
D A H o m e a n d C o m m u n i t y - B a s e d S e r v i c e s W a i v e r P r o g r a m
I N D I A N A H E A L T H C O V E R A G E P R O G R A M S
Division of Aging
Home and
Community-Based
Services Waiver Provider
Manual
L I B R A R Y R E F E R E N C E N U M B E R : P R P R 1 0 0 1 3
P U B L I S H E D : J U L Y 1 6 , 2 0 1 5
P O L I C I E S A N D P R O C E D U R E S A S O F M A Y 1 , 2 0 1 5
V E R S I O N 3 . 0
ARCHIVED
ARCHIVED

Library Reference Number: PRPR10013
Document Management System Reference: DA HCBS Waiver Provider Manual
Address any comments concerning the contents of this manual to:
HP Provider Relations Unit
950 North Meridian Street, Suite 1150
Indianapolis, IN 46204
© 2015 Hewlett-Packard Development Company, L.P.
Products and brand names are the trademarks of their respective owners.
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 iii
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Revision History
Version
Date
Reason for Revision
Completed by
1.0
Policies and Procedures as of
January 1, 2013
Published: June 10, 2013
Initial Release
FSSA
1.1
Policies and Procedures as of
November 1, 2013
Published December 19, 2013
Semi-annual review
FSSA and HP
Waiver Analyst
2.0
Policies and Procedures as of
May 1, 2014
Published August 5, 2014
Semi-annual review
FSSA and HP
Waiver Analyst
2.1
Policies and Procedures as of
November 1, 2014
Published January 8, 2015
Semi-annual review
FSSA and HP
Waiver Analyst
3.0
Policies and Procedures as of
May 1, 2015
Published July 16, 2015
Semi-annual review
FSSA and HP
Waiver Analyst
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 v
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Table of Contents
Table of Contents ....................................................................................................... v
Section 1: Introduction ...................................................................................... 1-1
Overview ............................................................................................................. 1-1
Indiana Health Coverage Programs Waiver Provider Responsibilities ............... 1-1
Provider Responsibilities Specific to the Waiver Program .................................. 1-2
Waiver Provider Application and Certification ................................................... 1-2
Waiver Provider Enrollment ................................................................................ 1-3
Helpful Tips for Completing the IHCP Enrollment Application ......................... 1-4
Waiver Provider Information Updates................................................................. 1-4
Section 2: Claims and Billing ............................................................................. 2-1
Overview ............................................................................................................. 2-1
Eligibility for HCBS Waiver Services Affects Billing ........................................ 2-1
Waiver Authorization .......................................................................................... 2-1
Billing Instructions .............................................................................................. 2-1
Claim Tips and Reminders .................................................................................. 2-2
Claim Voids and Replacements ........................................................................... 2-2
Division of Aging HCBS Waiver Rates .............................................................. 2-3
Section 3: Quality Assurance /Quality Improvement ...................................... 3-1
Quality Monitoring .............................................................................................. 3-1
Incident Reporting ............................................................................................... 3-1
Complaint Resolution .......................................................................................... 3-2
Mortality Review ................................................................................................. 3-2
Quality Reviews .................................................................................................. 3-3
QIS Process ......................................................................................................... 3-3
Section 4: Financial Oversight .......................................................................... 4-1
Waiver Audits ...................................................................................................... 4-1
FSSA Audit Oversight ......................................................................................... 4-1
Medicaid Fraud Control Audit Overview ............................................................ 4-1
Section 5: Division of Aging Waivers ................................................................ 5-1
Overview ............................................................................................................. 5-1
Level of Care (LOC) ........................................................................................... 5-1
Aged & Disabled Waiver .................................................................................... 5-1
Traumatic Brain Injury Waiver (TBI) ................................................................. 5-2
Section 6: Case Management ............................................................................. 6-1
For Aged & Disabled and Traumatic Brain Injury Waivers ................................ 6-1
Case Management Monitoring Standards ............................................................ 6-2
Section 7: Service Definitions ............................................................................ 7-1
Service Definition Overview ............................................................................... 7-1
Adult Day Services .............................................................................................. 7-1
Adult Family Care ............................................................................................... 7-4
Assisted Living .................................................................................................... 7-8
Attendant Care ................................................................................................... 7-10
Behavior Management/Behavior Program and Counseling .............................. 7-13
Case Management ............................................................................................. 7-15
Community Transition....................................................................................... 7-19
Environmental Modifications ............................................................................ 7-21
Environmental Modification Assessment .......................................................... 7-26
ARCHIVED
Table of Contents HCBS Waiver Program Provider Manual
I-vi Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Healthcare Coordination .................................................................................... 7-28
Home-Delivered Meals ..................................................................................... 7-30
Homemaker Services ......................................................................................... 7-32
Nutritional Supplements .................................................................................... 7-34
Personal Emergency Response System ............................................................. 7-36
Pest Control ....................................................................................................... 7-38
Residential-Based Habilitation .......................................................................... 7-40
Respite Services ................................................................................................ 7-42
Specialized Medical Equipment and Supplies ................................................... 7-44
Structured Day Program .................................................................................... 7-48
Structured Family Caregiving ........................................................................... 7-50
Supported Employment ..................................................................................... 7-53
Transportation ................................................................................................... 7-55
Vehicle Modifications ....................................................................................... 7-57
Section 8: Provider Help .................................................................................... 8-1
INsite Communication Instructions ..................................................................... 8-1
Helpful Websites ................................................................................................. 8-1
Helpful Contact Numbers .................................................................................... 8-1
Communications .................................................................................................. 8-3
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 1-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 1: Introduction
Overview
Section 1915(c) of the Social Security Act permits states to offer, under a waiver of statutory
requirements, an array of Home and Community-Based Services (HCBS) that an individual needs to
avoid institutionalization. These programs allow the state of Indiana’s Medicaid program to provide
services that would ordinarily be provided only in an institution to be provided in an individual’s home
or other community setting. Individuals must qualify for institutional care to be eligible for home and
community-based services. The term waiver refers to waiving of certain federal requirements that
otherwise apply to Medicaid program services. For example, home and community-based services or
“waivers” are not Medicaid entitlement programs.
The Family and Social Services Administration (FSSA) has overall responsibility for the waiver
programs; day-to-day administration and operation of individual waiver programs is delegated to
divisions within FSSA. The Division of Aging (DA) offers two waiver programs:
• The Aged & Disabled (A&D) waiver
• The Traumatic Brain Injury (TBI) waiver
This manual provides a primary reference for the A&D and TBI waiver providers. This manual
provides instruction to case managers, other service providers, State staff, family members, advocates,
and waiver participants, and is available to assist all those who administer, manage, and participate in
the A&D and TBI waiver programs. The information and direction in this manual replaces all previous
waiver manuals. Current waiver requirements can be found in the approved waiver applications and
the Aging Rule 455 IAC 2.
Individuals and their families may find additional information courtesy of the Indiana Governor’s
Council for People with Disabilities at in.gov/gpcpd.
Indiana Health Coverage Programs Waiver Provider
Responsibilities
IHCP Provider Agreement
Waiver providers are enrolled in the Indiana Health Coverage Programs (IHCP) and have executed an
IHCP Provider Agreement with the FSSA. This agreement states that the provider will comply, on a
continuing basis, with all the federal and State statutes and regulations pertaining to the IHCP,
including the waiver programs’ rules and regulations. Forms are available on the Forms page at
indianamedicaid.com. By signing the agreement, the provider agrees to follow the information
provided in the IHCP Provider Manual, as amended periodically, and the Division of Aging Home and
Community-Based Services Waiver Provider Manual, as amended periodically, as well as all provider
bulletins, banners, and notices. All amendments to the IHCP Provider Manual, the Division of Aging
Home and Community-Based Services Waiver Provider Manual, and all applicable Indiana
Administrative Codes (IACs), Rules, and Regulations are binding on publication. The Division of
Aging Home and Community-Based Services Waiver Provider Manual and all publications are
available online on the Manuals page at indianamedicaid.com.
ARCHIVED

Section 1: Introduction HCBS Waiver Program Provider Manual
I-1-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Provider Record Updates
To ensure timely communication of all information, providers must notify the FSSA and its fiscal
agent when enrollment record information changes. Provider information is stored in two systems:
IndianaAIM and INsite. IndianaAIM is maintained by the fiscal agent, and INsite is maintained by the
FSSA.
IndianaAIM is the Medicaid Management Information System (MMIS). The fiscal agent is responsible
for maintaining IndianaAIM; therefore, the fiscal agent must have accurate “pay to,” “mail to,” and
service location information on file for all providers. It is the provider’s responsibility to ensure that
the information on file with the fiscal agent is correct. Providers are required to submit address and
telephone change information to the fiscal agent within 10 days of any change. If the provider is
licensed through the Indiana State Department of Health, the provider must also notify the Indiana
State Department of Health of any changes to the provider’s name, address, or telephone number.
Forms are available on the Forms page at indianamedicaid.com.
INsite is the system that stores client eligibility information along with the client’s service plans,
Notice of Actions (NOAs), level of care (LOC) information, and case notes entered by the case
managers for individual clients. INsite also has a provider database that is maintained by Division of
Aging staff and is intended to provide up-to-date information about the certification status of waiver
providers. Provider selection profiles (pick lists) are generated from INsite; therefore, it is very
important that the information listed in INsite is the most current and up-to-date information available.
Provider information changes must be made by contacting the waiver/provider analyst, Indiana Health
Coverage Programs (IHCP), at Daproviderapp@fssa.in.gov.
Provider Responsibilities Specific to the Waiver Program
Providers must understand the service definitions and parameters for each service authorized on the
NOA. All waiver providers are subject to audit and potential recoupment if the services provided are
not in agreement with the services authorized as indicated on the approved NOA. If the needs of a
waiver participant change, the provider must contact the case manager to discuss revising the service
plan.
If a service can be funded under the State Plan or Medicaid waiver, it is the provider’s responsibility to
seek State Plan prior authorization before the service is requested as a Medicaid waiver service.
Documentation of an appropriate prior authorization (PA) denial is required before the service is
approved under waiver. An appropriate PA denial must be related to the actual service and not related
to the PA process. For example, a PA denial with the reason provider did not submit required
documentation would not be considered an appropriate PA denial.
Pursuant to the signed provider agreement, providers are required to furnish at least 30 days’ written
notice before terminating waiver services to an individual. This notice must be made to the individual,
the legal representative if applicable, the individual’s case manager, and the Division of Aging.
Waiver Provider Application and Certification
Becoming a waiver provider begins with the FSSA/DA certification process and is finalized with the
IHCP provider enrollment process. The DA must certify providers of the A&D and TBI waivers.
Applicants must complete the certification process through the DA and the IHCP enrollment process
through the fiscal intermediary (HP).
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 1: Introduction
Library Reference Number: PRPR10013 1-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Effective July 14, 2014, a revised application for provider certification became available. To
eliminate duplication, the provider application has been streamlined from five pages to one. The
revised application is an interactive document that can be completed electronically.
• An information and application packet (with accompanying required documents) is available on the
DA website’s Medicaid Waivers page at in.gov/fssa/da/3476.htm.
Prospective applicants are encouraged to submit application packets via email; however, paper
applications continue to be accepted. Please submit certification applications, updates, or terminations
to the following addresses:
Email: Da[email protected]
or
Mail: ATTN: Waiver/Provider Analyst
Family and Social Services Administration
Indiana Health Coverage Programs (IHCP)
DA Home and Community-Based Services Waivers
402 West Washington Street, Room W382, MS 07
P.O. Box 7083
Indianapolis, Indiana 46207-7083
Phone: 317-232-4650
Applicants and current providers are also encouraged to contact their local Area Agency on Aging
(AAA) for questions concerning FSSA DA waiver services. A list of current AAAs is located on the
Area Agencies on Aging webpage at in.gov/fssa/da/3478.htm.
• When a completed application is received, it is date stamped and reviewed by the Waiver/Provider
Analyst and the Division of Aging staff.
• If additional information is needed, applicants may be contacted via email or telephone with a
request for additional information. A 30-day time frame is given for submission of additional
information. If the necessary documentation is not submitted in a timely manner, the application
may be returned with the request to resubmit.
• If information is sufficient and meets the requirements for specific services, the provider is certified
for those requested services.
• Preliminary information is entered into the waiver provider database and the Waiver/Provider
Analyst sends the provider a Waiver Service Certification Letter.
• The Waiver Service Certification Letter directs the provider to contact the fiscal intermediary (HP)
to complete the IHCP provider enrollment process. The applicant is instructed to attach a copy of
the DA waiver certification to the IHCP application for processing. Providers may begin providing
services when they:
Receive their HP billing number
Are activated in the waiver provider database
Receive a Notice of Action (NOA)
Waiver Provider Enrollment
After a prospective provider receives the DA Waiver Service Certification Letter, the enrollment
process with the IHCP begins. The enrollment application MUST be submitted within 90 days of
certification.
• A prospective provider may obtain an IHCP Provider Enrollment Application by downloading it
from the Provider Enrollment page at indianamedicaid.com, or by contacting 1-877-707-5750 to
request an application by mail.
ARCHIVED

