
BAKER ACT
BENCHGUIDE
November 2016
A Project of the Florida Court Education Council’s Publications Committee

Baker Act Benchguide September 2016
ii
ACKNOWLEDGMENTS
The Publications Committee of the Florida Court Education Council acknowledges
and thanks Ms. Martha Lenderman, M.S.W., one of Florida’s recognized experts
on the Baker Act statute, and General Magistrate Sean Cadigan, Thirteenth Judicial
Circuit, for their diligent work on this Baker Act Benchguide. The materials in
Chapter Eight were created under the auspices of the Florida Department of Law
Enforcement.
This benchguide was partially extracted, with permission, from the “2014 Baker
Act User Reference Guide: The Florida Mental Health Act” written by Martha
Lenderman under a contract between USF Florida Mental Health Institute with the
Florida Department of Children and Families.
AUTHORS
Martha Lenderman, M.S.W., and General Magistrate Sean Cadigan, Thirteenth
Judicial Circuit
PURPOSE
The Baker Act Benchguide was developed to serve as an educational resource and
a user-friendly reference for Florida circuit judges who are dealing with
proceedings under the Baker Act. Although far-reaching, this benchook cannot
hope to be definitive; readers should always check cited legal authorities before
relying on them.
DISCLAIMER
Viewpoints reflected in this publication do not represent any official policy or
position of the Florida Supreme Court, the Office of the State Courts
Administrator, the Florida judicial conferences, the Florida Court Education
Council, or the Florida Court Education Council’s Publications Committee.

Baker Act Bench Guide November 2016
iii
FLORIDA COURT EDUCATION COUNCIL’S
PUBLICATIONS COMMITTEE
The Honorable Angela Cowden, Tenth Circuit, Chair
The Honorable Cory Ciklin, Fourth District Court of Appeal
The Honorable Josephine Gagliardi, Lee County
The Honorable Ilona Holmes, Seventeenth Circuit
The Honorable Matt Lucas, Second District Court of Appeal
The Honorable Ashley B. Moody, Thirteenth Circuit
The Honorable Louis Schiff, Broward County
Ms. Gay Inskeep, Trial Court Administrator, Sixth Circuit
AUTHORS
Ms. Martha Lenderman, MSW
Pinellas County
Sean Cadigan, General Magistrate,
Thirteenth Circuit
PUBLICATIONS COMMITTEE STAFF
Ms. Madelon Horwich, Senior Attorney, Publications Unit,
Office of the State Courts Administrator
_____________________________________________________________________________________
Baker Act Benchguide November 2016
iv
TABLE OF CONTENTS
Place your cursor over the item you would like to view and press
“Click” to go directly to that item.
Case law and most other legal citations are hyperlinked to the Westlaw database.
When you click on a link, you will be asked for your Westlaw sign-on information.
Once you are signed on, just minimize the screen. You should then be able to retrieve
all of the Westlaw hyperlinks you select. Due to technical difficulties, some legal
citations other than case law citations are linked to the primary sources.
Introduction: Development and Use of Baker Act Benchguide ................................. 1
Chapter One: History and Overview of Baker Act .................................................... 3
I. History ........................................................................................................... 3
II. Rights of Persons with Mental Illnesses ....................................................... 4
III. Voluntary Admissions ................................................................................... 6
A. In General .............................................................................................. 6
B. Selected Definitions .............................................................................. 6
C. Criteria for Voluntary Admissions ........................................................ 7
D. Voluntary Admission — Exclusions ..................................................... 7
E. Consent to Admission/Treatment .......................................................... 8
F. Transfer to Voluntary Status ................................................................. 8
G. Transfer to Involuntary Status ............................................................... 9
H. Discharge of Persons on Voluntary Status ............................................ 9
IV. Involuntary Examinations – § 394.463, Fla. Stat.; Fla. Admin. Code R.
65E-5.280 ....................................................................................................10
A. Criteria .................................................................................................10
B. Initiation of Involuntary Examination .................................................10
C. Definitions of Professionals ................................................................12
D. Selected Procedures for Involuntary Examinations ............................13
E. Initial Mandatory Examination ...........................................................14
F. Release from Involuntary Examination ..............................................14
G. Notice of Discharge or Release ...........................................................15
H. Reporting to DCF ................................................................................15
I. Transportation of Persons for Involuntary Examination .....................16
J. Persons with Criminal Charges ...........................................................18
K. Weapons Prohibited on Grounds of Hospital Providing Mental
Health Services ....................................................................................18
L. Paperwork Required by the Baker Act ................................................19
M. Involuntary Placement .........................................................................19
_____________________________________________________________________________________
Baker Act Benchguide November 2016
v
N. Continued Involuntary Services ..........................................................23
O. Discharge of Persons on Involuntary Status .......................................24
P. Transfers ..............................................................................................24
Q. Baker Act Oversight ............................................................................25
R. Immunity .............................................................................................25
S. Statute and Rule Matrix — Florida Mental Health Act
(Baker Act) ..........................................................................................27
V. Maps of Administrative Entities Regions ...................................................30
A. Judicial Circuits and DCF Regions .....................................................30
B. DCF Regions and Managing Entities ..................................................31
C. Managing Entities................................................................................32
VI. Psychiatric Diagnoses and Treatment/Medication .....................................33
A. Diagnoses ............................................................................................33
B. Psychotherapeutic Medication ............................................................34
1. Generally ........................................................................................35
2. Antipsychotic Medications ............................................................36
3. Medications for Mood Disorders ...................................................38
4. Anti-Anxiety Medications ..............................................................41
C. Importance of Medication Compliance ...............................................41
D. Electroconvulsive Therapy (ECT) ......................................................42
VII. Adult Mental Health System of Services and Support ...............................43
VIII. Children’s Mental Health System of Services and Support .......................52
IX. Glossary of Common Definitions, Acronyms, and Abbreviations .............55
Chapter Two: Express and Informed Consent .........................................................63
I. Guardian Advocates and Other Substitute Decision Makers .....................63
II. Documentation of Competence to Provide Express and Informed
Consent ........................................................................................................64
III. Persons Determined Incompetent to Consent to Treatment .......................65
IV. Persons Adjudicated Incapacitated .............................................................66
V. Persons with Health Care Surrogates/Proxies ............................................67
VI. Summary of Consent Issues ........................................................................68
VII. Bench Card on Substitute Decision-Making ..............................................70
VIII. Frequently Asked Questions .......................................................................72
A. Competence to Consent .......................................................................72
B. Incompetence to Consent ....................................................................75
C. Disclosure ............................................................................................77
D. Consent to Treatment ..........................................................................78
E. Initiation of Psychiatric Treatment ......................................................80
F. Mental Health Advance Directives .....................................................81
_____________________________________________________________________________________
Baker Act Benchguide November 2016
vi
G. Electroconvulsive Therapy ..................................................................83
H. Consent to Medical Treatment ............................................................85
I. Guardian Advocates and Other Substitute Decision Makers ..............87
1. In General .......................................................................................87
2. Court-Appointed Guardians (Ch. 744, Fla. Stat.) ..........................88
3. Guardian Advocates .......................................................................92
4. Health Care Surrogates/Proxies ...................................................100
5. Powers of Attorney ......................................................................105
IX. Selected Model Baker Act Forms for Informed Consent and Use of
Substitute Decision Makers ......................................................................106
A. Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate........................................107
B. Order Appointing Guardian Advocate ..............................................109
C. Petition Requesting Court Approval for Guardian Advocate to
Consent to Extraordinary Treatment .................................................110
D. Order Authorizing Guardian Advocate to Consent to Extraordinary
Treatment ...........................................................................................111
E. Authorization for Electroconvulsive Treatment................................112
F. Notification to Court of Person’s Competence to Consent to
Treatment and Discharge of Guardian Advocate ..............................113
G. Findings and Recommended Order Restoring Person’s
Competence to Consent to Treatment and Discharging the
Guardian Advocate ............................................................................114
Chapter Three: Admission and Treatment for Minors ..........................................115
I. Cautionary Note ........................................................................................115
II. Minority/Non-Age.....................................................................................115
A. Definition ...........................................................................................115
B. Removal of Disabilities of Non-Age .................................................116
C. Rights, Privileges, and Obligations of Persons 18 Years of Age
or Older ..............................................................................................117
D. Consent to Treatment ........................................................................117
III. Consent for Admission to a Mental Health Facility .................................119
A. Admission ..........................................................................................119
B. Hospitals ............................................................................................119
C. Children’s Crisis Stabilization Units .................................................120
IV. Consent to Psychiatric Treatment .............................................................121
A. Inpatient Treatment ...........................................................................121
B. Residential Treatment Centers ..........................................................121
C. Outpatient Crisis Intervention Services ............................................121
_____________________________________________________________________________________
Baker Act Benchguide November 2016
vii
V. Substance Abuse (Marchman Act) Admission and Treatment .................122
A. In General ..........................................................................................122
B. Criteria ...............................................................................................122
C. Initiation ............................................................................................123
D. Disposition .........................................................................................123
E. Parental Participation in Treatment ...................................................124
F. Release of Information ......................................................................124
G. Parental Participation/Payment .........................................................124
VI. Consent for General Medical Care and Treatment ...................................124
A. Power to Consent...............................................................................124
B. Emergency Care ................................................................................125
VII. Emergency Care of Youth in DCF or DJJ Custody ..................................126
VIII. Delinquent Youth ......................................................................................127
IX. Dependent Youth ......................................................................................128
A. Medical, Psychiatric, and Psychological Examination and
Treatment of Children in DCF Custody ............................................128
B. Psychotropic Medications for Children in DCF Custody .................130
C. Examination, Treatment, and Placement of Children in DCF
Custody ..............................................................................................134
X. Frequently Asked Questions .....................................................................135
A. Minority Defined ...............................................................................135
B. Informed Consent and Consent to Treatment ...................................136
C. Voluntary Admissions .......................................................................138
D. Involuntary Examinations .................................................................139
Chapter Four: Involuntary Examination ................................................................142
I. In General ..................................................................................................142
II. Criteria .......................................................................................................142
III. Initiation ....................................................................................................143
IV. Definitions of Mental Health Professionals ..............................................144
V. Initial Mandatory Involuntary Examination .............................................146
VI. Release ......................................................................................................146
VII. Notice of Discharge or Release .................................................................147
VIII. Involuntary Examination Flowchart .........................................................148
IX. Frequently Asked Questions .....................................................................150
A. Criteria and Eligibility .......................................................................150
B. Initiation in General...........................................................................156
C. Initiation by Courts ............................................................................158
D. Transport ...........................................................................................164
E. Examination and Release ..................................................................165
_____________________________________________________________________________________
Baker Act Benchguide November 2016
viii
X. Selected Baker Act Forms for Involuntary Examination..........................166
A. Petition and Affidavit Seeking Ex Parte Order Requiring
Involuntary Examination ...................................................................166
B. Ex Parte Order for Involuntary Examination ....................................171
Chapter Five: Involuntary Inpatient Placement .....................................................172
I. In General ..................................................................................................172
II. Criteria .......................................................................................................172
III. Initiation of Involuntary Inpatient Placement ...........................................173
IV. Petition for Involuntary Inpatient Placement ............................................173
V. Appointment of Counsel ...........................................................................173
VI. Continuance of Hearing ............................................................................174
VII. Independent Expert Examination ..............................................................174
VIII. Hearing on Involuntary Inpatient Placement ............................................174
IX. Admission to a State Treatment Facility ...................................................176
X. Release of Persons on Involuntary Status .................................................177
XI. Return of Persons ......................................................................................177
XII. Procedure for Continued Involuntary Inpatient Placement ......................178
XIII. Involuntary Inpatient Placement Flowchart ..............................................181
XIV. Continued Involuntary Inpatient Placement Flowchart ............................182
XV. Involuntary Inpatient Placement Hearing Colloquy .................................183
A. Introductory Remarks ........................................................................183
B. Preliminary Matters ...........................................................................185
C. Testimony and Evidence ...................................................................185
D. Closing Arguments ............................................................................188
E. Findings and Order of Court .............................................................188
1. Preliminary Contents ....................................................................188
2. When Baker Act Criteria Have Been Met ...................................189
3. When Baker Act Criteria Have Not Been Met ............................191
4. Sample Provisions for Short-Term Placement With
Reservation of Jurisdiction to Extend or Modify .........................191
XVI. Frequently Asked Questions .....................................................................192
A. Criteria and Eligibility .......................................................................192
B. Initiation and Filing of Involuntary Inpatient Placement ..................194
C. Public Defender and State Attorney ..................................................202
D. Independent Expert Examination ......................................................213
E. Continuances .....................................................................................214
F. Transfers for Medical Care ...............................................................216
G. Waiver of Hearings and Waiver of Patient Presence at Hearing ......216
H. Conversion between Voluntary and Involuntary Status ...................218
_____________________________________________________________________________________
Baker Act Benchguide November 2016
ix
I. Witnesses ...........................................................................................219
J. Hearings .............................................................................................222
K. Involuntary Placement Orders ...........................................................225
L. Continued Involuntary Inpatient Placement ......................................231
M. Baker Act Forms and Service of Process ..........................................232
N. Transfers of Persons under Involuntary Placement ..........................233
O. State Treatment Facilities and Transfer Evaluations ........................234
P. Convalescent Status ...........................................................................236
XVII. Selected Sample Baker Act Forms for Involuntary Inpatient
Placement ..................................................................................................238
A. Petition for Involuntary Inpatient Placement ....................................238
B. Notice of Petition for Involuntary Placement ...................................241
C. Application for Appointment of Independent Expert Examiner .......242
D. Notice to Court – Request for Continuance of Involuntary
Placement Hearing ............................................................................243
E. Order Requiring Involuntary Assessment and Stabilization for
Substance Abuse and for Baker Act Discharge of Person ................244
F. Order Requiring Evaluation For Involuntary Outpatient
Placement ..........................................................................................245
G. Notification to Court of Withdrawal of Petition for Hearing on
Involuntary Inpatient or Involuntary Outpatient Placement .............246
H. Order for Involuntary Inpatient Placement .......................................247
I. Petition Requesting Authorization for Continued Involuntary
Inpatient Placement ...........................................................................248
J. Notice of Petition for Continued Involuntary Inpatient
Placement ..........................................................................................250
K. Order for Continued Involuntary Inpatient Placement or for
Release ...............................................................................................251
Chapter Six: Involuntary Outpatient Services .......................................................252
I. Introduction ...............................................................................................252
II. Rights of Persons.......................................................................................252
III. Criteria .......................................................................................................252
IV. Petition ......................................................................................................254
V. Service Provider ........................................................................................255
VI. Treatment Plan ..........................................................................................256
VII. County of Filing ........................................................................................257
VIII. Notice of Petition ......................................................................................258
IX. Hearing ......................................................................................................259
X. Testimony ..................................................................................................260
_____________________________________________________________________________________
Baker Act Benchguide November 2016
x
XI. Court Order ...............................................................................................261
XII. Continued Involuntary Outpatient Services ..............................................261
A. Criteria ...............................................................................................261
B. Petition ...............................................................................................262
C. Notice of Petition for Continued Involuntary Outpatient
Services..............................................................................................262
D. Hearing on Continued Involuntary Outpatient Services ...................263
E. Order for Continued Involuntary Outpatient Services ......................264
XIII. Modification to Court Order for Involuntary Outpatient Services ...........264
XIV. Change of Service Provider ......................................................................265
XV. Noncompliance with Court Order .............................................................265
XVI. Discharge from Involuntary Outpatient Services .....................................267
XVII. Alternatives to Involuntary Outpatient Services Orders ...........................267
XVIII. Involuntary Outpatient Placement Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.) ............269
XIX. Continued Involuntary Outpatient Placement Flowchart .........................270
XX. Frequently Asked Questions .....................................................................271
XXI. Selected Model Baker Act Forms for Involuntary Outpatient
Services .....................................................................................................276
A. Petition for Involuntary Outpatient Placement .................................276
B. Designation of Service Provider for Involuntary Outpatient
Placement ..........................................................................................280
C. Proposed Individualized Treatment Plan for Involuntary Outpatient
Placement and Continued Involuntary Outpatient Placement ..........281
D. Order for Involuntary Outpatient Placement or Continued
Involuntary Outpatient Placement .....................................................284
E. Notice to Court of Modification to Treatment Plan for Involuntary
Outpatient Placement and/or Petition Requesting Approval of
Material Modifications to Plan ..........................................................286
F. Petition for Termination of Involuntary Outpatient Placement
Order ..................................................................................................287
G. Petition Requesting Authorization for Continued Outpatient
Placement ..........................................................................................288
H. Notice to Court of Waiver of Continued Involuntary Outpatient
Services Hearing and Request for an Order ......................................290
Chapter Seven: Rights of Persons with Mental Illnesses ......................................291
I. In General ..................................................................................................291
II. Frequently Asked Questions .....................................................................293
A. In General ..........................................................................................293
_____________________________________________________________________________________
Baker Act Benchguide November 2016
xi
B. Habeas Corpus ...................................................................................297
C. Clinical Records and Confidentiality ................................................299
D. Duty to Warn .....................................................................................307
E. Americans with Disabilities Act (ADA) ...........................................308
F. Right to Dignity and Privacy .............................................................309
G. Communication Restrictions .............................................................310
H. Custody of Personal Possessions ......................................................312
I. Designated Representative ................................................................314
J. Right to Discharge .............................................................................315
K. Advance Directives ...........................................................................317
III. Forms .........................................................................................................320
A. Notice of Right to Petition for Writ of Habeas Corpus or for
Redress of Grievances .......................................................................320
B. Petition for Writ of Habeas Corpus or for Redress of Grievances ...321
C. Advance Directive for Mental Health Care ......................................323
Chapter Eight: Firearm Prohibition for Certain Individuals With Mental
Illnesses .....................................................................................................330
I. Background ...............................................................................................330
II. Applicability of the Law ...........................................................................335
III. Responsibility of Various Entities to Implement Section 790.06,
Florida Statutes..........................................................................................336
A. Physicians Practicing at Baker Act Receiving or Treatment
Facilities ............................................................................................336
B. Baker Act Receiving Facility Administrators (or Designee) ............337
C. Clerks of Court ..................................................................................338
D. Judges or Magistrates ........................................................................339
E. Florida Department of Law Enforcement .........................................340
IV. Relief from a Firearm Disability ...............................................................341
V. Flowcharts .................................................................................................345
A. Admission by Voluntary Status.........................................................345
B. Admission by Involuntary Status ......................................................346
C. Firearm Prohibition Process ..............................................................347
D. Petition for Relief from Firearm Disability .......................................348
VI. Frequently Asked Questions .....................................................................349
A. Applicable State Statutes ...................................................................349
B. Mental Competency (MECOM) Database ........................................350
C. Substance Abuse ................................................................................353
D. Juveniles ............................................................................................354
E. Capacity/Competency .......................................................................355
_____________________________________________________________________________________
Baker Act Benchguide November 2016
xii
F. Relief from Disability ........................................................................355
G. Provisions of Chapter 2013-249, Laws of Florida ............................356
VII. Forms .........................................................................................................360
A. Firearm Prohibition Cover Sheet ......................................................361
B. Finding and Certification by an Examining Physician of Person’s
Imminent Dangerousness ..................................................................362
C. Patient’s Notice and Acknowledgment .............................................363
D. Application for Voluntary Admission of an Adult (Receiving
Facility)..............................................................................................364
E. Notification to Court of Withdrawal of Petition for Hearing on
Involuntary Inpatient or Involuntary Outpatient Placement .............365
F. Order of Court to Present Record of Finding to FDLE or
Requiring Further Documentation on Voluntary Transfer ...............366
G. Petition and Order for Relief from Firearm Disabilities Imposed
by Court .............................................................................................368
APPENDIX I: Recommendations from 1999 Report of the Supreme Court
Commission on Fairness, Subcommittee on Case Administration ...........371
APPENDIX II: Compendium of Appellate Cases, Attorney General Opinions, and
Other Legal References .............................................................................381
I. Evidence Supporting Criteria for Involuntary Inpatient Placement .........382
A. In General ..........................................................................................382
B. Outpatient Commitment ....................................................................388
C. Waiver of Patient’s Presence at Placement Hearing .........................392
D. Notice to and Participation of State Attorney at Involuntary
Placement Hearings ...........................................................................394
E. Duty of State Attorney and Role of Counsel for Receiving Facility
in Involuntary Placement Hearings ...................................................394
F. Deadline for Filing Petitions and Notices .........................................395
G. Appeal Not Moot ...............................................................................396
H. Jurisdiction of Courts ........................................................................397
I. Testimony ..........................................................................................397
II. Clinical Records and Confidentiality ........................................................398
III. Public Records ..........................................................................................403
IV. Payment of Involuntary Placement Bills ..................................................404
V. Transportation of Baker Act Patients ........................................................405
VI. Law Enforcement ......................................................................................408
A. Warrantless Entry — Exigent Circumstances ...................................408
B. Detention and Custody ......................................................................412
C. Use of Force ......................................................................................416
_____________________________________________________________________________________
Baker Act Benchguide November 2016
xiii
D. Weapons ............................................................................................417
VII. Responsibilities of and Lawsuits Against Doctors and Receiving
Facilities ....................................................................................................418
A. In General ..........................................................................................418
B. Duty to Warn .....................................................................................426
C. Malpractice vs. Ordinary Negligence ...............................................428
VIII. Guardianship and Protective Services ......................................................429
IX. Baker Act and Minors ...............................................................................431
X. Baker Act and Criminal Defendants .........................................................437
XI. Marchman Act ...........................................................................................442
APPENDIX III: List of FAQ Categories on DCF Website ...................................445
APPENDIX IV: List of All Mandatory and Recommended Baker Act Forms ....452

Introduction: Development and Use of Baker Act Benchguide
_____________________________________________________________________________________
Baker Act Benchguide November 2016
1
Introduction: Development and Use of Baker Act Benchguide
This benchguide is intended to help the courts appropriately carry out their
responsibilities related to the Baker Act, including:
To enter orders on ex parte petitions for involuntary examinations under the
Baker Act.
To conduct hearings on initial and continued involuntary inpatient placement
and involuntary outpatient services filed by administrators of Baker Act
receiving and treatment facilities.
To respond to petitions for writs of habeas corpus filed on behalf of
individuals held in Baker Act receiving or treatment facilities.
To respond to filings by Baker Act receiving facility administrators to limit
individuals’ access to firearm purchase or possession of a concealed weapon
permit.
This benchguide is intended to be used for informational purposes only. The
information presented herein is not legally binding and does not have any legal
authority. Only chapter 394, Florida Statutes, and chapter 65E-5, Florida
Administrative Code, as well as other federal and state laws, have legal authority.
The creation of administrative rules to implement and clarify the statute is
governed by chapter 120, Florida Statutes. The state law prohibits the repetition of
statute in administrative rules. Therefore, judges, magistrates, assistant state
attorneys, assistant public defenders, and clerks dealing with the Baker Act must
be familiar with and routinely reference both the statutes and the corresponding
rules to ensure correct implementation of the Baker Act law.
Please note that the forms and flowcharts included in this benchbook were
promulgated by DCF before the 2016 statutory amendments and do not incorporate
those changes.
To the extent possible, the word “individual” or “person” is used (rather than
“patient”) throughout this benchguide, except for direct quotes from the statutes
and for the purpose of clarity. Person-first language works to reduce stigma and
increases professional sensitivity to the dignity of persons served. Each chapter in
this benchbook contains useful material on select complex subjects derived from

Introduction: Development and Use of Baker Act Benchguide
_____________________________________________________________________________________
Baker Act Benchguide November 2016
2
the Baker Act law, administrative rules, forms, practices, and other statutes and
case law. A glossary of definitions, acronyms, and common terms is at the end of
Chapter One.
This benchguide was partially extracted from the “2014 Baker Act User Reference
Guide: The Florida Mental Health Act” written by Martha Lenderman under a
contract between USF Florida Mental Health Institute with the Florida Department
of Children and Families. The colloquy was prepared by General Magistrate Sean
Cadigan of the Thirteenth Judicial Circuit, who also reviewed the document for
usefulness to the judiciary.
The benchguide was otherwise prepared by Martha Lenderman. The material in
this benchguide was not prepared by attorneys, and reliance on its content should
not be considered as legal advice.
A separate benchguide for the Marchman Act governing substance abuse
impairment is in progress and will be available through the Office of the State
Courts Administrator.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
3
Chapter One: History and Overview of Baker Act
I. History
Statutes governing the treatment of mental illness in Florida date back to 1874.
Amendments to the law were passed many times over the years, but in 1971 the
Legislature enacted the Florida Mental Health Act. This Act brought about a
dramatic and comprehensive revision of Florida’s 97-year-old laws. It substantially
strengthened the due process and civil rights of persons in mental health facilities.
The Act, usually referred to as the “Baker Act,” was named after Maxine Baker,
the former State representative from Miami who sponsored the Act while serving
as chairperson of the House Committee on Mental Health. Referring to the
treatment of persons with mental illness before the passage of her bill,
Representative Baker stated: “In the name of mental health, we deprive them of
their most precious possession — liberty.”
Since the Baker Act became effective in 1972, a number of legislative amendments
have been enacted to protect persons’ civil and due process rights. The most recent
major revision was when Involuntary Outpatient Placement was added by the
Legislature effective January 2005. In 2016, three bills were passed that revised
mental health law in Florida. SB 12 was passed to improve access to court and
make the process more seamless for persons in crisis with substance abuse and
mental health issues. HB 439 authorizes the creation of mental health courts,
expands eligibility for veteran programs and courts, and HB 769 made changes,
such as reducing the period of time persons with certain nonviolent offenses may
be held in forensic facilities.
It is important that the Baker Act be used only in situations where the person has a
mental illness and meets all remaining criteria for voluntary or involuntary
admission. The Baker Act is the Florida Mental Health Act. It does not substitute
for any other law that may permit the provision of medical or substance abuse care
to persons who lack the capacity to request such care. For many persons, the use of
other statutes may be more appropriate. Alternatives to the Baker Act may include:
Developmental Disabilities, ch. 393, Fla. Stat.
Marchman Act (Substance Abuse Impairment), ch. 397, Fla. Stat.
Emergency Examination and Treatment of Incapacitated Persons, § 401.445,
Fla. Stat.
Federal Emergency Medical Treatment and Active Labor Act (EMTALA)

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
4
hospital “Anti-Dumping” law, 42 U.S.C. § 1395dd.
Hospital Access to Emergency Services and Care, § 395.1041, Fla. Stat.
Adult Abuse, Neglect, and Exploitation, § 415.1051, Fla. Stat.
Health Care Advance Directives, ch. 765, Fla. Stat.
Guardianship, ch. 744, Fla. Stat.
Expedited Judicial Intervention Concerning Medical Treatment Procedures,
Fla. Prob. R. 5.900
II. Rights of Persons with Mental Illnesses
See § 394.459, Fla. Stat.; Fla. Admin. Code R. 65E-5.140. The Baker Act ensures
many rights to persons who have mental illnesses. Some of these rights are as
follows:
Individual Dignity: Ensures all constitutional rights and requires that
persons be treated in a humane way while being transported or treated for
mental illness.
Treatment: Prohibits the delay or denial of treatment due to a person’s
inability to pay, requires prompt physical examination after arrival, requires
treatment planning to involve the person, and requires that the least
restrictive appropriate available treatment be used based on the individual
needs of each person.
Express and Informed Consent: Encourages people to voluntarily apply
for mental health services when they are competent to do so, to choose their
own treatment, and to decide when they want to stop treatment. The law
requires that consent be voluntarily given in writing by a competent person
after sufficient explanation to enable the person to make well-reasoned,
willful, and knowing decisions without any coercion.
Quality of Treatment: Requires medical, vocational, social, educational,
and rehabilitative services suited to each person’s needs to be administered
skillfully, safely, and humanely. Use of restraint, seclusion, isolation,
emergency treatment orders, physical management techniques, and elevated
levels of supervision are regulated. Grievance procedures and complaint
resolution is required.
Communication, Abuse Reporting, and Visits: Guarantees persons in
mental health facilities the right to communicate freely and privately with
persons outside the facilities by phone, mail, or visitation. If communication

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
5
is restricted, written notice must be provided. No restriction of calls to the
Abuse Registry or to the person’s attorney is permitted under any
circumstances.
Care and Custody of Personal Effects: Ensures that persons may keep
their own clothing and personal effects, unless they are removed for safety
or medical reasons. If they are removed, a witnessed inventory is required.
Voting in Public Elections: Guarantees individuals the right to register and
to vote in any elections for which they are qualified voters.
Habeas Corpus: Guarantees the right to ask the court to review the cause
and legality of the person’s detention or unjust denial of a legal right or
privilege or an authorized procedure.
Treatment and Discharge Planning: Guarantees the opportunity to
participate in treatment and discharge planning and to seek treatment from
the professional or agency of the person’s choice upon discharge.
Sexual Misconduct Prohibited: Provides that any staff who engages in
sexual activity with a person served by a receiving/treatment facility is guilty
of a felony. Failure to report such misconduct is a misdemeanor.
Right to a Representative: Ensures the right to a representative selected by
persons (or by facility when person can’t/won’t select their own) when
admitted on an involuntary basis or transferred from voluntary to
involuntary status. The representative must be promptly notified of the
person’s admission and all proceedings and restrictions of rights, receives
copy of the inventory of the person’s personal effects, has immediate access
to the person, and is authorized to file a petition for a writ of habeas corpus
on behalf of the person. The representative can’t make any treatment
decisions, can’t access or release the person’s clinical record without the
person’s consent, and can’t request the transfer of the person to another
facility.
Confidentiality: Ensures that all information about a person in a mental
health facility is maintained as confidential and released only with the
consent of the person or a legally authorized representative. However,
certain information may be released without consent to the person’s
attorney, in response to a court order (after a good cause hearing), after a
threat of harm to others, or in other very limited circumstances. Persons in

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
6
mental health facilities have the right to access their clinical records.
Violation of Rights: Provides that anyone who violates or abuses any rights
or privileges of persons provided in the Baker Act is liable for damages as
determined by law.
III. Voluntary Admissions
A. In General
See § 394.4625, Fla. Stat.; Fla. Admin. Code R. 65E-5.270.
The Baker Act encourages the voluntary admission of persons for psychiatric care,
but only when they are able to understand the decision and its consequences and
are able to fully exercise their rights for themselves. When this is not possible due
to the severity of the person’s condition, the law requires that the person be
extended the due process rights assured for those under involuntary status.
B. Selected Definitions
See § 394.455, Fla. Stat.
Several definitions are important to understanding the criteria for voluntary
admissions and consent to treatment:
“‘Mental illness’ means an impairment of the mental or emotional processes
that exercise conscious control of one’s actions or of the ability to perceive
or understand reality, which impairment substantially interferes with a
person’s ability to meet the ordinary demands of living. For the purposes of
this part, the term does not include developmental disabilities as defined in
chapter 393, intoxication, or conditions manifested only by antisocial
behavior or substance abuse.” § 394.455(28), Fla. Stat.
“‘Express and informed consent’ means consent voluntarily given in writing,
by a competent person, after sufficient explanation and disclosure of the
subject matter involved to enable the person to make a knowing and willful
decision without any element of force, fraud, deceit, duress, or other form of
constraint or coercion.” § 394.455(15), Fla. Stat.
“‘Incompetent to consent to treatment’ means a state in which a person’s
judgment is so affected by a mental illness or a substance abuse impairment
that he or she lacks the capacity to make a well-reasoned, willful, and

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
7
knowing decision concerning his or her medical, mental health, or substance
abuse treatment.” § 394.455(21), Fla. Stat.
C. Criteria for Voluntary Admissions
See § 394.459(3)(a).
Section 394.4625(1)(a), Florida Statutes, provides:
A facility may receive for observation, diagnosis, or treatment any
person 18 years of age or older making application by express and
informed consent for admission or any person age 17 or under for
whom such application is made by his or her legal guardian. If found
to show evidence of mental illness, to be competent to provide express
and informed consent, and to be suitable for treatment, such person 18
years of age or older may be admitted to the facility. A person age 17
or under can be admitted only after a hearing to verify the
voluntariness of the consent.
Each person entering a facility, regardless of age, must be asked to give
express and informed consent for admission and treatment. Express and
informed consent for admission and treatment of a person under 18 years of
age is required from the minor’s guardian. See Chapter Three of this
benchguide concerning who is a “guardian” of a minor.
D. Voluntary Admission — Exclusions
See § 394.4625(1), Fla. Stat.
A minor can be admitted on a voluntary basis only if willing and upon
application by his/her legal guardian and after a judicial hearing to verify the
voluntariness of the consent.
A facility may not admit a person on a voluntary basis who has been
adjudicated by a court as incapacitated.
The health care surrogate or proxy of a person on voluntary status may not
consent to mental health treatment for the person. Therefore, such a person
would be discharged from the facility or involuntary procedures initiated.
Certain individuals residing in or served by long-term facilities licensed
under chapters 400 and 429, Florida Statutes, may not be removed from their

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
8
residence for voluntary examination unless previously screened by an
independent authorized professional and found to be able to provide express
and informed consent to treatment.
A person on voluntary status who is unwilling or unable to provide express
and informed consent to mental health treatment must either be discharged
or be transferred to involuntary status.
E. Consent to Admission/Treatment
Before consent to admission or treatment can be given, the following information
must be given to the person or his/her legally authorized substitute decision maker:
Reason for admission
Proposed treatment, including proposed psychotropic medications
Purpose of treatment
Alternative treatments
Specific dosage range for medications
Frequency and method of administration
Common risks, benefits, and common short-term and long-term side effects
Any contraindications that may exist
Clinically significant interactive effects with other medications
Similar information on alternative medication that may have less severe or
serious side effects
Potential effects of stopping treatment
Approximate length of care
How treatment will be monitored
Disclosure that any consent for treatment may be revoked orally or in
writing before or during the treatment period by any person legally
authorized to make health care decisions on behalf of the individual.
Within 24 hours after a voluntary admission of an adult, the admitting physician
must document in the person’s clinical record that the person is able to give
express and informed consent for admission and treatment. If the adult is not able
to give express and informed consent, the facility must either discharge the adult or
transfer the person to involuntary status.
F. Transfer to Voluntary Status
See § 394.4625(4), Fla. Stat.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
9
A person on involuntary status who applies to be transferred to voluntary status
must be transferred unless the person has been charged with a crime or has been
involuntarily placed for treatment by a court and continues to meet the criteria for
involuntary placement. Before the transfer to voluntary status is processed, the
mandatory initial involuntary examination must be performed by a physician,
clinical psychologist, or psychiatric nurse, and a certification of the person’s
competence to consent must be completed by a physician. In addition, the
competent person must have formally applied for voluntary admission.
G. Transfer to Involuntary Status
See § 394.4625(5), Fla. Stat.
At any time a person on voluntary status is determined not to have the capacity to
make well-reasoned, willful, and knowing decisions about mental health or
medical care, he/she must be transferred to involuntary status. When a person on
voluntary status, or an authorized individual acting on the person’s behalf, makes a
request for his/her discharge, the request for discharge, unless freely and
voluntarily rescinded, must be communicated to a physician, clinical psychologist,
or psychiatrist as quickly as possible, but not later than 12 hours after the request is
made. If the person meets the criteria for involuntary placement, the administrator
of the facility must file a petition for involuntary placement with the court within
two court working days after the request for discharge is made. If the petition is not
filed within two court working days, the person must be discharged.
H. Discharge of Persons on Voluntary Status
See § 394.4625(2), Fla. Stat.
A facility must discharge a person on voluntary status under the following
circumstances:
The person has sufficiently improved so that retention in the facility is no
longer clinically appropriate. A person may also be discharged to the care of
a community facility.
The person requests discharge. A person on voluntary status, or a relative,
friend, or attorney of the person, may request discharge either orally or in
writing at any time following admission to the facility. The person must be
discharged within 24 hours of the request, unless the request is rescinded or
the person is transferred to involuntary status. The 24-hour time period may
be extended by a treatment facility (which generally is a state hospital) when

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
10
necessary for adequate discharge planning, but must not exceed three days,
exclusive of weekends and holidays.
A person on voluntary status who has been admitted to a facility refuses to
consent to or revokes consent to treatment. Such person must be discharged
within 24 hours after the refusal or revocation unless transferred to
involuntary status or unless the refusal or revocation is freely and voluntarily
rescinded by the person.
IV. Involuntary Examinations – § 394.463, Fla. Stat.; Fla. Admin. Code R.
65E-5.280
A. Criteria
A person may be taken to a receiving facility for involuntary examination if there
is reason to believe that he or she has a mental illness (as defined in the Baker Act)
and because of the mental illness
the person either
o has refused voluntary examination after conscientious explanation and
disclosure of the purpose of the examination, OR
o is unable to determine whether examination is necessary, AND
without care or treatment, the person is likely to either
o suffer from neglect or refuse to care for himself or herself, which “poses
a real and present threat of substantial harm to his or her well-being; and
it is not apparent that such harm may be avoided through the help of
willing family members or friends or the provision of other services,” OR
o cause serious bodily harm to himself or herself or others in the near
future, as evidenced by recent behavior.
§ 394.463(1), Fla. Stat.
B. Initiation of Involuntary Examination
See § 394.463(2), Fla. Stat.
An involuntary examination may be initiated by any one of the three following
means:

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
11
A circuit or county court may enter an ex parte order stating that a person
appears to meet the criteria for involuntary examination, specifying the
findings on which that conclusion is based. The ex parte order for
involuntary examination must be based on sworn testimony, written or
oral. No fee can be charged for the filing of a petition for an order for
involuntary examination.
A law enforcement officer, or other designated agent of the court, must take
the person into custody and deliver him or her to an appropriate, or the
nearest, facility within the designating receiving system under section
394.462, Florida Statutes, for involuntary examination. A law enforcement
officer acting in accordance with an ex parte order may serve and execute
such order on any day of the week, at any time of the day or night. A law
enforcement officer acting in accordance with an ex parte order may use
such reasonable physical force as is necessary to gain entry to the premises
and any dwellings, buildings, or other structures located on the premises,
and to take custody of the person who is the subject of the ex parte order.
The officer must execute a written report entitled “Transportation to
Receiving Facility,” detailing the circumstances under which the person was
taken into custody, and the report must be made a part of the person’s
clinical record. Fla. Admin. Code R. 65E-5.260(2).
The ex parte order is valid only until executed or, if not executed, for the
period specified in the order itself. If no time limit is specified in the order,
the order is valid for seven days after the date that the order was signed.
Once a person is picked up on the order and taken to a receiving facility for
involuntary examination and released, the same order cannot be used again
during the time period. The order of the court must be made a part of the
person’s clinical record.
A law enforcement officer must take a person who appears to meet the
criteria for involuntary examination into custody and deliver the person or
have him or her delivered to an appropriate, or the nearest, facility within the
designating receiving system under section 394.462 for examination. The
officer must execute a written report (form CF-MH 3052a) detailing the
circumstances (doesn’t require observations) under which the person was
taken into custody, and the report must be made a part of the person’s
clinical record.
A physician, clinical psychologist, clinical social worker, mental health

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
12
counselor, marriage and family therapist, or psychiatric nurse (each as
defined in the Baker Act) may execute a certificate (form CF-MH 3052b)
stating that he or she has examined the person within the preceding 48 hours
and finds that the person appears to meet the criteria for involuntary
examination and stating the observations of the authorized professional
upon which that conclusion is based. A law enforcement officer must take
the person named in the certificate into custody and deliver him or her to an
appropriate, or the nearest, facility within the designating receiving system
under section 394.462 for involuntary examination. The law enforcement
officer must execute a written report detailing the circumstances under
which the person was taken into custody. The report and certificate must be
made a part of the person’s clinical record. (While not authorized by statute,
Florida’s Attorney General wrote on May 28, 2008, that physician assistants
could under specific circumstances initiate Baker Act involuntary
examinations. Op. Att’y Gen. Fla. 08-31 (2008).)
C. Definitions of Professionals
See § 394.455, Fla. Stat.
“‘Physician’ means a medical practitioner licensed under chapter 458 or
chapter 459 who has experience in the diagnosis and treatment of mental
illness or a physician employed by a facility operated by the United States
Department of Veterans Affairs or the United States Department of
Defense.” § 394.455(32), Fla. Stat.
“Physician assistant” means a person licensed under chapter 458 or chapter
459 who has experience in the diagnosis and treatment of metal disorders.”
§ 394.455(33), Fla. Stat.
“‘Psychiatrist’ means a medical practitioner licensed under chapter 458 or
chapter 459 for at least 3 years, inclusive of psychiatric residency.” §
394.455(36), Fla. Stat.
“‘Clinical psychologist’ means a psychologist as defined in s. 490.003(7),
with 3 years of postdoctoral experience in the practice of clinical
psychology, inclusive of the experience required for licensure, or a
psychologist employed by a facility operated by the United States
Department of Veterans Affairs that qualifies as a receiving or treatment
facility under this part.” § 394.455(5), Fla. Stat.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
13
“‘Clinical social worker’ means a person licensed as a clinical social worker
under s. 491.005 or s.491.006.” § 394.455(7), Fla. Stat.
“‘Mental health counselor’ means a person licensed as a mental health
counselor under s. 491.005 or s.491.006.” § 394.455(26), Fla. Stat.
“‘Marriage and family therapist’ means a person licensed as a marriage and
family therapist under s. 491.005 or s.491.006.” § 394.455(25), Fla. Stat.
“‘Psychiatric nurse’ means an advanced registered nurse certified under s.
464.012 who has a master’s or doctoral degree in psychiatric nursing, holds
a national advanced practice certification as a psychiatric mental health
advanced practice nurse, and has 2 years of post-master’s clinical experience
under the supervision of a physician.” § 394.455(35), Fla. Stat.
“’Qualified professional’ means a physician or a physician assistant licensed
under chapter 458 or chapter 459; a psychiatrist licensed under chapter 458
or chapter 459; a psychologist as defined in s. 490.003(7); or a psychiatric
nurse as defined in s. 394.455. § 394.455(38), Fla. Stat.
D. Selected Procedures for Involuntary Examinations
See § 394.463(2), Fla. Stat.
Any receiving facility accepting a person based on a court’s ex parte order, a law
enforcement officer’s report, or a mental health professional’s certificate must send
a copy of the document with the required cover sheet to the Florida Department of
Children and Families (DCF) (via the Baker Act Reporting Center) on the next
working day.
A person can’t be removed from any long-term care program or residential
placement licensed under chapter 400 (nursing homes) or chapter 429, Florida
Statutes (assisted living facilities), and transported to a receiving facility for
involuntary examination unless an ex parte order, a law enforcement officer’s
report, or a mental health professional’s certificate is first prepared. If the condition
of the person is such that preparation of a law enforcement officer’s report is not
practicable before removal, the report must be completed as soon as possible after
removal, but in any case before the person is transported to a receiving facility. A
receiving facility admitting a person for involuntary examination who is not
accompanied by the required ex parte order, mental health professional certificate,
or law enforcement officer’s report must notify DCF of the admission by certified

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
14
mail or by email, if available, by the next working day. § 394.463(2)(b), Fla. Stat.
E. Initial Mandatory Examination
See § 394.463(2)(f), Fla. Stat.; Fla. Admin. Code R. 65E-5.2801.
A person must receive an initial mandatory examination by a physician or clinical
psychologist at a facility without unnecessary delay to determine whether the
criteria for involuntary services are met. Emergency treatment may be provided.
This initial mandatory involuntary examination must include:
a thorough review of any observations of the person’s recent behavior;
a review of the document initiating the involuntary examination and the
transportation form;
a brief psychiatric history; and
a timely face-to-face examination of the person to determine if he or she
meets the criteria for release.
The person can’t be released by a receiving facility “without the documented
approval of a psychiatrist or a clinical psychologist or, if the receiving facility is
owned or operated by a hospital or health system, the release may also be approved
by a psychiatric nurse performing within the framework of an established protocol
with a psychiatrist or an attending emergency department physician with
experience in the diagnosis and treatment of mental illness and after completion of
an involuntary examination pursuant to this subsection. A psychiatric nurse may
not approve the release of a patient if the involuntary examination was initiated by
a psychiatrist unless the release is approved by the initiating psychiatrist.”
§ 394.463(2)(f), Fla. Stat. The person must be given prompt opportunity to notify
others of his or her whereabouts.
F. Release from Involuntary Examination
See § 394.463(2)(g), Fla. Stat.
Within the 72-hour examination period, one of the following three actions must be
taken based on the individual needs of the person:
The person must be released unless he or she is charged with a crime, in
which case the person must be returned to the custody of a law enforcement
officer.
The person, unless charged with a crime, must be asked to give express and

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
15
informed consent to placement on voluntary status, and, if such consent is
given, the person must be voluntarily admitted. Such transfer from
involuntary to voluntary status must be conditioned on the certification by a
physician that the person has the capacity to make well-reasoned, willful,
and knowing decisions about medical, mental health, or substance abuse
treatment.
A petition for involuntary placement must be completed within 72 hours
and filed with the circuit court for involuntary inpatient placement, or with
the circuit or criminal county court for involuntary outpatient services,
within the 72 hours. If the 72 hours ends on a weekend or holiday, the filing
must be no later than the next working day thereafter.
G. Notice of Discharge or Release
See §§ 394.463(3), 394.469(2), Fla. Stat.
Notice of discharge or transfer of a person must be given as provided in section
394.4599, Florida Statutes. Notice of the release must be given to the individual
and his or her guardian, guardian advocate, health care surrogate or proxy,
attorney, and representative, to any person who executed a certificate admitting the
individual to the receiving facility, and to any court that ordered the individual’s
evaluation.
H. Reporting to DCF
See section 394.463(2)(a), Fla. Stat.
Any receiving facility accepting a person for involuntary examination must send
to DCF via the BA Reporting Center a cover sheet (form CF-MH 3118) and a copy
of the completed initiating form:
ex parte petition/order;
report of law enforcement officer; or
certificate of a professional.
All court orders for involuntary placement must also be sent to the BA Reporting
Center within one day, including:
involuntary inpatient placement order;
involuntary outpatient servicesorder; and
continued involuntary outpatient services order
Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
16
Receiving facilities must report directly to DCF by certified mail or email, within
one working day, any long-term care facility licensed under chapter 400 or chapter
429, Florida Statutes, that does not fully comply with Baker Act provisions
governing voluntary admissions, involuntary examinations, or transportation.
I. Transportation of Persons for Involuntary Examination
See § 394.462, Fla. Stat.; Fla. Admin. Code R. 65E-5.260.
Law enforcement has no responsibility to transport persons for voluntary
admission. Nor is law enforcement responsible for transferring persons from a
hospital ER where they may have been medically examined or treated to a Baker
Act receiving facility. In the latter case, the person’s transfer is the responsibility of
the sending hospital, pursuant to the federal EMTALA law, 42 U.S.C. § 1395dd.
Regardless of whether the involuntary examination is initiated by the courts, law
enforcement, or an authorized mental health professional, law enforcement is
responsible for transporting the person to the nearest receiving facility, or the
appropriate facility within the designated receiving system, for the
examination.
A law enforcement agency may decline to transport a person to a receiving facility
only when any of the following have occurred:
The county has contracted for transportation at the sole cost to the county,
and the law enforcement officer and medical transport service agree that the
continued presence of law enforcement personnel is not expected to be
necessary for the safety of the person to be transported or others. This statute
requires the law enforcement officer to report to the scene, assess the risk
circumstances, and, if appropriate, “consign” the person to the care of the
transport company.
When a jurisdiction has entered into a county-funded contract with a
transport service for transportation of persons to receiving facilities, such
service must be given preference for transportation of persons from nursing
homes, assisted living facilities, adult day care centers, or adult family care
homes, unless the behavior of the person being transported is such that
transportation by a law enforcement officer is necessary.
A law enforcement officer takes custody of a person under the Baker Act
and assistance is needed for the safety of the officer or the person in custody,
in which case the officer may request assistance from emergency medical

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
17
personnel.
If the law enforcement officer believes that a person has an emergency
medical condition, the person may be first transported to a hospital for
emergency medical treatment, regardless of whether the hospital is a
designated receiving facility. An emergency medical condition is defined in
chapter 395, Florida Statutes, as a “medical condition manifesting itself by
acute symptoms of sufficient severity, which may include severe pain, such
that absence of immediate medical attention could reasonably be expected to
result in” serious jeopardy to patient health (including pregnant women and
their fetus), serious impairment to bodily functions, or serious dysfunction of
any bodily organ or part. § 395.002(8), Fla. Stat.
Once the person is delivered by law enforcement to a hospital for emergency
medical examination or treatment and the person is placed in the hospital’s
care, the officer’s responsibility for the person is over, assuming no criminal
charges are pending. Eventual transfer of the person from the hospital
offering emergency medical treatment to the designated receiving facility for
an involuntary examination under the Baker Act is the responsibility of the
referring hospital, unless other appropriate arrangements have been made.
Other than when an emergency medical condition exists, the person must be
delivered to an appropriate or the nearest designated receiving facility — not
to a hospital emergency department that might be more convenient to the
law enforcement officer — unless a Transportation Plan has been approved
by the Board of County Commissioners and the Secretary of DCF. If the
person requires transfer to a different facility for specialized care, the
sending facility is responsible for arranging safe and appropriate
transportation.
A mental health professional member of a mental health overlay program or
mobile crisis response service (as defined in the statute) evaluates a person
and determines that transportation to a receiving facility is needed. In such
cases the service, at its discretion, may transport the person to the facility or
may call law enforcement or make other transportation arrangements best
suited to the needs of the person.
A transportation plan meeting the criteria set out in section 394.462, Florida
Statutes, has been approved by the Board of County Commissioners and the
Secretary of the Department of Children and Families.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
18
The appropriate facility within the designated receiving system or the nearest
receiving facility must accept persons brought by law enforcement officers or
EMS or private transport company authorized the county for involuntary
examination. § 394.462(1)(j), Fla. Stat. This means that the law enforcement
officer will never be legally obligated to further transport a person once presented
to the appropriate or nearest receiving facility or a hospital.
J. Persons with Criminal Charges
See § 394.462, Fla. Stat.; Fla. Admin. Code R. 65E-5.260.
When an officer has custody of a person based on either non-criminal or minor
criminal behavior that meets the statutory guidelines for involuntary examination
under the Baker Act, the law enforcement officer must transport the person to the
appropriate or nearest receiving facility for examination.
When any law enforcement officer has arrested a person for a felony and it appears
that the person meets the statutory guidelines for involuntary examination or
placement under the Baker Act, such person must first be processed in the same
manner as any other criminal suspect.
A receiving facility is not required to admit a person charged with a felony for
whom the facility determines and documents that it is unable to provide adequate
security, but must provide mental health examination and treatment to the person
where he or she is held. No person brought to a receiving facility on involuntary
status who is charged with a crime can be released except back to the custody of a
law enforcement officer.
The costs of transportation, evaluation, hospitalization, and treatment incurred by
persons who have been arrested for violations of any state law or county or
municipal ordinance may be recovered as provided in section 901.35, Florida
Statutes.
K. Weapons Prohibited on Grounds of Hospital Providing Mental Health
Services
See § 394.458, Fla. Stat.
Except as authorized by law or a hospital administrator, firearms or deadly
weapons cannot be brought into a hospital providing mental health services. Law
enforcement officers may choose to lock their firearms in their vehicle prior to
entering such a hospital or may place the firearms in a lock-box at the hospital, if

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
19
one exists.
L. Paperwork Required by the Baker Act
See §§ 394.462, 394.463, Fla. Stat.; Fla. Admin. Code R. 65E-5.280
A law enforcement officer must execute a written report detailing the
circumstances under which the person was taken into custody and the report must
be made a part of the person’s clinical record. A mandatory form entitled
“Transportation to Receiving Facility” (form CF-MH 3100) has been developed to
serve this purpose. An officer should not simply transport a person and leave him
or her at a receiving facility for involuntary examination under the Baker Act
unless the examination has been previously initiated by a court, an authorized
mental health professional, or a law enforcement officer.
If the officer takes an individual to an ED due to a medical emergency after
initiating the involuntary examination, the “Report of Law Enforcement Officer
Initiating Involuntary Examination” (form CF-MH 3052a) must be submitted to
hospital personnel to accompany the person to a receiving facility as well as the
transport form.
If the officer was only transporting a person whose involuntary examination was
initiated by a court or mental health professional, the officer must submit the
court’s Ex Parte Order or the Certificate of Professional Initiating Involuntary
Examination (form CF-MH 3052b), along with the Transportation to a Receiving
Facility form completed by the law enforcement officer, which will be made a part
of the person’s clinical record.
M. Involuntary Placement
See §§ 394.467, 394.4655, Fla. Stat.; Fla. Admin. Code R. 65E-5.290, 65E-5.285
A person may be ordered for involuntary inpatient placement upon a finding of
the court by clear and convincing evidence that he or she has a mental illness and
because of the mental illness the person has refused voluntary placement or
is unable to determine whether placement is necessary, and either
o he or she is incapable of surviving alone or with the help of others and
without treatment is likely to suffer from neglect that poses a real and
present threat of substantial harm to his or her well-being, or

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
20
o there is a substantial likelihood that in the near future he or she will
inflict serious bodily harm on himself or herself or another person, as
evidenced by recent behavior causing, attempting, or threatening such
harm;
and all available less restrictive treatment alternatives that would offer an
opportunity for improvement of the condition have been judged
inappropriate.
An adult may be involuntarily ordered for involuntary outpatient services upon a
finding of the court by clear and convincing evidence that:
(b) The person has a mental illness.
(c) The person is unlikely to survive safely in the
community without supervision, based on a clinical determination.
(d) The person has a history of lack of compliance with
treatment for mental illness.
(e) The person has:
1. At least twice within the immediately preceding 36
months been involuntarily admitted to a receiving or treatment facility as
defined in s. 394.455, or has received mental health services in a forensic or
correctional facility. The 36-month period does not include any period
during which the person was admitted or incarcerated; or
2. Engaged in one or more acts of serious violent behavior
toward self or others, or attempts at serious bodily harm to himself or herself
or others, within the preceding 36 months.
(f) The person is, as a result of his or her mental illness,
unlikely to voluntarily participate in the recommended treatment plan
and has refused voluntary services for treatment after sufficient and
conscientious explanation and disclosure of why the services are
necessary or is unable to determine for himself or herself whether
services are necessary.
(g) In view of the person’s treatment history and current
behavior, the person is in need of involuntary outpatient services in
order to prevent a relapse or deterioration that would be likely to

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
21
result in serious bodily harm to himself or herself or others, or a
substantial harm to his or her well-being as set forth in s. 394.463(1).
(h) It is likely that the person will benefit from involuntary
outpatient services.
(i) All available, less restrictive alternatives that would
offer an opportunity for improvement of his or her condition have
been judged to be inappropriate or unavailable.
§ 394.4655(2), Fla. Stat.
Within 72 hours of arrival at facility, or if the 72-hour period ends on a weekend or
holiday then no later than the next working day thereafter, a petition for
involuntary inpatient placement must be filed by the receiving facility
administrator (or a petition for involuntary outpatient services may be filed) and
supported by the opinion of a psychiatrist — and the second opinion of a clinical
psychologist or another psychiatrist, both of whom have personally examined the
person within the preceding 72 hours — that the criteria for involuntary placement
are met. If the administrator certifies that a psychiatrist or clinical psychologist is
not available to provide the second opinion, the second opinion may be provided
by a licensed physician, a physician assistant, a social worker, or by a psychiatric
nurse, each as defined in the Baker Act. The second opinion may be conducted by
electronic means. The public defender will be appointed by the court to represent
the person unless the person is otherwise represented by private counsel. The state
attorney represents the state, rather than the petitioning facility administrator, as
the real party in interest in the proceeding. The court will order an independent
expert examination if requested by the person. § 394.467, Fla. Stat. The filing of a
petition authorizes the facility to retain the person pending completion of a hearing.
The court is required to hold the involuntary placement hearing within five court
working days unless a continuance is requested by the person with concurrence of
counsel and granted by the court. The court may appoint a magistrate to preside at
the hearing. One of the two professionals who executed the involuntary placement
petition must testify at the hearing. The person’s attendance at the hearing may be
waived and the person may refuse to testify. All testimony must be given under
oath and recorded. At the hearing, the court must consider testimony and evidence
regarding the person’s competence to consent to treatment. If the court finds that
the person is incompetent to consent to treatment, it must appoint a guardian
advocate.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
22
If the court concludes that the person, by clear and convincing evidence, meets the
criteria for involuntary inpatient placement, it must order the person, on an
involuntary basis for a period of up to 90 days, or up to six months at a state
facility:
to be retained at/transferred to or treated at an appropriate receiving or
treatment facility, or
to be treated by an appropriate receiving or treatment facility.
The Florida Supreme Court has defined “clear and convincing evidence” as that
which is “precise, explicit, lacking in confusion, and of such weight that it
produces a firm belief or conviction, without hesitation, about the matter in issue.”
See, e.g., Fla. Stand. Jury Instr. (Civil) 405.4.
A petition for involuntary outpatient services can be filed only by an administrator
of a receiving or treatment facility; if by a receiving facility it must be filed in the
county where the facility is located, and if by a state hospital administrator it must
be filed in the county where the person will be living. In either case, a service
provider must be designated to develop with the person a proposed treatment plan
(that meets specific criteria) for the court’s consideration and attach the proposed
plan to the petition. The service provider cannot propose, nor can the court order,
services unless they are: readily available for the person in the community, funded,
determined by an authorized mental health professional to be clinically
appropriate, and services which the service provider agrees to deliver. The order
shall be for a period of up to 90 days.
A person can be held at a receiving facility pending the court hearing on
involuntary outpatient services unless stabilized, in which case the person must be
released pending the hearing.
If material modifications later need to be made to the involuntary outpatient
services order or approved treatment plan and there are no objections, the court
must be notified. If there are objections to proposed material changes, the court
must consider whether or not to approve those changes.
If, in the clinical judgment of a physician, the person has failed or refused to
comply with involuntary outpatient treatment ordered by the court and efforts
were made to solicit compliance, and the person meets criteria for involuntary
examination, the person may be brought to a receiving facility. If the person
doesn’t meet the criteria for involuntary inpatient placement, the person must be

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
23
discharged from the receiving facility. The service provider must then determine if
modifications should be made to the existing treatment plan and try to continue to
engage the person in treatment.
N. Continued Involuntary Services
See § 394.4655(8), Fla. Stat.; Fla. Admin. Code R. 65E-5.285(4).
If a person continues to meet the criteria for involuntary outpatient services, the
administrator is required, at least ten days prior to the expiration of the period
during which the treatment facility is authorized to retain the person or a service
provider is authorized to treat the person, to file, in the court that issued the order
for involuntary outpatient services, a petition requesting authorization for
continued involuntary services.
The request must be accompanied by a statement from the person’s physician or
clinical psychologist justifying the request, a brief description of the person’s
treatment during the time he or she was receiving involuntary services, and an
individualized plan of continued treatment.
Hearings on petitions for continued involuntary outpatient services are judicial
and are conducted by the court. Unless the person is otherwise represented by
private counsel, he or she will be represented at the hearing by the public defender.
If at a hearing it is shown that the person continues to meet the criteria for
involuntary placement, the judge will sign the order for continued involuntary
placement for a period not to exceed 90 days. The same procedure can be repeated
prior to the expiration of each additional period the person is retained.
Hearings on petitions for continued involuntary inpatient placement are
administrative rather than judicial hearings and are conducted by an administrative
law judge. However, if the placement was ordered for less than six months, case
law holds that the Florida Division of Administrative Hearings (DOAH) and the
judiciary have concurrent jurisdiction for continued inpatient placement. See, e.g.,
W.M. v. State, 992 So. 2d 383 (Fla. 5th DCA 2008) (within six-month maximum
period of order for involuntary inpatient placement, circuit court has concurrent
jurisdiction over commitment proceedings; after six-month period expires, all
placements must be handled through administrative hearings). (In 2016 the
maximum period was reduced to 90 days except for state treatment facilities,
where the maximum period remains six months.)

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
24
O. Discharge of Persons on Involuntary Status
See § 394.469, Fla. Stat.; Fla. Admin. Code R. 65E-5.320.
Receiving and treatment facilities, as well as service providers, are required to
discharge a person at any time the person no longer meets the criteria for
involuntary placement, unless the person has transferred, by express and informed
consent, to voluntary status. If the person being discharged is under a criminal
charge, he or she must be transferred to the custody of the appropriate law
enforcement agency at the time of release.
P. Transfers
See § 394.4685, Fla. Stat.; Fla. Admin. Code R. 65E-5.310.
Transfers of persons with emergency medical conditions (including psychiatric and
substance abuse emergencies) from hospital emergency departments are governed
by the federal EMTALA “anti-dumping” or “hospital transfer” law (42 U.S.C.
§ 1395dd) and Florida’s hospital licensing law (chapter 395, Florida Statutes). If a
person requires transfer from a hospital emergency department that has provided
the person evaluation or treatment for an emergency medical condition to a Baker
Act receiving facility, the transfer must take place within 12 hours after the
condition has stabilized. Otherwise, under provisions of the Baker Act governing
transfers between designated receiving and treatment facilities, the following
transfers may occur:
Between public facilities, upon the request of the person or specified others
or upon the discretion of the department to meet the medical or mental
health treatment needs of the person or the availability of appropriate facility
resources;
From public to private facilities, upon the request of the person, guardian, or
guardian advocate, and upon acceptance of the person by the private facility;
From private to public facilities upon the request of the person, guardian,
guardian advocate, or private facility, and upon acceptance of the person by
the public facility. The public facility must respond to a request for the
transfer within two working days after receiving the request. The cost of
such transfer requested by a private facility is the responsibility of the
sending facility.
Between private facilities upon the request of the person, guardian, or

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
25
guardian advocate, and upon acceptance of the person by the facility to
which transfer is sought.
Q. Baker Act Oversight
See § 394.457, Fla. Stat.
“The Department of Children and Families (DCF) is designated the ‘Mental Health
Authority’ of Florida. The department and the Agency for Health Care
Administration (AHCA) shall exercise executive and administrative supervision
over all mental health facilities, programs, and services.” § 394.457(1), Fla. Stat.
DCF is required to report to AHCA any violation of the rights or privileges of
persons, or of any procedures provided under the Baker Act, by any facility or
professional licensed or regulated by AHCA. § 394.459(9), Fla. Stat. DCF is also
required to adopt rules establishing forms and procedures relating to the rights and
privileges of persons seeking mental health treatment from designated receiving
and treatment facilities. Unless designated by DCF, facilities are not permitted to
hold or treat persons on involuntary status.
Disability Rights Florida (formerly known as the Advocacy Center for Persons
with Disabilities) is a private nonprofit organization that receives federal funding
to protect and advocate for the rights of persons who have disabilities. Disability
Rights Florida prioritizes services to people with psychiatric disabilities in
institutional inpatient and residential treatment settings. Some services are
provided to those living independently as resources allow. Services to individuals
include information and referrals, self-advocacy support, technical assistance,
investigations into complaints of abuse, neglect and rights violations, support in
dispute resolution, negotiation and mediation, as well as advocacy services.
Statewide initiatives include workshops and trainings, education of policymakers,
systemic and legal advocacy, collaborative work on disability rights issues and the
monitoring of public programs and facilities. Disability Rights Florida has offices
in Tallahassee, Tampa, and Fort Lauderdale, from which it serves the entire state
of Florida.
Contact can be made through www.disabilityrightsflorida.org or 1-800-342-0823
(1-800-346-4127 TDD).
R. Immunity
See § 394.459(10), Fla. Stat.
Any person who acts in good faith in compliance with the provisions of the Baker

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
26
Act is immune from civil or criminal liability for his or her actions in connection
with the admission, diagnosis, treatment, or discharge of a person to or from a
facility, unless that person commits negligence.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
27
S. Statute and Rule Matrix — Florida Mental Health Act (Baker Act)
Florida Statute
Corresponding Fla. Admin. Code Rule
394.451 Short title
N/A
394.453 Legislative intent
N/A
394.455 Definitions
65E-5.100 Definitions
394.457 Operation and administration
65E-5.110 Delegation of Authority
65E-5.120 Forms
394.4572 Screening of mental health personnel
N/A
394.4573 Continuity of care management
system; measures of performance; reports
65E-5.130 Continuity of Care Management System
65E-5.1301 Transfer Evaluations for Admission to
State Mental Health Treatment Facilities from
Receiving Facilities
65E-5.1302 Admissions to State Treatment Facilities
65E-5.1303 Discharge from Receiving and Treatment
Facilities
394.4574 Department responsibilities for a
mental health resident who resides in an
assisted living facility that holds a limited mental
health license
N/A
394.458 Introduction or removal of certain
articles unlawful; penalty
N/A
394.459 Rights of patients
65E-5.140 Rights of Persons.
65E-5.150 Person’s Right to Individual Dignity
65E-5.160 Right to Treatment
65E-5.1601 General Management of the Treatment
Environment
65E-5.1602 Individual Behavioral Management
Programs
65E-5.170 Right to Express and Informed Consent
65E-5.1703 Emergency Treatment Orders
65E-5.180 Right to Quality Treatment
65E-5.1802 Maintenance of the Facility
65E-5.190 Right to Communication and Visits
65E-5.200 Right to Care and Custody of Personal
Effects

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
28
65E-5.210 Right to Vote in Public Elections
65E-5.220 Right to Habeas Corpus
65E-5.601 Operation and Administration of State
Mental Health Treatment Facilities
65E-5.602 Rights of Residents of State Mental
Health Treatment Facilities
394.4593 Sexual misconduct prohibited;
reporting required; penalties
N/A
394.4595 Florida statewide and local advocacy
councils; access to patients and records
(Defunded by 2010 Legislature)
N/A
394.4597 Persons to be notified; patient’s
representative
N/A
394.4598 Guardian advocate
65E-5.230 Guardian Advocate
65E-5.2301 Health Care Surrogate or Proxy
394.4599 Notice
N/A
394.460 Rights of professionals
N/A
394.461 Designation of receiving and
treatment facilities and receiving systems
65E-5.350 Eligibility Criteria and Procedures for
Designation of Baker Act Receiving Facilities
65E-5.351 Minimum Standards for Designated
Receiving Facilities
65E-5.352 Procedures for Complaints and
Investigations in Receiving Facilities
65E-5.353 Criteria and Procedures for Suspension or
Withdrawal of Designation of Receiving Facilities
394.4612 Integrated adult mental health crisis
stabilization and addictions receiving facilities
N/A
394.4615 Clinical records; confidentiality
65E-5.250 Clinical Records; Confidentiality
394.462 Transportation
65E-5.260 Transportation
65E-5.2601 Transportation Exception Plan
394.4625 Voluntary admissions
65E-5.270 Voluntary Admission
394.463 Involuntary examination
65E-5.280 Involuntary Examination
65E-5.2801 Minimum Standards for Involuntary
Examination Pursuant to Section 394.463, F.S
394.4655 Involuntary outpatient services
65E-5.285 Involuntary Outpatient Placement
394.467 Involuntary inpatient placement
65E-5.290 Involuntary Inpatient Placement
65E-5.300 Continued Involuntary Inpatient
Placement at Treatment Facilities
Treatment Facilities
394.46715 Rulemaking authority
N/A

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
29
*The following sections of Part I of chapter 394, Florida Statutes (Baker Act), have been
intentionally omitted from this matrix: 394.4781, “Residential care for psychotic and emotionally
disturbed children”; 394.4786, “Intent; 394.47865, South Florida State Hospital; privatization”;
394.4787, “Definitions; ss. 394.4786, 394.4787, 394.4788, and 394.4789”; 394.4788, “Use of
certain PMATF funds for the purchase of acute care mental health services”; and 394.4789,
“Establishment of referral process and eligibility determination.”
394.4672 Procedure for placement of veteran
with federal agency
N/A
394.468 Admission and discharge procedures
N/A
394.4685 Transfer of patients among facilities
65E-5.310 Transfer of Persons Among Facilities
394.469 Discharge of involuntary patients
65E-5.320 Discharge of Persons on Involuntary
Status
394.473 Attorney’s fee; expert witness fee
N/A
394.475 Acceptance, examination, and
involuntary placement of Florida residents from
out-of-state mental health authorities
N/A
394.4784 Minors; access to outpatient crisis
intervention services and treatment
N/A
394.4785 Children and adolescents; admission
and placement in mental facilities
N/A
394.47891 Military veterans and service
members court programs
N/A
65E-5.330 Training
65E-5.400 Baker Act Funded Services Standards

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
30
V. Maps of Administrative Entities Regions
A. Judicial Circuits and DCF Regions
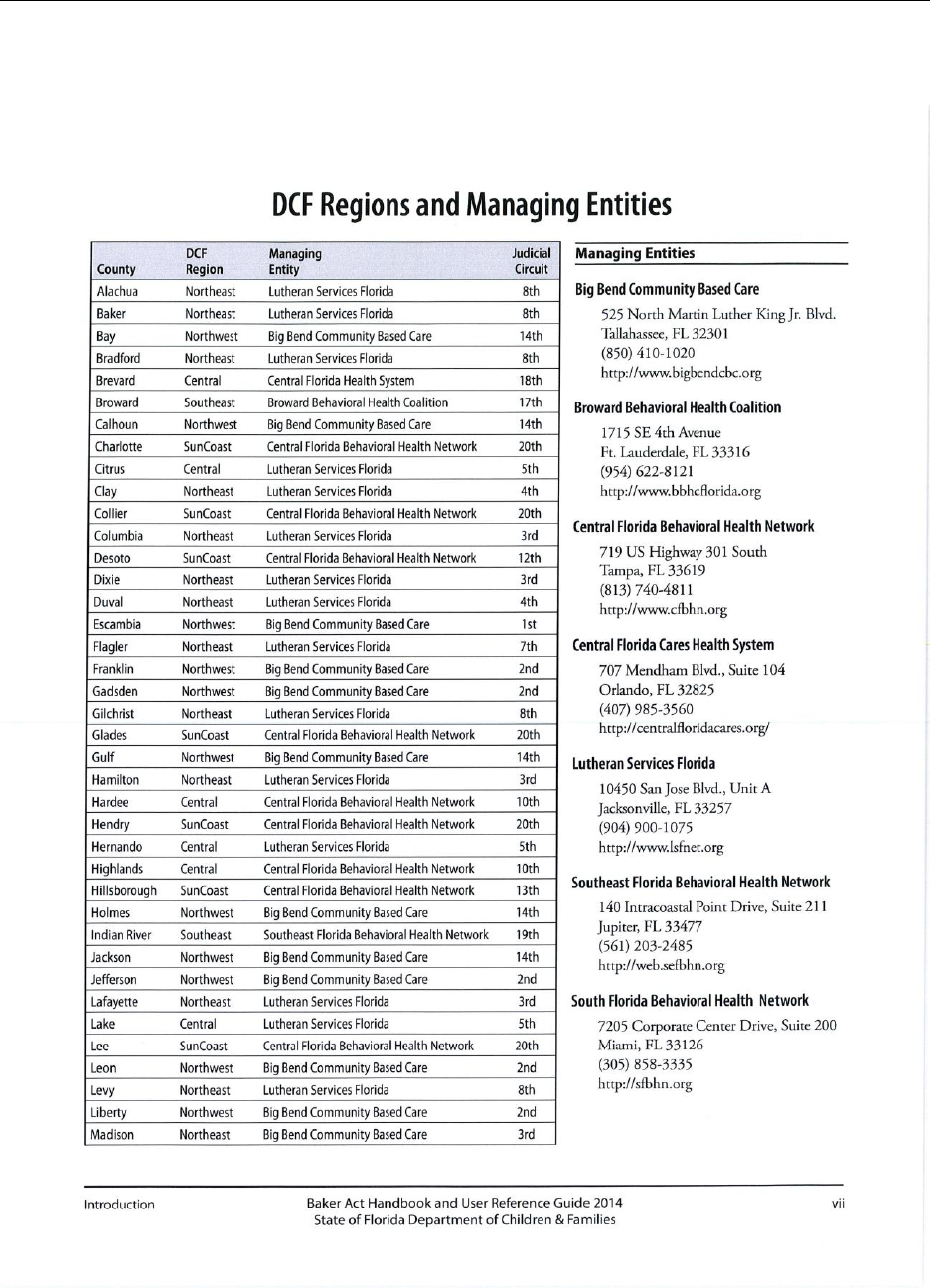
Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
31
B. DCF Regions and Managing Entities

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
32
C. Managing Entities

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
33
VI. Psychiatric Diagnoses and Treatment/Medication
A. Diagnoses
The Diagnostic and Statistical Manual of Mental Disorders (DSM) -IV, produced
by the American Psychiatric Association, noted five axes, or dimensions, to be
considered in assessment of psychological problems:
Axis I: Clinical Disorders
Axis II: Personality Disorders and Developmental Disabilities
Axis III: General Medical Conditions
Axis IV: Psychosocial and Environmental Problems
Axis V: Global Assessment of Functioning
However, in the DSM-5, released in 2013, the multiaxial diagnostic system was
removed and replaced with a simplified documentation approach. Former Axes I,
II, and III were combined into one list, with separate notations for former Axes IV
and V, covering psychosocial and environmental factors and disability.
“Mental illness” is defined in the Baker Act to mean “an impairment of the mental
or emotional processes that exercise conscious control of one’s actions or of the
ability to perceive or understand reality, which impairment substantially interferes
with the person’s ability to meet the ordinary demands of living. For the purposes
of this part, the term does not include a developmental disability as defined in
chapter 393, intoxication, or conditions manifested only by antisocial behavior or
substance abuse.” § 394.455(28), Fla. Stat. Impairments of the mental or emotional
processes that interfere with individuals’ ability to control their actions or to
perceive or understand reality are generally considered to be thought disorders or
mood disorders.
Thought disorders may include, but are not limited to, schizophrenia and
schizoaffective disorders:
Schizophrenia: a group of mental disorders involving disturbances of
thinking, mood, and behavior; may be an altered view of reality, may
include delusions and hallucinations. Mood changes include strange
emotional responses and inability to relate to others. Withdrawn, childlike,
and bizarre behavior may be noted. Schizophrenia is a chronic disorder of
both thought and mood. It interferes with the person’s ability to maintain
interpersonal relationships and to function in daily life. Antipsychotic
medications are used to help control the distressing signs and symptoms

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
34
suffered by an individual who has schizophrenia.
Schizoaffective disorder: combines major depressive episodes and manic
episodes with concurrent symptoms of schizophrenia.
Mood disorders are a category of mental health problems that includes a
disturbance in mood, usually deep sadness or indifference, excitement, or
irritability. These include bipolar disorder (previously called manic-depressive
disorder) and major depressive disorder. Mood stabilizers are primarily used to
treat bipolar disorder and to stabilize mood in other conditions. Antidepressants are
used to treat major depressive disorders and severe depression in other conditions.
Major depression: depressed mood with diminished interest or pleasure,
often with agitation, loss of concentration, insomnia or hypersomnia, fatigue,
feelings of worthlessness.
Manic episode: a distinct period of abnormally and persistently elevated,
expansive, or irritable mood, generally with decreased need for sleep,
pressured speech, flights of ideas, distractibility, excessive involvement in
pleasurable activities.
Bipolar disorder: cycling between depressive episodes and manic episodes.
B. Psychotherapeutic Medication
The term “psychotherapeutic medication” refers to all medications used to treat
brain disorders that result in primary disturbances in mental function. Depending
on the effect of the drug, treatment medications may be lumped into various
groups:
Antipsychotics
Antidepressants
Mood stabilizers
Hypnotics
Anti-anxiety medications
Properly used, psychotherapeutic medications can cause rapid and significant
improvement in the way the person feels and acts. However, psychotherapeutic

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
35
medications can have negative effects. The doctor must explain the likely benefits,
serious negative reactions, temporary and permanent side effects, and risk
associated with each proposed psychotherapeutic medication to the person, and to
any substitute decision maker when the individual is incompetent to make his or
her own treatment decisions.
The practice of prescribing psychotherapeutic medications has undergone
significant changes since they were first discovered in the early 1950s. From a
single medication, there are now many available medications for treating the
various psychiatric conditions. Any physician and any psychiatrist can prescribe
psychotherapeutic medications. An advanced registered nurse practitioner (ARNP)
or a physician assistant (PA) may also be able to prescribe under the supervision of
a physician. There have been many powerful advances made in the
pharmacological treatment of bodily illnesses and diseases, including the treatment
of mental illnesses. Medication advances have helped many persons with severe
mental illnesses to leave institutions and to progress toward recovery and
productive lives.
C. Allergies and Side Effects
1. Generally
Allergies are the body’s reaction to what it regards as “foreign” stimuli (allergen)
that cause reaction. Histamine release is at the root of many unpleasant body
events in such an allergic reaction. A few of these are listed below:
Runny nose and watery eyes. This is the classic hay fever. The histamine
release in the nose and eye tissues can be triggered by allergen particles in
the air that come into contact with the nasal passages and eyes.
Skin rashes. Rashes can affect a small or large percentage of the body.
Poison ivy oil, for example, causes histamine to be released. In response,
blood vessels dilate, fluid is released, and a rash or swelling forms.
Gastrointestinal disturbances. Although an allergic reaction such as hives or
swelling of the lips may occur after consuming something, GI symptoms
usually are not allergic reactions. Medication reactions can be widespread
and systemic. GI symptoms are usually a side effect, a result of the action of
serotonin change in the gut or in the brain (nausea).
Breathing difficulties. This is the most serious reaction. The histamine

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
36
release causes inflammation of the airways, which creates difficulty in
breathing. The inflammation can be severe enough to totally close the
airways. At this point the allergic reaction is truly life threatening.
It is possible to have any or all of these reactions to a medication. It is important to
clarify the difference between these allergic reactions and side effects. Most
symptoms that a person may describe as allergic reactions are often known side
effects. Most individuals are relieved to know the reaction is not a rare, deadly,
allergic response and that it is expected and treatable. An informed, reassured
person tolerates known side effects better and is more compliant. Depending on the
medication, a side effect may occur only a certain percentage of time (e.g., 5% vs.
20% is an important distinction).
If a medication appears to have caused an intolerable side effect, the doctor must
decide whether it is a side effect or an allergic reaction. A history of an allergic
reaction might eliminate a whole class of medications for possible use in the
individual. However, a serious side effect may eliminate only the specific offending
drug from consideration.
2. Antipsychotic Medications
There are older antipsychotic medications and newer classes of antipsychotic
medications; the latter are referred to as “atypicals.” Common side effects of
antipsychotics include:
Drowsiness and slowing, or activation and restlessness. The medication
might prevent a person from being totally alert. These side effects do not
always happen, and they usually lessen with time.
Weight gain.
Alteration in body temperature. The neuroleptic drugs can upset the
temperature-regulating center in the brain. A person who is taking a
neuroleptic may lose the ability to sweat, even to the point of heat stroke.
Some people, especially the elderly, are more at risk for hypothermia, or
lowered body temperature.
Abnormal involuntary movements. The person feels a compelling need to be
in constant movement. The person cannot sit still and may pace, squirm,
shuffle in place, tap the feet, drum the fingers, and more. The affected person
may talk about an “antsy” feeling of restless. These might be diagnosed as:

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
37
o Akathesia.
o Parkinsonism. This may include body tremors, slowed movements, and
postural changes. These go away when the medication is changed or the
dosage is reduced.
o Rigidity.
o Dystonias (a state of abnormal tonicity or prolonged tonic contractions).
Dystonia can be frightening and very painful. Every muscle in a leg, for
instance, may suddenly knot into hard cramps. Dystonia may also cause a
person’s tongue to stick out or make the eyes move rapidly. The person is
helpless to stop the muscle actions.
Blurred vision. This is generally a temporary side effect. Follow-up is
recommended. For people with narrow angle glaucoma, caution is
recommended.
Dry mouth or drooling. These conditions are uncomfortable but manageable.
Many medications used for relieving mental illness have these side effects.
Changes in blood pressure; for example, orthostatic hypotension, a
neuroleptic side effect, felt as being dizzy or faint when standing up. Falling
in a faint is rare. Normally, when someone stands or gets out of bed in the
morning, a reflex vasoconstriction occurs to maintain blood pressure.
Neuroleptics may slow this reflex for a person.
Constipation. This condition is uncomfortable but manageable. Many
medications used for relieving mental illness have this side effect.
Urinary retention or hesitancy. The person may become quite uncomfortable
with a full bladder.
Sexual dysfunction. This side effect is the most frequent reason given for no
longer taking helpful medication. The doctor may try to eliminate the effect
by lowering the dose or changing medications.
Sensitivity to sunlight. Thorazine is known to cause this, but it can also
happen with other antipsychotics. Some persons become much more
sensitive to the sun. Persons with this side effect may feel the skin burning
before the severe sunburn can be seen.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
38
Some adverse reactions possible from antipsychotics include:
Tardive dyskinesia (TD): a movement disorder where there are
uncontrolled facial movements and sometimes jerking or twisting
movements of other body parts. This condition may develop after several
years of taking antipsychotic medications. It occurs mostly in older adults.
The risk of developing TD is about 5% per year for people taking
“conventional” antipsychotics; e.g., four years of use would entail an
approximately 20% risk. For the “atypical” antipsychotics, the risk is
estimated to be 0.5% total, not per year. TD can be treated but not cured.
Neuroleptic Malignant Syndrome (NMS): a rare but very serious side
effect. Signs to watch for are muscle stiffness that occurs over one to three
days, a high fever, and confusion. If these symptoms occur, medical help
must be sought immediately.
3. Medications for Mood Disorders
For depression: Antidepressants are used in the treatment of depression, as well as
other psychiatric disorders. There are four major classes of antidepressants:
selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs),
monoamine oxidase inhibitors (MAOIs), and newer antidepressant medications.
Possible side effects are as follows:
Selective serotonin reuptake inhibitors (SSRIs), such as Prozac, Zoloft,
Paxil, Celexa, Lexapro, and others. Side effects of SSRIs may include
anxiety or nervousness, nausea and diarrhea, headache, insomnia, rash,
slight weight loss, and decrease in sexual ability or desire.
Tricyclic antidepressants (TCAs), such as Pamelor, Nopramin, Tofranil,
Elavil, and Anafranil, are older medications and are not used as much unless
in low doses for sleep or pain control, because of the potential for death. At
full doses, a person needs only a week’s worth of medication to die by an
intentional overdose. Also, because of interactions with some medications, a
person can develop cardiac arrhythmias. TCAs may have side effects
including:
o Sedation or activation/insomnia (because of possible activation, there can
be a temporary feeling of more anxiousness).
o Weight gain or weight loss.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
39
o Excessive sweating.
o Seizures – fairly rare; mostly the TCAs or bupropion.
o Headache.
o Blurred vision, worsening of narrow-angle glaucoma.
o Dry mouth.
o Cardiovascular effects, which may include hypertension or hypotension
depending on the medication. Increased heart rate is possible, but it is
usually benign.
o Gastrointestinal issues: nausea; diarrhea or constipation; decreased or
increased appetite.
o Urinary retention.
o Sexual dysfunction, including decreased desire or arousal.
Monoamine Oxidase Inhibitors (MAOIs), such as Parnate, Nardil, and
others, may cause side effects that include:
o Dizziness, rapid heartbeat, loss of sexual interest, and food interaction.
o Orthostatic hypotension.
o Dangerous interaction with food/drink/other medications. MAOIs react
with certain foods and alcoholic beverages, and some medications, to
produce a severe reaction which often does not appear for several hours
after taking the medication. This may include a dangerous rise in blood
pressure, as well as headache, nausea, vomiting, rapid heartbeat, possible
confusion, psychotic symptoms, seizures, stroke, and coma. Dietary
restrictions may be necessary. Foods that may be fatal include ripened
cheeses, fermented sausages, soy sauce, anchovies, pickled herring,
broad beans, and red wine. Hypertensive crisis (heart rate increases and
blood vessels constrict, producing a dramatically high blood pressure)
can occur when MAOIs are taken with certain foods or drugs. This can
be life threatening and is the major reason why MAOIs are not used more
often. The person must be alert to these drug and food interactions.
MAOI treatment should be re-evaluated as an option if the person is
unable to follow the necessary diet.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
40
Newer antidepressant medications, such as Effexor, Cymbalta, Wellbutrin,
Serzone, and Desyrel, are now in common use.
For bipolar disorder: Mood stabilizers — such as lithium, some anticonvulsant
medications, and some antipsychotic medications — are used primarily to treat
bipolar disorders and to stabilize mood in other conditions. Side effects of lithium
may include:
Nausea, stomach cramps, diarrhea, mild hand tremor, muscle weakness, dry
mouth, thirst, frequent urination, trouble concentrating, acne, and lethargy.
These are common but usually disappear after the person’s body becomes
accustomed to the lithium dosage.
Hand tremors. Simultaneous treatment with some types of antidepressants
can worsen this tremor. Heavy tremors may indicate lithium toxicity.
Renal toxicity. Lithium can reduce the kidney’s ability to concentrate urine
in some people. It is important to monitor kidney function.
Thyroid effects. Lithium therapy can induce hypothyroidism, causing weight
gain, fatigue, low energy, and slowed mental function, which may be
mistaken as being lithium side effects. Thyroid function testing and
monitoring for this complication and thyroid supplementation can be added
to the medication regimen.
Cardiac effects. Many cardiac dysfunctions are possible during lithium
intoxication. The main issue is to avoid toxicity. While a baseline ECG may
be done, it is not usually done, because the cardiac effects occur during toxic
high levels. Even a person with a normal baseline ECG can run into trouble
with toxicity. These cardiac effects can be life threatening. If pre-existing
cardiac disease is present, a consultation with a cardiologist is usually
recommended.
Lithium toxicity. Lithium can produce serious toxic reactions when there is
too little fluid in the blood, called dehydration. “Water pills,” caffeine, and
alcohol deplete blood fluids. Other factors that can reduce the body’s fluids
and increase lithium levels are exercise with excessive sweating, fever, flu,
diarrhea, vomiting, decrease in water intake, and slimming diets. A low
sodium diet will increase lithium levels because the kidneys need salt to
function well. During lithium therapy, the body must have enough salt and
10-12 glasses of water every day to prevent the buildup of lithium to toxic

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
41
levels. Most diuretics and NSAIDS (ibuprofen or Motrin and naproxen or
Aleve, for example) have an effect on the kidneys to retain more lithium,
creating toxic levels. Symptoms of lithium toxicity may include diarrhea,
vomiting, nausea, slurred speech, convulsions, confusion, drowsiness, and
severe trembling. The higher the level of lithium in the blood, the worse
these symptoms become. The doctor should be notified immediately if these
symptoms appear.
Medications can change lithium levels. Tetracycline increases lithium blood levels;
many asthma aids and certain headache remedies can lower them.
4. Anti-Anxiety Medications
Benzodiazepines are widely used to treat anxiety symptoms and sleep problems in
adults, and research shows some support for their use in children and youth. These
medicines are subject to potential nonmedical misuse. They can contribute to
excessive sedation and intoxication, especially when combined with alcohol. Side
effects may include dizziness, light-headedness, drowsiness, clumsiness,
unsteadiness, amnesia, forgetfulness, and slurred speech. Tolerance can occur and
the initial sedation may go away. But persons in safety-sensitive positions cannot
take these medications because there can still be slowed reaction times and
memory can be diminished. The memory impairment can be subtle or it can be
obvious. The elderly are especially prone to all the side effects and have an
increased incidence of falls and memory impairment.
C. Importance of Medication Compliance
All medications have the potential of producing dramatic significant benefits for an
individual. If the person does not take the medication, for whatever reason, its
benefit will not be felt. Noncompliance with medication (i.e., failing to regularly
follow the prescribed medication schedule necessary for the effectiveness of the
medication) is the major reason for re-admissions to crisis stabilization units
(CSUs) and hospitals. A person’s decompensation (returning to the previous
unmedicated state of illness) carries a high cost to the person in the form of
psychological pain, frustration, and worst case, death. It is also costly to society in
the form of increased health care expense.
Side effects are a major reason for medication noncompliance. Improved
medication compliance occurs when the person is stable and feels fine while taking
medications. The danger occurs when the person has been discharged from the
hospital and feels that he/she is “healed” and no longer sees the need for taking the

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
42
medication.
Chronic illnesses like hypertension and diabetes, for example, require persons to
take medication for the rest of their lives. Mental illness is also an illness that may
require life-long medications. Fortunately, in modem society there is no longer any
stigma in taking medications for chronic illnesses like diabetes. However, too
many people feel differently about medications taken to treat mental illnesses. This
stigma, sometimes expressed even by family members, may discourage the person
from taking the needed medication. For persons needing such medications, the
failure to sustain medication compliance is likely to cause repeated cycles of
hospitalization with an accompanying lowering of mental abilities.
D. Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (formerly known as electroshock therapy), whereby
seizures are electrically induced to provide relief from psychiatric illnesses, has
become a standard psychiatric treatment. The following is taken from the Mayo
Clinic Electroconvulsive therapy (ECT) webpage.
ECT is used to treat:
Severe depression, particularly when accompanied by detachment
from reality (psychosis), a desire to commit suicide, or refusal to
eat.
Treatment-resistant depression, a severe depression that doesn’t
improve with medications or other treatments.
Severe mania, a state of intense euphoria, agitation or
hyperactivity that occurs as part of bipolar disorder. Other signs of
mania include impaired decision making, impulsive or risky
behavior, substance abuse, and psychosis.
Catatonia, characterized by lack of movement, fast or strange
movements, lack of speech, and other symptoms. It’s associated
with schizophrenia and some other psychiatric disorders. In some
cases, catatonia is caused by a medical illness.
Agitation and aggression in people with dementia, which can be
difficult to treat and negatively affect quality of life.
ECT may be a good treatment option when medications aren’t
tolerated or other forms of therapy haven’t worked. In some cases
ECT is used:

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
43
During pregnancy, when medications can’t be taken because they
might harm the developing fetus
In older adults who can’t tolerate drug side effects
In people who prefer ECT treatments over taking medications
When ECT has been successful in the past
Although ECT is generally safe, risks and side effects may include:
Confusion. Immediately after an ECT treatment, you may
experience a period of confusion that can last from a few minutes
to several hours. You may not know where you are or why you’re
there. You may be able to return to normal activities right away, or
you may need to rest for several hours after treatment. Rarely,
confusion may last several days or longer. Confusion is generally
more noticeable in older adults.
Memory loss. ECT can affect memory in several ways. You may
have trouble remembering events that occurred before treatment
began, a condition known as retrograde amnesia. It may be hard to
remember things in the weeks or months leading up to treatment,
although some people do have problems with memories from
previous years as well. You may also have trouble recalling events
that occurred during the weeks of your treatment. And some
people have trouble with memory of events that occur even after
ECT has stopped. These memory problems usually improve within
a couple of months.
Physical side effects. On the days you have an ECT treatment, you
may experience nausea, vomiting, headache, jaw pain, muscle ache
or muscle spasms. These generally can be treated with
medications.
Medical complications. As with any type of medical procedure,
especially one that involves anesthesia, there are risks of medical
complications. During ECT, heart rate and blood pressure increase,
and in rare cases, that can lead to serious heart problems. If you
have heart problems, ECT may be more risky.
VII. Adult Mental Health System of Services and Support
The following is taken from the DCF webpages.
The kinds and amounts of publicly funded mental health services

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
44
available in an area are limited by the amount of funding available in
that area. The following list shows the kinds of services that can be
provided to people who meet the adult mental health priority
population criteria.
Florida’s service array can be put into the three broad categories:
treatment, rehabilitation, and support services. However, many of the
services identified in any one of the three categories could also be
identified in one or more of the others. Assertive Community
Treatment and Comprehensive Community Service Teams are two
examples of services falling into more than one broad category.
Treatment
Rehabilitation
Support
TREATMENT
Treatment is a systematic approach to relieving the primary symptoms
and life results of mental illnesses. Treatment is intended to lessen and
remove the symptoms of mental illnesses, prevent later reoccurrence
or worsening of symptoms, and help individuals cope with symptoms
when medications and other treatments are only partially successful.
Treatment typically contains four elements:
Medications;
Individual therapy
Crisis intervention; and when necessary
Psychiatric hospitalization.
Florida considers the following services as treatment options:
Florida Assertive Community Treatment (FACT)
Florida Assertive Community Treatment Team (FACT) services are
available on a statewide basis and are modeled after the original
Programs of Assertive Community Treatment (PACT) in Madison,
Wisconsin. There are 31 FACT teams across the state. Each team is
staffed with a program psychiatrist, peer specialist, and team leader,
with a total staffing of 12.3 Full Time Equivalents (FTEs). Each team
has an independent advisory committee to assist the team develop
resources in its community. FACT is unique in Florida - at present it

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
45
is the only service available that offers a housing, medication, and
flexible funding subsidy to enrolled individuals. Each team is
mandated to serve no more than 100 individuals. FACT guidelines
have recently been revised so that enhancement funds can be used for
an expanded variety of services and supports. FACT is not a self-
directed program, and participants do not receive fixed budget
amounts for discretionary use. Clinical services are provided entirely
within the FACT Team - that’s what makes it unique. However, an
expansion of acceptable uses for enhancement funds will provide
participants greater opportunities for articulating and achieving their
individualized recovery goals.
Assessment
These services assess, evaluate, and provide assistance to individuals
and families to determine level of care, motivation, and the need for
services and supports. Assessment also assists individuals and
families in identifying their strengths.
Integrated Treatment for Individuals with Co-occurring Disorders
Florida understands that many adults in our priority populations have
both a mental illness and substance use disorder. A good assessment
and treatment for both at the same time is required so that people can
get better. Making sure contracted providers in the public mental
health and substance abuse systems can do a thorough assessment and
provide or arrange for needed treatment is a current priority for the
state.
Crisis Support / Emergency
These are outpatient services generally available twenty-four hours
per day, seven days per week, or some other specific time period, to
intervene in a crisis or provide emergency care.
Crisis Stabilization Unit (CSU)
This is an emergency care intervention, available twenty-four hours
per day, seven days per week. People can go to a CSU, or be brought
there by police, friends or relatives. They are assessed and may be
admitted voluntarily or against their wishes until the mental health
emergency is over.
Health Services (see also Medical Services, which follows later in this
section)

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
46
Florida’s publicly-funded community mental health system does not
directly purchase other types of health services. However, as part of
the assessment process, case managers pursue needed health care
(e.g., medical services other than psychiatric; dental care; eye care /
glasses) by using resources available in the community. These efforts
could include referrals to local physicians who accept Medicaid,
county public health units, or physicians who provide free service
time. The issues are varied and can range from routine vaccinations to
treatment for diabetes or other life-threatening illnesses.
In-Home And On-Site Services
These are therapeutic services and supports rendered in non-mental
health provider settings, such as in nursing homes, assisted living
facilities (ALFs), residences, schools, detention centers, commitment
settings, foster homes, and other community settings.
Inpatient Services
Inpatient services are services provided in hospitals licensed under
Chapter 395, F.S., as general hospitals and psychiatric specialty
hospitals. They are designed to provide intensive treatment to persons
exhibiting violent behaviors, suicidal behaviors and other severe
disturbances due to substance abuse or mental illness.
Intervention - Individual or Group
These services focus on reducing risk factors generally associated
with the progression of substance abuse and mental health problems.
Intervention is accomplished through early identification of persons at
risk, performing basic individual assessments, and providing
supportive services that emphasize short-term counseling and referral.
These services are targeted toward individuals and families.
Medical and Dental Services
Medical services provide primary medical care, therapy, and
medication administration. This includes a psychiatric mental status
assessment, and the administration of psychiatric medications. For
adults, medical services are usually provided on a regular schedule
with arrangements for non-scheduled visits during times of increased
stress or crisis.
Case managers also make an assessment of the need for medical and
dental services (see also Health Services in this section, above), and

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
47
referrals are made to physicians or dentists in the community who
accept Medicaid. People who do not have Medicaid are referred to
whatever medical or dental services are available locally. These
resources may include Regional Workforce Board One-Stop Centers
and public health departments, medical societies, individual
physicians, and hospitals. The Department pays for medical and
dental care for individuals living in state mental health residential
treatment facilities.
Outpatient-Individual and Group
This cost center provides a therapeutic environment that is designed to
improve the functioning or prevent further deterioration of persons
with mental health and/or substance abuse problems. Outpatient
services are usually provided on a regularly scheduled basis by
appointment, with arrangements made for non-scheduled visits during
times of increased stress or crisis.
Residential Level 1
These are licensed services that provide structured, live-in, non-
hospital settings with 24-hour supervision daily. There is a nurse on
duty in these facilities at all times. For adult mental health, these
services include two different kinds of programs: group homes and
short-term residential treatment services. Group homes are for
residents who may require longer lengths of stay. These facilities offer
nursing supervision provided by, at a minimum, licensed practical
nurses, 24 hours a day, seven days per week.
Residential Level 2
These are licensed, structured rehabilitation-oriented group facilities
that have 24-hour a day, seven days per week supervision. Level 2
facilities are for persons who have significant deficits in independent
living skills and need extensive support and supervision.
Short-term Residential Treatment (SRT)
These individualized, acute, and immediately sub-acute care services
provide intensive mental health residential and rehabilitative services
24 hours a day, seven days per week. These services must meet the
needs of individuals who are experiencing an acute or immediately
sub-acute crisis and who, in the absence of a suitable alternative,
would require hospitalization. SRT services provide intensive
residential treatment for individuals in need of acute care for up to 120

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
48
days.
REHABILITATION
Rehabilitation is the process of helping individuals minimize the
effects of mental illnesses on major role skills and develop greater
competencies in employment, activities of daily living, social
performance. They promote recovery.
Florida considers the following services as rehabilitation options:
Aftercare services
These services include but are not limited to relapse prevention, and
are a vital part of recovery in every service level. Aftercare activities
include customer participation in daily activity functions that were
adversely affected by mental illness and/or substance abuse
impairments. New directional goals such as vocational education or
rebuilding relationships are often priorities. Relapse prevention
education is essential in assisting the customer’s recognition of
triggers and warning signs of regression. Aftercare services help
families and pro-social support systems reinforce a healthy living
environment.
Comprehensive Community Service Team - Individual or Group
Comprehensive Community Service Team (CCST) services render
assistance in identifying goals and making choices to promote resiliency and
facilitate recovery for adults and children with mental illnesses. The services
take place in either an outpatient or community setting. For individuals with
mental health problems, recovery is the personal process of overcoming the
negative impact of psychiatric illness despite its continued presence. CCST
services are intended to restore the individual’s function and participation in
the community. The services are designed to assist and guide individuals in
reconnecting with society and rebuilding skills in identified roles in their
environment. The focus is on the individuals’ strengths and resources as well
as their readiness and phase of recovery. A team approach of services will be
used to guide and support the adults and children served with development
of a recovery plan focusing on the areas of individual and family living,
learning, working, and socialization activities. Any therapy is brief and
oriented toward skill building. Services provided include Assessment, Case
Management, Intensive Case Management, Supported Housing, Aftercare,
Supported Employment, Outreach, Outpatient, In-home/On-site,

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
49
Intervention, Information and Referral, Prevention, Prevention/Intervention
and other transition and non-traditional support services as negotiated by the
Department and the provider.
Day-night Services
These services provide a structured schedule of non-residential services for
three (when Medicaid funded) or four or more consecutive hours per day.
This may include delivery of services during evening hours. Activities for
children and adult mental health programs are designed to assist individuals
to attain the skills and behaviors needed to function successfully in the
living, learning, work, and social environments of their community.
Generally, a person receives three or more services a week. Activities for
substance abuse programs emphasize rehabilitation, treatment, and education
services, using multidisciplinary teams to provide integrated programs of
academic, therapeutic, and family services.
Educational Services
Educational activities are provided in a variety of service settings. These
include providing educational assessments; day treatment; case
management; drop-in, self-help centers; and the Florida Assertive
Community Treatment Team (FACT) program’s specific educational service
entitled Education, Support and Consultation to Family, and Other Major
Supports. With the exception of the FACT-specific service for education,
most educational services may be provided on-site of providers, with
instructors funded through local school boards.
Florida Self-Directed Care
Florida Self-Directed Care is available in two parts of the state - the
Jacksonville area and Southwest Florida. People eligible for public mental
health services are given a budget and can choose the services and supports
they want to buy, and from whom they will buy them. Their purchases have
to be linked to a personal recovery plan, and some of the services have to be
clinical. This program has served as a national model for similar efforts in
other states.
Supportive Housing
Supported housing/living services are designed to help people with
substance abuse or psychiatric disabilities find and keep living arrangements
of their choice. They also provide services and supports to ensure continued
successful living in the community. The goal of Supportive Housing is to

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
50
ensure that everyone has the opportunity to live as independently as
possible.
Supportive Employment
Supported Employment programs help people get or get back to productive
employment. These services are community-based and take place in an
integrated work setting, which provides regular contact with non-disabled
co-workers or the public. A job coach provides long-term ongoing support
as needed to give an individual every opportunity to maintain employment.
Mental Health Clubhouse
Clubhouses are structured, community-based interventions where members
can strengthen and/or regain interpersonal skills, get psycho-social therapy
toward rehabilitation, develop the environmental supports necessary to
thrive in the community, meet employment and other life goals, and recover
from the bad effects of a mental illness. Services are typically provided in a
community-based program with trained staff and members working as teams
to address the person’s life goals and to perform the tasks necessary for the
operations of the program. Clubhouses use a holistic approach focusing on a
person’s strengths and abilities while challenging that individual to pursue
chosen life goals. Florida is invested in the International Center for
Clubhouse Development (ICCD) model. Though there are other programs
promoting employment across the system, Florida strongly encourages the
ICCD approach and certification.
Residential Level 3
These are licensed facilities, structured to provide 24-hour a day, seven days
per week supervised residential alternatives to persons who have developed
a moderate functional capacity for independent living. For adults with
serious mental illnesses, these are supervised apartments.
SUPPORT
Support is practical, hands-on assistance to help people handle the
necessities of daily living and assist them in their recovery process.
Florida considers the following services as support options:
Case Management

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
51
Case managers help people identify their needs, plan their services, link
them to the service system, coordinate the various system components,
monitor service delivery, and evaluate the effect of the services received.
Intensive Case Management
Same as above. Intensive case management is typically offered to persons
who are being discharged from a state mental health treatment facility or
crisis stabilization unit and in need of more support. They may also have
more needs for things like rental or regular transportation assistance to help
them live in the community.
Day Care Services
Day care services provide a structured schedule of activities for four hours
or more consecutive hours per day for children of persons who are
participating in a substance abuse or mental health day-night service or
residential service.
Drop-In / Self-Help Centers
These centers are intended to provide a range of opportunities for persons
with serious and persistent mental illnesses to independently develop,
operate, and participate in social, recreational, and networking activities.
Many are operated by consumers of mental health services.
Incidental Expenses
These may include the cost of medications that can’t be paid for any other
way, as well as things like clothing, medical care, educational needs,
housing subsidies, or one-time expenses like the cost of turning on utilities
for a new place to live.
Information and Referral
Provides information about resources in the community and
agencies/organizations that offer assistance; links people who need
assistance with people who can provide it.
Prevention
Prevention services involve strategies that avoid or put off the development
of substance abuse and mental health problems. They include increasing
public awareness through information, education, and alternative-focused
activities.
Residential Level 4

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
52
The facility may have less than 24 hours a day, seven days per week on-
premise supervision. This is the least intensive level of residential care and is
primarily a support service. For adults with serious mental illnesses, this
includes satellite apartments, satellite group homes, and therapeutic foster
homes.
Respite Services
Respite service is an organized program designed to sustain the family or
other primary care-giver by providing time-limited, temporary relief from
the ongoing responsibility of care giving.
Room and Board with Supervision Levels 1-3
This pays room and board costs for people living in Medicaid-funded
residential programs. Medicaid pays for the clinical services, and the SAMH
program pays for the rest.
VIII. Children’s Mental Health System of Services and Support
The following is taken from the DCF webpages.
The [DCF] Children’s Mental Health Program is a coordinated
network of community-based services and supports that is youth-
guided and family-driven to produce individualized, evidence-based,
culturally and linguistically competent outcomes that improve the
lives of children and their families.
This program provides funding for in-home and community based
outpatient services, crisis services and residential treatment (including
psychiatric residential treatment facilities, Therapeutic Foster Care,
and Therapeutic Group Homes provided through joint Medicaid and
Mental Health Program contracts with behavioral health managed
entities and providers).
The program also provides coordination and management of the
Juvenile Incompetent to Proceed (JITP) program. The system requires
that services are individualized, culturally competent, integrated, and
coordinated. The aim is to provide a smooth transition from children’s
mental health to the adult mental health system for continued age-
appropriate services and supports. These services are designed to
build resilience and to prevent the severity, duration and disabling
aspects of children’s mental and emotional disorders.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
53
Services in the Children’s Mental Health Program
Service Planning and Coordination - Multi-disciplinary planning
teams, often called Family Service Planning Teams are family-
focused and community-based, and serve as a focus for identifying
supports and service planning for the family.
Residential Treatment – In some cases, residential treatment may be
necessary for some children. . . . Section 394.4781, Florida Statutes,
authorizes the Department to pay a portion of the costs associated
with residential care for children who have been diagnosed with
severe emotional disturbance, who are recommended to need a
residential level of mental health treatment by a Florida licensed
psychologist or psychiatrist, and who are not eligible for public or
private insurance.
The Department has very limited state General Revenue funds to
purchase residential mental health treatment for children who qualify
and is required to review applications monthly to approve or
disapprove each application in accordance with:
The severity of the problems of the child
The financial means of the family
The availability of the needed residential care
Available funds
Each DCF region has a procedure for reviewing applications for
residential mental health treatment and determining whether
placement in such a setting is the least restrictive, most beneficial
treatment alternative for the child. Many children, even those with
severe conditions, can be more effectively served in the community
with a specially designed program of “wraparound” services for the
child and family.
The goal of mental health treatment is to assist the child to live
successfully in their community and with their families. Therefore, the
placement of a child into residential mental health treatment should be
made only after careful consideration is given to less restrictive
treatment alternatives. Regions use a staffing process involving the
child and parents or other caregivers and a multiagency group of
professionals to consider the strengths and needs of the child and

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
54
family and developed a service plan to enable the child either to
remain at home or to return home from the treatment setting as soon
as possible. Only if the needed services cannot be provided in a less
restrictive environment is placement in a residential mental health
treatment program considered.
If residential treatment is approved by the [DCF] regional office, it
must then be determined if funding is available to place the child. All
available sources of funds are explored, including insurance (public
and private) and cost-sharing with the family, the local school district,
and other programs involved with the child, such as child welfare and
juvenile justice.
Family Inclusion - Florida’s Children’s Mental Health program is
fully committed to the value of family involvement. We strongly
believe that families must be included in all decisions regarding the
planning and provision of mental health services for their children. It
is the responsibility of all who work within the system of care to make
every effort to assure families have a strong voice and are actively
involved in the decisions being made that impact their child and
family.
Additionally, we are equally committed to including families in
policy-making. Since families have personal experience with the
service delivery system, they provide a reality base for policymakers,
a fresh perspective on how the system of care is serving their children,
and ideas for improving services. . . .
Medicaid Eligibility
Medicaid - Children may be eligible for Medicaid. Medicaid-covered
services can be provided only to Medicaid-eligible children, only by
Medicaid-enrolled providers. . . .
Juvenile Incompetent to Proceed Program
JITP - Florida’s Juvenile Incompetent to Proceed (JITP) Program
provides competency restoration services to juveniles who have been
charged with a felony prior to their 18th birthday and do not have the
ability to participate in legal proceedings due to their mental illness,
[intellectual disability], or autism.

