If the person is on involuntary examination status and a
Petition for Involuntary Placement has already been led
with the court, the appropriate law enforcement agency
will be provided a copy of the petition form (CF-MH
3032) and requested to return the person to the facility
from which the petition was led.
5. If a person under a court’s Order for Involuntary Placement
(CF-MH 3008) at a treatment facility leaves the facility
without authorization, the administrator may authorize a
search for the person and the return of the person to the
facility. While the statute is silent with regard to receiving
facilities, it is presumed that the court order itself would
provide the required authority. e administrator of the
facility may request the assistance of a law enforcement
agency in the search for and return of the person and may
provide a copy of the order to law enforcement.
6. If a person elopes from a hospital emergency department,
he/she should be returned to the hospital for appropriate
transfer as required by the federal EMTALA law.
Confidentiality of Clinical Records
Many state and federal laws govern the condentiality of
medical information and some even require mandatory
reporting. For example:
Law enforcement ocers, in addition to many other
identied persons, have a duty to report suspected abuse,
neglect, or exploitation of children or vulnerable adults.
e Vienna Convention and bilateral agreements the
United States has with other countries require law
enforcement to notify the consulate whenever a Foreign
National (even those with dual citizenship) is detained in
any manner, including under the Baker and Marchman
Act. e ocer is not required to inform the consulate
of the reason for the detention, considering the privacy
rights of the person.
HIPAA doesn’t apply to law enforcement ocers, except
the medical records of inmates in the jail.
Laws governing condentiality of information on people
with communicable disease and substance abuse are
dierent than those applying to other medical or mental
health diagnoses.
Any person, agency, or entity receiving information pursuant
to the Baker Act has to maintain such information as
condential and exempt from the provisions of Florida’s
public records law [s. 119.07(1), F.S.].
erefore, any documents initiating an involuntary
examination, reports resulting from transportation of
the person to a receiving facility, responses to a person’s
elopement from a facility, or other information which could
provide for the identication of the person, may not be
released by law enforcement.
However, the Florida Attorney General has issued opinions
that state the ocers’ incident reports are public records and
can be released to the public, even if the reports have the
same information as is contained in the ocial forms.
e Baker Act permits release of condential information
when a person has declared an intention to harm other
persons. When such a declaration has been made, the
facility administrator can authorize the release of sucient
information to provide adequate warning to the person
threatened with harm by the person. e law does not allow
the release of condential information to law enforcement
about confessions the person may have made about past
crimes he or she may have committed. In fact, the 9th US
Circuit Court of Appeals has ruled that while therapists are
sometimes required to report incidents to authorities that
could lead to violence, the court ruled that prosecutors can’t
use testimony from therapists to help convict their patients.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
Appendix G - 8
G
Crisis Intervention Teams
e use of CIT – Crisis Intervention Teams based on the
Memphis Police Department model – has been a great
innovation in reducing ocer use of force and injuries to
ocers and to persons with mental illnesses.
Many Florida communities have implemented CIT to address
issues of ocer safety, consumer safety, and jail diversion. Over
6% of adults in the general population have a serious mental
illness. Many people with serious mental illnesses have limited
access to treatment or do not remain in treatment. As a result,
these people are at increased risk for crises. Law enforcement
ocers are often the rst responders in crisis situations after
calls from families or citizen call for help.
Many other jurisdictions around the country have modeled
their programs after the “Memphis Model.” While little State
or Federal funds have been provided to most communities,
program costs are minimal and deployment of non-law
enforcement personnel is not required. Six benets identied
in CIT studies showed:
Few injuries to law enforcement ocers
Reduction in arrest rates and use of force incidents
Few repeat commitments to inpatient care
Reduction in patient violence
Less ocer time involved per call
Reduction in jail days for oenders with mental illnesses
Conclusion
e role of law enforcement in dealing with persons having
serious mental illnesses is a dicult one. e Department of
Children and Families maintains extensive materials on its
website regarding the Baker Act and the Marchman Act that
can assist law enforcement personnel.
A specialized on-line Baker Act course for law enforcement
ocers can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.
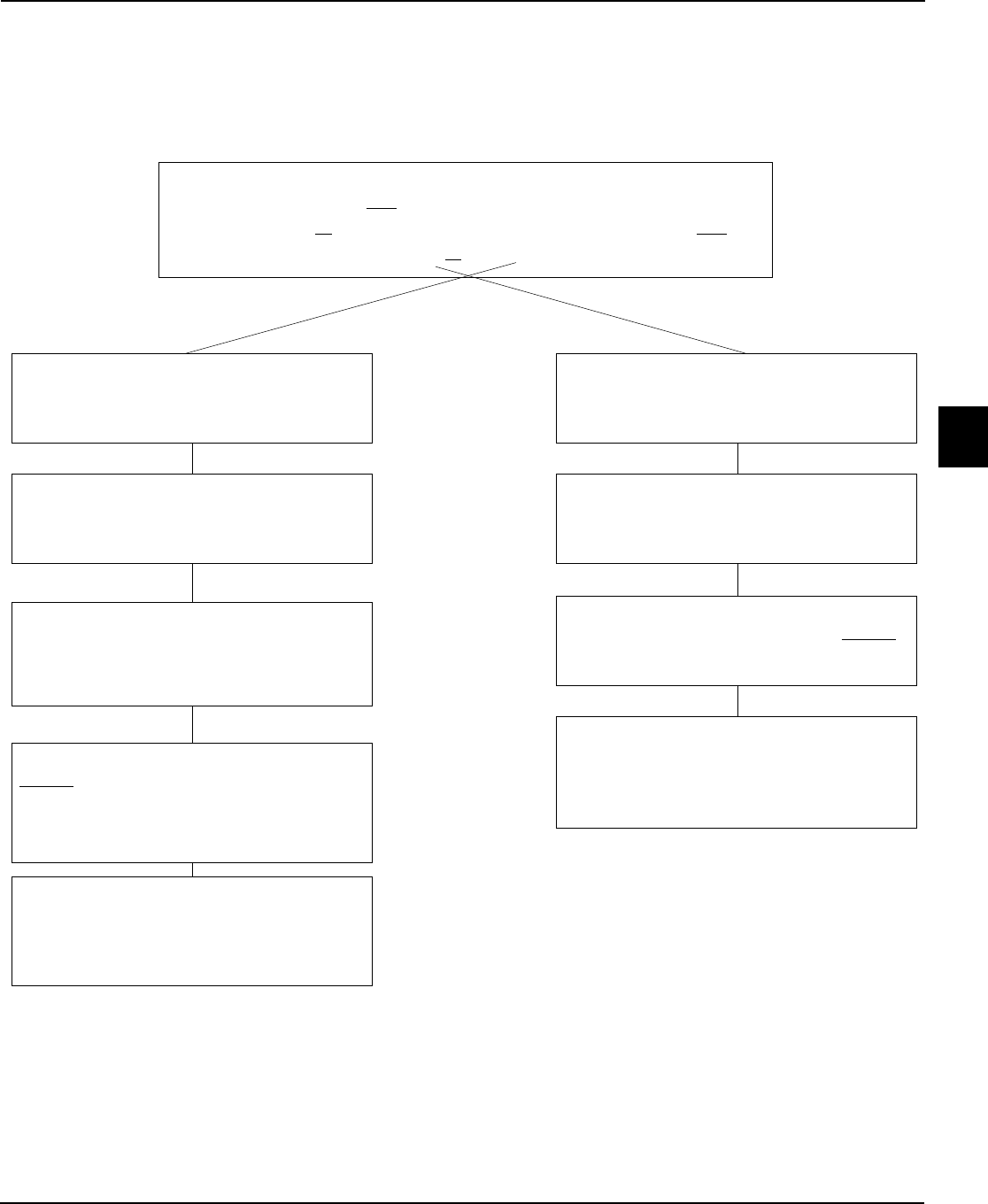
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 9
Law Enforcement
Appendix G
G
Law Enforcement Officer (LEO)*
Involuntary Examination Criteria: Reason to believe person has a mental
illness and because of the mental illness
Person refuses or is unable to determine examination is necessary; and
Likely to suffer from self-neglect or harm to self or others
When initiated by a court's ex parte order or a
professional's certificate
LEO takes person into custody. If under ex parte
order, at any hour of any day and using such
reasonable force as necessary to enter premises
and take person into custody
LEO delivers person with initiating document to
nearest receiving facility (unless Transportation
Exception Plan approved by Board of County
Commissioners and DCF Secretary
LEO completes and provides
transportation report describing
circumstances, then departs facility
CF-MH 3100
LEO takes person into custody and delivers
person, with initiating document to nearest
receiving facility (unless Transportation
Exception Plan approved)
Completes report of law enforcement
officer initiating involuntary examination
CF-MH 3052a
LEO picks up or otherwise
receives the original court order or
professional's certificate
LEO completes and provides
transportation report describing
circumstances, then departs facility
CF-MH 3100
*Law enforcement officers have no legal responsibility
to transport any person for voluntary admission. Once a
person is delivered to any receiving facility or hospital, law
enforcement responsibility under the Baker Act is over. The
nearest receiving facility must accept persons brought by law
enforcement for involuntary examination subject to the Baker
Act. Hospitals, subject to federal EMTALA, must accept persons
brought with emergency medical conditions (including
psychiatric and substance abuse).
When initiated by law enforcement officer

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
Appendix G - 10
G
The Baker Act — A Quick Reference Guide
for Law Enforcement Officers
SHOULD I OR SHOULDN’T I?
e BAKER ACT empowers law enforcement ocers to
initiate an involuntary evaluation of persons based on the
following facts:
ey have a mental illness, and
ey are either a danger to themselves or to others, or
Without treatment they are likely to suer from neglect,
which is potentially harmful.
Sometimes its hard to know whether or not you should
“Baker Act’ someone. You want to be a responsible ocer
and do the right thing to protect individuals and those
nearby, but you’re not sure whether or not to take a person
to jail or to initiate e Baker Act and take the person to a
receiving facility.
ere are three important key points for you to remember:
1. Your role is not to diagnose. However, if you have reason
to believe that someone appears to have a mental illness,
you can decide whether or not that person may be
putting himself/herself or others in danger and meets the
criteria for a complete evaluation.
2. You do not need to witness all of the behaviors personally.
You can consider credible eyewitness accounts from others
as you determine the need for further assessment.
3. Ocers must complete two forms when initiating the
Baker Act: Report of Law Enforcement Ocer Initiating
Involuntary Examination (CF-MH 3052a), and the
Transportation to Receiving Facility (CF-MH 3100).
TRANSPORTATION
You must take persons to the nearest receiving facility unless
they have a medical emergency or a Transportation Exception
Plan has been approved by the Board of Commissioners and
the DCF Secretary. It is very helpful if you call ahead to alert
the facility that you are on the way. e following receiving
facilities are available:
BEHAVIORS TO LOOK FOR
Individuals with mental illnesses who may need further
evaluation typically exhibit a combination of the following
behaviors, characteristics or indicators of their illness:
BEHAVIORS: rapid speech, ight of thought, no eye
contact, quick movements, disconnected speech
patterns, constantly moves or paces, can’t concentrate,
mood changes quickly and frequently from the highs to
the lows, disorganized thoughts, disoriented to time or
place, acts of violence, cutting self, combative / aggressive
behavior, inappropriate dress or nudity.
HALLUCINATIONS: sees people who aren’t there, hears
voices telling them to hurt themselves or others, reports
that the television is suggesting harm to others, turning
the head as if listening to an unseen person.
SELF-CARE ISSUES: insomnia or increased sleep, has not
eaten for days, not taking prescribed medications, home
is in disarray, neglects household, property or personal
hygiene—to the point of putting self/others at risk.
FEELINGS: low self esteem with feelings of hopelessness or
helplessness, at aect—not reacting with much feeling
or interest.
SUICIDAL RISKS: has weapons or access to weapons,
speaks about previous attempts, makes direct comments
about dying or hurting self, evidence of previous
attempts such as scars on the wrists.
ELDERLY ISSUES: wandering at night, leaving things on
stove unattended, not eating or sleeping or caring for
personal needs, unrealistic fears, uncontrollable anxiety,
confusion, quantity and age of unused foods in home.
SUBSTANCE ABUSE: abuse of prescribed medications, use
of alcohol or illegal substances while taking medications.
(If substance abuse appears to be the only issue, the
Marchman Act may be more appropriate.)
NOTE: If you have any doubts, don’t forget to contact
your CIT (Crisis Intervention Team) ocers or one of the
receiving facilities.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix G - 11
Law Enforcement
Appendix G
G
Family Interaction with Law Enforcement
Calling 911
Having to call 911 is an extremely stressful situation. It is by
denition an emergency. Not only do you have concern for
the person about whom you are making the call, but also you
want to make sure that you give law enforcement enough
information so that they will be able to respond eectively
and safely.
Try to control the volume of your voice. When you shout
over the phone it is dicult for the 911 Operator to
understand what you are saying. Certainly this is a very
emotionally charged time, but if the Operator can only
hear shouting, the information is not eciently received.
As calmly and clearly as possible, answer the Operator’s
questions, follow directions you are given, and tell the
Operator the following:
1. Your name and address
2. Name of person with mental illness
3. Your relationship to the person
4. at the person has a mental illness
5. Person’s diagnosis
6. Any medication being used
7. Has medication stopped? How long?
8. Describe what the person is doing now.
9. Do you feel threatened?
10.Is there a history of violent acting out?
11.Does the person hear voices?
12.Does the person have fears?
13.Location of person in house?
14.Are there weapons available? (Try to remove them)
15.Request a Crisis Intervention Trained (CIT) ocer,
if available
When Law Enforcement Arrives
Have all the lights in the house turned on, so that all
occupants can be clearly visible to the arriving ocers. Have
nothing in your hands if you come out of the house to meet
the ocers. Do not run up to the ocers. ey have no
idea who you are and anything you may carry can possibly
be interpreted as a weapon. It is essential that the ocers
responding to your emergency call establish a comfort zone
- knowing who the person is and that you, who possibly
may be also agitated, are not a threat. As calmly as possible,
identify yourself. Tell the ocers:
1. Who you are
2. Who you have called about
3. Your relationship to the person with a mental illness
4. at the person has a mental illness
5. What kind of mental illness it is
6. What medication is being taken
7. Has medication stopped? How long?
8. Is the person violent or delusional (paranoid)?
9. History of suicide attempts?
10.e attending psychiatrist’s or case manager’s names, if
any, and their phone #s
Ocers responding to a 911 emergency call are very focused
when they arrive on the scene. First, they will make the
scene safe for you, the patient, and themselves. e more
informed and at ease the ocers are, the less likelihood that
someone will get injured or that the situation will worsen.
Spend all the time that is necessary answering all of the
ocers’ questions. Answer directly and concisely. Oer any
advice you deem helpful. Do not ramble. Ocers tend to
tune out persons who try to tell their entire life’s story. After
this is done, they will usually be able to deal with you and
to answer any questions. Although it is dicult in times of
crisis, being patient is essential.
* is information was provided courtesy of NAMI California.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Law Enforcement
G
Appendix G - 12

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 1
Emergency Medical Conditions
Appendix H
H
Baker Act and Emergency Medical Conditions
ss. 394.463(2)(g) and (h), F.S.
Introduction
Florida’s Mental Heath Act – the Baker Act – is designed to
assure appropriate, responsive care for persons with acute
mental illness within a system of protections for the individual.
Major violation of federal and state law by hospital sta and
emergency physicians often revolve around the following issues:
Misuse of the Baker Act
Improper Initiation of Baker Act
Documentation of Examination
EMTALA Screening, Stabilization & transfers
Elopements
Rights of Persons
e Baker Act cannot be used to justify the examination
and treatment of non-psychiatric medical conditions or to
conduct diagnostic procedures or laboratory testing without
the express and informed consent of the person or his/her
legally authorized substitute decision-maker. e Baker Act
provides no such authority to provide medical examination
or treatment, other than the required physical examination
within 24 hours following admission to a receiving facility.
Neither can the Baker Act be used to hold a person against
his or her will at a hospital for medical examination or
treatment; it can only be used for initiating psychiatric
examination and psychiatric treatment.
Many persons with serious mental illness rst come to
the attention of law enforcement or emergency medical
personnel due to unusual or frightening behavior. rough
this mechanism, they eventually get to receiving facilities
where they can be examined and treated for their psychiatric
condition.
Conversely, many persons with serious medical problems
display what may appear to be psychiatric symptoms.
ese “mock symptoms” often disappear when the non-
psychiatric medical condition is appropriately diagnosed and
treated. is interrelationship between general medical and
psychiatric care systems is crucial to appropriate care.
A specialized on-line Baker Act course
for personnel responsible for examining or treating
medical conditions of persons held under the Baker Act
can be found at: http://www.bakeracttraining.org
Chapter 65E-5.280(4), F.A.C.
Voluntary Admission
s. 394.4625, F.S. Chapter 65E-5.270
Persons can be held on voluntary status only when they are
willing to be admitted and are making well-reasoned, willful
and knowing decisions about their medical and mental
health care. Otherwise, they must be held under the elevated
protections found in the involuntary provisions of the law.
Criteria for Involuntary Examination
Chapter 394.463(1), F.A.C.
A person may be taken to a receiving facility for involuntary
examination if there is reason to believe that he or she has a
mental illness, as dened in the Baker Act, and because of
his or her mental illness:
e person has refused voluntary examination or is
unable to determine for himself or herself whether
examination is necessary; and
Without care or treatment, the person is likely to suer
from neglect resulting in real and present threat of
substantial harm that can’t be avoided through the help
of others; or
ere is substantial likelihood that without care or
treatment the person will cause serious bodily harm
to himself or herself or others in the near future, as
evidenced by recent behavior.
ere are many clinical denitions of mental illness, but
only one legal denition in the State of Florida. at
denition is:
An impairment of the mental or emotional processes
that exercise conscious control of one’s actions or of
the ability to perceive or understand reality, which
impairment substantially interferes with a person’s
ability to meet the ordinary demands of living,
regardless of etiology. For the purposes of this part,
the term does not include a developmental disability
as dened in chapter 393, intoxication, or conditions
manifested only by antisocial behavior or substance
abuse impairment.
If a person’s symptoms or behavior are due to any form
of substance abuse, developmental disability, or antisocial
behavior, they do not meet the denition of having a mental
illness and cannot be held on involuntary examination
under the Baker Act. However, some people may have a

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
Appendix H - 2
H
serious thought or mood disorder and be intoxicated at the
same time – having co-existing disorders is not uncommon.
In such cases, if the thought or mood disorder is sucient
to warrant an involuntary examination, the substance abuse
condition would not be a barrier.
Initiation of Involuntary Examination
s. 394.463(2), F.S. Chapter 65E-5.280, F.A.C.
An involuntary examination may be initiated by any one of
the three following means:
A court may enter an ex parte order, based upon sworn
testimony, directing a law enforcement ocer to take
the person to the nearest receiving facility.
A law enforcement ocer shall take a person who
appears to meet the above criteria into custody and
deliver the person to the nearest receiving facility.
e ocer must execute a written report detailing
the circumstances under which the person was taken
into custody, and the report must be made part of the
person’s clinical record.
A mental health professional (physician, clinical
psychologist, psychiatric nurse, clinical social worker,
mental health counselor, or marriage and family
therapist – each as dened below) may execute a
certicate stating that he or she has examined a person
within the preceding 48 hours and nds that the
person appears to meet the criteria for involuntary
examination and stating their observations upon which
that conclusion is based.
Only those professionals specically authorized in the
Baker Act may initiate involuntary examinations. Further,
the denitions of each professional in the Baker Act may
dier from that in the licensure laws. When there is conict
between the general licensure laws and the specic Baker
Act law, the Baker Act prevails. ese professionals and
denitions are as follows:
Psychiatrist. A medical practitioner licensed under
chapter 458 or 459 who has primarily diagnosed/
treated mental/nervous disorders for a period of not
less than 3 years, inclusive of psychiatric residency.
Physician. A medical practitioner licensed under
chapter 458 or 459 who has experience in the
diagnosis/treatment of mental and nervous disorders
or a physician employed by a facility operated by the
U.S. Dept of Veterans Aairs which qualies as a
receiving or treatment facility.
Clinical Psychologist. A psychologist as dened in
s. 490.003(7) with 3 years of postdoctoral experience
in the practice of clinical psychology, inclusive of the
experience required for licensure, or a psychologist
employed by a facility operated by the United States
Department of Veterans Aairs that qualies as a
receiving or treatment facility.
Psychiatric Nurse. A registered nurse licensed under
chapter 464 who has a master’s degree or a doctorate in
psychiatric nursing and 2 years of post master’s clinical
experience under the supervision of a physician.
Clinical Social Worker. A person licensed as a clinical
social worker under chapter 491.
Mental Health Counselor. Means a mental health
counselor licensed under chapter 491, F.S.
Marriage and Family erapist. Means a marriage and
family therapist licensed under chapter 491, F.S.
In May 2008 the Florida Attorney General issued an opinion
that Physician Assistants could under some circumstances
initiate an involuntary examination. e opinion did not
authorize any other rights limited to a physician.
Certificate of a Professional
e certicate must:
Be signed within 48 hours of personally examining the
patient leading to the professional’s conclusion that he/
she met the criteria for involuntary examination.
Be initiated by a professional specically authorized in
the Baker Act.
Cite the professional’s observations on which his/her
conclusion is based. ose observations must relate to
the denition of mental illness and the specic criteria
for involuntary examination.
A Certicate of a Professional Initiating an Involuntary
Examination (CF-MH 3052b) is the mandatory form for a
professional authorized under the Baker Act to use. is form
must be complete and legible.
Section I must include a diagnosis consistent with the
denition of mental illness found in the Baker Act.
Section II must include the professional’s own
observations about the behaviors seen or statements
heard supporting the criteria for involuntary
examination. Otherwise, the exam cannot be initiated.
Section III permits the professional to consider other
information relied upon in reaching the conclusion that
may have been provided by credible third parties such as

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 3
Emergency Medical Conditions
Appendix H
H
sta, family, or others. is is only supplemental to the
professional’s own observations found in Section II.
Section IV is only used when having a person taken into
custody for failing to comply with the order of a court
for involuntary outpatient placement.
Section V is only used when the person has left the
premises and law enforcement has been asked to search
for the person and return him/her to a hospital or
receiving facility.
Section VI must be fully completed, identifying the
professional completing the form.
Baker Act Involuntary Examination
ss. 394.463(2)(g) and (h), F.S. Chapter 65E-5.2801, F.A.C
A person for whom an involuntary examination has been
initiated who is being evaluated or treated at a hospital for
an emergency medical condition must be examined at a
receiving facility within 72 hours. e only exception is
when a physician or clinical psychologist aliated with the
hospital conducts the involuntary examination.
A Mandatory Initial Involuntary Examination must be
completed and documented in the patient’s chart. is exam
must include:
A thorough review of any observations of the person’s
recent behavior;
Review of the “Transportation to Receiving Facility”
form (#3100) and
Review one of the following:
» “Ex Parte Order for Involuntary Examination” or
» “Report of Law Enforcement Ocer Initiating
involuntary Examination” or
» “Certicate of Professional Initiating Involuntary
Examination”
Conduct brief psychiatric history; and
Conduct face-to-face examination in a timely manner
to determine if person meets criteria for release.
A person held under involuntary examination status must
have the Mandatory Initial Involuntary Examination
conducted by a physician or clinical psychologist by one of
the following methods:
1. A physician or psychologist employed at the emergency
department can conduct the examination and if found
not to meet the criteria for involuntary inpatient/
outpatient placement, the person may be released or
accept voluntary placement. (Form CF-MH 3101), or
2. e hospital must notify within two hours of medical
stabilization a designated Baker Act receiving facility to
perform the involuntary examination of the person (form
CF-MH 3102). e law does not specify the nearest
facility.
If the person hasn’t already been released from the ED by a
physician or psychologist, one of the following must occur
within 12 hours of the determination of medical stability:
e person must be examined by a designated receiving
facility and released; or
e patient must be transferred to a designated receiving
facility in which appropriate medical treatment is
available.
In any case, any transfer from a hospital emergency
department of a person with a psychiatric or substance abuse
emergency must comply with all requirements of the federal
EMTALA law.
Emergency Medical Conditions (EMC)
ss. 394.463(2)(g) and (h), F.S. Chapter 65E-5.280(4), F.A.C.
If a law enforcement ocer transporting a person for
involuntary examination initiated by a court, by an
authorized mental health professional, or by law enforcement
believes that the person has an emergency medical condition,
the person may rst be transported to a hospital for
emergency medical treatment, regardless of whether the
hospital is a designated Baker Act receiving facility.
An emergency medical condition is dened in the law as a
medical condition manifesting itself by acute symptoms of
sucient severity, which may include severe pain, such that
the absence of immediate medical attention could reasonably
be expected to result in any one of the following:
Serious jeopardy to patient health
Serious impairment to bodily functions
Serious dysfunction of any bodily organ or part
e emergency medical condition should be addressed in
accordance with existing hospital policy without regard to
the initiation of the involuntary examination. e Baker
Act should never be used to authorize medical examination/
treatment or to detain a person wishing to leave a hospital
unless the person is held for psychiatric examination/
psychiatric treatment and also meets the criteria under the
Baker Act.
If a person on involuntary examination status has been taken
to a hospital for the evaluation or treatment of an emergency
medical condition, the 72-hour examination period begins

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
Appendix H - 4
H
when the person arrives at the hospital and is suspended
when the attending physician documents that the person has
an emergency medical condition. e 72-hour clock resumes
again upon the determination by a physician that the person’s
medical condition has stabilized or that an emergency
medical condition does not exist.
Duties of all Hospitals
Persons held under the Baker Act, whether at a designated
receiving facility or at a hospital where they may be
undergoing evaluation or treatment of an emergency medical
condition, must have their rights upheld.
Florida’s hospital licensure law places certain responsibilities on
all hospitals, not just those designated as Baker Act receiving
facilities. Some of these responsibilities are as follows:
395.003(5)(a) Adherence to patient rights, standards
of care, and examination and placement procedures
provided under Baker Act shall be a condition of
licensure for hospitals providing voluntary or involuntary
medical or psychiatric observation, evaluation, diagnosis,
or treatment.
395.1041(6) Rights of persons being treated.--A hospital
providing emergency services and care to a person who
is being involuntarily examined under the provisions of
s. 394.463 shall adhere to the rights of patients specied
in the Baker Act and the involuntary examination
procedures, regardless of whether the hospital, or any
part thereof, is designated as a receiving or treatment
facility and regardless of whether the person is admitted
to the hospital.
395.1055(5) AHCA shall enforce Baker Act law and
rules, with respect to the rights, standards of care,
and examination-placement procedures voluntarily or
involuntarily admitted to hospitals providing psychiatric
observation, evaluation, diagnosis, or treatment.
395.1065(4) In seeking to impose penalties against a
facility for a violation of Baker Act, AHCA is authorized
to rely on the investigation/ndings by the Department
of Health in lieu of conducting its own investigation.
395.3025 Patient and personnel records; copies;
examination. is section does not apply to records
maintained at any licensed facility the primary function
of which is to provide psychiatric care to its patients,
or to records of treatment for any mental or emotional
condition at any other licensed facility which are
governed by the provisions of s. 394.4615. is section
does not apply to records of substance abuse impaired
persons, which are governed by s. 397.501.
EMTALA and the Baker Act
Emergency Medical Treatment
and Active Labor Act
42 CFR 489.24
All public, for prot, or non-prot hospitals that oer
services for medical, psychiatric or substance abuse emergency
conditions are obligated to comply with all of EMTALA
requirements is includes freestanding psychiatric hospitals
that serve persons with emergency psychiatric conditions.
All licensed hospitals are required to comply with the Florida
law governing hospital licensure [s. 395.1041, F.S]. Conversely,
a facility that is not licensed as a hospital, such as a Crisis
Stabilization Unit (CSU), nursing home, assisted living facility,
outpatient clinic, or physician oce is not required to comply
with EMTALA or the hospital licensing law.
EMTALA applies to all transfers of persons from and to
hospitals of persons with emergency medical conditions;
which by federal denition includes psychiatric and substance
abuse emergencies. An involuntary examination under Baker
Act or protective custody under the Marchman Act would
constitute such emergencies.
EMTALA discourages lateral transfers between hospitals,
much less downward substitution of care for persons with
emergency medical conditions. However, it defers to state
and local plans to do so in some cases such as when CSU and
detox facilities are established and funded by the state solely
for persons unable to pay for care.
Once the person’s emergency medical condition has been
stabilized (dened as unlikely to experience a deterioration
in condition during or as a result of the transfer) and other
required conditions for an appropriate transfer have been
met, the person can be transferred to a facility that has the
capability and capacity to manage the person’s condition and
has agreed to accept the person, based on the prior review
of medical records. If the transferring hospital has licensed
psychiatric capability, it must have the consent of the patient
or legal representative; if it doesn’t have psychiatric capacity or
capability, a physician can certify the benets of the transfer
outweigh the risks. No delay or denial of emergency care due
to inability to pay can take place by either the transferring
facility or the facility to which a request for transfer is made.
When the federal EMTALA law is in conict with the state’s
Baker Act law, EMTALA takes precedence. When no conict
exists, hospitals must follow both.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 5
Emergency Medical Conditions
Appendix H
H
Medical & Psychiatric Screening
Generally, any hospital’s medical screening is a triage process
that places highest priority upon identifying and responding
to acute or volatile life-threatening situations such as
overdoses or metabolic toxicity.
A medical screening may be conducted by qualied medical
personnel authorized by the hospital’s policies and procedures
and in accordance with EMTALA. A Baker Act receiving
facility cannot require an emergency department to conduct
certain laboratory or diagnostic tests on a person under
the Baker Act prior to accepting the person. However, if a
receiving facility believes that a person’s emergency medical
condition has not been stabilized or the emergency medical
condition continues to exist, it can refuse the requested
transfer. A free-standing psychiatric facility is prohibited by
law from admitting any person if it doesn’t have appropriate
medical treatment available. is may require CSU sta to
determine in advance if the person requires services beyond
its medical capability. Recurring transfer problems should be
documented and reported to DCF circuits which contract for
Baker Act services.
All medically required tests should be requested at one
time (not sequentially) so that the transfer for psychiatric
examination is not delayed.
An emergency department of a non-receiving facility is not
required by the Baker Act to provide a psychiatric consult
prior to the transfer of a person to a receiving facility. e
Baker Act law and rule do not require that the ED provide
a psychiatrist to evaluate the person’s condition — that
occurs upon arrival at the receiving facility. Requiring a
psychiatric examination in an emergency department prior to
transferring a person to a receiving facility is generally a waste
of resources, duplicative, and creates unnecessarily delays.
e ED physician is permitted to perform the exam and, if
the person doesn’t meet the criteria for involuntary inpatient
or outpatient placement, can directly release the person or
convert a competent person to voluntary status. is assumes
that the hospital doesn’t have a higher standard that requires
evaluation by a psychiatrist.
Further, the Joint Commission on Accreditation of Health
Care Organizations (JCAHO) and the federal Center
for Medicare & Medicaid Services (CMS) Conditions of
Participation govern chemical restraints and mechanical
restraints for medical and behavioral purposes. If those
requirements are more stringent than those in the Baker Act,
they must be followed instead.
Where life threatening medical conditions may be present
and a person cannot provide informed consent, there is a
presumption of consent, absent a Do Not Resuscitate Order
(DNR). In those circumstances, emergency sta should
always attempt to obtain consent from another legally
authorized decision-maker whenever possible. ese may
include:
Substitute decision-makers such as guardians appointed
by the court or health care surrogates/proxies when a
physician determines the person lacks capacity to provide
consent.
Contact DCF to report suspected self-neglect (Chapter
415, F.S.)
Petition the court for Expedited Judicial Intervention
Concerning Medical Treatment Procedures (Rule 5.900)
For those individuals whose emergency medical conditions,
including those of a psychiatric and substance abuse nature,
have been resolved the physician has several options:
1. Discharge home with follow-up instructions. An
individual is considered stable and ready for discharge
when, within reasonable clinical condence, it is
determined that the individual has reached the point
where his/her continued care, including diagnostic work-
up and/or treatment, could be reasonably performed
as an outpatient or later as an inpatient, provided the
individual is given a plan for appropriate follow-up care as
part of the discharge instructions. e EMC that caused
the individual to present to the ED must be resolved, but
the underlying medical condition may persist. Hospitals
are expected within reason to assist/provide discharged
individuals the necessary information to secure the
necessary follow-up care to prevent relapse or worsening
of the medical condition upon release from the hospital;
or
2. Inpatient admission for continued care; or
3. Transfer, if all requirements of federal and state law are met.
Medical Clearance
A Baker Act receiving facility cannot require medical
clearance as a condition for acceptance when brought by a law
enforcement ocer. e Baker Act is clear that “e nearest
receiving facility must accept any person brought by law
enforcement ocers for involuntary examination.” ere is no
exception to this — not even medical emergencies. Once the
ocer arrives at a receiving facility, the sta can call 911 to get
an ambulance if they believe the person has an acute medical
condition requiring emergency examination or treatment. e
person should never be put back in a cruiser for the ocer to

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
Appendix H - 6
H
further transport in such a circumstance. e person should
instead be referred by the CSU to the nearest ER via medically
equipped and trained personnel, regardless of whether the
hospital has psychiatric capability.
It is not appropriate for a receiving facility or a CSU to
routinely utilize emergency departments to require “medical
clearance” or to refer all intoxicated persons for blood levels
unless an emergency medical condition is suspected.
A nursing assessment is required at a CSU and, if conditions
are noted which suggest the need for acute medical
treatment; the CSU would be required to refer the person
to a hospital. ese might include cases where there is
reason to believe the person has ingested a toxic substance, is
experiencing severe pain, has suered a severe injury, or is in
an acute medical crisis. e CSU would call 911 requesting
emergency medical services and begin any interventions
appropriate until EMS arrived.
However, once the person has been taken to a hospital that
is not designated as a receiving facility for evaluation or
treatment of an emergency medical condition, the person
must be transferred to a designated receiving facility at
which appropriate medical treatment is available within
12 hours of a physician determining the person’s medical
condition has stabilized or that an emergency medical
condition does not exist.
e federal EMTALA law (but not the state’s Baker Act)
may require a second medical clearance closer to the time of
transfer. Stabilization for transfer is determined at the time of
transfer – not at some earlier period.
If a CSU routinely requires an emergency department
to “medical clear” persons before acceptance, such
practice should be documented and reported to DCF for
investigation.
Baker Act Exam/Release
Many emergency department personnel use a phrase such
as “rescinding,” “lifting,” “abrogating,” or “overturning”
the Baker Act. is is incorrect in that once a Baker Act
involuntary examination is initiated by any one of the three
authorized methods, all components of the initial mandatory
involuntary examination must be conducted by a physician
or clinical psychologist.
Upon a determination by any physician or clinical
psychologist that any one of the criteria for involuntary
inpatient and outpatient placement doesn’t exist, the person
may be released, or if competent to provide express and
informed consent, become voluntary.
Some ED physicians are willing to initiate an involuntary
examination but refuse to conduct the exam and to authorize
release of persons from the Baker Act, resulting in hospitals
having to admit persons pending transfer. ese physicians
often believe that only a psychiatrist can release a person from
involuntary status. e law is explicit that a non-psychiatric
physician is authorized at a non-receiving facility to perform
the examination and to authorize the direct release of the
person after documenting the person doesn’t meet the criteria
for involuntary placement. A psychiatrist is not required
to perform the examination or to approve the release from
emergency departments.
If the hospital is designated as a receiving facility, the person’s
release from involuntary status must have the documented
approval of a psychiatrist, a clinical psychologist or, an
attending emergency department physician.
Transfers
All hospitals, even those licensed as free-standing psychiatric
hospitals are subject to EMTALA. EMTALA is based on
the belief that transfers of people with emergency medical
conditions are inherently dangerous and discourages them
unless certain criteria are met. ese include:
Conducting the medical screening within the capability
and capacity of the hospital to perform,
Stabilization,
Agreement of the person or his/her legal representative
to the transfer,
Sharing of all relevant medical records with the
destination hospital,
Approval of transfer by the destination hospital, and
Arranging safe/appropriate means of transportation.
Only then can the payment source (or lack of payment) be
considered. Transfer of a person who refuses consent can only
be performed when the sending hospital doesn’t have the
capability or capacity to meet the person’s needs.
EMTALA requires any hospital that goes over licensed or
stang capacity for any person must do so for indigent
persons as well. It cannot make such accommodations just
for paying persons. However, if the hospital never goes over
census for any person, it is not required to go over census for
an indigent person.
e capacity to render care is not reected simply by
the number of persons occupying a specialized unit, the
number of sta on duty, or the amount of equipment
on the hospital’s premises. Capacity includes whatever

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 7
Emergency Medical Conditions
Appendix H
H
a hospital customarily does to accommodate patients in
excess of its occupancy limits. If a hospital has customarily
accommodated patients in excess of its occupancy limits by
whatever means (e.g., moving patients to other units, calling
in additional sta, borrowing equipment from other facilities)
it has, in fact, demonstrated the ability to provide services to
patients in excess of its occupancy limits.
ere is some possible risk of an EMTALA violation by
selectively picking an indigent person for the transfer over
a paying person, but EMTALA does recognize state/local
plans for serving such persons. e only reason for the State
of Florida to have established and funded CSU’s is to serve
persons who don’t have the ability to pay for private care.
Uninsured persons served by a facility may be informed,
after the facility has met its EMTALA obligations, that they
will receive a bill for the full cost of care they receive at the
hospital. Most persons will agree to a transfer if it means they
will not get a bill or that the bill will be based on their ability
to pay.
Transfers from any licensed hospitals must rst meet all
requirements of the federal EMTALA law. Once those
federal requirements are met, the requirements of the state’s
Baker Act apply when the transfer is between designated
receiving facilities. e Baker Act [s.394.4685, F.S.] provides
conditions for:
» Transfers Between Public Facilities
» Transfers From Public To Private Facilities
» Transfers From Private To Public Facilities
» Transfers Between Private Facilities
If an emergency physician doesn’t conduct the exam and
release the person, it is the responsibility of the ED to
contact a designated receiving facility within 2 hours after
the person’s emergency medical condition has been stabilized
or determined not to exist. It is the receiving facility’s
responsibility to either accept transfer of the person when
it has capacity and appropriate medical treatment available
or to have its physician or clinical psychologist conduct the
initial mandatory examination and release the person or
transfer to voluntary status, if competent.
e federal EMTALA regulations and the Baker Act
require the sending hospital to arrange safe and appropriate
transportation of the person to the receiving facility, unless
other appropriate transportation arrangements can be made.
If one receiving facility refuses to accept the transfer, another
receiving facility should be contacted or the person should be
retained at the hospital in which the emergency department
is located until resolution is reached.
ere is no requirement that the person be transferred to the
nearest receiving facility. Obviously, if the nearest receiving
facility can meet the person’s clinical needs and it has the
capacity to accept the person, this is the ideal situation.
However, if the nearest facility doesn’t have either the
capacity (space), or capability (psychiatric unit), the person
should be transferred to the next closest receiving facility that
does have the capability and capacity.
Transfer diculties are most frequently reported over weekends.
is is often attributed to on-call physicians at receiving
facilities providing coverage for attending psychiatrists over
the weekend, but who may be unwilling to discharge another
doctor’s patient. Lack of discharge planners on weekends in
some receiving facilities also contributes to this problem.
e Baker Act doesn’t provide a remedy to the problem of
what happens when no Baker Act receiving facility can be
located for a person on involuntary status within the 12 hour
time frame permitted for transfer. e hospital should start
referring immediately upon the person’s medical clearance
and document each contact with the date, time, location,
person talked to, and his/her response. If it appears the
person won’t be transferred within the permitted 12 hour
period, from a non-designated hospital, DCF/Mental Health
Program sta should be contacted at the rst possible time
to report it. What cannot be done is to re-initiate another
involuntary initiation (Certicate of a Professional) on top
of the rst one. Neither should a person be released who still
meets the criteria for involuntary placement. However, an
emergency department physician may conduct the exam and
if the person doesn’t meet the involuntary placement criteria,
the examination and ndings can be documented in the
chart and the person can be either released or, if competent,
converted to voluntary status. (See form 3101.)
If a hospital subject to EMTALA routinely refuses to
accept transfers, a report to the Agency for Health Care
Administration may be appropriate if the refusal was based
on the nancial status of the person. If the receiving facility is
licensed under Chapter 394, F.S. (CSU), a complaint may be
directed to the circuit oce of DCF (funding source).
A hospital’s delay or denial of a request for a transfer based
on inability to pay may result in an EMTALA violation for
“reverse dumping.” Even the Florida law governing “Access
to Emergency Services and Care” [395.1041(3) (e) & (h),
FS] governs where a transfer can be made and prohibits
conditioning such acceptance on an individual’s ability to pay
as follows:
(e) Except as otherwise provided by law, all medically
necessary transfers shall be made to the geographically

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
Appendix H - 8
H
closest hospital with the service capability unless
another prior arrangement is in place or the
geographically closest hospital is at service capacity.
When the condition of a medically necessary transferred
patient improves so that the service capability of the
receiving hospital is no longer required, the receiving
hospital may transfer the patient back to the transferring
hospital and the transferring hospital shall receive the
patient within its service capability.
(h) A hospital may request and collect insurance
information and other nancial information from a
patient, in accordance with federal law, if emergency
services and care are not delayed. No hospital to which
another hospital is transferring a person in need of
emergency services and care may require the transferring
hospital or any person or entity to guarantee payment
for the person as a condition of receiving the transfer.
In addition, a hospital may not require any contractual
agreement, any type of preplanned transfer agreement,
or any other arrangement to be made prior to or at the
time of transfer as a condition of receiving an individual
patient being transferred.
CSU’s
Crisis stabilization units exist to serve indigent persons. e
benets derived by CSU’s from their tax exempt status and
the state/county appropriated funds place a responsibility on
them to coordinate care for persons with acute psychiatric
conditions. In exchange for receipt of public funding, the
Florida Administrative Code [chapter 65E-5.351(5) F.A.C.]
requires that a public receiving facility that is aliated with a
publicly funded community mental health center ensure the
centralized provision and coordination of acute care services
for eligible individuals with an acute mental illness. A public
receiving facility should take the leadership in solving local
transfer problems.
Statutorily, CSU’s serving adults are limited in size to a
maximum of 30 beds; those serving minors are limited to 20
beds. e law prevents CSU’s from exceeding their licensed
capacity by more than ten percent, nor may they exceed their
licensed capacity for more than three consecutive working
days or for more than seven days in a month. Exceeding
these limits would subject persons to a potentially dangerous
environment and the CSU to loss of license.
DCF contracts, to the extent of its appropriations, with CSUs
for indigent persons (up to 20% of the persons served by
a CSU’s may be nancially ineligible under federal poverty
guidelines). Due to limited funds, a CSU may still have beds
available for purchase from other funders, including managed
care organizations. However, if a persistent problem occurs in
accessing care for indigent persons, a report should be made to
the DCF region oce or the managing entity.
DCF and AHCA can check on the actual census of each
publicly funded CSU in the circuit to determine how many
persons were admitted, what percentage were nancially
eligible, and the average length of stay. If the ALOS exceeds
the statewide ALOS, it reduces the number of persons
who can be stabilized in the funded/licensed beds. DCF
can also check on the CSU policies for accepting transfers,
specically whether they accept up to the licensed or funded
capacity and what priority is placed on whether the transfer is
initiated from designated or non-designated facilities.
Law Enforcement
A law enforcement ocer’s duty is over once he/she has
presented the person and the required paperwork to
responsible sta at the ED where the person has been
taken for evaluation or treatment of an emergency medical
condition.
Law enforcement ocers should provide a copy of the
involuntary examination initiation form (court order, law
enforcement ocer’s report or mental health professional’s
certicate) and the required transportation form (3100 form)
at the time of arrival.
Law enforcement should not be expected to stay with the
person while awaiting medical screening or transfer unless the
person has criminal charges. e safety of the person while at
the hospital is the responsibility of hospital personnel.
Law enforcement agencies are under no obligation to further
transport the person after medical clearance. at is the duty
of the hospital under EMTALA.
It is not acceptable for a hospital to return the person to law
enforcement personnel for transfer to a designated receiving
facility. e transferring hospital is responsible for arranging
a safe and appropriate method to transport a person to a
receiving facility, as required by EMTALA, regardless of
whether the receiving facility is nearby or in a remote location.
Safety/Stabilization
While persons on Baker Act involuntary examination status are
in the emergency department awaiting medical screening or
transfer, it is the hospital’s responsibility to ensure their safety.
Safety can be arranged in many ways. Some hospitals use
one-on-one sitters or a single sitter in the doorway of a room
that has multiple persons awaiting transfer to receiving
facilities. It is important that sitters be trained as to their

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 9
Emergency Medical Conditions
Appendix H
H
responsibilities should the person try to leave the room.
Other hospitals place these persons in a room at the back of
the ED, farthest away from any exit doors. Some hospitals
provide gowns and paper slippers instead of street clothing.
Some facilities use video monitoring to reduce elopements.
In any case, the ideal is to expedite the person’s transfer and,
if the volume is sucient, a speciality psychiatric ED in part
of the existing ED may be appropriate. is would provide
secure space and specially trained sta.
However, if a person does elope from a hospital, sta may
want to be consider the following:
Voluntary not meeting criteria for involuntary
placement, law enforcement not notied by the facility.
Voluntary but meets criteria for involuntary placement,
3052b initiated and law enforcement requested to take
person into custody and deliver to nearest receiving
facility. Transfer of person, if appropriate, will be
arranged from facility-to-facility.
Involuntary examination status, within 72 hours
of arrival at facility, meets criteria for involuntary
placement, but prior to Petition for Involuntary
Placement being led with court. Law enforcement
given 3052 (a or b) or order and requested to take
person into custody and deliver to nearest receiving
facility. Transfer of person, if appropriate, then arranged
from facility-to-facility.
Petition for Involuntary Placement led with court,
law enforcement provided copy of petition (3032) and
requested to return person to the facility from which the
petition was led.
Under court’s Order for Involuntary Placement
(3008) and leaves facility without authorization,
administrator authorizes search and the return of person.
Administrator of facility may request law enforcement to
search for and return person and provide copy of order
(3008).
If the elopement is from an emergency department, the
person should be returned to the emergency department
by law enforcement for appropriate transfer required by
EMTALA.
If a person is locked up for behavioral reasons in a room of
the ED, this would be considered seclusion under the federal
Conditions of Participation. However, if the person has been
identied as meeting the criteria for involuntary examination
under the Baker Act and documentation exists that the person
is at imminent risk of danger from assault, suicide, elopement,
etc., seclusion or restraint can generally be justied if no less
restrictive alternative is appropriate and eective.
ere is no requirement that a CSU that refers a person to
a hospital remain with a referred person, once a responsible
hand-o of the person is performed. Once the person is
presented, federal EMTALA requirements that apply to
a hospital must be followed. is places responsibility on
the hospital sta to be sure the person is stabilized, which
may include safely retaining him/her at the ED until an
appropriate transfer back to the CSU or other receiving
facility can be arranged, along with the other EMTALA
requirements for an appropriate transfer.
Persons with psychiatric diagnoses are considered stable when
they are protected and prevented from injuring or harming
him/herself or others.
Informed Consent for Transfer
A hospital ED can transfer a person under involuntary
provisions of the Baker Act to a receiving facility without the
person’s consent only if the sending hospital doesn’t have the
capability or capacity to meet the person’s needs. is means
that if the hospital is part of a designated receiving facility,
it generally cannot transfer a person without the person’s
consent (or that of his/her representative). If the hospital is
not licensed for psychiatric services, a physician can generally
certify that the benets of the transfer outweigh the risks.
Florida’s hospital licensing law [s.395.1041, F.S]. and the
federal EMTALA law permit transfers of persons who have
come to a hospital as a result of an emergency medical
condition, only when one of the following has occurred:
(a) When the person, or a person who is legally responsible
for the person and acting on the person’s behalf, after being
informed of the hospital’s obligation pursuant to section
395.1041, F.S. and the risk of transfer, requests that the
transfer be eected; or
(b) If a physician or other qualied medical personnel,
certies that the benets to the condition of the person
outweigh the risks associated with the transfer.
It is not appropriate to simply note that a transfer is being
done because the person was “Baker Acted.” Initiation of an
involuntary examination doesn’t deprive people of any right
assured under federal or state law – the person actually has
enhanced rights under the law.
Funding
e Florida Agency for Health Care Administration has
determined that when a transfer from an emergency
department to a designated receiving facility must take place
and all other EMTALA requirements have been met, the

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
Appendix H - 10
H
transfer destination may be decided based on the person’s
paying status. Given that the person must be transferred
anyway from the non-designated hospital to a designated
receiving facility, as long as an appropriate transfer is initiated
pursuant to state (s.395.1041, F.S.) and federal EMTALA
law, then the person may be transferred to the nearest private
receiving facility that takes the person’s insurance.
Once a person’s emergency medical condition has been
stabilized, hospital personnel can inquire about the person’s
insurance even if the hospital has not psychiatrically screened
or examined the person’s psychiatric condition. Hospital
personnel can inquire as to a person’s ability to pay as long
as the inquiry does not in any way delay the provision of
emergency services and care being provided to the person.
After the determination of the person’s insurance status has
been made, it is appropriate to transfer the paying persons
to the nearest private receiving facility (even if it bypasses
a closer public receiving facility) and indigent persons to
the nearest public receiving facility (even if other private
receiving facilities are closer) for psychiatric screening,
examination and placement.
Just as an emergency department can’t refuse or delay
acceptance of a person based on inability to pay, a destination
hospital can’t refuse or delay a requested transfer of an
indigent person if it has the capability and capacity to
manage the person’s care and the sending hospital does
not. Refusal of a transfer under such circumstances would
constitute “reverse dumping” under EMTALA.
A sending hospital, after meeting all other EMTALA transfer
requirements, can consider the payment status of the person in
determining which facility the person will be sent – hopefully
avoiding yet another transfer for the person. e sending
hospital can consider state/local plans for how certain special
populations are served – thus allowing a lateral or even a
downward substitution of care if in accord with the plan.
However, EMTALA would not allow a destination hospital
to refuse to accept a transfer for nancial reasons or require
pre-certication of insurance or sending of a face sheet with
insurance information as a condition of acceptance.
However, if a non-designated hospital makes an error in
determining whether or not a person has insurance, a
hospital-based receiving facility can’t refuse the person due
to the person’s insurance status. Once contact is made with
a designated receiving facility, whether public or private,
by an initiating facility, if that hospital has the capability
and capacity to care for the person, the receiving hospital
is required to accept the person under state (s.395.1041,
F.S.) and federal EMTALA regulations. A private receiving
facility may transfer a person (pursuant to the transfer
requirements contained in s. 394.4685, F.S., s.395.1041, F.S.
and the EMTALA regulations) to a public receiving facility
for further treatment after the person has been screened and
stabilized.
Summary
Hospital emergency departments will always play a vital
role in the continuity of care for persons with acute mental
illnesses. Because of the overlap between the federal
EMTALA law and the state Baker Act law, it is critical that
hospitals meet their obligations. However, it is just as critical
that persons under Baker Act involuntary examination status
be transferred as quickly as possible to designated receiving
facilities to get the psychiatric examination and treatment
they need.
A specialized on-line Baker Act course can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.
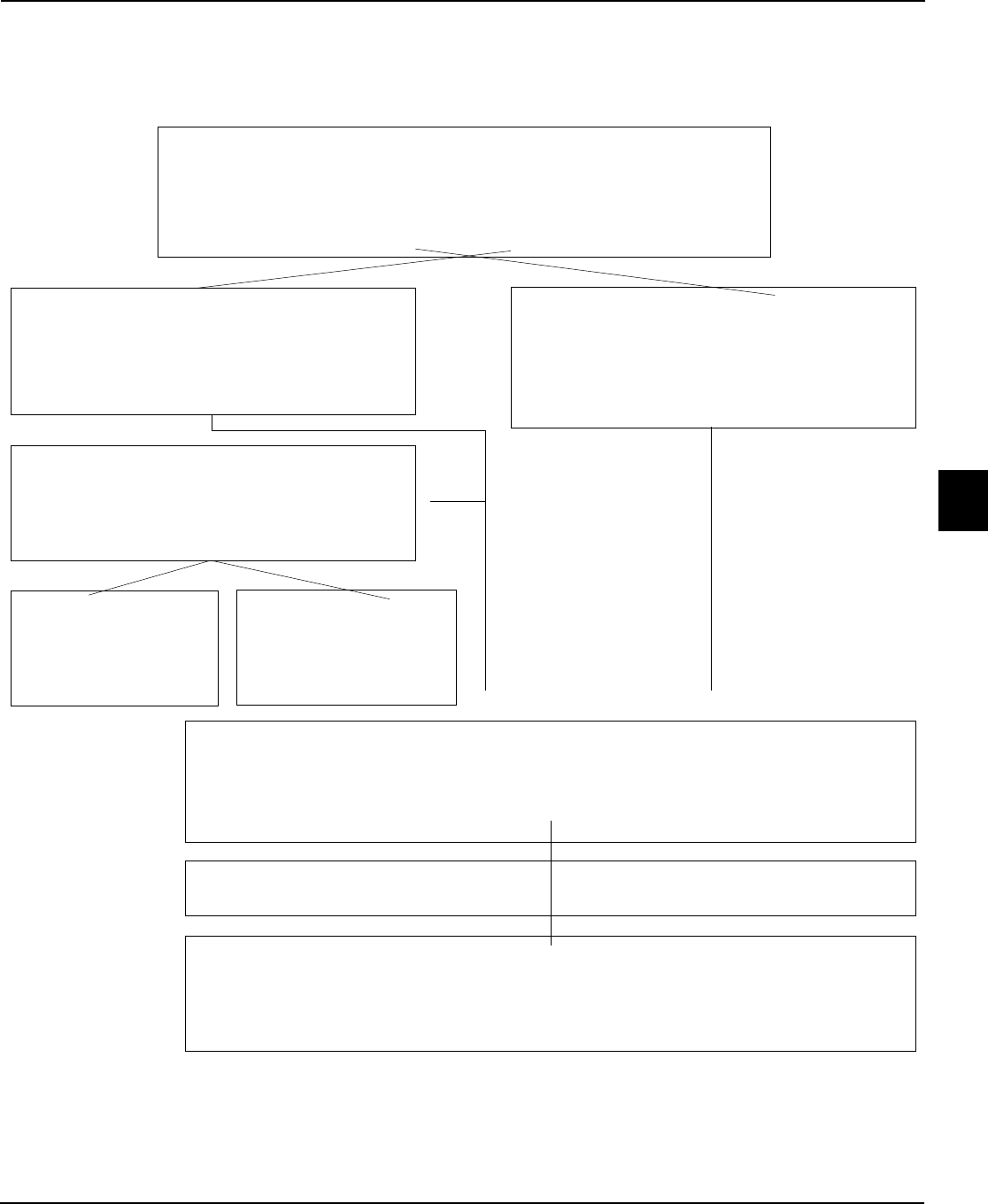
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix H - 11
Emergency Medical Conditions
Appendix H
H
Criteria: Reason to believe person has a mental illness (excludes
substance abuse, developmental disability and anti-social behavior) and
because of the mental illness
Person refuses or is unable to determine examination is necessary; and
Likely to suffer from self-neglect or harm self or others
Hospital physician or other authorized
professional may initiate an involuntary
examination if all the above criteria are met
Law enforcement may take person to any
hospital if an emergency medical condition is
believed to exist. Law enforcement may request
assistance from emergency medical personnel
if needed for safety of the officer or person in
custody
May be examined at hospital by clinical
psychologist or a licensed physician
If person does meet all
criteria for involuntary
placement, person
transferred to receiving
facility
If person does not meet
all criteria for involuntary
placement, person may be
released or offered voluntary
placement
*Transportation from a hospital to a receiving facility or between receiving facilities is the
responsibility of the referring facility unless other methods of transportation have been arranged
Emergency Medical Treatment of Persons
for Whom Involuntary Examination has been or will be Initiated
q
q
If not examined by authorized hospital personnel and released, person must be examined by
a receiving facility within 72 hours (clock starts when person arrives and stops when physician
documents the person has an emergency condition and begins again when physician
documents that the medical condition has stabilized or that an emergency medical condition
does not exist)
Within 12 hours after person has been medically cleared, the receiving facility must:
Examine and release the person from the hospital; or
Accept transfer of the person to a receiving facility in which appropriate medical
treatment is available
Within 2 hours after person has been medically cleared, the hospital must notify a
receiving facility of requested transfer
q

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Medical Conditions
H
Appendix H - 12

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 1 Emergency Treatment
Appendix I
I
Orders for Emergency Treatment
Including Restraints and Seclusion
s. 394.459(4), F.S. Chapter 65E-5.1703, F.A.C.
42 U.S.C. 1301 and 1395hh, Subpart B Administration Sec. 482.13 (e)
Cautionary Note:
Many statutes, federal/state regulations, accreditation standards, and even an organization’s own policies/procedures govern how
restraints and seclusion can be used. Facility staff must use the most stringent of these requirements that apply to persons served in
their facility, whether it be Hospital Conditions of Participation (as per Federal Code – 42 C.F.R. 482.1-482.66), The Joint Commission, or
the Commission on Accreditation of Rehabilitation Facilities (CARF). Administrative Code 65E-5.100 was revised in April 2013 to delete
definitions that were redundant with the Florida Statutes.
In 2007 the the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) was renamed The Joint Commission.
Introduction
394.453 and 394.457(5), F.S.]
e Florida Legislative expression of its intent for the Baker
Act includes the following provision:
It is the policy of this state that the use of restraint and
seclusion on clients is justied only as an emergency
safety measure to be used in response to imminent
danger to the client or others. It is, therefore, the intent
of the Legislature to achieve an ongoing reduction
in the use of restraint and seclusion in programs and
facilities serving persons with mental illness.
e Legislature requires the Department of Children and
Families to develop rules implementing all aspects of the
Baker Act, including provisions governing restraint and
seclusion, as follows:
1. Rules establishing forms and procedures relating to the
rights and privileges of patients seeking mental health
treatment from facilities.
2. A program subject to the Baker Act shall not be
permitted to operate unless rules designed to ensure
the protection of the health, safety, and welfare of
the patients treated through such program have been
adopted. Rules adopted must include provisions
governing the use of restraint and seclusion which
are consistent with recognized best practices and
professional judgment; prohibit inherently dangerous
restraint or seclusion procedures; establish limitations on
the use and duration of restraint and seclusion; establish
measures to ensure the safety of program participants
and sta during an incident of restraint or seclusion;
establish procedures for sta to follow before, during,
and after incidents of restraint or seclusion; establish
professional qualications of and training for sta
who may order or be engaged in the use of restraint
or seclusion; and establish mandatory reporting, data
collection, and data dissemination procedures and
requirements. Rules adopted under this subsection
must require that each instance of the use of restraint or
seclusion be documented in the record of the patient.
In addition to state requirements, the federal Center for
Medicare and Medicaid Services (CMS) issued Conditions
of Participation for hospitals participating in Medicare
and Medicaid programs due to the danger posed to health
and safety by violations of basic rights of persons, such as
freedom from inappropriate use of restraints and seclusion.
ese requirements are found in 42 CFR Part 482.13(e).
CMS has issued interpretive guidelines implementing the
regulations. e material included in this Handbook is accurate
as of its printing date. e reader needs to consider the
federal standards as the basis for determining how its own
policies and procedures will meet new emerging community
standards of care for the use of restraints and seclusion, as
a supplement to the requirements of Florida Statutes and
Administrative Code.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 2
I
General Management
of the Treatment Environment
[65E-5.1601, F.A.C.]
e Florida Administrative Code establishes minimum
standards for general management of the services in which
individuals admitted to or served in facilities under the Baker
Act must meet. ese included:
Management and personnel of the facility’s treatment
environment must use positive incentives in assisting
persons to acquire and maintain socially positive
behaviors as determined by the person’s age and
developmental level.
Interventions such as the loss of personal freedoms,
loss of earned privileges or denial of activities otherwise
available to other persons must be minimized and
utilized only after the documented failure of the unit’s
positive incentives for the individuals involved.
Facilities must ensure that any verbal or written
information provided to persons must be accessible in
the language and terminology the person understands.
Individual Behavior
Management Programs
[65E-5.1602, F.A.C.]
When an individualized treatment plan requires interventions
beyond the existing unit rules of conduct, the person shall be
included, and the person’s treatment plan shall reect:
(1) Documentation, signed by the physician that the
person’s medical condition does not exclude the
proposed interventions;
(2) Consent for the treatment to be provided;
(3) A general description of the behaviors requiring the
intervention, which may include previous emergency
interventions;
(4) Antecedents of that behavior;
(5) e events immediately following the behavior;
(6) Objective denition of the target behaviors, such
as specic acts, level of aggression, encroachment
on others’ space, self-injurious behavior or excessive
withdrawal;
(7) Arrangements for the consistent collection and
recording of data;
(8) Analysis of data;
(9) Based on data analysis, development of intervention
strategies, if necessary;
(10) Development of a written intervention strategy that
includes criteria for starting and stopping specic sta
interventions and the process by which they are to
occur;
(11) Continued data collection, if interventions are
implemented; and
(12) Periodic review and revision of the plan based upon
data collected and analyzed.
Emergency Treatment Orders
e Baker Act species under Quality of Treatment that each
individual must receive services, which are suited to his or
her needs, and which shall be administered skillfully, safely,
and humanely with full respect for the patient’s dignity and
personal integrity. is requires that facilities develop and
maintain, in a form accessible to and readily understandable
by individuals and consistent with rules adopted by the
department, the following:
Criteria, procedures, and required sta training for any
use of close or elevated levels of supervision, of restraint,
seclusion, or isolation, or of emergency treatment
orders, and for the use of bodily control and physical
management techniques.
Procedures for documenting, monitoring, and requiring
clinical review of all uses of the procedures above and
for documenting and requiring review of any incidents
resulting in injury to patients.
A facility can’t use seclusion or restraint for punishment,
to compensate for inadequate stang, or for the
convenience of sta. Facilities shall ensure that all sta are
made aware of these restrictions on the use of seclusion
and restraint and shall make and maintain records which
demonstrate that this information has been conveyed to
individual sta members.
Chapter 65E-5.100, F.A.C.) specically denes certain terms,
as follows:
Emergency treatment order (ETO) means a written
emergency order for psychotropic medications, as
described in Rule 65E-5.1703, F.A.C.; or a written
emergency order for seclusion or restraint, as described
in subsection (7) of Rule 65E-5.180, F.A.C.
e Florida Administrative Code governing the Baker Act
prohibits the use of PRN or standing orders for the purpose
of ordering any type of emergency treatment. is means that
an order initiating restraints or seclusion can only be initiated
or terminated upon the specic order of an authorized
professional – not “as needed.”