Section 1: Introduction HCBS Waiver Program Provider Manual
I-1-4 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Prospective providers must complete the enrollment application form and submit the completed
application form along with the Waiver Service Certification Letter to the following address:
Provider Enrollment
P.O. Box 7263
Indianapolis, IN 46207-7263
Helpful Tips for Completing the IHCP Enrollment Application
The application form asks the provider to choose a business structure. As a waiver provider, you are
enrolled as a sole practitioner (billing provider), or a group (a group must have members linked to the
group). The members linked to the group are called rendering providers and are enrolled as rendering
providers linked to the group. Rendering providers cannot bill for services; the group bills for services,
identifying the rendering provider as the performer of the service. To be a group with members, all of
the members must be certified by the DA.
Each prospective provider must designate a “type” and “specialty.” The IHCP provider type for HCBS
waiver providers is 32 (Waiver). The specialties the provider chooses must be the ones it is certified by
the Division of Aging (DA) to provide, and DA certifies services for the following:
• 350 – Aged & Disabled Waiver (AD)
• 356 – Traumatic Brain Injury Waiver (TBI)
The enrollment application must be signed and submitted with the requested documentation, including
form W-9; electronic funds transfer (EFT) form; and a copy of the Waiver Service Certification Letter.
All enrollment forms must be directed to the Provider Enrollment address listed previously (address is
also listed on the application form) to ensure proper processing.
Enrollment documents are logged into a document tracking system and issued a document tracking
number.
Provider Enrollment has a dedicated staff member assigned to coordinate and handle all waiver
provider enrollments and updates. This staff member works closely with the DA to ensure timely and
accurate maintenance of waiver files.
The staff member reviews the enrollment packet to ensure completeness according to the Provider
Enrollment guidelines and enter the provider’s information into IndianaAIM. A provider letter is
generated and sent to the provider detailing the assigned IHCP provider billing number and enrollment
information entered into IndianaAIM. Providers are encouraged to review this letter to ensure
enrollment accuracy.
If the packet needs correcting or is missing required documentation, the HP Provider Enrollment Unit
will contact the applicant by telephone, email, fax, or mail. This contact is intended to communicate
what needs to be corrected, completed, and submitted before the IHCP can process the enrollment
transaction.
Waiver Provider Information Updates
Updates to the following information must be submitted within 10 days of the change to the
waiver/provider analyst at Dapro[email protected] or (317) 232-4650:
• Name changes
• Tax identification changes
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 1: Introduction
Library Reference Number: PRPR10013 1-5
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Additional service locations (additional service location addresses)
Requires new DA Waiver Service Certification
• Changes to counties served
• Specialty changes (all specialties must be certified by the FSSA)
Requires new DA Waiver Service Certification
• Changes in ownership (CHOW)
Requires new DA Waiver Provider Application
Requires new DA Waiver Service Certification
After update certification requirements for the provider have been met, the Division of Aging sends a
new Waiver Service Certification Letter to the provider detailing the approved services and instructing
the provider to begin the update process with HP, the IHCP fiscal agent. The HP Provider Enrollment
staff member works closely with the DA to complete and maintain provider enrollment information.
Providers are required to obtain an IHCP Provider Enrollment Update Form on the Provider
Enrollment page at indianamedicaid.com or by contacting the Provider Enrollment helpline at 1-877-
707-5750 to request the update form. Providers must complete the update form with appropriate
signature and submit the form along with the waiver certification letter to the following address:
Provider Enrollment
P.O. Box 7263
Indianapolis, IN 46207-7263
Updates for the following information must be submitted to the IHCP Provider Enrollment Unit:
• Name changes
• Tax identification changes
• Additional service locations (additional Service Location Addresses)
Requires a copy of the new DA Waiver Service Certification Letter
• Specialty changes (all specialties must be certified by the FSSA)
Requires a copy of the new DA Waiver Service Certification Letter
• Changes in ownership (CHOW)
Requires a copy of the new DA Waiver Service Certification Letter
The IHCP Provider Enrollment analyst reviews the update form and documents to ensure completeness
according to the Provider Enrollment guidelines, and updates the provider’s information in
IndianaAIM. An automated provider letter is generated, detailing the changes made to the enrollment
record. Providers are encouraged to review this letter to ensure enrollment accuracy.
All questions regarding the status of the waiver provider’s enrollment or updates can be directed to the
Provider Enrollment helpline at 1-877-707-5750.
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 2-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 2: Claims and Billing
Overview
The Family and Social Services Administration (FSSA) has overall responsibility for the waiver
programs; day-to-day administration and operation of individual waiver programs is delegated to
divisions within the FSSA.
Eligibility for HCBS Waiver Services Affects Billing
All potential waiver members must enroll in the Indiana Health Coverage Programs (IHCP). At this
time, waiver participants may not be enrolled in managed care. To be eligible for reimbursement for
waiver services, the waiver member must have an open waiver level of care status in IndianaAIM. All
service providers must verify IHCP eligibility for each member before initiating services.
The Area Agencies on Aging (AAA) are the entry points for the Aged & Disabled and Traumatic
Brain Injury waivers. Initial eligibility (level of care) is determined by the entry point agencies. Before
the level of care is recorded in IndianaAIM, the level of care and the initial service plan must be
approved and a start date established. The level of care segment with the start date is then entered into
IndianaAIM by the Division of Aging (DA).
Note: The fiscal agent cannot add or correct a waiver level of care segment in
IndianaAIM nor terminate a managed care enrollment.
Waiver Authorization
The waiver case manager is responsible for completing the service plan, which results in an approved
Notice of Action (NOA). The NOA details the services and number of units to be provided, the name
of the authorized provider, and the approved billing code with the appropriate modifiers. The case
manager transmits this information to the waiver database, INsite. INsite communicates this data to
IndianaAIM, where it is stored in the prior authorization database. Claims deny if no authorization
exists in the database or if a code other than the approved code is billed. Providers are not to render or
bill services without an approved NOA. It is the provider’s responsibility to contact the case manager
if there is any discrepancy in the services authorized or rendered and the approved NOA.
Billing Instructions
Home and Community-Based Services (HCBS) waiver claims are billed on the paper CMS-1500 claim
form or via the 837P electronic transaction. Web interChange is an interactive web application that
allows providers to access IndianaAIM through the Internet. Web interChange is fast, free, and does
not require special software. The CMS-1500 form is available on the Forms page at
indianamedicaid.com. Instructions for completing the form are located in the IHCP Provider Manual.
Providers bill services based on an approved NOA, using an appropriate procedure code and the
pricing method associated with the procedure code, such as per unit, per day, or per month. Additional
pricing information is available on the Fee Schedule at indianamedicaid.com. General guidelines
include:
• Do not bill for services before they are provided.
ARCHIVED

Section 2: Claims and Billing HCBS Waiver Program Provider Manual
I-2-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• If a unit of service equals 15 minutes, a minimum of eight minutes must be provided to bill for one
unit.
• Activities requiring less than eight minutes may be accrued to the end of that date of service.
• At the end of the day, partial units may be rounded as follows: units totaling eight or more minutes
may be rounded up and billed as one unit.
• Partial units totaling less than eight minutes may not be billed.
• Monthly units are billed at the end of the month.
• Daily units may be billed daily, weekly, or monthly.
Note: If a waiver member is temporarily in an institutional setting, a provider may
not render nor be reimbursed for waiver services during that time.
Claim Tips and Reminders
When billing Medicaid waiver claims, the provider must consider the following:
• The IHCP does not reimburse time spent by office staff billing claims.
• Providers may bill only for services authorized on an approved NOA.
• A claim should include dates of service within the same month. Do not submit a claim with dates of
service that span more than one month on the same claim.
• The units of service as billed to the IHCP must be substantiated by documentation in accordance
with the appropriate Indiana Administrative Code (IAC) regulations and the waiver documentation
standards issued by the FSSA.
• Services billed to the IHCP must meet the service definitions and parameters as published in the
aforementioned rules and standards.
• Updated information is disseminated through IHCP provider bulletins, which is available on the
Bulletins page at indianamedicaid.com and DA bulletins (sent via email and posted on the State
agency websites). Each provider is responsible for obtaining the information and implementing new
or revised policies and procedures as outlined in these notices.
See the IHCP Provider Manual for instructions about how to complete the paper CMS-1500 claim
form. In addition, the fiscal agent and the FSSA recommend submitting claims electronically.
Providers may submit claims electronically using Web interChange. For information about Web
interChange, please see indianamedicaid.com or contact Provider Assistance. Telephone numbers are
available on the IHCP Quick Reference, which is available on the Contact Us page at
indianamedicaid.com.
Claim Voids and Replacements
If a paid or denied claim must be adjusted (replaced), the initial claim is voided and a new claim takes
the place of the old claim. If the claim was paid before the adjustment was made, any money paid is
recouped by setting up an accounts receivable (A/R) for the amount of the recoupment, which is
identified on the Remittance Advice (RA).
The CMS-1500 adjustment form is available on the Forms page at indianamedicaid.com. Instructions
for completing the form are located in the IHCP Provider Manual.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 2: Claims and Billing
Library Reference Number: PRPR10013 2-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Division of Aging HCBS Waiver Rates
The following table identifies procedure codes and modifiers, the waivers for which the service is
available, and the payment methodology associated with the procedure code.
Table 2.1 – Division of Aging HCBS Waiver Rates as of 5/01/14
INsite
Code
Service
Price
Code
Mod
1
Mod
2
Mod
3
Dsc Proc
Modified
A&D 127
TB 131
Notes
ADST
Adult Day
Service
Transportation
T2003
U7
U7=WAIVER
$18.19
$17.06
Per Trip
AL1
Assist Living
Waiver/Diem
T2031
U7
U1
U7=WAIVER
U1=LEVEL1
$67.88
$66.55
Day
AL2
Assist Living
Waiver/Diem
T2031
U7
U2
U7=WAIVER
U2=LEVEL2
$74.80
$73.33
Day
AL3
Assist Living
Waiver/Diem
T2031
U7
U3
U7=WAIVER
U3=LEVEL3
$82.55
$80.93
Day
ATTC
Attendant Care
Services
(Agency)
S5125
U7
UA
U7=WAIVER
UA=PROVIDE
R (AGENCY)
$4.79
$3.99
.25 Hour
ATTC
Attendant Care
Services
(Consumer
Directed)
S5125
U7
U1
U7=WAIVER
U1=ATTC FI
$2.75
N/A
.25 Hour
ATTC
Attendant Care
Services
(Nonagency)
S5125
U7
U7=WAIVER
$2.91
$2.44
.25 Hour
BMN1
Behavioral
Health Counsel
H0004
U7
U1
U7=WAIVER
U1=LEVEL 1
N/A
$17.38
.25 Hour
BMAN
Behavioral
Health Counsel
H0004
U7
U2
U7=WAIVER
U2=LEVEL 2
N/A
$17.38
.25 Hour
CMFR
Case
Management
T2022
U7
U7=WAIVER
$100.00
$100.00
Monthly Rate
HCC1
Case
Management,
Per
Mnth (Health
Care
Coordination)
T2022
U7
U3
U7=WAIVER
U3=LEVEL3
N/A
$144.18
Monthly Rate
HCC1
Case
Management,
Per
Mnth (Health
Care
Coordination)
T2022
U7
U4
U7=WAIVER
U4=LEVEL4
N/A
$192.24
Monthly Rate
HCC1
Case
Management,
Per Mnth
(Health Care
Coordination)
T2022
U7
U1
U7=WAIVER
U1=LEVEL1
Health Care
Coordination
N/A
$48.06
Monthly Rate
HCC1
Case
Management,
Per Mnth
(Health Care
Coordination)
T2022
U7
U2
U7=WAIVER
U2=LEVEL2
Health Care
Coordination
N/A
$96.12
Monthly Rate
ARCHIVED

