
This report was prepared by the Maryland
Department of Health pursuant to Maryland Code
Annotated, Health-General Article § 7.5–701. A copy
of this report was delivered to the Maryland General
Assembly pursuant to the Maryland State
Government Code § 2-1257 (2019).
Data
-
Informed Overdose Risk Mitigation
2022 Annual Report
Released: August 15, 2023
CONTENTS
I. EXECUTIVE SUMMARY .......................................................................................................... 3
Overview ........................................................................................................................................ 3
High-Level Findings......................................................................................................................... 3
Policy Implications .......................................................................................................................... 5
Next Steps ...................................................................................................................................... 6
II. OVERDOSE DEATHS IN MARYLAND ............................................................................... 8
Gender ............................................................................................................................................ 8
Age .................................................................................................................................................. 9
Race & Ethnicity ........................................................................................................................... 10
Geography .................................................................................................................................... 12
Educational Attainment ............................................................................................................... 13
Bystanders in Residential Settings ............................................................................................... 13
Medicaid Eligibility ....................................................................................................................... 14
Summary of Overdose Deaths in Maryland ................................................................................. 14
III. NON-FATAL OVERDOSES IN MARYLAND ..................................................................... 14
Demographics .............................................................................................................................. 15
Age ................................................................................................................................................ 15
Gender .......................................................................................................................................... 16
Race .............................................................................................................................................. 16
Geography .................................................................................................................................... 16
Payer Type .................................................................................................................................... 17
Post-NFOD Health Outcomes ....................................................................................................... 18
Post-NFOD Buprenorphine Access ............................................................................................... 19
Summary of Non-Fatal Overdoses in Maryland ........................................................................... 19
IV. OVERDOSE RISK FACTORS............................................................................................... 20
Drug Supply Characteristics.......................................................................................................... 20
HIDTA Drug Seizures ..................................................................................................................... 22
The Emergence of Xylazine .......................................................................................................... 22
Rapid Analysis of Drugs Program ................................................................................................. 23
Increasing Stimulant Use .............................................................................................................. 24
Recent Incarceration .................................................................................................................... 25
Comorbidities ............................................................................................................................... 25

MARYLAND DEPARTMENT OF HEALTH
2 | Page
Summary of Overdose Risk Factors .............................................................................................. 27
V. SERVICE UTILIZATION ........................................................................................................ 28
Medication for Opioid Use Disorder ............................................................................................ 28
Hospital-Level Data ...................................................................................................................... 33
Medicaid MOUD ........................................................................................................................... 59
Other (non-MOUD) Mental Health and SUD Services ................................................................. 61
Targeted Naloxone Distribution ................................................................................................... 61
Syringe Service Programs ............................................................................................................. 63
EMS Transportation ..................................................................................................................... 63
Hospital Characteristics ................................................................................................................ 64
Service Utilization by Medicaid Participants ................................................................................ 65
Summary of Service Utilization .................................................................................................... 67
Acknowledgments ........................................................................................................................ 68
VI. Considerations and Limitations to Analysis .............................................................. 69
Acronyms ...................................................................................................................................... 72
VII. DATA SOURCES & CITATIONS ......................................................................................... 73
VIII. APPENDIX A: CHRS ............................................................................................................. 74
IX. APPENDIX B: PBHS ............................................................................................................. 75
XI. APPENDIX C: JHSPH ........................................................................................................... 76
Non-Fatal Overdose Analysis ....................................................................................................... 76
MIEMSS ........................................................................................................................................ 81
XII. APPENDIX D: HSCRC .......................................................................................................... 84
XIV. APPENDIX E: EDDS ............................................................................................................. 87
XV. APPENDIX F: Medicaid (provided by Hilltop)............................................................. 88

DORM 2022 ANNUAL REPORT
3 | Page
I. EXECUTIVE SUMMARY
Overview
In 2018, House Bill (HB) 922, known as the Chapter 211 Act, was signed into law, requiring the Maryland
Department of Health (MDH) to produce an annual report examining the history of individuals in the State
of Maryland who suffered a fatal overdose (OD). As Chapter 211 specifies, this report shall include an
assessment of multiple factors associated with fatal and NFOD risk and programs and services related to
substance use (SU), among other issues., Where feasible, this report seeks to link de-identified, person-
level data from at least 18 distinct data sources or data sets possessed by multiple state agencies.
Collectively, the examination, collaboration, assessment, and report are subsequently referred to as the
Data-Informed Overdose Risk Mitigation (DORM) initiative. The report is due to the Governor and General
Assembly on July 1 of each year, with the statute sunsetting on July 1, 2024.
This year’s report builds on work from previous years and includes linked analyses using data sets provided
by the Vital Statistics Administration (VSA), the Prescription Drug Monitoring Program (PDMP), the Health
Services Cost Review Commission (HSCRC), the Public Behavioral Health System (PBHS), Maryland
Medicaid, and new to the report this year is data from the Maryland Institute for Emergency Medical
Services Systems (MIEMSS). Additionally, programmatic data was provided from numerous offices within
MDH, including the Center for Harm Reduction Services (CHRS) and the Environmental Health Bureau.
To support more secure usage of linked data, the Opioid Operational Command Center (OOCC), partnered
with the MDH Behavioral Health Administration (BHA), Chesapeake Regional Information System for our
Patients (CRISP), Maryland’s health information exchange, and the Johns Hopkins Bloomberg School of
Public Health (JHSPH) to migrate certain linked data sets supporting this project onto the Maryland Total
Human-services Integrated Network (MD THINK) platform, Maryland’s cloud-based data storage and
management system.
High-Level Findings
There were 2,800 OD-related fatalities in Maryland in 2021, according to preliminary data provided by the
VSA. This was the highest annual total in the State of Maryland’s history. Fentanyl continues to be the
leading contributor to OD deaths and was involved in 83.7 percent of OD deaths in 2021. Since 2018,
cocaine has consistently been the second-most common substance involved in fatal ODs and was involved
in 36.5 percent of OD deaths in 2021.
The Maryland Emergency Department Drug Surveillance (MD-EDDS) Program analyzes patient toxicology
results in electronic health records (EHRs) for OD patients treated in local emergency departments (EDs).
MD-EDDS provided 14 hospitals with urine dipsticks to test for fentanyl and found the substance in all of
the hospitals, none of which routinely tested for fentanyl at the time. Data collected by MD-EDDS shows
that 10 of 13 hospitals in the study had their lowest opioid-positive urine screens in 2022. For cocaine, 8
of 13 hospitals and, for methamphetamine/amphetamine, 7 of 13 hospitals, had their highest positive
urine screens in 2022.
The MIEMSS data set was the most recent addition to the linked data sets for research and analysis for
the DORM report. The addition of emergency medical services (EMS) encounter data could provide a more
detailed account of interactions between EMS encounters and connections to hospital care or other

MARYLAND DEPARTMENT OF HEALTH
4 | Page
services outside of the medical system. Preliminary analysis of this data identified opioid OD-related
incidents and examined the rate of transport for these incidents in 2021 and 2022. Overall, the rate of
opioid-related OD incidents that resulted in a transport increased from 2021 to 2022. Comparing patients
who were transported to patients who were not transported, patients not transported were found to be:
1) younger on average; 2) more likely to be male; 3) more likely to be recorded as of ‘white’ race; and 4)
more likely to be located in the Eastern Shore region.
Between January 1, 2021, and December 31, 2022, out of 1,251,050 unique incidents identified in the
MIEMSS data set, 34,094 were identified as related to an opioid OD (based on a definition of opioid OD
incident that was adapted from the MDH workgroups). This definition combines information from the
primary and secondary impression fields in EMS reports, narrative, and administered medications to
identify opioid-related OD incidents (more details in Appendix C).
The new partnership between MIEMSS and MDH to provide EMS data for linked analysis opens the door
for future linked analysis. This connects points of care from initial EMS encounter to hospital care to
outside linked services. With a new data set, new trends can emerge to help provide a clearer picture of
the factors surrounding OD events throughout Maryland and identify new opportunities to reduce the
overall number of fatal ODs.
Maryland has continued to experience growing disparity in OD-related deaths across demographic groups.
Between 2017 and 2021, OD deaths among non-Hispanic Black and Hispanic individuals increased, while
OD deaths among non-Hispanic Whites decreased. Black individuals were also more likely than White
individuals to have an all-cause ED visit or inpatient admission and were more likely to experience a
subsequent NFOD in the year following an initial NFOD. Only 13.7 percent of individuals that experienced
their first NFOD in Maryland between July 2016 and December 2021 received a prescription for
buprenorphine in the year following the index NFOD.
Between 2017 and 2021, fatal ODs among people aged 55 and over have increased, while decreasing
among those under the age of 25. Overall, the number of individuals who received a prescription for
buprenorphine was lower among older adults. Non-Hispanic Black individuals aged 55 and over have been
among the groups most impacted by fatal ODs in Maryland, with OD deaths among this cohort increasing
by 264 percent since 2016 while concurrently receiving low rates of buprenorphine prescriptions.
Data from Maryland’s PBHS, which provides publicly funded services for individuals who are enrolled in
Medicaid or who are uninsured, shows the number of individuals who received any type of substance use
disorder (SUD) service, excluding Medication for Opioid Use Disorder (MOUD), in Maryland increased by
32.0 percent from 2016 to 2020 before decreasing by 13.5 percent between 2020 and 2021. The number
of individuals who received MOUD through PBHS, including buprenorphine, methadone, and long-acting
naltrexone, increased by 11.7 percent from 2016 to 2021.
The majority of OD deaths in 2021 occurred in a residential setting and, in most cases, there was a
bystander present. In 2021, 57.2 percent of all fatal ODs occurred in a residence and did not have naloxone
administered. From 2020 to 2021, the percentage of overall naloxone administrations in situations where
there was a fatal OD in a residential setting decreased from 17.7 to 11.9 percent. This highlights the
continued need to promote bystander administration of naloxone through training and dispensing of
naloxone.

DORM 2022 ANNUAL REPORT
5 | Page
Policy Implications
The findings presented in this report highlight several important considerations and opportunities for
Maryland to continue its work to improve OD-related morbidity and mortality in the state.
1. Continue to Address Growing Racial Disparities
OD deaths in Maryland among non-Hispanic Black individuals continue to increase as OD deaths among
non-Hispanic White individuals continue to decrease. In August 2022, Maryland’s Racial Disparities in
Overdose Task Force released a report which included policies and programmatic considerations for
reducing OD mortality in Black communities. The OOCC will continue to work with state and local partners
to implement the recommendations from the report.
2. Explore and Address Factors Driving Increasing Overdose Death Rates Among Individuals 55+
Given the rising rates of OD among older populations overall and the high percentage of older adults with
first NFOD in the sample, expanding access to care coordination and buprenorphine for older adults and
Medicare beneficiaries is a key area of intervention to explore. The OOCC will work with the BHA in
coordination with the Maryland Department of Aging to further understand these trends and to identify
interventions that can be tailored to reach this highly impacted population.
3. Continue to Promote Naloxone Training and Distribution
Naloxone is our most effective tool in preventing fatal ODs. In 2021, 83.8 percent of OD decedents in
Maryland were not administered naloxone which shows the need for naloxone saturation. The majority
of OD deaths in 2021 occurred in a residential setting and, in most cases, there was a bystander present.
From 2020 to 2021, the percentage of overall naloxone administrations in situations where there was a
fatal OD in a residential setting decreased from 17.7 to 11.9 percent. This highlights the continued need
to promote bystander administration of naloxone through training and dispensing of naloxone, as well as
education on Maryland’s Good Samaritan Law. Particular attention should be focused on expanding
education and training among friends and family members of people who use drugs. OD education and
naloxone distribution targeted towards people who use drugs remains the top priority because they are
best positioned to respond to an OD due to the frequency with which they witness them.
CHRS operates a successful community-based naloxone distribution program, which has expanded based
on the enactment of the Statewide Targeted Overdose Prevention (STOP) Act of 2022. The STOP Act
expanded targeted naloxone distribution efforts in Maryland by requiring certain entities, such as hospital
systems, certain outpatient SUD treatment facilities, and correctional settings, to offer naloxone to certain
individuals they serve. Policymakers should consider taking steps to ensure that adequate and consistent
supply of naloxone is available for statewide distribution.
4. Increase Access to Low Barrier Buprenorphine
Only 13.7 percent of individuals that experienced their first NFOD in Maryland between July 2016 and
December 2021 received a prescription for buprenorphine in the year following the index NFOD. Data
show that individuals aged 55 and over had disproportionately low access to buprenorphine in the year
following their NFOD, and also accounted for the majority of fatal ODs in Maryland in 2021. Policymakers

MARYLAND DEPARTMENT OF HEALTH
6 | Page
should explore opportunities to expand low-barrier access to buprenorphine, such as EMS and ED
induction, and increased access in the community.
5. Gather Data on the Emerging Threat of Xylazine
Xylazine is not regulated under the Controlled Dangerous Substance Act as it is a veterinary anesthetic
and not Food and Drug Administration (FDA) approved for human use. The emerging trend is for xylazine
to be used as a cutting agent in fentanyl. Due to these two factors, and the fact that xylazine use in
combination with opioids has been relatively rare until recent years, lab seizure data is limited. Naloxone
is an opioid antagonist, and thus only works in reversing an opioid OD. Xylazine is not an opioid, and thus
naloxone is ineffective in reversing the effects of xylazine. Xylazine is almost always seen with opioids, so
administering naloxone is still important; however, the recovery from the OD may not appear the same
as in cases where xylazine is not present because naloxone will not reverse the sedating effects of xylazine.
The person may continue to be asleep or unconscious, and monitoring their breath and administering
rescue breathing is particularly important. Even if they are unconscious, if they are breathing it means
that the naloxone was effective at reversing the respiratory depression caused by opioids, and additional
doses of naloxone are probably not needed. Expanding data collection on xylazine and regular urine
screening for the substance will provide better information on trends relevant to OD-related factors.
During the 2023 legislative session, MD-EDDS testing results were used to support HB 811/SB 0914
Hospitals - Testing for Fentanyl (The Josh Siems Act). The bill was enacted and will take effect October 1,
2023, requiring Maryland hospitals to begin testing for fentanyl when administering urine drug screenings.
The OOCC is funding MD-EDDS in the 2024 fiscal year to continue the analysis of EHRs and to introduce
expanded testing for over 500 licit and illicit substances to identify emerging drug trends. This expanded
testing will enable the detection of additional substances, such as xylazine. The EHR data will be used to
conduct sophisticated geospatial analyses to describe local variations in SU and SU-related health
outcomes. The continued partnership between the OOCC and MD-EDDS will aid in gathering further
information about xylazine content with testing of over 500 substances including xylazine in MD hospitals.
This will enhance data for emerging trends and geographical identification of local variation in SU.
Next Steps
Data insights derived through the DORM initiative have informed state policy and funding decisions and
will continue to do so as MDH works to enhance DORM by adding additional data sets and improving
coordination among data owners. The 2023 report will include data from additional partners, including
the Department of Public Safety and Correctional Services (DPSCS), as well as a more in-depth analysis of
MIEMSS data.
Figure 1, below, represents the various levels of organization that guide how DORM is implemented. The
DORM Governance Steering Committee will work to onboard additional data sets, including data from
DPSCS within the next year.

DORM 2022 ANNUAL REPORT
7 | Page
Figure 1: Data-Informed Overdose Risk Mitigation Governance Structure

MARYLAND DEPARTMENT OF HEALTH
8 | Page
II. OVERDOSE DEATHS IN MARYLAND
The data overview below provides a demographic profile of individuals who experienced a fatal OD in
Maryland in recent years.
Preliminary data provided by VSA show that the number of unintentional drug-and-alcohol-related OD
fatalities increased from 799 deaths in 2012 to 2,800 deaths in 2021. Fatal ODs increased by 17.7 percent
in 2020, following the onset of the coronavirus pandemic. This followed a 1.2-percent decrease in 2019,
the first annual increase in fatal OD in over a decade.
1
Figure 2: Fatal Overdoses Involving All Substances (2012–2021*)
Source: MDH Vital Statistics Administration.
Gender
In 2021, 72.5 percent of OD decedents were male. This trend has been consistent in the last ten years;
males have consistently accounted for more OD fatalities than females, peaking with a high of 73.4
percent of total fatal ODs in 2018. Additionally, fatal ODs in the last five years have increased faster among
males than among females in Maryland. Between 2017 and 2021, fatal ODs among males grew by 24.9
percent while growing by 17.2 percent among females.
2
1
Maryland Department of Health Vital Statistics Administration: Fatal ODs in Maryland.
2
Ibid.
799
858
1,041
1,259
2,089
2,282
2,406
2,379
2,799 2,800
0
500
1,000
1,500
2,000
2,500
3,000
2012 2013 2014 2015 2016 2017 2018 2019 2020 2021*

DORM 2022 ANNUAL REPORT
9 | Page
Figure 3: Fatal Overdoses by Gender (2017–2021*)
Source: MDH Vital Statistics Administration.
Age
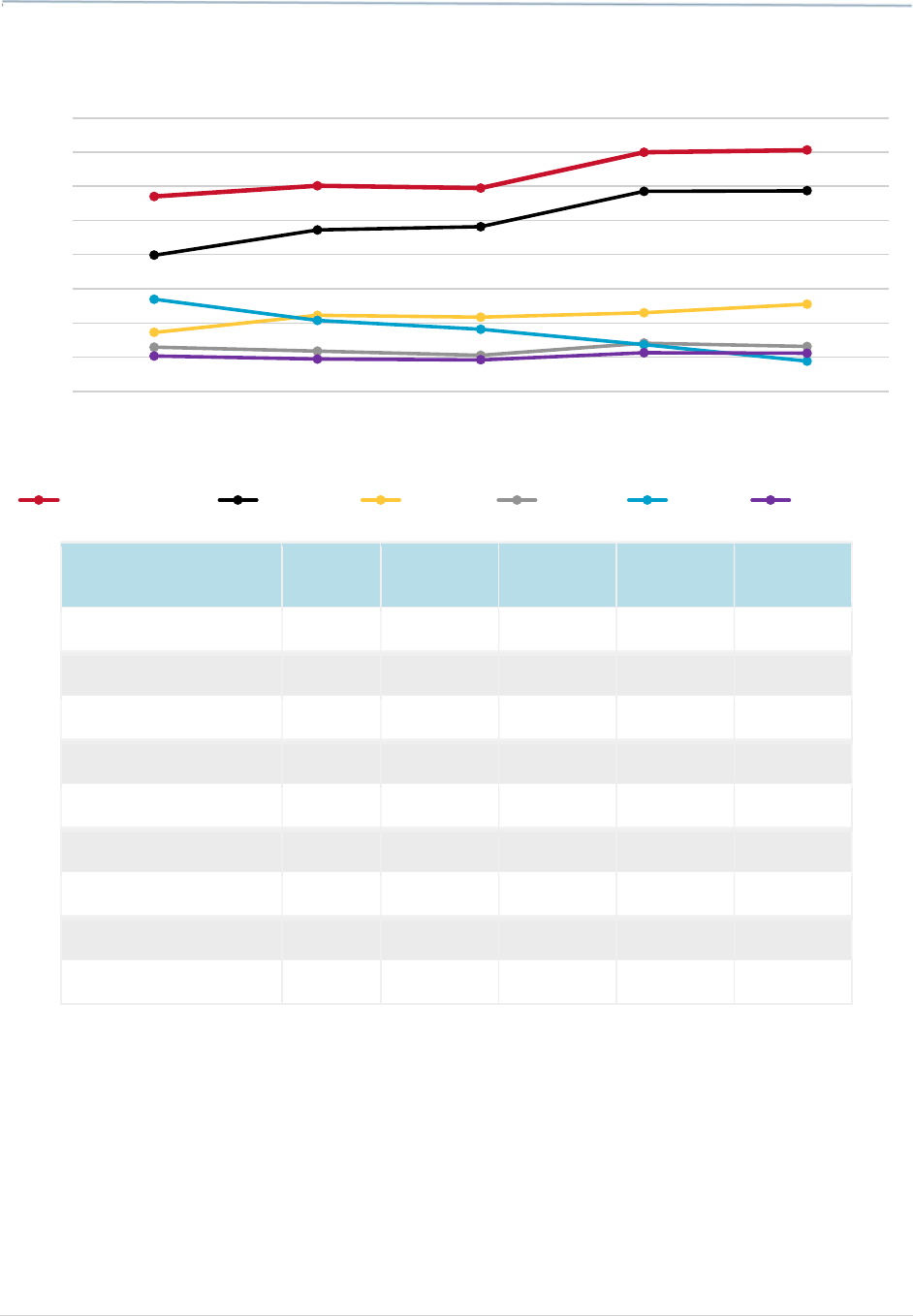
In the last five years, fatal OD trends have varied across age groups in Maryland. For example, fatal ODs
among people under 25 years of age have decreased by 14.9 percent while increasing by 65.8 percent
among individuals over the age of 55.
3
Figure 4: Fatal Overdoses by Age (2017–2021*)
Source: MDH Vital Statistics Administration.
3
Ibid.
1,626
1,766
1,723
2,019
2,031
656
640
654
780
769
0
500
1,000
1,500
2,000
2,500
2017 2018 2019 2020 2021
Male Female
0
200
400
600
800
1,000
2017 2018 2019 2020 2021
<25 y.o. 25-34 y.o. 35-44 y.o. 45-54 y.o. 55+ y.o.