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 3 Emergency Treatment
Appendix I
I
Pro re nata (PRN) means an individualized order for
the care of an individual person which is written after
the person has been seen by the practitioner, which
order sets parameters for attending sta to implement
according to the circumstances set out in the order
[65E-5.100(11), F.A.C.]. A PRN order shall not be
used as an emergency treatment order.
Standing order means a broad protocol or delegation of
medical authority that is generally applicable to a group
of persons, hence not individualized. As limited by this
chapter, it prohibits improper delegations of authority
to sta that are not authorized by the facility, or not
permitted by practice licensing laws, to independently
make such medical decisions; such as decisions involving
determination of need, medication, routes, dosages
for psychotropic medication, or use of restraints or
seclusion upon a person [65E-5.100(16), F.A.C.].
In many situations, the use of restraint, seclusion and
emergency medications can be minimized by the use of
Personal Safety Plans (CF-MH 3124) that identify what
types of events cause an individual to become upset and what
interventions will calm the individual. A Personal Safety Plan
should guide individualized intervention techniques [65E-
5.180(7)(C), F.A.C.].
Among the requirements governed by the Florida
Administrative Code concerning Right to Quality Treatment
[s65E-5.180(5), F.A.C.] includes that mental health services
provided must comply with standards including a clinical
safety assessment accomplished at admission to determine
the person’s need for, and the facility’s capability to provide,
an environment and treatment setting that meets the person’s
need for a secure facility or close levels of sta observation. A
Personal Safety Plan can help accomplish this goal and reduce
the need for restraint, seclusion and emergency medications.
Restraint and Seclusion
s. 394.455, FS and 65E-180, F.A.C.
All facilities serving persons under the Baker Act are required
to adhere to the standards and requirements for behavior
management programs and must comply with the standards
required by the state’s Baker Act law and rule, as well as with
national standards that may apply to their facilities (federal
Conditions of Participation, e Joint Commission, CARF,
etc.). In addition, each facility must comply with it’s own
organization’s policies and procedures. Whichever of these
standards applicable to the organization is most stringent on
a given issue is the one the organization must follow:
Restraint means
A physical device, method, or drug used to control
behavior. A physical restraint is any manual method or
physical or mechanical device, material, or equipment
attached or adjacent to the individual’s body so that he or
she cannot easily remove the restraint and which restricts
freedom of movement or normal access to one’s body.
A drug used as a restraint is a medication used to control
the person’s behavior or to restrict his or her freedom
of movement and is not part of the standard treatment
regimen of a person with a diagnosed mental illness who
is a client of the department. Physically holding a person
during a procedure to forcibly administer psychotropic
medication is a physical restraint.
Restraint does not include physical devices, such as
orthopedically prescribed appliances, surgical dressings
and bandages, supportive body bands, or other
physical holding when necessary for routine physical
examinations and tests; or for purposes of orthopedic,
surgical, or other similar medical treatment; when used
to provide support for the achievement of functional
body position or proper balance; or when used to protect
a person from falling out of bed.
e Florida Administrative Code implementing the Baker
Act further states that Protective medical devices mean a
specic category of medical restraint that includes devices, or
combinations of devices, to restrict movement for purposes of
protection from falls or complications of physical care, such as
geri-chairs, posey vests, mittens, belted wheelchairs, sheeting,
and bed rails. e requirements for the use and documentation
of use of these devices are for specic medical purposes rather
than for behavioral control. [65E-5.100(12), F.A.C.].
When ordering safety or protective devices such as posey vests,
geri-chairs, mittens, and bed rails which also restrain, facility
sta shall consider alternative means of providing such safety so
that the person’s need for regular exercise is accommodated to
the greatest extent possible. Where frequent or prolonged use
of safety or protective devices is required, the person’s treatment
plan must address debilitating eects due to decreased exercise
levels such as circulation, skin, and muscle tone and the
person’s need for maintaining or restoring bowel and bladder
continence. e treatment plan must include scheduled
activities to lessen deterioration due to the usage of such
protective medical devices.
Seclusion means the physical segregation of a person in
any fashion or involuntary isolation of a person in a room
or area from which the person is prevented from leaving.
e prevention may be by physical barrier or by a sta
member who is acting in a manner, or who is physically

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 4
I
situated, so as to prevent the person from leaving the room
or area. For purposes of this chapter, the term does not mean
isolation due to a person’s medical condition or symptoms.
[394.455(29), FS]
Elevated Levels of Supervision. Receiving and treatment
facilities must ensure that where one-on-one supervision is
ordered by a physician, it must be continuous and not be
interrupted as a result of shift changes or due to conicting
sta assignments. Such supervision must be continuous until
documented as no longer medically necessary by a physician
[65E-5.180(9)].
e Baker Act standards mandate that the health and safety
of the individual must be the primary concern at all times.
Seclusion or restraint can only be employed in emergency
situations when necessary to prevent a person from seriously
injuring self or others, and less restrictive techniques have
been tried and failed, or if it has been clinically determined
that the danger is of such immediacy that less restrictive
techniques cannot be safely applied.
ere is a high prevalence of past traumatic experience
among persons who receive mental health services. e
response to trauma can include intense fear and helplessness,
a reduced ability to cope, and an increased risk to exacerbate
or develop a range of mental health and other medical
conditions. e experience of being placed in seclusion or
being restrained is potentially traumatizing. Seclusion and
restraint practices shall be guided by the following principles
of trauma-informed care: assessment of traumatic histories
and symptoms; recognition of culture and practices that
are re-traumatizing; processing the impact of a seclusion or
restraint with the person; and addressing sta training needs
to improve knowledge and sensitivity.
Staff Training
Sta must be trained as part of orientation and subsequently
on at least an annual basis. Sta responsible for the
following actions must demonstrate relevant competency
in the following areas before participating in a seclusion or
restraint event or related assessment, or before monitoring or
providing care during an event:
Strategies designed to reduce confrontation and to calm
and comfort people, including the development and use
of a personal safety plan,
Use of nonphysical intervention skills as well as bodily
control and physical management techniques, based on a
team approach, to ensure safety,
Observing for and responding to signs of physical and
psychological distress during the seclusion or restraint event,
Safe application of restraint devices,
Monitoring the physical and psychological well-being
of the person who is restrained or secluded, including
but not limited to: respiratory and circulatory status,
skin integrity, vital signs, and any special requirements
specied by facility policy associated with the one hour
face-to-face evaluation,
Clinical identication of specic behavioral changes that
indicate restraint or seclusion is no longer necessary,
e use of rst aid techniques, and
Certication in the use of cardiopulmonary
resuscitation, including required periodic recertication.
e frequency of training for cardiopulmonary
resuscitation will be in accordance with certication
requirements.
Prior to the Implementation
of Seclusion or Restraint
Prior intervention must include individualized therapeutic
actions such as those identied in a personal safety plan
that address individual triggers leading to psychiatric crisis.
Recommended form CF-MH 3124, Feb. 05, “Personal Safety
Plan,” may be used for the purpose of guiding individualized
techniques. Prior interventions may also include verbal de-
escalation and calming strategies. Non-physical interventions
must be the rst choice unless safety issues require the use of
physical intervention.
A personal safety plan must be completed or updated as
soon as possible after admission and led in the person’s
medical record. is form must be reviewed by the recovery
team, and updated if necessary, after each incident of
seclusion or restraint. Specic intervention techniques
from the personal safety plan that are oered or used prior
to a seclusion or restraint event must be documented in
the person’s medical record after each use of seclusion or
restraint. All sta must be aware of and have ready access to
each person’s Personal Safety Plan.
Implementation of Seclusion or Restraint
Use of restraint or seclusion can be very high risk for
individuals with severe mental illnesses. To protect the safety
of these individuals for whom restraint or seclusion has been
determined to be unavoidable, the following represent some
of the minimum requirements for safety and dignity:
A person who is restrained cannot be located in areas,
whenever possible, subject to view by persons other than
involved sta or where exposed to potential injury by
other persons.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 5 Emergency Treatment
Appendix I
I
Seclusion or restraint use cannot be based on the person’s
seclusion or restraint use history or solely on a history of
dangerous behavior. Dangerous behaviors include those
behaviors that jeopardize the physical safety of oneself or
others.
Persons can’t be restrained in a prone position unless
required by the immediate situation to prevent
imminent serious harm to the person or others.
To reduce the risk of positional asphyxiation, the person
must be repositioned as quickly as possible. Objects
that impair respiration cannot be placed over a person’s
face. In situations where precautions need to be taken to
protect sta, sta may wear protective gear.
Unless necessary to prevent serious injury, a person’s
hands shall not be secured behind the back during
containment or restraint.
In order to protect the safety of each person served by
a facility, each person must be searched for contraband
before or immediately after being placed into seclusion
or restraints.
e person must be clothed appropriately for
temperature and at no time may a person be placed in
seclusion or restraint in a nude or semi-nude state.
Seclusion and restraint may not be used simultaneously
for children less than 18 years of age.
e use of walking restraints is prohibited except for purposes
of o-unit transportation and may only be used under
direct observation of trained sta. In this instance, direct
observation means that sta maintains continual visual
contact of the person and is within close physical proximity
to the person at all times.
Additional standards governing initiation of restraint or
seclusion include:
1. A registered nurse or highest level sta member, as
specied by written facility policy, who is immediately
available and who is trained in seclusion and restraint
procedures may initiate seclusion or restraint in
an emergency when danger to oneself or others is
imminent. An order for seclusion or restraint must
be obtained from the physician, Advanced Registered
Nurse Practitioner (ARNP), or Physician’s Assistant
(PA), if permitted by the facility to order seclusion and
restraint and stated within their professional protocol.
e treating physician must be consulted as soon as
possible if the seclusion or restraint was not ordered by
the person’s treating physician.
2. An examination of the person will be conducted within
one hour by the physician or may be delegated to an
Advanced Registered Nurse Practitioner, Physician’s
Assistant, or Registered Nurse (RN), if authorized
by the facility and trained in seclusion and restraint
procedures. is examination must include a face-to
face assessment of the person’s medical and behavioral
condition, a review of the clinical record for any pre-
existing medical diagnosis or physical condition which
may contraindicate the use of seclusion or restraint, a
review of the person’s medication orders including an
assessment of the need to modify such orders during the
period of seclusion or restraint, and an assessment of
the need or lack of need to elevate the person’s head and
torso during restraint. e comprehensive examination
must determine that the risks associated with the use
of seclusion or restraint are signicantly less than not
using seclusion or restraint and whether to continue
or terminate the intervention. A licensed psychologist
may conduct only the behavioral assessment portion
of the comprehensive assessment if authorized by the
facility and trained in seclusion and restraint procedures.
Documentation of the comprehensive examination,
including the time and date completed, must be
included in the person’s medical record. If the face-to-
face evaluation is conducted by a trained Registered
Nurse, the attending physician who is responsible for the
care of the person must be consulted as soon as possible
after the evaluation is completed.
3. Each written order for seclusion or restraint is limited to
four hours for adults, age 18 and over;
two hours for children and adolescents age nine
through 17; or
one hour for children under age nine.
A seclusion or restraint order may be renewed in
accordance with these limits for up to a total of 24
hours, after consultation and review by a physician,
ARNP, or PA in person, or by telephone with a
Registered Nurse who has physically observed and
evaluated the person. When the order has expired
after 24 hours, a physician, ARNP, or PA must see
and assess the person before seclusion or restraint can
be re-ordered. e results of this assessment must
be documented. Seclusion or restraint use exceeding
24 hours requires the notication of the Facility
Administrator or designee.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 6
I
4. All seclusion and restraint orders must be signed within
24 hours of the initiation of and cannot be issued as a
standing order or on an as-needed basis.
5. e order must include the specic behavior prompting the
use of seclusion or restraint, the time limit for seclusion or
restraint, and the behavior necessary for the person’s release.
Additionally, for restraint, the order must contain the type
of restraint ordered and the positioning of the person,
including possibly elevating the person’s head for respiratory
and other medical safety considerations. Consideration
must be given to age, physical fragility, and physical
disability when ordering restraint type.
6. Every secluded or restrained person must be immediately
informed of the behavior that resulted in the seclusion
or restraint and the behavior and the criteria reecting
absence of imminent danger that are necessary for release.
7. For each use of seclusion or restraint, the following
information must be documented in the person’s medical
record: the emergency situation resulting in the seclusion
or restraint event; alternatives or other less restrictive
interventions attempted, as applicable, or the clinical
determination that less restrictive techniques could not
be safely applied; the name and title of the sta member
initiating the seclusion or restraint; the date/time of
initiation and release; the person’s response to seclusion
or restraint, including the rationale for continued use of
the intervention; and that the person was informed of
the behavior that resulted in the seclusion or restraint
and the criteria necessary for release.
8. For persons under the age of 18, the facility must notify
the parent(s) or legal guardian(s) of the person who has
been restrained or placed in seclusion as soon as possible,
but no later than 24 hours, after the initiation of each
seclusion or restraint event. is notication must be
documented in the person’s medical record, including
the date and time of notication and the name of the
sta person providing the notication.
9. For each use of seclusion or restraint, the following
information must be documented in the person’s
medical record:
e emergency situation resulting in the seclusion or
restraint event;
Alternatives or other less restrictive interventions
attempted, as applicable, or the clinical determination
that less restrictive techniques could not be safely
applied;
e name and title of the sta member initiating the
seclusion or restraint;
e date/time of initiation and release;
e person’s response to seclusion or restraint,
including the rationale for continued use of the
intervention; and
at the person was informed of the behavior that
resulted in the seclusion or restraint and the criteria
necessary for release.
During Seclusion or Restraint
Monitoring the physical and psychological well-being of the
person who is secluded or restrained must include but is not
limited to: respiratory and circulatory status; signs of injury;
vital signs; skin integrity; and any special requirements
specied by facility policies. is monitoring must be
conducted by trained sta as required in rule.
When restraint is initiated, nursing sta must see and assess
the person as soon as possible but no later than 15 minutes
after initiation and at least every hour thereafter. e
assessment must include checking the person’s circulation
and respiration, including necessary vital signs (pulse and
respiratory rate at a minimum). Documentation of the
observations and the sta person’s name must be recorded at
the time the observation takes place.
A person over age 12 who is secluded must be observed
by trained sta every 15 minutes. At least one observation
an hour will be conducted by a nurse. Restrained persons
must have continuous observation by trained sta. Secluded
children age 12 and under must be monitored continuously
by face-to-face observation or by direct observation through
the seclusion window for the rst hour and then at least
every 15 minutes thereafter.
During each period of seclusion or restraint, the person
must be oered reasonable opportunities to drink and
toilet as requested. In addition, the person who is restrained
must be oered opportunities to have range of motion at
least every two hours to promote comfort. Each facility
must have written policies and procedures specifying the
frequency of providing drink, toileting, and check of bodily
positioning to avoid traumatizing a person and retaining the
person’s maximum degree of dignity and comfort during the
use of bodily control and physical management techniques.
Responders must pay close attention to respiratory function
of the person during containment and restraint. All sta
involved must observe the person’s respiration, coloring,
and other possible signs of distress and immediately respond
if the person appears to be in distress. Responding to the
person’s distress may include repositioning the person,
discontinuing the seclusion or restraint, or summoning
medical attention, as necessary.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 7 Emergency Treatment
Appendix I
I
When a person demonstrates a need for immediate medical
attention in the course of an episode of seclusion or
restraint, the seclusion or restraint must be discontinued,
and immediate medical attention must be obtained.
Release from Seclusion or Restraint
and Post-Release Activities
A person must be released from seclusion or restraint as
soon as he or she is no longer an imminent danger to self
or others. Upon release from seclusion or restraint, the
person’s physical condition must be observed, evaluated,
and documented by trained sta. Documentation must also
include the name and title of the sta releasing the person
and the date and time of release.
After a seclusion or restraint event, a debrieng process must
take place to decrease the likelihood of a future seclusion or
restraint event for the person and to provide support.
Each facility must develop policies to address:
A review of the incident with the person who was
secluded or restrained. e person must be given the
opportunity to process the seclusion or restraint event
as soon as possible but no longer than within 24 hours
of release. is debrieng discussion must take place
between the person and either the recovery team or
another preferred sta member. is review must seek
to understand the incident within the framework of the
person’s life history and mental health issues. It should
assess the impact of the event on the person and help
the person identify and expand coping mechanisms to
avoid the use of seclusion or restraint in the future. e
discussion must include constructive coping techniques
for the future. A summary of this review should be
documented in the person’s medical record.
A review of the incident with all sta involved in the
event and supervisors or administrators. is review
must be conducted as soon as possible after the
event and must address: the circumstances leading
to the event, the nature of de-escalation eorts and
alternatives to seclusion and restraint attempted, sta
response to the incident, and ways to eectively support
the person’s constructive coping in the future and avoid
the need for future seclusion or restraint. e outcomes
of this review should be documented by the facility for
purposes of continuous performance improvement and
monitoring. e review ndings must be forwarded to
the Seclusion and Restraint Oversight Committee, and
Support for other persons served and sta, as needed, to
return the unit to a therapeutic milieu.
Within two working days after any use of seclusion or
restraint, the recovery team must meet and review the
circumstances preceding its initiation and review the person’s
recovery plan and personal safety plan to determine whether
any changes are needed in order to prevent the further use
of seclusion or restraint. e recovery team must also assess
the impact the event had on the person and provide any
counseling, services, or treatment that may be necessary as a
result. e recovery team must analyze the person’s clinical
record for trends or patterns relating to conditions, events,
or the presence of other persons immediately before or
upon the onset of the behavior warranting the seclusion or
restraint, and upon the person’s release from seclusion. e
recovery team must review the eectiveness of the emergency
intervention and develop more appropriate therapeutic
interventions. Documentation of this review must be placed
in the person’s clinical record.
Oversight
Every facility permitting use of restraint or seclusion is
required to have a Seclusion and Restraint Oversight
Committee. is is a group of people at an agency or
facility that monitors the use of seclusion and restraint at the
facility. is committee is intended to assist in the reduction
of seclusion and restraint use at the agency or facility.
Membership includes, but is not limited to, the facility
administrator/designee, medical sta, quality assurance sta,
and a peer specialist or advocate, if employed by the facility
or otherwise available. If no such person is employed by
the facility, an external peer specialist or advocate may be
appointed. [65E-5.100(15), F.A.C.]
e Seclusion and Restraint Oversight Committee must
conduct timely reviews of each use of seclusion and restraints
and monitor patterns of use, for the purpose of assuring least
restrictive approaches are utilized to prevent or reduce the
frequency and duration of use.
Reporting
All facilities are required to report each seclusion and restraint
event to the Department of Children and Families. is
reporting must be done electronically using the Department’s
web-based application either directly via the data input
screens or indirectly via the File Transfer Protocol batch
process. e required reporting elements are:
Provider tax identication number;
Person’s social security number and identication
number;

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 8
I
Date and time the seclusion or restraint event was
initiated;
Discipline of the person ordering the seclusion or
restraint;
Discipline of the person implementing the seclusion or
restraint;
Reason seclusion or restraint was initiated;
Type of restraint used;
Whether signicant injuries were sustained by the
person; and
Date and time seclusion or restraint was terminated.
Facilities must report seclusion and restraint events on a
monthly basis. Events that result in death or signicant
injury either to a sta member or person must be reported
to the department’s web based system in accordance with
department operating procedures.
All facilities that are subject to CMS Conditions of
Participation for Hospitals, 42 Code of Federal Regulations,
part 482, must report to CMS any death that occurs in the
following circumstances:
While a person is restrained or secluded;
Within 24 hours after release from seclusion or
restraint; or
Within one week after seclusion or restraint, where
it is reasonable to assume that use of the seclusion
or restraint contributed directly or indirectly to the
person’s death.
Each death associated with restraint or seclusion must be
reported to CMS by telephone no later than the close of
business the next business day following knowledge of the
persons’ death. A report must simultaneously be submitted
to the Substance Abuse and Mental Health Director/
Designee in the Mental Health Program Oce headquarters
in Tallahassee, FL. e address is: 1317 Winewood Blvd.,
Tallahassee, FL, 32399-0700. e Department is required
to collect and review the data on a monthly basis. e
Director of Mental Health must be informed of any deaths
or signicant injuries related to seclusion or restraint and
signicant trends regarding seclusion and restraint use.
When Individual Behavioral Management is required,
it can only be implemented in compliance with chapter
65E-5.1602, F.A.C.. When an individualized treatment
plan requires interventions beyond the existing unit rules
of conduct, the person must be included, and the person’s
treatment plan must reect:
Documentation, signed by the physician that the
person’s medical condition does not exclude the
proposed interventions;
Consent for the treatment to be provided;
A general description of the behaviors requiring the
intervention, which may include previous emergency
interventions;
Antecedents of that behavior;
e events immediately following the behavior;
Objective denition of the target behaviors, such
as specic acts, level of aggression, encroachment
on others’ space, self-injurious behavior or excessive
withdrawal;
Arrangements for the consistent collection and
recording of data;
Analysis of data;
Based on data analysis, development of intervention
strategies, if necessary;
Development of a written intervention strategy that
includes criteria for starting and stopping specic sta
interventions and the process by which they are to
occur;
Continued data collection, if interventions are
implemented; and
Periodic review and revision of the plan based upon
data collected.
Emergency Orders
for Psychiatric Medications
e Baker Act statute and rules prohibit the administration
of psychiatric medication unless a competent adult
has provided express and informed consent to those
medications, or if not competent to provide this consent, it
be provided by the person’s, guardian, guardian advocate, or
a health care surrogate/proxy as specied by law. e only
exception is due to imminent danger in which a physician
can order an Emergency Treatment Order (ETO) for such
medications.
Among the requirements governed in the Florida
Administrative Code concerning Right to Quality Treatment
[s65E-5.180(5), F.A.C.] includes that mental health services
provided must comply with the following standards: e
development and implementation of protocols or procedures
for conducting and documenting the following must be
accomplished by each facility:

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 9 Emergency Treatment
Appendix I
I
Determination of a person’s competency to consent to
treatment within 24 hours after admission;
Identication of a duly authorized decision-maker for
the person upon any person being determined not to be
competent to consent to treatment;
Obtaining express and informed consent for treatment
and medications before administration, except in an
emergency; and
Required involvement of the person and guardian,
guardian advocate, or health care surrogate or proxy, in
treatment and discharge planning.
e Baker Act specically denes “Express and informed
consent” and “incompetent to consent to treatment” as
follows:
Express and Informed Consent means consent
voluntarily given in writing, by a competent person,
after sucient explanation and disclosure of the subject
matter involved to enable the person to make a knowing
and willful decision without any element of force, fraud,
deceit, duress, or other form of constraint or coercion.
[394.455(9), FS]
Incompetent to consent to treatment means that a
person’s judgment is so aected by his or her mental
illness that the person lacks the capacity to make a
well-reasoned, willful, and knowing decision concerning
his or her medical or mental health treatment.
[394.455(15), FS]
An individual, if competent has the right to refuse psychiatric
treatment, even if held for involuntary examination or court
ordered for involuntary placement. Only if a court has
appointed a guardian or guardian advocate or a physician
has determined the individual lacks the competence to
proved express and informed consent and a health care
surrogate/proxy has provided substitute decision-making, can
psychiatric treatment be administered, short of an emergency
treatment order.
Initiation of an Emergency Treatment
Order For Psychiatric Medications
[65E-5.1703(1), F.A.C.]
An emergency treatment order for psychotropic medication
supersedes the person’s right to refuse psychotropic medication
if based upon the physician’s assessment that the individual is
not capable of exercising voluntary control over his or her own
symptomatic behavior and that these uncontrolled symptoms
and behavior are an imminent danger to the person or to others
in the facility. When emergency treatment with psychotropic
medication is ordered for a minor or an incapacitated or
incompetent adult, facility sta must document attempts to
promptly contact the guardian, guardian advocate, or health
care surrogate or proxy to obtain express and informed consent
for the treatment in advance of administration where possible
and if not possible, as soon thereafter as practical.
An emergency treatment order must be consistent with
the least restrictive treatment interventions, including the
emergency administration of psychotropic medications or
the emergency use of restraints or seclusion.
To assure the safety and rights of the person, and since
emergency treatment orders by a physician absent express
and informed consent are permitted only in an emergency,
any use of psychotropic medications other than rapid
response psychotropic medications requires a detailed and
complete justication for the use of such medication. Both
the nature and extent of the imminent emergency and any
orders for the continuation of that medication must be
clearly documented daily as required above.
e need for each emergency treatment order must be
documented in the person’s clinical record in the progress
notes and in the section used for physician’s orders and must
describe the specic behavior which constitutes a danger to
the person or to others in the facility, and the nature and
extent of the danger posed.
e issuance of an emergency treatment order requires
a physician’s review of the person’s condition for causal
medical factors, such as insuciency of psychotropic
medication blood levels, as determined by drawing a blood
sample; medication interactions with psychotropic or other
medications; side eects or adverse reactions to medications;
organic, disease or medication based metabolic imbalances
or toxicity; or other biologically based or inuenced
symptoms.
All emergency treatment orders for medications may only
be written by a physician as dened in the Baker Act. e
physician must review, integrate and address such metabolic
imbalances in the issuance of an emergency treatment order.
e physician’s initial order for emergency treatment may
be by telephone but such a verbal order must be reduced to
writing upon receipt and signed by a physician within 24
hours. Each emergency treatment order is only valid and is
only the authority for emergency treatment for a period not
to exceed 24 hours.
Upon the initiation of an emergency treatment order the
facility must, within two court working days, petition the
court for the appointment of a guardian advocate to provide

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 10
I
express and informed consent, unless the person voluntarily
withdraws a revocation of consent or requires only a single
emergency treatment order for emergency treatment.
If a second emergency treatment order is issued for the
same person within any 7 day period, the petition for the
appointment of a guardian advocate to provide express and
informed consent must be led with the court within 1 court
working day.
While awaiting court action, treatment may be continued
without the consent of the person, but only upon the daily
written emergency treatment order of a physician who has
determined that the person’s behavior each day during the
wait for court action continues to present an immediate
danger to the safety of the person or others and who
documents the nature and extent of the emergency each day
of the specic danger posed. Such orders may not be written
in advance of the demonstrated need for same.
Health Care Surrogate and Proxy
65E-5.2301, F.A.C.
When an adult has been determined by a physician to be
incompetent to consent to his or her own treatment, it is
critical for facility sta to determine if a health care advance
directive had been prepared by the individual at a previous
time when competent to do so. Such an advance directive is
likely to have named a person to make health care decisions
on behalf of the individual and to include preferences for
care. Some denitions for this substitute decision making
include:
Advance directive means a witnessed written document
described in Section 765.101, F.S.
Health care surrogate means any competent adult
expressly designated by a principal’s advance directive
to make health care decisions on behalf of the principal
upon the principal’s incapacity.
Health care proxy means a competent adult who has
not been expressly designated by an advance directive to
make health care decisions for a particular incapacitated
individual, but is authorized pursuant to Section
765.401, F.S., to make health care decisions for such
individual.
When a person hasn’t completed a health care advance
directive or hasn’t named a surrogate or a named surrogate
is no longer able or willing to serve, a proxy can be named
by the facility from a list in the order of listing, as follows
[s.765.401(1), FS]:
1. Judicially appointed guardian of the patient
2. Spouse;
3. Adult child of the patient, or if the patient has more
than one adult child, a majority of the adult children
who are reasonably available for consultation;
4. Parent of the patient;
5. Adult sibling of the patient or, if the patient has more
than one sibling, a majority of the adult siblings who are
reasonably available for consultation;
6. Adult relative of the patient who has exhibited
special care and concern for the patient and who has
maintained regular contact with the patient and who is
familiar with the patient’s activities, health, and religious
or moral beliefs; or
7. Close friend of the patient.
8. LCSW selected by the provider’s bioethics committee
and must not employed by the provider. If the
provider doesn’t have a bioethics committee, then
such a proxy may be chosen through an arrangement
with the bioethics committee of another provider.
Documentation of eorts to locate proxies from prior
classes must be recorded in the patient record.
Any health care decision made must be based on the
surrogate or proxy’s informed consent and on the decision
the proxy reasonably believes the patient would have made
under the circumstances. If there is no indication of what the
individual would have chosen, the proxy may consider the
individual’s best interest in deciding that proposed treatments
are to be withheld or that treatments currently in eect are to
be withdrawn.
When a Health Care Surrogate or Proxy has been designated
to make medical and psychiatric decisions for an adult who
has been determined by a physician to be incompetent to
make his or her own decisions, the following requirements
govern this process
1. During the interim period between the time a person is
determined to be incompetent to consent to treatment
by one or more physicians and the time a guardian
advocate is appointed by a court to provide express and
informed consent to the person’s treatment, a health care
surrogate designated by the person may provide such
consent to treatment.
2. In the absence of an advance directive or when the
health care surrogate named in the advance directive is
no longer able or willing to serve, a health care proxy,
may also provide interim consent to treatment.
3. Upon the documented determination that a patient is
incompetent to make health care decisions for himself or

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 11 Emergency Treatment
Appendix I
I
herself by one or more physicians, the facility must notify
the surrogate or proxy in writing that the conditions under
which he or she can exercise his or her authority under
the law have occurred. Recommended form CF-MH
3122, Feb. 05, “Certication of Person’s Incompetence to
Consent to Treatment and Notication of Health Care
Surrogate/Proxy,” may be used for this purpose.
4. If the surrogate selected by the person is not available
or is unable to serve or if no advance directive had been
prepared by the person, a proxy may be designated as
provided by law. Recommended form CF-MH 3123, Feb.
05, “Adavit of Proxy,” may be used for this purpose.
5. A petition for adjudication of incompetence to consent
to treatment and appointment of a guardian advocate
must be led with the court within 2 court working
days of the determination of the patient’s incompetence
to consent to treatment by one or more physicians,
Recommended form CF-MH 3106, “Petition for
Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate,” may be used
for this purpose.
6. e facility must immediately provide to the health care
surrogate or proxy the same information required by
statute to be provided to the guardian advocate. In order
to protect the safety of the person, the facility must
make available to the health care surrogate or proxy the
training required of guardian advocates and ensure that
the surrogate or proxy communicate with the person
and person’s physician prior to giving express and
informed consent to treatment.
7. Each designated receiving and treatment facility must
adopt policies and procedures specifying how its direct
care and assessment sta will be trained on how to
honor each person’s treatment preferences as detailed in
his or her advance directives. e person being served
must be provided information about advance directives
and oered assistance in completing an advance
directive, if willing and able to do so.
Specialized on-line Baker Act courses can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Treatment
I
Quick Reference Guide to Restraint and Seclusion
(is guide does not substitute for use of state and federal statutes and regulations. e most restrictive provision applies.
Organizations accredited by e Joint Commission must also comply with Commission standards)
Federal Centers for
State Baker Act Statute and Rules
Medicare and Medicaid (CMS)
Legal Citation
Social Security Act (42 U.S.C. 1301 and
s. 394.455 and 394.459 (4), F.S.
1395hh, Subpart B Administration Sec.
Chapter 65E-5.180, F.A.C.
482.13 (e)
Application
All designated receiving and treatment facilities as well as other hospitals holding persons under the Hospitals participating in federal
authority of the Baker Act. Medicare and Medicaid programs
Principles
A facility can’t use seclusion/restraint for punishment, to compensate for inadequate staffing, or for the
convenience of staff.
Facilities shall ensure that all staff are made aware of these restrictions on the use of seclusion/restraint
and shall make/maintain records demonstrating this information has been conveyed to individual staff.
DCF must adopt rules establishing forms/procedures relating to rights/privileges of persons seeking
mental health treatment from Baker Act facilities;
Persons have a right to be free from
seclusion and restraints, of any form,
imposed as a means of coercion,
discipline, convenience, or retaliation
by staff.
Seclusion or a restraint can only
be used in emergency conditions
if needed to ensure the patient’s
physical safety and less restrictive
interventions have been determined
to be ineffective.
Definitions
Restraint means
(a) Physical device, method, or drug used to control behavior. A physical restraint is any manual method
or physical or mechanical device, material, or equipment attached or adjacent to the individual’s
body so that he or she cannot easily remove the restraint and which restricts freedom of movement
or normal access to one’s body.
(b) A drug used as a restraint is a medication used to control the person’s behavior or to restrict his or
her freedom of movement and is not part of the standard treatment regimen of a person with a
diagnosed mental illness who is a client of the department. Physically holding a person during a
procedure to forcibly administer psychotropic medication is a physical restraint.
(c) Restraint does not include physical devices, such as orthopedically prescribed appliances, surgical
dressings and bandages, supportive body bands, or other physical holding when necessary for
routine physical examinations and tests; or for purposes of orthopedic, surgical, or other similar
medical treatment; when used to provide support for the achievement of functional body position
or proper balance; or when used to protect a person from falling out of bed.
Seclusion means the physical segregation of a person in any fashion or involuntary isolation of a person
in a room or area from which the person is prevented from leaving. The prevention may be by physical
barrier or by a staff member who is acting in a manner, or who is physically situated, so as to prevent the
person from leaving the room or area. For purposes of this chapter, the term does not mean isolation
due to a person’s medical condition or symptoms.
Protective medical devices mean a specific category of medical restraint that includes devices, or
combinations of devices, to restrict movement for purposes of protection from falls or complications of
physical care, such as geri-chairs, posey vests, mittens, belted wheelchairs, sheeting, and bed rails. The
requirements for the use and documentation of use of these devices are for specific medical purposes
rather than for behavioral control.
Use of these devices are different from the general requirements for the use of restraint in this rule.
Emergency treatment order (ETO) means a written emergency order for psychotropic medications, as
described in Rule 65E-5.1703, F.A.C.; or a written emergency order for seclusion or restraint, as described
in subsection (7) of Rule 65E-5.180, F.A.C., of this rule chapter.
Restraint includes either a physical
restraint or a drug that is being used as
a restraint.
Physical restraint is any manual
method or physical or mechanical
device, material, or equipment
attached or adjacent to the patient’s
body that he or she cannot easily
remove that restricts freedom of
movement or normal access to one’s
body.
Drug used as a restraint is a medication
used to control behavior or to restrict
the patient’s freedom of movement
and is not a standard treatment for
the patient’s medical or psychiatric
condition.
Seclusion is the involuntary
confinement of a person in a room or
an area where the person is physically
prevented from leaving.
Emergency is a situation where
a person’s behavior is violent or
aggressive and where the behavior
presents an immediate and serious
danger to the safety of the person, or
other patients, staff, or others.
Appendix I - 12

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Treatment
Appendix I
I
Federal Centers for
State Baker Act Statute and Rules
Medicare and Medicaid (CMS)
Required of Facilities
Facilities must develop:
Criteria, procedures, and required staff training for any use of close or elevated levels of supervision,
of restraint, seclusion, or isolation, or of emergency treatment orders, and for the use of bodily
control and physical management techniques.
Procedures for documenting, monitoring, and requiring clinical review of all uses of the procedures
above and for documenting and requiring review of any incidents resulting in injury.
N/A
Training Required
Staff must be trained as part of orientation and subsequently on at least an annual basis. Staff
responsible for following actions must demonstrate relevant competency in following areas before
participating in a seclusion/restraint event or related assessment, or before monitoring/providing care
during an event:
Strategies designed to reduce confrontation and to calm/comfort people, including the
development/use of a personal safety plan,
All staff who have direct patient
contact must have ongoing
education and training in the
proper and safe use of seclusion
and restraint application and
techniques and alternative methods
for handling behavior, symptoms,
Use of nonphysical intervention skills as well as bodily control/physical management techniques,
based on a team approach, to ensure safety,
Observing for/responding to signs of physical/psychological distress during seclusion/restraint
event,
Safe application of restraint devices,
Monitoring the physical/psychological well-being of person who is restrained/secluded, including
but not limited to: respiratory/circulatory status, skin integrity, vital signs, and any special
requirements specified by facility policy associated with the one hour face-to-face evaluation,
Clinical identification of specific behavioral changes that indicate restraint/seclusion is no longer
necessary,
The use of first aid techniques, and
Certification in the use of cardiopulmonary resuscitation, including required periodic recertification.
The frequency of training for cardiopulmonary resuscitation will be in accordance with certification
requirements
and situations that traditionally
have been treated through the use
of restraints and seclusion.
Use of Restraints and Seclusion
Seclusion/restraint use cannot be based on the person’s seclusion/restraint use history or solely on
a history of dangerous behavior. Dangerous behaviors include those behaviors that jeopardize the
physical safety of oneself or others.
Each person shall be searched for contraband before or immediately after being placed into seclusion or
restraints.
The use of restraints or seclusion to
manage behavior is an emergency
measure that should be reserved
for those occasions when an
unanticipated, severely aggressive
or destructive behavior places
1. A registered nurse or highest level staff member immediately available and who is trained in
seclusion/restraint procedures may initiate seclusion/restraint in an emergency when danger to
self/others is imminent. An order must be obtained from a physician, ARNP, or PA, if permitted by
the facility to order seclusion/restraint and stated within their professional protocol. The treating
physician must be consulted as soon as possible if not ordered by the physician.
2. An examination of the person conducted within 1 hour by the physician or may be delegated to an
ARNP or PA, or RN, if authorized by the facility and trained in seclusion/restraint procedures. Must
include a face-to face assessment of person’s medical/behavioral condition, a review of clinical
record for any pre-existing medical diagnosis/physical condition which may contraindicate the use
of seclusion/restraint, a review of medication orders including an assessment of the need to modify
such orders, and assessment of need to elevate the person’s head and torso during restraint. A
psychologist may conduct only the behavioral assessment portion of the assessment if authorized
by the facility and trained in seclusion/restraint procedures. Documentation of the comprehensive
examination, including time/date completed, shall be included in medical record. If the face-to-face
evaluation is conducted by a trained RN, the physician responsible for the care of the person must be
the patient or others in imminent
danger.
Restraints and seclusion should only
be used:
When less restrictive measures
have been found to be
ineffective to protect the patient
or others from harm;
Upon order of a physician
In accordance with a written
modification to the patient’s
plan of care;
When employing safe
appropriate restraining
techniques;
consulted as soon as possible after the evaluation is completed.
3. All orders signed within 24 hours of initiation - no standing order or as-needed basis.
—Continued—
When the treating physician
has been consulted ASAP if
not ordered by the treating
physician; and
Appendix I - 13

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Treatment
I
Federal Centers for
State Baker Act Statute and Rules
Medicare and Medicaid (CMS)
Use of Restraints and Seclusion (Continued)
4. Order must include the specific behavior prompting the use of seclusion/restraint, time limit, and
behavior necessary for release. For restraint, order must contain type of restraint ordered and
positioning of person and other medical safety considerations. Consideration must be given to age,
physical fragility, and physical disability.
5. Every person must be immediately informed of the behavior that resulted in seclusion/restraint and
the behavior/criteria reflecting absence of imminent danger necessary for release.
6. Medical record must document: the emergency situation resulting in the seclusion/restraint event;
alternatives/less restrictive interventions attempted, as applicable; name and title of staff initiating
seclusion/restraint; date/time of initiation/release; person’s response to
7. Facility must notify the parent(s) or legal guardian(s) of a minor who has been restrained/ secluded
ASAP, but no later than 24 hours, after the initiation of each event. Notification must be documented
in medical record, including the date/ time of notification and name of staff providing notification.
When a physician sees and
evaluates the need for restraint
or seclusion within 1 hour after
initiation.
Length of Restraint or Seclusion
Each written order for seclusion or restraint is limited to
Four hours for adults, age 18 and over;
Two hours for children and adolescents age nine through 17; or
One hour for children under age nine.
Same as Florida
Ended at the earliest possible time,
regardless of the length of the
order.
Renewal of Order
A seclusion/restraint order may be renewed with these limits for up to a total of 24 hours, after
consultation and review by a physician, ARNP, or PA in person, or by telephone with a RN who has
physically observed and evaluated the person. When order has expired after 24 hours, a physician, ARNP,
or PA must see and assess the person before seclusion/restraint can be re-ordered. The results of this
assessment must be documented. Seclusion/restraint use exceeding 24 hours requires notification of
Facility Administrator/designee.
The original order may only be
renewed in accordance with these
limits for up to a total of 24 hours.
If discontinued prior to expiration
of original order, new order
required prior to reapplication.
Face-to-face by physician not
required to renew within 24
hours, but must return to renew
if restraint or seclusion exceed 24
hour total.
Monitoring
Monitoring physical/psychological well-being of person who is secluded/restrained must include but is
not limited to: respiratory and circulatory status; signs of injury; vital signs; skin integrity; and any special
requirements specified by facility policies and be conducted by trained staff
When restraint is initiated, nursing staff must see/assess the person ASAP but no later than 15 minutes
after initiation and at least every hour thereafter. The assessment must include checking circulation
and respiration, necessary vital signs (pulse and respiratory rate at a minimum). Documentation of
observations and staff name must be recorded at the time the observation takes place.
A person over age 12 who is secluded must be observed by trained staff every 15 minutes. At least
one observation an hour must be conducted by a nurse. Restrained persons must have continuous
observation by trained staff. Secluded children age 12 and under must be monitored continuously by
face-to-face observation or by direct observation through the seclusion window for the first hour and
then at least every 15 minutes thereafter.
During each period of seclusion/restraint, person must be offered reasonable opportunities to drink
and toilet as requested and be offered opportunities to have range of motion at least every two hours
to promote comfort. Each facility must have written policies and procedures on these issues to avoid
traumatizing person and retaining person’s maximum degree of dignity/comfort during the use of bodily
control/physical management techniques.
Responders must pay close attention to respiratory function during containment/ restraint. All
staff involved must observe person’s respiration, coloring, and other possible signs of distress and
immediately respond if person appears to be in distress. Responding to the person’s distress may
include repositioning, discontinuing seclusion/restraint, or summoning medical attention. When person
demonstrates need for immediate medical attention, the seclusion/restraint must be discontinued, and
immediate medical attention must be obtained.
The condition of the patient who is
in a restraint or in seclusion must
continually be assessed, monitored,
and reevaluated.
Continuous assessment and
reevaluation of the patient’s
condition.
Appendix I - 14

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Treatment
Appendix I
I
Federal Centers for
State Baker Act Statute and Rules
Medicare and Medicaid (CMS)
Clinical Oversight
Every facility using restraint/seclusion must have a Seclusion and Restraint Oversight Committee, to NA
monitors the use of seclusion/ restraint at the facility and to assist in the reduction of seclusion/restraint
use. The Committee must conduct timely reviews of each use of seclusion/restraints and monitor
patterns of use to assure least restrictive approaches are used and to prevent or reduce the frequency
and duration of use.
Specific Prohibition
PRN and Standing Orders may not be used to authorize restraints or seclusion or other specified actions,
as follows:
Pro re nata (PRN) means an individualized order for the care of an individual person which
is written after the person has been seen by the practitioner, which order sets parameters
for attending staff to implement according to the circumstances set out in the order. A PRN
order shall not be used as an emergency treatment order.
Standing order means a broad protocol or delegation of medical authority that is generally
applicable to a group of persons, hence not individualized. As limited by this chapter, it
prohibits improper delegations of authority to staff that are not authorized by the facility,
or not permitted by practice licensing laws, to independently make such medical decisions;
such as decisions involving determination of need, medication, routes, dosages for
psychotropic medication, or use of restraints or seclusion upon a person.
Other prohibitions include:
Cannot be located in areas in view by persons other than involved staff or where exposed to
potential injury by other persons.
Cannot be based on the person’s seclusion or restraint use history or solely on a history of dangerous
behavior. Dangerous behaviors include those behaviors that jeopardize the physical safety of oneself
or others.
Prone position can’t be used unless required by the immediate situation to prevent imminent serious
harm to the person or others and repositioned as quickly as possible. Objects that impair respiration
cannot be placed over a person’s face. In situations where precautions need to be taken to protect
staff, staff may wear protective gear.
Person’s hands shall not be secured behind the back during containment or restraint.
Person clothed appropriately for temperature and at no time shall a person be placed in seclusion or
restraint in a nude or semi-nude state.
May not be used simultaneously for children less than 18 years of age.
The use of walking restraints is prohibited except for purposes of off-unit transportation and may only
be used under direct observation of trained staff where staff maintains continual visual contact of the
person and is within close physical proximity to the person at all times.
Restraint and seclusion may not
be used simultaneously unless the
patient is:
Continually monitored face-
to-face by an assigned staff
member; or
Continually monitored by staff
using both video and audio
equipment.
This monitoring must be in close
proximity to the patient.
PRN and standing orders should
never be used with or as a part of
seclusion and restraints.
Release from Restraints and Seclusion
A person must be released from seclusion or restraint as soon as he or she is no longer an imminent
danger to self or others. Release from seclusion/restraint must occur as soon as the person no longer
appears to present imminent danger to self/others. Upon release from seclusion/ restraint, the person’s
physical condition must be observed, evaluated, and documented by trained staff. Documentation must
also include: the name and title of the staff releasing the person; and date/time of release.
After a seclusion or restraint event, a debriefing process must take place to decrease the likelihood of
a future seclusion/restraint event for the person and to provide support. Each facility must develop
policies to address:
A review of the incident with the person who was secluded/restrained. Person must be given
opportunity to process the seclusion/restraint event ASAP as soon as possible but no longer than
24 hours after release. This debriefing discussion must take place between person and either the
recovery team or another preferred staff member to understand the incident within the framework
of the person’s life history and MH issues. It should assess the impact of the event on the person and
help the person identify and expand coping mechanisms to avoid the use of seclusion/restraint in
future. A review summary should be documented in person’s medical record.
—Continued—
Restraints and seclusion should
be discontinued at the earliest
possible time; as soon as the
patient can commit to safety
and no longer pose a threat to
themselves or others.
Appendix I - 15

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency Treatment
I
Federal Centers for
State Baker Act Statute and Rules
Medicare and Medicaid (CMS)
Release from Restraints and Seclusion CONTINUED
A review of the incident with all staff involved in the event and supervisors or administrators. This
review must be conducted ASAP after the event and must address: the circumstances leading to
the event, the nature of de-escalation efforts and alternatives to seclusion/restraint attempted,
staff response to the incident, and ways to effectively support the person’s constructive coping in
the future and avoid the need for future seclusion/restraint. The outcomes of this review should be
documented for continuous performance improvement and monitoring. The review findings must
be forwarded to the Seclusion and Restraint Oversight Committee, and
Support for other persons served and staff, as needed, to return the unit to a therapeutic milieu.
Within two working days after any use of seclusion or restraint, the recovery team must meet and review
the circumstances preceding its initiation and review the person’s recovery plan and personal safety plan
to determine whether any changes are needed in order to prevent the further use of seclusion/restraint.
The recovery team must also assess the impact the event had on the person and provide any counseling,
services, or treatment that may be necessary as a result. The recovery team must analyze the person’s
clinical record for trends or patterns relating to conditions, events, or the presence of other persons
immediately before or upon the onset of the behavior warranting the seclusion/restraint, and upon
the person’s release from seclusion. The recovery team must review the effectiveness of the emergency
intervention and develop more appropriate therapeutic interventions. Documentation of this review
must be placed in the person’s clinical record.
Reporting Required
All facilities are required to report each seclusion and restraint event to the Department of Children and
Families. This reporting must be done electronically using the Department’s web-based application
either directly via the data input screens or indirectly via the File Transfer Protocol batch process. The
required reporting elements are:
Provider tax identification number;
Person’s social security number and identification number;
Date and time the seclusion or restraint event was initiated;
Discipline of the person ordering the seclusion or restraint;
Discipline of the person implementing the seclusion or restraint;
Reason seclusion or restraint was initiated;
Type of restraint used;
Whether significant injuries were sustained by the person; and
Date and time seclusion or restraint was terminated.
Facilities must report seclusion and restraint events on a monthly basis. Events that result in death or
significant injury either to a staff member or person must be reported to the department’s web based
system in accordance with department operating procedures.
All facilities that are subject to
CMS Conditions of Participation
for Hospitals, 42 Code of Federal
Regulations, part 482, must report
to CMS any death that occurs in the
following circumstances:
While a person is restrained or
secluded;
Within 24 hours after release
from seclusion or restraint; or
Within one week after
seclusion or restraint, where
it is reasonable to assume
that use of the seclusion or
restraint contributed directly or
indirectly to the person’s death.
Required of Facilities
Facilities must develop:
N/A
Criteria, procedures, and required staff training for any use of close or elevated levels of supervision,
of restraint, seclusion, or isolation, or of emergency treatment orders, and for the use of bodily
control and physical management techniques.
Procedures for documenting, monitoring, and requiring clinical review of all uses of the procedures
above and for documenting and requiring review of any incidents resulting in injury.
Appendix I - 16

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix I - 17 Emergency Treatment
Appendix I
I
Federal CMS regulations denes physical restraints as “any
manual method or physical or mechanical device that restricts
freedom of movement or normal access to one’s body,
material, or equipment, attached or adjacent to the patient’s
body that he or she cannot easily remove. Holding a patient
in a manner that restricts his/her movement constitutes
restraint for that patient.”
According to federal regulations, an object may be a restraint
by functional denition; that is, when an object restricts
a patient’s movement or access to his or her body, it is a
restraint. Under this denition, all sorts of more commonly
used hospital devices and practices could meet the federal
denition of a restraint, such as side rails or tucking a sheet
in tightly. Medical restraints may be used to limit mobility,
temporarily immobilizing a person related to a medical,
post-surgical or dental procedure. In such cases, it would not
be considered a restraint. However, if the same intervention
is used because of an unanticipated outburst of severe
aggression or destructive behavior that poses an imminent
danger to the person or others, it is a restraint. e federal
behavior management standard doesn’t apply to situations
where the hospital wishes to restrain a person to address the
risk of a fall or to control wandering. e use of restraint
for a non-violent or non-aggressive, otherwise cooperative
person may be governed by the medical/surgical care restraint
standards.
In 2009, e Joint Commission adopted requirements based
on the CMS requirements for only for hospitals that use
Joint Commission accreditation for deemed status purposes.
For example,
Hospitals that use e Joint Commission accreditation
for deemed status purposes must comply with standards
PC.03.05.01-PC .03.05.19; these hospitals do not have
to follow standards PC.03.02.01-PC03.03.031 and
RC.02.01.05 in the Record of Care chapter.
Hospitals that do not use e Joint Commission
accreditation for deemed status purposes must continue
to comply with the current e Joint Commission
standards PC.03.02.01-PC.03.03.031 and RC.02.01.05.
While these standards are quite similar to those found in the
state Baker Act rules and by the federal Centers for Medicare
and Medicaid (CMS), they are not identical. Facilities
accredited by e Joint Commission must be in compliance
with e Joint Commission standards, unless the standards
required by the Baker Act or CMS are more stringent on a
given subject.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Emergency TreatmentAppendix I - 18
I

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix J - 1 Involuntary Placement
Appendix J
J
Involuntary Inpatient Placement
s. 394.467, F.S. Chapter 65E-5.290, F.A.C.
e Baker Act encourages people to seek and receive voluntary
psychiatric care, but only when they are able to understand
the decision and its consequences and are able to fully exercise
their rights for themselves.
When individuals cannot understand and cannot fully exercise
their rights due to the severity of their condition, the law
requires that they be extended the due process rights assured
under the involuntary provisions of the Baker Act.
Involuntary inpatient placement (commitment) only occurs
after an examination and court hearing.
Criteria
s. 394.467(1), F.S.
A person may be involuntarily placed for inpatient treatment
upon a nding of the court by clear and convincing evidence
that he or she has a mental illness and because of his/her
mental illness:
1. He/she has refused voluntary placement for treatment
after sucient and conscientious explanation and
disclosure of the purpose of placement for treatment;
or he/she is unable to determine for himself or herself
whether placement is necessary; and
2. He/she is manifestly incapable of surviving alone or with
the help of willing and responsible family or friends,
including available alternative services, and without
treatment is likely to suer from neglect or refuse to care
for himself or herself, and such neglect or refusal poses a
real and present threat of substantial harm to his or her
well-being; or
3. ere is substantial likelihood that in the near future he or
she will inict serious bodily harm on himself or herself or
another person, as evidenced by recent behavior causing,
attempting, or threatening such harm; and
4. All available less restrictive treatment alternatives which
would oer an opportunity for improvement of his or her
condition have been judged to be inappropriate.
Each allegation must be supported by evidence sucient to
reach the high level of evidence required in the involuntary
inpatient placement hearing. Appellate courts have found that
expert opinions and conclusions are not sucient, without
evidence to prove the allegations. e Florida Supreme Court
dened clear and convincing evidence to mean:
Evidence that is precise, explicit, lacking in confusion, and
of such weight that it produces a rm belief or conviction,
without hesitation, about the matter at issue.
Initiation of Involuntary
Inpatient Placement
s. 394.467(2), F.S.
After an examination, a person meeting involuntary
inpatient placement criteria must be held pending a
court hearing. e hearing is initiated based upon the
recommendation of the administrator of a receiving facility
where the person has been examined.
e recommendation must be supported by the opinion
of a psychiatrist and the second opinion of a clinical
psychologist or another psychiatrist, both of whom have
personally examined the individual within the preceding
72 hours, that the criteria for involuntary inpatient
placement are met. e second opinion may be conducted
by electronic means in which all parties maintain visual
as well as audio communication. However, in counties of
less than 50,000 population, if the administrator certies
that no psychiatrist or clinical psychologist is available to
provide the second opinion, such second opinion may be
provided by a licensed physician with postgraduate training
and experience in diagnosis and treatment of mental and
nervous disorders or by a psychiatric nurse.
e recommendation must be entered on an involuntary
inpatient placement certicate (CF-MH 3032) or other
form approved by the court, which authorizes the receiving
facility to retain the person pending transfer to a treatment
facility or completion of a hearing.
Petition for Involuntary
Inpatient Placement
s. 394.467(3), F.S.
e administrator of the facility must le a petition for
involuntary inpatient placement (CF-MH 3032) or other
form approved by the court in the county where the person
is located.
Upon ling, the clerk of the court must provide copies
to the department, the person, the person’s guardian or
representative, and the state attorney and public defender
of the judicial circuit in which the person is located. No fee
can be charged for the ling of a petition for involuntary
inpatient placement.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary PlacementAppendix J - 2
J
Appointment of Counsel
s. 394.467(4), F.S.
Within one court working day after the ling of a
petition for involuntary inpatient placement, the court
must appoint the public defender to represent the person
who is the subject of the petition, unless the person is
otherwise represented by counsel. e clerk of the court
must immediately notify the public defender of such
appointment.
Any attorney representing the person shall have access to the
person, witnesses, and records relevant to the presentation
of the person’s case and shall represent the interests of the
person, regardless of the source of payment to the attorney.
e state attorney for the circuit in which the person is located
must represent the state, rather than the petitioning facility
administrator, as the real party in interest in the proceeding.
Continuance of Hearing
s. 394.467(5), F.S.
e person is entitled, with the concurrence of the person’s
counsel, to at least one continuance of the hearing. e
continuance shall be for a period of up to four weeks. is
continuance may be obtained by counsel for the person
by ling a Notice to Court – Request for Continuance
of Involuntary Placement Hearing (CF-MH 3113) or
other form approved by counsel or the court. Only the
person has standing to make such a request; not the facility
administrator or other parties.
Multiple continuances should not be sought to avoid
placement unless legally sucient express and informed
consent has been obtained for the person’s treatment.
Otherwise, facilities lack authority to routinely treat many
persons being held pending hearing.
Independent Expert Examination
s. 394.467(6)(a)2, F.S.
e person and the person’s guardian or representative must
be informed by the court of the right to an independent
expert examination. Recommended form “Application
for Appointment of Independent Expert Examiner”
(CF-MH 3022) may be used. If the person cannot
aord this examination, the court will provide for one.
In August of 2005, the Chair of the Florida Trial Court
Budget Commission advised the Chief Judges and Court
Administrators of all circuits that while the court must
appoint such an independent expert, the expert is a defense
witness and not a court expense. e independent expert’s
report is condential and not discoverable, unless the expert
is to be called as a witness for the person at the hearing.
Hearing on Involuntary
Inpatient Placement
s. 394.467(6), F.S.
e court will hold the hearing on involuntary inpatient
placement within ve court working days after the petition is
led, unless a continuance is granted. e 5th DCA held that
the computation of time for involuntary placement hearings
exclude Saturdays, Sundays, and legal holidays when the time
period is seven days or less. e hearing is not required to be
held within ve calendar days [DMH v. Pietilla, 33So. 3d
800 (Fla 5th DCA 2010)].
e hearing must be held in the county where the person is
located and must be as convenient to the person as may be
consistent with orderly procedure and must be conducted
in physical settings not likely to be injurious to the person’s
condition.
e court may appoint a magistrate to preside at the
hearing.
One of the two professionals who executed the
involuntary placement certicate must be a witness. is
role cannot be delegated to others.
e testimony in the hearing must be given under oath,
and the proceedings must be recorded. e person may
refuse to testify at the hearing.
If the court nds that the person’s attendance at the
hearing is not consistent with the best interests of the
person, and the person’s counsel does not object, the
court may waive the presence of the person from all
or any portion of the hearing. Several appellate courts
have ruled that if the patient waives his/her right to
be personally present and be constructively present
through counsel, the trial court must certify through
proper inquiry that a respondent’s waiver is knowing,
intelligent, and voluntary.
At the hearing on involuntary inpatient placement, the court
must consider testimony and evidence regarding the person’s
competence to consent to treatment. If the court nds that
the person is incompetent to consent to treatment, it must
appoint a guardian advocate (CF-MH 3107 or other form
approved by the court) as provided in s. 394.4598, F.S.
If the placement sought for the person is a state treatment
facility, the court must receive and consider the information
documented in the statutorily required Transfer Evaluation
(CF-MH 3089). e person who conducted the transfer
evaluation, or in the absence of the evaluator, another

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix J - 3 Involuntary Placement
Appendix J
J
knowledgeable sta employed by the community mental
health center or clinic, must be present at the hearing to
provide testimony as desired by the court.
If at any time prior to the conclusion of the hearing on
involuntary inpatient placement it appears to the court
that the person does not meet the criteria for involuntary
inpatient placement but instead meets the criteria for
substance abuse involuntary assessment, protective custody,
or involuntary admission pursuant to s. 397.675, F.S.,
then the court may order (Order Requiring Involuntary
Assessment and Stabilization for Substance Abuse and for
Baker Act Discharge of Patient CF-MH 3114 or other
form approved by the court) the person to be admitted for
involuntary assessment for a period of ve days pursuant
to s. 397.6811, F.S. ereafter, all proceedings must be
governed by Chapter 397, F.S. (Marchman Act).
If the court concludes that the person meets the criteria for
involuntary inpatient placement, it must enter an Order for
Involuntary Inpatient Placement (CF-MH 3008 or other
form approved by the court) for a period of up to six months
that:
the person be transferred to a treatment facility, or
if the person is at a treatment facility, that the person be
retained there, or
be treated at any other appropriate receiving or
treatment facility, or
the person receive services from a receiving or treatment
facility on an involuntary basis.
Admission to a Treatment Facility
s. 394.467(6)(e), F.S.
e administrator of the receiving facility must provide a
copy of the court order and adequate documentation of a
person’s mental illness to the administrator of a treatment
facility whenever a person is ordered for involuntary
inpatient placement, whether by civil or criminal court.
Such documentation shall include:
1. Any advance directives made by the person,
2. A psychiatric evaluation of the person,
3. Any evaluations of the person performed by a clinical
psychologist or a clinical social worker,
4. State Mental Health Facilities Admission Form (CF-
MH 7000) with attachments, and
5. Physician to Physician Transfer (CF-MH 7002).
e administrator of a treatment facility may refuse
admission to any person directed to its facilities on an
involuntary basis, whether by civil or criminal court order,
who is not accompanied at the same time by adequate orders
and documentation.
Release of Persons
s. 394.469, F.S. Chapter 65E-5.320, F.A.C.
e facility must discharge a person any time the person no
longer meets any one of the criteria for involuntary inpatient
placement, unless the person has transferred to voluntary
status. If the release or transfer to voluntary status occurs
prior to the hearing on involuntary inpatient placement,
the facility must immediately notify the court by telephone
and by ling a Notication to Court of Withdrawal of
Petition for Hearing on Involuntary Inpatient or Involuntary
Placement (CF-MH 3033).
e administrator must:
1. Discharge the person, unless the person is under a
criminal charge, in which case the person must be
transferred to the custody of the appropriate law
enforcement ocer;
2. Transfer the person to voluntary status on his or her own
authority or at the person’s request, unless the person is
under criminal charge or adjudicated incapacitated. Such
a transfer from involuntary to voluntary status must be
conditioned on the certication by a physician that the
person has the capacity to make well-reasoned, willful,
and knowing decisions about mental health and medical
issues; or
3. Place an improved person, except a person under a
criminal charge, on convalescent status in the care of a
community facility.
Return of Persons
s. 394.467(8), F.S.
When a person at a treatment facility leaves the facility without
authorization, the administrator may authorize a search for
the person and the return of the person to the facility. e
administrator may request the assistance of a law enforcement
agency in the search for and return of the person.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary PlacementAppendix J - 4
J
Procedure for Continued Involuntary
Inpatient Placement
s. 394.467(7), F.S. Chapter 65E-5.300, F.A.C.
Continued involuntary inpatient placement hearings are
conducted by Administrative Law Judges employed by the
State Division of Administrative Hearings, rather than circuit
court judges.
Hearings on petitions for continued involuntary inpatient
placement are administrative hearings and are be conducted
in accordance with the provisions of ss. 120.569 and
120.57(1), F.S. except that any order entered by the
Administrative Law Judge is nal and subject to judicial
review in accordance with s. 120.68, F.S.
e 5th DCA held that while continued involuntary inpatient
placement hearings are administrative, that the circuit court
retains concurrent jurisdiction during the rst six months after
the order is entered. After six months, only the Division of
Administrative Hearings DOAH) has jurisdiction [W.M. v.
State of Florida. No. 5D07-3762. October 10, 2008].
If the person continues to meet the criteria for involuntary
inpatient placement, the administrator must, prior to the
expiration of the period during which the treatment facility
is authorized to retain the person, le a petition requesting
authorization for continued involuntary inpatient placement
(CF-MH 3035).
If continued involuntary inpatient placement is necessary
for a person admitted while serving a criminal sentence,
but whose sentence is about to expire, or for a person
involuntarily placed while a minor but who is about to
reach the age of 18, the administrator must petition the
administrative law judge for an order authorizing continued
involuntary inpatient placement.
e Petition Requesting Authorization for Continued
Involuntary Inpatient Placement (CF-MH 3035) must be
led with:
State of Florida Division of Administrative Hearings
e Desoto Building
1230 Apalachee Parkway
Tallahassee, FL 32399-3060
Phone (850) 488-9675
Suncom 278-9675
Fax Filing (850) 921-6847
And accompanied by:
1. A statement from the person’s physician or clinical
psychologist justifying the request;
2. A brief description of the person’s treatment during the
time he or she was involuntarily placed; and
3. An individualized plan of continued treatment.
Notice of the hearing shall be provided as set forth in
s. 394.4599, F.S.
Unless the person is otherwise represented, he or she must
be represented at the hearing on the petition for continued
involuntary inpatient placement by the public defender of
the circuit in which the facility is located.
If at the hearing, the administrative law judge nds that
attendance at the hearing is not consistent with the best
interests of the person, the administrative law judge may
waive the presence of the person from all or any portion of
the hearing, unless the person, through counsel, objects to
the waiver of presence.
e testimony in the hearing must be under oath, and the
proceedings must be recorded.
If the person has been previously found incompetent to
consent to treatment, the administrative law judge shall
consider testimony and evidence regarding the person’s
competence. If the administrative law judge nds evidence
that the person is now competent to consent to treatment,
the administrative law judge may enter a recommended order
to the court that found the person incompetent to consent to
treatment that the person’s competence be restored and that
any guardian advocate previously appointed be discharged.
(Findings and Recommended Order Restoring Person’s
Competence to Consent to Treatment and Discharging the
Guardian Advocate CF-MH 3116).
If at a hearing it is shown that the person continues to
meet the criteria for involuntary inpatient placement, the
administrative law judge must sign the Order for Continued
Involuntary Inpatient Placement (CF-MH 3031) for a period
not to exceed six months. e same procedure must be
repeated prior to the expiration of each additional period the
person is retained.
*See attached owcharts for Involuntary Inpatient Placement
and Continued Involuntary Inpatient Placement. Also
attached is a Quick Reference Guide for Receiving and
Treatment Facilities regarding Involuntary Inpatient
Placement.
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix J - 5 Involuntary Placement
Appendix J
J
Quick Reference Guide for Receiving and Treatment Facilities
Involuntary Inpatient Placement
If it is determined that the person who has undergone involuntary examination has a mental illness and either refuses voluntary
placement or is unable to determine that such placement is needed and otherwise meets the criteria for involuntary inpatient
placement, the facility shall:
____ Complete the “Petition for Involuntary Inpatient Placement “ (CF-MH 3032), within 72 hours after the person’s arrival at a
receiving facility, signed by:
Psychiatrist who has examined the person within preceding 72 hours; and
Second psychiatrist or clinical psychologist, who has examined person within the preceding 72 hours (2nd opinion may be
conducted by electronic means in which all parties maintain visual and audio communication)
____ File the petition within the 72 hours or, if the 72-hour period ends on a weekend or holiday, no later than the next working day.
____ Provide the person and his/her guardian or representative with copies of the petition and notices, if agreement has been
reached between the clerk of the court and the receiving facility that this function shall be performed by the facility.
____ Explain the above forms to the person.
At the time of admission, the facility must open a clinical record for the person containing the following information and may include the
following completed recommended forms.
If a competent and willing person seeks voluntary admission (after notification of involuntary inpatient placement proceedings):
____ Person must sign “Request for Voluntary Admission (CF-MH 3040, 3097, or 3098)
____ Physician has certified the person’s competence to provide express and informed consent (CF-MH 3104)
____ Facility must provide court with “Notification to Court of Withdrawal of Petition for Hearing on Involuntary Inpatient or
Involuntary Outpatient Placement” (CF-MH 3033), with copies to person’s guardian or representative
____ If physician determines person is of imminent danger, packet of forms prohibiting firearm purchase to clerk of court
If involuntary inpatient placement in a state mental health treatment facility is sought for the person, the following shall be completed:
____ Transfer Evaluation (CF-MH 3089)
____ State Mental Health Facilities Admission Form (CF-MH 7000 with attachments)
____ Physician to Physician Transfer Form (CF-MH 7002)
If the court orders involuntary inpatient placement in a receiving or treatment facility, the following forms must be present in the
person’s clinical record:
____ Order for Involuntary Inpatient Placement (CF-MH 3008) or other form approved by the court
____ General Authorization for Treatment Except Psychotropic Medications (CF-MH 3042a) for those persons appearing to be
competent to consent to treatment or by their guardian or health care surrogate/proxy.
____ Completion of a Specific Authorization for Psychotropic Medications (CF-MH 3042b), prior to the administration of any
psychotropic medications, after a complete disclosure to the person, the guardian, guardian advocate, health care surrogate/
proxy, and to the guardian of a minor as to:
_____ Reason for admission or treatment
_____ Clinically significant interactive effects with other
_____ Proposed treatment, including proposed
medications
psychotropic medications
_____ Similar information on alternative medication which
_____ Purpose of treatment to be provided
may have less severe or serious side effects
_____ Alternative treatments
_____ Potential effects of stopping treatment
_____ Specific dosage range of medications
_____ Approximate length of care
_____ Frequency and method of administration
_____ How treatment will be monitored
_____ Common risks, benefits and common short-term and
_____ Any consent for treatment may be revoked orally or
long-term side effects
in writing before or during the treatment period by
_____ Any contraindications which may exist
the person legally authorized to make health care
decisions on behalf of the person