Section 2: Claims and Billing HCBS Waiver Program Provider Manual
I-2-4 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
INsite
Code
Service
Price
Code
Mod
1
Mod
2
Mod
3
Dsc Proc
Modified
A&D 127
TB 131
Notes
HCC1
Case
Management,
Per Mnth
(Health Care
Coordination)
T2022
U7
U1
U7=WAIVER
Health Care
Coordination
$ 9.74
N/A
.25 Hour rate,
max 8 Hrs –
New for
SFY2009
CT
Comm Trans
Waiver/Service
T2038
U7
U7=WAIVER
$1,500.00
$1,500.00
Lifetime Cap
AS14
Day Care
Services, Adult
S5100
U7
U1
U7=WAIVER
U1=LEVEL1
N/A
$1.38
.25 Hour
AS24
Day Care
Services, Adult
S5100
U7
U2
U7=WAIVER
U2=LEVEL2
N/A
$1.80
.25 Hour
AS34
Day Care
Services, Adult
S5100
U7
U3
U7=WAIVER
U3=LEVEL3
N/A
$2.14
.25 Hour
ADS1
Day Care
Services, Adult
S5101
U7
U1
U7=WAIVER
U1=LEVEL1
N/A
$21.95
1/2 Day Unit
ADS2
Day Care
Services, Adult
S5101
U7
U2
U7=WAIVER
U2=LEVEL2
N/A
$28.80
1/2 Day Unit
ADS3
Day Care
Services, Adult
S5101
U7
U3
U7=WAIVER
U3=LEVEL3
N/A
$34.29
1/2 Day Unit
AD1
Day Care
Services, Adult
S5100
U7
U1
U7=WAIVER
U1=LEVEL1
$3.06
N/A
.25 Hour
AD2
Day Care
Services, Adult
S5100
U7
U2
U7=WAIVER
U2=LEVEL2
$3.06
N/A
.25 Hour
AD3
Day Care
Services, Adult
S5100
U7
U3
U7=WAIVER
U3=LEVEL3
$3.06
N/A
.25 Hour
PRSI
Emergency
Response
S5160
U7
U7=WAIVER
$54.41
$52.07
Install
PRSM
Emergency
Response
S5161
U7
U7=WAIVER
$54.41
$52.07
Monthly Rate
AF1
Family Care,
Adult;
S5141
U7
U1
U7=WAIVER
U1=LEVEL1
$58.63
$57.48
Day
AF2
Family Care,
Adult
S5141
U7
U2
U7=WAIVER
U2=LEVEL2
$69.29
$67.93
Day
AF3
Family Care,
Adult
S5141
U7
U3
U7=WAIVER
U3=LEVEL3
$79.95
$78.38
Day
HDM
Home Delivered
Meals, Inc
S5170
U7
U7=WAIVER
$5.43
$5.32
Per Meal
SPEC
EXAM
Home
Modification
Assessment –
Spec
T1028
U7
U7=WAIVER
$500.00
N/A
Annual Cap
$300.00 Spec
$200.00 Exam
HOMI
Home
Modification
Install
S5165
U7
NU
U7=WAIVER
NU=NEW
DME
$15,000.00
$15,000.00
Life Cap
HOMM
Home
Modification
Maintenance
S5165
U7
U8
U7=WAIVER
U8=REPLACE
MENT AND
REPAIR
$500.00
$500.00
Annual Cap
HMK
Homemaker
Service, NOS
S5130
U7
UA
U7=WAIVER
UA=PROVIDE
R
$3.78
$3.15
.25 Hour
HMK
Homemaker
Service, NOS
(Nonagency)
S5130
U7
U7=WAIVER
$2.75
$2.29
.25 Hour
NUTS
Nutritional
Supplement
B4150
U7
U7=WAIVER
(Annual Cap)
$1,200.00
$1,200.00
Annual Cap
RBHA
Residential
Based
Habilitation
97535
U7
U7=WAIVER
N/A
$6.99
.25 Hour
RNUR
Respite Care
Services
T1005
U7
UA
TD
U7=WAIVER
UA=PROVIDE
R; TD=RN
$9.93
$7.79
.25 Hour
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 2: Claims and Billing
Library Reference Number: PRPR10013 2-5
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
INsite
Code
Service
Price
Code
Mod
1
Mod
2
Mod
3
Dsc Proc
Modified
A&D 127
TB 131
Notes
RNUR
Respite Care
Services
T1005
U7
UA
TE
U7=WAIVER
UA=PROVIDE
R, TE=LPN
$6.83
$5.91
.25 Hour
ATCH
Specialized
Medical Equip
T2029
U7
NU
U7=WAIVER
NU=NEW
DME
$50,000.00
$50,000.00
No Cap, $50k
is Manual
Review
ATCM
Specialized
Medical Equip
T2029
U7
U8
U7=WAIVER
U8=REPLACE
MENT AND
REPAIR
$500.00
$500.00
Annual Cap
HDG
Structured Day
Program-Group
T2021
U7
HQ
U7=WAIVER
HQ=GROUP
SETTING
N/A
$1.67
.25 Hour
HDI
Structured Day
Program-
Individual
T2021
U7
U7=WAIVER
N/A
$8.38
.25 Hour
SFC1
Structured
Family Care,
Level 1
S5140
U7
U1
U7=WAIVER
U1= LEVEL 1
$58.63
N/A
Day
SFC2
Structured
Family Care,
Level 2
S5140
U7
U2
U7=WAIVER
U2=LEVEL 2
$69.20
N/A
Day
SFC3
Structured
Family Care,
Level 3
S5140
U7
U3
U7=WAIVER
U3= LEVEL 3
$79.94
N/A
Day
HSE
Supported
Employ
H2023
U7
U7=WAIVER
N/A
$9.17
.25 Hour
RHHA
Unskilled
Respite Care, N
S5150
U7
UA
U9
U7=WAIVER
UA=PROVIDE
R; U9=HOME
HEALTH
AIDE
$5.12
$4.00
.25 Hour
VMOD
Vehicle
Modifications
T2039
U7
U7=WAIVER
$15,000.00
$15,000.00
Life Cap
VMOM
Vehicle
Modifications-
Maintenance
T2039
U7
U8
U7=WAIVER
U8=Maintenanc
e
$500.00
$500.00
Annual Cap
PEST
Waiver Service,
Nos
T2025
U7
U1
U7=WAIVER
U1=PEST
CONTROL
$600.00
$600.00
Annual Cap
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 3-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 3: Quality Assurance /Quality
Improvement
Quality Monitoring
The Division of Aging (DA) is responsible for monitoring compliance with the provider and case
management standards for the waivers administered by DA as detailed in 455 IAC. Noncompliance
with the standards may result in corrective action plans or other sanctions, up to and including
termination as a waiver provider.
The purpose of the Division of Aging Quality Assurance (QA) and Quality Improvement (QI) Unit is
to protect the safety and well-being of individuals by monitoring and ensuring the integrity and cost-
effectiveness of programs administered by the Division of Aging. The role of the DA QA/QI Unit is to:
• Monitor all providers who are not licensed by the Indiana State Department of Health (ISDH).
• Assure services to all participants are delivered in accordance with the participant’s service plan,
the specifications identified in the approved waiver and 455 IAC.
• Collect and analyze information and data in order to implement sound remediation of problems at
the individual, organization, and systemic levels.
• Participate with other stakeholders in the development of policies and procedures that all providers,
including case managers, must follow to assure compliance with Indiana Administrative Codes
(IAC) and Centers for Medicare and Medicaid Services (CMS) assurances, and to protect
participants’ health and welfare.
The components of the DA QA/QI program are:
• Incident reporting
• Complaint resolution
• Mortality review
• Coordination with Adult Protective Services (APS) and the local Area Agencies on Aging (AAAs)
and case managers
• Quality reviews (provider compliance surveys, participant-centered compliance surveys, participant
experience surveys)
• Coordination with Medicaid Surveillance and Utilization Review (SUR) and the ISDH
• Implementation of the Quality Improvement Strategy (QIS) process
Incident Reporting
Providers with first knowledge of a reportable event are required to report that event via the
designated website at https://ddrsprovider.fssa.in.gov/IFUR. To report incidents involving
consumers of non-waiver Division of Aging services, please use
https://myweb.in.gov/FSSA/aging/incident/incident.aspx.
Incidents are defined as unusual occurrences affecting the health and safety of Home and Community-
Based Services (HCBS) waiver participants, including death. Incidents are required to be reported
within 48 hours of knowledge of the event, or within 24 hours of knowledge if the incident involves
suspicion or evidence of abuse, neglect, exploitation, or death. Providers are required to send copies of
all incident reports to the participant’s case manager. Incidents involving suspicion or evidence of
abuse, neglect, exploitation, or death must also be reported to APS or Child Protective Services (CPS),
ARCHIVED
Section 3: Quality Assurance/Quality Improvement HCBS Waiver Program Provider Manual
I-3-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
as applicable. Each provider of services must establish and make available to the participant a written
procedure for reporting incidents to DA.
Reportable incidents include, but are not limited to:
• Alleged, suspected, reported, or observed abuse or battery, neglect, or exploitation of a participant.
The provider is required to suspend staff alleged to have committed abuse, neglect, or exploitation
from direct-care responsibilities, pending the outcome of the provider’s investigation.
• The death of a participant
• Significant injury to the participant
• Any suicidal ideation, threat, or attempt of suicide made by the participant
• A missing person (participant)
• Inadequate formal or informal support for a participant, including inadequate supervision, which
endangers the participant
• Medication error occurring in a 24/7 or day-program setting
• A residence that compromises the health and safety of a participant, including pest infestations that
represent a potential source of harm
• Suspected or observed criminal activity by staff, a family caregiver, or a participant receiving
services.
• Police arrest of the participant or any person responsible for the care of the participant
• A major disturbance or threat to public safety created by the participant
• Any use of restraint on the participant, including but not limited to, physical, mechanical, and
pharmaceutical
Providers are required to report incidents regardless of whether they were providing services at the
time of the incident. All provider staff should be familiar with incident reporting (IR) requirements and
procedures because knowledge of an incident begins as soon as any employee of the provider becomes
aware of the event. If a provider or case manager has confirmed with another provider that an incident
has already been reported, an additional report is not required, but the provider may wish to file an
additional report to relay additional information or another perspective of the event.
The DA reviews, codes, and determines the level of follow-up required for an incident. Additional
information may be requested from the provider or case manager. When formal follow-up is required,
the case manager is required to submit follow-up reports via the web-based incident reporting system
every seven days until the DA closes the report.
Complaint Resolution
The DA addresses complaints submitted by or on behalf of any individual receiving services through a
waiver administered by the DA. Complaints may be initiated by any individual through the IR system,
mail, telephone, or fax. Complaint investigations may result in findings requiring remediation. A
provider’s failure to complete remediation may result in sanctions up to and including termination as a
waiver provider.
Mortality Review
As part of its QA/QI process, the DA reviews all waiver consumer deaths to identify service delivery
failures or opportunities for improvement at the provider and system level. Providers may be asked to
submit case notes, service delivery records, or other pertinent information or records for review. The
Mortality Review Committee (MRC) may refer waiver providers, case managers, or non-waiver
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 3: Quality Assurance/Quality Improvement
Library Reference Number: PRPR10013 3-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
service providers to the relevant regulatory body, including law enforcement, for additional action. The
MRC may also refer complaints against a waiver provider or case manager for internal remediation
through the complaint resolution process.
Quality Reviews
The DA conducts Provider Compliance Reviews (PCRs) for all non-licensed waiver service providers,
and licensed providers when they also offer services which fall outside of the scope of the license. The
PCR includes a review of provider policies and adherence to State and federal requirements as well as
the provider’s own policies. Providers are reviewed at least every three years.
The State has contracted with a quality assurance organization to administer Person Centered
Compliance Reviews and Participant Experience Surveys. Person Centered Compliance Reviews will
entail a participant interview, an extensive review of provider and case manager documentation,
service delivery records, policies and procedures, and compliance with other waiver and State
requirements.
Findings of one or more deficiencies relating to provider standards will result in a remediation process
to correct the deficiencies. Provider failure to cooperate with the review procedure or to complete the
remediation process will result in a referral to the DA QA/QI Unit as a formal complaint, which may
result in sanctions up to and including termination as a waiver provider.
QIS Process
The Division of Aging QA/QI Unit aggregates and analyzes data from all waiver processes to identify
incidents of noncompliance with waiver requirements and opportunities to achieve more positive
outcomes. Findings are reviewed for viable remediation options at the individual and systemic levels.
Provider failure to complete required remediation may result in sanctions up to and including
termination as a waiver provider.
The QA/QI Unit, working in conjunction with the OMPP and the QA/QI Committee, recommends
systemic improvements and assesses the performance of the QA/QI components.
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 4-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 4: Financial Oversight
Waiver Audits
The state of Indiana employs a hybrid program integrity (PI) approach to oversight of the waiver
programs, incorporating oversight and coordination by a dedicated waiver specialist position within the
Surveillance and Utilization Review (SUR) Unit, as well as engaging the full array of technology and
analytic tools available through the Fraud and Abuse Detection System (FADS) contractor
arrangements. The Family and Social Services Administration (FSSA) has expanded its PI activities
using a multifaceted approach to SUR activity that includes provider self-audits, desk audits, and on-
site audits. The FADS team analyzes claims data, allowing them to identify providers and claims that
indicate aberrant billing patterns or other risk factors.
The PI audit process uses data mining, research, identification of outliers, problematic billing patterns,
aberrant providers, and issues that are referred by other divisions and State agencies. In 2011, the State
of Indiana formed a Benefit Integrity Team comprised of key stakeholders that meets biweekly to
review and approve audit plans, provider communications and make policy and system
recommendations to affected program areas. The SUR Unit also meets with all waiver divisions on a
quarterly basis, at a minimum, and receives referrals on an ongoing basis to maintain open lines of
communication and aid in understanding specific areas of concern such as policy clarification.
The SUR waiver specialist is a subject-matter expert (SME) responsible for directly coordinating with
the various waiver divisions. This specialist also analyzes data to identify potential areas of program
risk and identify providers that appear to be outliers warranting review. The SME may also perform
desk or on-site audits and be directly involved in review of waiver providers and programs.
The FSSA maintains oversight throughout the entire PI process. Although the FADS contractor may be
incorporated in the audit process, no audit is performed without the authorization of the FSSA. The
FSSA’s oversight of the contractor’s aggregate data is used to identify common problems to be
audited, determine benchmarks, and offer data to peer providers for educational purposes, when
appropriate.
The SUR Unit offers education regarding key program initiatives and audit issues at waiver provider
meetings to promote ongoing compliance with federal and State guidelines, including all Indiana
Health Coverage Programs (IHCP) and waiver requirements. Detailed information on SUR policy and
procedures is available in Chapter 13 of the IHCP Provider Manual.
FSSA Audit Oversight
The Audit Division of the FSSA reviews waiver audit team schedules and findings to reduce
redundancy and assure use of consistent methodology.
Medicaid Fraud Control Audit Overview
The Indiana Medicaid Fraud Control Unit (MFCU) is an investigative branch of the Attorney
General’s Office. MFCU conducts investigations in the following areas:
• Medicaid provider fraud
• Misuse of Medicaid members’ funds
ARCHIVED

