
Missouri State High School
Activities Association
2021-22
Interscholastic
Youth Sports
Brain Injury
Report

2021-2022
Interscholastic Youth Sports Brain Injury Prevention Report
SCS HCS HB 300, 334, and 387 became law in August 2011, and it mandates that an organization with
public schools as members must publish and distribute an annual report regarding the impact of student
athlete concussions and head injuries which should include efforts that may be made to minimize
damages from school sports injuries. The Department of Health and Senior Services, along with a
statewide association of school boards [Missouri School Board Association (MSBA)], a statewide
activities association that provides oversight for athletic or activity eligibility for students and school
districts, [Missouri State High School Activities Association (MSHSAA)], and an organization named by
the Department of Health and Senior Services that specializes in support services, education and
advocacy of those with brain injuries [Brain Injury Association of Missouri (BIA-MO)] developed
guidelines, pertinent information and forms to educate coaches, staff members, athletes and parents or
guardians of youth athletes of the nature and risk of concussion and brain injury including continuing to
play after a concussion or a brain injury (1).
MSHSAA has distributed and updated head injury materials annually since August of 2009 to its member
schools using a variety of sources (2). These materials provide information that will educate parents,
coaches, staff members, and athletes on the prevention, management, and dangers of head injuries in
interscholastic sports (3). In December of 2011, MSHSAA conducted its first annual survey of member
schools and the impact of head injuries. An eleventh survey was conducted from August 1, 2021 through
June 30, 2022, to collect data from the MSHSAA member schools. Five hundred and eighty-six schools
were contacted to complete the survey during the 2021-2022 school. Working with the Brain Injury
Association of Missouri, Department of Health and Senior Services, Missouri Athletic Trainers
Association, Missouri School Nurses Association and Missouri School Board Association, a pilot
program began for the winter and spring of 2014, Sports Concussions: Facts, Fallacies and New Frontiers.
The program was conducted in five regional sites presenting a one-day seminar educating staff members,
coaches, nurses and athletic trainers on the new research and policies pertaining to head injuries. Because
of the great success and attendance of the program, we are hopeful this partnership continues in future
years.
Harvey Richards, retired Associate Executive Director formerly in charge of Sports Medicine for
MSHSAA, was a part of the state legislative process for the head injury bill (4). Greg Stahl is the current
Assistant Executive Director in charge of Sports Medicine for MSHSAA, responsible for the distribution
of educational materials to member schools, and conducted the 2021-2022 Head Injury Survey (5).
(1) Timetable of Meetings, Appendix A.
(2) Fall membership-mailing, e-mails, website (mshsaa.org), district in-services.
(3) Educational packet for member schools, Appendix B.
(4) Harvey Richards, Retired Associate Executive Director
(5) Greg Stahl, Assistant Executive Director, 1 N Keene St., Columbia, MO 65201; greg@mshsaa.org
; (573) 875-4880.

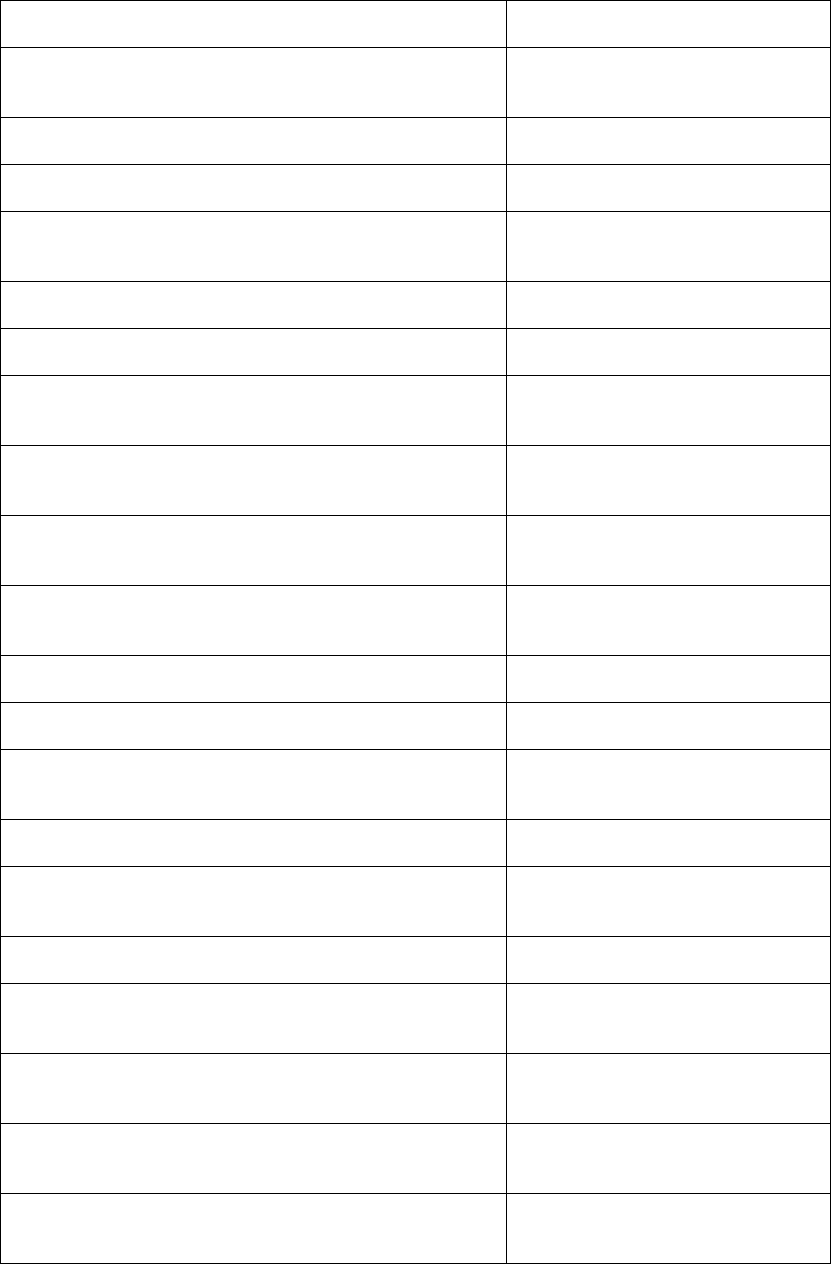
2021-2022 Head Injury Survey
School
Level
Total Schools
Completed Survey
Did Not Complete
the Survey
% of Member Schools
that Completed Survey
2022
2021
2020
2022
2021
2020
2022
2021
2020
2022
2021
2020
High
Schools
9-12
and
Combined
Schools
7-12
586 586 589 542 552 572 44 34 17 92.5% 94.2% 97.1%
Use of Online Video
The National Federation of High School Activities (NFHS) has produced and made available for free, the
online course “Concussions in Sports.” MSHSAA has approved this course for coaches to take as their
educational component of the law. Many school districts continue to view this course as an in-service
with the entire coaching staff, while other school districts have coaches complete the course individually
to meet the by-law requirement for completing concussion education. For the year July 1, 2021 through
June 30, 2022, 11,751 online courses were completed in Missouri.
The next table reflects the number of participants for each sport and/or activity by our member schools.
This number will include duplicates for students who are in multiple activities. Music/Band, Sideline
Cheerleading (Spirit) and Dance begin in the fall, but some schools will only participate in the winter or
spring. The following table reflects the participation rates for both the 2020-2021 and 2021-2022 school
years.
Note: In general, both student and school participation numbers, especially in contact sports,
during the 2021-2022 school increased back toward more traditional numbers pre Covid-19.

High School Sport/Activity
Participants
2021-2022
2020-2021
11-man Football
20,161
19,780
8-man Football
894
786
Baseball
14,536
14,088
Basketball-Boys
13,447
13,070
Basketball-Girls
9,164
8,913
Bass Fishing
212
237
Bowling
106
90
Chess
156
79
Cross Country-Boys
5,150
5,021
Cross Country-Girls
3,897
3,762
Dance/Pom Team
2,723
2,717
Esports
514
0
Field Hockey
1,168
1,147
Golf-Boys
4,072
3,864
Golf-Girls
2,068
1,898
Lacrosse-Girls
1,532
1,460
Music-Band
23,103
22,541
Scholar Bowl
5,131
4,625
Sideline Cheerleading (Spirit)
9,220
9,100
Soccer-Boys
8,065
7,887
Soccer-Girls
7,474
6,849
Softball-Girls
9,215
8,969
Speech/Debate/Theatre
7,333
5,872
Swimming and Diving-Boys
1,807
1,691
Swimming and Diving-Girls
2,887
2,867
Target Shooting
668
522
Tennis-Boys
3,308
2,983
Tennis-Girls
4,319
3.910
Track and Field-Boys
15,175
12,967
Track and Field-Girls
12,305
10,614
Volleyball-Boys
1,320
1,098
Volleyball-Girls
10,826
10,116
Water Polo
515
466
Wrestling-Boys
6,315
5,323
Wrestling-Girls
1,897
1,351
Totals
210,683
192,717
High School Sport/Activity
Total
Participation
Sport
161,517
*Taking into Account 20% Duplication of Athletes
32,303
Total Adjustment Participation Sport
129,214
Activity
49,166
*Taking into Account 20% Duplication of Students
9,833
Total Adjustment Participation Activity
39,333
Total Adjustment Participation Sport/Activity
168,547
*20% duplication is only an estimate and not an actual number.