MARYLAND DEPARTMENT OF HEALTH
10 | Page
Year
<25
Years Old
25-34
Years Old
35-44
Years Old
45-54
Years Old
55+
Years Old
2017 154 588 461 560 517
2018 131 561 513 582 618
2019 118 530 557 529 643
2020 143 647 589 651 769
2021 131 555 619 630 857
Source: MDH Vital Statistics Administration.
OD deaths among people aged 55 and up are a demographic of particular concern, with the increase in
OD deaths in this age group mirrored among people who accessed PBHS services.
Race & Ethnicity
Between 2017 and 2021, the growth of OD fatalities among non-Hispanic Black individuals has outpaced
those among non-Hispanic White individuals. During this time, the number of OD fatalities among non-
Hispanic White individuals decreased by 5.2 percent (from 1,505 to 1,427) and increased by 74.4 percent
(from 687 to 1,198) among non-Hispanic Black individuals.
4
OD fatalities increased by 110.2 percent (from
59 to 124) among Hispanic individuals during the same time frame.
Figure 5: Overdose Deaths by Race/Ethnicity (2017–2021*)
Source: MDH Vital Statistics Administration.
4
Ibid.
0
400
800
1,200
1,600
2,000
2017 2018 2019 2020 2021
NH White NH Black Hispanic All Other NH

DORM 2022 ANNUAL REPORT
11 | Page
Year NH White NH Black Hispanic All Other NH
2017 1,505 687 59 21
2018 1,479 823 67 37
2019 1,342 928 75 34
2020 1,556 1,076 126 41
2021 1,427 1,198 124 42
Source: MDH Vital Statistics Administration.
Non-Hispanic Black individuals above the age of 55 have been among the groups most impacted by fatal
ODs in Maryland. Deaths among Non-Hispanic Black individuals aged 55 and older have increased by 264
percent since 2016, from 197 to 519.
Figure 6: Fatal Overdoses Among Non-Hispanic Black Individuals
by Age (2016–2021*)
Source: MDH Vital Statistics Administration. Analysis performed by the Behavioral Health Administration.
0
100
200
300
400
500
600
2016 2017 2018 2019 2020 2021
<25 25-34 35-44 45-54 >55

MARYLAND DEPARTMENT OF HEALTH
12 | Page
Year <25 25-34 35-44 45-54 >55
2016 34 79 115 229 197
2017 24 83 102 241 235
2018 27 103 104 260 329
2019 41 121 154 245 367
2020 35 187 143 274 437
2021 44 159 191 287 519
Source: MDH Vital Statistics Administration. Analysis performed by the Behavioral Health Administration.
Geography
OD deaths in Maryland are largely concentrated in the central region of the state. In 2021, 60.4 percent
of all OD deaths occurred in Baltimore City (1,079), Baltimore County (390), and Anne Arundel County
(230).
5
Map 1: Fatal Overdoses by Jurisdiction, All Substances (2021*)
5
Ibid.
Legend
Source: MDH Vital Statistics Administration. * Data are preliminary.

DORM 2022 ANNUAL REPORT
13 | Page
Educational Attainment
According to Statewide Unintentional Drug Overdose
Reporting System (SUDORS) data, in 2021, 52.1 percent of
OD decedents had a high school diploma or equivalent, and
23.9 percent had less than a high school diploma or
equivalent.
6
8.6 percent of people who died from an OD
had an associate degree or higher.
7
These findings indicate lower educational attainment may
be associated with OD risk and higher educational
attainment may be a protective factor against fatal OD.
Bystanders in Residential Settings
In 2021, 64.9 percent of people who died from an OD were
found in a residence.
8
Of those who died in a residence,
there was a bystander present in 63 percent of cases, 85.8
percent of which were family members or friends.
Naloxone was administered in only 11.9 percent of all
residential cases, which illustrates an opportunity to
expand targeted naloxone distribution. This means 57.2
percent of fatal ODs were in a residence and did not receive
naloxone.
Among OD deaths that occurred in a residential setting in 2021 and in which naloxone was administered
to the decedent, naloxone was administered by a first responder
9
in 48.3 percent of cases. In contrast,
61.6 percent of naloxone administrations were conducted by a first responder in 2020. This highlights
decreased naloxone administration by first responders (61.6 to 48.3 percent) in situations where there
was a fatal OD in a residential setting, however there was an increase in bystander administration (38.4
to 51.7 percent) over first responder administration.
6
Statewide Unintentional Drug Overdose Reporting System (SUDORS) 2021.
7
Ibid.
8
Residential settings include nursing home, long-term care facility, decedent's home, or another person's residence.
9
First responder includes: EMS/fire; Law enforcement; MIEMSS.

MARYLAND DEPARTMENT OF HEALTH
14 | Page
Medicaid Eligibility
A large majority (68.8 percent) of individuals who died from
an OD in 2021 were enrolled in Medicaid in Maryland within
12 months of their death.
10
Between 2017 and 2021, OD decedents who were enrolled
in Medicaid within the 12 months preceding their death
ranged between 65.0 percent in 2017 to 74.6 percent in
2018.
Summary of Overdose Deaths in Maryland
There were 2,800 OD-related fatalities in Maryland in 2021, according to preliminary data provided by
VSA. Fentanyl and cocaine are the leading contributors to OD deaths, fentanyl involved in 83.7 percent
and cocaine involved in 36.5 percent of OD deaths in 2021. OD deaths among Non-Hispanic Black
individuals aged 55 and older have increased by 264 percent since 2016 and have been among the groups
most impacted. In 2021, 57.2 percent of all fatal ODs were in a residence and did not receive naloxone.
See Considerations and Limitations to Analysis section for more details.
10
The Hilltop Institute. (2023, April 14). Medicaid Data for DORM Report. Baltimore, MD: UMBC.
68.8 of overdose decedents were
eligible for Medicaid within 12
months of their death.
Source: SUDORS.

DORM 2022 ANNUAL REPORT
15 | Page
III. NON-FATAL OVERDOSES IN MARYLAND
Demographics
The data shown below provide a demographic profile of individuals who experienced a first NFOD in
Maryland between July 2016 and December 2020.
Data prepared and analyzed by JHSPH linked data from PDMP, HSCRC, and OCME to identify “first” NFOD
episodes, or an index NFOD event, meaning the first NFOD that occurs in the data period from July 2016
through December 2020. There were 41,558 individuals who experienced a first NFOD between July 1,
2016, and December 31, 2020.
Researchers at JHSPH examined characteristics in the six months prior to index NFOD and the following
year. Three sub-samples were examined to better illuminate characteristics associated with
buprenorphine use after the index NFOD: 1) people who did not get buprenorphine in the year following
the index NFOD; 2) people who had a buprenorphine prescription in the four weeks following the first
NFOD; 3) people who had a buprenorphine prescription more than four weeks but less than a year after
the first NFOD. Finally, subgroups of people who received buprenorphine by time were examined to
understand if the amount of time from an index NFOD to receiving buprenorphine was associated with
whether another health outcome occurred.
Age
40.6 percent of individuals with an index NFOD were aged 55 and over.
Figure 7: Non-Fatal Overdoses by Age (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
6.5%
20.1%
14.5%
18.3%
19.6%
21.1%
0%
5%
10%
15%
20%
25%
18-24 25-34 35-44 45-54 55-64 65+

MARYLAND DEPARTMENT OF HEALTH
16 | Page
Gender
55.5 percent of individuals with an index NFOD between July 1, 2016, and December 31, 2020, were male.
Race
60.4 percent of people in this sample were white, and 34.3 percent of people in the sample were Black.
Figure 8: Non-Fatal Overdoses by Race (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
Geography
59.3 percent of people in the sample resided in the Central Region, 13.7 percent in the Capital Region, 8.2
percent on the Eastern Shore, 5.4 percent in the Western Region, and 9.2 percent resided out of state or
had unknown residency status.
34.3%
60.4%
4.3%
0%
20%
40%
60%
80%
Black or African American White Other

DORM 2022 ANNUAL REPORT
17 | Page
Figure 9: Non-Fatal Overdoses by Region (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
Payer Type
41.9 percent of individuals in this sample were covered by Medicaid, 28 percent were covered by
Medicare, and 18.1 percent were covered by commercial insurance. 8.8 percent were self-pay, and 3.1
percent were unknown.
Figure 10: Non-Fatal Overdoses by Payer Type (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
13.7%
59.3%
8.2%
4.1%
5.4%
9.2%
0%
20%
40%
60%
80%
41.9%
28.0%
18.1%
8.8%
3.1%
0%
10%
20%
30%
40%
50%
Medicaid Medicare Commercial Self-pay/Cash Other/Unknown

MARYLAND DEPARTMENT OF HEALTH
18 | Page
Post-NFOD Health Outcomes
13.2 percent of individuals with an index NFOD experienced a subsequent NFOD in the year following
their index NFOD. ED visits in the year following an NFOD were somewhat common, with 62.5 percent of
individuals visiting an ED in the year after their NFOD. Some individuals also experienced a hospitalization
in the year following their NFOD, with 33.8 percent of the sample falling into that category.
Black individuals in the sample were more likely than White individuals to have either a subsequent ED
visit or hospitalization in the year after their index NFOD.
Figure 11: Subsequent Non-Fatal Overdose by Race (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
Figure 12: Subsequent Emergency Department Visit (All Causes)
by Race (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
15.1%
12.5%
0%
5%
10%
15%
20%
Black White
69.3%
59.7%
50%
55%
60%
65%
70%
75%
Black White

DORM 2022 ANNUAL REPORT
19 | Page
Post-NFOD Buprenorphine Access
Only 13.7 percent of people in the sample received a prescription for buprenorphine in the year following
their index NFOD. 41 percent of people who received buprenorphine did so in the first four weeks
following their index NFOD.
There were several important differences in buprenorphine access across demographics. Buprenorphine
access following an NFOD was lower among older adults. People aged 55-64 and aged 65 and over had
disproportionately low access to buprenorphine both in the four weeks immediately following their NFOD
as well as in the year following. For example, among the population that received buprenorphine within
a month of their index OD only 16.5 percent were age 55-64, and 3.3 percent were age 65 and over, but
20.3 percent of the population with no buprenorphine post index NFOD were age 55-64 and 24.4 percent
were age 65 and over.
Figure 13: Buprenorphine Access Following a First Non-Fatal Overdose
by Age (2016–2021)
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
Summary of Non-Fatal Overdoses in Maryland
Out of the sample of people who had a first NFOD in Maryland between July 2016 and December 2020,
only 13.7 percent of people in the sample received a prescription for buprenorphine in the year following
their index NFOD, 40.6 percent were aged 55 and over, and 13.2 percent experienced a subsequent NFOD
in the year following their index NFOD. ED visits in the year following an NFOD were common, with 62.5
percent of individuals visiting an ED in the year after their NFOD. Black individuals in the sample were
more likely than White individuals to have either a subsequent ED visit or hospitalization in the year after
their index NFOD.
See Considerations and Limitations to Analysis section for more details.
6.0%
18.1%
13.6%
17.9%
20.3%
24.0%
7.0%
30.5%
20.7%
21.9%
16.5%
3.3%
9.4%
34.0%
20.0%
20.2%
13.9%
2.4%
0%
10%
20%
30%
40%
18-24 25-34 35-44 45-54 55-64 65+
No Buprenorphine Received Post-NFOD
Buprenorphine Received ≤ 4 Weeks Post-NFOD
Buprenorphine Received >4 Weeks Post NFOD

MARYLAND DEPARTMENT OF HEALTH
20 | Page
IV. OVERDOSE RISK FACTORS
As the data in the following sections illustrate, there are various factors associated with an individual’s
risk of experiencing a fatal OD. These factors include, but are not limited to:
Involvement with illicit drug markets (i.e., purchasing or usage of illicit drugs) characterized by
inconsistency in drug potency and composition;
Compulsive use of opioids, such as that associated with a clinical diagnosis of opioid use disorder
(OUD), despite experiencing harm;
Previous NFOD events;
Medical and behavioral health comorbidities, including acute and chronic conditions such as
chronic pain;
Use of opioids in combination with other substances (“polysubstance use”), including prescription
medications and alcohol; and
Involvement with the criminal legal system, SUD treatment or detoxification programs, or
extended inpatient hospital stays that may result in reduced tolerance.
Drug Supply Characteristics
Illicitly manufactured fentanyl is the leading contributor to OD deaths in the state. In 2021, fentanyl was
involved in 83.7 percent of all fatal ODs. Fentanyl has largely displaced heroin in the illicit drug supply.
Between 2017 and 2021, heroin-related fatal ODs decreased by 67.2 percent, and in 2021, heroin was
involved in just 12.6 percent of all fatal ODs. Since 2018, cocaine has consistently been the second-most
common substance involved in fatal ODs, following the rapid decline in heroin-related fatal ODs.
11
11
Maryland Department of Health Vital Statistics Administration: Fatal overdoses in Maryland.
DORM 2022 ANNUAL REPORT
21 | Page
Figure 14: Overdose Deaths in Maryland by Select Substances (2017–2021)
Substance 2017 2018 2019 2020 2021
All Substances 2,282 2,406 2,379 2,799 2,800
Fentanyl 1,594 1,888 1,927 2,342 2,344
Cocaine 691 891 869 921 1,021
Alcohol 517 472 423 566 517
Heroin 1078 830 726 548 354
RX Opioids 413 379 369 453 447
Benzodiazepines 146 127 107 114 114
Methamphetamine 28 32 41 76 99
Phencyclidine 28 37 58 75 68
Source: MDH Vital Statistics Administration.
Note: Most fatal overdoses involve the simultaneous use of more than one substance. The
individual substance categories included here are not mutually exclusive (i.e., the sum total of
deaths related to individual substance categories does not equal the total number of fatalities for
a given time frame).
0
400
800
1,200
1,600
2,000
2,400
2,800
3,200
2017 2018 2019 2020 2021
All Substances Fentanyl Cocaine Alcohol Heroin RX Opioids

MARYLAND DEPARTMENT OF HEALTH
22 | Page
The market of illicit drugs is constantly evolving, and efforts to better understand the composition of
illicit drugs can help inform OD-related mitigation efforts. Two ways in which Maryland can track the
illicit drug supply are through drug-checking initiatives, such as the Rapid Analysis of Drugs (RAD)
partnership between MDH’s CHRS and the National Institutions of Standards and Technology (NIST), and
through drug seizures analysis from law enforcement partners, such as the Washington/Baltimore High-
Intensity Drug Trafficking Area (W/B HIDTA).
HIDTA Drug Seizures
Data provided by W/B HIDTA show that the amount of illicit drugs seized during HIDTA-funded law
enforcement operations varied between 2020 and 2022. Notably, large increases in the amount of
seized illicit drugs were reported in 2021 across all drug categories except for prescription narcotics.
However, seizures declined in all but two drug categories in 2022. For example, the amount of cocaine
seized in 2021 was 429.4 percent more than the amount of cocaine seized during the prior year
(increasing from 1,086 kg to 5,749 kg), before falling by 65.0 percent in 2022 (decreasing from 5,749 kg
to 2,015 kg). Similarly, the amount of heroin that was seized increased by 119.6 percent in 2021,
followed by a 90.4 percent decrease in 2022.
The amount of fentanyl and methamphetamine that was seized increased in both 2021 and 2022. The
amount of fentanyl that was seized increased by 46.8 percent between 2020 and 2022 (from 77 kg to
113 kg), and the amount of methamphetamine that was seized increased by 75.9 percent during the
same time frame (from 58 kg to 102 kg).
Lastly, the amount of prescription narcotics that were seized fell for two consecutive years. Between
2020 and 2022, the amount of prescription narcotics that were seized fell by 91.7 percent, from 60 kg to
5 kg.
Table 1: Kilograms of Illicit Drugs Seized by W/B HIDTA-Funded Law
Enforcement Operations (2020–2022)
Substance 2020 2021 2022
Cocaine 1,086 5,749 2,015
Methamphetamine 58 78 102
Heroin 51 112 40
Fentanyl 77 83 113
Prescription Narcotics 60 52 5
Cannabis 2509 13,377 5,546
Source: Washington/Baltimore High Intensity Drug Trafficking Area.
The Emergence of Xylazine
In March 2021 W/B HIDTA issued an informational bulletin identifying xylazine (also known as Tranq) as
an emerging threat in the region. Xylazine has become increasingly prevalent in Maryland and across the