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
55
IX. Glossary of Common Definitions, Acronyms, and Abbreviations
Acute: sudden and/or severe
Advance directive: a witnessed written document described in section 765.101(1),
Florida Statutes
Adverse reaction: sudden physical or mental crisis as a reaction to a medication
Agent: medication, drug
AHCA: Agency for Health Care Administration
Akathesia: inability to sit still, urgent need for movement to relieve anxiety
Anticonvulsant: medication to prevent or lessen seizures
Assessment: “the systematic collection and integrated review of individual-
specific data. It is the process by which individual-specific information such as
examinations and evaluations are gathered, analyzed, monitored and documented
to develop the person’s individualized plan of treatment and to monitor recovery.
Assessment specifically includes efforts to identify the person’s key medical and
psychological needs, competency to consent to treatment, patterns of a co-
occurring mental illness and substance abuse, as well as clinically significant
neurological deficits, traumatic brain injury, organicity, physical disability,
developmental disability, need for assistive devices, and physical or sexual abuse
or trauma.” Fla. Admin. Code Rule 65E-5.100(2).
BA-8: order for involuntary inpatient placement – recommended (short for form
CF-MH form 3008)
BA-32: petition for involuntary inpatient placement – recommended (short for
form CF-MH 3032)
BA-52A: initiation form used by law enforcement for involuntary examination –
mandatory (short for form CF-MH 3052a)
BA-52B: initiation form used by authorized mental health professionals for
involuntary examinations – mandatory (short for form CF-MH 3052b)
Baker Act: Florida’s Mental Health Act; chapter 394, part I, Florida Statutes
Behavioral Therapy: talk therapy directed at changing thinking habits (like

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
56
rational emotive therapy)
Chronic: constant condition, or always returning
Compliance: taking medication exactly as planned
Continued involuntary placement: involuntary placement that is subsequent to
the original involuntary placement hearing and order
Court: unless otherwise specified, the circuit court
Crisis: a peak in an illness
Decanoate: long duration medication injected into muscle
Decompensation: returning to the previous unmedicated state of illness
Delusion: a firmly held belief, not shared by other people, and not changed by
logic
Depression: mood condition of uncontrollable sadness, worry, slowed motion
Disassociate: to become separated from reality
Discharge plan: “the plan developed with and by the person which sets forth how
the person will meet his or her needs, including living arrangements,
transportation, aftercare, physical health, and securing needed psychotropic
medications for the post-discharge period of up to 21 days.” Fla. Admin. Code
Rule 65E-5.100(4).
Disorder: permanent medical problem (like diabetes or mania)
Dosage: how much medication is taken at a time
DSM: Diagnostic and Statistical Manual
Dysfunction: low or missing ability
Dystonia: muscle stiffness, a painful side effect
ECT: electroconvulsive therapy
ED: emergency department or emergency room

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
57
Edema: swelling due to fluid retention
Efficacy: how well a treatment works for a person
Emergency medical condition (EMC): a medical condition with acute symptoms
sufficiently severe that without immediate medical attention the condition could
result in serious harm to patient health, serious impairment to bodily functions, or
serious dysfunction of any bodily organ or part (defined in section 395.002(8),
Florida Statutes).
Emergency treatment order (ETO): “a written emergency order for psychotropic
medications . . . or a written emergency order for seclusion or restraint.” Fla.
Admin. Code Rule 65E-5.100(5).
Episode: event; usually one in a series
EPS: extrapyramidal symptoms; a side effect of medication formulation: the
combination of chemicals in a particular medication (see generic)
Examination: “the integration of the physical examination under Section
394.459(2), F.S., with other diagnostic activities to determine if the person is
medically stable, and to rule out abnormalities of thought, mood, or behavior that
mimic psychiatric symptoms but are due to nonpsychiatric medical causes such as
disease, infection, injury, toxicity, or metabolic disturbances. Examination includes
the identification of person-specific risk factors for treatment such as elevated
blood pressure, organ dysfunction, substance abuse, or trauma.” Fla. Admin. Code
Rule 65E-5.100(6).”
Express and informed consent: “consent voluntarily given in writing, by a
competent person, after sufficient explanation and disclosure of the subject matter
involved to enable the person to make a knowing and willful decision without any
element of force, fraud, deceit, duress, or other form of constraint or coercion.”
§ 394.455(15), Fla. Stat.
F/U: follow up
Generic: medication made by other companies; may vary in strength compared to
“brand”
Hallucination: hearing, seeing, touching, smelling or tasting unreal input
Health care proxy: “a competent adult who has not been expressly designated by

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
58
an advance directive to make health care decisions for a particular incapacitated
individual, but is authorized pursuant to Section 765.401, F.S., to make health care
decisions for such individual.” Fla. Admin. Code Rule 65E-5.100(7).
Health care surrogate: “any competent adult expressly designated by a
principal’s advance directive to make health care decisions on behalf of the
principal upon the principal’s incapacity.” Fla. Admin. Code Rule 65E-5.100(8).
Hematological: blood tests
Hypnotic: very calming
Hypothermia: body temperature drops below normal
ICD: International Classification of Diseases
IM: intramuscular injection of a medication
Incompetent to consent to treatment: “a state in which a person’s judgment is so
affected by a mental illness or a substance abuse impairment that he or she person
lacks the capacity to make a well-reasoned, willful, and knowing decision
concerning his or her medical, mental health, or substance abuse treatment.”
§ 394.455(21), Fla. Stat.
Interaction: one agent may change the way another one works
Involuntary examination: an examination performed under section. 394.463,
Florida Statutes, to determine if an individual qualifies for involuntary inpatient
treatment under section 394.467(1) or involuntary outpatient services under section
394.4655(2). § 394.455(34), Fla. Stat.
Involuntary placement: either involuntary outpatient services pursuant to section
394.4655, Florida Statutes, or involuntary inpatient treatment pursuant to section
394.467
IOP or AOT: involuntary outpatient treatment or assisted outpatient treatment,
which are synonymous; the former is used in Florida.
Lethargy: feeling of great tiredness
Maintenance dosing: dosing to prevent the person from having an acute episode
of the disorder

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
59
Malaise: tiredness, vague feeling of illness
Mania: mood condition of uncontrollable physical or mental activity
Marchman Act: Florida’s substance abuse impairment law; chapter 397, Florida
Statutes. A Baker Act & Marchman Act Comparison document is available on the
DCF website.
Medication regimen: overall medications, including kinds and amounts of each
drug
Mental illness: “an impairment of the mental or emotional processes that exercise
conscious control of one’s actions or of the ability to perceive or understand
reality, which impairment substantially interferes with the person’s ability to meet
the ordinary demands of living. For the purposes of this part, the term does not
include a developmental disability as defined in chapter 393, intoxication, or
conditions manifested only by antisocial behavior or substance abuse.”
§ 394.455(28), Fla. Stat.
Monitoring: watching and recording event
Mood: emotional state
Neuroleptic: a drug designed to treat an illness by calming the brain
NMS: Neuroleptic Malignant Syndrome, a rare and dangerous physical reaction to
a psychotherapeutic medication
Noncompliance: inability or refusal to take treatment as prescribed
NOS: not otherwise specified
Obsession: unshakable focus on an idea, emotion or action (like jealousy)
Obsessive compulsive disorder (OCD): brain disruption causing repetitive ritual
actions to relieve feelings of anxiety
Oculogyric: eyes are constantly moving
Orthostatic hypotension: sudden drop in blood pressure
Paranoia: unbreakable, rigid belief of being persecuted
Polydipsia: drinking too much fluid, from being constantly thirsty

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
60
Polypharmacy: use of two or more medications for the same problem at the same
time
PRN: pro re nata; take when needed. “[A]n individualized order for the care of an
individual person which is written after the person has been seen by the
practitioner. . . . A PRN order shall not be used as an emergency treatment order.”
Fla. Admin. Code Rule 65E-5.100(11).
Psychomotor: movements caused by brain activity, not conscious will
Psychosis: loss of contact with reality, with delusions and hallucinations
Psychotherapeutic medications: medications used to alter abnormal thinking,
feelings, or behavior
Psychotherapy: method of treating mental disorders by discussion and interaction
Receiving facility: a facility designated by DCF to receive and hold individuals
involuntarily under emergency conditions or for psychiatric evaluation and provide
short-term treatment; does not include county jails
Rehabilitation: bringing a person back to normal skills
SAMH: substance abuse and mental health program of DCF
Schizophrenia: a group of mental disorders involving disturbances of thinking,
mood and behavior; may be an altered view of reality, may include delusions and
hallucinations. Mood changes include strange emotional responses and inability to
relate to others. Withdrawn, childlike, and bizarre behavior may be noted.
Service provider: “a receiving facility, a facility licensed under chapter 397, a
treatment facility, an entity under contract with the department to provide mental
health or substance abuse services, a community mental health center or clinic, a
psychologist, a clinical social worker, a marriage and family therapist, a mental
health counselor, a physician, a psychiatrist, an advanced registered nurse
practitioner, a psychiatric nurse, or a qualified professional as defined in s. 39.01.”
§ 394.455(44), Fla. Stat.
Side effect: not part of the desired medical effect
Sign: visible evidence of illness, such as a fever or hearing non-existent voices
Standing order: “a broad protocol or delegation of medical authority that is

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
61
generally applicable to a group of persons, hence not individualized.” Fla. Admin.
Code Rule 65E-5.100(16).
Stat: emergency, act at once! (abbreviation of Latin “statim,” meaning
immediately)
Substance abuse impairment: “a condition involving the use of alcoholic
beverages or any psychoactive or mood-altering substance in such a manner that a
person has lost the power of self-control and has inflicted or is likely to inflict
physical harm on himself, herself, or another.” § 394.455(44), Fla. Stat.
Symptom: the person’s description of physical or mental illness; “the person is
complaining that . . . .”
Syndrome: a group of certain signs and symptoms that indicates a particular
diagnosis
Tardive dyskinesia: temporary to permanent side effect of neuroleptic
medications; involuntary tongue, eye, lip movement progressing to twisted body
posture
Titration: in medicine, a gradual increase
Tolerance: becoming used to an unpleasant situation
Tonic: muscles are tightened up, not relaxed
Transfer evaluation: the process by which a person who is being considered for
placement in a state treatment facility is evaluated for appropriateness of admission
to the facility. § 394.455(46), Fla. Stat. A civil patient may not be admitted to a
state treatment facility without previously undergoing a transfer evaluation. Before
a court hearing for involuntary placement in a state treatment facility, the court
must receive and consider the information documented in the transfer evaluation.
Treatment facility: “a state-owned, state-operated, or state-supported hospital,
center, or clinic designated by [DCF] for extended treatment and hospitalization,
beyond that provided for by a receiving facility, of persons with a mental illness.”
§ 394.455(32), Fla. Stat. It includes a private facility designated by DCF when
rendering those services to a person pursuant to the Baker Act.
Triage center: “a facility that has medical, mental health, and substance abuse
professionals present or on call to provide emergency screening and evaluation for

Chapter One History and Overview of Baker Act
_____________________________________________________________________________________
Baker Act Benchguide November 2016
62
mental health or substance abuse disorders for individuals transported to the center
by a law enforcement officer.” § 394.455(48), Fla. Stat.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
63
Chapter Two: Express and Informed Consent
I. Guardian Advocates and Other Substitute Decision Makers
See § 394.459(3), Fla. Stat.; Fla. Admin. Code R. 65E-5.170.
Consent in the mental health treatment context is simply the agreement of one
person to accept the actions or decisions of another as his/her own. Consent must
be voluntary, by a person who is competent to choose and who is fully informed
about and understands the consequences of that choice. Individuals competent to
consent to treatment are also competent to refuse or revoke consent to treatment.
When a person is not competent to choose, he or she must be transferred to
involuntary status. There are legally prescribed methods for obtaining substitute
decision-making in such circumstances.
“Express and informed consent” is defined in the Baker Act as “consent
voluntarily given in writing, by a competent person, after sufficient explanation
and disclosure of the subject matter involved to enable the person to make a
knowing and willful decision without any element of force, fraud, deceit, duress, or
other form of constraint or coercion.” § 394.455(15), Fla. Stat.
A person “incompetent to consent to treatment,” as defined in the Baker Act, is a
person whose “judgment is so affected by a mental illness or a substance abuse
impairment that he or she lacks the capacity to make a well-reasoned, willful, and
knowing decision concerning his or her medical, mental health, or substance abuse
treatment.” § 394.455(21), Fla. Stat.
Each person entering a facility, other than those who are incapacitated or
incompetent to consent to treatment, must be asked to give express and informed
consent for admission and treatment. If the person is a minor, express and informed
consent for admission and treatment is required from the guardian.
No person can be administered treatment in a receiving or treatment facility
without express and informed consent to the treatment having first been provided
by a person legally authorized to give that consent, except in documented cases of
imminent danger when a physician orders emergency treatment.
Prior to seeking such consent, the person and/or guardian (if incapacitated or a
minor), guardian advocate, or health care surrogate/proxy must be given at least
the following information, and the clinical record should reflect that the person or

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
64
substitute decision maker clearly understood the information, had an opportunity to
ask questions and get answers about the information, and understood the
consequences of providing or withholding consent:
Reason for admission or treatment.
Proposed treatment, including proposed psychotropic medications.
Purpose of treatment to be provided.
Alternative treatments.
Specific dosage range for medication.
Frequency and method of administration.
Common risks, benefits, and common short-term and long-term side effects.
Any contraindications which may exist.
Clinically significant interactive effects with other medications.
Similar information on alternative medication that may have less severe or
serious side effects.
Potential effects of stopping treatment.
Approximate length of care.
How treatment will be monitored.
That notification that any consent for treatment may be revoked orally or in
writing before or during the treatment period by any person legally
authorized to make health care decisions on behalf of the individual.
II. Documentation of Competence to Provide Express and Informed Consent
A physician must determine whether a person being admitted to a receiving or
treatment facility is competent to provide express and informed consent to
admission and treatment.
An adult admitted on a voluntary basis or transferred from involuntary to
voluntary status must be competent to provide his or her own consent. The
guardian of a minor must be willing to provide express and informed
consent for the minor.
A person admitted on an involuntary status may or may not be competent to
provide or refuse to provide express and informed consent for his or her own
treatment.
In any case, when an adult is permitted to provide consent for his or her own
treatment, the physician must document in the clinical record the adult’s
competence to make well-reasoned, willful, and knowing medical, mental health,

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
65
or substance abuse treatment. If the person is not competent to consent, as defined
above, the facility administrator must release the person or petition the court for
appointment of a guardian advocate, unless the person already has a court-
appointed guardian. Only when the safety of the person or others is in imminent
danger may the physician order emergency treatment.
Emergency psychiatric treatment (by Emergency Treatment Order, ETO)
may be rendered in the least restrictive manner upon the written order of a
physician, if it is determined that such treatment is necessary for the safety of the
person or others and express and informed consent from an authorized person is
unavailable. If the person has not had a guardian appointed by the court, a petition
for a guardian advocate must be initiated within 24 hours and submitted to the
court within two court working days (unless only one ETO is ordered within a
seven-day period). See Fla. Admin. Code R. 65E-5.1703.
Drugs used as a restraint are medications that are used to control behavior or to
restrict the person’s freedom of movement and are not part of the standard
treatment for the person’s medical or psychiatric condition. § 394.455(41)(b), Fla.
Stat. Chemical restraints are also regulated by federal conditions of participation
and accrediting organizations.
Electroconvulsive treatment (ECT) may be authorized by a competent person or
by a guardian, or by a guardian advocate who has been given express court
authority to consent to electroconvulsive treatment. § 394.459(3)(b), Fla. Stat.
Section 458.325, Florida Statutes, requires that electroconvulsive treatment be
agreed to by a second physician not directly involved with the responsibility for the
person’s care. Such agreement must be documented in the person’s treatment
record and must be signed by both physicians. See Chapter One of this benchguide
for more information on ECT.
III. Persons Determined Incompetent to Consent to Treatment
See § 394.4598, Fla. Stat.; Fla. Admin. Code R. 65E-5.230.
The administrator of a receiving or treatment facility may petition the court for the
appointment of a guardian advocate based upon the opinion of a psychiatrist that
the person is incompetent to consent to treatment ― unable to make well-reasoned,
willful, and knowing decisions about his or her medical, mental health, or
substance abuse treatment.
“Before giving consent to treatment, the guardian advocate must meet and talk
with the [individual] and the [individual’s] physician in person, if at all possible,

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
66
and by telephone, if not.” The guardian advocate must certify that such
communication with the individual and physician has taken place before
authorizing treatment. The guardian advocate must also complete statutorily
required training. See the Guardian Advocate Training and Resource Manual
online for extensive information about the duties of a guardian advocate. The
manual can be found on the DCF website http://www.myflfamilies.com/. A
specialized web-based training course for guardian advocates can be found at
http://www.dcf.state.fl.us/programs/samh/mentalhealth/training/index.shtml.
IV. Persons Adjudicated Incapacitated
See § 394.4625(1)(d), Fla. Stat.
The Baker Act prohibits the voluntary admission of any person who has been
adjudicated by a court as incapacitated even though the guardianship law (section
744.3725, Florida Statutes) defines specific steps the court must follow before
granting a guardian the authority to do so. The First District Court of Appeal has
ruled that where the Baker Act and the guardianship law conflict on least
restrictive alternatives, the Baker Act prevails. Handley v. Dennis, 642 So. 2d 115
(Fla. 1st DCA 1994). A concurring case from the Fourth District Court of Appeal
in 2012 is Auxier v. Jerome Golden Center for Behavioral Health, 85 So. 3d 1164
(Fla. 4th DCA 2012). A magistrate had discharged the public defender’s office in a
Baker Act case because the person who was the subject of the proceedings had a
plenary guardian, and her rights had been transferred to her guardian and counsel
for the guardian would represent her. The person was not present at the hearing on
which the order was based and did not have independent counsel, and she was
involuntarily committed. The public defender’s office sought review of the order
discharging it from representing her, and the Fourth District Court of Appeal
granted it and quashed the discharge and commitment orders. It held that “the
magistrate and the circuit court departed from the essential requirements of law
[which] requires appointment of the public defender’s office to represent the
patient in involuntary civil commitment proceedings ‘unless the person is
otherwise represented by counsel.’ The guardian’s attorney represents the
guardian, not the ward.” The court “agree[d] with the First District’s discussion of
the role of the public defender in Baker Act proceedings” in Handley v. Dennis.
The court order adjudicating the person as incapacitated will designate who is the
guardian. “Letters of guardianship shall be issued to the guardian and shall specify
whether the guardianship pertains to the person, or the property, or both, of the
ward. The letters must state whether the guardianship is plenary or limited, and, if
limited, the letters must state the powers and duties of the guardian.” § 744.345,

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
67
Fla. Stat. The guardian can only be permitted to perform those responsibilities that
have been expressly removed from the ward and delegated to the guardian.
V. Persons with Health Care Surrogates/Proxies
See ch. 765, Fla. Stat.; Fla. Admin. Code R. 65E-5.230.
Any competent adult may execute an advance directive designating any other adult
to make his/her health-related decisions should he/she ever become incompetent to
make these decisions. If the person has not executed an advance directive or the
surrogate selected by the person is not available, health care decisions may be
made by a proxy chosen from a statutorily authorized prioritized list of persons:
guardian, spouse, adult child, parent, adult sibling, adult relative, close friend, or
independent licensed clinical social worker (LCSW). Significant limitations are
placed on the designation of LCSWs.
If a person’s capacity to make health care decisions for himself or herself or
provide express and informed consent is in question, the attending physician
should evaluate the person’s capacity. If the attending physician concludes that the
person lacks such capacity to make mental health care decisions, the facility must
enter the physician’s evaluation in the person’s clinical record and notify the
surrogate or proxy in writing that his/her authority to act has commenced
(recommended form “Certification of Person’s Incompetence to Consent to
Treatment and Notification of Health Care Surrogate/Proxy” CF-MH 3122 may be
used). The authority thus activated remains in effect until a determination that the
person has regained his/her capacity. When a health care proxy is designated, the
proxy should also complete an affidavit (CF-MH 123). The 2015 Legislature
authorized a competent individual to designate a surrogate in an advance directive
to make his/her health care decisions without the need for a determination of
incapacity.
A specialized Mental Health Advance Directive has been developed for optional
use and can be found at the end of this chapter.
During the interim period between the time a person is determined by a physician
to be incompetent to consent to treatment and the time a guardian advocate is
appointed by a court to provide express and informed consent to the person’s
treatment, the health care surrogate or proxy may provide such consent to
treatment.
A petition for adjudication of incompetence to consent to treatment and
appointment of a guardian advocate must be filed with the court within two court

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
68
working days of the determination by the physician of the person’s incompetence
to consent to treatment. Recommended form “Petition for Adjudication of
Incompetence to Consent to Treatment and Appointment of a Guardian Advocate”
(CF-MH 3106) may be used.
The facility must immediately provide to the health care surrogate or proxy the
same information required by statute to be provided to the guardian advocate. In
order to protect the safety of the person, the facility must make available to the
health care surrogate or proxy the same training required of guardian advocates
and ensure that the surrogate or proxy communicates with the person and person’s
physician prior to giving express and informed consent to treatment.
The surrogate or proxy may provide consent for treatment only for persons on
involuntary status. The surrogate or proxy has the authority to do the following:
Make any and all health care decisions, but must make those decisions based
upon what he or she believes the principal would have decided if that
principal was capable of making such decisions (substitute judgment). Only
if the surrogate/proxy doesn’t know what the person would have wanted can
a “best interest” standard be used.
Access the person’s clinical record.
Authorize the release of information and clinical records to appropriate
persons to ensure the continuity of the person’s health care.
Apply for private, public, governmental, or veteran’s benefits to defray the
cost of health care and to have access to financial information of the
principal.
Authorize transfers to and from other facilities.
The 2016 Legislature added section 765.2035, Florida Statutes, permitting a
natural guardian, legal custodian, or legal guardian to designate a competent adult
as a health care surrogate to make health care decisions for a minor. However, a
health surrogate or proxy is not permitted under the Baker Act to apply for a
minor’s voluntary admission to, or authorize treatment at, a Baker Act facility.
VI. Summary of Consent Issues
A person who is competent to provide express and informed consent to admission
or treatment is competent to refuse or revoke such consent. A mere refusal or

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
69
revocation of consent does not justify a transfer to involuntary status without clear
documentation of other behaviors by the person that satisfy the involuntary
placement criteria.
However, a person who has been adjudicated incapacitated or found to be
incompetent to consent to treatment by a court is incapable of refusing treatment
that has been authorized, by express and informed consent, by a substitute decision
maker.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
70
Guardian
Guardian Advocate
Representative
Health Care
Surrogate
(
HCS
)
Health Care
Proxy
(
HCP
)
Statutory
Citation
Chapter 744,
F.S.
s.
394.4598,
F.S.
s.
394.4597,
F.S.
Chapter 765,
Part II,
F.S.
Chapter 765, Part
IV,
F.S.
Initiation
Petition to determine
incapacity filed by
an
adult.
Determination by
a
psychiatrist that
the
person is
incompetent
to
provide express
and
informed consent
to
treatment.
Conversion
from
voluntary
to
involuntary
status
or admission to
a
receiving or
treatment facility
on
involuntary
status.
Determination
by
attending
physician,
that
principal
lacks
capacity to
make
health care
decisions for
himself/her
self.
Same as Health
Care Surrogate
Appointment
Order of
a
Circuit
Judge
stating the nature of
the
guardianship as
either
plenary or
limited. If
limited, order states
the
rights which have
been
removed and delegated
to the
guardian.
Circuit judge
upon
petition of
Receiving or
Treatment
Facility
Administrator
and
adjudication
of
incompetence
to
consent to
treatment
.
Selected by
the
person
if possible;
if
not,
designated
by the facility
from
a
prioritized
list
specified
in law.
Healthcare
facility notifies
Surrogate
in
writing
that
authority under
the
advance
directive
has
commenced.
Health care
facility
notifies
Proxy
in
writing that authority
has commenced.
Qualifications
Competent adult;
if
non-
resident,
must
be related
by blood
or
adoption.
Preference
given to
wishes of
ward,
to
a
relative, and to
a
person
with ability
to
perform.
Prohibits
a
felon, an
incapacitated
person,
creditor, or
other
unsuitable person,
or
one
with
a
conflict
of interest.
If
providing
any
professional or
business
services, must be
a close
relative. Prohibits
a
judge
unless related
to ward.
See law for
other
limitations.
Same as
guardian but
gives
preference
to
HCS followed
by
spouse, adult
child,
parent, adult next
of
kin, adult friend,
or
trained adult. Prohibits
from serving: MH
professional,
facility
employee,
creditor,
person providing
substantial services,
or persons subject to
domestic violence
injunction for which
patient was petitioner.
Any
competent
adult
selected by
the
person.
Otherwise
preference
given
to
HCS, followed
by
spouse, adult
child,
parent, adult next
of
kin
or adult
friend.
Prohibits
from serving:
licensed
professional,
facility
employee,
creditor,
person
providing
substantial
services, or
persons subject to
domestic violence
injunction for which
patient was petitioner.
Any
competent adult
selected by
the
principal through
an
advance
directive.
Designated by
law
from
a
prioritized
list
of
persons
including
guardian,
spouse,
adult
child, parent,
adult
sibling,
adult
relative,
close friend*, or
clinical
social
worker*.
*Friend
is
defined
in
law
and LCSW
limits
provided
in law.
Requirements
40 hours training
on
duties, rights of
ward,
local resources,
and
plans/reports within
1
year of
appointment.
Professional and
public
guardian must take
oath
and file
a
bond
(unless
waived).
Agreement to
serve,
undergo
4-
hour
training course, meet
with
person and
physician
prior to
providing consent.
No prerequisites
or
training
required.
No prerequisites
or
training
required
by law.
65E-5.2301
FAC
requires HCS
to
be given
same
information
required to be
given
to
guardian
advocate.
Same as Health
Care
Surrogate
VII. Bench Card on Substitute Decision-Making
(Does not substitute for statutes or legal advice)
C

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
71
Guardian
Guardian Advocate
Representative
Health Care
Surrogate
(HCS)
Health Care
Proxy
(HCP)
Tenure
While person
is
incapacitated.
While person
is
incompetent to
c
onsent
to
treatment.
While person
is on
involuntary status
in
a
receiving or
treatment
facility.
While principal
is
physically or
mentally
unable
to
communicate
a
willful
and knowing
health
care
decision.
Same
authority
as
a
Health
Care
Surrogate.
Authority
Limited to
authority
granted by
Circuit
Court
in
Letters
of
Guardianship.
Plenary
Guardian
shall exercise
all
delegable
rights
while
Limited
Guardian
exercises only
those
removed from the
ward in
the
order.
Must
file
reports,
plans, inventory
,
and
accounting.
Consent to
psychiatric treatment,
access
client
record, and
release
of information for
continuity
of care.
Consent
to
medical
care,
ECT,
abortion,
sterilization,
psychosurgery,
and
experimental
treatment only upon
Court
approval.
Receives
all
notices
and
may
file
Habeas
petition.
Receives notices
of
proceedings and
any
restrictions during
the
time
a
person
is
held in
or admitted to
a
receiving or
treatment
facility.
Has standing
to file
a
Petition
for
Habeas
Corpus
if it is
believed the
person
is
being held illegally
or to file
a petition if
person
is
unjustly
denied
a
right
or
privilege.
Make written
consent
to health
care
decisions the
principal would have
made
if
capable of
making
such
decisions.
Have
access to
clinical
records,
authorize
release of records
for
continuity of
care,
authorize transfer
of
principal to or
from a
health care
facility,
and apply for
public
benefits.
Same as Health
Care
Surrogate.
Limitations
Prohibited from
having
ward admitted on
a
voluntary basis
for
psychiatric
examination or
treatment. May
only
consent to treatment
of
ward
if
on
involuntary
status.
Medical, ECT,
and
other extraordinary
interventions
are
prohibited
without
Court
approval.
Has no
authority
other than
described
above.
May not consent
to
psychiatric treatment
for
a
person on
a
voluntary
status.
May not
provide
consent for abortion,
sterilization,
ECT,
psychosurgery,
or
experimental
treatment
without
Court approval
or
express authority
in
an advance
directive
.
Same as Health
Care
Surrogate.
Termination
Upon resignation
of
guardian
and
appointment
of
successor
guardian;
upon restoration
of
capacity; or removal
of
guardian by the
Court.
Persons’ restoration
of
competency,
discharge from
involuntary
inpatient/outpatient
placement, or
transfer
to voluntary
status.
Transfer to
voluntary status or
discharge
from
receiving
or
treatment
facility.
Upon revocation
of
the advance
directive by
a
competent
principal, upon
the
principal’s
gaining
capacity to
consent,
or removal by
court.
Same as Health
Care
Surrogate.
C

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
72
VIII. Frequently Asked Questions
A. Competence to Consent
Who is eligible to consent or refuse consent to their own treatment?
Minors cannot make their own inpatient mental health treatment decisions; this is
the responsibility of their parent or guardian. Neither can persons who have a
court-appointed guardian or a health care surrogate or proxy currently making
decisions for them. Only adults who are consistently able to make well-reasoned,
willful, and knowing decisions about their own mental health or medical care can
consent, refuse consent, or revoke consent to their own treatment.
I’m an attorney representing a hospital that isn’t designated as a receiving
facility. The doctor wants to admit a patient on voluntary status who has a
guardian willing to consent to the admission. We are told that many other
facilities permit that type of admission. A person adjudicated by a court as
incapacitated wouldn’t be able to provide express and informed consent. How
is inpatient mental health care provided to patients who have guardians and
who need treatment, but do not meet the criteria for involuntary admission?
The issue about prohibiting voluntary admission of adjudicated persons with
guardians is a statutory prohibition:
394.4625. Voluntary admissions (emphasis added)
(d) A facility may not admit as a voluntary patient a person who
has been adjudicated incapacitated, unless the condition of incapacity
has been judicially removed. If a facility admits as a voluntary patient
a person who is later determined to have been adjudicated
incapacitated, and the condition of incapacity had not been removed
by the time of the admission, the facility must either discharge the
patient or transfer the patient to involuntary status.
(e) The health care surrogate or proxy of a voluntary patient
may not consent to the provision of mental health treatment for
the patient. A voluntary patient who is unwilling or unable to provide
express and informed consent to mental health treatment must either
be discharged or transferred to involuntary status.
(f) Within 24 hours after admission of a voluntary patient, the
admitting physician shall document in the patient’s clinical record that

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
73
the patient is able to give express and informed consent for admission.
If the patient is not able to give express and informed consent for
admission, the facility shall either discharge the patient or transfer the
patient to involuntary status pursuant to subsection (5).
The above references “facility,” not “receiving facility.” These are both defined in
the Baker Act. A facility is defined in the Baker Act as follows:
(16) “Facility” means any hospital, community facility, public or
private facility, or receiving or treatment facility providing for the
evaluation, diagnosis, care, treatment, training, or hospitalization of
persons who appear to have or who have been diagnosed as having a
mental illness or substance abuse impairment. The term does not
include a program or an entity licensed under chapter 400 or chapter
429.
§ 394.455, Fla. Stat. (emphasis added).
While the guardianship statute (chapter 744) has a provision where a guardian can
obtain extraordinary authority of the court to have his/her ward admitted
voluntarily to a receiving facility, this conflicts with the provisions of the Baker
Act, which is the more specific law and would take precedence.
If a person who arrives at a receiving facility for an involuntary examination
is cooperative and willing to take medications, is this sufficient to document
“express and informed consent”?
No. “Cooperative and willing” are helpful descriptors, but more important is
competence of the person to make such decisions. This is defined in the law as
being able to make well-reasoned, willful, and knowing decisions about one’s
medical, mental health, or substance abuse treatment. Without competence, as
defined in the Baker Act, no amount of cooperation or willingness is sufficient.
The standard under the Baker Act requires more than “implied consent” because
the person may have taken the medications prior to admission and/or is not
currently refusing the medications. “Med compliance” is a behavior, but it doesn’t
necessarily reflect competence.
Recently we had a question come up about a patient being able to sign legal
documents brought in by the family. The patient was not deemed incompetent
by our doctor, but was not here voluntarily either. Can the patient be able to
sign legally binding documents while inpatient in a mental health hospital or
Crisis Stabilization Unit?

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
74
It’s unclear what kind of legal documents are involved. Just because a person
hasn’t been adjudicated incapacitated by a court doesn’t mean he/she is competent
for various purposes. If the patient is on voluntary or involuntary status and has
been allowed to provide consent to his/her own treatment, a physician would have
had to document the person’s competence to provide express and informed consent
on a sustained basis (not just some “window of lucidity”). This medical statement
means that the person is able to make well-reasoned, willful, and knowing medical,
mental health, and substance abuse treatment decisions.
If the person’s clinical record has notes from nurses, social workers, or other
personnel that reflect the person’s judgment or insight was impaired at the time,
the legitimacy of any consent would be questionable, even for treatment, not to
mention other legal documents. The person could later challenge any document
signed at such a time and place due to diminished capacity or perceived coercion,
whether the documents are advance directives, quitclaim deeds, a will, powers of
attorney, or any other legal document.
Can a person on involuntary status still be competent to consent or refuse
consent to his or her own treatment?
Yes. The issue of competence to consent is considered separately from the
placement issue. If the person meets the criteria for involuntary examination or
involuntary placement but is capable of making well-reasoned, willful, and
knowing decisions about his or her medical, mental health, or substance abuse
treatment, he or she may continue to consent, withhold consent, or refuse consent
to treatment. A person on involuntary status may or may not be competent to
consent to his or her own treatment. If the individual who initiated the involuntary
examination noted on the form that the subject person was unable to determine the
exam was necessary, as opposed to refusing the exam, the person must be
presumed to be incompetent to consent to treatment until determined by a
physician to have such capacity.
Must we stop giving a patient psychotropic medication if the patient has been
transferred to incompetent status if that person had given consent for those
medications while still competent? I know we must get a guardian advocate
who will then be asked to consent to psychotropic medication; we’re
wondering about the interim period.
If the patient had been certified by a physician while on voluntary status as
competent to make well-reasoned, willful, and knowing medical and mental health
decisions (required within 24 hours of all voluntary admissions) and was provided
all disclosures about medications required by law and rule, that authority would be

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
75
valid only while the patient remained competent, not valid after a subsequent
determination that the patient was no longer competent to consent.
Consent given by a competent adult is valid only while the person remains
competent. However, if the basis for transferring the person from voluntary to
involuntary status is because the person is “refusing” to stay at the facility (as
opposed to being unable to determine that placement is necessary), and the doctor
continues to certify the person’s competence to consent or refuse consent to
treatment, it is possible that the consent could still be valid. However, if the doctor
has determined that the person is no longer able to provide such express and
informed consent and is requesting the court to appoint a guardian advocate, earlier
consents can’t be honored.
It is at this point that a relative or close personal friend, if any, should be asked to
serve as the person’s health care proxy unless the person had previously executed
an advance directive designating a different person as his/her health care surrogate.
Such a proxy or surrogate could serve as an interim decision maker until the court
appointed a guardian advocate, who might be the same person.
When a person is transferred from voluntary to involuntary status, the petition must
be filed with the clerk of court within two working days, not 72 hours.
B. Incompetence to Consent
If a person with a mental illness refuses to consent to treatment, is that an
indication of incompetence?
No. A person’s refusal to consent to treatment is not, in itself, an indication of
incompetence to consent. There may be many reasons why a person may decide
not to consent to a particular medication or to any medication ordered by a
particular physician, or to treatment ordered at a particular facility. The decision as
to whether a person is competent to consent is a clinical judgment of his or her
capacity to decide, not one based on whether the person does or doesn’t provide
such consent.
Once a patient has a petition for involuntary placement filed, but prior to the
hearing, do medication orders remain emergency treatment orders or do they
become regular orders once the petition is filed?
Emergency treatment orders cannot be done either before or following the filing of
the BA-32 (petition for involuntary placement, form CF-MH 3032) unless the
record documents imminent danger and that there are no less restrictive
interventions. Only after the appointment of a guardian advocate can such

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
76
medications needed for the person’s treatment be authorized/administered if the
person is found by the court to be incompetent to consent. Prior to that time, short
of imminent danger, only a health care surrogate/proxy can authorize medications
for which the person either refuses or lacks capacity to consent.
If a person is determined by a psychiatrist NOT to have capacity to consent, is
it true that he or she can’t be given any psychotropic medications unless
under an ETO if he or she has no one to serve as health care proxy until after
a court-appointed guardian advocate has been selected?
This is correct ― no psychiatric treatment can be rendered short of imminent
danger without the express and informed consent of a person authorized by law to
provide such consent.
Can a person be incompetent for admission and competent for treatment or
be competent for admission and incompetent for treatment?
No. If a person is incompetent to provide express and informed consent, it applies
to both admission and to treatment. The Baker Act definition of “express and
informed consent” requires that the consent be voluntarily given in writing by a
competent person. Competence requires that the person have the capacity of
providing a well-reasoned, willful, and knowing decision about his or her medical,
mental health, or substance abuse treatment. If the person has this capacity, he or
she can choose to be voluntary (or may be involuntary) and can choose to give or
withhold consent to treatment. If the person doesn’t have this capacity, he or she
must be held under the elevated protection of the involuntary provisions of the law
and a guardian advocate must be sought.
However, if a person is competent, he or she can potentially be either voluntary or
involuntary, although most people on involuntary status lack the capacity to give
well-reasoned, willful, and knowing decisions about their medical, mental health,
and substance abuse care (the legal definition for incompetence). In those
situations, the person is incompetent to consent and must have a guardian advocate
appointed.
If a person is incompetent to consent to treatment, he/she must be placed on
involuntary status. Physicians and staff need to understand that no person should
be allowed to consent to treatment unless he/she would also be allowed to refuse
treatment. It is the capacity of the person to make the decisions ― not the quality
of the decisions the person makes ― that controls.
Can a person who has been determined to be incapacitated/incompetent to
consent to treatment refuse consent to a particular psychiatric treatment?

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
77
No. If the proposed treatment has been fully disclosed to the legally authorized
substitute decision maker who has provided informed consent to the treatment, the
person does not have the authority to refuse. The person does have the right to file
a petition for a writ of habeas corpus so a judge can determine if the person’s rights
have been violated. However, if a person strongly objects to a particular form of
treatment, the guardian/guardian advocate or surrogate/proxy should talk with the
person to determine the reasons for the objections. If appropriate, the
guardian/guardian advocate or surrogate/proxy may, based on this information,
withdraw his or her consent for the proposed treatment and negotiate a revised
treatment plan with the physician.
C. Disclosure
What must be disclosed to a person before authorization for treatment can be
obtained?
Before giving express and informed consent for treatment, the following
information must be provided and explained in plain language to the authorized
decision maker:
Reason for admission or treatment.
Proposed treatment.
Purpose of the treatment to be provided.
Identification of the proposed psychotropic medication.
Common risks, benefits, and short- and long-term side effects thereof.
Specific dosage range for the medication.
Frequency and method of administration.
Any contraindications which may exist.
Clinically significant interactive effects with other medications.
Similar information on alternative medications that may have less severe or
serious side effects.
Alternative treatment modalities.
Potential effects of stopping treatment.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
78
Approximate length of care.
How treatment will be monitored.
That any consent given for treatment may be revoked orally or in writing
before or during the treatment period.
Does the facility have the same responsibility to a substitute decision maker as
it does to a competent adult with regard to disclosure?
Yes. Prior to the administration of treatment, a qualified staff person must provide
the same information to a guardian, guardian advocate, or health care
surrogate/proxy as it would to a patient competent to make his/her own decisions.
D. Consent to Treatment
Does all consent need to be provided in writing, or can we accept verbal
consent under certain circumstances?
While the statutory definition of express and informed consent refers to such
consent being given in writing by the legally authorized decision maker, there are
times when the guardian of a minor or a guardian, guardian advocate, or health
care surrogate/proxy of an adult is unavailable to provide the consent in writing.
It is standard practice in medical situations when the decision maker is not present
to provide the full disclosure by telephone and receive the verbal authorization for
treatment by the decision maker, with two witnesses for the facility. This is
followed up by a written consent. When the substitute decision maker is not
physically available to provide written consent to treatment prior to administration
of treatment, it may not be in the best interest of the child or adult held in a facility.
In some cases, the parent may even be out of the country and it is not possible to
fax or scan and email consent forms to and from the parent. If the individual
presents imminent danger, an ETO can be ordered by a physician. Otherwise,
treatment would have to be withheld.
I have questions about express and informed consent by non-literate persons
or persons who are physically unable to write. Is this addressed in the Baker
Act or by rule?
This has been handled in different ways, depending on the circumstances:

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
79
Laws recognize an “X” if a person generally signs his/her name this way due
to illiteracy. Forms may have a place for the witness to a signature to sign
and date.
Persons sometimes will give verbal authorization for treatment but won’t
sign the form. If the required disclosures and the authorization are witnessed
by staff members, this has always been considered as an acceptable
alternative. Verbal consent should be witnessed by two staff.
The most frequent problem is when a substitute decision maker is relied on
to provide consent for treatment. Guardians, guardian advocates, and health
care surrogates/proxies may live at a great distance or just be unable to come
to the receiving facility in a timely way to provide written consent. Again, it
has always been considered acceptable to have verbal consent if such
consent is witnessed by two staff who sign that they personally heard the
disclosures and the consent. The facility might consider sending a form by
courier, fax, or email to the substitute decision maker to sign and return,
even if after the fact.
I’m a psychiatrist treating a patient admitted involuntarily for assaultive
behavior. We filed a petition for placement and are awaiting a hearing next
week. The patient has repeatedly said he will stop taking medications once
discharged. We would like to give him a long-acting injectable medication
before he is discharged. I had assumed that the court hearing would need to
take place in order to establish a guardian advocate, who could then authorize
the treatment. I was recently told that the court didn’t need to make this
determination if we could demonstrate that (1) the patient lacks decisional
capacity for this treatment, and (2) there is a family member willing to serve
as a proxy decision maker. Both of these criteria are met for the patient; if it is
appropriate and legal, we would likely get started with the long-acting
medication long before his court hearing next week. Is this appropriate?
The Baker Act recognizes a guardian advocate appointed by the court as a
substitute decision maker. However, because that appointment might not occur
until seven to ten days after the individual’s admission, the Florida Administrative
Code has “borrowed” from the state’s advance directive statute (chapter 765,
Florida Statutes) that governs any and all health care decision-making for an
interim decision maker until a guardian advocate has been appointed pursuant to
rule 65E-5.2301, Florida Administrative Code.
As soon as a physician documents that an individual cannot provide express and
informed decisions for his/her own care, a health care proxy (relative or close

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
80
personal friend) can be designated by the facility to provide “substitute decision-
making” ― after getting full disclosure providing the decision the proxy believes
the individual would have made if competent. Only if the surrogate or proxy
doesn’t know what the individual would have chosen if competent can a “best-
interest” standard be used. This could include long-acting medications if the proxy
believes the person would have consented to this type of medication or route of
administration had he/she been competent. Otherwise, the only other alternative to
legally authorized decision-making would be an ETO based on documentation of
imminent danger. Use of long-acting medications as an ETO requires extraordinary
justification. However, if it is included in the individual’s treatment plan and
you’ve obtained express and informed consent from an authorized person, such
extraordinary justification wouldn’t be required.
E. Initiation of Psychiatric Treatment
If a person is determined not to have the capacity to make his or her own
treatment decisions and has no known family, can a facility legally administer
medications until a court hearing and appointment of a guardian advocate if
the person is willing to take the offered medications?
No. There is no “implied consent” for psychotropic medications. Even if a person
swallows the pills or has willingly taken the medications at a point prior to the
hospitalization, the law prohibits the administration of medications unless “express
and informed consent” has been obtained from the person or his/her substitute
decision maker. The only exception is when the physician has fully documented
the nature and extent of the person’s imminent dangerousness and has ordered
emergency treatment ― this is limited to rapid response medications since it is for
chemical restraints ― an issue controlled by federal regulations as well as state
law/rules. Unless such an emergency exists, psychotropic medications cannot be
administered unless the person or his/her substitute decision maker provides
express and informed consent to the medications.
Two additional choices may be available. An expedited court hearing can be
requested on the issue of adjudicating incompetence to consent to treatment and
appointing a guardian advocate. A second alternative is to appoint an independent
clinical social worker as proxy, as permitted in chapter 765, part IV, Florida
Statutes, and rule 65E-5.2301, Florida Administrative Code. Either of these
alternatives will allow you to provide medication without waiting for an
emergency to occur.
Can psychiatric treatment be initiated before informed consent is obtained?

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
81
No. Unless the person is displaying uncontrolled symptoms and behaviors that are
causing imminent danger, treatment cannot be initiated unless express and
informed consent is first obtained from a competent adult or from a legally
authorized substitute decision maker. At any time staff observes that the person
isn’t making such well-reasoned decisions, treatment must stop until a substitute
decision maker is found or when the physician has documented imminent danger,
in which case an emergency treatment order can be considered.
If a person is admitted on involuntary examination status and the box on the
BA-52 form is checked indicating the person was unable to determine a
voluntary examination was needed, should we presume the person is
incompetent to consent to psychotropic medications or other treatment? In
this case no psychotropic medications could be administered until the
physician has done a competency exam unless an ETO was ordered. Correct?
Yes, this is correct. If a person is unable to determine the examination is needed,
he/she is likely to be incompetent to consent to either admission or to treatment.
If an individual on involuntary status with a legal guardian arrives at our
facility, do we have to wait for a documentation of incompetence by the
physician in order for the legal guardian to consent? It seems like we wouldn’t
have to wait, because the courts have already made this determination, which
is why the person has a legal guardian. Is this correct?
If you have documentation through a copy of the court order that it is either a
plenary guardianship or that the right to consent to mental health care has been
removed from the person and delegated to the guardian, no assessment of
competence is required since the adjudication of incompetence would have already
been established by the court. Once you have documentation through the court
order and letters of guardianship, you would then have to get consent from the
court-appointed guardian.
F. Mental Health Advance Directives
Is there a form for a psychiatric advance directive in Florida that meets the
state and federal requirements? We are aware of the recommended Baker Act
form to use “Affidavit of Health Care Proxy”‘ (form CF-MH 3123) but do not
see a form that could be used for persons with mental illness to be proactive
and document their wishes should they become incapacitated.
Yes. A mental health advance directive can be found in chapter 7 of this
benchguide. It is based on the 20-page Bazelon Center form, but condensed and
adapted to Florida laws. It is recommended, but not mandatory. Form CF-MH

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
82
3122, as well as the affidavit form (3123), can be used by the physician to certify
incompetence to consent and notify the surrogate/proxy.
I am trying to get clarification of exactly what the expectations are of our
facility should one of our inpatients request to complete a mental health
advance directive. Can psychiatric inpatients complete a mental health
advance directive?
Only a person who is considered competent may complete a valid advance
directive, even one for mental health care. If the patient is competent and there are
two witnesses who attest that “at the time the advance directive was signed, the
person was of sound mind and under no constraint or undue influence,” the patient
would be eligible to complete the form. Many facilities feel that the mere presence
of a person in a receiving facility may suggest lack of competence and possibly
some undue influence by staff. You may want to select a health care proxy
(relative or close personal friend) while the person is hospitalized if not competent
to execute an advance directive, and provide the person the paperwork and
assistance as part of release from the hospital. That way the document is in place
should he/she be re-hospitalized at some future time.
I need information about mental health advance directives. At this time my
facility asks patients being admitted if they have one and, if they do, we get a
copy. Where in the statute does it discuss mental health advance directives?
Federal regulations require that any hospital inquire about a person’s advance
directives at the time of admission. In addition, the Florida Administrative Code
governing the Baker Act (Fla. Admin. Code Ch. 65E-5). requires that each
receiving facility (hospital and CSU) also make such an inquiry. The primary
statute that governs advance directives in Florida is chapter 765, Florida Statutes. It
includes several references to mental health issues:
765.101. Definitions
(6) “Health care decision” means:
(a) Informed consent, refusal of consent, or withdrawal of consent
to any and all health care, including life-prolonging procedures and
mental health treatment, unless otherwise stated in the advance
directives.
765.113. Restrictions on providing consent.
(1) . . . or voluntary admission to a mental health facility.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
83
765.202. Designation of a health care surrogate
(5) A principal may designate a separate surrogate to consent to
mental health treatment. . . .
765.204. Capacity of principal; procedure
However, the Baker Act (chapter 394, part 1, Florida Statutes) also makes
several references to advance directives and health care surrogates/proxies,
as does the Florida Administrative Code governing the Baker Act (Fla.
Admin. Code Ch. 65E-5).
G. Electroconvulsive Therapy
We are currently treating a patient with a severe psychotic disorder. We
petitioned the court for extension of the patient’s stay and asked for
Electroconvulsive Therapy (ECT) treatments. The judge appointed a
guardian advocate and also ordered the use of ECT. We want to help the
patient, but do not want to violate any rights. When a second opinion is
requested by the attending psychiatrist, does the consulting psychiatrist need
to physically assess the patient or can that psychiatrist just review the chart?
If the court appointed a guardian advocate under the Baker Act, the guardian
advocate authority to consent to ECT is governed as follows:
394.4598. Guardian advocate (emphasis added)
(7) If a guardian with the authority to consent to medical treatment
has not already been appointed or if the patient has not already
designated a health care surrogate, the court may authorize the
guardian advocate to consent to medical treatment, as well as mental
health treatment. Unless otherwise limited by the court, a guardian
advocate with authority to consent to medical treatment shall have the
same authority to make health care decisions and be subject to the
same restrictions as a proxy appointed under part IV of chapter 765.
Unless the guardian advocate has sought and received express court
approval in proceeding separate from the proceeding to determine the
competence of the patient to consent to medical treatment, the
guardian advocate may not consent to:
(a) Abortion.
(b) Sterilization.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
84
(c) Electroconvulsive treatment.
(d) Psychosurgery.
(e) Experimental treatments that have not been approved by a
federally approved institutional review board in accordance with 45
C.F.R. part 46 or 21 C.F.R. part 56.
The court must base its decision on evidence that the treatment or
procedure is essential to the care of the patient and that the treatment
does not present an unreasonable risk of serious, hazardous, or
irreversible side effects. The court shall follow the procedures set
forth in subsection (1) of this section.
The above requires a separate hearing after the appointment of the guardian
advocate (GA) to consider the need for ECT. However, if a guardian has been
appointed by the court under chapter 744, Florida Statutes, the guardianship law
(instead of a GA under the Baker Act), such a guardian has the authority to consent
to the ward’s ECT without further order of the court, unless the court has limited
the powers of the guardian in some way.
With regard to the actual administration of ECT, this is primarily governed by the
Florida Medical Practice Act as follows:
458.325. Electroconvulsive and psychosurgical procedures
(emphasis added)
(1) In each case of utilization of electroconvulsive or
psychosurgical procedures, prior written consent shall be obtained
after disclosure to the patient, if he or she is competent, or to the
patient’s guardian, if he or she is a minor or incompetent, of the
purpose of the procedure, the common side effects thereof, alternative
treatment modalities, and the approximate number of such procedures
considered necessary and that any consent given may be revoked by
the patient or the patient’s guardian prior to or between treatments.
(2) Before [electro]convulsive therapy or psychosurgery may be
administered, the patient’s treatment record shall be reviewed and the
proposed convulsive therapy or psychosurgery agreed to by one other
physician not directly involved with the patient. Such agreement
shall be documented in the patient’s treatment record and shall be
signed by both physicians.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
85
The above only requires the documented review and agreement by the second
physician. It isn’t addressed by the Baker Act.
Can a substitute decision maker consent to electroconvulsive treatment (ECT)
on behalf of the person?
A plenary guardian has the authority to make this decision on behalf of the person.
A guardian advocate has this authority only if specifically provided by the court in
a hearing separate from the one where the person was determined to be
incompetent to consent to medical treatment. A health care surrogate or proxy has
this authority only if a person specifically authorized this power in an advance
directive.
H. Consent to Medical Treatment
Is medical treatment provided to a person in a receiving facility governed by
the Baker Act?
No. The Baker Act is Florida’s Mental Health Act and doesn’t govern non-
psychiatric medical care. A facility would have to follow whatever medical
consent standards apply to non-psychiatric settings for aspirin, blood pressure
medications, etc.
Is there a statute or rule (other than the Baker Act) that requires informed
consent for general medical treatment, such as administration of non-
psychotropic drugs?
The Florida Medical Consent Law is set forth at section 766.103, Florida Statutes.
Does a Baker Act receiving facility have the right to take blood or urine
samples from an individual during the involuntary examination period
without consent?
As Florida’s Mental Health Act, the Baker Act doesn’t address medical consent
issues. Only if the physician had determined the individual has an emergency
medical condition requiring such diagnostic and laboratory testing could the
procedures be done without a competent patient’s consent or that of a legally
authorized decision maker.
Does the doctor’s finding of incompetent to consent for treatment under the
Baker Act relate to only psychiatric treatment or also to medications for
medical conditions? We frequently have individuals admitted who are on
routine diabetic medication, heart medication, or medication for COPD or

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
86
other chronic conditions. To stop these medications can be life threatening,
and it may take us two or three days to find a health care surrogate or proxy.
Thus, for the welfare of the patient we have allowed the patient to sign consent
for non-psychotropic medications. Please clarify.
The Baker Act is merely the state’s mental health law and doesn’t affect medical
treatment. The Baker Act is silent on this issue. For medical treatment, a provider
would follow whatever laws govern informed consent for medical care — it seems
to be much less stringent than for mental health. More to the point is that denial of
antihypertensive medications, insulin, and the entire range of other medications for
non-psychiatric conditions would probably represent medical neglect on the part of
a provider. Most receiving facilities will attempt to get a proxy to provide consent,
but if no proxy is available they will administer these drugs anyway. Given that the
patient was taking the medications prior to admission, an implied consent might be
acceptable where it is not sufficient for psychotropic medications.
We have a patient committed by the court to our unit on an order for
involuntary placement for up to 30 days. He was originally deemed competent
and the court did not appoint a guardian advocate. Just recently we found out
that he has a malignant melanoma that needs immediate surgery, but he is
refusing to have it done at this hospital due to his fixed paranoia about this
hospital. What legal procedures do we need to go through to get this man his
needed surgery? The psychiatrist now feels the man is incompetent. Do we
need to go back to court to get a guardian advocate appointed? Can a
guardian advocate sign the papers for a patient to get surgery or do we need
to do something else?
You have several alternatives.
If the doctor believes the man lacks competence, this can be documented in
the chart and a health care proxy can be designated from the list found in
chapter 765, part IV. The proxy can immediately exercise substitute
judgment, consenting to treatment that he/she believes the person would
have consented to if competent to do so.
You can file a petition (CF-MH 3106) for Adjudication of Incompetence to
Consent to treatment and Appointment of a Guardian Advocate with the
circuit court. The boxes for medical and for mental health treatment should
be checked. While surgery isn’t one of the procedures requiring a
specialized separate hearing before consent for extraordinary procedures can
be authorized, it might be wise to be sure the judge is aware of the
circumstances. It’s possible the court will provide an expedited hearing.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
87
You can file a petition for Expedited Judicial Intervention for Medical
Treatment (rule 5.900, Florida Probate Rules) with the circuit court.
I. Guardian Advocates and Other Substitute Decision Makers
1. In General
Who can authorize the admission of a person who lacks the capacity to make
his or her own treatment decisions?
A person who is incompetent to consent to treatment is incompetent to consent to
admission and must be admitted on involuntary status so his or her rights can be
protected — this would be by a law enforcement officer, circuit court judge, or
authorized mental health professional. If a person lacks the capacity to make his or
her own treatment decisions, only a guardian, guardian advocate, or health care
surrogate/proxy has the authority to make treatment decisions. These substitute
decision makers cannot have a person admitted on a voluntary basis, but once the
person is admitted on an involuntary basis, they can begin making treatment
decisions.
How can a substitute decision maker document his or her authority to make
decisions on behalf of another person prior to being allowed to consent to
treatment?
A guardian must provide a copy of the court order appointing him or her as a
person’s guardian and letters of guardianship to document the limits of the
authority of the guardian. A guardian advocate must provide a copy of the court
order appointing him or her that designates whether the guardian advocate has only
the authority to make mental health decisions or also has the authority to make
medical decisions. A health care surrogate must provide a copy of an advance
directive completed when the person was competent to determine what decisions
he or she would want to have made on his or her behalf. (See later questions about
each one of these types of decision makers.)
If a person refuses care that his or her guardian, guardian advocate, or health
care surrogate has authorized, does the physician have to issue an order for
emergency treatment in order to administer the medication?
No. If the person has been determined to lack the capacity to provide express and
informed consent and a legally authorized substitute decision maker has provided
consent for a specific treatment after full disclosure, the person’s consent to the
treatment is invalid and is not needed. This doesn’t mean that the facility shouldn’t
attempt to communicate the person’s objections to the specified treatment to the

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
88
guardian/guardian advocate to determine if the substitute decision maker wishes to
alter his or her consent.
2. Court-Appointed Guardians (Ch. 744, Fla. Stat.)
Does section 744.3215(4)(a), Florida Statutes, allow a guardian to seek
commitment of a ward for mental health treatment using the extraordinary
authority procedures of section 744.3725, without using Baker Act
involuntary examination and placement procedures?
No. The Baker Act is the more specific law, which would prevail over the more
general guardianship law when in conflict on this issue. Further, the First District
Court of Appeal ruled in Handley v. Dennis, 642 So. 2d 115 (Fla. 1st DCA 1994)
that the rights of the patient under the Baker Act supersede rights of the guardian
under the guardianship law when in conflict. Florida’s guardianship law has
traditionally provided for the extraordinary authority cited above, for a guardian
who has received the specific authority of the circuit court to commit the ward to a
facility, institution, or licensed service provider without formal placement
proceeding, pursuant to chapter 393, chapter 394, or chapter 397, as follows:
744.3215. Rights of persons determined incapacitated
(4) Without first obtaining specific authority from the court, as described
in s. 744.3725, a guardian may not:
(a) Commit the ward to a facility, institution, or licensed service provider
without formal placement proceeding, pursuant to chapter 393, chapter 394,
or chapter 397.
The court in Handley v. Dennis stated that
the Court has concluded that if there is a conflict in these laws, both the duty
of the guardian and the power of the circuit court in the guardianship
proceeding must give way to the ward’s right under the Baker Act to be
released to a less restrictive environment. . . .
[T]he court has concluded that § 744.2025 Fla.Stat. (1991) and all
other provisions of the guardianship law regarding the residence of the
ward, are inapplicable to Baker Act patients. . . .
In summary, the court concludes that a liberty interest asserted
on behalf of an involuntary mental patient in a Baker Act hearing is

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
89
superior to any conflicting right that could be asserted on behalf of the
patient under the guardianship laws.
642 So. 2d at 117–118. The Baker Act requires that any person who has been
adjudicated incapacitated be held under the involuntary procedures established
under chapter 394, Part I.
Our patient’s mother is her court-appointed guardian of person, and the
guardian is now terminally ill in late stages of Alzheimer’s disease. The
patient has an adult sibling; should we petition the court to have the sister
appointed her guardian advocate?
Yes. You can request a guardian advocate when a natural or court-appointed
guardian is no longer able to serve for an interim period until the court can appoint
a successor guardian. In the meantime, an adult sibling can serve as a health care
proxy providing interim decision-making for an individual on involuntary status
pending appointment as a guardian advocate.
Our MD is confused as to how a patient’s mother, who is the legal guardian
but who also has a “No Contact” order with her son due to his violence
toward her, can be his advocate for the involuntary placement hearing. We’ve
been told that a separate guardian advocate could not be appointed when
there’s a legal guardian. His mother does have an attorney who’ll be
representing her at the hearing that she will not attend.
It is correct that a guardian advocate is generally not needed when a person has a
legal guardian. There are a few exceptions, such as when the guardianship is
limited (e.g, for property only) or when the guardian is not available or not willing
to serve. In such cases the court will appoint a guardian advocate. It is essential
that you have a copy of the guardianship order as well as the letters of guardianship
in your files. These documents will verify whether the mother is a plenary guardian
or a limited guardian.
In Handley v. Dennis, 642 So. 2d at 117, regarding when the rights of a guardian
under chapter 744, Florida Statutes, conflict with the rights of an individual under
chapter 394, the First District Court of Appeal concluded that “if there is a conflict
in these laws, both the duty of the guardian and the power of the circuit court in the
guardianship proceeding must give way to the ward’s right under the Baker Act to
be released to a less restrictive environment” and that all “provisions of the
guardianship law regarding the residence of the ward, are inapplicable to Baker
Act patients.” This is the same appellate case that defines the role of the public
defender or private attorney representing a client in a Baker Act matter to serve “as

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
90
an independent advocate for the patient, not as a neutral party charged with the
responsibility of determining the best interests of the patient or the needs of
society.” Id.
If the guardian indeed has the authority provided in the court order to make
treatment decisions for the ward, she can do this without conversing with her son.
However, for a guardian advocate’s authority to make treatment decisions on
behalf of the individual, he/she must have spoken with the patient and the doctor in
person if possible, and, if not, by phone, before providing consent.
If there is a legal order prohibiting communication between the guardian and ward,
you may have another issue. If the patient violates the order, it could potentially
result in criminal charges for violating the order.
Since the attorney for the mother will be attending the hearing in her place, he/she
might be interested in the summary of a Sixth Circuit case (not appealed) when an
attorney other than the assistant state attorney wants to question witnesses, In In re
[V.S.], No. 95-577-IN 003 (Fla. 6th Cir. Ct. Feb. 13, 1995), with regard to the
participation of the attorney for a receiving facility in a Baker Act involuntary
placement hearing, the court held that
the facility has every right to employ legal counsel to represent their
legal interests in any proceeding where the facility’s legal rights,
liabilities or corporate interests are implicated.
Since future actions of the facility, either in providing ordered
treatment, or arranging for discharge of the patient, are predicated on
the outcome of the hearing, the facility is entitled to have counsel
present during the adjudicatory process. Counsel for the facility,
although present at the hearing, may not interpose evidentiary
objections or participate in questioning witnesses. This is the assigned
role of the state attorney. While the facility may be a party in interest
for the purpose of placing the controversy before the court, they do
not have a legally protectable interest in the outcome of an
adjudication of the need for involuntary mental health treatment. The
statute permits the facility administrator to throw out the first ball, but
the constitutional rights of the patient require that the state attorney
pitch the game.
If the assistant state attorney is prosecuting the Baker Act petition, he/she probably
won’t need any assistance to argue retention of the patient in the facility. You may
wish to discuss this issue with the patient’s attorney to see if some restriction on

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
91
communication should be placed to avoid legal harm to his/her client.
A guardian appointed by an out-of-state court has her ward in our facility.
Does the guardian need to have the court in Florida re-establish the
guardianship in this state?
There is no reason that the current guardian has to re-create the existing
guardianship in Florida that was previously established in another state. Florida’s
guardianship law recognizes “foreign” guardians and gives full faith and credit to
such orders. However, the order must be filed with the local circuit’s clerk of court,
and once filed with the clerk, the laws of Florida apply.
744.306. Foreign guardians.
(1) When the residence of a ward of a foreign guardian is moved to
this state, the guardian shall, within 60 days after such change of
residence, file the authenticated order of her or his appointment with
the clerk of the court in the county where the ward resides. Such order
shall be recognized and given full faith and credit in the courts of this
state. The guardian and the ward are subject to this chapter.
If a person who has a plenary guardian (with full guardianship over the
person and property) is ordered to involuntary outpatient services, does the
court still have to seek the guardian’s authority to determine housing and
treatment, or does the IOP takes precedence?
There is no legal reason why an IOP court order would need to include housing or
treatment because the circuit court has already authorized the plenary guardian to
make such decisions. It may be that the guardian believes that the additional IOP
court order will assist in getting the ward to comply, considering that a judge has
specifically ordered it rather than just authorizing the guardian to make the
decisions.
If a person already has a court-appointed guardian, does the guardian need to
complete the guardian advocate test and submit the results to the court?
No. A guardian is not responsible for taking the guardian advocate course. If a
person has a guardian appointed by the court, no guardian advocate is needed.
However, it is essential that the receiving facility obtain a copy of the court order
to ensure the guardian is actually the individual appointed by the court, as well as
the letters of guardianship that specify whether the guardianship is a plenary one
(all rights) or a limited one where only certain rights have been removed from the
person and assigned to the guardian. The guardianship, if limited, must specify that

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
92
the guardian has the power to make medical and mental health decisions for the
person.
Can a court-appointed guardian consent for outpatient electroconvulsive
treatment on a patient who has been found incompetent without court
approval, or is the court-appointed guardian and attending physician
required to submit a petition to the court requesting the authorization for
ECT?
A plenary guardian appointed by the court under chapter 744 can consent. A
guardian advocate cannot consent to ECT on behalf of the patient without the
express approval of the court provided in a second hearing. § 394.4598, Fla. Stat.
Baker Act form CF-MH 3108, titled “Petition Requesting Court Approval for
Guardian Advocate to Consent to Extraordinary Treatment,” has been developed
for use in this situation.
3. Guardian Advocates
Who is authorized to serve as a guardian advocate?
Section 394.4598(6), Florida Statutes (emphasis added), provides:
In selecting a guardian advocate, the court shall give preference to a
health care surrogate, if one has already been designated by the
patient. If the patient has not previously selected a health care
surrogate, except for good cause documented in the court record,
the selection shall be made from the following list in the order of
listing:
(a) The patient’s spouse.
(b) An adult child of the patient.
(c) A parent of the patient.
(d) The adult next of kin of the patient.
(e) An adult friend of the patient.
(f) An adult trained and willing to serve as guardian advocate for
the patient.
The Legislature was clear that the preferred candidate to be appointed as a

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
93
guardian advocate was to be a family member or friend of the patient. Only when
no such family member or friend is willing and able to serve may the court appoint
an “adult training and willing to serve” who isn’t a relative or friend. To skip over
any person in the order of listing in the law, the court must document good cause in
the record.
In 2016, a new subsection (2) was added to section 394.4598, Florida Statutes, to
prohibit the following persons from being appointed as a patient’s guardian
advocate:
(a) A professional providing clinical services to the patient under this part.
(b) The licensed professional who initiated the involuntary examination of the
patient, if the examination was initiated by professional certificate.
(c) An employee, an administrator, or a board member of the facility providing
the examination of the patient.
(d) An employee, an administrator, or a board member of a treatment facility
providing treatment of the patient.
(e) A person providing any substantial professional services, excluding public
and professional guardians, to the patient, including clinical services.
(f) A creditor of the patient.
(g) A person subject to an injunction for protection against domestic violence
under s. 741.30, whether the order of injunction is temporary or final, and for
which the patient was the petitioner.
(h) A person subject to an injunction for protection against repeat violence,
stalking, sexual violence, or dating violence under s. 784.046, whether the order of
injunction is temporary or final, and for which the patient was the petitioner.
Regardless of which person on the list of eligible persons is appointed as guardian
advocate, he/she is required to undergo the training required by law. The law
makes no exception. However, the court is authorized to waive some or all of the
training requirements for guardian advocates or impose additional requirements.
The court must make its decision on a case-by-case basis and consider the
experience and education of the guardian advocate, the duties assigned, and the
needs of the patient.
What is the court’s obligation regarding guardian advocate training
according to Florida Statutes?

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
94
Section 394.4598, Florida Statutes (emphasis added), provides:
(4) In lieu of the training required of guardians appointed pursuant
to chapter 744, a guardian advocate must, at a minimum, participate in
a 4-hour training course approved by the court before exercising his or
her authority. At a minimum, this training course must include
information about patient rights, psychotropic medications, the
diagnosis of mental illness, the ethics of medical decision-making,
and duties of guardian advocates.
(5) The required training course and the information to be supplied
to prospective guardian advocates before their appointment must be
developed by the department, approved by the chief judge of the
circuit court, and taught by a court-approved organization, which
may include, but is not limited to, a community college, a
guardianship organization, and a local bar association, or The Florida
Bar. The court may waive some or all of the training requirements
for guardian advocates or impose additional requirements. The
court shall make its decision on a case-by-case basis and, in
making its decision, shall consider the experience and education of
the guardian advocate, the duties assigned to the guardian
advocate, and the needs of the patient.
In 1996–1997 the chief judges in each of the 20 circuits approved a self-
instructional manual for guardian advocates developed by DCF that incorporated
the four hours of training in content required by the law. In addition, online
training is available at
http://www.dcf.state.fl.us/programs/samh/mentalhealth/training/index.shtml.While
the law seems to imply that instructor-led courses would be the norm similar to
those designed for plenary guardians who are authorized to make many decisions
even before training is completed, this wasn’t practical for guardian advocates for
whom there generally isn’t time to attend a course prior to having to make
decisions.
When does the training occur for newly appointed guardian advocates —
before or after their appointment?
The law says that facilities must provide the prospective guardian advocate with
information about the duties and responsibilities of GAs, including information
about the ethics of medical decision-making prior to the appointment. However,
the four-hour training course for GAs must be completed before the GA is
authorized to provide treatment decisions on behalf of the individual. The training

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
95
can be provided prior to appointment or after, as long as you’ve documented that
the training was complete and the GA passed the test. Of course, the GA must
speak with the individual and the physician before providing consent to treatment
— this must be done in person if possible; if not, by telephone.
Once a person has completed the guardian advocacy training for a patient,
does he/she ever have to take it again in the future for the same patient if the
patient ever returns to the Baker Act facility in the future, whether it is weeks,
months, or years later?
No. The proposed guardian advocate doesn’t need to undergo the four-hour
training course a second time if successful completion of the course is documented
in your records, unless the court requires additional training. There is a
recommended Baker Act form CF-MH 3120 that can be used as a “Certification of
Guardian Advocate Training Completion.”
The previous director of our unit has been serving as a volunteer guardian
advocate for persons found to be incompetent to provide express and
informed consent. Is there any problem with this role?
The Baker Act prohibits certain people from serving as a guardian advocate, as
follows:
394.4598. Guardian advocate (emphasis added)
(1) . . . . A guardian advocate must meet the qualifications of a
guardian contained in part IV of chapter 744, except that a
professional referred to in this part, an employee of the facility
providing direct services to the patient under this part, a departmental
employee, a facility administrator, or member of the Florida local
advocacy council shall not be appointed. A person who is appointed
as a guardian advocate must agree to the appointment.
Since the previous director is a licensed mental health counselor, he/she is “a
professional referred to in this part.” Some people believe this to mean a
professional currently serving in a clinical role for the person, but the law doesn’t
state this. Further, the law distinguishes the “professional” from those who are
employed by a facility providing direct services to the patient. Your hospital
attorney and the court need to determine if the previous director or any other
licensed professional can serve in this capacity.
Your unit’s previous director shouldn’t serve as a health care proxy (interim
decision maker) for anyone in your hospital. The list of people who can be

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
96
considered under chapter 765, Florida Statutes, is limited to family or a close
personal friend. The only other alternative is an LCSW under very limited
circumstances.
There are strong similarities between the list of eligible persons who can serve as
substitute decision makers under the Baker Act and under the advance directive
law. However, the lists are not identical. The advance directive statute limits a
proxy to a guardian, family, a close personal friend, or an independent LCSW.
§ 765.401, Fla. Stat. The Baker Act places preference on a health care surrogate
named by the patient, in an advance directive prepared when the patient was
competent, followed by family, a friend, or an adult trained and willing to serve.
In summary, no “adult trained and willing to serve” specified in the Baker Act to
serve as a guardian advocate can serve as a health care proxy. Neither can an
LCSW serve as a guardian advocate under the Baker Act. Otherwise, a health care
surrogate properly selected from the descending order listed in the advance
directive law will generally be eligible to be appointed as the patient’s guardian
advocate under the Baker Act.
Can a hospital train its own staff to serve as guardian advocates?
No. Section 394.4598(1), Florida Statutes, states that a professional referred to in
the Baker Act, an employee of the facility providing direct services to the person, a
DCF employee, a facility administrator, or a member of the Florida local advocacy
council cannot be appointed as a guardian advocate.
A staff member of a receiving facility would have a direct conflict of interest in
consenting or refusing consent to services recommended for a person in that
receiving facility. Further, no physician, psychologist, social worker, psychiatric
nurse, licensed mental health counselor, or licensed marriage and family therapist
could serve in this role for a person served in another receiving facility due to the
statutory prohibition.
What is the process for, and where would we send, a family member to receive
the training to become a guardian advocate? I currently have a patient in the
hospital and his health care surrogates are requesting this.
The Guardian Advocate Training Manual is available through the DCF website.
A web-based guardian advocate training course is available at
http://www.dcf.state.fl.us/programs/samh/mentalhealth/training/index.shtml.
Who would complete the certification to verify the guardian advocate

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
97
training?
A staff member could administer the “test” and sign the certification. This should
be placed in the patient’s clinical record with other legal forms.
Does the Baker Act prohibit an out-of-state family member guardian advocate
from being appointed?
No. Nothing precludes an out-of-state family member from serving. However,
there will be logistical problems. If the court doesn’t waive the four-hour training
course, the GA would be required to take the course. The Guardian Advocate
Training Manual is located on the DCF website and it is intended as a self-
instructional manual. The GA must speak with the individual and the physician
prior to providing consent for treatment — in person if possible, or by telephone if
not. Disclosure of all required information about treatment and the authorization
for treatment would probably have to be done by telephone — the facility would
want to have two witnesses participating on the call to document what was said by
both parties. Consent forms could be faxed or scanned and emailed to supplement
the verbal authorization received on the call.
Can a guardian advocate consent to laboratory tests or medical procedures?
No. Unless the court has specifically authorized the guardian advocate to consent
to medical treatment, authority is limited to decision-making about mental health
treatment only.
Is a separate second court hearing required to authorize the guardian
advocate to consent for blood draw? If the client is refusing and restraints are
required to obtain the sample, do we have to go to court for approval?
It shouldn’t be necessary to have a second court hearing for the guardian advocate
to get specific authorization to consent for blood draws or to have the person
restrained for such a blood draw if the guardian advocate has been specifically
authorized by the court to consent to medical treatment in addition to psychiatric
treatment. Even prior to the GA appointment, the person may meet the criteria to
serve as the person’s health care proxy. If so, the proxy could provide such consent
if he/she believed the person would have consented to the procedure if competent
to do so. A second hearing is required only in specific circumstances, including:
abortion, sterilization, electroconvulsive treatment, psychosurgery, and
experimental treatments.
An attending psychiatrist at our receiving facility wants to file a petition for a
guardian advocate to get court authority to consent for involuntary

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
98
sterilization of the GA’s sister. The patient is expected to deliver within the
next several days by C-section and the doctor recommends a tubal be done at
the same time. The patient is incompetent to consent. This current pregnancy
is a second one — the patient is entirely unable to raise her children — the
sister has custody of the first one and will likely have custody of the second
one when born. Can this be done?
Sterilization is one of the extraordinary procedures that must have a separate
petition filed by the guardian advocate. It is doubtful the court would approve a
non-reversible procedure like this. There is too much historical abuse of
sterilization and experimental studies done on persons with mental illness for this
to be uncontroversial. The public defender may strongly oppose it unless
convinced that this is what his/her client wants. You should have a “Plan B” if the
court doesn’t approve. These are reversible methods that might be more acceptable
if sterilization is not approved. The GA would already have authority to consent to
such an alternative plan. You need to alert the attorney representing your receiving
facility or risk management, since this petition might get significant visibility.
Can a guardian advocate charge a client for services?
There isn’t any prohibition for such a practice if the client is competent to contract
for this service. Given that a GA is appointed only when the person is adjudicated
incompetent to consent, this would be very questionable. Section 394.4598(1),
Florida Statutes, requires that a GA meet the qualifications of a guardian contained
in part IV of chapter 744 and specifically prohibits certain people from serving:
Individuals will be appointed to be a guardian advocate in this order: the health
care surrogate named by the person; a relative; or a friend. Only if none of these
people are available and willing to serve can an adult trained and willing to serve
as guardian advocate for the person be named by the court. § 394.4598(6), Fla.
Stat.
Can a petition for involuntary placement reflect that a person is competent to
consent to treatment? If yes, is the section of the petition regarding guardian
advocacy left incomplete? Does the person then need a proxy?
A person may “refuse” placement instead of being “unable to determine” that
placement is necessary. If refusing placement, it is possible that the person retains
competency to consent or refuse consent to his/her own treatment. This is the very
circumstance that the second question on page 2 of the involuntary placement
petition is intended to cover. If the person is competent to consent/refuse to
consent or a court-appointed guardian for mental health decision-making is already

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
99
appointed, #2 would be checked and the other questions on the petition would not
be answered. If the person is competent to make his/her own treatment decisions, a
proxy would be inappropriate.
If a guardian advocate is ordered for a patient who is subsequently
transferred to a state hospital, are we responsible for obtaining a different
guardian advocate?
A guardian advocate is appointed by the originating court to serve until the
person’s order expires, or until he/she transfers to voluntary status (must be
competent to make well-reasoned, willful, and knowing decisions about medical,
mental health, or substance abuse treatment) or is discharged from a facility (no
longer meeting involuntary placement criteria). The guardian advocate, generally a
family member, isn’t appointed just for the time in a single facility. The GA is
appointed to serve the person, wherever he/she is, not to serve a facility. If the
appointment was intended to apply only when the patient is at your facility, the
court should be notified of this so a different GA could be selected if possible. The
state mental health facility might not accept the person if no GA would be
available to make treatment decisions on behalf of the person and there may not be
access to a GA to serve.
If a guardian advocate is unexpectedly no longer able or willing to serve, a
procedure is laid out in rule 65E-5.230, Florida Administrative Code, as follows:
(3) When a guardian advocate previously appointed by the court
cannot or will not continue to serve in that capacity, and the person
remains incompetent to consent to treatment, the facility administrator
shall petition the court for a replacement guardian advocate. A copy of
the completed petition shall be given to the person, the current
guardian advocate, the prospective replacement guardian advocate,
person’s attorney, and representative, with a copy retained in the
person’s clinical record. Recommended form CF-MH 3106, “Petition
for Adjudication of Incompetence to Consent to Treatment and
Appointment of a Guardian Advocate,” as referenced in subparagraph
65E-5.170(1)(d)2., F.A.C., may be used for this documentation if
Parts I and III are completed.
Are guardian advocates immune from liability for treatment decisions they
make for patients?
You may need to consult with your attorney, but it doesn’t appear that the law
offers any immunity. If the GA appointed by the court is volunteering under the

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
100
supervision of a public or nonprofit organization, the volunteer is covered under
Florida’s Volunteer Protection Act (section 768.1355, Florida Statutes).
A corporation that provides guardian advocate services to patients of our
hospital often does not have anyone show up for the hearings, despite notice
given. The GA calls the next day and speaks to the client by phone. We then
have to find a way for the GA to talk to the psychiatrist. This all must be done
prior to the GA consenting for the medications. Any suggestions?
There is no legal requirement for the guardian advocate to actually attend the
hearing, and it is even questionable whether the GA would have the right to do so
until after the appointment took place, due to the confidentiality of the information
discussed. However, given that the person may have had medications delayed from
the time of admission until the time of the hearing (7-10 days), any further delay
seems unreasonable. If it is the corporation named in the order, it should be easy
enough to arrange for another agent of the corporation to come promptly to the
hospital after appointment.
Section 394.4598(3), Florida Statutes, provides: “Before giving consent to
treatment, the guardian advocate must meet and talk with the patient and the
patient’s physician in person, if at all possible, and by telephone, if not”
(emphasis added). A pattern of delay should cause your hospital to consider
finding an alternative service, especially since the hearing date is predictably the
same each week.
4. Health Care Surrogates/Proxies
What kind of liability does a health care surrogate/proxy have for his or her
decision-making on behalf of a person found incompetent to consent to
treatment?
The advance directive law provides the following immunity for surrogates/proxies,
as well as for providers in providing care under the statute:
765.109. Immunity from liability; weight of proof; presumption
(1) A health care facility, provider, or other person who acts under
the direction of a health care facility or provider is not subject to
criminal prosecution or civil liability, and will not be deemed to have
engaged in unprofessional conduct, as a result of carrying out a health
care decision made in accordance with the provisions of this chapter.
The surrogate or proxy who makes a health care decision on a
patient’s behalf, pursuant to this chapter, is not subject to criminal

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
101
prosecution or civil liability for such action.
(2) The provisions of this section shall apply unless it is shown by
a preponderance of the evidence that the person authorizing or
effectuating a health care decision did not, in good faith, comply with
the provisions of this chapter.
Our local CSU has asked me to serve as a proxy now that I’m no longer
working there, but I’m wondering about liability as an LCSW. I do not have
my own liability insurance. Do you have any thoughts on this?
The advance directive statute regarding health care proxies provides:
765.401. The proxy
(1) If an incapacitated or developmentally disabled patient has not
executed an advance directive, or designated a surrogate to execute an
advance directive, or the designated or alternate surrogate is no longer
available to make health care decisions, health care decisions may be
made for the patient by any of the following individuals, in the
following order of priority, if no individual in a prior class is
reasonably available, willing, or competent to act:
(a) The judicially appointed guardian of the patient or the guardian
advocate of the person having a developmental disability as defined in
s. 393.063, who has been authorized to consent to medical treatment,
if such guardian has previously been appointed; however, this
paragraph shall not be construed to require such appointment before a
treatment decision can be made under this subsection;
(b) The patient’s spouse;
(c) An adult child of the patient, or if the patient has more than one
adult child, a majority of the adult children who are reasonably
available for consultation;
(d) A parent of the patient;
(e) The adult sibling of the patient or, if the patient has more than
one sibling, a majority of the adult siblings who are reasonably
available for consultation;
(f) An adult relative of the patient who has exhibited special care
and concern for the patient and who has maintained regular contact

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
102
with the patient and who is familiar with the patient’s activities,
health, and religious or moral beliefs; or
(g) A close friend of the patient.
(h) A clinical social worker licensed pursuant to chapter 491, or
who is a graduate of a court-approved guardianship program. Such a
proxy must be selected by the provider’s bioethics committee and
must not be employed by the provider. If the provider does not have a
bioethics committee, then such a proxy may be chosen through an
arrangement with the bioethics committee of another provider. The
proxy will be notified that, upon request, the provider shall make
available a second physician, not involved in the patient’s care to
assist the proxy in evaluating treatment. Decisions to withhold or
withdraw life-prolonging procedures will be reviewed by the facility’s
bioethics committee. Documentation of efforts to locate proxies from
prior classes must be recorded in the patient record.
(2) Any health care decision made under this part must be based on
the proxy’s informed consent and on the decision the proxy
reasonably believes the patient would have made under the
circumstances. If there is no indication of what the patient would have
chosen, the proxy may consider the patient’s best interest in deciding
that proposed treatments are to be withheld or that treatments
currently in effect are to be withdrawn.
What’s most important is that you not be asked to serve if there is any guardian,
family member, or friend who is willing and able to serve. The receiving facility
should have already made a diligent effort to obtain such family or friend to serve
before even contacting you. If you are asked to serve, it must be after referral by an
ethics committee — most medical hospitals have such a committee if the CSU
does not. Most ethics committees have an expedited procedure, and there wouldn’t
have to be a delay for some scheduled meeting. Use of Baker Act forms CF-MH
3122 (Certification of Person’s Incompetence to Consent to Treatment and
Notification of Health Care Surrogate/Proxy) and CF-MH 3123 (Affidavit of
Health Care Proxy) may help in ensuring compliance with the law and rules.
If you agree to serve as a proxy, your exclusive obligation is to the patient, not the
convenience of the receiving facility. The decision is whether to consent and, if so,
what the individual would have consented to if competent (substitute judgment
standard). Only when this isn’t known can a “best interest” standard be used in
decision-making.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
103
The Baker Act rules permit use of a surrogate or proxy only on an interim basis —
a petition for involuntary placement and appointment of a guardian advocate must
be filed within two court working days of the certification of incapacity by the
physician. You must also be provided the same information that is required by law
to be provided to guardian advocates and can consent to treatment for the person
only after talking to the individual and to the physician — in person if possible and
if not, by telephone.
If a person needs medications but refuses them and has been determined by a
physician not to have capacity to make his or her own treatment decisions,
can a facility staff legally call a family member or close friend to be a health
care proxy without the person’s consent?
Yes. A facility can contact the person highest on the list of eligible proxies to seek
his or her involvement. The federal HIPAA law recognizes state statutory authority
to designate persons who will “stand in the shoes of the person,” such as guardians,
guardian advocates, and health care surrogates and proxies. Section 765.401(1),
Florida Statutes, lists individuals who, in the order of listing, can be selected by the
provider to act as proxy.
The Baker Act rules indicate that when a person has not executed an advance
directive, health care decisions may be made by an eligible proxy during the
interim period between the time the person is determined by the physician to
be incompetent to consent to treatment and the time a guardian advocate is
appointed by a court. Would there be any conflict with HIPAA allowing a
proxy to make decisions, since the person did not have an advance directive?
No. HIPAA defers to the state laws in recognizing individuals who are authorized
to “stand in the shoes of the person” for decision-making purposes in each state.
This includes guardians, guardian advocates, and health care surrogates/proxies in
Florida.
Can health care surrogates and proxies give consent to mental health
treatment?
Yes. Florida’s advance directive law is clear that it applies to any and all health
care decisions — this includes mental health decisions as well. The following
provisions help to reinforce this issue:
765.101. Definitions (emphasis added)
(10) “Incapacity” or “incompetent” means the patient is physically
or mentally unable to communicate a willful and knowing health care

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
104
decision. For the purposes of making an anatomical gift, the term also
includes a patient who is deceased.
765.205. Responsibility of the surrogate (emphasis added)
(1) The surrogate, in accordance with the principal’s instructions,
unless such authority has been expressly limited by the principal,
shall:
(a) Have authority to act for the principal and to make all health
care decisions for the principal during the principal’s incapacity.
765.202. Designation of a health care surrogate (emphasis added)
(5) A principal may designate a separate surrogate to consent to
mental health treatment in the event that the principal is determined
by a court to be incompetent to consent to mental health treatment and
a guardian advocate is appointed as provided under s. 394.4598.
However, unless the document designating the health care surrogate
expressly states otherwise, the court shall assume that the health care
surrogate authorized to make health care decisions under this chapter
is also the principal’s choice to make decisions regarding mental
health treatment.
765.204. Capacity of principal; procedure (emphasis added)
(1) A principal is presumed to be capable of making health care
decisions for herself or himself unless she or he is determined to be
incapacitated. Incapacity may not be inferred from the person’s
voluntary or involuntary hospitalization for mental illness or from
her or his intellectual disability.
The Florida Administrative Code governing the Baker Act also has extensive
provisions governing the use of health care surrogates and proxies as interim
decision makers until a guardian advocate is appointed by the court.
Can a health care surrogate or proxy make treatment decisions for a person
in a Baker Act facility?
Yes, but only for a person who is on involuntary status and for whom a petition is
to be filed with the court in a timely way requesting the appointment of a guardian
advocate.
If an involuntary placement petition is completed on the weekend and there is

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
105
a proxy, can we still medicate the patient before filing on the next business
day?
Yes, as long as the petition has been completed within the 72 hours permitted by
law and that point in time falls on a weekend or legal holiday and you file the
petition with the court on the next court working day. You can continue to seek
authorization for treatment from the health care proxy until the court acts on your
request for appointment of a guardian advocate.
Once a physician documents that a patient is incompetent and has no
healthcare surrogate or legal guardian, can we as a facility appoint a
healthcare proxy? Our local magistrate recently denied us permission to use a
proxy. Our interpretation was that we didn’t need the court’s permission. We
recognize that the proxy is time limited. Isn’t the point of a proxy to avoid
ETOs or, worse yet, a lack of treatment until the court hearing?
Rule 65E-5.2301, Florida Administrative Code, governing the use of a health care
surrogate or proxy, was added to the rules in 1998 to provide for an interim
decision maker between the time a person is determined to be incompetent to
consent to treatment by one or more physicians and the time a guardian advocate is
appointed by a court. The court has no role in issues relating to health care
surrogates or proxies unless a complaint is made and the court is responsible for
investigating the complaint. As long as a receiving or treatment facility submits a
petition for involuntary placement and appointment of a guardian advocate within
two court working days of the determination by a physician of an individual’s
incompetence to consent to treatment, the court shouldn’t have a concern.
5. Powers of Attorney
Does a power of attorney for health care override a Baker Act?
No. A person with a POA or a health care surrogate/proxy can consent only to
treatment, not to admission. Adults with a substitute decision maker must remain
on involuntary status because of their incapacity.
Can a power of attorney give consent to the admission or treatment of a
person in a Baker Act facility?
A durable power of attorney is insufficient to authorize the admission of a person
on a voluntary basis or to consent to treatment for a person, regardless of his or her
legal status. However, if the POA is in the form of an advance directive for health
care, the surrogate named in the advance directive can make treatment decisions
but not the decision to admit the person to a facility. Such admission must be on an

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
106
involuntary basis.
IX. Selected Model Baker Act Forms for Informed Consent and Use of
Substitute Decision Makers
Please note that these recommended forms were promulgated by DCF before
the 2016 statutory amendments and do not incorporate those changes.