Section 4: Financial Oversight HCBS Waiver Program Provider Manual
I-4-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Patient abuse or neglect in Medicaid facilities
When the MFCU identifies a provider that has violated one of these areas, the provider’s case is
presented to the State or federal prosecutors for appropriate action. Access information about the
MFCU at .in.gov/attorneygeneral.
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 5-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 5: Division of Aging Waivers
Overview
Indiana administers two home and community-based waivers for persons who meet eligibility for
nursing facility services:
• Waiver for persons who are aged or disabled
• Waiver for persons with a traumatic brain injury
Per agreement with the State Medicaid agency the Division of Aging (DA) has responsibility for the
day-to-day operations of these waivers according to the approved waiver documents. The State
Medicaid agency retains oversight authority.
Level of Care (LOC)
Persons who meet eligibility for the Aged & Disabled (A&D) Waiver must meet nursing facility (NF)
level of care. The criteria necessary to meet this level of care is outlined in 405 IAC 1-3. View the most
up-to-date version of 405 IAC 1-3 in its entirety at in.gov/legislative/iac. Persons who meet eligibility
for the Traumatic Brain Injury waiver must meet nursing facility level of care (LOC) or intermediate
care facility for individuals with intellectual disabilities (ICF/IID) LOC.
Aged & Disabled Waiver
The Aged & Disabled waiver is designed to provide an alternative to nursing facility admission for
Medicaid-eligible persons age 65 and older, and persons of all ages with disabilities by providing
supports to complement and supplement informal supports for persons who would require care in a
nursing facility if waiver services or other supports were not available. Indiana’s 16 Area Agencies on
Aging act as the entry points for this waiver. The services available through this waiver are designed to
help participants remain in their own homes, as well as to assist individuals residing in nursing
facilities to return to community settings, such as their own homes, apartments, assisted living, or adult
family care.
• Participant eligibility
Individuals meeting nursing facility LOC and Medicaid eligibility requirements must meet at
least one of the following criteria to receive services through this waiver:
o Age 65 and older
o Disabled
Entry to the waiver may be delayed due to the existence of a waiting list.
Priority admittance to the waiver may be made based on criteria outlined in the approved
waiver.
• Medicaid aid (MA) categories
Aged (MAA)
Blind (MAB)
Disabled (MAD)
Working disabled (MADW and MADI)
42 CFR 435.110 Parents and other caretaker relatives (MA GF)
ARCHIVED