Data Collected
Schools were asked to provide information that related to possible head injuries. If signs or symptoms of a head injury were
present, the student was to be withheld from that sport and or activity for a minimum of 24 hours and must have been seen by
a medical professional. They must also provide to the school a Return to Play form before return to the sport or activity. The
information below reflects those students who had to see a medical professional and provide a Return to Play form. Not all
incidents would have resulted in a concussion.
HIGH SCHOOL ACTIVITIES
Level
Activity
Activity
Related
Non-
Activity
Related
Days/
Class
Act
Days/
Class
Non-Act
Days
Missed
Activity
Days
Missed
Non-Act
Diagnosed
Activity
Diagnosed
Non-Act
Schools
Report-
ing
Schools
Partici-
pating
HS
Scholar Bowl
1
1
0
0
0
0
0
0
1
422
HS
Sideline Cheer
346
69
580
136
5,011
935
274
60
156
525
HS
Music Activities
4
6
5
2
16
64
2
5
8
532
HS
Dance/Pom
20
13
23
42
264
252
18
10
21
214
HS
Speech/Debate/Theatre
1
0
0
0
30
0
1
0
1
243
HS
Bass Fishing
0
0
0
0
0
0
0
0
0
27
HS
Bowling
0
0
0
0
0
0
0
0
0
11
HS
Chess
0
0
0
0
0
0
0
0
0
21
HS
Target Shooting
0
0
0
0
0
0
0
0
0
35
HS
Esports
0
0
0
0
0
0
0
0
0
45
TOTAL
372
89
608
180
5,321
1,251
295
75
187
2,075
HIGH SCHOOL SPORTS
Level
Activity
Sport
Related
Non-
Sport
Related
Days/
Class
Sport
Days/
Class
Non-Sport
Days
Missed
Sport
Days
Missed
Non-Sport
Diagnosed
Sport
Diagnosed
Non-Sport
Schools
Report-
ing
Schools
Partici-
pating
HS
Baseball - Spring
98
16
113
21
619
143
57
12
82
510
HS
Basketball - Boys
185
9
156
10
1,250
64
116
6
129
577
HS
Basketball - Girls
313
16
350
22
3,216
244
224
14
188
553
HS
Cross Country - Boys
4
7
8
9
38
67
3
6
8
442
HS
Cross Country - Girls
3
6
3
4
52
76
2
5
9
437
HS
Field Hockey - Girls
19
0
27
0
127
0
13
0
13
32
HS
11-Man Football
1,240
41
1,516
56
12,211
515
998
29
252
318
HS
8-Man Football
49
4
55
6
307
22
36
3
27
38
HS
Golf – Boys
2
4
1
7
14
9
1
3
6
331
HS
Golf - Girls
0
3
0
6
0
46
0
3
3
205
HS
Soccer - Boys
234
15
196
9
1,926
81
172
11
121
233
HS
Soccer – Girls
350
22
322
24
2,962
135
259
12
147
237
HS
Softball - Girls Fall
114
19
106
28
914
201
92
17
84
339
HS
Swim/Diving - Boys
10
6
2
11
133
82
7
5
13
118
HS
Swim/Diving - Girls
13
10
10
14
165
133
11
9
18
141
HS
Tennis-Boys
5
1
0
10
10
22
3
1
6
178
HS
Tennis - Girls
5
10
8
26
264
79
4
8
10
185
HS
Track/Field (B) Spring
18
12
8
8
120
108
10
10
20
520
HS
Track/Field (G) Spring
28
15
14
3
202
220
16
13
34
518
HS
Volleyball - Boys
10
4
6
0
63
30
9
2
11
52
HS
Volleyball - Girls
157
17
158
58
1,466
164
122
15
112
450
HS
Water Polo - Boys
9
0
0
0
19
0
2
0
5
21
HS
Water Polo - Girls
6
0
5
0
103
0
2
0
2
6
HS
Wrestling - Boys
244
12
299
27
2,880
205
193
10
118
245
HS
Wresting – Girls
119
6
132
3
1,586
89
94
6
73
202
HS
Baseball - Fall
6
1
10
3
42
10
2
1
6
101
HS
Softball - Girls Spring
16
1
15
0
138
0
12
0
15
152
HS
Lacrosse - Girls
36
5
38
18
284
47
24
5
18
38
TOTAL
3,293
262
3,558
383
31,111
2,792
2,484
206
1,530
7,179

2021-2022 Concussion Survey Results
Sports
Suspected Head Injuries
Number of Days
Sport was Missed
Number of Days
Class Missed
Male 2,133 19,759 2,397
Female
1,160
11,352
1,161
Total
3,293
31,111
3,558
Activities
# of Activity Reports
Number of Days
Activity was Missed
Number of Days
Class Missed
Total
372
5,321
608
GRAND TOTAL
3,665
36,432
4,166
There was a total of 2,133 males and 1,160 females held out of practices and contests due to a
“suspected” head injury, for a total of 19,759 (males) and 11,352 (females) days of missed participation.
This means that the male athletes were held out an average of 9.26 days per incident, and the female
athletes also were held out an average of 9.79 days per incident. This does show a good correlation to the
gradual return-to-play guidelines, which indicates at a minimum a five-day to seven-day return rate. The
number of days that a student missed class time still remains a low number compared to the total number
of days missed in the sport or activity practice/contest.
2021-2022
Top 7 Head Injury Sports/Activities
Sport/Activity Diagnosed Head Injuries
Football
1,034
Sideline Cheerleading
274
Soccer (G)
259
Basketball (G)
224
Wrestling (B)
193
Soccer (B)
172
Volleyball (G)
122
Note: Due to the increase in number of participants, similar to participant numbers pre Covid-19,
the sport specific and overall number of head injuries increased in comparison to the previous two
school years.
2021-2022
Percentage of Head Injuries per Total Occurrences
Sport/Activity % of total reported Head Injuries
Football
45.4%
Sideline Cheerleading
12.0%
Soccer (G)
11.4%
Basketball (G)
9.8%
Wrestling (B)
8.4%
Soccer (B)
7.6%
Volleyball (G)
5.4%
2020-2021
Top 7 Head Injury Sports/Activities
Sport/Activity Diagnosed Head Injuries
Football
654
Soccer (G)
217
Basketball (G)
178
Sideline Cheerleading
174
Wrestling (B)
124
Soccer (B)
111
Basketball (B)
94

Concussion Rates per 10,000 athletic exposures
From High School RIO Surveillance Study
Sport/Activity Rate
Football
7.85
Sideline Cheerleading
3.57
Soccer (G)
5.25
Basketball (G)
4.40
Wrestling (B)
4.06
Soccer (B)
2.54
Volleyball (G)
2.06
MSHSAA Athletic exposure was calculated from the first day of practice to the end of districts for that
sport. This is not a true actual count of participation but very accurate assumption. Example:
Football had on the average 84 days of practice and/or contests.
84 x 21, 055 participants = 1,768,620 exposures.
1289 reported head injuries.
1289 = X
1,768,620 10,000
MSHSAA – Top 7 Concussion in Sports/Activities
Concussion Rates per 10,000 Athletic Exposures
Sport/Activity *Rate #1 **Rate #2
Football
7.28
5.84
Sideline Cheerleading
4.69
3.71
Soccer (G)
6.50
4.81
Basketball (G)
3.63
2.60
Wrestling (B)
4.44
3.51
Soccer (B)
3.72
2.73
Volleyball (G)
1.86
1.44
*Rate #1: Student athletes removed from participation due to suspected concussion.
**Rate #2: Student athletes removed from participation due to diagnosed concussion.
There were several questions asked on this year’s survey:
1. Does your school have access to a licensed or certified Athletic Trainer or other medical care
provider?
2. Have you implemented the MSHSAA guidelines for using Wet Bulb Globe Thermometers for
measuring environmental conditions to determine the status of practices/competitions?
3. Does your school offer education for athletes, parents and coaches on heat illness, such as signs
and symptoms, hydration recommendations and ways to monitor hydration status?
4. Does your school currently require students to have a valid physical for participating in Contact
Days activities during the Summer?
5. Does your school have an AED located near every facility/venue your school uses to host regular
season contests?

Below are the results from these questions:
High School Responses
Question Answer
Number of
Responses
Does your school have access to a licensed or certified
Athletic Trainer or other medical care provider?
Yes, Full Time – All practices and games 184
Yes, Part Time – Some practices and
games
90
Yes, Part Time – Games only 78
Yes, Part Time – Drop in 40
None
150
Have you implemented the MSHSAA guidelines for using
Wet Bulb Globe Thermometers for measuring
environmental conditions to determine the status of
practices/competitions?
Yes 413
No 129
Does your school offer education for athletes, parents and
coaches on heat illness, such as signs and symptoms,
hydration recommendations and ways to monitor hydration
status?
Yes, education to coaches only 160
Yes, education to coaches and athletes 153
Yes, education to coaches, athletes and
parents
203
No, we do not offer educational material 26
Does your school currently require students to have a valid
physical for participating in Contact Days activities during
the Summer?
Yes 355
No 187
Does your school have an AED located near every
facility/venue your school uses to host regular season
contests?
Yes 499
No 43
Educational materials were distributed to all member schools and are available for the public to access
through our website (www.mshsaa.org
). Awareness of this serious issue has come to the forefront.
Several schools have requested an in-service to educate their coaching staff, with professionals
conducting the program. Our staff, along with several others, has put programs in place to continue the
educational effort and stay abreast of any new research available.
MSHSAA continues to support the Brain Injury Association of Missouri in putting together a program at
various locations throughout the state of Missouri: Sports Concussions: Facts, Fallacies and New
Frontiers.
MSHSAA will conduct an annual survey during each summer to collect yearlong data. The Sports
Medicine Committee will evaluate the questions and the report.