DORM 2022 ANNUAL REPORT
23 | Page
Northeastern United States. The substance is a veterinary anesthetic that, when used in humans, can slow
breathing and heart rate. It is not regulated under the Controlled Dangerous Substance Act. Xylazine is
most frequently found in combination with fentanyl when encountered by law enforcement.
Intelligence sources in the bulletin from 2019 to March 2021 showed a steady rise in xylazine availability
and use of xylazine as a cutting agent. During that same time, xylazine appeared to be a contributing factor
to fatal ODs when mixed with opioids, with some regional law enforcement reporting over a 200 percent
increase in fatal ODs where xylazine was present. Because xylazine in combination with opioids was
relatively rare until recent years and it is not classified as a controlled substance, available lab seizure data
is limited. Xylazine is especially dangerous because it can make ODs more difficult to reverse. Naloxone,
for example, is very effective at reversing the effects of opioids but it cannot reverse the effects of xylazine
because it is not an opioid. As such, additional OD response steps, such as rescue breathing, may be
needed to restore the breathing of someone experiencing an opioid OD if xylazine is present.
Although xylazine has been circulating the Washington/Baltimore area of responsibility (AOR) and beyond
for the past several years in mixed form, it has also been seen in pure and/or wholesale amounts. W/B
HIDTA and the Maryland State Police have partnered to analyze available drug seizure intelligence that is
voluntarily provided by law enforcement. The research indicated that out of the total number of samples
reported from June 2021 to December 2022, 19.7 percent tested positive for xylazine.
Out of the total number of xylazine-positive samples, 88 percent were mixed with other substances:
● 72 percent of xylazine-positive samples were also positive for fentanyl;
● 38 percent were also positive for cocaine;
● 22 percent contained mannitol;
● 16 percent contained caffeine; and
● 14 percent contained quinine.
Rapid Analysis of Drugs Program
RAD is a statewide drug-checking program that was launched in October 2021. The program uses de-
identified drug paraphernalia samples (e.g., syringes, pipes, cookers, capsules, foil, baggies, etc.) provided
voluntarily at Syringe Service Programs (SSPs) across Maryland, which are then tested using Direct Analysis
in Real-Time Mass Spectrometry (DART-MS) by NIST. RAD testing results are provided in near real-time,
and testing results are used by participating SSPs to tailor harm-reduction information to participants.
RAD data can also help public health officials and policymakers better under changing dynamics in the
supply of illicit drugs, including information regarding novel substances and emerging trends.
From July 1, 2020, through June 30, 2021, the RAD program analyzed 496 samples, 367 (74.0 percent) of
which tested positive for an opioid and 364 (73.4 percent) tested positive for fentanyl. RAD results during
this time frame also revealed that many samples submitted by SSP participants contained more
substances other than the substance that was intended for purchase.
MARYLAND DEPARTMENT OF HEALTH
24 | Page
For 248 of the 496 samples, SSP participants completed a questionnaire about the drugs they had
intended to purchase. Among the 212 participants who had intended to buy an opioid, 87.7 percent were
exposed to fentanyl, fentanyl analogs, or both, and 85.8 percent were unknowingly exposed to xylazine.
12
In response to an increasing number of ODs involving xylazine, Maryland’s Overdose Data to Action
initiative recently led a workgroup to examine fatal OD data and RAD program case data involving xylazine.
The workgroup is expected to release a report this year.
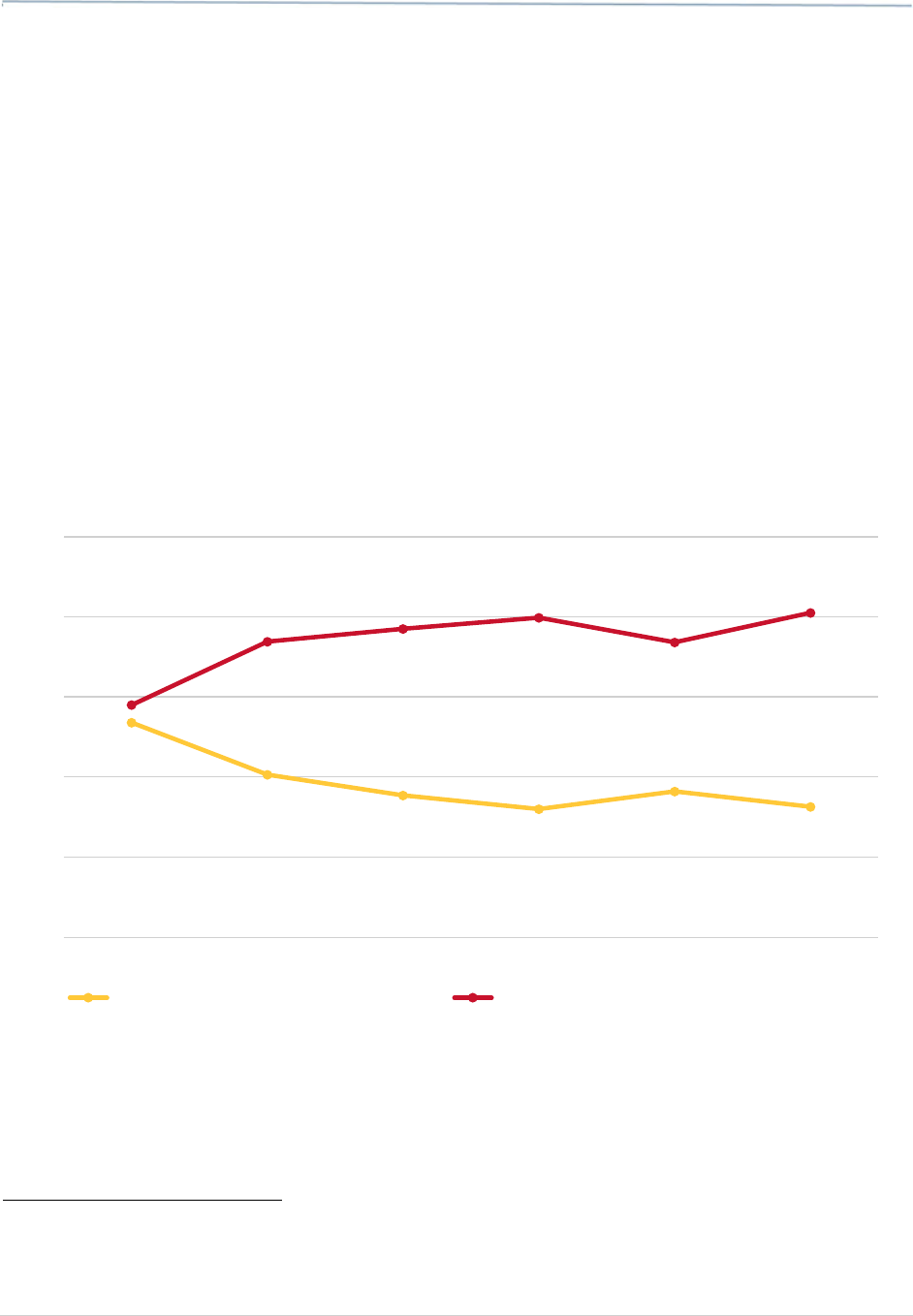
Increasing Stimulant Use
Stimulants are increasingly involved in opioid OD mortality. Among PBHS participants, stimulant-involved
OD deaths increased by 39.7 percent from 2016 to 2021. Over this same period, alcohol-involved OD
deaths decreased by 29.2 percent.
Figure 15. Overdose Deaths Among PBHS Participants Involving Opioid and
Stimulants (2016 – 2021)
Source: MDH Behavioral Health Administration.
12
Russell E, Sisco E, Thomson A, et al. Rapid Analysis of Drugs: A Pilot Surveillance System to Detect Changes in the Illicit Drug
Supply to Guide Timely Harm Reduction Responses — Eight Syringe Services Programs, Maryland, November 2021–August 2022.
MMWR Morb Mortal Wkly Rep 2023;72:458–462. DOI: http://dx.doi.org/10.15585/mmwr.mm7217a2.
26.8%
20.3%
17.7%
16.0%
18.2%
16.3%
29.0%
36.9%
38.5%
39.9%
36.8%
40.5%
0%
10%
20%
30%
40%
50%
2016 2017 2018 2019 2020 2021
Opioids with Alcohol Involvement Opioids with Stimulant Involvement

DORM 2022 ANNUAL REPORT
25 | Page
Year
Opioids with Alcohol
Involvement
Opioids with Stimulant
Involvement
2016 26.8% 29.0%
2017 20.3% 36.9%
2018 17.7% 38.5%
2019 16.0% 39.9%
2020 18.2% 36.8%
2021 16.3% 40.5%
Source: MDH Behavioral Health Administration.
Recent Incarceration
Data collected through SUDORS showed that at
least 2.2 percent of OD decedents in 2021 were
released from a prison, jail, or detention center in
the 30 days prior to their death.
Comorbidities
Data show that between 2016 and 2021, OD decedents with mental and behavioral health comorbidities
were much more likely to experience a fatal OD. According to data provided by HSCRC, individuals who
experienced a heroin-related NFOD had 42.0 times the risk of experiencing a subsequent fatal OD
involving any substance as compared to the general population accessing health services who did not
experience a heroin-related OD during the study period. While the degree of risk associated with each
diagnosis varied between each diagnosis, every combination raised the overall risk of a fatal OD.

MARYLAND DEPARTMENT OF HEALTH
26 | Page
Figure 16: Relative Risk of Overdose Death Predicted by Previous Diagnosed
Overdose and Related Conditions (2016–2021)
When comparing people with OUD, individuals who had an additional comorbidity were at higher risk for
a fatal OD as compared to those who only had an OUD diagnosis. For example, individuals with diagnosed
OUD who also had a diagnosis of cocaine dependency during the study period were 2.3 times more likely
to experience a fatal OD than an individual with OUD and no history of cocaine dependency.
Figure 17: Relative Risk of Overdose Death Predicted by Previous Overdose
Among Those with Diagnosed OUD Relative to Intoxication Deaths (2016-2021)
Source: Maryland Health Services Cost Review Commission.
41.99
34.73
29.63
20.97
17.23
15.1
14.65
11.66
9.57
4.11
3.74
2.58
1.85
0
10
20
30
40
50
2.57
2.39
2.29
1.69
1.51
1.39
1.29
1.01 1.01
0.87
0.83
0
1
2
3
Source: Maryland Health Services Cost Review Commission.

DORM 2022 ANNUAL REPORT
27 | Page
Summary of Overdose Risk Factors
In 2021, fentanyl was involved in 83.7 percent of all fatal ODs. Fentanyl has largely displaced heroin in the
illicit drug supply. Between 2017 and 2021, heroin-related fatal ODs decreased by 67.2 percent, and in
2021, heroin was involved in just 12.6 percent of all fatal ODs. Since 2018, cocaine has consistently been
the second-most common substance involved in fatal ODs, following the rapid decline in heroin-related
fatal ODs. Stimulants are increasingly involved in opioid OD mortality. Among PBHS participants,
stimulant-involved OD deaths increased by 39.7 percent from 2016 to 2021. The amount of prescription
narcotics that were seized fell for two consecutive years. Between 2020 and 2022, the amount of
prescription narcotics that were seized fell by 91.7 percent, from 60 kg to 5 kg. Additional comorbidities
have been found to increase the risk of a fatal OD.
See Considerations and Limitations to Analysis section for more details.

MARYLAND DEPARTMENT OF HEALTH
28 | Page
V. SERVICE UTILIZATION
Service expansion for individuals who use drugs and have clinically diagnosed SUDs has grown in recent
years. The following sections shown below provide data focused on healthcare service utilization for
medications for OUD, other mental health and SUD services, targeted naloxone distribution, SSPs, non-
behavioral health services, hospital characteristics, and service utilization by Medicaid participants.
Medication for Opioid Use Disorder
Data from Maryland’s PBHS, which provides publicly funded services for individuals who are enrolled in
Medicaid or who are uninsured, shows the number of individuals who received any type of SUD service,
excluding MOUD, in Maryland increased by 32.0 percent from 2016 to 2020 before decreasing by 13.5
percent between 2020 and 2021. This brought the total number of people receiving PBHS SUD services,
excluding MOUD, back near to the number that were receiving services in 2017 (73,201 in 2021 to 73,176
in 2017).
The number of individuals who received MOUD through PBHS, including buprenorphine, methadone, and
long-acting naltrexone, increased by 21.1 percent from 2016 to 2020 before decreasing by 7.7 percent
from 2020 to 2021. In total, the number of individuals who received MOUD through PBHS increased by
11.7 percent from 2016 to 2021.
Figure 18: All SUD and MOUD PBHS Service Participants by Year (2016–2021)
Source: MDH Behavioral Health Administration.
Note: Service utilization is analyzed based on a fiscal year from July to June as opposed to overdose
data, which is being analyzed on a calendar year basis
Trends involving fatal ODs among individuals who were dispensed controlled substances between 2016
and 2021 mirrored the trends seen in total fatal ODs during the same time frame. For example, between
2016 and 2021, the proportion of individuals over the age of 55 who were dispensed a controlled
91,872
105,421
115,013
117,592
118,241
104,226
27,764
32,245
33,457
34,135
33,625
31,025
64,108
73,176
81,556
83,457
84,616
73,201
0
20,000
40,000
60,000
80,000
100,000
120,000
140,000
2016 2017 2018 2019 2020 2021
All SUD MOUD SUD w/o MOUD

DORM 2022 ANNUAL REPORT
29 | Page
substance increased in the overall percentage of OD fatalities, while the proportion of individuals between
the ages of 25 and 34 who were dispensed a controlled substance decreased in the overall percentage of
OD fatalities. The proportion of OD decedents under the age of 25 remained comparatively low
throughout the time frame.
13
Figure 19: Overdose Decedents with Controlled Substance Dispense Records in
the PDMP by Age Category (2016–2021)
Year
<25
years
25-34
years
35-44
years
45-54
years
55+
years
2016 4.4% 22.2% 20.8% 28.3% 24.3%
2017 5.0% 23.5% 19.6% 25.5% 26.3%
2018 4.6% 21.0% 21.5% 25.5% 27.5%
2019 3.8% 19.4% 22.7% 23.7% 30.4%
2020 3.9% 22.3% 20.9% 24.3% 28.6%
2021 3.4% 17.7% 22.6% 22.8% 33.3%
Source: Maryland Prescription Drug Monitoring Program, MDH Behavioral Health Administration.
13
BHA linked PDMP and ODR data.
0%
5%
10%
15%
20%
25%
30%
35%
2016 2017 2018 2019 2020 2021
<25 years 25-34 years 35-44 years 45-54 years 55+ years

MARYLAND DEPARTMENT OF HEALTH
30 | Page
The number of male OD decedents dispensed a controlled substance increased from 62.4 percent in 2016
to 66.8 percent in 2021, while female decedents dispensed a controlled substance decreased from 37.6
percent in 2016 to 32.5 percent in 2021.
14
Figure 20: Percentage of Overdose Decedents with a Controlled Substance
Dispensed by Gender (2016–2021)
Source: MDH Prescription Drug Monitoring Program.
In 2021, non-Hispanic Black OD decedents with dispense records between 2016-2021 consisted of 33.2
percent of the overall decedents (2,694 of 8,106), while non-Hispanic White decedents consisted of 63.9
percent of the overall decedents (5,183 of 8,106). Non-Hispanic White decedents experienced a 73.6
percent increase during this time frame (from 576 to 1000) while non-Hispanic Black decedents saw an
increase of 227.3 percent (from 216 to 707) over the 5-year span. Similar to total fatal OD trends, OD
fatalities among non-Hispanic White individuals who were dispensed a controlled substance decreased
from 2016 to 2021, while OD fatalities among non-Hispanic Black individuals who received controlled
substances increased.
15
Hispanic individuals with a dispense record accounted for no more than 2 percent
of OD decedents in any year.
14
Ibid.
15
Ibid.
37.6%
35.4%
32.9%
32.3%
32.5%
33.2%
62.4%
64.6%
67.1%
67.7%
67.5%
66.8%
0%
20%
40%
60%
80%
2016 2017 2018 2019 2020 2021
Female Male

DORM 2022 ANNUAL REPORT
31 | Page
Figure 21: Percent of Overdose Decedents with a Controlled Substance
Dispensed by Race (2016-2021)
Source: Maryland Prescription Drug Monitoring Program.
Figure 22: Overdose Decedents with a Controlled Substance Dispensed
by Race (2016-2021)
Source: Maryland Prescription Drug Monitoring Program.
The age group of 55 years or older made up the majority of OD decedents with dispense records from
2016 to 2021 at 29.0 percent of the overall decedents (2,350 of 8,108). The second largest age group of
OD decedents with dispense records was 45–54 at 24.7 percent of the overall decedents (1,999 of 8,108)
from 2016 to 2021. OD decedents aged 35–44 with a dispense record increased from 2016 to 2021
climbing past the 25-34 age group and nearly matching the number of OD decedents aged 45–54 with
dispenses in 2021.
70.9%
71.5%
68.0%
62.1%
61.2%
56.7%
26.6%
26.4%
29.2%
35.6%
35.3%
40.1%
1.0%
1.2%
1.7%
1.1%
2.3%
2.1%
0%
10%
20%
30%
40%
50%
60%
70%
80%
2016 2017 2018 2019 2020 2021
NH White NH Black Hispanic
576
826
919
829
1,033
1,000
216
305
395
475
596
707
20
25
37
30
59
58
0
200
400
600
800
1,000
1,200
2016 2017 2018 2019 2020 2021
NH White NH Black Other

MARYLAND DEPARTMENT OF HEALTH
32 | Page
Figure 23: Overdose Decedents with a Controlled Substance Dispensed by Age
(2016–2021)
Year <25 years 25-34 years 35-44 years
45-54 years
55+ years
2016 36 180 169 230 197
2017 58 272 227 295 304
2018 62 283 291 344 371
2019 51 259 303 317 406
2020 66 376 353 410 483
2021 60 313 400 403 589
Source: Maryland Prescription Drug Monitoring Program.
Over the past six years, heroin has decreased by 53.9 percent (from 447 to 206) in overall fatal ODs among
those dispensed a controlled substance, while fentanyl has increased by 241.1 percent from 431 to 1470
in overall fatal ODs among those dispensed a controlled substance.
The highest number of OD deaths among decedents with a dispense record in the PDMP involve opioids,
totaling 41.3 percent of deaths from 2016 to 2021. The second highest cause-of-death substance is
fentanyl, making up 35.3 percent of OD deaths among decedents with a dispense record from 2016 to
2021. OD deaths involving heroin among decedents with dispense records have steadily decreased from
2016 to 2021, making up only 5.7 percent (206 of 3,610) of OD deaths among decedents with a dispense
record in 2021. Both opioid-related and fentanyl-related deaths among decedents with dispense records
increased slightly from 2020 to 2021 by 4.1 and 5.1 percent respectively.
0
100
200
300
400
500
600
700
2016 2017 2018 2019 2020 2021
<25 years 25-34 years 35-44 years 45-54 years 55+ years

DORM 2022 ANNUAL REPORT
33 | Page
Figure 24: Overdose Decedents with a Controlled Substance Dispensed by
Substance (2016-2021)
Year Any Opioid Fentanyl Rx Opioids Heroin
2016 732 431 236 447
2017 1021 795 267 555
2018 1201 1040 273 471
2019 1184 1068 242 395
2020 1531 1399 334 347
2021 1594 1470 340 206
Source: Maryland Prescription Drug Monitoring Program.
Hospital-Level Data
The data presented below comes from the MD-EDDS program which recruited 17 hospitals across the
state in the 2023 fiscal year to obtain limited data sets of quarterly EHR from patients visiting each
hospital’s ED for a drug OD. MD-EDDS also provided 50 fentanyl urinalysis dipstick test kits each to 14
hospitals that were not yet routinely testing for fentanyl. Map 2 shows that participating hospitals came
from each region of the State. The OOCC supports the MD-EDDS project at the University of Maryland’s
Center for Substance Use, Addiction & Health Research (CESAR). The following sections highlight key
findings from the analyses of the EHR data and the fentanyl dipstick testing.
0
400
800
1,200
1,600
2,000
2016 2017 2018 2019 2020 2021
Any Opioid Fentanyl Rx Opioids Heroin

MARYLAND DEPARTMENT OF HEALTH
34 | Page
Map 2 Hospitals Participating in MD-EDDS
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
# Hospital City
Years
Available
% Tested
Across
Timespan
1
UM
Shore Medical Center at
Chestertown
Chestertown 2019-2022 51
2
UPMC Western Maryland
Cumberland
2018
-
2022
25
3
Meritus Medical Center
Hagerstown
2019
-
2022
41
4
UM Harford Memorial Hospital
Havre De Grace
2020
-
2022
55
5
UM Baltimore Washington
Medical Center
Glen Burnie 2016-2022 53
6
UM Upper Chesapeake Medical
Center
Bel Air 2020-2022 54
7
UM Shore Medical Center at
Cambridge
Cambridge 2022 46
8
TidalHealth Peninsula Regional
Salisbury
2018
-
2022
44
14

DORM 2022 ANNUAL REPORT
35 | Page
# Hospital City
Years
Available
%
Tested
Across
Timespan
9
UM Capital Region Medical Center
Largo
2021
-
2022
60
10
UM Charles Regional Health
Center
La Plata 2019-2022 46
11
UM Shore Medical Center at
Easton
Easton 2019-2022 52
12
UM Bowie Health Center
Bowie
2021
-
2022
29
13
UM
Laurel Medical Center
Laurel
2021
-
2022
75
14
UM Medical Center
Baltimore
2016
-
2022
44
15
UM Medical Center, Midtown
Campus
Baltimore 2016-2022 49
16
UM Shore Emergency Center at
Queenstown
Queenstown 2019-2022 30
17
UM St. Joseph Medical Center
Baltimore
2016
-
2022
69
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*This represents the percentage of OD-related ED visits that had a toxicology screen. Not all visits had an accompanying
toxicology test, often common when clinical presentation is uncomplicated (i.e., the overdose has been resolved).
Overview of Findings from the Quarterly EHR Data
To date, 17 hospitals have joined MD-EDDS and submitted quarterly extracts from their EHRs for ED visits
involving a drug OD. An ED visit for a drug OD is defined as any ED visit involving a patient aged 18-90 who
reported a complaint of “OD” and/or had an International Classification of Diseases (ICD), Tenth Revision,
Clinical Modification (ICD-10-CM) T36-T50 initial encounter discharge diagnosis code of poisoning with
accidental (unintentional), intentional self-harm, or undetermined intent. The quarterly EHR extracts
include information on urine screen administration and urine drug screen results, where available, for
each identified ED drug OD visit, along with limited information about patient demographics, admission
date, patient complaint(s) at admission, discharge diagnoses, and ICD-10-CM diagnosis codes. The MD-
EDDS team is in the process of collecting EHR data from three additional hospitals, bringing the total
number of hospitals participating to 20.
Classification Scheme
Toxicology screens are typically ordered when patients have symptoms that may be related to non-
prescribed SU. Most commonly, this includes altered mental status, suspected OD, and psychiatric
evaluations. Toxicology screens may not be ordered for patients for which the clinical presentation is
uncomplicated - such as an opioid OD that appears to have been responsive to the administration of
naloxone. Doctors request urine drug screens for patients for a variety of reasons, and the substances
included in their screens often vary. As shown in the associated table for Map 2, the years for which drug
screen results were available and the percentage of drug OD visits tested varied by hospital. In 2022, the