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
107
A. Petition for Adjudication of Incompetence to Consent to Treatment and
Appointment of a Guardian Advocate
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: __________________________
Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate
PART I
I, __________________________________________________________________________, Administrator of
__________________________________________________________________________________________
Name of Facility
__________________________________________________________________________________________
Facility Address
hereby recommend that
_______________________________________________________________________ be adjudicated
incompetent to consent to:
Mental health treatment
Medical treatment
and that a guardian advocate be appointed to make such health care decisions for the person. The person
is presently placed in the County of _____________ and has residence in the County of _____________.
OR
Is presently ordered to involuntary outpatient placement in the County of :________________________.
PART II Psychiatric Opinion Supporting the Petition
I,_________________________________________________, a psychiatrist authorized to practice in the
State of Florida, have personally examined __________________________________________________
Name of Person Examined
on _____________, and found his/her judgment to be so affected by a mental illness that he/she lacks the
Date
capacity to make a well-reasoned, willful, and knowing decision concerning his/her medical and/or
mental health care. Observations which support this opinion are: _____________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
___________________________________________ _________________ ___________ am pm
Signature of Psychiatrist Date Time
___________________________________________ _________________________________
Typed or Printed Name of Psychiatrist License Number
CONTINUED OVER

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
108
Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate (Page 2)
PART III - Proposed Guardian Advocate
________________________________________________________________________, who resides at
____________________________________________________________________________ and whose
relationship to the person is ____________________________, has agreed to serve as guardian advocate.
He/she has been provided with information about the duties and responsibilities of guardian advocates,
including the information about the ethics of medical decision-making.
_____________________________________________ __________________ __________ am pm
Signature of Administrator or Designee Date Time
_____________________________________________
Typed or Printed Name of Administrator or Designee
Complete Parts I, II, and III to Petition for a Guardian Advocate
Complete Part I only to petition the Court to expand a current guardian advocate’s authority to provide
consent to medical treatment in addition to mental health treatment.
Complete Part I and Part III to request the circuit court to appoint a substitute guardian advocate for
one who cannot or will not perform his or her duties.
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy
Provided
Time Copy Provided
Initial of Who Provided
Copy
Person
am pm
Representative
am pm
Current Guardian Advocate
am pm
Prospective Guardian Advocate
am pm
Person’s Attorney
am pm
See s. 394.4598(1), (2), (3), (4), (5), (6), Florida Statutes
CF-MH 3106, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
109
B. Order Appointing Guardian Advocate
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: ______________________
Order Appointing Guardian Advocate
This matter came to be heard on the issue of whether the above-named person should be adjudicated incompetent to
consent to treatment, and the Court finds by clear and convincing evidence as follows:
1. Said person has been represented by counsel.
2. Said person is not presently adjudicated incapacitated with a duly appointed guardian with authority to consent
to treatment.
3. Said person meets the definition for being incompetent to consent to treatment pursuant to Section 394.455 (15),
Florida Statutes.
This finding is determined from the testimony of _________________________________________. The court
has considered testimony and other evidence regarding said person’s competence to consent to treatment and
based on such testimony and evidence has concluded that said person is not competent to consent to treatment.
On the basis of these findings, it is hereby,
ORDERED
That the above-named person presently within the county, is incompetent to consent to treatment because his/her
judgment is so affected by a mental illness that he/she lacks the capacity to make a well-reasoned, willful, and
knowing decision concerning his or her medical and/or mental health treatment.
___________________________________________________________, whose relationship to the person is:
Name of Guardian Advocate
1. Health Care Surrogate 2. Person’s Spouse 3. Person’s Adult Child 4. Person’s Parent
5. Person’s Adult Next of Kin 6. Person’s Adult Friend 7. Adult Trained and Willing to Serve
Has agreed to serve as guardian advocate and:
a. Will obtain from the facility sufficient information in order to decide whether to give express and informed
consent to the treatment, including information that the treatment is essential to the care of the person, and that
the treatment does not present an unreasonable risk of serious, hazardous, or irreversible side effects.
b. Has agreed to meet and talk to the person and the person’s physician in person, if at all possible, and by
telephone if not, before giving consent to treatment.
c. Has or will undergo a training course approved by this Court prior to exercising this authority, unless waived by
this Court.
d. Will be provided access to the appropriate clinical records of the person.
This guardian advocate has been given authority by this Court to consent, refuse consent, or revoke consent for:
mental health treatment medical treatment
but may not consent to abortion, sterilization, electroconvulsive treatment, psychosurgery, or experimental
treatments unless express Court approval in a separate proceeding is given.
This appointment as Guardian Advocate shall terminate upon the discharge of the person from an order for
involuntary outpatient placement or involuntary inpatient placement or the transfer of the person to
voluntary status, or an order of the court restoring the person’s competence.
DONE AND ORDERED this _______________ day of _________________________, _______________
____________________________________________ ____________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
cc: Person ___ Guardian Advocate ___ Representative ___ Facility Administrator ___ Person’s Attorney
See s. 394.455(15), 394.4598(1), (2), (3), (4), (6), (7), Florida Statutes
CF-MH 3107, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
110
C. Petition Requesting Court Approval for Guardian Advocate to Consent to
Extraordinary Treatment
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Petition Requesting Court Approval for
Guardian Advocate to Consent to Extraordinary Treatment
_____________________________________________, guardian advocate appointed on ____________________
Name of Guardian Advocate Date
for ______________________________________________,
Name of Person.
Said person is presently:
Placed on an inpatient basis in ______________________________________a receiving or treatment facility in
_____________________ County and has residence in __________________________________ County, or
Involuntarily placed on an outpatient basis in ______________County. The service provider is: _________________
Psychiatric or Medical Opinion Supporting the Petition
I,_________________________________, a psychiatrist or physician authorized to practice in the State of Florida,
Name of Psychiatrist or Physician
have personally examined _______________________________________ on ________________, and found
Name of Person Date
that he/she is in need of the following treatment or procedure: ___________________________________________
_____________________________________________________________________________________________
Observations which support this opinion are: _________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
This treatment or procedure is essential to the care of the person and the treatment does not present an unreasonable
risk of serious, hazardous, or irreversible side effects.
_____________________________________________ ___________________ __________ am pm
Signature of: Psychiatrist Physician Date Time
_____________________________________________ ____________________________
Typed or Printed Name of Psychiatrist or Physician License Number
_____________________________________________ ___________________ ___________ am pm
Guardian Advocate’s Signature Date Time
_____________________________________________
Typed or Printed Name of Guardian Advocate
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who
Provided Copy
Person
am pm
Guardian Advocate
am pm
Representative
am pm
Person’s Attorney
am pm
Facility Administrator
am pm
See s. 394.4598(6), Florida Statutes
CF-MH 3108, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
111
D. Order Authorizing Guardian Advocate to Consent to Extraordinary
Treatment
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Order Authorizing Guardian Advocate to Consent to Extraordinary Treatment
This matter came to be heard on the issue of whether ______________________________________ guardian
Name of Guardian Advocate
advocate for the above-named person who is involuntarily placed should be given express court approval for
extraordinary treatment. Upon the evidence presented, the Court finds as follows:
1. The petitioner was appointed as the guardian advocate for the above-named person by order previously
entered in this cause after an earlier hearing.
2. The person has been represented by counsel.
3. The treatment or procedure approved herein is essential to the care of the person and the treatment does
not present an unreasonable risk of serious, hazardous, or irreversible side effects.
On the basis of these findings, it is hereby,
ORDERED
That the above-named guardian advocate for the above-named person, presently within the county, is
authorized to provide consent for:
________________________________________________________________________________________.
The Guardian Advocate’s appointment shall terminate upon the discharge of the person from an order
for involuntary outpatient placement or involuntary inpatient placement, or when the person is
transferred to voluntary status, or by order of the court restoring the person’s competence.
DONE AND ORDERED this _______________ day of ___________________, _________________.
________________________________________________ __________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initial of Who
Provided Copy
Person
am pm
Guardian Advocate
am pm
Person’s Attorney
am pm
Facility Administrator
am pm
See s. 394.4598(6), Florida Statutes
CF-MH 3109, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
112
E. Authorization for Electroconvulsive Treatment
Authorization for Electroconvulsive Treatment
As the physician for this person, I have recommended a series of ____________ electroconvulsive treatments and have
provided sufficient information to ensure express and informed consent to the treatment.
__________________________ _______________________ ____________ ___________ am pm
Signature of Physician Printed Name of Physician Date Time
I have agreed with the need for this series of __________ electroconvulsive treatments after
examination of the person or review of the person’s treatment records. I am not directly involved with the person.
____________________________ _______________________________ ______________ ______ am pm
Signature of Second Physician Printed Name of Second Physician Date Time
I, the undersigned, competent adult, guardian, guardian advocate, health care surrogate
authorize ___________________________ Electroconvulsive Treatments for ______________________.
Number of treatments authorized Name of Person to Receive Treatment
a person in ___________________________________________________________________________________
Name of Facility
The information provided to the person to make the decision to consent to electroconvulsive treatment (which must
include the purpose of the procedure, the common side effects, alternative treatments, and the approximate number of
procedures considered necessary and that my consent may be revoked prior to or between treatments) is:
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
I have read and understood the information provided to me above and have been given an opportunity to ask questions and
receive answers about the procedures. Knowing the above, I hereby consent to the treatment described.
_________________________________________ ___________________ _______________ am pm
Signature of Competent Adult Date Time
________________________________________ __________________ ______________ am pm
Signature, * as appropriate, of: Date Time
Guardian, Guardian Advocate,
Parent of a Minor, Health Care Surrogate
____________________________________ __________________ ______________ am pm
Signature of Witness Date Time
Facility should attach information about or copies of educational materials provided to the person and/or
substitute decision maker.
* A guardian shall produce letters of guardianship prior to authorizing ECT to demonstrate authority to
provide consent. A guardian advocate requires express Court approval to provide consent to this
procedure. A health care surrogate requires an advance directive expressly delegating such authority to the
surrogate. In the absence of such an advance directive, a health care surrogate or proxy require express
court approval to consent to ECT. The authorizing documentation must be validated by staff and filed in the
person’s clinical record.
See s. 394.459(3)(b), 458.325, Florida Statutes
CF-MH 3057, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
113
F. Notification to Court of Person’s Competence to Consent to Treatment and
Discharge of Guardian Advocate
Notification to Court of Person’s Competence to Consent
to Treatment and Discharge of Guardian Advocate
________________________________________, a guardian advocate appointed by the court on
Name of guardian advocate
________________________ for __________________________________________ who was:
Date of appointment Name of person
Court ordered for involuntary inpatient placement located at _________________________________
Name of receiving or treatment facility
OR
Court ordered for involuntary outpatient placement with services provided by: _________________
Name of service provider
Has been discharged from his or her duties on __________, 20____ due to the person’s regaining
competence to consent to his or her own treatment.
________________________________________________________________
Printed Name of Facility Administrator/Service Provider or Designee
________________________________________________________________ _____________________
Signature of Facility Administrator/Service Provider or Designee Date
See s. 394.4598(6), Florida Statutes
CF-MH 3121, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Two Express and Informed Consent
_____________________________________________________________________________________
Baker Act Benchguide November 2016
114
G. Findings and Recommended Order Restoring Person’s Competence to
Consent to Treatment and Discharging the Guardian Advocate
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _____________________________________ CASE NO.: _______________
Findings and Recommended Order Restoring Person’s Competence
to Consent to Treatment and Discharging the Guardian Advocate
A hearing was held on _______________________, to consider the continued involuntary placement of
__________________________________, a person placed at ___________________________________
facility. This person was previously found incompetent to consent to treatment and _____________________
was appointed as guardian advocate.
Testimony and evidence was considered at this hearing regarding the person’s competence, including:
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
On the basis of this evidence, it is recommended that the Court restore this person’s competence to consent to
treatment and that the guardian advocate previously appointed be discharged.
_____________________________________________ __________________ ___________ am pm
Signature of Administrative Law Judge Date Time
_____________________________________________
Typed or Printed Name of Administrative Law Judge
It is hereby ordered, that ____________________________________________________ be restored to
competence to consent to treatment and that
_______________________________________________________, guardian advocate be discharged.
ORDERED this_______________ day of _____________________.
___________________________________ ___________________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.467(7)(f), Florida Statutes
CF-MH 3116, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
115
Chapter Three: Admission and Treatment for Minors
(Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
I. Cautionary Note
Many statutes, case law decisions, and rules govern how minors are to be treated in
Florida. Some of these legal requirements regarding mental health differ, based on
whether the minor lives with his/her own family or is in the custody of the DCF or
the Department of Juvenile Justice, whether the minor is on voluntary or
involuntary status, whether the issue relates to admission or to treatment, and
whether the issue relates to inpatient, residential, or outpatient settings. Mental
health requirements applying to minors are different than those applying to
substance abuse and general medical examination/treatment.
The Baker Act makes only a few distinctions between adults and minors. Where
distinctions are not made, adults and minors have the same rights. Specific
provisions regarding the admission and treatment of minors in the Baker Act and
other statutes are summarized here, with the corresponding statutory references.
Since the Baker Act contains so few specific references to minors, and since this
law must be carried out in the context of other coexisting statutes and case law, it is
important for each professional and mental health agency to involve legal counsel
in reviewing policies and procedures for properly carrying out one’s
responsibilities. Legal consultation on an ongoing basis is necessary to ensure
responsible and lawful conduct. In each circumstance in which consent to
admission and/or treatment is sought for a minor, it is essential that the
professional consider the nature and context of the consent in determining whether
the consent is legally sufficient.
II. Minority/Non-Age
A. Definition
“‘Adult’ means an individual who is 18 years of age or older or who has had the
disability of nonage removed under chapter 743.” § 394.455(4), Fla. Stat.
“‘Minor’ means an individual who is 17 years of age or younger and who has not
had the disability of nonage removed pursuant to s. 743.01 or s. 743.015.”
§ 394.455(29), Fla. Stat.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
116
While the text of the Baker Act occasionally uses the term “minor” or “adult,” in
which case these definitions apply, it also uses the phrases “age 17 and under,”
“under 18 years of age,” or “18 years of age or older” in many other citations. In
such instances, the more precise age limitation would apply rather than the more
generic term of “minor” or “adult.”
Regarding a “minor’s” access to outpatient crisis intervention and treatment
(section 394.4784), such access without consent of a parent or guardian is only
available to minors age 13 or older.
B. Removal of Disabilities of Non-Age
Married minors. “The disability of nonage of a minor who is married or has
been married or subsequently becomes married, including one whose
marriage is dissolved, or who is widowed, or widowered, is removed. The
minor may assume the management of his or her estate, contract and be
contracted with, sue and be sued, and perform all acts that he or she could do
if not a minor.” § 743.01, Fla. Stat.
Unwed pregnant minors or minor mothers. “An unwed pregnant minor may
consent to the performance of medical or surgical care or services relating to
her pregnancy by a hospital or clinic or by a physician licensed under
chapter 458 or chapter 459, and such consent is valid and binding as if she
had achieved her majority. [She] may consent to the performance of medical
or surgical care or services for her child by a hospital or clinic or by a
physician licensed under chapter 458 or chapter 459, and such consent is
valid and binding as if she had achieved her majority.” § 743.065, Fla. Stat.
However, this doesn’t affect the provisions of section 390.0111, Florida
Statutes, which governs termination of pregnancies.
Circuit court. “A circuit court has jurisdiction to remove the disabilities of
nonage of a minor age 16 or older residing in this state upon a petition filed
by the minor’s natural or legal guardian or, if there is none, by a guardian ad
litem. . . . The court shall consider the petition and, if satisfied that the
removal of the disabilities is in the minor’s best interest, shall remove the
disabilities of nonage; and shall authorize the minor to perform all acts that
the minor could do if he or she were 18 years of age.” § 743.015, Fla. Stat.
Minors adjudicated as adults. “The disability of nonage of a minor
adjudicated as an adult and in the custody or under the supervision of the
Department of Corrections is removed, as such disability relates to health

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
117
care services, except in regard to medical services relating to abortion and
sterilization.” § 743.066, Fla. Stat.
C. Rights, Privileges, and Obligations of Persons 18 Years of Age or Older
Section 743.07, Florida Statutes, provides in part:
(1) The disability of nonage is hereby removed for all persons in
this state who are 18 years of age or older, and they shall enjoy and
suffer the rights, privileges, and obligations of all persons 21 years of
age or older except as otherwise excluded by the State Constitution
immediately preceding the effective date of this section and except as
otherwise provided in the Beverage Law.
(2) This section shall not prohibit any court of competent
jurisdiction from requiring support for a dependent person beyond the
age of 18 years when such dependency is because of a mental or
physical incapacity which began prior to such person reaching
majority or if the person is dependent in fact, is between the ages of
18 and 19, and is still in high school, performing in good faith with a
reasonable expectation of graduation before the age of 19.
D. Consent to Treatment
Generally, persons under the age of 18 cannot consent to their own treatment
because they are presumed to be legally incompetent as a result of their age or
presumed immaturity of judgment. The mother and father jointly are natural
guardians of their biological and adopted children during minority, and they can
provide consent if necessary, unless their parental rights have been terminated
pursuant to chapter 39, Florida Statutes. § 744.301(1), Fla. Stat. That statute further
provides:
If one parent dies, the natural guardianship passes to the surviving parent,
and the right continues even if the surviving parent remarries.
If the marriage between the parents is dissolved, the natural guardianship
belongs to the parent to whom the responsibility of the child is given. (See
chapter 61, Florida Statutes, governing dissolution of marriage.)
If the parents share parental responsibility, then both continue as natural
guardians.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
118
“If the marriage is dissolved and neither parent is given parental
responsibility for the child, neither may act as natural guardian of the child.”
“The mother of a child born out of wedlock is the natural guardian of the
child and is entitled to primary residential care and custody of the child
unless a court enters an order stating otherwise.”
Upon petition of a parent, brother, sister, next of kin, or other person interested in
the welfare of a minor, the court can appoint a guardian for a minor without
appointing an examining committee or adjudicating the child incapacitated.
§§ 744.3021(1), 744.342. Fla. Stat. A guardian appointed for a minor, whether of
the person or property, has the authority of a plenary guardian. § 744.3021(1), Fla.
Stat. If the minor is age 14 or over, the court must consider the minor’s preference
as to who should be appointed guardian. § 744.312(3)(b), Fla. Stat.
“‘Legal custody’ means a legal status created by a court which vests in a custodian
of the person or guardian, whether an agency or an individual, the right to have
physical custody of the child and the right and duty to protect, nurture, guide, and
discipline the child and to provide him or her with food, shelter, education, and
ordinary medical, dental, psychiatric, and psychological care.” § 39.01(35), Fla.
Stat.
A guardian appointed by the court cannot commit the minor to a facility,
institution, or licensed service provider without a formal placement proceeding
pursuant to chapter 393, chapter 394, or chapter 397, unless the guardian first
obtains specific authority from the court as described in section 744.3725.
§ 744.3215(4)(a), Fla. Stat.
The 2008 Florida Legislature extensively rewrote state laws (chapter 61, Florida
Statutes) governing the dissolution of marriage (SB 2532). This action
substantially changed terms used as well as the relationship among the parties of a
divorce as it pertained to children. It removed the term “divorce,” exchanged the
term “custody” for “parental responsibility,” and changed the term “visitation” to
“time-sharing.” Some of these terms are as follows:
Parenting plan. A document that governs all circumstances among the
parties, including decision-making and time-sharing.
Shared parental responsibility. Court-ordered relationship where both
parents retain full parental rights/responsibilities and shared decision-
making. Certain decisions may be assigned to one parent.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
119
Sole parental responsibility. Court-ordered relationship where one parent
makes decisions (with or without visitation).
Time-sharing schedule. A timetable included in a parenting plan that
specifies the time the child will spend with each parent.
Access to information. Availability of treatment records to either parent
unless the court specifically revokes this right.
III. Consent for Admission to a Mental Health Facility
A. Admission
“A facility may receive for observation, diagnosis or treatment . . . any person age
17 or under and for whom such application is made by his or her guardian . . . only
after a hearing to verify the voluntariness of the consent.” § 394.4625(1), Fla. Stat.
A facility is defined in the Baker Act as “any hospital, community facility, public
or private facility, or receiving or treatment facility providing for the evaluation,
diagnosis, care, treatment, training, or hospitalization of persons who have been
diagnosed as having a mental illness or substance abuse impairment.”
§ 394.455(10), Fla. Stat.
Each person, regardless of age, who enters treatment must be asked to give express
and informed consent for admission and for treatment. If the person is a minor,
express and informed consent for admission and treatment is required from the
guardian. § 394.459(3)(a), Fla. Stat. A minor 13 years of age or older is authorized
to consent to outpatient crisis intervention services under section 394.4784.
B. Hospitals
Section 394.4785(2), Florida Statutes, provides:
A person under the age of 14 who is admitted to any hospital
licensed pursuant to chapter 395, Florida Statutes, may not be
admitted to a bed in a room or ward with an adult in a mental health
unit or share common areas with an adult in a mental health unit.
However, a person 14 years of age or older may be admitted to a bed
in a room or ward in the mental health unit with an adult if the
admitting physician documents in the case record that such placement
is medically indicated or for reasons of safety. Such placement must
be reviewed by the attending physician or a designee or on-call

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
120
physician each day and documented in the case record. (emphasis
added)
In addition, all hospitals are required to ensure full compliance with the Baker Act
as a condition of licensure, as follows:
Section 395.003(5)(a), Florida Statutes, governing licensure of all hospitals
states: “Adherence to patient rights, standards of care, and examination and
placement procedures provided under part I of chapter 394 shall be a
condition of licensure for hospitals providing voluntary or involuntary
medical or psychiatric observation, evaluation, diagnosis, or treatment.”
Section 395.003(5)(b), Florida Statutes, states: “Any hospital that provides
psychiatric treatment to persons under 18 years of age who have emotional
disturbances shall comply with the procedures pertaining to the rights of
patients prescribed in part I of chapter 394.”
Section 395.1041(6) , Florida Statutes, states: “A hospital providing
emergency services and care to a person who is being involuntarily
examined under the provisions of s. 394.463 shall adhere to the rights of
patients specified in part I of chapter 394 and the involuntary examination
procedures provided in s. 394.463, regardless of whether the hospital, or any
part thereof, is designated as a receiving or treatment facility under part I of
chapter 394 and regardless of whether the person is admitted to the
hospital.”
Section 395.1055(5), Florida Statutes, governing rules and enforcement,
states: “The agency shall enforce the provisions of part I of chapter 394, and
rules adopted thereunder, with respect to the rights, standards of care, and
examination and placement procedures applicable to patients voluntarily or
involuntarily admitted to hospitals providing psychiatric observation,
evaluation, diagnosis, or treatment.”
C. Children’s Crisis Stabilization Units
Minors under the age of 14 cannot be admitted to a bed in a room or ward with an
adult. They may share common areas with an adult only when under direct visual
observation by unit staff. Minors who are 14 years of age and older “may be
admitted to a bed in a room or ward in the mental health unit with an adult, if the
clinical record contains documentation by a physician that such placement is
medically indicated or for reasons of safety.” This must be reviewed and

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
121
documented by the physician on a daily basis. Fla. Admin. Code R. 65E-
12.106(22).
IV. Consent to Psychiatric Treatment
A. Inpatient Treatment
Persons entering a facility must be asked to give express and informed consent for
admission and treatment. Express and informed consent for admission and
treatment of a person under 18 is required from the person’s guardian, unless the
minor is seeking outpatient crisis intervention services (see below).
§ 394.459(3)(a), Fla. Stat.
B. Residential Treatment Centers
All rights specified in section 394.459, Florida Statutes, must be safeguarded for
minors in residential treatment centers as well as receiving facilities. Children must
be informed of their legal and civil rights, including the right to legal counsel and
all other requirements of due process. Therefore, the Baker Act describes the rights
of children in residential treatment centers. Fla. Admin. Code R. 65E-9.012.
C. Outpatient Crisis Intervention Services
The disability of non-age is removed for any minor age 13 years or older to access
services under the following circumstances, pursuant to section 394.4784, Florida
Statutes (emphasis added):
(1) Outpatient diagnostic and evaluation services.--When any minor
age 13 years or older experiences an emotional crisis to such degree that he
or she perceives the need for professional assistance, he or she shall have the
right to request, consent to, and receive mental health diagnostic and
evaluative services provided by a licensed mental health professional, as
defined by Florida Statutes, or in a mental health facility licensed by the
state. The purpose of such services shall be to determine the severity of the
problem and the potential for harm to the person or others if further
professional services are not provided. Outpatient diagnostic and evaluative
services shall not include medication and other somatic methods, aversive
stimuli, or substantial deprivation. Such services shall not exceed two visits
during any 1-week period in response to a crisis situation before parental
consent is required for further services, and may include parental
participation when determined to be appropriate by the mental health
professional or facility.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
122
(2) Outpatient crisis intervention, therapy and counseling services.--
When any minor age 13 years or older experiences an emotional crisis to
such degree that he or she perceives the need for professional assistance, he
or she shall have the right to request, consent to, and receive outpatient crisis
intervention services including individual psychotherapy, group therapy,
counseling, or other forms of verbal therapy provided by a licensed mental
health professional, as defined by Florida Statutes, or in a mental health
facility licensed by the state. Such services shall not include medication and
other somatic treatments, aversive stimuli, or substantial deprivation. Such
services shall not exceed two visits during any 1-week period in response to
a crisis situation before parental consent is required for further services, and
may include parental participation when determined to be appropriate by the
mental health professional or facility.
(3) Liability for payment.--The parent, parents, or legal guardian of a
minor shall not be liable for payment for any such outpatient diagnostic and
evaluation services or outpatient therapy and counseling services, as
provided in this section, unless such parent, parents, or legal guardian
participates in the outpatient diagnostic and evaluation services or outpatient
therapy and counseling services and then only for the services rendered with
such participation.
(4) Provision of services.--No licensed mental health professional shall
be obligated to provide services to minors accorded the right to receive
services under this section. Provision of such services shall be on a voluntary
basis.
V. Substance Abuse (Marchman Act) Admission and Treatment
A. In General
“The disability of minority for persons under 18 years of age is removed solely for
the purpose of obtaining voluntary substance abuse impairment services from a
licensed service provider, and consent to such services by a minor has the same
force and effect as if executed by an individual who has reached the age of
majority. Such consent is not subject to later disaffirmance based on minority.”
§ 397.601(4)(a), Fla. Stat. (emphasis added).
B. Criteria
A minor may be taken to a detox facility, hospital, or addictions receiving facility
(ARF) for involuntary admission if there is a good-faith reason to believe the

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
123
minor is substance abuse impaired (“a condition involving the use of alcoholic
beverages or any psychoactive or mood-altering substance in such a manner as to
induce mental, emotional, or physical problems and cause socially dysfunctional
behavior”), section 397.311(18), Florida Statutes, and who, because of such
condition
(1) Has lost the power of self-control with respect to substance
abuse; and:
(2)(a) Is in need of substance abuse services and, by reason of
substance abuse impairment, his or her judgment has been so impaired
that he or she is incapable of appreciating his or her need for such
services and of making a rational decision in that regard, although
mere refusal to receive such services does not constitute evidence of
lack of judgment with respect to his or her need for such services; or
(b) Without care or treatment, is likely to suffer from neglect or
refuse to care for himself or herself; that such neglect or refusal poses
a real and present threat of substantial harm to his or her well-being;
and that it is not apparent that such harm may be avoided through the
help of willing family members or friends or the provision of other
services, or there is substantial likelihood that the person has inflicted,
or threatened to or attempted to inflict, or, unless admitted, is likely to
inflict, physical harm on himself, herself, or another.
§ 397.675, Fla. Stat.
C. Initiation
Protective custody may be initiated through law enforcement. § 397.677, Fla. Stat.
A parent or guardian may apply for a certificate for a minor’s emergency
admission if a professional’s certificate has been obtained, see section 397.679, as
well as for admission to a juvenile addiction receiving facility, section 397.6798. A
parent/guardian or a licensed service provider can also petition the court for an
involuntary assessment and stabilization order. § 397.6811, Fla. Stat.
D. Disposition
Release of the minor from protective custody, emergency admission, involuntary
assessment, involuntary treatment, or alternative involuntary assessment, upon
approval of a qualified professional in a hospital, detoxification facility, addictions
receiving facility, or any less restrictive treatment component, must be to the

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
124
minor’s parent, legal guardian, or legal custodian, or the authorized designee
thereof, or to DCF or DJJ. § 397.6758, Fla. Stat.
E. Parental Participation in Treatment
“A parent, legal guardian, or legal custodian who seeks involuntary admission of a
minor . . . is required to participate in all aspects of treatment as determined
appropriate by the director of the licensed service provider.” § 397.6759, Fla. Stat.
F. Release of Information
Since a minor acting alone has the legal capacity to voluntarily apply
for and obtain substance abuse treatment, any written consent for
disclosure may be given only by the minor. This restriction includes,
but is not limited to, any disclosure of identifying information to the
parent, legal guardian, or custodian of a minor for the purpose of
obtaining financial reimbursement. . . . When the consent of a parent,
legal guardian, or custodian is required under this chapter in order for
a minor to obtain substance abuse treatment, any written consent for
disclosure must be given by both the minor and the parent, legal
guardian, or custodian.
§ 397.501(7)(e), Fla. Stat.
G. Parental Participation/Payment
A parent or legal guardian of a minor is required to contribute toward the cost of
substance abuse services in accordance with his/her ability to pay, unless otherwise
provided by law. § 397.431(2), Fla. Stat. “The parent, legal guardian, or legal
custodian of a minor is not liable for payment for any [voluntary] substance abuse
services provided to the minor without parental consent . . . , unless the parent,
legal guardian, or legal custodian participates or is ordered to participate in the
services, and only for the substance abuse services rendered. If the minor is
receiving services as a juvenile offender, the obligation to pay is governed by the
law relating to juvenile offenders.” § 397.431(3), Fla. Stat.
VI. Consent for General Medical Care and Treatment
A. Power to Consent
Persons who have the power to consent for a minor’s medical care and treatment
include a natural or adoptive parent, legal custodian, or legal guardian.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
125
§ 743.0645(1)(c), Fla. Stat. The treatment provider must maintain records that
show documentation that a reasonable attempt was made to contact the person who
has the power to consent to the minor’s treatment. § 743.0645(2), Fla. Stat.
Any of the following persons, in order of priority listed, may consent to the
medical care or treatment of a minor who is not committed to DCF or DJJ “when,
after a reasonable attempt, a person who has the power to consent as otherwise
provided by law cannot be contacted by the treatment provider and actual notice to
the contrary has not been given to the provider by that person”:
(a) A health care surrogate designated under s. 765.2035 after
September 30, 2015, or a person who possesses a power of attorney to
provide medical consent for the minor. . . .
(b) The stepparent.
(c) The grandparent of the minor.
(d) An adult brother or sister of the minor.
(e) An adult aunt or uncle of the minor.
§ 743.0645(2), Fla. Stat.
“‘Medical care or treatment’ includes ordinary and necessary medical and dental
examinations and treatment, . . . but does not include surgery, general anesthesia,
provision of psychotropic medications, or other extraordinary procedures for
which a separate court order, health care surrogate designation under s. 765.2035
executed after September 30, 2015, power of attorney executed after July 1, 2001,
or informed consent as provided by law is required.” § 743.0645(1)(b), Fla. Stat.
(emphasis added).
B. Emergency Care
Section 743.064, Florida Statutes, provides as follows:
(1) The absence of parental consent notwithstanding, a physician
licensed under chapter 458 or an osteopathic physician licensed under
chapter 459 may render emergency medical care or treatment to any
minor who has been injured in an accident or who is suffering from an
acute illness, disease, or condition if, within a reasonable degree of
medical certainty, delay in initiation or provision of emergency
medical care or treatment would endanger the health or physical

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
126
wellbeing of the minor, and provided such emergency medical care or
treatment is administered in a hospital licensed by the state under
chapter 395 or in a college health service. Emergency medical care or
treatment may also be rendered in the prehospital setting by
paramedics, emergency medical technicians, and other emergency
medical services personnel, provided such care is rendered consistent
with the provisions of chapter 401. These persons shall follow the
general guidelines and notification provisions of this section.
(2) This section shall apply only when parental consent cannot be
immediately obtained for one of the following reasons:
(a) The minor’s condition has rendered him or her unable to reveal
the identity of his or her parents, guardian, or legal custodian, and
such information is unknown to any person who accompanied the
minor to the hospital.
(b) The parents, guardian, or legal custodian cannot be immediately
located by telephone at their place of residence or business.
(3) Notification shall be accomplished as soon as possible after the
emergency medical care or treatment is administered. The hospital
records shall reflect the reason such consent was not initially obtained
and shall contain a statement by the attending physician that
immediate emergency medical care or treatment was necessary for the
patient’s health or physical well-being. The hospital records shall be
open for inspection by the person legally responsible for the minor.
VII. Emergency Care of Youth in DCF or DJJ Custody
Section 743.0645(3), Florida Statutes, provides:
(3) The Department of Children and Families or the Department of
Juvenile Justice caseworker, juvenile probation officer, or person
primarily responsible for the case management of the child, the
administrator of any facility licensed by the department under s.
393.067, s. 394.875, or s. 409.175, or the administrator of any state-
operated or state-contracted delinquency residential treatment facility
may consent to the medical care or treatment of any minor committed
to it or in its custody under chapter 39, chapter 984, or chapter 985,
when the person who has the power to consent as otherwise provided
by law cannot be contacted and such person has not expressly

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
127
objected to such consent. There shall be maintained in the records of
the minor documentation that a reasonable attempt was made to
contact the person who has the power to consent as otherwise
provided by law.
(4) The medical provider shall notify the parent or other person
who has the power to consent as otherwise provided by law as soon as
possible after the medical care or treatment is administered pursuant
to consent given under this section. The medical records shall reflect
the reason consent as otherwise provided by law was not initially
obtained and shall be open for inspection by the parent or other person
who has the power to consent as otherwise provided by law.
(5) The person who gives consent; a physician, dentist, nurse, or
other health care professional licensed to practice in this state; or a
hospital or medical facility, including, but not limited to, county
health departments, shall not incur civil liability by reason of the
giving of consent, examination, or rendering of treatment, provided
that such consent, examination, or treatment was given or rendered as
a reasonable prudent person or similar health care professional would
give or render it under the same or similar circumstances.
VIII. Delinquent Youth
See ch. 985, Fla. Stat.
Section 985.18, Florida Statutes, titled “Medical, psychiatric, psychological,
substance abuse, and educational examination and treatment,” provides as follows:
(1) After a detention petition or a petition for delinquency has been
filed, the court may order the child named in the petition to be
examined by a physician. The court may also order the child to be
evaluated by a psychiatrist or a psychologist. If it is necessary to place
a child in a residential facility for such evaluation, the criteria and
procedures established in chapter 393, chapter 394, or chapter 397,
whichever is applicable, shall be used.
(2) If a child has been found to have committed a delinquent act, or
before such finding with the consent of any parent or legal custodian
of the child, the court may order the child to be treated by a physician.
The court may also order the child to receive mental health, substance
abuse, or intellectual disability services from a psychiatrist,

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
128
psychologist, or other appropriate service provider. If it is necessary to
place the child in a residential facility for such services, the
procedures and criteria established in chapter 393, chapter 394, or
chapter 397, as applicable, must be used. . . .
(6) A physician must be immediately notified by the person taking
the child into custody or the person having custody if there are
indications of physical injury or illness, or the child shall be taken to
the nearest available hospital for emergency care. A child may be
provided mental health, substance abuse, or intellectual disability
services in emergency situations pursuant to chapter 393, chapter 394,
or chapter 397, as applicable. After a hearing, the court may order the
custodial parent or parents, guardian, or other custodian, if found able
to do so, to reimburse the county or state for the expense involved in
such emergency treatment or care.
(7) Nothing . . . eliminates the right of the parents or the child to
consent to examination or treatment for the child, except that consent
of a parent shall not be required if the physician determines there is an
injury or illness requiring immediate treatment and the child consents
to such treatment or an ex parte court order is obtained authorizing
treatment.
IX. Dependent Youth
A. Medical, Psychiatric, and Psychological Examination and Treatment of
Children in DCF Custody
See ch. 39, Fla. Stat.; Fla. Admin. Code Ch. 65C-35. Rule 65C-35.007, Florida
Administrative Code, provides as follows (emphasis added):
(1) Parents or legal guardians retain the right to consent to or
decline the administration of psychotropic medications for children
taken into state care until such time as their parental rights, or court
ordered guardianship or custodial rights, have been terminated.
(2) If the parents’ or guardians’ legal rights have been terminated;
their identity or location is unknown; or they decline to approve
administration of psychotropic medications, and any party believes
that administration of the medication is in the best interest of the child
and medically necessary, then authorization to treat with psychotropic
medication must be pursued through a court order [via Children’s

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
129
Legal Services].
(3) In no case may the dependency case manager, child
protective investigator, the child’s caregiver, representatives from
[DJJ], or staff from Residential Treatment Centers provide
express and informed consent for a child in out-of-home care to
be prescribed a psychotropic medication.
Section 39.407, Florida Statutes, provides in part:
(1) When any child is removed from the home and maintained in
an out-of-home placement, the department is authorized to have a
medical screening performed on the child without authorization from
the court and without consent from a parent or legal custodian. Such
medical screening shall be performed by a licensed health care
professional and shall be to examine the child for injury, illness, and
communicable diseases and to determine the need for immunization.
The department shall by rule establish the invasiveness of the medical
procedures authorized to be performed under this subsection. In no
case does this subsection authorize the department to consent to
medical treatment for such children.
(2) When [DCF] has performed the medical screening , . . . or when it is
otherwise determined by a licensed health care professional that a child who
is in an out-of-home placement, but who has not been committed to the
department, is in need of medical treatment, including the need for
immunization, consent for medical treatment shall be obtained in the
following manner:
(a) [From a parent or legal custodian of the child, or by court order.]
(b) If a parent or legal custodian of the child is unavailable and his or her
whereabouts cannot be reasonably ascertained, and it is after normal
working hours so that a court order cannot reasonably be obtained, an
authorized agent of the department shall have the authority to consent to
necessary medical treatment, including immunization, for the child. The
authority of the department to consent to medical treatment in this
circumstance shall be limited to the time reasonably necessary to obtain
court authorization.
(c) If a parent or legal custodian of the child is available but refuses to
consent to the necessary treatment, a court order shall be required unless the

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
130
situation meets the definition of an emergency in s. 743.064 or the treatment
needed is related to suspected abuse, abandonment, or neglect of the child by
a parent, caregiver, or legal custodian. In such case, [DCF] can consent to
necessary medical treatment. This authority is limited to the time reasonably
necessary to obtain court authorization.
B. Psychotropic Medications for Children in DCF Custody
See Fla. Admin. Code Ch. 65C-35.
Section 39.407, Florida Statutes, provides:
(3)(a)1. . . . . [B]efore the department provides psychotropic
medications to a child in its custody, the prescribing physician shall
attempt to obtain express and informed consent . . . from the child’s
parent or legal guardian. The department must take steps necessary to
facilitate the inclusion of the parent in the child’s consultation with
the physician. However, if the parental rights of the parent have been
terminated, the parent’s location or identity is unknown or cannot
reasonably be ascertained, or the parent declines to give express and
informed consent, the department may, after consultation with the
prescribing physician, seek court authorization to provide the
psychotropic medications to the child. Unless parental rights have
been terminated and if it is possible to do so, the department shall
continue to involve the parent in the decisionmaking process
regarding the provision of psychotropic medications. If, at any time, a
parent whose parental rights have not been terminated provides
express and informed consent to the provision of a psychotropic
medication, the requirements of this section that the department seek
court authorization do not apply to that medication until such time as
the parent no longer consents.
2. Any time the department seeks a medical evaluation to
determine the need to initiate or continue a psychotropic medication
for a child, the department must provide to the evaluating physician
all pertinent medical information known to the department concerning
that child.
(b)1. If a child who is removed from the home under s. 39.401 is
receiving prescribed psychotropic medication at the time of removal
and parental authorization to continue providing the medication

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
131
cannot be obtained, the department may take possession of the
remaining medication and may continue to provide the medication as
prescribed until the shelter hearing, if it is determined that the
medication is a current prescription for that child and the medication
is in its original container.
2. If the department continues to provide the psychotropic
medication to a child when parental authorization cannot be obtained,
the department shall notify the parent or legal guardian as soon as
possible that the medication is being provided to the child. . . . The
child’s official departmental record must include the reason parental
authorization was not initially obtained and an explanation of why the
medication is necessary for the child’s well-being.
3. If the department is advised by a [licensed] physician . . . that
the child should continue the psychotropic medication and parental
authorization has not been obtained, the department shall request court
authorization at the shelter hearing to continue to provide the
psychotropic medication and must provide to the court any
information in its possession in support of the request. Any
authorization granted at the shelter hearing may extend only until the
arraignment hearing on the petition for adjudication of dependency or
28 days following the date of removal, whichever occurs sooner.
4. Before filing the dependency petition, the department shall
ensure that the child is evaluated by a [licensed] physician to
determine whether it is appropriate to continue the psychotropic
medication. If, as a result of the evaluation, the department seeks court
authorization to continue the psychotropic medication, a motion for
such continued authorization shall be filed at the same time as the
dependency petition, within 21 days after the shelter hearing.
(c) . . . . [T]he department must file a motion seeking the court’s
authorization to initially provide or continue to provide psychotropic
medication to a child in its legal custody. The motion must be
supported by a written report prepared by the department which
describes the efforts made to enable the prescribing physician to
obtain express and informed consent for providing the medication to
the child and other treatments considered or recommended for the
child. In addition, the motion must be supported by the prescribing
physician’s signed medical report providing:

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
132
1. The name of the child, the name and range of the dosage of the
psychotropic medication, and that there is a need to prescribe
psychotropic medication to the child based upon a diagnosed
condition for which such medication is being prescribed.
2. A statement indicating that the physician has reviewed all
medical information concerning the child which has been provided.
3. A statement indicating that the psychotropic medication, at its
prescribed dosage, is appropriate for treating the child’s diagnosed
medical condition, as well as the behaviors and symptoms the
medication, at its prescribed dosage, is expected to address.
4. An explanation of the nature and purpose of the treatment; the
recognized side effects, risks, and contraindications of the medication;
drug-interaction precautions; the possible effects of stopping the
medication; and how the treatment will be monitored, followed by a
statement indicating that this explanation was provided to the child if
age appropriate and to the child’s caregiver.
5. Documentation addressing whether the psychotropic
medication will replace or supplement any other currently prescribed
medications or treatments; the length of time the child is expected to
be taking the medication; and any additional medical, mental health,
behavioral, counseling, or other services that the prescribing physician
recommends.
Chapter 65C-35, Florida Administrative Code, adopted in 2010, governs
“Psychotropic Medication for Children in Out of Home Care.” Several of the many
definitions in rule 65C-35.001, Florida Administrative Code, are as follows:
(1) “Assent” . . . means a process by which a provider of medical
services helps the patient achieve a developmentally appropriate
awareness of the nature of his or her condition; informs the patient of
what can be expected with tests and treatment; makes a clinical
assessment of the patient’s understanding of the situation and the
factors influencing how he or she is responding; and solicits an
expression of the patient’s willingness to accept the proposed care.
(10) “Express and Informed Consent” means . . . voluntary written
consent from a competent person who has received full, accurate, and
sufficient information and explanation about a child’s medical

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
133
condition, medication and treatment to enable the person to make a
knowledgeable decision without being subjected to any deceit or
coercion. Express and informed consent for the administration of
psychotropic medications may only be given by a parent whose rights
have not been terminated, or a legal guardian of the child. Sufficient
explanation includes but is not limited to the following information,
provided and explained in plain language by the prescribing physician
to the consent giver: the medication, reason for prescribing it, and its
purpose or intended result; side effects, risks, and contraindications,
including effects of stopping the medication; method for
administering the medication, and dosage range when applicable;
potential drug interactions; alternative treatments; and the behavioral
health or other services used to complement the use of medication,
when applicable.
(14) “Legal Guardian” means a permanent guardian as described in
Section 39.6221, F.S., or a “guardian” as defined in Section 744.102,
F.S., or a relative with a court order of temporary custody under
Chapter 751, F.S. Dependency case managers and Guardians ad Litem
do not meet the definition of legal guardian.
(15) “Medical Report” means a report prepared by the prescribing
physician that includes information required by Section 39.407(3)(c),
F.S. The form for the medical report is “Medical Report” (form CF-
FSP 5339 dated January 2010) which is hereby incorporated by
reference and is available by contacting the Family Safety Program
Office at 1317 Winewood Boulevard, Tallahassee, Florida 32399-
0700, or at
http://www.dcf.state.fl.us/dcfforms/Search/DCFFormSearch.aspx.
(18) “Psychotropic Medications” means, for the purpose of this rule,
any chemical substance prescribed with the intent to treat psychiatric
disorders; and those substances, which though prescribed with the
intent to treat other medical conditions, have the effect of altering
brain chemistry or involve any of the medications in the categories
listed below. The medications include, without limitation, the
following major categories:
(a) Antipsychotics;
(b) Antidepressants;

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
134
(c) Sedative Hypnotics;
(d) Lithium;
(e) Stimulants;
(f) Non-stimulant Attention Deficit Hyperactivity Disorder
medications;
(g) Anti-dementia medications and cognition enhancers;
(h) Anticonvulsants and alpha-2 agonists; and
(i) Any other medication used to stabilize or improve mood,
mental status, behavior, or mental illness.
Psychotropic medications may be administered in advance of a court order or
parental authorization under two circumstances, including:
if the prescribing physician certifies in writing on the medical report form
that “delay in providing a prescribed psychotropic medication would more
likely than not cause significant harm to the child,” or
in hospitals, crisis stabilization units, and psychiatric residential treatment
programs.
§ 39.407(3)(e), Fla. Stat. In the above two circumstances, the dependency case
manager or child protective investigator must assist the prescribing physician in
obtaining express and informed consent and must take steps to include the parent
or legal guardian in the child’s consultation with the prescribing physician. If
express and informed consent hasn’t been obtained, the dependency case manager
or child protective investigator must obtain a completed/signed copy of the medical
report and provide it to Children’s Legal Services in time for a motion to be filed
within three business days after the medication is begun.
C. Examination, Treatment, and Placement of Children in DCF Custody
Section 39.407, Florida Statutes, provides in part as follows (emphasis added):
(4) A judge may order a child in an out-of-home placement to be
examined by a licensed health care professional. . . . The judge may
also order such child to be evaluated by a psychiatrist or a
psychologist or, if a developmental disability is suspected or alleged,

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
135
by the developmental disability diagnostic and evaluation team of the
department. If it is necessary to place a child in a residential facility
for such evaluation, the criteria and procedure established in
s. 394.463(2) or chapter 393 shall be used, whichever is applicable.
(5) A judge may order a child in an out-of-home placement to be
treated by a licensed health care professional based on evidence that
the child should receive treatment. The judge may also order such
child to receive mental health or developmental disabilities services
from a psychiatrist, psychologist, or other appropriate service
provider. If it is necessary to place the child in a residential facility for
such services, the procedures and criteria established in s. 394.467
shall be used. A child may be provided mental health services in
emergency situations, pursuant to the procedures and criteria
contained in s. 394.463(1).
(6) Children who are in the legal custody of the department may be
placed by the department, without prior approval of the court, in a
residential treatment center licensed under s. 394.875 or a hospital
licensed under chapter 395 for residential mental health treatment or
may be placed by the court in accordance with an order of involuntary
examination or involuntary placement entered pursuant to s. 394.463
or s. 394.467. All children placed in a residential treatment program
under this subsection must have a guardian ad litem appointed.
X. Frequently Asked Questions
A. Minority Defined
How is a minor defined?
“‘Minor’ means an individual who is 17 years of age or younger and who has not
had the disability of nonage removed pursuant to s. 743.01 or s. 743.015.”
§ 394.455(29), Fla. Stat.
While the text of the Baker Act occasionally uses the term “minor” or “adult,” in
which case these definitions apply, it also uses the phrases “age 17 and under,”
“under 18 years of age,” or “18 years of age or older” in many other citations. In
such instances, the more precise age limitation would apply rather than the more
generic term of “minor” or “adult.”

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
136
Is there any difference in legal status for minors of different ages, such as
above or below age 14?
There is no difference between the ages of a minor regarding inpatient care. Ages
0-17 are handled identically. The only differences referred to in the law are the
status of co-location with adult patients and outpatient crisis intervention.
Who is a child’s guardian?
A child’s guardian is generally one or both of his or her natural or adoptive
parents. After a dissolution of marriage, decisions related to the child’s health care
will be made by the parent or parents as set forth in the approved parenting plan.
The mother of a child born out of wedlock is guardian of the child. In the absence
of a parent, a guardian must be appointed by a court and can be a relative or other
person interested in the welfare of the child.
B. Informed Consent and Consent to Treatment
We have a psychiatrist who is board-certified for treatment of adult, child,
and adolescent patients. He has been treating a 17-year-old who is resistant to
medications. The doctor wants to perform outpatient ECT, and the parents
are willing to consent for the treatment. If the patient is willing to go through
the procedure and the parents give consent, and the psychiatrist has all the
“typical” paperwork needed for ECT, can he perform the procedure?
This issue is addressed in the Baker Act and the Medical Practice Act. These
Florida Statutes provisions are as follows:
394.459. Rights of patients (emphasis added)
(3) Right to express and informed patient consent.—
* * *
(b) In the case of medical procedures requiring the use of a general
anesthetic or electroconvulsive treatment, and prior to performing the
procedure, express and informed consent shall be obtained from the
patient if the patient is legally competent, from the guardian of a
minor patient, from the guardian of a patient who has been
adjudicated incapacitated, or from the guardian advocate of the patient
if the guardian advocate has been given express court authority to
consent to medical procedures or electroconvulsive treatment as

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
137
provided under s. 394.4598.
Since the minor is not competent to provide consent as a result of age, the guardian
has the power to make this decision. It still must be made with full disclosure of
the risks, benefits, and all other factors required for consent to be “informed.”
458.325. Electroconvulsive and psychosurgical procedures
(emphasis added)
(1) In each case of utilization of electroconvulsive or
psychosurgical procedures, prior written consent shall be obtained
after disclosure to the patient, if he or she is competent, or to the
patient’s guardian, if he or she is a minor or incompetent, of the
purpose of the procedure, the common side effects thereof, alternative
treatment modalities, and the approximate number of such procedures
considered necessary and that any consent given may be revoked by
the patient or the patient’s guardian prior to or between treatments.
(2) Before convulsive therapy or psychosurgery may be
administered, the patient’s treatment record shall be reviewed and the
proposed convulsive therapy or psychosurgery agreed to by one other
physician not directly involved with the patient. Such agreement shall
be documented in the patient’s treatment record and shall be signed by
both physicians.
Assuming that administering ECT to minors is an accepted psychiatric practice,
there appears to be no legal barrier to a minor receiving ECT.
Does the court have authority to appoint a guardian advocate for a child when
the child’s guardian is refusing to consent for treatment?
A child’s natural guardian has the power to consent or refuse consent to treatment
on behalf of the minor, just as does a guardian (plenary or “of person”) appointed
by the court for an adult. In the case of an adult, a request can be filed for the court
to investigate any complaints against a court-appointed guardian’s decision-
making. In the case of a minor whose parent’s refusal to consent to medically
necessary treatments might rise to the level of “medical neglect,” a report to the
DCF Abuse Registry should be made. There have been occasions when the natural
parents/guardians of a minor have been unavailable and the child’s caretaker isn’t
authorized to consent to psychotherapeutic medications (chapter 743, Florida
Statutes) in which a guardian advocate was appointed to make such treatment
decisions. This is not the case where the parents refuse consent.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
138
C. Voluntary Admissions
Under what conditions can a minor be on voluntary status?
The Baker Act permits minors to be on voluntary status if they are agreeable to the
admission, but only when their parent or legal guardian has applied for their
admission and a judicial hearing has been conducted prior to the admission, to
confirm the voluntariness of the consent. Unless parental rights have been
terminated, natural or adoptive parents continue to have the right to make such
decisions on behalf of their children, even if they cannot or will not do so. In the
absence of a parent or legal guardian’s consent, the court must make this decision.
Any reference to “voluntariness hearings” done at facilities and by facility staff
was repealed from the Florida Administrative Code in 1997 because DCF was
found not to have the specific statutory authority to define a hearing as an
“administrative hearing” when all other references to hearings in the Baker Act are
judicial in nature. Therefore, it is DCF’s opinion that a judicial hearing of some
type is required prior to the admission of the minor on voluntary status. There are
no rules or model forms for this purpose.
A child has a right to be held on a voluntary basis if he/she meets the criteria and
the correct procedures are followed — especially if the child doesn’t meet the
criteria for involuntary status. However, due to the onerous nature of voluntary
admission of minors, especially those in DCF custody, many providers have
chosen to admit all such minors on involuntary status. Assuming the minor meets
the criteria for involuntary examination, it would be entirely proper to admit
him/her on involuntary status. While minors may state a willingness to be in a
psychiatric unit, they do not have the legal capacity to give independent consent to
the admission or to treatment.
Section 394.4625(1)(a), Florida Statutes, states that “[a] person age 17 or
under may be admitted only after a hearing to verify voluntariness of the
consent.” Please tell me what a hearing is comprised of and who must be
present, and what paper must confirm that this is valid and complete. If we
have a minor child and a parent or guardian in agreement with admission,
can we have the Application for Voluntary Admission – Minors (CF-MH
3097) signed? Do we need the psychiatrist to determine the patient’s
competence, or is it sufficient for a LMHC or LCSW to make this
determination? It seems that initiating a BA-52 by a professional does not
make sense when the person is willing.

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
139
The model form 3097, “Application for Voluntary Admission – Minors,” is an
approved document in the series of Baker Act forms. It allows for the
documentation of the parent/guardian’s consent and the minor’s assent. It is silent
as to the requirement for a hearing. However, the statutory language remains in
effect. DCF has proposed changes to this section of the Baker Act to allow for
certain licensed professionals, such as a clinical social worker or mental health
counselor, to conduct an evaluation of voluntariness. However, this bill would
have to be passed by the Legislature to take effect.
We admitted a 15-year-old girl to our CSU whose parents’ parental rights
were terminated, and she had been in the foster care system for many years.
The 72-hour period of the initial Baker Act expired yesterday, and the nurse
on duty obtained a consent for voluntary admission by telephone from the
child’s DCF or community-based care worker. The child signed the portion of
the voluntary admission form that asks if the child is willing to stay. The
question arose as to whether the DCF or community-based care worker has
the authority to sign the child in voluntarily, or whether a petition for
involuntary placement should have been initiated prior to the expiration of
the initial Baker Act. In the past we have petitioned the court for the
continuation of treatment, filing with the court a petition for involuntary
placement. We do know that this does not apply to treatment (medication)
and are fully aware of the need for a court order to administer medication.
The law requires that the application for voluntary admission be filed by the
minor’s guardian. If the court had formally appointed DCF or the community-
based care agency as the child’s legal guardian, consent by the authorized person
from that agency would be permissible. However, this isn’t the usual practice.
Absent a formal guardian appointed by the court, the court itself would act as the
child’s guardian and would be responsible for signing the voluntary application.
The only other alternative would have been to file a petition for involuntary
placement.
D. Involuntary Examinations
In order to initiate involuntary examination for a child or adolescent, do you
need the parent’s permission? This question came up after an agency director
reported having heard that parents must approve before a child or adolescent
can be Baker Acted.
No. There is no basis for a parent or guardian of a child to provide consent or
refuse consent to his/her child’s involuntary examination. This decision is entirely

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
140
up to a judge, law enforcement officer, or authorized mental health professional
who has reason to believe the involuntary examination criteria are met. In section
394.463, Florida Statutes, governing involuntary examination, no difference
between adults and minors is noted, and parental consent is not mentioned.
When a minor is brought to a receiving facility pursuant to an ex parte order
for involuntary examination, does consent for the admission and treatment by
the guardian specified under section 394.459(3)(a)1., Florida Statutes, still
apply? If so, is this for both admission and treatment or just treatment?
The minor must be accepted by the facility and must be examined (section
394.463) by a physician, psychologist, or psychiatric nurse, as each is defined in
the Baker Act, to determine if he/she meets criteria for involuntary placement
(section 394.467), regardless of whether consent is obtained from the guardian.
However, treatment is a different issue, since the court order is generally silent as
to this issue. The minor can’t be treated unless, after full disclosure, the child’s
legal guardian (parent or court-appointed guardian) provides consent. If a legal
guardian is not available or refuses such consent, a court order for treatment would
be required, short of an emergency treatment order resulting from documentation
of imminent danger.
A parent of a student who was recently Baker Acted from school by the school
resource officer stated that since there is Native American ancestry in the
child’s background, a federal order is required before he can be Baker Acted.
Since the need to hospitalize him again in the future may occur, we are hoping
that you can steer us in the right direction on this.
Contrary to the parent’s statement, there isn’t any exception in the Baker Act for
persons with Native American ancestry. People of all nationalities undergo
involuntary examination under the Baker Act. The Vienna Convention on Consular
Relations and bilateral treaties the United States has negotiated with other
countries require consulate notification and access to foreign nationals held against
their will in hospitals. Only a state circuit court (in addition to certified law
enforcement officers and authorized mental health professionals) has authority to
initiate an ex parte order under the Baker Act — federal courts have no such
authority. In fact, federal law enforcement officers can’t initiate involuntary
examinations, per the Florida Attorney General (Op. Att’y Gen. Fla. 99-68 (1999))
— only law enforcement officers who are certified under state law may do so.
Native American reservations are subject to federal law, just like military bases
and VA hospital properties. However, the Baker Act is applicable to persons of all
ages who are in Florida as residents, citizens, visitors, or otherwise, on legal or

Admission and Treatment for Minors
Chapter Three (Baker Act, Marchman Act/Substance Abuse, and Medical-Related Statutes)
_____________________________________________________________________________________
Baker Act Benchguide November 2016
141
illegal bases.
Our risk managers (attorneys) indicated there is a gap in the Baker Act law.
They instructed us that a child can be involuntarily examined, but cannot be
involuntarily placed. Usually families sign their children in voluntarily. If it is
true that you cannot treat a child on an involuntary status, what are our
options?
The information you’ve been given is incorrect. Minors are frequently
involuntarily placed by courts throughout the state, as the criteria for involuntary
examination and involuntary inpatient placement refer to “a person” regardless of
age. Minors cannot be ordered to involuntary outpatient services — this may have
caused some confusion. You should also consider the issues of admission/
placement separately from the issue of treatment.
No minor can provide consent for his/her own admission or treatment.
However, if the child refused to assent (agree) to the admission, it is
necessary to initiate the involuntary process — involuntary examination if
necessary to conduct the examination and involuntary inpatient placement if
the examination reflects that the minor meets the criteria under section
394.467, Florida Statutes.
With regard to voluntary admission of a minor, a parent or guardian must
actually sign the application, but a judicial hearing must be conducted prior
to the child’s admission.
With regard to a parent’s demand for release of the child, you may need to
consider a referral to the child abuse hotline if you believe the parent’s refusal of
care represents abuse or neglect, as defined in chapter 39, Florida Statutes.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
142
Chapter Four: Involuntary Examination
I. In General
See § 394.463, Fla. Stat.; Fla. Admin. Code R. 65E-5.280.
The Baker Act encourages the voluntary admission of persons for psychiatric care,
but only when they are able to understand the decision and its consequences and
are able to fully exercise their rights for themselves. When this is not possible due
to the severity of the person’s condition, the law requires that the person be
extended the due process rights ensured under the Baker Act’s involuntary
provisions. The definition of “mental illness” is not a part of this section of the
statute. However, because it is relevant to the content of this part of the statute, it is
included here:
“Mental illness” means an impairment of the mental or emotional
processes that exercise conscious control of one’s actions or of the
ability to perceive or understand reality, which impairment
substantially interferes with the person’s ability to meet the ordinary
demands of living. For the purposes of this part, the term does not
include a developmental disability as defined in chapter 393,
intoxication, or conditions manifested only by antisocial behavior or
substance abuse.
§ 394.455(28), Fla. Stat.
II. Criteria
Section 394.463(1), Florida Statutes (emphasis added), provides:
A person may be taken to a receiving facility for involuntary
examination if there is reason to believe that he or she has a mental
illness [as defined in the Baker Act] and because of his or her mental
illness:
(a)1. The person has refused voluntary examination after
conscientious explanation and disclosure of the purpose of the
examination; or
2. The person is unable to determine for himself or herself
whether examination is necessary; and

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
143
(b)1. Without care or treatment, the person is likely to suffer from
neglect or refuse to care for himself or herself; such neglect or refusal
poses a real and present threat of substantial harm to his or her
well‑being; and it is not apparent that such harm may be avoided
through the help of willing family members or friends or the provision
of other services; or
2. There is a substantial likelihood that without care or treatment
the person will cause serious bodily harm to self or others in the near
future, as evidenced by recent behavior.
III. Initiation
Under section 394.463(2)(a), Florida Statutes, an involuntary examination
may be initiated by the following three means:
A court may enter an ex parte order (form CF‑MH 3001 or other order
developed by the court) stating that the person appears to meet the criteria
for involuntary examination, specifying the findings on which that
conclusion is based. The order must be based on sworn testimony, written or
oral (form CF‑MH 3002 or other form developed by the court). No fee can
be charged for the filing of a petition for an order for involuntary
examination.
A law enforcement officer or other designated agent of the court must take
the person into custody and deliver the person to an appropriate, or the
nearest, facility within the designating receiving system under section
394.462, Florida Statutes, for an involuntary examination. “A law
enforcement officer acting in accordance with an ex parte order . . . may
serve and execute such order on any day of the week, at any time of the day
or night” and “may use such reasonable physical force as is necessary to
gain entry to the premises, and any dwellings, buildings, or other structures
located on the premises, and to take custody of the person who is the subject
of the ex parte order.” § 394.463(2)(c), (2)(d). The officer must execute a
written report titled “Transportation to Receiving Facility” (form CF‑MH
3100), detailing the circumstances under which the person was taken into
custody, and the report must be made a part of the person’s clinical record.
The ex parte order is valid only until executed or, if not executed, for the
period specified in the order. If no time limit is specified in the order, it is
valid for seven days after the date it was signed. Once a person is picked up

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
144
on the order and taken to a receiving facility for involuntary examination
and released, the same order cannot be used again during the time period.
The order must be made a part of the person’s clinical record.
A law enforcement officer shall take a person who appears to meet the
criteria for involuntary examination into custody and deliver the person, or
have the person delivered, to an appropriate or the nearest receiving facility
for examination. (CF‑MH 3052a). The officer must execute a written report
(CF‑MH 3100) detailing the circumstances under which the person was
taken into custody. The report must be made a part of the person’s clinical
record.
A physician, clinical psychologist, psychiatric nurse, mental health
counselor, marriage and family therapist, or clinical social worker (each
as defined in the Baker Act) may execute a certificate (CF‑MH 3052b)
stating that he or she has examined a person within the preceding 48 hours
and finds that the person appears to meet the criteria for involuntary
examination, The certificate must state the professional’s observations on
which that conclusion is based. A law enforcement officer must take the
person named in the certificate into custody and deliver the person to an
appropriate or the nearest receiving facility for involuntary examination, and
must execute a written report (CF‑MH 3100) detailing the circumstances
under which the person was taken into custody. The report and certificate are
to be made a part of the person’s clinical record.
See also Fla. Admin. Code R. 65E-5.280(1)–(3).
IV. Definitions of Mental Health Professionals
Under section 394.455, Florida Statutes, mental health professionals are defined as
follows:
(5) “Clinical Psychologist” means a psychologist as defined in
s. 490.003(7) with 3 years of postdoctoral experience in the practice
of clinical psychology, inclusive of the experience required for
licensure, or a psychologist employed by a facility operated by the
United States Department of Veterans Affairs that qualifies as a
receiving or treatment facility under this part.
* * *

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
145
(7) “Clinical social worker” means a person licensed as a clinical
social worker under s. 491.005 or s.491.006.
* * *
(25) “Marriage and family therapist” means a person licensed as a
marriage and family therapist under s. 491.005 or s.491.006.”
(26) “Mental health counselor” means a person licensed as a mental
health counselor under s. 491.005 or s.491.006.”
* * *
(32) “Physician” means a medical practitioner licensed under
chapter 458 or chapter 459 who has experience in the diagnosis and
treatment of mental illness or a physician employed by a facility
operated by the United States Department of Veterans Affairs or the
United States Department of Defense.
(33) “Physician assistant” means a person licensed under chapter
458 or chapter 459 who has experience in the diagnosis and treatment
of mental disorders.
* * *
(35) “Psychiatric nurse” means an advanced registered nurse
certified under s. 464.012 who has a master’s or doctoral degree in
psychiatric nursing, holds a national advanced practice certification as
a psychiatric mental health advanced practice nurse, and has 2 years
of post-master’s clinical experience under the supervision of a
physician.”
(36) “Psychiatrist” means a medical practitioner licensed under
chapter 458 or chapter 459 for at least 3 years, inclusive of psychiatric
residency.
* * *
(38) “Qualified professional” means a physician or a physician
assistant licensed under chapter 458 or chapter 459; a psychiatrist
licensed under chapter 458 or chapter 459; a psychologist as defined
in s. 490.003(7); or a psychiatric nurse as defined in s. 394.455.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
146
The Florida Attorney General issued an opinion in May 2008 that physician
assistants may, under certain conditions, initiate an involuntary examination. Op.
Att’y Gen. Fla. 08-31 (2008). The opinion did not extend any other authority
granted to physicians.
V. Initial Mandatory Involuntary Examination
A person must have an initial mandatory involuntary examination “by a physician
or a clinical psychologist, or by a psychiatric nurse performing within the
framework of an established protocol with a psychiatrist at a facility without
unnecessary delay to determine if the criteria for involuntary services are met.
Emergency treatment may be provided upon the order of a physician if the
physician determines that such treatment is necessary for the safety of the person
or others.” § 394.463(2)(f), Fla. Stat.
This initial mandatory involuntary examination must include:
a thorough review of any observations of the person’s recent behavior;
a review of the document initiating the involuntary examination and
transportation form;
a brief psychiatric history; and
a timely face-to-face examination to determine whether the person meets the
criteria for release.
Fla. Admin. Code R. 65E-5.2801(1).
A physical examination, which must be conducted within 24 hours of the person’s
arrival at the facility (section 394.459(2)(c)), is intended to rule out mock
psychiatric symptoms caused by non‑psychiatric medical illness, injury, metabolic
disorders, and drug toxicity.
The person cannot be released by the receiving facility without the documented
approval of a psychiatrist, a clinical psychologist, or the physician in the hospital’s
emergency department. The release can also be approved by a psychiatric nurse (as
defined in the Baker Act) performing under a protocol with a psychiatrist and as
otherwise provided in section 394.463(2)(f), Florida Statutes.
VI. Release
Section 394.463(2)(g), Florida Statutes, provides:

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
147
Within the 72-hour examination period or, if the 72 hours ends on a
weekend or holiday, no later than the next working day thereafter, one
of the following actions must be taken, based on the individual needs
of the person:
1. The patient shall be released, unless he or she is charged with a
crime, in which case the patient must be returned to the custody of a
law enforcement officer;
2. The patient shall be released . . . for voluntary outpatient
treatment;
3. The patient, unless he or she is charged with a crime, shall be
asked to give express and informed consent to placement as a
voluntary patient, and, if such consent is given, the patient shall be
admitted as a voluntarily patient [such transfer from involuntary to
voluntary status must be conditioned on the certification by a
physician that the person has the capacity to make well-reasoned,
willful, and knowing decisions about medical, mental health, or
substance abuse treatment]; or
4. A petition for involuntary placement shall be filed in the circuit
court if inpatient treatment is deemed necessary or with the criminal
county court, as defined in s. 394.4655(1), as applicable. If inpatient
treatment is deemed necessary, the least restrictive treatment
consistent with the optimum improvement of the patient’s condition
shall be made available. When a petition is to be filed for involuntary
outpatient placement, it shall be filed by one of the petitioners
specified in s. 394.4655(4)(a). A petition for involuntary inpatient
placement shall be filed by the facility administrator.
If the person is converted to voluntary status in lieu of involuntary placement being
sought, it may be necessary under some circumstances to file documents with the
clerk of court to prohibit firearm purchase. See Chapter Eight of this benchguide.
VII. Notice of Discharge or Release
Notice of discharge or transfer of a person must be given as provided in section
394.4599, Florida Statutes. § 394.469(2), Fla. Stat.
Notice of release (form CF-MH 3038) must be given to the person’s guardian or
representative, any person who executed a certificate admitting the person to the

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
148
receiving facility, and any court that ordered the person’s evaluation. § 394.463(3),
Fla. Stat.
VIII. Involuntary Examination Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.)

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
149

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
150
IX. Frequently Asked Questions
A. Criteria and Eligibility
I’m a detective with the sheriff’s office. I’m getting many calls regarding the
Baker Act and people with autism who are being violent. The callers want to
know if they can Baker Act if someone has autism. I explained you cannot
Baker Act based on the autism label alone, but you can Baker Act if the
person is a threat to himself/herself or someone else. The question then
becomes: if the violence is a behavioral aspect of the developmental disability,
can you still Baker Act? My position is that a mental health facility would be a
better choice than jail. I then suggest they explore all other alternatives that
may be available. Can you please give me some guidance?
Regarding your question about initiating involuntary examination under the Baker
Act, there must be a diagnosis of mental illness consistent with the definition in the
law, refusal or inability to determine examination is needed, and passive or active
danger. If any one of these isn’t present, an initiation wouldn’t be appropriate. Just
being a threat to self or others (active danger) wouldn’t be sufficient unless it
resulted from a mental illness. Autism is a diagnosis under chapter 393, Florida
Statutes, governing developmental disabilities that is excluded from the statutory
definition of mental illness:
394.455. Definitions (emphasis added)
(28) “Mental illness” means an impairment of the mental or
emotional processes that exercise conscious control of one’s actions
or of the ability to perceive or understand reality, which impairment
substantially interferes with a person’s ability to meet the ordinary
demands of living, regardless of etiology. For the purposes of this
part, the term does not include developmental disabilities as
defined in chapter 393, intoxication, or conditions manifested only
by antisocial behavior or substance abuse.
393.063. Definitions
For the purposes of this chapter, the term:
(3) “Autism” means a pervasive, neurologically based
developmental disability of extended duration which causes severe
learning, communication, and behavior disorders with age of onset
during infancy or childhood. Individuals with autism exhibit

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
151
impairment in reciprocal social interaction, impairment in verbal and
nonverbal communication and imaginative ability, and a markedly
restricted repertoire of activities and interests.
While a person cannot be Baker Acted for dangerous behavior resulting from
autism, a judge or law enforcement officer may have reason to believe the person
has a mental illness in addition to autism. In such a situation, the initiation of
involuntary examination may be appropriate. Judges and law enforcement officers
aren’t expected to be diagnosticians; they can be wrong just like a mental health
professional is sometimes wrong. They also need to be aware that the person is
only going to be examined and may be released immediately or within 72 hours
back to where they came from. If treated, the only treatment available is for
psychiatric conditions and not for a developmental disability. Initiating an
involuntary examination may alleviate an immediate danger situation but is
unlikely to have any lasting benefit. You are correct that criminalization of a
developmental disorder or a mental health diagnosis should be avoided whenever
possible.
One of my deputies was told by the local CSU that it doesn’t accept Alzheimer
patients and officers can’t Baker Act an Alzheimer’s patient. The deputy then
took the patient to the county hospital. The deputy told the social worker that
the man had beaten his wife earlier in the day and then stood out in the street
directing traffic. There was no medical issue with this man. Was the CSU
correct?
Section 394.462(1)(k), Florida Statutes, states: “The appropriate facility within the
designated receiving system pursuant to a transportation plan or an exception under
subsection (4), or the nearest receiving facility if neither apply, must accept
persons brought by law enforcement officers, or an emergency medical transport
service or a private transport company authorized by the county, for involuntary
examination pursuant to s. 394.463.” This means that if the person is on Baker Act
involuntary status and transport is by law enforcement or specified transport
services, there is no exception to the receiving facility being required to “accept”
the person from the officer. If the person is under the involuntary provisions of the
Marchman Act, the facility must provide such persons “a basic screening or triage
sufficient to refer the person to the appropriate services.” § 394.462(l). If the
facility can’t manage the person’s medical condition, the person has public or
private insurance that will pay at another facility, or for any other reason the
facility can’t accept the person, it is up to the receiving facility to arrange the
person’s transfer to a more appropriate facility. It may be true that the facility
won’t “admit” a person with Alzheimer’s or other medical conditions, but it must

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
152
“accept” the person and arrange for medical transport rather than having the officer
put such a person back into the cruiser.
As noted above, section 394.455(28), Florida Statutes, defines the term “mental
illness.” This definition excludes developmental disabilities, substance abuse
impairment, and antisocial behavior. It has no other exceptions for Alzheimer’s or
other conditions. If a person has Alzheimer’s and otherwise meets the criteria for
involuntary examination, the person can indeed be Baker Acted.
Is it possible to involuntarily hospitalize someone with severe anorexia, and if
so, what are the criteria used and what type of professional would evaluate
and sign the Baker Act forms?
A person must have a “mental illness” as defined in the Baker Act and meet the
criteria for involuntary examination, including that:
there is reason to believe that the person has a mental illness and
because of his or her mental illness:
(a)1. The person has refused voluntary examination after
conscientious explanation and disclosure of the purpose of the
examination; or
2. The person is unable to determine for himself or herself
whether examination is necessary; and
(b)1. Without care or treatment, the person is likely to suffer from
neglect or refuse to care for himself or herself; such neglect or refusal
poses a real and present threat of substantial harm to his or her well-
being; and it is not apparent that such harm may be avoided through
the help of willing family members or friends or the provision of other
services; or
2. There is a substantial likelihood that without care or treatment
the person will cause serious bodily harm to himself or herself or
others in the near future, as evidenced by recent behavior.
§ 394.463(1), Fla. Stat.
The involuntary examination can be initiated by a circuit court judge, a law
enforcement officer, or an authorized mental health professional.
Regarding your first question about anorexia as a diagnosis, professionals usually

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
153
consider a thought or mood disorder diagnosis to be required for the Baker Act. If
you as an authorized professional, based on your own evaluation of the person,
believe anorexia to be such a thought or mood disorder or that the person has a
thought or mood disorder in addition to the anorexia, that would suffice.
One of the criteria for commitment for involuntary examination is “The
person is unable to determine for himself or herself whether examination is
necessary.” Is there any guidance, case law, or criteria that are used to make
this determination?
Zinermon v. Burch, 494 U.S. 113, 110 S.Ct. 975, 108 L.Ed.2d 100 (1990), a U.S.
Supreme Court decision, was based on the definitions and other provisions of
chapter 394, part I, Florida Statutes, which include:
394.455. Definitions (emphasis added)
(15) “Express and informed consent” means consent voluntarily
given in writing, by a competent person, after sufficient explanation
and disclosure of the subject matter involved to enable the person to
make a knowing and willful decision without any element of force,
fraud, deceit, duress, or other form of constraint or coercion.
* * *
(21) “Incompetent to consent to treatment” means a state in which
a person’s judgment is so affected by a mental illness that he or she
lacks the capacity to make a well-reasoned, willful, and knowing
decision concerning his or her medical, mental health, or substance
abuse treatment.
394.459. Rights of patients
(3) Right to express and informed patient consent.--
(a)1. Each patient entering treatment shall be asked to give express
and informed consent for admission or treatment. . . .
394.4625 Voluntary admissions (emphasis added)
(1) Authority to receive patients.--
(a) A facility may receive for observation, diagnosis, or treatment
any person 18 years of age or older making application by express

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
154
and informed consent for admission or any person age 17 or under
for whom such application is made by his or her guardian. If found to
show evidence of mental illness, to be competent to provide express
and informed consent, and to be suitable for treatment, such person 18
years of age or older may be admitted to the facility. A person age 17
or under may be admitted only after a hearing to verify the
voluntariness of the consent.
* * *
(d) A facility may not admit as a voluntary patient a person
who has been adjudicated incapacitated, unless the condition of
incapacity has been judicially removed. If a facility admits as a
voluntary patient a person who is later determined to have been
adjudicated incapacitated, and the condition of incapacity had not
been removed by the time of the admission, the facility must either
discharge the patient or transfer the patient to involuntary status.
(e) The health care surrogate or proxy of a voluntary patient
may not consent to the provision of mental health treatment for
the patient. A voluntary patient who is unwilling or unable to provide
express and informed consent to mental health treatment must either
be discharged or transferred to involuntary status.
(f) Within 24 hours after admission of a voluntary patient, the
admitting physician shall document in the patient’s clinical record
that the patient is able to give express and informed consent for
admission. If the patient is not able to give express and informed
consent for admission, the facility shall either discharge the
patient or transfer the patient to involuntary status pursuant to
subsection (5).
The Baker Act has always required that an adult be competent to provide express
and informed consent in order to be admitted or retained on voluntary status. An
involuntary examination is based on, among other criteria, the person either
refusing the examination or being unable to determine for himself/herself whether
examination is necessary. Refusal is fairly clear. However, a finding of the
inability to determine whether examination is necessary can be based on any
number of situations; for example:
The person is like Burch in the case cited above, who was willing to go

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
155
anywhere, do anything, or sign any document because he thought he was in
Heaven. The U.S. Supreme Court found this to be de facto evidence of being
incompetent to provide express and informed consent.
The person repeatedly changes his/her mind.
The person is clearly manipulating a law enforcement officer to avoid
involuntary status.
The person may have a severe impulse control problem and is articulating a
desire for help, but may not be able/willing to act on the desire.
Generally “unable to determine” is someone who fits one or more of the above
types of situations or is determined to be unable to make consistent “a well-
reasoned, willful, and knowing decision concerning his or her medical, mental
health, or substance abuse treatment.” § 394.455(21), Fla. Stat.
Can an individual who is a non-resident of Florida be legally detained and
court committed under the Florida Baker Act?
Yes. Any person who is present in the state of Florida is subject to the Baker Act.
Such persons, if they meet the criteria for involuntary examination, can be taken
into custody and legally examined under the law. If they are found to meet the
criteria for involuntary placement, a petition can be filed to further detain them for
treatment. It may be advisable to arrange a return of the person to his/her own state
as soon as possible to ensure appropriate discharge and aftercare planning. Finally,
if the person is a foreign national with citizenship in another country (even if with
dual citizenship in the U.S.), there are obligations for consular notification and
access.
How is “self-neglect” defined as a criteria for involuntary examination?
The Baker Act doesn’t actually define self-neglect, but it does provide for the
situation when the person is likely to suffer a real and present threat of substantial
harm to his or her well-being that isn’t avoidable by intervention from family,
friends, or other services. The self-neglect must be a result of mental illness and
could take the form of refusing necessary prescription medications, refusing to eat
or drink, inability to sleep, placing oneself in imminently dangerous situations, or
other high risk behaviors. It would not include refusal of medical intervention by a
person with the capacity to make such decisions.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
156
B. Initiation in General
Does an authorized person have a duty to initiate an involuntary
examination?
Judges and mental health professionals do not have a statutory duty to initiate the
examination when they have reason to believe the criteria have been met.
However, they may have a responsibility under their code of ethics or under case
law. On the other hand, a law enforcement officer has no discretion as to initiating
an involuntary examination if he/she has reason to believe the criteria are met.
I’d like to know more about “reason to believe” the criteria are met — how
much discretion an authorized person has. If a court “may” do something
(discretionary) like initiate involuntary examination, what criteria is the court
to use in determining whether to actually do it? Is it just a matter of general
prudence? If you have the right but not the duty to do something, can you just
base the decision on whim, or are there some implied criteria?
That is correct — a judge and a mental health professional may initiate if they have
reason to believe the criteria are met, but have no duty to do so. A law enforcement
officer has the duty to do so if he/she has reason to believe the criteria are met. If a
law enforcement officer doesn’t believe the criteria are met and declines to initiate,
he/she may wish to document at the time, on an incident report, the reason for not
initiating.
Law enforcement officers are required to initiate if they have reason to believe;
judges are not required to initiate even if they have reason to believe. So a judge
could find all the criteria to be met and still decline to initiate examination. The
discretion offered by the “may” language comes down to whether the person with
the legal authority to make the decision has reason to believe each of the criteria is
met.
Some judges are more likely than others to sign orders for emergency action
(domestic violence, Baker Act, Marchman Act, etc.). Other judges won’t sign such
an order if it will deprive a person of liberty unless it’s first proven that the criteria
are met. The standard is simply having “reason to believe.” In Blair v. Razilou,
2010 WL 571980 (M.D. Fla. 2010), a federal lawsuit against the city of Naples
police department, the court held that under the facts known to the police officer at
the time of the Marchman Act initiation, a reasonable officer in the same
circumstances could have believed the plaintiff met the Marchman Act criteria.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
157
The criteria are clearly spelled out in the law. The person with the authority to
initiate must rely on those criteria — nothing more or less. However, everyone has
filters through which objective facts are applied against the criteria in determining
whether he or she has reason to believe the criteria are met. Some examples are:
A belief that both the clinical and functional aspects of the definition of
mental illness are met.
That the person has refused or is unable to determine the examination is
needed. Refusal is objective, but the inability to determine may be quite
subjective.
That the person’s self-neglect is “real, present and substantial.”
That the bodily harm is serious enough, and whether the actions on which
that conclusion is based are recent enough or the harm will occur in the near
enough future.
These aren’t “whims” but individual belief systems. While continued training can
add much more consistency for those who are authorized to initiate involuntary
examinations, the subjective differences in “reasons to believe” will and should
remain.
If persons with the authority to initiate an involuntary examination deviate far from
their professional standards, they can face discipline from groups such as licensing
boards, the Judicial Qualifications Commission, or Internal Affairs, depending on
whether the initiator is a mental health professional, judge, or law enforcement
officer.
Can a patient who requested voluntary status after coming in under
involuntary status be transferred to a public facility under a newly created
professional’s certificate? My thought is that the patient’s status should be
changed to involuntary and a petition filed. Is this correct?
Yes. Too frequently people are transferred from involuntary to voluntary status
who can’t consistently make well-reasoned, willful, and knowing decisions about
their medical, mental health, or substance abuse treatment — the very definition of
competence to consent. Then when the person requests discharge or refuses
treatment, the law requires that either the person be released within 24 hours or a
petition for involuntary inpatient placement be filed within two court working days
of the person’s request/refusal.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
158
A certificate of a professional is only used to have the person taken into custody
and delivered to a designated receiving facility. Once at a receiving facility, the
proper procedure is to release the person, convert to voluntary, or file the
placement petition within 72 hours. However, when a petition for involuntary
inpatient placement is filed on behalf of a person on voluntary status who requests
discharge or refuses treatment, it must be filed within two working days of the
request or refusal. Any transfer to another facility and re-evaluation at that facility
would have to fit within the original 72-hour period during which a person’s liberty
can be denied for the purpose of involuntary examination.
How does a family member get his or her adult child Baker Acted when the
parties reside in different states? Can the person obtain an ex parte order in
Florida that would be enforced in Delaware? Could the family member have
the receiving facility be a VA hospital in Delaware if the subject qualifies?
Each state has enacted its own mental health law, and each is different. The family
would have to contact the Delaware authorities to determine the basis for an
involuntary examination in that state. Any initiation of such action would probably
have to take place in the state where the person needing the examination actually
lives so his/her due process rights can be protected. It is unknown whether
Delaware would permit the family to communicate with the court or others having
authority to initiate such intervention by sworn testimony or whether their presence
would be required — it depends on the requirements of that state’s mental health
law. Regarding treatment at a VA hospital, this would be permitted in Florida, but
whether that would apply in Delaware is unknown.
C. Initiation by Courts
I am trying to find out the procedure for a family member to petition a judge
for an ex parte order to have someone involuntarily picked up for psychiatric
assessment. We have had times when we advise the family to get one but never
tell them how to do it. Does it require more than one person to get it? Can a
non-relative request an ex parte order for a friend or neighbor if no family is
around?
The Baker Act provides the following for an ex parte order:
A circuit or county court may enter an ex parte order stating that a
person appears to meet the criteria for involuntary examination and
specifying the findings on which that conclusion is based. The ex
parte order for involuntary examination must be based on written or

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
159
oral sworn testimony that includes specific facts that support the
findings. If other less restrictive means are not available, such as
voluntary appearance for outpatient evaluation, a law enforcement
officer, or other designated agent of the court, shall take the person
into custody and deliver him or her to an appropriate, or the nearest,
facility within the designated receiving system pursuant to s. 394.462
for involuntary examination. The order of the court shall be made a
part of the patient’s clinical record. A fee may not be charged for the
filing of an order under this subsection. . . . The order shall be valid
only until the person is delivered to the facility or for the period
specified in the order itself, whichever comes first. If no time limit is
specified in the order, the order shall be valid for 7 days after the date
that the order was signed.
§ 394.463(2)(a)1., Fla. Stat.
Any person who has first-hand knowledge of the individual’s mental health status
can file a petition with the probate office of the clerk of court. The law just states
that it must be based on sworn testimony, but doesn’t indicate how many people
must file. It generally requires only one petition if the judge believes the criteria to
be met. If the judge has any reservations, he/she might require a second petition.
The judge is going to want to be assured that the petitioner’s reason for filing isn’t
retaliatory in any way.
The four-page model petition form (CF-MH 3002) can be found on the DCF
website, but the court in your circuit may have modified the form. There is no
reason the petitioner couldn’t have a copy of the form in advance to know what
type of information may be required. The staff in the clerk’s office is not able to
provide the petitioner more than ministerial assistance. See § 28.215, Fla. Stat.
(“The clerk of the circuit court shall provide ministerial assistance to pro se
litigants. Assistance shall not include the provision of legal advice”); Op. Att’y
Gen. Fla. 94-80 (1994). Once the petitioner completes the form and swears to the
accuracy of the information provided, the clerk will take the form to the judge and
the judge will decide whether to sign an ex parte order for examination and a pick-
up order for the sheriff to execute. The whole process shouldn’t take more than
several hours, assuming the person can be easily found.
A judge completed a law enforcement BA form and marked out everywhere it
said law enforcement officer and wrote in “Judge.” If a judge wanted to
Baker Act someone, what would be the appropriate form to use? Now that the
law enforcement officer is at our door with the Baker Act form completed by

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
160
the judge, what would be the appropriate steps for the receiving facility to
take?
A judge doesn’t qualify to execute a law enforcement officer’s report initiating an
involuntary examination under the Baker Act. Only a certified law enforcement
officer is authorized to do so — this is defined below:
394.455. Definitions
As used in this part, unless the context clearly requires otherwise, the
term:
(24) “Law enforcement officer” has the same meaning as provided
in s. 943.10.
943.10. Definitions; ss. 943.085-943.255
The following words and phrases as used in ss. 943.085-943.255 are
defined as follows:
(1) “Law enforcement officer” means any person who is elected,
appointed, or employed full time by any municipality or the state or
any political subdivision thereof; who is vested with authority to bear
arms and make arrests; and whose primary responsibility is the
prevention and detection of crime or the enforcement of the penal,
criminal, traffic, or highway laws of the state. This definition includes
all certified supervisory and command personnel whose duties
include, in whole or in part, the supervision, training, guidance, and
management responsibilities of full-time law enforcement officers,
part-time law enforcement officers, or auxiliary law enforcement
officers but does not include support personnel employed by the
employing agency.
A judge is authorized to enter an order initiating an involuntary examination only
under the following circumstances:
394.463. Involuntary examination
(2) Involuntary examination.--
(a) An involuntary examination may be initiated by any one of the
following means:

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
161
1. A circuit or county court may enter an ex parte order stating
that a person appears to meet the criteria for involuntary examination
and specifying the findings on which that conclusion is based. The ex
parte order for involuntary examination must be based on written or
oral sworn testimony that includes specific facts that support the
findings. If other less restrictive means are not available, such as
voluntary appearance for outpatient evaluation, a law enforcement
officer, or other designated agent of the court, shall take the person
into custody and deliver him or her to an appropriate, or the nearest,
facility within the designated receiving system pursuant to s. 394.462
for involuntary examination. The order of the court shall be made a
part of the patient’s clinical record. A fee may not be charged for the
filing of an order under this subsection. A facility accepting the
patient based on this order must send a copy of the order to the
department on the next working day. The order may be submitted
electronically through existing data systems, if available. The order
shall be valid only until the person is delivered to the facility or for the
period specified in the order itself, whichever comes first. If no time
limit is specified in the order, the order shall be valid for 7 days after
the date that the order was signed.
The model petition that contains the statutorily required sworn testimony is form
CF-MH 3002, and the Ex Parte Order for Involuntary Examination is form CF-MH
3001. It would be good to work through your agency’s attorney to get information
to the judge as soon as possible so this doesn’t happen again. Judges are usually
grateful for the information. You may wish to inform your attorney of this event in
any case.
I’m a circuit court judge. I’ve heard that some judges believe that a judge can
enter an order in open court for an involuntary examination of a person who
appears in court exhibiting symptoms of a mental illness. I believe this would
be unlawful and that a petition must be filed, or that law enforcement could
make the determination if called to the courtroom but that the judge could
not.
You are correct. Section 394.463(2)(a)1., Florida Statutes, requires that any ex
parte order “be based upon written or oral sworn testimony.”
While the law permits oral testimony that could potentially be elicited in a
courtroom, the Florida Administrative Code requires use of the model state form
(CF-MH 3002) “or other form used by the court.” Fla. Admin. Code R. 65E-5.280.

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
162
Whatever form or method is used, the information included on the petition form is
considered by most courts to guide the appropriate application of the law.
Our CSU received two admissions yesterday on orders signed by a county
judge, titled “Order Releasing Defendant on His Recognizance for Psychiatric
Evaluation.” The patients came to us from the county jail with the language
“Ordered and Adjudged that the Defendant in the above-styled case is to be
released on his/her own recognizance contingent upon the Detention Center
personnel delivering him/her to the public receiving facility for evaluation and
treatment. The Defendant shall not be released from the facility unless 24
hour advance notice has been provided to this Court in writing so that the
Court may further consider his/her custodial status.” Do we treat this as an ex
parte order under the Baker Act and follow Baker Act procedure filing a
petition for placement to hold the patient beyond 72 hours, or do we consider
this court order sufficient to hold the patient and treat the patient without
further action? Can the patient consent to his/her own treatment if the
psychiatrist finds the individual competent to do so? If the patient is found by
the psychiatrist to be incompetent to consent to treatment, should we petition
the court for a guardian advocate, or is the fact that the order we received
includes the word treatment sufficient to treat the patient? We had an order
similar to this some time back, and the public defender had us file a BA-32
and have a guardian advocate appointed, stating that the order signed by the
judge denied the patient his rights under the Baker Act.
You must either accept a judge’s order or appeal it — otherwise you might be
subject to contempt. This is one that you may wish to have your attorney review,
perhaps with the DCF circuit legal counsel as well. Until July 1, 2016, only a
circuit judge has jurisdiction to enter an ex parte order for involuntary examination
under the Baker Act — not a county judge, unless the chief judge has appointed
that county judge to sit circuit for a temporary period. It sounds like the judge
didn’t initiate the involuntary examination under the Baker Act, the civil mental
health statute. Instead, it appears to be a forensic competency evaluation; this is
usually done while the person is in jail, by experts appointed by the court and at the
cost of the local judicial system.
It is important that the purpose of the examination/evaluation be clarified as
quickly as possible because the latter evaluation probably wouldn’t be possible at
your facility. If it is intended to be a civil ex parte order, you must release the
person back to law enforcement within 72 hours or file a BA-32 with the court for
further “detention.” At this point, the person will have a public defender to
represent him/her in the Baker Act proceedings. The person probably already has a

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
163
public defender for the criminal matter. Again, if it is a Baker Act issue, the person
can consent or refuse to consent to his/her own treatment if found by the physician
to be able to make a well-reasoned, willful, and knowing decision about medical,
mental health, or substance abuse treatment. Otherwise, a guardian advocate would
have to be requested per the Baker Act. Your attorney and the DCF counsel should
meet with the local judges about the appropriateness of certain court orders for
future reference.
Can a county court judge in a first appearance hearing order a misdemeanor
defendant to have an involuntary Baker Act assessment? In our county the
judge has been ordering the individual to cooperate with CSU in its Baker Act
assessment, not actually ordering the evaluation but rather leaving that to the
discretion of the mental health professional.
No. A circuit or county judge has jurisdiction under the Baker Act to enter an ex
parte order for “involuntary” examination. Such an order has to be based on sworn
testimony by an individual who has personal observations of the defendant’s
behavior.
However, in the circumstance you describe, the defendant is being ordered to be
“voluntary” under the law. This involves providing express and informed consent
to the examination. Such consent cannot involve any element of force, duress, or
coercion:
394.455. Definitions
(15) “Express and informed consent” means consent voluntarily given in
writing, by a competent person, after sufficient explanation and disclosure of
the subject matter involved to enable the person to make a knowing and
willful decision without any element of force, fraud, deceit, duress, or other
form of constraint or coercion.
However, a judge’s order prevails unless it is appealed by a party with standing to
do so. In such a circumstance, the defendant’s public defender or private counsel or
the assistant state attorney is probably the party with such standing. It might be
helpful for the attorney representing your agency to meet with the judge on the
issue for future reference.
When a judge issues a pick-up order for the sheriff to take a person into
custody under the Baker Act, what happens if law enforcement can’t find the
person within 14 days? Does the petitioner need to go back to the court and
resubmit the petition, or does the sheriff keep the order indefinitely?

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
164
Section 394.463(2)(a)1., Florida Statutes, states: “The order shall be valid only
until the person is delivered to the facility or for the period specified in the order
itself, whichever comes first. If no time limit is specified in the order, the order
shall be valid for 7 days after the date that the order was signed.” This means that
the judge can make the order for a period greater or less than seven days, but if no
time is specified by the judge, it expires seven days after it is signed. In the
example you describe, the order was written to provide up to 14 days for law
enforcement to find the person and take him/her into custody. If that occurs within
14 days, the order expires upon taking the person into custody and acceptance at
the receiving facility. If the person isn’t found within the 14 days, the order expires
and a new order would have to be sought to take the person into custody.
I am a general magistrate handling BA hearings. Is a hearing required when
an ex parte petition for involuntary examination is denied due to legal
insufficiency? That is, should an order denying the request for examination
provide a hearing date for a petitioner to address his or her concerns?
A hearing is not needed to deny the petition for legal insufficiency at the time of or
subsequent to a denial anywhere in the state. The law and rules governing this
process only require an ex parte process (without a hearing) for a court to enter an
order denying a person his or her liberty for the purpose of involuntary
examination. The sworn testimony in an affidavit should stand on its own as to
whether the information is persuasive in convincing a judge that there’s reason to
believe each of the criteria is met. There is no reason why a judge couldn’t conduct
a hearing with a petitioner if he/she believed it was needed. Neither is there any
reason why the petitioner couldn’t file a subsequent amended petition providing
additional information for the judge’s consideration. Finally, if the patient’s
condition escalated after the petition was filed/denied, the petitioner could contact
law enforcement in an emergency to request initiation of the examination.
D. Transport
Can a judge order an individual to be transported for involuntary
examination to a facility that is not the nearest?
No. A person must be taken by law enforcement to the facility designated in the
county’s transportation plan or the nearest receiving facility rather than to the
preferred facility. After arrival at the designated Baker Act receiving facility, the
person or legal representative can request a transfer to an alternate facility.
Exceptions are when law enforcement believes an emergency medical condition
exists or a transportation plan has been approved by the board of county

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
165
commissioners.
E. Examination and Release
Can you explain the timeframes for involuntary examination under the Baker
Act and when the petition for involuntary placement must be filed with the
court?
The 72-hour clock starts when the person under the Baker Act arrives at a hospital
or receiving facility for involuntary examination. This means if the person is
delivered to your ER by law enforcement, that is when the clock starts ticking. It
only stops if a physician documents that an emergency medical condition exists,
and it starts back up again as soon as the doctor documents that the emergency
medical condition has stabilized or doesn’t exist. If the involuntary examination is
initiated at your facility, the 72-hour period begins at the time the initiation form is
signed.
The BA-32 petition for involuntary placement must be completed within the 72-
hour period. It must also be filed with the court within the 72-hour period, unless
that period ends on a weekend or legal holiday. No mention is made of weeknights.
Therefore, if a person arrives at 5 a.m. on a Monday, you would have to file the
petition before close of court on Wednesday, unless electronic filing is available, in
which case it would be filed by 5 a.m. Thursday. Otherwise, the filing would
exceed the 72-hour period from the point of arrival. However, if the person arrives
at 5 a.m. on a Thursday, the petition must still be completed (signatures of both
experts and the administrator) within 72 hours, but it doesn’t need to be actually
filed with the court until Monday (the next working day). See rule 2.514(a),
Florida Rules of Judicial Administration, regarding computing time.
A petition for involuntary inpatient placement was recently dismissed in our
county because more than 72 hours had passed between the law enforcement
officer taking the patient into custody and the filing of the petition for
placement. Please clarify.
The date/time the person was taken into custody is not referenced in the law/rules.
In every case, the clock starts when the person arrives at the first facility (either ER
or receiving facility). It is important to remember that all parts of a hospital, not
just the psychiatric unit, are part of the receiving facility.
Who has to receive a notice of the person’s release from a receiving facility after
an involuntary examination?