Section 5: Division of Aging Waivers HCBS Waiver Program Provider Manual
I-5-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
42 CFR 435.118 Infants and children under age 19 (MA Y; MA Z; MA 2; MA 9)
42 CFR 435.145 Children for whom adoption assistance or foster care maintenance payments
are made (under title IV-E of the Act) (MA 4; MA 8)
42 CFR 435.150 Former Foster Care Children; Sec. 1902(a)(10)(A)(i)(IX) (MA 15)
42 CFR 435.226 Independent Foster Care Adolescents; Sec. 1902(a)(10)(A)(ii)(VII) (MA 14)
42 CFR 435.227 Individuals under age 21 who are under State adoption assistance agreements
(MA 8)
Sec 1925 of the Act –Transitional Medical Assistance (MA F)
• Services available (see Section 7 for service definitions):
Adult day services
Adult family care
Assisted living
Attendant care
Case management
Community transition
Environmental modification
Environmental modification assessment
Healthcare coordination
Home-delivered meals
Homemaker
Nutritional supplements
Personal emergency response system
Pest control
Respite care
Structured family caregiving
Specialized medical equipment and supplies
Transportation
Vehicle modification
Traumatic Brain Injury Waiver (TBI)
The Traumatic Brain Injury waiver provides home and community-based services to individuals who,
but for the provision of such services, would require institutional care.
Indiana defines a traumatic brain injury as a trauma that has occurred as a closed- or open-head injury
by an external event that results in damage to brain tissue, with or without injury to other body organs.
Examples of external agents are mechanical or events that result in interference with vital functions.
Traumatic brain injury means a sudden insult or damage to brain function, not of a degenerative or
congenital nature. The insult or damage may produce an altered state of consciousness and may result
in a decrease in cognitive, behavioral, emotional, or physical functioning resulting in partial or total
disability not including birth trauma related injury.
• Participant eligibility
Waiver participants must meet the minimal LOC requirements for that of a NF or intermediate
care facility for individuals with intellectual disabilities (ICF/IID) and have a diagnosis of
traumatic brain injury.
Entry to the waiver may be delayed due to the existence of a waiting list.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 5: Division of Aging Waivers
Library Reference Number: PRPR10013 5-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Priority admittance to the waiver may be made based on criteria outlined in the approved
waiver.
• Medicaid aid (MA) categories
Aged (MAA)
Blind (MAB)
Disabled (MAD)
Working disabled (MADW and MADI)
42 CFR 435.110 Parents and other caretaker relatives (MA GF)
42 CFR 435.118 Infants and children under age 19 (MA Y; MA Z; MA 2; MA 9)
42 CFR 435.145 Children for whom adoption assistance or foster care maintenance payments
are made (under title IV-E of the Act) (MA 4; MA 8)
42 CFR 435.150 Former Foster Care Children; Sec. 1902(a)(10)(A)(i)(IX) (MA 15)
42 CFR 435.226 Independent Foster Care Adolescents; Sec. 1902(a)(10)(A)(ii)(VII) (MA 14)
42 CFR 435.227 Individuals under age 21 who are under State adoption assistance agreements
(MA 8)
Sec 1925 of the Act – Transitional Medical Assistance (MA F)
-
• Services available (see to Section 7 for service definitions):
Adult day services
Adult family care
Assisted living
Attendant care
Behavior management/behavior program and counseling
Case management
Community transition
Environmental modification
Healthcare coordination
Home-delivered meals
Homemaker
Nutritional supplements.
Personal emergency response system
Pest control
Residential-based habilitation
Respite
Specialized medical equipment and supplies
Structured-day program
Supported employment
Transportation
Vehicle modification
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 6-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 6: Case Management
For Aged & Disabled and Traumatic Brain Injury Waivers
Medicaid waiver case managers coordinate and integrate all services required in a participant’s person
centered service plan, link participants to needed services, and ensure that participants continue to
receive and benefit from services. Waiver case managers enable participants to receive a full range of
services needed due to a medical condition, in a planned, coordinated, efficient, effective manner.
Case management is a comprehensive service comprised of specific tasks and activities designed to
coordinate and integrate all other services required in the participant’s service plan.
The components of case management are:
• Initial level of care (LOC) assessment
• Development of service plans including coordination of formal and informal supports
• Implementation of the service plan
• Assessment and care planning for discharge from institutionalization
• Bi-annual and ongoing reassessments of LOC
• Quarterly assessment of individual’s needs, per 90-Day Review tool
• Periodic updates of service plans
• Monitoring the quality of home care community services
• Determining and monitoring the cost effectiveness of providing home and community-based
services
• Information and assistance services
• Enhancement or termination of services based on need
• Administrative guidance
• Participation in Medicaid Fair Hearing process
Case management services for persons on the nursing facility Medicaid waivers are provided by
certified case managers, as approved by the Division of Aging (DA). The 16 local Area Agencies on
Aging (AAA) serve as the single point of entry for the nursing facility Medicaid waivers. A case
manager from the AAA is assigned to an applicant. After an applicant has been determined to meet the
eligibility criteria and approved to receive nursing facility Medicaid waiver services, he or she may
choose to retain his or her current AAA case manager or choose a non-AAA or independent case
manager, for ongoing case management services.
Minimum qualifications for case managers are the following:
• All case management services provided must comply with the case management standards.
• The minimum educational and experience criteria for providing this service under the A&D and
TBI waivers are:
A Qualified Mental Retardation Professional (QMRP) who meets the QMRP requirements at
42 CFR 483.430
A registered nurse with one year’s experience in human services; or
A bachelor’s degree in social work, psychology, sociology, counseling, gerontology, or
nursing; or health and human services; or
ARCHIVED
Section 6: Case Management HCBS Waiver Program Provider Manual
I-6-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
A bachelor’s degree in any field with a minimum of two years’ full-time direct-service
experience with the elderly or disabled (including assessment, care plan development, and
monitoring); or
A master’s degree in a related field may substitute for the required experience
An individual continuously employed as a case manager by an Area Agency on Aging (AAA)
since January 1, 1990 (A&D waiver only)
• All case managers must complete the Division of Aging Case Management Orientation Online
(CMO) Training Modules before providing waiver case management services. Until a case manager
has successfully completed the orientation, he or she may not work independently.
• All case managers must annually obtain at least 20 hours of training regarding case management
services. Ten hours of this training must be training approved by the DA under the nursing facility
waiver program.
If the DA identifies a systemic problem with a case manager’s services, the case manager must obtain
training on the topics recommended by the DA.
Case management may not be conducted by any organization, entity, or individual that also delivers
other in-home and community-based services under the DA waiver programs, or any organization,
entity, or individual related by common ownership or control to any other organization, entity, or
individual that also delivers other in-home and community-based services under the nursing facility
waiver program. The exception is an AAA that has been granted permission by the Family and Social
Services Administration (FSSA) to provide direct services to clients.
• Common Ownership exists when an individual, individuals, or any legal entity possesses ownership
or equity of at least 5% in the provider entity, as well as the institution or organization serving the
provider. Control exists where an individual or organization has the power or the ability, directly or
indirectly, to influence or direct the actions or policies of an organization or institution, whether or
not the control is actually exercised.
• Related means associated or affiliated with, or having the ability to control, or be controlled by.
Reimbursement of case management services, as defined in this manual, may not be made unless and
until the client becomes eligible for waiver service. Case management service provided to individuals
who are not eligible for DA waiver services will not be reimbursed as a waiver service.
Case Management Monitoring Standards
The Ongoing Medicaid Home and Community-Based Services Waiver Case Management Standards is
the document that delineates the standards each nursing facility waiver case manager must meet to
fulfill the FSSA DA guiding principles of:
• Responsive, efficient, effective, quality, and timely service delivery
• Effective communication
• Respect, dignity, integrity, and rights for all individuals
• Person-centered planning, informed choice, and personal empowerment
• Community-based services
• Fiscal stewardship
• Quality customer services
Case managers are to comply with all applicable DA standards. The following section is excerpted
from the Case Management Medicaid Waiver Provider Agreement.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 6: Case Management
Library Reference Number: PRPR10013 6-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Ongoing Medicaid Home and Community-Based Services Waiver Case
Management Standards
1. Case managers will maintain the highest professional and ethical standards in the conduct of their
business.
2. Case managers will comply with all DA-issued manuals, as well as all federal, state, and local law,
and all FSSA policy, rules, regulations and guidelines, including the Health Insurance Portability
and Accountability Act (HIPAA).
3. New case managers will complete case manager orientation as approved by the DA prior to being
eligible for Medicaid reimbursement. This orientation is now provided online and can be accessed at
www.in.gov/fssa/da/3491.htm. Completion of the modules is verified through completion of the
final certification test. Division of Aging grades the test and issues certification for any score of 80%
or higher.
4. Case managers are required to complete annual training as follows:
1) The following components of the online orientation must be reviewed annually by all active case
managers:
a) Level of care modules – general, narrative, skilled needs, and activities of daily living
b) Incident reporting module
c) Service definition module
2) An additional eighteen (18) hours of training must be completed annually by all active case
managers.
a) This training does not have to be preapproved by the Division of Aging.
b) This training does have to be relevant to core case management functions.
c) The Training Justification Form must be completed.
d) Training documentation is subject to review in compliance surveys and at Division of Aging
request.
e) Relevant topics can include the following:
i) Care coordination
ii) Documentation
iii) Medical terminology
iv) Other public or privately funded long-term services and support programs or benefits
v) Specific diagnosis or treatment topics affecting a broad spectrum of the client base,
including but not limited to:
(1) Fall prevention
(2) Adaptive equipment
(3) COPD
(4) Congestive heart failure
(5) Diabetes
(6) Traumatic brain injury
(7) Kidney disease
(8) Alzheimer’s Disease
(9) Seizures
(10) Stroke
(11) Heart disease
(12) Mental health issues
(13) Behavioral issues
3) The following will NOT be accepted as part of the required training:
a) Case management orientation
b) Required annual re-trainings as cited in 4)
c) Vendor fairs
d) Staff meetings (unless there is an outside speaker or expert speaking on a relevant topic or
someone who attended a State training as a trainer is sharing that information)
ARCHIVED
Section 6: Case Management HCBS Waiver Program Provider Manual
I-6-4 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
e) Presentations related to employment issues, e.g. performance appraisal process, retirement;
and;
f) Communications that are part of supervisory oversight, e.g. reinforcement or retraining on job
requirements, review of state guidelines, informational, or training, sessions specific to a
case, etc.
4) Required training hours are prorated in a case manager’s first year and are in addition to new case
manager orientation.
5. Individuals will choose their service provider, including their case manager, and have the right to
change any provider, including their case manager.
6. Case managers will provide individuals a list of potential providers, furnished by the state of
Indiana, including case managers and the services offered by each provider.
7. Case managers will provide, at a minimum but not limited to, a tate information guide to individuals
on how to choose a provider and will assist the individual to evaluate potential service providers.
8. A maximum response time between implementation of the initial service plan and the first
monitoring contact will be no more than 30 calendar days.
9. Case managers will have face-to-face contact with each individual a minimum of every 90 days to
assess the quality and effectiveness of the service plan. At least two of these face-to-face contacts
per year will be in the home setting.
10. Case managers will document, in the chronological narrative, each contact with the individual and
each contact with providers within seven days of activity.
11. Case manager documentation must show activity relevant to the service plan to be reimbursed.
12. Case managers will facilitate and monitor the formal and informal supports that are developed to
maintain the individual’s health and welfare in the community.
13. Case managers will provide each individual or guardian with clear and easy instructions for
contacting the case manager or case manager agency. The case manager will also provide additional
information and procedures for individuals who may need assistance or have an emergency that
occurs before or after business hours. This information will be located in the home in a location that
is visible from the telephone.
14. Case managers will complete face-to-face Annual Assessments and update the service plan as
needed, in collaboration with the individual, in a timely and appropriate manner to avoid gaps in
service authorization, including assuring that the individual or guardian receives instructions on how
to request an appeal through the Medicaid Fair Hearing process.
15. Case managers will communicate the individual’s needs, strengths, and preferences to the support
team.
16. Case managers will ensure that person centered planning is occurring on an ongoing basis.
17. Case managers will monitor the ongoing services to ensure that they reflect the service plan,
including the individual’s medication regime.
18. Case managers will base the service plan upon the individual’s needs, strengths, and preferences.
19. Case managers will ensure that the individual and all providers have a current, comprehensive
service plan that meets the needs of the individual.
20. Case managers will review and explain to the individual or guardian the services that will be
provided, and the individual or their designated representative will sign the service plan to show
understanding of, and agreement with, the plan.
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 6: Case Management
Library Reference Number: PRPR10013 6-5
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
21. Case managers will ensure that the individual or guardian, providers, and involved agencies have a
copy of relevant documentation, as specified in the Waiver Case Management Manual, including
instructions on how to request an appeal.
22. Case managers will obtain all required signatures on the service plan before submitting it to the
State. The service plan will not be implemented prior to receiving State approval.
23. Case managers will document the quality; timeliness; and appropriateness of care, services, and
products delivered by providers.
24. Case managers will initiate timely follow-up of identified problems, whether self-identified or
referred by others. Critical or crisis issues, including incident reports, will be acted upon
immediately, as specified by the DA. All follow-up and resolution will be documented in the
individual record.
25. Case managers will comply with all automation standards and requirements as prescribed by the DA
for documentation and processing of case management activities.
26. Case managers will maintain privacy and confidentiality of all individual records. No information
will be released or shared with others without the individual or guardian’s written consent.
27. Case managers will provide to the State upon request, ready access to all case manager
documentation, either electronic or hard copy.
28. Case manager documentation will demonstrate that the safety and welfare of the individual are
being monitored on a regular basis.
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 7-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 7: Service Definitions
Service Definition Overview
This section of the manual lists service definitions for the services currently approved for the Home
and Community-Based Services (HCBS) Nursing Facility Level of Care waiver program. Each service
definition includes the following information as appropriate:
• Service definition
• Allowable activities
• Service standards
• Documentation standards
• Limitations
• Activities not allowed
• Provider qualifications
A provider qualifications table identifies the waiver, the license or certification requirements,
and any additional standards that apply.
Table 2.1 shows procedure (billing) codes and modifiers, as well as unit rates.
Adult Day Services
Service Definition
Adult day services (ADS) are community-based group programs designed to meet the needs of adults
with impairments through individual service plans. These structured, comprehensive, nonresidential
programs provide health, social, recreational, and therapeutic activities, supervision, support services,
and personal care. Meals or nutritious snacks are required. The meals cannot constitute the full daily
nutritional regimen. However, each meal must meet one-third of the daily Recommended Dietary
Allowance. These services must be provided in a congregate, protective setting.
Participants attend ADS on a planned basis. The three levels of ADS are basic, enhanced, and
intensive. The ADS Assessment Tool may be obtained from the Division of Aging website. The
assessment should be conducted with the individual being served, his or her family, the case manager,
and the provider, when possible.
Allowable Activities
Basic adult day services (Level 1) include:
• Monitoring or supervising all activities of daily living (ADLs) – defined as dressing, bathing,
grooming, eating, walking, and toileting – with hands-on assistance provided as needed
• Comprehensive, therapeutic activities
• Health assessment and intermittent monitoring of health status
• Monitoring medication or medication administration
• Appropriate structure and supervision for those with mild cognitive impairment
• Minimum staff ratio of one staff for each eight individuals
• Registered nurse (RN) consultant available
ARCHIVED
Section 7: Service Definitions
I-7-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Enhanced adult day services (Level 2) include all Level 1 service requirements. Additional Level 2
services include:
• Hands-on assistance with two or more ADLs or hands-on assistance with bathing or other personal
care
• Health assessment with regular monitoring or intervention with health status
• Dispensing or supervising the dispensing of medication to individuals
• Psychosocial needs assessed and addressed, including counseling as needed for individuals and
caregivers
• Therapeutic structure, supervision, and intervention for those with mild to moderate cognitive
impairments
• Minimum staff ratio of one staff for each six individuals
• RN consultant available
• Minimum of one full-time licensed practical nurse (LPN) with monthly RN supervision
Intensive adult day services (Level 3) include all Level 1 and Level 2 service requirements. Additional
Level 3 services include:
• Hands-on assistance or supervision with all ADLs and personal care
• One or more direct health interventions required
• Rehabilitation and restorative services, including physical therapy, speech therapy, and
occupational therapy coordinated or available
• Therapeutic intervention to address dynamic psychosocial needs such as depression or family issues
affecting care
• Therapeutic interventions for those with moderate to severe cognitive impairments
• Minimum staff ratio of one staff for each four individuals
• RN consultant available
• Minimum of one full-time LPN with monthly RN supervision
• Minimum of one qualified full-time staff person to deal with participants’ psycho-social needs
Service Standards
Adult day services must follow a written service plan addressing specific needs determined by the
client’s assessment
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Evidence that the level of service provided is required by the individual
• Attendance record documenting the date of service and the number of units of service delivered that
day
• Completed Adult Day Service Level of Service Evaluation form. The case manager must give the
completed Adult Day Service Level of Service Evaluation form to the provider.
Limitations
Adult day services are allowed for a maximum of 10 hours per day.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Activities Not Allowed
Any activity that is not described in allowable activities is not included in this service. Services to
participants receiving assisted living waiver service are not allowed.
Note: Therapies provided through this service will not duplicate therapies provided
under any other service.
Provider Qualifications
Table 7.1 – Provider Qualifications Table for Adult Day Service
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA
approved
Adult Day
Service
Provider
Not required
DA approved
455 IAC 2 Provider Qualifications: Becoming an approved
provider; maintaining approval
455 IAC 2 Provider Qualifications: General requirements
455 IAC 2 Provider Qualifications: General requirements
for direct care staff
455 IAC 2 Procedures for Protecting Individuals
455 IAC 2 Unusual occurrence; reporting
455 IAC 2 Transfer of individual’s record upon change of
provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement
system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
ARCHIVED