MARYLAND DEPARTMENT OF HEALTH
36 | Page
percentage of OD ED visits with a urine screen varied across the 17 MD-EDDS hospitals from 25 percent
to 75 percent; 14 hospitals tested 40 percent or more. The median was 50 percent. The most frequently
included substances in standard urine screens were cocaine, opiates, amphetamine/methamphetamine,
and THC. Opiates, methadone, oxycodone, fentanyl, and buprenorphine are each identified by separate
drug screens. The opiate screens are sensitive to natural opioids, such as morphine (typically a metabolite
of heroin). Fentanyl is a semi-synthetic opioid and oxycodone is a synthetic opioid, so they are not
detected by an opiate screen.
EHR findings are presented below for UM Medical Center Midtown Campus (UMMC Midtown) and UM
St. Joseph Medical Center (UM SJMC) for two substance categories – opioids and stimulants. These
hospitals were selected because both are located in Central Maryland where the majority of fatal ODs
occur each year, however, they reflect distinct differences in the populations served – largely African
American urban communities and largely White suburban communities. The findings presented for each
hospital are only a subset of the information collected by MD-EDDS and additional information is available
from MD-EDDS upon request to CESAR. For UMMC Midtown and UM SJMC, the opioid category includes
opiates, oxycodone, methadone, and fentanyl. The stimulant category for these hospitals includes
cocaine, amphetamine, and methamphetamine. The substances included in these categories vary across
the other participating hospitals, depending on the specific substances included in standard drug screens.
University of Maryland Medical Center, Midtown Campus (UMMC Midtown), 2016-2022
UMMC Midtown is located in the heart of Baltimore City, where the majority of fatal ODs in Maryland
occur every year.
Number of Overdose-Related ED Visits by Year (2016–2022)
OD-related ED visits rose steadily from 2016 to 2018, when they peaked at 895 visits, (see Figure 25). After
2018, visits fell steadily, with the most dramatic drop occurring between 2021 and 2022, from 720 to 507,
a 29.6 percent decrease. In the entire study period of 2016 to 2022 there was a 25.6 percent decrease in
OD-related ED visits.
Figure 25: Number of OD-Related Emergency Department Visits
by Year – UMMC Midtown
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
681
881
895
859
746
720
507
0
200
400
600
800
1,000
2016 2017 2018 2019 2020 2021 2022

DORM 2022 ANNUAL REPORT
37 | Page
Overdose-Related ED Visits by Age, Race/Ethnicity, and Gender (2016–2022)
From 2016 to 2022, Non-Hispanic Black persons made up 77 percent to 82 percent of the OD-related ED
patients. About two-thirds each year were males and 35 years or older (see Figure 26).
Figure 26: Drug Overdose-Related Emergency Department Visits, by Age,
Race/Ethnicity, and Gender – UMMC Midtown
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Overdose-Related ED Visits with a Positive Result for Any Opioid or Stimulant, 2016-2022
The percentage of patients who tested positive for opioids increased most dramatically from 2018 to 2019
(when the hospital began testing regularly for fentanyl), from 54.5 percent to 82.2 percent, although the
total number of visits declined. From 2019 onwards, the percentages remained relatively similar, with a
small decrease in 2022 (see Figure 27).
69%
68%
69%
68%
73%
67%
31%
32%
31%
32%
27%
33%
2017
2018
2019
2020
2021
2022
Male Female
Gender
17%
17%
17%
21%
20%
16%
20%
82%
80%
81%
77%
78%
82%
77%
1%
2%
1%
2%
1%
1%
1%
1%
1%
1%
.5%
1%
1%
1%
2016
2017
2018
2019
2020
2021
2022
NH White NH Black Hispanic Other
Race/Ethnicity
7%
6%
5%
4%
5%
3%
2%
14%
15%
15%
18%
17%
18%
19%
17%
15%
16%
17%
18%
16%
16%
32%
33%
34%
30%
25%
23%
20%
30%
31%
31%
32%
35%
40%
43%
2016
2017
2018
2019
2020
2021
2022
18-24 25-34 35-44 45-54 55+
Age Group

MARYLAND DEPARTMENT OF HEALTH
38 | Page
The percentage of urine screens positive for stimulants ranged from 44 percent in 2016 to 57.7 percent
in 2022, a 31.1 percent increase. This is a different trend than seen with opioid positives, which were
consistently higher than stimulants and held relatively steady from 2019 onwards.
Figure 27: Percentage of Overdose-Related Emergency Department Visits with a
Positive Result for Opioids and Stimulants by Year – UMMC Midtown
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Demographic Characteristics of Patients Positive for Opioids, 2016-2022
Among patients positive for opioids, the proportion of those 55 or older increased from 27.1 percent in
2016 to 45.8 percent in 2022. The proportion of those aged 45-54 decreased, from 35.6 percent to 21.6
percent. Three-quarters or more of patients with a positive test for opiates each year were non-Hispanic
Black and across the entire study period, 63–73 percent of patients with a positive test for opiates were
males.
Figure 28: Overdose-Related Emergency Department Visits with Positive Opioid
Results by Age, Race/Ethnicity, and Gender – UMMC Midtown
66.1%
66.9%
54.5%
82.2%
85.7%
88.7%
85.0%
44.0%
52.7%
52.6%
51.1%
48.6%
48.7%
57.7%
0%
20%
40%
60%
80%
100%
2016 2017 2018 2019 2020 2021 2022
Percent Positive for Opioids Percent Positive for Stimulants
54%
48%
45%
51%
58%
49%
47%
46%
52%
55%
49%
42%
51%
53%
2016
2017
2018
2019
2020
2021
2022
Male Female
Gender

DORM 2022 ANNUAL REPORT
39 | Page
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Trends Across all Drug Categories
Figure 29 shows trends in the substances detected in urine drug screens from 2016-2022. From 2020
onwards, opiate positives declined dramatically, from 56 percent in 2016 to 18 percent in 2022. This
decrease is likely explained by the more limited availability of heroin, as fentanyl became more prominent
in the illicit drug market. UMMC Midtown started testing for fentanyl in 2019 and it was shown to be
present in approximately 80 percent of ODs since then.
Stimulant positives, including cocaine and amphetamine/methamphetamine, have been increasing in
recent years. Cocaine positives increased from 48 percent in 2021 to 57 percent in 2022.
Amphetamine/methamphetamine positives also increased during this time but remained below 10
percent. Benzodiazepine positives peaked at 37.1 percent in 2021 and decreased to 30.7 percent in 2022.
It is unknown if any of these substances were prescribed during the patients’ ED visits and thus caused
the positive result. THC-positive specimens reached a series high of 25 percent in 2022.
78%
68%
66%
66%
70%
61%
59%
18%
23%
26%
26%
23%
30%
29%
2%
2%
4%
4%
2%
7%
7%
2%
6%
4%
3%
5%
2%
5%
2016
2017
2018
2019
2020
2021
2022
NH White NH Black Hispanic Other
Race/Ethnicity
20%
21%
19%
21%
23%
21%
22%
23%
25%
22%
23%
30%
17%
16%
14%
13%
13%
16%
13%
16%
18%
17%
16%
15%
16%
14%
15%
7%
26%
25%
30%
26%
21%
31%
36%
2016
2017
2018
2019
2020
2021
2022
18-24 25-34 35-44 45-54 55+
Age Group

MARYLAND DEPARTMENT OF HEALTH
40 | Page
Figure 29: Drugs Detected Among Tested Patients, by Year – UM Medical Center,
Midtown Campus
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Substance 2016 2017 2018 2019 2020 2021 2022
Fentanyl — — — 78.9% 81.9% 82.0% 78.3%
Cocaine 42.9% 51.7% 51.9% 50.1% 47.0% 48.1% 56.6%
Benzodiazepines 24.6% 22.4% 28.3% 30.4% 28.7% 37.1% 30.7%
THC 22.7% 22.9% 18.5% 16.1% 22.7% 20.0% 25.1%
Methadone 21.8% 22.6% 22.8% 27.5% 25.5% 27.8% 24.7%
Opiates 55.9% 56.7% 40.4%
36.1% 38.6% 24.1% 18.0%
Oxycodone — — — 6.2% 4.4% 4.1% 6.7%
Amphetamine/
Methamphetamine
1.7% 2.0% 2.3% 1.9% 4.7% 1.7% 5.2%
Fentanyl
Cocaine
Benzodiazepines
THC
Methadone
Opiates
Oxycodone
Amphet./Methamphet.
Barbiturates
PCP
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
2016
2017
2018
2019
2020
2021
2022

DORM 2022 ANNUAL REPORT
41 | Page
Substance 2016 2017 2018 2019 2020 2021 2022
Barbiturates 2.8% 1.0% 1.5% 2.2% 1.6% 1.4% 1.9%
PCP 1.1% 0.7% 0.9% 0.7% 0.0% 0.0% 0.4%
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
The most common other substance to appear in specimens testing positive for opiates was cocaine. Just
over 60 percent of specimens testing positive for opiates also had cocaine present. Fentanyl was present
in 36.2 percent of specimens. Benzodiazepines, methadone, and THC followed at 32.9 percent, 25
percent, and 18.8 percent, respectively.
Figure 30: Percentage of Other Drugs Detected in Specimens that Tested
Positive for Opiates – UM Medical Center, Midtown Campus (2022)
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Nearly half of the cocaine-positive specimens also tested positive for opiates or fentanyl. The third most
common other substance found was benzodiazepines. Methadone and THC were found in 25.1 percent
and 21.2 percent of cocaine-positive specimens, respectively.
100.0%
61.0%
36.2%
32.9%
25.0%
18.8%
3.1%
2.0%
1.8%
0%
20%
40%
60%
80%
100%
Opiates
Cocaine
Fentanyl
Benzodiazepines
Methadone
THC
Oxycodone
Barbiturates
Amphet./Methamphet.

MARYLAND DEPARTMENT OF HEALTH
42 | Page
Figure 31: Percentage of Other Drugs Detected in Specimens that Tested
Positive for Cocaine– UM Medical Center, Midtown Campus, 2022
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
University of Maryland St. Joseph Medical Center (UM SJMC)
The data shown below represents a subset of the data collected by MD-EDDS. UM SJMC is located in
Baltimore County, which is the jurisdiction with the second-highest OD fatality rate in Maryland. Data
from UM SJMC differed compared to testing results from UMMC Midtown. For example, white patients
made up the majority of OD-related ED visits at this hospital, and opioids were not involved in the majority
of their OD-related ED visits between 2016 and 2022. It should be noted that fentanyl testing began at
UM SJMC in April 2022, and the opioid results before that point are likely undercounted in the data and
are not comparable to UMMC Midtown.
Number of Overdose-Related ED Visits (2016–2022)
There was a substantial decrease in drug OD-related ED visits at UM SJMC between 2016 and 2022, falling
from 333 to 188 (42.5 percent reduction). The largest decrease occurred from 2021 to 2022, from 255 to
188 visits, or 26.3 percent.
100.0%
48.6%
47.2%
29.7%
25.1%
21.2%
3.4%
1.9%
1.6%
0%
20%
40%
60%
80%
100%
Cocaine
Opiates
Fentanyl
Benzodiazepines
Methadone
THC
Amphet./Methamphet.
Barbiturates
Oxycodone

DORM 2022 ANNUAL REPORT
43 | Page
Figure 32: Number of Overdose-Related Emergency Department Visits
by Year – UM SJMC
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Drug Overdose ED Visits by Age, Race/Ethnicity, and Gender (2016–2022)
From 2016 to 2022, females accounted for 42–55 percent of patients with an OD-related ED visit, and 21–
36 percent were aged 55 or older. Non-Hispanic Whites were involved in the majority of the visits during
this period.
Figure 33: Overdose-Related Emergency Department Visits, by Age,
Race/Ethnicity, and Gender – UM SJMC
333
307
300
262
256
255
188
0
50
100
150
200
250
300
350
2016 2017 2018 2019 2020 2021 2022
64%
63%
63%
65%
73%
72%
65%
36%
37%
38%
35%
27%
28%
35%
2016
2017
2018
2019
2020
2021
2022
Male Female
Gender
24%
23%
18%
21%
20%
17%
21%
75%
75%
81%
78%
77%
81%
76%
1%
1%
.4%
1%
1%
1%
2%
1%
1%
1%
1%
1%
1%
2016
2017
2018
2019
2020
2021
2022
NH White NH Black Hispanic Other
Race/Ethnicity

MARYLAND DEPARTMENT OF HEALTH
44 | Page
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Drug Overdose-Related ED Patients Testing Positive for Any Opioid or Stimulant (2016–2022)
From 2016 to 2019, the number of patients who tested positive for an opioid decreased from 45.3 percent
to 18.7 percent. In 2022, the number increased to 32 percent. Following the inclusion of fentanyl in
toxicology screening in April 2022, the percentage who tested positive for fentanyl was higher than for all
other substance categories except for THC.
The percentage of ED visits with positive tests for stimulants increased from 25.1 percent in 2016 to 28.0
percent in 2022. This trend differed as compared to positive tests for opioids during the same time frame,
which had a decreasing trend.
Figure 34: Percentage of Drug Overdose-Related Emergency Department Visits
with a Positive Result for Opioids and Stimulants by Year – UM SJMC
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*UM SJMC did not begin reporting testing for fentanyl until the 2nd quarter of 2022 so there were
far fewer test results for fentanyl, compared with opiates and cocaine (86 tests for fentanyl vs.
1,306 for cocaine and opiates during the 2016-2022 time period).
3%
6%
1%
2%
4%
2%
2%
12%
12%
14%
13%
14%
15%
18%
22%
16%
16%
18%
16%
15%
13%
36%
39%
37%
34%
27%
25%
22%
27%
28%
32%
31%
39%
43%
46%
2016
2017
2018
2019
2020
2021
2022
18-24 25-34 35-44 45-54 55+
Age Group
45.3%
36.4%
28.4%
18.7%
26.7%
24.0%
32.0%
25.1%
23.0%
28.4%
25.7%
29.5%
25.1%
28.0%
0%
10%
20%
30%
40%
50%
2016 2017 2018 2019 2020 2021 2022
Percent Positive for Opioids Percent Positive for Stimulants

DORM 2022 ANNUAL REPORT
45 | Page
Demographic Characteristics of Patients Positive for Opioids, 2016-2022
The percentage of patients with positive test results for opioids who were 55 or older increased from 17.8
percent in 2016 to 50 percent in 2022. The 45–54 age category experienced a decrease from 23.8 percent
to 2.5 percent in the same time frame. In all of the years studied, White patients and females constituted
the majority of those testing positive for opioids.
Figure 35: Drug Overdose-Related Emergency Department Visits with Positive
Opioid Results, by Age, Race/Ethnicity, and Gender – UM SJMC
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Trends Across all Drug Categories
Figure 36 shows testing trends for various substances from 2016 to 2022. From 2020 onwards, the
percentage of specimens testing positive for opiates fell dramatically, from 38 percent in 2016 to 10
percent in 2022. This decrease may be explained by the more limited availability of heroin in the illicit
56%
62%
53%
71%
53%
67%
63%
44%
38%
47%
29%
47%
33%
38%
2016
2017
2018
2019
2020
2021
2022
Male Female
Gender
81%
72%
72%
57%
68%
76%
69%
17%
21%
23%
34%
23%
19%
28%
4%
5%
5%
2%
3%
9%
9%
3%
2016
2017
2018
2019
2020
2021
2022
NH White NH Black Hispanic Other
Race/Ethnicity
17%
11%
15%
9%
9%
8%
28%
29%
28%
26%
28%
17%
15%
14%
14%
20%
23%
11%
21%
25%
24%
20%
13%
20%
19%
12%
3%
18%
26%
23%
23%
34%
50%
50%
2016
2017
2018
2019
2020
2021
2022
18-24 25-34 35-44 45-54 55+
Age Group

MARYLAND DEPARTMENT OF HEALTH
46 | Page
drug supply as fentanyl became more prevalent. UM SJMC started testing for fentanyl in April 2022, after
which fentanyl became the second-most frequently detected substance. Fentanyl was detected in 30
percent of specimens in 2022.
THC was the most frequently detected substance from 2020 to 2022, reaching a series high of 37 percent
in 2022. The percentage positive for amphetamine/methamphetamine varied marginally but remained
below 11 percent each year, and cocaine positives ranged from 18.8 percent to 22.4 percent.
Benzodiazepine positives gradually declined from 2016 to 2022 and reached a series low of 17 percent in
2022.
Figure 36: Drugs Detected Among Tested Patients, by Year – UM SJMC
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Substance 2016 2017 2018 2019 2020 2021 2022
THC 19.7% 17.7% 26.1% 23.5% 33.0% 30.3% 36.8%
Fentanyl — — — — — — 30.2%
Cocaine 18.8% 21.1% 20.9% 19.8% 19.9% 21.7% 22.4%
THC
Fentanyl
Cocaine
Benzodiazepines
Opiates
Oxycodone
Amphet./Methamphet.
Methadone
PCP
Barbiturates
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
2016 2017 2018 2019 2020 2021 2022

DORM 2022 ANNUAL REPORT
47 | Page
Substance 2016 2017 2018 2019 2020 2021 2022
Benzodiazepines 36.3% 25.4% 26.5% 27.3% 19.3% 24.0% 16.8%
Opiates 38.1% 29.7% 22.3% 14.4% 21.0% 18.3% 9.6%
Oxycodone — — — — — — 7.0%
Amphetamine/
Methamphetamine
9.0% 2.9% 8.5% 5.9% 10.9% 5.8% 6.4%
Methadone 11.2% 10.5% 9.0% 8.1% 8.0% 9.7% 4.8%
PCP 1.3% 2.9% 0.9% 0.5% 0.6% 0.0% 0.8%
Barbiturates 1.3% 1.4% 2.8% 0.0% 4.0% 1.7% 0.0%
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
The most common substance found in combination with positive tests for cocaine were opiates at 40
percent. Benzodiazepines and THC followed at 38.4 and 33.2 percent, respectively).
Figure 37: Percentage of Other Drugs Detected in Specimens that Tested
Positive for Cocaine– UM Medical Center, UM SJMC, 2022
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
The most common substance found in combination with positive tests for opiates were benzodiazepines
at 42.4 percent. It is unknown if any of these substances were prescribed during the patients’ ED visits
and thus caused the positive result. Cocaine was present in 35.1 percent of opiate-positive specimens.
100.0%
39.6%
38.4%
33.2%
20.1%
6.7%
6.3%
0%
20%
40%
60%
80%
100%
Cocaine
Opiates
Benzodiazepines
THC
Methadone
Fentanyl
Amphet./Methamphet.

MARYLAND DEPARTMENT OF HEALTH
48 | Page
THC, methadone, and amphetamine/methamphetamine followed at 25.8 percent, 14.2 percent, and 8.9
percent, respectively.
Figure 38: Percentage of Other Drugs Detected in Specimens that Tested
Positive for Opiates – UM SJMC, 2022
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Cross-Site Comparisons of Drugs Detected
This section presents figures showing the high and low ranges of patients in 13 hospital EDs that tested
positive for each substance from 2016 to 2022. They also indicate the percentage positive in 2022. Four
hospitals were excluded from these analyses because they had very low positivity rates or too small a
range of results to plot.
Figure 39 shows that in 2022, opiates reached a series low in 10 hospitals, including 5 of the 6 hospitals in
Central Maryland. The decline in opiate-positive tests across Maryland reflects a decline in heroin use as
fentanyl became widely available.
100.0%
42.4%
35.1%
25.8%
14.2%
8.9%
0%
20%
40%
60%
80%
100%
Opiates
Benzodiazepines
Cocaine
THC
Methadone
Amphet./Methamphet.