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
166
Notice has to be given to the person’s guardian or representative, to any person who
executed a certificate admitting the person to the receiving facility, and to any court
that ordered the person’s evaluation.
X. Selected Baker Act Forms for Involuntary Examination
Please note that these recommended forms were promulgated by DCF before
the 2016 statutory amendments and do not incorporate those changes.
A. Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary
Examination

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
167
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _____________________________ CASE NO.: __________________________
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination
I, _____________________________ , being duly sworn, am filing this sworn statement requesting a
Print Name of Petitioner
court order for the involuntary examination of _____________________________________ (hereinafter referred to as
PERSON). Print Name of Person
This petition and affidavit will be included in the PERSON’s clinical record and may be viewed by the PERSON.
I understand that by filling out this form, the PERSON may be taken by law enforcement to a mental health facility for an
examination.
I SWEAR that the answers to the following questions are given honestly, in good faith, and to the best of my knowledge.
1. a. I live at: (Print Your Full Residence Address and Phone Number) Phone: (______) ________________________
Street Address: _____________________________________ City __________________ ST _____ Zip_______
b. I work as a: (Occupation) __________________________ Work Phone: (_____) ________________________
Work Street Address: _____________________ City _______________ ST _____ Zip _______
c. The PERSON lives at, or may be found at, the following address(es):
Street Address: ____________________________________________________ City _____________________
Street Address: ____________________________________________________ City _____________________
Street Address: ____________________________________________________ City _____________________
2. I have the following relationship with the PERSON: ____________________________________________________
______________________________________________________________________________________________
3. (Check the one box that applies)
a. I or a family member have or have not previously made allegations to law
enforcement involving this PERSON on _____________ (Date) such as domestic violence, trespassing,
battery, child abuse or neglect, Baker Act, neighborhood disputes, etc. as described: ___________________
_______________________________________________________________________________________
_______________________________________________________________________________________
b. This PERSON has or has not previously made allegations to law
enforcement about me or my family on ________________ (Date) such as domestic violence, trespassing,
battery, child abuse or neglect, Baker Act, etc. as described: ______________________________________
_______________________________________________________________________________________
CONTINUED OVER

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
168
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 2)
4. (Check the one box that applies)
a. I or a family member are not now, and have not in the past, been involved in a court case with the
PERSON.
b. I or a family member am now, or was, involved in a court case with the PERSON. This case is/was a
________________________________________________ in _______________________________
Type of Case When
Explain:_______________________________________________________________________________
______________________________________________________________________________________
5. I am on good terms with the PERSON at the present time. (Check one box) Yes No If "no",
please explain: _________________________________________________________________________
______________________________________________________________________________________
6. I have known the PERSON for ___________________________ (how long).
a. The PERSON has only recently displayed unusual kinds of behavior.
b. The PERSON has, over a period of time, always acted in a strange manner.
c. The PERSON’s behavior has developed over a period of time.
COMPLETE THE FOLLOWING ONLY IF THE SECTION APPLIES TO THIS CASE:
7. I have seen the following behavior, which causes me to believe that there is a good chance that the PERSON
will cause serious bodily harm to himself/herself or others. On ____________ at approximately ____ am pm,
Date Time
I saw the PERSON: _______________________________________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
8. Other similar behavior I have personally seen is as follows: __________________________________________
________________________________________________________________________________________
________________________________________________________________________________________
9. To my knowledge or belief, I do I do not believe these actions were a result of [intellectual
disability], developmental disability, intoxication, or conditions resulting from antisocial behavior or substance
abuse impairment.
CHECK AND/OR ANSWER APPLICABLE SECTIONS
10. a. I have attempted to get the PERSON to agree to seek assistance for a mental or emotional problem(s). I
explained the purpose of the examination (describe when, who was present, and whether you or another
person explained the need for the examination): _______________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
b. I did not try to get the PERSON to agree to a voluntary examination because: ______________________
______________________________________________________________________________________
c. The PERSON refused a voluntary examination because: _______________________________________
______________________________________________________________________________________
CONTINUED

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
169
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 3)
11. The following steps were taken to get the PERSON to go to a hospital for mental health care: __________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
These steps did not work because: _________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
12. I believe that the PERSON is unable to determine for himself/herself, why the examination is necessary
because: ______________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
13. I believe that the PERSON has a mental illness which will keep the PERSON from being able to meet the
ordinary demands of living because: ________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
14. I believe that without care or treatment, the PERSON is likely to suffer from neglect or refuse to care for
himself/ herself, because: ________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
15. I believe that this lack of care or neglect will lead to the PERSON hurting himself or herself because:
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
16. Can family or close friends now provide enough care to avoid harm to the PERSON? Yes No,
If not, why?
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
CONTINUED OVER

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
170
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (Page 4)
Provide the following identifying information about the person (if known) if it is determined
necessary to take the person into custody for examination:
County of Residence: Date of Birth:
Sex : Male Female Race: Attach a picture of the PERSON if possible. Picture attached: No Yes
Height: Weight: Hair Color: Eye Color:
Does the PERSON have access to any weapons? No Yes If yes, describe:
Is the PERSON violent now? No Yes Has the person been violent in the recent past? No Yes If Yes,
Describe:
Does the PERSON have any pending criminal charges against him/her? No Yes If yes, describe:
GUARDIANSHIP:
1) Does the PERSON have a legal guardian? No Yes
2) Is there a pending petition to determine the PERSON’s capacity and for the appointment of a guardian? No Yes
If YES to either of the above, provide the name, address and phone number of the current or proposed guardian.
Name: Phone: (___________) _____________________________
Address: City: Zip: ________
______________________________________________________________________________________________
PHYSICIAN: Name: Phone: ( )
MEDICATIONS: Provide name of medications if known.
CASE MANAGEMENT: Provide name and phone number of case manager or case management agency, if known.
I understand that this sworn statement is given under oath and will be treated as though it
was made before a judge in a court of law. I understand that any information in this sworn
statement which is not to the best of my knowledge and done in good faith may expose me to
a penalty for perjury and other possible penalties under the statutes of the State of Florida.
Under penalties of perjury, I declare that I have read the foregoing document and that the
facts stated in it are true.
Signature of Affiant/Petitioner: ________________________________________________
SWORN TO AND SUBSCRIBED before me OR SWORN TO AND SUBSCRIBED before me
this ______ day of ______________, __________ this ______ day of ______________, ___________
Day Month Year Day Month Year
by _____________________________________ who is personally known Clerk of Circuit Court
to me or presented ________________________________ as identification. _____________________________ County, Florida
___________________________________________________________ By: ______________________________________
Notary Public - State of Florida Deputy Clerk
My Commission expires: Date_____________________
A copy of the petition(s) must be attached to an Ex Parte Order for Involuntary Examination and
accompany the person to the nearest receiving facility.
See s. 394.463, Florida Statutes
CF-MH 3002, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Four Involuntary Examination
_____________________________________________________________________________________
Baker Act Benchguide November 2016
171
B. Ex Parte Order for Involuntary Examination
IN THE CIRCUIT COURT OF THE _______________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: _______________________
Ex Parte Order for Involuntary Examination
Pursuant to Section 394.463(2)(a)1, Florida Statutes, this Court having received sworn testimony, states that the
above-named person, presently within the county, appears to meet the following criteria for involuntary examination:
1. There is reason to believe the above-named person has a mental illness as defined in Section 394.455 (18), F.S.,
and because of this mental illness said person:
(a) has refused voluntary examination after conscientious explanation and disclosure of the purpose of the
examination; or
(b) is unable to determine for himself/herself whether examination is necessary, AND
2. Either (Check a and/or b)
(a) without care or treatment the above-named person is likely to suffer from neglect or refuse to care for
himself/herself, and such neglect or refusal poses a real and present threat of substantial harm to his or
her well-being and it is not apparent that such harm may be avoided through the help of willing family
members or friends or the provision of other services; OR
(b) There is substantial likelihood that without care or treatment the above-named person will cause serious
bodily harm to
himself or herself or another person in the near future, as evidenced by recent behavior.
One or more Petitions and Affidavits Seeking Order Requiring Involuntary Examination (CF-MH 3002 or equivalent)
on which the above conclusion is based is attached.
Additional information upon which this order is based is: _______________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Therefore, it is
ORDERED
That a law enforcement officer, or designated agent of the Court take the above-named person into custody and deliver
or arrange for the delivery of said person to the nearest receiving facility for involuntary examination, and that this
order and petition be made part of said person’s clinical record. A law enforcement officer or agent may serve and
execute this order on any day of the week, at any time of the day or night. A law enforcement officer or agent may
use such reasonable physical force as is necessary to gain entry to the premises, and any dwellings, buildings, or other
structures located on the premises, and to take custody of the person who is the subject of this ex parte order.
This order expires in ____________ days. If no time limit is specified in this order, the order shall be valid for 7
days after the date that the order was signed.
ORDERED THIS _____________ day of ______________________________, ____________
Date Month Year
_______________________________________________ _____________________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.463, Florida Statutes
CF-MH 3001, Jan 98 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
172
Chapter Five: Involuntary Inpatient Placement
I. In General
See § 394.467, Fla. Stat.; Fla. Admin. Code R. 65E-5.290
The Baker Act encourages people to seek and receive voluntary psychiatric care,
but only when they are able to understand the decision and its consequences and are
able to fully exercise their rights for themselves. When individuals cannot
understand and cannot fully exercise their rights due to the severity of their
condition, the law requires that they be extended the due process rights ensured
under the involuntary provisions of the Baker Act. Involuntary inpatient placement
(commitment) occurs only after an examination and court hearing.
II. Criteria
A person may be ordered for involuntary inpatient placement upon a finding of the
court by clear and convincing evidence that he or she has a mental illness and
because of the mental illness the person has refused voluntary placement or
is unable to determine whether placement is necessary, and either
o he or she is incapable of surviving alone or with the help of others and
without treatment is likely to suffer from neglect that poses a real and
present threat of substantial harm to his or her well-being, or
o there is a substantial likelihood that in the near future he or she will
inflict serious bodily harm on self or other persons, as evidenced by
recent behavior causing, attempting, or threatening such harm;
and all available less restrictive treatment alternatives that would offer an
opportunity for improvement of the condition have been judged
inappropriate.
§ 394.467(1), Fla. Stat.
Each allegation must be supported by evidence sufficient to reach the high level of
evidence required in the involuntary inpatient placement hearing. Appellate courts
have found that expert opinions and conclusions are not sufficient, without
evidence to prove the allegations. The Florida Supreme Court has defined “clear
and convincing evidence” to mean “evidence that is precise, explicit, lacking in

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
173
confusion, and of such weight that it produces a firm belief or conviction, without
hesitation, about the matter in issue.” Fla. Stand. Jury Instr. (Civil) 405.4.
III. Initiation of Involuntary Inpatient Placement
After an examination and timely filing of a petition for involuntary inpatient
placement, a person meeting that criteria may be held pending a court hearing. The
hearing is initiated based upon the recommendation of the administrator of a
receiving facility where the person has been examined.
“The recommendation must be supported by the opinion of a psychiatrist and the
second opinion of a clinical psychologist or another psychiatrist, both of whom
have personally examined the individual within the preceding 72 hours, that the
criteria for involuntary inpatient placement are met.” § 394.467(2), Fla. Stat. The
second opinion may be conducted by electronic means by which all parties
maintain visual as well as audio communication. If the administrator certifies that
no psychiatrist or clinical psychologist is available to provide the second opinion, it
may be provided by a licensed physician with postgraduate training and experience
in diagnosis and treatment of mental illness or by a psychiatric nurse.
The recommendation must be entered on a petition for an involuntary inpatient
placement certificate (form CF-MH 3032), or other form approved by the court,
that authorizes the facility to keep the person pending transfer to a treatment
facility or completion of a hearing. Id.
IV. Petition for Involuntary Inpatient Placement
The administrator of the facility must file a petition for involuntary inpatient
placement (CF-MH 3032), or other form approved by the court, in the court in the
county where the person is located. Upon filing, the clerk of the court must provide
copies to the department, the person, the person’s guardian or representative, and
the state attorney and public defender of the judicial circuit where the person is
located. No fee can be charged for the filing of the petition for involuntary
inpatient placement. § 394.467(3), Fla. Stat.
V. Appointment of Counsel
Within one court working day after the filing of a petition for involuntary inpatient
placement, the court must appoint the public defender to represent the person who
is the subject of the petition, unless the person has other counsel. The clerk of the
court must immediately notify the public defender of the appointment. Any
attorney representing the person shall have access to the person, witnesses, and

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
174
records relevant to the presentation of the person’s case and shall represent the
interests of the person, regardless of the source of payment to the attorney. The
state attorney for the circuit in which the person is located represents the state,
rather than the petitioning facility administrator, as the real party in interest in the
proceeding. § 394.467(4), Fla. Stat.
VI. Continuance of Hearing
The person is entitled, with the concurrence of the person’s counsel, to at least one
continuance of the hearing, for up to four weeks. § 394.467(5), Fla. Stat. This
continuance may be obtained by counsel for the person filing a Notice to Court –
Request for Continuance of Involuntary Placement Hearing (CF-MH 3113) or
other form approved by counsel or the court.
Only the person — not the facility administrator or other parties — has standing to
make such a request. Multiple continuances should not be sought to avoid
placement unless legally sufficient express and informed consent has been
obtained for the person’s treatment.
VII. Independent Expert Examination
The person and the person’s guardian or representative must be informed by the
court of the right to an independent expert examination. Recommended form
“Application for Appointment of Independent Expert Examiner” (CF-MH 3022)
may be used. If the person cannot afford this examination, the court will provide
for one. In August of 2005, the chair of the Florida Trial Court Budget
Commission advised the chief judges and court administrators of all circuits that
while the court must appoint such an independent expert, the expert is a defense
witness and not a court expense. August 24, 2005, Commission Minutes, Agenda
Item II.A. “The independent expert’s report is confidential and not discoverable,
unless the expert is to be called as a witness for the patient at the hearing.”
§ 394.467(6)(a)3., Fla. Stat.
VIII. Hearing on Involuntary Inpatient Placement
The circuit court will hold the hearing on involuntary inpatient placement within
five court working days after the petition is filed, unless a continuance is granted.
The Fifth District Court of Appeal has held that the computation of time for
involuntary placement hearings excludes Saturdays, Sundays, and legal holidays
when the time period is seven days or less; the hearing is not required to be held
within five calendar days but rather within five business days. D.M.H. v. Pietilla,
33 So. 3d 800 (Fla. 5th DCA 2010).

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
175
“Except for good cause documented in the court file, the hearing must be held in
the county or the facility, as appropriate, where the person is located, must be as
convenient to the [person] as is consistent with orderly procedure, and shall be
conducted in physical settings not likely to be injurious to the [person’s]
condition.” § 394.467(6)(a), Fla. Stat. Further:
The court may appoint a magistrate to preside at the hearing.
One of the two professionals who executed the petition for involuntary
placement certificate must be a witness. This role cannot be delegated to
others.
At the hearing, the testimony must be given under oath, and the proceedings
must be recorded. The person may refuse to testify.
If the court finds that the person’s attendance at the hearing is not consistent
with his or her best interests, and the person’s counsel does not object, the
court may waive the presence of the person from all or any portion of the
hearing. Several appellate courts have ruled that if the patient waives the
right to be personally present and be constructively present through counsel,
the trial court must certify through proper inquiry that the waiver is
knowing, intelligent, and voluntary.
The circuit court must consider testimony and evidence regarding the person’s
competence to consent to treatment, as defined in section 394.455(21), Florida
Statutes. If the court finds that the person is incompetent to consent to treatment, it
must appoint a guardian advocate (CF-MH 3107 or other form approved by the
court) as provided in section 394.4598, Florida Statutes. § 394.467(6)(d), Fla. Stat.
If the placement sought for the person is a state treatment facility, the court must
receive and consider the information documented in the statutorily required
Transfer Evaluation (CF-MH 3089). The person who conducted the transfer
evaluation, or in the absence of the evaluator, another knowledgeable staff person
must be present at the hearing to provide testimony as desired by the court.
If at any time before the hearing ends it appears to the court that the person does
not meet the criteria for involuntary inpatient placement but rather meets the
criteria for substance abuse involuntary assessment, protective custody, or
involuntary admission pursuant to section 397.675, Florida Statutes, the court may
order (Order Requiring Involuntary Assessment and Stabilization for Substance
Abuse and for Baker Act Discharge of Person, CF-MH 3114 or other form

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
176
approved by the court) the person to be admitted for involuntary assessment for
five days pursuant to section 397.6811, Florida Statutes. After that, all proceedings
will be governed by chapter 397, Florida Statutes (Marchman Act).
§ 394.467(6)(c), Fla. Stat.
If the court concludes that the person does meet the criteria for involuntary
inpatient placement, it may enter an Order for Involuntary Inpatient Placement
(CF-MH 3008 or other form approved by the court) providing that, for up to 90
days (many courts order a shorter period of time):
the person be transferred to a treatment facility, or
if the person is at a treatment facility, the person be retained there, or
the person is to be treated at any other appropriate receiving or treatment
facility, or is to receive services from a receiving or treatment facility on an
involuntary basis.
However, any order for involuntary mental health services in a treatment facility
may be for up to six months. “The court may not order an individual with
traumatic brain injury or dementia who lacks a co-occurring mental illness to be
involuntarily placed in a state treatment facility.” § 394.467(6)(b), Fla. Stat.
IX. Admission to a State Treatment Facility
Section 394.467(6)(e), Florida Statutes, provides that the administrator of the
petitioning facility must give a copy of the court order and adequate
documentation of a person’s mental illness to the administrator of a treatment
facility (state hospital) when a person is ordered for involuntary inpatient
placement, whether by a civil or a criminal court. The documentation must
include the following:
Any advance directives made by the person.
A psychiatric evaluation of the person.
Any evaluations of the person performed by a psychiatric nurse, a clinical
psychologist, marriage and family therapist, mental health counselor, or
clinical social worker.
State Mental Health Facility Admission Form (CF-MH 7000) with
attachments.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
177
Physician to Physician Transfer (CF-MH 7002). “The administrator of a
treatment facility may refuse admission to any patient directed to its
facilities on an involuntary basis, whether by civil or criminal court order,
who is not accompanied by adequate orders and documentation.”
X. Release of Persons on Involuntary Status
The facility must discharge a person any time the person no longer meets any one
of the criteria for involuntary inpatient placement, unless the person has transferred
to voluntary status. If the release or transfer to voluntary status occurs prior to the
hearing on involuntary inpatient placement, the facility must immediately notify
the court by telephone and by filing a Notification to Court of Withdrawal of
Petition for Hearing on Involuntary Inpatient or Involuntary Outpatient Placement
(CF-MH 3033). See § 394.469(2), Fla. Stat.; Fla. Admin. Code R. 65E-5.320.
The administrator must:
discharge the person, unless the person is under a criminal charge, in which
case the person must be transferred to the custody of the appropriate law
enforcement officer;
transfer the person to voluntary status on his or her own authority or at the
person’s request, unless the person is under criminal charge or adjudicated
incapacitated (this transfer from involuntary to voluntary status must be
conditioned on the certification by a physician that the person has the
capacity to make well‑reasoned, willful, and knowing decisions about
medical, mental health, or substance abuse treatment); or
place an improved person, except a person under a criminal charge, on
convalescent status in the care of a community facility.
§ 394.469(1), Fla. Stat.
XI. Return of Persons
“If a [person] involuntarily held at a treatment facility leaves the facility . . .
without the administrator’s authorization, the administrator may authorize a search
for the [person] and his or her return to the facility. The administrator may request
the assistance of a law enforcement agency in this regard.” § 394.467(8), Fla. Stat.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
178
XII. Procedure for Continued Involuntary Inpatient Placement
See Fla. Admin. Code R. 65E-5.300.
Continued involuntary inpatient placement hearings are administrative hearings
and are conducted by administrative law judges (ALJs) employed by DOAH,
rather than circuit court judges. The hearings “must be conducted in accordance
with s. 120.57(1), except that any order entered by the administrative law judge is
final and subject to judicial review in accordance with s. 120.68.” § 394.467(7)(a),
Fla. Stat. The Fifth District Court of Appeal has held that while continued
involuntary inpatient placement hearings are administrative, the circuit court
retains concurrent jurisdiction during the first six months after the order is entered.
After six months, only DOAH has jurisdiction. W.M. v. State, 992 So. 2d 383 (Fla.
5th DCA 2008). (The 2016 Legislature reduced the maximum period of an order to
90 days at a receiving facility, while retaining a maximum period of six months at
a state facility.)
If the person continues to meet the criteria for involuntary inpatient placement and
is being treated at a treatment facility, the administrator must, within 20 days prior
to the expiration of the period during which the treatment facility is authorized to
retain the person, file a Petition Requesting Authorization for Continued
Involuntary Inpatient Placement (CF-MH 3035). § 394.467(7)(b), Fla. Stat. “If
continued involuntary inpatient placement is necessary for a [person] admitted
while serving a criminal sentence, but his or her sentence is about to expire, or for
a minor involuntarily placed, but who is about to reach the age of 18, the
administrator shall petition the administrative law judge for an order authorizing
continued involuntary inpatient placement.” § 394.467(7)(e), Fla. Stat. The petition
must be filed with:
State of Florida, Division of Administrative Hearings
The Desoto Building
1230 Apalachee Parkway
Tallahassee, FL 32399-3060
Phone (850) 488-9675
Suncom 278-9675
Fax (850) 921-6847
The petition must be accompanied by:
a statement from the person’s physician or clinical psychologist justifying
the request;

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
179
a brief description of the person’s treatment while he or she was
involuntarily placed; and
an individualized plan of continued treatment.
Notice of the hearing must be provided as set forth in section 394.4599, Florida
Statutes. § 394.467(7)(b), Fla. Stat.
Unless the person “is otherwise represented or is ineligible, he or she shall be
represented at the hearing on the petition for continued involuntary inpatient
placement by the public defender of the circuit in which the facility is located.”
§ 394.467(7)(c), Fla. Stat.
If a person’s attendance at the hearing is voluntarily waived, the ALJ must
determine that the waiver is knowing and voluntary before waiving the person’s
from all or part of the hearing. Alternatively, if at the hearing the ALJ finds that
attendance at the hearing is not consistent with the best interests of the person, the
ALJ may waive the presence of the person from all or part of the hearing, unless
the person, through counsel, objects to the waiver. The testimony in the hearing
must be under oath, and the proceedings must be recorded. § 394.467(7)(b), Fla.
Stat.
If the person has been previously found incompetent to consent to treatment, the
ALJ shall consider testimony and evidence regarding the person’s competence. If
the administrative law judge finds evidence that the person is now competent to
consent to treatment, the ALJ may enter a recommended order to the court that
found the person incompetent to consent to treatment that the person’s competence
be restored and that any guardian advocate previously appointed be discharged
(Findings and Recommended Order Restoring Person’s Competence to Consent to
Treatment and Discharging the Guardian Advocate, CF-MH 3116). If the person
has been ordered to undergo involuntary inpatient placement and has previously
been found incompetent to consent to treatment, the court must consider testimony
and evidence regarding the person’s incompetence. If such competency is restored,
the discharge of the guardian advocate is governed by section 394.4598, Florida
Statutes.
If at a hearing it is shown that the person continues to meet the criteria for
involuntary inpatient placement, the ALJ must order continued placement in a
receiving facility for a period not to exceed 90 days. However, any order for
involuntary inpatient placement in a treatment facility (state hospital) may be for
up to six months via the Order for Continued Involuntary Inpatient Placement or

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
180
for Release (CF-MH 3031). The same procedure must be repeated before the
expiration of each additional period the person is retained. § 394.467(7)(d), Fla.
Stat.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
181
XIII. Involuntary Inpatient Placement Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.)

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
182
XIV. Continued Involuntary Inpatient Placement Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.)

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
183
XV. Involuntary Inpatient Placement Hearing Colloquy
A. Introductory Remarks
When the patient is present, giving an overview of the hearing process may be
beneficial:
Today we are holding a hearing on a petition for involuntary inpatient placement
filed under the Baker Act. The purpose of this hearing is to determine whether
clear and convincing evidence supports the criteria for such a court-ordered
placement and whether the patient is competent to make his/her own treatment
decisions or whether the petition should be dismissed. If an order is issued, it will
state the maximum duration of the placement.
As required by law, this hearing is being recorded. The patient has the right to
testify or to remain silent. However, the hearing must proceed in an orderly manner
and the patient must wait for his/her turn to be heard. First, the assistant state
attorney will present evidence as to why the patient should be retained in this or
another Baker Act receiving or treatment facility. Then the patient’s attorney will
present any evidence as to the patient’s wishes regarding this matter. If the state
attorney cannot establish the evidence, or does not wish to proceed with the case, I
will dismiss it without the need for further testimony.
All testimony taken today, including witness testimony, will also be taken under
oath. The state attorney and defense counsel will be allowed the opportunity to
fully respond to the testimony and evidence presented. Each party will be allowed
to call any witnesses and present any evidence they may have.
If an order is entered, it may be unlawful for the patient to purchase a firearm or
obtain a concealed weapons permit, pursuant to federal and Florida law.
Patient’s counsel may have a moment to confer with the client, if he/she has any
questions; otherwise we will proceed.
When the patient is not present, after having those who are present identify
themselves for the record the court should affirmatively address the waiver of the
patient’s presence, if the patient’s counsel did not already sufficiently cover that
when introducing himself/herself:
Is patient’s counsel requesting a waiver of the patient’s presence at the
hearing?

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
184
(If yes, without a sufficient explanation) Briefly state the basis for the
waiver. (If not a “knowing” waiver, the court must find that the patient’s
attendance at the hearing is not consistent with the best interests of the
patient before allowing the attorney to waive the client’s presence.)
More about WAIVING the patient’s presence:
The court must conduct an adequate inquiry of the facility staff or the
patient’s counsel.
At a minimum, the inquiry must ensure the following:
1. that patient received notice of the hearing;
2. that no one prevented the patient from attending the hearing;
3. that the patient was aware of his or her right to be present at the
hearing;
4. that the patient was aware of the nature and purpose of the hearing;
and
5. that the patient’s mental state was such that he or she could
comprehend the right being waived.
Such an inquiry is necessary even when the patient’s presence is waived
by his or her counsel.
Upon conclusion of the inquiry, the court must make an explicit finding
on the record as to whether the patient knowingly, intelligently, and
voluntarily waived his or her presence at the hearing. If a patient does
not have the ability to comprehend the right he/she is waiving, the court
cannot determine that the waiver was knowingly and intelligently
made.
In that event the patient must attend the hearing unless the court finds
that the patient’s attendance at the hearing is not consistent with the best
interests of the patient, and the patient’s counsel does not object. Where
such a finding is made and the patient’s counsel does not object, the
court may waive the presence of the patient from all or any portion of
the hearing.
When the petition requests involuntary placement in a state treatment facility
(e.g., state hospital), the court should acknowledge when the required transfer

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
185
evaluation has been provided to the court for consideration prior to the hearing.
A transfer evaluation completed by the state screener has been provided to the
court and concurs/does not concur with the requested placement. Have the
attorneys had an opportunity to review the transfer evaluation?
B. Preliminary Matters
All witnesses please raise your right hands and be sworn.
Does counsel for the state wish to make an opening statement? Patient’s
counsel?
Counsel for the state may call its first witness.
C. Testimony and Evidence
Testimony and evidence as to involuntary placement and the related appointment
of a guardian advocate (when the patient is alleged to be incompetent to make
his/her own treatment decisions) can generally be heard together. If the court
desires that the guardian advocate portion of the hearing occur only after the
presentation of the case on the petition for involuntary placement and after the
court makes a finding that the criteria have been met for such placement, then the
court should notify the attorneys of that at this time.
Testimony must be given under oath and the proceeding must be recorded. One of
the State’s witnesses must be one of the two professionals who executed the
petition for involuntary placement. After the State presents its case, counsel for the
patient may make an oral motion to dismiss the petition for involuntary inpatient
placement. If that motion is not granted, counsel for the patient must be given the
opportunity to present its own case in defense of the petition. The defense may or
may not include the testimony of the patient.
A patient cannot be required to testify. It is good practice, however, for the Court
to inquire of patient’s counsel if he or she intends to call the patient as a witness. It
may be the case that the patient makes it clear at the hearing that he or she wants to
testify, but counsel for the patient does not believe it is in the client’s best interests
to do so. Before allowing such a patient to testify against the advice of counsel, the
attorney for the patient should be offered a brief recess to permit the attorney to
meet privately with and advise the patient again in that regard. Sample hearsay
issues that may arise at the involuntary placement hearing are:

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
186
Circumstances surrounding admission: The circumstances that led to the current
admission are often significant to the determination as to whether the individual
meets the Baker Act criteria for involuntary placement. Given the short amount of
time that the state has to prepare for the hearing and the stringent statutory
requirements as to when the hearings must be held, witnesses with firsthand
knowledge of those circumstances, such as family members and law enforcement
officers, may not always be available to testify. A testifying physician who has
been qualified as an expert witness in the field of psychiatry may be able to testify
about what was reported in the certificate of the law enforcement officer or the
professional who initiated the involuntary examination.
Doctor, have you considered the circumstances of the patient’s admission as
part of your diagnosis and treatment? (If yes, the expert may give opinion
based on data reasonably relied on by experts, even if such data is not
admissible in evidence. § 90.704, Fla. Stat., basis of opinion testimony by
experts. Additionally, the patient statements in the report of the law
enforcement officer initiating the involuntary examination or in a related
police report may be admissible as evidence of the individual’s then existing
mental, emotional or physical condition. § 90.803(3), Fla. Stat., state of
mind/then-existing mental, emotional, or physical condition hearsay
exception. Further, what the patient told the doctor about these
circumstances may well be admissible. § 90.803(18)(a), Fla. Stat.,
admissions hearsay exception (statement that is offered against a party and is
the party’s own statement).)
Prior admissions: This may not be the first time that the testifying physician has
treated the patient. That knowledge of the patient’s condition and treatment, over
time, enhances the physician’s current diagnosis and opinions as to the involuntary
placement criteria.
Doctor, are you aware of any prior admissions to a psychiatric hospital? (If
yes:)
Did these prior admissions help form a basis for your diagnosis in this case?
(If relevant, the expert may give his or her opinion based on data reasonably
relied on by experts, even if such data is not admissible in evidence.
§ 90.704, Fla. Stat., basis of opinion testimony by experts.)
Patient’s Behavior: The physician should be able to testify about his or her direct
observations of the patient. However, the individual’s behavior during the
admission that the doctor did not personally observe may be just as significant, or

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
187
even more significant, to the determination as to whether the individual meets the
Baker Act criteria for involuntary placement. The physician may reasonably rely
on this information that was not personally observed. Such behavior is typically
documented in the patient’s medical chart, at or near the time the behavior was
observed by the staff member who did personally observe the behavior. The staff
who documented the behavior in the patient’s chart cannot always be available at
the time of the hearing. Often the incidents occur in the evening and the evening
staff members are not on duty at the time of the hearings. The state may be able to
introduce documentation of the behavior (e.g., the record maintained for an
emergency treatment order) from the patient’s medical record.
Doctor, have you had an opportunity to review the staff’s notes in the
record? (If yes:)
Are you familiar with the receiving facility’s record keeping procedures? (If
yes:)
I’m showing what has been pre-marked as State’s Exhibit #1.
Do you recognize this exhibit? (If yes:)
What do you recognize it to be? (If recognized — for example, as
documentation of an Emergency Treatment Order that resulted from the
patient’s behavior:)
Are the entries in this document made at or near the time of the events or
transactions recorded? (If yes:)
Are the entries in this document made from information transmitted by a
person with knowledge of the events or transactions recorded? (If yes:)
Is this record kept in the course of the regularly conducted business activities
of this hospital/receiving facility? (If yes:)
Is it the regular practice of this hospital/receiving facility to make this
record? (If yes:)
Is this exhibit a fair and accurate copy of the original Emergency Treatment
Order for this patient kept in the patient record at this hospital/receiving
facility? (If yes, the state may offer the exhibit into evidence. F.S.
§ 90.803(6), Fla. Stat., business records/records of regularly conducted
business activity exception (records of the hospital/receiving facility, with

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
188
the doctor serving as the qualified witness).)
Other witnesses:
Are there other witnesses to be called by the state?
Does the defense wish to call witnesses?
D. Closing Arguments
With no further evidence to be presented, the court will now hear closing
arguments.
Counsel for the state may proceed.
[Hear argument of assistant state attorney.]
Counsel for the patient may proceed.
[Hear argument of patient’s counsel.]
E. Findings and Order of Court
1. Preliminary Contents
There being no further evidence or argument, the Court is prepared to make
findings.
Having considered the case presented, the Court finds, by clear and
convincing evidence, that
The patient was admitted to this receiving facility on _____(date)_____
and the Petition was timely filed.
The patient does suffer from an apparent or manifest mental illness
diagnosed as ___________________. [If desired/appropriate: In support of
that finding, the Court notes the following facts in evidence _____________
(can describe the nature and extent of this illness and the relevant
accompanying exhibited behavior by the patient.)]
As a result of his/her mental illness, the patient
Has refused voluntary placement for treatment after sufficient and
conscientious explanation and disclosure of the purpose of placement; or

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
189
Is unable to determine for himself/herself whether placement is
necessary.
2. When Baker Act Criteria Have Been Met
and further:
The patient is manifestly incapable of surviving alone or with the help of
willing and responsible family or friends, including available alternative
services, and without treatment is likely to suffer from neglect or refuse to
care for himself/herself, and such neglect or refusal poses a real and present
threat of substantial harm to the patient’s well-being [You may want to refer
to some of the relevant facts/behavior that demonstrate this prong]; and/or
There is a substantial likelihood that in the near future the patient will
inflict serious bodily harm on himself/herself or another person, as
evidenced by recent behavior causing, attempting, or threatening such harm
[You may want to refer to some of the relevant facts/behavior that
demonstrate this prong];
and
All available, less-restrictive treatment alternatives that would offer an
opportunity for improvement of the patient’s condition, are inappropriate.
As a result of these findings, the Court will enter an order that the patient
be involuntarily placed in a designated mental health receiving or treatment
facility as authorized by section 394.467, Florida Statutes, for a period not to
exceed _____(period not to exceed 90 days, or six months if a state
treatment facility)_____* from the date of the order. The recommended
placement is _____(name of receiving or treatment facility)_____. [This
must be “any state treatment facility” when state placement, such as a state
hospital, is being authorized].
*If ordering less than the maximum amount that the court could
order, the court should announce whether it is with or without a
reservation of jurisdiction to extend or modify the court-ordered
placement; for example: The Court finds that this is a short-term
placement and reserves jurisdiction to extend the placement, up to a
full 90-day period from the date that the Involuntary Inpatient
Placement Order is entered, and to otherwise modify the Order to
permit placement in a state treatment facility, upon the filing of an
Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
190
appropriate petition and a hearing thereon. [The order should ideally
provide the specifics for handling extensions and modifications in
your circuit. Sample language is available at the end of this
Colloquy.]
GUARDIAN ADVOCATE APPOINTMENT:
[When required –
A guardian advocate is necessary to act on the patient’s behalf in issues
relating to express and informed consent to _____(psychiatric/medical/
psychiatric or medical)_____ treatment in that the patient is incompetent to
consent to treatment because the patient’s judgment is so affected by his/her
mental illness that the patient lacks the capacity to make a well-reasoned,
willful, and knowing decision concerning treatment.
The proposed guardian advocate, _____(name of individual/agency
proposed to serve as guardian advocate_____, who is a _____(family
member/friend/professional guardian advocate)_____, meets the
qualifications of a guardian pursuant to chapter 744, Florida Statutes; and
The Guardian Advocate has completed the four-hour training
course; or
The four hour training course shall be completed by the Guardian
Advocate as required by Section 394.4598, Florida Statutes, or
The training requirement is waived for the following
reason(s):____________________.
The guardian advocate is deemed discharged upon the discharge of the
patient from involuntary placement under the Baker Act or transfer of the
patient to voluntary status.]
[When not required –
A Guardian Advocate is not required because:
The patient is a minor and his/her parent(s) is/are available to
consent to treatment or
The patient has a legal guardian(s) who is/are authorized by court
order to provide consent to treatment. The legal guardian is:
____________________.]

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
191
3. When Baker Act Criteria Have Not Been Met
and further:
The patient does not meet the criteria for involuntary placement for the
following reasons: ____________________.
As a result, the Petition for the Involuntary Placement filed herein is
hereby _____(denied/dismissed)_____.
[When the patient instead meets applicable Marchman Act criteria:
The patient appears to meet the criteria for involuntary substance abuse
assessment and stabilization as defined in Chapter 397, Florida Statutes.
Based on the evidence presented, the Court will order that the patient be
retained for up to five (5) days for assessment and stabilization under
Chapter 397, Florida Statutes.]
4. Sample Provisions for Short-Term Placement With Reservation of
Jurisdiction to Extend or Modify
The Court finds that this is a short-term placement and reserves jurisdiction to
extend the placement up to a full six-month period from the date that this Order is
entered, and to otherwise modify the Order to permit placement in a state treatment
facility, upon the filing of an appropriate petition and a hearing thereon. Extensions
and modifications shall be handled as follows:
(a) Extensions Only: When a facility is seeking only to extend the current
placement, up to a full 90-day period (or six-month period, for a state
treatment facility) from the date of this Order, it must file a Supplemental
Petition for Involuntary Inpatient Placement (the regular form with
“Supplemental” added to the title). The Supplemental Petition must be
supported by the written statement of the patient’s attending physician
providing the treatment under this Involuntary Placement Order and must
allege additional facts and grounds for the continued treatment that have
occurred since the original petition was filed.
(b) Extensions and Modifications: When a facility is seeking to extend the
current placement up to a full 90-day period (or six-month period for a state
treatment facility) from the date of this Order and to have this Order
modified to authorize placement in a state treatment facility, the facility
must file a Supplemental Petition for Involuntary Inpatient Treatment (using

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
192
the DCF form for a Petition for Involuntary Inpatient Treatment and adding
the word “Supplemental” to the title) in the above-referenced court file,
noting this case number. The Supplemental Petition must be supported in the
same manner as an original involuntary inpatient placement petition (a first
and second opinion), but must also allege additional facts and grounds for
the continued treatment which have occurred since the original petition was
filed. Additionally, a Transfer Evaluation must be provided to the Court
prior to the hearing on the Supplemental Petition, in accordance with
applicable law.
Any Supplemental Petition filed pursuant to (a) or (b) above must be filed no later
than two (2) weeks prior to the expiration of the short-term placement period
ordered herein, UNLESS the placement was for 30 days or less, in which case the
Supplemental Petition must be filed within a reasonable time prior to the expiration
of the short-term placement order.
XVI. Frequently Asked Questions
A. Criteria and Eligibility
What is the difference between the criteria for involuntary examination and
involuntary placement?
The Baker Act requires that there be “clear and convincing evidence” that the
criteria are met for placement, rather than “reason to believe” by one of the
specified persons authorized to initiate the examination. Further, the criteria for
placement require that all less restrictive treatment alternatives that would offer an
opportunity for improvement of the person’s condition have been judged
inappropriate. The burden of proof is by “clear and convincing evidence,” defined
as “evidence that is precise, explicit, lacking in confusion, and of such weight that
it produces a firm belief or conviction, without hesitation, about the matter in
issue.” Fla. Stand. Jury Instr. (Civil) 405.4.
Our facility received an involuntary Baker Act client from our jail with an
order for Release on Own Recognizance and Direct Transport to Baker Act
Facility from the mental health court judge. We did a first and a second
opinion and filed a petition for involuntary placement with the court for 90
days and for appointment of her mother, who is a plenary guardian, as a
guardian advocate. When we arrived in court, the state attorney told the
magistrate we did not need an order to place the client; that the existing
guardianship order was all that was needed. The magistrate and state

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
193
attorney decided we were in error. Who is right?
Once a person is released from the criminal justice system into the civil system for
the involuntary examination or placement, the Baker Act prevails. A criminal court
order to a civil facility for examination and placement wouldn’t be sufficient on its
own — the provisions of section 394.467, Florida Statutes, would apply. There
have been two fairly recent appellate decisions issued by the Second District Court
of Appeal that criminal court orders were insufficient to justify civil placement
under the Baker Act: Perkins v. State, 84 So. 3d 336 (Fla. 2d DCA 2012); In re
Involuntary Placement of Linn, 79 So. 3d 783 (Fla. 2d DCA 2011).
The public defender has the duty to be present and to argue for the due process
rights of the individual. Handley v. Dennis, 642 So. 2d 115 (Fla. 1st DCA 1994),
identifies the role of a public defender in a Baker Act case, as well as clearly
stating that the rights of the patient under the Baker Act outweigh any rights of a
guardian under the guardianship statute. The Fourth District Court of Appeal in
Auxier v. Jerome Golden Center for Behavioral Health, 85 So. 3d 1164 (Fla. 4th
DCA 2012), agreed with the First District Court of Appeal decision in Handley.
While the guardian has no authority to voluntarily admit the ward to a Baker Act
receiving facility, she would have had the authority to consent to treatment once
the ward was there on an involuntary status. There was no need to seek
appointment of a guardian advocate to provide consent for treatment of an adult
with a plenary guardian appointed by the court. The guardian can make treatment
decisions — not admission decisions under the Baker Act.
If a psychotic patient who is not a U.S. citizen refuses medications needed for
stabilization, do we follow the same process of first and second opinion, obtain
a proxy, and have the court appoint a guardian advocate, or does the U.S.
Citizenship and Immigration Services act as the decision maker?
Any person who is present in the state of Florida is subject to the Baker Act. Such
persons, if they meet the criteria for involuntary examination, can be taken into
custody and legally examined under the law. If they are found to meet the criteria
for involuntary placement, a petition can be filed to further detain them for
treatment. This isn’t unusual in that Florida has many people visiting from other
countries, both legally and illegally. If the person is a foreign national with
citizenship in another country (even if with dual citizenship in the U.S.), you need
to remember your obligations for consular notification and access.
Regarding medications, if certified by a physician as able to make well-reasoned,

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
194
willful, and knowing decisions about his/her treatment, the person can consent or
refuse consent to treatment. If the person is not competent and is without a duly
executed advance directive, a relative or close personal friend can be designated as
a health care proxy until a guardian advocate is appointed by the court. Otherwise,
an emergency treatment order can be used if the physician has documented
imminent danger.
B. Initiation and Filing of Involuntary Inpatient Placement
We have a patient admitted on a voluntary basis and her MD changed her
status to involuntary. We filed the petition for placement within two working
days. Do we also have to complete a professional certificate?
No professional certificate is necessary in the circumstance you describe. The
statute refers to the certificate, a law enforcement officer’s report, or a court’s ex
parte order only as the methods to have a person taken into custody and delivered
to a receiving facility. Once in a receiving facility, none of these documents are
needed. You would just file the petition for involuntary placement within the two
working days as you described.
A BA-32 has been filed on a veteran for private placement. Mental health
providers are now seeking state placement and a court date has been
scheduled. What is the process required to amend the petition for state
placement in lieu of private placement?
The clerk of court can advise about the court’s procedures. There isn’t any
restriction in the rule about filing an amended petition; however, prior to the
hearing a transfer evaluation must be completed. One of the criteria for involuntary
inpatient placement is that “[a]ll available less restrictive treatment alternatives that
would offer an opportunity for improvement of his or her condition have been
judged to be inappropriate.” § 394.467(1)(b), Fla. Stat. The Florida Legislature
enacted provisions in the Baker Act requiring confirmation of the sworn statements
of experts testifying in involuntary inpatient placement hearings as to the
availability and appropriateness of less restrictive community alternatives. The
Baker Act also specifies in section 394.461(2), Florida Statutes, which governs the
designation of receiving and treatment facilities, that “[a] civil patient shall not be
admitted to a state treatment facility without previously undergoing a transfer
evaluation. Before a court hearing for involuntary placement in a state treatment
facility, the court shall receive and consider the information documented in the
transfer evaluation.”

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
195
I’m an assistant public defender. We have filed motions to dismiss Baker Act
petitions as legally insufficient when the first and/or second opinion doesn’t
contain sufficient facts/observations to support the conclusion that a patient
meets Baker Act criteria. While observations may support the conclusion that
the patient has a mental illness, they don’t support the conclusion that the
patient meets the Baker Act criteria. While we have no case law on this issue,
we are citing Fla. Admin. Code R. 65E-5.290(2), which states that “Each
criterion alleged must be supported by evidence.” We believe this refers to the
petition. Since Florida courts have consistently held that a Baker Act
commitment is a massive curtailment of a person’s liberty interest,
psychiatrists must sufficiently support their conclusion with facts/observations
that a patient meets Baker Act criteria, and failure to do so warrants
dismissal of the petition and release of the patient. Some facilities have tried to
remedy this situation by filing addendums to the Baker Act petitions. We
believe that there is no legal authority for this. Any thoughts or
recommendations?
Unless the evidence elicited at the hearing reaches a “clear and convincing” level
on each of the involuntary placement criteria, the court has no choice but to
dismiss the petition. A definition of clear and convincing evidence provided by the
Florida Supreme Court is “evidence that is precise, explicit, lacking in confusion,
and of such weight that it produces in your mind a firm belief or conviction,
without hesitation, about the matter in issue.” Fla. Stand. Jury Instr. (Civil) 405.4.
The statutes, rules, and cases require a “clear and convincing” showing for the
court to order placement. There is no indication that this also applies to the
opinions in the petition, which is a separate filing with the court and for which
evidence must be elicited at the hearing. While it’s up to the court to make a
determination as to what is sufficient, Florida appellate courts have done this many
times; they have reversed court orders for placement on sufficiency of evidence.
Appellate cases have found that expert opinions and conclusions of physicians
testifying at hearings aren’t sufficient without testimony of witnesses to facts. This
is why inclusion of a list of witnesses who will testify to facts supporting the
petition for involuntary placement is essential. Often staff fail to include these fact
witnesses in this section of the petition, and insufficient testimony is elicited by the
state attorney at the hearing. While the psychiatrist as an expert witness will render
opinions and conclusions, the facilities should also identify these fact witnesses to
support the opinions of the psychiatrist.
The Supreme Court Commission on Fairness did look at this issue. In its 1999

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
196
Report and Recommendations of the Subcommittee on Case Administration, it
recommended that the assistant state attorney review any such petition for
sufficiency. Pages 70–71 of that report have the following content (emphasis
added):
Issue:
What is the appropriate role of the state attorney’s office in
involuntary placement proceedings?
Discussion:
According to section 394.467(6)(a), Florida Statutes, “[t]he
state attorney for the circuit in which the patient is located shall
represent the state, rather than the petitioning facility administrator, as
the real party in interest in the proceeding.” It is important to
remember that while the facility is the petitioner, the state is the real
party of interest and must prosecute the petition.
The state is the only entity with the authority to restrict a
person’s liberty. In an adversarial proceeding, the state attorney is
required to meet a burden of proof for involuntary placement. The
state attorney should gather information independently, and evaluate
and confirm the information contained in the petitions. In involuntary
placement proceedings, the state has the responsibility to present
evidence and testimony as to the elements and requirements of the
applicable statutes.
As discussed previously in this report, participation by the state
attorney’s office is an integral part of the proceeding. In Jones v.
State, 611 So. 2d 577 (Fla. 1st DCA 1992), the court found that “in
the instant case, it appears the absence of the state was a contributing
factor in the due process deficiencies attendant upon the proceeding.”
Thus, the role of the state attorney is critical to the process. It is
incumbent upon the state attorney to vigorously investigate and
prosecute the petition, just as the public defender must protect the
patient’s rights and represent the patient’s expressed desires. Further,
if the state attorney’s independent review does not show the
statutory criteria are provable, then the state attorney should
withdraw the petition.
* * *

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
197
Recommendation
The Subcommittee recommends that:
a. Each state attorney’s office should independently evaluate and
confirm the allegations set forth in the petition for involuntary
placement. If the information is found to be correct, the state
attorney should vigorously prosecute the petition. If the
allegations are not substantiated, the state attorney should
withdraw the petition.
b. Assistant state attorneys representing the state in involuntary
placement proceedings must be bound to the same legal and
ethical obligations of assistant state attorneys prosecuting other
cases.
c. The bar should be educated as to attorneys’ roles and
responsibilities in handling involuntary placement proceedings.
d. The Florida Legislature should direct and fund an
interdisciplinary study on whether state attorneys should be
authorized to have access to clinical records, facility staff, and
other pertinent information.
If the assistant state attorney believes the petition is sufficient, the court should
hear it and either dismiss it if found to be insufficient or grant it if evidence raised
at the time of the hearing clearly met the clear and convincing standard. It’s clear
that the ASA has this authority; however, it isn’t as clear that the defense attorney
has the same authority. If the petition is patently insufficient, the patient or his/her
attorney could file a habeas petition for release from the facility.
Is it legal for the second opinion on a BA-32 to be dated and timed prior to the
first opinion, or must the first opinion be documented on the petition itself to
properly trigger a request for the second opinion? Being able to do the
opinions “out of order” would make the physicians’ lives easier.
There isn’t any prohibition against a psychiatrist “ordering” an initiation for
involuntary placement and completing the document later as long as he/she has
personally examined the patient face-to-face prior to such an order or signing the
petition form. However, it is unclear what is achieved by such an “order” — the
two expert examinations and documentation of these opinions on the petition form,
along with the administrator’s signature and filing of the petition with the clerk of

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
198
court, must all be done within 72 hours of the patient’s arrival at the facility
(perhaps even earlier if the patient had waited at a medical hospital for transfer
before arrival at the facility).
It is unclear why a second opinion would ever be conducted before a first opinion.
The petition form elicits more extensive input from the psychiatrist conducting the
first opinion, and the second opinion shouldn’t differ from the first. The
psychiatrist or psychologist providing the second opinion is simply concurring
with the first. Either of the psychiatrists is authorized to testify at the patient’s
hearing. § 394.467(6)(a)3., Fla. Stat.
A petition for involuntary inpatient placement was completed this morning
and the patient immediately rescinded her request for release. I haven’t even
completed the remaining documents necessary to file the petition with the
court. The doctor authorized her to sign consent and she did. What do I now
do with this petition? Just keep it in my files?
The patient appears to have been on involuntary status in order for the first and
second opinions to have been completed. She had no right to request release if on
involuntary status — this right applies only to persons on voluntary status.
However, if she requested to transfer from involuntary to voluntary status, the
following would have to be done:
She would sign an application for voluntary admission.
A physician or psychologist would document the completion of the initial
mandatory involuntary examination as required in rule 65E-5.280(1), Florida
Administrative Code.
A physician would sign form CF-MH 3104 certifying the patient’s sustained
ability to make well-reasoned, willful, and knowing decisions about her
medical, mental health, and substance abuse treatment. This means she has
the capacity and right to consent or refuse consent to treatment.
If it had just been certified by two psychiatrists that morning that she met the
criteria for involuntary inpatient placement, it takes more than just her statement
that she is willing to “rescind her right to release.” The psychiatrist should indicate
how her condition had changed over that short a period of time. If such an
improvement of condition is documented, the signed petition must remain in the
person’s chart as it pertains to physician documentation of meeting criteria at a
point in time of her hospitalization — it cannot be kept in any other place or

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
199
destroyed just because it isn’t actually filed with the court.
Can the second opinion be done by a psychiatrist who is in the same practice
as the psychiatrist who does the first opinion?
Yes. There is no prohibition on two authorized professionals in the same practice
from signing the two opinions required for an involuntary placement petition. As
long as each professional exercises independent judgment and the opinions are in
compliance with the criteria specified in the Baker Act, there isn’t a problem.
Can a psychiatric ARNP do a second opinion for involuntary placement, or
must it be a psychiatrist or psychologist?
Only a psychologist or second psychiatrist can provide the second opinion. The
only exception is that under section 394.467(2), Florida Statutes, the receiving
facility administrator may certify that no psychiatrist or psychologist is available to
provide a second opinion, and may obtain a second opinion from a licensed
physician with postgraduate training and experience in diagnosis and treatment of
mental illness, or by a psychiatric nurse as defined in section 394.455(23), Florida
Statutes. Many nurse practitioners, even those working in the psychiatric field,
don’t meet the specific Baker Act definition of “psychiatric nurse.”
If a person on voluntary status in a CSU subsequently was adjudicated
incapacitated by the court, must the CSU file a petition for involuntary
placement?
Yes. The Baker Act is very specific on this issue. Section 394.4625(1)(d), Florida
Statutes, states:
A facility may not admit as a voluntary patient a person who has been
adjudicated incapacitated, unless the condition of incapacity has been
judicially removed. If a facility admits as a voluntary patient a person
who is later determined to have been adjudicated incapacitated, and
the condition of incapacity had not been removed by the time of the
admission, the facility must either discharge the patient or transfer the
patient to involuntary status.
If a person on an involuntary inpatient placement petition requires admission
to a medical facility for emergency medical treatment, is the petition put on
medical hold, or does the petition become void upon discharge of the patient
from the psychiatric facility?

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
200
The only timeframe that is put on hold because of an emergency medical condition
is the BA-52 involuntary examination. If a person is on a BA-32 involuntary
placement petition or a BA-8 involuntary placement order, the Baker Act doesn’t
permit any variation to the statutorily prescribed time frames. However, if at any
time the person no longer meets the criteria for involuntary placement, the
administrator has a duty to either convert the person to voluntary (if the person is
competent and willing) or release the person. If the person continues to meet the
criteria for involuntary placement, he/she can’t be “discharged.” The person would
be “transferred” instead in order that the legal status and guardian advocate (if any)
are retained. The person could then be transferred back upon stabilization with all
the legal issues intact. While some type of back office administrative or financial
discharge would occur, to avoid having two bills for the same day of care, the
clinical record should reflect a “transfer” for medical purposes rather than a
“discharge.”
What should be done when a person is awaiting a hearing on involuntary
inpatient placement and the physician writes orders for the person to be
discharged? When the family refused to take the person back, the physician
cancelled the discharge order. Would the current BA-32 be nullified because
of the order for discharge and another petition have to be filed?
If the physician documented that the person didn’t meet criteria for involuntary
inpatient or outpatient placement as a prerequisite for the discharge order, the
facility couldn’t go forward on an existing petition and couldn’t file a new petition
unless the person’s condition had deteriorated after the discharge order was
written. If the person is willing to apply for voluntary status and the physician has
certified the person can make well-reasoned, willful, and knowing decisions about
his or her medical, mental health, or substance abuse treatment, such a transfer to
voluntary status can be done. If the person doesn’t meet the criteria for involuntary
status and is unwilling or unable to consent to voluntary status, the Baker Act
requires that the person be discharged. In that case, your discharge planners should
investigate alternate discharge plans other than the family.
Once a petition for involuntary placement has been filed by a receiving
facility, can that facility withdraw the petition when it transfers a patient to
another psychiatric facility and then immediately Baker Act the patient to
cover the legal status during transport to another treatment facility? The
patient is not returning to the original sending facility. We have one physician
provide all of our expert testimony in court. We don’t want to risk having an
acutely ill patient discharged because of a coordination problem that may
occur with inviting a physician from another facility to testify at a hearing at

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
201
our facility. In addition, we don’t want to assume liability for another
facility’s 32 petition if it is out of compliance with the Baker Act law.
It would not be appropriate to withdraw the petition, once filed with the court, and
start over with a new BA-52. This would result in the person being held longer
than permitted under the law for involuntary examination. Such a deprivation of
liberty would likely be frowned upon by the defense attorney once the person went
to court. The practice around the state is that the transfer should occur prior to
filing the petition or after the court hearing has taken place. That ensures that the
person’s due process rights are observed.
A receiving facility only has the power to discharge or release a person when a
psychiatrist, psychologist, ER physician, or psychiatric nurse (as defined in the
Baker Act) has determined the person doesn’t meet the criteria for involuntary
inpatient placement or involuntary outpatient services. Other than that, only a
transfer between receiving facilities is permissible as provided in section 394.4685,
Florida Statutes. A “transfer” maintains the legal status of the person.
The only alternative is if one of the two experts who signed the petition is willing
to attend the hearing at the second facility to provide the legally required
testimony. The attending psychiatrist at the second facility could provide
supplemental testimony to that provided by one of the two signing experts as to the
person’s condition since arrival at the second facility. It is actually the duty of the
assistant state attorney, as the real party in interest, to determine the legal
sufficiency of each petition. If not sufficient, the petition should be withdrawn by
the state attorney.
A magistrate for this judicial circuit called and said that the hospital has had
a number of late-filed petitions recently, resulting in dismissals. The hospital
has then refiled the petitions, resulting in persons being detained beyond the
period permitted by law. What should be done?
The only recourse is for the patients to file petitions for writs of habeas corpus.
However, the public defender could call the hospital administrator and the
hospital’s attorney to advise them of this. It is possible that the hospital
administration doesn’t even know a problem exists and will ensure that it gets
fixed immediately. If immediate corrective action doesn’t take place, a report to
DCF and AHCA should be made.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
202
C. Public Defender and State Attorney
What are the roles of the public defender and state attorney who conduct the
Baker Act hearings?
The Baker Act involuntary inpatient placement statute, section 394.467, Florida
Statutes, provides as follows:
(4) Appointment of counsel.--Within 1 court working day after the filing
of a petition for involuntary inpatient placement, the court shall appoint the
public defender to represent the person who is the subject of the petition,
unless the person is otherwise represented by counsel. The clerk of the court
shall immediately notify the public defender of such appointment. Any
attorney representing the patient shall have access to the patient, witnesses,
and records relevant to the presentation of the patient’s case and shall
represent the interests of the patient, regardless of the source of payment to
the attorney.
* * *
(6) Hearing on involuntary inpatient placement.--
(a)1. . . . . The state attorney for the circuit in which the patient is located
shall represent the state, rather than the petitioning facility administrator, as
the real party in interest in the proceeding.
The Supreme Court Commission on Fairness, in its 1999 report, indicated that the
state attorney and public defender have the same obligation to their Baker Act
clients as they do in any other form of legal representation.
The court in Handley v. Dennis, 642 So. 2d 115, 116–117 (Fla. 1st DCA 1994),
said the following about the role of the public defender:
[T]he duty of the Public Defender is a legal and professional duty that is
owed to the patient as a client. The Public Defender serves as an
independent advocate for the patient, not as a neutral party charged with the
responsibility of determining the best interests of the patient or the needs of
society. . . . If the patient wishes to be released or transferred and if there is a
basis for that request, the Public Defender has a duty to advocate the cause
of the patient.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
203
There are a number of appellate cases that relate to the notification and
participation of the state attorney in Baker Act hearings. One Sixth Circuit court
order (not appealed) defined the role of the state attorney. In In re [V.S.], No. 95-
577-IN 003 (Fla. 6th Cir. Ct. Feb. 13, 1995), the court held that
the facility has every right to employ legal counsel to represent their
legal interests in any proceeding where the facility’s legal rights,
liabilities or corporate interests are implicated.
Since future actions of the facility, either in providing ordered
treatment, or arranging for discharge of the patient, are predicated on
the outcome of the hearing, the facility is entitled to have counsel
present during the adjudicatory process. Counsel for the facility,
although present at the hearing, may not interpose evidentiary
objections or participate in questioning witnesses. This is the assigned
role of the state attorney. While the facility may be a party in interest
for the purpose of placing the controversy before the court, they do
not have a legally protectable interest in the outcome of an
adjudication of the need for involuntary mental health treatment. The
statute permits the facility administrator to throw out the first ball, but
the constitutional rights of the patient require that the state attorney
pitch the game.
In preparing for a Baker Act hearing, would the PD be correct in asserting/
demanding that he/she has the right to interview a Florida Assertive
Community Treatment (FACT) team leader prior to the hearing who serves
the client who has a court hearing for involuntary placement? I had
understood that the FACT team leader would actually be a witness for the
state attorney, and if the PD wanted to interview, he or she would have to do a
deposition or just question the team leader during the hearing. Other than the
CSU record, would the PD have a right to review the FACT record (different
provider) and require that the FACT team bring it to the PD’s office? Would
this only be able to happen via court order? This particular PD does not allow
anyone in the hearing room except the person who is testifying (and of course
the magistrate and client) and has also been known to question team leaders
for over an hour, and in some instances the hearings have run all day. What
responsibility does the state attorney’s office have in sending an informed SA
to these hearings to represent the interests of the state and be able to challenge
certain unfair practices of the PD?
The Baker Act is very explicit about the public defender’s right to access the

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
204
patient, medical records, and any witnesses in defending a client in Baker Act
proceedings. In terms of the receiving facility’s record, the confidentiality section
of the law states:
394.4615. Clinical records; confidentiality
(2) The clinical record shall be released when:
* * *
(b) The patient is represented by counsel and the records are needed by
the patient’s counsel for adequate representation.
Section 394.455(6), Florida Statutes, defines “clinical record” as “all parts of the
record required to be maintained and includes all medical records, progress notes,
charts, and admission and discharge data, and all other information recorded by
facility staff which pertains to the patient’s hospitalization or treatment” (emphasis
added).
It is unlikely that this definition would include medical records of the client other
than those at the receiving facility. However, the patient always has the right to
authorize release of his/her records at any facility unless adjudicated incapacitated
and a guardian has been appointed by the court. In such cases, if the guardian
didn’t release the records, a good cause hearing could be conducted by the court in
order to provide the records or any part of the records to the public defender in
preparation for hearing. There isn’t a requirement that you take these FACT
records off site for the convenience of the public defender unless ordered to do so
by the court.
In the involuntary inpatient placement provisions, the law extends beyond the
public defender just accessing the records to accessing his/her client and any
witnesses in the proceedings:
394.467. Involuntary inpatient placement (emphasis added)
(4) Appointment of counsel.--Within 1 court working day after the filing
of a petition for involuntary inpatient placement, the court shall appoint the
public defender to represent the person who is the subject of the petition,
unless the person is otherwise represented by counsel. The clerk of the court
shall immediately notify the public defender of such appointment. Any
attorney representing the patient shall have access to the patient,
witnesses, and records relevant to the presentation of the patient’s case

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
205
and shall represent the interests of the patient, regardless of the source
of payment to the attorney.
As of the end of the 2016 legislative session, the assistant state attorney as the “real
party in interest” doesn’t have the same access to the records and to the witnesses
in preparation for the Baker Act hearing and usually has to wait until the hearing to
access these resources. It is the responsibility of the petitioning facility to list the
names of all potential witnesses for the state in the petition form.
It would be very rare for a witness to require a subpoena to provide testimony for
the state or for the defense in a Baker Act hearing. The exclusionary rule is usually
invoked to prevent a witness from hearing the testimony of any other witness.
Due to the liberty interests of the patient, the courts would uphold whatever length
of time was needed for the state attorney to elicit material and relevant testimony
to support continued detention as well as for the defense attorney to challenge that
testimony through cross-examination as well as presenting any defense witnesses.
These hearings are intended to be adversarial in the best sense of the term — not a
clinical staff meeting to determine the best interests of the patient. There is a
plethora of appellate cases in which dozens of orders for involuntary inpatient
placement were reversed on procedural or evidentiary grounds. The magistrate and
circuit court judge would surely prefer to minimize the number of appeals and
reversals.
The role of the public defender in a Baker Act hearing was defined by the First
District Court of Appeal in Handley v. Dennis, 642 So. 2d 115, 116–117 (Fla. 1st
DCA 1994). The court stated:
The duty of the public defender is a legal and professional duty that is owed
to the patient as a client.
“The public defender serves as an independent advocate for the patient, not
as a neutral party charged with the responsibility of determining the best
interests of the patient or the needs of society.”
If the patient wants to be released or transferred and there is a basis for the
request, the public defender has a duty to advocate the cause of the patient.
The Florida Supreme Court Commission on Fairness, in its 1999 report, concluded
that the duty of the state attorney and the public defender was the same in a Baker
Act proceeding as in any other representation. Failure to uphold this legal and
ethical duty by the attorneys could subject them to disciplinary action by The

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
206
Florida Bar.
It is beneficial for assistant state attorneys to be as well trained in Baker Act
matters, and remain in the role long enough to provide equal representation to the
state, as public defenders do for their clients. See p. 69 of the 1999 report.
What is the role of the state attorney in an involuntary placement hearing?
The state attorney’s role is to represent the state, rather than the petitioning facility,
as the real party in interest in the proceeding. The Florida Supreme Court
Commission on Fairness stated that each state attorney should place a high priority
on involuntary placement proceedings and properly prepare the cases on behalf of
the state:
Each state attorney’s office should independently evaluate and
confirm the allegations set forth in the petition for involuntary
placement. If the information is found to be correct, the state attorney
should vigorously prosecute the petition. If the allegations are not
substantiated, the state attorney should withdraw the petition.
. . . . Assistant state attorneys representing the state in involuntary
placement proceedings must be bound to the same legal and ethical
obligations of assistant state attorneys prosecuting other cases.
Florida Supreme Court Commission on Fairness 1999 report, p. 69. The
Commission further stated the state attorney’s office must be represented at and
actively participate in every hearing. “If a representative of the state attorney’s
office is not present at the hearing, the court should halt the proceeding while the
state attorney is summoned.” See p. 68 of the 1999 report.
Can you explain more about the role of assistant state attorneys in preparing
and presenting Baker Act cases at involuntary placement hearings?
An excellent document titled “Preparation & Presentation of Baker Act Hearings
by Assistant State Attorneys” has been prepared by Mari S. Blumstein, Assistant
State Attorney, Office of the State Attorney, Seventeenth Judicial Circuit, 201 SE
Sixth Street, Ft. Lauderdale, FL 33301, (954) 831-7633.
Recently, staff at the state attorney’s office stated they felt “unsafe” when
doing hearings at the receiving facility. We have a dedicated room for the
hearings and have never had this problem before. I agreed to have an
additional mental health technician sit directly behind the clients while in

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
207
hearing. Subsequently, the state attorney’s office sent us letter stating they
will “cease” all BA hearings at the facility unless we can change the venue. I
have read the statute and find very little regarding this issue. Can you shed
some light, as having to bring our clients to the county courthouse would be
most traumatic?
This reason being given for an assistant state attorney to not attend a hearing may
be unique. If it is safe enough for the magistrate, public defender, and staff,
especially with the addition of another well-trained staff person, it’s difficult to
believe that safety should be an issue. The Baker Act addresses the location of the
hearing in the following provision:
394.467. Involuntary inpatient placement
(6) Hearing on involuntary inpatient placement.--
(a)1. The court shall hold the hearing on involuntary inpatient placement
within 5 court working days, unless a continuance is granted.
2. Except for good cause documented in the court file, the hearing must
be held in the county of the facility, as appropriate, where the patient is
located, must be as convenient to the patient as is consistent with orderly
procedure, and shall be conducted in physical settings not likely to be
injurious to the patient’s condition. . . .
While historically Baker Act hearings were held at courthouses, nearly all courts
conduct the hearings at the receiving facilities where the patient is held. The safety
of the patient in transporting is a very real concern as is the privacy and dignity of
moving such a person in the most acute phases of his/her illness through public
places. Providing for the personal care of the patient in a courthouse is also
incredibly difficult.
In addition, there have been some appellate decisions, such as Wickland v. State,
642 So. 2d 670 (Fla. 1st DCA 1994). In Wickland the court held that the trial court
failed to comply with the Baker Act when it did not serve notice of an involuntary
placement hearing on the state attorney, the state attorney did not appear at the
hearing, the state’s psychiatrist testified without asserting personal knowledge of
the underlying facts of the case, and the trial court’s order of involuntary
placement for treatment quoted verbatim from the petition. The court reversed the
trial court’s order of involuntary placement for treatment under the Baker Act.
Finally, the Florida Supreme Court Commission on Fairness, on pp. 29–32 of the

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
208
1999 report, had much to say about the venue of such hearings:
Issue:
Should involuntary placement hearings be conducted in the
courthouse or at the mental health facility? If the hearings are held in
the facilities, are measures being taken to ensure that the patients
understand the seriousness of the proceeding?
. . . . A balanced approach may be the most desirable resolution of this
issue. The receiving facility may be the location that is both the most
convenient to the patient and the safest. However, all involuntary
placement hearings held in receiving facilities should include
formalities consistent with a court hearing, to ensure that everyone
understands the seriousness of the proceeding. When liberty interests
are at stake, they should be addressed in a formal and appropriate
manner. Food, drink, and side conversations at hearings, coupled with
lax observance of procedures and rules of evidence, give the
appearance that the system is trivializing involuntary placement
cases. . . . .
Recommendation
The Subcommittee recommends that the chief judge of each
circuit court require involuntary placement hearings held at
mental health receiving facilities to be conducted in a room that is
set up in the manner of a courtroom. If possible, that room should
not be used for any other patient purposes. The presiding officer
should wear a robe. United States and Florida flags should be
present. Formal courtroom decorum should be observed. Patients
should be dressed in street clothing. Food, drink, and side
conversations should be prohibited. The presiding officer, state
attorney, public defender, and other participants should
introduce themselves prior to each case. Moreover, rules of
evidence and procedure should be observed.
Issue:
Should involuntary placement hearings be conducted by video?
Discussion:

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
209
Some court proceedings are conducted by video. An example is
video arraignments, in which the judge remains at the courthouse
while the defendant participates by live video link-up from the jail. At
the November 12, 1998, meeting it was suggested that video hearings
may be a convenient and less costly alternative for involuntary
placement hearings. One of the judges who responded to the survey
observed that allowing patients to attend hearings by video would
alleviate the need for them to be transported to the courthouse. . . .
Recommendation
The Subcommittee strongly recommends against the use of video
for involuntary placement hearings.
[Editor’s note: In Doe v. State, __ So. 3d __ (2016), 2016 WL
5407617 (Fla. 2d DCA 2016), the Second District Court of Appeal
rejected a challenge to an announcement in Lee County that judges
and magistrates would no longer travel to receiving facilities to hold
Baker Act hearings but would preside remotely from the courthouse
by videoconference. However, the court certified to the Florida
Supreme Court the following question: “DOES A JUDICIAL
OFFICER HAVE AN EXISTING INDISPUTABLE LEGAL DUTY TO
PRESIDE OVER SECTION 394.467 HEARINGS IN PERSON?” The
Supreme Court accepted jurisdiction, and oral argument is scheduled
for February 7, 2017.]
The Commission also had the following to say about assistant state attorneys in
such hearings, on pp. 67–68 of the 1999 report:
The state is the only entity with the authority to restrict a
person’s liberty. Involuntary mental health examination and
placement involve a balancing of individual rights with the state’s
parens patriae authority and police power. Under Florida law,
involuntary placement is clearly a state action; therefore, the facility
and its attorneys have no authority to prosecute the petition.
Nevertheless, the Subcommittee repeatedly heard that in some
jurisdictions the state attorney’s office never participates in
involuntary placement proceedings. It was further reported that at
some hearings the facility’s attorney appears to prosecute the petition.
It was even reported that in some instances the court takes on the
prosecutorial role, because the state attorney is not available.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
210
Active participation by the state attorney’s office is an integral
part of the proceeding. . . . The Subcommittee finds that the office of
the state attorney must be present at every involuntary placement
proceeding in order to comply with the statutory mandate and to
appropriately, adequately, and competently represent the state’s
interests.
. . . . [T]he state attorney is not represented at more than 10
percent of the involuntary placement proceedings.
Recommendation
The Subcommittee recommends that:
a. Each state attorney should ensure that an assistant state attorney
is present at every involuntary placement hearing.
b. The court should require the presence of the state attorney’s
office at every involuntary placement hearing. If a representative
of the state attorney’s office is not present at the hearing, the
court should halt the hearing while the state attorney is
summoned to immediately appear before the court.
Regarding preparation and presentation of cases by the state attorneys’ offices, the
Commission stated on pp. 72–73 of the 1999 report:
Regrettably, it appears they generally take little action to
prepare these cases.
The Subcommittee heard testimony about instances where
individuals who were believed to be dangerous were discharged
because the state attorney did not subpoena witnesses and conduct
other pre-trial preparations necessary to sustain the petition. The court
was left with no alternative but to dismiss the petition and discharge
the patient. This conduct may place the public’s safety at risk.
Meanwhile, the individuals do not receive necessary treatment. . . .
* * *
Recommendation
The Subcommittee recommends that:

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
211
a. The Florida Legislature should provide adequate resources
to enable state attorneys to provide quality representation
for the state in involuntary placement proceedings.
b. Each state attorney should place a high priority on
involuntary placement proceedings and properly prepare
the cases on behalf of the state.
c. Each state attorney should ensure that experienced and
trained attorneys are assigned to involuntary placement
cases.
d. The Florida Legislature should direct and fund an
interdisciplinary study on whether state attorneys should be
authorized to have access to clinical records, facility staff,
and other pertinent information.
The Subcommittee made recommendations for the Legislature and state
attorneys to improve the quality of representation for the state.
On pp. 70–71 of the 1999 report, the Commission stated:
The state attorney should gather information independently, and
evaluate and confirm the information contained in the petitions. It is
incumbent upon the state attorney to vigorously investigate and
prosecute the petition.
. . . . Further, if the state attorney’s independent review does not show
the statutory criteria are provable, then the state attorney should
withdraw the petition.
Chapter 394 specifically authorizes the attorney representing
the patient to have access to the clinical record, facility staff, and other
pertinent information. However, the law is silent as to whether the
state attorney has the authority to access the same information. Thus,
a study should be conducted on whether the law should be amended to
allow the state attorney access [to] this information in order to
evaluate the petition and prepare for the hearing.
Recommendation
The Subcommittee recommends that:

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
212
a. Each state attorney’s office should independently evaluate
and confirm the allegations set forth in the petition for
involuntary placement. If the information is found to be
correct, the state attorney should vigorously prosecute the
petition. If the allegations are not substantiated, the state
attorney should withdraw the petition.
b. Assistant state attorneys representing the state in
involuntary placement proceedings must be bound to the
same legal and ethical obligations of assistant state
attorneys prosecuting other cases.
c. The bar should be educated as to attorneys’ roles and
responsibilities in handling involuntary placement
proceedings.
d. The Florida Legislature should direct and fund an
interdisciplinary study on whether state attorneys should be
authorized to have access to clinical records, facility staff,
and other pertinent information.
While the Supreme Court Commission’s recommendations have, for the most part,
not been enacted by the Legislature, they should be persuasive in improving the
administration of justice by Florida courts.
What specific language in chapter 394 requires the state attorney to represent/
make the case for involuntary commitment?
There is no reference in chapter 394, Florida Statutes, for the state attorney’s
participation in continued involuntary inpatient placement or involuntary
outpatient services hearings (it is only mentioned with regard to the initial
hearings); nor is there specific reference to it in chapter 27. The public defender’s
role is specified in chapter 394 (initial and continued hearings) as well as chapter
27.
However, section 394.467(1), Florida Statutes, requires in the continued hearings
that there be clear and convincing evidence that all criteria for involuntary
inpatient placement continue to be met. Some attorneys question how this evidence
will get into the record if not by the state attorney. This may be of particular
concern when a state hospital has been privatized and the “state” isn’t present to
determine sufficiency of the petition or be concerned with the deprivation of a
person’s liberty as it would be in other such cases.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
213
Can the public defender and state attorney access the clinical record?
The public defender can access the clinical record, the person, and the staff in
preparing for the involuntary placement hearing. The law doesn’t expressly permit
this same access to the state attorney prior to a hearing for involuntary inpatient
placement (it is expressly permitted for involuntary outpatient services). In some
circuits the state attorney has access. In any case, the clinical record is always
available at the time of the hearing and is, at that time, available to the state
attorney.
D. Independent Expert Examination
Who is responsible for paying the independent expert examiner under section
394.467(6)(a), Florida Statutes? I know the court is responsible for providing
such an expert, but didn’t know if this equates to the court paying for one.
What specific authority has addressed the responsibility of the court paying
for the expert?
A memorandum was sent to the chief judges from Judge Stan R. Morris, then-chair
of the Trial Court Budget Commission, dated August 3, 2005. The paragraph in
question is on page two of the memorandum, which states the following:
More problematic are Baker Act evaluations under section
394.467(6)(a)1, Florida Statutes. In Baker Act situations, the patient
has the statutory right to request an independent expert evaluation.
This right arises after a professional has executed an involuntary
inpatient placement certificate and the involuntary commitment
process has started. The statute says: “If the patient cannot afford such
an examination, the court shall provide for one.” Thus, the statute
clearly evidences legislative intent that if the person is not indigent,
this cost is not paid by the public. However, when the person is
indigent, section 394.473, Florida Statutes, states that the expert
should be paid pursuant to section 27.5304, Florida Statutes. That
section provides for payment by the Justice Administrative
Commission. As a person subject to Baker Act commitment, the
patient has the right to the appointment of the public defender or
court-appointed counsel if indigent. Both section 29.006, Florida
Statutes, (public defender) and section 29.007, Florida Statutes,
(court-appointed counsel) specifically reference mental health
professionals appointed pursuant to section 394.473, Florida Statutes.
Clearly these witnesses are defense witnesses; they are appointed only

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
214
if requested by the patient and any report issued is confidential and
not discoverable. See: section 394.467(6)(a)2, Florida Statutes. The
language found in section 394.467(6)(a)2, Florida Statutes, {“the
court shall provide for one”} does not transform what is essentially a
defense witness into a state court expense when there is clear statutory
guidance to the contrary.
E. Continuances
The public defender in our circuit automatically continues almost all cases,
often two or three times. According to the CSU, the PD doesn’t see or talk to
the patient prior to requesting a continuance. We believe this may be adding
to our capacity issues, because when folks finally get court ordered to the state
hospital, they often have to wait an additional four to six weeks for admission,
meaning they are on the units for several months (following the above-
mentioned continuances). There are often legitimate reasons for continuance,
but this seems excessive. How can we address this with the PD?
Actually, only the patient has the standing to request a continuance — with
concurrence of counsel. No one else has such a right. There has been some
criticism of defense counsel making such requests for continuances unless
consistent with the client’s wishes.
The law requires the hearing to take place within five days, unless a continuance is
requested by the patient. This is the equivalent of a speedy trial in a criminal
setting, and a deprivation of the person’s liberty is at stake if the hearing is
delayed. The court in Handley v. Dennis, 642 So. 2d 115, 117 (Fla. 1st DCA
1994), clearly stated that the role of the public defender is to serve “as an
independent advocate for the patient, not as a neutral party charged with the
responsibility of determining the best interests of the patient or the needs of
society.” The attorney is the voice of the patient when the patient’s lack of capacity
makes him/her unable to speak for himself/herself.
While some defense attorneys take the position that they can act for their clients
without the client’s agreement for purposes of trial strategy, the language of the
law clearly indicates that the “patient” is the one with standing to request such a
continuance — with the concurrence of counsel. The Florida Supreme Court
Commission on Fairness emphasized that only the patient has the power to do this.
The Commission also indicated that an attorney’s duty to a Baker Act client is the
same as in any other type of case.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
215
The Commission also strongly recommended that whenever a continuance of a
hearing on involuntary placement is considered, the court should proceed with a
hearing to consider the person’s competence to consent to treatment and the
appointment of a guardian advocate if the person is found to be incompetent. The
actual placement hearing would then take place at a later time.
One public defender often makes such requests to avoid a hearing in which a
commitment to a state hospital might result, believing that another week or two of
treatment might result in improved clinical condition. He states that he always talks
to his clients before filing such a request for a continuance and lets the client know
of the benefit of a delay. However, he says that if his client still wants his/her “day
in court,” they go forward with the hearing as scheduled. If the court conducts a
hearing to appoint a guardian advocate, this might relieve part of the problem in
some situations.
You may want to talk with the PD in your circuit first to find out the reason for
routine continuances. While the PD’s sole priority must be representing the client’s
wishes, the PD may not know that this practice is an anomaly. The PD also may
not know that routine use of continuances results in serious service system issues
for others who might need acute care examination or treatment. If this doesn’t
work, you might have to talk with a supervisor.
If it appears that any of individuals who are detained past the five working days
following petition filing are unhappy about the delay in hearing, this needs to be
brought to The Florida Bar’s grievance process. This delay could potentially result
in an unwarranted deprivation of liberty without due process. You might want to
speak with the circuit DCF legal counsel about the situation. The patient could also
file a petition for a writ of habeas corpus with the court.
Can the receiving facility or a doctor testifying at an involuntary placement
hearing request a continuance?
No. Only the person is entitled, with the concurrence of counsel, to request a
continuance. The Florida Supreme Court Commission on Fairness urges courts,
when considering a motion for continuance, to “conduct a hearing and make a
finding as to the [person’s] capacity to consent to treatment if there is a pending
request. If the court finds that the capacity to consent to treatment is lacking, a
guardian advocate should be appointed at the time the involuntary placement
hearing is continued.” P. 49 of the 1999 report.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
216
F. Transfers for Medical Care
I’m a Baker Act magistrate. I recently found a person to meet Baker Act
criteria and entered a recommended order for her involuntary placement in a
state mental health facility. The circuit judge entered his order accepting the
recommendation the next day. The receiving facility (a general hospital)
became concerned over the patient’s heart rhythms and admitted her to the
med/surg unit of the hospital. There’s a notice of release or discharge in the
file. The receiving facility regards the above as a discharge, so it has filed a
new petition for involuntary placement. This new petition shows up on my
docket for tomorrow. Was the receiving facility correct in treating the medical
admission to the hospital as a discharge under the Baker Act? If so, is a new
petition and a new hearing is necessary?
The receiving facility should have “transferred” the person for medical treatment
instead of “discharging.” The facility has the power to discharge only when the
person no longer meets the involuntary criteria. While there is a “back office”
discharge for financial or administrative reasons to prevent dual billing for the
same day of care, the notation of “transfer” in the doctor’s order in the medical
record keeps the legal status and the guardian advocate intact. This is why persons
are “transferred” to the state mental health facility — not “discharged.”
Unfortunately, once the patient was “discharged” and a notice of discharge filed,
there may be no alternative to filing a new petition. It’s possible that the state and
defense can just stipulate to much of the evidence presented at the earlier hearing,
but you still have to have a record that the hearing was conducted and that clear
and convincing evidence was presented, prior to entering a new order. Hopefully,
this won’t happen again if you inform the receiving facility personnel at the
hearing of the proper procedure. It’s unfortunate that it happened because it has the
potential of resulting in an extended period of confinement.
G. Waiver of Hearings and Waiver of Patient Presence at Hearing
Can the involuntary inpatient placement hearing be waived?
No. While the hearing cannot be waived, the court can waive the person’s
attendance at all or any part of the hearing if it is consistent with the best interests
of the person and the person’s counsel does not object. Appellate courts have ruled
that such a waiver of the patient’s presence must be documented in the court record
as “knowing, intelligent, and voluntary.”

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
217
We have a patient at our receiving facility who had his court hearing
yesterday but did not attend because he was restrained at the time. He is
requesting to appeal the decision. To my knowledge there is no provision in
the Baker Act for an appeal process. What are this patient’s options, if any,
regarding being court ordered to receive treatment at this facility?
The appellate courts have found that involuntary placement under the Baker Act is
such a substantial deprivation of liberty that any limitation on a person’s ability to
be present at or testify at his or her own hearing is grounds for reversal of the court
order. The courts have said that a person’s refusal to attend or testimony by his/her
attorney of such refusal is an insufficient waiver of the right to be present without a
separate independent inquiry by the court to confirm that the refusal was knowing,
intelligent, and voluntary. In this situation, the individual wasn’t refusing to attend
— he was denied his strong desire and right to attend due to his/her acuity. The
hearing could have been conducted if necessary in the restraint room to allow the
person to attend/participate while preserving the safety of the person and others.
The person’s public defender has the standing to appeal an order for involuntary
placement if the hearing was conducted by a circuit court judge. If the hearing was
conducted by a magistrate instead of by a judge, the public defender has the right
to file an “exception” to the magistrate’s recommended order. According to the
First District Court of Appeal, the public defender “serves as an independent
advocate for the client, not as a neutral party charged with the responsibility of
determining the best interests of the patient or the needs of society.” Handley v.
Dennis, 642 So. 2d 115, 117 (Fla. 1st DCA 1994). The court also said that “if the
patient wishes to be released or transferred and if there is a basis for that request,
the public defender has a duty to advocate the cause of the patient.” Id. Other
relevant First District Court of Appeal cases include:
Ibur v. State, 765 So. 2d 275, 276 (Fla. 1st DCA 2000). The court held that
“[b]ecause involuntary commitment is a substantial deprivation of liberty at
which fundamental due process protections must attach, the patient cannot
be denied the right to be present, to be represented by counsel, and to be
heard.” It reversed the commitment order and remanded the case.
Joehnk v. State, 689 So. 2d 1179 (Fla. 1st DCA 1997). The court held that
the person’s lawyer informing the trial court that the person did not wish to
appear at an involuntary commitment hearing was an insufficient waiver of
the person’s fundamental right to be present at an involuntary commitment
hearing. While the person could waive his rights to be personally present or
constructively present through counsel, the trial court “must certify through

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
218
proper inquiry that the waiver is knowing, intelligent and voluntary.” Id. at
1180. The court reversed the involuntary commitment order and remanded.
Williams v. State, 692 So. 2d 257 (Fla. 1st DCA 1997). The court held that
the person has a fundamental right to be present at a Baker Act commitment
proceeding. Quoting Joehnk, the court stated that while the person may
waive the right to be personally present or constructively present through
counsel, “the court must certify through proper inquiry that the waiver is
knowing, intelligent and voluntary.” It reversed and remanded the case for a
new commitment hearing since the record did not reflect whether the person
had waived his right to be present at the commitment hearing.
If the patient believes his rights have been violated, he can file (or have filed on his
behalf) a petition for a writ of habeas corpus. If the Public Defender’s Office is
unwilling to file an appeal/exception, the individual can contact, e.g., a legal aid
organization or the ACLU to obtain legal representation. Finally, you may wish to
refer this matter to your corporate attorney for assistance.
H. Conversion between Voluntary and Involuntary Status
We have a patient who is voluntary, and the MD wants to file a petition for
involuntary placement. Does the MD also need to do a BA-52, or is initiating
the petition for placement sufficient and timely filing with the court?
No BA-52 is needed to transfer a person from voluntary to involuntary status. The
petition (BA-32) must be filed with the court within two court working days of the
person’s refusal of treatment, request for discharge, or determination by a
physician that the person is incompetent to consent to treatment. It is the court’s
responsibility to prepare the notice of petition unless the hospital has some
different understanding with the clerk of court.
If a petition for involuntary inpatient placement has been filed but the patient
was subsequently deemed competent (prior to court date), do we need to ask
him/her to sign a whole new consent?
Yes. If a person has first been found to meet the criteria for involuntary inpatient
placement and incompetent to consent to treatment, resulting in a petition being
filed with the circuit court, and subsequently stabilizes before the scheduled
hearing, you would indeed request withdrawal of the petition. The person would
sign an application for voluntary admission and other forms required for voluntary
status only after a physician had documented that the person is competent to

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
219
provide express and informed consent by use of the form CF-MH 3104, Certificate
of Competency.
I. Witnesses
I am a new psychiatrist at a receiving facility. We are running into a problem
with the opinions and are finding a need for the option of a “third opinion”
for the BA-32, as there might be occasions when the first and second opinion
psychiatrists may not be available. When this situation arose at a previous
hospital, a third psychiatrist would complete a third opinion (on another
“second opinion” portion), file it with the court, and present testimony at the
hearing. When this was suggested as an alternative here, I discovered there is
no provision in the statutes regarding this. The statute still explicitly states one
of the psychiatrists who initiated the first or second opinion must be present in
court. Can the law be amended to allow for a third opinion when neither the
first or second opinion psychiatrists are available? What do you advise?
The law is quite specific that one of the two experts providing opinions on the
petition must provide testimony at the involuntary placement hearing, but is silent
as to whether the testimony must be done in court or through other methods. While
the doctors know when the hearings are scheduled and usually make plans to
attend as required by law, the statute wouldn’t preclude such testimony from being
done telephonically in exceptional circumstances. This might involve having
someone available to swear in the doctor as a witness when done off site. If neither
of the two doctors is able to testify, the court would have no choice but to dismiss
the petition because there would be no clear and convincing testimony elicited to
support the petition. It is the person’s right to a hearing within the five-day period
of the filing of the petition, unless the person requests a continuance — a Baker
Act equivalent of “speedy trial” under criminal law.
The Florida Supreme Court Commission on Fairness addressing the Baker Act
recommended that the state attorney’s office withdraw the petition if the
allegations in it are not substantiated. This means that if one of the two experts
who prepared the petition is not available to testify, the petition must be withdrawn
by the state attorney or dismissed by the court. The only provision for a “third
opinion” is when the patient has requested an independent expert examination. The
findings of this examination are confidential and not discoverable unless the expert
is called as a witness for the patient at the hearing. One situation in which a
psychiatrist failed to appear at Baker Act hearings to testify in support of petitions
for involuntary placement resulted in her being reported to the Florida Board of
Medicine, which reached a probable cause finding against her medical license.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
220
Is there any provision in the Baker Act that prohibits psychiatrists who
complete the first and second opinions for involuntary placement from being
professionally affiliated; i.e., working in the same practice in the community?
There is no prohibition against psychiatrists who practice with each other from
signing the first and second opinions on the same Petition for Involuntary Inpatient
Placement (form CF-MH 3032). One would presume, unless there is evidence to
the contrary, that each psychiatrist performed an evaluation independent from the
other and reached their respective conclusions based on these evaluations.
Can an ARNP testify at the hearing on involuntary placement on behalf of the
psychiatrist who provided one of the two expert opinions? I told them that
they could not send an ARNP. However, in our county a clinical psychologist
is authorized to provide the second opinion supporting the petition and “One
of the two professionals who executed the involuntary placement certificate
must be a witness. This role cannot be delegated to others.” I would like to
know whether a clinical psychologist (the one giving the second opinion) could
replace the MD in the court.
You are correct that the ARNP is unable to provide the testimony on behalf of the
psychiatrist. Only a psychiatrist is permitted to provide a first opinion. Only a
second psychiatrist or a clinical psychologist is authorized to provide the second
opinion. Either can provide the statutorily required court testimony. Only when the
facility administrator has certified that neither a psychiatrist nor a psychologist is
available to provide the second opinion can a physician who has post-graduate
training and experience in diagnosis and treatment of mental illness or a
psychiatric nurse provide the second opinion. A psychiatric nurse is not the same
as an ARNP. The expert who performs one of the two examinations must testify
and be subject to cross-examination. Psychologists can provide the court testimony
instead of the psychiatrist, but they may be asked questions by the state attorney or
public defender about co-occurring medical conditions as well as the medications
that wouldn’t be within the psychologists’ area of expertise. The psychologist, if
one is used for one of the two opinions, is authorized by law to examine and to
testify as to the conclusions from that examination — an ARNP is not.
I provide most of the testimony at involuntary placement hearings for my
receiving facility. My question is about criterion (1)(a)2.a for involuntary
inpatient placement under section 394.467, Florida Statutes (“is incapable of
surviving alone or with the help of willing and responsible family or
friends, . . . and, without treatment, is likely to suffer from neglect or refuse to
care for himself or herself, and such neglect or refusal poses a real and

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
221
present threat of substantial harm”). I could not find a definition in the
Florida statutes for the terms “neglect” (for adults) or “well-being” or
regarding the concept of “self-care.” It seems that the court and public
defender’s office have no difficulty accepting for this criterion behaviors such
as not eating, not sleeping, neglect of hygiene, and refusal to take medical
medications — obvious physical behaviors — but struggle with the ideas of
refusing to take psychiatric medication, paranoia leading to isolation, having
persecutory delusions, or other “psychological” or “emotional” concepts
related to someone’s well-being. In short, there is resistance to say that
someone refusing psychiatric medication is experiencing neglect, even if they
are paranoid, delusional, and suffering emotionally. Has this been brought up
before?
Some assistant state attorneys don’t elicit the testimony on these issues to support
the petitions. As a result, some persons are released from receiving facilities who
need to be held longer. The statutory language for involuntary examination and
involuntary placement requires the neglect to be real, present, and substantial and
be due to mental illness as defined in the Baker Act. It also needs to be
documented that there isn’t any other help available to assist the person to avoid
this neglect and that there are no less restrictive treatment alternatives.
There aren’t any other Baker Act-related statutory or regulatory provisions that
would provide more guidance in this area. The only other statute governing the
issue of neglect is in the Florida Adult Protective Services law. That law defines
“neglect” as follows:
415.102. Definitions of terms used in ss. 415.101-415.113.
(16) “Neglect” means the failure or omission on the part of the
caregiver or vulnerable adult to provide the care, supervision, and
services necessary to maintain the physical and mental health of the
vulnerable adult, including, but not limited to, food, clothing,
medicine, shelter, supervision, and medical services, which a prudent
person would consider essential for the well-being of a vulnerable
adult. The term “neglect” also means the failure of a caregiver or
vulnerable adult to make a reasonable effort to protect a vulnerable
adult from abuse, neglect, or exploitation by others. “Neglect” is
repeated conduct or a single incident of carelessness which produces
or could reasonably be expected to result in serious physical or
psychological injury or a substantial risk of death.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
222
The burden of proof in the involuntary inpatient placement hearings is “clear and
convincing evidence.” Testimony given by witnesses that fails to meet this
standard is not likely to be helpful in supporting the petition. The best source of
information regarding your question is going to come directly from how the
appellate courts have ruled on the subject of what constitutes clear and convincing
evidence of self-neglect (see the compendium in Appendix II).
J. Hearings
I thought that hearings are to be held in each receiving facility, but I cannot
find this in the law. Section 394.467(6)(a)2., Florida Statutes, just says the
hearing “must be as convenient to the patient as is consistent with orderly
procedure, and shall be conducted in physical settings not likely to be
injurious to the patient’s condition.” In our county, hearings for three
facilities take place in one location.
Historically, these hearings were generally conducted in courthouses. Gradually,
the hearings have been moved to the various Baker Act receiving facilities in most
judicial circuits. This has been found to be much safer for the patients because they
avoid transport, and it increases their privacy and confidentiality. This practice was
recommended by the Florida Supreme Court Commission on Fairness, assuming
that facilities were using space for the hearings not used by patients for any other
program purpose. It is important, wherever the hearings are held, that the person
understands that they’ve had their day in court — not just a clinical staff meeting
or other event occurring in the cafeteria or activity room.
Can Baker Act involuntary placement hearings be done via remote video?
The Florida Supreme Court Commission on Fairness made many recommendations
regarding the Baker Act, including a very strong recommendation against the use
of any video or telephonic hearings or testimony in Baker Act related matters. This
is because the person’s appearance at a hearing done in this fashion may be altered
by the use of such electronic means, particularly if the person’s mental illness is
characterized by paranoia or hallucinations. Certain rules governing juvenile
procedures also limit video or telephonic means due to the minor’s diminished
capacity. By the same token, persons with mental illnesses may also have such a
diminished capacity. However, certain courts are currently considering or have
implemented video-conferenced hearings. In Doe v. State, __ So. 3d __ (2016),
2016 WL 5407617 (Fla. 2d DCA 2016), the Second District Court of Appeal
rejected a challenge to an announcement in Lee County that judges and magistrates
would preside remotely from the courthouse by videoconference. However, the

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
223
court certified to the Florida Supreme Court the following question: “DOES A
JUDICIAL OFFICER HAVE AN EXISTING INDISPUTABLE LEGAL DUTY
TO PRESIDE OVER SECTION 394.467 HEARINGS IN PERSON?” The
Supreme Court accepted jurisdiction, and oral argument is scheduled for February
7, 2017.
A new public defender was recently assigned to Baker Act court. The strict
wording of the statute on involuntary inpatient placement (section 394.467(6),
Florida Statutes) is: “The court shall hold the hearing on involuntary
inpatient placement within 5 days, unless a continuance is granted” (emphasis
added). Page Appendix J-2 of the Baker Act Handbook states: “The court will
hold the hearing on involuntary inpatient placement within five court working
days after the petition is filed, unless a continuance is granted.” This is
extremely important when it comes to weekends and holidays. The public
defender has successfully had most petitions overturned, especially in light of
extended holiday weekends such as at Thanksgiving and Christmas.
Until 2016, the statute referred only to “5 days,” and a 1997 Attorney General
opinion (Op. Att’y Gen. Fla. 97-81 (1997)) interpreted this as calendar days. Since
that time, however, the courts have determined that this is five court working days,
not calendar days. For example, in D.M.H. v. Pietilla, 33 So. 3d 800 (Fla. 5th DCA
2010), the appellate court held that rule 1.090, Florida Rules of Civil Procedure
(now rule 2.514(a), Florida Rules of Judicial Administration), governs the
computation of time prescribed for an involuntary inpatient placement hearing
under section 394.467(6)(a)1., Florida Statutes. That rule provides that Saturdays,
Sundays, and legal holidays are excluded when the time period is less than seven
days. Therefore, the appellate court affirmed the trial court’s denial of the patient’s
petition for a writ of habeas corpus that was based on the failure to hold a hearing
within five calendar days. And in 2016, the statutory wording was changed to
“within 5 court working days” (emphasis added).
If a petition for involuntary placement is filed on or near a holiday and the
court tells you there will not be a hearing due to the holiday schedule, how
should we proceed? The person is incompetent, and the immediate concern is
for his or her safety. Does the court or monitoring agencies see that as a viable
reason for keeping someone beyond the allotted time?
As long as your facility completes the petition (the facility administrator’s
signature and both opinions) and you have filed the petition with the clerk of court
within 72 hours of the individual’s arrival (could be less time if the individual had
been held at a hospital ED or other receiving facility prior to arrival), you have met

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
224
your duty under the law. The law allows for the actual filing to be delayed until the
next court working day only if the examination period ends on a weekend or legal
holiday (not just a weeknight).
Once the petition has been timely filed with the court, you’ve met your duty to the
individual and have the right to hold the individual until the hearing. The court
must conduct the involuntary placement hearing within five court working days
after the filing of the petition. The only legal way of delaying the hearing is if the
individual requests a continuance of the hearing with the concurrence of legal
counsel. If a holiday occurs on the day of a timely hearing, the court could conduct
a hearing on an earlier day than the day scheduled. Further, the patient could file a
petition for a writ of habeas corpus challenging the legality of any extended
detention.
What are the required elements of an involuntary placement hearing?
The hearing is to determine if there is clear and convincing evidence that the
person meets all criteria for involuntary placement and to consider testimony and
evidence regarding the person’s competence to consent to treatment. If the court
finds the person is incompetent to consent to treatment, it is required to appoint a
guardian advocate.
Can a judge merge a Baker Act involuntary placement hearing and an
emergency guardianship proceeding, allowing the family/temporary
guardians and the receiving facility status as intervenors in the Baker Act
hearing?
Handley v. Dennis, 642 So. 2d 115 (Fla. 1st DCA 1994), may be on point here.
The First District Court of Appeal held that when there is a conflict with the area
of guardianship law (chapter 744, Florida Statutes) and the Baker Act (chapter 394,
Florida Statutes), both the duty of the guardian and the power of the guardianship
court must give way to the ward’s rights under the Baker Act to be in the least
restrictive environment. The court went on to say that a liberty interest asserted on
behalf of an involuntary mental patient in a Baker Act hearing is superior to any
conflicting right that could be asserted on behalf of the patient under the
guardianship laws.
Another case that addressed this issue is Auxier v. Jerome Golden Center for
Behavioral Health, 85 So. 3d 1164 (Fla. 4th DCA 2012). A writ of certiorari was
granted after the public defender’s office sought review of an order discharging it
from representing a patient in a Baker Act proceeding. The magistrate dismissed

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
225
the PD because the patient had a plenary guardian and her rights had been
transferred to her guardian and counsel for the guardian would represent her. The
patient was not present at the hearing and did not have independent counsel. The
Fourth District Court of Appeal found the magistrate and the circuit court departed
from the essential requirements of the Baker Act, which requires appointment of
the PD’s office “unless the person is otherwise represented by counsel.” The
guardian’s attorney represents the guardian, not the ward. The Fourth District
concurred with the First District Court of Appeal ruling in Handley v. Dennis.
Having a combined hearing would be unusual. There could potentially be two
hearings, one right after another, that might be allowable as long as the required
notice was provided for each. Notice requirements for a Baker Act hearing are
listed in section 394.4599(2)(d), Florida Statutes, including an independent expert
provided by the court. Since the public defender’s office must be appointed to
represent the person in a Baker Act proceeding, unless the person is represented by
private counsel, it is presumed that the person was appointed a different attorney to
represent him/her under the guardianship matter. Both would be required to be an
independent advocate for the least restrictive alternative for the client.
Family/temporary guardians and the hospital staff have no standing as
“intervenors” in a Baker Act proceeding. Chapter 394 only permits the public
defender representing the person, and the state attorney as the “real party in
interest” representing the state, to call witnesses. These “intervenors” could have
been called as witnesses by the state in support of the continued detention of the
person, but counsel for the ward could have invoked the exclusionary rule to keep
them out of the rest of the hearing. They would have had no standing.
Chapter 744, Florida Statutes, doesn’t establish (nor could it) any superior rights of
the guardian over the ward in the Baker Act case. While section 744.3725 allows
extraordinary authority to be given to a guardian by the court, the court must first
provide for the required array of protections specified in this section of the statute
to the incapacitated person. Chapter 744 allows a court to give a guardian the
power to have the ward committed voluntarily, but the Baker Act prohibits a
facility from admitting as a voluntary patient anyone adjudicated incapacitated.
§ 394.4625(1)(d), Fla. Stat.
K. Involuntary Placement Orders
What is the statutory support for a person being ordered to a short-term
residential treatment facility (SRT) under the Baker Act? I am fully aware
that judges/magistrates order people to SRTs in other areas, but our Baker