Section 7: Service Definitions
I-7-4 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Adult Family Care
Service Definition
Adult family care (AFC) is a comprehensive service in which a participant resides with an unrelated
caregiver for the participant to receive personal assistance designed to provide options for alternative
long-term care to individuals who meet nursing facility level of care and whose needs can be met in a
home-like environment. The participant and up to three other participants who are elderly or have
physical or cognitive disabilities who are not members of the provider’s or primary caregiver’s family,
reside in a home that is owned, rented, or managed by the AFC provider.
The goal of the service is to provide necessary care while emphasizing the participant’s independence.
This goal is reached through a cooperative relationship between the participant (or the participant’s
legal guardian), the participant’s HCBS Medicaid waiver case manager, and the AFC provider.
Participant needs shall be addressed in a manner that supports and enables the individual to maximize
abilities to function at the highest possible level of independence. The service is designed to provide
options for alternative long-term care to persons who meet nursing facility level of care, and whose
needs can be met in an AFC setting.
Another goal is to preserve the dignity, self-respect, and privacy of the participant by ensuring high-
quality care in a non-institutional setting. Care is to be furnished in a way that fosters the independence
of each participant to facilitate aging in place in a home environment that will provide the participant
with a range of care options as the needs of the participant change.
Participants selecting AFC service may also receive case management service, adult day service,
specialized medical equipment and supplies, and healthcare coordination through the waiver.
Note: Participants living in AFC settings are entitled to retain at least their
personal needs allowance (PNA) as established by the state of Indiana. The
PNA is currently $52.00 per month.
A provider, after ensuring that the participants retain their PNA, may bill
participants up to the current maximum federal Supplemental Security
Income (SSI). Providers may not charge Medicaid waiver participants a
room and board rate that exceeds the maximum SSI rate. The maximum SSI
amount for 2015 is $733.00.
Allowable Activities
The following are included in the daily per diem for AFC:
• Attendant care
• Chores
• Companion services
• Homemaker services
• Medication oversight (to the extent permitted under State law)
• Personal care and services
• Transportation for community activities that are therapeutic in nature or assist with maintaining
natural supports. (Medicaid State Plan transportation should be requested for medical
transportation.)
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-5
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Consumer-focused activities that are appropriate to the needs, preferences, age, and condition of the
individual participant
• Assistance with correspondence and bill paying, if requested by participant
Service Standards
• AFC services must follow a written service plan addressing specific needs determined by the
individual’s assessment.
• Services must address the participant’s level of service needs.
• The provider must live in the AFC home, unless another provider-contracted primary caregiver,
who meets all provider qualifications, lives in the provider’s home.
• Backup services must be provided by a qualified individual familiar with the individual’s needs for
those times when the primary caregiver is absent from the home or otherwise cannot provide the
necessary level of care.
• AFC provides an environment that has the qualities of a home, including privacy, comfortable
surroundings, and the opportunity to modify one’s living area to suit one’s individual preferences.
• Rules managing or organizing the home activities in the AFC home that are developed by the
provider, a provider-contracted primary caregiver, or both, and approved by the Medicaid waiver
program must be provided to the individual before the start of AFC services and may not be so
restrictive as to interfere with a participant’s rights under State and federal law.
• Consumer-focused activity plans are developed by the provider with the participant or the
participant’s representative.
• AFC emphasizes the participant’s independence in a setting that protects and encourages the
participant’s dignity, choice, and decision-making while preserving self-respect.
• Providers or providers’ employees who provide medication oversight, as addressed under Allowable
Activities, must receive necessary instruction from a doctor, nurse, or pharmacist on the
administration of controlled substances prescribed to the participant.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Completed Adult Family Care Level of Service Evaluation form required. (The case manager must
give the completed Adult Family Care Level of Service Evaluation form to the provider.)
• Daily documentation to support services rendered by the AFC to address needs identified in the
Adult Family Care Level of Service Evaluation form
Participant’s status
Updates
Participation in consumer-focused activities
Medication management records, if applicable
• Maintenance of participant’s personal records to include:
Social Security number
Medical insurance number
Birth date
All medical information available, including all prescription and nonprescription drug
medication currently in use
Most recent prior residence
Hospital preference
Mortuary preference (if known)
ARCHIVED

Section 7: Service Definitions
I-7-6 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Religious affiliation and place of worship, if applicable
• Participant’s personal records must contain copies of all applicable documents:
Advance directive
Living will
Power of attorney
Healthcare representative
Do-not-resuscitate (DNR) order
Letters of guardianship
Note: If applicable, copies must be:
• Placed in a prominent place in the consumer file
• Sent with the consumer when transferred for medical care
Activities Not Allowed
• Services provided in the home of a caregiver who is related by blood or related legally to the
participant
• Adult family care services will not be reimbursed when provided as an individual provider by a
parent of a minor child participant, the spouse of a participant, the attorney-in-fact (POA) of a
participant, the healthcare representative (HCR) of a participant, or the legal guardian of a
participant
• Payments for room and board or the costs of facility maintenance, upkeep, or improvement
• Personal care services provided to medically unstable or medically complex participants as a
substitute for care provided by a registered nurse, licensed practical nurse, licensed physician, or
other health professional
The adult family care service per diem does not include room and board.
Separate payment will not be made for homemaker services, respite, environmental modifications,
vehicle modifications, transportation, personal emergency response system, attendant care, assisted
living, home-delivered meals, nutritional supplements, pest control, community transition, or
structured family caregiving services furnished to a participant selecting adult family care services, as
these activities are integral to and inherent in the provision of adult family care services.
Provider Qualifications
Table 7.2 – Provider Qualifications Table for Adult Family Care
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
approved Adult
Family Care
Individual
Not required
Provider and home must meet the requirements of the Indiana
Adult Family Care Service Provision and Certification
Standards. Adult family care service providers are required to
maintain Commercial General Liability insurance with the
Indiana Division of Aging identified as a Certificate Holder.
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider Qualifications; General requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-7
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Waiver
Provider
Licensure/
Certification
Other Standard
455 IAC 2 Transfer of individual’s record upon change of
provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Transportation of an individual
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service delivery
A&D,
TBI
FSSA/DA
approved Adult
Family Care
Agency
Not required
Provider and home must meet the requirements of the Indiana
Adult Family Care Service Provision and Certification
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider Qualifications: General Requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
455 IAC 2 Transfer of individual’s record upon change of
provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Transportation of an individual
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service delivery
ARCHIVED

Section 7: Service Definitions
I-7-8 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Assisted Living
Service Definition
Assisted living service is defined as personal care and services, homemaker services, chores, attendant
care and companion services, medication oversight (to the extent permitted under State law), and
therapeutic social and recreational programming provided in a home-like environment in a residential
facility that is licensed by the Indiana State Department of Health (ISDH), in conjunction with residing
in the facility. This service includes 24-hour, on-site response staff to meet scheduled or unpredictable
needs in a way that promotes maximum dignity and independence, and to provide supervision, safety,
and security. Other individuals or agencies may also furnish care directly or under arrangement with
the community care facility, but the care provided by these other entities supplements that provided by
the community care facility and does not supplant it.
Individuals reside in their own living units (which may include dually occupied units, when both
occupants request the arrangement), which include kitchenette, toilet facilities, and a sleeping area (not
necessarily designated as a separate bedroom from the living area). The individual has a right to
privacy. Living units may be locked at the discretion of the individual, except when a physician or
mental health professional has certified in writing that the individual is sufficiently impaired as to be a
danger to self or others if given the opportunity to lock the door. (This requirement does not apply
where it conflicts with fire code.) Each living unit is separate and distinct from each other. The facility
must have a central dining room, living room or parlor, and common activity centers, which may also
serve as living rooms or dining rooms. The individual retains the right to assume risk, tempered only
by the individual’s ability to assume responsibility for that risk. Care must be furnished in a way that
fosters the independence of each individual to facilitate aging in place. Routines of care and service
delivery must be individual-driven to the maximum extent possible and must treat each person with
dignity and respect.
Participants selecting assisted living service may also receive case management service, specialized
medical equipment and supplies, and community transition services through the waiver.
Note: Under 455 IAC 3-1-12, participants living in assisted living facilities are
entitled to retain at least their personal needs allowance (PNA) as
established by the state of Indiana. The PNA is currently $52.00 per month.
A provider, after ensuring that the participants retain their PNA, may bill
participants up to the current maximum federal Supplemental Security
Income (SSI). Providers may not charge Medicaid waiver participants a
room and board rate that exceeds the maximum SSI rate. The maximum SSI
amount for 2015 is $733.00.
Allowable Activities
The following are included in the daily per diem for assisted living services:
• Attendant care
• Chores
• Companion services
• Homemaker services
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-9
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Medication oversight (to the extent permitted under State law)
• Personal care and services
• Therapeutic social and recreational programming
Service Standards
Assisted living services must follow a written service plan addressing specific needs determined by the
client’s assessment.
Documentation Standards
• Services outlined in the service plan.
• Evidence that individual requires the level of service provided.
• Documentation to support service rendered.
• Negotiated risk agreement, if applicable.
• Completed Assisted Living Level of Service Evaluation form required. (The case manager must give
the completed Assisted Living Level of Service Evaluation form to the provider.)
Activities Not Allowed
• The assisted living service per diem does not include room and board.
• Personal care services provided to medically unstable or medically complex participants as a
substitute for care provided by a registered nurse, licensed practical nurse, licensed physician, or
other health professional.
Separate payment will not be made for homemaker services, respite, environmental modifications,
vehicle modifications, transportation, personal emergency response system, attendant care, adult
family care, adult day services, home-delivered meals, nutritional supplements, pest control, or
structured family caregiving furnished to a participant selecting assisted living services, as these
activities are integral to and inherent in the provision of the assisted living service.
Provider Qualifications
Table 7.3 – Provider Qualifications Table for Assisted Living
Waiver
Provider
Licensure/
Certification
Other Standard
A&D
Licensed Assisted
Living Agencies
IC 16-28-2
DA approved
410 IAC 16.2-5
ARCHIVED
Section 7: Service Definitions
I-7-10 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Attendant Care
Service Definition
Attendant care services primarily involve hands-on assistance for aging adults and persons with
disabilities. These services are provided to allow aging adults or persons with disabilities to remain in
their own homes and to carry out functions of daily living, self-care, and mobility.
Allowable Activities
Homemaker activities that are essential to the individual’s healthcare needs to prevent or postpone
institutionalization, when provided during the provision of other attendant care services, are allowed:
• Provision of assistance with personal care, which includes:
Bathing, partial bathing
Oral hygiene
Hair care, including clipping of hair
Shaving
Hand and foot care
Intact skin care
Application of cosmetics
• Provision of assistance with mobility, which includes:
Proper body mechanics
Transfers
Ambulation
Use of assistive devices
• Provision of assistance with elimination, which includes:
Assistance with bedpan, bedside commode, and toilet
Incontinent or involuntary care
Emptying urine collection and colostomy bags
• Provision of assistance with nutrition, which includes:
Meal planning, preparation, clean-up
• Provision of assistance with safety, which includes:
Use of the principles of health and safety in relation to self and individual
Identifying and eliminating safety hazards
Practicing health protection and cleanliness by appropriate techniques of hand washing
Waste disposal and household tasks
Reminding individuals to self-administer medications
Providing assistance with correspondence and bill paying
Escorting individuals to community activities that are therapeutic in nature or that assist with
developing and maintaining natural supports
Service Standards
• Attendant care services must follow a written service plan addressing specific needs determined by
the individual’s assessment
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-11
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• If direct care or supervision of care is not provided to the client and the documentation of services
rendered for the units billed reflects homemaker duties, an entry must be made to indicate why the
direct care was not provided for that day. If direct care or supervision of care is not provided for
more than 30 days and the documentation of services rendered for the units billed reflects
homemaker duties, the case manager must be contacted to amend the service plan to:
Add homemaker services and eliminate attendant care services, or
Reduce attendant care hours and replace with the appropriate number of hours of homemaker
services.
Documentation Standards
• Need must be identified in the service plan.
• Services must be outlined in the service plan.
• Data record of services must be provided, including:
Complete date and time of service (in and out)
Specific services or tasks provided
Signature of employee providing the service (minimally the last name and first initial)
o If the person providing the service is required to be a professional, the title of the
individual must also be included.
• Each staff member providing direct care or supervision of care to the individual must make at least
one entry on each day of service. All entries should describe an issue or circumstance concerning
the individual.
• Documentation of service delivery is to be signed by the participant or designated participant
representative.
Activities Not Allowed
• Attendant care services will not be provided to medically unstable individuals as a substitute for
care provided by a registered nurse, licensed practical nurse, licensed physician, or other health
professional
• Attendant care services will not be provided to household members other than to the participant
• Attendant care services will not be reimbursed when provided as an individual provider by a parent
of a minor child participant, the spouse of a participant, the attorney-in-fact (POA) of a participant,
the healthcare representative (HCR) of a participant, or the legal guardian of a participant
• Attendant care services to participants receiving adult family care waiver service, structured family
caregiving waiver service, or assisted living waiver service
Provider Qualifications
Table 7.4 – Provider Qualifications Table for Attendant Care
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1
IC 16-27-4
DA approved
A&D,
TBI
Licensed
Personal
Services Agency
IC 16-27-4
DA approved
A&D,
TBI
FSSA/DA
approved
Attendant Care
IC 16-27-4
DA approved
455 IAC 2 Provider Qualifications; General
requirements
ARCHIVED