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary PlacementAppendix J - 6
J
____ Certification of Person’s Competence to Provide Express and Informed Consent (CF-MH 3104) if the person was permitted to
sign a General Authorization for Treatment Except for Psychotropic Medications or a Specific Authorization for Psychotropic
Medications (CF-MH 3042b).
____ Inventory of Personal Effects (CF-MH 3043) documenting property brought by the person to the facility signed by the person, if
able, and witnessed by two staff members.
____ Authorization for Release of Information (CF-MH 3044) completed and signed only when such release is to take place. No blank
forms should be signed by the person or substitute decision-maker.
____ Notice of Right to Petition for Writ of Habeas Corpus or for Redress of Grievances (CF-MH 3036)
____ Signed copy of “Rights of Persons in Mental Health Facilities and Programs” (CF-MH 3103), after explanation given to person.
____ Documentation of a physical examination by a licensed health practitioner within 24 hours of arrival
____ Personal Safety Plan (CF-MH 3124)
____ An individualized treatment plan completed within five days of the person’s admission in which the person has had the
opportunity to assist in preparing, including space for the person’s comments and a copy of which has been provided to the
person, guardian, guardian advocate, and a minor’s guardian.
The following forms shall be included only if applicable:
____ Authorization for Electroconvulsive Treatment (CF-MH 3057)
____ Refusal or Revocation of Consent to Treatment (CF-MH 3105)
____ Restriction of Communication or Visitors (CF-MH 3049)
____ Restriction of Person’s Access to Own Record (CF-MH 3110)
____ Petition for Writ of Habeas Corpus or for Redress of Grievances (CF-MH 3090)
____ Application for and Notice of Transfer to Another Facility (CF-MH 3046)
____ Notification to Court of Withdrawal of Petition for Hearing on Involuntary Inpatient or Involuntary Outpatient Placement (CF-
MH 3033)
____ Notice of Release or Discharge (CF-MH 3038)
____ Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a Guardian Advocate (CF-MH 3106)
____ Order Appointing Guardian Advocate (CF-MH 3107)
____ Certification of Guardian Advocate Training Completion (CF-MH 3120)
____ Petition Requesting Court Approval for Guardian Advocate to Consent to Extraordinary Treatment (CF-MH 3108)
____ Order Authorizing Guardian Advocate to Consent to Extraordinary Treatment (CF-MH 3109)
At least 20 days prior to the expiration date of a person’s authorized period of involuntary inpatient placement:
____ Petition Requesting Authorization for Continued Involuntary Inpatient Placement (CF-MH 3035) shall be filed with the Division
of Administrative Hearings.
____ Notice of Petition for Continued Involuntary Inpatient Placement (CF-MH 3024)
____ Order for Continued Involuntary Inpatient Placement or Release (CF-MH 3031)
Recommended forms are those which are not required by the department, but which have been determined to satisfy the specific
requirements for which the form has been developed. Alteration of recommended forms may jeopardize this status. Mandatory forms
may not be altered. No blank forms should be signed by staff, the person, or substitute decision-maker.
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix J - 7 Involuntary Placement
Appendix J
Involuntary Inpatient Placement
s. 394.467, F.S. Chapter 65E-5.290, F.A.C.
Psychiatrist determines person does meet all criteria
for involuntary inpatient placement
Psychiatrist determines person does not meet one
or more of the criteria and person is discharged or
if person meets criteria for voluntary admission,
may be transferred to voluntar y status and required
notices given
Two opinions entered on petition for involuntary
inpatient placement, signed by administrator, and filed
with court within the 72 hour exam period
Hearing held within 5 working days by judge or
magistrate. Person's competence to consent to
treatment is considered and if found to be incompetent,
Guardian Advocate appointed (BA3107)
Court appoints a PD in 1 working day unless person
otherwise represented by counsel and notifies person of
right to an independent expert examination (BA3022)
Clerk immediately notifies PD of appointment and
SAO which represents the state as real party in
interest
Clerk provides copy of petition (BA3032) and notice
of Hearing (BA-3024) to DCF, person, guardian or
representative, state attorney, and public defender
Meets all criteria for involuntary inpatient
placement
Court ordered (BA3008) to treatment facility or
receiving facility for period of up to 6 months.
Clerk submits firearm Prohibition to FDLE.
Incompetent to consent to treatment
Guardian advocate appointed
Competent to consent to treatment
May consent or refuse to consent
to own treatment
Court ordered for 5 day substance
abuse impairment involuntary
assessment. Clerk submits Firearm
Prohibition to FDLE.
Criteria: Finding by court by clear and convincing evidence that the person has a mental illness and because of the mental illness
Person refused or unable to determine whether voluntary placement is necessary; and
Likely to suffer from self-neglect or harm self or others; and
All available less restrictive treatment alternatives judged to be inappropriate
Person meets criteria for involuntary
assessment, protective custody, or
involuntary admission pursuant to
Marchman Act
Second psychiatrist or a psychologist performs examination.
Second opinion can be done by electronic means if all parties
maintain visual and audio communication. If second professional
Person discharged
Does not meet one or more
criteria for involuntary inpatient
placement
J

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Placement
J
Continued Involuntary Inpatient Placement
s. 394.467(7), F.S. Chapter 65E-5.300, F.A.C.
Criteria: Finding by administrative law judge, by clear and convincing evidence, that person has a mental
illness and because of the mental illness
Person refused or unable to determine whether voluntary placement is necessary; and
Likely to suffer from self-neglect or harm to self or others; and
All available less restrictive treatment alternatives judged to be inappropriate
Prior to end of period facility is authorized to retain person, or for person placed while a minor but
about to reach age of 18, or person admitted while serving a criminal sentence but whose sentence
is about to expire; a petition for continued involuntary inpatient placement may be filed with the
state Division of Administrative Hearings (DOAH) for persons continuing to meet criteria, as follows:
Administrative law judge signs order
(BA3031) for continued involuntary inpatient
placement for up to 6 months
Person does not meet one or more placement criteria
Person continues to meet all placement criteria
Petition (BA3035) filed by facility administrator with
State Division of Administrative Hearings
Notice of hearing (BA3024) provided to person,
attorney, representative
Appointment of PD
Testimony under oath and proceedings recorded
If previously found incompetent to consent to
treatment, shall consider testimony about person's
competence
Does not meet all criteria
Person discharged or
transferred to voluntary
status
Appears to be competent
to consent to own
treatment
Administrative law judge sends
recommended order (BA3116) to court for
restoration of competency to consent and
discharge of guardian advocate
Continues to be
incompetent to consent
to treatment
Facility shall discharge a person any time the
person no longer meets all criteria for involuntary
inpatient placement unless the person has been
transferred to voluntary status
Appendix J - 8

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix K - 1
Involuntary Outpatient Placement
Appendix K
K
Involuntary Outpatient Placement
s.394.4655, F.S. s. 65E-5.285, F.A.C
Introduction
e 2004 Florida Legislature enacted a major revision to
the Florida Mental Health Act by adding an involuntary
outpatient placement provision to the involuntary
examination and involuntary inpatient placement provisions.
is revision was made eective on January 1, 2005.
e Legislature permits the administrator of a Baker Act
receiving facility or treatment facility to le a petition for
involuntary placement in the circuit court when outpatient or
inpatient treatment is deemed necessary. e Legislature also
stated that any person for whom an involuntary examination
has been initiated who is being evaluated or treated at a
hospital for an emergency medical condition can be released
by a physician or clinical psychologist if found not to meet the
criteria for involuntary inpatient or outpatient placement.
Rights of Persons
Rights of persons incorporated in the Florida Mental
Health Act apply to all persons whose services are governed
by the Baker Act – voluntary or involuntary and inpatient
or outpatient.
Each person must receive services, including those under
an involuntary outpatient placement court order which are
suited to his or her needs, and which must be administered
skillfully, safely, and humanely with full respect for the
person’s dignity and personal integrity.
Criteria
A person may be ordered to involuntary outpatient placement
upon a nding of the court by clear and convincing evidence
that each criterion below has been met. Each allegation must
be supported by evidence sucient to reach the high level of
evidence required in the involuntary outpatient placement
hearing. Appellate courts have found that expert opinions
and conclusions are not sucient, without evidence to prove
the allegations. e Florida Supreme Court dened clear and
convincing evidence to mean:
Evidence that is precise, explicit, lacking in confusion, and
of such weight that it produces a rm belief or conviction,
without hesitation, about the matter at issue.
e criteria are as follows:
1. Person is 18 years of age or older. Evidence of age must
be substantiated, whenever there is any question as to
whether the person may be age 18 or older.
2. Person has a mental illness. A diagnosis of mental
illness shall be substantiated by two professionals as
provided in Section 394.4655(2)(a), F.S. who have
recently examined the person and whose observations of
the person’s condition are consistent with the statutory
denition of mental illness, pursuant to Section
394.455(18), F.S., and the clinical description of that
diagnosis as described in the Diagnostic and Statistical
Manual of Mental Disorders, Fourth Edition, Text
Revision, American Psychiatric Association, which may
be obtained from the American Psychiatric Association,
1000 Wilson Boulevard, Arlington, VA 22209-3901.
3. Person is unlikely to survive safely in the community
without supervision, based on a clinical determination.
e clinical determination that a person is unlikely to
survive safely in the community without supervision
must be substantiated by evidence of current or past
behaviors.
4. Person has a history of non-compliance with treatment.
e person’s history of lack of compliance with
treatment for mental illness must be substantiated by
evidence showing specic previous incidents in which
the person was non-compliant with treatment, including
time periods in which the person was non-compliant
with treatment.
5. Person has either:
a. At least twice within last 36 months been
involuntarily admitted to receiving or treatment
facility or received mental health services in a
forensic or correctional facility or
b. Engaged in one or more acts of serious violent
behavior toward self or others, or attempts at serious
bodily harm to self or others, within the preceding
36 months.
In either of the above circumstances, ocial clinical
or legal documents must document that the person
was in fact admitted to and treated at such facilities in
the required time period. e person’s involuntarily
admission to a receiving or treatment facility or the
mental health services in a forensic or correctional
facility at least twice in the preceding 36 months, or the
person’s acts of serious violent behavior toward self or
others or attempted serious bodily harm to self or others
at least once during the preceding 36 months, shall be
substantiated by evidence.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Outpatient Placement
Appendix K - 2
K
6. Person is as a result of mental illness, unlikely to
voluntarily participate in the recommended treatment
plan and has either refused voluntary placement or is
unable to determine whether placement is necessary.
Evidence of the unlikelihood of the person to
voluntarily participate in the recommended treatment
plan, and either his or her refusal of voluntary
placement or inability to determine whether placement
is necessary must be substantiated by behaviors, events,
and statements by the person supporting this nding.
7. In view of person’s treatment history and current
behavior, the person is in need of involuntary outpatient
placement in order to prevent a relapse or deterioration
that would be likely to result in serious bodily harm to
self or others, or a substantial harm to his/her well-being.
Evidence of the person’s treatment history and current
behavior must be presented, including time periods of
such treatment to substantiate the conclusion that the
person needs involuntary placement in order to prevent
a relapse or deterioration that would be likely to result in
serious bodily harm to self or others or a substantial harm
to his or her well-being.
8. It is likely the person will benet from involuntary
outpatient placement. Evidence must be presented
to substantiate the likelihood of how the person will
benet from involuntary outpatient placement.
9. All available less restrictive alternatives that would oer
an opportunity for improvement of his or her condition
have been judged to be inappropriate or unavailable.
Evidence must be presented to substantiate each less
restrictive alternative that was examined that would
have oered an opportunity for the improvement of the
person’s condition.
e person must meet all the above criteria.
Petition
If a person is not released or transferred to voluntary
status within 72 hours after arrival at a receiving facility,
a petition for involuntary placement must be led with
the circuit court by the facility administrator within the
72-hour examination period, or if the 72 hours ends on a
weekend or legal holiday, the petition must be led no later
than the next court working day thereafter. If involuntary
outpatient placement is sought the form titled, “Petition for
Involuntary Outpatient Placement,” (CF-MH 3130) can be
used. A copy of the completed petition must be retained in
the person’s clinical record.
A petition by a Receiving Facility administrator must be
led in the circuit court where the facility is located. is
authorizes the person’s retention pending a hearing. If the
person has been stabilized and no longer meets the criteria for
involuntary examination, he/she must be released from the
receiving facility while awaiting the hearing on involuntary
outpatient placement. e petition must include a certicate
recommending placement completed by psychiatrist and a
psychologist or 2nd psychiatrist, both of who have examined
the person within the preceding 72 hours, that each of the
criteria for involuntary outpatient placement are met. A copy
of a proposed treatment plan must be attached. No fee can be
charged for filing of petition.
A Petition by a Treatment Facility administrator must be
led in the circuit court where the person will be living. A
copy of the petition, state mental health discharge form, and
a treatment plan prepared by the designated service provider
must be given to the DCF representative in the circuit where
person is to reside at the time it is led with the circuit court.
Service Provider
Prior to ling the petition for involuntary outpatient
placement, the receiving or treatment facility administrator
or DCF must identify the service provider that will have
primary responsibility for court ordered treatment. If the
person is currently participating in outpatient treatment
and is not in need of public nancing for that treatment,
the person, if eligible, may be ordered to involuntary
treatment to the existing psychiatric treatment relationship.
However, a proposed treatment plan must still be prepared,
in accordance with the law and rules, for submission to the
court with the petition.
A service provider, in the context of the Baker Act is dened as:
A public or private receiving facility
An entity under contract with DCF to provide mental
health services
A clinical psychologist
A licensed clinical social worker
A licensed mental health counselor
A licensed marriage and family therapist
A physician
A psychiatric nurse (as dened in the Baker Act), or
A community mental health center or clinic.
e department or receiving facility must designate which
service provider will be responsible for developing a treatment
plan for the person and for service provision. Recommended
form titled “Designation of Service Provider for Involuntary
Outpatient Placement” (CF-MH 3140) may be used.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix K - 3
Involuntary Outpatient Placement
Appendix K
K
No petition for involuntary outpatient placement may
be led with a court by a receiving or treatment facility
administrator unless a treatment plan, complying with the
requirements of the law and rule is attached to the petition,
along with a certication from the service provider that:
e proposed services are available,
ere is space for the person in the program,
ere is funding available,
e services proposed are clinically appropriate as
certied by an authorized mental health professional,
and
at the service provider agrees to provide the services.
Recommended form titled “Proposed Individualized
Treatment Plan for Involuntary Outpatient Placement and
Continued Involuntary Outpatient Placement” (CF-MH
3145) may be used.
Treatment Plan
A service provider must prepare a written proposed
treatment plan in consultation with person or guardian
advocate for the court’s consideration in an involuntary
outpatient treatment order. e treatment plan must specify:
Nature and extent of the person’s mental illness
Reduction of symptoms and include measurable
treatment goals and objectives
How the person will be assisted in living and
functioning or prevent relapse or deterioration
Services proposed in the treatment plan must be deemed
clinically appropriate by a physician, psychologist, clinical
social worker, mental health counselor, marriage and family
therapist, or psychiatric nurse.
e service provider selected by the receiving facility or DCF
to develop/render a service plan may select and supervise
others to implement aspects of the treatment plan. e
service provider must certify to court that the services in
plan are currently available and that the service provider
agrees to provide them.
e condentiality provisions of the Baker Act have been
revised for purpose of determining whether a person meets
the criteria for involuntary outpatient placement or for
preparing the proposed treatment plan. While any release
must be in accordance with state and federal law, the clinical
record may be released for this purpose to the:
State attorney,
Public defender or the person’s private legal counsel
Court, and
Appropriate mental health professionals, including the
service provider.
County of Filing
e petition initiated by a receiving facility administrator
must be led in the county where the facility is located.
e petition for involuntary outpatient placement initiated
by a treatment facility administrator must be led in the
county where the person will be living after discharge from
the facility. It must be led prior to the expiration of the
involuntary inpatient placement order. A copy of form
titled “State Mental Health Facility Discharge Form” (CF-
MH 7001) must be attached to the petition. e service
provider designated by the department that will have
primary responsibility for service provision must provide a
certication to the court, attached to the petition, whether
the services recommended in the discharge plan are available
in the local community and whether the provider agrees to
provide those services. Also attached to the petition must be
an individualized treatment or service plan that addresses
the needs identied in the discharge plan developed by the
treatment facility. Recommended form titled “Proposed
Individualized Treatment Plan for Involuntary Outpatient
Placement and Continued Involuntary Outpatient Placement
(CF-MH 3145) may be used. is plan must have been
deemed to be clinically appropriate by a physician, clinical
psychologist, clinical social worker, mental health counselor,
marriage and family therapist, or psychiatric nurse, as defined
in the Baker Act.
Notice of Petition
A copy of the petition for involuntary outpatient placement
and proposed treatment plan must be provided within one
working day after ling by the clerk of the court to the:
Respondent,
Department of Children & Families,
Guardian or representative,
State attorney, and
Counsel for the respondent.
A notice of ling of the petition must also be provided by
the clerk of court. Recommended form titled “Notice of
Petition for Involuntary Placement” (CF-MH 3021) or other
equivalent form adopted by the court may be used.
e person and his or her representative or guardian must
be informed by the court of the right to an independent

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Outpatient Placement
Appendix K - 4
K
expert examination and that if the person cannot aord
such an examination, the court shall provide for one.
In August of 2005, the Chair of the Florida Trial Court
Budget Commission advised the Chief Judges and Court
Administrators of all circuits that while the court must
appoint such an independent expert, the expert is a defense
witness and not a court expense. Recommended form
titled “Application for Appointment of Independent Expert
Examiner” (CF-MH 3022) may be used. e results of the
examination by an independent expert are condential and
not discoverable unless the expert is called as a witness.
Hearing
A hearing on the petition for involuntary outpatient
placement must be conducted within 5 working days after
the ling of the petition in the county in which the petition
is led.
e person is entitled, with the concurrence of counsel, to
at least one continuance of the hearing, for a period of up
to 4 weeks. Recommended form titled “Notice to Court –
Request for Continuance of Involuntary Placement Hearing”
(CF-MH 3113) may be used.
e Public Defender must be appointed by the court within
1 court working day after the petition is led, unless the
person is otherwise represented by private counsel. Counsel
for the person shall serve until the petition is dismissed,
the court order expires, or the person is discharged from
placement. e State attorney represents the state as the real
party in interest in the proceedings.
e hearing must be conducted in a setting as convenient to
the person as consistent with orderly procedure and not likely
to be harmful to person. A judge or magistrate may preside.
If the facility administrator seeks to withdraw the petition
for involuntary outpatient placement prior to the hearing,
recommended form 3033 titled “Notication to Court
of Withdrawal of Petition on Involuntary Inpatient or
Outpatient Placement” may be used. e facility must
retain a copy in the person’s clinical record. When a facility
withdraws a petition for involuntary placement, it must
notify by telephone the court, state attorney, attorney for the
person, and guardian or representative within one business
day of its decision to withdraw the petition unless the
decision is made within 24 hours prior to the hearing. In
such cases, the notication must be made immediately.
e Court must hear testimony and evidence regarding the
person’s competence to consent to treatment. If the person
is found incompetent, the Court must appoint a guardian
advocate. e guardian advocate appointed by the court for a
person who has been found to be incompetent to consent to
treatment must be discharged when:
e person is discharged from an order for involuntary
outpatient placement, or involuntary inpatient
placement, or
e person is transferred from involuntary to voluntary
status.
If the court determines the person instead meets the criteria
for involuntary inpatient placement, use of recommended
form titled “Ex Parte Order for Involuntary Inpatient
Examination” (CF-MH 3001) may be used.
If the court determines the person meets the criteria for
involuntary assessment, protective custody, or involuntary
admission, and issues an order, recommended form titled
“Order Requiring Involuntary Assessment and Stabilization
for Substance Abuse and for Baker Act Discharge of Person”
(CF-MH 3114) may be used.
If at any time prior to conclusion of the hearing on
involuntary inpatient placement, it appears to the court
that the person does not meet criteria for involuntary
inpatient placement but instead meets criteria for involuntary
outpatient placement, the court may order the person
evaluated for involuntary outpatient placement.
Testimony
All testimony must be given under oath and must be
recorded.
e court may waive the presence of the person from
all or any part of the hearing if consistent with the best
interests of the person and the person’s counsel does not
object. Several appellate courts have ruled that if the
patient waives his/her right to be personally present and
be constructively present through counsel, the trial court
must certify through proper inquiry that a respondent’s
waiver is knowing, intelligent, and voluntary. e person
may refuse to testify at the hearing.
One of the two professionals who executed involuntary
outpatient placement certicate must be a witness at the
hearing.
In addition to one of the two professionals who executed
the petition, other sta from the receiving or treatment
facility who have direct knowledge of how the person
meets the criteria for involuntary outpatient placement
and are expected to testify in support of the petition
must be identied on the petition and be present to
testify at the hearing, as desired by the court.
e court shall also allow testimony from individuals,
including family members, deemed by the court to

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix K - 5
Involuntary Outpatient Placement
Appendix K
K
be relevant, regarding the person’s prior history and
how that prior history relates to the person’s current
condition. Such testimony must be factual as to events
and dates, rather than only opinions and conclusions.
A representative of the designated service provider must
be present to provide testimony about the proposed
treatment or service plan as desired by the court
Court Order
If the court nds that the person meets all criteria for
involuntary outpatient placement, it shall issue an order
for a period of up to 6 months. Recommended form
titled “Order for Involuntary Outpatient Placement or
Continued Involuntary Outpatient Placement” (CF-MH
3155) may be used.
e court can’t order services that are not available in the
person’s local community, if no space is available, if funding
isn’t available, if the treatment plan hasn’t been certied
as clinically appropriate by an authorized mental health
professional, and if an eligible service provider hasn’t agreed
to provide the recommended services.
is signed order must be given to the person, guardian,
guardian advocate or representative, counsel for the person,
state attorney, and administrator of the receiving or treatment
facility, with a copy of the order retained in the person’s
clinical record.
A copy of the court order must also be sent by the service
provider to AHCA within one working day after received
from the court accompanied by mandatory form titled
“Cover Sheet to Agency for Health Care Administration”
(CF-MH 3118) to: BA Reporting Center, FMHI-MHC
2637, 13301 Bruce B. Downs Boulevard, Tampa, Florida
33612-3807.
e court order and treatment plan must be part of person’s
clinical record.
Continued Involuntary
Outpatient Placement
Criteria
If the person continues to meet the criteria for involuntary
outpatient placement, the service provider must, prior to
end of the court order, le in the circuit court a petition for
continued involuntary outpatient placement. e existing
order remains in eect until the continued involuntary
outpatient placement petition is disposed of.
Criteria for continued involuntary outpatient placement
are identical to the criteria for the original order, except that
the 36-month time period for having been at least twice
involuntarily admitted to a receiving/treatment facility or
received mental health services in a forensic or correctional
facility; or engaged in one or more acts of serious violent
behavior toward self/others, or attempts at serious bodily
harm to self/others is not applicable in determining the
appropriateness of additional periods of involuntary
outpatient placement.
Petition
In order to request continued involuntary outpatient
placement, the service provider administrator shall, prior
to the expiration of the period for which the treatment was
ordered, le a petition for continued involuntary outpatient
placement with the circuit court. Recommended form
titled “Petition Requesting Authorization for Continued
Involuntary Outpatient Placement” (CF-MH 3180) may be
used. e petition must be led with the circuit court in the
county where the person who is the subject of the petition
resides.
e petition must include:
A statement from person’s physician or clinical
psychologist justifying the request,
A brief description of person’s treatment during the
order,
An individualized plan of continued treatment
developed by the service provider, in consultation with
person or the guardian advocate, if appointed.
Notice of Petition for Continued
Involuntary Outpatient Placement
e clerk of court must provide copies of the petition and
attachments to the person, DCF, guardian advocate, state
attorney, and the person’s public defender or private counsel.
e clerk of court must provide notice of the hearing.
Recommended form titled “Notice of Petition for
Involuntary Placement” (CF-MH 3021) may be used.
Copies must be provided to the person, his or her attorney,
the state attorney, and guardian, guardian advocate or
representative, with a copy of the notice led in the person’s
clinical record.
Written notice of ling of petition for involuntary placement
must contain notice of:
Petition led with the circuit court in county where
person is hospitalized (receiving facility) or will be living
(treatment facility).
Oce of public defender appointed to represent person
if not otherwise represented by counsel.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Outpatient Placement
Appendix K - 6
K
Date, time, place of hearing, name of each examining
expert and every other person expected to testify in
support of continued involuntary outpatient placement.
e person, guardian, representative or administrator
may apply for change of venue for convenience of parties
or witnesses or because of person’s condition.
e person is entitled to independent expert
examination and, if person cannot aord an
examination, the court will provide for one.
e public defender must be appointed and notied within
1 court working day, who will represent the person until:
e petition is dismissed,
e order expires, or
e person discharged from placement.
e attorney for the person has access to the person,
witnesses and records, and represents interests of the person,
regardless of source of payment to the attorney. e State
Attorney is appointed to represent the state as the real party
in interest, rather than for the petitioner.
Hearing on Continued Involuntary
Outpatient Placement
e court may appoint a magistrate to preside over
continued involuntary placement hearings.
e person and his or her attorney may agree to a period of
continued outpatient placement without a court hearing.
Should such a hearing be waived recommended form titled
“Notice to Court of Waiver of Continued Involuntary
Outpatient Placement Hearing and Request for Order” (CF-
MH 3185) may be used.
If the person was previously found incompetent to consent to
treatment, the court must consider testimony and evidence
regarding the person’s competence. e guardian advocate
must be dismissed if the person is found competent to make
decisions about his or her own treatment.
If the administrator of the service provider withdraws the
petition for continued involuntary outpatient placement
prior to the hearing, recommended form titled “Notication
to Court of Withdrawal of Petition on Involuntary Inpatient
or Outpatient Placement” (CF-MH 3033) may be used. e
facility will retain a copy of the notice in the person’s clinical
record. When a facility withdraws a petition for involuntary
placement, it must notify the court, state attorney, public
defender or other attorney for the person, and guardian or
representative by telephone within one business day of its
decision to withdraw the petition, unless such decision is
made within 24 hours prior to the hearing. In such cases, the
notication must be made immediately. e same procedure
must be repeated before expiration of each additional period
the person is placed in treatment.
Order for Continued Involuntary
Outpatient Placement
Based on the ndings of the hearing, the court may extend
the period of involuntary outpatient commitment pending
the next statutorily required periodic hearing, release the
person from involuntary outpatient placement, or nd
the person eligible for voluntary status. Recommended
form titled “Order for Continued Involuntary Inpatient
Placement or for Release” (CF-MH 3031) may be used. A
copy of the completed order must be led in the person’s
clinical record and a copy provided to the person, attorney,
facility administrator, and guardian, guardian advocate or
representative.
A copy of the order must be sent to the Agency for Health
Care Administration by the designated service provider,
accompanied by mandatory form titled “Cover Sheet to
Agency for Health Care Administration” (CF-MH 3118) to:
BA Reporting Center, FMHI-MHC 2637, 13301 Bruce B.
Downs Boulevard, Tampa, Florida 33612-3807.
Modification to Court Order for
Involuntary Outpatient Placement
After an order for involuntary outpatient placement or
continued involuntary outpatient placement is entered,
the provider and the person (or his or her substitute
decision-maker, if appointed) may modify provisions of the
treatment plan. Any material modications where parties
agree require the provider to notice the court. If material
modications are contested, the court must approve or
disapprove the modications.
At any time material modications are proposed to the
court ordered treatment plan for which the person and
his or her substitute decision maker, if any, agree, or if
the person or his substitute decision-maker object to the
modications proposed by the service provider or wish
to propose modications not proposed by the service
provider, recommended petition titled “Notice to Court of
Modication to Treatment Plan for Involuntary Outpatient
Commitment and/or Petition Requesting Approval of
Material Modications to Plan” (CF-MH 3160) may be used.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix K - 7
Involuntary Outpatient Placement
Appendix K
K
Change of Service Provider
If the person who is subject to an order for involuntary
outpatient placement (or his or her substitute decision-
maker, if appointed) objects to the service provider that is
court ordered to provide his or her treatment or services,
recommended form titled “Notice to Court of Modication
to Treatment Plan for Involuntary Outpatient Commitment
and/or Petition Requesting Approval of Material
Modications to Plan” (CF-MH 3160) may be used.
Non-Compliance with Court Order
If a physician has determined that the person who is subject
to a court order for involuntary outpatient placement or
continued involuntary outpatient placement has failed or
has refused to comply with the treatment ordered by the
court, and in his or her clinical judgment, eorts were
made to solicit compliance and the person meets the
criteria for involuntary examination, the person may be
brought to a receiving facility pursuant to the involuntary
examination requirements of the Baker Act. Mandatory form
titled “Certicate of a Professional Initiating Involuntary
Examination” (CF-MH 3052b) may be used.
If the person doesn’t meet criteria for involuntary inpatient
placement, the person must be discharged from the receiving
facility.
e service provider must determine whether modications
should be made to the existing treatment plan and must
attempt to continue to engage the person in treatment.
Discharge from Involuntary
Outpatient Placement
A service provider has a duty to discharge a person at any
time the order for involuntary outpatient placement or
continued involuntary outpatient placement expires or at any
time the person no longer meets the criteria for involuntary
outpatient placement or to transfer the person to voluntary
status, if the person is able and willing to provide express and
informed consent.
Upon the person’s discharge, the service provider must send
a notice of discharge to the court. Recommended form titled
“Notice of Release or Discharge” (CF-MH 3038) may be
used. e administrator of the service provider will provide
notication to the person, guardian, guardian advocate,
representative, attorney for the person, and the court that
ordered such treatment, and a copy of the notice must be
placed in the person’s clinical record.
At any time the person who is subject to an order for
involuntary outpatient placement or continued involuntary
outpatient placement, or another person on his or her behalf,
believes any one of the criteria for involuntary outpatient
placement is no longer met, a petition for termination of the
order may be led with the circuit court having jurisdiction.
Recommended form titled “Petition for Termination
of Involuntary Outpatient Placement Order (CF-MH
3170) may be used. If the court determines a hearing on
the petition is to be conducted, a notice of the hearing, as
required by law, shall be provided by the clerk of court.
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Outpatient Placement
Appendix K - 8
K
Involuntary Outpatient Placement
s.394.4655, F.S. s. 65E-5.285, F.A.C
Criteria: Finding by court by clear and convincing evidence that an adult has a mental illness and
Is unlikely to survive safely in the community without supervision
Has a history of non-compliance with treatment
Has either at least twice within last 36 months been involuntarily admitted to receiving or treatment facility or received MH services in a forensic
or correctional facility; or engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm to self
or others, within the preceding 36 months;
Is unlikely to voluntarily participate in the recommended treatment plan and has either refused voluntary placement or is unable to determine
whether placement is necessary
Is in need of involuntary outpatient placement in order to prevent a relapse or deterioration that would be likely to result in serious bodily harm
to self or others, or a substantial harm to his/her well-being.
It is likely the person will benefit from involuntary outpatient placement; and
All available less restrictive alternatives that would offer an opportunity for improvement of his or her condition have been judged to be
inappropriate or unavailable.
Psychiatrist determines person doesn’t
meet one or more criteria and person is
discharged or is transferred to voluntary
status, if eligible
Psychiatrist determines person meets all criteria for involuntary outpatient
placement. Psychologist or second psychiatrist concurs. Both opinions entered
on petition, signed by administrator.
If some or all services needed by person
are unavailable or unfunded, submit
“Notification to DCF of Non-filing of
Petition or Diminished Treatment Plan”
Person discharged from facility
Service provider completes treatment plan in consult with person or guard-
ian/guardian advocate ensuring all proposed services are available and
funded and committing service provider to deliver services
Proposed service plan submitted to physician, psychologist, LCSW, or
psychiatric nurse employed by, consulting with or contracted by service
provider for certication of clinical appropriateness
Petition with treatment plan submitted to Clerk of Court. Copy of petition
and treatment plan sent by Clerk of Court to person, DCF, PD, and ASA
PD and ASA appointed and hearing scheduled within 5 working days
If person found incompetent to consent to own treatment, guardian advo-
cate appointed by court
If all criteria proven by clear and convincing evidence, court order issued
for up to 6 months and remains in affect until service provider determines
person no longer meets criteria or order expires
If person instead meets criteria for invol-
untary inpatient placement, court may
order involuntary exam under 394.463
If person instead meets involuntary ad-
mission criteria for Marchman Act, may
be ordered for 5 day assessment
Copy of court order sent within 1 work-
ing day to BA reporting center
Service Provider selected by DCF or receiving facility to develop treatment
plan

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix K - 9
Involuntary Outpatient Placement
Appendix K
K
Continued Involuntary Outpatient Placement
s.394.4655, F.S. s. 65E-5.285, F.A.C
Criteria: Finding by court by clear and convincing evidence that adult has a mental illness and
Is unlikely to survive safely in community without supervision
Has a history of non-compliance with treatment
Is unlikely to voluntarily participate in the recommended treatment plan and has either refused voluntary placement or is unable to determine
whether placement is necessary
Is in need of involuntary outpatient placement in order to prevent a relapse or deterioration that would be likely to result in serious bodily harm
to self or others, or a substantial harm to his or her well-being.
It is likely the person will benefit from involuntary outpatient placement; and
All available less restrictive alternatives that would offer an opportunity for improvement of his or her condition have been judged to be
inappropriate or unavailable.
If physician or clinical psychologist
determines person doesn’t meet one
or more criteria, person is discharged
or is transferred to voluntary status, if
eligible
Physician or clinical psychologist determines person meets all above criteria for
involuntary outpatient placement, entered on petition, signed by administrator.
Brief description of person’s treatment during placement; and an individualized
plan of continued treatment, developed in consult with person or guardian /
guardian advocate, if appointed, must be attached to petition
Petition, description of past treatment, and proposed treatment plan
submitted by service provider to Clerk of Court who will provide copies to
person, DCF, guardian/guardian advocate, PD and state attorney
Hearing scheduled within 5 working days unless person and his or her
attorney have agreed to waive hearing.
All procedures for initial hearing also apply to continued - same procedure
followed before expiration of each additional period person placed in
treatment.
Court order for up to 6 months of treatment.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Involuntary Outpatient Placement
Appendix K - 10
K
Non-Compliance with Treatment Order
Physician determines person has failed or refused to comply
with treatment ordered by court
Physician determines efforts made to solicit compliance
and person meets criteria for involuntary examination
Physician completes BA52b form, including Section IV, to have
person taken into custody and brought to a receiving facility
If criteria for Involuntary
for examination
Inpatient Placement not
met, person must be
discharged.
Service provider determines what modifications should be
made to existing treatment plan and attempts to continue
to engage person in treatment
Modification to Treatment Plans
Proposed Modification To Court Ordered Treatment Plan
Immaterial Modifications
in which all parties agree
No notice to court or petition
required at this time
If petition for continued involuntary
Material Modifications
No Disagreement from Person/
guardian/guardian advocate
Notice of modification sent to
Clerk of Court for court’s review
Material Modifications
Disagreement of person or
guardian/guardian advocate
Petition filed with Clerk of
Court for Court’s consideration
of whether to approve or
disapprove the recommended
modifications
placement is subsequently filed, a copy
of the modified treatment plan must
If petition was filed
If changes are
be submitted to court as part of the
by person seeking
approved, new order
description of person’s treatment during
termination of order, and
is issued compelling
time of placement
court agrees, order issued
compliance with
discharging person from
modified treatment
treatment
plan
* Material modification defined as “Important, more or less necessary, having influence or effect, going to the merits, having to do
with matter rather than form.”
** Material modification to treatment plan can be initiated by person, guardian, guardian/advocate or service provider

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix L - 1
Professional Credentials
Appendix L
L
Qualifications of Professionals & Others
to Perform Baker Act Related Functions
Cautionary Note:
The professionals identified as having some role in the examination or treatment of persons under the Baker Act law are specifically
defined in the Baker Act [Ch. 394, Part 1, Florida Statutes].
Some of these definitions differ from those in the professional licensing laws. Where difference between the Baker
Act and the licensing laws occur, the Baker Act, as the more specific statute, prevails.
The Baker Act and related rules may limit what some professionals are authorized to do more narrowly than under
the scope of practice specified in their license laws. Where there are differences between the Baker Act and the
professional scope of practice occur, the Baker Act as the more specific statute prevails.
If the Baker Act and related rules do not specify a particular definition or limitation as to which professional is
authorized to perform a particular function, the scope of practice identified in the professional’s license law
prevails.
The Department of Children and Families has proposed modification to the Baker Act definitions of certain professionals to bring
these definitions more closely in line with those in the professional licensing statutes. DCF has also proposed several changes
in which professionals can conduct specific roles. However, until the Florida Legislature enacts these proposed changes, the
information in this appendix must be followed.
Definitions
e Baker Act denes various professionals and other
categories of persons involved in providing services to and
protecting the rights of persons on voluntary and involuntary
status undergoing examination and treatment provisions of
the law as follows:
“Administrator” means the chief administrative ocer
of a receiving or treatment facility or his or her designee.
[394.455(1), F.S.]
“Clinical psychologist” means a psychologist as dened
in s. 490.003(7) with 3 years of postdoctoral experience
in the practice of clinical psychology, inclusive of the
experience required for licensure, or a psychologist
employed by a facility operated by the United
States Department of Veterans Aairs that qualies
as a receiving or treatment facility under this part.
[394.455(2), F.S.]
“Clinical social worker” means a person licensed as a
clinical social worker under chapter 491. [394.455(4), F.S.]
“Guardian” means the natural guardian of a minor, or a
person appointed by a court to act on behalf of a ward’s
person if the ward is a minor or has been adjudicated
incapacitated. [394.455(11), F.S.]
“Guardian advocate” or “GA” means a person appointed
by a court to make decisions regarding mental health
treatment on behalf of a patient who has been found
incompetent to consent to treatment pursuant to this
part. e guardian advocate may be granted specic
additional powers by written order of the court, as
provided in this part. [394.455(12), F.S.]
“Physician” means a medical practitioner licensed
under chapter 458 or chapter 459 who has experience
in the diagnosis and treatment of mental and nervous
disorders or a physician employed by a facility operated
by the United States Department of Veterans Aairs
which qualies as a receiving or treatment facility under
this part. [394.455(21), F.S.]
“Psychiatric nurse” means a registered nurse licensed
under part I of chapter 464 who has a master’s degree or
a doctorate in psychiatric nursing and 2 years of post-
master’s clinical experience under the supervision of a
physician. [394.455(23), F.S.]
“Psychiatrist” means a medical practitioner licensed
under chapter 458 or chapter 459 who has primarily
diagnosed and treated mental and nervous disorders for
a period of not less than 3 years, inclusive of psychiatric
residency. [394.455(24), F.S.]
“Marriage and family therapist” means a person
licensed as a marriage and family therapist under
chapter 491. [394.455(36), F.S.]

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Professional Credentials
Appendix L - 2
L
“Mental health counselor” means a person licensed
as a mental health counselor under chapter 491.
[394.455(37), F.S.]
“Health care proxy” means a competent adult who
has not been expressly designated by an advance
directive to make health care decisions for a particular
incapacitated individual, but is authorized pursuant to
Section 765.401, F.S., to make health care decisions
for such individual. [65E-5.100 (8), FAC]
“Health care surrogate” means any competent adult
expressly designated by a principal’s advance directive
to make health care decisions on behalf of the
principal upon the principal’s incapacity. [65E-5.100
(9), FAC]
Credentials
e professionals and other categories of persons authorized
by the Baker Act to perform specic functions on the
following Quick Reference Guide are the minimum
permitted by law. However, if the hospital or receiving
facility has policies that require increased level of credentials
to perform a specic function or if standards adopted in the
federal Conditions of Participation or by JCAHO or CARF
apply to the facility and are more stringent than the Baker
Act, those more stringent standards would apply.
A specialized on-line Baker Act course can be found at
http://www.bakeracttraining.org.
***
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Professional Credentials
Appendix L
L
Quick Reference Guide to Decision-Making
by Mental Health Professionals and Others
Non- Competent Adult,
psychiatric Physician Clinical LCSW LMHC Guardian, GA, Health
Function Psychiatrist Physician Assistant* Psychologist Psych Nurse LMFT Administrator Care Surrogate/Proxy
Voluntary
Certification of Competence to
Consent
X X
Transfer from Voluntary to
Involuntary (BA32)
X
Discharge X
Involuntary Examination
Initiate Examination X X X X X X
Conduct involuntary Examination X X X
Transfer to Voluntary X X X
Authorize Release from Receiving
Facility
X
X-ER
physician
only
X
Authorize Release from non-receiving
Facility
X X X
Involuntary Placement
1st Opinion on Petition X
2nd Opinion on Petition X X
Petition for Continued Involuntary
Placement
X X X
Discharge X
Treatment
Physical Examination X X X X if ARNP
Psychiatric Examination X
Psychological Examination X
Non-emergency treatment orders X X X X
Emergency medical treatment X X
Emergency Psychiatric Treatment X X
Determine Competence to consent to
Treatment
X X
Restraint or Seclusion X X X X
Consent, Refuse or Revoke Consent to
treatment
X
ECT X X
Restriction of Rights
Communication X
Personal Effects X
Access one’s own records X X
Transfers (hospitals must comply w/EMTALA)
Public to Public X DCF X
Public to Private X
Private to Public X X
Private to Private X
* Physician Assistants are not explicitly authorized in the Baker Act to initiate involuntary examinations. However, the
Florida Attorney General on May 28, 2008 interpreted the law to provide such authorization. is AGO didn’t authorize
Physician Assistants to perform any other responsibilities under the Baker Act assigned to psychiatrists or other physicians.
Appendix L - 3

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Professional Credentials
Appendix L - 4
L

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix M - 1
Baker Act Notices
Appendix M
M
Baker Act Notices
s. 394.4597 and s. 394.4599, F.S.
Voluntary Admission
At the time a person is voluntarily admitted to a receiving
or treatment facility, the identity and contact information
of a person to be notied in case of an emergency must be
entered in the person’s clinical record. Notice of a person’s
voluntary admission shall only be given at the request of the
person, except that in an emergency, notice shall be given as
determined by the facility.
Involuntary Examination
At the time a person is admitted to a facility for involuntary
examination or placement, or when a petition for involuntary
placement is led, the names, addresses, and telephone
numbers of the person’s guardian or guardian advocate or
representative if the person has no guardian, and the person’s
attorney must be entered in the clinical record.
If the person has no guardian, the person must be asked
to designate a representative. If unable or unwilling to
designate a representative the facility will select one with the
consultation of the person from the list below, in the order
of listing. e person has the authority to request that any
representative be replaced.
First preference must be given to a health care surrogate
selected by the person and named in an advance directive. If
the person hasn’t previously selected a health care surrogate,
the selection, except for good cause documented in the
clinical record must be made from the following list in the
order of listing:
1. Spouse
2. Adult child
3. Parent
4. Adult next of kin
5. Adult friend
A receiving facility must give prompt notice of the
whereabouts of a person who is being involuntarily held for
examination, by telephone or in person within 24 hours after
the person’s arrival at the facility to the person’s representative,
unless the person requests that no notication be made.
Notice of admission to a person’s guardian cannot be waived.
Contact attempts must be documented in the person’s clinical
record and must begin as soon as reasonably possible after
the person’s arrival. While the Baker Act permits a person
on involuntary status to request no notice of admission be
provided to his/her representative, other notices must be
provided – no waiver is permitted.
A treatment facility must provide notice of a person’s
involuntary admission on the next regular working day
after the person’s arrival at the facility. When a person is to
be transferred from one facility to another, notice must be
given by the facility where the person is located prior to the
transfer.
Whenever notice is required to be given, such notice must
be given to the person and the person’s guardian, guardian
advocate, attorney, and representative.
1. Notice must be given both orally and in writing, in
the language and terminology that the person can
understand, and, if needed, the facility must provide an
interpreter for the person.
2. Notice must be given by U.S. mail and by registered or
certied mail with the receipts attached to the person’s
clinical record. Hand delivery by a facility employee
may be used as an alternative, with delivery documented
in the clinical record. If notice is given by a state
attorney or an attorney for the department, a certicate
of service is sucient to document service.
e role of a Designated Representative includes:
• Receive notice of individual’s admission
• Have immediate access to the individual unless
documented to be detrimental
• Receive notice of any restriction of right to
communicate or receive visitors
• Receive written notice of any restriction of the
individual’s right to inspect his or her clinical record
• Petition on behalf of the individual for a writ of habeas
corpus
• Receive copy of the inventory of personal eects
• Receive notice of proceedings
• Receive copy of petition for the individual’s involuntary
placement led with the court
• Apply for change of venue for the involuntary placement
hearing for the convenience of the parties or the
individual’s condition
• Be informed by the court of the individuals right to an
independent expert evaluation

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act Notices
Appendix M - 2
M
• Receive notice of individual’s release from a receiving
facility
• Receive disposition of the individual’s clothing and
personal eects, if not returned to the individual
e written notice of the ling of the petition for involuntary
inpatient or outpatient placement must contain the
following:
1. Notice that the petition has been led with the circuit
court in which the person is hospitalized, and the
address of such court.
2. Notice that the oce of the public defender has been
appointed to represent the person in the proceeding, if
the person is not otherwise represented by counsel.
3. e date, time, and place of the hearing, and the
name of each examining expert and every other person
expected to testify in support of continued detention.
4. Notice that the person, the person’s guardian or
representative, or the administrator may apply for a
change of venue for the convenience of the parties or
witnesses or because of the condition of the person.
5. Notice that the person is entitled to an independent
expert examination and, if the person cannot aord such
an examination, that the court will provide for one.
See attached Quick Reference Guide for Provision of Baker
Act Notices.
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act Notices
Appendix M
M
Notices/Copies Quick Reference Guide
Facilities
Person Guard GA Rep Atty
AHCA/
Reporting
Center
Initiator Court DCF PD SAO
Rights of Persons (3103)
X X X X
Communication Restriction (3049)
X X X X X
Inventory of Personal Effects (3043)
X X X X
Restriction of Record Access (3110)
X X X X X
Right to Discharge Voluntary Persons
(3051a and b)
X
Notice of Right to Habeas Corpus (3036)
X X X X
Petition for Habeas Corpus (3090)
X X X X
Involuntary Initiation Forms (3001 & 3052a
X
and b)
Notice of Involuntary Admission (3045)
X X
Refusal or Revocation of Consent to
X X
Treatment (3105)
Petition for Adjudication of
Incompetence and Appt of Guardian
Advocate (3106)
X X X X
Petition Requesting GA to
X X X
Consent to Extraordinary Tx (3108)
Release from Involuntary Status (3038)
X X X X X X
Transfer Notice (3046)
X X X X X
Notice to Court of Withdrawal of Petition for
Involuntary Placement (3033)
X X X X
Petition Requesting Continued Involuntary
X X X X X X X X
Inpatient Placement (3035)
Order for Involuntary Outpatient Placement
X X X X X X
COURTS
Petition for Involuntary Placement (3032 &
3130)
X X X
Notice of Petition (3021) including:
X X X X X
(1) filed with court; (2) PD appointed; (3)
date/time/place; (4) change of venue; (5)
Independent expert
Right to Independent Expert (3022)
X X X
Order Appointing Guardian Advocate (3107)
X X X
Order Authorizing GA to Consent to
Extraordinary Treatment (3109)
X X
LEGEND
Guard:
GA:
Rep:
Atty:
Guardian
Guardian Advocate
Representative
Attorney
AHCA:
Initiator:
Agency for Health Care
Administration
(Baker Act Reporting Center)
Initiator
DCF:
PD :
SAO:
Department of Children & Families
Public Defender
State Attorney’s Office
Appendix M - 3

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act Notices
Appendix M - 4
M

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix N - 1
Marchman Act
Appendix N
N
Marchman Act History and Overview
Chapter 397, FS Chapter 65-D, FAC
History
e Florida Legislature enacted Chapter 397 governing the
Treatment and Rehabilitation of Drug Dependents in 1970.
e following year, it enacted Chapter 396 titled the Myers
Act as the state’s “Comprehensive Alcoholism Prevention,
Control, and Treatment Act,” modeled after the federal
Hughes Act. ese two laws, each governing dierent aspects
of addiction had a dierent Florida Administrative Code
(or rules) promulgated by the state to fully implement the
respective pieces of legislation.
Since persons with substance abuse issues often do not
contain their misuse to one substance or another, having two
separate laws dealing with the prevention and treatment of
addiction was cumbersome and did not address the problems
faced by Florida’s citizens.
In 1993 Representative Steven Wise of Jacksonville
introduced legislation to combine chapters 396 and 397
of Florida Statutes into a single law that clearly spelled out
legislative intent, licensure of service providers, client rights,
voluntary and involuntary admissions, oender and inmate
programs, service coordination, and children’s substance
abuse services.
e statute was named the Hal S. Marchman Alcohol and
Other Drug Services Act of 1993 -- generally referred to as
the Marchman Act. e Act was named after Rev. Hal. S.
Marchman, a tireless advocate for persons who suer from
alcoholism and drug abuse, who was recognized by the
Legislature for his contributions addressing the delivery of
substance abuse services.
To implement the new chapter 397, Florida Administrative
Code was developed to provide the standards that service
providers must uphold in order to be licensed to serve
persons with addictions. It also provided detailed policies
governing the entire licensing process as well as other
provisions. ese rules are identied as Chapter 65D-30 of
the Florida Administrative Code. ese rules have specic
legislative authority. Since the rules cannot restate language
from the statute, it is critical that individuals are aware of the
provision from the law AND the rules in order to carry out
the law, protect their agencies from liability, and protect their
clients from harm.
Related Legislation
e Marchman Act is the Florida Substance Abuse
Impairment Act and it does not serve any other purpose.
For many persons, the use of other statutes may be more
appropriate. Alternative statutes may include:
e Florida Mental Health Act—e Baker Act. Chapter
394, F.S. governs all issues related to mental illness. e
denition of mental illness specically excludes intoxication
and substance abuse impairment.
Emergency Examination and Treatment of Incapacitated
Persons Act s. 401.445, F.S. governs EMS examination and
treatment without consent where an emergency medical
condition is a life-threatening one and the individual is
unable to provide informed consent.
EMTALA, 42 USC 1395dd. A federal statute prohibiting
hospitals to delay or deny emergency medical services,
including psychiatric and substance abuse emergencies. e
law requires that each patient must have a medical screening
conducted within the full capability and capacity of the
hospital and must be stabilized before a transfer or discharge
takes place.
Access to Emergency Services and Care. 395.1041, F.S.
is a state statute, equivalent of the federal EMTALA law,
prohibiting the denial of emergency services and care by
hospitals and physicians and enforcing the ability of persons
to get all necessary and appropriate emergency care within
the capability and capacity of each hospital. is statute
also requires hospitals to adhere to rights and involuntary
examination procedures provided by the Baker Act,
regardless of whether the hospital is designated as a receiving
or treatment facility.
Adult Abuse, Neglect, and Exploitations. 415.1051, F.S. is a
state statute that may be appropriate when a vulnerable adult
(elderly or disabled) is alleged to be a victim of abuse, neglect,
or exploitation and lacks the capacity to consent. is means
a mental impairment that causes a person to lack sucient
understanding or capacity to make or communicate responsible
decisions concerning his person or property, including whether
or not to accept protective services from DCF.
Advance Directive. Chapter 765, F.S. provides that if a person
has previously executed an advance directive designating a
health care surrogate and a physician has found the person to
be incompetent or incapacitated to consent to his/her own

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Marchman Act
Appendix N - 2
N
treatment, the surrogate may instead be asked to provide
such consent. In the absence of an advance directive, a
health care proxy may be notied, if a person meeting the
degree of relationship is available to serve.
Guardianship. Chapter 744, F.S. governs guardianship
procedures. Some persons, due to their incapacity, require
either a limited or a plenary guardian appointed by the
court to make many life decisions. An incapacitated
person is one who has been judicially determined to lack
the capacity to manage at least some of his/her property
or to meet at least some of the essential health and safety
requirements of such person.
Legislative Intent
e 1993 Florida Legislature studied issues surrounding
the use and abuse of alcohol and other drugs. e
legislators made the following ndings:
1. Substance abuse is a major health problem and
leads to such profoundly disturbing consequences
as serious impairment, chronic addiction, criminal
behavior, vehicular casualties, spiraling health care
costs, AIDS, and business losses, and profoundly
aects the learning ability of children within our
schools and educational systems. Substance abuse
impairment is a disease, which aects the whole
family and the whole society and requires specialized
prevention, intervention, and treatment services that
support and strengthen the family unit.
2. Provide for a comprehensive continuum of accessible
and quality substance abuse prevention, intervention,
and treatment services in the least restrictive
environment of optimum care that protects and
respects the rights of clients, especially for involuntary
admissions, primarily through community-based
private not-for-prot providers working with local
governmental programs involving a wide range of
agencies from both the public and private sectors.
3. Ensure within available resources a full continuum of
substance abuse services based on projected identied
needs, delivered without discrimination and with
adequate provision for specialized needs.
4. Discourage substance abuse by promoting healthy
lifestyles and drug-free schools, workplaces, and
communities.
5. Integrate program evaluation eorts, adequate
administrative support services, and quality assurance
strategies with direct service provision requirements
and to ensure funds for these purposes.
6. Require the cooperation of departmental programs,
services, and program oces in achieving the goals of
this chapter and addressing the needs of clients.
7. Provide, for substance abuse impaired adult and
juvenile oenders, an alternative to criminal
imprisonment by encouraging the referral of such
oenders to service providers not generally available
within the correctional system instead of or in addition
to criminal penalties.
8. Provide, within the limits of appropriations and safe
management of the correctional system, substance
abuse services to substance abuse impaired oenders
who are incarcerated within the Department of
Corrections, in order to better enable these inmates to
adjust to the conditions of society presented to them
when their terms of incarceration end.
9. Provide for assisting substance abuse impaired persons
primarily through health and other rehabilitative
services in order to relieve the police, courts,
correctional institutions, and other criminal justice
agencies of a burden that interferes with their ability to
protect people, apprehend oenders, and maintain safe
and orderly communities.
10. Establish a clear framework for the comprehensive
provision of substance abuse services in the context of a
coordinated and orderly system.
11. Freedom of religion of all citizens shall be inviolate.
Nothing in this act shall give any governmental
entity jurisdiction to regulate religious, spiritual, or
ecclesiastical services.
Selected Definitions
397.311, F.S.
“Substance abuse” means the misuse or abuse of, or
dependence on alcohol, illicit drugs, or prescription
medications. As an individual progresses along this
continuum of misuse, abuse, and dependence, there is
an increased need for substance abuse intervention and
treatment to help abate the problem. (36)
“Impaired” or “substance abuse impaired” means a
condition involving the use of alcoholic beverages or any
psychoactive or mood-altering substance in such a manner as
to induce mental, emotional, or physical problems and cause
socially dysfunctional behavior. (14)
“Qualified professional” means a physician or a physician
assistant licensed under chapter 458 or chapter 459; a
professional licensed under chapter 490 or chapter 491; an
advanced registered nurse practitioner having a specialty

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix N - 3
Marchman Act
Appendix N
N
in psychiatry licensed under part I of chapter 464; or a
person who is certied through a department-recognized
certication process for substance abuse treatment services
and who holds, at a minimum, a bachelor’s degree. A person
who is certied in substance abuse treatment services by
a state-recognized certication process in another state at
the time of employment with a licensed substance abuse
provider in this state may perform the functions of a
qualied professional as dened in this chapter but must
meet certication requirements contained in this subsection
no later than 1 year after his or her date of employment. (26)
“Service provider” or “provider” means a public agency, a
private for-prot or not-for-prot agency, a person who is a
private practitioner, or a hospital licensed under this chapter
or exempt from licensure under this chapter. (33)
“Licensed service provider” means a public agency under
this chapter, a private for-prot or not-for-prot agency
under this chapter, a physician or any other private
practitioner licensed under this chapter, or a hospital that
oers substance abuse services through one or more licensed
service components. (17)
Client Rights
e Marchman Act provides an array of statutorily protected
rights of persons seeking and or receiving substance abuse
services as well as due process rights of those persons for
whom involuntary interventions are sought. ese include:
1. INDIVIDUAL DIGNITY must be respected at all
times and upon all occasions, including any occasion
when the client is admitted, retained, or transported.
Substance abuse clients who are not accused of a crime
or delinquent act may not be detained or incarcerated
in jails, detention centers, or training schools of the
state, except for purposes of protective custody in strict
accordance with this chapter. A client may not be
deprived of any constitutional right.
2. NONDISCRIMINATORY SERVICES. Service
providers may not deny a client access to substance
abuse services solely on the basis of race, gender,
ethnicity, age, sexual preference, HIV status, prior
service departures against medical advice, disability,
or number of relapse episodes. Service providers may
not deny a client who takes medication prescribed by
a physician access to substance abuse services solely on
that basis. Service providers who receive state funds
to provide substance abuse services may not, provided
space and sucient state resources are available, deny a
client access to services based solely on inability to pay.
3. QUALITY SERVICES. Each client must be delivered
services suited to his or her needs, administered
skillfully, safely, humanely, with full respect for his or
her dignity and personal integrity, and in accordance
with all statutory and regulatory requirements. Each
client in treatment must be aorded the opportunity
to participate in the formulation and periodic review
of his or her individualized treatment or service plan
to the extent of his or her ability to so participate.
It is the policy of the state to use the least restrictive
and most appropriate services available, based on the
needs and the best interests of the client and consistent
with optimum care of the client. Each client must be
aorded the opportunity to participate in activities
designed to enhance self-image.
4. COMMUNICATION. Each client has the right to
communicate freely and privately with other persons
within the limitations imposed by service provider
policy. Because the delivery of services can only be
eective in a substance abuse free environment, close
supervision of each client’s communications and
correspondence is necessary, particularly in the initial
stages of treatment, and the service provider must
therefore set reasonable rules for telephone, mail,
and visitation rights, giving primary consideration
to the well-being and safety of clients, sta, and the
community. It is the duty of the service provider to
inform the client and his or her family if the family is
involved at the time of admission about the provider’s
rules relating to communications and correspondence.
5. CARE AND CUSTODY OF PERSONAL EFFECTS.
A client has the right to possess clothing and other
personal eects. e service provider may take
temporary custody of the client’s personal eects only
when required for medical or safety reasons, with the
reason for taking custody and a list of the personal
eects recorded in the client’s clinical record.
6. EDUCATION OF MINORS. Each minor client in a
residential service component is guaranteed education
and training appropriate to his or her needs. e service
provider shall coordinate with local education agencies
to ensure that education and training is provided to
each minor client in accordance with other applicable
laws and regulations and that parental responsibilities
related to such education and training are established
within the provisions of such applicable laws and
regulations. Nothing in this chapter may be construed
to relieve any local education authority of its obligation
under law to provide a free and appropriate education
to every child.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Marchman Act
Appendix N - 4
N
7. CONFIDENTIALITY OF CLIENT RECORDS.
e records of service providers which pertain to
the identity, diagnosis, and prognosis of and service
provision to any individual client are condential
in accordance with this chapter and with applicable
federal condentiality regulations and are exempt from
the provisions of s. 119.07(1) and s. 24(a), Art. I of the
State Constitution. Such records may not be disclosed
without the written consent of the client to whom they
pertain except that appropriate disclosure may be made
without such consent. Federal regulations also provides
extensive protections regarding condentiality.
8. COUNSEL. Each client must be informed that he or
she has the right to be represented by counsel in any
involuntary proceeding for assessment, stabilization, or
treatment and that he or she, or if the client is a minor
his or her parent, legal guardian, or legal custodian,
may apply immediately to the court to have an attorney
appointed if he or she cannot aord one.
9. HABEAS CORPUS. At any time, and without notice,
a client involuntarily retained by a provider, or the
client’s parent, guardian, custodian, or attorney on
behalf of the client, may petition for a writ of habeas
corpus to question the cause and legality of such
retention and request that the court issue a writ for the
client’s release.
10. LIABILITY AND IMMUNITY. Service provider
personnel who violate or abuse any right or privilege
of a client under this chapter are liable for damages as
determined by law. All persons acting in good faith,
reasonably, and without negligence in connection with
the preparation or execution of petitions, applications,
certicates, or other documents or the apprehension,
detention, discharge, examination, transportation,
or treatment of a person under the provisions of this
chapter shall be free from all liability, civil or criminal,
by reason of such acts.
Voluntary Admission
A person, whether adult or minor, who wishes to enter
treatment for substance abuse may apply to a service provider
for voluntary admission. Within the nancial and space
capabilities of the service provider, a person of any age must
be admitted to treatment when sucient evidence exists that
the person is impaired by substance abuse and the medical
and behavioral conditions of the person are not beyond the
safe management capabilities of the service provider.
Involuntary Admissions
e Marchman Act encourages persons to seek out
treatment on a voluntary basis and to be actively involved
in planning their own services with the assistance of
qualied professionals. However, denial of addiction is a
common symptom, raising a barrier to early intervention
and treatment. As a result, treatment often comes as a result
of a spouse, employer, doctor, judge or other person with
inuence over one’s life to obtain needed substance abuse
services.
e Marchman Act established a variety of methods under
which substance abuse assessment, stabilization and treatment
could be obtained on an involuntary basis. ere are ve
involuntary admission procedures. ree of the procedures
do not involve the court, while two require direct petitions to
the circuit court. e three non-court procedures are:
Protective Custody
Emergency Admission
Alternative Involuntary Assessment for Minors
However, the law also oers a court-related procedure titled
“Involuntary Assessment and stabilization.”
Based on ndings of one of the four methods above, a
petition for Involuntary Treatment can be led with the
circuit court seeking up to 60 days of treatment.
Regardless of the court-involved or non court-involved
nature of the proceedings, the same criteria for involuntary
admission apply.
Criteria
e criteria for all involuntary admissions includes:
ere is good faith reason to believe the person is substance
abuse impaired and, because of such impairment:
1. Has lost the power of self-control with respect to
substance use; and either
a. Has inicted, or threatened or attempted to inict,
or unless admitted is likely to inict, physical harm
on himself or herself or another; or
b. Is in need of substance abuse services and, by reason
of substance abuse impairment, his or her judgment
has been so impaired that the person is incapable
of appreciating his or her need for such services
and of making a rational decision in regard thereto;
however, mere refusal to receive such services does
not constitute evidence of lack of judgment with
respect to his or her need for such services.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix N - 5
Marchman Act
Appendix N
N
Each of the ve methods of initiating an involuntary
admission specied above has dierent requirements and
procedures. See the quick reference guide at the end of this
appendix for a summary of the provisions of each method of
initiating involuntary admission.
Protective Custody
is procedure is used by law enforcement ocers when a
person is intoxicated in public or brought to the attention
of the ocer. e purpose is to take the person to a safe
environment where the person can be assessed to determine
the need for treatment e ocer may take the person
home, to a hospital, a detoxication center, or addiction
receiving facility, or in certain circumstances, to a jail,
whichever the law enforcement ocer believes is most
appropriate. Minors cannot be taken to jail. A person can be
held for assessment for up to 72 hours prior to release, unless
converting to voluntary status or a petition for involuntary
treatment led with the court.
Emergency Admission
is procedure permits a person who appears to meet
the criteria for involuntary admission to be admitted to a
hospital, an addiction receiving facility or a detoxication
facility for emergency assessment and stabilization. is
procedure may be initiated by a physician, spouse, guardian,
relative, or any responsible adult who has personal knowledge
of the person. In the case of a minor, emergency admission
can be initiated by a parent, legal guardian or legal custodian.
In any case, the application for an emergency admission must
be accompanied by the certicate of a physician.
A person can be held up to 72-hours under Emergency
Admission status before being released, unless converting to
voluntary status or a petition for involuntary treatment is
led with the court.
Alternative Involuntary Assessment
for Minors
is procedure provides a way for a parent, legal guardian
or legal custodian to have a minor admitted to an addiction
receiving facility to assess the minor’s need for treatment. e
minor can be held for up to 72 hours, but this period can be
extended to ve total days upon a physician’s assessment.
Involuntary Assessment & Stabilization
is procedure involves ling a petition with the Clerk of
the Court. e petition may be led by the person’s spouse,
guardian, any relative, a private practitioner, the director of a
licensed service provider, or any three adults with knowledge
of the person. If the person is a minor, the petition may be
led by a parent, a legal guardian, a legal custodian, or a
licensed service provider. e court can schedule a hearing
to take place within 10 days or can issue an ex parte order
immediately. e person can be admitted to a hospital, an
addictions receiving facility or a detoxication facility for
assessment and stabilization to determine the person’s need
for treatment.
A person can be held up to ve days for court ordered
assessment and stabilization, unless the person transfers
to voluntary status or a petition for involuntary treatment
is led with the court. If additional time is required to
complete the assessment, the court may grant an additional
7 days upon a timely written request.
Involuntary Treatment
is procedure involves ling a petition with the Clerk
of the Court after the person has been involved in at least
one of the four previously mentioned procedures. e
petition may be led by the same petitioners as involuntary
assessment and stabilization. e person can be court
ordered for involuntary treatment up to 60 days, but the
term of treatment can be extended by the court upon a
timely ling of a petition for an extension.
Provider Responsibilities
Service provider responsibilities regarding involuntary
admissions are as follows:
Ensure that a person who is admitted to a licensed
service component meets the admission criteria
specied in the law;
Ascertain whether the medical and behavioral
conditions of the person, as presented, are beyond the
safe management capabilities of the service provider;
Provide for the admission of the person to the service
component that represents the least restrictive available
setting that is responsive to the person’s treatment
needs;
Verify that the admission of the person to the service
component does not result in a census in excess of its
licensed service capacity;
Determine whether the cost of services is within
the nancial means of the person or those who are
nancially responsible for the person’s care; and
Take all necessary measures to ensure that each
individual in treatment is provided with a safe