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
226
Act judge wants to know what gives her the authority to do so. Is it classified
as a “receiving facility” or a “treatment facility”?
The Baker Act gives the court the authority to order persons to a state mental
health facility (treatment facility), to any receiving facility, or to receive services
from a receiving facility. It is this last provision that has allowed courts in other
circuits to order people for involuntary inpatient placement at SRTs for services
provided by a receiving facility.
Your facility is designated as receiving facility. If the SRT is operated by or
considered as part of the receiving facility, there is no problem with the judge
ordering a person there for involuntary inpatient placement. If located on the same
premises or at the same address as found on the CSU designation letter, there
definitely wouldn’t be a problem. However, if this is not the case, a petition for
involuntary outpatient services might be needed to obtain a court order to services
that aren’t at or by a receiving or treatment facility.
When a court order for involuntary placement at a state hospital has been
entered, there is often so long a wait for a bed that the person stabilizes and a
less restrictive alternative is found to be appropriate. Is a subsequent order
rescinding the involuntary placement order required, or does section 394.469,
Florida Statutes, suffice?
The law requires the administrator of the facility to discharge the person at any
time he/she is found to no longer meet the criteria for involuntary placement. The
release of the person doesn’t require an order of the court.
While a resident was at our SRT, the doctor filed a petition for involuntary
treatment under the Marchman Act and an order for up to 60 days was
entered by the circuit court. However, no bed has been available in the
substance abuse program for him. Does the Baker Act expire when a
Marchman Act is granted by the court?
Generally, the Baker and Marchman laws are considered mutually exclusive since
substance abuse impairment is specifically excluded under the Baker Act definition
of mental illness and substance abuse impairment is specifically required for
involuntary admissions under the Marchman Act. While the two laws can’t be
applied simultaneously, they can be applied sequentially if it is determined as part
of the clinical evaluation that one condition exists to the exclusion of the other or
one is primary and the other secondary. The Baker Act states:
If at any time before the conclusion of the hearing on involuntary

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
227
inpatient placement it appears to the court that the person does not
meet the criteria for involuntary inpatient placement under this
section, but instead meets the criteria for involuntary outpatient
services, the court may order the person evaluated for involuntary
outpatient services pursuant to s. 394.4655. The petition and hearing
procedures set forth in s. 394.4655 shall apply. If the person instead
meets the criteria for involuntary assessment, protective custody,
or involuntary admission pursuant to s. 397.675, then the court
may order the person to be admitted for involuntary assessment
for a period of 5 days pursuant to s. 397.6811. Thereafter, all
proceedings are governed by chapter 397.
§ 394.467(6)(c), Fla. Stat. (emphasis added).
Co-occurring mental health and substance abuse disorders are frequent and should
often be treated concurrently rather than sequentially. This can be done under a
Baker Act order we long as the Baker Act criteria continue to be met.
Say a patient is admitted under the Baker Act to an inpatient unit of a
receiving facility and the facility files the petition within 72 hours, the hearing
is held, and the court orders the patient to remain in the facility for a period
not to exceed 30 days. What does the law require the facility to do if the
patient is in the hospital for 28 out of those 30 days, still needs continued
inpatient treatment, and the 30 days will expire before the patient can be
discharged? Also, the magistrate presiding over the Baker Act hearing is now
required to provide the patient’s date of birth for the court to include on the
court order for the patient. The magistrate has concerns about the patient’s
confidentiality and would like to know if this is a new requirement.
In the circumstances you describe, you should file a petition for continued
involuntary placement with the clerk of court prior to the expiration of the original
order. The court may require you to file it sufficiently in advance of the order’s
expiration so a hearing can be conducted within that period of time. The court in
W.M. v. State, 992 So. 2d 383 (Fla. 5th DCA 2008), held that the judiciary has
concurrent jurisdiction with DOAH for continuation of all involuntary inpatient
orders up to a six-month maximum.
It is unclear why the magistrate has to place the patient’s birth date on the order.
The model form CF-MH 3031 (Order for Continued Involuntary Inpatient
Placement or for Release) doesn’t have any such information included. The
judiciary has the right to modify any form recommended by the executive branch

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
228
of government to achieve the purpose set forth in the law. Adding the birth date is
not required by the Baker Act and is not a result of any requirement by the
Legislature or DCF.
Does an order for involuntary placement need to be for six months?
No. The maximum period for which a person can be ordered for involuntary
placement has traditionally been six months. However, most courts order the
period of placement to be the length of time it is expected to take to stabilize the
person. However, the 2016 Florida Legislature reduced the maximum length of an
involuntary placement order to 90 days, effective July 1, 2016, other than orders to
state treatment facilities, which are permitted for up to six months.
Magistrates in our area have been placing time restrictions on the orders for
periods of weeks instead of the six months permitted by law. It is difficult to
estimate how long it will take to stabilize the person on medication or predict
difficulty with discharge placement issues that may prohibit the person from
being discharged prior to the end of the order. Would this become subject to
involuntary inpatient placement criteria requiring an administrative law
judge from Tallahassee (requires a minimum of 20 days’ notice prior to the
expiration of the order) to perform the hearing? Or do we re-file a form CF-
MH 3032 to get the hearing scheduled and a new court order entered?
Judges and magistrates throughout the state typically entered orders for less than
six months, unless it was expected that the person would be sent to a state hospital.
Section 394.467(6)(b), Florida Statutes, states that “[i]f the court concludes that the
patient meets the criteria for involuntary placement, it may order that the patient be
[transferred, retained, or treated] for up to 90 days. However, any order for
involuntary mental health services in a [state] treatment facility may be for up to 6
months. . . . The facility shall discharge a patient any time the patient no longer
meets the criteria for involuntary placement, unless the patient has transferred to
voluntary status.”
The Baker Act was originally written to place the burden on the receiving or
treatment facility to make the clinical decision as to when, during the six-month
period, the person no longer met the criteria. However, there has been an
increasing use of shorter court orders, transferring the control over the maximum
length of time a person could be held from the facility to the court.
The “continued involuntary inpatient placement” procedures provided for in
section 394.467(7), Florida Statutes, are administrative hearings rather than

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
229
judicial ones. However, courts around the state have handled this issue in several
ways. Some have considered anything within the first six months as within the
court’s jurisdiction. They do this by having the facility request a reconsideration of
the court’s original order or an amendment of the original order to extend the
period of time the person can be held. Others have the facilities file a new petition
for involuntary inpatient placement, prior to the expiration of the original order,
initiating a new involuntary inpatient placement order. This allowed the facility to
retain the person pending the second hearing and allowed the court to hear
evidence as to what factors require a longer than anticipated length of stay (should
the person still be retained when the second hearing is held).
This matter needs to be negotiated with the local courts. Each person has an
attorney, and if that attorney and the assistant state attorney concur with the
procedures used locally, due process has been provided.
In W.M. v. State, 992 So. 2d 383 (Fla. 5th DCA 2008), the Fifth District Court of
Appeal established that concurrent jurisdiction between the judiciary and DOAH
exists within the six months of the original order. The circuit court had ordered a
patient involuntarily committed for three weeks. When she didn’t respond to
treatment, a petition for continued involuntary placement was filed and the court
ordered six more months of treatment. The patient appealed, arguing that the court
had no jurisdiction to order the continued treatment. The appellate court affirmed
the order, stating that while continued involuntary placement hearings are to be
administrative, the circuit court retains concurrent jurisdiction. The Legislature’s
intent was that the administrative hearing requirement applies after a patient is
committed to long-term treatment at a treatment facility instead of a community-
based receiving facility. Because the initial treatment ordered by the court was
short-term, the court properly exercised jurisdiction to order further treatment.
However, once long-term treatment is ordered, a petition for continued treatment
must be addressed in an administrative hearing.
What authority does the court have to specify a particular program or facility
in an involuntary inpatient placement order?
The court has the power to order that a person be transferred to a treatment facility
or, if the person is at a treatment facility, that he/she be retained there or be treated
at or receive services from any designated receiving or treatment facility. The
recommended order for involuntary inpatient placement intentionally doesn’t
include a space for the name of a facility, so that a person’s right to request transfer
from one facility to another is expedited without having to return to court for an
amended order. The court may modify the form. If it enters its order on a modified

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
230
form that includes a specific facility or program, the only alternative that program
would have is to request the court to reconsider or amend its order or file an appeal
of the order. An uncontested court order must be followed.
A circuit judge entered an order for our receiving facility to accept a person
who was in jail on felony charges. The order provided that the inmate be sent
to a state hospital as soon as a bed became available. Is this proper?
No. This is not a proper use of the Baker Act. However, one can’t ignore a court
order. There are procedures to be followed in challenging a court order —
requesting reconsideration or having a rehearing, or appealing the order, as
determined by the receiving facility’s attorney. The attorney will probably want to
discuss this matter with the judge to avoid having to respond to such orders later.
The only way to legally order someone into a state hospital is under chapter 394,
part I, Florida Statutes (Baker Act), or chapter 916, Florida Statutes (forensic). If
the judge didn’t follow either of these two statutes, it is essential that the facility
properly question the order. The state hospital’s attorney should also be consulted
on the matter.
Does a facility have the discretion to release a person from an order for
involuntary placement without the consent of the court?
Yes. The administrator has the duty to discharge a person at any time the person no
longer meets the criteria for involuntary placement, unless the person has
transferred to voluntary status.
Are there any Baker Act or Marchman Act appellate cases having to do with
elopements after an order for involuntary placement has been entered?
There isn’t any appellate case addressing elopements from facilities under the
Baker Act. However, there is a Marchman Act case on point: S.M.F. v. Needle, 757
So. 2d 1265 (Fla. 4th DCA 2000). The circuit court had granted a petition for
involuntary substance abuse treatment for a minor in response to a petition filed by
her parent. The order was for 60 days of involuntary treatment, the maximum
period permitted under law at that time, commencing upon her admission to the
facility. However, the minor ran away prior to commencing treatment and was
returned to the program after the initial court order had expired. She filed a petition
for a writ of habeas corpus, arguing that she was entitled to immediate release
because section 397.6977, Florida Statutes (1999), provided that “[a]t the
conclusion of the 60-day period of court-ordered involuntary treatment, the client
is automatically discharged unless a motion for renewal of the involuntary

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
231
treatment order has been filed with the court.” The appellate court held that the
automatic discharge would occur “at the ‘conclusion of the 60-day period of court-
ordered involuntary treatment,’ not merely sixty-days after the entry of the order
for treatment,” and that the 60-day period had not expired, because the petitioner
ran away before commencing treatment. The petition for writ of habeas corpus was
denied.
L. Continued Involuntary Inpatient Placement
Why are continued involuntary inpatient placement orders under the
jurisdiction of ALJs instead of circuit judges? Since the law authorized “up to
6 months” for these initial orders, why do the circuit courts enter the orders
for shorter periods of time?
When the Baker Act was first enacted in the early 1970s, state-operated mental
hospitals represented the majority of the care offered in Florida. Once persons were
sent from their home communities to state hospitals on involuntary placement
orders, it would have been a logistical nightmare for the patients to be brought
back to their own circuits for continued involuntary hearings at the expiration of
the original orders, and it would have created an undue burden on the circuits
where the state hospitals were located to take on this workload. The problem was
resolved by having ALJs from the DOAH circuit ride to the various state hospitals
to conduct these hearings.
The law was written to allow up to six months for the orders and required
receiving/treatment facility administrators to release the person or transfer to
voluntary status at any time the criteria for involuntary placement were no longer
met (section 394.467(6), Florida Statutes). For many years, all involuntary
placement orders entered reflected a six-month time frame. Over the past decade or
more, a trend emerged that fundamentally transferred the control over the time
period a person could be held from facility administrators to the judiciary by
limiting the period of time of the order to the length of time that evidence
documented it would take to stabilize the person’s condition. These shortened
periods, as well as court order of persons to SRT settings, resulted in court orders
for involuntary inpatient placement expiring while persons are still in the
community. As of July 1, 2016, the maximum length or orders is 90 days, with the
exception of orders to state treatment facilities, which remains six months.
I’m an assistant public defender. I received a copy of a Petition Requesting
Authorization for Continued Involuntary Inpatient Placement (form CF-MH
3035). Where did this form originate, and was it ever approved for

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
232
implementation?
This form, along with most of the Baker Act form series, is a recommended one,
but is not required. It was developed in 1998 and revised in 2005 — promulgated
under the Administrative Procedure Act. The recommended forms can be modified
as long as they retain the legal requirements. The recommended form tracks the
requirements of section 394.467(7), Florida Statutes, but could be amended.
M. Baker Act Forms and Service of Process
Can we fax or email documents to the clerk of court if a hard copy is sent
within a specific amount of time?
This issue isn’t governed by the Baker Act. Many judicial circuits accept emailed
or faxed filings and others do not. Clerks are actively working toward such
electronic systems; some use FTP (File Transfer Protocol), which allows secure
transfer of files over the Internet. You need to contact the office of clerk of court
serving your county and determine what their requirements may be. The judicial
branch determines how to conduct its business. Whatever is acceptable to your
courts on petition filing would suffice.
Is the circuit court required to use the model Baker Act forms developed by
DCF?
No. Separation of powers between each branch of government ensures that the
executive branch can’t compel the judicial branch to a specific action. However,
the Florida Supreme Court Commission on Fairness recommended that each
judicial circuit review and consider adapting and adopting the model forms
prepared by DCF.
If a petition for involuntary inpatient placement is filed with the court, is the
clerk of the court responsible for providing copies of the petition and the
notice of hearing to all required parties?
Yes. Section 394.467(3), Florida Statutes, states that upon the filing of a petition
for involuntary inpatient placement, “the clerk of the court shall provide copies of
the petition to the department, the patient, the patient’s guardian or representative,
and the state attorney and public defender of the judicial circuit in which the
patient is located.” Section 394.4655(4)(c) assigns the same responsibility (along
with including a copy of the proposed treatment plan) to the clerk of the court for
involuntary outpatient services.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
233
Section 394.4599(2)(d), governing notice of the filing of petitions for involuntary
(inpatient or outpatient) placement, doesn’t specify who is responsible for filing
the notice of hearing. However, one can only conclude that responsibility lies with
the clerk’s office, because the procedure requires confirmation of petition filing,
public defender appointment, the date/time/place of hearing, court appointment of
an independent expert, change of venue information, etc. — all issues that are the
responsibility of the court.
Who uses the form titled Order Requiring Involuntary Assessment and
Stabilization for Substance Abuse and for Baker Act Discharge of Person
(CF-MH 3114)? Does this take the place of a Marchman Act proceeding?
That form is used by the court when, prior to the conclusion of a hearing for
involuntary inpatient placement or involuntary outpatient services under the Baker
Act, it finds that the person instead meets the criteria for involuntary admission
under the Marchman Act. This form can then be used to order the person to
undergo such admission for involuntary assessment under the Marchman Act.
The magistrate recently dismissed our petition (CF-MH 3032) because we
hadn’t submitted a number of forms, including the Notice of Petition for
Involuntary Placement, Notice of Right to Petition for Writ of Habeas Corpus
or for Redress of Grievances, Certificate of Professional Initiating
Involuntary Examination, Petition for Adjudication of Incompetence to
Consent to Treatment and Appointment of a Guardian Advocate, and
Certification of Person’s Incompetence to Consent to Treatment and
Notification of Health Care Surrogate/Proxy. Was this correct?
No. There is no requirement that these forms, other than the 3032 petition, be filed
by the petitioner with the court. The public defender and state attorney generally
review these forms at the facility prior to or at the time of the hearing. Submitting
copies simultaneous with petition filing seems to be unnecessary.
N. Transfers of Persons under Involuntary Placement
Can persons on involuntary inpatient placement orders be transferred from
one facility to another?
Yes. The Baker Act law and rules don’t require that the name of the facility be
incorporated into the court order for placement. In fact, the recommended model
Involuntary Placement Order form (CF-MH 3008) doesn’t include space for such
limitation. This was deliberately done to facilitate a patient’s right to request
transfer from one facility to another without the delay involved in scheduling a

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
234
court hearing. It appears that the circuit court in your county has added the specific
name of the facility to the form, retaining control over where the patient may be
placed as opposed to allowing the patient, guardian, or facility the right given in
the Baker Act to transfer from one facility to another without delay in waiting for
another hearing.
The public defender assigned to represent persons on involuntary status in
our receiving facility said that when an involuntary patient is transferred
from our facility to another facility, it is his opinion that the Baker Act
involuntary order is void because by transferring the patient our hospital
effectively discharged the patient, and that by the discharge of the patient the
Baker Act order is automatically rescinded and the patient has to have a new
petition for involuntary placement filed. Could you clarify?
The Baker Act makes a very distinct difference between transfers and discharges.
While a receiving facility would have to do some sort of a back-office
(administrative/financial) discharge of a patient when a transfer to another
receiving or treatment facility takes place, the Baker Act record should reflect that
a transfer is taking place. A facility only has the power to discharge a person who
no longer meets the criteria for involuntary placement. Otherwise the facility must
retain the person or transfer to another facility.
O. State Treatment Facilities and Transfer Evaluations
Our hospital-based receiving facility has an individual who appears
appropriate for the state hospital. I believe I read somewhere that before an
individual can be admitted, a transfer evaluation must be made by the public
receiving facility. Is this correct? If so would you please provide me with the
law or rule that states this requirement?
In summary, no one may be transferred to a state mental health treatment facility
(voluntary or involuntary) without a transfer evaluation. The following should
help:
Criteria:
Whether the person meets the statutory criteria for admission to a state
treatment facility.
Whether there are appropriate, more integrated, and less restrictive treatment
resources available to meet the person’s needs.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
235
Process:
Following evaluation of the person, the community mental health center
director recommends admission to a state treatment facility or, if the criteria
for involuntary placement are not met, to alternative treatment programs, by
completing and signing the “Transfer Evaluation” (form CF-MH 3089).
The evaluation is forwarded to the court prior to the hearing (“the court shall
receive and consider the information,” section 394.461(2), Florida Statutes).
Testimony is presented at the hearing by the evaluator or other
knowledgeable staff as desired by the court.
Requirements in Florida Statutes:
394.455. Definitions
(9) “Community mental health center or clinic” means a publicly
funded, not-for-profit center that contracts with the department for the
provision of inpatient, outpatient, day treatment, or emergency
services.
* * *
(46) “Transfer evaluation” means the process by which a person
who is being considered for placement in a state treatment facility is
evaluated for appropriateness of admission to the facility.
The rules implementing the requirements for transfer evaluations are found in rules
65E-5.1301, 65E-5.1302, and 65E-5.290, Florida Administrative Code.
394.461. Designation of receiving and treatment facilities.--
(2) Treatment facility.--The department may designate any state-
owned, state-operated, or state-supported facility as a state treatment
facility. A civil patient shall not be admitted to a state treatment
facility without previously undergoing a transfer evaluation.
Before a court hearing for involuntary placement in a state treatment
facility, the court shall receive and consider the information
documented in the transfer evaluation. Any other facility, including a
private facility or a federal facility, may be designated as a treatment

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
236
facility by the department, provided that such designation is agreed to
by the appropriate governing body or authority of the facility.
Prior to July 1, 2016, the definition of “treatment facility” required that the
community mental health center or clinic prepare the transfer evaluation.
However, the 2016 Legislature eliminated any specification as to
responsibility for this function. The Florida Administrative Code continues
to require this of the community health center or clinic, but there is no longer
any specific statutory basis for this requirement.
A patient at a private receiving facility is scheduled to go to the state hospital.
Which public entity should conduct the transfer evaluation?
The statutorily required transfer evaluation must be done prior to the person’s
involuntary inpatient placement hearing pursuant to the provisions in the Florida
Administrative Code. See FAQs above regarding the entity to conduct the transfer
evaluation. DCF could designate a single CMHC to do this county- or circuit-wide
or assign to each CMHC the nearest private receiving facilities. A CMHC that has
a public receiving facility would conduct transfer evaluations on persons in its own
CSU. Since the 2016 legislative change eliminating specification of the community
mental health center or clinic, DCF could designate the managing entity or other
entity this responsibility.
P. Convalescent Status
I work for a clerk of court. Section 394.469(1)(c), Florida Statutes, refers to
the placement of an improved patient “on convalescent status in the care of a
community facility.” What is convalescent status? There is confusion among
the discharge planners at the facility as to the judges’ authority to order a
patient who no longer meets inpatient criteria into a secure facility upon
discharge from the receiving facility. Would it be more appropriate to include
the ALF placement as part of the treatment plan in an outpatient placement
petition? Or does the judge actually have authority to include in the inpatient
placement order discharge to a secure facility?
All references to convalescent status were removed from the statute in 1996 except
for the one you reference regarding persons on involuntary inpatient placement:
394.469. Discharge of involuntary patients.-- (emphasis added)
(1) Power to discharge.--At any time a patient is found to no longer meet
the criteria for involuntary placement, the administrator shall:
Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
237
(a) Discharge the patient, unless the patient is under a criminal charge, in
which case the patient shall be transferred to the custody of the appropriate
law enforcement officer;
(b) Transfer the patient to voluntary status on his or her own authority or
at the patient’s request, unless the patient is under criminal charge or
adjudicated incapacitated; or
(c) Place an improved patient, except a patient under a criminal
charge, on convalescent status in the care of a community facility.
While this may have been an oversight by the Legislature, it remains in the statute.
The decision to place an individual on Convalescent Status is made by a facility
administrator, not the judge. When used, Convalescent Status is a temporary “leave
of absence” from the facility where the individual has been ordered on involuntary
inpatient status to determine whether a community placement will be successful
before the individual is formally “discharged” from the order. This avoids the
necessity for beginning the entire involuntary inpatient placement procedure all
over again should the community placement be unsuccessful.

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
238
XVII. Selected Sample Baker Act Forms for Involuntary Inpatient Placement
Please note that these recommended forms were promulgated by DCF before
the 2016 statutory amendments and do not incorporate those changes.
A. Petition for Involuntary Inpatient Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Petition for Involuntary Inpatient Placement
COMES NOW the Petitioner, _____________________________________________________ , and alleges:
1. That Petitioner is Administrator of ___________________________ _____________________________
Name of Facility Facility Address
2. That (Name of Person ) ______________________________________________________________ , is a
patient of said facility and has been examined at such facility.
3. The last four (4) digits of the person’s social security number are ______ and date of birth is: ___________.
Date
4. That this petition is being filed within the following time frames: (Check one below)
A. This person was admitted for involuntary examination and this petition is being filed within the 72-
hour examination period, or if the examination period ends on a weekend or legal holiday, on the
next court working day
OR
B. This person was transferred to involuntary status after examination or after refusing/revoking
consent to treatment or requesting discharge from the facility and this petition is filed within two
court working days.
5. That attached hereto and by reference made a part hereof, are two (2) opinions regarding the mental health
of said person necessitating involuntary inpatient placement.
6. That based thereon Petitioner recommends that the person/respondent be involuntarily placed in
_____________________________________, a (public/private) designated receiving or treatment facility.
7. In addition to at least one of the two experts whose opinions are attached, the following persons may
testify:
Witness Witness Witness
Name: _________________________ _________________________ _________________
Relationship _________________________ _________________________ _________________
Address _________________________ _________________________ _________________
_________________________ _________________________ _________________
Telephone: (______)_________________ (______)_________________ (______)_________
CONTINUED OVER

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
239
Petition for Involuntary Placement (Page 2)
COMES NOW THE PETITIONER and further alleges that:
1. A Guardian Advocate is necessary to act on the person’s behalf on issues related to express and
informed consent to mental health or medical treatment and a Petition for Adjudication of
Incompetence to Consent to Treatment and Appointment of a Guardian Advocate is attached; OR
2. The person/respondent is competent to provide express and informed consent to his or her own
treatment or the person has a guardian authorized to consent to treatment and no Guardian Advocate is
requested.
_______________________________________ ________________ __________ am pm
Signature of Facility Administrator or Designee Date Time
______________________________________________
Typed or Printed Name of Administrator or Designee
The person does or does not have a private attorney. If so, the name and address of the
private attorney is:
Private Attorney Name: ________________________________________________________________
Private Attorney Address: ______________________________________________________________
cc: The Clerk of the Court shall provide a copy of this petition to the: (Check when applicable and
initial/date/time when copy provided)
Individual
Date Copy Provided
Time Copy Provided
Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Public Defender
am pm
Representative
am pm
State Attorney
am pm
Dept. of Children &
Families
am pm
CONTINUED / SUPPORTING OPINIONS ON PAGE 3

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
240
Petition for Involuntary Placement (Page 3)
First Opinion Supporting the Petition
I, ____________________________ a psychiatrist authorized to practice in the State of Florida, have personally examined
_______________________________________ on _________________ (within 72 hours of the signing hereof) and find
Name of Person Date
from such examination that the person meets the following criteria for involuntary placement:
1. Said person is mentally ill and because of a mental illness (check one):
a. Said person has refused voluntary placement for treatment after sufficient and conscientious explanation and
disclosure of the purpose of placement for treatment; OR
b. Said person is unable to determine for himself/herself whether placement is necessary:
AND
2. Either (Check one or both):
a. Said person is manifestly incapable of surviving alone or with the help of willing and responsible family or
friends, including available alliterative services, and without treatment, he/she is likely to suffer from neglect
or refuse to care for himself/herself and such neglect or refusal poses a real and present threat of substantial
harm to his or her well-being; OR
b. There is substantial likelihood that in the near future said person will inflict serious bodily harm on himself/
herself or another person as evidenced by recent behavior causing, attempting, or threatening such harm.
AND
All available less restrictive treatment alternatives which would offer an opportunity for improvement of said person’s
condition have been judged to be inappropriate based on contact with the following programs/agencies: _______________
__________________________________________________________________________________________________
Observations which support this opinion are:
____________________________________________ _____________ ____________ am pm
Signature of Psychiatrist Date Time
____________________________________________ __________________________________
Typed or Printed Name of Psychiatrist License Number
Second Opinion Supporting the Petition
I,______________________, a psychiatrist, clinical psychologist, licensed physician *, psychiatric nurse
*, authorized to provide a second opinion on this petition pursuant to Section 394.467 (2), F.S., have personally examined
________________________________________________ on ______________, (within 72 hours of signing hereof), and
Name of Person Date
find that he/she meets the criteria for involuntary inpatient placement as stated in this petition. Observations which support this
opinion are:
_______________________________________________ ____________ _____________ am pm
Signature of Examiner Date Time
_______________________________________________ ________________ ____________________
Typed or Printed Name of Examiner Profession License Number
I certify that the county in which the person is detained has less than 50,000 population and no psychiatrist or
psychologist is available to provide the second opinion.
_____________________________________________________________ __________________________
Printed Name and Signature of Administrator or Designee Date
* A licensed physician or psychiatric nurse may only provide such second opinion in counties of less
than 50,000 population in cases where the facility administrator certifies that no psychiatrist or clinical
psychologist is available to provide the second opinion (by countersigning above).
See s. 394.4599(2)[d]3, 394.467, Florida Statutes
CF-MH 3032, Nov 11 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
241
B. Notice of Petition for Involuntary Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _______________________________ CASE NO.: ___________________________
Notice of Petition for Involuntary Placement
YOU ARE HEREBY NOTIFIED that a petition for a hearing has been filed with the Circuit Court in
___________________ County, Florida where the above-named person is hospitalized on the question of whether
he/she should be ordered or confined for:
Involuntary Inpatient Placement
Involuntary Outpatient Placement
Continued Involuntary Outpatient Placement
Said person will be represented by the Public Defender if he/she is not otherwise represented by counsel.
A hearing has been scheduled by the court and will be conducted pursuant to Section 394.467, F.S., on
____________ at ______ am pm at __________________________________________________________.
Date Time at Place/address
At least one of the following examining experts will testify in support of continued detention:
___________________________________________ _____________________________________________
In addition to at least one of the professionals listed above, the following persons are also expected to testify in support of
involuntary inpatient placement or involuntary outpatient placement or continued involuntary outpatient placement:
Guardian or Representative Other Witness Other Witness
Name: ______________________ ________________________ ____________________
Relationship ______________________ ________________________ ____________________
Address ______________________ ________________________ ____________________
______________________ ________________________ ____________________
Telephone: (______)_______________ (______)_________________ (______)_____________
The person, the person’s guardian, or representative, or the administrator may apply for a change of venue for the
convenience of the parties or witnesses or because of the condition of the person.
The person has a right to an independent expert examination and if he/she cannot afford such an examination the Court
shall provide for one.
_____________________________________________ _________________ _________ am pm
Signature of Court Date Time
_____________________________________________
Printed Name of Court
Certificate of Mailing
I hereby certify that I mailed the above and foregoing notice to the named parties by depositing the same in the United
States Post Office on the ______________ day of _________________, ___________. In addition, I sent this notice by
registered or certified mail to each person listed below who was not given a copy by hand delivery.
_____________________________________________ __________________ __________ am pm
Signature of Court Date Time
This form may be completed and mailed by the Receiving Facility instead of the Court, with the court’s
concurrence.
cc: Person Guardian Representative Public Defender or Private Attorney
See s. 394.4599(2)(a), [d], Florida Statutes
CF-MH 3021, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
242
C. Application for Appointment of Independent Expert Examiner
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Application for Appointment of Independent Expert Examiner
I, ______________________________________________________________________________ hereby
petition the Court to order an independent expert examination pursuant to:
Involuntary Inpatient Placement (s.394.467(6)(a)2, FS)
Involuntary Outpatient Placement (s.394.4655(6)(a)2, FS)
Continued Involuntary Outpatient Placement (s.394.4599(2)[d]5, FS)
____________________________________________________________ ________________________
Signature of Person or Representative Date
____________________________________________________________
Typed or Printed Name of Person or Representative
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who Provided Copy
Person
am pm
Guardian
am pm
Representative
am pm
See s. 394.467(6)(a)2, Florida Statutes
CF-MH 3022, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
243
D. Notice to Court – Request for Continuance of Involuntary Placement
Hearing
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________ CASE NO.: _________________
Notice to Court
Request for Continuance of Involuntary Placement Hearing
_________________________________________________________, a person awaiting a hearing on:
Involuntary Inpatient Placement, pursuant to 394.467, FS, or
Involuntary Outpatient Placement, pursuant to 394.4655, FS
at _____________________________________________ Receiving or Treatment Facility has requested
a continuance of his/her hearing for a period of _______________ (not to exceed a period of four weeks).
Any independent expert examination, if requested, will be completed and results provided to the
undersigned attorney of record during the period of this continuance.
__________________________________________ _______________ _________ am pm
Signature of Counsel Date Time
__________________________________________________________
Typed or Printed Name of Counsel
cc: Person Facility Administrator State Attorney Guardian Representative
See s. 394.467(5), Florida Statutes
CF-MH 3113, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
244
E. Order Requiring Involuntary Assessment and Stabilization for Substance
Abuse and for Baker Act Discharge of Person
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________ CASE NO.: __________________
Order Requiring Involuntary Assessment and Stabilization
for Substance Abuse and for Baker Act Discharge of Person
THIS MATTER came to be heard pursuant to s. 394.467, F.S., on the issue of whether the above-named person
should be ordered to involuntary inpatient placement or involuntary outpatient placement, and the court having
considered testimony and evidence and having heard the argument of counsel, has concluded as follows:
1. The above-named person does not meet the criteria for involuntary inpatient placement in a treatment
facility or involuntary outpatient placement, pursuant to the provisions of Chapter 394, Florida Statutes.
2. There is a good faith reason to believe that the above-named person is substance abuse impaired, and,
because of such impairment, has lost the power of self-control with respect to substance use, and
has inflicted, or threatened or attempted to inflict, or unless admitted to involuntary treatment for
substance abuse is likely to inflict physical harm on himself or herself or another.
is in need of substance abuse services, and, by reason of substance abuse impairment, has such impaired
judgment that said person is incapable of appreciating his or her need for such services and of making a
rational decision in regard thereto.
3. The above-named person should be admitted to a hospital or to a licensed detoxification facility or
addictions receiving facility for involuntary assessment and, if necessary, stabilization, pursuant to s.
394.467(6) and s. 397.6811, Florida Statutes.
4. The admission ordered herein below is the least restrictive appropriate alternative for the assessment and
stabilization of the above-named person who may be substance abuse impaired.
Whereupon, it is
ORDERED
That the above-named person shall be discharged this date from any involuntary status for a mental illness
pursuant to Chapter 394, Florida Statutes.
That the above-named person shall be admitted for a period not to exceed 5 days to ____________________
_________________________ for substance abuse involuntary assessment and, if necessary, stabilization.
_________________________________________________________________ shall take the above-
named person into custody and deliver said person to the licensed service provider specified above, or, if
none is specified, to the nearest appropriate licensed service provider for involuntary assessment.
The Public Defender is discharged, and _______________________________________________________
is appointed counsel for all matters pursuant to s. 397, F.S.
DONE AND ORDERED in _______________ County, Florida, this _____ day of _______________, __________.
_____________________________________________ ___________________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.467(6)(c), Florida Statutes
CF-MH 3114, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
245
F. Order Requiring Evaluation For Involuntary Outpatient Placement
IN THE CIRCUIT COURT, _________________ JUDICIAL CIRCUIT,
IN AND FOR ____________________ COUNTY, FLORIDA
IN RE: ___________________________ Case No.: __________________________
ORDER REQUIRING EVALUATION FOR
INVOLUNTARY OUTPATIENT PLACEMENT
THIS MATTER came to be heard on ___________________________, pursuant to s.
394.467, F.S., on petition for involuntary inpatient placement of the above-named person and
the court being advised in the premises, finds as follows:
1. The above-named person does not meet the criteria for involuntary inpatient placement in a mental
health treatment or receiving facility.
2. The above-named person is 18 years of age or older, has a mental illness, and has a history of lack of
compliance with treatment for mental illness.
3. The above-named person is unlikely to survive safely in the community without supervision; this
finding is supported by testimony of _______________________________ as to his/her clinical
determination.
4. The above-named person has:
A. At least twice within the preceding 36 months been involuntarily admitted to a receiving
or treatment facility as defined in s.394.455, or received mental health services in a forensic
or correctional facility, or
B. Engaged in or attempted to engage in one or more acts of serious violent behavior toward
self or others within the preceding 36 months.
5. The above-named person is, as a result of mental illness, unlikely to voluntarily participate in
recommended treatment and has either refused voluntary placement for recommended treatment after
sufficient and conscientious explanation and disclosure of the purpose of placement, or is unable to
determine whether placement is necessary.
6. In view of the person’s treatment history and current behavior, the person is in need of involuntary
outpatient placement in order to prevent a relapse or deterioration that would be likely to result in
serious bodily harm to the person or others, or a substantial harm to the person’s well-being through
neglect or refusal to care for self as set forth in s. 394.463(1);
7. It is likely that the person will benefit from involuntary outpatient placement. All available less
restrictive alternatives that would offer an opportunity for improvement of his or her condition are either
inappropriate or unavailable.
Whereupon, IT IS ORDERED
1. That the above-named person be discharged this date from any involuntary inpatient
placement and treatment for mental illness.
2. That the above-named person shall be evaluated by _____________________ located at
_________ for involuntary outpatient placement within __ days of the date of this hearing.
DONE AND ORDERED in Chambers at ______ County, Florida, this __ day of ______, 20__.
_____________________________ ______________________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.4655(6)(c), Florida Statu[t]es
CF-MH 3115, Feb 05 (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
246
G. Notification to Court of Withdrawal of Petition for Hearing on Involuntary
Inpatient or Involuntary Outpatient Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ________________________________________ CASE NO.: _____________________
Notification to Court of Withdrawal of Petition
For Hearing on Involuntary Inpatient or involuntary Outpatient Placement
YOU ARE HEREBY INFORMED THAT ______________________________________________________
Name of Person
at ______________________________________________________________________________________
Facility Name and Address
has made application by express and informed consent for voluntary admission, due to an improvement in
his/her condition.
was discharged on ____________________ to ____________________________________________
Date Destination (if known)
was transferred on ____________________ to ____________________________________________
Date Destination (if known)
was converted to Marchman Act on ______________________________________
Date
Other (specify): ________________________________________________________________________
_____________________________________________________________________________________
Please withdraw my Petition for:
Involuntary Inpatient Placement
Involuntary Outpatient Placement
Continued Involuntary Outpatient Placement
filed on ________________(date). The Petition for Adjudication of Incompetence to Consent to Treatment
and Appointment of a Guardian Advocate, if any, is also being withdrawn.
__________________________________________ _______________ ___________ am pm
Signature of Administrator or Designee Date Time
__________________________________________
Printed Name of Administrator or Designee
cc: Clerk of the Court (Probate Division) Person Guardian
Assistant State Attorney Representative Person’s Attorney
When a petition for involuntary placement is withdrawn, the court, state attorney, public defender or other
attorney for the person, and guardian or representative must be notified by telephone within one business
day of the decision, unless such decision is made within 24 hours prior to the hearing. In such cases, the
notification must be made immediately.
See s. 394.467, 394.4685, 394.469, Florida Statutes
CF-MH 3033, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
247
H. Order for Involuntary Inpatient Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Order for Involuntary Inpatient Placement
This matter came to be heard pursuant to a Petition for Involuntary Inpatient Placement filed herein on the issue of
whether the above-named person should be involuntarily placed in a mental health treatment or receiving facility, and the
Court being fully advised in the premises, finds by clear and convincing evidence, as follows:
1. Said person has been represented by counsel; Said person appeared at the hearing, or
said person’s presence at the hearing was waived, without objection of said person’s counsel.
2. Said person meets the following criteria for involuntary inpatient placement pursuant to s. 394.467(1), F.S. :
(a) He or she is mentally ill and because of a mental illness:
(1) has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure of
the purpose of placement for treatment; or
(2) is unable to determine for himself or herself whether placement is necessary; AND
(b) Either
(1) He or she is manifestly incapable of surviving alone or with the help of willing and responsible family or
friends, including available alternative services, and, without treatment, is likely to suffer from neglect or
refuse to care for himself or herself, and such neglect or refusal poses a real and present threat of substantial
harm to his or her well-being; or
(2) There is substantial likelihood that in the near future he or she will inflict serious bodily harm on himself or
herself or another person, as evidenced by recent behavior causing, attempting, or threatening such harm; and
(c) All available less restrictive treatment alternatives which would offer an opportunity for improvement of his or
her condition have been judged to be inappropriate.
3. The nature and extent of the above-named person’s mental illness is as follows: _______________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
4. The Court considered testimony and evidence regarding the person’s competence to consent to treatment. The person
was found to be
competent incompetent to consent to treatment. If found to be incompetent, ________________________
_________________________________________________________________ was appointed as guardian advocate.
(name and address)
5. If the petition was referred to and heard by a general master, the Master’s Report and Recommendation are attached,
incorporated by reference, and/or adopted by the Court.
ORDERED
That the above-named person be placed in a designated mental health receiving or treatment facility on an involuntary
basis for a period of up to ____________________________, not to exceed 6 months from the date of this order, or until
discharged by the administrator or transferred to voluntary status.
DONE AND ORDERED in _____________ County, Florida, this ______ day of ____________, ____________.
___________________________________________ _________________________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
This form must accompany person to the treatment facility.
See s. 394.467(1), Florida Statutes
CF-MH 3008, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
248
I. Petition Requesting Authorization for Continued Involuntary Inpatient
Placement
IN RE: ___________________________________ CASE NO.: ______________________
Petition Requesting Authorization for Continued Involuntary Inpatient
Placement
The petition of __________________________________________________________ who is the
Administrator of ___________________________________________________________ Facility shows that:
1. The above named person, ________________________________ of _______________________ County,
Florida, is currently in the aforesaid facility and was admitted to this facility on ____________________.
Date
2. That according to the provisions of Section 394.467 (7), F.S., this person may not be retained after
_____________________, (Date) without an order authorizing continued involuntary inpatient placement.
3. That the person continues to meet the criteria for involuntary inpatient placement pursuant to Section
394.467(1), F.S., and
that legally authorized period has nearly expired, or
the person was admitted while serving a criminal sentence whose sentence will expire on _______ , or
Date
the person was placed while a minor and will reach the age of majority on _________________.
Date
Wherefore, it is requested an Order be issued authorizing this Facility to retain the person for a period not to
exceed six (6) months.
_______________________________________ __________________ ___________ am pm
Signature of Administrator or Designee Date Time
____________________________________________________
Printed or Typed Name of Administrator or Designee
CONTINUED OVER

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
249
Petition Requesting Authorization for Continued Involuntary Placement (Page 2)
Physician’s or Clinical Psychologist’s Statement
I hereby state that the above named person continues to meet the criteria for involuntary placement.
Behavior which supports this opinion is: ___________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Person’s treatment during placement was: __________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Less restrictive settings which were investigated and the reasons they were ruled out are as follows: ____
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Support for facts in this statement is attached.
The individualized treatment plan for the person is attached.
_____________________________________________ _______________ _________ am pm
Signature of Physician Clinical Psychologist Date Time
________________________________________ _______________________________
Printed Name of Physician/Clinical Psychologist License Number
File this completed form with the Administrative Law Judge.
Person does or does not have a private attorney. If so, the name and address of the
private attorney is: ____________________________________________________________________
Private Attorney Name: ________________________________________________________________
Private Attorney Address: ______________________________________________________________
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
Public Defender or
Private Attorney
am pm
See s. 394.467(7), Florida Statutes
CF-MH 3035, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
250
J. Notice of Petition for Continued Involuntary Inpatient Placement
IN RE: __________________________________ CASE NO.: __________________________
Notice of Petition for Continued Involuntary Inpatient Placement
YOU ARE HEREBY NOTIFIED that a petition for a hearing has been filed with the State Division of Administrative
Hearings on the question of whether ___________________________________________________________________
who is hospitalized at _________________________________________________________________ should be ordered
for continued involuntary inpatient placement.
The person will be represented by the Public Defender if the person is not otherwise represented by counsel.
A hearing will be conducted pursuant to Section 394.467 (7), F.S., at ___________ am pm on _____________ (date)
at_________________________________________________________________________________________________
The following physician(s) or clinical psychologist(s) are expected to testify in support of continued detention:
_____________________________________________ _______________________________________________
In addition, the following persons are also expected to testify in support of continued involuntary inpatient placement:
Name: ____________________________ _________________________ ______________________
Relationship ____________________________ _________________________ ______________________
Address ____________________________ _________________________ ______________________
____________________________ _________________________ ______________________
The person, the person’s guardian, or representative, or the administrator may apply for a change of venue for the
convenience of the parties or witnesses or because of the condition of the person.
The person has a right to an independent expert examination and if he/she cannot afford such an examination, one shall be
provided for him or her.
__________________________________________ _________________ ______________ am pm
Signature of Administrative Law Judge Date Time
__________________________________________
Typed or Printed Name of Administrative Law Judge
Certificate of Mailing
I hereby certify that I mailed the above and foregoing notice to the named parties by depositing the same in the United
States Post Office on the __________ day of ________________, __________ . In addition, I sent this notice by
registered or certified mail to each person listed below who was not given a copy by hand delivery.
____________________________________________________
Signature of Administrative Law Judge
cc: Check when applicable Person Guardian Guardian Advocate Representative Public Defender or
Private Attorney
See s. 394.4599(2)(a), [d], 394.467(7), Florida Statutes
CF-MH 3024, Oct 11 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Five Involuntary Inpatient Placement
_____________________________________________________________________________________
Baker Act Benchguide November 2016
251
K. Order for Continued Involuntary Inpatient Placement or for Release
IN RE: ________________________________________ CASE NO.: ____________________
Order for Continued Involuntary Inpatient Placement or for Release
This matter coming on to be heard, pursuant to the requirements of Section 394.467(7), Florida Statutes, that
the mental status and necessity to continue involuntary inpatient placement of persons be periodically
reviewed, and the person having
appeared in person appeared through counsel, the following findings of fact are made from the evidence
designated:
1. The person, on ___________________________________ , was involuntarily placed on a Court order.
Date
2. The person does does not continue to meet the criteria for involuntary inpatient placement.
This finding is determined from the testimony of ______________________________________________
and __________________________________________________________________. As evidenced by:
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
Based on the above findings of fact, the Administrative Law Judge makes the following conclusions:
On the basis of the above, it is hereby
ORDERED
The person be returned to involuntary inpatient placement pending the next periodic review
required by Section 394.467, Florida Statutes.
The person be processed for release from involuntary inpatient placement and be completely
discharged from the facility.
The person is eligible for and has applied for voluntary status.
ORDERED at
this _____________ day of ________________________ , _________________.
Date Month Year
______________________________________ ________________________________________
Printed Name of Administrative Law Judge Signature of Administrative Law Judge
cc: Check when applicable
Person Guardian Guardian Advocate Representative Public Defender Facility
Administrator
See s. 394.467(7), Florida Statutes
CF-MH 3031, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
252
Chapter Six: Involuntary Outpatient Services
I. Introduction
See generally section 394.4655, Florida Statutes, and rule 65E-5.285, Florida
Administrative Code.
The 2004 Florida Legislature enacted a major revision to the Florida Mental Health
Act by adding an involuntary outpatient placement provision to the involuntary
examination and involuntary inpatient placement provisions. This revision was
made effective on January 1, 2005. See ch. 2004-385, Laws of Fla.
The legislative revisions permit the administrator of a Baker Act receiving facility
or treatment facility to file a petition for involuntary placement in the circuit court
when inpatient or outpatient treatment is deemed necessary. § 394.463(2)(g)4.,
Fla. Stat.
The 2016 Legislature renamed involuntary outpatient placement as involuntary
outpatient services. Some references in text, forms, or FAQs might still use the
term “IOP” or the word “placement” instead of “services,” but this does not change
the meaning of the law or other document.
II. Rights of Persons
Rights of persons incorporated in the Florida Mental Health Act apply to all
persons whose services are governed by the Baker Act — voluntary or involuntary
and inpatient or outpatient. Each person must receive services, including those
under an involuntary outpatient services court order, “which are suited to his or her
needs, and which must be administered skillfully, safely, and humanely with full
respect for the [person’s] dignity and personal integrity.” § 394.459(4)(a), Fla. Stat.
III. Criteria
A person may be ordered to involuntary outpatient services upon a finding by the
court of clear and convincing evidence that each criterion below has been met.
Each allegation must be supported by evidence sufficient to reach the high level of
evidence required in the involuntary outpatient services hearing. Appellate courts
have found that expert opinions and conclusions are not sufficient, without
evidence to prove the allegations. The Florida Supreme Court has defined clear and
convincing evidence to mean “evidence that is precise, explicit, lacking in
confusion, and of such weight that it produces a firm belief or conviction, without

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
253
hesitation, about the matter in issue.” Fla. Stand. Jury Instr. (Civil) 405.4.
The criteria, set forth at section 394.4655(2), Florida Statutes, are as follows:
The person must be 18 years of age or older. Evidence of age must be
substantiated whenever there is any question about it.
The person has a mental illness. A diagnosis of mental illness must be
substantiated by two professionals as provided in section 394.4655(3)(a),
Florida Statutes, who have recently examined the person and whose
observations of the person’s condition are consistent with the statutory
definition of mental illness, pursuant to section 394.455(28), Florida
Statutes, and the clinical description of that diagnosis as described in the
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,
American Psychiatric Association, which may be obtained from the
American Psychiatric Association, 1000 Wilson Boulevard, Arlington, VA
22209-3901.
The person is unlikely to survive safely in the community without
supervision, based on a clinical determination. The clinical determination
must be substantiated by evidence of current or past behaviors.
The person has a history of noncompliance with treatment. The person’s
history of lack of compliance with treatment for mental illness must be
substantiated by evidence showing specific previous incidents in which the
person was noncompliant with treatment, including specific time periods.
The person has either
o at least twice within the last 36 months been involuntarily admitted to a
receiving or treatment facility or received mental health services in a
forensic or correctional facility or
o engaged in one or more acts of serious violent behavior toward self or
others, or attempts at serious bodily harm to self or others, within the
preceding 36 months.
In either of the above circumstances, official clinical or legal documents
must document that the person was in fact admitted to and treated at such
facilities in the required time period. Either circumstance must be
substantiated by evidence.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
254
The person is, as a result of mental illness, unlikely to voluntarily participate
in the recommended treatment plan and has either refused voluntary
placement or is unable to determine whether placement is necessary. This
finding must be substantiated by behaviors, events, and statements by the
person.
In view of person’s treatment history and current behavior, the person is in
need of involuntary outpatient services to prevent a relapse or deterioration
that would be likely to result in serious bodily harm to self or others, or a
substantial harm to his/her well-being. Evidence of the person’s treatment
history and current behavior must be presented, including time periods of
such treatment.
It is likely that the person will benefit from involuntary outpatient services.
Evidence must be presented to substantiate this.
All available less restrictive alternatives that would offer an opportunity for
improvement of the person’s condition have been judged to be inappropriate
or unavailable. Evidence must be presented to substantiate each less
restrictive alternative that was examined.
The person must meet all the above criteria.
IV. Petition
If the person is not released or transferred to voluntary status within 72 hours after
arrival at a receiving facility, a petition for involuntary placement must be filed
with the circuit court by the facility administrator within the 72-hour examination
period, or, if the 72-hour period ends on a weekend or legal holiday, the petition
must be filed no later than the next court working day thereafter. If involuntary
outpatient services are sought, the form titled “Petition for Involuntary Outpatient
Placement” (CF-MH 3130) can be used. A copy of the completed petition must be
retained in the person’s clinical record.
A petition by a receiving facility administrator must be filed in the circuit court
where the facility is located. This authorizes the person’s retention pending a
hearing. If the person has been stabilized and no longer meets the criteria for
involuntary examination, he/she must be released from the receiving facility while
awaiting the hearing on involuntary outpatient services. The petition must include
a certificate recommending placement completed by psychiatrist and a
psychologist or second psychiatrist, who have both examined the person within the

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
255
preceding 72 hours, that each of the criteria for involuntary outpatient services is
met. A copy of a proposed treatment plan must be attached. No fee can be charged
for filing the petition.
A petition by a treatment facility administrator must be filed in the circuit court
where the person will be living. A copy of the petition, the state mental health
discharge form, and a treatment plan prepared by the designated service provider
must be given to the DCF representative in the circuit where the person is to reside
at the time it is filed with the circuit court.
V. Service Provider
Prior to filing the petition for involuntary outpatient services, the receiving or
treatment facility administrator or DCF must identify the service provider that will
have primary responsibility for court-ordered treatment. If the person is currently
participating in outpatient treatment and is not in need of public financing for that
treatment, the person, “if eligible, may be ordered to involuntary treatment
pursuant to the existing psychiatric treatment relationship.” § 394.4655(3)(a)2.,
Fla. Stat. However, a proposed treatment plan must still be prepared, in accordance
with the law and rules, for submission to the court with the petition. A service
provider, in the context of the Baker Act, is defined as:
a receiving facility;
a facility licensed under chapter 397, Florida Statutes;
a treatment facility;
an entity under contract with DCF to provide mental health or substance
abuse services;
a community mental health center or clinic;
a psychologist;
a clinical social worker;
a marriage and family therapist;
a mental health counselor;
a physician;

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
256
a psychiatrist;
an advanced registered nurse practitioner;
a psychiatric nurse (as defined in the Baker Act); or
a qualified professional as defined in section 39.01, Florida Statutes (which
includes physician assistants).
§ 394.455(44), Fla. Stat. The department or receiving facility must designate which
service provider will be responsible for developing a treatment plan for the person
and for service provision. Recommended form titled “Designation of Service
Provider for Involuntary Outpatient Placement” (CF-MH 3140) may be used.
No petition for involuntary outpatient services may be filed with a court by a
receiving or treatment facility administrator unless a treatment plan complying
with the requirements of the law and rule is attached to the petition, along with a
certification from the service provider that:
the proposed services are available;
there is space for the person in the program;
there is funding available;
the services proposed are clinically appropriate as certified by an authorized
mental health professional; and
the service provider agrees to provide the services.
Recommended form titled “Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient
Placement” (CF-MH 3145) may be used.
VI. Treatment Plan
A service provider must prepare a written proposed treatment plan in consultation
with the person or the person’s guardian advocate for the court’s consideration in
an involuntary outpatient treatment order. The treatment plan must:
specify the nature and extent of the person’s mental illness;
address the reduction of symptoms; and

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
257
include measurable goals and objectives for the services and treatment
provided to help the person function in the community and to prevent a
relapse or deterioration.
Section 394.4655(3)(a)3., Fla. Stat. Services proposed in the treatment plan must
be deemed clinically appropriate by a physician, psychologist, clinical social
worker, mental health counselor, marriage and family therapist, or psychiatric
nurse.
The service provider selected by the receiving facility or DCF to develop/render a
service plan may select and supervise others to implement aspects of the treatment
plan. The service provider must certify to the court that the services in the plan are
currently available and that the service provider agrees to provide them.
The confidentiality provisions of the Baker Act have been revised for purposes of
determining whether a person meets the criteria for involuntary outpatient services
or for preparing the proposed treatment plan. While any release must be in
accordance with state and federal law, the clinical record may be released for this
purpose to the:
state attorney,
public defender or the person’s private legal counsel,
court, and
appropriate mental health professionals, including the service provider.
VII. County of Filing
The petition initiated by a receiving facility administrator must be filed in the
county where the facility is located.
The petition for involuntary outpatient services initiated by a treatment facility
administrator must be filed in the county where the person will be living after
discharge from the facility. It must be filed prior to the expiration of the
involuntary inpatient placement order. A copy of the “State Mental Health Facility
Discharge Form” (CF-MH 7001) must be attached to the petition. The service
provider designated by the department that will have primary responsibility for
service provision must provide a certification to the court, attached to the petition,
as to whether the services recommended in the discharge plan are available in the
local community and whether the provider agrees to provide those services. Also

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
258
attached to the petition must be an individualized treatment or service plan that
addresses the needs identified in the discharge plan developed by the treatment
facility. Recommended form titled “Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient
Placement (CF-MH 3145) may be used. This plan must have been deemed to be
clinically appropriate by a physician, clinical psychologist, clinical social worker,
mental health counselor, marriage and family therapist, or psychiatric nurse, as
defined in the Baker Act.
VIII. Notice of Petition
A copy of the petition for involuntary outpatient services and proposed treatment
plan must be provided within one working day after filing by the clerk of the court
to the:
respondent;
DCF;
guardian or representative;
state attorney, and
counsel for the respondent.
A notice of filing of the petition must also be provided by the clerk of court.
Recommended form titled “Notice of Petition for Involuntary Placement” (CF-MH
3021) or equivalent form adopted by the court may be used.
The person and his or her representative or guardian must be informed by the court
of the right to an independent expert examination and that if the person cannot
afford such an examination, the court will provide for one.
In August of 2005, the Chair of the Florida Trial Court Budget Commission
advised the chief judges and court administrators of all circuits that while the court
must appoint such an independent expert, the expert is a defense witness and not a
court expense. August 24, 2005, Commission Minutes, Agenda Item II.A.
Recommended form titled “Application for Appointment of Independent Expert
Examiner” (CF-MH 3022) may be used. The results of the examination by an
independent expert are confidential and not discoverable unless the expert is called
as a witness. § 394.467(6)(a)3., Fla. Stat.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
259
IX. Hearing
A hearing on the petition for involuntary outpatient services must be conducted
within five working days after the filing of the petition in the county in which the
petition is filed.
The person is entitled, with the concurrence of counsel, to at least one continuance
of the hearing, for a period of up to four weeks. Recommended form titled “Notice
to Court – Request for Continuance of Involuntary Placement Hearing” (CF-MH
3113) may be used.
The public defender must be appointed by the court within one court working day
after the petition is filed, unless the person is otherwise represented. Counsel for
the person must serve until the petition is dismissed, the court order expires, or the
person is discharged from placement. The state attorney represents the state as the
real party in interest in the proceedings.
The hearing must be conducted in a setting as convenient to the person as
consistent with orderly procedure and not likely to be harmful to the person. A
judge or magistrate may preside. If the facility administrator seeks to withdraw the
petition for involuntary outpatient services prior to the hearing, recommended form
CF-MH 3033, titled “Notification to Court of Withdrawal of Petition for Hearing
on Involuntary Inpatient or Outpatient Placement,” may be used. The facility must
retain a copy in the person’s clinical record. When a facility withdraws a petition
for involuntary placement, it must notify by telephone the court, state attorney,
attorney for the person, and guardian or representative within one business day of
its decision to withdraw the petition (see Fla. Admin. Code R. 65E-5.285(2)(d))
unless the decision is made within 24 hours prior to the hearing. In such cases, the
notification must be made immediately.
The court must hear testimony and evidence regarding the person’s competence to
consent to treatment. If the person is found incompetent, the court must appoint a
guardian advocate. The guardian advocate appointed by the court for a person who
has been found to be incompetent to consent to treatment must be discharged when
the person is:
discharged from an order for involuntary outpatient services or
involuntary inpatient placement; or
transferred from involuntary to voluntary status.
If the court determines the person instead meets the criteria for involuntary

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
260
inpatient placement, use of recommended form titled “Ex Parte Order for
Involuntary Inpatient Examination” (CF-MH 3001) may be used.
If the court determines the person meets the criteria for involuntary assessment,
protective custody, or involuntary admission, and issues an order, recommended
form titled “Order Requiring Involuntary Assessment and Stabilization for
Substance Abuse and for Baker Act Discharge of Person” (CF-MH 3114) may be
used.
“If at any time before the conclusion of the hearing on involuntary inpatient
placement it appears to the court that the person does not meet the criteria for
involuntary inpatient placement . . . but instead meets the criteria for involuntary
outpatient services, the court may order the person evaluated for involuntary
outpatient services.” § 394.467(6)(c), Fla. Stat.
X. Testimony
All testimony must be given under oath and must be recorded.
The court may waive the presence of the person from all or any part of the
hearing if consistent with the best interests of the person and the person’s
counsel does not object. Several appellate courts have ruled that if the
patient waives the right to be personally present and constructively present
through counsel, the trial court must certify through proper inquiry that a
respondent’s waiver is knowing, intelligent, and voluntary. The person may
refuse to testify at the hearing.
One of the two professionals who executed the involuntary outpatient
services certificate must be a witness at the hearing.
In addition to one of the two professionals who executed the petition, other
staff from the receiving or treatment facility who have direct knowledge of
how the person meets the criteria for involuntary outpatient services and are
expected to testify in support of the petition must be identified in the petition
and be present to testify at the hearing, as desired by the court.
The court shall also allow testimony from individuals, including family
members, deemed by the court to be relevant, regarding the person’s prior
history and how that prior history relates to the person’s current condition.
The testimony must be factual as to events and dates, rather than opinions
and conclusions.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
261
A representative of the designated service provider must be present to
provide testimony about the proposed treatment or service plan as desired by
the court.
XI. Court Order
If the court finds that the person meets all criteria for involuntary outpatient
services, it shall issue an order for a period of up to 90 days. Recommended form
titled “Order for Involuntary Outpatient Placement or Continued Involuntary
Outpatient Placement” (CF-MH 3155) may be used.
The court can’t order services that are not available in the person’s local
community, if no space is available, if funding isn’t available, if the treatment plan
hasn’t been certified as clinically appropriate by an authorized mental health
professional, and if an eligible service provider hasn’t agreed to provide the
recommended services.
This signed order must be given to the person, guardian, guardian advocate or
representative, counsel for the person, state attorney, and administrator of the
receiving or treatment facility, with a copy of the order retained in the person’s
clinical record.
A copy of the court order must also be sent by the service provider to DCF, via the
BA Reporting Center, within one working day after received from the court
accompanied by mandatory form titled “Cover Sheet to Department of Children
and Families” (CF-MH 3118) to:
BA Reporting Center
FMHI - MHC 2637
13301 Bruce B. Downs Blvd.
Tampa, FL 33612-3807
The court order and treatment plan must be part of the person’s clinical record.
XII. Continued Involuntary Outpatient Services
A. Criteria
If the person continues to meet the criteria for involuntary outpatient services, the
service provider must, prior to the end of the court order, file in the circuit court a
petition for continued involuntary outpatient services. The existing order remains
in effect until the continued involuntary outpatient services petition is disposed of.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
262
Criteria for continued involuntary outpatient services are identical to the criteria for
the original order, except that the 36-month time period for having (1) been at least
twice involuntarily admitted to a receiving/treatment facility or received mental
health services in a forensic or correctional facility, or (2) engaged in one or more
acts of serious violent behavior toward self/others, or attempts at serious bodily
harm to self/others, is not applicable in determining the appropriateness of
additional periods of involuntary outpatient services.
B. Petition
To request continued involuntary outpatient services, the service provider
administrator shall, at least ten days prior to the expiration of the period for which
the treatment was ordered, file a petition for continued involuntary outpatient
services with the court that issued the order for involuntary outpatient services. The
court must immediately schedule a hearing on the petition to be held within 15
days after the petition was filed. Recommended form titled “Petition Requesting
Authorization for Continued Involuntary Outpatient Placement” (CF-MH 3180)
may be used.
The petition must include:
a statement from the person’s physician or clinical psychologist justifying
the request;
a brief description of the person’s treatment during the time period in the
order; and
an individualized plan of continued treatment developed by the service
provider, in consultation with the person or the guardian advocate, if
applicable.
§ 394.4655(8), Fla. Stat.
C. Notice of Petition for Continued Involuntary Outpatient Services
The clerk of court must provide copies of the petition and attachments to the
person, DCF, guardian advocate, state attorney, and the person’s attorney.
The clerk of court must provide notice of the hearing. Recommended form titled
“Notice of Petition for Involuntary Placement” (CF-MH 3021) may be used.
Copies must be provided to the person, his or her attorney, the state attorney, and
guardian, guardian advocate or representative, with a copy of the notice filed in the

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
263
person’s clinical record.
Written notice of filing of petition for involuntary placement must contain:
Notice that the petition was filed with the with the criminal county court or
the circuit court, as applicable, in the county in which the individual is
hospitalized and the address of such court..
Notice that a public defender has been appointed to represent the person, if
the person is not otherwise represented.
The date, time, and place of the hearing, and the name of each examining
expert and every other person who is expected to testify in support of
continued involuntary outpatient placement.
Notice that the person, guardian/representative, health care surrogate or
proxy, or administrator may apply for a change of venue for the convenience
of the parties or witnesses or because of the person’s condition.
Notice that the person is entitled to an independent expert examination, and
that if he/she can’t afford an examination, the court will provide for one.
§ 394.4599(2)(d), Fla. Stat.
The public defender must be appointed and notified within one court working day,
and will represent the person until:
the petition is dismissed;
the order expires; or
the person discharged from placement.
The attorney for the person has access to the person, witnesses, and records, and
represents the interests of the person, regardless of the source of payment to the
attorney. The state attorney is appointed to represent the state as the real party in
interest, rather than the petitioner.
D. Hearing on Continued Involuntary Outpatient Services
The court may appoint a magistrate to preside over continued involuntary services
hearings.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
264
K
The person and his or her attorney may agree to a period of continued outpatient
placement without a court hearing. Should such a hearing be waived,
recommended form titled “Notice to Court of Waiver of Continued Involuntary
Outpatient Placement Hearing and Request for Order” (CF- MH 3185) may be
used.
If the person was previously found incompetent to consent to treatment, the court
must consider testimony and evidence regarding the person’s competence. The
guardian advocate must be dismissed if the person is found competent to make
decisions about his or her own treatment.
If the administrator of the service provider withdraws the petition for continued
involuntary outpatient services prior to the hearing, recommended form titled
“Notification to Court of Withdrawal of Petition on Involuntary Inpatient or
Outpatient Placement” (CF-MH 3033) may be used. The facility will retain a copy
of the notice in the person’s clinical record. When a facility withdraws a petition
for involuntary placement, it must notify the court, state attorney, public defender
or other attorney for the person, and guardian or representative by telephone within
one business day of its decision to withdraw the petition, unless the decision is
made within 24 hours prior to the hearing, in which case notification must be made
immediately. The same procedure must be repeated before expiration of each
additional period the person is placed in treatment.
E. Order for Continued Involuntary Outpatient Services
Based on the findings of the hearing, the court may extend the period of
involuntary outpatient commitment pending the next statutorily required periodic
hearing, release the person from involuntary outpatient services, or find the person
eligible for voluntary status. Recommended form titled “Order for Continued
Involuntary Inpatient Placement or for Release” (CF-MH 3031) may be used. A
copy of the completed order must be filed in the person’s clinical record and a
copy provided to the person, attorney, facility administrator, and guardian,
guardian advocate, or representative.
A copy of the order must be sent to the Agency for Health Care Administration by
the designated service provider, accompanied by mandatory form titled “Cover
Sheet to Agency for Health Care Administration” (CF-MH 3118).
XIII. Modification to Court Order for Involuntary Outpatient Services
After an order for involuntary outpatient placement or continued involuntary
outpatient services is entered, the provider and the person (or his or her substitute

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
265
decision maker, if appointed) may modify provisions of the treatment plan. Any
material modifications where parties agree require the provider to notice the
court. If material modifications are contested, the court must approve or
disapprove the modifications.
At any time material modifications are proposed to the court-ordered treatment
plan for which the person and any substitute decision maker agree, or if the person
or substitute decision maker objects to the modifications proposed by the service
provider or wishes to propose modifications not proposed by the service provider,
recommended petition titled “Notice to Court of Modification to Treatment Plan
for Involuntary Outpatient Commitment and/or Request for Approval of Material
Modifications to Plan” (CF-MH 3160) may be used.
XIV. Change of Service Provider
If the person who is subject to an order for involuntary outpatient services (or his
or her substitute decision maker, if appointed) objects to the service provider that is
court ordered to provide his or her treatment or services, recommended form titled
“Notice to Court of Modification to Treatment Plan for Involuntary Outpatient
Commitment and/or Petition Requesting Approval of Material Modifications to
Plan” (CF-MH 3160) may be used.
XV. Noncompliance with Court Order
If a physician has determined that the person who is subject to a court order for
involuntary outpatient services or continued involuntary outpatient services has
failed or refused to comply with the court-ordered treatment, and in his or her
clinical judgment efforts were made to solicit compliance and the person meets the
criteria for involuntary examination, the person may be brought to a receiving
facility pursuant to the involuntary examination requirements of the Baker Act.
Mandatory form titled “Certificate of a Professional Initiating Involuntary
Examination” (CF-MH 3052b) may be used.
If the person doesn’t meet criteria for involuntary inpatient placement, the person
must be discharged from the receiving facility.
The service provider must determine whether modifications should be made to the
existing treatment plan and must attempt to continue to engage the person in
treatment.
Some courts have considered whether contempt powers should be used to compel
compliance with the approved treatment plan. Two appellate cases, one related to

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
266
the Baker Act and the other to the Marchman Act, might be considered as reasons
why contempt should not be used:
C.N. v. State, 433 So. 2d 661 (Fla. 3d DCA 1983). A petition for the
involuntary hospitalization of C.N. was filed, and the court found that she
met the statutory criteria for involuntary placement, but ordered outpatient
treatment as the “least restrictive means of intervention.” After C.N. failed to
continue the outpatient treatment, she was found in contempt of court and
ordered into involuntarily placement. She appealed, and the appellate court
reversed, holding that “exercise of the court’s contempt power to compel
hospitalization and treatment was inappropriate. . . . The evidence presented
did not support a finding of contemptuous intent, an element of criminal
contempt” because all three physicians who testified at the contempt hearing
said C.N. had a personality problem related to her disorder that gave her
“difficulty in following directions.” It held further that “where a court has
ordered outpatient care . . . as an alternative to involuntary hospitalization,
that least restrictive intervention can be revoked and the patient deprived of
her liberty only in proceedings which substantially meet the requirements of
Section 394.467. There is no statutory authority for the court to retain
jurisdiction for the purpose of modifying an action taken on an earlier
petition. The imposition of a more restrictive intervention, i.e., involuntary
placement, requires, at the minimum, a new petition for involuntary
hospitalization, a notice of hearing and a hearing on the petition. For a court
to order involuntary hospitalization, it is not sufficient that the patient
merely failed to follow a plan for outpatient treatment.”
Steven Cole v. State, 714 So. 2d 479 (Fla. 2d DCA 1998). The circuit court
convicted Cole of indirect criminal contempt for violating its order to
complete a substance abuse treatment program and sentenced him to 90 days
in jail. He filed petitions for a writ of habeas corpus, a writ of certiorari to
quash the conviction and sentence, and a writ of mandamus (treated as a
petition for writ of prohibition) to prevent further improper proceedings in
his Marchman Act case. The appellate court issued the writs. While it held
that “the proceedings were flawed to an astonishing degree,” most of the
errors were not appealable because of time issues. But the conviction of
indirect criminal contempt was erroneous because “Cole was not given
meaningful prior notice of the charges against him” and the written
judgment “includes findings of fact that contradict the record.” Further, he
“was tried without notice to the public defender.” The Marchman Act
proceedings were “void for lack of subject matter and personal jurisdiction.”
Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
267
XVI. Discharge from Involuntary Outpatient Services
A service provider has a duty to (1) discharge a person at any time the order for
involuntary outpatient services or continued involuntary outpatient services expires
or at any time the person no longer meets the criteria for involuntary outpatient
services, or (2) transfer the person to voluntary status, if the person is able and
willing to provide express and informed consent.
Upon the person’s discharge, the service provider must send a notice of discharge
to the court. Recommended form titled “Notice of Release or Discharge” (CF-MH
3038) may be used. The administrator of the service provider will provide
notification to the person, guardian, guardian advocate, representative, attorney for
the person, and the court that ordered the treatment, and a copy of the notice must
be placed in the person’s clinical record.
At any time the person who is subject to an order for involuntary outpatient
services or continued involuntary outpatient services, or another person on his or
her behalf, believes any one of the criteria for involuntary outpatient services is no
longer met, a petition for termination of the order may be filed with the circuit
court having jurisdiction. Recommended form titled “Petition for Termination of
Involuntary Outpatient Placement Order” (CF-MH 3170) may be used. If the court
determines a hearing on the petition is to be conducted, a notice of the hearing, as
required by law, shall be provided by the clerk of court.
XVII. Alternatives to Involuntary Outpatient Services Orders
Use of the involuntary outpatient services provisions of the Baker Act have been
scarce and inconsistent, partly due to the lack of appropriate community-based
treatment programs. One circuit has continued to use the involuntary inpatient
placement provisions under section 394.467(6)(b), Florida Statutes, which permits
the court to order an individual not only to be treated at an appropriate receiving
facility, but to receive services from a receiving facility on an involuntary basis
for up to six months:
If the court concludes that the patient meets the criteria for
involuntary inpatient placement, it may order that the patient be
transferred to a treatment facility or, if the patient is at a treatment
facility, that the patient be retained there or be treated at any other
appropriate facility, or that the patient receive services, on an
involuntary basis, for up to 90 days. . However, any order for
involuntary mental health services in a treatment facility may be for

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
268
up to 6 months. The order shall specify the nature and extent of the
patient’s mental illness. The court may not order an individual with
traumatic brain injury or dementia who lacks a co-occurring mental
illness to be involuntarily placed in a state treatment facility. The
facility shall discharge a patient any time the patient no longer meets
the criteria for involuntary inpatient placement, unless the patient has
transferred to voluntary status. (emphasis added)
In addition to the above, section 394.469, Florida Statutes (emphasis added),
governing the discharge of involuntary patients, states:
(1) Power to discharge.--At any time a patient is found to no
longer meet the criteria for involuntary placement, the administrator
shall:
(a) Discharge the patient, unless the patient is under a criminal
charge, in which case the patient shall be transferred to the custody of
the appropriate law enforcement officer;
(b) Transfer the patient to voluntary status on his or her own
authority or at the patient’s request, unless the patient is under
criminal charge or adjudicated incapacitated; or
(c) Place an improved patient, except a patient under a
criminal charge, on convalescent status in the care of a
community facility.
(2) Notice.--Notice of discharge or transfer of a patient shall be
given as provided in s. 394.4599.
The above provision permits convalescent status in a less restrictive setting while
the person is still under an involuntary inpatient placement order. This allows the
individual to be returned to the receiving or treatment facility that arranged the
convalescent status within the term of the existing court order without requiring a
new involuntary examination or involuntary placement order.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
269
XVIII. Involuntary Outpatient Placement Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.)

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
270
XIX. Continued Involuntary Outpatient Placement Flowchart
(DCF flowchart; 2016 legislative changes are not incorporated.)

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
271
XX. Frequently Asked Questions
We have a person who we think meets the criteria for involuntary outpatient
services. He has a long history of noncompliance and is at high risk for a
stroke. My question is around the treatment plan. We have two mental health
residential treatment beds — a part of the unit. While they are on the locked
unit, the persons in the beds have the freedom to come and go and are there
voluntarily. Can we use an RTF bed placement as part of the involuntary
outpatient services treatment plan?
There should be no reason why a licensed residential treatment bed couldn’t be
used as part of an involuntary outpatient services treatment plan. It needs to be
clear to the individual and staff that the person must be able to enter and exit at
will; otherwise the involuntary inpatient placement provisions would apply.
If a person who has a plenary guardian is ordered to involuntary outpatient
services, does the court still have to seek the guardian’s authority to determine
housing and treatment, or does the IOP takes precedence?
There is no legal reason why an IOP court order would need to include housing or
treatment, because the circuit court has already authorized the plenary guardian to
make such decisions. It may be that the guardian believes that the additional IOP
court order will assist in getting the ward to comply, considering that a judge has
specifically ordered it rather than just authorizing the guardian to make the
decisions.
Can the court order treatment that is not readily available in the community?
No. A court order is based on a proposed treatment plan developed by a service
provider with the person. The plan cannot be submitted to the court for
consideration unless the provider has certified that:
sufficient services for improvement and stabilization are currently available
in the local community;
there is space available for the person;
funding is available for the program or service;
services are clinically appropriate as determined by a physician, clinical
psychologist, clinical social worker, or psychiatric nurse (each as defined in
the Baker Act); and

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
272
a service provider agrees to provide the services.
One of our group homes is providing treatment for a person under an
involuntary outpatient commitment order. The person has a guardian
advocate appointed who approves the course of treatment, including
medication (injections). The person is verbally refusing the injections. Can we
give the injection or is an emergency treatment order (ETO) required?
Regardless of whether the person is on an involuntary inpatient or involuntary
outpatient services order, if found by the court to be incompetent to consent to
treatment, he/she is also incompetent to refuse consent to treatment. If the guardian
advocate has been provided full disclosure so express and informed consent has
been obtained, and the GA has spoken directly to the doctor and the person about
the proposed treatment, the GA can provide the consent and no ETO is necessary.
An ETO is needed only when no legally authorized consent can be obtained.
Logistically this can be a problem in that the person may actually fight against the
injection. However, this would happen whether or not it was a result of an ETO.
Efforts need to be made to prevent any physical harm to the person or others in the
process. Physically holding a person during a procedure to forcibly administer
psychotropic medication is a physical restraint.
The involuntary outpatient provisions of the Baker Act refer to notifying the
court of material changes to a treatment plan ordered by the court. How is
“material” defined?
“Material” is defined in Black’s Law Dictionary as “Important; more or less
necessary; having influence or effect; going to the merits; having to do with matter,
as distinguished from form.”
Our CMHC is serving a man under an involuntary outpatient order. He
recently switched to a Medicaid HMO that contracts with a private mental
health center to provide services. The new provider would like for him to
remain under the IOP. Does the Baker Act allow us to submit to the court a
service modification for a different (private) provider? Should the new
provider submit a new treatment plan, listing it as the provider? Is the
modification the only documentation that is necessary if the treatment plan
remains the same? Does the new provider submit the modification or should
we?
This shouldn’t be a difficult matter if the man agrees with the change of provider.
If he agrees and the treatment plan remains the same — just a change of provider

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
273
— simple notice to the court should suffice. However, before doing that you
should get written confirmation from the new service provider that it agrees to be
the provider and that the services identified in the court-ordered treatment plan are
available and will be provided. The court may require such a statement since this
must have been provided by the original service provider and it remains a
condition of IOP. While a change of provider agreeable to the client may not be
“material,” it would always be appropriate to notify the court since this modifies
the terms of the court’s order.
Section 394.4655(7)(b)2., Florida Statutes, deals with this issue:
After the order for involuntary services is issued, the service provider
and the patient may modify the treatment plan. For any material
modification of the treatment plan to which the patient or, if one is
appointed, the patient’s guardian advocate agrees, the service provider
shall send notice of the modification to the court. Any material
modifications of the treatment plan which are contested by the patient
or the patient’s guardian advocate, if applicable, must be approved or
disapproved by the court consistent with subsection (3).
If a person on an involuntary outpatient order is re-hospitalized, is that order
void?
No. An order for involuntary outpatient services would not be invalidated by an
admission for involuntary examination. In fact, section 394.4655(7)(b)3., Florida
Statutes, provides:
If, in the clinical judgment of a physician, the patient has failed or has
refused to comply with the treatment ordered by the court, and, in the
clinical judgment of the physician, efforts were made to solicit
compliance and the patient may meet the criteria for involuntary
examination, a person may be brought to a receiving facility pursuant
to s. 394.463. If, after examination, the patient does not meet the
criteria for involuntary inpatient placement pursuant to s. 394.467, the
patient must be discharged from the facility. The involuntary
outpatient services order shall remain in effect unless the service
provider determines that the patient no longer meets the criteria
for involuntary outpatient services or until the order expires. The
service provider must determine whether modifications should be
made to the existing treatment plan and must attempt to continue to
engage the patient in treatment. For any material modification of the

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
274
treatment plan to which the patient or the patient’s guardian advocate,
if applicable, does agree, the service provider shall send notice of the
modification to the court. Any material modifications of the treatment
plan that are contested by the patient or a guardian advocate must be
approved or disapproved by the court consistent with subsection (3).
(emphasis added)
Section 394.4655(7)(b)1., Florida Statutes, provides:
If the court concludes that the patient meets the criteria for
involuntary outpatient services pursuant to subsection (2), the court
shall issue an order for involuntary outpatient services. The court
order shall be for a period of up to 90 days. The order must specify the
nature and extent of the patient’s mental illness. The order of the court
and the treatment plan must be made part of the patient’s clinical
record. The service provider shall discharge a patient from
involuntary outpatient services when the order expires or any
time the patient no longer meets the criteria for involuntary
placement. Upon discharge, the service provider shall send a
certificate of discharge to the court. (emphasis added)
How can organizations share information about treatment planning for
involuntary outpatient treatment, given protections offered by the state’s
Baker Act and the federal HIPAA law?
The Baker Act allows such exchange of information pursuant to involuntary
outpatient services. Even HIPAA permits release of information for purposes of a
person’s treatment.
What can be done when a person under an involuntary outpatient services
order refuses to comply with court-ordered treatment?
If a physician determines that:
the person has failed or refused to comply with the treatment ordered by the
court,
efforts were made to solicit compliance, and
the person may meet the criteria for involuntary examination,
the physician can then complete the appropriate sections of the Certificate of a

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
275
Mental Health Professional form (CF-MH 3052b) and have the person brought to a
receiving facility. It is important that all appropriate efforts to remind the person of
appointments, arrange transportation, provide medications, and other efforts be
demonstrated before noncompliance is found.
If it is determined after examination at a receiving facility that the person doesn’t
meet the criteria for involuntary inpatient placement, he/she must be discharged.
The service provider must determine whether modifications should be made to the
existing treatment plan and must attempt to continue to engage the person in
treatment.
Some courts have considered whether the court’s contempt powers should be used
to compel compliance with the approved treatment plan. The case of C.N. v. State,
433 So. 2d 661 (Fla. 3d DCA 1983) might be considered when determining
whether contempt should be used. A petition for the involuntary hospitalization of
C.N. was filed, and the court found that she met the statutory criteria for
involuntary placement, but ordered outpatient treatment as the “least restrictive
means of intervention.” After C.N. failed to continue the outpatient treatment, she
was found in contempt of court and ordered into involuntarily placement. She
appealed, and the appellate court reversed, holding that “exercise of the court’s
contempt power to compel hospitalization and treatment was inappropriate. . . .
The evidence presented did not support a finding of contemptuous intent, an
element of criminal contempt” because all three physicians who testified at the
contempt hearing said C.N. had a personality problem related to her disorder that
gave her “difficulty in following directions.” It held further that “where a court has
ordered outpatient care . . . as an alternative to involuntary hospitalization, that
least restrictive intervention can be revoked and the patient deprived of her liberty
only in proceedings which substantially meet the requirements of Section 394.467.
There is no statutory authority for the court to retain jurisdiction for the purpose of
modifying an action taken on an earlier petition. The imposition of a more
restrictive intervention, i.e., involuntary placement, requires, at the minimum, a
new petition for involuntary hospitalization, a notice of hearing and a hearing on
the petition. For a court to order involuntary hospitalization, it is not sufficient that
the patient merely failed to follow a plan for outpatient treatment.”

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
276
XXI. Selected Model Baker Act Forms for Involuntary Outpatient Services
Please note that these recommended forms were promulgated by DCF before
the 2016 statutory amendments and do not incorporate those changes.
A. Petition for Involuntary Outpatient Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ____________________________________ CASE NO.: __________________________
Petition for Involuntary Outpatient Placement
COMES NOW the Petitioner, _____________________________________________________ , and alleges:
1. That Petitioner is Administrator of: _________________________________________________________.
Name of Receiving or Treatment Facility Facility Address
2. That ____________ , is served in said receiving or treatment facility and has been examined at such facility
3. The last four (4) digits of the person’s social security number are ___________ and date of birth is _______
Date
4. That this petition is being filed within the following time frames: (Check one below)
A.
This person was admitted for involuntary examination and this petition is being filed within
the 72-hour examination period, or if the examination period ends on a weekend or legal
holiday, on the next court working day OR
B.
This person was transferred to involuntary status after examination or after refusing/revoking
consent to treatment or requesting discharge from the facility and this petition is filed within
two court working days.
C.
This person is currently on an order for involuntary inpatient placement, and this petition is
being filed before the expiration of that order
D. A petition for involuntary inpatient placement has been filed and a hearing is pending.
5. That attached hereto and by reference made a part hereof, are two (2) opinions and supporting facts
regarding the mental health of said person necessitating involuntary outpatient placement.
6. In addition to at least one of the two experts whose opinions are attached, the following persons may testify
in support of the petition for involuntary outpatient placement:
Witness Witness Witness
Name: ____________________ ____________________ ____________________
Relationship ____________________ ____________________ ____________________
Address ____________________ ____________________ _____________________
____________________ ____________________ _____________________
Telephone: (______)_____________ (______)_______________ (______)______________
CONTINUED OVER

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
277
Petition for Involuntary Outpatient Placement (Page 2)
COMES NOW THE PETITIONER and further alleges that:
1. A Guardian Advocate is necessary to act on the person’s behalf on issues related to express and
informed consent to:
Mental health treatment only, or
Both mental health and medical treatment decisions
And a Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of a Guardian
Advocate is attached;
OR
2. The person/respondent is competent to provide express and informed consent to his or her own
treatment or the person has a guardian authorized to consent to treatment and no Guardian Advocate is
requested.
____________________________________ _______________________ _____________ am pm
Signature of Facility Administrator or Designee Date Time
___________________________________________
Typed or Printed Name of Administrator or Designee
Person does or does not have a private attorney. If so, the name and address of the private attorney
is:
Private Attorney Name: ______________________________________________________________________
Private Attorney Address: _____________________________________________________________________
cc: The Clerk of the Court shall provide a copy of this petition to the: (Check when applicable and
initial/date/time when copy provided)
Individual
Date Copy
Provided
Time Copy Provided
Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Public Defender
am pm
Representative
am pm
State Attorney
am pm
Dept. of Children & Families
am pm
CONTINUED / SUPPORTING OPINIONS ON PAGE 3

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
278
Petition for Involuntary Outpatient Placement (Page 3)
First Opinion Supporting the Petition
I, ____________________________ a psychiatrist authorized to practice in the State of Florida, have personally examined
_________________________________ on _______________ (within 72 hours of the signing hereof) and find from such
Name of Person Date
examination that the person meets each of the following criteria for involuntary outpatient placement. Each of the
following required criterion must be alleged and substantiated by evidence in this petition.
1. The person is 18 years of age or older, corroborated by: ___________________________________________________
[2]. The person has a mental illness, as substantiated by the following evidence ___________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
[3]. The person is unlikely to survive safely in the community without supervision, based on a clinical determination, as
substantiated by the following evidence: __________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
4. The person has a history of lack of compliance with treatment for a mental illness, as substantiated by the following
evidence: __________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
5. The person has:
a. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving or treatment
facility as defined in s. 394.455, or has received mental health services in a forensic or correctional facility. The
36-month period does not include any period during which the person was admitted or incarcerated, as
substantiated by the following evidence: __________________________________________________________
__________________________________________________________________________________________
or
b. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm
to himself or herself or others, within the preceding 36 months, as substantiated by the following evidence _______:
__________________________________________________________________________________________
6. The person is, as a result of a mental illness, unlikely to voluntarily participate in the recommended treatment plan and
either he or she has refused voluntary placement for treatment after sufficient and conscientious explanation and disclosure
of the purpose of placement for treatment or he or she is unable to determine for himself or herself whether placement is
necessary, as substantiated by the following evidence: ______________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
7. In view of the person’s treatment history and current behavior, the person is in need of involuntary outpatient placement
in order to prevent a relapse or deterioration that would be likely to result in serious bodily harm to himself or herself or
others, or a substantial harm to his or her well-being as set forth in the criteria for involuntary examination, as substantiated
by the following evidence: ____________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
8. It is likely that the person will benefit from involuntary outpatient placement, as substantiated by the following
evidence; __________________________________________________________________________________________
__________________________________________________________________________________________________
AND
9. All available less restrictive treatment alternatives than court-ordered involuntary outpatient placement which would
offer an opportunity for improvement of said person’s condition have been judged to be inappropriate, based on contact
with the following programs/agencies: ___________________________________________________________________
__________________________________________________________________________________________________
_______________________________________ _______________________ _______________ am pm
Signature of Psychiatrist Date Time
_______________________________________ __________________________________
Typed or Printed Name of Psychiatrist License Number
CONTINUED OVER

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
279
Second Opinion Supporting the Petition (page 4)
I,________________________________________, a psychiatrist, clinical psychologist, licensed physician *,
psychiatric nurse *, authorized to provide a second opinion on this petition pursuant to Section 394.467 (2), F.S., have
personally examined ____________________________ on___________________, (within 72 hours of signing hereof), and find
Name of Person Date
that he/she meets the criteria for involuntary outpatient placement as stated in this petition. Observations and supporting evidence
which support this opinion are: ______________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
________________________________________________________________________________________________________
_________________________________________ ___________________ ___________ am pm
Signature of Examiner Date Time
_________________________________________ _________________________ ___________________
Typed or Printed Name of Examiner Profession License Number
*I certify that the county in which the person is detained has less than 50,000 population and no psychiatrist or psychologist is
available to provide the second opinion.
______________________________________________________________ ___________________________
Printed Name and Signature of Administrator or Designee Date
* A licensed physician or psychiatric nurse may only provide such second opinion in counties of less
than 50,000 population in cases where the facility administrator certifies that no psychiatrist or clinical
psychologist is available to provide the second opinion (by countersigning above).
See s. 394.4599(2)[d]3, 394.467, Florida Statutes BAKER ACT
CF-MH 3130, Nov 11 (Recommended Form)

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
280
B. Designation of Service Provider for Involuntary Outpatient Placement
Designation of Service Provider for Involuntary Outpatient Placement
Pursuant to chapter 394.4655, Florida Statutes, a petition for Involuntary Outpatient Placement has been filed to
require ____________________________________ to comply with a treatment plan approved by the court.
The following service provider has been identified by:
______________________________________, a representative of the Department of Children and Families, or
____________________________________________, a representative of a designated receiving facility
Name of Assigned Service Provider:
Address of Provider:
Phone Number of Provider:
The service provider will have primary responsibility for service provision under an order for involuntary outpatient placement.
The service provider will prepare a written proposed treatment plan, in consultation with the person or the person’s guardian,
guardian advocate, or health care surrogate/proxy, if appointed, to be attached to the petition for involuntary outpatient
placement for the court’s consideration for inclusion in the involuntary outpatient placement order. The Baker Act requires that
each person shall have an opportunity to assist in preparing and reviewing such a plan prior to its implementation and that the
plan shall include a space for the person’s comments.
For purpose of determining whether a person meets the criteria for involuntary outpatient placement or for preparing the
proposed treatment plan, the clinical record may be released to the state attorney, the person’s attorney, and to the appropriate
mental health professionals, including the proposed service provider, in accordance with federal and state law.
The treatment plan must specify the nature and extent of the person’s mental illness. The treatment plan must also address the
reduction of symptoms that necessitate involuntary outpatient placement and include measurable goals and objectives for the
services and treatment that will be provided to treat the person’s mental illness and to assist the person in living and functioning
in the community or to attempt to prevent a relapse or deterioration.
Service providers may select and provide supervision to other individuals to implement specific aspects of the treatment plan.
The services in the treatment plan must be deemed to be clinically appropriate by a physician, clinical psychologist, psychiatric
nurse, mental health counselor, marriage and family therapist, or clinical social worker, as defined in s. 394.455, Florida Statutes,
who consults with, or is employed or contracted by, the service provider.
The service provider must certify to the court in the proposed treatment plan whether sufficient services for improvement and
stabilization are currently available in the local community, whether there is space available to serve this person, that funding is
available to finance the care, and whether the service provider agrees to provide those services. If the service provider certifies
that the services or funding required by the proposed treatment plan are not available, the petitioner may not file the petition.
A petition for Involuntary Outpatient Placement will be filed with the circuit court no later than ___________________________.
A copy of the proposed treatment plan developed by the assigned service provider, in consultation with the person, must be
attached, including a certification by the service provider that the proposed services and funding are available to support the
proposed treatment/service plan. The service provider shall also provide a copy of the of the proposed treatment plan to the
person and the administrator of the receiving facility.
The service provider identified above shall prepare a treatment plan, consistent with the above requirements, no later than
___________________ to be attached to the petition for involuntary outpatient placement, unless the service provider cannot
certify the availability of funded services to meet the person’s needs.
_________________________________________________ _________________________
Signature of DCF Receiving Facility representative Date
__________________________________________________ ___________________________________________
Printed Name of Representative Address and Telephone Number of Representative
See s. 394.4655(2)(a), Florida Statutes
CF-MH 3140, Sept 06 (obsoletes previous edition) (Recommended Form)

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
281
C. Proposed Individualized Treatment Plan for Involuntary Outpatient
Placement and Continued Involuntary Outpatient Placement
Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient Placement
Pursuant to chapter 394.4655, Florida Statutes, a petition for Involuntary Outpatient Placement has been filed to
require ___________________________________________ to comply with a treatment plan approved by the court.
The following proposed treatment plan has been developed in consultation with the above named person (or his/her
legally authorized substitute decision-maker, if appointed) for the court’s consideration by the following service
provider designated by
the Department of Children and Families or a designated receiving facility.
Name of Assigned Service Provider:
Name & Credentials of Person Developing the Treatment Plan:
Address:
Phone Number:
The nature and extent of the person’s mental illness is as follows:
The following specific services are proposed in this treatment plan, including the specific service
to be provided, the organization to provide each service, the licensure or other credentials of the
organization or professional to provide each service, and the frequency and duration of each
service:
1. Services that will reduce symptoms that necessitate involuntary outpatient placement, including measurable goals
and objectives for the services and treatment that will be provided to treat the person’s mental illness:
CONTINUED OVER

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
282
Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient Placement
(page 2)
2. Services that will reduce symptoms, including measurable goals and objectives for the services and treatment, that
are provided to assist the person in living and functioning in the community.
3. Services that will reduce symptoms, including measurable goals and objectives, for the
services and treatment that are provided to attempt to prevent a relapse or deterioration:
Service providers may select and provide supervision to other individuals to implement specific aspects of the treatment plan.
Other individuals than those employed by the above named service provider, and their credentials, who are expected to assist in
providing the services described in this proposed treatment plan are:
CONTINUED OVER

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
283
Proposed Individualized Treatment Plan for
Involuntary Outpatient Placement and Continued Involuntary Outpatient Placement
(page 3)
I am a physician, clinical psychologist, psychiatric nurse, mental health counselor, marriage and family therapist,
or clinical social worker, as defined in s. 394.455, F.S. I consult with, or am employed or contracted by, the service provider
and I have determined that the services, personnel, and organizations described in this proposed treatment plan are clinically
appropriate.
________________________________________ _____________________________ ___________________
Signature of Clinical Professional Printed Name of Clinical Professional Date
The service provider certifies to the court that all services described in the proposed treatment plan for person’s
improvement and stabilization are:
Currently available in the local community There is space available to serve this person
Funding is available to finance the care, and The service provider agrees to provide those services.
The nature and extent of the person’s involvement in the preparation of this proposed treatment plan is as follows:
Comments about the proposed treatment plan by the person are as follows:
________________________________ ______________________________ ____________________
Signature of Preparer of Plan Printed Name of Preparer of Plan Date
The service provider shall also provide a copy of the proposed treatment plan to the person and the
administrator of the receiving facility. For persons in state treatment facilities who are ordered to
involuntary outpatient treatment, a copy of the state mental health discharge form must be sent by the
treatment facility to a department representative in the county where the person will be residing, which
is the county where the petition must be filed.
See s. 394.467(6)(c), Florida Statutes
CF-MH 3145, Sept 06 (obsoletes previous edition) (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
284
D. Order for Involuntary Outpatient Placement or Continued Involuntary
Outpatient Placement
IN THE CIRCUIT COURT OF THE ________________ JUDICIAL
CIRCUIT, IN AND FOR ____________________ COUNTY, FLORIDA
IN RE: _________________________, Case No.: _____________________
ORDER FOR INVOLUNTARY OUTPATIENT PLACEMENT
OR CONTINUED INVOLUNTARY OUTPATIENT PLACEMENT
This matter came to be heard pursuant to s.394.4655, F.S., and on Petition for Involuntary Outpatient
Placement or, Petition for Continued Involuntary Outpatient Placement, and the Court being fully advised in
the premises, finds by clear and convincing evidence as follows:
1. The above-named person has been represented by counsel; said person appeared at the hearing, or
presence at the hearing was waived, without objection of said person’s counsel.
2. The above-named person meets the following criteria for involuntary outpatient placement pursuant to
s.394.4655(1), F.S.: the person is 18 years of age or older; has a mental illness; is unlikely to survive safely
in the community without supervision, based on a clinical determination; and, has a history of lack of
compliance with treatment for a mental illness.
3. The above-named person has: (not applicable to continued involuntary outpatient placement)
A. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving
or treatment facility as defined in s.394.455, or has received mental health services in a forensic or
correctional facility; or
B. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious
bodily harm to self or others, within the preceding 36 months.
4. The above-named person is, as result of mental illness, unlikely to voluntarily participate in the
recommended treatment plan and has refused voluntary placement for treatment after sufficient and
conscientious explanation and disclosure of the purpose of placement for treatment, or is unable to determine
whether placement is necessary.
5. The above-named person’s treatment history and current behavior mandates the conclusion that the person
is in need of involuntary outpatient placement in order to prevent a relapse or deterioration that would be
likely to result in serious bodily harm to the person or others, or a substantial harm to his or her well-being
through neglect or refusal to care for self as set forth in s.394.463 (1), F.S..
6. It is likely that the above-named person will benefit from involuntary outpatient placement. All available
less restrictive treatment alternatives which would offer an opportunity for improvement of said person’s
condition are inappropriate.
7. The treatment plan which is attached hereto specifies the nature and extent of the above-named person’s
mental illness and specifies the outpatient treatment to be provided. The treatment plan contains a
certification to the court that sufficient services for improvement and stabilization are currently available,
funded, and that the service provider agrees to provide those services.
8. The services described in the treatment plan are clinically appropriate. This finding is supported by evidence
presented, including the testimony of _______________________________________________
9. The Court considered testimony and evidence regarding the above-named person’s competence to consent
to treatment. The person is found to be competent, incompetent to consent to treatment. If found to
be incompetent, a guardian advocate is appointed by separate order.
10. If the petition was referred to and heard by a Magistrate, the Magistrate’s Report and Recommendation are
attached, incorporated by reference, and adopted by the Court.