APPENDIX A
2010-2022 Timetable of Meetings
Place Date of Meeting
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
April 28, 2010
NFHS Summer Meeting
- Sports Medicine Committee
July 6-9, 2010
Parkway School District
- Concussion Presentation
August 12, 2010
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
January 6, 2011
Capitol, Jefferson City, MO
- Concussion Bill
January 11, 2011
Capitol, Jefferson City, MO
- Meeting – House Bill 300
February 7, 2011
Phone Conference
- House Bill 300
February 25, 2011
St. Louis Children’s Hospital
- Press Conference House Bill 300
March 4, 2011
MSHSAA Office
- Phone Conference - House Bill 300
March 7, 2011
NFHS Summer Meeting
- Sports Medicine Committee
June 27 – July 1, 2011
MSHSAA Office
- Conference Call - Concussions
August 16, 2011
MSHSAA Office
- Concussion Meeting
August 25, 2011
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
January 5, 2012
Conference Call
- Adult Brain Injury (MO Dept. of Health/Sr. Svc.)
January 19, 2012
Conference Call
- Adult Brain Injury (MO Dept. of Health/Sr. Svc.)
February 14, 2012
Meeting in St. Louis
- St. Louis Brain Association Meeting
March 1, 2012
Mercy Sports Medicine Conference
- Exertional Heat Illnesses
March 30-31, 2012
MSHSAA Office
- Adult Brain Injury (MO Dept. of Health/Sr. Svc.)
August 30, 2012
University of Missouri Research
- Survey of all Injuries
June 1, 2012
Coaches Training Meeting (Chillicothe)
- Head/Spinal Injuries (Hedrick Medical Building)
- St. Luke’s College of Health Sciences
October 12, 2012
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
December 13, 2012
MSHSAA Office
- Meeting with Dr. Hubbard, St. Luke’s
April 3, 2013
Conference Call
- Brain Injury Association of Missouri
April 16, 2013
University of Missouri Research
- Survey of all Injuries
June 2, 2013
NFHS Summer Meeting
- Sports Medicine Committee
June 24-28, 2013
Stoney Creek Inn
- Brain Injury Association of Missouri
- Annual Meeting Planning
September 6, 2013
Coaches Training Meeting
- St. Luke’s College of Health Sciences
October 2, 2013
Conference Call
- St. Luke’s College of Health Sciences
October 23, 2013
Conference Call
- University of Missouri Journalism
- Concussion Interview
November 12, 2013
NFL – Chiefs
- Head’s Up Mom’s Football Safety Clinic
December 3, 2013
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
December 12, 2013
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Springfield, MO
January 14, 2014
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Kansas City, MO
January 22, 2014
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Columbia, MO
January 27, 2014
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
February 4, 2014
NFHS Summer Meeting
- Sports Medicine Committee
June 27 – July 2, 2014
Summer’s AD Workshop
- Emergency Action Planning
July 31, 2014
Stoney Creek Inn
- Brain Injury Association of Missouri
- Concussion Seminar Planning
October 8, 2014
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
December 11, 2014
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Springfield, MO
January 16, 2015
NFHS Football Meeting
- Indianapolis, IN
January 23-25, 2015
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Columbia, MO
January 27, 2015
Missouri United Schools Insurance Council
- Concussion Seminar
- Lake of the Ozarks
January 29-30, 2015
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
February 5, 2015
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Kansas City, MO
February 12, 2015

MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
February 18, 2015
USA/NFL Football Meeting
- Indianapolis, IN
February 22, 2015
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Cape Girardeau, MO
February 26, 2015
USA/NFL Football Meeting
- New York, New York
March 26-27, 2015
MIAAA Conference
- Concussion Information Booth/Heads Up Football
- Lake Ozark, MO
April 10-14, 2015
Sports Medicine Advisory Committee Meeting
- Overuse Injuries in Baseball
- Indianapolis, IN
June 8-10, 2015
NFHS Summer Meeting
- Sports Medicine Committee
- New Orleans, LA
June 26 – July 3, 2015
Officiate Missouri Day
- St. Louis, MO
July 24-25, 2015
SERC Sports Medicine Symposium
- Kansas City, MO
August 1, 2015
Brain Injury Association
- Statewide Conference Call
August 18, 2015
KBIA Radio Interview
- Athletic Trainers at High School Sporting Events
September 18, 2015
Brain Injury Association Meeting
- St. Louis, MO
September 23, 2015
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
December 10, 2015
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Columbia, MO
February 17, 2016
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Cape Girardeau, MO
February 18, 2016
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
February 22, 2016
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Springfield, MO
February 25, 2016
USA/NFL Football Meeting
- Indianapolis, IN
March 21-23, 2016
MIAAA Conference
- Concussion Information Booth
- Lake Ozark, MO
April 8-12, 2016
NFHS Summer Meeting
- Sports Medicine Committee
- Reno, NV
June 28 – July 3, 2016
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
December 3, 2016
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
January 26, 2017
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Kansas City, MO
February 2, 2017
Sports Concussion: Facts, Fallacies and New Frontiers
February 9, 2017

- Brain Injury Association
- Columbia, MO
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Springfield, MO
February 23, 2017
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Cape Girardeau, MO
March 2, 2017
Solutions for Safety in Sports Seminar
- Kansas City, MO
March 28-29, 2017
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
- Lake Ozark, MO
April 7-11, 2017
NFHS Summer Meeting
- Sports Medicine Committee
- Providence, RI
June 28 – July 3, 2017
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
September 5, 2017
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
January 29, 2018
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Columbia, MO
February 2, 2018
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Cape Girardeau, MO
February 6, 2018
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Springfield, MO
February 8, 2018
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Kansas City, MO
February 12, 2018
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
March 1, 2018
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
- Lake Ozark, MO
April 8-10, 2018
NFHS SMAC Summit
- Indianapolis, IN
April 21-23, 2018
NFHS Summer Meeting
- Sports Medicine Committee
- Chicago, IL
June 27-July 3, 2018
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
September 10, 2018
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- St. Louis, MO
February 26, 2019
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
February 28, 2019
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Kansas City, MO
March 4, 2019

Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
- Columbia, MO
March 11, 2019
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
- Lake Ozark, MO
April 7-9, 2019
NFHS Summer Meeting
- Sports Medicine Committee
- Indianapolis, IN
June 26-July 2, 2019
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
September 16, 2019
Sports Concussion: Facts, Fallacies and New Frontiers
- Brain Injury Association
Columbia, MO
February 7, 2020
MSHSAA Sports Medicine Advisory Committee Meeting
Columbia, MO
March 15, 2020
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
Lake Ozark, MO
Postponed – COVID19
NFHS Summer Meeting
- Sports Medicine Committee
Via ZOOM
June 26 - July 2, 2020
MSHSAA Sports Medicine Advisory Committee Meeting
- Sports Medicine Committee
- COVID Planning Meeting
Via ZOOM
June 4, 2020
MSHSAA Sports Medicine Advisory Committee Meeting
- Via Zoom
September 3, 2020
MSHSAA Sports Medicine Advisory Committee Meeting
Via Zoom
March 25, 2021
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
Lake Ozark, MO
April 11-13, 2021
NFHS Summer Meeting
- Sports Medicine Committee
Orlando, Florida
June 28 - July 2, 2021
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
September 2, 2021
MSHSAA Sports Medicine Advisory Committee Meeting
- Columbia, MO
March 24, 2022
MIAAA Conference
- Concussion Information Booth – Head Injury Survey Info
Lake Ozark, MO
April 3-5, 2022
NFHS Summer Meeting
- Sports Medicine Committee
San Antonio, Texas
June 28 - July 2, 2022
APPENDIX B

MSHSAA INTERSCHOLASTIC BRAIN INJURY SURVEY
2021-2022
HOUSE BILL 300 – Brain Injury Prevention Act
As a reminder to all MSHSAA member schools, House Bill 300 requires the MSHSAA and it’s member schools to report
and collect information on head injuries each school year. At this time your school needs to start/continue collecting
information in order to the complete the MSHSAA Brain Injury Survey for the 2020-2021 school year. The MSHSAA Brain
Injury Survey is open during the course of the school and will close on June 30
th
. An email blast has been and will
continue to be sent to all Athletic Directors, ATC’s and School Nurses notifying you of the survey and instructions for
locating the survey. In order for your school’s Athletic Trainer (ATC) or School Nurse to receive this email blast, please
make sure they are added to your school’s Administrators page at www.mshsaa.org
.
PLEASE START/CONTINUE WITH COLLECTING DATA IN RELATION TO THE FOLLOWING AREAS/TOPICS SO YOUR
SCHOOL CAN BE PREPARED FOR COMPLETING THE 2020-2021 MSHSAA INTERSCHOLASTIC BRAIN INURY SURVEY.
**Your school’s use of Emergency Action Plans for each sport/activity practices, games/contests, venues.
**Your school’s use of an Athletic Trainer(ATC) or other medical providers. At practices? At games/contests? Full time?
Part-time?
**Your schools use of EMT services(ambulance) at athletic contests. All contests? Sport specific contests?
**Does your school use the NFHS video “Concussion in Sports – What you need to know”, to educate your coaching
staffs during the school year?
HEAD INJURIES OCCURING “DURING” SPORT OR ACTIVITY
1. Number of Students removed from sport or activity practices and contests due to signs and symptoms of a concussion
and had to obtain a medical Return To Play form.
2. Number of Return To Play forms that indicated a diagnosis of a concussion.
3. Total number of days of practices and contests that were missed by student athletes in each sport/activity due to
diagnosis and requirement dictated on through the Return To Play protocol.
4. Total number of days of classroom attendance that students missed due diagnosed concussion.
HEAD INJURIES OCCURING “OUTSIDE” OF A SPORT OR ACTIVITY
1. Number of Students removed from sport or activity due to head injury occurring outside of the sport/activity (car
accident, accident at home, etc.) and had to obtain a medical Return To Play form.
2. Number of Return To Play forms that indicated a diagnosis of a concussion.
3. Total number of days that were missed by students in each sport/activity who were required to follow Return To Play
protocol.
4. Total number of days of classroom attendance that students missed due diagnosed concussion.
(Additional Information - See Back Page)