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Marchman Act
Appendix N - 6
N
environment, and to ensure that each individual whose
medical condition or behavioral problem becomes
such that he or she cannot be safely managed by the
service component is discharged and referred to a more
appropriate setting for care.
When, in the judgment of the service provider, the person
who is being presented for involuntary admission should
not be admitted because of his or her failure to meet
admission criteria, because his or her medical or behavioral
conditions are beyond the safe management capabilities of
the service provider, or because of a lack of available space,
services, or nancial resources to pay for his or her care, the
service provider, in accordance with federal condentiality
regulations, must attempt to contact the referral source,
which may be a law enforcement ocer, physician, parent,
legal guardian if applicable, court and petitioner, or other
referring party, to discuss the circumstances and assist in
arranging for alternative interventions.
When the service provider is unable to reach the referral
source, the service provider must refuse admission and
attempt to assist the person in gaining access to other
appropriate services, if indicated.
Upon completing these eorts, the service provider must,
within one workday, report in writing to the referral sources,
in compliance with federal condentiality regulations:
1. e basis for the refusal to admit the person, and
2. Documentation of the service provider’s eorts to
contact the referral source and assist the person, when
indicated, in gaining access to more appropriate
services.
When, in the judgment of the service provider, the medical
conditions or behavioral problems of an involuntary
individual become such that they cannot be safely managed
by the service component, the service provider must
discharge the individual and attempt to assist him or her
in securing more appropriate services in a setting more
responsive to his or her needs. Upon completing these
eorts, the service provider must, within 72 hours, report
in writing to the referral source, in compliance with federal
condentiality regulations:
1. e basis for the individual’s discharge; and
2. Documentation of the service provider’s eorts to assist
the person in gaining access to appropriate services.
Upon giving his or her written informed consent, an
involuntarily admitted individual may be referred to a service
provider for voluntary admission when the service provider
determines that the individual no longer meets involuntary
criteria.
An individual involuntarily admitted to a licensed service
provider may be released without further order of the court
only by a qualied professional in a hospital, a detoxication
facility, an addictions receiving facility, or any less restrictive
treatment component. Notice of the release must be provided
to the applicant in the case of an emergency admission or
an alternative involuntary assessment for a minor, or to
the petitioner and the court if the involuntary assessment
or treatment was court ordered. In the case of a minor, the
release must be:
1. To the individual’s parent, legal guardian, or legal
custodian or the authorized designee;
2. To the Department of Children and Family Services; or
3. To the Department of Juvenile Justice.
Oversight
e Department of Children and Family Services is
designated the “Substance Abuse Authority” of Florida. It
is required to adopt rules establishing standards relating to
the rights and privileges of persons seeking substance abuse
prevention and treatment from licensed service providers.
For further assistance visit: http://www.dcf.state.fl.us/
programs/samh/MentalHealth/laws/index.shtml to view
DCF’s most Frequently Asked Questions list.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Marchman Act
Appendix N
N
Quick Reference Guide to Involuntary Admissions under the Marchman Act
Appendix N - 7
Admission How Initiated Means Requirements Length of Stay Disposition
Protective
Custody
397.677, FS
Law Enforcement LEO Report Initiating
Protective Custody
Release by Qualified
Professional*
Up to 72 hours Discharge/Refer
Voluntarily Remain
Retain if petition filed
Emergency
Admission
397.679, FS
Adult: physician, spouse,
guardian, relative, or other
responsible adult
Minor: parent, guardian, or
legal custodian
Application and Physician’s
Certificate
Physician assessment &
qualified professional*
assessment to determine
need for further services
and approve release
Up to 72 hours or 5 days
to a non-residential
component
Discharge/Refer
Voluntarily Remain
Retain if petition filed
Alternative
Involuntary
Admission for
Minors
397.6798, FS
Minor’s parent, guardian,
or legal custodian to
Addiction Receiving Facility
Application by eligible
person
Assessment by qualified
professional*
Up to 72 hours – can
be extended to 5 days
total upon physician
assessment.
Discharge to parent,
guardian, custodian,
DCF, or DJJ
Voluntarily Remain
Retain if Petition Filed
Court-Ordered
Assessment
397.681, FS
Adult: spouse, guardian,
relative, private
practitioner, director of
licensed provider, or 3
adults.
Minor: parent, guardian,
legal custodian or licensed
service provider
Civil Order from a Circuit
Judge – can be ex parte
or following a scheduled
hearing. Sheriff may be
ordered to transport
Assessed by qualified
professional* and by a
physician.
Up to 5 days. Court may
grant up to 7 additional
days to complete
the assessment and
stabilization
Discharge/Refer
Voluntarily Remain
Retain if petition filed
Involuntary
Treatment:
after 1 of the
4 assessments
above.
397.693, FS
Adult: spouse, guardian,
relative, service provider, or
any 3 adults
Minor: parent, legal
guardian, or service
provider
Civil Order from a Circuit
Judge. Sheriff may be
ordered to transport
Authorizes the provider to
require client to undergo
treatment that will be
beneficial until released by
qualified professional
Up to 60 days Discharge/Refer
Voluntarily Remain
Retain if extension
requested
Extension of
Involuntary
Treatment
Service Provider at least 10
days prior to end of order
Hearing within 15 days and
order from a Circuit Judge
Same as involuntary
treatment.
Each extension up to 90
days
Same as involuntary
treatment
Habitual
Abusers
397.701, FS
Agent specified in local
ordinance files petition
Hearing within 10 days Participation in treatment
program
Up to 90 days in licensed
secure facility with
extensions of 180 days
each
Discharge/Refer
Voluntarily Remain
Retain if extension
requested
Off ender
Referral
397-705
Court Court order in addition
to any other penalty or
sentence
Screening, assessment, and
treatment services from
licensed service provider
Up top maximum length
of sentence for the
off ense.
Inmate
Programs
397.752 FS
Federal and State
Departments of Correction
Individualized treatment Up top maximum length
of sentence for the
off ense
One month before
EOS given options for
continuing services
Qualified Professional: * Physician licensed under 458 or 459; or Professional licensed under chapter 490 or 491 (Psychologist, Clinical SW, Marriage & Family Therapist or Mental Health
Counselor); or Person who is certified through a DCF recognized certification process for substance abuse treatment services and who holds, at a minimum, a bachelor’s degree.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Marchman Act
Appendix N - 8
N

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act and Marchman Act Comparison
Denitions ...................................................................... 1
Service Providers ............................................................. 3
Voluntary Admissions...................................................... 3
Involuntary Examination/ Admission Criteria ................. 4
Procedure for Involuntary Examination/Assessments....... 5
Transportation Requirements for Involuntary
Examination / Admission ................................................ 9
Examination or Assessment ........................................... 12
Release or Discharge...................................................... 13
Notice of Release from Involuntary Examination /
Involuntary Admission .................................................. 14
Involuntary Placement / Involuntary Treatment —
Procedure for Filing Petitions ........................................ 15
Appointment of Counsel ............................................... 17
Hearings for Involuntary Placement / Treatment ........... 17
Initial Order .................................................................. 17
Hearings on Continued Involuntary Placement /
Treatment...................................................................... 17
Baker Act
Introduction and History
The Baker Act was enacted by the 1971 Florida Legislature
and took effect in 1972. It was named after its legislative
sponsor, Representative Maxine Baker from Miami. The
legislative Intent was to provide for the least restrictive form
of intervention and to provide a Bill of Rights for persons of
all ages who had mental illnesses. It has been frequently
amended over the years, but continues to balance liberty
interests against safety of individual and society.
Definitions
Baker Act (394.455, FS and 65E-5.100, FAC)
Mental Illness means:
Impairment of the mental or emotional processes that
exercise conscious control of one’s actions or of the ability to
perceive or understand reality.
Impairment substantially interferes with a person’s ability to
meet the ordinary demands of living regardless of etiology;
excluding intellectual or developmental disability as defined
in chapter 393, intoxication, or conditions manifested only by
antisocial behavior or substance abuse impairment.
Introduction and History ................................................ 1
Release from Involuntary Placement /
Treatment & Notices..................................................... 19
Responsibilities of Providers .......................................... 20
Rights: General ............................................................ 21
Rights: Individual Dignity............................................ 21
Rights: Treatment ......................................................... 21
Rights: Express and Informed Consent......................... 22
Rights: Quality Treatment / Services.............................. 24
Rights: Condentiality ................................................. 25
Rights: Communication, Abuse Reporting & Visitation 26
Rights: Care & Custody of Personal Eects ................... 26
Rights: Non-Discrimination......................................... 27
Rights: Voting in Public Elections ................................ 27
Rights: Right to Counsel.............................................. 27
Rights: Habeas Corpus ................................................. 27
Rights: Separation of Children from Adults.................. 28
Rights: Education of Minors ........................................ 28
Special Issues ................................................................. 28
Marchman Act
Hal S. Marchman Alcohol & Other Drug Services Act of
1993 -- addresses the entire array of substance abuse
impairment issues. It replaced the Myers Act (396, FS) –
alcohol abuse only and the Florida Drug Dependency Act
(397, FS) which addressed other drugs. The Marchman Act
is not just the substance abuse version of the Baker Act.
Marchman Act (397.311, FS)
Substance Abuse Impairment means:
A condition involving the use of alcohol or any
psychoactive or mood-altering substance in such a manner
as to induce:
mental, or
emotional, or
physical problems, and
Cause socially dysfunctional behavior
Appendix O - 1

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Marchman Act
Informed Consent required for voluntary admission, but not
defined in Marchman Act.
Baker Act
Express & Informed Consent
Consent voluntarily given in writing by a competent person after
sufficient explanation and disclosure of the subject matter involved
to enable the person to make a knowing and willful decision
without any element of force, fraud, deceit, duress, or other form of
constraint or coercion.
Incompetent to Consent
That a person’s judgment is so affected by his or her mental illness
That the person lacks the capacity To make a well-reasoned, willful
and knowing decision concerning his or her medical or mental
health treatment.
Qualified Professionals
394.455(2), (4), (21), (23) and (24), FS
Psychiatrist: A medical practitioner licensed under chapter 458
or 459 who has primarily diagnosed/treated mental/nervous
disorders for a period of not less than 3 years, inclusive of
psychiatric residency.
Physician: A medical practitioner licensed under chapter 458 or
459 who has experience in the diagnosis/treatment of mental
and nervous disorders or a physician employed by a facility
operated by the U.S. Dept of Veterans Affairs which qualifies as
a receiving or treatment facility.
Clinical Psychologist: A psychologist as defined in s. 490.003(7)
with 3 years of postdoctoral experience in the practice of
clinical psychology, inclusive of the experience required for
licensure, or a psychologist employed by a facility operated by
the United States Department of Veterans Affairs that qualifies
as a receiving or treatment facility.
Psychiatric Nurse: A registered nurse licensed under chapter 464
who has a master’s degree or a doctorate in psychiatric nursing
and 2 years of post master’s clinical experience under the
supervision of a physician.
Clinical Social Worker: A person licensed as a clinical social
worker under chapter 491.
Mental Health Counselor: Means a mental health counselor
licensed under chapter 491, F.S.
Marriage and Family Therapist: Means a marriage and family
therapist licensed under chapter 491, F.S.
Physician Assistants not eligible in statute, but recognized
by Florida Attorney General in May 2008 Opinion to initiate
involuntary exam (but not to perform other duties of a
physician)
Not defined in Marchman Act
A physician licensed under Chapter 458 or 459, F.S.,
A practitioner licensed under Chapter 490 or 491, F.S., or
A person who is certified through a department-recognized
certification process. Individuals who are certified
are permitted to serve in the capacity of a qualified
professional, but only within the scope of their certification.
Reciprocity with other states – meet Florida requirements
within 1 year.
Grandfather Clause – certified in Florida prior to 1/1/95.
Appendix O - 2

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Service Providers
Baker Act (394.455(26) and (30), FS)
Unless designated by DCF, facilities are not permitted to hold
or treat persons against their will or without their express and
informed consent (involuntary status) for mental illness, except
as required under federal EMTALA law.
Receiving Facility: Any public or private facility designated by
DCF to receive and hold persons on involuntary status under
emergency conditions for psychiatric evaluation and to provide
short-term treatment (excludes jails).
Treatment Facility: State Mental Health Facilities (state
hospitals)
Service provider means any public or private receiving facility,
an entity under contract with the Department of Children and
Family Services to provide mental health services, a clinical
psychologist, a clinical social worker, a marriage and family
therapist, a mental health counselor, a physician, a psychiatric
nurse as defined in subsection (23), or a community mental
health center or clinic as defined in this part.
Voluntary Admissions
Baker Act (394.4625, FS and 65E-5.270, FAC)
Adults: 394.4625, FS and 65E-5.270, FAC
Have a mental illness
Be suitable for treatment
Be competent to provide express and informed consent
Minors:
Have a mental illness (same definition as for adults)
Be suitable for treatment
Guardian applies by express and informed consent for minor’s
admission
Minor agrees (assents) to the admission
Judicial hearing to confirm the voluntariness of the admission
Special provisions for dependent children in custody of DCF
Requirements for Voluntary Status:
Must be on involuntary status if a guardian has been appointed
by a court or if a person has a healthcare surrogate proxy
because a physician has found the person to be incompetent to
make his or her own health care decisions.
A Certification of Competence must be completed by a
physician within 24 hours of arrival or adult must be released or
converted to involuntary.
Marchman Act (397.405, FS)
Public agencies,
Private for-profit or not-for-profit agencies,
Specified private practitioners,
Hospitals that are DCF licensed or exempt from licensure
under the Marchman Act.
Exempt from licensure: hospitals, nursing homes, federal
facilities, physicians (458/459), psychologists, chapter
491 professionals, DD facilities, churches under certain
circumstances, and substance abuse education programs
(s.1003.42) – generally limited to voluntary services only.
“Detoxification” is a service involving subacute care that
is provided on an inpatient or an outpatient basis to
assist individuals to withdraw from the physiological and
psychological effects of substance abuse and who meet the
placement criteria for this component.
“Addictions receiving facility” is a secure, acute care facility
that provides, at a minimum, detoxification and stabilization
services; is operated 24 hours per day, 7 days per week; and
is designated by the department to serve individuals found
to be substance use impaired as described in s. 397.675 who
meet the placement criteria for this component.
Marchman Act (397.601, FS)
Any person, regardless of age, who wishes to enter
substance abuse treatment may apply to a service provider
for voluntary admission if meeting diagnostic criteria for
substance abuse related disorders.
Disability of minority (under 18) removed solely for purpose
of voluntary admission, but not for involuntary when
parental participation may be required by the court.
Setting must be least restrictive setting appropriate to
person’s treatment needs.
Upon giving written informed consent, a person on involuntary
status may be referred to a service provider for voluntary
admission when the provider determines person no longer
meets involuntary criteria.
Appendix O - 3

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Release from Voluntary Status:
394.4625(2), FS and 65E-5.270, FAC
Notice of right to request release given at time of admission
Request for discharge -- notice within 12 hours to physician or
psychologist & release within 24 hours (3 working days from State
Treatment Facility)
Refusal or revocation of consent to treatment – discharge within
24 hours
Petition for involuntary placement filed with the circuit court
within 2 court working days after request for discharge or
refusal of treatment is made
Involuntary Examination/ Admission Criteria
Baker Act (394.463(1),FS)
The Baker Act provides for an involuntary examination that
may be initiated by two non-court procedures or one court
procedure. The following criteria is the same regardless of
which of the three methods of initiation is used:
1. Reason to believe person has a mental illness and because of
mental illness, person has refused or is unable to determine if
examination is necessary, and either:
2. Without care or treatment, is likely to suffer from neglect or
refuse to care for self, and such neglect or refusal poses a real
and present threat of substantial harm to one’s well-being and
it is not apparent that such harm may be avoided through the
help of willing family members, friends, or the provision of other
services; or
3. There is substantial likelihood that without treatment person
will cause in the near future serious bodily harm to self or others,
as evidenced by recent behavior.
Must meet all criteria
Initiation of Involuntary Examination: Upon determination
that person appears to meet criteria for involuntary
examination, the exam may be initiated by any one of the
following three means:
Court Order - the circuit court may enter an ex parte order; or
A law enforcement officer shall take into custody a person who
appears to meet the criteria describing circumstances; or
A mental health professional may execute a certificate stating
that s/he has examined the person within the preceding 48
hours and found the person met the criteria and stating his/her
observations upon which that conclusion is based.
More detail on each of the above methods of initiation is
found below.
Marchman Act (397.675, FS)
The Marchman Act provides three distinct non-court
procedures (protective custody, emergency admission,
alternative assessment and stabilization of minors) and one
court procedure (involuntary assessment and stabilization)
for conducting assessments, which may include
detoxification, stabilization, and short-term treatment. The
criteria is:
There is good faith reason to believe the person
is substance abuse impaired and, because of such
impairment:
1. Has lost the power of self-control with respect to substance
use; and either
2a. Has inflicted, or threatened or attempted to inflict, or unless
admitted is likely to inflict, physical harm on himself or
herself or another; or
2b. Is in need of substance abuse services and, by reason of
substance abuse impairment, his or her judgment has been
so impaired that the person is incapable of appreciating
his or her need for such services and of making a rational
decision in regard thereto; however, mere refusal to receive
such services does not constitute evidence of lack of
judgment with respect to his or her need for such services.
Eligibility for initiation of involuntary admission proceedings
under the Marchman Act is different depending on the age of
the individual and the circumstances:
The court may order an involuntary assessment /
stabilization,
A law enforcement officer can initiate Protective Custody,
A parent/guardian can initiate assessment of a minor to a
JARF, or
a variety of individuals can initiate an Emergency Admission
if a physician’s certificate has been obtained.
Appendix O - 4

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Procedure for Involuntary Examination/Assessments
Assessment & Examination Options
The Baker Act provides that involuntary examinations be conducted
only at designated hospital and non-hospital receiving facilities, as
well as at hospitals that have provided examination and treatment
of emergency medical conditions.
Reporting Requirements
394.459(9), 394.463(2)b, and 400.102(1)(c), FS
The Baker Act requires that the ex parte order, law enforcement
officer’s report, or executed certificate be forwarded to the Agency
for Healthcare Administration (AHCA) on the next working day
following admission of a person to a receiving facility.
Any receiving facility accepting person for involuntary examination
must send to BA Reporting Center cover sheet (#3118) and copy of
completed initiation form:
Ex Parte Petition/Order
Report of Law Enforcement Officer
Certificate of a Professional
All court orders for Involuntary Placement must also be sent to the
BA Reporting Center within 1 day:
Involuntary Inpatient Placement Order
Involuntary Outpatient Placement Order
Receiving facilities must report to AHCA, by certified mail within
one working day, facilities licensed under chapter 400 / 429, FS that
do not fully comply with Baker Act provisions governing:
Voluntary admission
Involuntary examination
Transportation
The Marchman Act provides several placement options for
assessing persons (e.g., hospitals, addictions receiving facilities,
detoxification facilities, less restrictive environments, jail).
The Marchman Act does not require contact with AHCA
regarding involuntary admissions.
Appendix O - 5

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
MH/SA Professional Initiation (394.463(2)(a)3, FS and 65E-
5.280(3), FAC)
The Baker Act permits a physician, clinical psychologist,
psychiatric nurse, clinical social worker, mental health
counselor, or marriage and family therapist to execute a
certificate if a person has been examined within the preceding
48 hours. The Florida Attorney General issued an opinion in
2008 that a Physician Assistant was also eligible to initiate
and involuntary examination, but didn’t authorize the PA to
perform any other activities permitted for a physician.
The authorized professional must cite his/her own
observations on which his/her conclusion is based on a
Certificate of a MH Professional (3052b) form and can’t rely
only upon the observations or input of others. The individual
must be transported to the nearest receiving facility unless the
County Commission and DCF have approved a Transportation
Exception Plan (can transfer later if appropriate).
Emergency Admissions (397.679, FS)
An application for emergency admission may be initiated:
For a minor by the parent, guardian or legal custodian or
for adults by:
Certifying physician
Spouse or guardian
Any relative
Any other responsible adult who has personal knowledge of
the person’s substance abuse impairment.
An application for Emergency Admission must be accompanied
by a Physician’s Certificate. The Physician’s Certificate must
include:
Name of client
Relationship between client and physician
Relationship between physician and provider
Statement that exam & assessment occurred within 5 days of
application date, and
Factual allegations about the need for emergency admission:
Reasons for physician’s belief the person meets each criteria
for involuntary admission
Recommend the least restrictive type of service
Be signed by the physician
State if transport assistance is required and specify the type
needed.
Accompany the person and be in chart with signed copy of
application.
A person meeting involuntary admission criteria may be
admitted for emergency assessment and stabilization upon
receipt of a completed application with an attached completed
physician’s certificate to:
A hospital, or
A licensed detox, or
An ARF, or
A less intensive component of a licensed service provider for
assessment only
Release from Emergency Admission:
Within 72 hours after emergency residential admission,
client must be assessed by attending doctor to determine
need for further services (5 days in OP). Based on
assessment, a qualified professional* must:
Release the client / refer
Retain the client voluntarily
Retain the client and file a petition for involuntary
assessment or treatment (authorizes retention pending
court order).
Appendix O - 6

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Law Enforcement 384.463(2)(a)2, FS and 65E-5.280(2), FAC
Law enforcement officer is defined to mean a law enforcement
officer as defined in s. 943.10, FS. The Florida Attorney General
has issued several opinions excluding various federal law
enforcement agencies from this definition because they are not
certified by the State of Florida.
A Law Enforcement Officer is required to describe the
circumstances under which he/she has taken the individual
into custody under the involuntary examination provisions of
the Baker Act. The officer is not required to personally observe
the behavior leading to the Baker Act, as is a Mental Health
Profession who initiates the examination.
The mandatory Report of Law Enforcement Officer -- Form
(3052a) – must be completed by the officer and accompany the
individual to a receiving facility or hospital.
Transportation by the law enforcement officer must be to the
nearest receiving facility unless the individual has an emergency
medical condition. He/she can be transferred later by the
facility if appropriate
Protective Custody (397.677, FS)
A law enforcement officer means a law enforcement officer
as defined in 943.10(1), FS
Law enforcement may implement for adults or minors
when involuntary admission criteria appears to be met
who is in a public place or is brought to attention of LEO.
A person may consent to LEO assistance to:
home, or
hospital, or
licensed detox center, or
addictions receiving facility, whichever the LEO determines
is most appropriate.
Law enforcement officer may take person (after
considering wishes of person) without consent to:
Hospital, or Detox, or ARF, or
An adult may be taken to jail. Not an arrest and no record
made. Jail must notify nearest appropriate licensed provider
within 8 hours and shall arrange transport to provider with
an available bed. The person must be assessed by jail’s
attending physician without unnecessary delay but within
72-hours
Release from Protective Custody must be by a qualified
professional* when:
Client no longer meets the involuntary admission criteria, or
The 72-hour period has elapsed; or
Client has consented to remain voluntarily, or
Petition for involuntary assessment or treatment has been
initiated. Timely filing of petition authorizes retention of
client pending further order of the court.
No corresponding provision in the Baker Act Alternative Assessment for Minors
Admission to a Juvenile Addiction Receiving Facility (JARF)
for a minor meeting involuntary criteria upon application
from:
Parent,
Guardian, or Legal custodian
Application must establish need for immediate admission and
contain specific information, including reasons why applicant
believes criteria is met.
Assessment by qualified professional within 72 hours to
determine need for further services.
Physician can extend to total of 5 days if further services are
needed.
Minor must be timely released or referred for further
voluntary or involuntary treatment, whichever is most
appropriate to minor’s needs.
Appendix O - 7

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Circuit Court Order 394.463(2)(a)1, FS and 65E-5.280(1),
FAC
Ex Parte means one-sided communication with the court and is
generally used in emergency situations. The judge doesn’t hear
testimony about the circumstances of the petition, but only
considers the information on the petition.
The Baker Act requires that an Ex Parte order be based on sworn
testimony. This can be as few as one petitioner or as many as
needed to inform the circuit court judge that the criteria for
involuntary examination appears to be met.
Recommended petition form (#3002) may be used by the
courts.
The petition must be filed with Clerk of the Court (Probate) and
no fee can be charged
The Ex Parte Order is valid for seven days unless the court has
specified a longer or shorter time limit for execution of order
Law enforcement can execute the Ex Parte Order any hour of the
day, on any day of the week and is authorized to use whatever
reasonable force is needed to enter the premises to take the
person into custody.
Transportation must be to the nearest receiving facility (unless a
transportation exception plan has been approved by the Board
of County Commissioners and the DCF Secretary) the facility will
transfer the individual later to a different facility if appropriate.
Ex parte Order (397. 681, FS)
The Marchman Act permits entering an ex parte order based
solely on the contents of a petition for involuntary assessment
and stabilization.
Petitions (397.6811, FS)
Petitions filed with Clerk of Court in county where person is
located.
Circuit court has jurisdiction
Chief judge may appoint general or special master.
Person has right to counsel at every stage of a petition for
involuntary assessment or treatment.
Court will appoint counsel if requested or if needed and
person cannot afford to pay.
Un-represented minor must have court-appointed guardian
ad litem to act on the minor’s behalf.
Adult: Petition may be filed by:
Spouse,
Guardian,
Any relative,
Private practitioner,
Any three adults having personal knowledge of person’s
condition, or
Service provider director/designee.
Minor: Petition may be filed by:
Parent
Legal guardian
Legal custodian, or
Licensed service provider.
Providers may initiate petitions for involuntary assessment
and stabilization, or involuntary treatment when that provider
has direct knowledge of the respondent’s substance abuse
impairment or when an extension of the involuntary admission
period is needed.
Petition for Assessment & Stabilization (397.6814, FS)
must contain:
Name of applicants and respondent
Relationship between them
Name of attorney, if known
Ability to afford an attorney
Facts to support the need for involuntary admission,
including why petitioner believes person meets each criteria
for involuntary intervention.
Appendix O - 8

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Role of the Court:
Clerk must determine whether person is represented by
an attorney, and if not, whether an attorney should be
appointed.
Based on a hearing or solely on petition and without an
attorney, enter an ex parte order authorizing assessment &
stabilization.
If hearing is scheduled, a summons issued to respondent
and hearing scheduled within 10 days
Court Determination (397.6818, FS)
Court shall hear all relevant testimony at hearing.
Respondent must be present unless injurious and a guardian
advocate is appointed.
Right to examination by court-appointed qualified
professional.
Determination by court whether a reasonable basis to
believe person meets involuntary admission criteria.
Court may either enter an order authorizing assessment &
stabilization or dismiss petition.
Court may initiate Baker Act if condition is due to mental
illness other than or in addition to substance abuse
Respondent or court may choose provider
Order must include findings as to availability &
appropriateness of least restrictive alternatives & need for
attorney to represent respondent.
If court determines that person meets criteria, he/she may
be admitted:
Up to 5 days to hospital, detox or ARF for assessment &
stabilization, or
Less restrictive licensed setting for assessment only
Provider Response for Court Ordered Evaluation
(397.6819, FS)
Licensed provider may admit person for assessment without
unnecessary delay, for a period of up to 5 days.
Assessment must be conducted by a “qualified professional”.
Assessment must be reviewed by a physician prior to end of
assessment period.
Provider may request court to extend time for assessment &
stabilization for 7 more days, if timely filed within the 5-day
assessment period.
Based upon involuntary assessment (397.822, FS), person may
be:
Released
Remain voluntarily
Retained if a petition for involuntary treatment has been
initiated.
Timely petition authorizes retention of client pending further
order of the court.
Appendix O - 9

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Transportation Requirements for Involuntary Examination / Admission
Baker Act 394.462, FS and 65E-5.260, FAC
Law enforcement is mandated to provide the transportation
of persons under involuntary status to the nearest receiving
facility regardless of how the examination was initiated (court,
law enforcement or MH professional), except transfers from a
hospital that is governed by the federal EMTALA law.
The designated law enforcement agency may decline to
transport the person to a receiving facility only if one of the
following exceptions applies:
1. The jurisdiction designated by the county has contracted on
an annual basis with an emergency medical transport service
or private transport company for transportation of persons to
receiving facilities at the sole cost of the county; and the law
enforcement agency and the emergency medical transport
service or private transport company agree that the continued
presence of law enforcement personnel is not necessary for the
safety of the person or others.
2. When a jurisdiction has entered into a contract with an
emergency medical transport service or a private transport
company for transportation of persons to receiving facilities,
such service or company shall be given preference for
transportation of persons from nursing homes, assisted living
facilities, adult day care centers, or adult family-care homes,
unless the behavior of the person being transported is such that
transportation by a law enforcement officer is necessary.
3. When a law enforcement officer takes custody of a person
pursuant to this part, the officer may request assistance from
emergency medical personnel if such assistance is needed for
the safety of the officer or the person in custody.
4. If the law enforcement officer believes that a person has an
emergency medical condition as defined in s. 395.002, the
person may be first transported to a hospital for emergency
medical treatment, regardless of whether the hospital is a
designated receiving facility.
5. When a member of a mental health overlay program or a mobile
crisis response service it may call on the law enforcement
agency or other transportation arrangement best suited to the
needs of the patient.
6. When a Transportation Exception Plan has been approved by the
Board of County Commissioners and the Secretary of DCF.
Criminal Charges:
When any law enforcement officer has custody of a person based
on either noncriminal or minor criminal behavior that meets
the statutory guidelines for involuntary examination, the law
enforcement officer shall transport the person to the nearest
receiving facility for examination.
Marchman Act
Transportation for Emergency Admission may be provided
by:
An applicant for a person’s emergency admission, or
Spouse or guardian, or
Law enforcement officer, or
Health officer
The Court may order law enforcement to transport a
person to nearest appropriate licensed service provider for
a court-ordered assessment and stabilization.
Appendix O - 10

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Baker Act 394.462, FS and 65E-5.260, FAC
When any law enforcement officer has arrested a person for
a felony and it appears that the person meets the statutory
guidelines for involuntary examination or placement under
this part, such person shall first be processed in the same
manner as any other criminal suspect. The law enforcement
agency shall thereafter immediately notify the nearest public
receiving facility, which shall be responsible for promptly
arranging for the examination and treatment of the person.
A receiving facility is not required to admit a person charged
with a crime for whom the facility determines and documents
that it is unable to provide adequate security, but shall
provide mental health examination and treatment to the
person where he or she is held.
Each law enforcement agency shall develop a memorandum
of understanding with each receiving facility within the law
enforcement agency’s jurisdiction which reflects a single set of
protocols for the safe and secure transportation of the person
and transfer of custody of the person. These protocols must
also address crisis intervention measures.
The nearest receiving facility must accept persons brought by
law enforcement officers for involuntary examination.
Procedures, facilities, vehicles, and restraining devices used for
criminals may not be used with persons who have a mental
illness, except for protection of the person or others. (Right to
Individual Dignity)
Law enforcement has no responsibility to provide
transportation of individuals on voluntary status or to
“treatment” facilities.
Paperwork Required:
Form Initiating Involuntary Exam:
BA 52a (Law Enforcement) or
BA 52b (MH Professional) or
Ex Parte Order (Circuit Judge), and
BA 3100 (transportation form)
Appendix O - 11

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Admission Notices
Baker Act 394.4599, FS
Voluntary Admission – No notice for adults except in
emergencies
Involuntary Admission -- Prompt notice (within 24 hours) of
arrival by phone or in person to:
Guardian/Guardian Advocate or Representative
May waive notice of admission to designated representative
only if person requests no notification. No other required
notices to representatives may be waived.
Case Manager must be notified (65E-5.130(1) and (2), FAC)
Identity of case manager noted in chart
Contact, with consent, of Case Management agency within 12
hours
CM visit within 2 working days after notice to assist with
discharge & aftercare planning
If case manager out of district, telephone call may substitute
Other required notices (394.4599, FS) require prompt delivery to:
Individual
Representative
Guardian or Gardian Advocate
Attorney
Notice to individuals held in facilities must be provided:
Orally and in writing
Using language/terminology person can understand
Using an interpreter if needed
To others, notices provided by U.S. mail and by registered
or certified mail, with receipts in chart or by hand delivery
documented in chart.
Marchman Act
Nearest relative of a minor must be notified by the law
enforcement officer of protective custody, as must the
nearest relative of an adult, unless the adult requests that
there be no notification.
Upon receipt of petition for a court-ordered assessment
and stabilization and if a hearing is scheduled, a copy
of petition & notice of hearing (394.6815, FS) must be
provided to:
Respondent,
Attorney,
Petitioner,
Spouse or guardian,
Parent of a minor, and
Others as directed by the court
Appendix O - 12

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Examination or Assessment
Baker Act (394.463(2)(f )and 65E-5.2801(1), FAC)
The Baker Act provides that a person must be examined within 72
hours of admission by a physician or a clinical psychologist. The
person may not be released by the receiving facility without the
documented approval of a psychiatrist, a clinical psychologist, or if
the receiving facility is a hospital, the release may also be approved
by an emergency department physician.
A “Baker Act” is not lifted, rescinded, overturned, reversed, or
abrogated! Once an Involuntary Exam is initiated, the Initial
Mandatory Involuntary Examination must be conducted without
unnecessary delay by a physician or licensed clinical psychologist
at a receiving facility or a hospital and documented in the clinical
record.
Minimum standards for Initial Mandatory Involuntary Examination
as required in law and rule (394.463(2)(f ), FS and65E-5.2801, FAC)
must include:
Thorough review of any observations of the person’s recent
behavior;
Review “Transportation to Receiving Facility” form (#3100) and
Review one of the following:
“Ex Parte Order for Involuntary Examination” or
“Report of Law Enforcement Officer Initiating involuntary
Examination” or
“Certificate of Professional Initiating Involuntary Examination”
Conduct brief psychiatric history; and
Conduct face-to-face examination in a timely manner to
determine if person meets criteria for release.
Within the 72 hour examination period:
Person shall be released, unless charged with a crime. If so,
returned to law enforcement, or
Person, unless charged with a crime, shall be asked to give
express and informed consent to voluntary placement, or
Petition for involuntary placement filed with Clerk of Circuit
Court.
Marchman Act
Under protective custody and emergency admission, the
assessment must be completed by a physician within 72
hours of admission.
For alternative involuntary assessment of a minor, the
assessment must be completed by a qualified professional
within 72 hours of admission but the minor may be
retained for an additional 2 days if further assessment is
determined necessary by a physician.
For involuntary assessment and stabilization, the
assessment must be completed by a “qualified
professional” within 5 days of the court’s order with sign-
off by a physician. If additional time is needed to complete
an assessment the court, if requested by the service
provider, may grant an extension not to exceed 7 days after
the renewal order.
Appendix O - 13

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Release or Discharge
Baker Act 394.459(11), FS and 65E-5.1303, FAC
Notification of right upon discharge to seek treatment from
the professional or agency of person’s choice
Discharge planning, beginning at admission, must include:
Transportation resources
Access to stable living arrangements
Assistance in securing need living arrangements or shelter for
those at risk of readmission within 3 weeks due to homelessness
and prior to discharge shall request a commitment from a
shelter provider that assistance will be rendered
Education and written information about the person’s mental
illness and medications
Information about & referral to community resources, including
peer support
Referral to substance abuse treatment programs, trauma
services, or other self-help programs
Assistance in obtaining a timely aftercare appointment
for needed services, including continuation of prescribed
psychotropic medications within 7 days of discharge
Access to psychotropic medications or prescriptions or a
combination thereof provided until scheduled aftercare
appointment or 21 calendar days
Marchman Act (65E-30.004(22), FAC)
A minor may only be released to:
Parent, legal guardian or legal custodian
To DCF pursuant to s.39, FS
To DJJ pursuant to s.984, FS
Summaries required for all voluntary and involuntary departures
from services.
Transfer Summary: Completed immediately for clients
transferring between components of same provider and
within 5 calendar days when transferring to another
provider. Entry must be made in record about circumstances
of the transfer signed and dated by primary counselor. A
Transfer Summary is defined to mean a written justification
of the circumstances of the transfer of a client from one
component to another or from one provider to another.
Discharge Summary: A Discharge Summary is legally
defined to mean a written narrative of the client’s treatment
record describing the client’s accomplishments and
problems during treatment, reasons for discharge, and
recommendations for further services. A written discharge
summary signed and dated by primary counselor must
be completed for clients completing or leaving prior to
completion including client’s involvement in services, reason
for discharge, and services needed following discharge,
including aftercare.
Discharge from State Hospitals 65E-5.1305, FAC
Completion of State Mental Health Facility Discharge form (CF-
MH 7001)
7 days prior notice to community case management agency
On day of discharge, physician or charge nurse immediately
notifies aftercare provider using the Physician-to-Physician
Transfer form (#7002)
Appendix O - 14

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Notice of Release from Involuntary Examination / Involuntary Admission
Baker Act
Notice of release must be given to the individual’s guardian,
guardian advocate, attorney, designated representative, to
any person who executed a certificate admitting the patient,
and to any court which ordered the examination.
Involuntary Placement / Involuntary Treatment — Procedure for Filing Petitions
Baker Act (394.467, FS)
Criteria: 394.467(1), FS and 65E-5.290, FAC
Finding of the court by clear and convincing evidence that the
individual:
Has a mental illness and because of the mental illness:
Has refused voluntary placement for treatment after sufficient
and conscientious explanation and disclosure of the purpose of
placement for treatment; or was unable to determine whether
placement is necessary; and
Is manifestly incapable of surviving alone or with the help of
willing and responsible family or friends, including available
alternative services, and, without treatment, is likely to suffer
from neglect or refuse to care for self, and such neglect or
refusal poses a real and present threat of substantial harm to his
or her well being; or
There is substantial likelihood that in the near future s/he will
inflict serious bodily harm on self or others, as evidenced by
recent behavior causing, attempting, or threatening such harm;
and
All available less restrictive treatment alternatives which would
offer an opportunity for improvement of his or her condition
have been judged to be inappropriate.
All criteria must be met
Marchman Act
Notice of release must be given to the applicant in the case
of emergency admission or an alternative assessment of
a minor, or to the petitioner and the court in the case of
involuntary assessment and that minor client can only be
released to authorized individuals or agencies.
A client involuntarily admitted may be released without
further order of the court only by a qualified professional.
(397.6758, FS)
Marchman Act
Criteria: There is good faith reason to believe the person
is substance abuse impaired and, because of such
impairment:
1. Has lost the power of self-control with respect to substance
use; and either
2a. Has inflicted, or threatened or attempted to inflict, or unless
admitted is likely to inflict, physical harm on himself or
herself or another; or
2b. Is in need of substance abuse services and, by reason of
substance abuse impairment, his or her judgment has been
so impaired that the person is incapable of appreciating
his or her need for such services and of making a rational
decision in regard thereto; however, mere refusal to receive
such services does not constitute evidence of lack of
judgment with respect to his or her need for such services.
In addition to meeting the above criteria for involuntary
admissions, a person for whom a petition for involuntary
treatment is filed must have met additional conditions
including:
Having been placed under protective custody within the
previous 10 days;
Having been subject to an emergency admission within the
previous 10 days,
Having been assessed by a qualified professional within the
previous 5 days;
Having been subject to a court ordered involuntary
assessment and stabilization within the previous 12 days
Having been subject to alternative involuntary admission
within the previous 12 days.
Appendix O - 15

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Marchman Act Baker Act
Petition for Involuntary Placement
The Baker Act permits the administrator of a receiving facility to
recommend placement in a treatment facility and to file a petition
with the court as long as the recommendation is supported by a
psychiatrist and a second opinion by another psychiatrist or clinical
psychologist, both of whom have personally examined the patient
within the preceding 72 hours and the criteria for involuntary
examination are met. (2nd opinion may be electronic, maintaining
visual & audio communication). Case law requires factual
substantiation of each criteria alleged in the petition for involuntary
inpatient placement – not just opinions, conclusions, or hearsay
Petition (#3032) completed and filed within 72 hours of person’s
arrival at facility or filed on next court working day if 72-hour
period ended on weekend or legal holiday – no exception for
weeknights
No fee charged.
Duties of the Court
Clerk of Court – provides required copies of the petition to
individual, DCF, guardian, or representative, state attorney and
public defender
Written notice of filing of petition for involuntary placement must
contain: (394.4599(2)(c), FS)
Petition filed with the circuit court in county where person is
hospitalized.
Office of public defender appointed to represent person if not
otherwise represented by counsel.
Date, time, and place of hearing, and name of each examining
expert and every other person expected to testify in support of
continued detention.
Person entitled to independent expert examination and, if
person cannot afford examination, court will provide for one;
and
Notice that person, guardian, representative or administrator
may apply for change of venue for convenience of parties or
witnesses or because of person’s condition.
Marchman Act (397.6951, FS)
The Marchman Act permits an adult’s spouse or guardian,
any relative, a service provider, or any three adults that
have knowledge of the respondent and prior course of
assessment or treatment to file a petition with the court.
If the respondent is a minor, the petition may be filed by a
parent, legal guardian, or service provider.
The Marchman Act also requires that the respondent have
been involved in at least one of the other involuntary
admission procedures within specified time frames before
a petition can be filed for involuntary treatment:
Contents of Petition must include:
Name of respondent
Name of petitioner(s)
Relationship between the respondent & petitioner
Name of respondent’s attorney
Statement of petitioner’s knowledge of respondent’s ability
to afford an attorney
Findings & recommendations of the assessment performed
by qualified professional
Factual allegations presented by the petitioner establishing
need for involuntary treatment, including:
Reason for petitioner’s belief that respondent is substance
abuse impaired; and
Reason for petitioner’s belief that because of such
impairment, respondent has lost power of self-control with
respect to substance abuse; and either
Reason petitioner believes the respondent has inflicted or is
likely to inflict physical harm on self/others unless admitted;
or
Reason petitioner believes respondent’s refusal to voluntarily
receive care is based on judgment so impaired by reason of
substance abuse to be incapable of appreciating need for
care and making a rational decision
Marchman Act (397.6955, FS)
Upon filing of petition with clerk of court, court shall
immediately determine if respondent has attorney or if
appointment of counsel is appropriate
Court scheduled hearing w/i 10 days.
Copy of petition and notice of hearing provided to
respondent; attorney, spouse or guardian if applicable,
petitioner, (parent, guardian or custodian of a minor), and
other persons as the court may direct; and
Issue a summons to respondent.
Appendix O - 16

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Burden of Proof by Clear and Convincing Evidence
Evidence that is precise, explicit, lacking in confusion, and of
such weight that it produces a firm belief or conviction, without
hesitation, about the matter at issue (Standard Jury Instructions
– Criminal Cases, published by the Supreme Court of Florida, No.
SC95832, June 15, 2000).
Appointment of Counsel
The Baker Act sets the time for appointing a Public Defender within
1 court working day, unless the person is otherwise represented by
private counsel.
The State Attorney’s Office is appointed as the “real party in interest”
to represent the state.
Hearings for Involuntary Placement / Treatment
Hearing held within 5 court working days unless continuance
requested by person, with concurrence of counsel. No waiver of
hearing.
Held as convenient to person as consistent with orderly
procedure and not likely to be injurious to person’s condition
Judge or magistrate presides
Person’s attendance at hearing -- any waiver of right to be
personally present at hearing must be knowing, intelligent, and
voluntary.
Witnesses:
1 of the 2 examining professionals who executed placement
certificate must be a witness
Anyone else that has fact testimony to support continued
detention. (staff, family, case manager, others)
Person may refuse to testify at the hearing
Competence to consent to treatment must be considered – If
incompetent, guardian advocate appointed
Initial Order
If a court concludes person meets all criteria for involuntary
inpatient placement, it shall order person, for a period of up to 6
months:
Transferred to a treatment facility or, if the person is at a
treatment facility, that the person be retained there, or
Treated at any other appropriate receiving or treatment facility,
or
Receive services from a receiving or treatment facility
Hearings on Continued Involuntary Placement / Treatment
Hearings on petitions for continued placement or extensions are
administrative hearings and conducted in accordance with section
120.57(1), F.S. Any order entered by a hearing officer is final and
subject to judicial review. Appellate case established that Courts
and Division of Administrative Hearings (DOAH) have concurrent
jurisdiction within the first six months of an order.
Evidence that is precise, explicit, lacking in confusion, and of
such weight that it produces a firm belief or conviction, without
hesitation, about the matter at issue (Standard Jury Instructions
– Criminal Cases, published by the Supreme Court of Florida, No.
SC95832, June 15, 2000).
The Marchman Act requires that the court immediately
determine whether the respondent is represented by counsel or
whether appointment of an attorney is appropriate. No specific
time is specified.
Neither the Public Defender nor the State Attorney is assigned
responsibility in the Marchman Act or chapter 27, FS.
Marchman Act (397.6957, FS)
The hearing must occur within 10 days of the petition with
no possibility of a continuance.
All relevant evidence, including results of all involuntary
interventions must be considered
Judge or magistrate presides
Client to be present unless injurious – if so, court will appoint
guardian advocate
Petitioner has burden of proving by clear & convincing
evidence that all criteria for involuntary admission are met
Court will either dismiss petition or order client to involuntary
treatment.
Marchman Act (397.697, FS)
Order for involuntary treatment by licensed provider up to
60 days
Order authorizes provider to require client to undergo
treatment that will benefit.
Order must include court’s requirement for notification of
proposed release.
Court may order Sheriff to transport
Court retains jurisdiction over case for further orders.
The Marchman Act requires that the petition be filed not more
than 10 days prior to the end of the initial period.
Appendix O - 17

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Extension of Order
Baker Act (394.467(6), FS)
The Baker Act provides that petitions on continued placement
be filed prior to the expiration of the period the treatment
facility is authorized to retain the patient. The Baker Act
permits a continued placement extension of up to 6 months.
If person continues to meet criteria for involuntary inpatient
placement, administrator shall, 20 days prior to expiration of
period during which treatment facility is authorized to retain
person, file petition (#3035) requesting authorization for
continued involuntary inpatient placement.
The request for continued involuntary placement must be
accompanied by:
A statement from person’s physician or clinical psychologist
justifying the request
A brief description of person’s treatment during the time he/she
was involuntarily placed
An individualized plan of continued treatment
Waiver of person’s presence at hearing may be filed, but no
waiver of hearing. The testimony in the hearing must be under
oath and the proceedings must be recorded
If previously found incompetent to consent to treatment,
testimony and evidence regarding the person’s competence
must be considered. If person is now competent to consent
to treatment, the administrative law judge may issue a
recommended order to court that found person incompetent
to consent to treatment that person’s competence be restored
and any guardian advocate previously appointed be discharged.
(#3116)
If at hearing person continues to meet criteria for involuntary
placement, administrative law judge will sign order (#3031) for
continued involuntary inpatient placement for period not to
exceed 6 months. Same procedure repeated prior to expiration
of each additional period the person is retained.
If person is found not to meet criteria for involuntary inpatient
placement, he/she must be released or transferred to voluntary
status
Marchman (397.6975, FS)
When criteria still exists, a renewal of involuntary treatment
order may be requested if filed at least 10 days prior to the end
of the 60-day period.
Hearing scheduled within 15 days of filing
Copy of petition to all parties
If grounds exist, may be ordered for up to 90 additional days.
Further petitions for 90 day periods may be filed if grounds
for involuntary treatment persist.
Appendix O - 18

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Release from Involuntary Placement / Treatment & Notices
At any time a person is found to no longer meet the criteria for
involuntary placement, the administrator shall:
Discharge person, unless under a criminal charge, in which
case the person shall be transferred to the custody of law
enforcement; or
Transfer person to voluntary status if willing and competent
to provide express and informed consent, unless the person is
under criminal charges or adjudicated incapacitated; or
Place improved person, unless under a criminal charge, on
convalescent status in the care of a community facility.
Notice of discharge/transfer shall be given (#3038).
After 60-day involuntary treatment, client automatically
discharged unless petition timely filed with court.
Person may be released by a qualified professional without
court order.
Notice of release provided to applicant for a minor or to
petitioner and court if court-ordered.
Release of minor must be to parent or guardian, DCF or DJJ.
An involuntarily admitted client may, upon giving written
informed consent, be referred to a service provider for
voluntary admission when the provider determines that the
client no longer meets involuntary criteria.
When a court ordering involuntary treatment includes
requirement in court order for notification of proposed
release, provider must notify the original referral source in
writing.
Early Release: Client must be released when: (397.6971, FS)
Basis for involuntary treatment no longer exist
Converts to voluntary upon informed consent
No longer in need of services
Client is beyond safe management of the provider
Further treatment won’t bring about further significant
improvements.
Notification shall comply with legally defined conditions and
timeframes and conform to federal and state confidentiality
regulations.
Appendix O - 19

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Responsibilities of Providers
Baker Act (394.461, FS and 65E-5.350 and 65E-5.180(5),
FAC)
Provide onsite emergency reception, screening & inpatient
treatment services 24 hours a day, 7 days a week, regardless of
ability to pay
Accept any person brought by law enforcement for involuntary
examination (hospitals must accept regardless of leagal status).
Accept persons of all ages
Assess all persons for clinical safety, co-occurring disorders,
substance abuse, physical/sexual abuse or trauma
Comply with all EMTALA requirements, if a hospital
Public receiving facilities affiliated with community mental
health centers must ensure the centralized provision and
coordination of acute care services for eligible persons with
acute mental illnesses. (394.459(11), FS and 65E-5.1304, FAC)
Failure to have the original form initiating involuntary admission
or an original signature on the form is not a basis for refusing an
admission.
The hospital licensing law requires all hospitals that examine or
treat an individual of any age who is held under the Baker Act
must adhere to all requirements as it applies to that individual,
as follows:
395.003(5)(a), FS “Adherence to patient rights, standards of
care, and examination and placement procedures provided
under part I of chapter 394 shall be a condition of licensure
for hospitals providing voluntary or involuntary medical or
psychiatric observation, evaluation, diagnosis, or treatment”.
395.003(5)(b), FS ”Any hospital that provides psychiatric
treatment to persons under 18 years of age who have emotional
disturbances shall comply with the procedures pertaining to the
rights of patients prescribed in part I of chapter 394”.
395.1041(6), FS Rights of Persons being Treated.-- A hospital
providing emergency services and care to a person who is being
involuntarily examined under the provisions of s.394.463 shall
adhere to the rights of patients specified in part I of chapter
394 and the involuntary examination procedures provided
in s.394.463, regardless of whether the hospital, or any part
thereof, is designated as a receiving or treatment facility under
part I of chapter 394 and regardless of whether the person is
admitted to the hospital.
395.1055(5), FS “The agency (AHCA) shall enforce the provisions
of part I of chapter 394, and rules adopted thereunder, with
respect to the rights, standards of care, and examination
and placement procedures applicable to patients voluntarily
or involuntarily admitted to hospitals providing psychiatric
observation, evaluation, diagnosis, or treatment”.
Marchman Act (397.6751, FS and65D-30.004, FAC)
Person must be admitted when sufficient evidence exists
that:
Person is substance abuse impaired
Setting Is the least restrictive and most appropriate
Within licensed capacity
Medical & behavioral conditions can be safely managed
Within financial means of person (Other than licensed
hospitals per EMTALA)
Providers receiving state funds for substance abuse services
can’t deny access based on inability to pay if space and sufficient
state resources are available.
Access cannot be denied based on race, gender, ethnicity,
age, sexual preference, HIV status, disability, use of prescribed
medications, prior service departures against medical advice, or
number of relapse episodes.
If admission is refused (397.6751, FS) the provider must, in
compliance with federal confidentiality regulations:
1. Attempt to contact referral source to discuss circumstances
and assist in arranging alternate intervention.
2. Provider must within 1 workday of refusal, report in writing
to referral source:
• Basis for refusal
• Documentation of provider’s eorts to contact the referral
source and assist person to access more appropriate
services.
3. If medical or behavior can’t be safely managed, provider
must discharge and assist to secure more appropriate
services. Within 72 hours, report to referral source basis for
discharge and provider’s efforts to assist client.
Persons on involuntarily status can only be placed in licensed
service providers in components authorized to accept
involuntary clients.
Providers accepting person on involuntary status must provide
a description of the eligibility and diagnostic criteria and the
placement process to be followed for each of the involuntary
placement procedures
Each person involuntarily admitted shall be assessed by
a qualified professional to determine need for additional
treatment and most appropriate services.
Decision to refuse to admit or to discharge shall be made
only by a qualified professional.
Failure to have the original form initiating involuntary admission
or an original signature on the form is not a basis for refusing an
admission.
Appendix O - 20

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Rights: General
Written copy of rights at admission
Signed by person
Copies to significant others
Discussion of rights during hospitalization
Posting of rights & phone numbers near phone:
Abuse Registry / Hotline
Disabilities Rights Florida, Inc.
ADA
Copy of Baker Act statute & rules on each unit
Rights: Individual Dignity
Baker Act (394.459(1), FS and 65E-5.150 FAC)
All Constitutional Rights
Freedom of Movement – no restraint or seclusion except for
safety of person or others (imminent danger)
Outdoors & Exercise – at least ½ hour per day out of doors
unless prohibited by physician’s order when suitable area is
immediately adjacent to unit
Special Clothing – prohibited for identification purposes
Procedures, facilities, vehicles, and restraining devices used for
criminals not be used with persons who have a mental illness,
except for protection of the person or others
Rights: Treatment
Baker Act (394.459(2), FS and 65E-5.160, FAC)
No denial or delay of treatment due to inability to pay – may
collect appropriate reimbursement
Least restrictive appropriate & available treatment required
Physical examination within 24 hours by authorized health care
practitioner
Posted schedule of daily activities
Individualized treatment plan within 5 days. Person must have
had opportunity to assist in preparing and reviewing plan. Form
must have space for person’s comments
Marchman Act (397.501, FS and 65D-30.004, FAC)
Clients receiving substance abuse services from any service
provider are guaranteed protection of fundamental human,
civil, constitutional and statutory rights including those
specified in the Marchman Act unless otherwise expressly
provided, and service providers must ensure the protection of
such rights.
Basic client rights include provisions for informing the client,
family member, or authorized guardian of their rights and
responsibilities, assisting in the exercise of those rights, and an
accessible grievance system for resolution of conflicts;
Marchman Act 397.501(1), FS
Guaranteed the protection of all fundamental human, civil,
constitutional, and statutory rights.
Respect at all times, including when admitted, retained, or
transported.
Cannot be placed in jail unless accused of a crime except for
adults under protective custody.
Must permit grievances to be filed for any reason
Marchman Act
See right to quality services below
Services suited to client’s needs, administered skillfully,
safely, humanely, with full respect for dignity/integrity, and
in compliance with all laws and requirements.
Opportunity to participate in formulation & review of
individualized treatment / service plan.
Appendix O - 21

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Treatment Planning (394.459(2)(d), FS and 65E-5.160 (2),
FAC) must include:
Advance directives-person’s preferences for mental health care
Diagnostic testing
Person’s treatment goals
Housing
Social supports
Financial supports
Health, including mental health
Observable, measurable & time-limited objectives
Progress notes
Periodic reviews
Integrated approach to treatment
Updates & physician summary every 30 days
“Treatment Plan” means an individualized, written plan of action
that directs all treatment services and is based upon information
from the assessment and input from the client served. The
plan establishes client goals and corresponding measurable
objectives, time frames for completing objectives, and the type
and frequency of services to be provided.
Each client shall be afforded the opportunity to participate in
the development and subsequent review of the treatment plan.
The treatment plan shall include:
Goals and related measurable behavioral objectives to be
achieved by the client,
Tasks involved in achieving those objectives,
Type and frequency of services to be provided, and
Expected dates of completion.
The treatment plan shall be signed and dated by the
person providing the service, and signed and dated by the
client. If the treatment plan is completed by other than a
qualified professional, the treatment plan shall be reviewed,
countersigned, and dated by a qualified professional within 10
calendar days of completion.
Rights: Express and Informed Consent
Baker Act 394.459(3), FS and 65E-5.170, FAC
Competence is well reasoned, willful & knowing decision-making.
Prior to requesting consent to treatment, the following must be
provided and explained in plain language:
The reason for admission or treatment,
Proposed treatment, including psychotherapeutic medications
Purpose of treatment
Alternative treatments
Specific dosage range for medications
Frequency and method of administration
Common risks, benefits and short-term/long-term side effects
Contraindications
Clinically significant interactive effects with other medications,
Similar information on alternative medication which may have
less severe or serious side effects.
Potential effects of stopping treatment
Approximate length of care
How treatment will be monitored, and that
Any consent for treatment may be revoked orally or in writing
before or during the treatment period by the person legally
authorized to make health care decisions for the person.
Informed consent required, but not separately defined or
described in Marchman Act.
Appendix O - 22

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Who can give consent?
Competent adult
Guardian of a child
Court Appointed Guardian
Court Order
Letters of Guardianship
Guardian advocate / court order
Health care surrogate or proxy / Advance Directive
If competent to consent, person is competent to refuse or revoke
consent!
If incompetent to consent, person is incompetent to refuse or
revoke consent and a substitute decision-maker must be appointed.
Who can give consent?
Adults
Minors
Authorization for Treatment 65E-5.170(2), FAC
General Authorization for Treatment (#3042a)
Routine medical care
Psychiatric assessment
Assessment/treatment other than medications
Specific Authorization for Psychotropic Medications
(#3042b)
Disclosure by qualified personnel
Completed prior to administration
By authorized decision-maker
No corresponding provisions
Emergency Treatment Orders 394.463(2)(f ), 394.4625(5),
FS and 65E-5.1703, FAC
Document specific nature & extent of imminent danger to self
or others (not just “agitated” or “disruptive”)
Must attempt to contact guardian, guardian advocate or health
care surrogate / proxy to obtain consent
Medical review of person’s condition for causal medical factors
Written order of a physician required-Initial order by phone
Written order signed within 24-hours
No PRN or standing orders
Each order valid not to exceed 24-hours; daily renewal by
physician if dangerousness continued
No corresponding provisions
Petition for Guardian Advocate:
Petition must be initiated within 24 hours of ETO & submitted to
court within 2 court working days thereafter unless only single
ETO is needed.
If 2nd ETO written within 7 days, petition must be filed
with court within 1 court working day thereafter requesting
appointment of a guardian advocate.
No corresponding provisions
Appendix O - 23

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Rights: Quality Treatment / Services
Baker Act 394.459(4), FS and 65E-5.180, FAC
Receiving and treatment facilities are required to maintain in a form
accessible to and readily understandable:
Criteria, procedures, & staff training required for any use of &
procedures for documenting, monitoring, and requiring clinical
review of:
Close or elevated levels of supervision
Use of bodily control and physical management techniques
Restraint, seclusion or isolation
Emergency treatment orders
Procedures for documenting and reviewing incidents resulting
in injury.
A system for investigating, tracking, managing, and responding
to complaints by persons or others acting on their behalf.
Marchman Act 397.501(3), FS
Least restrictive and most appropriate services, based on needs
and best interests of client.
Services suited to client’s needs, administered skillfully,
safely, humanely, with full respect for dignity/integrity, and in
compliance with all laws and requirements.
Methods used to control aggressive client behavior that pose an
immediate threat to the client or others – used by staff trained &
authorized to do so – in accordance with rule.
Opportunity to participate in formulation & review of
individualized treatment / service plan.
Emergency Orders
Facilities must comply with the most stringent standards that apply
to their facility, including ETO’s, restraints, seclusion, and other
emergency interventions. These may include:
Baker Act law and rules --Baker Act rules governing restraints &
seclusion rewritten in 2008.
Joint Commission on Accreditation of Healthcare Organizations
or CARF
Federal Conditions of Participation (CMS)
Facility policies and procedures
Appendix O - 24

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Rights: Confidentiality
Variety of federal/state statutes and case law govern confidentiality:
Baker Act
Psychotherapist / patient privilege
Substance Abuse
HIPAA (treatment, operations and payment exempted)
Substitute Decision-Makers
Communicable Diseases
Duty to report abuse, neglect & exploitation of children &
vulnerable adults
Foreign Nationals – Consular Notification & Access
Unless person, guardian, guardian advocate, or surrogate/proxy
waives by express and informed consent, confidentiality of record
shall not be lost.
Information from record may be released:
By court order after good cause hearing
After declaration of intent to harm – may release sufficient
information to adequately warn person threatened. Tarasoff
warning not required in Florida
Inform guardians of threats by minors
Warn of threats of future harm, but not confessions of past
crimes
Person has right of reasonable access to own clinical record unless
determined by physician to be harmful. If restricted:
Recorded, with reasons, in clinical record
Notice to person, attorney, and others
Expires in 7 days but can be renewed
Facility policies should identify:
What is reasonable access?
Is this all “persons” – minors? incapacitated?
Who will review for harmfulness?
How, where & with whom actual review will take place?
Identity, diagnosis, prognosis, and service provision to any client
is confidential.
Disclosure requires written consent of client, except:
Medical personnel in emergency
Provider staff on “need to know” to carry out duties to client.
DCF Secretary/designee for research (non-identifying)
Audit or evaluation by federal, state, local governments, or
3rd party payor
Court order for good cause based on whether public
interest/need for disclosure outweigh potential injury to
client or provider to authorize disclosure but subpoena then
required.to compel.
Other Confidentiality Considerations:
Restrictions inapplicable to reporting of suspected child
abuse.
Minor may consent to own disclosure – consent can only be
given by the minor
If consent of guardian required to obtain services for minor,
both minor & guardian must consent to disclosure
42 CFR (Code of Federal Regulations) and HIPAA also control
how information can be released – most stringent prevails.
Release to Law Enforcement directly related to commission of a
crime on premises or against staff or threat to do so. Limited to:
Client’s name and address
Circumstances of incident
Client status
Client’s last known whereabouts.
Court can authorize for criminal investigation or prosecution
only if all the following criteria are met:
Crime is extremely dangerous
Records will be of substantial value
No other methods available or effective
Potential injury to client or program outweighed by public
interest and need to know
Confidentiality and the Court:
Court order authorizes but does not compel disclosure of
client identifying data.
Subpoena must then be issued to compel disclosure.
Client and provider must be given notice and opportunity to
respond or to appear to provide evidence.
Oral argument, review of evidence or hearing in chambers.
Appendix O - 25