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
285
Whereupon, IT IS ORDERED that the above-named person be treated as an outpatient in accordance
with the treatment plan attached hereto, for a period not to exceed 6 months from the date of this order, or
________________________, or until discharged by the administrator or transferred to voluntary status.
DONE AND ORDERED in ____________ County, Florida, this _____ day of ____________, 20___.
_________________________________ __________________________________
Printed Name of Circuit Court Judge Signature of Circuit Court Judge
See s. 394.4655(6)(c), Florida Statu[t]es
CF-MH 3155, Feb 05 (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
286
E. Notice to Court of Modification to Treatment Plan for Involuntary
Outpatient Placement and/or Petition Requesting Approval of Material
Modifications to Plan
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Notice to Court of Modification to Treatment Plan for
Involuntary Outpatient Placement and/or
Petition Requesting Approval of Material Modifications to Plan
This court issued an order on _______________ requiring :
involuntary outpatient placement OR continued involuntary outpatient placement for the above-named person.
Material modifications to the treatment plan previously approved by the Court
For which the person or the person’s guardian or guardian advocate, if appointed AGREE have been made.
For which the person or the person’s guardian or guardian advocate, if appointed DO NOT AGREE are being
proposed for the court’s consideration.
A hearing is requested to review the proposed changes for which the person or the person’s guardian
or guardian advocate, if appointed, do not agree and the reasons for the objections to the proposed
changes.
The changes or proposed changes to the currently approved treatment plan, including why the
modifications are necessary and appropriate, are as follows: ____________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Any objections to the changes or proposed changes to the currently approved treatment plan by the person
or the person’s guardian or guardian advocate, if appointed, are as follows: ______________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
If this petition is filed by the service provider, a copy of the complete treatment plan, including proposed changes, is attached to
this filing.
____________________________________ ____________________________ ____________
Signature of Petitioner Printed Name of Petitioner Date
Person Guardian Guardian Advocate Service Provider Attorney for Person
__________________________________________________________________________________
Printed Name of Petitioner Printed Address and Telephone Number of Petitioner
ORDERED
That the proposed changes to the currently approved treatment plan are:
Approved
Disapproved
DONE AND ORDERED in __________________ County, Florida, this _____date of __________, 20____
_______________________________________ __________________________________
Signature of Circuit Court Judge Printed Name of Circuit Court Judge
Pursuant to 394.4655(6)(b)3, Florida Statutes,
See s. 394.467(6)(c), Florida Statutes
CF-MH 3160, Feb 05 (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
287
F. Petition for Termination of Involuntary Outpatient Placement Order
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ___________________________________ CASE NO.: __________________________
Petition for Termination of Involuntary Outpatient Placement Order
COMES NOW the petitioner, _________________________ alleging that _____________________
No longer meets one or more of the following criteria for involuntary outpatient placement:
The person is 18 years of age or older;
The person has a mental illness;
The person is unlikely to survive safely in the community without supervision, based on a clinical determination;
The person has a history of lack of compliance with treatment for a mental illness;
The person has:
1. At least twice within the immediately preceding 36 months been involuntarily admitted to a receiving or treatment
facility as defined in s. 394.455, or has received mental health services in a forensic or correctional facility. The
36-month period does not include any period during which the person was admitted or incarcerated; or
2. Engaged in one or more acts of serious violent behavior toward self or others, or attempts at serious bodily harm to
himself or herself or others, within the preceding 36 months;
The person is, as a result of a mental illness, unlikely to voluntarily participate in the recommended treatment plan and
either he or she has refused voluntary placement for treatment after sufficient and conscientious explanation and
disclosure of the purpose of placement for treatment or he or she is unable to determine for himself or herself whether
placement is necessary;
In view of the person’s treatment history and current behavior, the person is in need of involuntary outpatient placement
in order to prevent a relapse or deterioration that would be likely to result in serious bodily harm to himself or herself
or others, or a substantial harm to his or her well-being as set forth in s. 394.463(1);
It is likely that the person will benefit from involuntary outpatient placement; and
All available less restrictive treatment alternatives which would offer an opportunity for improvement of said person’s
condition have been judged to be inappropriate based on contact with the following programs/agencies:
For each criteria checked above that the petition alleges is not currently met, substantiating evidence is provided as
follows: ______________________________________________________________________________________
_____________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________
Wherefore, it is requested that the Court issue an order terminating its order issued on ______________________
requiring involuntary outpatient placement.
____________________________________ _________________ __________ am pm
Signature of Petitioner Date Time
Person Guardian Guardian Advocate Service Provider Attorney for Person
____________________________________ ____________________________________
Printed or Typed Name of Petitioner Address of Petitioner
See s. 394.467(6)(c), Florida Statutes
CF-MH 3170, Feb 05 (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
288
G. Petition Requesting Authorization for Continued Outpatient Placement
IN RE: _______________________________________ CASE NO.: _____________________
Petition Requesting Authorization for Continued Involuntary Inpatient
Placement
The petition of __________________________________________________________ who is the
Administrator of ___________________________________________________________ Facility shows that:
1. The above named person, _______________________________ of _______________________ County,
Florida, is currently in the aforesaid facility and was admitted to this facility on ____________________ .
Date
2. That according to the provisions of Section 394.467 (7), F.S., this person may not be retained after
_____________________, (Date) without an order authorizing continued involuntary inpatient placement.
3. That the person continues to meet the criteria for involuntary inpatient placement pursuant to Section
394.467(1), F.S., and
that legally authorized period has nearly expired, or
the person was admitted while serving a criminal sentence whose sentence will expire on _______ , or
Date
the person was placed while a minor and will reach the age of majority on _________________.
Date
Wherefore, it is requested an Order be issued authorizing this Facility to retain the person for a period not to
exceed six (6) months.
_____________________________________________ ____________ __________ am pm
Signature of Administrator or Designee Date Time
_____________________________________________
Printed or Typed Name of Administrator or Designee
CONTINUED OVER

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
289
Petition Requesting Authorization for Continued Involuntary Placement (Page 2)
Physician’s or Clinical Psychologist’s Statement
I hereby state that the above named person continues to meet the criteria for involuntary placement.
Behavior which supports this opinion is: __________________________________________________
___________________________________________________________________________________
___________________________________________________________________________________
Person’s treatment during placement was: _________________________________________________
___________________________________________________________________________________
___________________________________________________________________________________
Less restrictive settings which were investigated and the reasons they were ruled out are as follows: ___
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Support for facts in this statement is attached.
The individualized treatment plan for the person is attached.
____________________________________________________ _______________ _________ am pm
Signature of Physician Clinical Psychologist Date Time
________________________________________ _______________________________
Printed Name of Physician/Clinical Psychologist License Number
File this completed form with the Administrative Law Judge.
Person does or does not have a private attorney. If so, the name and address of the
private attorney is:
Private Attorney Name: ________________________________________________________________
Private Attorney Address: ______________________________________________________________
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
Public Defender or
Private Attorney
am pm
See s. 394.467(7), Florida Statutes
CF-MH 3035, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Six Involuntary Outpatient Services
_____________________________________________________________________________________
Baker Act Benchguide November 2016
290
H. Notice to Court of Waiver of Continued Involuntary Outpatient Services
Hearing and Request for an Order
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ______________________________ CASE NO.: ______________________
Notice to Court of Waiver of Continued Involuntary Outpatient Placement Hearing
And Request for an Order
________________________________, a person being treated under an Order for Involuntary Outpatient
Placement by __________________________________ (service provider) and who has been found by
the court to be competent to consent to make decisions about his or her treatment, has agreed to a period
of continued involuntary outpatient placement without a court hearing.
As counsel for this person, I agree to this waiver of hearing and request the issuance of an order for
continued involuntary outpatient placement for a period of ______________________ (up to six months)
_________________________________________ _____________________
Signature of Person Agreeing to Waiver of Hearing Date of Person’s Signature
_________________________________________ _____________________ _____________________
Signature of Counsel Printed Name of Counsel Date
cc: Person Service Provider State Attorney Guardian Guardian Advocate Representative
See s. 394.4655(7)(d), Florida Statutes
CF-MH 3185, Feb 05 (Recommended Form) BAKER ACT

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
291
Chapter Seven: Rights of Persons with Mental Illnesses
I. In General
The Baker Act ensures many rights to persons who have mental illnesses. See
§ 394.459, Fla. Stat.; Fla. Admin. Code R. 65E-5.140. Some of these rights are as
follows:
Individual dignity: All constitutional rights are ensured, and persons must
be treated in a humane way while being transported or treated for mental
illness.
Treatment: The Baker Act prohibits the delay or denial of treatment due to
a person’s inability to pay and requires prompt physical examination after
arrival, requires treatment planning to involve the person, and requires that
the least restrictive appropriate available treatment be used based on the
individual needs of each person.
Express and informed consent: People are encouraged to voluntarily apply
for mental health services when they are competent to do so, choose their
own treatment, and decide when they want to stop treatment. The law
requires that consent be voluntarily given in writing by a competent person
after sufficient explanation to enable the person to make well-reasoned,
willful, and knowing decisions without any coercion.
Quality of treatment: The Baker Act requires medical, vocational, social,
educational, and rehabilitative services suited to each person’s needs to be
administered skillfully, safely, and humanely. Use of restraint, seclusion,
isolation, emergency treatment orders, physical management techniques, and
elevated levels of supervision are regulated. Grievance procedures and
complaint resolution are required.
Communication, abuse reporting, and visits: Persons in mental health
facilities have the right to communicate freely and privately with persons
outside the facilities by phone, mail, or visitation. If communication is
restricted, written notice must be provided. No restriction of calls to the
Abuse Registry or to the person’s attorney is permitted under any
circumstances.
Care and custody of personal effects: Persons may keep their own clothing

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
292
and personal effects, unless they are removed for safety or medical reasons.
If they are removed, a witnessed inventory is required.
Voting in public elections: Persons are guaranteed the right to register and
vote in any elections for which they are qualified voters.
Habeas corpus: Persons are guaranteed the right to ask the court to review
the cause and legality of the person’s detention or unjust denial of a legal
right or privilege or an authorized procedure.
Treatment and discharge planning: The Baker Act guarantees the
opportunity to participate in treatment and discharge planning and to seek
treatment from the professional or agency of the person’s choice upon
discharge.
Sexual misconduct prohibited: Any staff member who engages in sexual
activity with a person served by a receiving/treatment facility is guilty of a
felony. Failure to report such misconduct is a misdemeanor.
Right to a representative: There is a right to a representative selected by
the person (or by the facility when the person can’t/won’t make the
selection) when admitted on an involuntary basis or transferred from
voluntary to involuntary status. The representative must be promptly notified
of the person’s admission and all proceedings and restrictions of rights,
receives a copy of the inventory of the person’s personal effects, has
immediate access to the person, and is authorized to file a petition for a writ
of habeas corpus on behalf of the person. The representative can’t make any
treatment decisions, access or release the person’s clinical record without the
person’s consent, or request the transfer of the person to another facility.
Confidentiality: All information about a person in a mental health facility is
maintained as confidential and released only with the consent of the person
or a legally authorized representative. However, certain information may be
released without consent to the person’s attorney, in response to a court
order (after a good cause hearing), after a threat of harm to others, or in other
very limited circumstances. Persons in mental health facilities have the right
to access their clinical records.
Violation of rights: Anyone who violates or abuses any rights or privileges
of persons provided in the Baker Act is liable for damages as determined by
law.

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
293
II. Frequently Asked Questions
A. In General
The Baker Act uses terms such as “shall,” “may,” “may not,” etc. What are
the legal differences of these terms?
This staff in the Florida Legislature Bill Drafting Office state as follows (see pp.
17–18 of the Florida Senate Manual for Drafting Legislation (6th ed. 2009)):
“Shall” requires.
“May” grants permission.
“May not” prohibits — it is not in any way permissive as some believe.
If a federal and a state statute are in conflict, which one takes precedence?
When a federal law and a state law are in conflict, the federal law generally takes
precedence. Where both laws deal with a subject and are not in conflict, both laws
must be followed. The law most protective of the individual’s rights will generally
prevail. Generally, if two state laws governing the same issue are in conflict, the
more specific law takes precedence over the more general law.
Should all patients receive a copy of their rights, even if they are involuntary
and incompetent to consent? Should we amend the recommended form to
reflect the patients’ responsibilities while they are at our hospital to include
that their financial obligations should be fulfilled as promptly as possible, that
they may be civilly or criminally liable if they deliberately hurt another
patient/employee or destroy or steal property, etc.?
The Baker Act requires that all persons, regardless of age, stage of development,
legal status, or competency, be provided with a written copy and verbal
explanation of their rights, along with copies to their designated representative and
substitute decision maker. This must be documented in the chart. The CF-MH
3103 form generally used for this purpose could be amended if you wish, but it
might be better if the responsibilities of the patients are listed on a separate form.
I work at a receiving facility for persons who are age 55 and over. Most of the
patients have guardian advocates because they suffer from different stages of
dementia. When involuntary patients are served with court-related paper
work, they become extremely agitated, causing unnecessary stress. Do these
patients need to see/receive this paper work? Most of these patients don’t
understand and/or misinterpret what they are looking at.

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
294
The law requires that the person who is subject of an involuntary placement
petition be provided notice of the filing of the petition, along with his or her
guardian, guardian advocate, attorney, and representative. While sensitivity by
staff to the feelings of persons served is commendable, deprivation of liberty
entailed in a Baker Act proceeding is sufficient to require due process — part of
this is being advised of such proceedings. No exception is made when a person
lacks capacity. If the notice isn’t given as required by law, it could result in any
order for placement being denied by the court or reversed by an appellate court.
Does a patient have the right to request a transfer from one receiving facility
to another?
Yes. A patient or the guardian, guardian advocate, or health care surrogate/proxy
can request a transfer between public and private receiving facilities and between
private receiving facilities. The facility to which the person would be transferred
must approve the transfer in advance. In the case of a transfer from a private to a
public receiving facility, the cost of the transfer is the responsibility of the
transferring facility. A public facility must respond within two working days after
the receipt of the transfer request, except from a hospital that has treated a person’s
emergency medical condition, in which case the patient must be transferred within
12 hours. In any transfer situation, the federal EMTALA law prevails where a
conflict with state law exists.
Does a person or someone on his or her behalf have the right to request a
change of physicians?
The relationship between doctor and patient could be considered a contract, and if
one of the two parties wishes to terminate or change the conditions of the contract
he or she may do so. If a person wants to terminate the relationship with his or her
psychiatrist and retain another psychiatrist instead, this should be allowed unless
there is some very unusual reason for disapproving it, such as daily requests for
change of physician, drug seeking behavior, etc., in which case it should be
referred to the hospital’s medical review process.
If a person has an emergency medical condition and cannot or will not
provide informed consent to examination and treatment, can the person be
Baker Acted in order to authorize these procedures?
No. The Baker Act is Florida’s Mental Health Act and it can’t be used to authorize
medical intervention, with the exception of the physical examination of each
person within 24 hours of arrival at a receiving facility. Other statutes must be

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
295
used, including chapter 395 (hospitals), 401 (EMS), 765 (advance directives), 744
(guardianship), or 415 (adult protective services), or rule 5.900, Florida Probate
Rules, governing expedited medical treatment.
If it is posted as part of our protocol, can we lock patients out of their rooms
during group times when they refuse to attend group?
Neither the Baker Act law nor the administrative rules prohibit locking patients out
of their rooms. You would need to check your national accrediting standards as
well as the federal Conditions of Participation (developed by Health and Human
Services (HHS) and Centers for Medicare and Medicaid Services (CMS)) to ensure
that they don’t prohibit the practice. If this practice is used, it might be limited to
when treatment activities are conducted. Each facility — public and private — is
required to post the times of daily activities as described in rule 65E-5.1601,
Florida Administrative Code (General Management of the Treatment
Environment). Locking people out of their rooms when therapeutic activities aren’t
scheduled, for the convenience of staff, would not be appropriate.
A police officer initiated a Baker Act proceeding for a person after a suicide
attempt and took him to an ER. The person was discharged the following day
after the psychiatrist certified that he did not meet Baker Act criteria. The
person is very upset with the police because she received an itemized bill from
the ER for $4,429.23.
The Baker Act doesn’t speak to the issue of who pays for care initiated under the
Act. The Legislature appropriates a very limited amount of funding to support
public receiving facilities, which are required to charge fees on a sliding scale
based on ability to pay. Care at private receiving facilities or other hospitals are the
responsibility of the person or the person’s insurer, if any. The law requires law
enforcement officers to take any person they have reason to believe meets the
criteria of the Act to the appropriate or nearest receiving facility, unless they
believe the person to have an emergency medical condition, in which case the
person is to be taken to the nearest ER regardless of whether it is designated as a
receiving facility. Officers aren’t expected to be diagnosticians. The situation you
describe sounds as though it was handled appropriately by all concerned — the law
enforcement officer and the receiving facility.
The Florida Attorney General has addressed the issue of payment in several
opinions, including:
Op. Att’y Gen. Fla. 07-11 (2007), regarding hospital authorities and

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
296
undocumented immigrants: “The intent of the West Volusia Hospital
Authority’s enabling legislation appears to be to provide medical services to
those indigents who are living within the district. . . . [T]he term ‘residents
of the district’ . . . was intended by the Legislature as a pure residence
requirement, and not as a requirement for domicile, legal residence, or
citizenship. Thus, the enabling legislation for the authority would appear to
permit the authority to provide services to otherwise qualified indigent
illegal aliens living within the district. Inasmuch as Chapter 04-421, Laws of
Florida, does not distinguish between the types of indigent residents, it
appears that the hospital authority should provide healthcare access to these
aliens on the same basis as other indigent residents.” The opinion quoted
Warren v. Warren, 75 So. 35, 42 (Fla. 1917): “Any place of abode or
dwelling place constitutes a ‘residence,’ however temporary it may be, while
the term ‘domicile’ relates rather to the legal residence of a person, or his
home in contemplation of law. As a result one may be a resident of one
jurisdiction although having a domicile in another.”
Op. Att’y Gen. Fla. 93-49 (1993), regarding who is responsible for the
payment of an involuntary Baker Act placement: The opinion advised the
Lafayette County Board of County Commissioners that “[t]he county is not
the primary source for reimbursement of hospital costs for the treatment of
an involuntary Baker Act commitment. However, a county may be liable for
such payments in the event a person in the county is arrested for a felony
involving violence against another person, is taken to a receiving facility and
specified sources for reimbursement are not available.” The patient is
responsible for the payment of any hospital bill for involuntary placement
under the Baker Act, but if the patient is indigent the state (formerly the
Department of Health and Rehabilitative Services) “is obligated to provide
treatment at a receiving or treatment facility [and] provides treatment for
indigent Baker Act commitments without any cost to the county.”
Op. Att’y Gen. Fla. 74-271 (1974), regarding involuntary hospitalization in a
psychiatric facility: “A circuit court judge may order a patient involuntarily
hospitalized at a private psychiatric facility not under contract with the
State . . . provided the patient meets the statutory criteria for involuntary
hospitalization, the facility has been designated by [DCF], and the cost of
treatment is to be borne by the patient, if he is competent, or by his guardian
if the patient is incompetent. When state funds are to be expended for
involuntary hospitalization of a patient in a private psychiatric facility, such
facility must be under a contract with the state.”

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
297
Do mental health professionals have any specified rights under the Baker Act?
Section 394.460, Florida Statutes, “Rights of Professionals,” states: “No
professional referred to in this part shall be required to accept patients for treatment
of mental, emotional, or behavioral disorders. Such participation shall be
voluntary.” Just because a professional employed at or under contract with or with
privileges at a hospital or other receiving facility refuses to provide a service
doesn’t mean the facility doesn’t remain responsible for carrying out its duties. It
must find another professional to perform the duty.
B. Habeas Corpus
Does a voluntary patient need to be advised of the right to habeas corpus?
Yes. The Baker Act requires that all persons “held” in a facility be advised of their
right to file a petition for habeas corpus. No distinction is made regarding the
patient’s age, legal status, or competency. Since patients are entitled to file a
petition for being unjustly denied a right or privilege granted under the law, this
may apply to persons on voluntary as well as involuntary status.
Who has standing to file a petition for a writ of habeas corpus?
The Baker Act limits the individuals who have standing to file a petition for a writ
to the patient regardless of age or legal status, a relative, friend, guardian, guardian
advocate, representative, or attorney, or DCF. As a receiving facility, you must be
sure that each person admitted to one of your facilities (and representative) has
been informed of the right to file a habeas petition and, if requested, provide a copy
of the petition form and offer assistance. Any petition received must be filed by the
facility with the clerk of court within one working day after receipt.
Can a petition for writ of habeas corpus be used to file a grievance about staff
treatment or conditions at a facility if you are a voluntary patient? I directed
the patient to our facility grievance procedures as a voluntary patient. For
practical purposes, the petition will not be heard by a judge for matters more
appropriately handled by the internal grievance procedure — the judge’s
time is more valuable than that.
Every person who enters a receiving facility or who is held in any hospital while
under voluntary and involuntary status must be informed of the right to file a
petition for a writ of habeas corpus. While habeas usually refers to detention, the
right to petition for redress of grievances is covered in the same section of the law.
In any case, the Baker Act ensures that all constitutional rights of each person at a

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
298
receiving or treatment facility or held in a hospital under the Baker Act be
protected.
Any person held in a receiving or treatment facility may file a petition for a writ of
habeas corpus at any time. This petition may be used to question the legality of the
detention and/or allege that a right or privilege has been denied or a procedure of
the Baker Act has been abused. A person held voluntarily has the same right to file
a petition for a writ of habeas corpus as a person held involuntarily. The law makes
no distinction between persons held voluntarily and involuntarily in this regard.
Facility staff should not be in the position of deciding, based on legal criteria or
otherwise, whether a petition for a writ of habeas corpus is valid or appropriate.
The petition is an opportunity for individuals to seek redress directly from the
court; it is up to the court to decide the merits of the petition. While it may be true
that these petitions are often unlikely to have practical consequences, it is not for
facility staff to make that determination; that would be the fox guarding the
henhouse.
None of this is to disparage internal complaint procedures, which certainly have
value and are required to be made available to individuals in receiving facilities
(see Fla. Admin. Code R. 65E-5.180(6)).
What is the facility’s responsibility when a patient wants to file a petition for a
writ of habeas corpus for what appears to be a frivolous matter?
The facility has no discretion to determine what is serious and what is frivolous. In
any case, the staff should give the petition form (CF-MH 3090 recommended) to
the person and offer assistance in completing the form. No matter what form is
chosen by the patient to file a petition or whether the patient accepts the assistance
of staff, the petition must be filed with the clerk of court within one working day.
We have an incompetent patient who drafts written complaints about her
treatment in the facility. We interpret her documents as writ petitions and file
with the circuit court. Upon direction from the judge we drafted responses to
the petition for redress of grievances, which we believe will satisfy the judge.
The patient continues to write similar complaints and she is addressing her
complaints “Dear Judge.” These complaints consist of her being held hostage
and being given medications that cause severe side effects. Should we continue
to interpret her handwritten documents as writ petitions and continue to file
with the court? Or should we contact the guardian advocate (her mother) and
ask what she would like us to do with the document?

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
299
You were correct in interpreting the woman’s complaints as a writ petition and
filing them with the court. Such a complaint doesn’t have to be on the
recommended state form. You should forward current and future complaints to the
court if she is addressing them as “Dear Judge.” The Baker Act doesn’t limit the
filing of such petitions to persons with capacity — it clearly says “person,” which
could be of any age, legal status, or competence status. It further specifically
includes persons who have been adjudicated incapacitated with a guardian or
incompetent to consent with a guardian advocate. § 394.459, Fla. Stat.
If at any time, the patient wants access to the Abuse Registry or other advocacy/
regulatory agencies, such access should also be facilitated. It is unlikely she’ll be
satisfied with a grievance procedure within the hospital, but section 394.459,
Florida Statutes, sets forth the following requirement:
(4) Quality of treatment.--
(b) Facilities shall develop and maintain, in a form accessible to
and readily understandable by patients and consistent with rules
adopted by the department, the following:
* * *
3. A system for investigating, tracking, managing, and responding
to complaints by persons receiving services or individuals acting on
their behalf.
How is the court expected to respond to a petition for a writ of habeas corpus?
The Florida Supreme Court Commission on Fairness strongly urged all courts to
treat petitions for a writ of habeas corpus as emergency matters and expeditiously
resolve these issues and ensure that the petitioner receives notice of the disposition.
However, judicial response is solely subject to the courts.
C. Clinical Records and Confidentiality
How is a clinical record defined? What is considered a part of the clinical
record?
Section 394.459, Florida Statutes, defines “clinical record” to mean “all parts of
the record required to be maintained and includes all medical records, progress
notes, charts, and admission and discharge data, and all other information recorded
by a facility which pertains to the patient’s hospitalization and treatment.”

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
300
Does a person have a right to see his or her own clinical record?
Yes. The Baker Act requires that persons have reasonable access to their clinical
records, unless such access is determined by the person’s physician to be harmful
to the person. Facilities and mental health professionals should make every
possible effort to ensure persons have this access. Facilities should have policies
and procedures addressing what is “reasonable access,” what is “harmful,” who
makes the decision to permit access, who is authorized to restrict access, how the
record will be reviewed to determine if harmful material is included, how the
record’s integrity will be protected, and whether a copy of the record will be
provided to the person, if requested.
A patient’s sister is his court-appointed guardian, and she has asked the
hospital for his records. The hospital’s risk manager says we don’t have to
provide those records until after discharge, per section 395.3025(1), Florida
Statutes. However, section 395.3025(2) clearly states that subsection (1) does
not apply to records maintained at any facility governed by the provisions of
section 394.4615. Is the hospital correct?
The hospital is not correct. All hospitals are required to uphold the rights of
persons held under the Baker Act, regardless of whether the hospital is designated
as a receiving facility. With regard to access to records, section 395.3025 provides
(emphasis added):
(1) Any licensed facility shall, upon written request, and only after
discharge of the patient, furnish . . . a true and correct copy of all
patient records. . . .
(2) This section does not apply to records maintained at any
licensed facility the primary function of which is to provide
psychiatric care to its patients, or to records of treatment for any
mental or emotional condition at any other licensed facility which
are governed by the provisions of s. 394.4615.
(3) This section does not apply to records of substance abuse
impaired persons, which are governed by s. 397.501.
Section 394.4615 (clinical records; confidentiality) provides:
(2) The clinical record shall be released when:
(a) The patient or the patient’s guardian authorizes the release. The

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
301
guardian or guardian advocate shall be provided access to the
appropriate clinical records of the patient. The patient or the patient’s
guardian or guardian advocate may authorize the release of
information and clinical records to appropriate persons to ensure the
continuity of the patient’s health care or mental health care.
If the guardianship is plenary rather than limited, the guardian has all rights the
person would have if capacitated. HIPAA yields to state law regarding substitute
decision makers who are standing in the shoes of the patient.
Our facility will be going live with electronic medical records. Is it okay to
have bar codes with the hospital logo on the mandatory Baker Act forms so
they can be scanned into the electronic record after a person’s discharge? We
can download directly into the chart an electronically signed BA 52b and it
can be signed via an ePad. Can we copy this form and give this to a law
enforcement officer? Technically there is no “hard copy” with an “original”
signature, since it is all done electronically.
Yes. Generally, the mandatory forms cannot be altered. In this situation the
mandatory form is not being altered; only a logo and bar code are added for
purposes of electronic recordkeeping or preprinting the name and address of the
receiving facility to the form. However, retyping the form or changing the format
in any significant way is not acceptable.
The Baker Act makes no reference to “originals,” and all references to “originals”
have been removed from the rule and the forms. DCF has actively encouraged the
use of electronic medical records, and the technology has progressed faster than the
law or rules. As long as the mental health professional’s initiation form (BA-52b)
replicates the form adopted in rule, there shouldn’t be any problem with lack of a
hard copy with an “original” signature. If the law enforcement officer hesitates,
there should be no reason why the initiating professional couldn’t initial next to the
electronic signature on the copied completed form.
We are now on electronic records, including treatment plans. Since we need to
have the patient review, make comments on, and sign the treatment plan, how
would we do this in a paperless system? We thought we could review the plan
via the computer, type patients’ comments for them on the plan, and then
state that the patient signed it by using two patient identifiers as we use in any
electronic signature for patients. Would this meet the standard for the Baker
Act relating to the patient acknowledging the treatment plan?

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
302
DCF has consistently supported hospital efforts to develop electronic medical
records. The law never makes reference to originals of documents, and all
references to originals in the rule and forms have been removed. However, the law
states that the person must have had an opportunity to assist in preparing and
reviewing the treatment plan prior to its implementation and there must be space
for the person’s comments. What you propose would meet the statutory
requirements. It would be best to include the person’s own words to reflect that
he/she actually understood the contents of the plan and agreed to it.
A psychiatrist who was ordered to perform an independent expert
examination pursuant to an involuntary placement hearing is requesting a
copy of the inpatient record to take with him for his review. Is there any
provision that would allow this, outside of patient consent or court order?
Since the independent expert is appointed by the court and would be a witness for
the individual’s defense, access to the record is implied. Review of existing clinical
records is a normal part of a psychiatric examination. If you are asking whether the
psychiatrist can remove a copy of the record from the premises of the receiving
facility rather than access the record itself, the above provisions don’t address this
issue. However, copies of charts (or information from the charts) are frequently
sent to other entities outside the organization creating the record with the consent
of the person or an order of the court. The psychiatrist’s request would be handled
the same way.
When can a court order the release of clinical records from a Baker Act
receiving facility, and is the law the same regarding orders for the release of
records from an outpatient therapist?
Summaries of several appellate cases are included below that clearly distinguish
between the authority of the court to order release of Baker Act records after a
good cause hearing and the lack of authority to order release of other psychiatric
records in an outpatient context. This is further supported by appellate courts:
Katlein v. State, 731 So. 2d 87 (Fla. 4th DCA 1999). As the Florida Supreme
Court stated in State v. Roberson, 884 So. 2d 976, 978 (Fla. 2004), the court
in Katlein
set out a mechanism for determining when it is appropriate for a
court to order the release of [Baker Act] records, which we find
to be fair and reasonable. The party seeking the records must
first make a threshold showing that the privileged records are

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
303
likely to contain relevant evidence. “The defendant must
advance a good faith factual basis which is not ‘merely a
desperate grasping at a straw.’ . . . In other words, no fishing
expeditions.” Katlein, 731 So.2d at 90. If a showing is made
that the records are likely to contain relevant evidence, the court
will do an in camera inspection. If the court concludes after
inspecting the records that they contain relevant information, it
should then allow the parties access to them in order to
determine whether disclosure of the information to the trier of
fact is required to ensure a fair trial. The burden is on the party
seeking disclosure to demonstrate that disclosure is required.
However, privilege has also been addressed as follows:
Jaffee v. Redmond, 518 U.S. 1, 116 S.Ct. 1923, 135 L.Ed.2d 337 (1996).
This case involved a fatal shooting by a police officer. The administrator of
the decedent’s estate sought records of the officer’s post-shooting sessions
with her therapist, but the U.S. Supreme Court held a psychotherapist
privilege existed under the federal rules of evidence. The Court stated:
Like the spousal and attorney-client privileges, the
psychotherapist-patient privilege is “rooted in the imperative
need for confidence and trust.” . . . Effective psychotherapy
depends upon an atmosphere of confidence and trust in which
the patient is willing to make a frank and complete disclosure of
facts, emotions, memories, and fears. Because of the sensitive
nature of the problems for which individuals consult
psychotherapists, disclosure of confidential communication
made during counseling sessions may cause embarrassment or
disgrace. For this reason, the mere possibility of disclosure may
impede disclosure of the confidential relationship necessary for
successful treatment.”
The Court stated that protecting the confidentiality of communications
between a patient and psychotherapist serves private and public interests.
The patient is able to talk more freely to the therapist, and society benefits
because “appropriate treatment for individuals suffering the effects of a
mental or emotional problem” is facilitated. The Court also extended the
privilege to licensed social workers providing psychotherapy. “Their clients
often include the poor and those of modest means who could not afford the
assistance of a psychiatrist or psychologist, . . . but whose counseling

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
304
sessions serve the same public goals.”
While rejecting the balancing component of the privilege implemented by
some jurisdictions, where the trial judge may in camera weigh the patient’s
privacy interests and the other party’s “evidentiary need for disclosure,” the
Court in a footnote stated that it did “not doubt that there are situations in
which the privilege must give way, for example, if a serious threat of harm
to the patient or to others can be averted only by means of a disclosure by
the therapist.”
State v. Famiglietti, 817 So. 2d 901 (Fla. 3d DCA 2002). The court held that
a defendant in a criminal case could not “invade the victim’s privileged
communications with her psychotherapist [even] if the defendant can
establish a reasonable probability that the privileged matters contain material
information necessary to his defense.” The only exceptions are for
communications that are (1) relevant in proceedings to compel
hospitalization of a patient for mental illness, (2) made during a court-
ordered examination of a patient’s mental or emotional condition, or (3)
relevant to the patient’s mental or emotional condition in a proceeding where
the patient is relying on the condition as an element of his/her own claim or
defense “or, after the patient’s death, in any proceeding in which any party
relies upon the condition as an element of the party’s claim or defense.”
§ 90.503(4), Fla. Stat.
The court noted that in State v. Pinder, 678 So. 2d 410, 417 (Fla. 4th DCA
1996), the court found a due process balancing test existed (“To obtain in
camera review of confidential communications or records under section
90.5035, a defendant must first establish a reasonable probability that the
privileged matters contain material information necessary to his defense.
Only then may a trial court conduct an in camera hearing to determine if, in
fact, the privileged communications contain such information”). But the
court disagreed and certified conflict with Pinder.
Can information from a psychiatric clinical record for a person in a Baker
Act facility be released in response to a subpoena?
No. A court order is required. In determining whether there is good cause for
disclosure, the court must weigh the need for the information to be disclosed
against the possible harm of disclosure to the person to whom the information
pertains.

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
305
Can a guardian advocate review the contents of the clinical record?
Yes. The Baker Act requires that the guardian advocate be given access to the
appropriate clinical records of the patient and may also authorize the release of
information and clinical records to appropriate persons to ensure the continuity of
the patient’s health care or mental health care.
Is there a requirement for facilities to give notice when a foreign national is
held involuntarily under the Baker Act?
Yes. These are individuals who are citizens of another country, even if they have
dual citizenship with the United States. The Vienna Convention on Consular
Relations is clear in the treaty itself that the consulate must be notified anytime a
foreign national is detained by law enforcement.
The following FAQs from the United States Department of State Consular
Notification and Access website may be helpful:
Q. If we have a foreign national detained in a hospital, do we have to
provide consular notification?
A. Yes, if the foreign national is detained pursuant to governmental
authority (law enforcement, judicial, or administrative) and is not
free to leave. He/she must be treated like a foreign national in
detention, and appropriate notification must be provided.
Q. When we notify the consulate, should we tell them the reasons for
the detention?
A. Generally you may use your discretion in deciding how much
information to provide consistent with privacy considerations and
the applicable international agreements. Under the VCCR, the
reasons for the detention do not have to be provided in the initial
communication. The detainee may or may not want this information
communicated. Thus we suggest that it not be provided unless
requested specifically by the consular officer, or if the detainee
authorizes the disclosure. Different requirements may apply if there
is a relevant bilateral agreement. (Some of the bilateral agreements
require that the reasons for the detention be provided upon request.)
If a consular official insists that he/she is entitled to information
about an alien that the alien does not want disclosed, the Department
of State can provide guidance.

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
306
The State Department’s website on Consular Notification and Access provides
excellent information on this requirement, based on the Vienna Convention. You
can get any information from the State Department website at:
http://travel.state.gov/content/travel/english/consularnotification.html
The U.S. State Department website is www.state.gov. The department’s Consular
Notification and Access Manual (4th ed. 2014) has extensive information about
consular notification and access for foreign nationals, including FAQs, contact
information for foreign embassies and consulates in the U.S., and instructions for
federal, state, and local law enforcement and other officials concerning the rights
of foreign nationals in the United States.
If an individual is deemed incompetent, can a facility notify the “emergency
contact” when it is obvious the patient cannot notify anyone because of the
patient’s current mental status? We are only wishing to notify someone of the
client’s whereabouts and safety or verify admission if the family is calling to
find the patient. Sometimes individuals are transferred not once but twice to
get to us, which causes confusion for the family.
The current statute requires that you notify the person’s representative. The law
doesn’t require express and informed consent for the notification of the
representative to be made.
How does the HIPAA privacy rule change the laws concerning consent for
treatment?
The privacy rule relates to uses and disclosures of protected health information, not
to whether a person consents to the health care itself. As such, the privacy rule
does not affect informed consent for treatment, which is addressed by state law.
Does the HIPAA privacy rule change how a person can grant another person
health care power of attorney?
No. Nothing in the privacy rule changes the way in which an individual grants
another person power of attorney for health care decisions. State (or other) law
regarding health care powers of attorney continues to apply. The intent of the
provisions regarding personal representatives was to complement, not interfere
with or change, current practice regarding health care powers of attorney or the
designation of other personal representatives. Such designations are formal, legal
actions which give others the ability to exercise the rights of, or make treatment
decisions related to, an individual. The privacy rule provisions regarding personal
representatives generally grant persons who have authority to make health care

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
307
decisions for an individual under other law the ability to exercise the rights of that
individual with respect to health information.
D. Duty to Warn
If a patient in a Baker Act receiving facility discloses information that poses a
possible risk of harm to a potential victim, is there a duty to warn the
intended victim?
The Baker Act permits such disclosure but does not create a duty to warn. HIPAA
and professional codes of ethics also permit such disclosure. Even though no duty
to warn exists in Florida, a legitimate threat should always be taken seriously and
warning provided to the intended victim, assuming this is also the position of the
facility’s attorney, risk manager, or compliance officer. See section
394.4615(3)(a), Florida Statutes, which provides: “Information from the clinical
record may be released . . . [w]hen a patient has declared an intention to harm other
persons. When such declaration has been made, the administrator may authorize
the release of sufficient information to provide adequate warning to the person
threatened with harm by the patient.”
Federal and state appellate courts have further addressed this issue. Many people
believe that Tarasoff v. Regents of University of California, 551 P.2d 334 (Cal.
1976) (therapist who determines, or should determine, patient presents serious
danger of violence to another has duty to exercise reasonable care to protect
intended victim), applies to Florida. However, since Florida law makes such
disclosure permissive rather than mandatory, appellate courts to date have found
no liability for failure to disclose such a threat; see, e.g.:
Boynton v. Burglass, 590 So. 2d 446 (Fla. 3d DCA 1991). The Third District
Court of Appeal rejected the approach taken in Tarasoff and found no duty
to warn.
Green v. Ross, 691 So. 2d 542 (Fla. 2d DCA 1997). The Second District
Court of Appeal agreed with Boynton and concluded that “the permissive
language waiving confidentiality in sections 455.2415 [now section 456.059
and 491.0147 does not equate to the legislative creation of a cause of action
not previously recognized in Florida.”
However, the First District Court of Appeal did establish a “duty to inform” the
guardians of a minor of such threats. O’Keefe v. Orea, 731 So. 2d 680 (Fla. 1st
DCA 1998), was a medical malpractice action by the mother of a 17-year old

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
308
patient. Three days after the patient’s discharge, his mother told the psychiatrist
that her son was out of control and she and the boy’s father, who were also patients
of the psychiatrist, could no longer care for him at home. Allegedly, the
psychiatrist’s response was to order a different medication. The next day the
patient attacked his parents, injuring his mother and killing his father. The court
stated that the psychiatrist’s
duty to warn the O’Keefes concerning their son’s condition derives
from the fiduciary relationship between [him] and the parents of his
minor patient, as well as the physician-patient relationship between
[him] and Mr. and Mrs. O’Keefe. In view of these fiduciary
relationships, [the psychiatrist] had a duty to inform [the patient’s]
parents concerning their child’s diagnosis, including the diagnosis of
other physicians who had observed [him], together with his personal
treatment recommendations and the treatment recommendations of
other physicians. In addition, [the psychiatrist] had a duty to disclose
the information available in the nurse’s notes concerning [the
patient’s] hallucinations, violence, threats to staff, suicidal tendencies,
and the fact that at various times two male guards were required to
control him.
The federal circuit court in U.S. v. Chase, 340 F.3d 978 (9th Cir. 2003) held that
psychiatrists can’t testify against patients who make dangerous or threatening
confessions during therapy. It held that although psychiatrists are sometimes
required to report incidents to authorities that could lead to violence, prosecutors
couldn’t use testimony from doctors to help convict their patients. The court
concluded that “the gain from refusing to recognize a dangerous-patient exception
to the psychotherapist-patient testimonial privilege in federal criminal trials
outweighs the gain from recognizing the exception.” Id. at 991–992. It stated that
“although incarceration is one way to eliminate a threat of imminent harm, in many
cases treatment is a longer-lasting and more effective solution. A criminal
conviction with the help of a psychotherapist’s testimony is almost sure to spell the
end of any patient’s willingness to undergo further treatment for mental health
problems.” Id. at 991. The court did note that its ruling doesn’t extend to
proceedings in civil court to determine whether the patient should be committed to
a hospital.
E. Americans with Disabilities Act (ADA)
How does the federal ADA apply to people held in Baker Act facilities?

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
309
Reports of facilities failing to provide qualified interpreters for persons with
hearing problems and of people being refused by receiving facilities for being
obese (no staff or equipment for lifting/transferring), for using a cane, crutches, or
walkers (without an offer of a wheelchair as an accommodation), for having a
service animal, for being incontinent, etc. have arisen recently — all these may be
ADA violations. The Baker Act has the following provision in section 394.459,
Florida Statutes (emphasis added):
(12) Posting of notice of rights of patients.--Each facility shall post
a notice listing and describing, in the language and terminology that
the persons to whom the notice is addressed can understand, the rights
provided in this section. This notice shall include a statement that
provisions of the federal Americans with Disabilities Act apply
and the name and telephone number of a person to contact for
further information. This notice shall be posted in a place readily
accessible to patients and in a format easily seen by patients. . . .
All hospitals and receiving facilities should establish criteria that include, rather
than exclude, people needing the services. This may mean making accommoda-
tions as necessary.
F. Right to Dignity and Privacy
Can we have Baker Act patients in our ER, mixed with non-Baker Act
patients?
There is nothing in the Baker Act that would prevent you from co-locating persons
under the Baker Act with other patients in your hospital, just as there is nothing to
prevent persons on voluntary vs. involuntary status from being co-located.
Can facility staff, while doing safety checks, routinely go through a patient’s
belongings, bedside cabinets, and closets to look for contraband, or does this
violate the patient’s right to privacy and dignity? I understand we need to
search belongings upon admission or with a doctor’s order if there is clear
evidence a patient has contraband.
With regard to searches, there are several references in the law and rules, as
follows:
Rules 65E-5.180(9)(a) and (10)(h)1., Florida Administrative Code, require
that persons be searched before they are placed into seclusion or restraint.
However, the law and rule don’t specifically address searches of persons

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
310
upon arrival at the facility or otherwise, except as designated below. Practice
throughout the state generally includes a complete search of the person and
the person’s belongings upon arrival at the facility.
Section 394.459(6), Florida Statutes, and rule 5E-5.200, Florida
Administrative Code, govern the right of persons to the care and custody of
personal effects. This guarantees persons the right to the possession of their
clothing and personal effects, but allows the facility to take temporary
custody of such effects when required for medical and safety reasons. The
rule and law require that an inventory be conducted/witnessed. This certainly
would entail a search of the person and his/her belongings to determine
whether there are items to be removed for safety reasons.
Section 394.459(5)(b), Florida Statutes, governing communication, requires
that persons be able to receive sealed, unopened correspondence and that
such correspondence can’t be “opened, delayed, held, or censored by the
facility unless there is reason to believe it contains items or substances
which may be harmful to the person or others, in which case the
administrator may direct reasonable examination of such mail and may
regulate the disposition of such items or substances.” In these circumstances,
staff typically has the person open any packages in the presence of staff.
Many facilities prohibit visitors from bringing handbags and other items onto a
psychiatric unit. Some even “wand” every patient and visitor upon arrival at the
unit. The federal Conditions of Participation or the Joint Commission accreditation
standards may require additional standards in terms of searches.
G. Communication Restrictions
Can a facility enforce visiting hours for family members without any clinical
justification? Does the Baker Act permit a facility to restrict family members
from visiting an individual outside of normal visiting hours, without providing
specific clinical justification for the particular case? Recently, a question has
arisen regarding the Baker Act’s requirements regarding visitation and
visiting hours.
Section 394.459(5)(c)–(5)(d), Florida Statutes, governs the access that the
facility must provide. Language is fairly directive that denial of visitation to
specified parties can be done only when “access would be detrimental to the
patient.”

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
311
While the law requires visitation rules, such rules can’t be contrary to the express
language of the statute. Limitation on visitation by the above parties can be
imposed only when access is documented as detrimental, and it must be
communicated to the patient, attorney, guardian, guardian advocate, and
representative. However, the right to visits by friends or others is not specified in
the law as it is as to those specified above and can be restricted to visiting hours
established by the facility. Other types of restrictions of communication (phone or
mail) to any person (other than abuse reporting and communication with his/her
attorney) can be governed by facility policies as well and would require notice of
such restriction and that the reasons for the restriction be served on the patient and
the patient’s guardian, guardian advocate, health care surrogate or proxy, attorney,
and representative.
Is a Baker Act patient entitled to visitors during the time he/she is in the ED?
We have several issues with nursing staff allowing inappropriate people in the
room. Do we also have to make phones available?
Rights of persons held under the Baker Act who are held in hospital EDs are
addressed in the Florida hospital licensing law (chapter 395, Florida Statutes),
under which the rights of any person held under the Baker Act on voluntary or
involuntary placement in any licensed hospital must be protected, regardless of
whether the hospital has been designated as a receiving facility or whether the
individual is held in the psychiatric unit or in a different unit because of the
individual’s clinical needs or space availability of the hospital. There are multiple
provisions of the licensure law in the Florida Statutes that apply to persons held
under the Baker Act (see sections 395.003(5)(a), 394.003(5)(b), 395.1041(6),
395.1055(5), 395.1065(4), and 395.3025, Florida Statutes).
The rights guaranteed to any person held under the Baker Act are enumerated in
section 394.459(5), Florida Statutes, one of which is the right to communication
and visits. Families must be allowed immediate access to any patient unless such
access would be detrimental to the patient. Your hospital can’t have a policy
prohibiting family contact with your ED patients held under the Baker Act, but it
can limit such contact on a case-by-case basis with sufficient justification
documented in the chart of how the visit by family would be detrimental. There is
no right to have persons visit other than those specified in the law.
Can a parent restrict the communication of his or her child in a receiving
facility?
No. Only the physician or authorized facility staff is permitted to restrict a person’s

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
312
communication, regardless of the age of the patient. Staff should be aware of the
parents’ reason for requesting no communication, as the physician may concur and
issue such an order.
Does a court-appointed guardian have the power to restrict a person’s
visitation rights when in a Baker Act receiving facility?
No. Section 394.459, Florida Statutes, governs rights of persons in receiving
facilities and all hospitals in the state of Florida. Further, the statute is clearly
supported by Handley v. Dennis, 642 So. 2d 115 (Fla. 1st DCA 1994), which states
that the rights of the person protected by the Baker Act trump the rights of the
guardian under chapter 744. For instance, if the person wishes to have visits by
family members or others, he or she should be allowed to do so. If staff believes
the individual has abused, neglected, or exploited the person, a report to the abuse
line should be made. Otherwise, the preferences of the person should prevail.
Further, if the guardian is not acting in the best interests of the ward, this should be
reported to the court. This may be especially important if it is a temporary
emergency guardianship, where the court may decide to appoint someone else as
guardian at the time when the hearing takes place, based on such information.
H. Custody of Personal Possessions
What restrictions does the Baker Act place on a person’s right to keep his/her
own belongings?
Section 394.459, Florida Statutes, governs rights of persons in psychiatric
facilities. Subsection (6) ensures persons the right to retain their clothing and
personal effects. If the right is restricted for medical or safety reasons, the reasons
must be documented in the person’s clinical record. The items removed must be
identified on an inventory that must be given to the patient, guardian, guardian
advocate, or representative. Form CF-MH 3043, “Inventory of Personal Effects,”
can be used to document this removal, although you may use a different form if it
contains no less than the statutorily required information.
Can a person be forced to wear specialized clothing in a receiving facility to
designate his/her status as a suicide or escape risk?
No. Use of special clothing for identification purposes would be a violation of
individual dignity, confidentiality, and privacy. However, if the physician orders
special clothing for medical reasons, no such violation would occur.
I am an assistant state attorney. Can you tell me how the Baker Act addresses

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
313
a person’s right to have a firearm and/or the ability of law enforcement to
remove such a weapon?
The Baker Act is silent on the issue of weapons with two exceptions. One is that no
one is allowed to bring firearms or other deadly weapons onto the grounds of a
hospital providing mental health services. § 394.458(1)(b), Fla. Stat. In addition,
persons served in such facilities are allowed to keep their personal effects, other
than those removed for medical or safety reasons. However, the items removed
must be returned to the person or, if detrimental to the person, to his/her
representative, at the time of release from the facility. § 394.459(6), Fla. Stat.
The legal advisor for the Miami-Dade Police Department gave direction to officers
related to return of weapons in a Baker Act situation. Legal Note 2005-4. If the
incident report prepared by law enforcement in a Baker Act situation referenced
“breach of peace,” the weapon could be taken and returned only upon an order of
the court.
However, according to Op. Att’y Gen. Fla. 09-04 (2009) (regarding confiscation
and return of firearms by law enforcement agencies when a firearm owner is
subject to Baker Act evaluation), “[i]n the absence of an arrest and criminal charge
against the person sent for evaluation under the Baker Act, the Sheriff . . . may not
retain firearms confiscated. . . . Baker Act proceedings are not criminal
proceedings.” The opinion suggested that the sheriff seek legislation to address the
problem.
Other Florida statutes that relate to persons with mental health issues include:
Sections 790.17 and 790.175 (furnishing or transferring of weapons) refer to
people of “unsound mind.”
Section 790.06 (license for concealed carry) refers to adjudication of
incapacity (under chapter 744, guardianship), commitment under the
Marchman Act (chapter 397), and commitment under the Baker Act (chapter
394). Commitment isn’t defined here, but presumably this would pertain to
involuntary placement provisions ordered by a court after a judicial hearing
and not an involuntary examination initiated by a law enforcement officer or
mental health professional.
Section 790.065 (sale and delivery) was modified effective February 1,
2007, to require the clerk of court to notify FDLE whenever the court enters
an order under the guardianship statute or the Marchman Act, or for Baker

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
314
Act involuntary inpatient placement. It was further revised by the 2013
Florida Legislature to require that before individuals can be transferred from
involuntary to voluntary status under the Baker Act and continue to be
considered “imminently dangerous,” they must be reported to the circuit
court for review and reporting to FDLE/FBI to prevent purchase of weapons
or eligibility for a concealed weapon permit.
I. Designated Representative
We often use the next of kin name and address that is identified on the
medical record as the representative. Should we verify with the patient that
the patient wants this person acting as his/her representative?
The patient must be allowed to select his/her own representative. Only when he/she
can’t or won’t select a representative is the receiving facility required to select one
from the prioritized list included in the Baker Act.
Can you explain the difference between a representative and an “emergency
contact”?
Persons on voluntary status only have an emergency contact, not a designated
representative. However, an adult on involuntary status who doesn’t have a court-
appointed guardian will always have a representative designated. That
representative will serve as the person’s emergency contact. For persons
determined by a physician to be incompetent to consent to their own admission or
for their own treatment (unable to made well-reasoned, willful, and knowing
decisions), they must be on involuntary status and a guardian advocate must be
appointed by the court.
What is the role of a designated representative?
A representative is designated when a person is admitted to a facility on an
involuntary basis or is transferred from voluntary to involuntary status.
§ 394.4597(2), Fla. Stat. The representative must:
receive notice of the individual’s admission;
receive notice of proceedings affecting the individual;
have immediate access to the individual held or admitted for mental health
treatment, unless such access is documented to be detrimental to the
individual;

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
315
receive notice of any restriction of the individual’s right to communicate or
receive visitors;
receive a copy of the inventory of personal effects upon the individual’s
admission and may request amendment to the inventory at any time;
receive disposition of the individual’s clothing and personal effects, if not
returned to the individual, or to approve an alternate plan;
be notified of the right to petition on behalf of the individual for a writ of
habeas corpus to question the cause and legality of the individual’s
detention, or to allege that the individual is being unjustly denied a right or
privilege granted or that an authorized procedure is being abused;
be notified of the right to apply for a change of venue for the individual’s
involuntary placement hearing for the convenience of the parties or
witnesses or because of the condition of the individual;
receive written notice of any restriction on the individual’s right to inspect
his or her clinical record;
receive notice of release of the individual from a receiving facility where an
involuntary examination was performed;
receive a copy of any petition for the individual’s involuntary placement
filed with the court; and
be informed by the court of the individual’s right to an independent expert.
The designated representative does not have the authority to make any treatment
decisions, cannot access or release the patient’s clinical record without the patient’s
consent, and cannot request the transfer of the patient to another facility.
J. Right to Discharge
A hospital discharged our client last week and told us that, according to the
Baker Act, our client must have a doctor’s appointment within seven days, so
the hospital would give the client a prescription for only seven days of
medication. The Baker Act says the client must have access to psychotropic
medications or prescriptions until aftercare appointment or 21 calendar days.
Does this acknowledge that clients cannot always get an appointment with
their psychiatrist within seven days?

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
316
Rule 65E-5.1303, Florida Administrative Code, which governs discharge from
receiving and treatment facilities, states in paragraph (2)(e) that
prescribed psychotropic medications, prescriptions, or multiple partial
prescriptions for psychotropic medications, or a combination thereof,
shall be provided to a person when discharged to cover the
intervening days until the first scheduled psychotropic medication
aftercare appointment, or for a period of up to 21 calendar days,
whichever occurs first. Discharge planning shall address the
availability of and access to prescribed psychotropic medications in
the community.
The “aftercare appointment” specified in the rule is not defined because each
community has different access to resources. The greater the amount of time
between inpatient discharge and the first aftercare appointment, the greater the
likelihood the person won’t show up at all.
The hospital staff’s statement that the treatment center must give a doctor’s
appointment within seven days, and thus limiting the prescription to seven days,
reflects a lack of knowledge on the hospital’s part. It is the hospital’s responsibility
to make these arrangements for the person as part of its discharge planning
obligations, and if it takes up to 21 days for the aftercare appointment, that is the
period for which the hospital should provide medications, prescriptions, or a
combination of such. However, in the absence of the person’s psychiatrist,
arranging for another psychiatrist or ARNP at the community mental health center
(CMHC) to temporarily oversee the person’s care is entirely appropriate. It appears
that you very appropriately provided for the person’s care. This should ideally be
an appointment with the attending psychiatrist who will follow the person on an
outpatient basis. It might be the person’s primary care physician. It might be an
ARNP with the CMHC who can continue the medications prescribed by the
inpatient psychiatrist. It might even be a case manager who can link the person to
an appropriate provider in a timely way. Whatever it takes to ensure the person
connects to continuity of care would meet this requirement.
If the appointment can’t be arranged within the seven-day period called for in the
rules, the inpatient provider may have to prescribe medications for a period of up
to 21 days. Some of those inpatient settings can provide medications only in-house
because they don’t have an outpatient pharmacy license. In such cases, they may
be able to only provide prescriptions. For safety’s sake, they may not want to give
21 days of medication at a single time and may be able to give a smaller amount of
medications, along with prescriptions for the remainder of the 21 days. Some

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
317
communities have quick access to IDP (indigent drug program) medications, while
others have access to emergency centers, free clinics, samples, or county clinics.
K. Advance Directives
We recently had our Joint Commission survey and had some issues with
advance directives. Our chaplains had been told in the past not to complete
living wills with Baker Act patients. Are advance directives addressed in the
Baker Act? What is the law regarding persons under the Baker Act making
advance directives if they have a guardian advocate acting on their behalf? I
understand that a demented, confused person is unable to make a living will,
but if the person is under the Baker Act due to suicidal ideation, paranoia,
etc., can the person make a living will?
An advance directive can be completed only by a person competent to do so. Issues
related to advance directives are governed by chapter 765, Florida Statutes, which
has several provisions that may apply to your situation:
765.204. Capacity of principal; procedure
(1) A principal is presumed to be capable of making health care
decisions for herself or himself unless she or he is determined to be
incapacitated. While a principal has decisionmaking capacity, the
principal’s wishes are controlling. Each physician or health care
provider must clearly communicate to a principal with
decisionmaking capacity the treatment plan and any change to the
treatment plan prior to implementation of the plan or the change to the
plan. Incapacity may not be inferred from the person’s voluntary or
involuntary hospitalization for mental illness or from her or his
intellectual disability.
765.101. Definitions
(10) “Incapacity” or “incompetent” means the patient is physically
or mentally unable to communicate a willful and knowing health care
decision. . . .
765.104. Amendment or revocation
(1) An advance directive may be amended or revoked at any time
by a competent principal. . . .

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
318
765.202. Designation of a health care surrogate
(5) A principal may designate a separate surrogate to consent to
mental health treatment in the event that the principal is determined
by a court to be incompetent to consent to mental health treatment and
a guardian advocate is appointed as provided under s. 394.4598.
However, unless the document designating the health care surrogate
expressly states otherwise, the court shall assume that the health care
surrogate authorized to make health care decisions under this chapter
is also the principal’s choice to make decisions regarding mental
health treatment.
If a person has a guardian advocate appointed by the court, it is because the person
has been found by clear and convincing evidence to be incompetent to provide
consent to treatment. Clearly such a person wouldn’t at that time be competent to
complete any type of advance directive.
You should discuss this issue with your hospital’s attorney as it might be presumed
that a person meeting criteria for an acute care psychiatric hospital stay might not
be competent to make such a directive. Further, a setting like this might be
perceived to have some coercive aspect. It might be considered wise to give a form
and instructions to a person interested in having such an advance directive at the
time of discharge rather than at admission or during acute psychiatric treatment.
The Baker Act recognizes advance directives for mental health care prepared at a
time when the person was competent. A recommended mental health advance
directive is provided at the end of this chapter. This is not a living will — it relates
only to mental health care. It includes language that witnesses sign stating the
person is of sound mind and under no constraint or undue influence. This might be
a difficult thing for a person in an acute psychiatric episode.
The Baker Act rules indicate that when a person has not executed an advance
directive, health care decisions may be made by an eligible proxy during the
interim period between the time the person is determined by the physician to
be incompetent to consent to treatment and the time a guardian advocate is
appointed by a court to provide express and informed consent. Would there
be any conflict with HIPAA allowing a proxy to make decisions, since the
person did not have an advance directive?
No. HIPAA defers to the state laws in recognizing who is authorized to “stand in
the shoes of the person” for decision-making purposes in each state. This includes

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
319
guardians, guardian advocates, and health care surrogates/proxies in Florida.

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
320
III. Forms
Please note that these recommended forms were promulgated by DCF before
the 2016 statutory amendments and do not incorporate those changes.
A. Notice of Right to Petition for Writ of Habeas Corpus or for Redress of
Grievances
Notice of Right to Petition for
Writ of Habeas Corpus or for Redress of Grievances
To: ___________________________________________________
PLEASE BE ADVISED that you may petition the Circuit Court for a Writ of Habeas Corpus to question
the cause and legality of your detention. Furthermore, a petition may be filed in the Circuit Court in the
county in which you are placed for Redress of Grievances alleging that you are being unjustly denied a
right or privilege or that an authorized procedure is being abused.
A Petition for Writ of Habeas Corpus and Redress of Grievances (CF MH Form 3090) may be used for
this purpose. A petition must be signed by either you, your relative, friend, guardian, guardian advocate,
representative, attorney, or the Department of Children and Families.
Staff of this facility will provide a copy of the Writ form to you immediately upon your request. Staff will
assist you in completing this Writ form if you request such help. The Petition for a Writ will be submitted
by the staff to the Circuit Court no later than the next working day after you submit the form.
_________________________________ __________________ __________ am pm
Signature of Administrator or Designee Date Time
This completed form must be given to all persons admitted to a facility and to those
individuals listed below as applicable.
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
Health Care Surrogate/Proxy
am pm
See s. 394.459(8), Florida Statutes
CF-MH 3036, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
321
B. Petition for Writ of Habeas Corpus or for Redress of Grievances
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: _________________________________________ CASE NO.: _____________________
_____________________________________,
Petitioner,
vs.
_____________________________________,
Administrator,
_____________________________________,
Facility Respondent.
Petition for Writ of Habeas Corpus or for Redress of Grievances
1. This Court has jurisdiction pursuant to Section 394.459 (8), Florida Statutes.
2. Petitioner is being held by _________________________________________________, (Administrator) in
______________________________________, (Facility), in ________________________ (City), Florida.
3. Petitioner believes that he/she is being deprived of her/his freedom for invalid and illegal reasons.
Petitioner believes that her/his confinement is illegal because: _______________________________
__________________________________________________________________________________
__________________________________________________________________________________
__________________________________________________________________________________
and/or
4. Petitioner believes that he/she is being unjustly denied a right or privilege or that a procedure
authorized by law is being abused. Petitioner believes that he/she is being unjustly denied a right or
privilege or that a procedure authorized by law is being abused because: _______________________
__________________________________________________________________________________
__________________________________________________________________________________
__________________________________________________________________________________
5. Petitioner is unable to afford counsel and would like the Office of the Public Defender or other counsel to
be appointed to represent her/him in the above captioned matter.
CONTINUED OVER

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
322
Petition for Writ of Habeas Corpus or for Redress of Grievances (Page 2)
WHEREFORE, Petitioner respectfully requests that this Court:
Appoint the Office of Public Defender or other counsel to represent your Petitioner in these
proceedings; and
Enter an Order setting a return hearing on this Petition for Writ of Habeas Corpus for respondent to
show by what legal authority he/she holds petitioner, and/or
Set a hearing for the purpose of a judicial inquiry into the allegations of this Petition for Redress of
Grievances and for ordering a correction of abuse of rights or privileges granted under Chapter 394,
Part I, F.S.
I HEREBY CERTIFY that the above stated matters In the Petition for Writ of Habeas Corpus and Redress of
Grievances are true and correct to the best of my information, knowledge, and belief.
_________________________________ __________________ __________ am pm
Signature of Administrator or Designee Date Time
_________________________________
Printed Name of Petitioner
There
is
or
is not
a petition for involuntary placement pending.
The person
is
or
is not
currently represented by counsel.
Facilities must provide this form to any person making a verbal request for access to the Court.
The completed form must be filed with the Clerk of the Court no later than the next working
day and a copy retained in the person’s clinical record. A copy of the completed Petition for
Writ must be provided immediately to the person and copies of the Petition provided to those
listed below, as applicable.
cc: Check when applicable and initial/date/time when copy provided:
Individual
Date Copy Provided
Time Copy Provided
Initials of Who
Provided Copy
Person
am pm
Guardian
am pm
Guardian Advocate
am pm
Representative
am pm
Health Care Surrogate/Proxy
am pm
See s. 394.459(8), Florida Statutes
CF-MH 3090, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT
Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
323
C. Advance Directive for Mental Health Care
Advance Directive for Mental Health Care
If you believe you may be hospitalized for mental health care in the future and that
your doctor may think you aren’t able to make good decisions about your treatment,
then completing a mental health advance directive now will ensure that your
treatment choices are known at a time of crisis. You can choose now what types of
treatment you do or do not want and appoint a friend or family member to make the
mental health care decisions that you want carried out. You can always change your
mind about your care or surrogate later.
You can use the following advance directive form to direct your future care.
Read each section of the form carefully and talk about your choices with
someone you trust.
The person you choose to be your health care surrogate and alternate must be
a competent adult whose civil rights have not been taken away. The person
you choose should not be a mental health professional, an employee of a
facility that might provide services to you, an employee of the Department of
Children and Families, or a member of the Florida Local Advocacy Council.
Make sure your surrogate understands your wishes and is willing to accept the
responsibility. Your surrogate (and a back-up alternate surrogate if you wish)
should sign this form now or at a later time to show he/she is aware you have
chosen him/her to be your surrogate. The advance directive is still valid if
he/she doesn’t sign the form or if a surrogate or alternative is not named in the
document.
You must sign the form in front of two witnesses.
Have copies made and give them to your surrogate, alternate, your case
manager, your doctor, the hospital or crisis unit at which you are most likely
be treated, your family, or anyone else who might be involved in your care.
Discuss your choices with each of them.
The document should be available quickly if you need it.
Your advance directive doesn’t take effect unless a physician decides that you are
not competent to make your own treatment decisions. If you are in a mental health
facility on an involuntary basis, you will have an attorney appointed to represent

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
324
your interests and a hearing will be conducted in front of a judge or hearing master.
A health care surrogate can’t have you admitted to a facility on a voluntary basis or
consent to your treatment if you are on voluntary status. If voluntary, you will make
the decisions for yourself.
I, _____________________, being of sound mind, willfully and voluntarily execute
this mental health advance directive to assure that if I should be found incompetent
to consent to my own mental health treatment, my choices regarding my treatment
will be carried out despite my inability to make informed decisions for myself.
If a guardian, guardian advocate, or other decision maker is appointed by a court to
make health care or mental health decisions for me, I intend this document to take
precedence over all other means of determining my intent while competent. This
document represents my wishes, and it should be given the greatest possible legal
weight and respect. If the surrogate(s) named in this directive is/are not available,
my wishes shall be binding on whoever is appointed to make such decisions.
If I become incompetent to make decisions about my own mental health treatment,
I have authorized a mental health care surrogate to make certain treatment decisions
for me. My surrogate is also authorized to apply for public benefits to defray the cost
of my health care, to release information to appropriate persons, and to authorize my
transfer from a health care facility.
I hereby appoint and request immediate notification of my mental health care
surrogate, who is:
Name: ______________________________________________________
Address: ____________________________________________________
Day Telephone: ________________ Evening Telephone: ______________
If the person named above is unable or unavailable to serve as my mental health care
surrogate, I hereby appoint and request immediate notification of my alternate
mental health care surrogate as follows:
Name of Alternate: ________________________________________
Address: ____________________________________________________
Day Telephone: ________________ Evening Telephone: ______________
Complete the following or initial in the blank marked “Yes” or “No”:

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
325
A. If I become incompetent to give consent to mental health treatment, I give my
mental health care surrogate full authority to make mental health care
decisions for me. This includes the right to consent, refuse consent, or
withdraw consent to any mental health care, treatment, service, or procedure
consistent with any instructions and/or limitations I have stated in this advance
directive. If I have not expressed a choice in this advance directive, I authorize
my surrogate to make the decision that he/she determines is the decision I
would make if I were competent to do so.
_____Yes _____No
B. My choice of treatment facilities is as follows:
In the event my psychiatric condition is serious enough to require 24-
hour care, I would prefer to receive this care in this/these facilities:
Facility: ___________________________________
Facility: ___________________________________
I do not wish to be admitted to the following facilities for psychiatric
care (optional):
Facility: ___________________________________
Facility: ___________________________________
C. My choice of a treating physician is:
First choice of physician: _____________________
Second choice of physician: ___________________
I do not wish to be treated by the following physicians: (optional)
Name of physician: __________________________
Name of Physician: __________________________
D. My wishes about confidentiality of my admission to a facility and my
treatment while there are as follows:
______ My representative may be notified of my involuntary admission
___ Yes ___ No
______ Any person who seeks to contact me while I am in a facility
may be told I am there.
___ Yes ___ No

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
326
______ If I am incompetent to give consent, I want staff to immediately
notify the following persons that I have been admitted to a psychiatric
facility:
Name: _____________________________________________
Relationship: ________________________________________
Address: ___________________________________________
Day Phone: ______________ Evening Phone: _____________
Name: _____________________________________________
Relationship: ________________________________________
Address: ___________________________________________
Day Phone: ______________ Evening Phone: _____________
I consent to release of information about my current condition and
treatment plan
____ Yes ____ No
To the following persons: _______________ _______________
_______________ _______________
_______________ _______________
E. If I am not competent to consent to my own treatment or to refuse medications
relating to my mental health treatment, I have initialed one of the following,
which represents my wishes:
_____ I wish to have the medications that Dr. ____________________
recommends.
_____ I wish to have the medications agreed to by my mental health
care surrogate after consulting with my treating physician and any other
individuals my surrogate deems appropriate, with the exceptions found
in #3 below.
_____ I specifically do not want and I do not authorize my mental health
care surrogate to consent to the administration of the following
medications or their respective brand name, trade name, or generic
equivalents: (list name of drug):
________________________________________________________
________________________________________________________

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
327
_____ I want the medications that are excluded in #3 above if my only
reason for excluding them is their side effects and the dosage can be
adjusted to eliminate those side effects.
I have the following other preferences about psychiatric treatment and
medications:
________________________________________________________
________________________________________________________
________________________________________________________
________________________________________________________
________________________________________________________
F. Florida law prohibits a mental health care surrogate from consenting to
experimental treatments that have not been approved by a federally approved
institutional review board without my prior written consent or the express
approval of the court.
_____ I want to be included in experimental drug studies or drug trials
_____ I do not want to participate in experimental drug studies or drug trials
G. My wishes regarding Electroconvulsive Therapy (ECT) are as follows:
1 ____ My surrogate may not consent to ECT without express court
approval.
2. _____ I authorize my surrogate to consent to ECT, but only (initial one
of the following):
a. _____ with the number of treatments the attending psychiatrist
thinks is appropriate; OR
b. _____ with the number of treatments that Dr. ____________
thinks is appropriate; OR
c. _____ for no more than the following number of ECT treatments:
________.
3. Other instructions and wishes regarding ECT are as follows:
________________________________________________________
________________________________________________________

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
328
H. I _____ have / _____ have not attached a Personal Safety Plan to this advance
directive.
I. Other instructions I wish to make about my mental health or medical care are
(use additional pages if needed): ___________________________________
_____________________________________________________________
_____________________________________________________________
_____________________________________________________________
_____________________________________________________________
_____________________________________________________________
Check here (____) if other pages are used
Signature
By signing here I indicate that I fully understand that this advance directive will
permit my mental health care surrogate to make decisions and to provide, withhold,
or withdraw consent for my mental health or medical treatment.
Signature (Declarant): ________________________ Date: _________________
Printed Name (Declarant) ___________________________________________
Witnesses
This advance directive was signed by _____________________________ in our
presence. At his/her request, we have signed our names below as witnesses. We
declare that, at the time this advance directive was signed, the Declarant, according
to our best knowledge and belief, was of sound mind and under no constraint or
undue influence. We further declare that we are both adults, are not designated in
this advance directive as the health care surrogate, and at least one of us is neither
the person’s spouse nor blood relative.
Dated at ______________________ this ________ day of ____________, _____.
(County and State) (Day) (Month) (Year)
Witness 1: Witness 2:
______________________________ ______________________________
Signature of witness 1 Signature of witness 2
______________________________ ______________________________
Printed name of witness 1 Printed name of witness 2

Chapter Seven Rights of Patients
_____________________________________________________________________________________
Baker Act Benchguide November 2016
329
______________________________ ______________________________
Address of witness 1 Address of witness 2
______________________________ ______________________________
City, State, Zip Code of witness 1 City, State, Zip Code of witness 2
Acknowledgement of Health Care Surrogate/Alternate*
I, _________________________________, mental health care surrogate designated
by _________________________________, hereby accept the designation.
__________________________________________ ___________________
(Signature of mental health care surrogate) (Date)
I, _________________________________, alternate mental health care surrogate
designated by _____________________________, hereby accept the designation.
__________________________________________ ___________________
(Signature of alternate mental health care surrogate) (Date)
*Signed acknowledgment by the surrogate/alternate is not required for the advance
directive to be valid.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
330
Chapter Eight: Firearm Prohibition for Certain Individuals
With Mental Illnesses
I. Background
In 2013 the Florida Legislature passed House Bill 1355, which became state law
on July 1, 2013. It provides conditions under which an individual who has been
allowed to transfer to voluntary status in lieu of court-ordered involuntary
commitment after being admitted for involuntary examination at a Baker Act
receiving facility, and is certified by a physician to be of imminent danger to self
or others, may be prohibited from purchasing firearms or obtaining or retaining a
license for a concealed weapon.
There are key components of this bill that may directly impact a variety of
individuals and organizations. Mental health receiving facilities, the doctors who
work in or contract with the facilities, magistrates and judges who review the
documents, clerks of court who must process the documents and forward
information to FDLE, and FDLE itself (which must provide the information to the
FBI for the National Instant Criminal Background Check System (NICS)) are all
stakeholders in this process.
Before addressing the new provisions of Florida’s weapons statute, it is important
to address the application of the law prior to 2013. The law’s application may not
have been apparent to staff of mental health and substance abuse facilities
throughout the state, but it is well known to the clerks of court, judges and
magistrates, and FDLE. In the past, when courts have found in certain
circumstances that an individual has met conditions of impairment due to mental
illness or substance abuse (and other reasons), they were required to report
information to FDLE for incorporation into state and federal databases to prevent
such individuals from purchasing firearms. These sections of the law include:
790.06. License to carry concealed weapon or firearm (emphasis
added)
(2) The Department of Agriculture and Consumer Services shall
issue a license if the applicant:
* * *

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
331
(f) Does not chronically and habitually use alcoholic beverages
or other substances to the extent that his or her normal faculties are
impaired. It shall be presumed that an applicant chronically and
habitually uses alcoholic beverages or other substances to the extent
that his or her normal faculties are impaired if the applicant has been
committed under chapter 397 or under the provisions of former
chapter 396 or has been convicted under s. 790.151 or has been
deemed a habitual offender under s. 856.011(3), or has had two or
more convictions under s. 316.193 or similar laws of any other state,
within the 3-year period immediately preceding the date on which the
application is submitted;
* * *
(i) Has not been adjudicated an incapacitated person under s.
744.331, or similar laws of any other state, unless 5 years have
elapsed since the applicant’s restoration to capacity by court order;
(j) Has not been committed to a mental institution under
chapter 394, or similar laws of any other state, unless the applicant
produces a certificate from a licensed psychiatrist that he or she has
not suffered from disability for at least 5 years before the date of
submission of the application[.]
* * *
(10) A license issued under this section shall be suspended or
revoked pursuant to chapter 120 if the licensee:
* * *
(e) Is committed as a substance abuser under chapter 397, or is
deemed a habitual offender under s. 856.011(3), or similar laws of any
other state;
* * *
(g) Is adjudicated an incapacitated person under s. 744.331, or
similar laws of any other state; or
(h) Is committed to a mental institution under chapter 394, or
similar laws of any other state.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
332
Notwithstanding s. 120.60(5), service of a notice of the suspension or
revocation of a concealed weapon or firearm license must be given by
either certified mail, return receipt requested, to the licensee at his or
her last known mailing address furnished to the Department of
Agriculture and Consumer Services, or by personal service. If a notice
given by certified mail is returned as undeliverable, a second attempt
must be made to provide notice to the licensee at that address, by
either first-class mail in an envelope, postage prepaid, addressed to the
licensee at his or her last known mailing address furnished to the
department, or, if the licensee has provided an e-mail address to the
department, by e-mail. Such mailing by the department constitutes
notice, and any failure by the licensee to receive such notice does not
stay the effective date or term of the suspension or revocation. A
request for hearing must be filed with the department within 21 days
after notice is received by personal delivery, or within 26 days after
the date the department deposits the notice in the United States mail
(21 days plus 5 days for mailing). The department shall document its
attempts to provide notice and such documentation is admissible in
the courts of this state and constitutes sufficient proof that notice was
given.
790.065. Sale and delivery of firearms
(2) Upon receipt of a request for a criminal history record check,
the Department of Law Enforcement shall, during the licensee’s call
or by return call, forthwith:
(a) Review any records available to determine if the potential buyer
or transferee:
* * *
4. Has been adjudicated mentally defective or has been
committed to a mental institution by a court or as provided in sub-
sub-subparagraph b.(II), and as a result is prohibited by state or
federal law from purchasing a firearm.
a. As used in this subparagraph, “adjudicated mentally defective”
means a determination by a court that a person, as a result of marked
subnormal intelligence, or mental illness, incompetency, condition,
or disease, is a danger to himself or herself or to others or lacks the

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
333
mental capacity to contract or manage his or her own affairs. The
phrase includes a judicial finding of incapacity under s.
744.331(6)(a), an acquittal by reason of insanity of a person charged
with a criminal offense, and a judicial finding that a criminal
defendant is not competent to stand trial.
b. As used in this subparagraph, “committed to a mental
institution” means:
(I) Involuntary commitment, commitment for mental
defectiveness or mental illness, and commitment for substance
abuse. The phrase includes involuntary inpatient placement as defined
in s. 394.467, involuntary outpatient [services] as defined in s.
394.4655, involuntary assessment and stabilization under s. 397.6818,
and involuntary substance abuse [services] under s. 397.6957, but
does not include a person in a mental institution for observation or
discharged from a mental institution based upon the initial review by
the physician or a voluntary admission to a mental institution. . . .
* * *
c. In order to check for these conditions, the department [FDLE]
shall compile and maintain an automated database of persons who are
prohibited from purchasing a firearm based on court records of
adjudications of mental defectiveness or commitments to mental
institutions.
(I) Except as provided in sub-sub-subparagraph (II), clerks of court
shall submit these records to the department within 1 month after the
rendition of the adjudication or commitment. Reports shall be
submitted in an automated format. The reports must, at a minimum,
include the name, along with any known alias or former name, the
sex, and the date of birth of the subject.
The 2013 Florida Legislature amended the above provisions of the state’s
weapons law to expand its applicability to individuals at designated Baker
Act receiving facilities who meet certain criteria for imminent danger due to
their mental illnesses but do not have a court order for placement under the
Baker Act or for substance abuse assessment, stabilization, or treatment. The
following selected provisions of section 790.065(2)(a)4, Florida Statutes,
govern who can be denied a license to carry a concealed weapon or purchase

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
334
a firearm, including the responsibilities of various individuals in carrying out
these provisions:
b. . . . .
(II) Notwithstanding sub-sub-subparagraph (I), voluntary admission
to a mental institution for outpatient or inpatient treatment of a person
who had an involuntary examination under s. 394.463, where each
of the following conditions have been met:
(A) An examining physician found that the person is an imminent
danger to himself or herself or others.
(B) The examining physician certified that if the person did not
agree to voluntary treatment, a petition for involuntary outpatient
or inpatient treatment would have been filed under s.
394.463(2)([g])4., or the examining physician certified that a petition
was filed and the person subsequently agreed to voluntary treatment
prior to a court hearing on the petition.
(C) Before agreeing to voluntary treatment, the person received
written notice of that finding and certification, and written notice
that as a result of such finding, he or she may be prohibited from
purchasing a firearm, and may not be eligible to apply for or retain a
concealed weapon or firearms license under s. 790.06 and the person
acknowledged such notice in writing, in substantially the following
form:
“I understand that the doctor who examined me believes I am a
danger to myself or to others. I understand that if I do not agree
to voluntary treatment, a petition will be filed in court to require
me to receive involuntary treatment. I understand that if that
petition is filed, I have the right to contest it. In the event a
petition has been filed, I understand that I can subsequently
agree to voluntary treatment prior to a court hearing. I
understand that by agreeing to voluntary treatment in either of
these situations, I may be prohibited from buying firearms and
from applying for or retaining a concealed weapons or firearms
license until I apply for and receive relief from that restriction
under Florida law.”

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
335
(D) A judge or a magistrate has, pursuant to sub-sub-subparagraph
c.(II), reviewed the record of the finding, certification, notice, and
written acknowledgment classifying the person as an imminent danger
to himself or herself or others, and ordered that such record be
submitted to the department.
c. . . . .
(II) For persons committed to a mental institution pursuant to sub-sub-
subparagraph b.(II), within 24 hours after the person’s agreement
to voluntary admission, a record of the finding, certification,
notice, and written acknowledgment must be filed by the
administrator of the receiving or treatment facility, as defined in
s. 394.455, with the clerk of the court for the county in which the
involuntary examination under s. 394.463 occurred. No fee shall be
charged for the filing under this sub-sub-subparagraph. The clerk
must present the records to a judge or magistrate within 24 hours
after receipt of the records. A judge or magistrate is required and
has the lawful authority to review the records ex parte and, if the
judge or magistrate determines that the record supports the
classifying of the person as an imminent danger to himself or
herself or others, to order that the record be submitted to the
department. If a judge or magistrate orders the submittal of the
record to the department, the record must be submitted to the
department within 24 hours.
II. Applicability of the Law
The law doesn’t apply to persons in the following circumstances:
Persons entering a facility on voluntary status and remaining on voluntary
status regardless of their potential imminent dangerousness. The Baker Act
law and multiple appellate cases place no duty on mental health
professionals to initiate involuntary status even if the criteria for involuntary
status are documented.
Persons entering a facility on involuntary status on the basis of self-neglect
instead of active danger, regardless of the severity of their mental illnesses.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
336
Persons on involuntary examination status who are discharged because they
fail to meet any one of the involuntary placement criteria, without being
converted to voluntary status.
Persons whose potential for ”dangerousness” is not considered by a
physician as “imminent.”
Persons whose hearing on involuntary placement takes place and the petition
is dismissed by the court because a less restrictive setting is found,
regardless of the criteria related to active danger.
Persons on involuntary examination status who are first taken to hospitals
not designated by DCF as receiving facilities for examination or treatment of
medical conditions and are released directly by a physician or psychologist
or are transferred by such hospitals to voluntary status before transfer to a
designated receiving facility.
Persons subject to the involuntary provisions of the Marchman Act (chapter
397, Florida Statutes) unless ordered by the court to undergo involuntary
assessment and stabilization or involuntary treatment.
The law doesn’t apply to guns currently owned by and in the possession of
persons who have been reported as imminently dangerous due to mental illness —
it applies only to future purchases (sale and delivery) or obtaining/retaining a
concealed weapons permit.
III. Responsibility of Various Entities to Implement Section 790.06, Florida
Statutes
A. Physicians Practicing at Baker Act Receiving or Treatment Facilities
A person for whom an involuntary examination has been initiated must have a
physician or clinical psychologist, without unnecessary delay, conduct and
document the mandatory initial involuntary examination, including:
review the person’s recent behavior;
review the “Transportation to Receiving Facility” form (CF-MH 3100);
review one of the following:
o “Ex Parte Order for Involuntary Examination” or

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
337
o “Report of Law Enforcement Officer Initiating Involuntary Examination”
or
o “Certificate of Professional Initiating Involuntary Examination”;
conduct a brief psychiatric history; and
conduct a face-to-face examination to determine whether the person meets
the criteria for release.
An individual who has had an involuntary examination initiated and been found to
be of imminent danger, who requests transfer to voluntary status in lieu of a
petition for involuntary placement (form CF-MH 3032) or requests withdrawal of a
petition already filed, is subject to this reporting to the court.
Since chapter 790, Florida Statutes, doesn’t define “imminent danger,” the
definition found in the criteria for involuntary placement (section 394.467(1)(a)2.b,
Florida Statutes) may be used: “There is substantial likelihood that in the near
future he or she will inflict serious bodily harm on self or others, as evidenced by
recent behavior causing, attempting, or threatening such harm.”
The law requires a notification to and acknowledgement by the individual that
information will be provided by the facility to the court that will lead to a
prohibition against firearm purchases or having a concealed weapon permit. A
certification of competence (form CF-MH 3104) conducted by a physician should
be completed to ensure the individual is competent to make well-reasoned, willful,
and knowing decisions.
The form included in this chapter titled “Finding and Certification by an
Examining Physician of Person’s Imminent Dangerousness” can be used to
document the individual’s imminent dangerousness and competence to fully
understand the meaning and consequences of converting to voluntary status.
The physician’s finding and certification must be provided to facility staff to give
the patient a full explanation that the conversion to voluntary status may result in a
prohibition against firearm purchase. A copy of the physician’s finding and
certification must be retained in the individual’s clinical record.
B. Baker Act Receiving Facility Administrators (or Designee)
If an individual who is found competent to consent to treatment isn’t released from
the facility and desires to convert to voluntary status but is found by the physician

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
338
to be imminently dangerous, and the patient is permitted to convert from
involuntary to voluntary status, the physician must document that finding and
certification. Facility staff should fully explain to the individual that the conversion
to voluntary status may result in a prohibition against firearm purchases and
obtaining or retaining a concealed weapons permit. The form titled “Patient’s
Notice and Acknowledgment” found below can be used for this purpose. A copy of
the signed and witnessed Notice and Acknowledgment form must be retained in
the individual’s clinical record.
Staff will submit to the administrator of the receiving or treatment facility the
following:
Cover Sheet
Physician’s Finding and Certification
Patient’s Notice and Acknowledgment forms
Application for Voluntary Admission
If a petition for involuntary inpatient placement has already been submitted to the
clerk of court, a Notification to Court of Withdrawal of Petition (form CF-MH
3033) must be filed within one business day of the decision to convert to voluntary
status with the court and sent to the state attorney, public defender, and guardian or
designated representative. If the decision is made within 24 hours prior to the
hearing, the notification must be made immediately by phone to all required
parties, followed by submission of the written notice.
The packet of forms referenced above must be submitted by the facility to the clerk
of court within 24 hours of the decision to convert the individual from involuntary
to voluntary status. This cannot be delayed because of weekends or legal holidays.
No fee shall be charged for this filing.
C. Clerks of Court
Upon receipt of the packet of forms from a Baker Act Receiving or Treatment
Facility, the clerk will assign a case number and other activities routinely done
upon petition filing. Within 24 hours, the clerk will submit the petition and other
related forms to a judge or magistrate for review.
Rule 2.514, Florida Rules of Judicial Administration, defines how hours and days
are computed for court use when a statute doesn’t specify how it is to be done

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
339
(applies only to courts, not to mental health facilities). Rule 2.514(a)(2) provides
that when a law states a period of time in “hours,” the computation of hours is as
follows:
(A) begin counting immediately on the occurrence of the event that
triggers the period;
(B) count every hour, including hours during intermediate
Saturdays, Sundays, and legal holidays; and
(C) if the period would end on a Saturday, Sunday, or legal holiday,
or during any period of time extended through an order of the chief
justice . . . , the period continues to run until the same time on the next
day that is not a Saturday, Sunday, or legal holiday and does not fall
within any period of time extended through an order of the chief
justice.
D. Judges or Magistrates
Upon receipt of the petition and related forms from the clerk of court, the judge or
magistrate must review the record of the finding, certification, notice, and written
acknowledgment classifying the person as an imminent danger to self or others.
A judge or magistrate is required and has the lawful authority to
review the records ex parte and, if the judge or magistrate determines
that the record supports the classifying of the person as an imminent
danger to himself or herself or others, to order that the record be
submitted to the department [FDLE]. If a judge or magistrate orders
the submittal of the record to the department, the record must be
submitted to the department within 24 hours.
§ 790.065(2)(a)4.c.(II), Fla. Stat. The clerk of court must submit these records of
an individual converting from involuntary to voluntary status to FDLE within 24
hours (as defined above) in an automated format. The reports must include at least
the individual’s name (including any known aliases or former names), sex, and
date of birth. § 790.065(2)(a)4.c, Fla. Stat.
Other records relating to firearm prohibition must be submitted by the court within
one month after the rendition of the adjudication or commitment, including:
Ordered to involuntary substance abuse assessment (§ 397.6818)

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
340
Ordered to involuntary substance abuse services (§ 397.6957)
Ordered to involuntary inpatient placement (§ 394.467)
Ordered to involuntary outpatient services (§ 394.4655)
Adjudicated incapacitated under § 744.331 or any similar law of any other
state
Acquittal by reason of insanity of a person charged with a criminal offense
(§ 916.15)
Judicial finding that a criminal defendant is not competent to stand trial
(§ 916.12)
Deemed a habitual offender under § 856.011(3) or other similar laws of
Florida
Convicted under § 790.151
Has had two or more convictions under § 316.193 or similar laws of any
other state
§ 790.06(1), (10), Fla. Stat.
E. Florida Department of Law Enforcement
In order to check for these conditions, the department [FDLE] shall
compile and maintain an automated database of persons who are
prohibited from purchasing a firearm based on court records of
adjudications of mental defectiveness or commitments to mental
institutions. . . . The department is authorized to disclose data
collected . . . to agencies of the Federal Government and other states
for use exclusively in determining the lawfulness of a firearm sale or
transfer. The department is also authorized to disclose this data to the
Department of Agriculture and Consumer Services for purposes of
determining eligibility for issuance of a concealed weapons or
concealed firearms license and for determining whether a basis exists
for revoking or suspending a previously issued license pursuant to s.
790.06(10).
§ 790.065(2)(a)4., Fla. Stat.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
341
IV. Relief from a Firearm Disability
Persons who have had their right to purchase a firearm prohibited may petition the
court for relief of this firearm disability under section 790.065(2)(a)4.d, Florida
Statutes, as follows:
A person who has been adjudicated mentally defective or committed
to a mental institution, as those terms are defined in this paragraph,
may petition the court that made the adjudication or commitment, or
the court that ordered that the record be submitted to the department
pursuant to sub-sub-subparagraph c.(II), for relief from the firearm
disabilities imposed by such adjudication or commitment. A copy of
the petition shall be served on the state attorney for the county in
which the person was adjudicated or committed. The state attorney
may object to and present evidence relevant to the relief sought by the
petition. The hearing on the petition may be open or closed as the
petitioner may choose. The petitioner may present evidence and
subpoena witnesses to appear at the hearing on the petition. The
petitioner may confront and cross-examine witnesses called by the
state attorney. A record of the hearing shall be made by a certified
court reporter or by court-approved electronic means. The court shall
make written findings of fact and conclusions of law on the issues
before it and issue a final order. The court shall grant the relief
requested in the petition if the court finds, based on the evidence
presented with respect to the petitioner’s reputation, the petitioner’s
mental health record and, if applicable, criminal history record, the
circumstances surrounding the firearm disability, and any other
evidence in the record, that the petitioner will not be likely to act in a
manner that is dangerous to public safety and that granting the relief
would not be contrary to the public interest. If the final order denies
relief, the petitioner may not petition again for relief from firearm
disabilities until 1 year after the date of the final order. The petitioner
may seek judicial review of a final order denying relief in the district
court of appeal having jurisdiction over the court that issued the order.
The review shall be conducted de novo. Relief from a firearm
disability granted under this sub-subparagraph has no effect on the
loss of civil rights, including firearm rights, for any reason other than
the particular adjudication of mental defectiveness or commitment to
a mental institution from which relief is granted.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
342
The above provisions of chapter 790 apply to persons for whom the court
has ordered specified interventions, including:
Ordered to involuntary substance abuse assessment (§ 397.6818)
Ordered to involuntary substance abuse services (§ 397.6957)
Ordered to involuntary inpatient placement (§ 394.467)
Ordered to involuntary outpatient services (§ 394.4655)
Adjudicated incapacitated under § 744.331 or any similar law of any other
state
Acquittal by reason of insanity of a person charged with a criminal offense
(§ 916.15)
Judicial finding that a criminal defendant is not competent to stand trial
(§ 916.12)
A person who has been adjudicated mentally defective or committed
to a mental institution, as those terms are defined in this paragraph,
may petition the court that made the adjudication or commitment, or
the court that ordered that the record be submitted to [FDLE], for
relief from the firearm disabilities imposed by such adjudication or
commitment. A copy of the petition shall be served on the state
attorney for the county in which the person was adjudicated or
committed. The state attorney may object to and present evidence
relevant to the relief sought by the petition.
§ 790.065(2)(a)4.d, Fla. Stat.
The hearing on the petition may be open or closed as the petitioner
may choose. The petitioner may present evidence and subpoena
witnesses to appear at the hearing on the petition. The petitioner may
confront and cross-examine witnesses called by the state attorney. A
record of the hearing shall be made by a certified court reporter or by
court-approved electronic means. The court shall make written
findings of fact and conclusions of law on the issues before it and
issue a final order. The court shall grant the relief requested in the
petition if the court finds, based on the evidence presented with
respect to the petitioner’s reputation, the petitioner’s mental health

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
343
record and, if applicable, criminal history record, the circumstances
surrounding the firearm disability, and any other evidence in the
record, that the petitioner will not be likely to act in a manner that is
dangerous to public safety and that granting the relief would not be
contrary to the public interest.
Id.
“Upon receipt of proper notice of relief from firearm disabilities [FDLE] shall
delete any mental health record of the person granted relief from the automated
database of persons who are prohibited from purchasing a firearm based on court
records of adjudications of mental defectiveness or commitments to mental
institutions.” § 790.065(2)(a)4.e, Fla. Stat.
If the final order denies relief, the petitioner may not petition again for
relief from firearm disabilities until 1 year after the date of the final
order. The petitioner may seek judicial review of a final order denying
relief in the district court of appeal having jurisdiction over the court
that issued the order. The review shall be conducted de novo. Relief
from a firearm disability granted under this sub-subparagraph has no
effect on the loss of civil rights, including firearm rights, for any
reason other than the particular adjudication of mental defectiveness
or commitment to a mental institution from which relief is granted.
§ 790.065(2)(a)4.d, Fla. Stat.
Below are four flowcharts that reflect the decision points to be made:
Admission by Voluntary Status
Admission by Involuntary Status
Firearm Prohibition Process
Petition for Relief from Firearm Disability
Also below are sample forms that can be used to implement the provisions of
firearm prohibition legislation:
Cover Sheet to be filed by a Receiving or Treatment Facility Administrator
to the Clerk of Court

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
344
Finding and Certification by an Examining Physician of Person’s Imminent
Dangerousness
Patient’s Notice and Acknowledgment
Application for Voluntary Admission of an Adult to a Receiving Facility
Notification to Court of Withdrawal of Petition for Hearing on Involuntary
Inpatient or Involuntary Outpatient Placement
Order of Court to Present Record of Finding to FDLE or Requiring Further
Documentation on Voluntary Transfer
Petition and Order for Relief from Firearm Disabilities Imposed by the Court

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
345
V. Flowcharts
A. Admission by Voluntary Status

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
346
B. Admission by Involuntary Status

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
347
C. Firearm Prohibition Process

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
348
D. Petition for Relief from Firearm Disability

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
349
VI. Frequently Asked Questions
A. Applicable State Statutes
What state law requires the submission of mental health data to FDLE for the
purpose of firearm purchase approval?
Section 790.065(2)(a), Florida Statutes, “Sale and delivery of firearms,” outlines
the firearm purchase prohibition for persons adjudicated as mentally defective or
committed to a mental institution. The terms are defined in section 790.065(2)(a)4.
as follows:
a. . . . . “[A]djudicated mentally defective” means a determination
by a court that a person, as a result of marked subnormal intelligence,
or mental illness, incompetency, condition, or disease, is a danger to
himself or herself or to others or lacks the mental capacity to contract
or manage his or her own affairs. The phrase includes a judicial
finding of incapacity under s. 744.331(6)(a), an acquittal by reason of
insanity of a person charged with a criminal offense, and a judicial
finding that a criminal defendant is not competent to stand trial.
b. . . . . “[C]ommitted to a mental institution” means . . . an
involuntary commitment, commitment for mental defectiveness or
mental illness, and commitment for substance abuse. The phrase
includes involuntary inpatient placement as defined in s. 394.467,
involuntary outpatient [services] as defined in s. 394.4655,
involuntary assessment and stabilization under s. 397.6818, and
involuntary substance abuse [services] under s. 397.6957, but does not
include a person in a mental institution for observation or discharged
from a mental institution based upon the initial review by the
physician or a voluntary admission to a mental institution. . . .
Chapter 2013-249, Laws of Florida, effective July 1, 2013, amended the definition
of “committed to mental institution” to include
voluntary admission to a mental institution for outpatient or inpatient
treatment of a person who had an involuntary examination under s.
394.463, where each of the following conditions has been met:
(A) An examining physician found that the person is an imminent
danger to himself or herself or others.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
350
(B) The examining physician certified that if the person did not
agree to voluntary treatment, a petition for involuntary outpatient or
inpatient treatment would have been filed under s. 394.463(2)([g])4.,
or the examining physician certified that a petition was filed and the
person subsequently agreed to voluntary treatment prior to a court
hearing on the petition.
(C) Before agreeing to voluntary treatment, the person received
written notice of that finding and certification, and written notice that
as a result of such finding, he or she may be prohibited from
purchasing a firearm, and may not be eligible to apply for or retain a
concealed weapon or firearms license under s. 790.06 and the person
acknowledged such notice in writing. . . .
(D) A judge or a magistrate has . . . reviewed the record of the
finding, certification, notice, and written acknowledgment classifying
the person as an imminent danger to himself or herself or others, and
ordered that such record be submitted to the department.
B. Mental Competency (MECOM) Database
What is the Mental Competency (MECOM) Database?
Section 790.065(2)(a)4.c, Florida Statutes, authorizes FDLE to establish and
maintain “an automated database [designated as the Mental Competency
(MECOM) database] of persons who are prohibited from purchasing a firearm
based on court records of adjudications of mental defectiveness or commitments to
mental institutions.” The database contains information submitted by the clerks of
court.
FDLE must check this database before approving the sale of a firearm by a
licensed dealer, to determine whether the potential purchaser is prohibited by
federal law from purchasing (or possessing) a firearm because of having been
adjudicated mentally defective or committed to a mental institution. The data
entered by the clerks gets uploaded to the National Instant Criminal History
Background Check System (NICS), maintained by the FBI, to comply with federal
law requiring background checks on prospective firearm purchasers. The data is
included in the NICS Index, which is used nationwide in determining firearm
purchase eligibility. The MECOM database is also used by the Florida Department
of Agriculture and Consumer Services, Division of Licensing (DOACS), for the
purpose of issuing or retaining a concealed weapon/firearm license.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
351
Can the mental health data be submitted to FDLE in more than one way?
Entry by the clerk directly into the MECOM database is the preferred method.
FDLE has assisted clerks by accepting faxes and mailed or emailed submissions
because of the critical nature of the information. FDLE will continue to so as
resources permit; however, the responsibility to enter the data remains with the
clerks.
What are the mandated fields for MECOM database entry?
The fields necessary for entry into the MECOM database include name, any known
alias or former name, sex, date of birth, and uniform case number (UCN). The
MECOM database is designed to reject records that do not meet the minimum
identification requirements outlined in the law. Because the system is structured to
allow for searching records based on name and other personal identifying
information, the more information provided to FDLE, the easier it will be to
identify an individual attempting to purchase a firearm. For this reason, the clerks’
offices may receive calls requesting additional data to assist in making informed
decisions.
What kind of information would be beneficial as additional record subject
identifiers?
If available, the subject’s social security number, place of birth, driver license
number, and last known address would be helpful.
What timeframe does the information need to be entered or submitted into
the MECOM database?
Under section 790.065(2)(a)4.c.I, Florida Statutes, “clerks of court shall submit
these records to the department within 1 month after the rendition of the
adjudication or commitment.” These records would include:
Ordered to involuntary substance abuse assessment (§ 397.6818)
Ordered to involuntary substance abuse services (§ 397.6957)
Ordered to involuntary inpatient placement (§ 394.467)
Ordered to involuntary outpatient services (§ 394.4655)

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
352
Adjudicated incapacitated under § 744.331 or any similar law of any other
state
Acquittal by reason of insanity of a person charged with a criminal offense
(§ 916.15)
Judicial finding that a criminal defendant is not competent to stand trial
(§ 916.12)
Deemed a habitual offender under § 856.011(3) or other similar laws of
Florida
Convicted under § 790.151
Has had two or more convictions under § 316.193 or similar laws of any
other state
§§ 790.06, Fla. Stat., 790.065, Fla. Stat.
However, when persons are committed to a mental institution following an
involuntary examination under section 394.463, Florida Statutes, clerks must
submit the record to FDLE within 24 hours of the order.
If a person is the subject of more than one qualifying adjudication of mental
defectiveness or commitment to a mental institution, should data on the later
adjudications or commitments continue to be entered in the MECOM
database?
Yes. The most recent data will be displayed when the database is queried. It is
important for all persons involved in the firearm purchase background check
process to have access to the most complete, current, and accurate information.
Such information will be vital in making the correct decisions at the initial
approval stage, during any appeal of a denial, and when removal of a name from
the database is requested.
How do clerks and their employees access the MECOM database?
The MECOM database is available through the Florida Criminal Justice Network
(CJNet). The access form found on the first page of the database must be
completed and then faxed, mailed, or emailed to FDLE, after which a password
and username will be assigned to the individual. As a security precaution, the
password and username (logon) should not be shared with anyone else. Whenever

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
353
information is added or updated in the database, the system automatically records
the date and identifies the person who updated or added the information by his or
her logon name.
If an error is found in the MECOM database, should the clerks correct the
error?
If an error is identified, contact the Firearm Purchase Program at (850) 410-8139
for correction.
Is the data in the MECOM database public record?
FDLE understands civil orders (adjudication or commitment) to be confidential.
Under section 790.065(2)(a)4.f, Florida Statutes, if the records submitted by the
clerks are confidential or exempt from disclosure in the custody of the courts, they
will retain that status in the MECOM database. See the Florida Attorney General’s
Government-In-The-Sunshine Manual (2015 ed.), Part II.D.10. FDLE is authorized
by the law to disclose information to the Department of Agriculture and Consumer
Services for determining the eligibility of an applicant for a concealed weapons
license. FDLE is also authorized to disclose data to federal or state agencies with
regard to the lawfulness of the sale or transfer of a firearm.
Who should be called with questions about the MECOM database?
Questions should be directed to the Firearm Purchase Program at (850) 410-8139.
C. Substance Abuse
Does the law apply to substance abuse?
Yes, the definition of “committed to a mental institution” in the law includes
“commitment for substance abuse” and refers to “s. 397.6818, and involuntary
substance abuse [services] under s. 397.6957.”
Should defendants who have been referred to drug court be entered in the
database?
Referral to drug court, alone, is not a sufficient basis to enter a person in the
MECOM database. See the previous answer.
Should all persons detained or held under the Baker or Marchman Acts be
reported to FDLE?