Section 7: Service Definitions
I-7-12 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Waiver
Provider
Licensure/
Certification
Other Standard
Individual
455 IAC 2 General requirements for direct care
staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements
455 IAC 2 Personnel Records
The division may reject any applicant with a
conviction of a crime against persons or
property, a conviction for fraud or abuse in any
federal, state, or local government program,
(42 USC §1320a-7) or a conviction for illegal
drug possession. The division may reject an
applicant convicted of the use, manufacture, or
distribution of illegal drugs (42 USC §1320a-
7). The division may reject an applicant who
lacks the character and fitness to render
services to the dependent population or whose
criminal background check shows that the
applicant may pose a danger to the dependent
population. The division may limit an applicant
with a criminal background to caring for a
family member only if the family member has
been informed of the criminal background.
Compliance with IC 16-27-4, if applicable.
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-13
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Behavior Management/Behavior Program and Counseling
Service Definition
Behavior management includes training, supervision, or assistance in appropriate expression of
emotions and desires, assertiveness, acquisition of socially appropriate behaviors, and the reduction of
inappropriate behaviors.
Behavior plans must be developed, monitored, and amended by a master’s level psychologist or a
master’s in special education, supervised by an individual with a Ph.D. in behavioral science. Persons
providing behavior management/behavior program and counseling who are employed by a qualified
agency must be a Master’s level behaviorist; a Certified Brain Injury Specialist (CBIS); a Qualified
Intellectual Disability Professional ; or a Certified Social Worker who is supervised by a Master’s level
behaviorist. An individual practitioner providing this service must be a Master’s level behaviorist.
Allowable Activities
• Observation of the individual and environment for purposes of development of a plan and to
determine baseline
• Development of a behavioral support plan and subsequent revisions
• Training in assertiveness
• Training in stress reduction techniques
• Training in the acquisition of socially accepted behaviors
• Training staff, family members, roommates, and other appropriate individuals implementation of
the behavior support plan
• Consultation with members
• Consultation with health service provider in psychology (HSPP)
Service Standards
• Behavior management/behavior program and counseling services must follow a written service plan
addressing specific needs determined by the individual’s assessment
• The behavior specialist will observe the individual in his or her own environment and develop a
specific plan to address identified issues.
• The efficacy of the plan must be reviewed not less than quarterly and adjusted as necessary.
• The behavior specialist will provide a written report to pertinent parties at least quarterly. “Pertinent
parties” include the individual, guardian, waiver case manager, all service providers, and other
involved entities.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Service plan must have the identified level clinician
• Behavioral support plan
• Data record of clinician service documenting the date and time of service, and the number of units
of service delivered that day with the service type
ARCHIVED

Section 7: Service Definitions
I-7-14 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Activities Not Allowed
• Aversive techniques
• Any techniques not approved by the individual’s person-centered planning team and the Division of
Aging
• Behavior management/behavior program and counseling services will not be reimbursed when
provided as an individual provider by a parent of a minor child participant, the spouse of a
participant, the attorney-in-fact (POA) of a participant, the healthcare representative (HCR) of a
participant, or the legal guardian of a participant.
Provider Qualifications
Table 7.5 – Provider Qualifications Table for Behavior Management/Behavior Program and
Counseling
Waiver
Provider
Licensure/
Certification
Other Standard
TBI
FSSA/DA
Approved
Behavior
Management/
Behavior
Program and
Counseling
Individual
Not required
DA approved
455 IAC 2 Provider Qualifications; General requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements
455 IAC 2 Personnel Records
An individual practitioner providing this service must be
a master’s level behaviorist.
TBI
FSSA/DA
approved
Behavior
Management/
Behavioral
Program and
Counseling
Agency
Not required
DA approved
455 IAC 2 Provider Qualifications; General requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements
455 IAC 2 Personnel Records
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-15
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Case Management
Service Definition
Case management is a comprehensive service comprising a variety of specific tasks and activities
designed to coordinate and integrate all other services required in the individual’s service plan.
Allowable Activities
• Assessments of eligible individuals to determine eligibility for services, functional impairment
level, and corresponding in-home and community-based services needed by the individual
• Development of service plans to meet the individual’s needs
• Implementation of the service plans linking individual with needed services, regardless of the
funding source
• Assessment and care planning for discharge from institutionalization
• Annual and quarterly face-to-face reassessments of individual’s needs
• Periodic updates of care plans
• Monitoring of the quality of home care community services provided to the individual
• Determination of and monitoring the cost effectiveness of providing in-home and community-based
services
• Information and assistance services
• Enhancement or termination of services based on need
• Administrative guidance as described in Appendix E-1-j of the waiver application for participants
who have selected self-directed attendant care
Service Standards
Case management services must be reflected in the service plan of the individual. Services must
address needs identified in the service plan.
Documentation Standards
• Must be an approved provider.
• Must provide documentation identifying the provider as the case manager of record for the
individual. (The pick list is appropriate documentation.)
• Must document all activities on behalf of individual being served within seven days of service.
Clinical/progress documentation standards for case management include:
• Services must be outlined in the service plan.
• Evidence must be provided that individual requires the level of service.
• Documentation to support services rendered must be provided.
• Case manager must ensure that the LOC review form is sent to the participant or applicant within
10 working days of the issue date and must document in the electronic case management database
system the date the LOC review form was delivered.
Activities Not Allowed
ARCHIVED

Section 7: Service Definitions
I-7-16 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Case management may not be conducted by any organization, entity, or individual that also delivers
other in-home and community-based services, or by any organization, entity, or individual related
by common ownership or control to any other organization, entity, or individual who also delivers
other in-home and community-based services, unless the organization is an Area Agency on Aging
that has been granted permission by the Family and Social Services Administration Division of
Aging to provide direct services to individuals.
Note: Common ownership exists when an individual, individuals, or any legal
entity possess ownership or equity of at least 5% in the provider entity, as
well as the institution or organization serving the provider. Control exists
where an individual or organization has the power or the ability, directly or
indirectly, to influence or direct the actions or policies of an organization or
institution, whether or not actually exercised. Related means associated or
affiliated with, or having the ability to control, or be controlled by.
• Independent case managers and independent case management companies may not provide initial
applications for Medicaid waiver services.
• Reimbursement of case management under Medicaid waivers may not be made unless and until the
individual becomes eligible for Medicaid waiver services. Case management provided to
individuals who are not eligible for Medicaid waiver services will not be reimbursed as a Medicaid
waiver service.
• Case management services will not be reimbursed when provided as an individual provider by a
parent of a minor child participant, the spouse of a participant, the attorney-in fact (POA) of a
participant, or the HCR of a participant, or the legal guardian of a participant.
Provider Qualifications
Table 7.6 – Provider Qualifications Table for Case Management
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA
Approved
Case
Management
Individual
Not required
DA, or its designee, approved
455 IAC 2 Documentation of qualifications
455 IAC 2 Case Management
Liability Insurance
Training in the nursing facility level of care process by
the Division of Aging or designee
Education and work experience:
• A Qualified Intellectual Disability Professional who
meets the requirements at 42 CFR 483.430
• A registered nurse with one year’s experience in
human services
• A bachelor’s degree in social work, psychology,
sociology, counseling, gerontology, or nursing; health
and human services
• A bachelor’s degree in any field with a minimum of
two years of full-time, direct-service experience with
the elderly or disabled (this experience includes
assessment, care plan development, and monitoring)
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-17
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Waiver
Provider
Licensure/
Certification
Other Standard
• A master’s degree in a related field may substitute for
the required experience
A&D
FSSA/DA
approved Case
Management
Agency
Not required
DA, or its designee, approved
455 IAC 2 Provider Qualifications; General requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
455 IAC 2 Transfer of individual’s record upon change
of provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement
system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Case Management
Training in the nursing facility level of care process by
the Division of Aging or designee – education and work
experience:
• An individual continuously employed as a case
manager by an Area Agency on Aging (AAA) since
January 1, 1990
• A Qualified Intellectual Disability Professional who
meets the requirements at 42 CFR 483.430
• A registered nurse with one year’s experience in
human services; or
• A bachelor’s degree in social work, psychology,
sociology, counseling, gerontology, nursing or
health and human services; or
• A bachelor’s degree in any field with a
minimum of two years full-time, direct service
experience with the elderly or disabled (this
experience includes assessment, care plan
development, and monitoring); or
• A master’s degree in a related field may
substitute for the required experience
TBIA
FSSA/DA
approved Case
Management
Agency
Not Required
DA, or its designee, approved
455 IAC 2 Provider Qualifications; General requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
ARCHIVED

Section 7: Service Definitions
I-7-18 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Waiver
Provider
Licensure/
Certification
Other Standard
455 IAC 2 Transfer of individual’s record upon change
of provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement
system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
455 IAC 2 Case Management
Education and work experience
• A Qualified Intellectual Disability Professional who
meets the requirements at 42 CFR 483.430
• A registered nurse with one year’s experience in
human services; or
- A bachelor’s degree in social work, psychology,
sociology, counseling, gerontology, or nursing;
or
- A bachelor’s degree in any field with a
minimum of two years of full-time, direct
service experience with the elderly or disabled
(this experience includes assessment, care plan
development, and monitoring); or
- A master’s degree in a related field may
substitute for the required experience
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-19
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Community Transition
Service Definition
Community transition services include reasonable setup expenses for individuals who make the
transition from an institution to their own home where the person is directly responsible for his or her
own living expenses in the community and will not be reimbursable on any subsequent move.
Note: “Own home” is defined for this service as any dwelling, including a house,
an apartment, a condominium, a trailer, or other lodging that is owned,
leased, or rented by the individual or the individual’s guardian or family, or
a home that is owned or operated by the agency providing supports.
Items purchased through community transition are the property of the individual receiving the service,
and the individual takes the property with him or her in the event of a move to another residence, even
if the residence from which he or she is moving is owned by a provider agency. Nursing facilities are
not reimbursed for community transition because those services are part of the per diem. For those
receiving this service under the waiver, reimbursement for approved community transition
expenditures are reimbursed through the local AAA.
Allowable Activities
• Security deposits that are required to obtain a lease on an apartment or home
• Essential furnishings and moving expenses required to occupy and use a community domicile
including a bed, table or chairs, window coverings, eating utensils, food preparation items,
microwave, and bed or bath linens
• Setup fees or deposits for utility or service access including telephone, electricity, heating, and
water
• Health and safety assurances including pest eradication, allergen control, or one-time cleaning prior
to occupancy
Service Standards
Community transition services must follow a written service plan addressing specific needs determined
by the individual’s assessment.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Documentation requirements include maintaining receipts for all expenditures, showing the amount
and what item or deposit was covered
Limitations
Reimbursement for community transition is limited to a lifetime cap for setup expenses, up to $1,500.
ARCHIVED