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Marchman Act Baker Act
Patient and personnel records in hospitals; copies; examination
Baker Act (395.3025(2), FS)
This section of the hospital statute does not apply to records
maintained at any licensed facility the primary function of which is
to provide psychiatric care to its patients, or to records of treatment
for any mental or emotional condition at any other licensed facility
which are governed by the provisions of s. 394.4615.
Rights: Communication, Abuse Reporting & Visitation
Baker Act 394.459(5), FS and 65E-5.190, FAC
Guaranteed regardless of age or development, but facility
shall establish reasonable rules governing visitors and use of
telephones
Visits: Immediate access by family, guardian, guardian
advocate, representative, or attorney, unless found to be
detrimental
Telephone:
Free local calls / Access to long-distance
Private and confidential communication
Phone located near posters giving advocate phone numbers
Unlimited telephone for abuse reporting, attorney, & Disability
Rights Florida, Inc.
Correspondence
Stationery/stamps/gifts
Send / receive unopened correspondence without delay
Reasonable examination of suspected contraband & disposal
Restriction of Communication (#3049)
Written notice with reasons to person, attorney, guardian,
guardian advocate, or representative
Reviewed every 7 days
Waiver: Competent adults may waive the confidentiality of
their presence in a receiving or treatment facility
Rights: Care & Custody of Personal Effects
Baker Act 394.459(6), FS and 65E-5.200, FAC
Right to possess clothing / personal effects except for medical
and safety reasons. Receiving and treatment facilities must
develop policies and procedures governing:
What will be removed for reasons of personal or unit safety
How it will be safely retained by the facility
How/when it will be returned
How contraband will be addressed when not returned
Inventory:
Witnessed by person and two staff
At time of admission and when amended
Marchman 395.3025(3), FS
This section of the hospital statute does not apply to records of
substance abuse impaired persons, which are governed by s.
397.501.
Marchman Act 397.501(4), FS
Free & private communication within limits imposed by
provider policies.
Close supervision of all communication & correspondence
required.
Reasonable rules for mail, telephone & visitation to ensure
the well-being of clients, staff & community.
Clients and families must be informed about provider rules
related to communication and correspondence
Marchman Act 397.501(5), FS
Right to possess clothing and other personal effects.
Provider may take temporary custody of personal effects
only when required for medical or safety reasons.
If removed, reasons for taking custody and a list of the
personal effects must be recorded in clinical record.
Appendix O - 26

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Rights: Non-Discrimination
Baker Act
No corresponding provision.
Rights: Voting in Public Elections
Baker Act 394.459(7), FS and 65E-5.210, FAC
A person in a facility who is eligible to vote has the right to vote
in the primary and general elections
Receiving and treatment facilities shall have voter registration
forms and applications for absentee ballots readily available at
the facility (or in accordance with the procedures established by
the County supervisor of elections), and shall assure that each
person who is eligible to vote and wishes to do so, may exercise
his or her franchise
Each designated facility shall develop policies and procedures
governing how persons will be assisted in exercising their right
to vote
Rights: Right to Counsel
Baker Act (394.467(4), FS)
The Public Defender is responsible for representing all persons
on involuntary placement status unless represented by private
counsel
Rights: Habeas Corpus
Marchman Act (2)
Service providers may not deny a client access to substance
abuse services solely on the basis of race, gender, ethnicity, age,
sexual preference, HIV status, prior service departures against
medical advice, disability, or number of relapse episodes.
Service providers may not deny a client who takes medication
prescribed by a physician access to substance abuse services
solely on that basis. Service providers who receive state funds to
provide substance abuse services may not, provided space and
sufficient state resources are available, deny a client access to
services based solely on inability to pay.
Marchman Act
No corresponding provisions
Marchman Act 397.501(8), FS
Client must be informed of right to counsel at every stage of
involuntary proceedings.
May be represented by counsel in any involuntary
proceeding for assessment, stabilization, or treatment.
Person (or guardian of a minor) may immediately apply to
court to have attorney appointed, if unable to afford one.
No reference to Public Defender in Marchman Act or Chapter
27, FS.
Baker Act 394.459(8), FA and 65E-5.220, FAC
Each person (any age or legal status) admitted to a receiving
or treatment facility must have written notice of right to
petition (#3036) for writ:
Cause and legality of detention
Unjustly denied a right or privilege
Abuse of procedure authorized in law
Petition (#3090) filed any time/without notice by:
Individual Guardian Advocate
Relative Representative
Friend Attorney
Guardian DCF
Facility files petition (any format preferred by the individual)
with clerk of court on next working day. No fee charged
Marchman Act 397.501(9), FS
Filed at any time and without notice
Filed by client involuntarily retained or parent, guardian,
custodian, or attorney on behalf of client
May petition for writ to question cause and legality of
retention and request the court to issue a writ for client’s
release
Appendix O - 27
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Marchman Act
No corresponding provisions
Baker Act
Rights: Separation of Children from Adults
Baker Act 394.4785, FS and 65E-12, FAC
Hospitals:
Age 0-13 no contact with adults
Age 14-17 share common areas with adults but share bedroom
with adult only if doctor documents medical or safety issues
daily
Children and adolescents can be mixed
CSUs:
Age 0-13 can share common areas with adult when under direct
visual observation by staff but cannot share bedroom with an
adult
Age 14-17 share common areas with adults but share bedroom
with adult only if doctor daily documents medical or safety
issues
Rights: Education of Minors
No corresponding provision.
Special Issues
Sexual Misconduct Prohibited
Baker Act 394.4593, FS
Sexual Misconduct means any sexual activity between an
employee and a patient, regardless of the consent of the
patient.
An employee engaging in sexual misconduct with patient in
DCF custody or in a receiving/treatment facility commits a
felony.
An employee who witnesses, knows of, or has reasonable cause
to suspect sexual misconduct must immediately report to the
Abuse Registry and to law enforcement. Failure to do so is a
misdemeanor.
Employee must prepare, date, sign independent report
describing nature of the sexual misconduct, location/time
of incident, and persons involved. Report must be given to
program director for submitting to DCF Inspector General who
will immediately investigate.
Each minor client in a residential service component is
guaranteed education and training appropriate to his or
her needs. The service provider shall coordinate with local
education agencies to ensure that education and training
is provided to each minor client in accordance with
other applicable laws and regulations and that parental
responsibilities related to such education and training are
established within the provisions of such applicable laws
and regulations. Nothing in this chapter may be construed
to relieve any local education authority of its obligation
under law to provide a free and appropriate education to
every child.
Marchman Act
No corresponding provisions
Appendix O - 28

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Complaints and Grievances
Baker Act 394.459(4)(b)3, FS and 65E-5.180 FAC
Policy/procedures required to receive, review, investigate, track,
manage and respond to formal/informal complaints by person or
others.
Process explained verbally at orientation and provided in
writing:
How complaints can be addressed informally and formally with
staff
Informed of Abuse Registry, Advocacy Center or others to
request assistance
Process, including phone numbers for above posted next to
phones.
Life-safety issues acted upon immediately
Formal complaints:
Person not named in complaint will assist.
Will include date/time of complaint and detail issue/remedy
sought
Forward to staff assigned to track/monitor
All formal complaints must contain:
Name of complainant
Name of person receiving services
Nature of complaint
Date/time received by staff
Date/time received by person who will track
Name of person assigned to investigate
Date person notified of who will investigate
Due date for written response
Written disposition of formal complaint.
Written response provided to person within 24 hours of
disposition. If complainant other than patient, not given
details of disposition without consent, unless having right to
information.
Disposition can be appealed to administrator who will review
and make final decision within 5 working days and provide
written response within 24 hours thereafter.
Client Responsibility for Cost of Care
Chapter 394, Part I, FS, the Baker Act, makes no reference to
payment for care and treatment. However, the Florida Attorney
General has issued opinions stating that DCF (with county matching
funds) is responsible for establishing public receiving facilities but
that persons served in private receiving facilities are responsible for
their own cost of care.
Marchman Act (65D-30.004 (29) FAC)
Grievance procedure must include:
Provisions assuring that a grievance may be filed for any
reason with cause;
The prominent posting of notices informing clients of the
grievance system;
Access to grievance submission forms;
Education of staff in the importance of the grievance system
and client rights;
Specific levels of appeal with corresponding time frames for
resolution;
Timely receipt of a filed grievance;
The logging and tracking of filed grievances until resolved or
concluded by actions of the provider’s governing body;
Written notification of the decision to the appellant; and
Analysis of trends to identify opportunities for improvement.
Marchman Act (397.431, FS)
Publicly funded providers must have a fee system based
upon a client’s ability to pay, and if space and sufficient
state resources are available, may not deny a client access to
services solely on the basis of client’s inability to pay.
Full cost and fee charged must be disclosed to client
Client (or guardian of minor) required to contribute toward
costs, based on ability to pay
Guardian of minor not liable if services provided without
parent consent unless guardian ordered to pay
Appendix O - 29

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Marchman Act Baker Act
Parental Responsibility
No corresponding provisions other than the consent to
treatment for the minor and the application for voluntary
admission must be filed by the parent or guardian with the
agreement (assent) of the minor.
Designated Representative
Parental Participation (397.6759, FS)
A parent, legal guardian, or legal custodian who seeks involuntary
admission of a minor to substance abuse treatment is required to
participate in all aspects of treatment as determined appropriate
by the director of the licensed service provider.
Voluntary: No notice except emergency
Involuntary: Name/address/phone # of guardian, guardian
advocate & attorney in record. If no guardian, person selects
own representative. Only if person unable/unwilling to select,
facility must select from list, in order of listing:
Health care surrogate
Spouse
Adult child
Parent
Adult next of kin
Adult friend
The following shall not be designated:
Licensed professional serving the person
Employee of facility serving the person
DCF employee
Person in professional/business services
Creditor of person
Role of Designated Representative:
To receive notice of individual’s admission;
To receive notice of proceedings affecting the individual;
To have immediate access to the individual held or admitted for
mental health treatment, unless such access is documented to be
detrimental to the individual;
To receive notice of any restriction of the individual’s right to
communicate or receive visitors;
To receive copy of the inventory of personal effects upon
the individual’s admission and to request amendment to the
inventory at any time;
To receive disposition of the individual’s clothing and personal
effects, if not returned to the individual, or to approve an alternate
plan;
To petition on behalf of the individual for a writ of habeas corpus
To apply for a change of venue for the individual’s involuntary
placement hearing for the convenience of the parties or witnesses
or because of the condition of the individual;
To receive written notice of any restriction of the individual’s right
to inspect his or her clinical record;
To receive notice of release of the individual from a receiving
facility where an involuntary examination was performed;
To receive a copy of any petition for the individual’s involuntary
placement filed with the court; and
To be informed by the court of the individual’s right to an
independent expert evaluation, pursuant to involuntary
placement procedures.
No corresponding provisions in the Marchman Act
Appendix O - 30

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act
Marchman Act
No corresponding provisions in the Marchman Act
Baker Act
Guardian Advocate
Baker Act 394.4598, FS and 65E-5.230, FAC
Duties begin after appointment by court and completion of
training
Duties terminate upon person’s discharge, transfer to
voluntary status, restoration of competency, or expiration of
involuntary placement order.
Prior to appointment:
Receive information about duties/ethics of medical decision-
making
Agree to serve
Prior to decision-making:
Full disclosure of treatment information
Attend 4-hour training course approved by court (GA manual
and/or DCF on-line course)
Successfully pass test
Meet and talk with individual and physician in person if
possible; by telephone if not
Authority:
Mental health decisions and court may also authorize medical
decisions.
Extraordinary decisions after separate hearing (#3108-3109) for the
following:
Electroconvulsive treatment
Experimental treatments not approved by IRB
Sterilization
Abortion
Psychosurgery
Decisions by guardian advocate may be reviewed by court, upon
petition of person’s attorney, family or facility administrator
Replacement guardian advocate can be appointed by the court
Appendix O - 31

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Health Care Surrogates & Proxies
Baker Act 765 FS and 65E-5.2301, FAC
Advance Directive: instruction given by a person expressing his/her
desires about health care, including the designation of a health care
surrogate
Surrogate: Selected by the person, when competent, in an advance
directive. Person can designate an alternative surrogate, or a
separate surrogate for mental health than one for other medical
care
Proxy: In the absence of an advance directive, selected in priority
order from statutory list:
Guardian
Spouse
Adult child
Parent
Adult sibling
Adult relative
Close friend*
Clinical Social Worker*
Incapacity may not be inferred from the person’s voluntary or
involuntary hospitalization for mental illness or intellectual
disability.
Policy: On interim basis, between time person is determined
by a physician to be incapacitated to consent to treatment
and time guardian advocate is appointed by court to provide
express and informed consent to treatment, a health care
surrogate or proxy may provide or refuse consent.
Marchman Act
No corresponding provisions in the Marchman Act.
However, a health care surrogate or proxy provided under
chapter 765, FS is authorized to make any and all health
care decision for an individual who has been found by a
physician to be incompetent/incapacitated to make his/her
own health care decisions. Substitute Judgment required
if preference of individual is known.
Appendix O - 32

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Marchman Act Baker Act
Authority:
To make all health care decisions, including mental health,
based on the decisions the person would have made if
competent to do so – “Substitute Judgment”
Apply for benefits
Access person’s clinical record
Authorize release of information and clinical records
Authorize transfer to another facility.
Prohibited Procedures:
Voluntary admission to MH facility
Consent to treatment for persons on voluntary status
ECT
Experimental treatment not approved by IRB
Sterilization
Abortion
Psychosurgery
Process:
Attending physician documents incapacity of person
Surrogate or proxy notified in writing that authority has
commenced (#3122)
Proxy signs Affidavit (#3123)
Authority in effect until determination that person has regained
capacity
Petition for Adjudication of Incompetence to Consent to
Treatment and Appointment of Guardian Advocate (#3106) filed
within 2 court working days of physician determination
Provide to surrogate or proxy same information required to be
given to guardian advocate and make same training available
Ensure surrogate or proxy talks with individual and physician in
person if possible, if not, by telephone
Surrogate or proxy given full disclosure prior to requesting
authorization for treatment
Advance Directives can be revoked at any time by a competent
person
Decisions of a health care surrogate or proxy may be reviewed by a
judge at the request of the persons’ family, the facility, or physician,
or other interested person
Appendix O - 33

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Restraints & Seclusion
Baker Act 394.459(4), FS 65E-5.180(7), FAC
Restraint is a physical device, method, or drug used to control
behavior.
Physical restraint is any manual method or physical or mechanical
device, material, or equipment attached or adjacent to individual’s
body so he/she cannot easily remove the restraint and which
restricts freedom of movement or normal access to one’s body.
Physically holding a person during a procedure to forcibly
administer psychotropic medication is a physical restraint.
Drug used as a restraint is medication to control person’s behavior
or restrict freedom of movement & is not part of standard
treatment regimen of a person with a diagnosed mental illness.
(ETO not necessarily a chemical restraint)
Restraint excludes physical devices or other physical holding
when necessary for routine physical examinations and tests; or for
purposes of medical treatment; used to provide support for body
position or proper balance; or when used to protect a person from
falling out of bed.
Seclusion means physical segregation of person in any fashion or
involuntary isolation of person in an area person is prevented from
leaving by physical barrier or by a staff member who is acting in a
manner, or who is physically situated, so as to prevent person from
leaving.
Marchman Act (65D-30.005(14), FAC)
Restraint means:
Any manual method used or physical or mechanical device,
material, or equipment attached or adjacent to a client’s
body that he or she cannot easily remove and that restricts
freedom of movement or normal access to one’s body; and
A drug used to control a client’s behavior when that drug is
not a standard treatment for the client’s condition.
Seclusion means the use of a secure, private room designed to
isolate a client who has been determined by a physician to pose
an immediate threat of physical harm to self or others.
Prohibitions
Can’t be based on person’s history or on PRN or standing order
Can’t be restrained in prone position unless required to prevent
imminent serious harm
Objects impairing respiration can’t be placed over person’s face
-- staff may wear protective gear when needed.
Hands can’t be secured behind back except to prevent serious
injury
Walking restraints prohibited except for off-unit transportation
under direct observation of staff
Simultaneous S/R not used for minors
Can’t locate restrained person in areas subject to view by
anyone other than involved staff or where exposed to potential
injury by other persons.
Can’t be placed in S/R in nude or semi-nude state.
Prior to Restraint or Seclusion
Staff must be trained as part of orientation and on annual basis.
Specific required training itemized in rule.
Personal Safety Plan (3124) address individual triggers leading
to psychiatric crisis completed ASAP after admission and filed in
the person’s record.
Plan reviewed by team & updated as needed after each S/R.
Specific intervention techniques from personal safety plan
offered or used prior to S/R event documented in record.
Each person must be searched for contraband before or
immediately after being placed into seclusion or restraints
Appendix O - 34

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Initiating Restraint or Seclusion
RN or highest level staff permitted by policy, immediately
available & trained in S/R may initiate in emergency when
danger is imminent. S/R order obtained from physician, ARNP,
or PA, if permitted by the facility & stated within professional
protocol. If treating physician didn’t order S/R, must be
consulted ASAP.
Examination conducted within 1 hour by physician or delegated
to an ARNP, PA or RN, if authorized by facility & trained in S/R
including:
Face-to-face assessment of person’s medical/behavioral
condition
Review of record for pre-existing medical condition
contraindicating use of S/R
Review of person’s medication orders including an assessment
of the need to modify such orders during the period of S/R, and
Assessment of need or lack of need to elevate person’s head and
torso during restraint.
Orders for Restraint or Seclusion
Each written order for S/R limited to:
4 hours for adults, age 18 and over
2 hours for minors age 9 - 17; or
1 hour for children under age 9
All orders signed within 24 hours of initiation. S/R order may be
renewed up to total of 24 hours, after consultation/review by
physician, ARNP, or PA in person, or by telephone with a RN who
has physically observed/evaluated person.
When order has expired after 24 hours, physician, ARNP, or PA
must see/assess person before S/R can be re-ordered. Results
of assessment documented. Administrator notified of S/R use
exceeding 24 hours.
Order shall include specific behavior prompting use of S/R, the
time limits, & behavior necessary for release. Restraint orders
must contain type of restraint ordered & positioning of person,
considering age, physical fragility & physical disability.
Appendix O - 35

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
During Restraint and Seclusion
Each person immediately informed of behavior resulting in S/R
and criteria necessary for release.
Facility must notify guardian of minors in S/R ASAP, but no later
than 24 hours and document notice in record, including date/
time of notification & name of staff providing notification.
For each use of S/R, following information shall be documented
in record:
The emergency situation resulting in S/R; Alternatives/other less
restrictive interventions attempted or clinical determination
that less restrictive techniques could not be safely applied;
Name/title of staff initiating S/R
Date/time of initiation & release;
Person’s response to S/R, including rationale for continued use
of the intervention; and
That the person was informed of behavior resulting in S/R &
criteria necessary for release.
When restraint initiated, nurse must assess person ASAP but
no later than 15 minutes after initiation and at least every hour
thereafter. Assessment includes person’s circulation/respiration,
including vital signs
Seclusion of persons over age 12 must be observed by trained
staff every 15 minutes. At least one observation an hour
conducted by nurse. Restrained persons must have continuous
observation by trained staff. Secluded children age 12 and
under must be monitored continuously by face-to-face
observation or by direct observation through the seclusion
window for first hour and at least every 15 minutes thereafter.
During Restraint and Seclusion (continued)
Monitoring physical/psychological well-being of R/S person
by trained staff must include: respiratory and circulatory
status; signs of injury; vital signs; skin integrity & any special
requirements specified in facility policies.
During each period of S/R, person must be offered reasonable
opportunities to drink & toilet as requested and restrained
person must be offered opportunities for range of motion at
least every 2 hours.
Documentation of observations & staff ’s name recorded at each
observation.
Appendix O - 36

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
Appendix O
O
Baker Act Marchman Act
Release from Restraint and Seclusion
Release must occur as soon as person no longer an imminent
danger to self/others, followed by debriefing to decrease risk of
future S/R event & to provide support.
Review incident with person, giving opportunity to process the
S/R event ASAP – at least within 24 hours of release.
Review incident with all staff involved and supervisors ASAP
after the event and address:
Circumstances leading to the event,
Nature of de-escalation efforts and alternatives to seclusion and
restraint attempted,
Staff response to the incident, ways to effectively support the
person’s coping in the future and avoid the need for future S/R.
Review documented for continuous performance improvement/
monitoring. Review findings forwarded to Oversight Committee,
and within 2 working days, team meets to review circumstances
preceding initiation, review the person’s treatment plan and
Personal Safety Plan to determine if changes are needed to
prevent the further use of R/S.
Team will assess impact event had on person & provide
counseling, services, or treatment needed as a result. Team
must analyze person’s record for patterns relating to conditions,
events, or presence of other persons immediately before or
upon onset of behavior warranting S/R. Team must review
effectiveness of emergency intervention & develop more
appropriate therapeutic interventions.
Seclusion and Restraint Oversight Committee must conduct
timely reviews of each use of S/R and monitor patterns of use to
assure least restrictive approaches are used to prevent/reduce
frequency / duration of use.
Reporting Restraints and Seclusion
All facilities must electronically report monthly S/R events to
DCF - Webinar training to be scheduled when reporting process
is finalized
All facilities subject to CoP’s must report by telephone by next
business day to CMS (written report to DCF) any death that
occurs:
While a person is restrained or secluded;
Within 24 hours after release from R/S; or
Within one week after S/R, where it is reasonable to assume that
use of the S/R contributed directly or indirectly to the person’s
death.
Not Applicable
Immunity (consult with your attorney)
Any person who acts in good faith in compliance with the Baker
Act is immune from civil or criminal liability for his or her actions
in connection with the admission, diagnosis, treatment, or
discharge of a person to or from a facility. However, this section
does not relieve any person from liability if such person commits
negligence. (394.459)
No professional is required to accept persons for treatment of
mental, emotional, or behavioral disorders. Such participation is
voluntary (394.460)
A LEO acting in good faith pursuant to the Marchman Act
protective custody provisions may not be held criminally or
civilly liable for false imprisonment.
All persons acting in good faith, reasonably, and without
negligence in connection with the preparation of
petitions, applications, certificates, or other documents
or the apprehension, detention, discharge, examination,
transportation or treatment under the Marchman Act shall
be free from all liability, civil or criminal, by reason of such
acts
Appendix O - 37

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Baker Act & Marchman Act
Comparison
O
Baker Act Marchman Act
Training Resources
Baker Act
http://myflfamilies.com/service-programs/substance-abuse/baker-
act-manual
Copy of Baker Act law (394, Part I, FS) and rules (65E-5, FAC and
65E-12, FAC)
Baker Act forms – mandatory and recommended
Selected forms in Spanish & Creole
2014 Baker Act Handbook
Baker Act monitoring/survey instruments
Frequently Asked Questions (FAQ’s) on 21 subject areas
List of all public and private receiving facilities throughout the
state
Mental Health Advance Directives
Other relevant materials
Online Training www.bakeracttraining.org
On demand - at your convenience
Up-to-date material
No fee
Certificate of Achievement
CEC’s offered @ low cost
Courses Offered:
Introduction to the Baker Act
Emergency Medical Conditions & the Baker Act
Law Enforcement & the Baker Act
Long Term Care Facilities & the Baker Act
Consent for Minors
Rights of Persons in Mental Health Facilities
Guardian Advocacy
Suicide Prevention
Why People Die by Suicide
Trauma Series
Marchman Act
http://myflfamilies.com/service-programs/substance-abuse/
marchman-act
Contents include:
2003 Marchman Act User Reference Guide includes among
other issues:
Statute & Rules
History & Overview
Marchman Act Model Forms
Law Enforcement and Protective Custody
Quick Reference Guide for Involuntary Provisions
Flow Charts for Involuntary Provisions
Admission & Treatment of Minors
Where to Go for Help
Marchman Act Pamphlet
Substance Abuse Program Standards
Common Licensing Standards
Marchman Act PowerPoint Presentation
Array of substance abuse related courses funded by DCF and
offered through FADAA, FADAA@FADAA.org.
Appendix O - 38

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix P - 1
Resources
Appendix P
P
Resources
The following sites may contain information that may be of interest to you in a professional or advocacy capacity.
This list does not constitute endorsement. Information accurate as of December 15, 2013.
Many communities have adopted the “211” toll-free
information programs that can guide a person in seeking
any type of health and social service program. Some of these
programs are operated on a 24-hour a day, 7-day a week basis.
ere are several resources that you may turn to for help
in implementing the Baker Act and in protecting the
rights of persons served under the Act. In most instances,
problems can be resolved with facility sta and ultimately,
the facility administrator. However, any one of the
following may be helpful.
Department of Children & Family
Services
e Department (DCF) is designated by the Florida
Legislature as the State’s Mental Health Authority. It is
responsible for designating receiving facilities to serve persons
under the Baker Act. It shares responsibility with the Agency
for Health Care Administration to supervise all mental health
facilities, programs and services. DCF oce phone numbers
can be found at the front of this Handbook. Visit http://www.
dcf.state..us/programs/samh/mentalhealth/index.shtml/
Managing Entities
e Florida Legislature amended Chapter 394.9082, FS in
2008 authorizing behavioral health managing entities under
contract with DCF to manage the day-to-day operational
delivery of behavioral health services through an organized
system of care. is is accomplished through “Provider
networks” that are the direct service agencies that are under
contract with a managing entity and that together constitute
a comprehensive array of emergency, acute care, residential,
outpatient, recovery support, and consumer support services.
While private receiving facilities are generally overseen
directly by DCF, those designated as public receiving facilities
that benet from legislatively appropriated Baker Act funds
are overseen by the local Managing Entity.
Baker Act Website
e primary DCF website is http://www.MyFlorida.com.
To access extensive Baker Act information, visit http://www.
dcf.state..us/programs/samh/mentalhealth/laws/index.shtml.
Updated information about the Baker Act can also be found
at the Baker Act Reporting Center website
(http://bakeract.fmhi.usf.edu).
Receiving Facility List
e Baker Act Receiving Facility List and table describing
Transportation Exception Plans are no longer contained
within the manual. is is because of the changing nature
of this information and the desire to make the most up
to date information available. Documents containing this
information can be found online at
http://bakeract.fmhi.usf.edu
Baker Act Training Online
As a substitute for attending a face to face training, you
may wish to take the online courses instead. Continuing
Education credits are available for licensed professionals for a
fee. ere is NO FEE for this training! To get started, please
visit: http://www.bakeracttraining.org
Florida Abuse Registry
e Registry, operated by the Department of Children
and Families, accepts calls reporting abuse, neglect or
exploitation of vulnerable persons, including children,
elders, and disabled adults. e statewide toll-free Registry is
available at all times at 1-800-96-ABUSE.
Agency for Health Care Administration
AHCA is responsible for licensing all hospitals, crisis
stabilization units, and residential treatment facilities in
Florida, as well as other types of health care facilities and
programs. It is also responsible to the federal Centers
for Medicare and Medicaid Services (CMS) for ensuring
hospitals’ compliance with all applicable federal laws
and regulations. AHCA’s statewide toll-free complaint
telephone number is 1-888-419-3456.
Professional Regulation
Reports on physicians, psychologists, social workers, and
other mental health professionals can be directed to e
Florida Department of Health, Oce of Medical Quality
Assurance, at a statewide, toll-free number 1-888-419-3456.
Reports on nurses can be directed to e Florida Board of
Nursing in Jacksonville at 1-850-245-4125, press #6.
Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Resources
Appendix P - 2
P
Other State Agencies
Official Portal for the State of Florida
http://www.myorida.com
State of Florida Agencies
http://www.myorida.com/directory/
Department of Mental Health Law & Policy
Louis de la Parte Florida Mental Health Institute
USF College of Behavioral & Community Sciences
813-974-4510
http://mhlp.fmhi.usf.edu
Baker Act Reporting Center
http://bakeract.fmhi.usf.edu/
Florida Department of Corrections
http://www.dc.state..us
Florida Department of Elder Affairs
4040 Esplanade Way, Tallahassee, FL 32399-7000
850-414-2000
http://elderaairs.state..us
Florida Department of Juvenile Justice
850-488-1850
http://www.djj.state..us
Federal Agencies
The Centers for Disease Control and Prevention (CDC)
http://www.cdc.gov/
Center for Substance Abuse Treatment (CSAT )
http://csat.samhsa.gov/
Federal Food and Drug Administration
MedWatch is a service of the federal FDA Medical
Products Reporting Program for professionals and
consumers to report problems with medications and
other products.
5600 Fishers Lane
Rockville, MD 20857-9787
1-800-FDA-1088
http://www.fda.gov/Safety/MedWatch/default.htm
National Coalition of Hispanic Health & Human Services
Organizations
1501 16
th
Street NW
Washington, DC 20036
202-387-5000
http://www.cossmho.org
National Criminal Justice Reference Service
http://www.ncjrs.org
National Domestic Violence Hotline
800-799-SAFE (7233)
http://www.thehotline.org/
National Health Information Center
P.O. Box 1133
Washington, DC 20013-1133
240-453-8280
email: [email protected]
http://www.health.gov/nhic
National Institute on Justice
http://www.nij.gov/Pages/welcome.aspx
National Institute of Mental Health
http://www.nimh.nih.gov
Office of Juvenile Justice and Delinquency Prevention
http://www.ojjdp.gov/
Social Security Administration
http://www.ssa.gov
Society for Prevention Research
http://www.preventionresearch.org
Substance Abuse and Mental Health Service
Administration
U.S. Department of Health and Human Services
http://www.samhsa.gov
Treatment locator: www.ndtreatment.samhsa.gov
U.S. Department of Health and Human Services
http://www.hhs.gov

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix P - 3
Resources
Appendix P
P
Advocacy Organizations
Disability Rights Florida, Inc.
e Disability Rights Florida, Inc. is a private non-
prot organization that receives federal funding to
protect and advocate for the rights of persons of all ages
who have disabilities. e Center provides a wide range
of services to persons who have mental illnesses who
believe they have experienced serious incidents of abuse
or neglect, or civil rights violations related to their
disabilities. e Center prioritizes services to people
in institutional, inpatient, or residential treatment
settings, but also provides services to individuals living
in their communities, as resources allow. e Center
has oces in Tallahassee, Tampa, and Ft. Lauderdale,
from which it serves the entire state of Florida. e
statewide toll-free phone number is 1-800-342-0823.
http://www.disabilityrightsorida.org/
Bazelon Center for Mental Health Law
e Bazelon Center for Mental Health Law is a
nonprot organization devoted to improving the lives
of people with mental illnesses through changes in
policy and law.
e Bazelon Center envisions an America where people
who have mental disabilities exercise their own life
choices and have access to the resources that enable
them to participate fully in their communities.
http://www.bazelon.org
Florida Partners in Crisis
Florida Partners in Crisis is a unique statewide
organization. Membership includes judges, law
enforcement, prosecutors, public defenders, mental
health and substance abuse providers, hospital
administrators, people recovering from mental illnesses
and/or substance use disorders and their families
and loved ones. Membership in Partners is a way
to stay informed of mental health, substance abuse
and criminal justice system policy developments and
funding decisions. It also oers members opportunities
for eective advocacy on behalf of mental health and
substance abuse services for people in need.
http://www.pic.org/
Family Support
National Alliance on Mental Illness of Florida
NAMI has its state oce in Tallahassee, which can be
reached at 850-671-4445. Local chapters of NAMI are
located throughout the state. www.nami.org
Al-Anon/Alateen Family Group
http://www.al-anon.alateen.org/
Bi-Polar and Depressive Alliance
Check phone book for chapter in your area.
www.dbsalliance.org/
Families Anonymous
http://www.familiesanonymous.org
Florida’s Center for the Advancement of Child Welfare
Practice
e Center’s mission is to support and facilitate the
identication, expansion, and transfer of expert knowledge
and best practices in child welfare case practice, direct
services, management, nances, policy, and organizational
development to child welfare and child protection
stakeholders throughout Florida.
http://centerforchildwelfare.fmhi.usf.edu
Mental Health America
(formerly: National Mental Health Association)
From its inception in 1909, MHA has been dedicated to
improving the lives of individuals and families aected by
mental illness.
http://www.mentalhealthamerica.net/
Florida Affiliates
MHA of Broward County
http://www.mhabroward.org/
MHA of Central Florida, Inc.
http://www.mhacf.org/
MHA of Greater Tampa Bay, Inc.
http://www.mhagreatertampabay.org/
MHA of Indian River County
http://www.mhairc.org/
MHA of Northeast Florida, Inc.
http://www.mhajax.org/
MHA of Okaloosa & Walton Counties
http://www.mhaow.org/
MHA of Palm County
http://www.mhapbc.org/index.cfm
MHA of Southwest Florida
http://www.mhasw.org/
MHA of Volusia and Flagler Counties
http://www.mhavolusia.org/
MHA of West Florida, Inc.
http://www.mhaw.org/

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Resources
Appendix P - 4
P
Older Adults Addictions
AARP Health Advocacy Services
601 E Street, NW
Washington, DC 20049
1-888-OUR-AARP (1-888-687-2277)
AARP Policy & Research
AARP’s sta of policy analysts, economists, attorneys,
researchers and industry experts specializes in a vast
range of topics relating to older adults and aging both
domestically and globally.
http://www.aarp.org/research/
Aging Related Web Sites
http://www.publichealth.uga.edu/geron/
Area Agencies on Aging (Aging Resource Center)
http://elderaairs.state..us/doea/aaa.php
Clearinghouse on Abuse and Neglect of the Elderly (CANE)
Department of Consumer Studies and Research
University of Delaware
297 Graham Hall
Newark, DE 19716
http://www.cane.udel.edu/
Elder Helpline
1-800-96-Elder (1-800-963-5337)
Institute for Memory Impairments and Neurological
Disorders
http://www.alz.uci.edu
National Center on Elder Abuse
Part of the federal Administration on Aging, the National
Center on Elder Abuse (NCEA) serves as a national
resource center dedicated to the prevention of elder
mistreatment.
http://www.ncea.aoa.gov/
National Institute on Aging Information Center
Building 31, Room 5C27
31 Center Drive, MSC 2292
Bethesda, MD 20892
800 222-4225
http://www.nia.nih.gov/
Senior Citizens’ Resources
Ocial information and services from the U.S.
government
http://www.usa.gov/Topics/Seniors.shtml
Alcoholics Anonymous World Services Inc
475 Riverside Drive at West 120th St.
New York, NY 10115
212 870-3400
http://www.aa.org
Center for Substance Abuse Treatment
National Drug & Alcohol Treatment Referral Service
800 662-HELP (4357)
http://beta.samhsa.gov/about-us/who-we-are/
oces-centers/csat
Florida Alcohol and Drug Abuse Association
http://www.fadaa.org
National Association of Drug Court Professionals (NADCP)
http://www.nadcp.org/
Gamblers Anonymous
P.O. Box 17173, Los Angeles, CA 90017
626-960-3500
http://www.gamblersanonymous.org/
Narcotics Anonymous
http://www.na.org/index.php
National Families in Action
http://www.nationalfamilies.org
National Institute on Alcoholism and Alcohol Abuse
(NIAAA)
http://www.niaaa.nih.gov/
Overeaters Anonymous
http://www.oa.org

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix P - 5
Resources
Appendix P
P
Other Resources
Criminal Justice/Mental Health Justice Center
The Council of State Governments
CSG Center: http://csgjusticecenter.org/mental-health/
SAMHSA’s GAINS Center for Behavioral Health and Justice
Transformation
http://gainscenter.samhsa.gov/
National Association of State Mental Health Program
Directors (NASMHPD)
http://www.nasmhpd.org/index.aspx
Center for the Study and Prevention of Violence (CSPV)
e CSPV, a research program of the Institute of
Behavioral Science at the University of Colorado at
Boulder, was founded in 1992 to provide informed
assistance to groups committed to understanding and
preventing violence, particularly adolescent violence.
Since that time, our mission has expanded to encompass
violence across the life course.
http://www.colorado.edu/cspv/index.html
Florida Council for Community Mental Health
e Florida Council for Community Mental Health
(FCCMH) is a statewide association of 70 community-
based mental health and substance abuse agencies.
http://www.fccmh.org/
National Strategy for Suicide Prevention
A collaborative eort of
SAMHSA, CDC, NIH, HRSA, HIS
http://www.samhsa.gov/prevention/suicide.aspx
National Suicide Prevention Lifeline
1-800-273-TALK (8255)
http://www.suicidepreventionlifeline.org/
Baker Act Online Training
Training is available online. is training was developed by
the Louis de la Parte Florida Mental Health Institute sta
and faculty at the University of South Florida with funds
from the Florida Department of Children and Families. e
online training consists of seven training modules, as well
as four Web Events that were recorded and are available for
viewing online.
e online training is free. Continuing education credits are
available for a wide variety of professionals. ere is a fee for
the administration of the continuing education credits.
Training is available at http://www.bakeracttraining.org/
Online Training Modules
Introduction to the Baker Act
Emergency Medical Conditions
Individual Rights & the Bake Act
Law Enforcement & the Baker Act
Long Term Care & the Baker Act
Minors and the Baker Act
Suicide Prevention
Recorded Web Events Available Online
Seclusion & Restraint
Kevin Huckshorn, PhD, RN, MSN, CAP, ICADC
Trauma Series
Norin Dollard, PhD., & Victoria Hummer, LCSW
Why People Die by Suicide
omas Joiner, PhD
Baker Act & Marchman Act Comparison & Co-Occurring
Disorders
Martha Lenderman, MSW & Holly Hills, PhD
Online Guardian Advocate Training
is training was developed by the same faculty/sta who
developed the Baker Act online training mentioned above.
As of December 2013, this Guardian Advocate training has
been approved for Florida Judicial Circuits 2, 3, 5, 7, 8, 9,
11, 12, 13, 14, 17 and 20. e Guardian Advocate Training
is available at this site: http://guardianadvocate.org/.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Resources
Appendix P - 6
P

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix Q - 1
Military Service Members
and Veterans
Appendix Q
Q
Military Service Members and Veterans
Some people subject to various aspects of the Baker Act, such
as involuntary examination or inpatient placement, may be
serving or may have served in the US military. Services, benets
and information available to veterans may be considered for
these individuals. Some of the resources mentioned below may
also be relevant to those who are still in the military. Although,
with a few exceptions, services oered by the Veterans’ Health
Administration are not available to those who have not yet
separated from the military.
ere are many services, exemptions and designations available
to veterans. However, these usually require proof of veteran
status. How people, various agencies, and particular laws or
rules dene the term “veteran” varies. Not all people who
served in the US Armed Forces are considered veterans based
on the denition some use for the term “veteran.” Further,
not all veterans are eligible for VA Benets, such as pensions
or VA health care. Eligibility for such services is based on a set
of complicated factors, including length of service, nature of
service, era of service, income, disability status according to the
VA, and discharge status. Discharge status can be:
Honorable
General (Honorable Conditions)
General (Without Honorable Conditions)
Other than Honorable
Bad Conduct
Dishonorable
Just because a person does not have an Honorable discharge
does not mean he/she has a Dishonorable discharge. ere are
some VA funded services available to people with less than an
Honorable, but more than a Dishonorable discharge status.
Further, there is a process that can be pursued to try to get
a person’s discharge status reclassied. e Real Warrior site
describes this reclassication process: http://www.realwarriors.
net/veterans/discharge/upgrade.php
DD-214
Getting access to benets and other oers available to
veterans usually requires proof of veteran status. is often
means having a DD-214 – the “Report of Separation.” is
document lists, among other things, the person’s discharge
status. DD-214s may be requested via the National Archives in
St. Louis (see http://www.archives.gov/veterans/). e process
for emergency requests is described here: http://www.archives.
gov/veterans/military-service-records/#emergency.
Identifying Veterans
Providers would ideally have a systematic way to identify
veterans. e question “are you a veteran?” is not the best
question to ask in order to determine if someone is a veteran.
Rather, asking “have you ever served in the US Armed Force?”
is a better question. is is because some people who are
veterans may not consider themselves veterans. is may be
because they think they must access benets or health care at
the VA to be considered a veteran. Some people also may have
discharge statuses that are not Honorable, so do not consider
themselves veterans because of their discharge status.
Asking if a person has served in the US Armed Forces is the
broadest question. It will allow agency sta to determine if a
person is currently in the armed forces or if he/she has ever
been in the armed forces. For people who say they served in
the US armed forces in the past, then asking about discharge
status, if they have a DD-214, if they have accessed VA
services, and where they access these VA services may be
helpful. If the person does not have a DD-214 assisting
him/her to order one may be helpful. One suggestion is to
keep copies of the form used to request a DD-214 on hand
to give to veterans, and if needed, to assist them to ll it out
and fax it. For form see: http://www.archives.gov/veterans/
military-service-records/
A GAINS Center report that focuses on justice involved
veterans has a helpful set of suggested questions to gather
information about veteran status. It is available at: http://
gainscenter.samhsa.gov/pdfs/veterans/CVTJS_Report.pdf
Organizations
It is helpful to establish contacts with various agencies/
organizations to address issues for veterans. Some of these
organizations are listed below.
Florida Department of Veterans Affairs (FDVA)
Mission: “To advocate with purpose and passion for
Florida veterans and link them to superior services,
benets and support.”
Vision: “FDVA is the premier point of entry for Florida
veterans to accessed earned services, benets and
support.”
e FDVAs Florida Veterans’ Benets Guide may be
found here: http://oridavets.org/?page_id=110. e
FDVA website has a wealth of information that can be
helpful to veterans and their families.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Military Service Members
and Veterans
Appendix Q - 2
Q
e “Resources” section of the FDVAs website a
wealth of information: http://oridavets.org/?page_
id=31
Locations and phone numbers for FDVAs 24 Claim
Examiner Sites can be found here: http://oridavets.
org/?page_id=91
US Veterans’ Administration
e US Veterans’ Administration is composed
of three organizational parts: a) VBA (Veteran
Benet Administration), VHA (Veteran Health
Administration), and the VA National Cemetery
Administration. Vet Centers, discussed later in
this appendix, are separate from the US Veterans’
Administration.
A list of and links to a variety of services oered by
the United States Department of Veterans’ Aairs
is available at http://www.va.gov/directory/guide/
fac_list_by_state.cfm?State=FL&dnum=1&isash=0.
is includes
» VA Medical Centers
» Outpatient Clinics
» Community Service Programs
» Community Based Outpatient Clinics
» Vet Centers
Links to the VBA or Veteran Benet Administration
Oces in Florida are also listed on this web page.
An interactive search to nd services oered by the VA
can be done here: http://www.va.gov/directory/guide/
home.asp?isash=1. is will search locations for the
following services:
» VHA Facilities (Health Care, as well as Homeless
programs)
» VBA Facilities (Benets)
» Vet Centers
» PTSD Programs
» Substance Use Disorder (SUD) Programs
Facilities in Florida are listed here: http://www2.
va.gov/directory/guide/fac_list_by_state.cfm?State=FL
County Veteran Service Officers
Each of Florida’s 67 counties has a Veteran Service Oce.
A list of these may be found at: http://oridavets.org/
wp-content/uploads/2013/10/CVSO_Directory_1-
October-2013.pdf
Florida’s Veteran Service Organizations
Florida has several congressionally designated Veteran Service
Organizations. ese organizations have departments, posts
and chapters in Florida. ey serve Florida’s veterans in a
variety of ways. Below is a list of some of these organizations.
is list can also be found at the Florida Department of
Veteran Aairs website at http://oridavets.org/?page_id=52
American Gold Star Mothers
http://www.goldstarmoms.com/Depts/AllDepts/
AllDepts.htm
American Legion
http://oridalegion.org/
AMVETS
http://amvets.org/
Disabled American Veterans
http://www.davmembersportal.org//
Korean War Veterans Association
http://d.kwva.org/
Military Ocers Association of America
http://www.moaa.org/
Military Order of the Purple Heart
http://www.oridapurpleheart.org/
Paralyzed Veterans of America
http://www.pva.org/site/c.ajIRK9NJLcJ2E/b.6463495/k.
C5D5/Florida.htm
Veterans of Foreign Wars
http://myoridavfw.org/
Vietnam Veterans of America
http://vvafsc.org/
Specific Populations
Combat Veterans
Vet Centers oers services, but are separate from the VA
Health Administration, including VA Health Centers. Vet
Centers focus their services on “War Zone Veterans” (see
http://www.vetcenter.va.gov/Eligibility.asp for eligibility).
Vet Centers also oer assessment and referral for Military
Sexual Trauma Counseling oered by VA Health Centers.
is assessment and referral service is available at Vet
Centers not just War Zone Veterans, but for any veteran
who has experienced this type of trauma (see http://www.
vetcenter.va.gov/Military_Sexual_Trauma.asp).
Vet Centers also oer services to family members who
meet certain eligibility requirements.
Vet Center information during normal business hours is
available at 1-800-905-4675.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix Q - 3
Military Service Members
and Veterans
Appendix Q
Q
Information in Spanish is available at: http://www.
vetcenter.va.gov/Servicios.asp
Women
e Women Veterans Call Center number is 1-855-VA-
WOMEN or 1-855-829-6636
Woman Veterans Program Information can be found at
http://www.va.gov/womenvet/
Justice Involved Veterans
Each VA Medical Center has at least one Veteran Justice
Outreach (VJO) specialist. If a person has justice system
involvement, the VJO may be a resource. Additional
information about justice involved veterans, as well as
contact information for VJOs is available at http://www.
va.gov/HOMELESS/VJO.asp
In 2012, language was added to the Florida Statutes specic
to military veterans and service members court programs.
394.47891 Military veterans and service members court
programs
e chief judge of each judicial circuit may establish a Military
Veterans and Service members Court Program under which
veterans, as dened in s. 1.01, and service members, as dened
in s. 250.01, who are convicted of a criminal oense and
who suer from a military-related mental illness, traumatic
brain injury, substance abuse disorder, or psychological
problem can be sentenced in accordance with chapter 921 in a
manner that appropriately addresses the severity of the mental
illness, traumatic brain injury, substance abuse disorder,
or psychological problem through services tailored to the
individual needs of the participant. Entry into any Military
Veterans and Service Members Court Program must be based
upon the sentencing court’s assessment of the defendant’s
criminal history, military service, substance abuse treatment
needs, mental health treatment needs, amenability to the
services of the program, the recommendation of the state
attorney and the victim, if any, and the defendant’s agreement
to enter the program.
OEF/OIF/OND Veterans
Links to VA resources and other information for people
who served in Operation Enduring Freedom (OEF),
Operation Iraqi Freedom (OIF), and/or Operation New
Dawn (OND) are available at http://www.oefoif.va.gov/
VA Medical Centers have people working as OEF/OIF
Coordinators. Links to the OEF/OIF resources at each
of Florida’s six VA Medical Centers can be found here:
http://www.oefoif.va.gov/map.asp
Veterans who Experienced Trauma
e National Center for PTSD has many resources
related to trauma (see: http://www.ptsd.va.gov/index.
asp)
Veterans Who Experienced Military Sexual Trauma
Information about many resources for veterans who
experienced Military Sexual Trauma are available here:
http://www.mentalhealth.va.gov/msthome.asp
Veterans Who Are Homeless or Who Are At Risk for
Homelessness
Over the past several years the VA has put a great deal of
focus on ending homelessness among veterans. Several
programs – such as HUD-VASH and Grants-Per-
Diem are available to veterans (see http://www.va.gov/
homeless/index.asp or call 1-877-424-3838).
Veterans Health Initiative
While most of the resources in this appendix
address information, referral, assessment and service
provision for veterans, the VHI focuses on training for
professional.
e VHI website states that the “VA developed the
Veterans Health Initiative (VHI) independent study
courses to increase VA providers’ knowledge of military
service-related diseases and illnesses. e VHI study
guides are useful as well for non-VA providers, VA
employees (through the VA Talent Management System),
Veterans and the public. e courses are accredited and
meet medical licensure requirements” (see http://www.
publichealth.va.gov/vethealthinitiative/index.asp).
is includes information on a variety of topics:
» Agent Orange
» Traumatic Brain Injury (TBI)
» Traumatic Amputation
» Military Sexual Trauma
» Hearing Impairment
» Visual Impairment
» Gulf War
» War Wounded (OEF/OIF/OND)
» Post-Traumatic Stress Disorder

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Military Service Members
and Veterans
Appendix Q - 4
Q
Veterans’ Crisis Line
e Veterans’ Crisis Line’s website has text stating that it
“connects Veterans in crisis and their families and friends with
qualied, caring Department of Veterans Aairs responders
through a condential toll-free hotline, online chat, or text.
Veterans and their loved ones can call 1-800-273-8255 and
Press 1, chat online, or send a text message to 838255 to
receive condential support 24 hours a day, 7 days a week, 365
days a year.” (See http://veteranscrisisline.net/)
Support for deaf and hard of hearing individuals is available.
TTY Number: 1-800-799-4889
Key Phone Numbers
Veterans’ Crisis Line 1-800-799-4899; TTY
1-800-799-4889
VA Benets 1-800-827-1000
VA Homeless Programs 1-877-424-3838
VA Women Veterans Call Center 1-855-VA-WOMEN or
1-855-829-6636
Vet Centers 1-800-905-4675
Florida Department of Veterans 1-805-487-1533
Aairs (FDVA)
Veteran’s Issues and the Baker Act
ere are two sections of the Baker Act that directly address issues specic to veterans. Information on the Military Veterans
and Service Members Court Program (394.47891, F.S.) was mentioned on page Q-3. Below is the other section of the Baker
Act that addresses veterans.
394.4672 Procedure for placement of veteran with federal agency.
(1)Whenever it is determined by the court that a person
to the application of the law of the placing state or district
meets the criteria for involuntary placement and it appears
with respect to the authority of the chief ocer of any
that such person is eligible for care or treatment by the
facility of the United States Department of Veterans Aairs
United States Department of Veterans Aairs or other
or other federal agency operated in this state to retain
agency of the United States Government, the court, upon
custody or to transfer, parole, or discharge the person.
receipt of a certicate from the United States Department
(3)Upon receipt of a certicate of the United States
of Veterans Aairs or such other agency showing that
Department of Veterans Aairs or such other federal
facilities are available and that the person is eligible for
agency that facilities are available for the care or treatment
care or treatment therein, may place that person with the
of mentally ill persons and that the person is eligible for
United States Department of Veterans Aairs or other
care or treatment, the administrator of the receiving or
federal agency. e person whose placement is sought shall
treatment facility may cause the transfer of that person
be personally served with notice of the pending placement
to the United States Department of Veterans Aairs or
proceeding in the manner as provided in this part, and
other federal agency. Upon eecting such transfer, the
nothing in this section shall aect his or her right to appear
committing court shall be notied by the transferring
and be heard in the proceeding. Upon placement, the
agency. No person shall be transferred to the United States
person shall be subject to the rules and regulations of the
Department of Veterans Aairs or other federal agency
United States Department of Veterans Aairs or other
if he or she is conned pursuant to the conviction of any
federal agency.
felony or misdemeanor or if he or she has been acquitted
(2)e judgment or order of placement by a court of
of the charge solely on the ground of insanity, unless prior
competent jurisdiction of another state or of the District
to transfer the court placing such person enters an order
of Columbia, placing a person with the United States
for the transfer after appropriate motion and hearing and
Department of Veterans Aairs or other federal agency for
without objection by the United States Department of
care or treatment, shall have the same force and eect in this
Veterans Aairs.
state as in the jurisdiction of the court entering the judgment
(4) Any person transferred as provided in this section
or making the order; and the courts of the placing state or of
shall be deemed to be placed with the United States
the District of Columbia shall be deemed to have retained
Department of Veterans Aairs or other federal agency
jurisdiction of the person so placed. Consent is hereby given
pursuant to the original placement.

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
Appendix R - 1
FAQ
Appendix R
R
Frequently Asked Baker Act Questions
Frequently Asked Questions can be found on the States Baker Act internet site
located at www.dcf.state..us/programs/samh/mentalhealth/laws/index.shtml.
Nearly a thousand pages of Frequently
EMTALA / Insurance Examination
Asked Questions about the Baker Act
and related issues categorized in 21
major groups and up to 17 subgroups
are posted to the DCF Mental Health
Program website. ese FAQs may
provide signicant guidance, but do
not represent legal advice. ese are
all real questions that have been asked
and answered over the years with all
identiers removed.
Baker Act Forms
Clinical Records &
Confidentiality
Clinical Record
Condentiality
HIPAA
Public Records
Discharge Planning
Emergency Medical
Conditions, EMTALA, Hospital
Transfers
Emergency Medical Condition
Dened
Medical Conditions of Persons
under the Baker Act
EMTALA Applicability
Medical Clearance
EMTALA / Medical Screening
Baker Act Involuntary Examination
Stabilization
Informed Consent for Transfer
Forms / Paperwork
Transfers
Nearest Facility for Transfer
Transfers under the Baker Act
Crisis Stabilization Units (CSU’s)
EMTALA / Reverse Dumping
Transportation
Law Enforcement
Emergency Treatment Orders
Restraints
Chemical Restraints
Initiation of Emergency Treatment
Emergency Medications
Guardian Advocates & Other
Substitute Decision-Makers
PRN & Standing Orders Prohibited
Forms
Involuntary Placement Petition
ETO’s for Medical Treatment
Express and Informed Consent
Competence to Consent
Incompetence to Consent
Disclosure
Consent to Treatment
Initiation of Psychiatric Treatment
Mental Health Advance Directives
Electroconvulsive erapy
Consent to Medical Treatment
Guardian Advocates & Other
Substitute Decision Makers
General
Court Appointed Guardians
(Chapter 744, FS)
Guardian Advocates
Health Care Surrogates & Proxies
Other Substitute Decision Makers
Medical Consent
Involuntary Examinations
Professional Credentials
Criteria
Initiation
Transport
Acceptance
Conversion to Voluntary Status
Release from Involuntary
Examination
Transfers
Baker Act Reporting
Nursing Home / ALF Initiations
Notices
Medical Conditions
Elopement
Miscellaneous
Involuntary Inpatient
Placement
Criteria
Initiation & Filing of Petitions
Public Defender & State Attorney
Witnesses
Continuances
Waiver of Hearings
Conversion to Voluntary Status
Hearings
Involuntary Placement Orders
Continued Involuntary Inpatient
Placement
Baker Act Forms
Elopements
Transfers of Persons under
Involuntary Placement
State Treatment Facilities &
Transfer Evaluations
Discharge of Persons under
Involuntary Placement
Convalescent Status

Baker Act Handbook and User Reference Guide s 2014
State of Florida Department of Children & Families
FAQ
Appendix R - 2
R
Involuntary Outpatient
Placement
Law Enforcement
Denition of Law Enforcement
Ocer
Voluntary Admissions
Initiation of Involuntary
Examination
Execution of Involuntary
Examination
Criminal Charges
Restraining Devices
Receiving Facility Responsibilities
Paperwork Required
Rights of Persons
Consular Notication & Access
Training
Warrantless Entry
Long-Term Care Facilities
Alternatives to the Baker Act
Voluntary Admissions
Involuntary Examination
Transportation
Transfers
Refusal to Accept Back
Marchman Act
General
Protective Custody – Law
Enforcement
Transportation
Licensed Substance Abuse Facilities
Responsibilities of Licensed
Facilities
Emergency Medical Conditions
Involuntary Admissions
Involuntary Treatment
Appellate Cases
Minors
Minority Dened
Informed Consent for Treatment
Voluntary Admissions
Involuntary Examinations
Transportation & Transfers
Involuntary Placement
Separation of Minors from Adults
Juvenile Delinquency
Receiving Facilities
Professional Credentials
General
Physicians
Physician Assistants
Psychologists
Psychiatric Nurses
Chapter 491 Professionals
Veteran’s Aairs
Involuntary Placement
Receiving Facilities
General
Designation
Public Receiving Facilities & CSU’s
Involuntary Status
Inducements
State Hospital Transfers
Rights of Persons in Mental
Health Facilities
General
Right to Dignity & Privacy
Advance Directives
Right to Treatment
Communication Restrictions
Clinical Records & Condentiality
Custody of Personal Possessions
Designated Representatives
Habeas Corpus
Right to Discharge
Training
Transportation under the
Baker Act
General
Transportation Exception Plans
Voluntary Status
Responsibility of Receiving
Facilities & Hospitals
Nearest Receiving Facility
Criminal Charges
Delegation of Transportation to
Medical Transport
Transfers
EMTALA/Transportation
Transport to State Hospitals
(Treatment Facilities)
Juvenile Justice
Transport for Involuntary
Placement
Marchman Act
Voluntary Admissions – Adults
Requirements for Voluntary
Admission
Competence to Provide Express &
Informed Consent
Right to Request Release
Guardians & Other Substitute
Decision-Makers
Transfers in Legal Status
Requirements for Voluntary
Admission
Access to State Mental Health
Facilities
Weapons & Contraband
Weapons in Field
Weapons at Psychiatric Hospitals
Contraband

Baker Act Forms
Baker Act Forms – Table of Contents
Form # Title Page #
3001* Ex Parte Order for Involuntary Examination 1
3002* Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (2-sided; 4 pages) 3
3008* Order for Involuntary Inpatient Placement 7
3021* Notice of Petition for Involuntary Placement 9
3022* Application for Appointment of Independent Expert Examiner 11
3024* Notice of Petition for Continued Involuntary Inpatient Placement 13
3031* Order for Continued Involuntary Inpatient Placement or for Release 15
3032* Petition for Involuntary Inpatient Placement (2-sided; 3 pages) 17
3033* Notification to Court of Withdrawal of Petition for Hearing on Involuntary Inpatient or Involuntary Outpatient Placement 21
3035* Petition Requesting Authorization for Continued involuntary Inpatient Placement (2-sided 2 pages) 23
3036* Notice of Right to Petition for Writ oh Habeas Corpus or for Redress of Grievances 25
3038* Notice of Release or Discharge 27
3040* Application for Voluntary Admission of an Adult (Receiving Facility) 29
3042a* General Authorization for Treatment Except Psychotropic Medications 31
3042b* Specific Authorization for Psychotropic Medications 33
3043* Inventory of Personal Effects 35
3044* Authorization for Release of Information 37
3045* Notice of Person’s Admission for Involuntary Examination 39
3046* Application for and Notice of Transfer to Another Receiving or Treatment Facility 41
3048* Confidentiality Agreement 43
3049* Restriction of Communication or Visitors 45
3051a* Notice of Right of Person on Voluntary Status to Request Discharge From a Receiving Facility (2-sided; 2 pages) 47
3051b* Notice of Right of Person on Voluntary Status to Request Discharge From a Treatment Facility (2-sided; 2 pages) 49
3052a** Report of Law Enforcement Officer Initiating Involuntary Examination (MANDATORY) 55
3052b** Certificate of Professional Initiating Involuntary Examination (2-sided; 2 pages) (MANDATORY) 53
3057* Authorization for Electroconvulsive Treatment 55
3084** Baker Act Service Eligibility (MANDATORY ) 57
3089* Transfer Evaluation (To a State Mental Health Treatment Facility) (MANDATORY) 59
3090* Petition for Writ of Habeas Corpus or for Redress of Grievances (2-sided; 2-pages) 61
3097* Application for Voluntary Admission –Minors 63
3098* Application for Voluntary Admission (State Treatment Facility) 65
3099* Certification of Ability to Provide Express and Informed Consent for Voluntary Admission and Treatment of Selected Persons
From Facilities Licensed Under Chapter 400, F.S.
67
3100** Transportation to Receiving Facility (2-sided; 2 pages) (Mandatory) 69
3101 * Hospital Determination That Person Does Not Meet Involuntary Placement Criteria 71
3102* Request for Involuntary Examination After Stabilization of Emergency Medical Condition 73
* Recommended **Mandatory
Baker Act Forms - i

Form # Title Page #
3103* Rights of Persons in Mental Health Facilities and Programs (2-sided; 2 pages) 75
3104* Certification of Person’s Competence to Provide Express and Informed Consent 77
3105* Refusal or Revocation of Consent to Treatment 79
3106* Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a Guardian Advocate (2- pages; 2
sided)
81
3107* Order Appointing Guardian Advocate 83
3108* Petition Requesting Court Approval for Guardian Advocate to Consent to Extraordinary Treatment 85
3109* Order Authorizing Guardian Advocate to Consent to Extraordinary Treatment 87
3110* Restriction of Person’s Access to Own Record 89
3111* Approval for Release of Person on Involuntary Status from a Receiving a Facility 91
3113* Notice to Court Request for Continuance of Involuntary Placement Hearing 93
3114* Order Requiring Involuntary Assessment and Stabilization for Substance and for Baker-Act Discharge of Person 95
3115* Order Requiring Evaluation for Involuntary Outpatient Placement 97
3116* Findings and Recommended Order Restoring Person’s Competence to Consent to Treatment and Discharging the Guardian
Advocate
99
3118** Cover Sheet to Agency for Health Care Administration (MANDATORY ) 101
3119* Notification of a Facility’s Non-Compliance 103
3120* Certification of Guardian Advocate Training Completion 105
3121* Notification to Court of Person’s Competence to Consent to Treatment and Discharge of Guardian Advocate 107
3122* Certification of Person’s Incompetence to Consent to Treatment and Notification of Health Care Surrogate/Proxy (2-sided; 2
pages)
109
3123* Affidavit of Health Care Proxy 111
3124* Personal Safety Plan (2-sided; 3 pages) 113
3125** Application for Designation as a Receiving Facility (2-sided; 3 pages) (MANDATORY ) 117
3130* Petition for Involuntary Outpatient Placement (2-sided; 4 pages) 121
3140* Designation of Service Provider for Involuntary Outpatient Placement 125
3145* Proposed Individualized Treatment Plan for Involuntary Outpatient Placement and Continued Involuntary Outpatient
Placement
127
3150* Notice to Department of Children and Families of Non-Filing of Petition for Involuntary Outpatient Placement or Diminished
Treatment Plan Due to Non- Availability of Services or Funding
129
3155* Order for Involuntary Outpatient Placement or Continued Involuntary Outpatient Placement 131
3160* Notice to Court of Modification to Treatment Plan for Involuntary Outpatient Placement and/or Petition Requesting
Approval of Material Modifications to Plan
133
3170* Petition for Termination of Involuntary Outpatient Placement Order 135
3180* Petition Requesting Authorization for Continued Involuntary Outpatient Placement (2-sided; 2 pages) 137
3185* Notice to Court of Waiver of Continued Involuntary Outpatient Placement Hearing and Request for an Order 139
7000* State Mental Health Facility Admission Form (2-sided; 6 pages) 141
7001* State Mental Health Facility Discharge Form (2-sided; 12 pages) 147
7002* Physician to Physician Transfer Form 149
* Recommended **Mandatory
ii - Baker Act Forms
Baker Act Forms
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
_______________________________________________ ____________________________________________________
Page 5
Baker Act Forms
IN THE CIRCUIT COURT OF THE _______________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: __________________________
Ex Parte Order for Involuntary Examination
Pursuant to Section 394.463(2)(a)1, Florida Statutes, this Court having received sworn testimony, states that the above-named person,
presently within the county, appears to meet the following criteria for involuntary examination:
1. There is reason to believe the above-named person has a mental illness as defined in Section 394.455 (18), F.S., and because of
this mental illness said person:
(a) has refused voluntary examination after conscientious explanation and disclosure of the purpose of the examination; or
(b) is unable to determine for himself/herself whether examination is necessary, AND
2. Either (Check a and/or b)
(a) without care or treatment the above-named person is likely to suffer from neglect or refuse to care for himself/herself,
and such neglect or refusal poses a real and present threat of substantial harm to his or her well-being and it is not
apparent that such harm may be avoided through the help of willing family members or friends or the provision of other
services; OR
(b) There is substantial likelihood that without care or treatment the above-named person will cause serious bodily harm to
himself or herself or another person in the near future, as evidenced by recent behavior.
One or more Petitions and Affidavits Seeking Order Requiring Involuntary Examination (CF-MH 3002 or equivalent) on which the
above conclusion is based is attached.
Additional information upon which this order is based is: _____________________________________________________________
Therefore, it is
ORDERED
That a law enforcement officer, or designated agent of the Court take the above-named person into custody and deliver or arrange for
the delivery of said person to the nearest receiving facility for involuntary examination, and that this order and petition be made part
of said person's clinical record. A law enforcement officer or agent may serve and execute this order on any day of the week, at any
time of the day or night. A law enforcement officer or agent may use such reasonable physical force as is necessary to gain entry to
the premises, and any dwellings, buildings, or other structures located on the premises, and to take custody of the person who is the
subject of this ex parte order.
This order expires in ____________ days. If no time limit is specified in this order, the order shall be valid for 7 days after the date
that the order was signed.
ORDERED THIS _____________ day of ______________________________, ____________
Date Month Year
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.463, Florida Statutes
CF-MH 3001, Jan 98 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 1