PLEASE MAKE SURE THE FOLLOWING REQUIREMENTS ARE IN PLACE
Concussion Information and Materials
All coaches must take a course on the signs, symptoms, and prevention of concussions annually.
• There is a free-of-charge course that is located on the NFHS Learning Center website
(www.nfhslearn.com). Once there, go to the FREE/ELECTIVE COURSES section. Click on the right
arrow until you come to the “Concussion in Sports – What You Need To Know” course.
• There is also a link to this course on our website located at (www.mshsaa.org) located on the
Sports Medicine Tab in the CONCUSSION section.
All parents and athletes must receive and sign for the concussion materials as indicated on the
MSHSAA Pre-Participation Physical Form.
The concussion information for parents and athletes can be found in the following three locations:
• The free NFHS “Concussion in Sports” course described above;
• The materials that are provided on our website (www.mshsaa.org) by clicking on the Sports
Medicine Tab.
• The Concussion Information PowerPoint located on our website (www.mshsaa.org) by clicking on
the Sports Medicine Tab and then on “MSHSAA Concussion Video Introduction.”
Athletic Directors must keep accurate records of this information and be able to provide it to MSHSAA
if asked to do so.
Emergency Action Planning Guide
On the MSHSAA web site under Sports Medicine is information for your school to set up and
implement the “Anyone Can Save a Life” program.
This program is free of charge.
If you have any question, please contact MSHSAA.
Online Sports Medicine Information
The Sports Medicine information is located online by going to the MSHSAA website (www.mshsaa.org)
and clicking on the Sports Medicine tab.
Reminder: Mandatory Heat/Hydration requirements are to be followed for the start of Fall practice.
Please see information on heat/hydration found on the Sports Medicine page of our website.
Reminder: The use of WBGT (Wet Bulb Glob Thermometer) is now the procedure for monitoring
environmental conditions to determine when practices/contests may be permitted to occur relative to
heat/humidity conditions and the safety of athletes. The WBGT Guidelines along with websites where
a WBGT may be purchased are located on the Sports Medicine page of our website.
Reminder: Physical Forms (PPE’s) can now be valid for two years from the date the physical is
received; however, there are still Pre-Participation Documentation – Annual Requirements that must
continue to be collected from your students/parents annually. Go to Sports Medicine tab at
www.mshsaa.org, MSHSAA Resources, “New MSHSAA Pre-Participation Documentation – Annual
Requirements” link.
Reminder: The Covid19 resources and mandatory Covid19 Return To Play form remains located online by going to
the MSHSAA website (www.mshsaa.org) and clicking on the Sports Medicine tab
REMINDERS FOR
ALL ATHLETIC DIRECTORS

Pre-participation Physical Evaluations – (PPE/Physicals)
There are no exemptions or relief to MSHSAA bylaws requiring all students to have a current/valid physical
Go to the Sports Medicine page at www.mshsaa.org and use the following links listed under MSHSAA
Resources to review the details of the current PPE requirements:
-Current MSHSAA PPE Form – (Last Update – April 2019)
-Current MSHSAA Pre-Participation Documentation - Annual Requirements
-MSHSAA PPE Information and Background
Concussion Information and Materials
It is mandatory that each member school (Middle Schools and High Schools) of the MSHSAA provide
Concussion Education to their coaches, players and parents annually. There are a number of different ways to
meet this requirement, whether that be scheduling coaches/players/parent meetings and showing the free
NFHS Concussion Education course/video or whether that be choosing to distribute Concussion Education
information to each of these three groups. Several resources for Concussion Education is located on the Sports
Medicine page at
www.mshsaa.org.
Concussion Education Resources:
http://www.nfhs.org/media/1014739/parents_guardians_guide_to_concussion_final_2016.pdf
https://nfhslearn.com/courses/61151/concussion-in-sports
Return To Play Form (Mandatory): When your school has a student that has been removed from a
game/contest due to signs and symptoms of a concussion and is then diagnosed with a concussion, your school
must use the MSHSAA Concussion Return To Play Form/Guidelines in consultation with an
MD/DO/PAC/LAT/ARNP/Neuropsychologist in order for the student return to practice/competition. The use of
this form is critical in an effort to protect the student athlete’s well-being and the schools position of liability.
Return To Play Form: http://www.mshsaa.org/resources/pdf/18%20RTP%20Form.pdf
Athletic Directors must keep accurate records and documentation of concussion education for coaches, athletes
and parents and be able to provide it to MSHSAA when requested
.
Mandatory Head Injury Reporting
All schools are required by HB300 to track any suspected head injuries to student athletes throughout the
school year. MAKE SURE TO DOCUMENT AND KEEP ON FILE ANY AND ALL OCCURENCES OF CONCUSSED
ATHLETES THROUGOUT THE SCHOOL YEAR SO THAT YOU CAN ACCURATELY RESPOND TO THE MSHSAA HEAD
INJURY SURVEY WHICH IS REQUIRED OF US BY STATE LAW – HB 300. The Head Injury Survey reporting portal
can be accessed from your school’s “Account” page through the entire school year so that you are able to report
head injuries at the conclusion of each sport season.
SPORTS MEDICINE REMINDERS FOR
ALL ATHLETIC DIRECTORS

Emergency Action Planning Guide
On the MSHSAA web site under Sports Medicine is information for your school to set up and implement the
“Anyone Can Save a Life” program. This program is free of charge. If you have any question, please contact
MSHSAA.
It is absolutely necessary that each member school implements an Emergency Action Plan for each sport,
activity and venue at your school. The MSHSAA promotes to our schools the program titled “ANYONE CAN
SAVE A LIFE”, which is a highly effective Emergency Action Plan Program being used at the middle school and
high school level across the country.
Emergency Action Planning: http://www.mshsaa.org/resources/pdf/emergencyPlanning.pdf
Wet Bulb Globe Thermometers (WBGT)
The use of a Wet Bulb Globe Thermometer (WBGT) is the recognized practice for determining unsafe
heat/humidity conditions for all outdoor sports, marching band and spirit. Note: Indoor sports, such as
Volleyball, are subject to these guidelines “if” air condition facilities are not used.
WBGT Recommendations and Guidelines, Background and Rationale and a resource list of websites to secure a
WBGT are posted on the Sports Medicine page at www.mshsaa.org
.
Online Sports Medicine Information
All Sports Medicine information is located online by going to the MSHSAA website (www.mshsaa.org) and
clicking on the Sports Medicine tab.
Reminder - F
all Sports: Mandatory 16 Day Heat Acclimatization requirements are to be followed for the start of fall
practices. Please see information on heat/hydration found on the Sports Medicine page of our website. Please keep
in mind that many students have been inactive since March due to the Covid-19 pandemic. The MSHSAA SMAC will
pass along additional recommendations to include and consider in addition to the 16 Day Heat Acclimatization