DORM 2022 ANNUAL REPORT
49 | Page
Figure 39: High and Low Yearly Percentages Testing Positive for Opiates
at 13 Hospital EDs
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Note: UM Bowie Health Center, UM Capital Region Medical Center, UM Laurel Medical Center, and
UM Shore Medical Center at Cambridge not shown because of very low rates or too small a range
to plot. Only 11% of ED drug overdose visits to UPMC Western Maryland received urine drug screens
in 2022. If the same percentage occurred in more than one year, the latest occurrence is shown.
Figure 40 shows that cocaine reached a series high in eight hospitals in 2022, including all six in Central
Maryland in 2022. However, two hospitals on the Eastern Shore (UM Shore Easton, UM Shore
Chestertown) and one in Western Maryland (University of Pittsburgh Medical Center-UPMC) reported a
series low. Three hospitals reported that more than half of their specimens tested positive for cocaine –
two in Baltimore City (UMMC Midtown, UMMC) and one in Washington County (Meritus Medical Center).
14%
16%
13%
10%
12%
18%
18%
0%
23%
7%
10%
13%
9%
Meritus Medical Center
TidalHealth Peninsula Regional Hospital
UM Baltimore Washington Medical Center
UM Charles Regional Medical Center
UM Harford Memorial Hospital
UM Medical Center
UM Medical Center, Midtown Campus
UM Shore Emergency Center at Queenstown
UM Shore Medical Center at Chestertown
UM Shore Medical Center at Easton
UM St. Joseph Medical Center
UM Upper Chesapeake Medical Center
UPMC Western Maryland
28%
(2019)
22%
(2018)
40%
(2016)
22%
(2019)
12%
(2022)
48%
(2017)
57%
(2017)
38%
(2019)
31%
(2019)
23%
(2019)
38%
(2016)
16%
(2021)
22%
(2019)
14%
(2022)
15%
(2021)
13%
(2022)
10%
(2022)
7%
(2021)
18%
(2022)
18%
(2022)
0%
(2022)
2021
15%
7%
(2022)
10%
(2022)
13%
(2022)
9%
(2022)
0% 10% 20% 30% 40% 50% 60%
2022 Result (Opiates)

MARYLAND DEPARTMENT OF HEALTH
50 | Page
Figure 40: High and Low Yearly Percentages Testing Positive for Cocaine
at 13 Hospital EDs
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Figure 41 shows that amphetamine/methamphetamine also reached series highs in seven hospitals in
2022, which included both hospitals in Western Maryland (UPMC, Meritus Medical Center). The series
high percentages positive for amphetamine/methamphetamine ranged from 5 percent to 27 percent.
52%
32%
30%
20%
30%
52%
57%
38%
30%
17%
22%
29%
15%
Meritus Medical Center
TidalHealth Peninsula Regional Hospital
UM Baltimore Washington Medical Center
UM Charles Regional Medical Center
UM Harford Memorial Hospital
UM Medical Center
UM Medical Center, Midtown Campus
UM Shore Emergency Center at Queenstown
UM Shore Medical Center at Chestertown
UM Shore Medical Center at Easton
UM St. Joseph Medical Center
UM Upper Chesapeake Medical Center
UPMC Western Maryland
52%
(2022)
32%
(2022)
30%
(2022)
23%
(2020)
30%
(2022)
52%
(2022)
57%
(2022)
45%
(2020)
43%
(2021)
27%
(2019)
22%
(2022)
29%
(2022)
23%
(2021)
30%
(2020)
26%
(2018)
22%
(2020)
19%
(2019)
26%
(2021)
37%
(2016)
43%
(2016)
33%
(2019)
30%
(2022)
17%
(2022)
19%
(2016)
18%
(2020)
15%
(2022)
0% 10% 20% 30% 40% 50% 60%
2022 Result (Cocaine)

DORM 2022 ANNUAL REPORT
51 | Page
Figure 41: High and Low Yearly Percentages Testing Positive for
Amphetamine/Methamphetamine at 13 Hospital Eds
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Positive tests for THC reached a series high in nine hospitals in 2022, with two other hospitals nearing a series
high (UMMC, UM Baltimore Washington). Ten hospitals reported that more than 30 percent tested positive
for THC.
27%
3%
9%
11%
22%
5%
5%
0%
7%
10%
6%
22%
17%
Meritus Medical Center
TidalHealth Peninsula Regional Hospital
UM Baltimore Washington Medical Center
UM Charles Regional Medical Center
UM Harford Memorial Hospital
UM Medical Center
UM Medical Center, Midtown Campus
UM Shore Emergency Center at Queenstown
UM Shore Medical Center at Chestertown
UM Shore Medical Center at Easton
UM St. Joseph Medical Center
UM Upper Chesapeake Medical Center
UPMC Western Maryland
27%
(2022)
6%
(2020)
9%
(2022)
12%
(2020)
22%
(2022)
5%
(2022)
5%
(2022)
17%
(2019)
10%
(2021)
14%
(2019)
11%
(2020)
22%
(2022)
17%
(2022)
10%
(2019)
3%
(2022)
5%
(2019)
11%
(2022)
19%
(2020)
1%
(2016)
2%
(2021)
0%
(2022)
4%
(2019)
8%
(2020)
3%
(2017)
10%
(2020)
10%
(2019)
0% 5% 10% 15% 20% 25% 30%
2022 Result (Amphetamine/methamphetamine)

MARYLAND DEPARTMENT OF HEALTH
52 | Page
Figure 42: High and Low Yearly Percentages Testing Positive for THC at 13 Eds
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Summary of Cross-Hospital Comparisons
Table 2, below, shows substances that reached an annual series high or low in 2022 in 13 hospitals. Six-
year highs/lows could not be calculated for the three hospitals in the Capital Region and one on the
Eastern Shore because they had very low positivity rates or too small a range of results to establish a
meaningful range. All six of the hospitals in Central Maryland reached series highs for cocaine-positive
test results in 2022, and five of them also reached series highs for amphetamine and/or
methamphetamine. This suggests that stimulant use may be increasing among ED patients in these
hospitals. In contrast, four of the six Central Maryland hospitals reached series lows in opiate-positive test
results, reflecting a national trend towards lower heroin use as it is being displaced by fentanyl. Nine of
the 13 hospitals, including four in Central Maryland, reached series highs for THC-positive test results. It
is important to note that the presence of a positive test for THC does not necessarily indicate that cannabis
use was related to the reason a patient came to the ED. Four hospitals – Meritus, UM Upper Chesapeake,
UM Harford, and UMMC Midtown – reached series highs in three or more of the substances shown.
48%
37%
31%
34%
44%
25%
25%
69%
28%
34%
37%
40%
35%
Meritus Medical Center
TidalHealth Peninsula Regional Hospital
UM Baltimore Washington Medical Center
UM Charles Regional Medical Center
UM Harford Memorial Hospital
UM Medical Center
UM Medical Center, Midtown Campus
UM Shore Emergency Center at Queenstown
UM Shore Medical Center at Chestertown
UM Shore Medical Center at Easton
UM St. Joseph Medical Center
UM Upper Chesapeake Medical Center
UPMC Western Maryland
48%
(2022)
43%
(2021)
34%
(2021)
34%
(2022)
44%
(2022)
26%
(2020)
25%
(2022)
69%
(2022)
36%
(2020)
34%
(2022)
37%
(2022)
40%
(2022)
35%
(2022)
39%
(2019)
26%
(2018)
24%
(2019)
24%
(2019)
32%
(2021)
15%
(2018)
16%
(2019)
2019
33%
24%
(2019)
31%
(2021)
18%
(2017)
28%
(2020)
32%
(2020)
0% 20% 40% 60% 80%
2022 Result (THC)

DORM 2022 ANNUAL REPORT
53 | Page
Table 2: MD-EDDS Hospitals with Yearly Series Highs and Lows
for Four Substances in 2022
Hospital THC Opiates
Amphetamine/
Methamphetamine
Cocaine
Western Maryland
Meritus Medical Center
H (48%) L (14%) H (27%) H (52%)
UPMC
H (35%) L (9%) H (17%) L (15%)
Southern Maryland
UM Charles Regional Medical
Ctr.
H (34%) L (10%) L (11%)* —
Central Maryland
UM
Balt Wash Medical Center
— L (13%) H (9%) H (30%)
UM Upper Chesapeake Med Ctr
.
H (40%) L (13%) H (22%) H (29%)
UM Harford Memorial Hospital
H (44%) H (12%) H (22%) H (30%)
UM Medical Center
— L (18%) H (5%) H (52%)
UM Medical Center, Midtown
H (25%) L (18%) H (5%)* H (57%)
UM St. Joseph Medical Center
H (37%) L (10%) — H (22%)*
Eastern Shore**
UM Shore Med Ctr Chestertown
— — — L (30%)
UM Shore Emergency
Ctr.
Queenstown
H (69%) L (0%) L (0%) —
UM Shore Med
.
Ctr
.
Easton
H (34%) L (7%) — L (17%)
TidalHealth Peninsula Regional
Hospital
— — L (3%)* H (32%)
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*If the same percentage occurred in more than one year, the latest occurrence is shown.
**Series highs/lows not calculated for four hospitals: UM Bowie Health Center, UM Capital Region Medical
Center, UM Laurel Medical Center, and UM Shore Medical Center Cambridge. Only 1-2 years in current data
run.

MARYLAND DEPARTMENT OF HEALTH
54 | Page
Statewide Hospital Demographics
Individuals aged 55 and older are represented in a higher proportion of OD-related ED visits compared to
other age groups, regardless of whether there was an opioid-positive urine specimen or not. Non-Hispanic
Whites made up the majority of OD-related ED visits. However, when looking specifically at visits that
involved an opioid-positive specimen, non-Hispanic Whites and non-Hispanic Blacks experienced similar
rates, at 48.6 percent and 47.4 percent, respectively. Males comprised a majority in all OD-related ED
visits and those with an opioid-positive urine specimen with 55.0 percent and 62.6 percent, respectively.
Figure 43: Drug Overdose-Related ED Visits, with and without a Positive Opioid
Specimen, by Age, Race/Ethnicity, and Gender – Statewide
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
Fentanyl Dipstick Study Results
MD-EDDS staff offered 50 fentanyl dipstick tests to each MD-EDDS hospital that was not yet routinely
testing fentanyl with which to test urine specimens they had collected. Each hospital tested up to 50
consecutive specimens obtained from adult patients that had tested positive for at least one substance
on the hospital’s toxicology screen. Patients came from any unit of the hospital that had not been
administered fentanyl as part of their medical care. The results from the dipstick testing were reported to
EDDS.
In 2023, the findings (below) from this sub-study were used to support Maryland’s passage of the Josh
Siems Act, which requires all Maryland hospitals to begin routinely testing for fentanyl in urine toxicology
55.0%
62.6%
44.96%
37.39%
Total
Positive
for Opioids
Male Female
Gender
63.7%
48.6%
31.0%
47.4%
2.8%
2.2%
2.6%
4.5%
Total
Positive
for Opioids
White NH Black NH Hispanic Other
Race/Ethnicity
9.9%
3.8%
19.0%
18.5%
18.2%
19.0%
13.5%
18.4%
39.2%
40.3%
Total
Positive
for Opioids
18-24 25-34 35-44 45-54 55+
Age Group
DORM 2022 ANNUAL REPORT
55 | Page
screens when used for patient diagnoses. Between 2–4 percent of patient samples were positive for
fentanyl. Three hospitals saw rates of 20 percent or more – UM Shore Medical Center in Chestertown,
UPMC Western Maryland in Cumberland, and Meritus Medical Center in Hagerstown. Across all of the
hospitals, only 23 percent of samples also tested positive for opiates like heroin by the hospitals’ standard
screens, suggesting that the opiate screen would have not identified these patients.
Table 3: MD-EDDS Fentanyl Dipstick Study Results by Hospital
(50 positive specimens submitted by each hospital)*
Hospital
Positive for Fentanyl by
Dipstick
UM Shore Medical Center at Chestertown, Chestertown, MD (n=50) 24%
UPMC Western Maryland, Cumberland, MD (50) 22%
Meritus Medical Center, Hagerstown, MD (50) 20%
UM Harford Memorial Hospital, Havre de Grace, MD (50) 18%
UM Baltimore Washington Medical Center, Glen Burnie, MD (50) 14%
UM Upper Chesapeake Medical Center, Bel Air, MD (50) 14%
UM Shore Medical Center at Cambridge, Cambridge, MD (50) 12%
TidalHealth Peninsula Regional, Salisbury, MD (50) 8%
UM Laurel Medical Center, Laurel, MD*
(38) 8%
UM Capital Region Medical Center, Largo, MD (50) 6%
UM Charles Regional Health Center, La Plata, MD (50) 4%
UM Shore Medical Center at Easton, Easton, MD (50) 2%
All Above Hospitals (588) 13%
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*Consecutive specimens were selected from any hospital unit that the hospital’s testing had found
positive for at least one drug. Patients that were administered fentanyl as part of their medical care
at the hospital were excluded. UM Laurel Medical Center only had 38 specimens collected. UM
Bowie Health Center (N=11) and UM Shore Emergency Center at Queenstown (N=10) were
excluded due to low specimen counts.

MARYLAND DEPARTMENT OF HEALTH
56 | Page
The map below shows a red dot for the hospitals included in this study, with their corresponding locations.
The size of the red dot reflects the percentage who tested positive for fentanyl.
Map 3: Hospitals Included in Study (2022)
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*Consecutive specimens were selected from any hospital unit that the hospital’s testing had found
positive for at least one drug. Patients that were administered fentanyl as part of their medical care
at the hospital were excluded.
Table 4, below, shows that patients testing positive for fentanyl were more likely to be males than persons
testing negative (67 percent vs. 54 percent, p < .05). White patients made up the majority of patients
testing positive or negative for fentanyl. The average age of both groups of patients was similar (39.4/40.5
years).

DORM 2022 ANNUAL REPORT
57 | Page
Table 4: MD-EDDS Fentanyl Dipstick Study—Patient Demographics by Fentanyl
Dipstick Result, None of Which Routinely Test Patients for Fentanyl
(588 specimens submitted by 12 hospitals)*
Demographics
Positive for Fentanyl
by Dipstick
(N=75) %
Negative for Fentanyl
by Dipstick
(N=513) %
Gender
Male 67* 54*
Female 33 46
Total 100% 100%
Race
*
White 58 58
Black/African American 39 36
Asian 1 1
Other 3 5
Total 100% 100%
Mean Age
39.4
(range 20
-
63)
40.5
(range 18
-
91)
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*Consecutive specimens were selected from any hospital unit that the hospital’s testing had found
positive for at least one drug. Patients that were administered fentanyl as part of their medical care
at the hospital were excluded.
Hospitals include: UM Shore Medical Center at Chestertown (Chestertown, MD), Meritus Medical
Center (Hagerstown, MD), UM Baltimore Washington Medical Center (Glen Burnie, MD), UM Upper
Chesapeake Medical Center (Bel Air, MD), UM Shore Medical Center at Cambridge (Cambridge,
MD), UM Capital Region Medical Center (Largo, MD), UM Charles Regional Health Center (La Plata,
MD), UM Shore Medical Center at Easton (Easton, MD), UM Harford Memorial Hospital (Havre de
Grace, MD), TidalHealth Peninsula Regional (Salisbury, MD), UPMC Western Maryland
(Cumberland, MD), and UM Laurel Medical Center (Laurel, MD).
UM Laurel Medical Center only had 38 specimens collected. UM Bowie Health Center (N=11) and
UM Shore Emergency Center at Queenstown (N=10) were excluded due to low specimen counts.
*p<.05 by Chi-Square.
**One patient was missing race information.

MARYLAND DEPARTMENT OF HEALTH
58 | Page
Table 5 shows the other substances found through routine testing in specimens that tested positive or
negative for fentanyl. Cocaine, THC, and benzodiazepines were the substances most common in
specimens positive for fentanyl. There were some differences in the substances detected between the
two groups. Specimens positive for fentanyl were more likely to also test positive for cocaine (57 percent
vs. 24 percent, p < .001), opiates (23 percent vs. 11 percent, p < .01), and methadone (27 percent vs. 8
percent, p < .001) and less likely to test positive for THC (43 percent vs. 59 percent, p < .05).
Table 5: Other Drugs Detected by the Hospital’s Routine Tests
by Fentanyl Dipstick Result
(N=588 specimens submitted by 12 hospitals)*
Hospital Also
Found Positive for:
Specimens Positive
for Fentanyl
(N=75) %
Specimens
Negative for
Fentanyl
(N=513) %
Cocaine 57*** 24***
THC (n=74) 43* (n=511) 59*
Benzodiazepines 28 20
Methadone (n=63) 27*** (n=340) 8***
Opiates 23** 11**
Amphetamines 17 10
Oxycodone (n=26) 8 (n=224) 10
PCP (n=56) 7 (n=382) 6
Barbiturates 3 4
Buprenorphine (n=10) 0 (n=47) 9
Source: University of Maryland Center for Substance Use, Addiction & Health Research.
*Consecutive specimens were selected from any hospital unit that the hospital’s testing had found
positive for at least one drug. Patients that were administered fentanyl as part of their medical care
at the hospital were excluded.
Hospitals include: UM Shore Medical Center at Chestertown (Chestertown, MD), Meritus Medical
Center (Hagerstown, MD), UM Baltimore Washington Medical Center (Glen Burnie, MD), UM Upper
Chesapeake Medical Center (Bel Air, MD), UM Shore Medical Center at Cambridge (Cambridge,
MD), UM Capital Region Medical Center (Largo, MD), UM Charles Regional Health Center (La Plata,
MD), UM Shore Medical Center at Easton (Easton, MD), UM Harford Memorial Hospital (Havre de
Grace, MD), TidalHealth Peninsula Regional (Salisbury, MD), UPMC Western Maryland
(Cumberland, MD), and UM Laurel Medical Center (Laurel, MD).
UM Laurel Medical Center only had 38 specimens collected. UM Bowie Health Center (N=11) and
UM Shore Emergency Center at Queenstown (N=10) were excluded due to low specimen counts.
Ns vary due to hospitals not testing for each drug; *p<.05, **p<.01, ***p<.001 by Chi-Square.

DORM 2022 ANNUAL REPORT
59 | Page
Medicaid MOUD
Table 6, below, presents the number and percentage of individuals who were enrolled in Medicaid at any
point within 12 months of their death and received any form of MOUD between 2017 and 2021.
Buprenorphine treatment was consistently the most utilized type of MOUD among participants. The
number of participants who received buprenorphine treatment increased by 5.1 percentage points during
this time frame. Methadone treatment was the next most commonly utilized MOUD among participants,
decreasing by 5.5 percentage points across the evaluation period.
16
Naltrexone treatment was the least
common type of MOUD, with a slight decrease of 0.8 percentage points in participants from 2017 to 2018
followed by a sudden increase in 2019 of 2.8 percentage points, a sharp decline in 2020 of 5 percentage
points, and a slight increase in 2021 of 0.9 percentage points. The number of relevant dispenses and
services billed for buprenorphine and methadone increased sharply between 2017 and 2018, as well as
between 2019 and 2020. Trends for participants enrolled in Medicaid within 12 months of an OD death
and for participants enrolled in Medicaid at the time of an OD death are similar.
Table 6 Medicaid Participants Who Received MOUD
within a Year of Their Death (2017–2021)
Event Type
Eligible Within One Year of Death
2017
2018
Number of
Participants
Percent
of Total
Number of
MOUD
Dispenses or
Services
Number of
Participants
Percent
of Total
Number of
MOUD
Dispenses or
Services
At least one
buprenorphine
treatment
242 52.4% 2,921 294 53.3% 5,637
At least one
methadone
treatment
236 51.1% 5,720 263 47.6% 6,884
At least one
Naltrexone
treatment
68 14.7% 214 77 13.9% 183
Total 462 - 8,855 552 - 12,704
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).
16
The Hilltop Institute. (2023, April 14). Medicaid Data for DORM Report. Baltimore, MD: UMBC.
MARYLAND DEPARTMENT OF HEALTH
60 | Page
2019 2020
Number of
Participants
Percent of
Total
Number of
MOUD
Dispenses or
Services
Number of
Participants
Percent of
Total
Number of
MOUD
Dispenses or
Services
At least one
buprenorphine
treatment
338 58.7% 5,568 384 58.3% 9,148
At least one
methadone
treatment
254 44.1% 6,408 293 44.5% 8,628
At least one
Naltrexone
treatment
96 16.7% 281 77 11.7% 254
Total 576 - 12,257 659 - 18,025
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).
2021
Number of
Participants
Percent of Total
Number of MOUD
Dispenses or
Services
At least one
buprenorphine
treatment
371 57.5% 7,592
At least one
methadone
treatment
294 45.6% 9,073
At least one
Naltrexone
treatment
81 12.6% 196
Total 649 - 16,861
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).