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
354
Only persons who are committed to a mental institution or adjudicated mentally
defective should be entered into the MECOM database. If such a court order was
not issued as a result of the Baker Act or Marchman Act, the person should not be
entered into the MECOM database.
Should data on persons who voluntarily admit themselves for substance abuse
treatment be entered into the database?
No, unless there is further action by a physician and court under the process
established by chapter 2013-249, Laws of Florida. See the section on chapter 2013-
249, Laws of Florida, for further details about the new requirements.
Should an order for involuntary treatment, pursuant to section 397.6818,
Florida Statutes, which orders the subject to attend an outpatient treatment
program, such as AA meetings or group therapy sessions, be entered into the
database?
An order for involuntary assessment and stabilization under section 397.6818,
Florida Statutes, qualifies for entry in the database. Following involuntary
assessment and stabilization, per section 397.6822, Florida Statutes, the client may
“where appropriate, [be] refer[red] . . . to another treatment facility or service
provider, or to community services.” Such referral could include attending AA
meetings, group therapy sessions, etc.
Where a petition for involuntary treatment for substance abuse is filed under
chapter 397, Florida Statutes, and the respondent signed a waiver of hearing
authorizing the court to enter an order for involuntary treatment, should such
an order be entered into the database?
A court order placing someone in a substance abuse services program under the
authority of chapter 397, Florida Statutes, is a prohibitor for the purchase of a
firearm and should be entered into the database. The waiver of hearing does not
negate the effect of the order.
D. Juveniles
Should juveniles who are not able to stand trial because of their age be
entered into the MECOM database?
No. If a minor defendant is found to be “incompetent” to proceed solely because of
his or her age, the resulting order is not considered to be an adjudication of mental
incompetency and does not qualify for entry into the MECOM database.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
355
Should juveniles who have been found mentally incompetent be entered into
the MECOM database?
The federal law that prohibits a person “who has been adjudicated as a mental
defective or who has been committed to a mental institution” from purchasing a
firearm, 18 U.S.C. § 922(g)(4), does not mention an age limit for such adjudication
or commitment, nor does the expanded definition of this phrase, found at 27 C.F.R.
§ 478.11. Accordingly, it has been concluded that an adjudication or commitment
of a minor meeting the requirements of the law should be reported.
E. Capacity/Competency
Should an order determining someone totally incapacitated which does not
refer to section 744.331, Florida Statutes, be entered into the database?
An order determining someone to be totally incapacitated as authorized under
section 744.331, Florida Statutes, would qualify for entry, even if a different (or
no) statute is cited.
If a defendant is found incompetent to stand trial, should he or she be entered
into the database? What happens if the defendant is later found competent to
stand trial?
If a defendant is found incompetent to stand trial by the court, that should be
entered in the MECOM database. If the defendant is later determined to be
competent to proceed to trial, that fact alone will not authorize removal from the
database. The law authorizes a process for restoration of firearm rights following
loss due to, for example, a finding of incompetency to stand trial. The outcome of
the trial may or may not impose a separate firearm purchase prohibitor (e.g., a
felony conviction).
F. Relief from Disability
How can a person be removed from the MECOM database?
A process for restoration of firearm rights, also referred to as “Relief from
Disability,” is authorized at section 790.065(2)(a)4.d, Florida Statutes, which could
allow for the removal of persons from the MECOM database.
Is the process for removal from the MECOM database automatic following
the restoration of firearm rights?

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
356
No, “upon receipt of proper notice of relief from firearm disabilities granted [by a
court],” FDLE will remove the subject from the database; the process is not
automatic.
If a person believes his or her name should be removed from the database, or
needs information in this regard, to whom should the clerk’s office direct him
or her?
Contact the Firearm Purchase Program at (850) 410-8139. The person should be
referred to section 790.065, Florida Statutes, for the legal basis for removal.
G. Provisions of Chapter 2013-249, Laws of Florida
How did this law amend section 790.065, Florida Statutes, “Sale and Delivery
of Firearms”?
Chapter 2013-249, Laws of Florida, effective July 1, 2013, amended the definition
of “committed to mental institution” to include
voluntary admission to a mental institution for outpatient or inpatient
treatment of a person who had an involuntary examination under s.
394.463, where each of the following conditions has been met:
(A) An examining physician found that the person is an imminent
danger to himself or herself or others.
(B) The examining physician certified that if the person did not
agree to voluntary treatment, a petition for involuntary outpatient or
inpatient treatment would have been filed under s. 394.463(2)([g])4.,
or the examining physician certified that a petition was filed and the
person subsequently agreed to voluntary treatment prior to a court
hearing on the petition.
(C) Before agreeing to voluntary treatment, the person received
written notice of that finding and certification, and written notice that
as a result of such finding, he or she may be prohibited from
purchasing a firearm, and may not be eligible to apply for or retain a
concealed weapon or firearms license under s. 790.06 and the person
acknowledged such notice in writing. . . .
(D) A judge or a magistrate has . . . reviewed the record of the
finding, certification, notice, and written acknowledgment classifying

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
357
the person as an imminent danger to himself or herself or others, and
ordered that such record be submitted to the department.
What are examples where the new law does not apply?
The law doesn’t apply to persons in the following circumstances:
Persons entering a facility on voluntary status and remaining on voluntary
status regardless of their potential imminent dangerousness. The Baker Act
law and multiple appellate cases place no duty on mental health
professionals to initiate involuntary status even if the criteria for involuntary
status are documented.
Persons entering a facility on involuntary status on the basis of self-neglect
instead of active danger, regardless of the severity of their mental illnesses.
Persons on involuntary examination status who are discharged because they
fail to meet any one of the involuntary placement criteria, without being
converted to voluntary status.
Persons whose potential for “dangerousness” is not considered by a
physician as “imminent.”
Persons whose hearing on involuntary placement takes place and the petition
is dismissed by the court because a less restrictive setting is found,
regardless of the criteria related to active danger.
Persons on involuntary examination status who are first taken to hospitals
not designated by DCF as receiving facilities for examination or treatment of
medical conditions and are released directly by a physician or psychologist
or are transferred by such hospitals to voluntary status before transfer to a
designated receiving facility.
Persons subject to the involuntary provisions of the Marchman Act (chapter
397, Florida Statutes) unless ordered by the court to undergo involuntary
assessment and stabilization or involuntary treatment.
What is the duty of physicians at receiving or treatment facilities?
The physician or clinical psychologist must, without unnecessary delay, conduct
and document the mandatory initial involuntary examination, including:

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
358
review the person’s recent behavior;
review the “Transportation to Receiving Facility” form (CF-MH 3100);
review one of the following:
o “Ex Parte Order for Involuntary Examination” or
o “Report of Law Enforcement Officer Initiating Involuntary Examination”
or
o “Certificate of Professional Initiating Involuntary Examination”;
conduct a brief psychiatric history; and
conduct a face-to-face examination to determine whether the person meets
the criteria for release.
Under the 2013 requirements, what forms must the receiving or treatment
facility file with the clerk of court?
Upon meeting the conditions, the administrator of the receiving or treatment
facility must file the following forms with the clerk of court for the county in
which the involuntary examination occurred:
Finding and Certification by an Examining Physician of Person’s Imminent
Dangerousness.
Patient’s Notice and Acknowledgment (of firearm disabilities).
If applicable, Notification to Court of Withdrawal of Petition for Hearing on
Involuntary Inpatient or Involuntary Outpatient Placement.
When must the receiving or treatment facility file the forms with the clerk of
court?
Forms must be filed with the clerk of court within 24 hours of the patient’s
certification as an imminent danger and agreement to transfer to voluntary status.
When must the clerk of court present the filed records to a judge or
magistrate?

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
359
The clerk of court is required to present the records to a judge or magistrate within
24 hours after receipt of such records from the receiving or treatment facility.
If a judge or magistrate issues an order, when must the clerk of court enter
the information into the MECOM database?
The law requires the clerk of court to submit the record to FDLE, by entering the
information directly into the MECOM database, within 24 hours of the order.
What is meant by the timeframe of 24 hours for the courts?
Rule 2.514, Florida Rules of Judicial Administration, defines how hours and
days are computed for court use when a statute doesn’t specify how it is to
be done (applies only to courts, not to mental health facilities). Rule
2.514(a)(2) provides that when a law states a period of time in “hours,” the
computation of hours is as follows:
(A) begin counting immediately on the occurrence of the event that
triggers the period;
(B) count every hour, including hours during intermediate Saturdays,
Sundays, and legal holidays; and
(C) if the period would end on a Saturday, Sunday, or legal holiday, or
during any period of time extended through an order of the chief justice . . . ,
the period continues to run until the same time on the next day that is not a
Saturday, Sunday, or legal holiday and does not fall within any period of
time extended through an order of the chief justice.
What must the patient’s notice and acknowledgment include?
Under section 790.065(2)(a)4.b(II)c, Florida Statutes, the notice must be
substantially as follows:
I understand that the doctor who examined me believes I am a danger
to myself or to others. I understand that if I do not agree to voluntary
treatment, a petition will be filed in court to require me to receive
involuntary treatment. I understand that if that petition is filed, I have
the right to contest it. In the event a petition has been filed, I
understand that I can subsequently agree to voluntary treatment prior
to a court hearing. I understand that by agreeing to voluntary
treatment in either of these situations, I may be prohibited from

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
360
buying firearms and from applying for or retaining a concealed
weapons or firearms license until I apply for and receive relief from
that restriction under Florida law.”
Am I required to use the forms included in this chapter?
No. Receiving and treatment facilities may develop their own forms. The sample
forms below are provided as examples, but they may also be used if a facility
chooses to do so.
VII. Forms
The following forms at A, B, C, F, and G are recommended forms and were
developed by the Florida Department of Law Enforcement. The forms at D
and E are recommended forms promulgated by DCF.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
361
A. Firearm Prohibition Cover Sheet
Firearm Prohibition
Cover Sheet
Confidential Information
Submission to Clerk of Court of Statutorily Required Documents for Review
by Judge or Magistrate Regarding Purchase of Firearms or Applying/Retaining
Concealed Weapons or Firearms License by Persons Who Have a Mental Illness
and Are Deemed Imminently Dangerous
Attached are the following forms regarding the determination an individual in this receiving or treatment
facility has been found to be an imminent danger to self or others:
□ Finding and Certification by an Examining Physician of Person’s Imminent Dangerousness
□ Patient’s Notice and Acknowledgment (Purchase of Firearms and Application for or Retention of a
Concealed Weapons or Firearms License)
□ Application for Voluntary Admission of an Adult (Receiving Facility)
□ Notification to Court of Withdrawal of Petition for Hearing on Involuntary Inpatient or Involuntary
Outpatient Placement
__________________________________ _______________ ___________
Signature of Administrator or Designee Date Time
__________________________________ ___________________________________
Printed Name of Administrator or Designee Name of Receiving or Treatment Facility
Printed Name of Patient ___________________________ Gender ___________________
Date of Birth ____________________________________ Race _______________
Social Security Number: ___________________________
See s. 394.463(2)(i)4, 790.06 and 790.065 Florida Statutes
Confidential Information
Revised 03/14

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
362
B. Finding and Certification by an Examining Physician of Person’s Imminent
Dangerousness
Finding and Certification by an Examining Physician
of Person’s Imminent Dangerousness
I, ________________________________________, a physician licensed pursuant to chapter 458 or
459, Florida Statutes, examined __________________________, a patient in
______________________________________________ (name of receiving or treatment facility) on
_______________ (date) at ________ a.m./p.m.
I determined this individual is an imminent danger to self or others based on the following:
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Please Check One
□ I certify if the person had not agreed to voluntary treatment, a petition for involuntary outpatient or
inpatient treatment would have been filed.
□ I certify a petition was filed and the person subsequently agreed to voluntary treatment prior to a court
hearing on the petition.
I have found this person has the capacity to make well-reasoned, willful, and knowing decisions
concerning his or her medical or mental health treatment and therefore is competent to transfer to
voluntary status and to consent to treatment.
__________________________________ _______________ ____________
Signature of Examining Physician Date Time
__________________________________ ____________________________________
Printed Name of Examining Physician License Number
Printed Name of Patient ___________________________ Gender _____________
Date of Birth ____________________________________ Race _______________
Social Security Number: ___________________________
See s. 790.06 and 790.065 Florida Statutes
Confidential Information
Revised 03/14

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
363
C. Patient’s Notice and Acknowledgment
Patient’s Notice and Acknowledgment
Purchase of Firearms and Application for or Retention of a
Concealed Weapons or Firearms License
I, __________________________________________________________________ do hereby
(Full printed name of person whose admission is being requested)
confirm I have received written notice of the finding and certification from an examining physician advising
if I do not agree to voluntary admission, a petition for involuntary outpatient or inpatient treatment will be
filed under s. 394.463(2)(i)4, F.S., or the examining physician certified a petition was filed and I have
subsequently agreed to voluntary treatment prior to a court hearing on the petition.
I further acknowledge I understand the doctor who examined me believes I am an imminent danger to
myself or to others. I understand if I do not agree to voluntary treatment, a petition will be filed in court to
require me to receive involuntary treatment. I understand if that petition is filed, I have the right to contest
it. I understand by agreeing to voluntary treatment in either of these situations, I may be prohibited from
purchasing firearms and from applying for, or retaining, a concealed weapons or firearms license until I
apply for, and receive, relief from that restriction under Florida law.
I understand that the doctor’s finding and certification, this notice and signed acknowledgment, and my
application for voluntary admission will be filed with the court.
______________________________________________________________________________
Signature of Competent Adult Printed Name Date Time
______________________________________________________________________________
Signature of Witness Printed Name Date Time
Printed Name of Patient ___________________________ Gender _____________
Date of Birth ____________________________________ Race _______________
Social Security Number: ___________________________
See s. 394.463(2)(i)4, 790.06 and 790.065, Florida Statutes
Confidential Information
Revised 03/14

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
364
D. Application for Voluntary Admission of an Adult (Receiving Facility)
Application for Voluntary Admission of an Adult
(Receiving Facility)
I, _________________________________________________ do hereby apply for admission to
Full printed name of person whose admission is being requested
________________________________________________________________________________________________________
Fill in name of facility
for observation, diagnosis, care, and treatment of a mental illness, and I certify the information given on this
application is true and correct to the best of my knowledge and belief.
I am making this application for voluntary admission after sufficient explanation and disclosure to make a
knowing and willful decision without any element of force, fraud, deceit, duress, or other form of constraint or
coercion. The reason for my admission to this facility is:
_____________________________________________________________________________________
_____________________________________________________________________________________
____________________________________________________________________________________.
I am a competent adult with the capacity to make well-reasoned, willful, and knowing decisions concerning my
medical or mental health treatment. I do not have a guardian, guardian advocate, or currently have a health care
surrogate/proxy making health care decisions for me.
I have have not provided a copy of advance directive(s).
If so, the advance directives include my:
Living Will
Health Care Surrogate,
Mental Health Care Surrogate,
Other as specified:
I have been provided with a written explanation of my rights as a person on voluntary status and they have been
fully explained to me. I understand this facility is authorized by law to detain me without my consent for
up to 24 hours after I make a request for discharge; unless a petition for involuntary inpatient placement or
involuntary outpatient placement is filed with the Court within two (2) court working days of my request for
discharge in which case I may be held pending a hearing on the petition.
I understand that I may be billed for the cost of my treatment.
____________________________________ ______________ ________ a.m. p.m.
Signature of Competent Adult Date Time
________________________ ___________________ _____________ ________ a.m. p.m.
Printed Name of Witness Signature of Witness Date Time
No notice of this admission is to be made without the consent of the person except in case of
an emergency. The use of this form for a voluntary admission requires that a “Certification of
Person’s Competence to Provide Express and Informed Consent” be completed within 24
hours and if the form is used for a transfer of a person from involuntary to voluntary status,
the “Certification” must be completed prior to the “Application”. The “Application” and
“Certification” must be placed in the person’s clinical record.
See s. 394.455(9), 394.459, 394.4625, Florida Statutes
CF-MH 3040, Feb 05 (obsoletes previous editions) (Recommended Form) BAKER ACT

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
365
E. Notification to Court of Withdrawal of Petition for Hearing on Involuntary
Inpatient or Involuntary Outpatient Placement
IN THE CIRCUIT COURT OF THE __________ JUDICIAL CIRCUIT
IN AND FOR ___________________________ COUNTY, FLORIDA
IN RE: ______________________________________ CASE NO.: __________________________
Notification to Court of Withdrawal of Petition
for Hearing on Involuntary Inpatient or Involuntary Outpatient Placement
YOU ARE HEREBY INFORMED THAT ____________________________________________________
Name of Person
at __________________________________________________________________________________
Facility Name and Address
has made application by express and informed consent for voluntary admission, due to an
improvement in his/her condition.
was discharged on ____________________ to ______________________________________
Date Destination (if known)
was transferred on ____________________ to ______________________________________
Date Destination (if known)
was converted to Marchman Act on ___________________________
Date
Other (specify): ________________________________________________________________
_____________________________________________________________________________
Please withdraw my Petition for:
Involuntary Outpatient Placement Involuntary Inpatient Placement Continued Involuntary
Outpatient Placement
The respondent has or has not been determined to be an imminent danger to self or others.
If yes, the record of the finding, certification, notice, and written acknowledgement is attached to this
Notification filed on Date: _________________. The Petition for Adjudication of Incompetence to Consent
to Treatment and Appointment of a Guardian Advocate, if any, is also being withdrawn.
_________________________________________________ _______________ _________
Signature of Administrator or Designee Date Time
__________________________________________
Printed Name of Administrator or Designee
cc: Clerk of the Court (Probate Division) Person Guardian
Assistant State Attorney Representative Person’s Attorney
When a petition for involuntary placement is withdrawn, the court, state attorney, public defender or other
attorney for the person, and guardian or representative must be notified by telephone within one business
day of the decision, unless such decision is made within 24 hours prior to the hearing. In such cases, the
notification must be made immediately.
Printed Name of Patient: ___________________________ Gender: _____________
Date of Birth: ____________________________________ Race: ________________
Social Security Number: __________________________
Confidential Information
Revised 03/14

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
366
F. Order of Court to Present Record of Finding to FDLE or Requiring Further
Documentation on Voluntary Transfer
IN THE CIRCUIT COURT OF THE ____________ JUDICIAL CIRCUIT
OF THE STATE OF FLORIDA, IN AND FOR ___________________COUNTY
IN RE: CASE NO: _____________________
_____________________________
(Patient)
DIVISION:______________________
(When provided)
Gender: _______ Race: _______ Date of Birth: __________ Social Security Number: ____________
ORDER OF COURT:
TO PRESENT RECORD OF FINDING TO FLORIDA DEPARTMENT OF LAW ENFORCEMENT or
REQUIRING FURTHER DOCUMENTATION ON VOLUNTARY TRANSFER
THIS MATTER came before the Court on _____________________, 20___, upon the filing of a
record by ____________________________________ (name of receiving facility) on _______________,
20___, relating _____________________________ (patient), who is now voluntarily in a mental health
treatment facility pursuant to the provisions of Chapter 394, Florida Statutes, and having been considered
by the undersigned judge or magistrate, pursuant to Section 790.065, Florida Statutes, and the
undersigned having reviewed the filing, finds as follows:
The following records were filed by the administrator of the receiving or treatment facility with the
Clerk of the Court for the county in which the involuntary examination occurred:
Record of findings and certification by examining physician of patient’s imminent
dangerousness;
Record of examining physician’s certification relating to filing of petition for involuntary
treatment
Record of written notice provided to patient
Record of patient’s written acknowledgement of notice
Record of application for voluntary admission
Record Notification to Court of Withdrawal of Petition (when applicable)
The examining physician found that the patient is an imminent danger to himself or herself or
others; and
The examining physician certified that if the patient did not agree to voluntary treatment, a petition
for involuntary outpatient or inpatient treatment would have been filed; or
The examining physician certified that a petition for involuntary outpatient or inpatient treatment
was filed and the patient subsequently agreed to voluntary treatment prior to a court hearing on
the petition, and
The patient received written notice of that finding and certification, and written notice that as a
result of such finding, he or she may be prohibited from purchasing a firearm, and may not be
eligible to apply for or retain a concealed weapon or firearms license, and the person
acknowledged such notice in writing.
(continued)

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
367
ORDER OF COURT:
TO PRESENT RECORD OF FINDING TO FLORIDA DEPARTMENT OF LAW ENFORCEMENT or
REQUIRING FURTHER DOCUMENTATION ON VOLUNTARY TRANSFER (Page 2)
The records described were / were not (circle one) filed within the 24-hour time prescribed by law
and computed as specified by Rule of Judicial Administration 2.514, after the patient’s agreement
to voluntary admission.
Within 24 hours after receipt, computed as specified by Rule of Judicial Administration 2.514, the
Clerk of the Court presented the record to the undersigned.
The record supports the classifying of the patient as an imminent danger to self or others and
therefore meets the criteria for forwarding to the Florida Department of Law Enforcement.
In consideration of the foregoing it is hereby
ORDERED AND ADJUDGED that the record be submitted to the Florida Department of Law
Enforcement within 24 hours for the purpose of entering the patient’s name into the National Instant
Check System database of people who are prohibited from purchasing firearms. The 24-hour period shall
be computed as provided in Rule of Judicial Administration 2.514(a)(2).
or
ORDERED AND ADJUDGED that the record presented to the Court is incomplete and the
Court cannot at this time find that the above-referenced patient’s voluntary commitment procedure met
the requirements of Section 790-065, Florida Statutes, so as to require that he/she be prohibited from
purchasing a firearm or that his/her name be added to the FDLE’s Mental Competency (MECOM)
database. It is therefore further
ORDERED that the ____________________________________ (name of receiving facility) file
with this Court adequate documentation of this voluntary commitment procedure within 3 days. The Court
reserves jurisdiction to enter further orders in this matter. It is further
ORDERED that a failure to timely file the documentation requested will result in:
(a) A dismissal of the matter with prejudice, without further order of this Court,
(b) The person’s record will not be submitted to the FDLE database, and
(c) The person will not be precluded from purchasing a firearm because of this specifically
referenced voluntary admission to a mental institution.
DONE AND ORDERED in Chambers in _________ County, Florida, on _____________, 20___.
Circuit Court Judge
General Magistrate
Copies to:
Receiving Facility*
Patient*
SAO
PDO/Patient’s Counsel
*The Receiving Facility is to print the patient’s copy and provide it to patient at the facility.
Confidential Information
Revised 03/14

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
368
G. Petition and Order for Relief from Firearm Disabilities Imposed by Court
IN THE CIRCUIT COURT OF THE _______ JUDICIAL CIRCUIT
IN AND FOR _________________ COUNTY, FLORIDA
IN RE: __________________________ CASE #: ______________
DIVISION: ____________
PETITION FOR RELIEF FROM FIREARM DISABILITIES IMPOSED BY THE COURT
1. THIS MATTER is presented to the Court on ____________ (date) by Petitioner, ________________,
on a Petition for Relief from Firearms Disabilities Imposed by the Court on _____________________.
2. The Petitioner was:
Ordered to Involuntarily Substance Abuse Assessment and Stabilization (s. 397.6818, F.S.) on
_____________________
Ordered to Involuntary Substance Abuse Treatment (s. 397.6957, F.S.) on __________________
Ordered to Involuntary Inpatient Placement (s. 394.467(6), F.S.) on _______________________
Ordered to Involuntary Outpatient Placement (394.4655, F.S.) on _________________________
Found by Court to be of Imminent Danger but permitted by physician to transfer to voluntary
status in lieu of involuntary placement order above (s. 790.065, F.S.) on ____________________
Adjudicated incapacitated (s. 744.331, F.S.) or any similar law of any other state on ___________
Acquitted by reason of insanity (s. 916.15 F.S.) of a person charged with a criminal offense on
_____________________
Criminal defendant found by Court to be not competent to stand trial (s. 916.12, F.S.) on _______
3. The Petitioner will not be likely to act in a manner that is dangerous to public safety and that granting
the relief would not be contrary to the public interest as follows:
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
4. Based upon these facts, THE FOLLOWING IS REQUESTED:
a. That the firearms disability imposed dated _____________, be set aside and are no further in
force and effect.
b. That pursuant to Florida Statute (790.065), The court shall grant the relief requested in the
petition if the court finds, based on the evidence presented with respect to the petitioner’s reputation, the
petitioner’s mental health record and, if applicable, criminal history record, the circumstances surrounding
the firearm disability, and any other evidence in the record, that the petitioner will not be likely to act in a
manner that is dangerous to public safety and that granting the relief would not be contrary to the public
interest.
(Continued)

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
369
PETITION FOR RELIEF FROM FIREARM DISABILITIES IMPOSED BY THE COURT (Page 2)
c. That pursuant to Florida Statute (790.065), the Florida Department of Law Enforcement shall
delete any mental health record of __________________________________ from the automated
database of persons who are prohibited from purchasing a firearm based on court records.
5. Under penalties of perjury, I declare that I have read the foregoing Petition for Relief from the Firearm
Disabilities Imposed by the Court and that the facts stated in it are true.
Signature of Petitioner __________________________________
Printed Name of Petitioner: __________________________________
Date of Birth: __________________________________
Mailing Address: __________________________________
__________________________________
City State ZIP Code
Race: ______________ Gender: __________________
Social Security Number: __________________________________
Name and Address of Attorney for Petitioner (if any):
_____________________________________________
_____________________________________________
Confidential Information
Revised 03/14
+++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++
For use of the Court only:
Office of the State Attorney notified of this petition on ___________ via ___________________.

Chapter Eight Firearm Prohibition for Certain Individuals With Mental Illnesses
_____________________________________________________________________________________
Baker Act Benchguide November 2016
370
IN THE CIRCUIT COURT OF THE _______ JUDICIAL CIRCUIT
IN AND FOR _________________ COUNTY, FLORIDA
IN RE: __________________________ CASE #: ______________
ORDER ON PETITION FOR RELIEF FROM FIREARM DISABILITIES
THIS MATTER is presented to the Court by Petitioner, ____________________________ on a Petition
for Relief from Firearms Disabilities Imposed as a result of the _________________________________
order issued by the Court on ___________(date).
The Court, having heard testimony and having received other evidence, finds as follows:
1. __________________ was ordered to ______________________________________________
2. __________________ successfully ________________________________________________
3. __________________ currently lives with ___________________________________________
Works at ___________________________, and ______________________________________
Office of the State Attorney was notified of this petition on ___________ via ___________________.
Based on the evidence presented and the Court’s conclusions derived therefrom, IT IS THEREFORE
ORDERED AND ADJUDGED that:
The firearm disability imposed on __________________________ shall remain in force and effect and
the petition filed on ________________________ (date) is DENIED.
The firearm disability imposed on __________________________ on _________________________
(date) is SET ASIDE and is of no further in force and effect.
Pursuant to Florida Statute 790.065, the Court grants the relief requested in the petition. With
respect to evidence presented as to petitioner’s reputation, mental health, the absence of criminal record
that would preclude gun ownership, the firearm disability, and other evidence in the record, the petitioner
will not be likely to act in a manner that is dangerous to public safety and that granting the relief would not
be contrary to the public interest.
Pursuant to Florida Statute 790.065, the Florida Department of Law Enforcement shall delete any
mental health record of _________________________ from the automated database of persons who are
prohibited from purchasing a firearm based on court records of ________________________ (MECOM).
DONE AND ORDERED in __________ County, Florida this ____ day of _____________, 20___.
________________________________
Circuit Court Judge
Full name of Petitioner ____________________ Date of Birth ______________________
Mailing Address: ____________________ Race: _____________ Gender _____________
____________________
City State Zip Code Social Security Number:___________________
Confidential Information -- Revised 03/14

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
371
APPENDIX I:
Recommendations from 1999 Report of the Supreme Court Commission on
Fairness, Subcommittee on Case Administration

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
372
Supreme Court Commission on Fairness
Subcommittee on Case Administration
Judicial Administration of the Baker Act
and Its Effect on Florida’s Elders
The following recommendations were included in the 1999 Report, and are taken from the
Executive Summary of the full report.
The Executive Office of the Governor and the Florida Supreme Court should jointly
sponsor a statewide interdisciplinary summit on mental health issues related to Chapter 394.
The objectives of the summit should include:
• educating participants on mental health issues;
• sharing information on “best practices” in regard to Baker Act cases; and
• providing a forum for the participants to discuss new and emerging mental health
issues.
Participants should include chief judges, probate judges, general masters, state attorneys,
public defenders, clerks of court, administrative law judges, law enforcement officers,
service providers, individuals with psychiatric disabilities, advocates, public and private
guardians, and others involved in Baker Act proceedings.
Courts
1. The State Courts System, state attorneys, public defenders, and clerks of court should
continue to seek, and the Florida Legislature should fund adequate resources for,
proceedings under Chapter 394
2. The Florida Legislature should direct and fund an interdisciplinary study on whether
probable cause hearings should be held within 24 to 48 hours for all individuals who are
involuntarily examined pursuant to Chapter 394.
3. The State Courts System should request, and the Legislature should approve, additional
funding to allow the establishment of general masters for involuntary placement
proceedings in every jurisdiction that needs and wants such a resource.
4. All participants should be mindful that patients must be treated with respect and
consideration.
5. Chief judges, state attorneys, and public defenders should ensure continuity and
consistency of the judges, general masters, assistant state attorneys, and assistant public
defenders assigned to Baker Act proceedings.
6. Judges, general masters, assistant state attorneys, and assistant public defenders should
be adequately trained and educated on general mental health and elder issues, including
community resources and issues identified in this report, prior to being assigned to Baker
Act proceedings.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
373
7. Judges, general masters, public defenders, and state attorneys should have a working
knowledge of community mental health resources and visit the less restrictive alternatives
available within their community.
8. Judges, general masters, state attorneys, and public defenders should be educated on
the financial relationships and incentives that may exist among mental health providers
and the situations in which conflict of interest or abuses may occur.
9. Continuing educational programs on elder, mental health, and disability laws and issues
should be made available to all Florida judges and lawyers on an on-going basis.
10. The court should treat petitions for writ of habeas corpus as emergency matters and
expeditiously resolve these issues and ensure that the petitioner receives notice of the
disposition.
11. The trial courts presently allowing county judges to preside over mental health
proceedings, including Chapter 394, should review their practices to ensure that those
practices comply with current Florida law.
12. Clerks of court and judges should implement a system whereby the clerk’s office checks
felony, misdemeanor, injunction, abuse, neglect, exploitation, and divorce records to
determine if there are any cases pending within the jurisdiction for the respondent or
petitioner. If there are any pending cases, the relevant files should be presented to the
judge together with the ex parte petition.
13. The bar should be educated as to their responsibilities in handling involuntary placement
proceedings.
14. When involuntary placement hearings are held in receiving facilities, steps should be
taken to increase the probability that patients understand that a formal court hearing is
taking place:
• the proceedings should not be conducted by video;
• courtroom formalities should be observed; and
• the presiding officer should wear a robe.
15. While the five-day issue is being clarified by the Legislature, the Chief Justice of the
Florida Supreme Court should contact every chief judge and probate judge and
encourage them to ensure that involuntary placement hearings are conducted within at
least five working days of the petition being filed, unless a continuance is requested by
the patient with consent of counsel, and granted. In order to comply with the statute, in
most jurisdictions hearings would have to be held at least twice a week.
16. The chief judge of every judicial circuit should immediately implement procedures to
ensure that involuntary placement hearings are conducted within five working days,
unless a continuance is granted. In order to comply with the statute, most circuits will
need to hold hearings at least twice a week.
17. The Probate Section of the Florida Conference of Circuit Judges should immediately
address the five-day issue (for conducting involuntary placement hearings) with its
members.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
374
18. The Probate Rules Committee and the Civil Procedure Rules Committee of The Florida
Bar should determine whether probate or civil rules apply to Chapter 394 proceedings.
Then the appropriate rules committee should consider whether to propose rules to clarify
the procedures in regard to involuntary placement hearings.
19. If a petition for the appointment of a guardian advocate is filed, the court should conduct
a hearing and make a finding as to the patient’s capacity to consent to treatment at the
earliest possible time.
20. At the time the court considers a motion for continuance, the court should conduct a
hearing and make a finding as to the capacity to consent to treatment if there is a pending
request. If the court finds that the capacity to consent to treatment is lacking, a guardian
advocate should be appointed at the time the involuntary placement hearing is continued.
21. The courts should comply with section 394.467(5), Florida Statutes, and ensure that
continuances are granted only when they are requested by the patient with consent of
counsel.
22. Judges and general masters should ensure that the evaluation of less restrictive
treatment alternatives (section 394.467(1)(b)) are given equal weight under the law with
the criteria found in section 394.467(1)(a).
23. The Florida Bar Probate Rules Committee and The Florida Bar Civil Procedure Rules
Committee should consider amending the rules of procedure to allow parties to waive the
waiting period for entry of a court order in Chapter 394 proceedings when no exceptions
will be filed, or alternatively allow for procedures similar to those used for hearing officers
in family law cases (Rule 12.491).
24. The Subcommittee strongly recommends against allowing guardians to voluntarily place
a ward in a mental health facility without judicial review.
25. Judges, general masters, state attorneys, and public defenders should receive training
on “dumping” and vigilantly guard against that or other abuses of the Baker Act in
situations involving elder residents of nursing homes or assisted living facilities. If
dumping or abuse is suspected, it should be immediately reported to the Agency for
Health Care Administration and the Long-Term Care Ombudsman.
26. The Florida Bar Commission on the Legal Needs of Children should study the legal needs
of children under the Baker Act.
27. Each judicial circuit, which has not already done so, should review and consider adapting
and adopting the model forms prepared by the Department of Children and Families.
Public Defenders
1. Each public defender should ensure that experienced and trained attorneys are assigned
to involuntary placement cases.
2. To ensure quality representation of patients, each public defender should place a high
priority on representing patients in involuntary placement proceedings and ensure that
each case to which that office is appointed is adequately prepared prior to hearing. The

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
375
Florida Legislature should provide adequate resources to enable public defenders to
provide quality representation for all patients in involuntary placement proceedings.
3. Every attorney representing a patient in involuntary placement proceedings must
vigorously represent the patient’s expressed desires. Every attorney representing
patients in involuntary placement proceedings must be bound to the same legal and
ethical obligations of any lawyer representing a client.
4. The Florida Public Defenders Association should develop a model curriculum or training
videotape on involuntary examination and placement procedures, and associated issues.
5. State attorneys and public defenders should be provided with training on jail diversion
programs for individuals with mental illnesses.
State Attorneys
1. Each state attorney should ensure that experienced and trained attorneys are assigned
to involuntary placement cases.
2. Each state attorney should place a high priority on involuntary placement proceedings
and properly prepare the cases on behalf of the state. The Florida Legislature should
provide adequate resources to enable state attorneys to provide quality representation
for the state in involuntary placement.
3. Each state attorney’s office should independently evaluate and confirm the allegations
set forth in the petition for involuntary placement. If the information is found to be correct,
the state attorney should vigorously prosecute the petition. If the allegations are not
substantiated, the state attorney should withdraw the petition.
4. Assistant state attorneys representing the state in involuntary placement proceedings
must be bound to the same legal and ethical obligations of assistant state attorneys
prosecuting other cases.
5. The state attorney’s office must be represented at and actively participate in every
hearing. The court should require the presence of the state attorney’s office at every
involuntary placement hearing. If a representative of the state attorney’s office is not
present at the hearing, the court should halt the proceeding while the state attorney is
summoned.
6. At involuntary placement hearings, judges and general masters should require the state
attorneys to comply with the statutory requirement to prove that all less restrictive
alternatives have been investigated and found to be inappropriate.
7. The Florida Association of Prosecuting Attorneys should develop a model curriculum
and/or training videotape on involuntary examination and placement procedures and
associated issues.
8. The Florida Association of Prosecuting Attorneys and The Florida Bar should ensure that
continuing legal education programs on elder, mental health, and disability laws and
issues are made available on an on-going basis.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
376
9. The bar should be educated as to attorneys’ roles and responsibilities in handling
involuntary placement proceedings.
10.State attorneys and public defenders should be provided with training on jail diversion
programs for individuals with mental illnesses.
Division of Administrative Hearings
The Division of Administrative Hearings should ensure that hearings on petitions for
continued involuntary placement are conducted prior to the expiration of the original
placement order.
Department of Children & Families
1. The Florida Legislature, the Department of Children and Families, and other policy
makers should adequately fund quality community supports and services for persons with
mental illnesses.
2. The Florida Legislature should fund positions within the Department of Children and
Families for the purpose of exploring less restrictive alternatives to involuntary placement
and require the Department to report to the court on same.
3. The Florida Legislature should direct the Department of Children and Families to create
a pamphlet that explains the purpose and statutory requirements of the ex parte process.
The Department should provide copies of the pamphlet to the clerks of court for
distribution to everyone seeking to file an ex parte petition. The Department should make
the pamphlet available in large print and other accessible formats as required by the
Americans with Disabilities Act, as well as in English, Spanish, Creole, and other common
languages reflective of Florida’s population.
4. The Florida Statutes should be revised to mandate that the rights pamphlet prepared by
the Department of Children and Families be distributed to every mental health patient–
both voluntary and involuntary–upon admission. The pamphlet should be available in
large print and other accessible formats as required by the Americans with Disabilities
Act, as well as English, Spanish, Creole, and other common languages reflective of
Florida’s population.
5. The Department of Children and Families, Department of Elder Affairs, appropriate
sections of The Florida Bar, and mental health activists should collaborate on the
production of a videotape that explains the rights of individuals with psychiatric
disabilities.
6. The Department of Children and Families, The Department of Elder Affairs, appropriate
sections of The Florida Bar, the medical community, and mental health activists should
publicize the availability of mental health advance directives, to allow individuals to
maximize self-determination.
7. The Department of Children and Families, The Department of Elder Affairs, local bar
associations, and mental health activists should conduct community workshops to
educate qualified individuals about mental health issues and the opportunity to volunteer
as a guardian advocate.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
377
8. The Florida Department of Law Enforcement and the Department of Children and
Families should jointly initiate a comprehensive training program for law enforcement
officers, incorporating a minimum:
• A videotaped orientation to the Baker Act for statewide use, which emphasizes the
criteria for initiating an involuntary examination; and
• Crisis intervention training for appropriate interaction with persons with mental
illnesses.
Human Rights Advocacy Committees (Later known as Florida Local Advocacy Councils
and defunded by the Florida Legislature in 2010 despite being cited in numerous places in
the Baker Act)
1. The Florida Legislature should consider authorizing and funding the Statewide Human
Rights Advocacy Committee and the local Human Rights Advocacy Committees to meet
with patients and make them aware of their rights.
2. The Florida Legislature should consider authorizing and adequately funding the
Statewide Human Rights Advocacy Committee and local Human Rights Advocacy
Committees to assess the ability of all voluntary patients to give express and informed
consent to treatment.
3. The Florida Legislature should extend standing to file petitions for writ of habeas corpus
to the Statewide Human Rights Advocacy Committee and the local Human Rights
Advocacy Committees, to further protect the rights of persons who are voluntarily and
involuntarily hospitalized.
Agency for Health Care Administration
1. The Florida Legislature should adequately fund the Agency for Health Care
Administration and require the Agency to actively monitor and vigorously enforce
regulations related to community facilities, such as assisted living and other facilities, to
improve the quality of care and services for residents.
2. The Florida Legislature should provide the Agency for Health Care Administration with
adequate funds and staff, and direct the Agency to vigorously enforce regulations in
regard to violations by mental health facilities and professionals.
3. The Florida Legislature should require facilities to provide all petitions and orders for
involuntary placement to the Agency for Health Care Administration within one working
day.
4. The Florida Legislature should review the statutes and regulations to ensure that
community facilities are adequately regulated. The Florida Legislature should also require
community facilities that house people who require mental health treatment to facilitate
those persons’ access to such treatment by qualified professionals.
5. The Florida Legislature should direct the Department of Children and Families, the
Agency for Health Care Administration, the Long-Term Care Ombudsman, or other
appropriate entity to study whether nursing homes and other facilities are "dumping"

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
378
residents because of a lack of funding to treat conditions not covered by governmental
programs and private insurance, as well as for fraudulent financial gain.
6. Forms related to involuntary examination and placement, including disposition, should be
collected, monitored, and analyzed by the Agency for Health Care Administration on an
on-going basis in order to detect and address abuses in a timely fashion. All forms should
include the patient’s date of birth, race, gender, and other demographic information, so
that the impact of Chapter 394 on elders, children, racial minorities, and other population
groups can be collected and analyzed. The results of this statewide data collection and
analysis should be reported to the Florida Legislature, Department of Children and
Families, and the State Courts System on an annual basis. Adequate funding should be
provided by the Legislature to permit such data collection, research, and analysis.
Miscellaneous Appropriations:
1. The Florida Legislature should make funding available to jurisdictions that are willing to
coordinate an interdisciplinary exploration of innovative alternatives designed to reduce
the traumatic effect of involuntary examinations. Such pilot projects should be monitored
and evaluated by independent entities, to determine their effectiveness.
2. The Florida Legislature should review and correct any funding inequities that are created
when residents of one county are involuntarily placed in another county (relates to costs
of hearings, independent expert examinations, etc.).
3. The Florida Legislature should fund a guardian advocate system that provides each
geographical area with a readily available pool of guardian advocates who have training
in mental health issues and psychotropic pharmacology, to serve on behalf of individuals
with psychiatric disabilities for whom no family or friends are willing or able to serve.
Recommended Changes to 394
1. The Florida Legislature should review rights and protections afforded to individuals with
mental illnesses under Chapter 394 and ensure that they are no less than the rights and
protections afforded to nursing home residents under Chapter 400.
2. The Florida Legislature should consider revising the statutes to specify that violation of a
mental health patient’s rights constitutes "abuse" within the meaning of the law.
3. The Florida Legislature should consider whether the definition of mental illness should be
amended to exclude dementia, Alzheimer’s disease, and traumatic brain injury.
4. The Florida Legislature should consider expanding the list of professionals in
394.4625(1)(c) (independent assessment of residents in facilities licensed under chapter
400 seeking voluntary admission to a receiving facility) to prohibit the involvement of any
professional who has a financial interest in the outcome of the assessment.
5. The Florida Legislature should consider the feasibility and appropriateness of extending
the protections of section 394.4625(1)(c), Florida Statutes (independent assessment of
residents in facilities licensed under chapter 400), to involuntary as well as voluntary
examination situations.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
379
6. The Florida Legislature should amend the statutes to expressly permit the use of less-
restrictive alternatives to involuntary in-patient examinations.
7. The Florida Legislature should consider amending Chapter 394 to allow county courts to
issue ex parte orders for involuntary examination, but maintain exclusive circuit court
jurisdiction over involuntary placements.
8. The Florida Legislature should consider improvements to the ex parte provisions of
section 394.463, Florida Statutes, including but not limited to:
• requiring and funding a pre-screening process;
• requiring a hearing prior to the issuance of an ex parte order; and
• clarifying the time frame within which the behavior in question must be observed.
9. The Florida Legislature should consider amending Chapter 394 in regard to petitions for
ex parte orders, to require a factual recitation of the circumstances that support the finding
that the criteria for involuntary examination have been met.
10. The Florida Legislature should amend the statutes to clarify that the 72-hour involuntary
examination period is not extended over weekends or holidays, unless a petition for
involuntary placement will be filed on the next working day.
11. The Florida Legislature should amend the statutes to clarify whether the five-day
requirement includes or excludes weekends and holidays. If the Legislature determines
that involuntary placement hearings must be held within five consecutive days, adequate
additional funding must be provided to the courts, clerks, state attorneys, and public
defenders to enable them to conduct meaningful, as well as timely, proceedings.
12. The Florida Legislature should consider amending section 394.467(5), Florida Statutes
(continuance of involuntary placement hearings), as indicated hereinafter in this report.
13. The Florida Legislature should direct and fund an interdisciplinary study on whether state
attorneys should be authorized to have access to clinical records, facility staff, and other
pertinent information.
14. The Florida Legislature should direct and fund an interdisciplinary study on the continued
involuntary placement process.
15. The Florida Legislature should consider amending the statutes to provide an explicit right
for independent examinations in continued involuntary placement proceedings.
16. The Florida Legislature should amend the statutes to clarify the duties, responsibilities,
and authority of patient representatives.
17. The Florida Legislature should direct the Statewide Public Guardian to recommend a
process and responsible entity to initiate a guardianship evaluation for persons who are
mentally incapacitated and need intervention but who do not meet the statutory criteria of
the Baker Act.

Recommendation from 1999 Report of the Supreme Court Commission on Fairness
Appendix I Subcommittee on Case Administration
_____________________________________________________________________________________
Baker Act Benchguide November 2016
380
18. The Florida Legislature should consider providing limited liability protection for family
members, friends, and individuals who serve as guardian advocates on a volunteer basis.
Community workshops should be conducted to educate qualified individuals about mental
health issues and the opportunity to volunteer as a guardian advocate.
19. The Florida Legislature should consider amending Chapter 394 to permit Chapter 744
guardians and Chapter 393 guardian advocates to participate in alternative placement
decisions and receive adequate notice of the decision-making process.
20. The Florida Legislature should direct and fund a comprehensive interdisciplinary study
on the legal needs of children under the Baker Act, including but not limited to:
• whether children under the age of 18 should have the right to voluntarily consent to in-
patient mental health treatment, without the consent of their guardian.
• whether the Human Rights Advocacy Committees or another independent entity should
have the authority to make contact with a child confined to a mental health facility, to
confirm the voluntariness of the child’s consent.
• whether a child’s right to petition for a writ of habeas corpus pursuant to Chapter 394
is adequately protected and whether legal counsel should be provided.
• whether judicial review of placement of children in mental health facilities should be
required, to ensure the appropriateness of involuntary placements and the
voluntariness of voluntary admissions.
General
Family members and persons who are designated as mental health surrogates should
participate in guardian advocate training prior to the time their service is needed, to avoid
unnecessary delay in the provision of treatment.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
381
APPENDIX II:
Compendium of Appellate Cases, Attorney General Opinions, and Other
Legal References
Outline of Topics
I. Evidence Supporting Criteria for Involuntary Inpatient Placement
A. In General
B. Outpatient Commitment
C. Waiver of Patient’s Presence at Placement Hearing
D. Notice to and Participation of State Attorney at
Involuntary Placement Hearings
E. Duty of State Attorney and Role of Counsel for Receiving Facility in
Involuntary Placement Hearings
F. Deadline for Filing Petitions and Notices
G. Appeal Not Moot
H. Jurisdiction of Courts
I. Testimony
II. Clinical Records and Confidentiality
III. Public Records Law
IV. Payment of Involuntary Placement Bills
V. Transportation of Baker Act Patients
VI. Law Enforcement
A. Warrantless Entry — Exigent Circumstances
B. Detention and Custody
C. Use of Force
D. Weapons
VII. Responsibilities of and Lawsuits Against Doctors and Receiving Facilities
A. Duty to Warn
B. Malpractice vs. Ordinary Negligence
VIII. Guardianship and Adult Protective Services
IX. Baker Act and Minors
X. Baker Act and Criminal Defendants
XI. Marchman Act

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
382
I. Evidence Supporting Criteria for Involuntary Inpatient Placement
A. In General
Zinermon v. Burch, 494 U.S. 113, 110 S.Ct. 97, 108 L.Ed.2d 1005 (1990). Burch,
while allegedly medicated and disoriented, signed forms for voluntary admission to
a state mental hospital. After his release he sued physicians, administrators, and
staff of the hospital, among others, for depriving him of his liberty without due
process of law, alleging that “they violated state law by admitting him as a
voluntary patient when they knew or should have known that he was incompetent
to give informed consent to his admission, and that their failure to initiate Florida’s
involuntary placement procedure denied him constitutionally guaranteed
procedural safeguards.” The U.S. District Court for the Northern District of Florida
granted the defendants’ motion to dismiss because “a deprivation of a
constitutionally protected property interest caused by a state employee’s random,
unauthorized conduct does not give rise to a § 1983 procedural due process claim
unless the State fails to provide a postdeprivation remedy,” and Burch appealed.
The U.S. Circuit Court of Appeals affirmed, but after rehearing en banc reversed
and remanded. The Supreme Court affirmed the reversal of the motion to dismiss,
stating: “The characteristics of mental illness . . . create special problems regarding
informed consent. Even if the State usually might be justified in taking at face
value a person’s request for admission to a hospital for medical treatment, it may
not be justified in doing so, without further inquiry, as to a mentally ill person’s
request for admission and treatment at a mental hospital.” Further, the defendants
could not
escape § 1983 liability by characterizing their conduct as a “random,
unauthorized” violation of Florida law which the State was not in a
position to predict or avert, so that all the process Burch could
possibly be due is a postdeprivation damages remedy. Burch,
according to the allegations of his complaint, was deprived of a
substantial liberty interest without either valid consent or an
involuntary placement hearing, by the very state officials charged with
the power to deprive mental patients of their liberty and the duty to
implement procedural safeguards. Such a deprivation is foreseeable,
due to the nature of mental illness, and will occur, if at all, at a
predictable point in the admission process.
O’Connor v. Donaldson, 422 U.S. 563, 95 S.Ct. 2486, 45 L.Ed.2d 396 (1975).
The Court held that a state “cannot constitutionally confine, without more, a
nondangerous individual who is capable of surviving safely in freedom by himself

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
383
or with the help of willing and responsible family members and friends,” and there
is “no constitutional basis for confining [mentally ill] persons involuntarily if they
are dangerous to no one and can live safely in freedom.”
Standard Jury Instructions-Criminal Cases (99-2), 777 So. 2d 366 (Fla. 2000).
“Clear and convincing evidence” is defined as “evidence that is precise, explicit,
lacking in confusion, and of such weight that it produces in your mind a firm belief
or conviction, without hesitation, about the matter in issue.”
In re Beverly, 342 So. 2d 481 (Fla. 1977). The Florida Supreme Court stated that
the Baker Act, authorizing involuntary commitment of mentally ill persons, “has
withstood the attack of vagueness and overbreadth. We hold the statute to be
constitutional on its face.” But it reversed the order for involuntary hospitalization,
noting, among other things, that the state and the examining physician had sought
an order for involuntary hospitalization of the appellant for up to six months even
though the examining physician stated that the appellant “would be ready to leave
the hospital in one month.” Further, one psychiatrist did not conclude that the
appellant “was likely to injure himself or others and that he was in need of care but
unable to make a responsible application on his own behalf.” And “the evidence is
not clear and convincing that appellant would likely injure himself or others if
allowed to remain at liberty. Appellant is mentally ill and in need of care or
treatment, but it does not appear by clear and convincing evidence that he is
dangerous or that he lacks sufficient capacity to make a responsible application on
his own behalf.”
Lischka v. State, 901 So. 2d 1025 (Fla. 1st DCA 2005). The state filed a
confession of error, and the appellate court reversed the order of involuntary
commitment, stating:
Although we are concerned about the significant problems that can
occur when mental health patients refuse to take their prescribed
medication, the statute and case law require reversal. . . . It is well-
settled that the need for treatment and medication and the refusal to
take medication despite a deteriorating mental condition, standing
alone, do not justify involuntary commitment under the Baker Act. . . .
Rather, there must also be clear and convincing evidence that without
treatment, the patient would pose a real and present threat of
substantial harm to himself, or a substantial likelihood that in the near
future he will inflict serious bodily harm on himself or another, as
evidenced by recent behavior.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
384
A.E. v. State, 83 So. 3d 1000 (Fla. 3d DCA 2012). The appellate court affirmed an
involuntary civil commitment order, finding competent substantial evidence to
support it. The appellant, who was arrested and charged with aggravated battery,
had been found incompetent due to schizophrenia and paranoia “and has remained
incompetent with no substantial probability that she will become competent to
stand trial in the foreseeable future. [She] has a long history of mental illness,
perceptual disturbances, substance abuse, numerous hospitalizations, and non-
compliance with treatment and medication.” Further, the trial court noted that the
appellant “has poor insight as to her condition and mental health needs, she had to
be placed on suicidal precautions approximately two weeks prior to the hearing,
and numerous attempts to place her in the community have failed.”
Rosicka v. State, 898 So. 2d 1098 (Fla. 1st DCA 2005). The trial court entered an
order for involuntary placement, finding that the appellant had a history of multiple
suicidal gestures. But the appellate court reversed, stating that “review of court
record does not reveal any evidence to support that determination [or] any
competent substantial evidence that the appellant posed a threat to herself through
neglect.”
Craig v. State, 804 So. 2d 532 (Fla. 3d DCA 2002). The appellant was arrested for
stalking a news reporter and was ordered to involuntary placement for treatment.
The appellate court affirmed the order, stating: “A threat can be express or implied.
. . . In determining whether there has been a threat, the court must look at the
totality of the circumstances, including not only the words and deeds of the patient,
but diagnoses and expert opinions of the mental health professionals.” The
appellate court also stated: “Under the statutory standard, there must be a showing
of a ‘substantial likelihood that in the near future he or she [the patient] will inflict
serious bodily harm on himself or herself or another person, as evidenced by recent
behavior causing, attempting, or threatening such harm,’” and that “serious bodily
harm would include any harm that would necessitate medical treatment. Because
of potential for death or serious injury in kidnapping cases, a threat of kidnapping
or false imprisonment would satisfy the statute.”
Boller v. State, 775 So. 2d 408 (Fla. 1st DCA 2000). The appellate court held that
testimony that the patient refused to take her psychotropic medication, had slapped
a hospital staff member, and believed others were trying to kill her, and the expert
psychiatrist’s conclusory testimony “that it was ‘more likely than not’ that [the
patient] might inflict serious bodily harm on herself or another person,” was not
“clear and convincing evidence that she pose[d] a present threat of substantial
harm” to justify involuntary commitment. “[T]estimony that a person may have
threatened someone in the past does not amount to clear and convincing evidence

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
385
that she is a current danger to others.”
Singletary v. State, 765 So. 2d 180 (Fla. 1st DCA 2000). The appellate court held
that the state failed to prove by clear and convincing evidence that a Baker Act
patient met the criteria for involuntary placement. Testimony that the patient “may
have threatened others at some point in the past” did not amount to clear and
convincing evidence that she was a danger to others. In addition, testimony that she
“would likely have to be rehospitalized, if she did not take her medication” was
insufficient to prove “a real and present threat of substantial harm to . . . her well-
being.” Further, “the state did not present clear and convincing evidence that less
restrictive treatment alternatives were unavailable,” since the patient’s mother
testified that she wanted to have her daughter live with her in a better environment
and that “she would ensure that her daughter continued to take her medication, and
promised to initiate involuntary commitment proceedings if she did not.”
Blue v. State, 764 So. 2d 697 (Fla. 1st DCA 2000). The appellate court held that
evidence that a Baker Act patient was unstable and threatening to others, that her
emotional outbursts scared her family, and that she was “generally very
argumentative and hostile” did not constitute clear and convincing evidence “that
there is a substantial likelihood that in the near future she will inflict serious bodily
harm on herself or another person.” The court reversed the order of involuntary
placement and treatment and remanded.
Berry v. State, 751 So. 2d 764 (Fla. 1st DCA 2000).The court reversed the trial
court’s order of involuntary placement for treatment, stating that “the record does
not clearly and convincingly establish the nature, extent, and likelihood of any
future harm. . . . While the appellant might derive some benefit from further
treatment in a structured living arrangement, this does not justify a Baker Act
commitment.”
Lyon v. State, 724 So. 2d 1241 (Fla. 1st DCA 1999). The appellate court reversed
the trial court order of involuntary commitment that was based on a doctor’s
opinion that if the schizophrenic woman did not take her medication, “she w[ould]
be almost incoherent in her speech, not able to take care of herself, she’ll require
supervision, she’ll require structure.” The appellate court held that the trial court’s
finding was not based on clear and convincing evidence; there was no specific
showing that any self-neglect posed a real and present threat of substantial harm to
the appellant’s well-being.
Adams v. State, 713 So. 2d 1063 (Fla. 1st DCA 1998). The court reversed the trial
court’s order of involuntary placement for treatment, holding that a Baker Act

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
386
commitment was not justified by clear and convincing evidence where the order
referred to
a purported witness who did not testify, and describes the factual basis
of the ruling by merely quoting from the petition for involuntary
placement. Furthermore, while the court also made oral findings at the
conclusion of the hearing, a need for treatment and medication does
not in itself justify a Baker Act commitment. . . . Rather, there must be
clear and convincing evidence that without treatment the appellant
would pose a real and present threat of substantial harm to his own
well-being, or a substantial likelihood that in the near future he would
inflict serious bodily harm on himself or another, as evidenced by
recent behavior.
Archer v. State, 681 So. 2d 296 (Fla. 1st DCA 1996). The appellate court reversed
an order for involuntary placement, finding that there was no clear and convincing
evidence that the patient “was ‘incapable of surviving alone,’ or that she was
‘likely to suffer from neglect or refuse to care for” [her]self if released. The
testifying psychologist acknowledged that the patient had not threatened to hurt
herself or anyone else. Further, the patient also testified that if she were released
she would take her medication.
Wade v. Northeast Florida State Hosp., 655 So. 2d 125 (Fla. 1st DCA 1995). The
court reversed an order for continued involuntary placement, holding that “these
conclusory recitations” regarding “the appellant’s potential for aggression, and the
possibility of substantial harm to his well-being . . . are not fully substantiated by
the facts in evidence.”
Bradley v. Akins, 650 So. 2d 1069 (Fla. 2d DCA 1995). The administrator of a
hospital challenged a final administrative order denying his request for continued
involuntary placement of the appellee. The appellate court reversed, holding that
the administrator “showed by clear and convincing evidence that [the appellee]
continued to meet the criteria for continued involuntary placement.” The appellee
had killed his girlfriend in1986, “based on the delusion that she had taken his
money. He was judged incompetent to proceed to trial and was committed to
psychiatric care at Florida State Hospital, where he spent six years.” He was
transferred to another hospital pursuant to an order finding that he “remained
incompetent to proceed to trial and was unlikely to regain competency in the
foreseeable future.” At the continued involuntary placement hearing, the
administrator’s sole witness was a doctor who testified that the appellant “would
not be capable of surviving off the grounds of the hospital either alone or with the

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
387
help of willing family or friends, that without treatment he would suffer from
neglect and refuse to care for himself, and that he was a danger to himself and
others” based on recent threats he had made.
Hedrick v. Florida Hospital Medical Center, 633 So. 2d 1153 (Fla. 5th DCA
1994). The court held that a Baker Act patient’s “potential for the exercise of ‘poor
judgment’” was insufficient to satisfy the statutory test for involuntary
examination. The psychiatrist’s testimony lacked a factual basis to show a present
threat of substantial harm to the patient’s well-being.
Salter v. State, 618 So. 2d 352 (Fla. 1st DCA 1992). A person was involuntarily
committed to a state hospital pursuant court order. A psychiatrist testified that the
person “refused to cooperate with any treatment recommended,” but he did not
state what treatment or medication was recommended or necessary. He testified
that the person “was in danger of self-neglect or some violent act and needed to be
involuntarily placed for further care and supervision . . . , but he did not state the
nature of the self-neglect.” The court held that the psychiatrist’s testimony was
insufficient to support involuntary commitment.
Welk v. State, 542 So. 2d 1343 (Fla. 1st DCA 1989). The appellate court reversed
the trial court order for involuntary placement at a state hospital, finding “the
evidence legally insufficient to support the necessary finding that appellant poses a
real and present threat of substantial harm to herself or others.” The court stated:
As stated by both expert witnesses, the ideal situation would be a
facility in the local community to provide minumum [sic] supervision
less than that required in a mental hospital. But a declaration of
incompetency and involuntary incarceration in a mental institution is
not the appropriate solution to this problem. The strict test for
involuntary commitment imposed by the statute is intended to prevent
the incarceration in mental institutions of people who are in need only
of alternative means for minimum care and maintenance.
Everett v. State, 524 So. 2d 1091 (Fla. 1st DCA 1988). The appellate court
reversed an order of involuntary placement “because the state failed to present
evidence that, because of her mental illness, appellant refused voluntary placement
for treatment, or was unable to determine whether placement was necessary.” The
only evidence “was that appellant was hospitalized ‘on multiple occasions’ as a
result of her failure to take medication prescribed for her condition.” The record
didn’t indicate “whether the hospitalizations were voluntary or involuntary,
initiated by appellant or someone else.” Further, the appeal took so long that the

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
388
appellant had already been ordered to “continued” involuntary placement upon
expiration of the original court order. The appellate court held that the original
placement order was not superseded by the order of continued involuntary
placement and stated: “If a circuit judge’s order of initial involuntary placement is
erroneous, subsequent administrative orders of continued involuntary placement,
predicated as they are on the initial order, do not render challenges to that order
moot.” The appellate court urged those who challenge involuntary placement
orders “to seek expedited appellate review, or to promptly challenge the order in a
habeas corpus petition to the circuit court.”
Schexnayder v. State, 495 So. 2d 850 (Fla. 1st DCA 1986). The trial court entered
an order for involuntary commitment of the appellant, who “forgets to take her
medication, without which she becomes disoriented, nervous, and agitated, and
ultimately in need of hospitalization.” The appellate court reversed the order,
noting: “Appellant has a place to live, financial resources . . . , insight into her
mental illness, knowledge of the necessity for medication, and a history of self-
admissions to hospitals. . . . The mere conclusion that a person is in need of care or
treatment . . . is insufficient.”
Asman v. State, 268 So. 2d 464 (Fla. 4th DCA 1985). The appellate court
affirmed the trial court’s order for involuntary placement, which stated that the
appellant met the criteria and referred to two expert opinions. The court stated:
“While it is unfortunate that the individual’s present loss of control over his life is
based on a split decision, the majority of the panel are of the opinion, after review
of the record, which admittedly in large part is the transcript of an inferior tape,
that the statutory criteria have all been met. . . . [I]t is not our province to substitute
our judgment for the trier who observed the witnesses as well as appellant.”
Neff v. State, 356 So. 2d 901 (Fla. 1st DCA 1978). Even though the appellant was
mentally ill and there was testimony that he was unable to recognize his illness, the
order of involuntary commitment was reversed because there was no evidence that
he “was incapable of caring for himself in freedom.”
B. Outpatient Commitment
C.N. v. State, 433 So. 2d 661 (Fla. 3d DCA 1983). The circuit court had ordered
that C.N. “obtain outpatient psychiatric treatment as the ‘least restrictive means of
intervention’” and retained jurisdiction in case she failed to do so. When C.N. did
not continue outpatient treatment, the court entered a contempt judgment against
her. The appellate court reversed, noting that for contempt there must be a willful
disregard or disobedience of a court order, and in this case all three physicians who

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
389
were witnesses at the contempt hearing testified that C.N. had “a ‘basic personality
problem’ related to the psychiatric disorder which gives her ‘difficulty in following
directions.’ The evidence presented did not support a finding of contemptuous
intent, an element of criminal contempt.” Further, the appellate court stated:
There is no statutory authority for the court to retain jurisdiction for
the purpose of modifying an action taken on an earlier petition. The
imposition of a more restrictive intervention, i.e., involuntary
placement, requires, at the minimum, a new petition for involuntary
hospitalization, a notice of hearing and a hearing on the petition. For a
court to order involuntary hospitalization, it is not sufficient that the
patient merely failed to follow a plan for outpatient treatment. There
must be clear and convincing proof that an individual is dangerous to
herself or others before the state may deprive her of her freedom on
the basis of mental illness alone.
G.T. v. Stone, 622 A.2d 491 (Vt. 1993). G.T. was released from a Vermont state
hospital on conditional discharge. The discharge was revoked, and G.T. brought a
declaratory judgment action challenging the constitutionality of Vermont’s statute
governing conditional discharges. The Supreme Court of Vermont reversed and
remanded, holding that “a postrevocation hearing under [18 V.S.A. ]§ 8008(e) is
insufficient to meet Vermont’s due process standards, and that a prerevocation
hearing is required except in an emergency, whether or not requested by the
patient.”
The following appellate cases around the country regarding involuntary outpatient
commitment laws may be of interest:
Standards used
Matter of Maricopa County Cause No. MH-90-00566, 840 P.2d 1042
(Ariz. Ct. App. 1992). L.R. was committed to a state hospital for inpatient
treatment followed by supervised outpatient treatment. The appellate court
rejected his argument that the statute defining “persistently or acutely
disabled” in relation to the provision defining “mentally disorder” was
unconstitutionally vague and overbroad. It also held the evidence was
sufficient “to support the [trial] court’s conclusion that he was persistently or
acutely disabled.”
Hermann v. Arkansas, 1998 WL 118116 (Ark. Ct. App. 1998). The
appellate court reversed a commitment order (for a combination of inpatient

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
390
and outpatient) on “danger to self or others” grounds. The state failed to
prove Hermann was dangerous, although he had refused his medication and
was acting erratically.
In re Johnson, 691 A.2d 628 (D.C. Ct. App. 1997). A voluntary outpatient
can be committed involuntarily for outpatient treatment if he or she meets
the statutory requirements.
In re J.P., 574 N.W.2d 340 (Iowa 1998). The evidence was insufficient to
support that a depressed woman who stopped taking her medication and took
her children to a battered women’s shelter was “seriously mentally
impaired” and in need of treatment. The order requiring involuntary
outpatient commitment was reversed.
In re LaBelle, 728 P.2d 138 (Wash. 1986). The appellate court upheld a
commitment for a mix of inpatient and outpatient treatment. The statutory
standard of “grave disability” was not unconstitutionally vague or
overbroad.
In Matter of William S., 570 N.W.2d 253 (Wis. Ct. App. 1997).
(unpublished disposition). The appellate court affirmed an outpatient
commitment order because the trial court’s finding of dangerousness wasn’t
“clearly erroneous.” Two doctors, who disagreed about the degree of
possible danger but agreed with the treatment order, had testified.
Revocation of Outpatient Status
Matter of Plummer, 608 A.2d 741 (D.C. Ct. App. 1992). A patient whose
outpatient status was revoked but who was later released on indefinite
convalescent leave status has “the same due process rights as a patient who
is originally committed as an outpatient.”
Matter of Stokes, 546 A.2d 356 (D.C. Ct. App. 1988). Absent a finding of
dangerousness, the revocation of outpatient status for noncompliance
(medication) violates D.C.’s commitment law.
In re James, 507 A.2d 155 (D.C. Ct. App. 1986). Before revoking
outpatient status, “the trial court must make an explicit finding that inpatient
treatment is the least restrictive alternative.”
In re Richardson, 481 A.2d 473 (D.C. Ct. App. 1984). “[A] trial court may
authorize an outpatient’s summary rehospitalization in certain

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
391
circumstances, provided the patient is detained only temporarily and the
Hospital complies with the affidavit and notice requirements.” The
procedures used for summary rehospitalization don’t violate due process.
Matter of Mills, 467 A.2d 971 (D.C. Ct. App. 1983). The court was not
required to apply a “clear and convincing” standard of evidence in a
proceeding redetermining that a committed outpatient was mentally ill and
dangerous, resulting in his indefinite hospitalization.
Application of True, 645 P.2d 891 (Idaho 1982). The minimum
requirements for revocation of outpatient status are “prompt written notice”
and “a revocation hearing before a neutral hearing body to be held as soon as
is reasonably possible following the patient’s rehospitalization.”
In re K.B., 562 N.W.2d 208 (Mich. Ct. App. 1997). K.B. spent 30 days in a
hospital and then was outpatient committed. Her outpatient status was
revoked, without notice or a hearing, for medication noncompliance. The
court held that no due process violation occurred: “The various measures to
ensure that the individual’s rights are protected in the initial treatment
determination, combined with the continued right of the individual to appeal
during treatment, afford satisfactory protection. . . . In addition, the brief
duration of the treatment period minimizes the risk of any erroneous
deprivation of liberty resulting from changed circumstances.”
Matter of Commitment of B.H., 514 A.2d 85 (N.J. Super. Ct. Law Div.
1986). “This summary revocation of B.H.’s conditional discharge by
recommitment, although done under emergent conditions, constitutes a
violation of her due process rights since it was not done by court review.”
State v. Bryant, 871 P.2d 129 (Or. Ct. App. 1993). Due process does not
require “the state to prove that the person remains mentally ill at the time of
the [outpatient commitment status] revocation proceeding.”
In re Cross, 662 P.2d 828 (Wash. 1983). The trial court “had no authority,
absent a finding that [the gravely disabled person] had not adhered to the
conditions attached to her less restrictive treatment or initiation of a second
original commitment proceeding, to order [her] returned to inpatient status.”
Even if it had such authority, the patient was not given adequate notice of
the grounds on which her return to inpatient status was sought.
In re P.S., 702 A.2d 98 (Vt. 1997). An order of nonhospitalization may be
revoked without “a showing of dangerousness.” It is sufficient if the state

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
392
proves the patient is “in need of further treatment” (the statute allows use of
a “patient in need of further treatment” standard, under which the effect of
discontinuing treatment is relevant).
G.T. v. Stone, 622 A.2d 491 (Vt. 1992). “[D]ue process requires a judicial
hearing prior to recommitment, whether or not requested by the patient,
unless immediate recommitment is required because the person poses an
imminent danger of harm to himself or another.”
In re G.K., 514 A.2d 1031 (Vt. 1986). Orders for involuntary treatment of
indeterminate duration violate due process, “absent provision for state-
initiated periodic review.”
Other
Randolph v. Cervantes, 950 F.Supp. 771 (S.D. Miss. 1996). While residing
at a state-associated mental health care facility, the plaintiff injected her eyes
with a roommate’s insulin and lost her vision. She brought a civil rights
lawsuit against the facility and an employee, which the trial court dismissed.
The appellate court affirmed, holding that the court order for outpatient
treatment was “insufficient to give rise to a special relationship . . . which
would have imposed an affirmative duty on the part of the State to provide
for her safety.” The state does not have a duty “to protect an individual
against private violence.”
Matter of Utley, 565 N.E.2d 1152 (Ind. Ct. App. 1991). Although rendered
moot, it was error for the trial court to find the person in contempt for failure
to comply with an outpatient commitment order without determining
“whether his conduct was willful or a manifestation of his mental illness.”
In Interest of T.J., 482 N.W.2d 850 (S.D. 1992). An indefinite treatment
order is subject to periodic review even if it is for outpatient treatment.
C. Waiver of Patient’s Presence at Placement Hearing
Mouliom v. Northeast Florida State Hosp., 128 So. 3d 979 (Fla. 1st DCA 2014).
A hearing for continued involuntary inpatient placement was held by an ALJ, and
the assistant public defender representing the appellant waived her presence. The
ALJ entered an order continuing placement for another six months, which the
appellant contended was fundamental error. The appellate court agreed and
reversed the order, stating: “Even though [her] attorney affirmatively waived her
presence at the hearing, we are not precluded from considering the issue raised in

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
393
this appeal because ‘a denial of the due process right to be present at an
involuntary commitment hearing is fundamental error which may be raised on
appeal even if not preserved below.’” The right is not limited to initial commitment
hearings. “The patient also has a fundamental right to be present at the periodic
hearings held by an ALJ . . . to consider whether to continue the patient’s
commitment. The patient can waive the right to be present at the hearing, but for
such a waiver to be valid, the ALJ ‘must certify through proper inquiry that the
waiver is knowing, intelligent, and voluntary.’” While the record showed that the
patient was aware of the hearing and voluntarily chose not to attend, there was no
indication that she “knew of her right to be present at the hearing or the purpose of
the hearing. Without such knowledge, [she] could not have knowingly and
intelligently waived her right to be present.” Also, “the ALJ did not make any
inquiry into [her] mental state on the morning of the hearing and whether she had
the ability to comprehend the right that she was waiving.”
Register v. State, 946 So. 2d 50 (Fla. 1st DCA 2006). “[A] patient has a
fundamental right to be present at a commitment proceeding [and] a court must
certify through proper inquiry that the waiver is knowing, intelligent, and
voluntary.”
Ibur v. State, 765 So. 2d 275 (Fla. 1st DCA 2000). The court held that a hearing
officer committed reversible error by not permitting a Baker Act patient to testify
at his hearing for involuntary hospitalization, stating: “Because involuntary
commitment is a substantial deprivation of liberty at which fundamental due
process protections must attach, the patient cannot be denied the right to be
present, to be represented by counsel, and to be heard.”
Williams v. State, 692 So. 2d 257 (Fla. 1st DCA 1997). The appellate court
reversed an order for involuntary commitment and remanded, holding that the
record did not show that the appellant had waived his right to be present. While an
individual may waive the right “to be personally present and be constructively
present through counsel, the court must certify through proper inquiry that the
waiver is knowing, intelligent and voluntary.”
Joehnk v. State, 689 So. 2d 1179 (Fla. 1st DCA 1997). The appellate court
reversed an order for involuntary commitment and remanded, holding that the
appellant’s lawyer informing the trial court that the appellant did not wish to
appear at an involuntary commitment hearing was an insufficient waiver of his
fundamental right to be present. While an individual may waive the right “to be
personally present and be constructively present through counsel, the court must
certify through proper inquiry that the waiver is knowing, intelligent and

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
394
voluntary.”
D. Notice to and Participation of State Attorney at Involuntary Placement
Hearings
Wickland v. State, 642 So. 2d 670 (Fla. 1st DCA 1994). The appellate court held
that the trial court failed to comply with the requirements of the Baker Act when it
did not serve notice of an involuntary placement hearing on the state attorney’s
office, the state attorney did not appear at the hearing, the state’s psychiatrist did
not assert personal knowledge of the underlying facts of the case, and the trial
court’s order of involuntary placement quoted verbatim from the petition.
Jones v. State, 611 So. 2d 577 (Fla. 1st DCA 1992). The appellate court reversed
the trial court’s order for involuntary placement because the former patient’s due
process rights were violated:
The state attorney’s office was not represented at the hearing, and
there is nothing in the record to indicate that notice was served on the
state. We are cognizant that in proper circumstances, the absence of a
representative for the state in a Baker Act proceeding may be deemed
harmless. . . . However, in the instant case, it appears the absence of
the state was a contributing factor in the due process deficiencies
attendant upon the proceeding. Appellant’s treating psychiatrist was
the only witness. He testified in a loose, narrative fashion, marked by
generalities and speculation concerning appellant’s potential for
violence. The psychiatrist’s opinions seemingly were based upon
reports received from other unidentified persons, which hearsay went
unchallenged.
Jordan v. State, 597 So. 2d 352 (Fla. 1st DCA 1992). The appellate court affirmed
the trial court’s orders for involuntary placement. Although no state attorney was
present at the hearings and the trial judge examined the witnesses, any error was
harmless because “the trial judge conducted the proceeding in an impartial and
neutral manner and accorded appellants all of the constitutional and statutory rights
to which they are entitled.”
E. Duty of State Attorney and Role of Counsel for Receiving Facility in
Involuntary Placement Hearings
In re [V.S.], No. 95-577-IN 003 (Fla. 6th Cir. Ct. Feb. 13, 1995). With regard to
the participation of the attorney for a receiving facility in a Baker Act involuntary
placement hearing, the court held that

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
395
the facility has every right to employ legal counsel to represent their
legal interests in any proceeding where the facility’s legal rights,
liabilities or corporate interests are implicated.
Since future actions of the facility, either in providing ordered
treatment, or arranging for discharge of the patient, are predicated on
the outcome of the hearing, the facility is entitled to have counsel
present during the adjudicatory process. Counsel for the facility,
although present at the hearing, may not interpose evidentiary
objections or participate in questioning witnesses. This is the assigned
role of the state attorney. While the facility may be a party in interest
for the purpose of placing the controversy before the court, they do
not have a legally protectable interest in the outcome of an
adjudication of the need for involuntary mental health treatment. The
statute permits the facility administrator to throw out the first ball, but
the constitutional rights of the patient require that the state attorney
pitch the game.
Op. Att’y Gen. Fla. 74-53 (1974), Duties of state attorney in habeas proceedings.
“Absent express statutory authority, the state attorney is not responsible for
representing the administrator of a private treatment facility, which has a contract
to take patients in need of hospitalization pursuant to [the Baker Act] in a habeas
corpus proceeding involving a petition for involuntary hospitalization in which the
state is not a party.”
F. Deadline for Filing Petitions and Notices
Pullen v. State, 802 So. 2d 1113 (Fla. 2001). Pullen appealed an order for her
continued involuntary civil commitment. Her public defender filed an Anders brief,
“stating that he could discern no reversible error in the proceedings below. Despite
being given the opportunity to file her own pro se brief, Pullen did not do so. The
State filed a motion to dismiss the appeal, arguing that the Anders procedure does
not apply to civil commitment proceedings. The First District Court of Appeal
agreed and dismissed Pullen’s appeal.” But the supreme court reversed, noted that
“[i]n a criminal context, a ‘no-merit’ letter and withdrawal, such as the procedure
used in the instant case, would clearly not be sufficient,” and held that “the Anders
procedure should apply to involuntary civil commitments.” But it stated further
that it was
concerned that it may be a hollow remedy for those appellants who
pursue an Anders appeal. At oral argument, the parties recognized that

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
396
under the present time frame the appeals process often exceeds the
six-month commitment period. . . . In fact, this delay would also occur
in cases where counsel files an arguably meritorious appeal of a civil
commitment order under the Baker Act.
In light of this time frame, we request the Appellate Rules
Committee to consider the adoption of expedited procedures for the
appeal of civil commitment orders under the Baker Act. Procedures
that the committee should consider include, but are not limited to, an
expedited time frame for the filing of the notice of appeal, a shortened
time for the serving of briefs, and a provision requiring the
appointment of a guardian ad litem.”
D.M.H. v. Pietilla, 33 So. 3d 800 (Fla. 5th DCA 2010). The appellate court held
that rule 1.090, Florida Rules of Civil Procedure (now rule 2.514(a), Florida Rules
of Judicial Administration), governs the computation of time prescribed for an
involuntary inpatient placement hearing under section 394.467(6)(a)1., Florida
Statutes. That rule provides that Saturdays, Sundays, and legal holidays are
excluded when the time period is less than seven days. Therefore, the appellate
court affirmed the trial court’s denial of the patient’s petition for a writ of habeas
corpus that was based on the failure to hold a hearing within five calendar days.
Johnson v. Johnson, 585 So. 2d 1188 (Fla. 2d DCA 1991). A master entered
findings and recommendations awarding sole custody of the parties’ minor child to
the father. The next day the trial court issued an order adopting those findings and
recommendations, which deprived the mother of the right to serve exceptions to
the master’s report within 10 days of service on her under rule 1.490, Florida Rules
of Civil Procedure. The appellate court therefore vacated the order and remanded.
G. Appeal Not Moot
Godwin v. State, 593 So. 2d 211 (Fla. 1992). The Supreme Court of Florida held
that an appeal from a civil commitment order under the Baker Act does not
become moot solely because the person subject to the order has already been
released. The court considered the “collateral legal consequences” of involuntary
commitment; i.e., unpaid fees for patient services constituting a lien on property. It
also mentioned other consequences that, while not rising to the level of collateral
legal consequences, are significant, such as societal stigma, restrictions on
privileges and opportunities (e.g., restriction on driver licenses, the right to vote,
and the right to carry a concealed weapon).

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
397
H. Jurisdiction of Courts
W.M. v. State, 992 So. 2d 383 (Fla. 5th DCA 2008). The trial court ordered the
patient to be involuntarily committed for three weeks. The patient didn’t respond to
treatment, so the hospital administrator sought continued treatment, and the court
ordered six more months of treatment. The patient appealed, arguing that the court
had no jurisdiction to order the continued treatment. The appellate court affirmed,
holding that although continued involuntary placement hearings are administrative,
“the circuit court retains concurrent jurisdiction over the involuntary commitment
proceedings. . . . [T]he Legislature’s intent was that the administrative hearing
requirement applies after a patient is committed to a long-term treatment period at
a treatment facility” instead of a community-based receiving facility. Because the
initial order was for short-term treatment, the court properly exercised jurisdiction
to order further treatment. “However, once long-term treatment is ordered, a
petition for continued treatment must be addressed in an administrative hearing.”
Liebman v. State, 555 So. 2d 1242 (Fla. 4th DCA 1989). “[A] determination that
a person is incompetent . . . is clearly within the constitutionally described
jurisdiction of a circuit court and is of a judicial nature.” However, a hearing
officer can determine continued incompetency after a circuit court has made the
initial determination.
I. Testimony
U.S. v. Chase, 340 F.3d 978 (9th Cir. 2003). The appellate court held that
psychiatrists can’t testify against patients who make dangerous or threatening
confessions during therapy, but affirmed the defendant’s conviction because the
admission of the psychiatrist’s testimony in this case was harmless. The court ruled
that although psychiatrists are sometimes required to report certain threats to
authorities, prosecutors can’t use testimony from psychotherapists to help convict
their patients. The court concluded that “the gain from refusing to recognize a
dangerous-patient exception to the psychotherapist-patient testimonial privilege in
federal criminal trials outweighs the gain from recognizing the exception.” It stated
that “although incarceration is one way to eliminate a threat of imminent harm, in
many cases treatment is a longer-lasting and more effective solution. A criminal
conviction with the help of a psychotherapist’s testimony is almost sure to spell the
end of any patient’s willingness to undergo further treatment for mental health
problems.” The court noted that its ruling doesn’t extend to proceedings in civil
court over whether the patient should be committed to a hospital.
Linn v. Fossum, 946 So. 2d 1032 (Fla. 2006). The Florida Supreme Court

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
398
resolved a conflict between the First and Fourth district courts of appeal, holding
an expert may not “testify on direct examination that the expert relied on
consultations with colleagues or other experts in forming his or her opinion. . . .
[S]uch testimony is inadmissible because it impermissibly permits the testifying
experts to bolster their opinions and creates the danger that [they] will serve as
conduits for the opinions of others who are not subject to cross-examination.” The
court emphasized that its opinion “in no way precludes experts from relying on
facts or data that are not independently admissible in evidence ‘[i]f the facts or data
are a type reasonably relied upon by experts in the subject.’”
Rogers v. State, 40 So. 3d 888 (Fla. 5th DCA 2010). The trial court permitted the
state to have the arresting officer testify from China via satellite, finding that “the
State interest and necessities of the case warranted the use of the satellite
procedure.” The defendant appealed, arguing that his constitutional right to
confront a witness was violated. But the appellate court affirmed, stating that his
rights of confrontation had been protected: “The methodology utilized allowed the
witness to be fully cross examined by the defense, and the jury was fully able to
observe the demeanor of the witness as he testified.” The appellate court also held
that “the oath element, backed up by the possibility of the imposition of the
penalties of perjury, was met.”
Mitchell v. State, 98 So. 3d 694 (Fla. 2d DCA 2012). After being convicted of
being a sexually violent predator, Mitchell was ordered to civil commitment. The
trial court denied his petition for release from commitment, relying on the state’s
medical expert witness’s testimony that it was not safe for Mitchell to be at large,
although Mitchell’s medical expert testified to the contrary. The appellate court
affirmed, stating: “The trial court’s determination of the weight and credibility of
competing expert opinions in chapter 394 proceedings will not be overturned
unless clearly erroneous.”
II. Clinical Records and Confidentiality
Jaffee v. Redmond, 518 U.S. 1, 116 S.Ct. 1923, 135 L.Ed.2d 337 (1996).
“[C]onfidential communications between a licensed psychotherapist and her
patients in the course of diagnosis or treatment are protected from compelled
disclosure.” The Court stated:
Effective psychotherapy depends upon an atmosphere of confidence
and trust, and therefore the mere possibility of disclosure of
confidential communications may impede development of the
relationship necessary for successful treatment. The privilege also

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
399
serves the public interest, since the mental health of the Nation’s
citizenry, no less than its physical health, is a public good of
transcendent importance. In contrast, the likely evidentiary benefit
that would result from the denial of the privilege is modest. That it is
appropriate for the federal courts to recognize a psychotherapist
privilege is confirmed by the fact that all 50 States and the District of
Columbia have enacted into law some form of the privilege.”
The Court explained the rationale for extending the privilege to “confidential
communications made to licensed social workers in the course of psychotherapy.”
The Court rejected the use of in camera inspections as a means to balance the
competing interests of the criminal defendant and the witness, saying that
“[m]aking the promise of confidentiality contingent upon a trial judge’s later
devaluation of the relative importance of the patient’s interest in privacy and the
evidentiary need for disclosure would eviscerate the effectiveness of the privilege.”
Opis Management Resources, LLC v. Secretary, Florida Agency for Health Care
Admin., 713 F.3d 1291 (11th Cir. 2013). Section 400.145, Florida Statutes,
“which provides for the release of medical records of deceased residents of nursing
homes to certain specified individuals,” is preempted by the confidentiality
provisions and regulations of the federal HIPAA Act. Therefore, nursing facilities
properly declined to provide requested records of deceased residents to spouses
and attorneys-in-fact who had not been appointed personal representatives of the
residents’ estates. The HIPAA privacy rule prohibits “covered entities” from
disclosing “protected health information” except in specified circumstances.
Sections 164.502(a)(1)(i) and (g)(1) of 45 C.F.R. allow disclosure to a “personal
representative.” The court refused to interpret the term “personal representative” to
include a spouse as provided in section 400.145, Florida Statutes. Therefore, for
disclosure of the medical records of a deceased nursing home resident, an estate
would have to be opened and a personal representative will have to be appointed.
Caraballo v. State, 39 So. 3d 1234 (Fla. 2010). The defendant was convicted of
first degree murder, among other crimes, and sentenced to death. The appellate
court affirmed the convictions but vacated the sentence and remanded for a new
penalty phase. It held that the trial court erred in permitting the mental health
expert who had conducted the defendant’s competency evaluation to testify, over
defense objections, during the penalty phase. His testimony was introduced by the
state to show that the expert opined at the time of the evaluation that the defendant
was being untruthful and was malingering. The trial court abused its discretion by
permitting this testimony as rule 3.211, Florida Rule of Criminal Procedure, clearly
protects its confidentiality, and the error was not harmless.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
400
State v. Roberson, 884 So. 2d 976 (Fla. 5th DCA 2004). The defendant sought
production of the mental health records of his alleged victim (a juvenile). The trial
court ordered an in camera inspection of the records to determine whether
disclosure was warranted. The state sought review and the appellate court quashed
the order, stating that while the records of the alleged victim’s Baker Act
proceedings were subject to in camera inspection and possible disclosure, her other
mental health records were not: “[N]either the Evidence Code, nor any applicable
constitutional principle allows the invasion of a victim’s privileged
communications with her psychotherapist.”
Cedars Healthcare Group, Ltd. v. Freeman, 829 So. 2d 390 (Fla. 3d DCA 2002).
Freeman sued Cedars Healthcare Group, alleging she was assaulted by at least two
male patients while she was a patient there. The trial court granted her motion for
production of photographs of all male patients who were in the ward during a
specified three-day period. The appellate court quashed the order granting her
motion, stating that she did not show a compelling need for the evidence “that
outweighs the constitutional privacy rights of these non-party psychiatric patients.”
Community Psychiatric Centers of Florida, Inc. v. Michael Bevelacqua, 673 So.
2d 948 (Fla. 4th DCA 1996). The trial court granted the plaintiff’s discovery
request for the names and addresses of certain former patients of the defendant
psychiatric hospital who witnessed a personal injury incident, and the identity of a
patient who had been involved in a similar incident. The hospital sought review,
and the appellate court quashed the trial court order, stating that clinical records are
confidential unless waived by “express and informed consent”; there is no “waiver
by silence.” Further, the patient’s need for the information did not outweigh “the
possible harm of disclosure to the patients.”
State v. Famiglietti, 817 So. 2d 901 (Fla. 3d DCA 2002). A defendant in a
criminal case cannot “invade the victim’s privileged communications with her
psychotherapist [even] if the defendant can establish a reasonable probability that
the privileged matters contain material information necessary to his defense.” The
court disagreed with State v. Pinder, 678 So. 2d 410 (Fla. 4th DCA 1996), in
which the Fourth District Court of Appeal held otherwise. It also noted that “the
more recent decision of the United States Supreme Court in Jaffee rejects the idea
of applying a balancing test to the psychotherapist-patient privilege.”
Trainor v. State, 768 So. 2d 1123 (Fla. 2d DCA 2000). The trial court excluded
from evidence the records relating to the victim’s hospitalization two years earlier
under the Baker Act and “the victim’s other mental health records associated with
the hospitalization.” The defendant appealed, but the appellate court affirmed,

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
401
finding no evidence that the victim’s mental health records indicated that his
mental condition “affected his propensity to tell the truth” or that he suffered from
a mental condition at the time of the incident or trial that “affected his ability to
observe, remember, and accurately recount matters about which he testified.”
Butterworth v. X Hosp., 763 So. 2d 467 (Fla. 4th DCA 2000). In its investigation
of Medicaid fraud, the Attorney General’s Office served subpoenas on a hospital.
The hospital produced the requested business records but did not produce the
mental health treatment records of adolescent Medicaid patients, some of which
contained information regarding substance abuse treatment. The Attorney
General’s Office agreed that substance abuse records required a court order, but
argued that it was entitled to the mental health treatment records without a court
order. The circuit court issued an order “requiring court approval of investigative
subpoenas for Medicaid patient records involving adolescent mental health
treatment,” holding that the Attorney General must show good cause for the release
of the records. The Attorney General sought certiorari review, which the appellate
court denied, agreeing with the circuit court.
NOTE: The court had applied the 1997 version of section 394.4615, Florida
Statutes, but the statute was amended in 2000 to specifically provide: “Clinical
records relating to a Medicaid recipient shall be furnished to the Medicaid Fraud
Control Unit in the Department of Legal Affairs, upon request.” § 394.4615(6),
Fla. Stat.
Katlein v. State, 731 So. 2d 87 (Fla. 4th DCA 1999). The court set out a
mechanism for determining when it is appropriate for a court to order the release of
Baker Act records. The party seeking the records must first make a threshold
showing that the privileged records “‘are likely to contain relevant evidence.’ . . .
The defendant must advance a good faith factual basis which is not ‘merely a
desperate grasping at a straw.’ . . . In other words, no fishing expeditions.” If the
showing is made, “the court will do an in camera inspection.” Then if the court
concludes that the records do contain relevant information, it should allow the
parties access to them “in order to determine whether disclosure of the information
to the trier of fact is ‘required to ensure the defendant a fair trial.’” The burden is
on the party seeking disclosure to demonstrate that disclosure is required.
Op. Att’y Gen. Fla. 08-20 (2008), Patient Records -- Emergency Medical
Services.
Section 401.30(4), Florida Statutes, makes specific provision for
records of emergency calls: “Records of emergency calls which
contain patient examination or treatment information are confidential

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
402
and exempt from the provisions of s. 119.07(1) and may not be
disclosed without the consent of the person to whom they pertain, but
appropriate limited disclosure may be made without such consent. . . .
This subsection does not prohibit providing information to any law
enforcement agency or any other regulatory agency responsible for the
regulation or supervision of emergency medical services and
personnel.
While the . . . subsection recognizes the sensitive nature of medical
records, the statute authorizes access to specified individuals and
entities without the patient’s consent. Section 401.30(4), Florida
Statutes, clearly provides that the subsection, which makes emergency
call records containing patient examination or treatment information
confidential and exempt from disclosure without the patient’s consent,
does not prohibit a licensee from providing information to any law
enforcement agency.
Accordingly, I am of the opinion that section 401.30(4), Florida
Statutes, permits an emergency medical services transportation
licensee to release records of emergency calls which include the
patient’s name, address, and pertinent medical information to a local
law enforcement agency that does not provide regulatory or
supervisory responsibility over the emergency medical services
licensee.
See also:
State v. Johnson, 814 So. 2d 390 (Fla. 2002)
Acosta v. Richter, 671 So. 2d 149 (Fla. 1996)
Estate of Stephens ex rel. Clark v. Galen Health Care Inc., 911 So. 2d 277 (Fla.
2d DCA 2005)
Lemieux v. Tandem Health Care of Florida Inc., 862 So. 2d (Fla. 2d DCA 2003)
O’Neill v O’Neill, 823 So. 2d 837 (Fla. 5th DCA 2002)
Attorney ad Litem for D.K. v. Parents of D.K., 780 So. 2d 301 (Fla. 4th DCA
2001)
Ussery v. State, 654 So. 2d 561 (Fla. 4th DCA 1995)

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
403
Hunter v. State, 639 So. 2d 72 (Fla. 5th DCA 1994)
III. Public Records
Tribune Co. v. D.M.L, 566 So. 2d 1333 (Fla. 2d DCA 1990). The court held that a
Baker Act hearing is a closed hearing which the media and the public cannot
attend. The hearings contain the clinical record of the patient, which is not a public
record and which is deemed confidential pursuant to then-section 394.459(9),
Florida Statutes (now see section 394.4615). The public policy for having a closed
Baker Act hearing is “to avoid substantial injury” to the patient’s liberty interest
and individual dignity.
Op. Att’y Gen. Fla. 97-67 (1997), clerk’s authority to maintain confidentiality of
confidential information contained in the official records.
It is the clerk’s responsibility . . . to devise a method to ensure the
integrity of the Official Records while also maintaining the
confidential status of information contained therein. . . . Nothing in
the Public Records Law or the statutes governing the duties of the
clerk authorizes the clerk to alter or destroy Official Records.
However, the statute does impose a duty on the clerk to prevent the
release of confidential material that may be contained in the Official
Records. . . . [T]here is nothing that precludes the clerk from altering
reproductions of the Official Records to protect confidential
information. The manner in which this is to be accomplished rests
within the sound discretion of the clerk.
Op. Att’y Gen. Fla. 93-51 (1993), regarding whether law enforcement records
under the Baker Act are public records. A law enforcement officer’s “event or
incident report prepared after a specific crime has been committed which contains
information given during the initial reporting of the crime, and which is filed with
the law enforcement agency as a record of that event, is not confidential [and is a
public record subject to inspection and copying pursuant to ch. 119, F.S.”
However, the “written report detailing the circumstances under which the person
was taken into custody” is made a part of the patient’s clinical record and is
confidential and exempt from the Public Records Law.
Op. Att’y Gen. Fla. 91-10 (1991), regarding the inspection and copying
requirements of Baker Act and Marchman Act records in the possession of the
clerk of court. Baker Act patients’ clinical records produced pursuant to then-
section 394.459(9), Florida Statutes (now see section 394.4615), are specifically

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
404
made confidential and are exempt from being inspected and copied by the public as
provided for in chapter 119, Florida Statutes. “Generally, when materials are filed
with the clerk of court, such records are open to the public. In AGO 89-94, this
office concluded that in the absence of a specific statutory provision or court rule
making a record confidential or dictating the manner of its release and absent a
court order closing a particular court record, probate records filed with the clerk of
court are subject to Ch. 119, F.S.”
Op. Att’y Gen. Fla. 86-101 (1986), regarding whether the statutorily required
reports of a law enforcement officer under the Baker Act are exempt from
disclosure. A law enforcement agency prepares an “event form,” an “incident
report–narrative form,” and a “report of law enforcement officer” form when a
person is taken into custody under the Baker Act. Only the latter “report of law
enforcement officer” form, “which is statutorily required to be included in the
clinical record of a patient, is confidential and statutorily declared not to be a
public record. The event forms or incident reports, “which appear to be analogous
to crime and arrest reports,” are public records.
IV. Payment of Involuntary Placement Bills
Op. Att’y Gen. 07-11 (2007), regarding hospital authorities and immigrants
without legal status.
The intent of the . . . Hospital Authority’s enabling legislation appears
to be to provide medical services to those indigents who live within
the district. [Therefore] the term “residents of the district” . . . was
intended by the Legislature as a pure residence requirement, and not
as a requirement for domicile, legal residence, or citizenship. Thus,
the enabling legislation for the authority would appear to permit the
authority to provide services to otherwise qualified indigent illegal
aliens living within the district. Inasmuch as Chapter 04-421, Laws of
Florida, does not distinguish between the types of indigent residents, it
appears that the hospital authority should provide healthcare access to
these aliens on the same basis as other indigent residents.
The opinion quoted case law that held: “Any place of abode or dwelling place
constitutes a ‘residence,’ however temporary it may be, while the term ‘domicile’
relates rather to the legal residence of a person, or his home in contemplation of
law. As a result one may be a resident of one jurisdiction although having a
domicile in another.”