CONCUSSION EDUCATION AND MANAGEMENT PROTOCOL
Education
Concussions are common in sports. The Missouri State High School Activities Association (MSHSAA)
believes that education of coaches, officials, athletes, and their parents or guardians are key to safely
returning a student athlete to play. Appropriate immediate care after a suspected concussion, and follow
up incorporating a multi-disciplinary team that includes the coach, parent or guardian, athlete’s physician,
team physician and athletic trainer (if available), and school representatives, also are important for the
proper management of a sport-related concussion.
Each school district will receive educational materials for coaches, athletes, parents, and school officials,
required forms for student athlete participation and parent/guardian consent, and recommended medical
clearance forms for return to play.
Annually, MSHSAA member school districts will ensure that every coach, student athlete, and parents or
guardians of a student athlete completes a concussion and head injury information sheet and returns it to
the school district prior to the student athlete's participation in practice or competition. Officials will
receive training from their parent organization. Each official’s organization will require annual
concussion training and maintain a signed head injury information sheet for each official.
Recognition and Evaluation of the Athlete with a Concussion
1. Recognition of the signs and symptoms of a concussion is important. Every member of the team-
athlete, teammates, coaches, parents or guardians, officials, athletic trainers, and team physicians
have a duty to report a suspected concussion. Not all school districts have medical personnel
available to cover every practice and competition; therefore, the coach is the person in the best
position to protect the player and must be aware that not all student athletes will be forthcoming about
their injury.
2. An official shall not be responsible for making the diagnosis of a concussion. The official can assist
coaches and medical staff by recognizing signs and symptoms of a concussion and informing the
coach and medical staff of their concerns.
3. The coach, (Athletic Trainer) AT, or physician on site should evaluate the athlete in a systemic
fashion:
a. Assess for airway, breathing, and circulation (basic CPR assessment)
b. Assess for concussion
i. Any unconscious athlete should be assumed to have a severe head and/or neck injury and
should have their cervical spine immobilized until a determination can be made that the
cervical spine has not been injured. If no medical professional can make the assessment, the
athlete should be transported to an appropriate emergency care facility.
ii. A conscious athlete with no neck pain can be further evaluated on the sideline.
4. An athlete experiencing ANY of the signs/symptoms of a concussion should be immediately removed
from play. Signs/Symptoms of a concussion include:
PHYSICAL COGNITIVE EMOTIONAL
Headache Feeling mentally “foggy” Irritability
Nausea/Vomiting Feeling slowed down Sadness
Dazed/Stunned Difficulty concentrating More emotional
Balance problems Difficulty remembering Nervousness
Visual problems Forgetful of recent information
Fatigue Confused about recent events
Sensitivity to light Answers questions slowly
Sensitivity to noise Repeats questions
5. Evaluation
a. Following any first aid management, the medical team, or coach in the absence of medical
personnel, should assess the athlete to determine the presence or absence of a concussion. The
current version of the Sport Concussion Assessment Tool (SCAT) is an assessment tool that is
readily available and can assist with the assessment. The athlete should be monitored for
worsening or change in signs and symptoms over the next 24 hours. Instructions should be given
to the parent or guardian as to signs and symptoms that may require further or more emergent
evaluation.
6. Management of a Concussion and Return to Play
a. An athlete determined to have a concussion or have concussion-like symptoms will be removed
from practice or competition and is not allowed to return to practice or competition that same day.
b. If an athlete displays concussion-like signs or symptoms, the athlete should be assumed to have a
concussion until further medical evaluation can occur. “WHEN IN DOUBT, SIT THEM OUT!”
c. Written clearance from a physician (MD or DO), Advanced Nurse Practitioner in written
collaborative practice with a physician, Certified Physician Assistant in written collaborative
practice with a physician, Athletic Trainer or Neuropsychologist in written supervision of a
physician must be provided prior to return to play.
d. Following a concussion, current accepted guidelines on physical and cognitive activity should be
practiced until symptoms have resolved.
e. An athlete must be asymptomatic at rest and with exertion prior to return to play
f. A graduated return to play progression should be followed to guide return to activity following
medical clearance as outlined on the MSHSAA Concussion Return to Play form.
1
Recommendations and Guidelines for Minimizing Head
Impact Exposure and Concussion Risk in Football
National Federation of State High School Associations (NFHS)
Report from the July 2014 NFHS Concussion Summit Task Force
The National Federation of State High School Associations (NFHS) and its member associations
firmly believe that athletic participation by students promotes health and fitness, academic
achievement, healthy lifestyles, and good citizenship. While there will always be a risk of injury,
minimizing the risk of head trauma and concussion in all sports is a priority for the NFHS. Over the
past several years, the NFHS and the NFHS Sports Medicine Advisory Committee (SMAC) have:
1) Produced a 20-minute online educational course with the Centers for Disease Control (CDC)
on “Concussion in Sports.”
2) Specifically addressed concussion management in the rules books of all sports, including
football.
3) Written several Points of Emphasis in the football rules book focused on limiting helmet-to-
helmet contact and blows to the head with the shoulder, forearm, and hand.
4) Disseminated multiple publications regarding concussion management to the member state
associations.
In July of 2014, at the request of the NFHS Board of Directors, a task force of medical and scientific
experts, high school football coaches, state association personnel, and representatives of several
stakeholder organizations met to discuss strategies to reduce head impacts and minimize concussion
risk in high school football players during contests and practices, as well as during activities
conducted outside of the traditional fall football season (spring and summer practices). The
Fundamentals outlined below represent the task force’s recommendations and guidelines developed
following two days of presentations and discussion of the relevant medical literature and current
expert opinion.
The members of the task force fully acknowledge the present limited – though evolving – scientific
evidence available to support the Fundamentals outlined below with absolute certainty and explicit
detail. Accordingly, the outcomes and clinical relevance of an increasing number of research studies
may eventually alter these recommendations and guidelines. Ideally, this emerging data will clarify
the potential for long-term adverse cognitive, emotional, and/or neurologic effects from concussions
and repetitive blows to the head that may not result in the clinical symptoms of concussion. Based on
what is currently known, the guiding principles in developing this report for young athletes and those
who oversee, support and administer high school football programs were to reasonably limit overall
2
exposure to multiple blows to the head and body (head impact exposure) and minimize concussion
risk, while maintaining the integrity of the game and attempting to avoid unintended consequences.
The Fundamentals below are designed to allow flexibility for the state associations that collectively
oversee the more than 15,000 high schools playing football across the country. The teams fielded by
these schools may vary tremendously in the number of available players. Team size dictates
numerous variables that may affect an athlete’s potential head impact exposure. Those variables
cannot be easily accounted for by stringent guidelines. For example:
An athlete playing on offense, defense and special teams will have greater cumulative head
impact exposure and will be at higher risk for injury than an athlete playing a single position.
The fewer the number of players on a team, the greater the chance some players will need to
participate in repeated drills, raising head impact exposure and potential injury risk.
As additional evidence emerges, these Fundamentals will evolve and may become more or less
restrictive. While the current level of knowledge keeps this task force from making proposals that are
specific and rigid, there is consensus that lessening the frequency of contact (and thus head impact
exposure) is likely beneficial to overall brain health. The task force also recognizes multiple
contributing factors that affect head impact exposure and the parallel effects on an individual football
player’s brain. For example:
Position played (linemen receive more total blows than other positions)
Two-way players versus those who only play offense or defense
Tackling and blocking techniques
Practice frequency and duration
Players that practice and/or compete on multiple levels (such as varsity and sub-varsity)*
Concussion history
Genetic predisposition to concussion
*Note: This contributing factor was added to the document by the NFHS SMAC.
It is very likely that each athlete has a unique level of resilience or susceptibility to concussion and
further brain injury. While there is currently no definitive way to measure or quantify this resilience or
susceptibility, the task force recommends reasonably limiting head impact exposure through the
Fundamentals presented below. Individual risk factors that are modifiable, such as position played,
total time spent on field, and sport technique, must be also considered when implementing contact
limitations.
Fundamentals for Minimizing Head Impact Exposure and Concussion Risk in Football
1. Full-contact should be limited during the regular season, as well as during activity outside of the
traditional fall football season. For purposes of these recommendations and guidelines, full-contact
consists of both “Thud” and “Live Action” using the USA Football definitions of Levels of Contact.
Rationale: By definition, “Thud” involves initiation of contact at, or up to, full speed with no
pre-determined winner and no take-down to the ground. Accordingly, the task force supports
that initial contact, particularly with linemen, is just as violent with “Thud” as with “Live Action.”
However, the task force also recognizes that “Live Action” likely carries a higher risk for other
3
injuries to the body than does “Thud.” The USA Football Levels of Contact “Air,” “Bags,” and
“Control” are considered no- or light-contact, and thus no limitations are placed on their use.
2. Member state associations should consider a variety of options for limiting contact in practices.
The task force strongly recommends full-contact be allowed in no more than 2-3 practices per week.
Consideration should also be given to limiting full-contact on consecutive days and limiting full-contact
time to no more than 30 minutes per day and no more than 60-90 minutes per week.
Rationale: The task force acknowledges that there are insufficient data to specify with
certainty a research-validated “best practices” standard for contact limitations. Several states
(Alabama, Arizona, Maryland, and Texas) adopted varying limitations on contact prior to the
2013 football season. Preliminary High School RIO injury surveillance data suggest these
states have seen a statistically significant decrease in concussion rates during practices, with
no increase in concussion or other injuries during games.
3. Pre-season practices may require more full-contact time than practices occurring later in the
regular season, to allow for teaching fundamentals with sufficient repetition.
A. Pre-season acclimatization protocols and regulations regarding heat and hydration take
precedent and should always be followed.
B. While total full-contact practice days and time limitations may be increased during the pre-
season, the emphasis should focus on the proper principles of tackling and blocking during the
first several practices, before progressing to “Thud” and “Live Contact.”
Rationale: The task force acknowledges regular season practice limitations may need to be
revised during the pre-season. This should be done in a specific and systematic manner to
allow coaches to spend sufficient time teaching proper tackling and blocking techniques.
Emphasis should be placed upon inexperienced players, as they slowly work through tackling
and blocking progressions with “Air,” “Bags,” and “Control” using the USA Football definitions
of “Levels of Contact.”
4. During pre-season twice-daily practices, only one session per day should include full contact.
Rationale: The adolescent brain needs sufficient recovery time following full-contact
practices. In addition, concussion signs and/or symptoms may not develop for several hours
after the initial injury.
5. Each member state association should review its current policies regarding total quarters or
games played during a one-week time frame.
Rationale: High School RIO injury surveillance data consistently show that competition
presents the highest risk for concussion. The task force is concerned that participation in
games at multiple levels of competition during a single week increases risk for head injury and
unnecessarily increases head impact exposure. In addition, games played on consecutive
days or those scheduled on the same day (Freshman and Junior Varsity games or Junior
Varsity and Varsity games) may not allow the brain an opportunity to adequately recover.
Consideration should be given to moderating these situations as much as possible.
4
6. Consistent with efforts to minimize total exposure to full-contact, head impact exposure, and
concussion risk, member state associations with jurisdiction over football outside of the traditional fall
football season should review their current policies to assess if those policies stand in alignment with
the Fundamentals discussed within this report and, if needed, modify the policies accordingly.
Rationale: Football played outside of the traditional fall football season presents an
opportunity for learning, physical activity, and skill development. However, athletes are at
further risk for head impact exposure and concussion during any full-contact activity.
Consideration should be given to significantly limiting the total time of full contact. Other factors
to consider include time elapsed since the previous football season and whether individual
athletes have recently been, or are currently, participating in other contact/collision sports (e.g.,
Ice Hockey, Lacrosse, Soccer and Wrestling).
7. Each member state association should reach out to its respective state coaches’ association on
designing and implementing a coach education program that appropriately integrates youth, middle
school, and high school football programs in every community. USA Football and the NFHS
Fundamentals of Coaching courses should be the primary education resources for all coaches.
Education for coaches should also include the proper fitting and care of helmets.
Rationale: The game of football continues to evolve and proper coaching technique at each
level is fundamental to keeping the game safe and enjoyable. A proper fitting helmet may help
decrease, but not eliminate concussion risk.
8. Each member state association should regularly educate its schools on current state concussion
law and policies and encourage schools to have a written Concussion Management Protocol. Schools
should also be encouraged to share this information with coaches, parents, and students annually.
Rationale: Many schools experience frequent turnover of Athletic Directors and coaches.
Frequent “refreshers” on state concussion laws and policies as well as sample concussion
management protocols should be made available to ensure all schools are current on, and
prepared for, safe and effective concussion management.
9. An Emergency Action Plan (EAP) with clearly defined written and practiced protocols should be
developed and in place at every high school. When possible, an athletic trainer should be present at
all practices and games.
Rationale: An effective EAP should be in place, as a prompt and appropriate response to any
emergency situation can save a life. The EAP should be designed and practiced to address all
teams (Freshman, Junior Varsity, and Varsity) and all practice and game sites. An athletic
trainer is a key component in any strategy to minimize injury risk and optimize safety for all
participants.