DORM 2022 ANNUAL REPORT
61 | Page
Other (non-MOUD) Mental Health and SUD Services
PBHS Service Connection
The following six jurisdictions had over 60 percent of their OD decedents engaged in PBHS services:
Allegany County, Anne Arundel County, Baltimore City, Cecil County, Queen Anne’s County, Washington
County, and Wicomico County. The following five jurisdictions had less than 40 percent of their OD
decedents engaged in PBHS services: Dorchester County, Garrett County, Kent County, Prince George’s
County, and Talbot County.
Map 4: Overdose Decedents Engaged in PBHS Services by Jurisdiction of
Residence (2021)
Source: MDH Behavioral Health Administration.
Targeted Naloxone Distribution
Providing naloxone to individuals who are at the highest risk for OD is a critical strategy for reducing OD-
related mortality. Targeted naloxone distribution programs work best when: 1) naloxone is provided to
people at high risk of experiencing or witnessing an OD; and 2) outreach workers, harm reduction staff,
trusted clinicians and first responders who are properly educated and comfortable distributing naloxone
to those using illicit opioids or receiving a high-risk opioid prescription. To have the greatest impact in
preventing OD death, individuals need to feel comfortable carrying and using naloxone. In 2021, 83.8
Legend

MARYLAND DEPARTMENT OF HEALTH
62 | Page
percent of OD decedents in Maryland were not administered naloxone showing the need for naloxone
saturation.
17
To better understand how local jurisdictions are reaching people at the highest risk for OD with naloxone
distribution efforts, CHRS developed a naloxone saturation formula to track and identify the correlation
between the level of distributed naloxone compared to the number of OD fatalities in each corresponding
jurisdiction.
Applying the naloxone saturation formula provides a framework for how to best address naloxone
distribution in communities. Technical assistance and resource allocation can be provided to jurisdictions
to ensure jurisdictions are able to reach people at greatest risk for OD with naloxone and to ensure
naloxone is distributed at levels where it can contribute to the greatest possible decrease in OD fatalities.
The map below shows naloxone saturation in 2022 by jurisdiction. In 2022, eleven jurisdictions did not
reach naloxone saturation targets, one jurisdiction was between 0.0 and 49.9 percent above saturation
targets, six jurisdictions achieved naloxone saturation between 50 and 100 percent, and six jurisdictions
achieved more than 100 percent of their targeted naloxone saturation.
Map 5: Naloxone Saturation* Map of Maryland (2022)
Source: MDH Center for Harm Reduction Services.
*Saturation numbers are based on Overdose Response Program (ORP) Distribution only.
17
Statewide Unintentional Drug Overdose Reporting System (SUDORS): overdose fatality circumstances and decedent
characteristics.
Legend

DORM 2022 ANNUAL REPORT
63 | Page
Syringe Service Programs
SSPs are community-based programs that offer an array of services, including provisions to curtail the
transmission of infectious disease, linkages to SUD treatment, and other social support resources, such as
vaccinations, OD education and naloxone distribution, wound care, and both testing and linkage to care
for infectious disease. There were 23 approved SSPs in Maryland by the end of the 2022 calendar year,
three more than last year.
In 2022, 22,959 individuals were served by SSPs with 6,987 new/registered participants during calendar
year 2022. There were 69,505 linkages to care made for individuals engaged with SSPs in 2022, up 59.2
percent from last year, demonstrating the importance of these programs in serving people who use drugs
with low-barrier services.
Figure 44: Individuals Served Through SSPs by Quarter (2020–2021)
Source: MDH Center for Harm Reduction Services.
EMS Transportation
MIEMSS provided emergency encounter data to support the research and analysis of linked data sets
related to EMS incidents involving opioid OD. Between January 1, 2021, and December 31, 2022, there
were 34,094 EMS incidents identified as involving an opioid OD (out of a total of 1,251,050 incidents).
Incidents were divided based on whether the patient was transported, not transported, or deceased.
Incidents reflect only a unique incident, not necessarily a unique individual; thus, an individual may have
had more than one opioid-involved incident with an EMS response.
72.5 percent of opioid-related OD incidents resulted in a transport in 2021, and 73.1 percent resulted in
a transport in 2022. Comparing demographics of patients who were transported to patients who were
not transported, data showed that patients who were transported tended to be younger, were more likely
to be male, were more likely to be White, and were more likely to be in the Eastern Shore region.
2,039
4,553
5,058
3,166
5,913
5,424
3,922
6,703
6,627
4,352
5,065
5,850
0
2,000
4,000
6,000
8,000
2020 2021 2022
Quarter 1 Quarter 2 Quarter 3 Quarter 4

MARYLAND DEPARTMENT OF HEALTH
64 | Page
Hospital Characteristics
The HSCRC collects a variety of demographic, financial, and other clinical information related to patient
care (e.g., nature of admission, diagnostic codes, etc.) at acute care and licensed specialty hospitals across
the State of Maryland. Between January 1, 2016, and December 31, 2021, 8,958 OD decedents received
care through Maryland’s hospital system in an inpatient or ED facility at some point during the same six-
year period.
Of the individuals who died from an OD with an HSCRC record between 2016 and 2021, 40.9 percent had
received care for an OD-related encounter at some point in the seven-year study period. Over one-quarter
(24.2 percent) of individuals who died from an OD had a chronic pain diagnosis, as compared to 7.2
percent of non-OD decedents with HSCRC records. About one-fifth (22.0 percent) of non-OD decedents
had a mental health diagnosis, while 51.5 percent of individuals with an HSCRC record who died from an
OD had a mental health diagnosis. Less than half (45.9 percent) of people with an HSCRC record who died
from an OD were previously diagnosed with OUD and 58.1 percent of people with an HSCRC record who
died from an OD were previously diagnosed with a non-opioid SUD.
Table 7: HSCRC Encounters by Prior Diagnosis (2016–2021)
Non-OD decedents with
HSCRC records
OD decedents with
HSCRC records
p
value**
Total Individuals
3,392,034 8,958
N % N %
OD-related encounters, ever
100,907 3.0 3,666 40.9 <0.001
OD-related encounters, by substance...
Heroin
20,427 0.6 1,949 21.8 <0.001
Methadone
3,071 0.1 176 2.0 <0.001
Other Opioid
41,224 1.2 1,405 15.7 <0.001
Alcohol
3,252 0.1 152 1.7 <0.001
Benzodiazepine
13,163 0.4 515 5.7 <0.001
Cocaine
6,507 0.2 608 6.8 <0.001
Other Substance*
40,036 1.2 936 10.4 <0.001
OUD
90,523 2.7 4,111 45.9 <0.001
SUD (non-opioid)
356,089 10.5 5,203 58.1 <0.001
Non-poisoning Injury
1,288,577 38.0 4,764 53.2 <0.001
Chronic Pain Diagnosis
242,681 7.2 2,168 24.2 <0.001
Mental Health Diagnosis
747,161 22.0 4,612 51.5 <0.001

DORM 2022 ANNUAL REPORT
65 | Page
Injection SU-related wounds
418,099 12.3 2,390 26.7 <0.001
Source: Maryland Health Services Cost Review Commission.
Health services encounters were compared between overdose decedents and non-overdose decedents with records captured within
the HSCRC case mix data stream between 2016-2021. Individuals identified as non-overdose decedents may either be alive or
deceased due to means other than drug intoxication during the study period. Overdose-related encounters encapsulate any overdose
encounter (overall or by substance) during the study period as a binary (0/1) count per individual. An individual may have had
multiple overdoses, by multiple substances but would only be counted once under "Overdose-related encounters, ever" and once per
specified substance(s). Thus, the total of "Overdose-related encounters, by substance" will sum to a greater total than overall
overdose-related encounters.
* Other drugs include amphetamine, barbiturates, non-opioid analgesics, and other drug poisonings.
**Chi-squared test of independence was used to assess any associations between the predictor variables of various overdose types
and related diagnoses and overdose death.
Source: HSCRC case mix and overdose death records data, 2016-2021
Even though there was an increase in fatal ODs nearly every year, this data illustrates a downward trend
among individuals with OUD, SUD, or mental health diagnoses who were not interacting with hospital
services at the same level they were in previous years. Fewer people reporting to hospitals for services
could be attributed to expanded community-based services.
Table 8: HSCRC Encounters by Prior Diagnosis (2016–2021)
2016 2017 2018 2019 2020 2021
Total deaths (N) 1,848 2,008 2,241 2,235 2,629 2,632
N % N % N % N % N % N %
Any service utilization 966 52.3
1004
50.0
1047
46.7
969
43.4
1091
41.5
1133
43.0
Any OD-related services 336 34.8
339 33.8
347 33.1
316
32.6
342 31.3
326 28.8
OUD 354 36.6
358 35.7
364 34.8
357
36.8
359 32.9
379 33.5
SUD (non-opioid) 461 47.7
469 46.7
477 45.6
442
45.6
496 45.5
515 45.5
Non-poisoning Injury 268 27.7
265 26.4
299 28.6
308
31.8
311 28.5
326 28.8
Chronic Pain Diagnosis 161 16.7
140 13.9
164 15.7
143
14.8
162 14.8
163 14.4
Mental Health Diagnosis
382 39.5
407 40.5
438 41.8
405
41.8
447 41.0
422 37.2
Source: Maryland Health Services Cost Review Commission.
Inpatient and emergency department health services utilization among MD resident drug intoxication decedents aged 15-90 during
calendar year of death, 2016-2021. Decedents' service utilization and diagnoses are only counted here if they occurred during the
same calendar year as their death. Decedents may have accessed services in previous years for overdose or other diagnoses, either
during the study period or prior to 2016. Such service utilization is not captured here to maintain consistency across the years and
avoid artificial inflation of service use in later years of the study period.
The denominator for (%) service utilization is "Total Deaths" in the year; otherwise, the (%) for subsequent care (e.g., any overdose-
related services, opioid use disorder diagnosis, etc.) are calculated from the total (N) of "Any service utilization."
Source: HSCRC case mix and overdose death records data, 2016-2021
Service Utilization by Medicaid Participants

MARYLAND DEPARTMENT OF HEALTH
66 | Page
Table 9, below, presents the number and percentage of
participants who had an ambulatory care visit, outpatient
ED visit, or inpatient admission during the year of their fatal
OD. Between 2017 and 2021, the majority of these
individuals had an ambulatory care visit during the year of
their fatal OD; the percentage with an ambulatory care visit
rose from 59.4 percent in 2017 to 63.8 percent in 2020 and
fell to 61.9 percent in 2021.
18
The percentages of participants with a fatal OD who had an outpatient ED visit and an inpatient admission,
respectively, each experienced a decrease of 4 percentage points each over the evaluation period.
19
Table 9: Service Utilization of Medicaid Participants (Any Period of Eligibility)
before a Fatal Overdose (2017–2021)
Service Type
2017 2018 2019 2020 2021
# % # % # % # % # %
Ambulatory Care 822
59.4%
897
59.4%
901
62.0%
1,132 63.8%
1,107
61.9%
Outpatient ED 677
48.9%
711 47.1%
674
46.4%
789 44.5%
804 44.9%
Inpatient
Admission
407
29.4%
411 27.2%
386
26.6%
440 24.8%
454 25.4%
Total 1,384 1,509 1,453 1,774 1,789
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).
Table 10, below, displays data for inpatient admissions with a diagnosis of poisoning within one year of
death and within one day of death. Across both timeframes, the percentage of participants who had an
inpatient admission with a diagnosis of poisoning during the respective timeframe decreased over the
evaluation period. The number of participants who had an admission with a diagnosis of poisoning within
a year of death decreased from 8.6 percent in 2017 to 6.2 percent in 2021, and the percentage of
participants who had an admission with a diagnosis of poisoning within one day of their death fell from
3.0 percent to 1.7 percent. The number of users and the number of visits also decreased for both
timeframes over the evaluation period. Trends for participants enrolled in Medicaid within 12 months of
OD death and for participants enrolled in Medicaid at the time of OD death are similar.
20
Table 10. Number of Visits and Participants (Any Period of Eligibility) with an
Inpatient Admission with a Diagnosis of Poisoning Before a Fatal Overdose
(2017–2021)
18
The Hilltop Institute. (2023, April 14). Medicaid Data for DORM Report. Baltimore, MD: UMBC.
19
Ibid.
20
Ibid.

DORM 2022 ANNUAL REPORT
67 | Page
Year of Fatal
Overdose
Within Year of Death Within 1 Day of Death
Visits Users
Total
Eligible
% of
Total
Visits Users
Total
Eligible
% of
Total
2017 149 121 1,413 8.6% 46 43 1,413 3.0%
2018 142 121 1,548 7.8% 50 47 1,548 3.0%
2019 151 118 1,513 7.8% 38 33 1,513 2.2%
2020 141 116 1,834 6.3% 35 34 1,834 1.9%
2021 133 112 1,795 6.2% 31 31 1,795 1.7%
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).
Summary of Service Utilization
The percent of OD decedents with a controlled substance dispensed by race from 2016-2021 shows a
continued trend of decreasing percent of NH White individuals and an increasing percent of NH Black
individuals. Six jurisdictions achieved more than 100 percent of their targeted naloxone saturation. In
2022, 22,959 individuals were served by SSPs with 6,987 new/registered participants and there were
69,505 linkages to care made for individuals engaged with SSPs in 2022, up 59.2 percent from last year. In
2021 and 2022, opioid-related OD incidents resulting in EMS transport, occurred 72.5 and 73.1 percent of
the time respectively. In 2023, the findings from the EDDS fentanyl dipstick sub-study were used to
support Maryland’s passage of the Josh Siems Act, which requires all Maryland hospitals to begin routinely
testing for fentanyl in urine toxicology screens when used for patient diagnoses. Over the past six years,
heroin has decreased by 53.9 percent (from 447 to 206) in overall fatal ODs among those dispensed a
controlled substance, while fentanyl has increased by 241.1 percent from 431 to 1470 in overall fatal ODs
among those dispensed a controlled substance.
See Considerations and Limitations to Analysis section for more details.

MARYLAND DEPARTMENT OF HEALTH
68 | Page
Acknowledgments
The OOCC would like to acknowledge and thank the following partners for their contribution to the 2022
DORM report:
Behavioral Health Administration (BHA)
Chesapeake Regional Information Systems for our Patients (CRISP)
Johns Hopkins Bloomberg School of Public Health (JHSPH)
Maryland Department of Health (MDH)
Center for Harm Reduction Services (CHRS)
Environmental Health Bureau
Health Services Cost Review Commission (HSCRC)
Overdose Data to Action Program (OD2A)
Prescription Drug Monitoring Program (PDMP)
Vital Statistics Administration (VSA)
Maryland Total Human-services Integrated Network (MD THINK)
The Hilltop Institute, University of Maryland Baltimore County
The University of Maryland School of Medicine Systems Evaluation Center
Maryland Institute for Emergency Medical Services Systems (MIEMSS)
Emergency Department Drug Surveillance (EDDS)
Center for Substance Use, Addiction & Health Research (CESAR)

DORM 2022 ANNUAL REPORT
69 | Page
VI. CONSIDERATIONS AND LIMITATIONS TO ANALYSIS
Health Services Cost Review Commission
The validity of matching individuals across disparate data sets is not wholly guaranteed and is
limited by the availability and accuracy of the data contained within the informant data sources.
Official substance and alcohol intoxication deaths are considered preliminary and subject to
change until officially validated and released by VSA.
Demographics and geographic residence were compared between OD decedents and non-OD
decedents with inpatient and/or ED records captured within the HSCRC or OD death registry
between 2016-2021
o Individuals identified as non-OD decedents may either be alive or deceased due to means
other than substance intoxication during the study period.
Encounters consist of any health services encounter captured in the HSCRC between 2016-2021
Small data sets have been suppressed to protect privacy.
The total of "OD-related encounters, by substance" will sum to a greater total than overall OD-
related encounters.
o An individual may have had multiple ODs, by multiple substances but would only be
counted once under "OD-related encounters, ever" and once per specified substance(s)
Other substances include amphetamine, barbiturates, non-opioid analgesics, and other drug
poisonings.
Prescription Drug Monitoring Program
Data sets were linked in SQL Server on unique PatientID.
Only the most recent dispense records were used from the PDMP data set to get patient-level
data.
The values in these tables represent the number of individuals who had a dispense record in the
PDMP and an OD death record.
All tables evaluate the OD decedents from 2016 to 2021 who also had dispense records in the
PDMP.
Center for Harm Reduction Services
Some active ORPs may be missing reports due to reporting lag.
Kit/unit estimates are based on the assumption of two doses dispensed per kit/unit, which may
occasionally be incorrect.
o CHRS collects naloxone dispense data in terms of doses.
Each kit/unit of naloxone includes two (2) doses.
Incomplete (not yet submitted) reports could impact data totals.
Saturation numbers are based on ORP Distribution only, no pharmacy distribution due to a delay
in reporting.
Washington/Baltimore High-Intensity Drug Trafficking Area
The samples in this report are not representative of all drugs seized in the entire state of
Maryland.

MARYLAND DEPARTMENT OF HEALTH
70 | Page
Hilltop
The data provided follow the Department’s cell suppression guidelines (i.e., cells with 10 or fewer
participants are suppressed to avoid potential identification of participants)
Hilltop used the list of OD deaths provided by the VSA to identify Medicaid participants who died
of an OD.
o After confirming that participants were enrolled in Medicaid at any point, Hilltop
identified participants who had been enrolled in Medicaid for at least one day in the year
prior to their death and/or at the time of their death.
o Only participants who were enrolled in Medicaid within a year of their death were
included in the analysis.
“eligible/eligibility” and “enrolled/enrollment” are used interchangeably.
Hilltop gathered all fee-for-service (FFS) claims and managed care organization encounters for the
services targeted for this analysis (e.g., MOUD, non-fatal poisoning, ED visits, ambulatory care
visits, and inpatient admissions)
Medicaid participants who died due to an OD may have died due to a non-opioid-related
substance.
ED visits were defined as an institutional claim or encounter with a revenue code starting with
“045” or “0981.”
o ED visits resulting in an inpatient admission were classified as inpatient admissions.
Inpatient admissions were defined as inpatient institutional claims or encounters
with a claim type of “I” or “M.”
Poisoning events were identified using the International Classification of Diseases, Tenth Revision,
Clinical Modification (ICD-10-CM) diagnosis codes selected by the Department.
The data presented are current as of March 2022
Johns Hopkins Bloomberg School of Public Health Center for Population Health Information Technology
Data reported is analysis of matched records from PDMP, HSCRC, and OCME.
Data linkage performed by CRISP.
Analysis performed by research partners at JHSPH.
JHSPH identified “first” NFOD episodes, or an index NFOD event, meaning the first NFOD occurring
in the data between July 2016 - December 2020, and examined characteristics in the six months
prior to the index NFOD and the following year.
To understand the characteristics associated with buprenorphine use after an index NFOD, three
subsamples were examined:
o People who did not get buprenorphine in the year following the index NFOD;
o People who had a buprenorphine prescription in the four weeks following the index
NFOD; and
o People who started buprenorphine more than four weeks but less than a year after the
index NFOD.
Rates displayed in Table 14 are crude (unadjusted) and do not account for differences in severity
of SUD or underlying comorbidities at baseline between the three groups.
Regions in Table 15 were specified as follows: 1) Capital: Frederick, Montgomery, Prince George’s;
2) Central: Anne Arundel, Baltimore City, Baltimore County, Carroll, Harford, Howard; 3) Eastern
Shore: Caroline, Cecil, Dorchester, Kent, Queen Anne’s Somerset, Talbot, Wicomico, Worcester;
4) Southern: Calvert, Charles, St. Mary’s; 5) Western: Allegany, Garrett, Washington.