2 - Baker Act Forms

Baker Act Forms
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
______________________________________________________________________________________________________
Page 7
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _____________________________ CASE NO.: __________________________
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination
I, ___________________________________________ , being duly sworn, am filing this sworn statement requesting a court order for the
Print Name of Petitioner
involuntary examination of ___________________________________________________________ (hereinafter referred to as PERSON).
Print Name of Person
This petition and affidavit will be included in the PERSON’s clinical record and may be viewed by the PERSON.
I understand that by filling out this form, the PERSON may be taken by law enforcement to a mental health facility for an examination.
I SWEAR that the answers to the following questions are given honestly, in good faith, and to the best of my knowledge.
1. a. I live at:
(Print Your Full Residence Address and Phone Number) Phone: (_______) ____________________________
Street Address: ___________________________________________________ City ________________ ST _____ Zip_______
b. I work as a: (Occupation) ___________________________________________ Work Phone: (_______) ___________
Work Street Address: __________________________________________________ City ____________ ST _____ Zip _______
c. The PERSON lives at, or may be found at, the following address(es):
Street Address: ____________________________________________________________________ City __________________
Street Address: ____________________________________________________________________ City __________________
Street Address: ____________________________________________________________________ City __________________
2. I have the following relationship with the PERSON: _________________________________________________________________
___________________________________________________________________________________________________________
3. (Check the one box that applies)
a. I or a family member have or have not previously made allegations to law enforcement involving this
PERSON on _____________
(Date) such as domestic violence, trespassing, battery, child abuse or neglect, Baker Act,
neighborhood disputes, etc. as described: ____________________________________________________________________
b. This PERSON has or has not previously made allegations to law enforcement about me or my
family on ________________
(Date) such as domestic violence, trespassing, battery, child abuse or neglect, Baker Act, etc. as
described:______________________________________________________________________________________________
CONTINUED OVER
Baker Act Forms - 3

_________________________________________________________________________________________________
Page 8
Baker Act Forms
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 2)
4. (Check the one box that applies)
a. I or a family member are not now, and have not in the past, been involved in a court case with the PERSON.
b. I or a family member am now, or was, involved in a court case with the PERSON. This case is/was a
___________________________________________________________ in ________________________________
Type of Case When
Explain:__________________________________________________________________________________________
_________________________________________________________________________________________________
5. I am on good terms with the PERSON at the present time. (Check one box)
Yes No If "no", please explain:
_________________________________________________________________________________________________
6. I have known the PERSON for ___________________________ (how long).
a. The PERSON has only recently displayed unusual kinds of behavior.
b. The PERSON has, over a period of time, always acted in a strange manner.
c. The PERSON's behavior has developed over a period of time.
COMPLETE THE FOLLOWING ONLY IF THE SECTION APPLIES TO THIS CASE:
7. I have seen the following behavior, which causes me to believe that there is a good chance that the PERSON will cause serious
bodily harm to himself/herself or others. On _________________ at approximately ____________ am pm,
Date Time
I saw the PERSON: ___________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
8. Other similar behavior I have personally seen is as follows: _______________________________________________________
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
9.
To my knowledge or belief, I do I do not believe these actions were a result of retardation, developmental
disability, intoxication, or conditions resulting from antisocial behavior or substance abuse impairment.
CHECK AND/OR ANSWER APPLICABLE SECTIONS
10.
a. I have attempted to get the PERSON to agree to seek assistance for a mental or emotional problem(s). I explained
the purpose of the examination (describe when, who was present, and whether you or another person explained the need for
the examination): ____________________________________________________________________________________
___________________________________________________________________________________________________
___________________________________________________________________________________________________
b. I did not try to get the PERSON to agree to a voluntary examination because: ___________________________________
___________________________________________________________________________________________________
c. The PERSON refused a voluntary examination because: ____________________________________________________
___________________________________________________________________________________________________
CONTINUED
4 - Baker Act Forms

Baker Act Forms
Page 9
Baker Act Forms
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 3)
11. The following steps were taken to get the PERSON to go to a hospital for mental health care: __________________
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
These steps did not work because: __________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
12. I believe that the PERSON is unable to determine for himself/herself, why the examination is necessary because:
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
13. I believe that the PERSON has a mental illness which will keep the PERSON from being able to meet the ordinary
demands of living because: ________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
14. I believe that without care or treatment, the PERSON is likely to suffer from neglect or refuse to care for himself/ herself,
because: ______________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
15. I believe that this lack of care or neglect will lead to the PERSON hurting himself or herself because:
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
16. Can family or close friends now provide enough care to avoid harm to the PERSON?
Yes No, If not, why?
_____________________________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
CONTINUED OVER
Baker Act Forms - 5

Page 10
Baker Act Forms
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 4)
Provide the following identifying information about the person (if known) if it is determined necessary to take the
person into custody for examination:
County of Residence: Social Security No.: Date of Birth:
Sex : Male Female Race: Attach a picture of the PERSON if possible. Picture attached: No Yes
Height: Weight: Hair Color: Eye Color:
Does the PERSON have access to any weapons? No Yes If yes, describe:
Is the PERSON violent now? No Yes Has the person been violent in the recent past? No Yes If Yes, Describe:
Does the PERSON have any pending criminal charges against him/her? No Yes If yes, describe:
GUARDIANSHIP:
1) Does the PERSON have a legal guardian? No Yes
2) Is there a pending petition to determine the PERSON’s capacity and for the appointment of a guardian? No Ye s
If YES to either of the above, provide the name, address and phone number of the current or proposed guardian.
Name: Phone: (___________) _____________________________
Address: City: Zip: ____________
_________________________________________________________________________________________________________________________
PHYSICIAN: Name: Phone: ( )
MEDICATIONS: Provide name of medications if known.
CASE MANAGEMENT: Provide name and phone number of case manager or case management agency, if known.
I understand that this sworn statement is given under oath and will be treated as though it was made before a judge in a
court of law. I understand that any information in this sworn statement which is not to the best of my knowledge and
done in good faith may expose me to a penalty for perjury and other possible penalties under the statutes of the State of
Florida.
Under penalties of perjury, I declare that I have read the foregoing document and that the facts stated in it are true.
Signature of Affiant/Petitioner: ________________________________________________
SWORN TO AND SUBSCRIBED before me OR SWORN TO AND SUBSCRIBED before me
this __________ day of ________________________, ______________ this __________ day of ________________________, ______________
Day Month Year Day Month Year
by _____________________________________ who is personally known Clerk of Circuit Court
to me or presented ________________________________ as identification. _____________________________ County, Florida
___________________________________________________________ By: _______________________________________________________
Notary Public - State of Florida Deputy Clerk
My Commission expires: Date_____________________
A copy of the petition(s) must be attached to an Ex Parte Order for Involuntary Examination and accompany the
person to the nearest receiving facility.
See s. 394.463, Florida Statutes
CF-MH 3002, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
6 - Baker Act Forms

Baker Act Forms
___________________________________________ ___________________________________________________________
Page 11
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Order for Involuntary Inpatient Placement
This matter came to be heard pursuant to a Petition for Involuntary Inpatient Placement filed herein on the issue of whether the above-
named person should be involuntarily placed in a mental health treatment or receiving facility, and the Court being fully advised in the
premises, finds by clear and convincing evidence, as follows:
1. Said person has been represented by counsel; Said person
appeared at the hearing, or
said person’s presence at the hearing was waived, without objection of said person’s counsel.
2. Said person meets the following criteria for involuntary inpatient placement pursuant to s. 394.467(1), F.S. :
(a) He or she is mentally ill and because of a mental illness:
(1) has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the purpose of
placement for treatment; or
(2) is unable to determine for himself or herself whether placement is necessary; AND
(b) Either
(1) He or she is manifestly incapable of surviving alone or with the help of willing and responsible family or friends, including
available alternative services, and, without treatment, is likely to suffer from neglect or refuse to care for himself or herself, and
such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; or
(2) There is substantial likelihood that in the near future he or she will inflict serious bodily harm on himself or herself or another
person, as evidenced by recent behavior causing, attempting, or threatening such harm; and
(c) All available less restrictive treatment alternatives which would offer an opportunity for improvement of his or her condition have
been judged to be inappropriate.
3. The nature and extent of the above-named person’s mental illness is as follows: _____________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
4. The Court considered testimony and evidence regarding the person’s competence to consent to treatment. The person was found to be
competent incompetent to consent to treatment. If found to be incompetent, ____________________________________
__________________________________________________________________________ was appointed as guardian advocate.
(name and address)
5. If the petition was referred to and heard by a general master, the Master’s Report and Recommendation are attached, incorporated by
reference, and/or adopted by the Court.
ORDERED
That the above-named person be placed in a designated mental health receiving or treatment facility on an involuntary basis for a period of up
to ____________________________, not to exceed 6 months from the date of this order, or until discharged by the administrator or
transferred to voluntary status.
DONE AND ORDERED in ___________________ County, Florida, this ______ day of ___________________, ____________.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
This form must accompany person to the treatment facility.
See s. 394.467(1), Florida Statutes
CF-MH 3008, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 7

8 - Baker Act Forms

Baker Act Forms
___________________________________________ _________________________________________________
______________________ ________________________ ______________________
Page 13
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: ________________________________
Notice of Petition for Involuntary Placement
YOU ARE HEREBY NOTIFIED that a petition for a hearing has been filed with the Circuit Court in ___________________ County,
Florida where the above-named person is hospitalized on the question of whether he/she should be ordered or confined for:
Involuntary Inpatient Placement
Involuntary Outpatient Placement
Continued Involuntary Outpatient Placement
Said person will be represented by the Public Defender if he/she is not otherwise represented by counsel.
A hearing has been scheduled by the court and will be conducted pursuant to Section 394.467, F.S., on ____________ at
______ am pm
Date Time
at ________________________________________________________________________________________________________ .
Place/address
At least one of the following examining experts will testify in support of continued detention:
In addition to at least one of the professionals listed above, the following persons are also expected to testify in support of involuntary
inpatient placement or involuntary outpatient placement or continued involuntary outpatient placement:
Guardian or Representative Other Witness Other Witness
Name: ______________________ ________________________ ______________________
Relationship ______________________ ________________________ ______________________
Address ______________________ ________________________ ______________________
Telephone: (______)_______________ (______)_________________ (______)_______________
The person, the person’s guardian, or representative, or the administrator may apply for a change of venue for the convenience of the parties
or witnesses or because of the condition of the person.
The person has a right to an independent expert examination and if he/she cannot afford such an examination the Court shall provide for one.
______________________________________________________ _________________ _________ am pm
Signature of Court Date Time
______________________________________________________
Printed Name of Court
Certificate of Mailing
I hereby certify that I mailed the above and foregoing notice to the named parties by depositing the same in the United States Post Office on
the ______________ day of _________________, ___________. In addition, I sent this notice by registered or certified mail to each person
listed below who was not given a copy by hand delivery.
________________________________________________ ________________________ ___________ am pm
Signature of Court Date Time
This form may be completed and mailed by the Receiving Facility instead of the Court, with the court’s concurrence.
cc:
Person Guardian Representative Public Defender or Private Attorney
See s. 394.4599(2)(a), (c ), Florida Statutes
CF-MH 3021, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 9

10 - Baker Act Forms

Baker Act Forms
____________________________________________________________ ________________________
____________________________________________________________
See s. 394.467(6)(a)2, Florida Statutes
CF-MH 3022, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Page 15
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Application for Appointment of Independent Expert Examiner
I, ______________________________________________________________________________ hereby petition the Court to
order an independent expert examination pursuant to:
Involuntary Inpatient Placement (s.394.467(6)(a)2, FS)
Involuntary Outpatient Placement (s.394.4655(6)(a)2, FS)
Continued Involuntary Outpatient Placement (s.394.4599(2)(c)5, FS)
____________________________________________________________ ________________________
Signature of Person or Representative Date
____________________________________________________________
Typed or Printed Name of Person or Representative
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who Provided Copy
Person
am pm
Guardian
am pm
Representative
am pm
BAKER ACT
Page 15
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Application for Appointment of Independent Expert Examiner
I, ______________________________________________________________________________ hereby petition the Court to
order an independent expert examination pursuant to:
Involuntary Inpatient Placement (s.394.467(6)(a)2, FS)
Involuntary Outpatient Placement (s.394.4655(6)(a)2, FS)
Continued Involuntary Outpatient Placement (s.394.4599(2)(c)5, FS)
Signature of Person or Representative Date
Typed or Printed Name of Person or Representative
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who Provided Copy
Person
am pm
Guardian
am pm
Representative
am pm
See s. 394.467(6)(a)2, Florida Statutes
CF-MH 3022, Feb 05 (obsoletes previous editions) (Recommended Form)
Baker Act Forms - 11

12 - Baker Act Forms

Baker Act Forms
_____________________________________________ ________________________________________________
____________________________________________________
Page 17
Baker Act Forms
IN RE: _________________________________________ CASE NO.: __________________________
Notice of Petition for Continued Involuntary Inpatient Placement
YOU ARE HEREBY NOTIFIED that a petition for a hearing has been filed with the State Division of Administrative Hearings on the
question of whether ___________________________________________________________________ who is hospitalized at
_________________________________________________________________ should be ordered for continued involuntary inpatient
placement.
The person will be represented by the Public Defender if the person is not otherwise represented by counsel.
A hearing will be conducted pursuant to Section 394.467 (7), F.S., at ___________ am pm on _____________
(date)
at_____________________________________________________________________________________________________________
The following physician(s) or clinical psychologist(s) are expected to testify in support of continued detention:
In addition, the following persons are also expected to testify in support of continued involuntary inpatient placement:
Name: _______________________________ _______________________________ _______________________________
Relationship _______________________________ _______________________________ _______________________________
Address _______________________________ _______________________________ _______________________________
_______________________________ _______________________________ _______________________________
Telephone: (______)________________________ (______)________________________ (______)________________________
The person, the person’s guardian, or representative, or the administrator may apply for a change of venue for the convenience of the parties
or witnesses or because of the condition of the person.
The person has a right to an independent expert examination and if he/she cannot afford such an examination, one shall be provided for him
or her.
__________________________________________________ __________________ ______________ am pm
Signature of Administrative Law Judge Date Time
__________________________________________
Typed or Printed Name of Administrative Law Judge
Certificate of Mailing
I hereby certify that I mailed the above and foregoing notice to the named parties by depositing the same in the United States Post Office on
the __________ day of ________________, __________ . In addition, I sent this notice by registered or certified mail to each person
listed below who was not given a copy by hand delivery.
Signature of Administrative Law Judge
cc: Check when applicable Person Guardian Guardian Advocate Representative Public Defender or Private Attorney
See s. 394.4599(2)(a), (c ), 394.467(7), Florida Statutes
CF-MH 3024, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 13

14 - Baker Act Forms

Baker Act Forms
___________________________________________________________________________________________________
___________________________________________________________________________________________________
________________________________________ ________________________________________________
Page 19
Baker Act Forms
IN RE: _______________________________________________ CASE NO.: __________________________
Order for Continued Involuntary Inpatient Placement or for Release
This matter coming on to be heard, pursuant to the requirements of Section 394.467(7), Florida Statutes, that the mental status
and necessity to continue involuntary inpatient placement of persons be periodically reviewed, and the person having
appeared in person appeared through counsel, the following findings of fact are made from the evidence designated:
1. The person, on ___________________________________ , was involuntarily placed on a Court order.
Date
2. The person
does does not continue to meet the criteria for involuntary inpatient placement. This finding is
determined from the testimony of ______________________________________________________
and ________________________________________________________________________________. As evidenced by:
___________________________________________________________________________________________________
Based on the above findings of fact, the Administrative Law Judge makes the following conclusions:
On the basis of the above, it is hereby
ORDERED
The person be returned to involuntary inpatient placement pending the next periodic review required by Section
394.467, Florida Statutes.
The person be processed for release from involuntary inpatient placement and be completely discharged from the
facility.
The person is eligible for and has applied for voluntary status.
ORDERED at
this _____________ day of ________________________ , _________________.
Date Month Year
Printed Name of Administrative Law Judge Signature of Administrative Law Judge
cc: Check when applicable
Person Guardian Guardian Advocate Representative Public Defender Facility Administrator
See s. 394.467(7), Florida Statutes
CF-MH 3031, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 15

16 - Baker Act Forms

Baker Act Forms
___________________________ _____________________________ ___________________________
Page 21
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Petition for Involuntary Inpatient Placement
COMES NOW the Petitioner, __________________________________________________________________ , and alleges:
1. That Petitioner is Administrator of ___________________________ __________________________________________
Name of Facility Facility Address
2. That (
Name of Person ) ________________________________________________________________________ , is a
patient of said facility and has been examined at such facility.
3. The person’s social security number is___________________________ and date of birth is:______________________.
Date
4. That this petition is being filed within the following time frames: (Check one below)
A. This person was admitted for involuntary examination and this petition is being filed within the 72-hour examination
period, or if the examination period ends on a weekend or legal holiday, on the next court working day
OR
B. This person was transferred to involuntary status after examination or after refusing/revoking consent to treatment or
requesting discharge from the facility and this petition is filed within two court working days.
5. That attached hereto and by reference made a part hereof, are two (2) opinions regarding the mental health of said person
necessitating involuntary inpatient placement.
6. That based thereon Petitioner recommends that the person/respondent be involuntarily placed in
________________________________________________ , a (public/private) designated receiving or treatment facility.
7. In addition to at least one of the two experts whose opinions are attached, the following persons may testify:
Guardian or Representative Other Witness Other Witness
Name: ___________________________ _____________________________ ___________________________
Relationship ___________________________ _____________________________ ___________________________
Address ___________________________ _____________________________ ___________________________
Telephone: (______)___________________ (______)______________________ (______)____________________
CONTINUED OVER
Baker Act Forms - 17

______________________________________________
Page 22
Baker Act Forms
Petition for Involuntary Placement (Page 2)
COMES NOW THE PETITIONER and further alleges that:
1. A Guardian Advocate is necessary to act on the person’s behalf on issues related to express and informed consent to
mental health or medical treatment and a Petition for Adjudication of Incompetence to Consent to Treatment and
Appointment of a Guardian Advocate is attached; OR
2. The person/respondent is competent to provide express and informed consent to his or her own treatment or the person
has a guardian authorized to consent to treatment and no Guardian Advocate is requested.
________________________________________ _______________________ ____________ am pm
Signature of Facility Administrator or Designee Date Time
Typed or Printed Name of Administrator or Designee
The person
does or does not have a private attorney. If so, the name and address of the private attorney
is:
Private Attorney Name: ______________________________________________________________________________
Private Attorney Address: ____________________________________________________________________________
cc: The Clerk of the Court shall provide a copy of this petition to the: (Check when applicable and initial/date/time when
copy provided)
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Public Defender am pm
Representative am pm
State Attorney
am pm
Dept. of Children & Families
am pm
CONTINUED / SUPPORTING OPINIONS ON PAGE 3
18 - Baker Act Forms

Baker Act Forms
____________________________________________________________________________________________________________
_________________________________________________ __________________________________
________________________________________ ________________________ ______________
______________________________________________________________ _________________________________
Page 23
Baker Act Forms
Petition for Involuntary Placement (Page 3)
First Opinion Supporting the Petition
I, ____________________________________ a psychiatrist authorized to practice in the State of Florida, have personally examined
_______________________________________ on _________________ (within 72 hours of the signing hereof) and find from such
Name of Person Date
examination that the person meets the following criteria for involuntary placement:
1. Said person is mentally ill and because of a mental illness (check one):
a. Said person has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the
purpose of placement for treatment; OR
b. Said person is unable to determine for himself/herself whether placement is necessary:
AND
2. Either (Check one or both):
a. Said person is manifestly incapable of surviving alone or with the help of willing and responsible family or friends, including
available alliterative services, and without treatment, he/she is likely to suffer from neglect or refuse to care for himself/herself
and such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; OR
b. There is substantial likelihood that in the near future said person will inflict serious bodily harm on himself/herself or another
person as evidenced by recent behavior causing, attempting, or threatening such harm.
AND
All available less restrictive treatment alternatives which would offer an opportunity for improvement of said person's condition have been
judged to be inappropriate based on contact with the following programs/agencies: _________________________________________
Observations which support this opinion are:
_________________________________________________ ________________ ____________ am pm
Signature of Psychiatrist Date Time
Typed or Printed Name of Psychiatrist License Number
Second Opinion Supporting the Petition
I,____________________________________________, a psychiatrist, clinical psychologist, licensed physician *,
psychiatric nurse *, authorized to provide a second opinion on this petition pursuant to Section 394.467 (2), F.S., have personally examined
________________________________________________________ on ________________, (within 72 hours of signing hereof), and
Name of Person Date
find that he/she meets the criteria for involuntary inpatient placement as stated in this petition. Observations which support this opinion are:
_________________________________________ ___________________ ___________ am pm
Signature of Examiner Date Time
Typed or Printed Name of Examiner
Profession License
Number
I certify that the county in which the person is detained has less than 50,000 population and no psychiatrist or psychologist is available
to provide the second opinion.
Printed Name and Signature of Administrator or Designee Date
* A licensed physician or psychiatric nurse may only provide such second opinion in counties of less than 50,000
population in cases where the facility administrator certifies that no psychiatrist or clinical psychologist is available to
provide the second opinion (by countersigning above).
See s. 394.4599(2)(c)3, 394.467, Florida Statutes
CF-MH 3032, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 19

20 - Baker Act Forms

Baker Act Forms
__________________________________________
Page 25
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: __________________________________________ CASE NO.: __________________________
Notification to Court of Withdrawal of Petition
For Hearing on Involuntary Inpatient or involuntary Outpatient Placement
YOU ARE HEREBY INFORMED THAT ___________________________________________________________________
Name of Person
at ___________________________________________________________________________________________________
Facility Name and Address
has made application by express and informed consent for voluntary admission, due to an improvement in his/her condition.
was discharged on ____________________ to ______________________________________________
Date Destination (if known)
was transferred on ____________________ to ______________________________________________
Date Destination (if known)
was converted to Marchman Act on ______________________________________
Date
Other (specify):_______________________________________________________________________________
___________________________________________________________________________________________
Please withdraw my Petition for:
Involuntary Inpatient Placement
Involuntary Outpatient Placement
Continued Involuntary Outpatient Placement
filed on ________________(date). The Petition for Adjudication of Incompetence to Consent to Treatment and Appointment
of a Guardian Advocate, if any, is also being withdrawn.
_________________________________________________ _______________ _________ am pm
Signature of Administrator or Designee Date Time
Printed Name of Administrator or Designee
cc:
Clerk of the Court (Probate Division) Person Guardian
Assistant State Attorney Representative
Person’s Attorney
When a petition for involuntary placement is withdrawn, the court, state attorney, public defender or other attorney for the
person, and guardian or representative must be notified by telephone within one business day of the decision, unless
such decision is made within 24 hours prior to the hearing. In such cases, the notification must be made immediately.
See s. 394.467, 394.4685, 394.469, Florida Statutes
CF-MH 3033, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 21

22 - Baker Act Forms
Baker Act Forms
____________________________________________________
Page 27
Baker Act Forms
IN RE: ________________________________________ CASE NO.: __________________________
Petition Requesting Authorization for Continued Involuntary Inpatient Placement
The petition of __________________________________________________________ who is the Administrator of
_______________________________________________________________________________ Facility shows that:
1. The above named person, __________________________________ of _______________________ County,
Florida, is currently in the aforesaid facility and was admitted to this facility on ____________________________ .
Date
2. That according to the provisions of Section 394.467 (7), F.S., this person may not be retained after
______________________________,
(Date) without an order authorizing continued involuntary inpatient placement.
3. That the person continues to meet the criteria for involuntary inpatient placement pursuant to Section 394.467(1), F.S., and
that legally authorized period has nearly expired, or
the person was admitted while serving a criminal sentence whose sentence will expire on ________________ , or
Date
the person was placed while a minor and will reach the age of majority on _________________.
Date
Wherefore, it is requested an Order be issued authorizing this Facility to retain the person for a period not to exceed six (6)
months.
_________________________________________________ ___________________ _____________ am pm
Signature of Administrator or Designee Date Time
Printed or Typed Name of Administrator or Designee
CONTINUED OVER
Baker Act Forms - 23

________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________ _______________________________
Page 28
Baker Act Forms
Petition Requesting Authorization for Continued Involuntary Placement (Page 2)
Physician's or Clinical Psychologist's Statement
I hereby state that the above named person continues to meet the criteria for involuntary placement. Behavior which
supports this opinion is: ____________________________________________________________________________
Person’s treatment during placement was: ______________________________________________________________
Less restrictive settings which were investigated and the reasons they were ruled out are as follows: ________________
Support for facts in this statement is attached.
The individualized treatment plan for the person is attached.
____________________________________________________ _______________ _________ am pm
Signature of
Physician Clinical Psychologist Date Time
Printed Name of Physician/Clinical Psychologist License Number
File this completed form with the Administrative Law Judge.
Person does or does not have a private attorney. If so, the name and address of the private attorney is:
Private Attorney Name: ______________________________________________________________________________
Private Attorney Address: ____________________________________________________________________________
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who Provided Copy
Person am pm
Guardian am pm
Guardian Advocate am pm
Representative am pm
Public Defender or
Private Attorney
am pm
See s. 394.467(7), Florida Statutes
CF-MH 3035, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
24 - Baker Act Forms

Baker Act Forms
Page 29
Baker Act Forms
Notice of Right to Petition for
Writ of Habeas Corpus or for Redress of Grievances
To: ___________________________________________________
PLEASE BE ADVISED that you may petition the Circuit Court for a Writ of Habeas Corpus to question the cause and
legality of your detention. Furthermore, a petition may be filed in the Circuit Court in the county in which you are placed
for Redress of Grievances alleging that you are being unjustly denied a right or privilege or that an authorized procedure
is being abused.
A Petition for Writ of Habeas Corpus and Redress of Grievances (CF MH Form 3090) may be used for this purpose. A
petition must be signed by either you, your relative, friend, guardian, guardian advocate, representative, attorney, or the
Department of Children and Families.
Staff of this facility will provide a copy of the Writ form to you immediately upon your request. Staff will assist you in
completing this Writ form if you request such help. The Petition for a Writ will be submitted by the staff to the Circuit
Court no later than the next working day after you submit the form.
___________________________________________ __________________ __________ am pm
Signature of Administrator or Designee Date Time
This completed form must be given to all persons admitted to a facility and to those individuals listed
below as applicable.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative am pm
Health Care Surrogate/Proxy
am pm
See s. 394.459(8), Florida Statutes
CF-MH 3036, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 25

26 - Baker Act Forms

Baker Act Forms
__________________________________________________ ________________________________________________
Page 31
Baker Act Forms
Notice of Release or Discharge
IN RE: ________________________________________ CASE NO. _____________________________
YOU ARE HEREBY NOTIFIED that ______________________________________________________ , admitted for
Involuntary examination
Involuntary inpatient placement
Involuntary outpatient placement
has this ________ day of __________________ , 20__ been released or discharged from this facility and or order.
Any guardian advocate appointed to provide express and informed consent to treatment on the person’s behalf, if any, has
been discharged from his or her duties, unless the person was released from involuntary inpatient placement to involuntary
outpatient placement and the appointment of the guardian advocate was continued by the court.
__________________________________________________ _______________________ ___________ am pm
Signature of Administrator or Designee Date Time
Printed Name of Administrator or Designee Name of Facility
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian am pm
Guardian Advocate am pm
Representative am pm
Person’s Attorney am pm
Initiating Person am pm
Circuit Court am pm
Person’s Clinical Record am pm
See s. 394.4599, 394.463(3), Florida Statutes
CF-MH 3038, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 27

28 - Baker Act Forms

Baker Act Forms
______________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
I
Page 33
Baker Act Forms
Application for Voluntary Admission of an Adult
(Receiving Facility)
I, ________________________________________________________________________ do hereby apply for admission to
Full printed name of person whose admission is being requested
Fill in name of facility
for observation, diagnosis, care, and treatment of a mental illness, and I certify that the information given on this application is
true and correct to the best of my knowledge and belief.
I am making this application for voluntary admission after sufficient explanation and disclosure to make a knowing and willful
decision without any element of force, fraud, deceit, duress, or other form of constraint or coercion. The reason for my
admission to this facility is:
_____________________________________________________________________________________________________.
I am a competent adult with the capacity to make well-reasoned, willful, and knowing decisions concerning my medical or
mental health treatment. I do not have a guardian, guardian advocate, or currently have a health care surrogate/proxy making
health care decisions for me.
have have not provided a copy of advance directive(s).
If so, the advance directives include my:
Living Will
Health Care Surrogate,
Mental Health Care Surrogate,
Other as specified:
I have been provided with a written explanation of my rights as a person on voluntary status and they have been fully explained
to me. I understand that this facility is authorized by law to detain me without my consent for up to 24 hours after I
make a request for discharge; unless a petition for involuntary inpatient placement or involuntary outpatient placement is filed
with the Court within two (2) court working days of my request for discharge in which case I may be held pending a hearing on
the petition.
I understand that I may be billed for the cost of my treatment.
_____________________________________________ ________________ __________ am pm
Signature of Competent Adult Date Time
_______________________________ ___________________________ _______________ __________ am pm
Printed Name of Witness Signature of Witness Date Time
No notice of this admission is to be made without the consent of the person except in case of an
emergency. The use of this form for a voluntary admission requires that a “Certification of Person’s
Competence to Provide Express and Informed Consent” be completed within 24 hours and if the form is
used for a transfer of a person from involuntary to voluntary status, the “Certification” must be completed
prior to the “Application”. The “Application” and “Certification” must be placed in the person’s clinical
record.
See s. 394.455(9), 394.459, 394.4625, Florida Statutes
CF-MH 3040, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 29

30 - Baker Act Forms

Baker Act Forms
_____________________________________________________________________________________________________________
Page 35
Baker Act Forms
General Authorization for Treatment Except Psychotropic Medications
I, the undersigned, a competent adult, guardian, guardian advocate, or health care surrogate/proxy
hereby authorize the professional staff of this facility to administer assessment and treatment specified below.
Routine medical care ___________ (Initials of Person or Authorized Decision Maker)
Psychiatric Assessment __________ (Initials of Person or Authorized Decision Maker)
Other (Specify & Initial) _______________________________________________ ___________
_______________________________________________ ___________
_______________________________________________ ___________
I understand that more information will be provided to me before my informed consent will be requested for the administration
of any psychotropic medications.
I understand that my consent can be revoked orally or in writing prior to, or during the treatment period.
I have read and had this information fully explained to me and I have had the opportunity to ask questions and
receive answers about the treatment.
___________________________________________________ ____________________ _____________ am pm
Signature of Competent Adult Date Time
___________________________________________________ ____________________ _____________ am pm
Signature of Witness for Person Date Time
___________________________________________________ ____________________ _____________ am pm
Signature of: (check one when applicable) Date Time
Guardian Guardian Advocate
Health Care Surrogate Health Care Proxy
If I am the guardian advocate, health care surrogate, or health care proxy for the person, I certify that I have met and talked with the person
and the person’s physician in person, if at all possible, and by telephone, if not about the proposed treatment prior to signing this form.
Talked to person on:_________(date)
In person By telephone. If not in person, explain why not._________________________
Talked to person’s physician on: _____(date)
In person By telephone. If not in person, explain why not.____________________
________________________
_____________ am pm
Signature of: (check one when applicable) Date Time
Guardian
Guardian Advocate
Health Care Surrogate
Health Care Proxy
________________________________________________ ____________________
_____________ am pm
Signature of Witness for Substitute Decision-Maker Date Time
The person shall always be asked to sign this authorization form. However, if the person is a minor, is incapacitated, or is
incompetent to consent to treatment, the consent of his or her guardian, guardian advocate, or health care surrogate/proxy is
required. Court orders, letters of guardianship, or advance directives must be retained in the clinical record if an individual
other than the person signs the consent to treatment. The guardian, guardian advocate, or health care surrogate/proxy must
agree to keep the facility informed of their whereabouts during the term of the hospitalization.
See s. 394.459(3), Florida Statutes
CF-MH 3042a, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 31

32 - Baker Act Forms

Baker Act Forms
_________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
Page 37
Baker Act Forms
Specific Authorization for Psychotropic Medications
Discussion of psychotropic medication should occur within the context of the person’s
medical history and current overall medication regimen.
I, the undersigned, a competent adult, guardian, guardian advocate, or health care surrogate/proxy hereby
authorize the professional staff of this facility to administer treatment, limited to mental health medications, as follows:
I have been given detailed information about:
1. The proposed medications and dosage range and frequency;
2. The purpose of my treatment;
3. Common short- and long-term side effects of my proposed medication, including contraindications and clinically
significant interactions with other medications;
4. Alternative medications;
5. Approximate length of care
I further understand that a change of medication dosage range from that listed above or on the attached will require my
express and informed consent.
I understand that my consent can be revoked orally or in writing prior to, or during the treatment period.
The information I have relied upon to make the decision to consent to treatment, including full disclosure of each of the
above subjects, is attached to this authorization and signed by me. I have read and had this information fully explained to
me and I have had the opportunity to ask questions and receive answers about the treatment.
___________________________________________________ ______________________
_____________ am pm
Signature of Person Date Time
________________________________________________ _______________
_____________ am pm
Signature of Witness for Person Date Time
________________________________________________ _______________
_____________ am pm
Signature of: (check one when applicable) Date Time
Guardian Guardian Advocate
Health Care Surrogate Health Care Proxy
If I am the guardian advocate, health care surrogate, or health care proxy for the person, I certify that I have met and talked with the person
and the person’s physician in person, if at all possible, and by telephone, if not about the proposed treatment prior to signing this form.
Talked to person on:_________(date)
In person By telephone. If not in person, explain why not._________________________
Talked to person’s physician on: _____(date)
In person By telephone. If not in person, explain why not.___________________
_______________________________________________ _______________
_____________ am pm
Signature of: (check one when applicable) Date Time
Guardian Guardian Advocate
Health Care Surrogate Health Care Proxy
_______________________________________________ _______________
_____________ am pm
Signature of Witness for Substitute Decision-Maker Date Time
* The person shall always be asked to sign this authorization form. However, if the person is a minor, is incapacitated, or is incompetent
to consent to treatment, the consent of his or her guardian, guardian advocate, or health care surrogate/proxy is required. Court orders,
letters of guardianship, or advance directives must be retained in the clinical record if a person other than the person signs the consent
to treatment. The guardian, guardian advocate, or health care surrogate/proxy must agree to keep the facility informed of their
whereabouts during the term of the hospitalization. Facilities may devise unique disclosure forms or use commercially prepared forms,
but in either case, the material must include all statutorily required elements.
See s. 394.459(3), Florida Statutes
CF-MH 3042b, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 33

34 - Baker Act Forms

Baker Act Forms
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
_______________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
________________________________ _________________________________ ______________________________
_____________________________________________________________________________________________________
Page 39
Baker Act Forms
Inventory of Personal Effects
The following person ______________________________________________________________________ has retained these
articles in his or her own custody:
The person has, for medical and safety reasons, placed the following articles in the temporary custody of this facility. (Attach
additional sheets if necessary)
This is a correct listing of my personal effects and belongings which I hereby place in custody of the facility.
______________________________________________________ _______________________ __________ am pm
Signature of Person Date Time
______________________________________________________ _______________________ __________ am pm
Signature/Title of Witness to Inventory Date Time
______________________________________________________ _______________________ __________ am pm
Signature/Title of Witness to Inventory Date Time
If the person is unable or unwilling to sign the above, the reason(s) are as follows: __________________________________
_____________________________________________________________________________________________________.
Amendment to the above inventory shall be made on a separate Inventory form, signed by the person, and witnessed by two
persons.
This inventory must be amended upon the request of the person, guardian, guardian advocate or representative. All effects
held by the facility shall be returned to the person immediately upon the person’s discharge or transfer from the facility,
unless such return would be detrimental to the person. If not returned to the person, the reason must be documented in the
clinical record along with the disposition of the personal effects. The inventory form must be filed in the person’s clinical
record.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initial of Who
Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
See s. 394.459(6), Florida Statutes
CF-MH 3043, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 35

36 - Baker Act Forms

Baker Act Forms
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
____________________________________________________
___________________________________________________
Page 41
Baker Act Forms
Authorization for Release of Information
I hereby request and authorize:
Name of Person(s) or Agency Holding the Information
Address
to release written or verbal information specified below:
To:________________________________________________________________________________________________
Name of Person(s) or Agency Requesting the Information
Address
For the purpose of: ______________________________________________________________________________________
I understand that this form may be used to release information related to mental health treatment, including assessments and lab
reports. Any release of substance abuse information must be pursuant to 42 CFR. There are other special restrictions which
apply to the release of information regarding HIV, abuse reports, etc.
I understand that I have the right to refuse to sign this Authorization or to rescind my consent at any time prior to the release of
the information.
Expiration Date: ___________________ Social Security Number of Person: ________________________________________
__________________________________ _________________________________ _______________ ________ am pm
Signature of Competent Adult Printed Name of Competent Adult Date Time
__________________________________ __________________________________ _______________ ________ am pm
When applicable, Signature of: Printed Name of Substitute Decision Maker Date Time
Guardian, Guardian Advocate, Health Care Surrogate/Proxy,
or
Personal Representative/Equivalent (if deceased)
__________________________________ _________________________________ _______________ ________ am pm
Signature of Witness Printed Name of Witness Date Time
PROHIBITION ON REDISCLOSURE: This information has been disclosed to you from records whose confidentiality is
protected. Any further redisclosure is strictly prohibited unless the person provides specific written consent for the subsequent
disclosure of this information. Florida Law requires that any person, agency, or entity receiving information shall maintain
such information as confidential and exempt from the provisions of the public records law.
Any release of information must be in compliance with the federal HIPAA law and state laws governing such releases.
See s. 394.4615(1), Florida Statutes
CF-MH 3044, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 37

38 - Baker Act Forms

Baker Act Forms
________________________________________________________________________________________________
_______________________________________
Page 43
Baker Act Forms
Notice of Person’s Admission for Involuntary Examination
Name of Guardian or Representative: ______________________________________________________________________
YOU ARE HEREBY NOTIFIED THAT _______________________________________________________________
Printed Name of Person Admitted for Examination
Was admitted to: ________________________________________________________ (Name of Facility)
Facility Address City State Zip Code
(_____)___________________on ____________________for an involuntary examination.
Facility Telephone Number Date
You are notified of this admission because you have been designated as the person’s
representative and the person did not
object to you being notified or as his or her
guardian. Prompt notice by telephone or in person was given to you within
24 hours of the person’s arrival at the facility.
You will be informed of his/her legal proceedings, rights and any restriction of these rights, and of the person’s discharge or
transfer to another facility. You have the legal right to petition the Court on the person’s behalf, question the cause and legality
of his/her detention in a facility or if you believe the person is being unjustly denied a right or privilege.
______________________________________ ___________________ _______________ am pm
Signature of Administrator or Designee Date Time
Printed or Typed Name of Administrator or Designee
Notice to the local Florida Local Advocacy Council must be given for all persons on involuntary status; such notice may not be
waived. A person may choose his or her representative. Only if the person is unable to unwilling to designate a representative, the
facility shall select a representative. When the facility selects the representative, the selection shall be made from the following list
in the order of listing:
1. Health Care Surrogate 5. Person’s Adult Next of Kin
2. Person’s Spouse 6. Person’s Adult Friend
3. Person’s Adult Child 7. Florida Local Advocacy Council
4. Person’s Parent
The person shall be consulted with regard to the selection of a representative by the receiving or treatment facility and shall have
authority to request that any such representative be replaced. The following shall not be appointed as the person’s representative:
a licensed professional providing services to the person, an employee of a facility providing direct services to the person, an
employee of the Department of Children and Families, an individual providing other substantial services to a person in a
professional or business capacity, or a creditor of the person.
Distribution: Check when applicable and initial/date/time when copy is provided.
Individual Date Copy
Provided
Method Copy
Provided
Time Copy
Provided
Initials of Person
Providing Copy
Guardian am pm
Representative am pm
Florida Local Advocacy Council am pm
Person’s clinical record
am pm
See s. 394.4597, 394.4599, Florida Statutes
BAKER ACT
CF-MH 3045, Feb 05 (obsoletes previous editions) (Recommended Form)
Baker Act Forms - 39

Page 44
Baker Act Forms
40 - Baker Act Forms

Baker Act Forms
Page 45
Baker Act Forms
IN RE: _________________________________________________________
Application for and Notice of Transfer to Another Receiving or Treatment Facility
Part I - Application for Transfer
I, ___________________________________________________________________________, hereby apply for transfer from
_____________________________________ to _________________________________________
on or before ____________________, ____________
I understand that in transfers:
From a public receiving facility to a private receiving facility, I am responsible for the cost of transportation and
personnel required to assist with the transfer.
From a private receiving facility to a public receiving facility, the cost of transfer is the responsibility of the private
facility if the transfer is requested by the private facility.
_______________________________________________________ ________________ ___________ am pm
Signature of Person, Guardian, Guardian Advocate Date Time
Health Care Surrogate Health Care Proxy
Part II - Notice of Transfer to Another Facility
YOU ARE HEREBY NOTIFIED that ____________________________________________ will be transferred from
_______________________________________, to _________________________________________ located at
_________________________________________________________________ on ___________________.
Date
___________________________________________________ ________________ _____________ am pm
Signature of Administrator or Designee Date Time
Part I is to be completed by the person or other authorized person to request a transfer. Part II is completed by the
sending facility administrator prior to the date of transfer. Only Part II is completed when the transfer is initiated by
the facility administrator rather than by the person or other person authorized to act on the person’s behalf.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian am pm
Guardian Advocate am pm
Representative am pm
Attorney am pm
See s. 394.4685, Florida Statutes
CF-MH 3046, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 41

42 - Baker Act Forms

Baker Act Forms
_______________________________________________________________________
________________________________________________________________________
__________________________________ ___________________________________________
___________________________________ ___________________________________________
Page 47
Baker Act Forms
Confidentiality Agreement
While receiving services at _________________________________________ Facility, you have the right
to decide who may and who may not receive information about your presence and treatment in this facility.
This form is for you to document your choices. Please initial indicating your choice in the following areas:
Visitors:
_____ I choose to have visitors
_____ I choose to limit the specific visitors to the following:
_____ I choose to have no visitors
Telephone Use:
_____ I choose to receive all phone calls
_____ I choose to limit my calls to specific callers, including:
_____ I choose to receive no phone calls
Medical Records:
_____ I choose not to limit access to my medical records
_____ I choose to limit access to my medical records to the following:
________________________________________________________________________
_____ I choose that my records be accessible only by staff and people in the profession involved in my treatment
Other:
_____ I understand that federal and state laws, courts, and medical conditions may limit any of the above decisions
_____ I understand that though these are my present choices, I may change this document at any time, and
that it will be placed in my clinical record while treatment continues.
Signature of Person Printed Name of Person
Date Name of Witness
See s. 394.459(5), Florida Statutes
CF-MH 3048, Feb 05 (Recommended Form) BAKER ACT
Baker Act Forms - 43

44 - Baker Act Forms

Baker Act Forms
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Page 49
Baker Act Forms
Restriction of Communication or Visitors
Notice is hereby given to ________________________________________________________________________________
Full Name of Person
this date, that under the provisions of s.394.459(5)(c), Florida Statutes, a restriction on communications has been
placed for a period of ________ days, starting at ____________ am pm on (
Date) ___________________ and ending
at ____________ am pm on (
Date) ________________
The nature of the restriction is as follows: ___________________________________________________________________
The restriction has been ordered because _____________________________________________________________________
This restriction of communication shall be reviewed at least every 7 days and lifted as soon as possible.
__________________________________________________ _________________ ___________ am pm
Signature of Administrator or Designee Date Time
A person’s right to report an alleged abuse or to contact and to receive communication from his/her
attorney shall not be limited. This completed form must be placed in the person’s clinical record as
individualized justification for depriving the person of his/her right to communicate with others. Any
renewal of this restriction shall be justified. A copy of this form and any renewal of the restriction shall be
provided to all persons listed below, as applicable. The right to communicate or receive visitors shall not
be restricted as a means of punishment.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initial of Who
Provided Copy
Person am pm
Guardian am pm
Guardian Advocate am pm
Representative am pm
Attorney am pm
Health Care Surrogate/Proxy am pm
See s. 394.459(5)(c ), Florida Statutes
CF-MH 3049, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 45

46 - Baker Act Forms

Baker Act Forms
Page 51
Baker Act Forms
Part I
Notice of Right of Person on Voluntary Status
To Request Discharge From a Receiving Facility
A person on voluntary status or a relative, friend, or attorney of the person may request discharge either orally or in
writing at any time following admission to the facility. If the request for discharge is made by a person other than the
person, the discharge may depend on the express and informed consent of the person.
If you request discharge, your doctor will be notified and you will be discharged within 24 hours after your request for
discharge unless you withdraw your request or you meet the criteria for involuntary inpatient placement or involuntary
outpatient placement. If you meet the criteria for involuntary inpatient or outpatient placement, the facility administrator
may file a petition with the court for your continued detention within two (2) court working days and you will be detained
without your consent, pending a court hearing.
If you wish to request discharge at any time during your stay at this facility, complete the Application for Discharge on the
reverse side of page. No action on your part is required, unless you wish to make arrangements for release.
The procedure for requesting discharge has been explained to me and I have had the opportunity to ask questions and
receive answers about my right to request discharge.
_______________________________ ________________________________ _______________ ________ am pm
Printed Name of Person Signature of Person Date Time
_______________________________ ________________________________ _______________ ________ am pm
Printed Name of Guardian of Minor Signature of Guardian of Minor Date Time
_______________________________ ________________________________ _______________ _________ am pm
Printed or Typed Name of Witness Signature of Witness Date Time
cc: Check when applicable and provide date/time/initial when copy provided:
Person
Date: Time: am pm Initial:
Guardian of Child
Date: Time: am pm Initial:
Parts II and Part III are continued on back
Baker Act Forms - 47

----------------------------------------------------------------------------------------------------------------------------------------------------------------
---------------------------------------------------------------------------------------------------------------------------------------------------------------
Page 52
Baker Act Forms
Page 2
Part II Application for Discharge
Pursuant to Section 394.4625 (2), Florida Statutes, I, _____________________________________________________
hereby apply for my release or that of ________________________________________________________________
who is a voluntary patient at (
Name of Facility) ___________________________________________________________.
My relationship to the said person is that of (
Relationship) __________________________________________________.
___________________________________________________________ ___________________ __________ am pm
Signature of Person or Authorized Individual on his or her behalf Date Time
An oral request for discharge was made by _______________________________ on __________________ _________ am pm
Name of Requester Date Time
______________________________________ ________________________________ _______________ ________ am pm
Signature of Staff Printed Name of Staff Date Time
If this request for discharge was made by someone other than me, I concur with the above request for my discharge. If
not, I have completed Part III below.
_____________________________________________________________ _________________ _______ am pm
Signature of Adult Date Time
_____________________________________________________________ _________________ _______ am pm
Signature of Guardian of Minor Date Time
_____________________________________________________________ _________________ _______ am pm
Signature of Witness Date Time
cc: Check when applicable and date/time/initial when copy provided:
Person
Date: Time: am pm Initials:
Guardian of
Minor
Date: Time: am pm Initials:
Part III Withdrawal of Application for Discharge
I, ____________________________________________, freely and voluntarily rescind my previous oral or written
Application for Discharge or do not concur with the request for discharge made by another person. No force, fraud,
deceit, duress, or other form of constraint or coercion were used to obtain this withdrawal of my Application for
Discharge.
_________________________________________________________ _________________ _______ am pm
Signature of Person Date Time
________________________________________ __________________ ____________________ _______ am pm
Signature of Witness Credentials of Witness Date Time
cc: Check when applicable and date/time/initial when copy provided:
Person
Date: Time: am pm Initials:
Guardian of Minor
Date: Time: am pm Initials:
See s. 394.455(9), 394.4625(2), (3), Florida Statutes
CF-MH 3051a, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
48 - Baker Act Forms

Baker Act Forms
Page 53
Baker Act Forms
Notice of Right of Person on Voluntary Status
To Request Discharge from a Treatment Facility
Part I
A person on voluntary status or a relative, friend, or attorney of the person may request discharge either orally or in
writing at any time following admission to the facility. If the request for discharge is made by an individual other than the
person, the discharge may depend on the express and informed consent of the person.
If you request discharge, your doctor will be notified and you will be discharged within 3 days, not including weekends
and holidays, after your request for discharge unless you withdraw your request or you meet the criteria for involuntary
inpatient placement or involuntary outpatient placement. If you meet the criteria for involuntary placement, the facility
administrator may file a petition with the Court for your continued detention within two (2) court working days and you
will be detained without your consent, pending a court hearing.
If you wish to request discharge at any time during your stay at this facility, complete the Application for Discharge on
reverse side of page. No action on your part is required, unless you wish to make arrangements for release.
________________________________ ________________________________ __________________ _______ am pm
Printed or Typed Name of Person Signature of Person Date Time
________________________________ _______________________________ __________________ _______ am pm
Printed or Typed Name of Witness Signature of Witness Date Time
cc: Check when applicable and date/time/initial when copy provided:
Person
Date: Time: am pm Initials:
Parts II and III are continued on back
Baker Act Forms - 49

---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
----------------------------------------------------------------------------------------------------------------------------------------------------------------
Page 54
Baker Act Forms
Page 2
Part II Application for Discharge
Pursuant to Section 394.4625 (2), Florida Statutes, I, _____________________________________________________
hereby apply for my release or that of _________________________________________________________________
who is on voluntary status at
(Name of Facility) ___________________________________________________________.
My relationship to the said person is that of
(Relationship) __________________________________________________.
______________________________________________ ___________________ __________ am pm
Signature of Person or Authorized Individual Date Time
An oral request for discharge was made by _____________________________ on ______________ ______ am pm
Name of Requester Date Time
____________________________________ ___________________________ _______________ _____ am pm
Signature of Staff Printed Name of Staff Date Time
If this request was made by someone other than me, I concur with the above request for my discharge. If not, I have
completed Part III below.
__________________________________________________________ _________________ ___________ am pm
Signature of Person Date Time
__________________________________________________________ _________________ ___________ am pm
Signature of Witness Date Time
cc: Check when applicable and date/time/initial when copy provided:
Person
Date: Time: am pm Initials:
Part III Withdrawal of Application for Discharge
I, ____________________________________________, freely and voluntarily rescind my previous oral or written
Application for Discharge. No force, fraud, deceit, duress, or other form of constraint or coercion were used to obtain this
withdrawal of my Application for Discharge.
___________________________________________________________ _________________ ____________ am pm
Signature of Person Date Time
______________________________________________ ___________________ ________________ _________ am pm
Signature of Witness Credentials of Witness Date Time
cc: Check when applicable and date/time/initial when copy provided:
Person
Date: Time: am pm Initials:
See s. 394.455(9), 394.4625(2), (3), Florida Statutes
CF-MH 3051b, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
50 - Baker Act Forms

Baker Act Forms
Page 55
Baker Act Forms
Report of Law Enforcement Officer Initiating Involuntary Examination
State of Florida, County of ______________________, Florida
I,______________________________________________________, am a law enforcement officer certified by the State of Florida. In my opinion
_______________________________________________________ appears to meet the following criteria for involuntary examination:
1. I have reason to believe said person has a mental illness pursuant to Section 394.455 (18), F.S., and because of the mental illness (check a or b):
a. Person has refused voluntary examination after conscientious explanation and disclosure of the purpose of the examination; OR
b. Person is unable to determine for himself/herself whether examination is necessary, AND
2. Either (check all that apply)
a.Without care or treatment said person is likely to suffer from neglect or refuse to care for himself/herself, and such neglect or refusal
poses a real and present threat of substantial harm to his/her well-being and it is not apparent that such harm may be avoided through the
help of willing family members or friends or the provision of other services; AND/OR,
b There is substantial likelihood that without care or treatment the person will cause serious bodily harm to (check one or both)
self others in the near future, as evidenced by recent behavior.
Circumstances supporting this opinion, including specific information about the person’s behavior, threats and actions and information offered by
others:
______________________________________________ __________ / __________ / 20________ ________ am pm
Signature of Law Enforcement Officer Time
____________________________________________ ___________________________________________________
Printed Name of Law Enforcement Officer Full Name of Law Enforcement Agency (printed)
____________________________________________ ___________________________________________________
Badge or ID Number Law Enforcement Case Number
By Authority of s. 394.463(2)(a) 2, Florida Statutes
CF-MH 3052a, Sept 06 (obsoletes previous editions) (Mandatory Form) BAKER ACT
Baker Act Forms - 51

52 - Baker Act Forms

Baker Act Forms
Page 57
Baker Act Forms
Certificate of Professional Initiating Involuntary Examination
All sections of this form must be completed and legible (please print)
I have personally examined (printed name of person) _____________________________________________ at time _________ am pm (time must be
within the preceding 48 hours) on _________/ ________/ 20 ______ in ________________________________ County and that person appears to
meet criteria for involuntary examination OR I am a physician who has determined that (printed name of person) _______________________________
has failed or has refused to comply with the treatment ordered by the court, and, in my clinical judgment, efforts were made to solicit compliance and the
person appears to meet the criteria for involuntary examination. Section IV of this form is completed to document the requirements of the law.
This is to certify that my professional license number is:
Psychiatrist Physician (non-psychiatric) Clinical Psychologist Psychiatric Nurse
and I am a (check one box)
Clinical Social Worker
Mental Health Counselor Marriage and Family Therapist Each as defined in s.394.455, F.S.
Section I: CRITERIA
There is reason to believe person has a mental illness as defined in Section 394.455(18), Florida Statutes (excludes retardation or developmental
disabilities, intoxication, or conditions manifested only by antisocial behavior or substance abuse impairment).
Diagnosis of
Mental Illness is:
List all mental
health diagnoses
applicable to this
person
DSM Code(s)
(if known)
AND BECAUSE OF MENTAL ILLNESS
OR
A. Person has refused voluntary examination after
B. Person is unable to determine for
Statute requires that at
conscientious explanation of disclosure of the purpose himself/herself whether examination is
least one be checked,
of examination necessary
but both may be
checked if both apply
A. Without care and treatment the person is likely to suffer AND EITHER B. There is substantial likelihood that without care
from neglect or refuse to care for himself/herself, and or treatment the person will cause serious bodily
(A and/or B)
such neglect or refusal poses a real and present threat harm to (check one or both):
of substantial harm to his or her well-being and it is not
apparent that such harm may be avoided through the
self others
help of willing family members or friends or the provision
in the near future, as evidenced by recent
of other services
behaviors (describe behaviors at top of page 2)
Section II: SUPPORTING EVIDENCE
A. My observations supporting these criteria including the person’s behaviors and statements, specifically those related to suicidal ideation, previous
suicide attempts, homicidal ideation or self-injury are as follows:
CONTINUED OVER
Baker Act Forms - 53

Page 58
Baker Act Forms
Certificate of Professional Initiating Involuntary Examination (Page 2)
Section III: OTHER INFORMATION
Other information, including source relied upon to reach this conclusion is as follows. If information is obtained from other persons, describe these
sources (e.g., reports of family, friends, other mental health professionals or law enforcement officers, as well as medical or mental health records).
Section IV: NON-COMPLIANCE WITH INVOLUNTARY OUTPATIENT PLACEMENT ORDER
Complete this section if you are a physician who is documenting non-compliance with an involuntary outpatient placement order:
This is to certify that I am a physician, as defined in Florida Statutes 394.455(21), F.S. and in my clinical judgment, the person has failed or has refused to
comply with the treatment ordered by the court, and the following efforts have been made to solicit compliance with the treatment plan:
Section V: INFORMATION FOR LAW ENFORCEMENT
Provide identifying information (if known) if needed by law enforcement to find the person so he/she may be taken into custody for examination:
Age: ___________ Male Female Race/ethnicity: _________________________
Other details (such as height, weight, hair color, clothing worn when last seen, where last seen):
If relevant, information such as access to weapon, recent violence or pending criminal charges:
This form must be transported with the person to the receiving facility to be retained in the clinical record. Copies may be retained by the initiating
professional and by the law enforcement agency transporting the person to the receiving facility.
Section VI: SIGNATURE
Signature of Professional: Date Signed
Typed or Printed Name of Professional: Phone ( )
Address of Professional:
By Authority of s. 394.455(18), 394.463(2)(a)3, 394.4655, Florida Statutes
CF-MH 3052b, Sept 06 (obsoletes previous editions) (Mandatory Form) BAKER ACT
54 - Baker Act Forms

Baker Act Forms
Page 59
Baker Act Forms
Authorization for Electroconvulsive Treatment
As the physician for this person, I have recommended a series of ____________ electroconvulsive treatments and have provided sufficient
information to ensure express and informed consent to the treatment.
__________________________________ ______________________________ _______________ ________ am pm
Signature of Physician Printed Name of Physician Date Time
I have agreed with the need for this series of __________ electroconvulsive treatments after
examination of the person or review of the person’s treatment records. I am not directly involved with the person.
__________________________________ ______________________________ ________________ _________ am pm
Signature of Second Physician Printed Name of Second Physician Date Time
I, the undersigned, competent adult, guardian, guardian advocate, health care surrogate
authorize ____________________________ Electroconvulsive Treatments for ____________________________________________.
Number of treatments authorized Name of Person to Receive Treatment
a person in __________________________________________________________________________________________________
Name of Facility
The information provided to the person to make the decision to consent to electroconvulsive treatment (which must include the purpose of the
procedure, the common side effects, alternative treatments, and the approximate number of procedures considered necessary and that my
consent may be revoked prior to or between treatments) is:
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
__________________________________________________________________________________________________________
I have read and understood the information provided to me above and have been given an opportunity to ask questions and receive answers
about the procedures. Knowing the above, I hereby consent to the treatment described.
_________________________________________________________ ___________________ __________ am pm
Signature of Competent Adult Date Time
________________________________________________________ __________________ __________ am pm
Signature, * as appropriate, of: Date Time
Guardian, Guardian Advocate,
Parent of a Minor, Health Care Surrogate
________________________________________________________ __________________ __________ am pm
Signature of Witness Date Time
Facility should attach information about or copies of educational materials provided to the person and/or substitute decision
maker.
* A guardian shall produce letters of guardianship prior to authorizing ECT to demonstrate authority to provide consent. A
guardian advocate requires express Court approval to provide consent to this procedure. A health care surrogate requires an
advance directive expressly delegating such authority to the surrogate. In the absence of such an advance directive, a health
care surrogate or proxy require express court approval to consent to ECT. The authorizing documentation must be validated
by staff and filed in the person’s clinical record.
See s. 394.459(3)(b), 458.325, Florida Statutes
CF-MH 3057, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 55

56 - Baker Act Forms

Baker Act Forms
________________________________________________________
Page 61
Baker Act Forms
Baker Act Service Eligibility
Public Receiving Facility Name: ___________________________________________________________________
1. IDENTIFYING INFORMATION:
Person’s Name: _______________________________
Date of Birth: __________________________________Gender: Male Female Race: ______________
2. FINANCIAL INFORMATION: Prospective monthly income (6-month average) $__________________
Number of Family Members: _________________ Title XX Eligible: Yes No
3. LEGAL STATUS: Voluntary Admission Involuntary Examination
4. CRITERIA: (check the appropriate criteria)
There is reason to believe the above-named person has a mental illness, as defined in 394.455(18), AND
Without care or treatment, the person is likely to suffer from neglect or refuse to care for himself or herself, such
neglect or refusal poses a real and present threat of substantial harm to his or her well-being, and it is not
apparent that such harm may be avoided through the help of willing family members or friends or the provision of
other services,
OR
There is a substantial likelihood that without care or treatment the person will cause serious bodily harm to himself
or herself or others in the near future, as evidenced by recent behavior.
5. MOST RECENT DSM OR ICD ADMISSION DIAGNOSIS AND CODE NUMBER: ___________________________
6. SUMMARY: Behavioral manifestations justifying diagnosis. (A completed CF-MH 3052a or 3052b or Ex Parte Order
may be attached for persons on involuntary status)
7. RECOMMENDED DISPOSITION / PLACEMENT:
8. WHY IS A LESS RESTRICTIVE PLACEMENT NOT BEING UTILIZED?
9. APPROVAL OF DISPOSITION/PLACEMENT does does not include authorization for payment of
contracted 24-hour care.
______________________________________________________ _________________ __________ am pm
Signature of Administrator or Designee Date Time
Printed Name of Administrator or Designee
By authority of s. 394.74, 394.875, 394.879, Florida Statutes
CF-MH 3084, Feb 05 (obsoletes previous editions) (Mandatory Form for Public Receiving Facilities) BAKER ACT
Baker Act Forms - 57

58 - Baker Act Forms

Baker Act Forms
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
Page 63
Baker Act Forms
Transfer Evaluation
(To a State Mental Health Treatment Facility)
I, ________________________________________________________________________ concur do not concur
Full Name of Mental Health Center/Clinic Director or Chief Clinical Officer
that ______________________________________________ , residing at ____________________________________________
Full Name of Person Name and Address of Receiving Facility
meets statutory criteria for voluntary or involuntary admission to a state mental health treatment facility.
I find that less restrictive community based treatment alternatives have been considered for this person and were determined to be
(Check one): inappropriate unavailable appropriate and available.
If placement at a State Mental Health Treatment Facility is recommended, specify the reason for the recommendation:
If it is determined that the person does not meet criteria for admission to a state mental health treatment facility, and consequently a
diversion to a less restrictive voluntary community-based service is appropriate, specify the recommended facility and type of
service:
____________________________ _____________________________ _______________ ___________ am pm
Signature of Evaluator Printed Name and Title of Evaluator Date Time of Evaluation
______________________________________ ________________________ ____________ am pm
Original Signature of Date Time
Executive Director or Chief Clinical Officer
_______________________________________________________ (______)_____________________
Name and Address of Community Mental Health Center or Clinic Telephone Number
This form is to be completed by a designated staff member employed by a Community Mental Health Center or Clinic
whenever a person is being considered for admission to a state mental health treatment facility either on a voluntary or
involuntary basis. In the case of potential involuntary admission, the original copy of this form shall be provided for the
Court's consideration prior to the hearing on the petition for involuntary placement. The evaluator or another
knowledgeable person from the center or clinic shall be present at the court hearing to provide testimony as desired by the
court.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Circuit Court
am pm
District DCF Mental Health Office
am pm
By Authority of s. 394.455(29), 394.461, Florida Statutes
CF-MH 3089, Feb 05 (obsoletes previous editions) (Mandatory Form) BAKER ACT
Baker Act Forms - 59