5
Resources:
Bailes JE, Petraglia AL, Omalu BI, Nauman E, Talavage T. Role of subconcussion in repetitive mild
traumatic brain injury. J Neurosurg. 2013 Nov;119(5):1235-45.
Breedlove EL, Robinson M, Talavage TM, Morigaki KE, Yoruk U, O'Keefe K, King J, Leverenz LJ,
Gilger JW, Nauman EA. Biomechanical correlates of symptomatic and asymptomatic
neurophysiological impairment in high school football. J Biomech. 2012 Apr 30;45(7):1265-72.
Broglio SP, Cantu RC, Gioia GA, Guskiewicz KM, Kutcher J, Palm M, Valovich McLeod TC. National
Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014
Mar-Apr;49(2):245-65.
Broglio SP, Martini D, Kasper L, Eckner JT, Kutcher JS. Estimation of head impact exposure in high
school football: implications for regulating contact practices. Am J Sports Med. 2013
Dec;41(12):2877-84.
Broglio SP, Eckner JT, Martini D, Sosnoff JJ, Kutcher JS, Randolph C. Cumulative head impact
burden in high school football. J Neurotrauma. 2011 Oct;28(10):2069-78.
Davenport EM, Whitlow CT, Urban JE, Espeland MA, Jung Y, Rosenbaum DA, Gioia GA, Powers AK,
Stitzel JD, Maldjian JA. Abnormal White Matter Integrity Related to Head Impact Exposure in a
Season of High School Varsity Football. J Neurotrauma. 2014 Jul 14. [Epub ahead of print].
Urban JE, Davenport EM, Golman AJ, Maldjian JA, Whitlow CT, Powers AK, Stitzel JD.
Head impact exposure in youth football: high school ages 14 to 18 years and cumulative impact
analysis. Ann Biomed Eng. 2013 Dec;41(12):2474-87.
Approved by the NFHS Concussion Summit Task Force in August 2014; Approved by the
NFHS SMAC in October 2014; and Approved by the NFHS Board of Directors in October 2014.
DISCLAIMER – NFHS Position Statements and Guidelines
The NFHS regularly distributes position statements and guidelines to promote public awareness of certain health and safety-related issues. Such
information is neither exhaustive nor necessarily applicable to all circumstances or individuals, and is no substitute for consultation with appropriate
health-care professionals. Statutes, codes or environmental conditions may be relevant. NFHS position statements or guidelines should be considered in
conjunction with other pertinent materials when taking action or planning care. The NFHS reserves the right to rescind or modify any such document at
any time.

1
A PARENT’S / GUARDIAN’S GUIDE TO CONCUSSION
National Federation of State High School Associations (NFHS)
Sports Medicine Advisory Committee (SMAC)
What is a concussion?
A concussion is a traumatic brain injury that interferes with the normal function of the brain.
Concussions were previously referred to as a “ding” or a “bell-ringer” but this undermines the
seriousness of problem. Any suspected concussion must be taken very seriously. An athlete does not
need to lose consciousness (be “knocked-out”) to suffer a concussion. In fact, less than 5% of
concussed athletes suffer a loss of consciousness.
Concussion Facts
Structural injuries, like torn ligaments and broken bones, can be seen on an x-ray or on scans like an
MRI. On the other hand, a concussion is a disruption of how the brain works, or its function, and not in
its structure. That is why CAT scans and MRIs are typically normal. The injury affects the way the brain
works, not how it looks.
It is estimated that over 300,000 high school athletes across the United States suffer a concussion each
year. (Data from the NFHS Injury Surveillance System, “High School RIO
TM
”)
Concussions can happen in any sport. While they are more common in sports that involve collisions,
athletes in all sports are at risk for a concussion. When researchers looked at 14 different high school
sports, they found that over two-thirds of concussions result from contact with another athlete and the
second leading cause of concussion, is player-to-surface contact. This includes falling and hitting the
ground.
An athlete may report many physical, behavioral, and cognitive symptoms. Physical symptoms include
headaches, nausea, vomiting, dizziness, and sleep changes. Some behavioral changes include
irritability, anxiety, and depression. Cognitive symptoms are changes in the way we think and include
feeling sluggish, hazy, or foggy, difficulty concentrating or memory problems, and confusion.
Many symptoms appear immediately after the injury, while others may develop over the next several
days. The symptoms can interfere with normal daily life in addition to difficulty with school, work, and
social life.
Concussion symptoms may last from a few days to several months. It is important to remember that
each student athlete responds and recovers differently.
Athletes should not return to sports or activities that will put them at risk for another head injury until
the concussion has completely resolved. To do so puts them at risk for worsening and prolonged
symptoms and a more severe injury. While rare, a repeat concussion can also result in severe swelling
and bleeding in the brain. This condition can lead to death or permanent disability.

2
What should I do if I think my child has had a concussion?
If your child sustains a head injury, it is good to be aware of the signs and symptoms of a concussion. If you
suspect an athlete has a concussion, the athlete must be immediately removed from activity. Continuing to
participate in a contact or collision sport while experiencing concussion symptoms can lead to worsening of
symptoms, increased risk for further injury and sometimes death.
Parents and coaches should not make the diagnosis of a concussion. Any athlete suspected of having a
concussion should be evaluated by a medical professional trained in the diagnosis and management of
concussions.
When in doubt, sit them out!
All athletes who sustain a concussion need to be evaluated by an appropriate health-care professional who is
experienced in concussion management. If your child's school has an athletic trainer (AT), please inform the
AT of your concerns. You should also call your child’s primary care provider and explain what has happened
and follow the instructions you are given. Sometimes, an injury is more severe than it appears. If your child
has persistent vomiting, a worsening headache, a seizure, or is acting differently, you should take your child to
an emergency department for immediate attention.
What are the signs and symptoms of a concussion?
SIGNS OBSERVED BY PARENTS,
ATHLETIC TRAINERS, FRIENDS,
TEACHERS OR COACHES
SYMPTOMS REPORTED BY
ATHLETE
• Dazed or stunned appearance.
• Headache or “pressure” in
head.
• Confusion about assignment or
position.
• Nausea
• Forgetfulness.
• Balance problems or dizziness
• Uncertainty of game, score, or
opponent.
• Double or blurry vision
• Clumsy movements.
• Sensitivity to light or noise
• Slow response to questions.
• Feeling sluggish, hazy, foggy
or groggy
• Mood, behavior or personality
changes.
• Concentration or memory
problems
• Can’t recall events prior to or after
hit or fall.
• Confusion
• “Not feeling right” or “feeling
down”

3
How can a concussion affect schoolwork?
Following a concussion, many students have difficulty in school due to difficulties with short-term memory,
concentration, and organization.
In many cases after the injury, it is best to decrease the athlete’s class load early in the recovery phase. This
may include staying home from school for no more than 1 or 2 days, followed by academic adjustments (such
as a reduced class schedule), until the athlete has fully recovered. Decreasing the stress on the brain and not
allowing the athlete to push through symptoms will shorten the recovery time and ensure total resolution of
symptoms. The academic adjustments are best managed by a school concussion team. Speak with the school
guidance counselor, school nurse, or athletic trainer to help with this process.
When can an athlete return to play following a concussion?
After suffering a concussion, or if you suspect an athlete has a concussion, no athlete should EVER return to
play or practice on that same day.
Concerns over athletes returning to play too quickly led lawmakers in all 50 states and the District of Columbia
to pass laws stating that no player shall return to play the day of a concussion, and the athlete must be
cleared by an appropriate health-care professional before being allowed to return to play in either games or
practices. Many of these laws require players, parents and coaches to receive education on the dangers of
concussion in addition to recognizing the signs and symptoms of concussion. Click here to see what your
state law requires:
http://www.ucdenver.edu/academics/colleges/medicalschool/departments/pmr/documents/concussion_t
oolkit/laws/state.htm
Once an athlete no longer has symptoms of a concussion AND is cleared by an appropriate health-care
professional to begin a return to play progression, the athlete must proceed with activity in a step-wise
fashion in a carefully controlled and monitored environment to allow the brain and body to re-adjust to
exertion. On average, the athlete will complete a new step every 24-48 hours. An example of a typical return-
to-play schedule is shown below:
Return to Play Progression:
Step 1: Back to Regular Activities
To enter into the return to play protocol the athlete should first be back to regular activities (such as school)
and has the cleared by their health-care professional to begin the return to play process. In most all cases, the
athlete should have all concussion-related academic adjustments removed prior to beginning the Return to
Play Program.
Step 2: Light Aerobic Activity
Begin with light aerobic exercise only to increase heart rate. This means about 5 to 10 minutes on an exercise
bike, brisk walking, or light jogging. No anaerobic activity such as weight lifting should be done at this stage.
Step 3: Moderate Activity
Continue with activities that increase an athlete’s heart rate while adding movement. This includes running
and skating drills.