DORM 2022 ANNUAL REPORT
71 | Page
Maryland Institute for Emergency Medical Services Systems
MIEMSS manages the EMS system throughout Maryland in various ways. MIEMSS has partnered
with MDH to provide emergency encounter data to support the research and analysis of linked
data sets for the DORM report. This is the first year in partnership and this partnership opens the
door for future linked analysis from EMS encounter to hospital to outside linked care.
Data were drawn from the MIEMSS data set between January 1, 2021, and December 31, 2022.
During this two-year period, out of 1,251,050 unique incidents identified in the MIEMSS data set,
34,094 were identified as related to an opiate OD, using a definition of opioid OD incident that
was adapted from the MDH workgroups.
Incidents are grouped into individuals who were transported, not transported, or deceased.
Incidents reflect just that of one incident, not one patient. One patient may have multiple
incidents over time in this data set.
Public Behavioral Health System
● Data is subject to change from delayed claims.
○ Outpatient services are generally not covered by Medicare.
● Sources of OD Deaths:
○ Office of the Chief Medical Examiner/VSA Database.
○ Unintentional OD Deaths Only.
● All data is provisional and subject to updating.
● Prior to January 1, 2020, race was collected independently as part of the registration process; a
decision was made that this violated parity laws and race had to be determined using Medicaid
eligibility data that does not have race information in many records drastically increasing the
amount of unknown race records from 2020 on
● The decreases in the age group of 55 and over in 2020 are due to Medicare beginning to cover
the service starting 1/1/2020.
● Mental health outpatient services are covered by Medicare, so any Medicare recipients will not
be represented in mental health outpatient counts.
● PBHS sections of last year’s report may not align with the 2022 report.
○ On January 1, 2000, a new provider, Optum, took over the duties of the Administrative
Services Organization that included the adjudication and payment of claims.
○ A change in the reported number of people treated across multiple years took place due
to retractions of claims previously approved, wrongfully rejected claims, and
inconsistencies throughout the claims process.
○ PBHS sections of last year’s report were based on claims data that had not been cleaned
and reprocessed, and because of the effects of the pandemic, some reductions in the
numbers of people treated will appear in the current report.

MARYLAND DEPARTMENT OF HEALTH
72 | Page
Acronyms
Area of Responsibility (AOR)
Behavioral Health Administration (BHA)
Center for Harm Reduction Services (CHRS)
Center for Substance Abuse Research (CESAR)
Center for Population Health Information Technology (CPHIT)
Chesapeake Region Information System for our Patients (CRISP)
Data-Informed OD Risk Mitigation (DORM)
Direct Analysis in Real Time Mass Spectrometry (DART-MS)
Department of Public Safety and Correctional Services (DPSCS)
Emergency Department (ED)
Electronic Health Record (EHR)
Emergency Medical Services (EMS)
Food and Drug Administration (FDA)
Fee for Service (FFS)
Health Services Cost Review Commission (HSCRC)
House Bill (HB)
International Classification of Disease (ICD)
Johns Hopkins University Bloomberg School of Public Health (JHSPH)
Maryland Emergency Department Drug Surveillance (MD-EDDS)
Maryland Department of Health (MDH)
Maryland Total Human Services Integrated Network (MD THINK)
Maryland Institute for Emergency Medical Services Systems (MIEMSS)
Medication for Opioid Use Disorder (MOUD)
National Institute of Standards and Technology (NIST)
Non-fatal Overdose (NFOD)
Opioid Operational Command Center (OOCC)
Opioid Use Disorder (OUD)
OD (OD)
Overdose Death Record (ODR)
Overdose Response Program (ORP)
Public Behavioral Health System (PBHS)
Prescription Drug Monitoring Program (PDMP)
Rapid Analysis of Drugs (RAD)
Statewide Targeted Overdose Prevention (STOP)
Statewide Unintentional Drug Overdose Reporting System (SUDORS)
Substance Use (SU)
Substance Use Disorder (SUD)
Syringe Service Programs (SSPs)
University of Maryland Medical Center (UMMC)
University of Maryland St. Joseph Medical Center (UM SJMC)
University of Pittsburgh Medical Center (UPMC)
Vital Statistics Administration (VSA)
Washington/Baltimore High-Intensity Drug Trafficking Area (W/B HIDTA)

DORM 2022 ANNUAL REPORT
73 | Page
VII. DATA SOURCES & CITATIONS
MDH Vital Statistics Administration: fatal ODs in Maryland, fatal OD demographics.
Statewide Unintentional Drug OD Reporting System (SUDORS): OD fatality circumstances and
decedent characteristics.
University of Maryland, Center for Substance Use, Addiction & Health Research (CESAR):
Maryland Emergency Department Drug Surveillance (MD-EDDS) program. Hospital emergency
department electronic health records and urinalysis.
The Center for Population Health Information Technology (CPHIT) in the Department of Health
Policy & Management of the Johns Hopkins Bloomberg School of Public Health. Relative risk
factors for OD.
Analysis by the University of Maryland Systems Evaluation Center using OD Death data from the
Vital Statistics Administration and Office of the Chief Medical Examiner and claims data from BHA
and Optum.
Rhonda R. Moody, Director of Data Insights, CRISP.
The Hilltop Institute. (April 14, 2023). Medicaid Data for DORM Report. Baltimore, MD: UMBC.
Medicaid claims.
“Heroin, Fentanyl, Cocaine and Prescription Opioid Drug Trends in the State of Maryland 2020-
2022”; Washington/Baltimore HIDTA Investigative Support Center; 2023. Drug seizure sample
testing results.
Russell E, Sisco E, Thomson A, et al. Rapid Analysis of Drugs: A Pilot Surveillance System to Detect
Changes in the Illicit Drug Supply to Guide Timely Harm Reduction Responses — Eight Syringe
Services Programs, Maryland, November 2021–August 2022. MMWR Morb Mortal Wkly Rep
2023; 72:458–462. DOI: http://dx.doi.org/10.15585/mmwr.mm7217a2.
MDH Center for Harm Reduction Services: Participant date from Syringe Services Programs,
Naloxone distribution through Maryland’s Overdose Response Program (ORP).
Health Services Cost Review Commission (HSCRC): service utilization at Maryland hospitals.
Prescription Drug Monitoring Program: dispense records for controlled dangerous substances.
MDH Behavioral Health Administration: Service utilization through the Public Behavioral Health
System.

MARYLAND DEPARTMENT OF HEALTH
74 | Page
VIII. APPENDIX A: CHRS
Table 11: Naloxone Distribution and Training Saturation by Jurisdiction (2022)
Jurisdiction
Kits Distributed to At-Risk Individuals
Calculation, Calendar year 2022 Q1
Kit Distribution Target
Calculation, Calendar year
2021 Q1
Diff.: Target - Actual
(E - G)
Est. # At-Risk
People Trained
Medicaid Rx
Claims
(Pharmacy
Location)
Est. # Kits
Distributed to
At-Risk People
Opioid OD
Deaths
(Incident
Location)
Kit Distribution
Target
(20x # deaths)
# %
Allegany County
2,488 0 1,244 40 800 444 156%
Anne Arundel County
6,889 0 3,444 209 4,180 -736 82%
Baltimore City
70,898 0 35,449 1,010 20,200 15,249 175%
Baltimore County
4,144 0 2,072 360 7,200 -5,128 29%
Calvert County
684 0 342 17 340 2 101%
Caroline County
46 0 23 8 160 -137 14%
Carroll County
1,129 0 565 52 1,040 -475 54%
Cecil County
19,168 0 9,584 76 1,520 8,064 631%
Charles County
217 0 108 31 620 -512 17%
Dorchester County
2,569 0 1,285 20 400 885 321%
Frederick County
5,656 0 2,828 44 880 1,948 321%
Garrett County
927 0 464 6 120 344 386%
Harford County
6,743 0 3,372 85 1,700 1,672 198%
Howard County
1,045 0 523 32 640 -117 82%
Kent County
703 0 351 8 160 191 220%
Montgomery County
186 0 93 121 2,420 -2,327 4%
Prince George's County
16,190 0 8,095 168 3,360 4,735 241%
Queen Anne's County
228 0 114 14 280 -166 41%
Somerset County
616 0 308 9 180 128 171%
St. Mary's County
2,659 0 1,330 37 740 590 180%
Talbot County
215 0 108 12 240 -132 45%
Washington County
3,305 0 1,653 94 1,880 -227 88%
Wicomico County
1,186 0 593 40 800 -207 74%
Worcester County
1,053 0 527 16 320 207 165%
Total
148,945 0 74,472 2,509 50,180 24,292 148%

DORM 2022 ANNUAL REPORT
75 | Page
IX. APPENDIX B: PBHS
Table 12: Overdose Decedents Active in PBHS at Time of Death (2020-2021)
Jurisdiction
% of
Decedents
Engaged in
PBHS
Services
(2020)
% of
Decedents
Engaged in
PBHS Services
(2021)
Jurisdiction
% of
Decedents
Engaged in
PBHS Services
(2020)
% of
Decedents
Engaged in
PBHS Services
(2021)
Allegany
63.30% 44.12%
Harford
64.95% 51.82%
Anne Arundel
51.90% 54.18%
Howard
33.93% 43.90%
Baltimore
50.50% 57.56%
Kent
40.00% 65.50%
Baltimore City
58.20% 59.12%
Montgomery
33.58% 40.82%
Calvert
62.50% 58.06%
Prince George's
27.27% 27.17%
Caroline
65.00% 78.33%
Queen Anne's
42.11% 57.14%
Carroll
67.24% 61.90%
Somerset
28.57% 63.64%
Cecil
50.59% 48.68%
St. Mary's
44.12% 58.54%
Charles
41.38% 41.46%
Talbot
44.44% 50.00%
Dorchester
33.33% 75.00%
Washington
60.82% 63.22%
Frederick
45.59% 46.30%
Wicomico
44.19% 65.00%
Garrett
50.00% 50.00%
Worcester
56.25% 68.42%

MARYLAND DEPARTMENT OF HEALTH
76 | Page
XI. APPENDIX C: JHSPH
Non-Fatal Overdose Analysis
FOLLOW UP AFTER FIRST NON-FATAL OVERDOSE
Table 13: Overdose and Healthcare Outcomes in the Year Following “First” Non-
Fatal Overdose, 2016-2021
Total
(n= 41,558)
No buprenorphine
post-NFOD
(n=35,815)
Buprenorphine
received <= 4
weeks post NFOD
(n=2,357)
Buprenorphine
received >4
weeks post
NFOD
(n=3,386)
Likelihood
Chi-2 Ratio
Test
Subsequent
non-fatal
overdose
n % n % n % n % p-value
5490
13.2
4053
11.3%
508
21.6%
929
27.4%
<.0001
Fatal overdose 91 0.2 81 0.2% 3 0.1% 7 0.2% 0.5874
ED Visit
-
all
cause
25980 62.5 21524 60.1 1722 73.1% 2734 80.7% <.0001
Inpatient
Admission-all
cause
14059 33.8 11912 33.3 785 33.3% 1362 38.2% <.0001
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review
Commission, and Office of the Chief Medical Examiner.
Note: Rates displayed in the table are crude (unadjusted) and do not account for differences in
severity of substance use disorder or underlying comorbidities at baseline between the three
groups.

DORM 2022 ANNUAL REPORT
77 | Page
Table 14: Demographics by Buprenorphine Receipt in the Year Following Index
Non-Fatal Overdose, 2015-2017
Total
(n= 41,558)
No
buprenorphine
post-NFOD
(n=35,815)
Buprenorphine
received <= 4
weeks post NFOD
(n=2,357)
Buprenorphine
received >4 weeks
post NFOD
(n=3,386)
Likelihood
Chi-2 Ratio
Test
n
%
n
%
n
%
n
%
p
-
value
Age at time of NFOD
18-24 2683 6.5 2199 6.1 165 7.0 319 9.4 <.0001
25-34 8367 20.1 6495 18.1 720 30.5 1152 34.0
35-44 6029 14.5 4864 13.6 488 20.7 677 20.0
45-54 7611 18.3 6411 17.9 517 21.9 683 20.2
55-64 8126 19.6 7264 20.3 390 16.5 472 13.9
65+ 8742 21.1 8582 24.0 77 3.3 83 2.4
Sex
Female 18499 44.5 16486 46.0 812 34.5 1201 35.5 <.0001
Male 23054 55.5 19324 54.0 1545 65.5 2185 64.5
Missing/Unknown 5 0.0 5 0.0 5 0.2 0 0.0
Race
Black or African
American
14239 34.3 12218 34.1 837 35.5 1184 35.0 0.7278
White 25108 60.4 21561 60.2 1445 61.3 2102 62.1
Other 1822 4.3 1690 4.7 58 2.5 64 1.9
Missing/Unknown 389 0.9 346 1.0 17 0.7 26 0.8
Ethnicity
Hispanic or Latino 1020 2.5 946 2.6 34 1.4 40 1.2 0.9757
Not Hispanic or
Latino
39372 94.7 33857 94.5 2257 95.8 3258 96.2
Missing/Unknown 1166 2.8 1012 2.8 66 2.8 88 2.6
Payer
<.0001
Medicaid 17417 41.9 13420 37.5 1685 71.5 2312 68.3
Medicare 11657 28.0 11112 31.0 230 9.8 315 9.3
Commercial 7509 18.1 6767 18.9 289 12.3 453 13.4
Self-pay/Cash 3676 8.8 3310 9.2 116 4.9 250 7.4
Other/Unknown 1278 3.1 1206 3.4 37 1.6 56 1.7
Region
Capital 5679 13.7 5233 14.6 173 7.3 273 8.1 <.0001
Central 24642 59.3 20851 58.2 1587 67.3 2204 65.1
Eastern shore 3395 8.2 2846 7.9 219 9.3 330 9.7
Southern 1718 4.1 1419 4.0 128 5.4 171 5.1
Western 2262 5.4 1869 5.2 157 6.7 236 7.0
Other/Unknown 3826 9.2 3597 10.0 93.0 3.9 172 5.1

MARYLAND DEPARTMENT OF HEALTH
78 | Page
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review
Commission, and Office of the Chief Medical Examiner.
Note: Regions were specified as follows: 1) Capital: Frederick, Montgomery, Prince George’s; 2)
Central: Anne Arundel, Baltimore City, Baltimore County, Carroll, Harford, Howard; 3) Eastern
Shore: Caroline, Cecil, Dorchester Kent, Queen Anne’s, Somerset, Talbot, Wicomico, Worcester; 4)
Southern: Calvert, Charles, St. Mary’s; 5) Western: Allegany, Garrett, Washington.

DORM 2022 ANNUAL REPORT
79 | Page
Table 15: Overdose and Healthcare Outcomes in the Year Following “First” Non-
Fatal Overdose by Race, 2016-2021
Total
(n= 41,558)
Black
(n=14,239)
White
(n=25,108)
Other/Missing
(n=2,211)
Likelihood
Chi-2 Ratio
Test
n
%
n
%
n
%
n
%
p
-
value
Buprenorphin
e received <= 4
weeks post
NFOD
2357 5.7 837 5.9 1445 5.8 75 3.4
0.2347
Buprenorphin
e received >4
weeks post
NFOD
3386 8.1 1184 8.3 2102 8.4 100 4.5
Subsequent
non-fatal
overdose
5490 13.2 2149 15.1 3129 12.5 212 9.6 <.0001
Fatal overdose 91 0.2 34 0.2 51 0.2 6 0.3 0.291
ED
Visit
-
all
cause
25980 62.5 9861 69.3 14988 59.7 1131 51.2 <.0001
Inpatient
Admission-all
cause
14059 33.8 5173 36.3 8255 32.9 631 28.5 <.0001
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review Commission, and
Office of the Chief Medical Examiner.
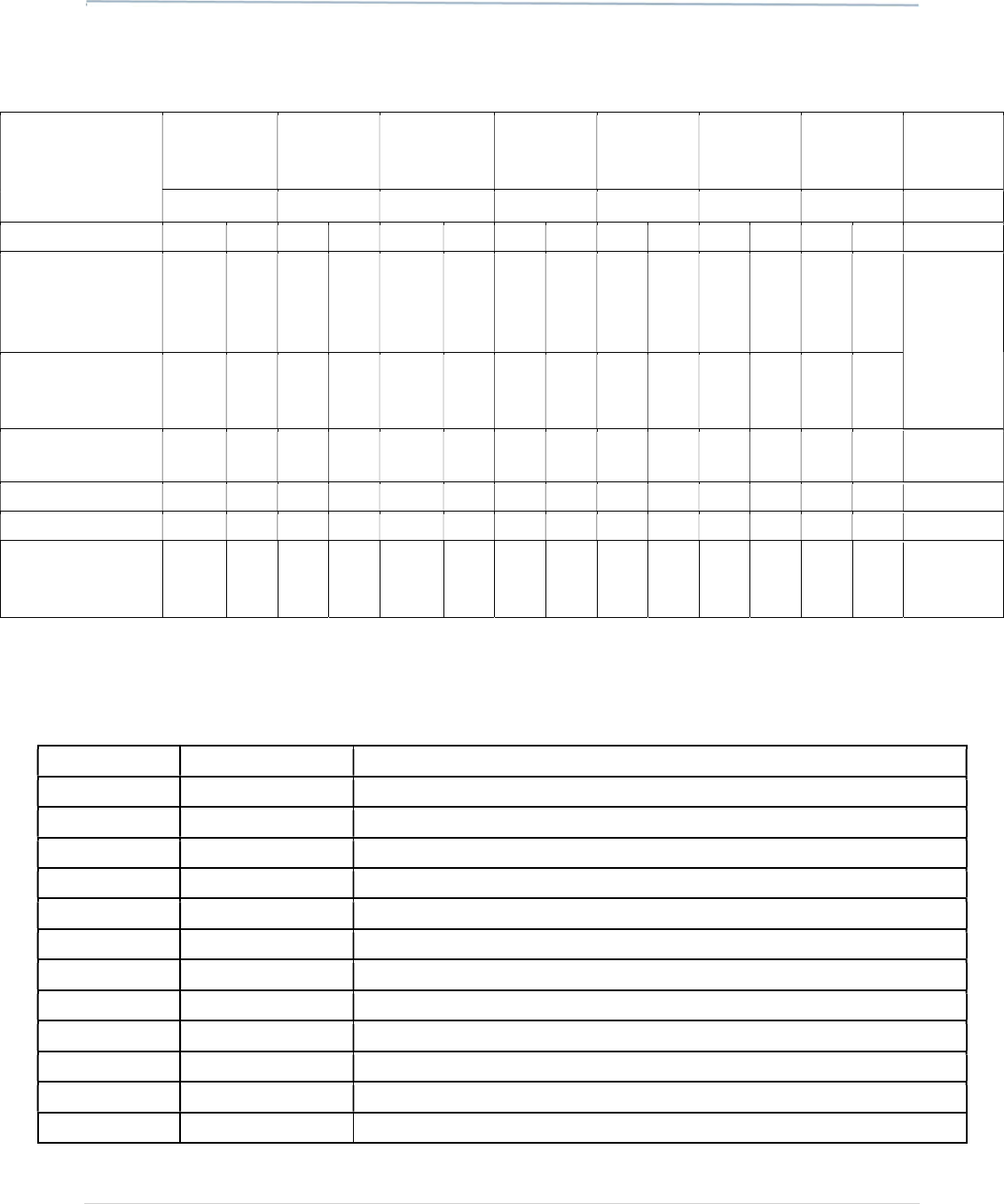
MARYLAND DEPARTMENT OF HEALTH
80 | Page
Table 16: Overdose and Healthcare Outcomes in the Year Following “First” Non-
Fatal Overdose by Region of Residence, 2016-2021
Total Capital Central
Eastern
Shore
Southern Western
Out of
State/
Unknown
Likelihood
Chi-2 Ratio
Test
(n= 41,558) (n=5,679) (n=24,642) (n=3,395) (n=1,718) (n=2,262) (n=3,862)
n
%
n
%
n
%
n
%
n
%
n
%
n
%
p
-
value
Buprenorphine
received <= 4
weeks post
NFOD
2357 5.7 173 3.0 1587 6.4 219 6.5 128 7.5 157 6.9 93 2.4
0.2347
Buprenorphine
received >4 weeks
post NFOD
3386 8.1 273 4.8 2204 8.9 330 9.7 171 10.0
236 10.4
172 4.5
Subsequent non
-
fatal overdose
5490 13.2
548 9.6 3637 14.8
463 13.6
197 11.5
277 12.2
368 9.5 <.0001
Fatal
overdose
91
0.2
12
0.2
54
0.2
5
0.1
2
0.1
8
0.4
10
0.3
0.5837
ED Visit
-
all cause
25980
62.5
3345
58.9
16385
66.5
2202
64.9
1122
65.3
1433
63.4
1493
38.7
<.0001
Inpatient
Admission - all
cause
14059
33.8
1996
35.1
9146 37.1
929 27.4
502 29.2
710 31.4
776 20.1
<.0001
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review
Commission, and Office of the Chief Medical Examiner.
Table 17: Overdose Diagnosis Codes
Code Number
Code source
Descriptor
96500
ICD
-
9
Poisoning by opium (alkaloids), unspecified
96501
ICD
-
9
Poisoning by heroin
96502
ICD
-
9
Poisoning by methadone
96509
ICD
-
9
Poisoning by other opiates and related narcotics
E8500
ICD
-
9
Accidental poisoning by heroin
E8501
ICD
-
9
Accidental poisoning by methadone
E8502
ICD
-
9
Accidental poisoning by other opiates and related narcotics
T400*
ICD
-
10
Poisoning by adverse effect of and underdosing of opium
T401*
ICD
-
10
Poisoning by and adverse effect of heroin
T402*
ICD
-
10
Poisoning by adverse effect of and underdosing of other opioids
T403*
ICD
-
10
Poisoning by adverse effect of and underdosing of methadone
T404
ICD
-
10
Poisoning
by
adverse effect of and underdosing of other synthetic narcotics