60 - Baker Act Forms

Baker Act Forms
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Page 65
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: _____________________
_____________________________________,
Petitioner,
vs.
_____________________________________,
Administrator,
_____________________________________,
Facility Respondent.
Petition for Writ of Habeas Corpus or for Redress of Grievances
1. This Court has jurisdiction pursuant to Section 394.459 (8), Florida Statutes.
2. Petitioner is being held by _______________________________________________________ ,
(Administrator) in
___________________________________________,
(Facility), in __________________________ (City), Florida.
3.
Petitioner believes that he/she is being deprived of her/his freedom for invalid and illegal reasons. Petitioner believes
that her/his confinement is illegal because: ____________________________________________________________
and/or
4.
Petitioner believes that he/she is being unjustly denied a right or privilege or that a procedure authorized by law is
being abused. Petitioner believes that he/she is being unjustly denied a right or privilege or that a procedure authorized by
law is being abused because: __________________________________________________________________________
5. Petitioner is unable to afford counsel and would like the Office of the Public Defender or other counsel to be appointed to
represent her/him in the above captioned matter.
CONTINUED OVER
Baker Act Forms - 61

_______________________________________________________
Petition for Writ of Habeas Corpus or for Redress of Grievances (Page 2)
WHEREFORE, Petitioner respectfully requests that this Court:
Appoint the Office of Public Defender or other counsel to represent your Petitioner in these proceedings; and
Enter an Order setting a return hearing on this Petition for Writ of Habeas Corpus for respondent to show by what legal
authority he/she holds petitioner, and/or
Set a hearing for the purpose of a judicial inquiry into the allegations of this Petition for Redress of Grievances and for
ordering a correction of abuse of rights or privileges granted under Chapter 394, Part I, F.S.
I HEREBY CERTIFY that the above stated matters In the Petition for Writ of Habeas Corpus and Redress of Grievances are
true and correct to the best of my information, knowledge, and belief.
________________________________________________________ ____________________ __________ am pm
Signature of Petitioner Date Time
Printed Name of Petitioner
There is or is not a petition for involuntary placement pending.
The person
is or is not currently represented by counsel.
Facilities must provide this form to any person making a verbal request for access to the Court. The
completed form must be filed with the Clerk of the Court no later than the next working day and a copy
retained in the person’s clinical record. A copy of the completed Petition for Writ must be provided
immediately to the person and copies of the Petition provided to those listed below, as applicable.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
Attorney
am pm
Health Care Surrogate/Proxy
am pm
See s. 394.459(8), Florida Statutes
CF-MH 3090, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
Page 66
Baker Act Forms
62 - Baker Act Forms

Baker Act Forms
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Page 67
Baker Act Forms
Application for Voluntary Admission - Minors
I _______________________________________________________________________ do hereby apply on behalf of
Full printed name of guardian of minor whose admission is being requested
__________________________________________ for admission to ____________________________________________
Full printed name of minor Name of facility
for observation, diagnosis, care, and treatment of a mental illness, and I certify that the information given on this application is
true and correct to the best of my knowledge and belief.
I am making this application for voluntary admission after sufficient explanation and disclosure so me and the minor so we can
make a knowing and willful decision without any element of force, fraud, deceit, duress, or other form of constraint or coercion.
The reason for admission to this facility is: ___________________________________________________________________
As guardian of this minor, I am a competent adult with the capacity to make well-reasoned, willful, and knowing decisions
concerning medical or mental health treatment. I understand that I must keep the facility informed of my whereabouts during
the time of this admission.
The minor and I have been provided with a written explanation of rights of a person on voluntary status and they have been
fully explained to us. I understand that this facility is authorized by law to detain the minor without my consent for up to 24
hours after I or the minor make a request for discharge from a receiving facility; unless a petition for involuntary placement is
filed with the Court as required by law within two (2) court working days of the request for discharge.
I understand that I may be billed for the cost of the minor’s treatment.
_________________________________ _______________________________ _______________ ___________ am pm
Printed Name of Guardian Signature of Guardian Date Time
_________________________________ _______________________________ _______________ ___________ am pm
Printed Name of Witness Signature of Witness Date Time
I agree with the decision for me to be voluntarily admitted to this facility. This agreement is being given without
any element of force,
fraud, deceit, duress, or other form of constraint or coercion. I have been provided with a written explanation of my rights and
they have been fully explained to me.
_________________________________ _______________________________ _______________ ___________ am pm
Printed Name of Minor Signature of Minor Date Time
_________________________________ _______________________________ _______________ ___________ am pm
Printed Name of Witness Signature of Witness Date Time
No notice of this admission is to be made without the consent of the minor’s guardian except in case of an
emergency. The original of this signed form must be filed in the clinical record.
See s. 394.459, 394.4625, Florida Statutes
CF-MH 3097, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 63

64 - Baker Act Forms

Baker Act Forms
____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
I
Page 69
Baker Act Forms
Application for Voluntary Admission
(State Treatment Facility)
I, _________________________________________________________________________ do hereby apply for admission to
Full printed name of person whose admission is being requested
Fill in name of facility
for observation, diagnosis, care, and treatment of a mental illness, and I certify that the information given on this application is
true and correct to the best of my knowledge and belief.
I am making this application for voluntary admission after sufficient explanation and disclosure to make a knowing and willful
decision without any element of force, fraud, deceit, duress, or other form of constraint or coercion. The reason for my
admission to this facility is:
_____________________________________________________________________________________________________.
I am a competent adult with the capacity to make well-reasoned, willful, and knowing decisions concerning my medical or
mental health treatment. I do not have a guardian, guardian advocate, or currently a health care surrogate/proxy making health
care decisions for me.
have have not provided a copy of advance directive(s). If so, the advance directives include my
Living Will,
Health Care Surrogate,
Mental Health Care Surrogate, or
Other as specified: _________________.
I have been provided with a written explanation of my rights as a person on voluntary status and they have been fully explained
to me. I understand that this facility is authorized by law to detain me without my consent for up to 3 days, not including
weekends and holidays, after I make a request for discharge unless a petition for involuntary placement is filed with the Court
within two (2) court working days of my request for discharge.
I understand that I will be asked to complete a financial disclosure form and may be billed for the cost of my treatment.
I understand that the facility is authorized by law to transfer me to another departmental facility when it is necessary to meet my
medical needs or for the efficient use of the department’s facilities. I understand that prior to transfer, the administrator of the
facility will give me written notice.
___________________________________________________________ __________________ ___________ am pm
Signature of Adult Date Time
________________________________ ______________________________ _________________ _________ am pm
Printed Name of Witness Signature of Witness Date Time
No notice of this admission is to be made without the consent of the person except in case of an
emergency. The use of this form for a voluntary admission requires that a “Certification of Person’s
Competence to Provide Express and Informed Consent” be completed within 24 hours and if the form is
used for a transfer of a person from involuntary to voluntary status, the “Certification” must be completed
prior to the “Application”. The “Application” and “Certification” must be placed in the person’s clinical
record.
See s. 394.455(9), 394.459, 394.4625, Florida Statutes
CF-MH 3098, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 65

66 - Baker Act Forms

Baker Act Forms
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
_____________________________________________ ___________________ _____________________
Page 71
Baker Act Forms
Certification of Ability to Provide Express and Informed Consent
For Voluntary Admission and Treatment of Selected Persons
From Facilities Licensed under Chapter 400, F.S.
On __________________________, at ______________ (a.m.) (p.m.) _____________________________________,
Date Time Print Name of the Person
who resides at ___________________________________________________________________________________
Person’s Residence Name and Address
made application by express and informed consent for voluntary admission to __________________________________
facility located at __________________________________________________________________________________.
Address of Facility
He or she is:
(Check the box that applies)
A person 60 years of age or older diagnosed with dementia for whom transfer is being sought from nursing home,
assisted living facility, adult day-care center, or adult family-care home.
A person 60 years of age or older for whom emergency transfer is being sought from a nursing home pursuant to s.
400.0255(6).
A person for whom all decisions concerning medical treatment are currently being lawfully made by the health care
surrogate or proxy designated under Chapter 765, F.S.
He/she
does or does not have the capacity to make a well-reasoned, willful, and knowing
decision concerning his or her medical or mental health treatment.
has or has not consented in writing, after sufficient explanation and disclosure of
the need for admission, without any element of force, fraud, deceit,
duress, or other form of constraint or coercion.
He/she
The observations on which I have reached this conclusion are:
_____________________________________________ ___________________________ ______________ am pm
Signature of Assessor * Date of Assessment Time of Assessment
Typed or Printed Name of Assessor Profession License Number (if any)*
* If publicly funded assessor is not licensed, specify the name, profession and license number of supervising professional:
Name: _______________________________________ Profession: _________________________ License #: ________________
Name of Mental Health Overlay Program (a service provided under contract with the Department of Children & Families and attached to a public
receiving facility): _____________________________________________________________________________________________________
Name of Mobile Crisis Response Service (a service provided under contract with the Department of Children & Families and attached to a public
receiving facility): _____________________________________________________________________________________________________
Name of Community Mental Health Center or Clinic (publicly funded, not-for-profit center under contract with the Department of Children &
Families): ____________________________________________________________________________________________________________
OVER FOR USE BY INDEPENDENT PROFESSIONAL
Baker Act Forms - 67

____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
_________________________________________________ ___________________________ ____________________
Baker Act Forms
Certification of Ability to Provide Express and Informed Consent
For Voluntary Admission and Treatment of Selected Persons
From Facilities Licensed Under Chapter 400, F.S.
(Page 2)
When an initial assessment of the ability of a person to give express and informed consent to treatment is required and a
mobile crisis response service does not or cannot respond to the request for an assessment within two (2) hours after the
request is made, the requesting facility may arrange for assessment by any licensed professional authorized to initiate an
involuntary examination, pursuant to s. 394.463 who is not employed by or under contract with, and does not have a
financial interest in, either the facility initiating the transfer or the receiving facility to which the transfer may be made. I
certify that the mobile crisis service, if one exists, has been contacted and cannot respond within the 2-hour period and
that I have no conflict of interest as defined above.
NOTICE: Under the provisions of s. 400 F.S. and 394.4625(1)(c), it is unlawful for this assessment to be conducted
by any professional who is employed by, under contract with, or who has a financial interest in, either the facility
initiating the transfer or the receiving facility to which the transfer may be made.
The person applying for voluntary admission
does or does not have the capacity to make a well-reasoned,
willful, and knowing decision concerning
his or her medical or mental health treatment.
He/she
has or has not consented in writing, after sufficient explanation and disclosure of the need for
admission, without any element of force, fraud, deceit, duress, or other form of
constraint or coercion.
The observations on which I have reached this conclusion are:
_________________________________________________ _____________________ _________________ am pm
Signature of Independent Professional Date Time of Assessment
Typed or Printed Name of Professional Profession * License Number
* Physician, Clinical Psychologist, Clinical Social Worker, or Psychiatric Nurse whose education, training, experience, and
licensure comply with statutory provisions of s. 394.455, F.S. A Licensed Mental Health Counselor is also authorized to
perform this assessment on or after July 1, 2005.
Distribution:
Original to the Receiving Facility for retention in person’s clinical record
Facility at which the person was assessed
Assessor
See s. 395.455(9), 394.4625(1)(a), (b), (c), Florida Statutes
CF-MH 3099, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
Page 72
68 - Baker Act Forms

Baker Act Forms
________________________________________________ ____________________________________________
________________________________________________ _____________________________________________
Page 73
Baker Act Forms
Transportation to Receiving Facility
Part I: General Information
The circumstances, under which (Name of Person) _____________________________ was taken into custody are as follows:
Time: am pm Date:
Place or Facility Name:
Pick Up Address:
Family members or others present when person was taken into custody
Name Address Relationship Phone Number
Next of Kin (if known)
Indicate personal knowledge by family members and others about the person’s condition.
Delivered to
(Nearest Receiving Facility):
Basis for Custody: (Check one) Ex Parte Order Certificate of Mental Health Professional Report of Law Enforcement Officer
________________________________________________ __________________ _____________ am pm
Signature of Law Enforcement Officer Date Time
Printed Name of Law Enforcement Officer Full Name of Law Enforcement Agency
Badge or ID Number Law Enforcement Case Number
CONTINUED OVER
Baker Act Forms - 69

Page 74
Baker Act Forms
Part II - Used When Law Enforcement Consigns Persons to Contract Transport (Page 2)
or to Emergency Medical Personnel
If transport is used due to the medical condition of the person or due to a county-funded contract with a transport company,
print the name of the company _____________________________________________________________________________
which will transport the person to the nearest emergency room in the case of a medical emergency or, if not a medical
emergency, to the nearest designated receiving facility _________________________________________________________.
(specify facility to which person is to be taken)
The law enforcement agency and the transport service must agree that the continued presence of law enforcement personnel is
not expected at the time of consignment to be necessary for the safety of the person or others.
I, _______________________________________________ of the ______________________________________________
Printed Name of Law Enforcement Officer Printed Name of Law Enforcement Agency
and
I, ______________________________________________ of the _______________________________________________
Printed Name of Medical Transport Service Representative Printed Name of Medical Transport Service
agree that the continued presence of the law enforcement agency is not expected to be necessary for the safety of
______________________________________________________________ or others. By affixing my legal signature and
date/time of signing below, I understand that continued transporting of the person named above to a receiving facility is no
longer the responsibility of law enforcement agency. The responsibility is assumed by the medical transport service in
accordance with s. 394.462 (1), F.S.
_____________________________________________ ________________________ ______________ am pm
Signature of Law Enforcement Officer Date Signed Time Signed
_____________________________________________ ________________________ ______________ am pm
Signature of Representative of Medical Transport Service Date Signed Time Signed
This form must be delivered with the person to the receiving facility for inclusion in the clinical record. A
copy may be retained by the law enforcement agency and by the medical transport service.
By Authority of s. 394.462(18), 394.463, Florida Statutes
CF-MH 3100, Feb 05 (obsoletes previous editions) (Mandatory Form) BAKER ACT
70 - Baker Act Forms

Baker Act Forms
_______________________________________________________ _________________________________
Page 75
Baker Act Forms
Hospital Determination That
Person Does Not Meet Involuntary Placement Criteria
I have personally examined ___________________________________________________, a person for whom an
involuntary examination has been initiated pursuant to 394.463 who was brought to __________________________________
Hospital (not designated as a Baker Act receiving facility) for evaluation or treatment of an emergency medical condition.
I have conducted the initial mandatory involuntary examination, including documenting observations of the person’s recent
behavior, reviewing the form initiating this examination and the transportation form, conducting a brief psychiatric history, and
conducting a face-to-face examination of the person.
Check at least one box from each of the two categories below:
I have determined that he/she does NOT meet the criteria for involuntary inpatient placement pursuant to 394.467 based upon
one or more of the following reasons:
Does not suffer from a mental illness, as defined in s. 394.455(18)
Has not refused placement or is able to determine for himself or herself that placement is necessary
Is not likely to suffer from neglect posing a real and present threat of substantial harm nor is there substantial likelihood that in the
near future he/she will inflict serious bodily harm on self or others as evidenced by recent behavior causing, attempting, or
threatening such harm.
There are available less restrictive treatment alternatives offering an opportunity for improvement of his/her condition
AND
I have determined that he/she does NOT meet the criteria for involuntary outpatient placement pursuant to394.4655 based
upon one or more of the following reasons:
Person is under age 18;
Does not suffer from a mental illness, as defined in s. 394.455(18)
Person is likely to survive safely in the community without supervision, based on my clinical determination;
Person has no history of lacking compliance with treatment for a mental illness
Person has not within the preceding 36 months been involuntarily admitted to a Baker Act receiving or treatment facility, or
received mental health services in a forensic correctional facility or engaged in one or more acts of serious violent behavior
toward self or other, or attempts at serious bodily harm to self/others;
Person has not been found to be unlikely to voluntarily participate in recommended treatment and has not either refused voluntary
placement or been found to be unable to determine whether placement is necessary;
Person hasn’t been found, based on his/her treatment history and current behavior, to need involuntary outpatient placement to
prevent a relapse or deterioration that would be likely to result in serious bodily harm to self or others, or a substantial harm to
his/her well-being;
There has been no finding that it is likely the person will benefit from involuntary outpatient placement; or
There are less restrictive treatment alternatives available that offer an opportunity for improvement of his/her condition
This examination was conducted at _________________ a.m. p.m. on ________________________________.
Time of Examination Date of Examination
As a physician or licensed clinical psychologist and recognized by this hospital as eligible to perform the involuntary
examination, I have:
Offered voluntary placement of this person OR Approved the direct release of this person
from the hospital.
______________________________________________________ __________________ _____________ am pm
Signature of
Physician Clinical Psychologist Date Time
Typed or Printed Name of Examiner License Number
If a person is released from a hospital after being evaluated or treated for an emergency medical condition, this
completed form or its equivalent must be completed and retained in the person’s clinical record and a Notice of
Release or Discharge (CF-MH 3038 or equivalent) must be given or sent to the person, the person’s guardian, to
any person who executed a Certificate, and to any Court which ordered the person’s examination.
See s. 394.455(2), (18), (21), 394.463(2)(f), (g), (h), 394.467, Florida Statutes
CF-MH 3101, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 71

72 - Baker Act Forms

Baker Act Forms
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
__________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
___________________________________________________ _________________________________________________
Page 77
Baker Act Forms
Request for Involuntary Examination after Stabilization of Emergency Medical Condition
The following person ____________________________________________________, for whom an involuntary examination has been
initiated has been evaluated or treated at ____________________________________________________________ Hospital located at
________________________________________________________________________________ for an emergency medical condition.
a. The person arrived at this hospital at: __________ am pm on _________________________, 20_____.
b. The attending physician documented that the person had an emergency medical condition at:
__________ am pm on ________________, 20__.
c. The attending physician documented at __________ am pm on ___________________, 20___
That the person’s medical condition had stabilized, or
That an emergency medical condition did not exist
This hospital is notifying ___________________________________________________________________________________________, a
designated receiving facility or the psychiatric unit within this hospital, within two (2) hours of the time noted in (c ) above that the person
must be examined by a designated receiving facility and released; or the person must be transferred to a designated receiving facility in which
appropriate medical treatment is available.
Within 12 hours of the time noted in (c) above, the designated receiving facility:
(check one or both boxes)
Shall perform the involuntary examination at this hospital or,
Shall, if it has available the appropriate medical treatment, accept transfer of the person.
The nature and extent of this person’s current medical problems: _____________________________________________________________
This hospital, pursuant to federal and state statutes, will provide or secure transport of this person via: _______________________________
with expected time of arrival of: ___________ am pm on ______________, 20______ unless other methods of transportation
have been arranged as specified:
_________________________________________ __________________ __________________ __________ am pm
Signature of Administrator or Designee Credentials Date Time
Typed or Printed Name Name of Hospital
* Transfers of persons in a psychiatric emergency must be performed in compliance with the federal EMTALA law. This
completed form must be given to the receiving facility with the form initiating the involuntary examination prior to or at
the time of the transfer of the person with a copy retained in the clinical record. The person shall not be held for
involuntary examination longer than a total of 72 hours plus the period during which an emergency medical condition
was declared by the attending physician.
See s. 394.463(g), (h), Florida Statutes
CF-MH 3102, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 73

74 - Baker Act Forms

Baker Act Forms
Page 79Baker Act Forms
Rights of Persons
In Mental Health Facilities and Programs
The following rights are guaranteed to you under Florida law. These will be fully explained to you at the time of and following admission
to this facility. A copy of this form will be given to you to keep. You have the right to read the Baker Act law and rules at any time. Your
signature on the form, if you choose to sign, only acknowledges that you have had the rights explained and that a copy of this form was
provided to you.
Individual Dignity
You have the right to individual dignity and access to all constitutional rights. The federal Americans with Disabilities Act (ADA) applies
to persons in this facility.
Right to Request Discharge by Persons on Voluntary Status
If you request discharge, your doctor will be notified and you will be discharged within 24 hours from a designated community facility
and within 3 working days from a state hospital, unless you withdraw your request or you meet the criteria for involuntary plac ement. If
you meet the criteria for involuntary inpatient placement or involuntary outpatient placement, the hospital administrator must file a
petition with the Court for your continued stay within two (2) working days of your request for discharge.
Designation of Representative
You will be asked to identify a person to be notified in case of an emergency. Further, if you are at this facility for involuntary
examination and do not have a guardian appointed by the court, you will be asked to designate a person of your choice to receive
notification of your presence in this facility, unless you request that no notification be made. If you do
not or cannot designate a
representative, a representative will be selected for you by the facility from a prioritized list of persons. You have the right to be
consulted about the person selected by the facility and you can request that such a representative be replaced.
Communication
You have the right to communicate openly and privately by phone, mail, or visitation with persons of your choice during your stay at this
facility. You have the right to make free local calls and will be given access to a long distance service for collect calls. If communication
is restricted, you will be given a written notice including the reasons for the restrictions. This facility is required to develop reasonable
rules governing visitors, visiting hours, and the use of telephones but you cannot be limited in your access to your attorney, to a phone
for the purpose of reporting abuse, in contacting the Florida Local Advocacy Council or the Advocacy Center for Persons with
Disabilities. Several toll-free telephone numbers you may wish to keep are:
Florida Abuse Registry 1 800 96-ABUSE (962-2873) TDD: 1-800-453-5145
Advocacy Center for Persons with Disabilities 1 800 342-0823
Confidentiality of Information and Records
Information about your stay in this facility is confidential and may not be released, except under special circumstances, without your
consent (or the consent of your guardian or guardian advocate or health care surrogate/proxy if you have one). Special circumstances
include release of information to your attorney, in response to a court order, to an aftercare treatment provider, or after a threat of harm
to another person. You have the right of reasonable access to your clinical record unless such access is determined to be harmful to
you by your physician.
Treatment
You have the right to receive the least restrictive, available, appropriate treatment in this facility. You will get a physical examination
within 24 hours of arrival and you will be asked to help develop a treatment plan to meet your individual needs. The criteria,
procedures, and required staff training used by this facility for restraints, seclusion, isolation, emergency treatment orders, close levels
of supervision, or physical management are available for your review. Such interventions may never be used for punishment,
convenience of staff, or to compensate for inadequate staffing.
Advance Directives
You have the right to prepare an advance directive when competent to do so that specifies the mental health care you want or don’t
want and to designate a health care surrogate to make those decisions for you at the time of crisis. The facility is required to make
reasonable efforts to honor those choices or transfer you to another facility that w
ill honor your choices. The facility must document
whether you have an advance directive and inform you of its policies about advance directives. There are organizations that can help
you prepare an advance directive.
(Continued Over)
Baker Act Forms - 75

____________________________________________________________ ____________________ ____________
Page 80
Baker Act Forms
Rights of Persons
In Mental Health Facilities and Programs (page 2)
Informed Consent
Before any treatment is given to you, you will be given information about the proposed treatment, the purpose of the treatment, the
common side effects of medication you receive, alternative treatments, the approximate length of care, and that any consent given may
be revoked at any time by you, your guardian your guardian advocate, or your health care surrogate/proxy. There are additional
disclosures that must be made for mediations you receive. If the treatment for which you have given consent is changed at any time
during your stay in this facility, it will be fully explained by the staff prior to asking for your written consent to the revised treatment.
Clothing and Personal Effects
You have the right to keep your clothing and personal effects unless they are removed for safety or medical reasons. If they are taken
from you, an inventory of the possessions will be prepared and given to you to sign. The possessions will be immediately returned to
you or your representative upon your discharge or transfer from this facility.
Habeas Corpus
You or your representative has the right to ask the Court to review the cause and legality of your detention in this facility or if you
believe you have been unjustly denied a legal right or privilege or an authorized procedure is being abused. A petition form w ill be
given to you by staff upon your request. If you wish to file a habeas corpus petition, you can submit it to a facility staff member, and it
will be filed with the court for you by the facility no later than the next court working day.
Voting
You have the right to register to vote and to cast your vote in any elections unless the court has removed this right from you. Staff will
assist you in arranging for registration or voting.
Discharge
You have the right to seek treatment from the professional or agency of your choice after your discharge from this facility.
____________________________________________________________ ___________________ ____________ am pm
Person’s Signature Date Time
am pm
Signature, if applicable, of
Guardian Guardian Advocate Date Time
Representative Health Care Surrogate/Proxy
____________________________________________________________ ____________________ ____________ am pm
Witness Signature Date Time
This form must be retained in the clinical record as a receipt that the person received notice of his/her rights at the time of
admission. A copy must be given to the person and to any authorized decision-maker for persons incompetent or
incapacitated by age or disability.
cc: Check when applicable and initial/date/time when copy provided
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian am pm
Guardian Advocate a m pm
Representative am pm
Health Care Surrogate/Proxy am pm
See s. 394.459, 394.4615, Florida Statutes
CF-MH 3103, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
76 - Baker Act Forms

Baker Act Forms
________________________________________ ___________________________________
Page 81
Baker Act Forms
Certification of Person’s Competence
To Provide Express and Informed Consent
I have personally examined______________________________, a person being served at _________________
_____________________________________
facility on __________________, 20____ at ___________ am pm.
Express and informed consent means consent voluntarily given in writing, by a competent person, after sufficient
explanation and disclosure of the subject matter involved to enable the person to make a knowing and willful decision
without any element of force, fraud, deceit, duress, or other form of constraint or coercion.
This person is 18 years of age or older, is not now known to be incapacitated with a guardian, is not now known to be
incompetent to consent to treatment with a guardian advocate, and does not have a health care surrogate or proxy
currently making medical treatment decisions. I have found this person to be one of the following:
Competent to provide express and informed consent, as defined above, for voluntary admission to this facility and is
competent to provide express and informed consent for treatment. He/she has the consistent capacity to make well
reasoned, willful, and knowing decisions concerning his or her medical or mental health treatment. The person fully
and consistently understands the purpose of the admission for examination/placement and is fully capable of
personally exercising all rights assured under section 394.459, F.S.
Incompetent to provide express and informed consent to voluntary admission. and thus is incompetent to provide
express and informed consent to treatment. The person must be transferred to involuntary status and a petition for a
guardian advocate filed with the Circuit Court. .
Refusing to provide express and informed consent to voluntary admission but is competent to provide express and
informed consent for treatment. The person must be discharged or transferred to involuntary status.
Signature of Physician License Number
_______________________________________ ____________________ _________ am pm
Typed or Printed Name of Physician Date Time
Form shall be completed within 24 hours of a person’s arrival at the receiving facility and filed in the clinical record of each
person:
1. Admitted on a voluntary basis
2. Permitted to provide express and informed consent to his/her own treatment.
3. Allowed to transfer from involuntary to voluntary status
4. Prior to permitting a person to consent to his or her own treatment after having been previously found incompetent to
consent to treatment.
See s. 394.459(3), 394.4625(1)(f), Florida Statutes
CF-MH 3104, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 77

78 - Baker Act Forms

Baker Act Forms
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
__________________________________________________ _______________________________________________
_________________________________________________________________________________________________________________
Page 83
Baker Act Forms
Refusal or Revocation of Consent to Treatment
PART I
________________________________________, a person in this facility, refuses consent revokes previous consent;
OR _____________________________________, the guardian,
guardian advocate, or health care surrogate/proxy for
_____________________________________, a person who is incapacitated or incompetent to consent to treatment in this facility,
refuses consent revokes previous consent for: All treatment, or The following treatment:
The reason given for this refusal/revocation, if any, is: _________________________________________________________________
___________________________________________________________ _______________ ___________ am pm
Signature of Competent Adult (or staff if oral refusal) Date Time
___________________________________________________________ _______________ ___________ am pm
If incompetent, signature of
Guardian, Guardian Advocate, Date Time
Health Care Surrogate, Health Care Proxy
PART II Facility Response
A person on voluntary status who has been admitted to a facility and who refuses to consent to or revokes consent to treatment shall be
discharged within 24 hours after such refusal or revocation, unless transferred to involuntary status or unless the refusal or revocation is
freely and voluntarily rescinded by the person. The guardian, guardian advocate, or health care surrogate/proxy has the right to refuse or
revoke consent to treatment. The decision of the guardian, guardian advocate, or health care surrogate/proxy may be reviewed by the court,
upon petition of the person’s attorney, the person’s family, or the facility administrator.
The facility’s response to the refusal/revocation of consent was: _____________________________________________________________
Staff Signature Profession
_________________________________________________________ ___________________________ ____________ am pm
Typed or Printed Name of Staff Date Time
PART III Withdrawal of Refusal or Revocation of Consent to Treatment
I, _____________________________________________, freely and voluntarily rescind my previous refusal or revocation of consent to
treatment for the following reason(s): ___________________________________________________________________________________
___________________________________________________________ __________________ ____________ am pm
Signature of Authorized Decision-Maker Date Time
Person, Guardian, Guardian Advocate,
Health Care Surrogate, Health Care Proxy
_______________________________________________ _________________ _________________ _______ am pm
Signature of Witness Credentials Date Time
See s. 394.4625(2)(b), Florida Statutes
DCF-MH 3105, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 79

80 - Baker Act Forms

Baker Act Forms
Page 85
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________________ CASE NO.: __________________________
Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate
PART I
I, __________________________________________________________________________, Administrator of
__________________________________________________________________________________________
Name of Facility
__________________________________________________________________________________________
Facility Address
hereby recommend that _______________________________________________________________________ be
adjudicated incompetent to consent to:
Mental health treatment
Medical treatment
and that a guardian advocate be appointed to make such health care decisions for the person. The person is presently
placed in the County of ________________________ and has residence in the County of _____________________.
OR
Is presently ordered to involuntary outpatient placement in the County of :__________________________________.
PART II Psychiatric Opinion Supporting the Petition
I,____________________________________________________, a psychiatrist authorized to practice in the
State of Florida, have personally examined __________________________________________________________
Name of Person Examined
on __________________, and found his/her judgment to be so affected by a mental illness that he/she lacks the
Date
capacity to make a well-reasoned, willful, and knowing decision concerning his/her medical and/or mental
health care. Observations which support this opinion are: ________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_____________________________________________________ _______________________ _____________ am pm
Signature of Psychiatrist Date Time
____________________________________________________ _________________________________________
Typed or Printed Name of Psychiatrist License Number
CONTINUED OVER
Baker Act Forms - 81

___________________________________________________________
Page 86
Baker Act Forms
Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate
(Page 2)
PART III - Proposed Guardian Advocate
______________________________________________________________________________, who resides at
_______________________________________________________________________________________ and whose
relationship to the person is ___________________________________, has agreed to serve as guardian advocate.
He/she has been provided with information about the duties and responsibilities of guardian advocates, including the
information about the ethics of medical decision-making.
____________________________________________________________ __________________ __________ am pm
Signature of Administrator or Designee Date Time
Typed or Printed Name of Administrator or Designee
Complete Parts I, II, and III to Petition for a Guardian Advocate
Complete Part I only to petition the Court to expand a current guardian advocate’s authority to provide consent to
medical treatment in addition to mental health treatment.
Complete Part I and Part III to request the circuit court to appoint a substitute guardian advocate for one who cannot or
will not perform his or her duties.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy
Provided
Time Copy Provided Initial of Who Provided
Copy
Person am pm
Representative am pm
Current Guardian Advocate am pm
Prospective Guardian Advocate am pm
Person’s Attorney am pm
See s. 394.4598(1), (2), (3), (4), (5), (6), Florida Statutes
CF-MH 3106, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
82 - Baker Act Forms

Baker Act Forms
________________________________________________ _______________________________________________
Page 87
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: __________________________________________ CASE NO.: __________________________
Order Appointing Guardian Advocate
This matter came to be heard on the issue of whether the above-named person should be adjudicated incompetent to consent to
treatment, and the Court finds by clear and convincing evidence as follows:
1. Said person has been represented by counsel.
2. Said person is not presently adjudicated incapacitated with a duly appointed guardian with authority to consent to treatment.
3. Said person meets the definition for being incompetent to consent to treatment pursuant to Section 394.455 (15), Florida Statutes.
This finding is determined from the testimony of _______________________________________________________. The court
has considered testimony and other evidence regarding said person’s competence to consent to treatment and based on such
testimony and evidence has concluded that said person is not competent to consent to treatment.
On the basis of these findings, it is hereby,
ORDERED
That the above-named person presently within the county, is incompetent to consent to treatment because his/her judgment
is so affected by a mental illness that he/she lacks the capacity to make a well-reasoned, willful, and knowing decision
concerning his or her medical and/or mental health treatment.
______________________________________________________________________, whose relationship to the person is:
Name of Guardian Advocate
Health Care Surrogate
2.
Person’s Spouse
3.
Person’s Adult Child
4.
Person’s Parent
1.
Person’s Adult Next of Kin
6.
Person’s Adult Friend
7.
Adult Trained and Willing to Serve
5.
Has agreed to serve as guardian advocate and:
a. Will obtain from the facility sufficient information in order to decide whether to give express and informed consent to the treatment,
including information that the treatment is essential to the care of the person, and that the treatment does not present an unreasonable
risk of serious, hazardous, or irreversible side effects.
b.
Has agreed to meet and talk to the person and the person’s physician in person, if at all possible, and by telephone if not, before giving
consent to treatment.
c. Has or will undergo a training course approved by this Court prior to exercising this authority, unless waived by this Court.
d. Will be provided access to the appropriate clinical records of the person.
This guardian advocate has been given authority by this Court to consent, refuse consent, or revoke consent for:
mental health treatment medical treatment
but may not consent to abortion, sterilization, electroconvulsive treatment, psychosurgery, or experimental treatments unless express
Court approval in a separate proceeding is given.
This appointment as Guardian Advocate shall terminate upon the discharge of the person from an order for involuntary
outpatient placement or involuntary inpatient placement or the transfer of the person to voluntary status, or an order of the
court restoring the person’s competence.
DONE AND ORDERED this _______________ day of _________________________, _______________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
cc: Person _____ Guardian Advocate _____ Representative _____ Facility Administrator _____ Person’s Attorney
See s. 394.455(15), 394.4598(1), (2), (3), (4), (6), (7), Florida Statutes
CF-MH 3107, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 83

84 - Baker Act Forms

Baker Act Forms
_______________________________________________________________________________________________________________
_______________________________________________________________________________________________________________
_______________________________________________________________________________________________________________
________________________________________________________ __________________________________
Page 89
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Petition Requesting Court Approval for
Guardian Advocate to Consent to Extraordinary Treatment
_________________________________________________________, guardian advocate appointed on
Name of Guardian Advocate
____________________
Date
for _____________________________________________________,
Name of Person.
Said person is presently:
Placed on an inpatient basis in ________________________________________________________a receiving or treatment facility in
___________________________ County and has residence in __________________________________ County, or
Involuntarily placed on an outpatient basis in ____________________County. The service provider is: ___________________________
Psychiatric or Medical Opinion Supporting the Petition
I,_________________________________, a psychiatrist or physician authorized to practice in the State of Florida,
Name of Psychiatrist or Physician
have personally examined ___________________________________________________________ on ___________________, and found
Name of Person Date
that he/she is in need of the following treatment or procedure: _____________________________________________________________
Observations which support this opinion are: ___________________________________________________________________________
This treatment or procedure is essential to the care of the person and the treatment does not present an unreasonable risk of serious,
hazardous, or irreversible side effects.
______________________________________________________________ ___________________ __________ am pm
Signature of: Psychiatrist Physician Date Time
Typed or Printed Name of Psychiatrist or Physician License Number
___________________________________________________________
Guardian Advocate’s Signature
_________________
Date
__________
Time
am pm
________________________________________________________________
Typed or Printed Name of Guardian Advocate
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian Advocate am pm
Representative am pm
Person’s Attorney am pm
Facility Administrator am pm
See s. 394.4598(6), Florida Statutes
CF-MH 3108, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 85

86 - Baker Act Forms

Baker Act Forms
________________________________________________ _______________________________________________
Page 91
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Order Authorizing Guardian Advocate to Consent to Extraordinary Treatment
This matter came to be heard on the issue of whether ____________________________________________________ guardian
Name of Guardian Advocate
advocate for the above-named person who is involuntarily placed should be given express court approval for extraordinary
treatment. Upon the evidence presented, the Court finds as follows:
1. The petitioner was appointed as the guardian advocate for the above-named person by order previously entered in this cause
after an earlier hearing.
2. The person has been represented by counsel.
3. The treatment or procedure approved herein is essential to the care of the person and the treatment does not present an
unreasonable risk of serious, hazardous, or irreversible side effects.
On the basis of these findings, it is hereby,
ORDERED
That the above-named guardian advocate for the above-named person, presently within the county, is authorized to provide
consent for:
______________________________________________________________________________________________________.
The Guardian Advocate’s appointment shall terminate upon the discharge of the person from an order for involuntary
outpatient placement or involuntary inpatient placement, or when the person is transferred
to voluntary status, or by
order of the court restoring the person’s competence.
DONE AND ORDERED this _______________ day of ___________________, _________________.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initial of Who
Provided Copy
Person am pm
Guardian Advocate am pm
Person’s Attorney am pm
Facility Administrator am pm
See s. 394.4598(6), Florida Statutes
CF-MH 3109, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 87

88 - Baker Act Forms

Baker Act Forms
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
___________________________________________________ ___________________________________
Page 93
Baker Act Forms
Restriction of Person’s Access to Own Record
________________________________________________________, served currently or in the past by this facility made a
request on ________________________________
(Date) to inspect his /her clinical record. The clinical record means all parts
of the record required to be maintained and includes all medical records, progress notes, charts, and admission and discharge
data, and all other information recorded by a facility which pertains to the person’s hospitalization and treatment. This access
was restricted in the following way: ________________________________________________________________________
The reasons for this restriction were: _______________________________________________________________________
The harm to the person as a result of such access was determined by the person’s physician to be: ______________________
This restriction will expire on ___________________
(Date) (automatically expires after 7 days but may be renewed after
review for subsequent 7 day periods).
_________________________________________________________ _________________ ____________ am pm
Signature of Person’s Physician Date Time
Typed or Printed Name License Number
This form must be completed and filed in the person’s clinical record at any time an oral or written request is made by a
person to see his/her record and the facility does not produce the requested information. Facility policies and
procedure shall govern criteria for determining what information may be harmful to persons served by the facility,
establishing a reasonable time for responding to requests for access, identifying methods of providing access that
ensure clinical support to the person while securing the integrity of the record, etc. Any renewal of the restriction of
access shall require written justification.
cc: Check when applicable and initial/date/time when copy provided:
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian am pm
Guardian Advocate am pm
Representative am pm
Attorney am pm
See s. 394.455(3), 394.4615(9), Florida Statutes
CF-MH 3110, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 89

90 - Baker Act Forms

Baker Act Forms
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
______________________________________________________________ ________________
Page 95
Baker Act Forms
Approval for Release of Person on Involuntary Status From a Receiving Facility
I approve the release of __________________________, a person brought to ___________________________________
Receiving Facility for involuntary examination pursuant to s. 394.463.
Check at least one box from each of the two categories below
I have determined that he/she does not meet the criteria for involuntary inpatient placement pursuant to 394.467 based upon one or
more of the following reasons:
Does not suffer from a mental illness, as defined in s. 394.455(18)
Has not refused placement OR is able to determine for himself or herself that placement is necessary
Is not likely to suffer from neglect posing a real and present threat of substantial harm nor is there substantial likelihood that in the
near future he/she will inflict serious bodily harm to self or others as evidenced by recent behavior causing, attempting, or
threatening such harm
There are less restrictive treatment alternatives available offering an opportunity for improvement of his/her condition. Specify:
_______________________________________________________________________________________________________.
Other. Specify ___________________________________________________________________________________________.
AND
I have further determined that he/she does NOT meet the criteria for involuntary outpatient placement pursuant
to394.4655 based upon one or more of the following reasons:
Person is under age 18;
Does not suffer from a mental illness, as defined in s. 394.455(18)
Person is likely to survive safely in the community without supervision, based on my clinical determination;
Person has no history of lacking compliance with treatment for a mental illness
Person has not within the preceding 36 months been involuntarily admitted to a Baker Act receiving or treatment facility, or
received mental health services in a forensic correctional facility or engaged in one or more acts of serious violent behavior
toward self or other, or attempts at serious bodily harm to self/others;
Person has not been found to be unlikely to voluntarily participate in recommended treatment and has not either refused voluntary
placement or been found to be unable to determine whether placement is necessary;
Person hasn’t been found, based on his/her treatment history and current behavior, to need involuntary outpatient placement to
prevent a relapse or deterioration that would be likely to result in serious bodily harm to self or others, or a substantial harm to
his/her well-being;
There has been no finding that it is likely the person will benefit from involuntary outpatient placement; or
There are available less restrictive treatment alternatives offering an opportunity for improvement of his/her condition.
Observations upon which this determination was made are: __________________________________________________
A face-to-face examination was conducted at ___________ am pm on_______________Date
by: _____________________________________________________.
Signature of Psychiatrist Clinical Psychologist Emergency Department Physician License Number
________________________________________________ __________________ ______ am pm
Typed or Printed Name of Examiner Date Time
See s. 394.455(18), 394.463(2)(f), (g), 394.467, Florida Statutes
CF-MH 3111, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 91

92 - Baker Act Forms

Baker Act Forms
Page 97Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ______________________________________ CASE NO.: _________________
Notice to Court
Request for Continuance of Involuntary Placement Hearing
____________________________________________________________ , a person awaiting a hearing on:
Involuntary Inpatient Placement, pursuant to 394.467, FS, or
Involuntary Outpatient Placement, pursuant to 394.4655, FS
at _____________________________________________________ Receiving or Treatment Facility has requested a
continuance of his/her hearing for a period of _________________________ (not to exceed a period of four weeks).
Any independent expert examination, if requested, will be completed and results provided to the undersigned attorney of
record during the period of this continuance.
__________________________________________________________ _______________ _________ am pm
Signature of Counsel Date Time
__________________________________________________________
Typed or Printed Name of Counsel
cc: Person Facility Administrator State Attorney Guardian Representative
See s. 394.467(5), Florida Statutes
CF-MH 3113, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 93

94 - Baker Act Forms

Baker Act Forms
_____________________________________________ ______________________________________________________
Page 99
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: __________________________
Order Requiring Involuntary Assessment and Stabilization
for Substance Abuse and for Baker Act Discharge of Person
THIS MATTER came to be heard pursuant to s. 394.467, F.S., on the issue of whether the above-named person should be ordered to
involuntary inpatient placement or involuntary outpatient placement, and the court having considered testimony and evidence and
having heard the argument of counsel, has concluded as follows:
1. The above-named person does not meet the criteria for involuntary inpatient placement in a treatment facility or involuntary
outpatient placement, pursuant to the provisions of Chapter 394, Florida Statutes.
2. There is a good faith reason to believe that the above-named person is substance abuse impaired, and, because of such
impairment, has lost the power of self-control with respect to substance use, and
has inflicted, or threatened or attempted to inflict, or unless admitted to involuntary treatment for substance abuse is likely
to inflict physical harm on himself or herself or another.
is in need of substance abuse services, and, by reason of substance abuse impairment, has such impaired judgment that said
person is incapable of appreciating his or her need for such services and of making a rational decision in regard thereto.
3. The above-named person should be admitted to a hospital or to a licensed detoxification facility or addictions receiving facility
for involuntary assessment and, if necessary, stabilization, pursuant to s. 394.467(6) and s. 397.6811, Florida Statutes.
4. The admission ordered herein below is the least restrictive appropriate alternative for the assessment and stabilization of the
above-named person who may be substance abuse impaired.
Whereupon, it is
ORDERED
That the above-named person shall be discharged this date from any involuntary status for a mental illness pursuant to Chapter
394, Florida Statutes.
That the above-named person shall be admitted for a period not to exceed 5 days to _________________________________
__________________________________________ for substance abuse involuntary assessment and, if necessary,
stabilization.
_________________________________________________________________ shall take the above-named person into
custody and deliver said person to the licensed service provider specified above, or, if none is specified, to the nearest
appropriate licensed service provider for involuntary assessment.
The Public Defender is discharged, and _______________________________________________________________ is
appointed counsel for all matters pursuant to s. 397, F.S.
DONE AND ORDERED in __________________ County, Florida, this ______ day of __________________, ___________.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.467(6)(c), Florida Statutes
CF-MH 3114, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 95

96 - Baker Act Forms

Baker Act Forms
________________________________ ____________________________________________________________
Page 101
Baker Act Forms
IN THE CIRCUIT COURT, _________________ JUDICIAL CIRCUIT,
IN AND FOR ____________________ COUNTY, FLORIDA
IN RE: ___________________________ Case No.: __________________________
ORDER REQUIRING EVALUATION FOR
INVOLUNTARY OUTPATIENT PLACEMENT
THIS MATTER came to be heard on ___________________________, pursuant to s. 394.467, F.S.,
on petition for involuntary inpatient placement of the above-named person and the court being advised in the
premises, finds as follows:
1. The above-named person does not meet the criteria for involuntary inpatient placement in a mental health treatment or
receiving facility.
2. The above-named person is 18 years of age or older, has a mental illness, and has a history of lack of compliance with
treatment for mental illness.
3. The above-named person is unlikely to survive safely in the community without supervision; this finding is supported
by testimony of __________________________________________________________________________ as to
his/her clinical determination.
4. The above-named person has:
A. At least twice within the preceding 36 months been involuntarily admitted to a receiving or treatment
facility as defined in s.394.455, or received mental health services in a forensic or correctional facility, or
B. Engaged in or attempted to engage in one or more acts of serious violent behavior toward self or others
within the preceding 36 months.
5. The above-named person is, as a result of mental illness, unlikely to voluntarily participate in recommended treatment
and has either refused voluntary placement for recommended treatment after sufficient and conscientious explanation
and disclosure of the purpose of placement, or is unable to determine whether placement is necessary.
6. In view of the person’s treatment history and current behavior, the person is in need of involuntary outpatient
placement in order to prevent a relapse or deterioration that would be likely to result in serious bodily harm to the
person or others, or a substantial harm to the person’s well-being through neglect or refusal to care for self as set forth
in s. 394.463(1);
7. It is likely that the person will benefit from involuntary outpatient placement. All available less restrictive alternatives
that would offer an opportunity for improvement of his or her condition are either inappropriate or unavailable.
Whereupon, IT IS ORDERED
1. That the above-named person be discharged this date from any involuntary inpatient placement and
treatment for mental illness.
2. That the above-named person shall be evaluated by __________________________________located
at ___________________________________________for involuntary outpatient placement within
_______days of the date of this hearing.
DONE AND ORDERED in Chambers at _____________ County, Florida, this __ day of _________, 20____.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.4655(6)(c), Florida Statues
CF-MH 3115, Feb 05 (Recommended Form) BAKER ACT
Baker Act Forms - 97

98 - Baker Act Forms

Baker Act Forms
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________
______________________________________________ ____________________________________________________
Page 103
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _______________________________________ CASE NO.: _______________
Findings and Recommended Order Restoring Person’s Competence
to Consent to Treatment and Discharging the Guardian Advocate
A hearing was held on _______________________, to consider the continued involuntary placement of
_______________________________________, a person placed at _______________________________________________
facility. This person was previously found incompetent to consent to treatment and ___________________________________
was appointed as guardian advocate.
Testimony and evidence was considered at this hearing regarding the person’s competence, including:
On the basis of this evidence, it is recommended that the Court restore this person’s competence to consent to treatment and that
the guardian advocate previously appointed be discharged.
_____________________________________________________ ________________ ___________ am pm
Signature of Administrative Law Judge Date Time
Typed or Printed Name of Administrative Law Judge
It is hereby ordered, that ____________________________________________________ be restored to competence to consent
to treatment and that _______________________________________________________, guardian advocate be discharged.
ORDERED this_______________ day of _____________________.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.467(7)(f), Florida Statutes
CF-MH 3116, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 99

100 - Baker Act Forms

Baker Act Forms
Page 105
Baker Act Forms
Cover Sheet to Agency for Health Care Administration
This form must be completed, attached to each of the forms listed below and sent by the receiving/treatment facility or
service provider within one working day of the person’s arrival at the facility/provider or upon the facility/provider’s receipt
of a court order for involuntary inpatient placement or involuntary outpatient placement to:
Questions about form completion and receipt may be addressed to
BA Reporting Center
or by calling 813-974-9665.
FMHI – MHC 2637
Additional information about form completion can be found at
13301 Bruce B. Downs Blvd.
Tampa, FL 33612-3807 http://bakeract.fmhi.usf.edu.
Check the box to indicate the type of form attached:
Ex-Parte Order for Involuntary Examination Involuntary Inpatient Placement Order
Report of Law Enforcement Officer Initiating Involuntary Examination Involuntary Outpatient Placement Order
Certificate of Professional Initiating Involuntary Examination Continued Involuntary Outpatient Placement Order
Identifying Information about the person (if known)
Person’s Name (Please Print):
Florida County of Residence:
Florida Zip Code of Residence:
Social Security Number: ______
Date of Birth
M
__________________________________ or State (If not FL) ____________
________ ________ ________ ________ ________ Homeless (no zip code)
______ ______ - ______ ______ - ______ ______ ______ ______
-- --
M D D Y Y Y Y
Immediately prior to this exam and/or placement, was the person in:
Yes No Answer for Adults ONLY (18 and over)
A nursing home?
An assisted living facility?
Jail (i.e., sent for examination from jail)?
Yes No Answer for Children Only (under 18)
Department of Juvenile Justice Custody?
DCF custody (such as shelter or foster care)?
Gender
Female
Male
Race
Caucasian/White
African-American/Black
Asian
Other
Hispanic
Origin?
Yes
No
School?
Name of Provider:
Address:
OR
FMHI
Assigned
Provider #
Provider Phone Number (________) __________ - ______________ ext __________
Name of Person Completing Form (Please Print):
Date Person Arrived at Facility: ____________________ Date Mailed to BA Reporting Center: _____________________
By Authority of s. 394.463, Florida Statutes
CF-MH 3118, Sept 06 (obsoletes previous editions) (Mandatory Form but name/address/phone number/FMHI number for provider may be
preprinted.)
Baker Act Forms - 101

102 - Baker Act Forms

Baker Act Forms
__________________________________________________________________ ______________________________
________________________________________________________ ___________________________________
Page 107
Baker Act Forms
Notification of a Facility’s Non-Compliance
(Pursuant to Chapter 400, F.S.)
TO: Agency for Health Care Administration FROM: ________________________________________
Consumer Assistance Unit
Name of Receiving Facility
2727 Mahan Drive, Building 3
Tallahassee, FL 32308 ________________________________________
Address of Receiving Facility
Please be advised that ____________________________________________ was received by
Name of Person
________________________________________________ on ______________________. The above-named person
Name of This Receiving Facility Date
was transported from ________________________________ located at ____________________________________
Sending Facility Sending Facility’s Address
by _________________________________________ for one of the following:
Method and Title of Transporter
Involuntary examination without the required ex parte order, professional certificate, or report of a law
enforcement officer pursuant to s.394.463 (2)(b), F.S. OR
Voluntary admission without the required assessment of the person’s ability to give express and informed
consent to treatment pursuant to s.394.4625 (1)(b), F.S.
You may contact me at this telephone number with any questions regarding the above: __________________________.
Signature of Person Completing this Form Date
Printed Name of Person Completing this Form Title
This notification shall be made by certified mail no later than the first working day after the admission of the person to the
receiving facility. A copy shall be placed in the person’s clinical record.
See s. 394.463(2)(b) 400.102(1) Florida Statutes
CF-MH 3119, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 103

104 - Baker Act Forms

Baker Act Forms
_________________________________________ _________________________________________ ________________
__________________________________________ _______________________________________ _________________
Page 109
Baker Act Forms
Certification of Guardian Advocate Training Completion
Guardian Advocate Self-Test
(Completion Required as a part of the training, before certification)
1. Briefly, what are the eight recommended steps to prepare for decision-making as a Guardian Advocate? (See Chapter 2 of
Manual)
a. _______________________________________ e. _______________________________________
b. _______________________________________ f. _______________________________________
c. _______________________________________ g. _______________________________________
d. _______________________________________ h. _______________________________________
2. Briefly, what does “Express and Informed Consent” mean? (See Chapter 4 of Manual) ____________________
__________________________________________________________________________________________
__________________________________________________________________________________________
3. Briefly, what role does “Substitute Judgment” play in the Guardian Advocate decision making process? (See Chapter 4 of
Manual)
__________________________________________________________________________________________
__________________________________________________________________________________________
4. List the three types of consent that may be authorized by the court? (See Chapter 1 of Manual)
a. _________________________ b. _________________________ c. _________________________
5. List the types of consent authorized on your order of appointment as a Guardian Advocate. (See the court order appointing
you as Guardian Advocate)
a. _________________________ b. _________________________ c. _________________________
Certification
This is to certify that I ___________________________________________________________, guardian
Name of guardian advocate
advocate appointed to represent ______________________________________ on ___________________
Name of Person Date of Appointment
by the circuit court completed the training course required by the court on __________________________.
Date training completed
The completion of training occurred prior to my providing any consent to the person’s treatment.
Printed Name of Guardian Advocate Signature of Guardian Advocate Date
Printed Name of Facility Witness Signature of Facility Witness Date
See s. 394.4598(3), Florida Statutes
CF-MH 3120, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 105

106 - Baker Act Forms

Baker Act Forms
________________________________________________________________
_________________________________________________________________ ________________________
Page 111
Baker Act Forms
Notification to Court of Person’s Competence to Consent
to Treatment and Discharge of Guardian Advocate
________________________________________________, a guardian advocate appointed by the court on
Name of guardian advocate
________________________ for ______________________________________________ who was:
Date of appointment Name of person
Court ordered for involuntary inpatient placement located at______________________________________
Name of receiving or treatment facility
OR
Court ordered for involuntary outpatient placement with services provided by:______________________________
Name of service provider
Has been discharged from his or her duties on ___________, 20____ due to the person’s regaining competence
to consent to his or her own treatment.
Printed Name of Facility Administrator/Service Provider or Designee
Signature of Facility Administrator/Service Provider or Designee Date
See s. 394.4598(6), Florida Statutes
CF-MH 3121, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 107

108 - Baker Act Forms

Baker Act Forms
___________________________________________________ __________________________________
Page 113
Baker Act Forms
Certification of Person’s Incompetence to Consent to Treatment and
Notification of Health Care Surrogate/Proxy
I have personally examined ____________________________, a person at _______________________________________
Printed Name of Person Name of Facility
I have determined that the above-named person is incompetent to consent to treatment because his or her judgment is so
affected by a mental illness that he/she lacks the capacity to make a well-reasoned, willful, and knowing decision concerning his
or her medical or mental health treatment.
A Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a Guardian Advocate will be filed
with the court within the time period required by law. Until the guardian advocate is appointed by the court, a health care
surrogate or proxy
will will not be asked to make treatment decisions for the above-named person.
If a health care surrogate or proxy is to be used, complete the following:
The person has executed an advance directive naming a surrogate to make health care decisions on his or her behalf
upon the person’s incapacity. (
Specify: _____________________________________________________________)
The person has not executed an advance directive or designated a surrogate or the surrogate named above is now
unable or unwilling to serve, but the following individual, in the following order of priority,
(Specify:
_______________________________________________) will be asked to serve as a health care proxy:
Judicially appointed guardian authorized to consent to medical treatment;
Person’s spouse;
Adult child of the person;
Parent of the person;
Adult relative of the person who has exhibited special care and concern for the person; or
Close friend of the person who has exhibited special care and concern for the person, who has presented an
affidavit to the facility that he or she is willing to assume the proxy role and has maintained such regular
contact with the person so as to be familiar with the person’s activities, health, and religious or moral beliefs.
Licensed clinical social worker selected by the provider’s bioethics committee or through an arrangement
with the bioethics committee of another provider and not employed by the provider. Documentation of efforts
to locate proxies from prior classes must be recorded in the person’s record.
Signature of Physician License Number
___________________________________________________ ________________________ ____________ am pm
Typed or Printed Name of Physician Date of Exam Time of Exam
CONTINUED OVER
Baker Act Forms - 109

___________________________________________________
__________________________________________________ __________________
Page 114
Baker Act Forms
Notification to Health Care Surrogate or Proxy (Page 2)
You, ____________________________________________________________________________________, have been
designated as the Health Care Surrogate or Proxy for __________________________________________________, a
person being served in ___________________________________________________________________________
facility. Until the court considers the facility’s Petition for Adjudication of Incompetence to Consent to Treatment and
Appointment of a Guardian Advocate for the above-named person, you have been named as the person authorized to make
treatment decisions for the person. Prior to making any treatment decisions for the person, you will:
1. Be provided the same information required by statute to be provided to a guardian advocate; and
2. Meet and talk with the person and person’s physician in person if at all possible, by telephone if not.
As a health care surrogate or proxy, you have the authority to provide informed consent only for health care decisions for
the person which you believe the person would have made under the circumstances if he or she were capable of making
such decisions. You may access appropriate clinical records, apply for public benefits, and authorize the release of
information and clinical records to appropriate persons to ensure the continuity of the person’s health care, and may
authorize the transfer of the person to or from a health care facility. You do not have the authority to consent to abortion,
sterilization, electroshock therapy, psychosurgery, experimental treatments, and can not have the person admitted to a
psychiatric facility on a voluntary basis or provide consent to treatment for a person on voluntary status.
Printed Name of the Administrator or Designee
Signature of Administrator or Designee Date
This form shall be provided to the health care surrogate or proxy, with a copy provided to the person and representative. A
copy shall be retained in the person’s clinical record.
See s. 394.455(15), 394.4598, Florida Statutes
CF-MH 3122, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
T
110 - Baker Act Forms
Baker Act Forms
See s. 394.4598 and s. 765, Part IV, Florida Statutes and s.65E-5.2301,FAC
CF-MH 3123, Feb 05 (Recommended Form) BAKER ACT
Page 115
Baker Act Forms
Affidavit of Health Care Proxy
I, _________________________________________, am willing to serve as a health care proxy for
____________________________________. I certify that I am one of the following:
Judicially appointed guardian authorized to consent to medical treatment (Appointed by the
______________Court on the following date ______________________. A copy of the court order and
letters of guardianship have been provided to the facility).
Person’s spouse;
Adult child of the person;
Parent of the person;
Adult relative of the person who has exhibited special care and concern for the person (Specify the degree of
relationship ____________________)
Close friend of the person who has exhibited special care and concern for the person, who has presented an
affidavit to the facility that he or she is willing to assume the proxy role and has maintained such regular
contact with the person so as to be familiar with the person’s activities, health, and religious or moral beliefs.
Licensed clinical social worker selected by the provider's bioethics committee or through an arrangement with
the bioethics committee of another provider and not employed by the provider. Documentation of efforts to
locate proxies from prior classes must be recorded in the person’s record.
To my knowledge, the person has not executed an advance directive designating another person as his or her health care
surrogate, or if one was previously designated, the surrogate named by the person is not able or willing at this time to
serve as the health care surrogate. If a previously designated health care surrogate is unable or unwilling to serve, please
describe the circumstances: ___________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
_____________________________________ ___________________________________
Signature of Health Care Proxy Date
________________________________________ ___________________________________
Printed Name of Health Care Proxy Signature of Witness:
BAKER ACT
Page 115
Baker Act Forms
Affidavit of Health Care Proxy
I, _________________________________________, am willing to serve as a health care proxy for
____________________________________. I certify that I am one of the following:
Judicially appointed guardian authorized to consent to medical treatment (Appointed by the
______________Court on the following date ______________________. A copy of the court order and
letters of guardianship have been provided to the facility).
Person’s spouse;
Adult child of the person;
Parent of the person;
Adult relative of the person who has exhibited special care and concern for the person (Specify the degree of
relationship ____________________)
Close friend of the person who has exhibited special care and concern for the person, who has presented an
affidavit to the facility that he or she is willing to assume the proxy role and has maintained such regular
contact with the person so as to be familiar with the person’s activities, health, and religious or moral beliefs.
Licensed clinical social worker selected by the provider's bioethics committee or through an arrangement with
the bioethics committee of another provider and not employed by the provider. Documentation of efforts to
locate proxies from prior classes must be recorded in the person’s record.
To my knowledge, the person has not executed an advance directive designating another person as his or her health care
surrogate, or if one was previously designated, the surrogate named by the person is not able or willing at this time to
serve as the health care surrogate. If a previously designated health care surrogate is unable or unwilling to serve, please
describe the circumstances: ___________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
_____________________________________ ___________________________________
Signature of Health Care Proxy Date
________________________________________ ___________________________________
Printed Name of Health Care Proxy Signature of Witness:
See s. 394.4598 and s. 765, Part IV, Florida Statutes and s.65E-5.2301,FAC
CF-MH 3123, Feb 05 (Recommended Form)
Baker Act Forms - 111

112 - Baker Act Forms

Baker Act Forms
Name: _______________________________ DATE: ____________ Facility: ______________________________
Personal Safety Plan
You can document on this form suggested calming strategies IN ADVANCE of a crisis. You can list things that are
helpful when you are under stress or are upset. You can also identify things that make you angry. Staff and
individuals receiving services can enter into a “partnership of safety” using this form as a guide to assist in your
treatment plan. The information is intended only to be helpful; it will not be used for any purpose other than to
help staff understand how to best work with you to maintain your safety or to collect data to establish trends. This
is a tool that you can add to at any time. Information should always be available from staff members for updates
or discussion. Please feel free to ask questions.
1. Calming Strategies:
It is helpful for us to be aware of things that help you feel better when you’re having a hard time. Please indicate (5)
activities that have worked for you, or that you believe would be the most helpful. If there are other things that work well
for you that we didn’t list, please add them in the box marked “Other”. We may not be able to offer all of these
alternatives, but we would like to work together with you to determine how we can best help you while you’re here.
Listen to music Exercise
Read a book Pace in the halls
Wrapping in a blanket Have a hug with my consent
Write in a journal Drink a beverage
Watch TV Dark room (dimmed lights)
Talk to staff Medication
Talk with peers on the unit Read religious or spiritual material
Call a friend or family member Write a letter
Voluntary time in the quiet room/comfort room Hug a stuffed animal
Take a shower Do artwork (painting, drawing)
Go for a walk with staff Other? (Please list below)
2. What are some of the things that make you angry, very upset or cause you to go into crisis? What are your
“triggers”?
Being touched Called names or made fun of
Security in uniform Being forced to do something
Yelling Physical force
Loud Noise Being isolated
Contact with person who is upsetting Some else lying about my behavior
Being restrained Being threatened
3. Signals of Distress:
Please describe your warning signals, for example, what you know about yourself, and what other people may notice
when you begin to lose control. Check those things that most describe you when you’re getting upset. This information
will be helpful so that together we can create new ways of coping with anger and stress:
Sweating Clenching teeth
Crying Not taking care of self
Breathing hard Running
Yelling Clenching fists
Hurting others: Swearing
Throwing Objects Not eating
Pacing Being rude
Injuring self: (Please be specific) Other? (Please list below)
CONTINUED OVER
Baker Act Forms
Page 117
Baker Act Forms - 113

________________________________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
Page 118
Baker Act Forms
Personal Safety Plan (page 2)
4. Preferences Regarding Gender and Others:
Do you have any preferences or concerns regarding who serves you when you are upset or angry?
Women staff_________ Men staff_____________ No preference_________ Language______________________
Ethnicity________________________ Culture ____________________ Of a particular religion________________
5. Preferences Regarding Physical Contact:
We would like to know about your preferences regarding physical contact. For example, you may not like to be touched
at all or you may find it helpful to have a hug or be touched appropriately when you are upset.
Do you find it helpful to be hugged or touched appropriately when you are upset?
Yes___ No___ Comments:___________________________________________________
6. Seclusion and Restraint:
This facility is trying to eliminate the use of seclusion and restraints, therefore, it would be helpful to know if you have
ever been placed in a seclusion room or been restrained. This information will be used only for collecting data and for
training purposes, not to predict any future behaviors.
Have you ever been placed in a seclusion room? Yes ____ No ____
Have you ever been restrained? Yes ____ No ____
7. In Extreme Emergencies:
In extreme emergencies seclusion and restraint may be used as a last resort. Is there anything you find helpful in
emergency situations that could prevent them from being used?
Alternative physical spaces such as:
Comfort Room _____ Quiet Room_____
Other such as exercise _____ Medication by mouth________
Emergency injection_______ Other:__________________________________________________
8. Medical Conditions:
Do you have any physical conditions, disabilities, or medical problems such as asthma, high blood pressure, back
problems, etc., that we should be aware of when caring for you during an emergency situation?
9. Helpful Medications:
We may be required to give medications if other measures do not help you to calm down. In this case, we would like to
know what medications have been especially helpful to you? Please describe. _________________________
10. Not Helpful Medications:
Are there any medications that are not helpful? What and why? _____________________________________
CONTINUED
114 - Baker Act Forms