4
Step 4: Non-Contact Training Activity
Add sports specific, more intense, non-contact physical activity, such as such as passing in hockey, dribbling in
basketball or soccer, high-intensity stationary biking, regular weightlifting routine.
Step 5: Practice and Full Contact
The athlete may return to practice and full contact (if appropriate for the sport) in a controlled practice setting
where the skills can be assessed by the coaches.
Step 6: Competition
The athlete may return to competition.
If symptoms occur at any step, the athlete should immediately stop activity and consult with
a qualified appropriate health-care professional before moving on to the next step.
What can I do?
Both you and your child should learn to recognize the “Signs and Symptoms” of concussion as listed
above.
Encourage your child to tell the medical and/or coaching staff if any of these signs and symptoms
appear after a blow to the head or body.
Emphasize to administrators, coaches, physicians, athletic trainers, teachers and other parents your
concerns and expectations about concussion and safe play.
Encourage your child to tell the medical and coaching staff if there is suspicion that a teammate has
suffered a concussion.
Ask teachers to monitor any decrease in grades or changes in behavior in students that could indicate a
concussion.
Report concussions that occurred during the school year to appropriate school staff. This will help in
monitoring injured athletes as they move to the next season’s sports.
Click here for more information about returning to school after a concussion:
http://www.cdc.gov/headsup/basics/return_to_school.html
Other Frequently Asked Questions:
Why is it so important that athletes not return to play until they have completely recovered from a
concussion?
Students that return to play too soon may worsen concussion symptoms, prolong the recovery time, and they
also risk catastrophic consequences if they suffer another head injury. These consequences are preventable if
each athlete is allowed time to recover from their concussion including completing the stepwise return-to-play
protocol. No athlete should return to sport or other at-risk activity when signs or symptoms of concussion are
present and recovery is ongoing.
Is a “CAT scan” or MRI needed to diagnose a concussion?
No! The diagnosis of a concussion is based upon the athlete’s history of the injury and an appropriate health-
care professional’s physical examination and testing. CT and MRI scans are rarely needed following a

5
concussion since this is a functional injury and not a structural one. However, they are helpful in identifying
life-threatening head and brain injuries such as skull fractures, bleeding or swelling.
What is the best treatment to help my child recover quickly from a concussion?
Treatment for concussion varies from one person to the next. Immediately after a concussion, the best
treatment is physical and cognitive rest. Exposure to loud noises, bright lights, computers, tablets, video
games, television and smart phones may worsen the symptoms of a concussion. You should allow your child
to rest in the days following a concussion. As the symptoms lessen, an appropriate health-care professional
may allow increased physical and cognitive activity, but this has to be monitored closely for a recurrence of
symptoms.
There are no medications to treat concussions, but an appropriate health-care professional may prescribe
medications and therapies to treat symptoms of a concussion, such as headache, dizziness, sleep changes, etc.
Some athletes may require rehabilitative therapies, such as physical, occupational, vestibular, ocular or
speech/cognitive. Others may require treatment for mood and behavior changes. All of these interventions
are done on a personalized basis.
How long do the symptoms of a concussion usually last?
For most concussions, symptoms will usually go away within 2–3 weeks after the initial injury. You should
anticipate that your child will not fully participate in sports for several weeks following a concussion. In some
cases, symptoms may last longer, sometimes several months. Since recovery differs from person to person, all
concussions should be carefully managed.
How many concussions can an athlete have before we should consider retiring from playing sports?
There is no “magic number” of concussions that determine when an athlete should give up playing sports that
put one at high risk for a concussion. The circumstances that surround each individual injury, such as how the
injury occurred as well as the number and duration of symptoms following the concussion, are very important.
These circumstances must be individually considered when assessing an athlete’s risk for potential long-term
consequences and potentially more serious brain injuries. The decision to “retire” from sports is a decision
best reached after a complete evaluation by your child’s primary care provider and consultation with an
appropriate health-care professional who specializes in treating concussions.
I’ve read recently that concussions may cause long-term brain damage in athletes, especially professional
football players. Is this a risk for high school athletes who have had a concussion?
Recently, increasing attention has been directed at CTE or Chronic Traumatic Encephalopathy. CTE is a brain
disease that results from changes in the brain. These changes can affect how a person thinks, feels, acts, and
moves. The cause of CTE has not been definitively established. Traumatic brain injuries, including
concussions, and repeated hits to the head, called sub-concussive head impacts, may contribute to CTE.
Sub-concussive head impacts are impacts to the head that do not cause a concussion. Unlike concussions,
which cause symptoms, sub-concussive head impacts do not cause symptoms. A collision while playing sports
is one way a person can get a sub-concussive head impact.
Early evidence suggested that the more years a person has repeated sub-concussive head impacts or other
brain injuries, the higher the chance they have of getting CTE. However, we have now learned that CTE does

6
not just occur in athletes. And, most people with head impacts or brain injuries will not get CTE. Furthermore,
CTE has been diagnosed in people who have never had any history of brain trauma.
In light of the suggestion of a correlation between head impacts and CTE, the NFHS SMAC recommends
limiting full contact during practice sessions and limiting the total number of quarters or periods played per
week in sports at high risk for head impacts, such as football and ice hockey. These recommendations and
guidelines were defined in the report from the July 2014 NFHS Concussion Summit Task Force. The guiding
principles used to develop this report were to reasonably limit the opportunity for multiple hits to the head
and to minimize concussion risk. The goal is also to maintain the integrity of the games and avoid unintended
consequences. The report can be read in its entirety in the Resources section on the Sports Medicine page of
the NFHS Website.
We cannot eliminate all of the risk of concussion from sports. However, we can take what we learn from
science to reduce the chance for injury and set policy to ensure that students with a concussion get the care
they need.
Everyone involved in high school sports plays an active role in educating others about concussion and other
serious brain injuries. Please check out the Resource section on the Sports Medicine page of the NFHS
Website for more information on how you can take an active role and get involved in keeping students safe,
healthy and active.
Some of this information has been adapted from the CDC’s “Heads Up: Concussion in High School Sports”
materials by the NFHS’s Sports Medicine Advisory Committee. Please go to
www.cdc.gov/ncipc/tbi/Coaches_Tool_Kit.htm for more information.
Revised and Approved April 2019
April 2016
April 2013
April 2010
DISCLAIMER – NFHS Position Statements and Guidelines
The NFHS regularly distributes position statements and guidelines to promote public awareness of certain health and safety-related issues. Such information is
neither exhaustive nor necessarily applicable to all circumstances or individuals and is no substitute for consultation with appropriate health-care professionals.
Statutes, codes or environmental conditions may be relevant. NFHS position statements or guidelines should be considered in conjunction with other pertinent
materials when taking action or planning care. The NFHS reserves the right to rescind or modify any such document at any time.

1
SUGGESTED GUIDELINES FOR MANAGEMENT OF
CONCUSSION IN SPORTS
National Federation of State High School Associations (NFHS)
Sports Medicine Advisory Committee (SMAC)
Introduction
A concussion is a type of traumatic brain injury that impairs the function of the brain. It occurs when the
brain moves within the skull as a result of a blow to the head or body. What may appear to be only a mild jolt
or blow to the head or body can result in a concussion or other serious brain injury.
The understanding of sports-related concussion continues to evolve. We now know that young athletes are
particularly vulnerable to the effects of a concussion. Once considered a “ding” to the head, it is now
understood that a concussion has the potential to result in a variety of short- or long-term changes in brain
function and, rarely, death.
What is a concussion?
A concussion is a traumatic brain injury that interferes with the normal function of the brain. Simply stated – a
concussion results from an injury to the brain, and there is no such thing as a minor brain injury! Concussions
should never be referred to as a “ding” or a “bell-ringer.” Any suspected concussion must be taken very
seriously.
An athlete does not need to lose consciousness (be “knocked-out”) to suffer a concussion. In fact, less than
5% of concussed athletes suffer a loss of consciousness.
What happens to the brain during a concussion is not completely understood. It is a complex process,
primarily affecting the function of the brain. The sudden movement of the brain causes stretching and tearing
of brain cells, damaging the cells and creating chemical changes in the brain. Once this injury occurs, the brain
is vulnerable to further injury and very sensitive to any increase in stress, such as another head injury, until it
fully recovers.
Common sports injuries such as torn ligaments and broken bones are structural injuries that can be seen on x-
rays or MRI. A concussion, however, is an injury that interferes with how the brain works and cannot be seen
on MRI or CT scans. Therefore, even though the brain is injured, the brain looks normal on these tests.
Recognition and Management
If an athlete exhibits any signs, symptoms, or behaviors that make you suspicious of a concussion, the athlete
must be removed from play and not be allowed to return to play until they are evaluated and cleared by a
health-care professional. Failure to remove the athlete from activity puts them at risk for sustaining another

2
head injury while concussed, which can lead to worsening concussion symptoms, increased risk for further
injury, and, sometimes even death.
Parents/guardians and coaches are not expected to “diagnose” a concussion. However, everyone involved in
athletics must be aware of the signs, symptoms and behaviors associated with a concussion. If you suspect
that an athlete may have a concussion, then the athlete must be immediately removed from all physical
activity.
Signs Observed by Coaching Staff
• Dazed or stunned appearance.
• Confusion about assignment or position.
• Forgetfulness.
• Uncertainty of game, score, or opponent.
• Clumsy movements.
• Slow response to questions.
• Mood, behavior or personality changes.
• Can’t recall events prior to or after hit or fall.
Symptoms Reported by Athlete
• Headache or “pressure” in head.
• Nausea.
• Balance problems or dizziness.
• Double or blurry vision.
• Sensitivity to light or noise.
• Feeling sluggish, hazy, foggy or groggy.
• Concentration or memory problems.
• Confusion.
• Emotions of “not feeling right” or “feeling down”.
When in doubt, sit them out!
If you suspect that a player has a concussion, follow the “Heads Up” 4-step Action Plan.
1. Remove the athlete from play.
2. Ensure the athlete is evaluated by an appropriate health-care professional.
3. Inform the athlete’s parents/guardians about the possible concussion and give them information on
concussion.
4. Keep the athlete out of play the day of the injury, and until an appropriate health-care professional has
given written clearance that the athlete is symptom-free and may return to activity.
The signs and symptoms associated with a concussion are not always apparent immediately after a bump,
blow, or jolt to the head or body and may develop over a few hours or longer. However, until an athlete is
evaluated by an appropriate health-care professional, they should be closely watched following a suspected
concussion and should not be left alone.
3
Athletes should never try to “tough out” a concussion. Teammates, parents/guardians, and coaches should
never encourage an athlete to “play through” the symptoms of a concussion. In addition, there should never
be an attribution of bravery or courage to athletes who play despite having concussion signs and/or
symptoms. The risks of such behavior must be emphasized to all members of the team, as well as coaches and
parents.
If an athlete returns to activity before being fully healed from an initial concussion, their reaction time and
reflexes may be compromised, placing the athlete at greater risk for sustaining another head injury. A second
injury that occurs before the brain has a chance to recover from the initial concussion will delay recovery and
increase the chance for long-term problems. In rare cases, a repeat head injury can result in severe swelling
and bleeding in the brain that can be fatal.
What Are Some Danger Signs to Look Out For?
In rare cases, a dangerous collection of blood (hematoma) may form between the brain and skull after a
bump, blow, or jolt to the head or body. The pressure from this blood can squeeze the brain within the skull.
Call 9-1-1 for any athlete that demonstrates any of the following signs or symptoms after a bump, blow, or jolt
to the head or body for transport to the emergency department:
• One pupil larger than the other.
• Drowsiness or inability to wake up.
• A headache that gets worse and does not go away.
• Slurred speech, weakness, numbness, or decreased coordination.
• Repeated vomiting or nausea
• Convulsions or seizures (shaking or twitching).
• Unusual behavior, increased confusion, restlessness, or agitation.
• Loss of consciousness (passed out/knocked out). Even a brief loss of consciousness should be taken
seriously.
Management Until Recovery
Rest
The first step in recovering from a concussion is rest. Rest is essential to help the brain heal. Athletes with a
concussion need rest from physical and mental activities that require concentration and attention as these
activities may worsen symptoms and delay recovery. Exposure to loud noises, bright lights, computers, video
games, television and phones (including texting) all may worsen the symptoms of concussion. Athletes
typically require 24-48 hours of rest, though some may require a longer period of time.
Return to Learn
Following a concussion, many athletes will have difficulty in school. These problems may last from days to
weeks and often involve difficulties with short- and long-term memory, concentration, and organization. In
many cases, it is best to lessen the student’s class load early on after the injury. This may include staying
home from school during the short period of rest (typically no more than 1-2 days) followed by a lighter school
schedule for a few days, or longer, if necessary. Decreasing the stress to the brain in the early phase after a
concussion may lessen symptoms and shorten the recovery time. Additional academic adjustments may
include decreasing homework, allowing extra time for assignments/tests, and taking breaks during class. Such
academic adjustments are best made using a team approach collaborating with teachers, counselors, and
school nurses.