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
405
Op. Att’y Gen. Fla. 93-49 (1993), regarding who is responsible for the payment of
an involuntary Baker Act placement. A county is not primarily responsible for the
payment of hospital costs. However, it may be liable for hospital costs if a person
“is arrested for a felony involving violence to another person, is arrested for a
felony involving violence against another person, is taken to a receiving facility
and specified sources for reimbursement are not available.” Depending on the
Baker Act patient’s ability to pay, the patient is primarily responsible for the
payment of any hospital bill for involuntary placement under the Baker Act.
However, if the patient is indigent, the state “is obligated to provide treatment at a
receiving or treatment facility . . . without cost to the county.”
Op. Att’y Gen. Fla. 74-271 (1974), Involuntary Hospitalization in Private
Psychiatric Facility.
A circuit court judge may order a patient involuntarily hospitalized at
a private psychiatric facility not under contract with the State . . .
provided the patient meets the statutory criteria for involuntary
hospitalization, the facility has been approved by [DCF], and the cost
of treatment is to be borne by the patient, if he is competent, or by his
guardian if the patient is incompetent.
When state funds are to be expended for involuntary hospitalization of
a patient in a private psychiatric facility, such facility must be under a
contract with the state.
V. Transportation of Baker Act Patients
Administrator, Retreat Hosp. v. Johnson In and For Broward County, 660 So.
2d 333 (Fla. 4th DCA 1995). Four patients were certified by a hospital for
involuntary placement and were transported to the hospital’s facility by private
individuals. The patients’ public defender filed habeas corpus petitions, alleging
that the patients had been transported by someone other than law enforcement,
which violated the Baker Act. The trial court ordered that the sheriff devise a plan
for transportation services in compliance with the law and that another hearing be
held within 90 days to review the plan, and also ordered that “[a]ny person
initiating a certificate or other document which is used to initiate an involuntary
examination pursuant to either §§ 394.463(2) and (3), F.S. shall file with the clerk
of courts within 24 hours of its execution the original certificate or other original
document.” At the hearing the hospital moved to strike all pleadings and vacate the
order “for lack of subject matter jurisdiction, arguing that the trial court was
conducting an improper regulatory and advisory inquiry without subject matter

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
406
jurisdiction because the matters were now moot as a result of the patients’ release
and because the writs had been dismissed.” The trial court denied the motion and
rendered another order, which the hospital also claimed was outside the court’s
authority and it sought a writ of prohibition. The appellate court disagreed with the
hospital on certain issues, stating that “the trial court had jurisdiction to conduct a
judicial inquiry into the means by which the patients had been transported to the
facility for involuntary examination if in violation of the statutory mandate and to
issue appropriate orders to correct abuses of the provisions alleged to be violated,”
and the jurisdiction did not end just because the patients had been released. The
appellate court also disagreed with the hospital that the special assistant public
defender did not have standing to file the habeas petitions. But it granted the writ
of prohibition, stating: “[W]hen the trial court, in its . . . order indicated its intent to
consider additions to the statutory requirements for hospitalizing Baker Act
patients by requiring a trial court order before hospitalization would be
permissible, it was engaging in a process of statutory amendment beyond the scope
of its powers.”
Pruessman v. Dr. John T. MacDonald Foundation, 589 So. 2d 948 (Fla. 3d
DCA 1991). A patient was discharged from a hospital but refused to leave. The
hospital administrator contacted an outside doctor to have the patient Baker Acted.
The patient sued the hospital and the city, and the trial court dismissed the case.
The appellate court affirmed, stating that the outside doctor was not alleged to be
an agent of the hospital, “the mere request by [the hospital] for a proper Baker Act
commitment does not in itself constitute a cognizable cause of action,” and the city
was not liable, as a matter of law, “for the act of its police officers in taking the
plaintiff in custody [based on the doctor’s] facially valid, executed certificate” and
transporting him to a mental health facility because “the police had no discretion to
refuse to do so” under the circumstances.
Op. Att’y Gen. Fla. 01-73 (2001), Mentally ill person transported to treatment
facility.
[S]ection 394.462, Florida Statutes, describes a comprehensive
scheme for the transportation of persons to a receiving facility for
involuntary examination and treatment when they are in the custody
of a law enforcement agency. The general rule is that where statutory
language is plain and definite in meaning without ambiguity, it fixes
the legislative intention and statutory interpretation and construction
are not needed.
. . . . [I]f a person is the subject of an ex parte order or certificate

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
407
requiring involuntary examination and treatment under Florida’s
Baker Act, the single law enforcement agency designated by the
county for this purpose is responsible for transporting that person to
the nearest receiving facility. If a person is taken into custody by a law
enforcement officer for minor criminal behavior or noncriminal
behavior that meets the statutory guidelines for involuntary
examination under the act, the law enforcement officer taking the
person into custody is responsible for transporting the person to the
nearest treatment facility. If a law enforcement officer arrests a person
for commission of a felony and believes that the person meets the
guidelines for involuntary examination or placement, the person
arrested shall be processed through the criminal justice system as any
other criminal suspect and is entitled to examination and treatment in
the facility where he or she is held.
Op. Att’y Gen. Fla. 85-81 (1985), Transporting and Receiving Baker Act Patients.
“[T]he law enforcement agency designated by the county is the only agency
authorized to transport persons to the receiving facility in the absence of an
agreement with an emergency medical transport service to perform this
transportation” or a court order otherwise.
The statutes do not require a county facility to have the capability to
house patients for 72 hours in order to be qualified to be designated by
[DCF] as a receiving facility. Where a person is being transported to a
so-called “alternate receiving facility” for an involuntary examination,
the transportation provisions . . . remain applicable. . . . The Sheriff’s
Office is liable for negligent ministerial acts committed in the
transportation of patients under [the Baker Act].
Op. Att’y Gen. Fla. 78-123 (1978), Counties, patient transportation. The Baker
Act “does not authorize or require counties to pay the costs of transferring
nonindigent, nonresident mentally ill patient in treatment facilities in Florida to
treatment facilities in the states of their residence.”
Op. Att’y Gen. 74-108 (1974), regarding costs of transporting mental patients.
“[A] municipal police department is required to transport patients to a receiving
facility pursuant to an ex parte order of the court or a physician’s certificate or
when a law enforcement officer makes an independent judgment that a person is in
need of emergency examination and treatment.” The Baker Act doesn’t require any
patient or guardian or representative to pay for transportation to a receiving
facility. Instead, when “a law enforcement officer is required to transport patients

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
408
to a receiving facility, the costs incurred are simply a part of the budgeted
operating expenses of the municipal police department.”
VI. Law Enforcement
A. Warrantless Entry — Exigent Circumstances
Michigan v. Fisher, 558 U.S. 45, 130 S.Ct. 546, 175 L.Ed.2d 410 (2009).
Officers had been called to the residence because the decedent was “going crazy.
They “found a household in considerable chaos” and saw blood on a pickup truck
in the driveway and on a door of the house and could see Fisher through a window,
screaming and throwing things. The front door was blocked by a couch and the
back door was locked. The officers knocked, but Fisher did not answer. They saw
he had cut his hand and asked him whether he needed medical attention. He
ignored their questions and “demanded, with accompanying profanity, that the
officers go to get a search warrant.” When an officer pushed the front door open
and started going into the house, he saw Fisher pointing a gun at him and
withdrew. Fisher was charged with assault with a dangerous weapon and
possession of a firearm during the commission of a felony.
Fisher filed a motion to suppress the officer’s statement about him pointing a gun,
which the state trial court granted, holding that the officer violated the Fourth
Amendment of the U.S. Constitution when he entered the house. The state
appellate court affirmed. But the U.S. Supreme Court reversed, holding that the
search was proper under the “emergency aid” exception to the warrant
requirement, under which officers “may enter a home without a warrant to render
emergency assistance to an injured occupant or to protect an occupant from
imminent injury.”
Brigham City, Utah v. Stuart, 547 U.S. 398, 126 S.Ct. 1943, 164 L.Ed.2d 650
(2006). Officers responding to a call about a loud party saw juveniles drinking in
the yard and “saw through a screen door and windows an altercation in the kitchen
between four adults and a juvenile, who punched one of the adults, causing him to
spit blood in a sink. An officer opened the door and announced the officers’
presence,” but no one noticed. So the officer went into the kitchen and again called
out, and the fight stopped. The officers arrested the participants and charged them
with various misdemeanors. The trial court granted the defendants’ motion to
suppress, the state appellate court affirmed, and the state supreme court affirmed as
well, finding that the officers had violated the Fourth Amendment protection
against unreasonable search and seizure: “The injury caused by the juvenile’s

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
409
punch was insufficient to trigger the so-called ‘emergency aid doctrine’” and the
officers weren’t seeking to help the injured adult but rather were acting in their law
enforcement capacity. Further, the state supreme court held that “the entry did not
fall within the exigent circumstances exception to the warrant requirement.” But
the U.S. Supreme Court granted certiorari and reversed, stating:
It is a “basic principle of Fourth Amendment law that searches
and seizures inside a home without a warrant are presumptively
unreasonable.” . . . Nevertheless, because the ultimate touchstone of
the Fourth Amendment is “reasonableness,” the warrant requirement
is subject to certain exceptions. . . . We have held, for example, that
law enforcement officers may make a warrantless entry onto private
property to fight a fire and investigate its cause, . . . to prevent the
imminent destruction of evidence, . . . or to engage in “hot pursuit” of
a fleeing suspect. . . . “[W]arrants are generally required to search a
person’s home or his person unless ‘the exigencies of the situation’
make the needs of law enforcement so compelling that the warrantless
search is objectively reasonable under the Fourth Amendment.” . . .
One exigency obviating the requirement of a warrant is the need
to assist persons who are seriously injured or threatened with such
injury. . . . Accordingly, law enforcement officers may enter a home
without a warrant to render emergency assistance to an injured
occupant or to protect an occupant from imminent injury. . . .
The Court reiterated that the officers’ subjective motivations were not dispositive;
an officer’s action is reasonable under the Fourth Amendment if the circumstances,
viewed objectively, justified the action. It also stated that the Fourth Amendment
requires a “knock and announce” and “once the announcement was made the
officers were free to enter. They did not have to wait until further danger was done.
“The role of a peace officer includes preventing violence and restoring order, not
simply rendering first aid to casualties.”
Seibert v. State, 923 So. 2d 460 (Fla. 2006). After Seibert locked out his roommate
and said he was going to kill himself, the roommate called 911. Police officers
responded, and Seibert opened the door a few inches, told them he was okay, and
said they could leave. They entered anyway, saw a severed foot through a partly
open bathroom door, and arrested Seibert for murder. He was convicted and
sentenced to death and appealed, claiming, among other things, that “the trial court
erred in denying his motion to suppress evidence discovered and statements made
as a result of the nonconsensual, warrantless entry and search by the police of his

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
410
apartment.” The Florida Supreme Court affirmed, stating that the roommate’s 911
call about suicide established the necessary exigent circumstance because the
officers had an objectively reasonable belief that Seibert’s life was in danger. The
court also cited “Seibert’s strange behavior in not answering the door for four or
five minutes after the officers first knocked, after which he immediately slammed
the door.”
The court also held that the officers’ search after entry was constitutional, stating
that “[t]he officers’ quick look around the apartment was not an extensive search
because they did not open any containers or even enter any other rooms. There has
been no evidence that any pretense existed on the part of the police in this case. It
was objectively reasonable for them to glance around to ensure that the apartment
and Seibert were secure. Moreover, insufficient time had elapsed for the officers to
determine that the exigency had passed.”
Riggs v. State, 918 So. 2d 274 (Fla. 2005). In the middle of the night, deputies
were summoned to an apartment complex where a four-year-old girl had been seen
wandering, naked and alone. The child was disoriented and “had no idea where she
had wandered out of,” so the deputies decided to search each apartment for her
caretakers. They noticed that every door on the second floor was closed except
one, and they thought the child might have come out of that apartment. They
pounded on the door at least three dozen times, identifying themselves as police
officers, but no one in the apartment responded. Concerned that “something had
happened to the child’s caregiver and that maybe there was a medical concern in
there,” the deputies entered the apartment. In the third room they looked in, they
found Riggs and the child’s babysitter. Riggs was arrested and filed a motion to
suppress the evidence, which the trial court granted. The Second District Court of
Appeal reversed, holding that “[t]he officers believed it was their duty to see that
the child’s caregiver was not incapacitated and justifiably entered the residence.”
The Florida Supreme Court approved the decision and disapproved the conflicting
opinion of Eason v. State, 546 So. 2d 57 (Fla. 1st DCA 1989). It stated that the
child “did not lead the deputies in any particular direction. A search based on a
feared medical emergency, however, does not require certainty. The Fourth
Amendment, which protects against unreasonable searches, requires only that the
police reasonably believe that an emergency exists.”
Zakrzewski v. State, 866 So. 2d 688 (Fla. 2004). After Zakrzewski failed to report
for class, his Air Force Sergeant called his home, hospitals, the Sheriff’s Office,
and the police. Unable to locate him, the sergeant went to his home, where he saw
a broken window and accumulated mail and asked the Sheriff’s Office to send a
deputy. The deputy told dispatch that he “was going to enter the house through the

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
411
broken window to check on the welfare and see if there had been any kind of
burglary inside.” In the home the deputy found the dead bodies of Zakrzewski’s
wife and two children, and eventually Zakrzewski was tried for murder and
sentenced to death. In a motion for postconviction relief he claimed, among other
things, ineffective assistance of counsel for failure to move to suppress evidence.
But the Supreme Court affirmed the trial court’s denial of relief on that claim,
stating that the deputy “did not enter Zakrzewski’s home with the intent to seize
evidence or make an arrest,” and that in any case Zakrzewski had not shown that
his attorney’s failure to file a motion to suppress caused him prejudice; i.e., that he
would not have pled guilty but for counsel’s errors.
Ortiz v. State, 24 So. 3d 596 (Fla. 5th DCA 2009). One evening a school called
the Sheriff’s Office to report that the parents of a six-year-old child had not picked
him up. A deputy picked the child up and took him home, and knocked on the
door, but got no response. The child led the officer into the garage, and the deputy
could then see that a light was on in the house. The child invited the deputy to
come into the house, and before entering the deputy announced his presence, but
no one responded. The deputy and the child looked around but didn’t find the
parents, so the child led the deputy to the parents’ bedroom, which was locked, and
no one responded to the deputy knocking and announcing his presence again.
Believing there might be an medical emergency “or worse,” the deputy unlocked
the door and looked under the bed and in closets “for a body,” and saw bags of
cocaine in the adjoining bathroom. When Ortiz entered the room, the deputy
arrested him on drug charges. Ortiz filed a motion to suppress, arguing that
“exigent circumstances did not justify a warrantless entry into his home, and
specifically, the locked bedroom,” and that “the six-year-old child did not have the
authority to consent to the warrantless entry into the house.” The trial court denied
the motion, and the appellate court affirmed, stating that the deputy could have
reasonably concluded that something was wrong. The appellate court noted that
such cases require a balancing of two important values:
our desire to have police officers perform the community caretaking
function particularly in perceived emergent circumstances, and the
warrant requirement to underpin a search. . . . [T]he benefit obtained
by allowing officers to act without a warrant in perceived emergency
situations must trump the marginal curtailment of the warrant
requirement. This case does not present a new exception, nor does it
diminish the respect for the sanctity of the home. Rather, it simply
adheres to the holding of our supreme court in Riggs, and applies a
recognized exception to the warrant requirement.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
412
Eastes v. State, 960 So. 2d 873 (Fla. 5th DCA 2007). Police were called to Eastes’
apartment after a “[d]isturbance call, possible suicide.” When they arrived, they
saw Eastes in his doorway, with blood running down his arms. An officer could
see broken glass on the apartment floor and “furniture in a state of disarray,” along
with other damage. The officer followed Eastes into his apartment, concluded he
was “very intoxicated,” and decided to take him to a mental health facility. The
officer explained to Eastes that he was not under arrest, but Eastes began swinging
his arms and hit the officer. He was taken to an ER and then to the police
department, and was not taken to the Baker Act receiving facility because it
wouldn’t accept an arrested person. The officer did request in his police report that
Eastes “be sent to the jail’s ‘physician unit’” because it “had mental health staff to
treat suicidal individuals.”
Eastes was charged with battery of a law enforcement officer, resisting an officer
with violence, and resisting an officer without violence (for refusing to cooperate
during booking). He filed a motion to suppress, which the trial court denied. The
appellate court affirmed, stating: “The Fourth Amendment does not bar a police
officer from making a warrantless entry into a residence when the officer
reasonably believes that a person within is in need of immediate aid. . . . It was
immaterial whether an actual emergency existed. The test is whether the officer
reasonably believed an emergency existed at the time of the warrantless entry.”
Eastes also argued that the trial court erred in denying his motion for judgment of
acquittal, claiming “the evidence was insufficient to establish that he met the
criteria for an involuntary examination, and therefore, the officers were not
engaged in the lawful execution of a legal duty.” But the appellate court rejected
that argument, stating:
The Florida Mental Health Act authorizes a law enforcement officer
to take a person who appears to meet the criteria for involuntary
examination into custody. . . . Here, the evidence supports a
determination that Eastes met the criteria for an involuntary
examination. His behavior, his physical condition, and the condition
of his apartment suggested a substantial likelihood that, without care
or treatment, Eastes would cause serious injury to himself in the near
future. The evidence further supported a conclusion that Eastes was
possibly suicidal and unable to determine for himself whether an
exam was necessary. Under these circumstances, the officers were
justified in placing him in protective custody for involuntary
examination.
B. Detention and Custody
Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
413
Graham v. Connor, 490 U.S. 386, 109 S.Ct. 1865, 104 L.Ed.2d 443 (1989).
Graham, a diabetic, noticed he was having an insulin reaction and asked a friend to
drive him to a store to get orange juice. When Graham saw how many people were
in the checkout line, he left the store and asked his friend to take him to another
friend’s house. A police officer saw Graham “hastily enter and leave the store”
and, suspicious, followed him and stopped the car he was in. The officer ordered
Graham and his friend to “wait while he found out what, if anything, had
happened” at the convenience store, and when the officer went to his car to call for
backup, Graham exited the car he was in, ran around it twice, and passed out on the
curb. An officer rolled him over and cuffed him, ignoring the friend’s “pleas to get
him some sugar.” Once Graham regained consciousness, the officers ignored his
request to check his wallet for his diabetic decal, and when a friend brought some
orange juice the officers would not let Graham have it. After getting a report that
nothing had happened at the convenience store, the officers drove Graham home
and released him. He later brought an action under 42 U.S.C. § 1983 based on
injuries he allegedly sustained during the investigatory stop, alleging that the
excessive force they used caused him to sustain “a broken foot, cuts on his wrists, a
bruised forehead, and an injured shoulder; he also claims to have developed a loud
ringing in his right ear.”
The federal trial court granted the defendants’ motion for a directed verdict,
“applying a four-factor test for determining when excessive use of force gives rise
to a § 1983 cause of action, which inquires, inter alia, whether the force was
applied in a good faith effort to maintain and restore discipline or maliciously and
sadistically for the very purpose of causing harm.” The appellate court affirmed,
“rejecting Graham’s argument that it was error to require him to prove that the
allegedly excessive force was applied maliciously and sadistically to cause harm,
and holding that a reasonable jury . . . could not find that the force applied was
constitutionally excessive.” But the U.S. Supreme Court vacated and remanded the
case, holding that the Court of Appeals erred in applying the four-part Johnson v.
Glick test (“which requires consideration of whether the individual officers acted in
‘good faith’ or ‘maliciously and sadistically for the very purpose of causing
harm’”), rather than the reasonableness test, and stating:
Determining whether the force used to effect a particular
seizure is “reasonable” under the Fourth Amendment requires a
careful balancing of “ ‘the nature and quality of the intrusion on the
individual’s Fourth Amendment interests’ ” against the countervailing
governmental interests at stake. . . . Our Fourth Amendment
jurisprudence has long recognized that the right to make an arrest or

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
414
investigatory stop necessarily carries with it the right to use some
degree of physical coercion or threat thereof to effect it. . . . [The
proper application [of the test of reasonableness] requires careful
attention to the facts and circumstances of each particular case,
including the severity of the crime at issue, whether the suspect poses
an immediate threat to the safety of the officers or others, and whether
he is actively resisting arrest or attempting to evade arrest by flight.
. . .
The “reasonableness” of a particular use of force must be
judged from the perspective of a reasonable officer on the scene,
rather than with the 20/20 vision of hindsight. . . . The Fourth
Amendment is not violated by an arrest based on probable cause, even
though the wrong person is arrested, . . . nor by the mistaken
execution of a valid search warrant on the wrong premises. . . . With
respect to a claim of excessive force, the same standard of
reasonableness at the moment applies: “Not every push or shove, even
if it may later seem unnecessary in the peace of a judge’s chambers,”
Johnson v. Glick, 481 F.2d, at 1033, violates the Fourth Amendment.
The calculus of reasonableness must embody allowance for the fact
that police officers are often forced to make split-second judgments—
in circumstances that are tense, uncertain, and rapidly evolving—
about the amount of force that is necessary in a particular situation.
As in other Fourth Amendment contexts, however, the
“reasonableness” inquiry in an excessive force case is an objective
one: the question is whether the officers’ actions are “objectively
reasonable” in light of the facts and circumstances confronting them,
without regard to their underlying intent or motivation. . . . An
officer’s evil intentions will not make a Fourth Amendment violation
out of an objectively reasonable use of force; nor will an officer’s
good intentions make an objectively unreasonable use of force
constitutional.
As to the federal civil rights violation count, the federal district court found that the
civil commitment was constitutionally permissible under the facts, and therefore
“there can be no policy or custom that officially sanctioned or ordered a
constitutional violation.” The court declined to retain jurisdiction over the state law
claims.
Thomas v. State, 748 So. 2d 363 (Fla. 5th DCA 2000). On their way to investigate

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
415
a call about a fight, officers saw Thomas walking 2½ blocks from the fight
location, with blood on his face, chest, and arms. They questioned him, but he was
“loud, incoherent, and flailing his arms around.” He said he had weapons, so the
deputies patted him down and found cocaine, and they arrested him. He filed a
motion to suppress, which the trial court denied, stating that the stop and search
were lawful “as a result of law enforcement exercising other activities other than
criminal law enforcement.” He appealed, but the appellate court affirmed, stating
that the initial detention was justified by the Baker Act.
Op. Att’y Gen. Fla. 99-68 (1999), regarding who may take a person who appears
to meet the criteria for involuntary examination into custody: state law
enforcement, federal law enforcement, or both. The opinion advised a federal
Veterans Affairs police officer that federal law enforcement officers are not law
enforcement officers for purposes of the Baker Act, and they “possess no authority
under the act to initiate the involuntary examination of a person or to transport
such person [to a receiving facility] as law enforcement officers.” The Baker Act
provisions imposing certain transportation responsibilities on law enforcement
officers “are not applicable to a federal veterans affairs police officer” unless,
under the Florida Mutual Aid Act, state and local law enforcement agencies in
Florida have entered into a mutual aid agreement with a federal law enforcement
agency.
Op. Att’y Gen. Fla. 92-46 (1992), regarding the duties of law enforcement
personnel. “Section 401.445(1), Florida Statutes, provides protection from
recovery in any action brought for examining or treating a patient without his or
her informed consent and extends such protection to ‘any person acting under the
direct medical supervision of a physician.’” But this does “not apply to law
enforcement personnel acting under the direction of an emergency medical
technician or paramedic” in restraining a patient who is refusing medical treatment.
However, if a law enforcement officer is “personally receiving ‘medical direction’
from a physician [through two-way voice communication], he or she would be
protected by the provisions of the statute.”
Op. Att’y Gen. Fla. 85-86 (1985), Definition of minor criminal behavior.
Words in statutes should be given the meaning accorded to them in
common usage unless a different connotation is expressed in or
necessarily implied from the context of the statute in which they
appear. . . . As no definition of “minor” or “minor criminal behavior”
has been provided in [the Baker Act] from which guidance may be
obtained, the term must be construed in its plain and ordinary sense.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
416
. . . The language of [the Baker Act] distinguishes minor criminal
behavior or noncriminal behavior from behavior which constitutes a
felony.
However, in the absence of a legislative or judicial determination otherwise, the
phrase “minor criminal behavior” “refers to criminal behavior which is not
dangerous or not as serious as other criminal behavior” and “is not limited to
crimes chargeable as misdemeanors but may include felonies which do not involve
violence against another person.”
Op. Att’y Gen. Fla. 74-39 (1974), Mental Health--Treatment of Federal Prisoner
at Receiving Facility--Law Enforcement Officers--U.S. Marshals not Peace
Officers under State Law. A federal prisoner held in a county jail pursuant to
contract tried to kill himself. Fearing liability, the jail had marshals remove the
prisoner, and they took him to a receiving facility for emergency admission. In
response to the inquiries of the marshal’s office, the attorney general opined that
section 394.463, Florida Statutes, does “not exclude the admission of a federal
prisoner to a receiving facility. Neither a United States marshal nor his deputy is a
law enforcement officer within the meaning of s. 394.463. The State of Florida is
not responsible for the cost incurred when a federal prisoner is admitted to a
receiving facility pursuant to s. 394.463. A United States marshal is not a peace
officer under Florida law.” The opinion stated that 28 U.S.C.A. § 570 (see current
28 U.S.C.A. § 564),which provided that “[a] United States marshal and his
deputies, in executing the laws of the United States within a State, may exercise
the same powers which a sheriff of the State may exercise in executing the laws
thereof,” refers to when the marshal is executing the laws of the United States “and
does not purport to authorize a marshal to execute the laws of a state.”
C. Use of Force
Valle v. City of Houston, 613 F.3d 536 (5th Cir. 2010). The plaintiffs’ son, who
suffered from depression and anxiety, was shot and killed by police officers who
responded to a call at the family home. The plaintiffs sued the city, seeking relief
under 42 U.S.C. § 1983, alleging excessive force. The district court granted the
city’s motion for summary judgment, and the appellate court affirmed. Although
the court found “the actions and decisions of the officers involved in this
unfortunate shooting to be very troubling, . . . the Valles did not present sufficient
evidence to show that the highly predicable consequence of sending non-[Crisis
Intervention Team] officers in response to their call for help would result in the
shooting of their son.”

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
417
Oliver v. Fiorino, 586 F.3d 898 (11th Cir. 2009). The plaintiff’s decedent died
after being tased by police officers at least eight times in a two-minute period. The
plaintiffs brought a 42 U.S.C. § 1983 claim alleging excessive force. The officers
filed a motion for summary judgement based on qualified immunity. The trial court
denied the motion, and the appellate court affirmed, stating that the officers were
not entitled to qualified immunity:
The facts, when viewed in a light most favorable to [the plaintiff],
show that [the decedent] was neither accused nor suspected of a crime
at the time of the incident, that Officer Fiorino tasered [him] at least
eight and as many as eleven or twelve times with each shock lasting at
least five seconds, that the officers made no attempt to handcuff or
arrest [him] at any time during or after any Taser shock cycle, that the
officer continued to administer Taser shocks to [the decedent] while
he was lying on the hot pavement, immobilized and clenched up, and,
finally, that these Taser shocks resulted in extreme pain and ultimately
caused [his] death.
The appellate court agreed with the trial court “that the force employed was so
utterly disproportionate to the level of force reasonably necessary that any
reasonable officer would have recognized that his actions were unlawful.”
Furtado v. Yun Chung Law, 51 So. 3d 1269 (Fla. 4th DCA 2011). A man
contacted the Sheriff’s Office because his wife “was in a ‘persistent severe
delusional and agitated state,’ had a ‘long history of severe depression,’ and had
been ‘walking around the house with knives.’” The Baker Act certificate stated that
the wife “‘essentially included everyone in her delusions system including her
husband and [the psychiatrist]’ and was ‘probably holding knives at the moment.’”
Three deputies responded, two with unholstered weapons and one with a Taser. In
searching the house for the wife they entered the bathroom, where she came at the
lead deputy with a knife raised over her head. The back-up deputy used his Taser
but apparently missed, resulting in the lead deputy firing his weapon, killing the
wife. The husband sued for a civil rights action under 42 U.S.C. § 1983, wrongful
death under Florida law, and a claim under the ADA. The trial court granted the
defendants’ motion for summary judgment, and the appellate court affirmed,
holding that exigent circumstances existed which the deputies did not create.
D. Weapons
Legal Note 2005-4, Miami-Dade Police Legal Bureau, May 5, 2005.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
418
Florida Statutes Section 933.14(3) states that no pistol or firearm
taken by any officer with a search warrant or without a search warrant
upon a view by the officer of a breach of the peace shall be returned
except pursuant to an order of a trial court judge. If a firearm was
seized pursuant to a search warrant, it cannot be returned without a
court order.
Breach of the peace is a generic term which includes disturbances of
public peace or order. In the context of Section 933.14(3) [it] also
includes behavior which would be a violation of law. Use of a firearm
or a threat or reference to use of a firearm would constitute a breach of
the peace. An incident which resulted in taking a person into custody
pursuant to the Baker Act would also constitute a breach of the peace.
As a general rule, when an officer impounds a firearm for safekeeping
only, this is an indication that no breach of the peace occurred. With
every case, review of the police report should indicate whether the
incident was a breach of the peace, and if the narrative so indicates,
the firearm should not be returned without a court order [see the AGO
below]. If the facts are unclear, questions concerning these elements
should be referred to the Police Legal Bureau.
Op. Att’y Gen. Fla. 09-04 (2009), confiscation and return of firearms by law
enforcement agencies when firearm owner subject to Baker Act evaluation. “In the
absence of an arrest and criminal charge against the person sent for evaluation
under the Baker Act, the Sheriff . . . may not retain firearms confiscated” at the
time of the event. “Baker Act proceedings are not criminal proceedings.” The
Attorney General suggested the sheriff seek legislation to address the problem.
VII. Responsibilities of and Lawsuits Against Doctors and Receiving Facilities
A. In General
Chirillo v. Granicz, 199 So. 3d 246 (Fla. 2016). The plaintiff Granicz’s wife, the
decedent, who had a history of depression, called her primary care doctor’s office,
reporting that she was under mental strain and having gastrointestinal problems.
Her physician, Dr. Chirillo, changed her antidepressant medication and referred her
to a gastroenterologist. His staff told the decedent she could pick up samples of the
medication and a prescription, but they did not schedule an appointment with Dr.
Chirillo. The decedent picked up the samples and prescription but hanged herself
and was found the next day. Granicz filed a medical malpractice lawsuit against

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
419
Dr. Chirillo, alleging that he breached a duty of care that resulted in the suicide.
The trial court granted Chirillo’s motion for summary judgment, finding that he
“did not have a duty to prevent the unforeseeable suicide.” But the appellate court
disagreed and reversed, and the Supreme Court approved the appellate decision,
stating that while the decedent was an outpatient of Chirillo’s and therefore “there
was no duty to prevent her suicide, . . . the nonexistence of one specific type of
duty does not mean that Dr. Chirillo owed the decedent no duty at all. . . .
Although the inpatient duty to prevent suicide does not apply here, there still
existed a statutory duty . . . to treat the decedent in accordance with the standard of
care. We find that the Second District properly evaluated the . . . case based on the
statutory duty owed to the decedent and also properly classified the foreseeability
of the decedent’s suicide as a matter of fact for the jury to decide in determining
proximate cause.”
Moses v. Providence Hosp. and Medical Centers, Inc., 561 F.3d 573 (6th Cir.
2009). A woman took her husband, who had severe psychiatric symptoms and had
“demonstrated threatening behavior, which made her fearful for her safety,” to a
hospital ER for severe psychiatric symptoms. A psychiatrist examined him several
times during his stay at the hospital and determined that he “was not ‘medically
stable from a psychiatric standpoint,’” and should be transferred to the hospital’s
psychiatric unit for reassessment. The psychiatrist’s order notes stated that the
psychiatric unit would accept the patient “if [his] insurance will accept criteria.”
But the patient was released instead of transferred, and ten days later he murdered
his wife. The plaintiff (the personal representative of the deceased wife’s estate)
sued the hospital and the psychiatrist under the Emergency Medical Treatment and
Active Labor Act (EMTALA), 42 U.S.C. § 1395dd, and for common law
negligence. The defendants filed a motion for summary judgment. The trial court
declined to exercise jurisdiction over the negligence claims and granted the motion
for summary judgment as to the EMTALA claim, stating that EMTALA
was not designed or intended to establish guidelines for patient care or
to provide a suit for medical negligence or malpractice. Under the
clear and unambiguous language of the statute, the Plaintiff’s claim
must be dismissed. The hospital admitted [the patient] and did not turn
him away, as was required. . . . The patient was undisputedly
completely screened, as the statute requires, even if on the basis of a
wrong diagnosis; and he was thereafter admitted to the Defendant
hospital, and no emergency medical condition was recognized on the
screening.
The appellate court affirmed as to the psychiatrist but reversed as to the hospital,

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
420
reiterating that “EMTALA requires hospitals to do more for patients with
emergency medical conditions than just admit them.” It “requires more than the
admission and further testing of a patient; it requires that actual care, or treatment,
be provided as well,” and the hospital did not satisfy the requirements under
EMTALA by merely screening the patient “and admitting him to conduct further
testing.”
The defendants argued that a rule promulgated by Centers for Medicare and
Medicaid Services (CMS), the agency responsible for implementing EMTALA,
effectively ends a hospital’s EMTALA obligations upon admitting an
individual as an inpatient. . . . According to the CMS regulation, “[i]f
a hospital has screened an individual under paragraph (a) of this
section and found the individual to have an emergency medical
condition, and admits that individual as an inpatient in good faith in
order to stabilize the emergency medical condition, the hospital has
satisfied its special responsibilities under this section with respect to
that individual.”
But the appellate court stated:
Although “[a]n agency’s construction of a statutory scheme that it is
entrusted to administer is entitled to a degree of deference .... we must
... ‘reject administrative constructions which are contrary to clear
congressional intent.’ ” . . . The CMS rule appears contrary to
EMTALA’s plain language, which requires a hospital to “provide ...
for such further medical examination and such treatment as may be
required to stabilize the medical condition.” . . . Although “treatment”
is undefined in the statute, it is nevertheless unambiguous, because it
is unreasonable to believe that “treatment as may be required to
stabilize” could mean simply admitting the patient and nothing
further. Moreover, the statute requires the patient to be “stabilized”
upon release; “[i]f an individual at a hospital has an emergency
medical condition which has not been stabilized ... the hospital may
not transfer the individual unless” the patient requests a transfer in
writing or a physician or qualified medical person certifies that the
risks of further treatment outweigh the benefits. . . . Therefore, a
hospital may not release a patient with an emergency medical
condition without first determining that the patient has actually
stabilized, even if the hospital properly admitted the patient. Such a
requirement would be unnecessary if a hospital only needed to admit

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
421
the patient in order to satisfy EMTALA.
The court also discussed what constitutes an “emergency medical condition” and
held, without “guidance from the legislative history,” that a mental health
emergency could qualify.
Moody v. Lawnwood Medical Center, Inc., 125 So. 3d 246 (Fla. 4th DCA 2013).
A child was injured in an playground accident, and her pediatrician diagnosed a
fractured hip and sent her to Lawnwood, where he had staff privileges. The
orthopedist on call concluded that the child did not have a hip fracture, and the
pediatrician discharged her. Her condition worsened, and her mother took her to
another hospital, where she was diagnosed with a fractured hip, septic arthritis,
septic shock, heart failure, MRSA, and infections throughout her body. Her parents
sued the pediatrician, the pediatrician’s clinic, the orthopedist, the orthopedist’s
practice, and Lawnwood, but signed releases as to all defendants but Lawnwood.
The trial court granted Lawnwood’s motion for summary judgment, holding that
the plaintiffs’ release of the two doctors released the hospital for vicarious liability
for the doctors’ negligence. But the appellate court reversed, noting that the
releases specifically stated that the hospital was not released and that all claims
against the hospital were preserved. In addition, there was an issue of fact as to
whether the hospital had a non-delegable duty to provide competent care to the
plaintiffs’ child; i.e., whether the mother had read and signed, “or otherwise
acquiesced to,” provisions in the hospital admission form “purportedly discharging
Lawnwood from liability for the acts of independent contractor physicians.”
Tuten v. Fariborzian, 84 So. 3d 1063 (Fla. 1st DCA 2012). The plaintiff Tuten’s
husband had been treated as an outpatient and as a voluntary inpatient, and after his
second suicide attempt the facility administrator filed a petition for involuntary
placement, supported by the psychiatrist. Before the involuntary placement
hearing, the husband requested release. The psychiatrist certified that the husband
was competent to provide consent, and the husband was released. The next day he
shot Tuten and fatally shot himself. Tuten brought a wrongful death/negligence
action against the psychiatrist and the mental health facility. The court dismissed it,
“noting that no amendment to the complaint could state a cause of action.” Tuten
appealed, arguing that under the Baker Act the facility and psychiatrist had a duty
to keep her husband in the facility until the trial court ruled on the petition for
involuntary placement. She also argued that they owed her husband a duty of care
that was breached when he was released. But the appellate court affirmed, holding
that the Baker Act does not
expressly provide that, once a petition for involuntary placement has

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
422
been filed, it cannot be withdrawn. In fact, a plain reading of section
394.469 would indicate that a petition could be withdrawn prior to a
ruling. Also, the grant by a court of a petition for involuntary
placement requires proof that a patient meets the criteria outlined in
section 394.467(1)(a) and (b), and the criteria must be established by
clear and convincing evidence. Since [the psychiatrist] concluded that,
in his professional opinion, [the patient] could determine for himself
whether commitment was necessary, there was no proof [the facility
or the psychiatrist] could offer in continuing support of a petition for
involuntary placement.
And because, for involuntary placement, the court must find that all available less
restrictive treatment alternatives are inappropriate, “[i]f a patient improves and is
able to function in an ‘available less restrictive environment’ then the State
has no alternative but to place the patient in that environment. To do
otherwise, would violate the constitutional rights of the patient as well as the plain
requirements of the Baker Act.”
The appellate court also noted that Florida law “does not impose a duty upon a
psychiatrist to hospitalize or otherwise involuntarily detain a patient.” It rejected
the argument that the facility and psychiatrist had a common law duty to keep the
husband committed against his will despite the psychiatrist’s opinion that he was
competent to make his own decision: “Because the ‘internal workings of the
human mind remain largely mysterious,’ to impose a general duty on a psychiatrist
would require such doctors to have the gift of ‘clairvoyance.’” The court also
stated: “It has been recognized that mental illness may be caused or intensified by
institutionalizing mental patients. Emerging from these roots, the science and
profession of psychiatry has burgeoned into a multifaceted social institution. The
practice of psychiatry is no longer limited to the institutionalization of the mentally
ill.”
The court also reiterated that case law establishes no duty to warn even if the
patient is dangerous and involuntarily committed. It noted “the unpredictability and
inexactness inherent in the practice of psychiatry. Thus, because the future
behavior of a psychiatric patient is unknowable, under Florida law risk of harm is
not foreseeable and therefore no duty exists to lessen the risk or protect others from
the type of risk which a psychiatric patient might pose.”
Estate of Smith v. Florida Dept. of Children and Families, 34 So. 3d 181 (Fla.
1st DCA 2010). The decedent, an employee at the Florida State Hospital in
Chattahoochee forensic unit, had a fatal heart attack after intervening in a

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
423
confrontation between an inmate and a co-worker. His estate brought a wrongful
death action alleging that DCF concealed and failed to disclose the criminal and
violent background of the inmate and that the decedent’s death was foreseeable.
The trial court dismissed the lawsuit as barred by sovereign immunity, and the
appellate court affirmed.
Wax v. Tenant Health System Hospitals, Inc., 955 So. 2d 1 (Fla. 4th DCA 2007).
The plaintiff’s husband died during surgery, and she sued the hospital and surgeon.
The trial court granted the defendants’ motion for summary judgment, after
stopping the plaintiff’s experts from testifying as to certain issues, holding that
“such testimony would have been outside the designations of these expert
witnesses in the pretrial disclosure, or it would have been cumulative.” The
appellate court disagreed and reversed, stating that
both a statutory and a contractual basis for the hospital’s duty of
providing non-negligent, competent surgical anesthesia services to its
patient. Under the admission consent form, we find that the patient
consented to the Group’s administration of anesthesia services. . . .
[H]owever, we find no language at all in this form that might fairly
and reasonably be construed to stand as an agreement to discharge the
hospital from its primary statutory and contractual duty of providing
non-negligent anesthesia services. If there were negligence in the
provision of anesthesia services, then the Hospital would be liable as a
matter of law.
Sweet v. Sheehan, 932 So. 2d 365 (Fla. 2d DCA 2006). After sustaining “severe
neurological damage as a result of a failed suicide attempt,” Sweet sued his
psychiatrist for medical malpractice. He alleged that after he told his psychiatrist
about the attempt to overdose, his psychiatrist was negligent by “(1) failing to
appropriately recognize and treat Sweet’s severe depression, (2) failing to
recommend to Sweet and his family that Sweet needed immediate hospitalization
after his [previous] suicide attempt, (3) failing to adequately inform Sweet and his
family of the risks of not being hospitalized, and (4) failing to appropriately
monitor the amount of medication prescribed.” The trial court granted the
psychiatrist’s motion for summary judgment, holding that the psychiatrist “owed
no duty to Sweet and that there was no causal connection between [his] alleged
negligence and Sweet’s injuries.” But the appellate court reversed and remanded,
holding that the psychiatrist had not shown “conclusively the absence of any
genuine issues of material fact.” It stated that “Florida law unquestionably
recognizes that physicians owe their patients a duty to ‘use the ordinary skills,
means and methods that are recognized as necessary and which are customarily

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
424
followed in the particular type of case according to the standard of those who are
qualified by training and experience to perform similar services in the community
or in a similar community.’”
Lawlor v. Orlando, 795 So. 2d 147 (Fla. 1st DCA 2001). After the decedent
committed suicide, his estate sued his psychotherapist for negligence. The trial
court granted final summary judgment in favor of the psychotherapist, finding that
“the suicide of a former patient was not sufficiently foreseeable to impose a duty
under the circumstances of this case.” The appellate court affirmed, holding that
“[a]lthough Florida law would clearly impose a duty on a psychotherapist for
failure to safeguard a patient from harming himself in a custodial setting, . . . no
Florida cases extend the duty of custodial supervision and care to the outpatient
relationship between a psychotherapist and a patient.” However, in Granicz v.
Chirillo, 147 So. 3d 544 (Fla. 2d DCA 2014), the Second District Court of Appeal
reversed a summary judgment in favor of the physician and certified conflict with
Lawlor. It stated:
As did the trial court in this case, the First District [in Lawlor]
determined that the psychotherapist did not have a legal duty to
prevent the patient’s suicide because the suicide was unforeseeable.
. . . And the appellate court rejected the plaintiff’s expert testimony
setting forth the applicable standard of care, how it was breached, and
how the breach proximately caused the patient’s suicide. . . . For the
reasons set forth above, we disagree with the Lawlor court’s
description of the psychotherapist’s legal duty as a duty to prevent the
patient’s suicide. Instead, we agree with . . . the dissent that the
psychotherapist had a “duty to provide ‘appropriate psychotherapy’ ”
and that the plaintiff’s expert affidavit precluded summary judgment.
. . . [The dissenting judge in Lawlor] correctly noted that because a
legal duty existed, the issue of whether the doctor’s actions
proximately caused the plaintiff’s suicide was to be resolved by a jury.
. . . Similarly in this case, based on the record evidence, a jury
question remains as to the proximate cause issue.
The Florida Supreme Court granted conflict review in Chirillo v. Granicz, 168 So.
3d 224 (Fla. 2014), and heard oral argument on September 2, 2015.
Garcia v. Lifemark Hospitals of Florida, 754 So. 2d 48, 49 (Fla. 3d DCA 2000).
The decedent was admitted to the hospital after a crash. Before the physical
workup was complete, he requested release and was released against medical
advice. Once home, he committed suicide. His estate sued the hospital and ER

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
425
staff, alleging that the police report “should have put the hospital on notice that the
accident was a suicide attempt.” The trial court dismissed the action, and the
appellate court affirmed, stating:
Doctors do not have a duty to treat each of their patients for every
conceivable medical condition that they might have. For example, if a
person goes to an ophthalmologist because they have an eye infection,
one could hardly contend that there is a duty for the doctor to
diagnose and treat that patient for hemorrhoids. Likewise, it is even
more difficult to argue that this doctor has a duty to diagnose and treat
that patient for obsessive compulsive disorder. Imposing such a duty
takes us down the path of clairvoyance. . . because of the nature of
psychiatry.
Santa Cruz v. Northwest Dade Community Health Center, Inc., 590 So. 2d 444
(Fla. 3d DCA 1991). Police took Santa Cruz to the hospital “pursuant to an ex
parte court order describing him as violent and delusional.” He was transferred to
another hospital, from which he escaped, and returned to the first hospital about
two weeks later and began outpatient treatment there. A few weeks later he shot his
brother and another person, and they sued the hospital. The trial court dismissed
their case for failure to state a cause of action, and the appellate court affirmed,
stating: “This was a correct ruling by the trial court. There is no recognized basis
for these appellants to assert a third party claim against the medical facility. They
were not patients of the medical staff at Northwest Dade nor did they fit into any
exception to the physician/patient requirement. Thus, it is clear there was no
special relationship between Northwest Dade and the appellants which would
support a claim for medical malpractice.” On appeal the plaintiffs had argued that
the hospital had a duty to detain or hospitalize Santa Cruz under the circumstances,
but the court disagreed because Santa Cruz was not in its custody.
Paddock v. Chacko, 522 So. 2d 410 (Fla. 5th DCA 1988). The plaintiff sustained
injuries after her failed suicide attempt. She sued a psychiatrist whom she had seen
once, four days before her suicide attempt, and who had recommended
hospitalization, but the plaintiff’s father did not consent and the recommendation
was rejected. A jury awarded her $2,150,000, but the trial court granted the
defendant’s motion for judgment NOV/new trial. The plaintiff appealed, but the
DCA affirmed, holding that “the existence of a legal duty was a question of law for
the court and not for the jury,” and “the trial court determined that the law did not
impose a legal duty on a psychiatrist to involuntarily take a patient into his
custody; that he was not legally obligated (nor empowered) to take control of her
life away from her against her will to protect her from her self-destructive

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
426
tendencies.”
There was also testimony that the increased dosage of Navane that the psychiatrist
prescribed was inadequate, but there was no testimony that, even if it was, it was a
proximate cause of the plaintiff’s injuries.
While a facility may have liability based on “the negligent failure to safeguard and
protect a psychiatric patient with suicidal tendencies,” such cases involve patients
who were already committed to the custody of the facility. But the appellate court
“found no case that has held a doctor liable for the failure to take his patient into
custody. Under the circumstances and facts of this case, we are unwilling to extend
the duty of custodial supervision and care to the out-patient relationship between a
psychiatrist and a patient.”
Op. Att’y Gen. 93-88 (1993), Florida Volunteer Protection Act. Volunteers for
nonprofit organizations who receive a stipend (other than reimbursement of actual
expenses) are not covered by the Florida Volunteer Protection Act.
Op. Att’y Gen. 73-220 (1973), Responsibility of Admitting Physician in
Receiving Facility. “The admitting physician in a receiving facility is responsible
for the care of any person eligible to be admitted to the receiving facility and must
make a good faith effort to comply with the provisions of the Florida Mental
Health Act and the guidelines by the [responsible agency] in the administering of
care to such eligible individuals until the receiving facility’s overload is eased or a
transfer of the patient to another receiving facility is accomplished.”
B. Duty to Warn
Nova University, Inc. v. Wagner, 491 So. 2d 1116 (Fla. 1986). Nova University
ran a residential rehabilitation center for children with behavior problems. The
children were not allowed to leave without permission, but two residents who
“exhibited a propensity toward physical violence” ran away and killed a four-year-
old and injured a six-year-old. The victims’ mother sued Nova, and the trial court
granted the defendants’ motions for summary judgment, “finding that as a matter
of law they owed no duty to the plaintiffs.” The appellate court reversed, “finding
that the Center stood in loco parentis to its residents and that the proper application
of that theory precluded summary judgment for the defendants,” and certified the
following question: “DOES KNOWLEDGE OF A CHILD’S VIOLENCE
REQUIRE A PARENT TO EXERCISE CONTROL TO AVOID INJURY TO
ANOTHER CAUSED BY SUBSEQUENT VIOLENCE WHICH IS MORE
SEVERE?”

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
427
The Supreme Court restated the question as: “Does a child care institution that
accepts as residents delinquent, emotionally disturbed and/or ungovernable
children have a duty to exercise reasonable care in its operation to avoid harm to
the general public?” and answered in the affirmative, stating that the center “for a
fee, undertakes to rehabilitate children with emotional and behavior problems. We
do not think it too onerous a burden to place upon it the duty to exercise reasonable
care in carrying out its efforts.” It approved the appellate court decision.
O’Keefe v. Orea, 731 So. 2d 680 (Fla. 1st DCA 1998). The plaintiff was a
psychiatric nurse at Charter Hospital, which had recently admitted, as a transfer
from another hospital, a schizophrenic patient who had a history of violence and
making threats. While being escorted to seclusion by the plaintiff and two male
staff members, the patient hit the plaintiff in the back of the head, and she
“apparently suffered a moderate degree of brain damage.” The plaintiff sued,
among others, Mental Health Care (MHC), which had previously treated the
patient, based on vicarious liability, and alleged, among other claims, that the
patient’s clinical case manager at MHC was negligent for failing to inform staff at
Charter about the patient’s “potential for violence.” The trial jury awarded the
plaintiff $901,415.72, assigning no negligence to the plaintiff or any of the Fabre
defendants. But the appellate court reversed, stating that “a case manager at a
community mental health facility who has provided non-custodial mental health
care for a client has no duty to warn the nursing staff at a psychiatric hospital that
the client may be dangerous when the client is admitted to the hospital as a result
of a Baker Act proceeding initiated by a third party.”
Mental Health Care, Inc. v. Stuart, 909 So. 2d 371 (Fla. 2d DCA 2005). Four
days after being released from the hospital, a 17-year-old patient attacked his
parents, who were also patients of his psychiatrist, killing the father. The mother
sued the psychiatrist and his P.A. for medical malpractice. The trial court
dismissed the complaint for failure to state a cause of action, but the appellate court
reversed, stating that “when the prevailing standard of care creates a duty that is
obviously for the benefit of certain identified third parties and the physician knows
of the existence of those third parties, then the physician’s duty runs to those third
parties.” It also noted that the duty to warn “derives from the fiduciary relationship
between [the psychiatrist] and the parents of his minor patient, as well as the
physician-patient relationship between [the psychiatrist] and [the parents].”
Green v. Ross, 691 So. 2d 542 (Fla. 2d DCA 1997). The appellate court affirmed
the trial court order dismissing for failure to state a cause of action a complaint
against a mental health worker. The appellate court agreed with and relied on
Boynton v. Burglass, 590 So. 2d 446 (Fla. 3d DCA 1991) (see below), and rejected

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
428
the argument that “the permissive language of section 491.0147 created an
affirmative duty to warn so as to support a cause of action for a failure to warn.”
Liles v. P.I.A. Medfield, Inc., 681 So. 2d 711 (Fla. 2d DCA 1995). “[I]nvoluntary
commitment procedures do not involve the rendering of medical care or services.
Although a medical diagnosis is necessary in order to involuntarily commit a
patient, the process of complying with the statute does not require medical skill or
judgment.” Therefore, a guardian filing suit against a hospital and doctor for false
imprisonment did not have to comply with the medical malpractice presuit
screening requirements and his complaint should not have been dismissed.
Boynton v. Burglass, 590 So. 2d 446 (Fla. 3d DCA 1991). The court declined to
adopt the rule in Tarasoff v. Regents of University of California, 551 P.2d 334
(Cal. 1976), that “a psychiatrist who allegedly ‘knows, or should know,’ that a
patient of his presents a serious threat of violence to a third party has a duty to
warn the intended victim.” Instead it held that there is no such duty and affirmed
the trial court order dismissing the complaint for failure to state a cause of action.
It stated that to impose such a duty “is neither reasonable nor workable and is
potentially fatal to effective patient-therapist relationships.”
Op. Att’y Gen. 2006-36 (2006), regarding sovereign immunity of a nonprofit
corporation. When a county health foundation “is acting primarily as an
instrumentality” of the county hospital board “for purposes of section 768.28,
Florida Statutes, [it] would appear to be subject to the sovereign immunity
provisions of that section.”
C. Malpractice vs. Ordinary Negligence
Shands Teaching Hosp. and Clinics, Inc. v. Estate of Lawson ex rel. Lawson,
175 So. 3d 327 (Fla. 1st DCA 2015). Lawson had been admitted to Shands’
psychiatric hospital. She took an employee’s keys and escaped, and was killed by a
truck on a nearby highway. Her estate sued Shands, and Shands filed a motion to
dismiss, arguing that the complaint was actually for medical negligence and the
estate had not complied with mandatory presuit requirements for such actions. The
trial court denied the motion, but the appellate court quashed the order denying the
motion, concluding that “because the claim arises from the services and care
Shands was giving to a patient in a locked psychiatric unit, the complaint alleges
medical negligence under section 766.106(1)(a), Florida Statutes.”
Pierrot v. Osceola Mental Health, 106 So. 3d 491 (Fla. 5th DCA 2013). The
appellate court reversed a trial court order dismissing with prejudice a wrongful

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
429
death action for failure to comply with Florida’s medical malpractice presuit
requirements. The complaint alleged violations of the deceased patient’s rights
under the Baker Act, not medical malpractice, and therefore the plaintiff did not
have to comply with the medical malpractice presuit requirement. Further, the
facility was not a health care provider.
Southern Baptist Hosp. of Florida, Inc. v. Ashe, 948 So. 2d 889 (Fla. 1st DCA
2007). The trial court found that the plaintiff did not need to comply with the
medical malpractice presuit requirements because the “cause of action did not
sound in medical malpractice, but instead in ordinary negligence.” The defendant
sought review, but the appellate court denied review, agreeing with the trial court.
It noted that the complaint did not “challenge any medical diagnosis or decision
that required professional skill or judgment.”
Doe v. HCA Health Services of Florida, Inc., 640 So. 2d 1177 (Fla. 2d DCA
1994). A Baker Act patient’s mother sued the receiving doctors and hospitals that
treated him, “alleging false imprisonment, malicious prosecution, negligent hiring
and failure to train, assault and battery, misrepresentation, and intentional infliction
of emotional distress.” The trial court dismissed her lawsuit for failure to comply
with the medical malpractice presuit requirements, and the appellate court
affirmed, stating that each of the allegations “arose out of the rendering of medical
care by licensed health care providers subject to the prevailing professional
standard of care, and compliance . . . was required.”
VIII. Guardianship and Protective Services
Auxier v. Jerome Golden Center for Behavioral Health, 85 So. 3d 1164 (Fla. 4th
DCA 2012). A magistrate had discharged the public defender’s office in a Baker
Act case because the person who was the subject of the proceedings had a plenary
guardian, and her rights had been transferred to her guardian and counsel for the
guardian would represent her. The person was not present at the hearing on which
the order was based and did not have independent counsel, and she was
involuntarily committed. The public defender’s office sought review of the order
discharging it from representing her, and the Fourth District Court of Appeal
granted it and quashed the discharge and commitment orders. It held that “the
magistrate and the circuit court departed from the essential requirements of law
[which] requires appointment of the public defender’s office to represent the
patient in involuntary civil commitment proceedings ‘unless the person is
otherwise represented by counsel.’ The guardian’s attorney represents the
guardian, not the ward.” The court “agree[d] with the First District’s discussion of
the role of the public defender in Baker Act proceedings” in Handley v. Dennis

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
430
(see below).
Handley v. Dennis, 642 So. 2d 115 (Fla. 1st DCA 1994). The court defined the
role of the public defender in involuntary placement proceedings:
The Public Defender has a duty under the law to represent
indigent mental patients in hearings to determine the need for
continued involuntary placement. . . . In such cases, the duty of the
Public Defender is a legal and professional duty that is owed to the
patient as a client. The Public Defender serves as an independent
advocate for the patient, not as a neutral party charged with the
responsibility of determining the best interests of the patient or the
needs of society.
. . . . If the patient wishes to be released or transferred and if there is a
basis for that request, the Public Defender has a duty to advocate the
cause of the patient.
The court also stated that when there is a conflict between guardianship law and
the Baker Act, “both the duty of the guardian and the power of the circuit court in
the guardianship proceeding must give way to the ward’s rights under the Baker
Act to be released to a less restrictive environment,” and “if a ward must be moved
to a facility outside the circuit to accommodate a ruling in a Baker Act proceeding,
the Public Guardian need only to file a motion to withdraw and transfer the
guardianship case to the appropriate circuit,” and the circuit judge in the circuit to
which the ward has been transferred will appoint a successor guardian.
DCF General Counsel Opinion regarding which substitute decision maker
controls approval of a treatment plan presented by a facility (January 28,
2000). DCF concluded that the appropriate order of deference should be the
guardian advocate, legal guardian, health care surrogate, and the proxy.
[T]he Legislature has recognized that the patient, to the extent that he
is able to do so, is responsible for, and should be allowed to exercise
control over, his own health care decisions. Guardian advocates,
health care surrogates, health care proxies, and legal guardians should
be considered as substitute consent givers only after it has been
determined that the patient is unable to consent for himself, whether
for reasons of mental incompetence or physical disability.
* * *

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
431
The guardian advocate is appointed when a patient has specifically
been found to be incompetent to consent to treatment pursuant to . . .
the Baker Act. The guardian, on the other hand, although also
appointed by the court, is appointed because the principal has been
adjudicated “incapacitated” as that term is defined in Chapter 744 and
not as the result of having been determined “incompetent to consent to
treatment.”
* * *
There can be no question that the use of a substitute consent giver is to
be undertaken only with a high degree of assurance that the patient’s
rights will be protected. It must be remembered, however, that it is the
court which acts as the impartial protector of individual rights, civil
liberties and due process. Therefore, court involvement assures to the
fullest extent possible that these decisions will be accomplished
within the parameters of due process and with adequate protection of
the patient’s individual rights.
* * *
[B]ecause the court appoints a guardian advocate with assistance in
making mental health care decisions specifically in mind, . . . the
greatest deference should be given to the guardian advocate in
determining who should approve the treatment plan when the patient
cannot do so for himself. Thereafter the person . . . referred to as the
“legal guardian”, assuming that the ability to make mental health care
decisions is included within the court’s order appointing a person to
that office, should be next in order of priority. The court involvement
in appointing each of these substitute consent givers is significantly
persuasive in coming to this conclusion.
. . . [N]ext in order of precedence should be the mental health care
surrogate and then the health care surrogate. It is these two in that
order, who are most likely to make the decisions which offer the
greatest protection to the patient. The proxy, who can be appointed by
someone other than the patient, then falls to the rank of the least
reliable of all the substitute consent givers.
IX. Baker Act and Minors
Parham v. J. R., 442 U.S. 584, 99 S.Ct. 2493, 61 L.Ed.2d 101 (1979). A class

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
432
action based on 42 U.S.C. § 1983 was brought on behalf of children being treated
in a Georgia state mental hospital, which “sought a declaratory judgment that
Georgia’s voluntary commitment procedures for children under the age of 18 . . .
violated the Due Process Clause of the Fourteenth Amendment and requested an
injunction against their future enforcement.” The federal district court held that the
statutory procedures were unconstitutional and violated due process rights. It
enjoined future commitments based on the procedures and ordered Georgia to
spend whatever was “reasonably necessary” to provide appropriate nonhospital
treatment for the plaintiffs, and held that due process “includes at least the right
after notice to be heard before an impartial tribunal” and that “a judicial or quasi-
judicial body should review voluntary commitment decisions.” The state
Department of Human Resources and its commissioner appealed.
The U.S. Supreme Court stated that the basic issues were “what process is
constitutionally due a minor child whose parents or guardian seek state
administered institutional mental health care for the child and specifically whether
an adversary proceeding is required prior to or after the commitment,” and it
reversed and remanded. It stated:
Although we acknowledge the fallibility of medical and
psychiatric diagnosis, . . . we do not accept the notion that the
shortcomings of specialists can always be avoided by shifting the
decision from a trained specialist using the traditional tools of medical
science to an untrained judge or administrative hearing officer after a
judicial-type hearing. Even after a hearing, the nonspecialist
decisionmaker must make a medical-psychiatric decision. Common
human experience and scholarly opinions suggest that the supposed
protections of an adversary proceeding to determine the
appropriateness of medical decisions for the commitment and
treatment of mental and emotional illness may well be more illusory
than real. . . .
Another problem with requiring a formalized, factfinding
hearing lies in the danger it poses for significant intrusion into the
parent-child relationship. Pitting the parents and child as adversaries
often will be at odds with the presumption that parents act in the best
interests of their child. It is one thing to require a neutral physician to
make a careful review of the parents’ decision in order to make sure it
is proper from a medical standpoint; it is a wholly different matter to
employ an adversary contest to ascertain whether the parents’
motivation is consistent with the child’s interests.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
433
Moreover, it is appropriate to inquire into how such a hearing
would contribute to the successful long-range treatment of the patient.
Surely, there is a risk that it would exacerbate whatever tensions
already exist between the child and the parents. . . .
Although our review of the record in this case satisfies us that
Georgia’s general administrative and statutory scheme for the
voluntary commitment of children is not per se unconstitutional, we
cannot decide on this record, whether every child in appellees’ class
received an adequate, independent diagnosis of his emotional
condition and need for confinement under the standards announced
earlier in this opinion. On remand, the District Court is free to and
should consider any individual claims that initial admissions did not
meet the standards we have described in this opinion.
In addition, we note that appellees’ original complaint alleged
that the State had failed to provide adequate periodic review of their
need for institutional care and claimed that this was an additional due
process violation. Since the District Court held that the appellees’
original confinement was unconstitutional, it had no reason to
consider this separate claim. Similarly, we have no basis for
determining whether the review procedures of the various hospitals
are adequate to provide the process called for or what process might
be required if a child contests his confinement by requesting a release.
These matters require factual findings not present in the District
Court’s opinion. We have held that the periodic reviews described in
the record reduce the risk of error in the initial admission and thus
they are necessary. Whether they are sufficient to justify continuing a
voluntary commitment is an issue for the District Court on remand.
The District Court is free to require additional evidence on this issue.
The majority opinion concluded by stating: “Georgia’s medical factfinding
processes are reasonable and consistent with constitutional guarantees.
Accordingly, it was error to hold unconstitutional the State’s procedures for
admitting a child for treatment to a state mental hospital.”
In re Amendments to the Florida Rules of Juvenile Procedure, 952 So. 2d 517
(Fla. 2007). The Florida Supreme Court refused to adopt a rule change that would
require that a guardian ad litem and attorney ad litem be appointed for children
under state care when judges decide whether the children should be given
psychotropic medication without parental permission. The court stated that section

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
434
39.407(3), Florida Statutes, imposes “detailed requirements” on DCF when it
“seeks a medical evaluation to determine the need for psychotropic medication for
a child,” and “[t]he court is also authorized to order additional medical consultation
and to require the department to obtain a second opinion.” Statutes and rules exist
“to ensure that the court’s ruling on the motion for court authorization to
administer the medication is based upon the most complete medical information
that is available.”
The court also noted that “in most cases, children in the custody and care of the
department should already have representation in the form of a guardian ad litem.”
And the court already has discretion to appoint such representation for children in
such cases.
M.W. v. Davis, 756 So. 2d 90 (Fla. 2000). The Florida Supreme Court stated that
all the parties “agree that section 39.407(4) requires dependency courts to comply
with the procedures outlined in the Baker Act prior to placing a child who has been
taken into emergency shelter into a residential mental health treatment facility” and
that “a hearing before a judge is required before a child who has been adjudicated
dependent may be placed by the [DCF] into a residential mental health treatment
facility against the child’s wishes. At issue, however, is whether that hearing must
comply with the procedural requirements of the Baker Act, the factors to be
considered by the dependency court, and whether evidence should be allowed.”
The Fourth District Court of Appeal had certified the following question:
IS A HEARING WHICH COMPLIES WITH THE
REQUIREMENTS OF SECTIONS 39.407(4) AND 394.467(1),
FLORIDA STATUTES, NECESSARY WHEN A COURT ORDERS
THAT A CHILD BE PLACED IN A RESIDENTIAL FACILITY
FOR MENTAL HEALTH TREATMENT, WHERE THE CHILD
HAS BEEN COMMITTED TO THE LEGAL CUSTODY OF THE
DEPARTMENT OF CHILDREN AND FAMILY SERVICES, AND
THE DEPARTMENT IS SEEKING RESIDENTIAL TREATMENT?
The Florida Supreme Court answered in the negative. It held that the Florida
Legislature intended for the Baker Act procedures to apply only to children who
have been placed in emergency shelter and not to children who have been
adjudicated dependent and placed in the temporary legal custody of DCF and who
are in need of mental health treatment. It also cited the GAL program of the
Eleventh Judicial Circuit, which “advocates that proper procedures exercised by
the dependency courts will better assure the child’s safety and mental health than

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
435
the procedures required by the Baker Act,” which would limit the placing of a
dependent child into residential psychiatric treatment only when “the child is so
disturbed that the child meets the criteria of being manifestly incapable of
surviving alone or dangerous.”
The court further noted: “The judge was already familiar with M.W. and had
reviewed his case at several hearings in the months preceding his placement,” and
“[a]lthough the dependency judge did not hold an evidentiary hearing before
placing M.W. in [the locked facility], she did recognize the need for an evidentiary
hearing and scheduled one for a date six weeks in the future. Accordingly, the
procedure followed . . . satisfied minimum constitutional due process
requirements.”
K.D. v. Department of Juvenile Justice, 694 So. 2d 817 (Fla. 4th DCA 1997).
The appellate court held that section 394.467(2), Florida Statutes, is inapplicable
when determining whether a delinquent juvenile is incompetent to proceed to trial
on a delinquency petition and whether a delinquent juvenile should be
involuntarily hospitalized by a juvenile judge. It upheld the trial court’s order
committing the child to DCF for placement in a residential program, holding that a
determination of involuntary commitment of a juvenile pursuant to section
39.0517(2), Florida Statutes (1996) (see current section 985.19), is analogous to a
determination of competency of an adult pursuant to Fla. R. Crim. P. 3.210–3.212,
which — unlike section 394.467(2) — require the appointment of “experts” to
examine the juvenile/defendant and not the receipt of a psychiatrist’s testimony or
report (which is needed to involuntarily place a patient in a treatment facility).
Department of Health and Rehabilitative Services v. A.E., 667 So. 2d 429 (Fla.
2d DCA 1996). The trial court found the 10-year-old child incompetent to proceed
to trial and ordered him committed to DCF for placement in a mental health
treatment facility pursuant to section 916.13, Florida Statutes. DCF appealed, the
minor’s counsel conceded error, and the appellate court reversed and remanded for
further proceedings under sections 39.046 (now 985.224), 394.467, and 393.11,
holding that the juvenile court did not have jurisdiction to order the involuntary
commitment under section 916.13(2) of a child alleged to be delinquent.
Department of Health and Rehabilitative Services v. State, 655 So. 2d 227 (Fla.
5th DCA 1995). The appellate court held that the juvenile court lacks the power to
order the involuntary placement of minors who are alleged to be delinquent under
section 916.13, Florida Statutes. It determined that section 916.13 specifically set
forth “procedure for court-ordered involuntary commitment of adult offenders
found incompetent to stand trial or to be sentenced” and did not apply to juvenile

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
436
delinquents. It reversed and remanded for further proceedings.
Department of Health and Rehabilitative Services v. V.L., 583 So. 2d 765 (Fla.
5th DCA 1991). The appellate court held that the circuit court had jurisdiction to
place a foster child in a long-term residential treatment facility at HRS cost but
could not place a limitation on how much time HRS would have in order to come
up with the money. HRS can provide the placement to the child only when funds
become available.
State, Dept. of Health and Rehabilitative Services v. Brooke, 573 So. 2d 363 (Fla.
1st DCA 1991). Two juvenile court judges ordered the Secretary of HRS to appear
at hearings regarding the status of dependent children who had been committed to
HRS custody, to explain why HRS did not have sufficient funding to place the
children in residential treatment facilities. The appellate court reversed the orders,
noting that “budgetary decision-making is strictly within the secretary’s executive
discretion,” and “the secretary’s appearance or non-appearance could not lead to
the disclosure of any facts upon which the judges would have jurisdiction to act or
against which to issue an order to show cause. The judges were therefore clearly
without jurisdiction to require the secretary’s appearance regarding his transfer of
monies or his making of budgetary decisions.”
HRS also claimed that the judges’ orders interfered with its “executive discretion
concerning the placement of dependent children in derogation of the doctrine of
separation of powers,” but the appellate court stated that “simply because the trial
court cannot order a child to be placed in a specific institution does not necessarily
preclude the court from placing other conditions on the exercise of the
Department’s discretion to place the child.” It was clear that in one case the judge
only directed that HRS
place the child “in available placement as recommended” by the
[Case Review Committee]. No order for placement in a specific
institution was made . . . and the language arguably is consistent with
the discretionary authority granted to the Department pursuant to
section 394.4781, insofar as the order may be interpreted so that the
Department need not place the children as recommended by the CRC
if there are neither funds nor facilities available. Thus, this particular
portion of the . . . orders under review . . . do not necessarily
contravene the statutory scheme. . . in derogation of the doctrine of
separation of powers.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
437
X. Baker Act and Criminal Defendants
Thomas v. Bryant, 614 F.3d 1288 (11th Cir. 2010). Ten Florida State Prison
inmates brought a § 1983 action against officers and employees of the Florida
Department of Corrections, “alleging that the use of chemical agents on inmates
with mental illness and other vulnerabilities violates the Eighth Amendment’s
prohibition on cruel and unusual punishment.” The plaintiffs settled their claims
against the individual corrections officers, and a trial was held on the claims for
declaratory judgment and injunctive relief against the Secretary of DOC and the
prison warden. The federal district court entered judgment in favor of two of the
remaining six plaintiffs, concluding that they had “demonstrated that at times in
which they were sprayed with chemical agents they were unable to conform their
behavior to prison standards due to their mental illnesses such that the DOC’s use
of force for purposes of prison discipline amounted to cruel and unusual
punishment.” The district court permanently enjoined the defendants “from
allowing the non-spontaneous use of chemical agents [on the two plaintiffs]
without first consulting with the DOC’s trained mental health staff to evaluate their
mental health status.” The defendants appealed, and the federal circuit court
affirmed, stating: “Although it is well-established that the use of chemical agents
on recalcitrant prisoners is not per se unconstitutional, . . . there are constitutional
boundaries to its use. . . . We agree with the district court that ‘if the DOC fails to
account for an inmate’s decompensation, with the result that he is gassed when he
cannot control his actions due to his mental illness, then the force no longer has a
necessary penological purpose and becomes brutality.’” The circuit court also
agreed with the district court that
the “lasting psychological injuries” suffered by [the plaintiff] as a
result of his subjection to repeated chemical sprayings at FSP are
sufficiently serious injuries to satisfy the objective harm requirement.
[He] need not have suffered lasting physical injury from the sprayings
to subject DOC conditions to 8
th
Amendment scrutiny. The case law
establishes that “mental health needs are no less serious than physical
needs” for purposes of the 8
th
Amendment. Accordingly, the court
held that the policy and practice of spraying inmates with chemical
agents, when fully secured in a cell and not presenting a threat of
immediate harm to himself or others, and when unable to understand
and comply with officers’ orders due to mental illness—are extreme
deprivations violating the “broad and idealistic concepts of dignity,
civilized standards, humanity and decency” embodied in the 8
th
Amendment.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
438
Onwu v. State, 692 So. 2d 881 (Fla. 1997). A county court had found the
defendant in a misdemeanor case incompetent and entered an order of
commitment. The defendant filed a petition for habeas corpus, and the chief circuit
judge, in his appellate capacity, directed the defendant’s release, holding that
“although the county court had inherent authority to determine issues of
competency, it did not have the authority to commit mentally incompetent
persons” to HRS. The judge then issued an administrative order that “assigned all
of the county judges of the Seventeenth Judicial Circuit to act as circuit judges for
the purpose of determining the competency of any person who may appear within
the courts of Broward County, Florida, and thereafter entering a proper order of
commitment.” The county judge presiding over the defendant’s criminal case
found him incompetent and ordered a commitment hearing, and the defendant filed
a petition for prohibition, to stop the commitment proceedings. He argued that
because under section 916.106, Florida Statutes, “court” means the circuit court,
only the circuit court can make the findings necessary for a forensic commitment.
The Florida Supreme Court agreed and declared the administrative order invalid.
Perkins v. State, 84 So. 3d 336 (Fla. 2d DCA 2012). The appellate court
concluded that
the probate court erred in ruling that the doctrine of collateral estoppel
precluded it from determining whether Mr. Perkins met the criteria for
civil commitment. . . . [N]o one presented any evidence at the hearing
in the criminal proceeding to establish that Mr. Perkins met the civil
commitment criteria. Thus the record doesn’t establish that the facts
supporting [his] commitment in the criminal proceedings are the same
and based upon the same evidence presented in the probate
proceedings.
The court also noted that it was not shown that that Perkins
affirmatively waived his right to be present at a hearing to determine
whether he met the criteria for civil commitment. . . . The defense
attorney’s primary goal in the . . . criminal proceeding was to obtain a
dismissal of the criminal charges based upon Mr. Perkins’ continued
incompetence to proceed to trial. There is no support in the record for
the proposition that Mr. Perkins should be bound by any
determination of his mental status resulting from a hearing at which
everyone stipulated to the dismissal of the criminal proceeding.
A.E. v. State, 83 So. 3d 1000 (Fla. 3d DCA 2012). A.E. was charged with

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
439
aggravated battery and found incompetent, and appealed the involuntary civil
commitment judgment. The appellate court affirmed, finding competent substantial
evidence to support the commitment:
A.E . . . has remained incompetent with no substantial probability that
she will become competent to stand trial in the foreseeable future.
A.E. suffers from schizophrenia and is paranoid. Despite taking her
medications, when evaluated just prior to the hearing conducted by
the trial court, A.E. was agitated, exhibited “unusual gestures,” was
easily distractible, had difficulty focusing, was seen responding to
voices, and at times appeared disorganized, unable to express herself
in a rational manner, and delusional. A.E. has a long history of mental
illness, perceptual disturbances, substance abuse, numerous
hospitalizations, and non-compliance with treatment and medication.
The trial court additionally noted that A.E. has poor insight as to her
condition and mental health needs, she had to be placed on suicidal
precautions approximately two weeks prior to the hearing, and
numerous attempts to place her in the community have failed.
Johnson v. State, 40 So. 3d 883 (Fla. 4th DCA 2010). The 37-year-old defendant
was convicted of lewd or lascivious battery based on his relationship with a 13-
year-old girl. He appealed, arguing that “the trial court erred by admitting evidence
that the victim twice attempted to commit suicide [and was Baker Acted] after the
relationship was revealed and the defendant was arrested.” The appellate court
reversed and remanded for a new trial “[b]ecause any probative value of this
evidence was substantially outweighed by the danger of unfair prejudice, and the
error in admitting it was not harmless.”
Amador v. State, 712 So. 2d 1179 (Fla. 3d DCA 1998). In 1984 Amador was
charged with multiple crimes, including the murder of his mother. The trial court
found him incompetent to stand trial and committed him to HRS custody. Seven
years later the trial court dismissed the charges without prejudice, “finding that
there was no substantial probability that he would regain mental competency in the
foreseeable future,” and committed him again, retaining jurisdiction and ordering
that he not be released without court approval. Two years after that, because of a
lack of hospital space, Amador was transferred from a forensic hospital to a civil
treatment facility, where he was evaluated on a six-month basis. In 1997, a hearing
examiner determined that Amador no longer met the criteria for involuntary
placement (which the appellate court called an “astonishing result”), and the
hospital notified the state that Amador “would be ‘removed from the hospital’.”

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
440
The state attorney’s office filed a motion for competency hearing and/or to
continue its commitment or to recommit Amador to the custody of DCF, and the
trial court entered an order recommitting him. The public defender filed a petition
for a writ of habeas corpus on behalf of Amador, which the circuit court granted,
ordering release within 30 days, to give the trial court time to act. An arrest warrant
was then issued for the original criminal charges against Amador. The state and the
defendant stipulated that the defendant was incompetent to proceed. Meanwhile,
the Third District Court of Appeal held in State v. Heidrick, 707 So. 2d 1165 (Fla.
3d DCA 1998), that “once a defendant’s charges have been dismissed without
prejudice in light of a determination that the defendant-who has been involuntarily
hospitalized-is not competent to stand trial, the committing court lacks jurisdiction
to determine whether the defendant continues to meet the criteria for involuntary
hospitalization.” However, the opinion further stated that it “in no way prohibits
the State or any other interested party from once again initiating an action to
involuntarily hospitalize the defendants pursuant to the Baker Act.”
Two days after Heidrick was decided, the state refiled the original criminal charges
against Amador. He moved to dismiss “on the basis that the trial court, under
Heidrick, lacked jurisdiction to continue involuntary hospitalization.” The trial
court found that Amador met the criteria to undergo an involuntary examination,
ordered him to a receiving facility, lodged a capias against him, and “directed that
if the receiving facility determined that he did not meet the criteria for involuntary
placement, ‘he shall be returned to the county jail.’” The receiving facility refused
to accept Amador, even for examination, because the state had refiled the criminal
charges against him, so the state nolle prossed the charges. The trial court then
dismissed the criminal charges and republished its previous order, leaving the
capias. Amador admitted himself voluntarily to a treatment facility and remained
subject to the capeas.
Amador petitioned the Third District Court of Appeal for a writ of habeas corpus
to challenge the two court orders that directed him to a receiving facility and
directed that he be returned to county jail if the receiving facility determined that
he did not meet the criteria for involuntary placement. The court granted the writ,
quashed in part the two trial court orders, and quashed the capias, stating:
Under Heidrick, once the charges against the defendant have been
dismissed, the committing court lacks jurisdiction to order the
continued involuntary hospitalization of a defendant. However,
consistent with . . . Heidrick and section 394.463(2)(a)1, Florida
Statutes, . . . the trial court has the authority to order an involuntary
examination of the defendant under the Baker Act.” The court

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
441
remanded the case for further proceedings under section
394.463(2)(a)1, Florida Statutes.
State v. Heidrick, 707 So. 2d 1165 (Fla. 3d DCA 1998). Two defendants were
adjudicated incompetent to stand trial and were involuntarily hospitalized pursuant
to section 916.13, Florida Statutes. Five years later the circuit courts entered orders
finding that “there was no substantial probability that the defendants would regain
mental competency in the foreseeable future” and that they met the criteria for
involuntary placement. “Therefore, the circuit courts dismissed the defendants’
charges without prejudice to the State to refile the charges should the defendants be
declared competent to stand trial in the future. Further, the circuit courts committed
the defendants to [HRS].” As required by rule 3.213(b), Florida Rules of Criminal
Procedure, the orders instructed the facility administrator to notify the state
attorney at least 30 days before the defendants’ anticipated release dates.
A few years later, HRS gave the 30-day notice to the state attorney, explaining that
the defendants were unlikely to achieve competency to stand trial, but that they
“were no longer dangers to themselves or others and that they could live and
function in a less restrictive environment.” The state attorney “moved to have the
committing courts determine whether the defendants should remain involuntarily
hospitalized,” and both courts found that they “lacked jurisdiction to make such a
determination.” The state filed petitions for writ of mandamus, but the appellate
court denied the petitions, holding that the two circuit courts properly found that
they lacked jurisdiction to determine whether the defendants continued to meet the
criteria for involuntary hospitalization. The court also stated that “this decision in
no way prohibits the State or any other interested party from once again initiating
an action to involuntarily hospitalize the defendants pursuant to the Baker Act.”
The appellate court held that the once a defendant’s charges are dismissed without
prejudice pursuant to rule 3.213, the state must either release the defendant or
commit the defendant for involuntary hospitalization pursuant to the Baker Act
rather than chapter 916.16, Florida Statutes (Mentally Deficient and Mentally Ill
Defendants). It also noted that Baker Act discharge procedures are to be followed:
[S]ection 394.469(1), Florida Statutes, . . . provides that the
administrator of the facility is the one who has the power to discharge
the patient. Chapter 394 does not allow the State to seek review of the
administrator’s decision to discharge the defendant before the court
that initially committed the defendant. Therefore, contrary to the
State’s assertion, the discharge provision of section 916.16 is
inapplicable, and pursuant to section 394.469(1), the decision to

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
442
discharge the defendants rests solely with the administrator of the
facility.
The appellate court also found that the policy purpose of the notification
requirements of rule 3.213(b), Florida Rules of Criminal Procedure, “is to provide
the state attorney of the committing circuit with the opportunity to decide whether
he or she will refile the charges against the defendant [and] not for the purpose of
providing the State with an opportunity to challenge the administrator’s decision to
discharge the defendant from the facility.”
Cuervo v. State, 603 So. 2d 654 (Fla. 3d DCA 1992). The Third District Court of
Appeal held that the circuit court, which ordered the commitment of a criminal
defendant to the custody of HRS, retained jurisdiction over the defendant for the
purpose of determining continued hospitalization or release, and that a later
decision by a circuit court to transfer a criminal defendant to HRS after five years
of Baker Act hospitalization pursuant did not divest the circuit court of jurisdiction
over the person. It further held that the circuit court “may amend the commitment
order to require that the administrator of the H.R.S. facility comply with [the
notification requirements of] Florida Rule of Criminal Procedure Rule 3.213(b).”
However, in State v. Heidrick, 707 So. 2d 1165 (Fla. 3d DCA 1998), the Third
District Court of Appeal held that Cuervo was incorrectly decided and receded
from it on this issue.
XI. Marchman Act
Blair v. Razilou, 2010 WL 571980 (M.D. Fla. 2010). Blair and her husband had
been drinking one night, and on the way home her husband was pulled over and
arrested for DUI. Because Blair was intoxicated, a relative who could give her a
ride home was 40 minutes away, and officers at the scene were concerned that
Blair “may stumble into the road and get hit by a car,” Officer Razilou handcuffed
her and took her to jail for involuntary civil commitment under the Marchman Act.
Blair later filed a complaint against the city and Officer Razilou, alleging (1)
violation of her Fourth and Fourteenth amendment rights to be free from
involuntary commitment, (2) that the city failed to properly instruct its employees
regarding probable cause and the Marchman Act, (3) false arrest (under state law),
and (4) false imprisonment (under state law). The defendants filed a motion for
summary judgment, claiming qualified immunity on the part of Officer Razilou,
who was acting within his discretionary authority. The court granted the
defendants’ motion for summary judgment on the first two counts, finding that
because Officer Razilou had “arguable probable cause to civilly commit plaintiff,”
he was entitled to qualified immunity. Judgment was entered only on the federal

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
443
claims; the court declined to retain jurisdiction over the state-law claims.
Cole v. State, 714 So. 2d 479 (Fla. 2d DCA 1998). The circuit court convicted
Cole of indirect criminal contempt for violating its order directing him to complete
a substance abuse treatment program and sentenced him to 90 days in jail. He filed
a petition for writ of habeas corpus and other relief. The appellate court ordered his
release, quashed his conviction and sentence for indirect criminal contempt, and
prohibited the circuit court from enforcing the involuntary treatment order. As
grounds, the appellate court noted that the trial court failed to inform Cole of his
right to counsel, Cole “was not given meaningful prior notice of the charges
against him,” the trial was not recorded as required by law, and the court order
“included directives and prohibitions that were beyond the judicial authority
granted by the Marchman Act.” It stated that
even if the proceeding had not been so fundamentally flawed, the
printed directory provisions of the . . . form order would have been
unenforceable because they exceeded the court’s authority. Although
the Act empowers the court to order a respondent’s submission to
involuntary substance abuse treatment, and, pursuant to section
397.697, to enter such further orders as the circumstances may
require, that authority does not extend to prescribing the specific
modalities of the treatment. Under the Act that authority is placed
with the licensed service provider.
S.M.F. v. Needle, 757 So. 2d 1265 (Fla. 4th DCA 2000). The circuit court had
granted a petition for involuntary substance abuse treatment for a minor in
response to a petition filed by her parent. The order was for 60 days of involuntary
treatment, the maximum period permitted under law, commencing upon her
admission to the facility. However, the minor ran away prior to commencing
treatment and was returned to the program after the initial court order had expired.
She filed a petition for a writ of habeas corpus, arguing that she was entitled to
immediate release because section 397.6977, Florida Statutes, provided that “[a]t
the conclusion of the 60-day period of court-ordered involuntary treatment, the
client is automatically discharged unless a motion for renewal of the involuntary
treatment order has been filed with the court.” The appellate court held that the
automatic discharge would occur “at the ‘conclusion of the 60-day period of court-
ordered involuntary treatment,’ not merely sixty-days after the entry of the order
for treatment,” and that the 60-day period had not expired, because the petitioner
ran away before commencing treatment. The petition for writ of habeas corpus was
denied.

Compendium of Appellate Cases,
Appendix II Attorney General Opinions, and Other Legal References
_____________________________________________________________________________________
Baker Act Benchguide November 2016
444
Department of Health and Rehabilitative Services v. Straight, Inc., 497 So.
2d 692 (Fla. 1st DCA 1986). The trial court entered a final summary
judgment granting declaratory relief to a nonprofit corporation that operated a
drug treatment and rehabilitation program, declaring that chapter 397, Florida
Statutes, “does not prevent a parent from placing a minor child in a drug
treatment program without obtaining either the child’s consent or judicial
review of the child’s involuntary commitment.” The appellate court affirmed.

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
445
APPENDIX III:
List of FAQ Categories on DCF Website
Nearly a thousand pages of Frequently Asked Questions about the Baker Act and
related issues categorized in 21 major groups and up to 17 subgroups are posted to
the DCF Mental Health Program website.
These
FAQs may provide significant
guidance, but do not represent legal advice.
These
are all real questions that have
been asked and answered over the years with all identifiers removed. Questions can
be found on the State’s Baker Act internet site located at
http://myflfamilies.com/service-programs/mental-health/baker-act-faq.

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
446
FAQ Table of Contents
Baker Act Forms
Clinical Records & Confidentiality
Clinical Record
Confidentiality
HIPAA
Public Records
Discharge Planning
Emergency Medical Conditions, EMTALA, Hospital Transfers
Emergency Medical Condition
Defined
Medical Conditions of Persons under the Baker Act
EMTALA Applicability
Medical Clearance
EMTALA / Medical Screening
Baker Act Involuntary Examination
Stabilization
Informed Consent for Transfer
Forms/Paperwork
Transfers
Nearest Facility for Transfer?
Transfers under the Baker Act
Crisis Stabilization Units (CSU’s)
EMTALA/Reverse Dumping
EMTALA/Insurance
Transportation
Law Enforcement
Emergency Treatment Orders
Restraints
Chemical Restraints
Initiation of Emergency Treatment
Emergency Medications
Guardian Advocates & Other Substitute Decision-Makers
PRN & Standing Orders Prohibited
Forms

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
447
Involuntary Placement Petition
ETO’s for Medical Treatment
Express and Informed Consent
Competence to Consent
Incompetence to Consent
Disclosure
Consent to Treatment
Initiation of Psychiatric Treatment
Mental Health Advance Directives
Electroconvulsive Therapy
Consent to Medical Treatment
Guardian Advocates & Other Substitute Decision Makers
General
Court Appointed Guardians (Chapter 744, FS)
Guardian Advocates
Health Care Surrogates & Proxies
Other Substitute Decision Makers
Medical Consent
Involuntary Examinations
Professional Credentials
Criteria
Initiation
Transport
Acceptance
Examination
Conversion to Voluntary Status
Release from Involuntary
Examination
Transfers
Baker Act Reporting
Nursing Home/ALF Initiations
Notices
Medical Conditions
Elopement
Miscellaneous
Involuntary Inpatient Placement
Criteria

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
448
Initiation & Filing of Petitions
Public Defender & State Attorney
Witnesses
Continuances
Waiver of Hearings
Conversion to Voluntary Status
Hearings
Involuntary Placement Orders
Continued Involuntary Inpatient
Placement
Baker Act Forms
Elopements
Transfers of Persons under
Involuntary Placement
State Treatment Facilities &
Transfer Evaluations
Discharge of Persons under
Involuntary Placement
Convalescent Status
Involuntary Outpatient Placement
Law Enforcement
Definition of Law Enforcement Officer
Voluntary Admissions
Initiation of Involuntary Examination
Execution of Involuntary Examination
Criminal Charges
Restraining Devices
Receiving Facility Responsibilities
Paperwork Required
Rights of Persons
Consular Notification & Access Training
Training
Warrantless Entry
Long-Term Care Facilities
Alternatives to the Baker Act
Voluntary Admissions
Involuntary Examination
Transportation
Transfers
Refusal to Accept Back

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
449
Marchman Act
General
Protective Custody – Law Enforcement
Transportation
Licensed Substance Abuse Facilities
Responsibilities of Licensed Facilities
Emergency Medical Conditions
Involuntary Admissions
Involuntary Treatment
Appellate Cases
Minors
Minority Defined
Informed Consent for Treatment
Voluntary Admissions
Involuntary Examinations
Transportation & Transfers
Involuntary Placement
Separation of Minors from Adults
Juvenile Delinquency
Receiving Facilities
Professional Credentials
General
Physicians
Physician Assistants
Psychologists
Psychiatric Nurses
Chapter 491 Professionals
Veteran’s Affairs
Involuntary Placement
Receiving Facilities
General
Designation
Public Receiving Facilities & CSU’s
Involuntary Status
Inducements
State Hospital Transfers

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
450
Rights of Persons in Mental Health Facilities
General
Right to Dignity & Privacy
Advance Directives
Right to Treatment
Communication Restrictions
Clinical Records & Confidentiality
Custody of Personal Possessions
Designated Representatives
Habeas Corpus
Right to Discharge
Training
Transportation under the Baker Act
General
Transportation Exception Plans
Voluntary Status
Responsibility of Receiving
Facilities & Hospitals
Nearest Receiving Facility
Criminal Charges
Delegation of Transportation to Medical Transport Transfers
EMTALA/Transportation
Transport to State Hospitals (Treatment Facilities)
Juvenile Justice
Transport for Involuntary Placement
Marchman Act
Voluntary Admissions – Adults
Requirements for Voluntary Admission
Competence to Provide Express & Informed Consent
Right to Request Release
Guardians & Other Substitute Decision-Makers
Transfers in Legal Status
Requirements for Voluntary Admission
Access to State Mental Health Facilities
Weapons & Contraband

Appendix III List of FAQ Categories on DCF Website
_____________________________________________________________________________________
Baker Act Benchguide November 2016
451
Weapons in Field
Weapons at Psychiatric Hospitals
Contraband

Appendix IV List of All Mandatory and Recommended Baker Act Forms
_____________________________________________________________________________________
Baker Act Benchguide November 2016
452
APPENDIX IV:
List of All Mandatory and Recommended Baker Act Forms

Appendix IV List of All Mandatory and Recommended Baker Act Forms
_____________________________________________________________________________________
Baker Act Benchguide November 2016
453
Baker Act Forms – Table of Contents
Form #
T
itle
3001*
Ex Parte Order for Involuntary
Examination
3002*
Petition and Affidavit Seeking Ex Parte Order Requiring Involuntary Examination (2-sided;
4 pages)
3008*
Order for Involuntary Inpatient
Placement
3021*
Notice of Petition for Involuntary
Placement
3022*
Application for Appointment of Independent Expert
Examiner
3024*
Notice of Petition for Continued Involuntary Inpatient
Placement
3031*
Order for Continued Involuntary Inpatient Placement or for
Release
3032*
Petition for Involuntary Inpatient Placement (2-sided;
3 pages)
3033*
Notification to Court of Withdrawal of Petition for Hearing on Involuntary Inpatient or
Involuntary Outpatient
Placement
3035*
Petition Requesting Authorization for Continued involuntary Inpatient Placement (2-sided
2 pages)
3036*
Notice of Right to Petition for Writ of Habeas Corpus or for Redress of
Grievances
3038*
Notice of Release or
Discharge
3040*
Application for Voluntary Admission of an Adult (Receiving
Facility)
3042a*
General Authorization for Treatment Except Psychotropic
Medications
3042b*
Specific Authorization for Psychotropic
Medications
3043*
Inventory of Personal
Effects
3044*
Authorization for Release of
Information
3045*
Notice of Person’s Admission for Involuntary
Examination
3046*
Application for and Notice of Transfer to Another Receiving or Treatment
Facility
3048*
Confidentiality
Agreement
3049*
Restriction of Communication or
Visitors
3051a*
Notice of Right of Person on Voluntary Status to Request Discharge From
a
Receiving
Facility (2-sided;
2 pages)
3051b*
Notice of Right of Person on Voluntary Status to Request Discharge From a Treatment
Facility (2-sided;
2 pages)
3052a**
Report of Law Enforcement Officer Initiating Involuntary Examination
(MANDATORY)
3052b**
Certificate of Professional Initiating Involuntary Examination (2-sided;
2
pages)
(MANDATORY)
3057*
Authorization for Electroconvulsive
Treatment
3084**
Baker Act Service Eligibility
(MANDATORY)
3089*
Transfer Evaluation (To
a
State Mental Health Treatment Facility)
(MANDATORY)
3090*
Petition for Writ of Habeas Corpus or for Redress of Grievances (2-sided;
2-pages)
3097*
Application for Voluntary Admission
–Minors
3098*
Application for Voluntary Admission (State Treatment
Facility)
3099*
Certification of Ability to Provide Express and Informed Consent for Voluntary Admission
and Treatment of Selected Persons From Facilities Licensed Under Chapter 400,
F.S.
3100**
Transportation to Receiving Facility (2-sided;
2
pages)
(MANDATORY)
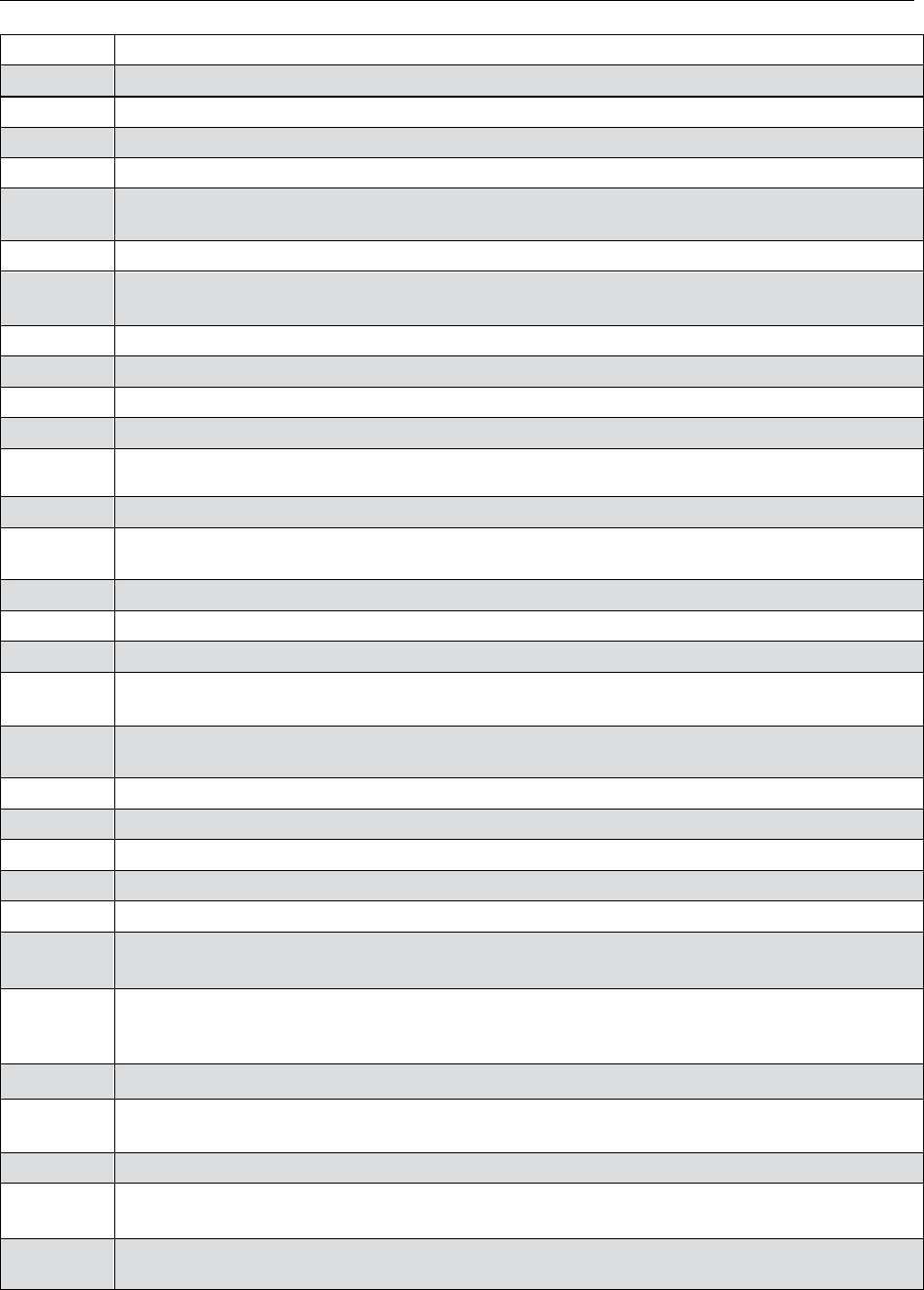
Appendix IV List of All Mandatory and Recommended Baker Act Forms
_____________________________________________________________________________________
Baker Act Benchguide November 2016
454
3101
*
Hospital Determination That Person Does Not Meet Involuntary Placement
Criteria
3102*
Request for Involuntary Examination After Stabilization of Emergency Medical
Condition
3103*
Rights of Persons
in
Mental Health Facilities and Programs (2-sided;
2 pages)
3104*
Certification of Person’s Competence to Provide Express and Informed
Consent
3105*
Refusal or Revocation of Consent to
Treatment
3106*
Petition for Adjudication of Incompetence to Consent to Treatment and Appointment of
a
Guardian Advocate
(2-
pages;
2 sided)
3107*
Order Appointing Guardian
Advocate
3108*
Petition Requesting Court Approval for Guardian Advocate to Consent to Extraordinary
Treatment
3109*
Order Authorizing Guardian Advocate to Consent to Extraordinary
Treatment
3110*
Restriction of Person’s Access to Own
Record
3111*
Approval for Release of Person on Involuntary Status from
a
Receiving
a Facility
3113*
Notice to Court Request for Continuance of Involuntary Placement
Hearing
3114*
Order Requiring Involuntary Assessment and Stabilization for Substance and for Baker-Act
Discharge of
Person
3115*
Order Requiring Evaluation for Involuntary Outpatient
Placement
3116*
Findings and Recommended Order Restoring Person’s Competence to Consent to
Treatment and Discharging the
Guardian Advocate
3118**
Cover Sheet to Agency for Health Care Administration
(MANDATORY)
3119*
Notification of
a
Facility’s
Non-Compliance
3120*
Certification of Guardian Advocate Training
Completion
3121*
Notification to Court of Person’s Competence to Consent to Treatment and Discharge of
Guardian
Advocate
3122*
Certification of Person’s Incompetence to Consent to Treatment and Notification of Health
Care Surrogate/Proxy (2-sided;
2 pages)
3123*
Affidavit of Health Care
Proxy
3124*
Personal Safety Plan (2-sided;
3 pages)
3125**
Application for Designation as
a
Receiving Facility (2-sided;
3
pages)
(MANDATORY)
3130*
Petition for Involuntary Outpatient Placement (2-sided;
4 pages)
3140*
Designation of Service Provider for Involuntary Outpatient
Placement
3145*
Proposed Individualized Treatment Plan for Involuntary Outpatient Placement and
Continued Involuntary
Outpatient Placement
3150*
Notice to Department of Children and Families of Non-Filing of Petition for Involuntary
Outpatient Placement or
Diminished
Treatment Plan Due to Non- Availability of Services
or
Funding
3155*
Order for Involuntary Outpatient Placement or Continued Involuntary Outpatient
Placement
3160*
Notice to Court of Modification to Treatment Plan for Involuntary Outpatient Placement
and/or Petition
Requesting
Approval of Material Modifications to
Plan
3170*
Petition for Termination of Involuntary Outpatient Placement
Order
3180*
Petition Requesting Authorization for Continued Involuntary Outpatient Placement (2-sided;
2 pages)
3185*
Notice to Court of Waiver of Continued Involuntary Outpatient Placement Hearing and
Request for an
Order

Appendix IV List of All Mandatory and Recommended Baker Act Forms
_____________________________________________________________________________________
Baker Act Benchguide November 2016
455
7000*
State Mental Health Facility Admission Form (2-sided;
6 pages)
7001*
State Mental Health Facility Discharge Form (2-sided; 12
pages)
7002*
Physician to Physician Transfer
Form
*Recommended **Mandatory