Baker Act Forms
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Page 119
Baker Act Forms
Personal Safety Plan (page 3)
11. Room Checks:
Room checks are done at night to make sure you are okay. In order to make room checks as non-intrusive as possible is
there anything that would make room checks more comfortable for you? ____________________________
12. Trauma History:
Do you have any issues regarding abuse such as sexual or physical abuse that you would like to talk about with staff, or
with counselor? Yes___ No___
Would you like more information on these issues in classes or support groups? Yes____ No____
13. Anything Else?
Is there anything else that would make your stay easier and more comfortable? For example do you have any special
issues like cultural, diet, sexual preference, appearance, etc. that you think could contribute to misunderstandings or cause
problems for you? Please describe:
The Personal Safety Form Information should be presented to the treatment team and incorporated
into the treatment plan for this individual. Each individual shall receive a copy. This form has been
adapted from an original form created by the Massachusetts Department of Mental Health
See s. 394.453, and 394.459(4) Florida Statutes
CF-MH 3124, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 115

116 - Baker Act Forms

Baker Act Forms
Page 121
Baker Act Forms
Application for Designation as a Receiving Facility
Name of Applicant Facility: ___________________________________________________________________
Street Address: ______________________________________________________________________________
City: ____________________________________ , FL Zip Code: _____________ - _____________________
Telephone Number: (
)_________________________________
Administrator: ______________________________________________________________________________
Provide complete responses to the following questions and issues, attaching additional sheets where necessary.
1. Designation requested for:
All populations
Adults Only – Approved Transportation Exception Plan attached
Minors Only – Approved Transportation Exception Plan attached
2. The following are the street addresses for each location at which persons will be received or treated for involuntary
examination. Each will operate 24 hours / 7 day a week emergency services and psychiatric licensed beds.
Name of Facility Street Address City Zip Code
3. Psychiatric services, including any distinct programs to be provided to each of the following consumer groups, and the
projected numbers of persons to be served in each group are as follows:
Psychiatric Services Distinct Programs Projected
Number
Minors below
10 years of age
Minors between the ages
of 10 to 17 years
Adults
Persons 60 or more years
of age
Other specialty groups
CONTINUED OVER
Baker Act Forms - 117

Page 122
Baker Act Forms
Application For Designation as a Receiving Facility (Page 2)
4. The community need for maintaining or expanding the present level of service to meet the existing need, and why this
applicant is best suited for this purpose. Included is information about the public’s need for specialty services to
specific age or disability groups. Evidence of such need may include certificate of need data and other information
published by the Agency for Health Care Administration, the organization’s or community’s utilization of available or
licensed psychiatric bed capacity, geographic accessibility information, input from local governmental agencies.
(Attach response on separate sheet(s).)
5. The facility’s compliance program, including key facility protocols which will be used to assure all involved
practitioners and staff are knowledgeable of, and implement legal rights of persons served by the facilities and
providers, key psychiatric care, records standards, complaint reporting, and investigation and reviews, to maintain a
consistently high level of compliance with applicable Baker Act laws, ethical principles, and rights protections are as
follows: (Attach response on separate sheet(s).)
6. The facility’s complaint and grievance system, including any mandatory time frames is as follows. Attach pamphlet
used by the facility to educate persons served by the facility and family members about this system. (Attach response
on separate sheet(s).)
7. Protocols to prevent the organization, its staff, its contractors, and its privileged professionals from economic
exploitation of, trafficking persons among facilities for economic purposes or similar activities prohibited by s.
817.505, F.S., and related statutes are as follows: (Attach response on separate sheet(s).)
8. Frequent, if not daily opportunity for persons to receive exercise, fresh air and sunshine, except as individually
restricted and documented in the person’s record and within the physical limitations of the facility are assured by the
following: (Attach response on separate sheet(s).)
9. The means utilized to create a low stimulation or separate psychiatric emergency reception and triage area that
minimizes individual’s exposure to undue and exacerbating environmental stresses while awaiting or receiving
services is as follows (general hospitals only): (Attach response on separate sheet(s).)
10. Continuing aftercare or post discharge psychiatric care services provided at the receiving facility other than referral or
transfer are as follows: (Attach response on separate sheet(s).)
11. The facility’s discharge planning policies provide for continuity of medication availability until post-discharge
follow-up services are scheduled are as follows. (Attach response on separate sheet(s).)
CONTINUED
118 - Baker Act Forms

Baker Act Forms
Page 123
Baker Act Forms
Application For Designation as a Receiving Facility (Page 3)
Certifications:
Submission of this application constitutes authorization by the applicant and release for the Department of Children and
Families, to make inquiries and obtain information about the conduct of the applicant, its key employees and contractors,
and it’s psychiatric services management company, to verify the representations and information provided in this
application. Application for designation as a receiving facility is agreement to abide by all statutes and rules governing
the Baker Act and related laws.
I certify that the above information and information on the attachments is correct:
Signed for the Facility ____________________________________________ Date __________________
Typed Name: __________________________________ Title: ____________________________________
Attachments:
1. A copy of the facility’s license issued pursuant to chapter 394 or 395, F.S., evidencing its eligibility to apply
for designation.
2. A copy of the most recent state monitoring or licensing survey report.
3. Copy of the most recent survey report of the organization by the Joint Commission for the Accreditation of
Healthcare Organizations (JCAHO) or, if not JCAHO accredited, by another national accrediting body.
4. A current Certificate of Good Standing for the applicant organization issued by the Florida Secretary of
State.
5. Documentation of the applicant’s governing authority, authorizing the application for designation.
By Authority of s. 394.461, Florida Statutes
CF-MH 3125, Feb 05 (obsoletes previous editions) (Mandatory Form) BAKER ACT
Baker Act Forms - 119

120 - Baker Act Forms

Baker Act Forms
___________________________ _____________________________ ___________________________
Page 125
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Petition for Involuntary Outpatient Placement
COMES NOW the Petitioner, ________________________________________________________ , and alleges:
1. That Petitioner is Administrator of:____________________________________________________________________
Name of Receiving or Treatment Facility Facility Address
2. That __________________________ , is served in said receiving or treatment facility and has been examined at such facility
3. The person’s social security number is_____________________________ and date of birth is:________________________
4. That this petition is being filed within the following time frames: (Check one below)
A. This person was admitted for involuntary examination and this petition is being filed within the 72-hour
examination period, or if the examination period ends on a weekend or legal holiday, on the next court working
day OR
B. This person was transferred to involuntary status after examination or after refusing/revoking consent to
treatment or requesting discharge from the facility and this petition is filed within two court working days.
C. This person is currently on an order for involuntary inpatient placement, and this petition is being filed before the
expiration of that order
D. A petition for involuntary inpatient placement has been filed and a hearing is pending.
5. That attached hereto and by reference made a part hereof, are two (2) opinions and supporting facts regarding the mental
health of said person necessitating involuntary outpatient placement.
6. In addition to at least one of the two experts whose opinions are attached, the following persons may testify in support of the
petition for involuntary outpatient placement:
Guardian or Representative Other Witness Other Witness
Name: ___________________________ _____________________________ ___________________________
Relationship ___________________________ _____________________________ ___________________________
Address ___________________________ _____________________________ ___________________________
Telephone: (______)___________________ (______)______________________ (______)____________________
CONTINUED OVER
Baker Act Forms - 121

______________________________________________
Page 126
Baker Act Forms
Petition for Involuntary Outpatient Placement (Page 2)
COMES NOW THE PETITIONER and further alleges that:
1. A Guardian Advocate is necessary to act on the person’s behalf on issues related to express and informed consent to:
Mental health treatment only, or
Both mental health and medical treatment decisions
And a Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a Guardian Advocate is attached;
OR
2. The person/respondent is competent to provide express and informed consent to his or her own treatment or the person
has a guardian authorized to consent to treatment and no Guardian Advocate is requested.
________________________________________ _______________________ ____________ am pm
Signature of Facility Administrator or Designee Date Time
Typed or Printed Name of Administrator or Designee
Person
does or does not have a private attorney. If so, the name and address of the private attorney is:
Private Attorney Name: ______________________________________________________________________________
Private Attorney Address: ____________________________________________________________________________
cc: The Clerk of the Court shall provide a copy of this petition to the: (Check when applicable and initial/date/time when
copy provided)
Individual Date Copy Provided Time Copy Provided Initials of Who
Provided Copy
Person am pm
Guardian am pm
Public Defender am pm
Representative am pm
State Attorney am pm
Dept. of Children & Families am pm
CONTINUED / SUPPORTING OPINIONS ON PAGE 3
122 - Baker Act Forms

Baker Act Forms
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________ __________________________________
Page 127
Baker Act Forms
Petition for Involuntary Outpatient Placement (Page 3)
First Opinion Supporting the Petition
I, _______________________________ a psychiatrist authorized to practice in the State of Florida, have personally examined
__________________________________ on _________________ (within 72 hours of the signing hereof) and find from such
Name of Person Date
examination that the person meets each of the following criteria for involuntary outpatient placement. Each of the following required
criterion must be alleged and substantiated by evidence in this petition.
1. The person is 18 years of age or older, corroborated by: ________________________________________________________________
1. The person has a mental illness, as substantiated by the following evidence:________________________________________________
2. The person is unlikely to survive safely in the community without supervision, based on a clinical determination, as substantiated by the
following evidence: _____________________________________________________________________________________________
4. The person has a history of lack of compliance with treatment for a mental illness, as substantiated by the following evidence: _______
5. The person has:
a. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving or treatment facility as
defined in s. 394.455, or has received mental health services in a forensic or correctional facility. The 36-month period does not
include any period during which the person was admitted or incarcerated, as substantiated by the following evidence: __________
or
b. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm to himself or herself
or others, within the preceding 36 months, as substantiated by the following evidence : ____________________________________
6. The person is, as a result of a mental illness, unlikely to voluntarily participate in the recommended treatment plan and either he or she
has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the purpose of placement for
treatment or he or she is unable to determine for himself or herself whether placement is necessary, as substantiated by the following
evidence:_________________________________________________________________________________________________________
7. In view of the person's treatment history and current behavior, the person is in need of involuntary outpatient placement in order to
prevent a relapse or deterioration that would be likely to result in serious bodily harm to himself or herself or others, or a substantial harm to
his or her well-being as set forth in the criteria for involuntary examination, as substantiated by the following evidence:_________________
8. It is likely that the person will benefit from involuntary outpatient placement, as substantiated by the following evidence;____________
AND
9. All available less restrictive treatment alternatives than court-ordered involuntary outpatient placement which would offer an
opportunity for improvement of said person's condition have been judged to be inappropriate, based on contact with the following
programs/agencies: _________________________________________________________________________________________________
_________________________________________________ ________________ ____________ am pm
Signature of Psychiatrist Date Time
Typed or Printed Name of Psychiatrist License Number
CONTINUED OVER
Baker Act Forms - 123

________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________ ________________________ ______________
______________________________________________________________ _________________________________
Page 128
Baker Act Forms
Second Opinion Supporting the Petition (page 4)
I,____________________________________________, a psychiatrist, clinical psychologist, licensed physician *,
psychiatric nurse *, authorized to provide a second opinion on this petition pursuant to Section 394.467 (2), F.S., have personally examined
________________________________________________ on______________________________, (within 72 hours of signing hereof), and find
Name of Person Date
that he/she meets the criteria for involuntary outpatient placement as stated in this petition. Observations and supporting evidence which support this
opinion are: _____________________________________________________________________________________________________________
_________________________________________ ___________________ ___________ am pm
Signature of Examiner Date Time
Typed or Printed Name of Examiner Profession License Number
*I certify that the county in which the person is detained has less than 50,000 population and no psychiatrist or psychologist is available to provide
the second opinion.
Printed Name and Signature of Administrator or Designee Date
* A licensed physician or psychiatric nurse may only provide such second opinion in counties of less than 50,000
population in cases where the facility administrator certifies that no psychiatrist or clinical psychologist is available to
provide the second opinion (by countersigning above).
See s. 394.4599(2)(c)3, 394.467, Florida Statutes BAKER ACT
CF-MH 3130, Feb 05 (Recommended Form)
124 - Baker Act Forms

Baker Act Forms
Page 129
Baker Act Forms
Designation of Service Provider for Involuntary Outpatient Placement
Pursuant to chapter 394.4655, Florida Statutes, a petition for Involuntary Outpatient Placement has been filed to require
_____________________________________ to comply with a treatment plan approved by the court.
The following service provider has been identified by:
___________________________________________, a representative of the Department of Children and Families, or
____________________________________________, a representative of a designated receiving facility
Name of Assigned Service Provider:
Address of Provider:
Phone Number of Provider:
The service provider will have primary responsibility for service provision under an order for involuntary outpatient placement. The service provider
will prepare a written proposed treatment plan, in consultation with the person or the person’s guardian, guardian advocate, or health care
surrogate/proxy, if appointed, to be attached to the petition for involuntary outpatient placement for the court’s consideration for inclusion in the
involuntary outpatient placement order. The Baker Act requires that each person shall have an opportunity to assist in preparing and reviewing such
a plan prior to its implementation and that the plan shall include a space for the person’s comments.
For purpose of determining whether a person meets the criteria for involuntary outpatient placement or for preparing the proposed treatment plan,
the clinical record may be released to the state attorney, the person’s attorney, and to the appropriate mental health professionals, including the
proposed service provider, in accordance with federal and state law.
The treatment plan must specify the nature and extent of the person's mental illness. The treatment plan must also address the reduction of
symptoms that necessitate involuntary outpatient placement and include measurable goals and objectives for the services and treatment that will be
provided to treat the person's mental illness and to assist the person in living and functioning in the community or to attempt to prevent a relapse or
deterioration.
Service providers may select and provide supervision to other individuals to implement specific aspects of the treatment plan. The services in the
treatment plan must be deemed to be clinically appropriate by a physician, clinical psychologist, psychiatric nurse, mental health counselor, marriage
and family therapist, or clinical social worker, as defined in s. 394.455, Florida Statutes, who consults with, or is employed or contracted by, the
service provider.
The service provider must certify to the court in the proposed treatment plan whether sufficient services for improvement and stabilization are
currently available in the local community, whether there is space available to serve this person, that funding is available to finance the care, and
whether the service provider agrees to provide those services. If the service provider certifies that the services or funding required by the proposed
treatment plan are not available, the petitioner may not file the petition.
A petition for Involuntary Outpatient Placement will be filed with the circuit court no later than ___________________________. A copy of the
proposed treatment plan developed by the assigned service provider, in consultation with the person, must be attached, including a certification by
the service provider that the proposed services and funding are available to support the proposed treatment/service plan. The service provider shall
also provide a copy of the of the proposed treatment plan to the person and the administrator of the receiving facility.
The service provider identified above shall prepare a treatment plan, consistent with the above requirements, no later than ___________________to
be attached to the petition for involuntary outpatient placement, unless the service provider cannot certify the availability of funded services to meet
the person’s needs.
_________________________________________________ _________________________
Signature of
DCF Receiving Facility representative Date
__________________________________________________ _______________________________________________________
Printed Name of Representative Address and Telephone Number of Representative
See s. 394.4655(2)(a), Florida Statutes
CF-MH 3140, Sept 06 (obsoletes previous edition) (Recommended Form)
Baker Act Forms - 125

126 - Baker Act Forms

Baker Act Forms
Page 131
Baker Act Forms
Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient Placement
Pursuant to chapter 394.4655, Florida Statutes, a petition for Involuntary Outpatient Placement has been filed to require
____________________________________________________ to comply with a treatment plan approved by the court.
The following proposed treatment plan has been developed in consultation with the above named person (or his/her
legally authorized substitute decision-maker, if appointed) for the court’s consideration by the following service provider
designated by
the Department of Children and Families or a designated receiving facility.
Name of Assigned Service Provider:____________________________________________________________________
Name & Credentials of Person Developing the Treatment Plan:_______________________________________________
Address:__________________________________________________________________________________________
Phone Number_____________________________________________________________________________________
The nature and extent of the person's mental illness is as follows:
The following specific services are proposed in this treatment plan, including the specific service to be provided,
the organization to provide each service, the licensure or other credentials of the organization or professional to
provide each service, and the frequency and duration of each service:
1. Services that will reduce symptoms that necessitate involuntary outpatient placement, including measurable goals and
objectives for the services and treatment that will be provided to treat the person's mental illness:
2. Services that will reduce symptoms, including measurable goals and objectives for the services and treatment, that are
provided to assist the person in living and functioning in the community.
3. Services that will reduce symptoms, including measurable goals and objectives, for the services and treatment that are
provided to attempt to prevent a relapse or deterioration:
Service providers may select and provide supervision to other individuals to implement specific aspects of the treatment
plan. Other individuals than those employed by the above named service provider, and their credentials, who are
expected to assist in providing the services described in this proposed treatment plan are:
CONTINUED OVER
Baker Act Forms - 127

___________________________________ ______________________________ ________________
________________________________ ______________________________ ____________
Page 132
Baker Act Forms
Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient Placement (page 2)
I am a
physician, clinical psychologist, psychiatric nurse, mental health counselor, marriage and family
therapist, or clinical social worker, as defined in s. 394.455, F.S. I consult with, or am employed or contracted by, the
service provider and I have determined that the services, personnel, and organizations described in this proposed
treatment plan are clinically appropriate.
Signature of Clinical Professional Printed Name of Clinical Professional Date
The service provider certifies to the court that all services described in the proposed treatment plan for person’s
improvement and stabilization are:
Currently available in the local community There is space available to serve this person
Funding is available to finance the care, and The service provider agrees to provide those services.
The nature and extent of the person’s involvement in the preparation of this proposed treatment plan is as follows:
Comments about the proposed treatment plan by the person are as follows:
Signature of Preparer of Plan Printed Name of Preparer of Plan Date
The service provider shall also provide a copy of the proposed treatment plan to the person and the administrator of the
receiving facility. For persons in state treatment facilities who are ordered to involuntary outpatient treatment, a copy of
the state mental health discharge form must be sent by the treatment facility to a department representative in the county
where the person will be residing, which is the county where the petition must be filed.
See s. 394.467(6)(c), Florida Statutes
CF-MH 3145, Sept 06 (obsoletes previous edition) (Recommended Form) BAKER ACT
128 - Baker Act Forms
Baker Act Forms
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
_______________________________________ ___________________________________________
_______________________________________ ___________________________________________
Page 133
Baker Act Forms
Notice to Department of Children and Families of
Non-Filing of Petition for Involuntary Outpatient Placement Or Diminished Treatment Plan
Due to Non-Availability of Services or Funding
I have evaluated _____________________________Social Security #________________________ a person referred for:
Involuntary Outpatient Placement
Continued Involuntary Outpatient Placement
I have found that services needed by the person are:
Unavailable in the community
Unavailable due to waitlists
Unfunded
As a result of this finding,
No petition for involuntary outpatient placement or continued involuntary outplacement was filed or
A petition for involuntary outpatient or continued involuntary outplacement was filed but omitted services
that were unavailable or unfunded.
Please check which of the following services are needed by the person but are unavailable for any of the above reasons:
Residential Treatment
Vocational Program
Psychotropic Medications
Drop-In Center
Counseling Peer Support Services
Club House Others as specified below
FACT or Intensive Case Management
The nature of the service unavailability or lack of funding is described as follows:
Signature of Service Provider Representative Printed Name of Representative Date
Name of Service Provider Address of Service Provider Telephone
See s. 394.4655(2)(a)3, Florida Statutes
CF-MH 3150, Feb 05 (Recommended Form)
BAKER ACT
Baker Act Forms - 129

130 - Baker Act Forms

Baker Act Forms
_________________________________ __________________________________________
Page 135
Baker Act Forms
IN THE CIRCUIT COURT OF THE ________________ JUDICIAL
CIRCUIT, IN AND FOR ____________________ COUNTY, FLORIDA
IN RE: _________________________, Case No.: _____________________
ORDER FOR INVOLUNTARY OUTPATIENT PLACEMENT
OR CONTINUED INVOLUNTARY OUTPATIENT PLACEMENT
This matter came to be heard pursuant to s.394.4655, F.S., and on Petition for Involuntary Outpatient Placement or,
Petition for Continued Involuntary Outpatient Placement, and the Court being fully advised in the premises, finds by clear
and convincing evidence as follows:
1. The above-named person has been represented by counsel; said person
appeared at the hearing, or
presence at the hearing was waived, without objection of said person’s counsel.
2. The above-named person meets the following criteria for involuntary outpatient placement pursuant to s.394.4655(1), F.S.:
the person is 18 years of age or older; has a mental illness; is unlikely to survive safely in the community without
supervision, based on a clinical determination; and, has a history of lack of compliance with treatment for a mental illness.
3. The above-named person has: (not applicable to
continued involuntary outpatient placement)
A. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving or treatment
facility as defined in s.394.455, or has received mental health services in a forensic or correctional facility; or
B. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm to
self or others, within the preceding 36 months.
4. The above-named person is, as result of mental illness, unlikely to voluntarily participate in the recommended treatment
plan and has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the
purpose of placement for treatment, or is unable to determine whether placement is necessary.
5. The above-named person’s treatment history and current behavior mandates the conclusion that the person is in need of
involuntary outpatient placement in order to prevent a relapse or deterioration that would be likely to result in serious
bodily harm to the person or others, or a substantial harm to his or her well-being through neglect or refusal to care for self
as set forth in s.394.463 (1), F.S..
6. It is likely that the above-named person will benefit from involuntary outpatient placement. All available less restrictive
treatment alternatives which would offer an opportunity for improvement of said person’s condition are inappropriate.
7. The treatment plan which is attached hereto specifies the nature and extent of the above-named person’s mental illness and
specifies the outpatient treatment to be provided. The treatment plan contains a certification to the court that sufficient
services for improvement and stabilization are currently available, funded, and that the service provider agrees to provide
those services.
8. The services described in the treatment plan are clinically appropriate. This finding is supported by evidence presented,
including the testimony of ___________________________________________________________.
9. The Court considered testimony and evidence regarding the above-named person’s competence to consent to treatment.
The person is found to be
competent, incompetent to consent to treatment. If found to be incompetent, a guardian
advocate is appointed by separate order.
10. If the petition was referred to and heard by a Magistrate, the Magistrate’s Report and Recommendation are attached,
incorporated by reference, and adopted by the Court.
Whereupon, IT IS ORDERED that the above-named person be treated as an outpatient in accordance with the treatment
plan attached hereto, for a period
not to exceed 6 months from the date of this order, or
______________________________, or until discharged by the administrator or transferred to voluntary status.
DONE AND ORDERED in __________________ County, Florida, this _____ day of ______________, 20___.
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.4655(6)(c), Florida Statues
CF-MH 3155, Feb 05 (Recommended Form)
BAKER ACT
Baker Act Forms - 131

132 - Baker Act Forms

Baker Act Forms
______________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________
____________________________________ _______________________________________________ ________________
___________________________________________________________________________________________________
___________________________________________ __________________________________
Page 137
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Notice to Court of Modification to Treatment Plan for
Involuntary Outpatient Placement and/or
Petition Requesting Approval of Material Modifications to Plan
This court issued an order on _______________ requiring :
involuntary outpatient placement OR continued involuntary outpatient placement for the above-named person.
Material modifications to the treatment plan previously approved by the Court
For which the person or the person’s guardian or guardian advocate, if appointed AGREE have been made.
For which the person or the person’s guardian or guardian advocate, if appointed DO NOT AGREE are being proposed for the court’s
consideration.
A hearing is requested to review the proposed changes for which the person or the person’s guardian or guardian
advocate, if appointed, do not agree and the reasons for the objections to the proposed changes.
The changes or proposed changes to the currently approved treatment plan, including why the modifications are necessary
and appropriate, are as follows:
_______________________________________________________________________________________
Any objections to the changes or proposed changes to the currently approved treatment plan by the person or the person’s
guardian or guardian advocate, if appointed, are as follows: __________________________________________________
If this petition is filed by the service provider, a copy of the complete treatment plan, including proposed changes, is attached to this filing.
Signature of Petitioner Printed Name of Petitioner Date
Person Guardian Guardian Advocate Service Provider Attorney for Person
Printed Name of Petitioner Printed Address and Telephone Number of Petitioner
ORDERED
That the proposed changes to the currently approved treatment plan are:
Approved
Disapproved
DONE AND ORDERED in __________________ County, Florida, this _____date of __________, 20____
Signature of Circuit Court Judge Printed Name of Circuit Court Judge
Pursuant to 394.4655(6)(b)3, Florida Statutes,
See s. 394.467(6)(c), Florida Statutes
CF-MH 3160, Feb 05 (Recommended Form)
BAKER ACT
Baker Act Forms - 133

134 - Baker Act Forms

Baker Act Forms
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________________
____________________________________ ____________________________________
Page 139
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Page 140
Baker Act Forms
Petition for Termination of Involuntary Outpatient Placement Order
COMES NOW the petitioner, ____________________________________ alleging that ______________________
No longer meets one or more of the following criteria for involuntary outpatient placement:
The person is 18 years of age or older;
The person has a mental illness;
The person is unlikely to survive safely in the community without supervision, based on a clinical determination;
The person has a history of lack of compliance with treatment for a mental illness;
The person has:
1. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving or treatment facility as defined
in s. 394.455, or has received mental health services in a forensic or correctional facility. The 36-month period does not include any
period during which the person was admitted or incarcerated; or
2. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm to himself or herself
or others, within the preceding 36 months;
The person is, as a result of a mental illness, unlikely to voluntarily participate in the recommended treatment plan and either he or she
has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the purpose of placement
for treatment or he or she is unable to determine for himself or herself whether placement is necessary;
In view of the person's treatment history and current behavior, the person is in need of involuntary outpatient placement in order to
prevent a relapse or deterioration that would be likely to result in serious bodily harm to himself or herself or others, or a substantial
harm to his or her well-being as set forth in s.
394.463(1);
It is likely that the person will benefit from involuntary outpatient placement; and
All available less restrictive treatment alternatives which would offer an opportunity for improvement of said person's condition have
been judged to be inappropriate based on contact with the following programs/agencies:
For each criteria checked above that the petition alleges is not currently met, substantiating evidence is provided as follows:
Wherefore, it is requested that the Court issue an order terminating its order issued on ______________________
requiring involuntary outpatient placement.
____________________________________ _________________ _____am pm
Signature of Petitioner Date Time
Person Guardian Guardian Advocate Service Provider Attorney for Person
Printed or Typed Name of Petitioner Address of Petitioner
See s. 394.467(6)(c), Florida Statutes
CF-MH 3170, Feb 05 (Recommended Form) BAKER ACT
Baker Act Forms - 135

136 - Baker Act Forms

Baker Act Forms
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
Page 141
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Petition Requesting Authorization for
Continued Involuntary Outpatient Placement
COMES NOW the Petitioner, __________________________ and alleges:
1. That Petitioner is Administrator of: _____________________________________________________________________
Name of Service Provider Address
2. That (Name of Person): ____________________________ has been served by said service provider under an order for
Involuntary Outpatient Placement entered by this Court on ____________________,
3. That according to the provisions of s.394.4655(7), F.S. this person may not be involuntarily placed after
__________________________(Date) without an order authorizing continued involuntary outpatient placement
4. That this petition is being filed within the allowed time frame
5. That the person continues to meet the criteria for involuntary outpatient placement pursuant to s. 394.4655(1), F.S., as follows:
a.. The person is 18 years of age or older;
b. The person has a mental illness
c. The person is unlikely to survive safely in the community without supervision, based on a clinical determination, as
substantiated by the following evidence:_______________________________________________________________________
d. The person has a history of lack of compliance with treatment for a mental illness.
e. The person is, as a result of a mental illness, unlikely to voluntarily participate in the recommended treatment plan and either he
or she has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of the purpose
of placement for treatment or he or she is unable to determine for himself or herself whether placement is necessary, as
substantiated by the following evidence: ______________________________________________________________________
Continued (Over)
Baker Act Forms - 137

________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
_________________________________________________ __________________________________
________________________________________
Page 142
Baker Act Forms
f. In view of the person's treatment history and current behavior, the person is in need of involuntary outpatient placement in order
to prevent a relapse or deterioration that would be likely to result in serious bodily harm to himself or herself or others, or a
substantial harm to his or her well-being as set forth in s.
394.463(1), as substantiated by the following evidence:
g. It is likely that the person will benefit from involuntary outpatient placement, as substantiated by the following evidence;
AND
h. All available less restrictive treatment alternatives than court-ordered involuntary outpatient placement which would offer an
opportunity for improvement of said person's condition have been judged to be inappropriate, based on contact with the following
programs/agencies: ______________________________________________________________________________________
_________________________________________________ ________________ ____________ am pm
Signature of Physician or Clinical Psychologist Date Time
Typed or Printed Name of Physician or Clinical Psychologist License Number
A description of the person’s treatment during the time he or she was involuntarily placed on an outpatient basis is attached to this
petition, as is a proposed individualized plan of continued treatment, that has been developed in consultation with the person or the
person’s guardian or guardian advocate, if appointed.
Wherefore, it is requested that an Order be issued authorizing this service provider to continue to treat this person on an involuntary
outpatient basis until __________________ or for a period not to exceed six (6) months.
___________________________________ _______________ ________am pm
Signature of Administrator or Designee Date Time
Printed or Typed Name of Administrator or Designee
See s. 394.467(6)(c), Florida Statutes
CF-MH 3180, Feb 05 (Recommended Form) BAKER ACT
T
138 - Baker Act Forms

Baker Act Forms
_________________________________________ ______________________
________________________________________ ______________________ _________________
Page 143
Baker Act Forms
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Notice to Court of Waiver of Continued Involuntary Outpatient Placement Hearing
And Request for an Order
________________________________, a person being treated under an Order for Involuntary Outpatient Placement by
__________________________________ (service provider) and who has been found by the court to be competent to
consent to make decisions about his or her treatment, has agreed to a period of continued involuntary outpatient placement
without a court hearing.
As counsel for this person, I agree to this waiver of hearing and request the issuance of an order for continued involuntary
outpatient placement for a period of _____________________________________(up to six months)
Signature of Person Agreeing to Waiver of Hearing Date of Person’s Signature
Signature of Counsel Printed Name of Counsel Date
cc:
Person Service Provider State Attorney Guardian Guardian Advocate Representative
See s. 394.4655(7)(d), Florida Statutes
CF-MH 3185, Feb 05 (Recommended Form) BAKER ACT
Baker Act Forms - 139

140 - Baker Act Forms

Baker Act Forms
Page 145
Baker Act Forms
Florida Department of Children & Families
State Mental Health Facility Admission Form
(Submit Prior to Pre-Admission Meeting)
A. Client Identifying Information
1. Name ____________________________________________________________________________________________________________
Last Maiden First M.I.
2. Discharge Address __________________________________________________________________________________________________
3. County of Residence/Referral __________________/___________________ 4. Last Living Environment ______________________
5. Date of Birth ______/ ______ / __________ 6. SSN __________ - ________ - ___________
7. Age _______ yrs. 8. Sex M F 9. Race ___________________ 10. Religion __________________________
11. Birthplace _____________________________ 12. USA Citizen? Yes No 13. Language _______________________________
14. Immigration Status _____________________________________ 15. Country ________________________________________________
16. Marital Status (check one): Single Married Divorced Widow(er) Separated
B. Client Status Information
17. Legal Status (check one) Voluntary Involuntary
18. Competency Status (check one) Competent Incompetent Not Guilty by Reason by Insanity Incompetent to Proceed
19. Date Competency Hearing Held _______/________/__________ 20. Hearing Site ____________________________________________
21. Has legal guardian been appointed? YES NO (If yes, complete following)
Legal Guardian for client only client’s property only both client and property
Guardian’s Name ___________________________________________________________ Phone # (_____) ________________________
Guardian’s Mailing Address _________________________________________________________________________________________
Guardian Advocate’s Name ___________________________________________________ Phone # (_____) ________________________
Guardian Advocate’s Mailing Address _________________________________________________________________________________
22. Name of Designated Representative (if any) _________________________________________ Phone # (_____) _____________________
23. Should anyone else be contacted in an emergency? YES NO If yes, relationship to client _________________________________
Name ____________________________________________________________________ Phone # (_____) _________________________
Mailing Address ___________________________________________________________________________________________________
24. If Charges Pending Specify __________________________________________________________________________________________
Criminal Statute Number ___________________ Name of Court ____________________________ Case Number ___________________
Judge’s Name ____________________________________ Probation Officer: ________________________________________________
Probation Officer Mailing Address _____________________________________________________________________________________
Probation Officer Phone # (______) ______________________
CONTINUED OVER
Baker Act Forms - 141

Page 146
Baker Act Forms
State Mental Health Facility Admission Form (Page 2)
C. Transferring or Screening Agency Identifying Information
25. Name of Agency _________________________________________________________________________________
26. Agency Contact (Continuity of Care Case Manager) __________________________ Phone # (_____) _____________
27. Mailing Address __________________________________________________________________________________
28. Date Case Manager Notified (mm/dd/yyyy) ___________/____________/____________
D. Client Medical Information / History
29. Current Diagnoses (Current edition of DSM and ICD for Axis III): _________________________________________________
Treating Psychiatrist: __________________________________ Treating Physician: __________________________________
AXIS I: _____________________________________________________________________________________
AXIS II: ____________________________________________________________________________________
AXIS III: ___________________________________________________________________________________
AXIS IV: ___________________________________________________________________________________
AXIS V: ____________________________________________________________________________________
(Indicate most recent GAF score & Date Given (mm/dd/yyyy) ____________________)
Attached Documents
(Assessments, Evaluations, etc.)
Documents
Provided
by Case
Manager
If No or N/A Indicate Rationale
Provided by
Receiving
Facility
If No or N/A Indicate Rationale
30. Mental Status and Psychiatric
Evaluation
Yes
No
N/A
Yes
No
N/A
31. Psychiatrist’s Notes
(Up to 90 days)
Yes
No
N/A
Yes
No
N/A
32. Diagnostic Summary/ Clinical
Impressions &
Recommendations
Yes
No
N/A
Yes
No
N/A
33. Significant Lab and Diagnostic
Reports
Yes
No
N/A
Yes
No
N/A
34. Psychological Evaluation
Yes
No
N/A
Yes
No
N/A
35. Psychosocial History
(Comprehensive if available)
Yes
No
N/A
Yes
No
N/A
36. Substance Abuse
Developmental Disability
Other
Yes
No
N/A
Yes
No
N/A
CONTINUED
142 - Baker Act Forms

Baker Act Forms
Page 147
Baker Act Forms
State Mental Health Facility Admission Form (Page 3)
D. Client Medical Information / History
(continued)
Attached Documents (Assessments, Evaluations, etc.) continued
Documents
Provided
by Case
Manager
If No or N/A Indicate
Rationale
Provided by
Receiving
Facility
If No or N/A Indicate
Rationale
37. Physical Exam and Medical History
Yes
No
N/A
Yes
No
N/A
38. Medication History including current
prescribed medications
Yes
No
N/A
Yes
No
N/A
39. Appropriate Legal Documents including
Court Order, Police Report and Petition for
Involuntary Placement, Form 3089, 3052a,
3052b, and ex-parte order when applicable
Yes
No
N/A
Yes
No
N/A
40. Client Service Plan and/or Treatment Plan
Yes
No
N/A
Yes
No
N/A
41. Clinician’s Progress Notes (Up to past year)
Yes
No
N/A
Yes
No
N/A
42. Functional Assessments (Most recent)
Yes
No
N/A
Yes
No
N/A
43. Receiving Facility Admissions Summary,
and, if available, Emergency Room Report
Yes
No
N/A
44. Primary Issues of Strength Checklist: Place scoring code (see key) in appropriate column to indicate extent of strength, or need
in each subject area listed below, and briefly describe problem, if any.
* Key: 0 = No Data; 1 = Minor; 2 = Moderate; 3 = Severe
Strength Issue/Need Description of Strengths, Issues, Needs
(attach information, if necessary)
Health
Mental Health
Family
Social
Work
Police, Law
Violence
Accidents
Education
Other (specify)
CONTINUED OVER
Baker Act Forms - 143

Page 148
Baker Act Forms
State Mental Health Facility Admission Form (Page 4)
D. Client Medical Information / History
(continued)
45. The issues/needs checked above co-occur with:
Alcohol Drugs Psychiatric Disorder Developmental Disability Other (Specify) _______________________
46. Reason for transfer to the state facility ________________________________________________________________________
________________________________________________________________________________________________________
47. What steps have already been taken to explore less restrictive placement ______________________________________________
________________________________________________________________________________________________________
48. List Previous State Hospital Admissions (attach additional sheets if necessary):
Admission Date (mm/dd/yyyy) Facility Name Length of Stay
49. List previous Local Hospitals, Crisis Stabilization Units, or Intensive Residential Treatment Programs serving client prior to
admission (include facility/program name and mailing address):
Facility Name Program Name Mailing Address
E. Current Financial Information About Client
50. Monthly Income: $_________________ 51. Check one: Owns Home Rents
52. Complete the following charts as appropriate:
Other _____________________________
Monthly
Benefit
Type of Claim/
Policy Number
If Filed For Date
Filed
I.D. Number Where Filed Approved/Denied
(Indicate why if denied)
Social
Security
Medicare
S.S.I. Medicaid
Veteran’s
Benefits
Champus
Pensions Medical
Insurance
Insurance/
HMO
Hospitaliza-
tion
Other
(Specify)
Other
(Specify)
53. List any other financial resources:
CONTINUED
144 - Baker Act Forms

Baker Act Forms
Page 149
Baker Act Forms
State Mental Health Facility Admission Form (Page 5)
F. Recommendations and Pre-Release Plans
(Items 54, 55 and 56 completed jointly by Receiving Facility & Community Case
Manager)
54. List expectations of the State Facility
By Client ______________________________________________________________________________________________
By Family _____________________________________________________________________________________________
By Community Services __________________________________________________________________________________
55. List ALL potential recommended alternatives for this client’s return to the community (include the name, address, and phone
number of services/programs to which the client may be referred):
Client _________________________________________________________________________________________________
______________________________________________________________________________________________________
Family ________________________________________________________________________________________________
______________________________________________________________________________________________________
Community Services _____________________________________________________________________________________
______________________________________________________________________________________________________
56. Describe briefly how the community staff will remain involved in the therapeutic process during this client’s hospitalization (to be
developed through mutual effort of Hospital and Continuity of Care Facilitator.
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
57. Describe briefly how the family will remain involved in the therapeutic process during this client’s hospitalization (to be
developed through mutual effort of Hospital and Continuity of Care Facilitator:
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
G. Receiving Facility’s General Referral Comments
(Include statement indicating eligibility for placement in a Mental Health or Developmental Services Facility)
______________________________________ _________________________________ _______/_______/________
Signature of Person(s) Completing Form Title Date Signed (mm/dd/yyyy)
______________________________________ _________________________________ _______/_______/________
Signature of Person(s) Completing Form Title Date Signed (mm/dd/yyyy)
CONTINUED OVER
Baker Act Forms - 145

Page 150
Baker Act Forms
State Mental Health Facility Admission Form (Page 6)
Client Name
Receiving Facility
Signature
This side to be completed by the Receiving Facility
and sent with the admission packet prior to
admission
Check
if included in packet or Circle “NA”
1. Form 7000
A. Identifying Information
B. Status Information
C. Tansfer/Screen Agency ID Info
D. Medical Info/History
29. Current Diagnosis
30. Psychiatric Eval/Diag Sum
31. Psychiatric Notes
34. Psychological Evaluation
35. Psychosocial Eval/History
37. Physical Examination
39. Appropriate Legal Docs
40. Service Treatment Plan
41. Clinicians’ Progress Notes
42. Functional Assessment
43. Rec Fac Admission Summary
44. Prim Issue/Strength Ck List
45. Issues/Needs Co-occuring
46. Reason for Transfer
47. Steps taken to explore less
restrictive placement
48. Previous Psychiatric Admis
49. Previous Other Admissions
E. Current Financial Information
F. Recommend./Pre-Release Plan
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
NA
3. Satisfaction of the State Mental Health Facility Staff
Person (Please Circle Appropriate Rating)
A. Overall, I am very satisfied with the admission packet
information and process.
SS#
Phone #
Date Admission Packet Sent
(mm/dd/yyyy)
This side to be completed by the State Mental Health Facility Staff Person after receiving admission packet
Rating
Complete
Info
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
Incomplete
Info
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2. Joint Review (of admission packet information) (State Mental Health Facility Staff Person Completes)
A. Who Reviewed? State Mental Health Facility _________________________________ Receiving Facility ______________________________
B. When Reviewed? Date(s) (mm/dd/yyyy) ___________________________________ _______________________________
C. What incomplete/missing information items need to be resolved? (Use back if needed)
Above Item # Action to Resolve
No
Info
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Notes
(Please Note Incomplete And/Or Missing information Items)
(Use Back if Necessary)
Rating
Strongly
Neutral
Agree
Disagree
Agree
5 4 3
2
Date Due (mm/dd/yyyy)
Who to Resolve
Strongly
Disagree
Comments
(Please Explain Low Ratings: 3 or Less)
(Use Back if Necessary)
B. State Mental Health Facility Staff Person Signature ______________________________________ Phone # (______) ___________________________
See s. 394.4573 and s. 394.468, Florida Statutes
CF-MH 7000, Jan 98 (Recommended Form) BAKER ACT
146 - Baker Act Forms

Baker Act Forms
Page 151
Baker Act Forms
Department of Children & Families
State Mental Health Facility Discharge Form
Instructions: This form will be faxed to the community case manager the day of discharge and to the medical service
provider in jail, if appropriate. A copy of this form with the attachments will be mailed by the next working day.
Attach copies of Need/Issue Lists, Service Plan, current status, significant lab reports, physical exam (completed in last 30
days), attach copy of latest clinical summary/competency exam completed within 30 days prior to discharge, and
comprehensive social history with latest update.
TO (Agency) _______________________________________________________________________________________________
Phone # (_______) ________________________ Fax # (_______) ____________________________
Mailing Address ____________________________________________________________________________________________
____________________________________________________________________________________________
ATTN (Case Manager ) _____________________________________________ Phone # (_______) _________________________
A. Social Worker’s Section: (Include all relevant demographic information)
1. Client’s Name _______________________________________________ Hospital Number ____________________________
Legal Status __________________________________ Date of Admission (mm/dd/yyyy) ________/___________/_________
Social Security Number ___________ - _________ - ___________ Date of Birth (mm/dd/yyyy) ______/________/_________
County of Residence ______________________________ County of Admission ___________________________________
Guardian or First Representative ________________________________________ Relationship _______________________
Address ______________________________________________________________________________________________
Phone # (_______) __________________________
2. Discharged Status Including Conditional Release Plans: ________________________________________________________
________________ _________________________ Discharge To ________________________________________________
Discharge Address ______________________________________________________________________________________
Phone Number # (_______) ___________________________
3. Financial Status: Type of Benefit(s) ________________________________________________________________________
Name of Payee _____________________________________________ Amount of Benefits __________________________
Date Applied For _____/_____/______ Date Accepted/Rejected _____/_____/______ Appeals _____/_____/______
(mm/dd/yyyy) (mm/dd/yyyy) (mm/dd/yyyy)
4. Who takes responsibility for the client upon discharge? (List name, relationship, responsibilities)
________________________________________ ______/______/________ Phone # (_______) __________________
Social Worker’s Signature Date (mm/dd/yyyy)
CONTINUED OVER
Baker Act Forms - 147
Page 152
Baker Act Forms
State Mental Health Facility Discharge Form (Page 2)
B. Psychiatrist’s Section:
Current Diagnoses (Current edition of DSM [Axis I, II, IV & V] and ICD [Axis III]):
AXIS I: __________________________________________ AXIS II: _____________________________________________
AXIS III: _________________________________________ AXIS IV: ____________________________________________
AXIS V: GAF = ____________ On Admission SCI-PANSS = ____________ On Admission
GAF = ____________ On Discharge SCI-PANSS = ____________ On Discharge
Course of Hospitalization:
1. Reason for Admission (Circumstances which brought client to hospital):
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
2. Assessment and Findings (Diagnostic assessments completed and findings including mental status exam):
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
3. Treatment and Response (Types, frequencies, and response from admission to present):
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
4. Homicidal/Suicidal History (Address any issues related to these behaviors):
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
5. Medication History for current admission, including any dosages, court ordered medications, significant labs for psychiatric management, (i.e.,
lithium levels, etc.), and side effects. (See also Medical Physician’s section, page 3).
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
6. Prognosis including recommendations for follow up and early warning signs of decompensation (address delusional speech).
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
____________________________________ _______/_______/_______ Phone # (_______) ___________________
Psychiatrist’s Signature Date (mm/dd/yyyy)
CONTINUED
148 - Baker Act Forms

Baker Act Forms
Page 153
Baker Act Forms
State Mental Health Facility Discharge Form (Page 3)
C. Medical Physician’s Section:
(summary of current hospital course as it relates to medical issues, note special consultations, need for follow up)
Allergies ______________________________________________ Diet _____________________________________________________
Medical Diagnoses ________________________________________________________________________________________________
________________________________________________________________________________________________________________
Lab and Other Studies including Pap Smear and Blood Levels appropriate for management of medical conditions.
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Immunizations: PPD DT Influenza Pneumovax
Hospital Course, Special Issues/Concerns, Recommendations for Follow-up (List some descriptive items such as important salient treatment
modalities, special issues/concerns, successful treatment modalities):
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Medication Regime including dosages, significant labs, and side effects. (See also Psychiatrist section page 2)
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________ ________/________/________ Phone # (_______) ____________________
Medical Physician’s Signature Date (mm/dd/yyyy)
CONTINUED OVER
Baker Act Forms - 149

__________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
Page 154
Baker Act Forms
State Mental Health Facility Discharge Form (Page 4)
D. Nurse’s Section:
1. Adaptive Equipment: Indicate below if client has items listed or if client needs items listed.
Has Needs Dentures (Type) _________________ Has Needs Hearing Aid
Has Needs Wheelchair Has Needs Crutches
Has Needs Glasses Has Needs Contacts
Has Needs Prosthesis ______________________ Has Needs Cane
Has Needs Walker
2. Describe skin condition: __________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
3. Is client at risk for choking? (check one) Yes No
Does the attached Service Implementation Plan contain information related to prevention of aspiration? (check one)
Yes No
4. Is client is on Blood/Body Fluid Precautions? (check one) Yes No
5. Side Effects/Adverse Reactions: ____________________________________________________________________________
__________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________
6. Current Medications as ordered for separation (include date/time of last dose): _______________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
Number of days supply sent with client: _________________
7. Medication not sent (per facility policy) _____________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
8. Is client capable of taking his/her own medication? (check one) Yes No
Has medication education been provided? (check one) Yes No
9. History of medication compliance while in hospital. Never Sometimes Usually Always
CONTINUED
150 - Baker Act Forms

Baker Act Forms
________________________________________________________________________________________________________________
Page 155
Baker Act Forms
State Mental Health Facility Discharge Form (Page 5)
D. Nurse’s Section:
(continued)
10. Summary of pertinent nursing information including recent changes in the physical condition/mental status and current weight,
blood pressure, pulse/respiration, patterns of elimination, nutrition including feeding and eating habits and any special dietary
needs (address choking risk), personal hygiene, menstrual cycle (as indicated) and identifying any nursing/individual needs and
recommendations for nursing care plans.
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
_________________________________________________ _______/_______/__________ Phone # (_______) __________________
Nurse’s Signature Date (mm/dd/yyyy)
Pre-Release Contacts (Nurse will notify the community agencies, or jail, regarding any relevant medical/nursing issues):
Person Contacted ______________________________________________________________________________
Phone # (_______) __________________ (_______) __________________
FAX # (_______) __________________ (_______) __________________
Response _____________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
Nurse Making Contact _________________________________________ Date ____/____/_________ Time ________ am pm
(mm/dd/yyyy)
Phone # (_______) __________________________ Fax # (_______) _________________________
CONTINUED OVER
Baker Act Forms - 151

__________________________________________________________________________________________________________
Page 156
Baker Act Forms
State Mental Health Facility Discharge Form (Page 6)
E. Rehabilitation Section
Instructions: Check (3) the appropriate response.
Primary Language ____________________________ Secondary Language ______________________________
Writes Speaks Signs Writes Speaks
Presently Attending Education: Yes No Reads Writes Counts Tells Time
Has completed: High School Vocational College
Interested in attending classes: High School Vocational College Graduate
Requires Therapeutic Devices: Glasses Hearing Aid
Behavioral Response Level
Language Skills Verbal Non-Verbal
Receptive Language (check one) Expressive Language (check one)
Doesn’t understand speech Makes no sounds
Understands simple conversation/instructions Uses simple words
Understands complex conversation/instructions Uses sentences
Carries on conversation
Attention Span: 0-3 min. 4-9 min. 10+ min. Other ______________________________________
Group Therapy Skills Social Skills (check all that apply)
Likes Working in Group Expresses Feelings
Expresses Feelings to Group Expresses Affection Appropriately
Sets Goals for Self Initiates Conversations with Others
Speaks in Turn Responds to Criticism (Pos/Neg)
Responds to Feelings Converses About Family
Identifies Interpersonal Barriers Compliments Others
Offers Assistance
Leisure Activities Responds to Personal Statements
Initiates Leisure Activities Requests Assistance When Needed
Schedules Own Leisure Activities Expresses Opinions
Selects Preferred Leisure Activities Asks Before Borrowing Items From Others
Participates in Offered Leisure Activities Isolative
Invites Friends to Participate Speaks in Normal Tone of Voice
Evaluates Satisfaction Boundary Issues (Personal Space)
Activity Preferences: (Mark boxes indicated by client)
Arts/Crafts Parties/Programs Religious Services Music
Horticulture Discussion Groups Exercising Outings
Library Recreation Reading Movies
Plays Sports Watches Sports Other _________________________
Past Employment (check): Sheltered Workshops Supported Employment Private Sector
Presently Employed With ____________________________________________________________________________________
Comments (recap client participation in Rehab. activities)___________________________________________________________
________________________________________ ______/______/______ Phone # (_____) ______________________
Rehab. Employee Signature Date (mm/dd/yyyy)
CONTINUED
152 - Baker Act Forms

Baker Act Forms
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
Page 157
Baker Act Forms
State Mental Health Facility Discharge Form (Page 7)
F. Direct Care Section:
Instructions: Place an “I” for independent, “E” for needs encouragement or
“A” for requires assistance. In comment section, reflect on encouragement and assistance required.
Housekeeping: Grooming: Other:
___ Makes Beds ___ Bathes ___ Removes Items from Other’s Rooms
___ Operates Washer ___ Dresses ___ Closes Bathroom Door
___ Operates Dryer ___ Brushes Teeth ___ Flushes Toilet
___ Folds Clothes ___ Washes Hair ___ Wash Hands after Using Rest Room
___ Keeps room neat ___ Shaves ___ Washes Hands
___ Grooms Hair ___ Crosses Street Safely
Eating Habits: ___ Wears Clean Clothes ___ Hoards Things
___ Eats Breakfast, Lunch, and Dinner ___ Wears Appropriate Clothes ___ Dresses Appropriate to Season
___ Steals Food ___ Uses Deodorant
___ Shares Food
___ Uses Good Table Manners Uses Telephone: Use of Tobacco Products:
___ Follows Diet ___ Local ___ Maintains a Schedule
___ Rate or Speed of Eating ___ Long Distance ___ Chain Smokes
___ Feeds Self Independently ___ Can Dial 911 ___ Doesn’t Smoke
___ Smokeless Tobacco Products
Budgets:
Spends $_______________ Weekly
Spends Moderately Excessively on Snacks and Cigarettes
___ Can manage own money
___ Shops for Clothing
___ Saves Money
___ Saves for Leisure
Independent Living Clients Only
Sexual Acting Out: Use of Transit Systems
Knowledge about Develop a Budget
Sexually Intruding on Others Knows Food Safety Rules
Exposing Self Knows Safety Rules for Kitchen
Public Masturbation Knows how to Evacuate in a Emergency
Urinates in Public Knows Items to Stock for Emergencies
Comments _______________________________________________________________________________________________
___________________________________________ _______/_______/__________ Phone # (_________) _________________
Direct Care Staff Signature Date (mm/dd/yyyy)
CONTINUED OVER
Baker Act Forms - 153

Page 158
Baker Act Forms
State Mental Health Facility Discharge Form (Page 8)
G. Post Hospital Aftercare Recommendations by Service Team:
1. Check (3) indicates behavior as applicable to client:
Item Previous History Never Sometimes Often Usually Always
Violent to Self/Others/Property
Suicidal
Assaultive
At Risk of Leaving
Medication Compliance
Therapeutic Activity Compliance
Cooperative
Demonstrates Understanding of Illness
Has Supportive Family/Other
2. List of circumstances under which relapse is apt to occur (early warning signs to look out for).
______________________________________________________________________________________________________
______________________________________________________________________________________________________
3. List crucial intervention needed to help promote successful placement (frequency of family contact, participation in AA, Day
Treatment Group Therapy).
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
4. Description of the degree of supervision needed by the client. None Minimal Close
Comments (describe circumstances): ________________________________________________________________________
______________________________________________________________________________________________________
5. Treatment Recommendations: _____________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
6. Client Preferences or Recommendations: ____________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
7. Appointment at Local Community Mental Health Agency Date ______/______/________ Time _____________ am pm
(mm/dd/yyyy)
Name of Therapist ________________________________ Appointment Confirmed By ____________________________
8. Appointment for Medical Problems Date ______/_______/_________ Time _____________ am pm
(mm/dd/yyyy)
Street Address ________________________________________________________________________________________
Physician’s Name _______________________________________ Phone # (_____) __________________________
Name of Person Responsible for Medical Treatment (including financially) ________________________________________
9. Additional Follow-up ___________________________________________________________________________________
__________________________________________ Date Signed ___/___/________ Phone # (_____) ____________________
Service Team Leader or Designee (mm/dd/yyyy)
CONTINUED
154 - Baker Act Forms

Baker Act Forms
Baker Act Forms - 155
State Mental Health Facility Discharge Form (Page 10)
H. Client’s Copy of Discharge Summary:
Psychiatric Services:
PsychiatricServiceswillbeprovidedby Dr.:_____ ________________________________________
Address: ____________________________________________________________________________________________
Phone: (_______)___________________________ Contact Person: ___________________________________________
My first appointment will be: Date: ______________________________________ Time: ______________ampm
(mm/dd/yyyy)
Medical Services:
Provisionofmedical care will beprovided byDr.: ___________________________________________
Address: ____________________________________________________________________________________________
Phone: (_______)____________________________ Contact Person: ___________________________________________
My special medical needs are: ___________________________________________________________________________
Medication:
My medicationsare for_____________________________________ dosage_________________________
I understandthe importanceof medicationandagree totake it as
prescribed. If I haveproblems, I will contact mycase mana
ger who
is: _________________________________________________at (_______)______________________
Financial:
I will receive incomeof Amount Source
$
___________________________ ___________________________
$
___________________________ ___________________________
My cost of care will be $____
______________________ I will receive for spending $__________________________
Transportation:
Upon discharge, transportationwill beprovided by: ________________________________________________
My daily transportation needtoDr. appointments, day
treatment andrecreational activities will beprovidedby
___________________________________________________.
CaseManagement Services:
_______________________________________________________ will serve asmycase manager.
________________________________________________ will bemylinkto community services. I should let him/her know what
my needs orconcernsare. I will meet withhim/her on
(mm/dd/yyyy)_______________at_________ am pmfor our first
community visit at ______________________________________________________________________. He/Sheworks for:
______________________________________________________________________________________________________.
Address: _________________________________________________________ Phone#: (_____)_____________________
Provision forState HospitalFollow Up & Continuity of Care:
I will beona _________________day leave of absence to
ensure myadjustmentand smoothtransitionintocommunity living.
_____________
____________________________ will follow up with _______________phonecalls and/orfacetoface visits.
Social Worker’s Name
Number/frequency
I may feel free tocontact treatmentteammembers du
ringthis transition. My treatmentcontacts are:
Names Phone
#’s
___________________________________________________________ (_____)_____________________
___________________________________________________________ (_____)_____________________
CONTINUED
Page 160
Baker Act Forms
State Mental Health Facility Discharge Form (Page 9)
H. Client’s Copy of Discharge Summary:
(To be completed with the client and assigned unit staff. A copy of this plan shall given to
the client at the time of discharge).
Date: ___________________ Name:________________________________________________________________________
(mm/dd/yyyy)
Hospital #:_____________________________________ SSN: ____________________________________________
Legal Status: Voluntary Involuntary
Competent Incompetent Incompetent to Proceed Not Guilty by Reason of Insanity
Advance Directive Health Care Surrogate
Guardian: Person Property
This individualized discharge plan has been developed by:
________________________________________ ________________________________________ _______________________________
Staff Person Client Case Manager
Guardian’s Name: __________________________________________________ (______)_________________________
Address Phone
Address ________________________________________________________________________________________________
Provision for Placement: {For persons returning to jail, the following information is submitted for consideration in regards to potential placement
and follow-up services.}
I will reside at: ___________________________________________________________________________________________
Address
(________)__________________________ ______________________________________________________
Phone # Contact Person
I understand the client rules are: __________________________________________________________________________________________
_____________________________________________________________________________________________________________________
I agree do not agree to abide by the rules. (Check one)
Family: My family has has not been notified of my discharge or has not been by my request.
They will assist me through ______________________________________________________________________________________________
_____________________________________________________________________________________________________________________
Family was provided education on ________________________________________________________________________________________
Community Services Recommended Available in Community Recommended by Team Agreed to by Client Comments
Intensive Case Management
Case Management
Medical
Substance Abuse
Therapy
Sheltered Employment
Supported Employment
Home Help
Independent Living Skills Training
Day Treatment
Religious Services
Financial
Legal
Educational
Other (Specify):
CONTINUED OVER
Page 159
Baker Act Forms

___________________________
Page 160
Baker Act Forms
State Mental Health Facility Discharge Form (Page 10)
H. Client’s Copy of Discharge Summary:
Psychiatric Services: Psychiatric Services will be provided by Dr.: _____________________________________________
Address: ____________________________________________________________________________________________
Phone: (_______)___________________________ Contact Person: ___________________________________________
My first appointment will be: Date: ______________________________________ Time: ______________ am pm
(mm/dd/yyyy)
Medical Services: Provision of medical care will be provided by Dr.: ___________________________________________
Address: ____________________________________________________________________________________________
Phone: (_______)____________________________ Contact Person: ___________________________________________
My special medical needs are: ___________________________________________________________________________
Medication: My medications are for _____________________________________ dosage _________________________
I understand the importance of medication and agree to take it as prescribed. If I have problems, I will contact my case manager who
is: _________________________________________________ at (_______) ______________________
Financial: I will receive income of Amount Source
$ ___________________________ ___________________________
$ ___________________________
My cost of care will be $__________________________ I will receive for spending $__________________________
Transportation: Upon discharge, transportation will be provided by: ________________________________________________
My daily transportation need to Dr. appointments, day treatment and recreational activities will be provided by
___________________________________________________.
Case Management Services: _______________________________________________________ will serve as my case manager.
________________________________________________ will be my link to community services. I should let him/her know what
my needs or concerns are. I will meet with him/her on (mm/dd/yyyy) _______________ at _________ am pm for our first
community visit at ______________________________________________________________________. He/She works for:
______________________________________________________________________________________________________.
Address: _________________________________________________________ Phone #: (_____)_____________________
Provision for State Hospital Follow Up & Continuity of Care: I will be on a _________________ day leave of absence to
ensure my adjustment and smooth transition into community living.
_________________________________________ will follow up with _______________ phone calls and/or face to face visits.
Social Worker’s Name Number/frequency
I may feel free to contact treatment team members during this transition. My treatment contacts are:
Names Phone #’s
___________________________________________________________ (_____)_____________________
___________________________________________________________ (_____)_____________________
CONTINUED
156 - Baker Act Forms

Baker Act Forms
__________________________________________________ _________________________________________________
__________________________________________________ __________________________________________________
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
Page 161
Baker Act Forms
State Mental Health Facility Discharge Form (Page 11)
Other Significant Information:
This treatment plan has been approved and agreed upon this ___________ day of ____________________, ____________
by affixed signatures:
Client Hospital Personnel
Case Manager Legal Guardian
Client did not agree to sign. Reason: ________________________________________________________________________
CONTINUED OVER
Baker Act Forms - 157

Page 162
Baker Act Forms
State Mental Health Facility Discharge Form (Page 12)
Client Name Client ID#: SS#
State Mental Health Facility Staff Person Phone #
Signature Date Discharge Packet Sent (mm/dd/yyyy)
This side to be completed by the State Mental
Health Facility Staff Person and sent with
discharge packet prior to discharge
Check
if included in packet or circle “NA”
This side to be completed by the Community Case Manager after receiving the discharge packet
Rating Notes
(Please Note Incomplete and/or Missing information Items)
(Use Back if Necessary)
1. Form 7001
A. Social Worker’s Section
NA
3 2 1
B. Psychiatrist’s Section NA
3 2 1
C. Medical Physician’s Section NA
3 2 1
D. Nurse’s Section NA
3 2 1
. Rehabilitation Section E NA
3 2 1
. Direct Care Section F NA
3 2 1
G. Post Hospital Aftercare NA
3 2 1
H. Discharge Plan NA
3 2 1
I. Attachments
1. Service Plan
NA
3 2 1
2. Court Orders NA
3 2 1
3. Clinical Summaries NA
3 2 1
4. Physical Exam NA
3 2 1
5. Psychosocial History NA
3 2 1
6. Other NA
3 2 1
7. Other NA
3 2 1
8. Other NA
3 2 1
2. Joint Review (of admission packet information) (Community Case Manger Completes)
A. Who Reviewed? State Mental Health Facility Community Case Manager
B. When Reviewed? Dates(s) (mm/dd/yyyy) ______________________________ __________________________________________
C. What incomplete/missing information items need to be resolved? (Use back if needed)
Above Item # Action to Resolve Who to Resolve Date Due
(mm/dd/yyyy)
3. Satisfaction of the Community Case Manager
Please Circle Appropriate Rating
Rating Comments
(Please Explain Low Ratings: 3 or Less)
(Use Back if Necessary)
A. Overall, I am very satisfied with the admission packet
inoformation and process. 5 4 3 2 1
B. Community Case Manager Signature __________________________________________________Phone # (________) ______________________________
Complete
Info
No
Incomplete
Info
Info
Strongly
Agree
Agree
Neutral
Disagree
Strongly
Disagree
See s. 394.4573 and s. 394.468 Florida Statutes
CF-MH 7001, Jan 98
(Recommended Form) BAKER ACTT
158 - Baker Act Forms

Baker Act Forms
Page 163
Baker Act Forms
Physician to Physician Transfer Form
Must be completed at time of transfer to and from the State Hospital
Person’s Name: DOB:
Referring Facility: Phone # ( )
Referring Physician: Phone # ( )
Date of Admission to Referring Facility:
Discharge Diagnosis AXIS I:
AXIS II: AXIS III:
Significant/Critical Events During Hospitalization (current status, suicide attempts/gestures, self injurious behavior, restraints, special
precautions, etc.:
____________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Significant Medical History, Treatment & Diagnosis (Allergies, recent significant laboratory findings, med/surg procedures, etc.)
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Current Medications (List using additional sheet if necessary or attach current MAR)
Name of Medications Dosage Frequency Lab Values Taken Day of Transfer
Yes Time Taken No
Failed Medication Regimens:_____________________________________________________________________________________
______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
Current Precautions (suicide precautions, elopement precautions, etc.):____________________________________________________
______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
Management Suggestions:_______________________________________________________________________________________
______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
Signature of Physician *: _________________________________________________ Date_____________________________
Printed Name of Physician ______________________________________ Physician’s approved designee may sign in the absence of
the physician
Use reverse or attach additional sheets if needed
By authority of s. 394.455(29) and s. 394.461(2), Florida Statutes
CF-MH 7002, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Baker Act Forms - 159

160 - Baker Act Forms