DORM 2022 ANNUAL REPORT
81 | Page
Source: Linked data from the state prescription drug monitoring program, Health Services Cost Review
Commission, and Office of the Chief Medical Examiner.
MIEMSS
Table 18: Descriptive Characteristics for MIEMSS-Recorded Opiate-Related
Overdose Incidents, for Years 2021 and 2022, Cross-Tabulated with Transport
Status. All Percentages Reflect Totals for Transport Status Group, for Each Year
2021
2022
Transported
Not
Transported
Deceased Transported
Not
Transported
Deceased
TOTAL
INCIDENTS
13563 (100%) 4870 (100%) 276 (100%)
11240 (100%) 3897 (100%) 248 (100%)
% of Total
Incidents
72.5% of
18,709
26.0% of
18,709
.01% of
18,709
73.1% of
15,385
25.3 % of
15,385
.01% of
15,385
Mean age (sd) 46.19 (15.16) 43.26 (13.98)
45.72
(13.74)
46.11 (15.44) 43.77 (13.87)
45.05
(14.38)
< 18
124 (0.91%)
11 (0.23%)
-
172 (1.53%)
16 (0.41%)
-
18
–
25
894 (6.59%)
298 (6.12%)
-
716 (6.37%)
204 (5.23%)
-
26 – 35
2874
(21.19%)
1345
(27.62%)
58
(21.01%)
2357
(20.97%)
1036
(26.58%)
54
(21.77%)
36 – 45
2470
(18.21%)
925 (18.99%)
64
(23.19%)
2096
(18.65%)
805 (20.66%)
57
(22.98%)
46 – 55
2556
(18.85%)
837 (17.19%)
56
(20.29%)
1908
(16.98%)
627 (16.09%)
41
(16.53%)
56 – 65
2925
(21.57%)
800 (16.43%)
48
(17.39%)
2452
(21.81%)
708 (18.17%)
46
(18.55%)
> 65 1214 (8.95%) 288 (5.91%) 25 (9.06%)
1181
(10.51%)
226 (5.8%) 19 (7.66%)
Missing Age
506 (3.73%)
366 (7.52%)
13 (4.71%)
358 (3.19%)
275 (7.06%)
15
(6.05%)
SEX
Female
4146
(30.57%)
1359
(27.91%)
-
3726
(33.15%)
1184
(30.38%)
-
Male
9170
(67.61%)
3438 (70.6%)
192
(69.57%)
7278
(64.75%)
2645
(67.87%)
156
(62.9%)
Missing Sex
247 (1.82%)
73 (1.5%)
-
236 (2.1%)
68 (1.74%)
-
RACE
Black
5513
(40.65%)
1669
(34.27%)
82
(29.71%)
4225
(37.59%)
1214
(31.15%)
97
(39.11%)
White
4539
(33.47%)
1797 (36.9%)
175
(63.41%)
3683
(32.77%)
1396
(35.82%)
135
(54.44%)
Other Race
367 (2.71%)
110 (2.26%)
-
359 (3.19%)
88 (2.26%)
-
Missing Race
3098
(22.84%)
1280
(26.28%)
-
2924
(26.01%)
1187
(30.46%)
-

MARYLAND DEPARTMENT OF HEALTH
82 | Page
2021
2022
Transported
Not
Transported
Deceased Transported
Not
Transported
Deceased
INCIDENT
REGION
Capital
1545
(11.39%)
535 (10.99%)
33
(11.96%)
1456
(12.95%)
541 (13.88%) 24 (9.68%)
Central
9924
(73.17%)
3545
(72.79%)
154
(55.8%)
7865
(69.97%)
2650 (68%)
147
(59.27%)
Eastern Shore 573 (4.22%) 271 (5.56%)
37
(13.41%)
542 (4.82%) 236 (6.06%) 31 (12.5%)
Southern
439 (3.24%)
147 (3.02%)
25 (9.06%)
386 (3.43%)
117
(3%)
21 (8.47%)
Western
943 (6.95%)
322 (6.61%)
-
831 (7.39%)
284 (7.29%)
-
Missing/Non
-
MD Region
139 (1.02%) 50 (1.03%) - 160 (1.42%) 69 (1.77%) -
Source: Maryland Institute for Emergency Medical Services Systems.
Notes: Columns are defined by grouping the eDisposition12 code into transported (4212023,
4212033, 4212035, 4212037), not transported (4212007, 4212009, 4212011, 4212021, 4212025,
4212027, 4212029, 4212031), deceased at the scene (4212013, 4212015, 4212017, 4212019), or
other disposition (4212001, 4212003, 4212005, 4212039, 4212041, 4212043). There were no
incidents associated with the “other” disposition in our sample, so a column is not shown for this
category.
Definitions
1. Incidents: Incidents are defined using the IncidentKey variable in MIEMSS. The same patient may
have multiple incidents during the sample period, but each IncidentKey is associated with exactly
one individual. Multiple patients at the same scene would thus be associated with multiple
incidents under this definition.
2. Opioid-Related Overdose Definition: The working definitions of the CSTE and MDH workgroups
have been adapted for identifying opioid-related overdoses to this current deployment of
MIEMSS records. This definition builds from four criteria: (1) “Overdose Incident”: the
PrimaryImpression or SecondaryImpression reflects some term/phrase related to being an
‘overdose,’ and eDispatch01 is coded for ‘Overdose/Poisoning/Ingestion’, (2) “Opioid-Specific”:
the eNarrative01 free text field includes specific language for opioids or two or more terms
consistent with symptoms of opioid overdose (e.g., miosis, respiratory depression, loss of
consciousness, etc.), (3) “Naloxone Administered”: MedicationsAdministered or eNarrative01
include ‘Naloxone,’ and (4) “Patient Improvement with Naloxone”: ResponseToMeds is
‘Improved’ with the administration of ‘Naloxone.’ Opioid-related overdoses are then identified
using the four combination rules shown in the rows of the table below. An incident that meets
any of these four rules is considered an opioid-related overdose in this report.
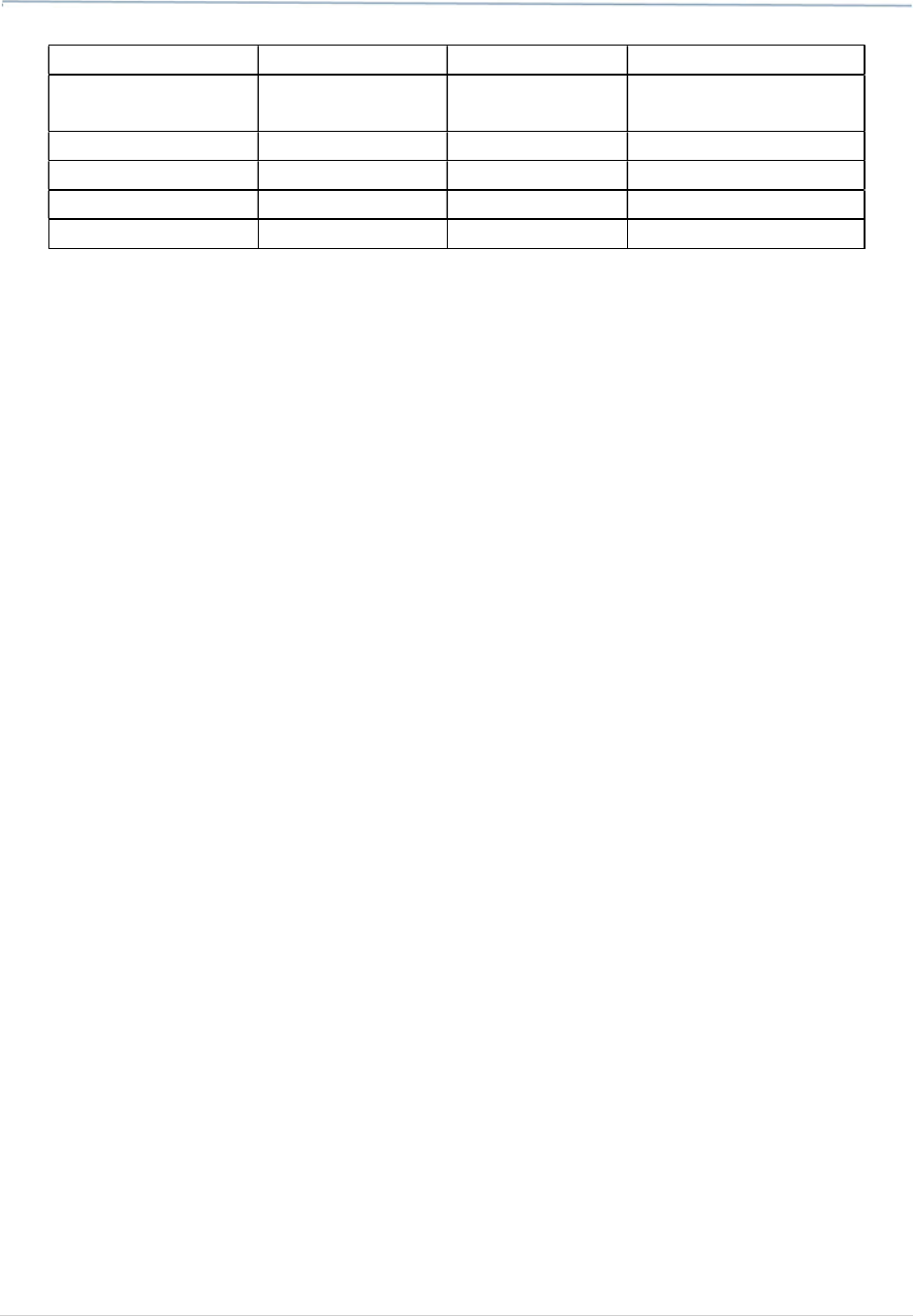
DORM 2022 ANNUAL REPORT
83 | Page
Criterion 1
Criterion 2
Criterion 3
Criterion 4
Overdose Incident Opioid Specific
Naloxone
Administered
Patient Improvement
w/ Naloxone
X
X
X
X
X
X
X
3. Transport Status: We grouped eDisposition12 codes according to whether the patient was
transported (4212023, 4212033, 4212035, 4212037), not transported (4212007, 4212009,
4212011, 4212021, 4212025, 4212027, 421209, 4212031), deceased at the scene (4212013,
4212015, 4212017, 4212109). All other values of eDisposition12 (4212001, 4212003, 4212005,
4212039, 4212041, 4212043) were not observed in our sample, so these groups cover the full
sample of opioid-related overdoses. Patients who were transported included those transported
by the responding EMS unit (over 99 percent of transported cases) and those transported by law
enforcement or other vehicles. Patients who were not transported included patients who were
evaluated and did not need transport, patients who were treated at the scene and released per
protocol, patients who were treated at the scene and then refused transport, and patients who
refused evaluation/care at the scene and also refused transport.
4. Patient Demographics. Patient race is contained in the ePatient14 field. We group these
responses into Black, White, and Other Race (which includes patients whose race was listed as
American Indian or Alaska Native, Hispanic or Latino, and Native Hawaiian or Other Pacific
Islander). There is no separate field for ethnicity in the MIEMSS data. Patient demographics were
evaluated at the patient level by considering demographics to be static and aggregating non-
missing observations per PatientID across all incidents. These patient-level demographics were
then assigned to every incident belonging to a particular PatientID. In cases where there was
disagreement across incidents for the same patient on a particular demographic variable, this
variable was assigned to missing. Of the incidents involving opioid overdose, 11,719 (34.4 percent)
were missing race. This was improved by patient-level imputation to 8,501 (24.9 percent) still
missing race. Only 15 (0.0 percent) incidents were explicitly missing documentation of sex initially
and this rose to 629 (1.8 percent) after the patient-level imputation process, because some
PatientIDs were associated with more than one value for sex. Patient age was calculated at the
incident level using recorded date of birth.
5. Incident Jurisdiction. Incident jurisdiction was used to determine the region an incident took
place in. This value is distinct from both the home jurisdiction of the patient, and the transport
destination jurisdiction.

MARYLAND DEPARTMENT OF HEALTH
84 | Page
XII. APPENDIX D: HSCRC
Table 19: ICD-10 Codes Used to Define Hospital-Based Predictors
Predictors Diagnosis Codes
Any non-fatal overdose
Includes all codes for non-fatal overdose defined by substance type below
Non-fatal heroin overdose
ICD10: T401
Non-fatal methadone overdose
ICD10: T403*
Non-fatal other opioid overdose
(includes prescription opioids,
opium, or synthetic opioids)
ICD10: T400*, T402*, T404, T40601*, T40604*, T40691*, T40694*
Non-fatal alcohol overdose
ICD10: T510X1*, T510X4*, T511X1*, T511X4*, T512X1*, T512X4*, T513X1*,
T513X4*, T518X1*, T518X4*, T520X1*, T520X4*,
T521X1*, T521X4*, T5191*,
T5194*
Non-fatal benzodiazepine
overdose
ICD10: T424*
Non-fatal cocaine overdose
ICD10: T405*
Non-fatal other drug overdose
(includes amphetamine,
barbiturates, non-opioid
analgesics, other drug poisoning)
ICD10:
T390*
-
T394*, T398*, T399*, T423*, T4362*, T407X1*, T407X4*,
T408X1*, T408X4*, T40901*, T40904*, T40991*, T40994*, T410X1*, T410X4*,
T411X1*, T411X4*, T41201*, T41204*, T41291*, T41294*, T413X1*, T413X4*,
T423X1*, T423X4*, T426X1*, T426X4*, T428X1*, T428X4*
, T43011*, T43014*,
T43021*, T43024*, T431X1*, T431X4*, T43201*, T43204*, T43211*, T43214*,
T43221*, T43224*, T43291*, T43294*, T433X1*, *T433X4*, T434X1*,
T434X4*, T43501*, T43504*, T43591*, T43594*, T43601*, T43604*, T43611*,
T43614*, T43621*, T43624*, T
43631*, T43634*,T43691* ,T43694*, T438X1*,
T438X4*, T481X1*, T481X4*, T483X1*, T483X4*, T507X1*, T507X4*, T508X1*,
T508X4*, T50901*, T50904*, T50991*, T50994*, T4141*, T4144*, T4271*,
T4274*, T4391*, T4394*
Opioid use disorder (OUD)
ICD10: F11*
Other Substance Use Disorder
(SUD)
ICD10: F10*, F12*-F16*, F18*F19*
Non-poisoning injury diagnosis
ICD10: S00-S99, T07-T34, T66-T76, T79

DORM 2022 ANNUAL REPORT
85 | Page
Chronic pain diagnosis
ICD10: G892, G8921, G8922, G8928, G8929, G894
Mental health diagnosis
ICD10: F20-F25, F28-F34, F39-F48, F60, F68, F69
Injection drug use-related wounds
ICD10:
[Endocarditis] B376, I330, I39, I339, I340, I348, I350, I351, I352, I358, I359,
I360, I368, I370, I378, I38, I39, I38;
[Bacteremia or Sepsis] A409, A412, A4101, A4102, A411, A403, A4
14, A4150,
A413, A4151, A4152, A4153, A4159, A4189, A419, I2690, I400, I76, R6521,
R7881, R6510, A419, R6520, M8610,M8620, M86119, M86219, M86129,
M86229, M86139, M86239, M86149, M86249, M86159, M86259, M86169,
M86269, M86179, M86279, M8618, M8628, M8619,
M8629, M8660,
M86619, M86629, M86639, M86641, M86642, M86659, M86669, M86679,
M8668, M8669, M869, M4630;
[Wound botulism] A480, A4852, I96;
[Necrotizing fasciitis] M726;
[Cellulitis] L03019, L03029, L03019, L03039, L03049, L03029, L03039, K122,
L03211, L03212, L03221, L03222, L03319, L03329, L03119, L03129, L03317,
L03811, L03818, L03891, L03898, L0390, L0391, L03116, L03115, L03114,
L03113;
[Skin and soft tissue infections] G060,G061, G062, G09, K651, K6812, K6819,
K630, K750, N10, L942, L988, M5402, M793, M793;
[Open wounds] S41009A, S41109A, S51809A, S51009A, S61509A, S61409A,
S61429A, S66929A, S61209A, S61229A, S61109A, S66529A, S71009A,
S71109A, S76929A, S81109A, S81809A, S91009A, S91309A, S91329A,
S96929A, S91109A;
[Ulcers] L8990, L89009, L8
9209, L89309, L89509, L89819, L89899, L97909,
L97109, L97209, L97309, L97509, L97809, L98419, L98429, L98499

MARYLAND DEPARTMENT OF HEALTH
86 | Page
Table 20: Inpatient and Emergency Department Health Services Utilization
Among MD Resident Drug Intoxication Decedents Aged 15-90 During Calendar
Year of Death, 2016-2021
2016 2017 2018 2019 2020 2021
Total deaths (N)
1,848 2,008 2,241 2,235 2,629 2,632
N % N % N % N % N % N %
Any service utilization
966
52.3 1004 50.0
1047 46.7 969 43.4 1091 41.5 1133 43.0
Any overdose-related
services
336
34.8 339 33.8
347 33.1 316 32.6 342 31.3 326 28.8
Opioid Use Disorder
354
36.6 358 35.7
364 34.8 357 36.8 359 32.9 379 33.5
Substance Use Disorder (non-
opioid)
461
47.7 469 46.7
477 45.6 442 45.6 496 45.5 515 45.5
Non-poisoning Injury
268
27.7 265 26.4
299 28.6 308 31.8 311 28.5 326 28.8
Chronic Pain Diagnosis
161
16.7 140 13.9
164 15.7 143 14.8 162 14.8 163 14.4
Mental Health Diagnosis
382
39.5 407 40.5
438 41.8 405 41.8 447 41.0 422 37.2
Injection drug use-related
wounds
147
15.2 147 14.6
160 15.3 144 14.9 163 14.9 210 18.5

DORM 2022 ANNUAL REPORT
87 | Page
XIV. APPENDIX E: EDDS
Table 21: Substances Tested in Urine Screens
Substance Category
Substance Name
Benzodiazepines
Benzodiazepines
Opioids
Fentanyl
Methadone
Opiates
Oxycodone
Other Drugs
Barbiturates
Phencyclidine (PCP)
Phencyclidine (PCP)
Stimulants
Amphetamines
Cocaine
Tetrahydrocannabinol (THC)
Tetrahydrocannabinol (THC)

MARYLAND DEPARTMENT OF HEALTH
88 | Page
XV. APPENDIX F: MEDICAID (PROVIDED BY HILLTOP)
Table 22: Number and Percentage of Fatal Overdoses Who Were Medicaid
Participants in Maryland, CY 2017 - CY 2021*
Calendar Year
Any Medicaid Eligibility
within 12 Months Prior to
Month of Death
Medicaid Eligibility at Time
of Death
Total
Overdose
Deaths*
Number Percent Number Percent
CY 2017
1,413 65.0% 1,329 61.2% 2,173
CY 2018
1,548 74.6% 1,431 69.0% 2,074
CY 2019
1,513 68.3% 1,408 63.6% 2,214
CY 2020
1,834 70.4% 1,753 67.3% 2,605
CY 2021
1,795 68.8% 1,781 68.2% 2,610
Source: The Hilltop Institute, Maryland Medicaid Administration, Maryland Vital Statistics Administration and Maryland’s
Medicaid Management Information System (MMIS2).
*Total includes only viable records.