4
Return to Play
After suffering a concussion, no athlete should return to play or practice on that same day.
An athlete should never be allowed to resume play following a concussion until symptom free and given the
approval to resume physical activity by an appropriate health-care professional.
Once an athlete no longer has signs or symptoms of a concussion and is cleared to return to activity by an
appropriate health-care professional, they should proceed in a step-wise fashion to allow the brain to re-
adjust to exercise. In most cases, the athlete should progress no more than one step each day, and at times
each step may take more than one day. Below is an example of a return to physical activity program:
Progressive Return to Play Protocol
Step 1: Back to Regular Activities (such as school)
To enter into the stepwise return to play protocol the athlete should first be back to regular activities (such as
school) and has been cleared by their appropriate health-care professional to begin the return to play process.
In most all cases, the athlete should have all concussion-related academic adjustments removed prior to
beginning the Return to Sports Activity Program
Step 2: Light Aerobic Activity
Begin with light aerobic exercise only to increase heart rate. This means about 5 to 10 minutes on an exercise
bike, brisk walking, or light jogging. No anaerobic activity such as weight lifting should be done at this stage.
Step 3: Moderate Activity
Continue with activities that increase an athlete’s heart rate while adding movement. This includes running
and skating drills.
Step 4: Non-Contact Training Activity
Add sports specific, more intense, non-contact physical activity, such as such as passing in hockey, dribbling in
basketball or soccer, high-intensity stationary biking, regular weightlifting routine.
Step 5: Practice and Full Contact
The athlete may return to practice and full contact (if appropriate for the sport) in a controlled practice setting
where the skills can be assessed by the coaches.
Step 6: Competition
The athlete may return to competition.
If symptoms of a concussion recur, or if concussion signs and/or behaviors are observed at any time during
the return-to-play program, the athlete must discontinue all activity immediately. The athlete may need to
be re-evaluated by the appropriate health-care professional or may have to return to the previous step of
the return-to-activity program, as pre-determined by the appropriate health-care professional.
Summary of Suggested Concussion Management
1. No athlete should return to play (RTP) or practice on the same day of a concussion.
2. Any athlete suspected of having a concussion should be evaluated by an appropriate health-care
professional.

5
3. Any athlete diagnosed with a concussion should have written clearance from an appropriate
health-care professional prior to resuming participation in any practice or competition.
4. After medical clearance, RTP should follow a step-wise protocol as outlined above with
provisions for delayed RTP based upon return of any signs or symptoms.
References:
Halstead ME, Walter KD, Moffatt K; COUNCIL ON SPORTS MEDICINE AND FITNESS.
Sport-Related Concussion in Children and Adolescents. Pediatrics. 2018 Dec;142(6). pii: e20183074. doi:
10.1542/peds.2018-3074. Epub 2018 Nov 12.
McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, Cantu RC, Cassidy D, Echemendia RJ,
Castellani RJ, Davis GA, Ellenbogen R, Emery C, Engebretsen L, Feddermann-Demont N, Giza CC, Guskiewicz
KM, Herring S, Iverson GL, Johnston KM, Kissick J, Kutcher J, Leddy JJ, Maddocks D, Makdissi M, Manley GT,
McCrea M, Meehan WP, Nagahiro S, Patricios J, Putukian M, Schneider KJ, Sills A, Tator CH, Turner M, Vos
PE. Consensus statement on concussion in sport-the 5th international conference on concussion in sport
held in Berlin, October 2016. Br J Sports Med. 2017 Jun;51(11):838-847. doi: 10.1136/bjsports-2017-097699.
Epub 2017 Apr 26.
Additional Resources:
Brain 101 – The Concussion Playbook.
Concussion in Sports- What you need to know.
https://nfhslearn.com/courses/61151/concussion-in-sports
Heads Up: Concussion in High School Sports
http://www.cdc.gov/concussion/headsup/high_school.html
REAP Concussion Management Program.
http://www.rockymountainhospitalforchildren.com/sports-medicine/concussion-management/reap-
guidelines.htm
Revised and Approved April 2019
April 2017
October 2013
January 2011
April 2009
October 2008
October 2005
DISCLAIMER – NFHS Position Statements and Guidelines
The NFHS regularly distributes position statements and guidelines to promote public awareness of certain health and safety-related issues. Such information is
neither exhaustive nor necessarily applicable to all circumstances or individuals and is no substitute for consultation with appropriate health-care professionals.
Statutes, codes or environmental conditions may be relevant. NFHS position statements or guidelines should be considered in conjunction with other pertinent
materials when taking action or planning care. The NFHS reserves the right to rescind or modify any such document at any time.

Revised 3/1/18
MSHSAA Concussion Return to Play Form
If diagnosed with a concussion, an athlete must be cleared for progression to activity by an approved healthcare provider,
MD/DO/PAC/LAT/ARNP/Neuropsychologist (Emergency Room physician cannot clear for progression).
Athlete’s Name: DOB: Date of Injury:
THIS RETURN TO PLAY IS BASED ON TODAY’S EVALUATION
Date of Evaluation: Return to School On (Date):
The following are the return to physical activities recommendations at the present time:
□ Diagnosed with a concussion: Cannot return to physical activity, sport or competition (must be re-evaluated).
□ Diagnosed with a concussion: May return to sports participation under the supervision of your school’s
administration after completing the return to play protocol (see below).
□ Not diagnosed with a concussion. Patient has diagnosis of _____________________________________________
and MAY/MAY NOT return to play at this time.
Medical Office Information (Please Print/Stamp):
Evaluator’s Name: Office Phone:
Evaluator’s Specialty:
Evaluator’s Signature:
Evaluator’s Address:
Return to Play (RTP) Procedures After a Concussion
Return to activity and play is a medical decision. Progression is individualized, must be closely supervised according to the school’s
policies and procedures, and will be determined on a case-by-case basis. Factors that may affect the rate of progression include:
previous history of concussion, duration and type of symptoms, age of the athlete, and sport/activity in which the athlete participates.
An athlete with a prior history of concussion, one who has had an extended duration of symptoms, or one who is participating in a
collision or contact sport may be progressed more slowly as determined by the healthcare provider who has evaluated the athlete.
After the student has not experienced symptoms attributable to the concussion for a minimum of 24 hours and has returned to school
on a full-time basis (if school is in session), the stepwise progression below shall be followed:
Step 1: Light cardiovascular exercise.
Step 2: Running in the gym or on the field. No helmet or other equipment.
Step 3: Non-contact training drills in full equipment. Weight-training can begin.
Step 4: Full, normal practice or training (a walk-through practice does not count as a full, normal practice).
Step 5: Full participation. Must be cleared by MD/DO/PAC/LAT/ARNP/Neuropsychologist before returning to play.
The athlete should spend a minimum of one day at each step before advancing to the next. If concussion symptoms return with any
step, the athlete must stop the activity and the treating healthcare provider must be contacted. Depending upon the specific type and
severity of the symptoms, the athlete may be told to rest for 24 hours and then resume activity at a level one step below where he or
she was at when the symptoms returned.
Return to Play Protocol (Steps 1-4) Completed (Date/Signature):
Cleared for Return to Play (Step 5) by: Date:
I accept responsibility for reporting all injuries and illnesses to my school and medical staff (athletic trainer/team physician) including any signs and
symptoms of a CONCUSSION.
Signature of Student Athlete: _______________________________________________ Date: _____________
May be advanced back to competition after phone conversation with the healthcare professional that evaluated the athlete
(MD/DO/PAC/LAT/ARNP/Neuropsychologist) and documented above.
This form is adapted from the Acute Concussion Evaluation (ACE) care plan on the CDC website (www.cdc.gov/injury). All medical providers are encouraged to
review this site if they have questions regarding the latest information on the evaluation and care of the scholastic athlete following a concussion injury.

WWW.MSHSAA.ORG • 573.875.4880
Missouri State High School Activities Association
1 North Keene St. • Columbia, MO 65201
@MSHSAAorg