Section 7: Service Definitions
I-7-20 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Activities Not Allowed
• Apartment or housing rental or mortgage expenses
• Food
• Appliances
• Diversional or recreational items such as hobby supplies
• Television
• Cable TV access
• VCRs
• Regular utility charges
• Services to participants receiving adult family care waiver service
Provider Qualifications
Table 7.7 – Provider Qualifications Table for Community Transition
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA
Approved
Community
Transition
Service
Agency
Not required
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: General requirements
455 IAC 2 Transfer of individual’s record upon change of
provider
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Transportation of an individual
455 IAC 2 Professional qualifications and requirements;
documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service
delivery
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-21
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Environmental Modifications
Service Definition
Environmental modifications are minor physical adaptations to the home, as required by the
individual’s service plan which are necessary to ensure the health, welfare and safety of the individual,
which enable the individual to function with greater independence in the home, and without which the
individual would require institutionalization.
Home Ownership
Environmental modifications shall be approved for the individual’s own home or family-owned home.
Rented homes or apartments are allowed to be modified only when a signed agreement from the
landlord is obtained. The signed agreement must be submitted along with all other required waiver
documentation.
Choice of Provider
The individual chooses which approved/certified providers will submit bids or estimates for this
service. The provider with the lowest bid will be chosen, unless there is a strong written justification
from the case manager detailing why a provider with a higher bid should be selected.
Requirements
All environmental modifications must be approved by the waiver program prior to services are
rendered.
• Environmental modification requests must be provided in accordance with applicable State or local
building codes and should be guided by Americans with Disability Act (ADA) or ADA Accessibility
Guidelines (ADAAG) requirements when in the best interest of the individual and his or her
specific situation.
• Environmental modifications shall be authorized only when it is determined to be medically
necessary and shall have direct medical or remedial benefit for the waiver individual. This
determination includes the following considerations:
The modification is the most cost effective or conservative means to meet the individual’s
needs for accessibility within the home.
The environmental modification is individualized, specific, and consistent with, but not in
excess of, the individual’s needs.
• Requests for modifications at two or more locations may only be approved at the discretion of the
DA director or designee.
• Requests for modifications may be denied if the State division director or State agency designee
determines that the documentation does not support residential stability or the service requested.
Allowable Activities
Justification and documentation is required to demonstrate that the modification is necessary to meet
the individual’s identified needs.
• Adaptive door openers and locks − Limited to one per individual primary residence for an
individual living alone or who is alone without a caregiver for substantial periods of time but needs
to open, close, or lock the doors and cannot do so without special adaptation.
ARCHIVED
Section 7: Service Definitions
I-7-22 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Bathroom modification − Limited to one existing bathroom per individual primary residence when
no other accessible bathroom is available. The bathroom modification may include:
Removal of existing bathtub, toilet, or sink
Installation of roll in shower, grab bars, ADA toilet, and wall-mounted sink
Installation of replacement flooring, if necessary due to bath modification
• Environmental control units − Adaptive switches and buttons to operate medical equipment,
communication devices, heat and air conditioning, and lights for an individual living alone or who
is alone without a caregiver for a substantial portion of the day.
• Environmental safety devices limited to:
Door alarms
Antiscald devices
Hand-held shower head
Grab bars for the bathroom
• Fence – Limited to 200 linear feet (individual must have a documented history of elopement)
• Ramp – Limited to one per individual primary residence and only when no other accessible ramp
exists:
In accordance with the ADA or ADAAG, unless this is not in the best interest of the client
Portable – Considered for rental property only
Permanent
Vertical lift – May be considered in lieu of a ramp if there is photographic and written
documentation that shows it is not possible for a ramp to be used
• Stair lift – If required for access to areas of the home necessary to meet the direct medical or
remedial benefit of the individual per service plan.
• Single-room air conditioners/single-room air purifiers – If required for access to areas of the home
necessary to meet the direct medical or remedial benefit of the individual per service plan:
There is a documented medical reason for the individual’s need to maintain a constant external
temperature. The documentation necessary for this equipment includes a prescription from the
primary care physician.
The room air conditioner size is consistent with the room size (square feet) capacity to be
cooled.
• Widen doorway − To allow safe egress:
Exterior − Modification limited to one per individual primary residence when no other
accessible door exists.
Interior − Modification of bedroom, bathroom, or kitchen door or doorway as needed to allow
for access. (A pocket door may be appropriate when there is insufficient room to allow for the
door swing.)
• Windows − Replacement of glass with Plexiglas
®
or other shatterproof material when there is a
documented medical/behavioral reason.
• Upon the completion of the modification, painting, wall coverings, doors, trim, flooring, and so
forth will be matched (to the degree possible) to the previous color/style/design.
• Maintenance − Limited to $500 annually for the repair and service of environmental modifications
that have been provided through an HCBS waiver:
Requests for service must detail parts cost and labor cost.
If the need for maintenance exceeds $500, the case manager will work with other available
funding streams and community agencies to fulfill the need. If service costs exceed the annual
limit, those parts and labor costs funded through the waiver must be itemized clearly to
differentiate the waiver service provision from those parts and labor funded through a non-
waiver funding source.
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-23
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Items requested that are not listed above must be reviewed and decision rendered by the State
division director or State agency designee.
Service Standards
• Environmental modification must be of direct medical or remedial benefit to the individual.
• Environmental modifications must meet applicable standards of manufacture, design, and
installation and should be guided by ADA or ADAAG requirements when in the best interest of the
individual and his or her specific situation.
• Environmental modifications must be compliant with applicable building codes.
Documentation Standards
• The identified direct benefit or need must be documented within a:
Service plan
Physician prescription and/or clinical evaluation, as deemed appropriate
• Documentation/explanation of the service within the Request for Approval to Authorize Services
(RFA) including the following:
Property owner of the residence where the requested modification is proposed
Property owner’s relationship to the individual
What, if any, relationship the property owner has to the waiver program
Length of time the individual has lived at this residence
If a rental property, length of lease
Written agreement of landlord for modification
Verification of individual’s intent to remain in the setting
Land survey may be required when exterior modifications approach property line
• Signed and approved RFA
• Signed and approved service plan
• Provider of services required to maintain receipts for all incurred expenses related to the
modification
• Must be in compliance with FSSA- and division-specific guidelines and policies
Limitations
A lifetime cap of $15,000 is available for environmental modifications. The cap represents a cost for
basic modification of an individual’s home for accessibility and safety, and accommodates the
individual’s needs for housing modifications. The cost of an environmental modification includes all
materials, equipment, labor, and permits to complete the project. No parts of an environmental
modification may be billed separately as part of any other service category (for example, specialized
medical equipment). In addition to the $15,000 lifetime cap, $500 is allowable annually for the repair,
replacement, or an adjustment to an existing environmental modification that was funded by an HCBS
waiver.
Activities Not Allowed
Examples and descriptions of activities not allowed include, but are not limited to the following:
• Adaptations or improvements that are not of direct medical or remedial benefit to the individual:
Central heating and air conditioning
Routine home maintenance
ARCHIVED

Section 7: Service Definitions
I-7-24 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Installation of standard (non-ADA, non-ADAAG) home fixtures (such as sinks, commodes,
tub, wall, window and door coverings, and so forth) that replace existing standard (non-ADA,
non-ADAAG) home fixtures
Roof repair
Structural repair
Garage doors
Elevators
Ceiling track lift systems
Driveways, decks, patios, sidewalks, or household furnishings
Replacement of carpeting and other floor coverings
Storage (such as cabinets, shelving, or closets), sheds
Swimming pools, spas, or hot tubs
Video monitoring system
Adaptive switches or buttons to control devices intended for entertainment, employment, or
education
Home-security systems
• Modifications that create living space or facilities where they did not previously exist (such as
installation of a bathroom in a garage or basement, and so forth).
• Modifications that duplicate existing accessibility (such as a second accessible bathroom, a second
means of egress from home, and so forth).
• Modifications that will add square footage to the home.
• Individuals living in foster homes, group homes, assisted living facilities, or homes for special
services (any licensed residential facility) are not eligible to receive this service.
Note: The responsibility for environmental modifications rests with the facility
owner or operator.
• Individuals living in a provider-owned residence are not eligible to receive this service
Note: The responsibility for environmental modifications rests with the facility
owner or operator.
• Completion of, or modifications to, new construction, or significant remodeling or reconstruction
are excluded unless there is documented evidence of a significant change in the individual’s
medical or remedial needs that now require the requested modification.
• Services to participants receiving adult family care.
• Services to participants receiving assisted living.
• Environmental modification services will not be reimbursed when provided as an individual
provider by a minor child participant, the spouse of a participant, the attorney-in-fact (POA) of a
participant, the healthcare representative (HCR) of a participant, or the legal guardian of a
participant.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-25
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.8 – Provider Qualifications Table for Environmental Modifications
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
Approved
Environmental
Modification
Individual
Any applicable
licensure must be
in place
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes/ permits.
A&D,
TBI
FSSA/DA-
Approved
Environmental
Modification
Agency/
Contractor
Any applicable
licensure
IC 25-20.2 Home
inspector
IC 25-28.5
Plumber
Evaluator
IC 25-23.5
Certification
IC 25-4 Architect
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and permits
A&D,
TBI
Plumber
IC 25-28.5
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and permits
A&D,
TBI
Architect
IC 25-4
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and permits
ARCHIVED
Section 7: Service Definitions
I-7-26 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Environmental Modification Assessment
Service Definition
Environmental modification assessment services will be used to objectively determine the
specifications for an environmental modification that is safe, appropriate, and feasible in order to
ensure accurate bids and workmanship.
The environmental modification assessment will assess the home for minor physical adaptations,
which as indicated by individual’s service plan, are necessary to ensure the health, welfare, and safety
of the individual enable the individual to function with greater independence in the home and without
which the individual would require institutionalization.
The assessor will be responsible for writing the specifications, reviewing of feasibility, and the post-
project inspection. Upon completion of the specifications and review of feasibility, the assessor will
prepare and submit the project specifications to the case manager and individual for the bidding
process and will be paid the first installment of $300 for completing of home specifications. After the
project is complete, the assessor, consumer, and case manager will then inspect the work and sign off,
indicating that it was completed per the agreed--upon bid and be paid the final installment of $200.
This payment is not included in the actual environmental modification cost category and shall not be
subtracted from the participant’s lifetime cap of $15,000. The case management provider entity will be
is responsible for maintaining related records that can be accessed by the State.
Allowable Activities
• Evaluation of the current environment, including the identification of barriers that may prevent the
completion of desired modifications
• Reimbursement for nonfeasible assessments
• Review of participant’s plan of care
• Drafting of specifications: electrical, plumbing, and interior framing
• Preparation and submission of specifications
• Post-project inspection/approval
Service Standards
• Need for environmental modification must be indicated in the participant’s plan of care
• Modification must address the participant’s level of service needs
• Proposed specifications for modification must conform to the requirements and limitations of the
current approved service definition for environmental modification services
• Assessment should be conducted by an approved, qualified individual who is independent of the
entity providing the environmental modifications
Limitations
An annual cap of $500 is available for environmental modification assessment services.
Activities Not Allowed
• Environmental modification assessment services will not be reimbursed when provided as an
individual provider by a parent of a minor child participant, the spouse of a participant, the
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-27
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
attorney-in-fact (POA) of a participant, the healthcare representative (HCR) of a participant, or the
legal guardian of a participant.
• Payment will not be made for environmental modifications under this service.
• Payment will not be made for an environmental modification assessment for the maintenance,
repair, or service of an existing environmental modification that was funded by a Home and
Community-Based Services (HCBS) waiver.
Provider Qualifications
Table 7.9 – Provider Qualifications Table for Environmental Modification Assessor
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
FSSA/DA-
Approved
Environmental
Modification
Assessment
Individual
License: IC 25-
20.2 Home
Inspector
OR:
Certified
Aging-In-Place
Specialist
(CAPS
Certification –
National
Association of
Home Builders)
OR:
Executive
Certificate in
Home
Modifications
(University of
Southern
California)
AND:
Verification
required every
three years
DA Approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of
qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and
permits
A&D
Architect
License:
IC 23-4
AND
Frequency of
verification up
to every three
years
DA Approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of
qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and
permits
ARCHIVED
Section 7: Service Definitions
I-7-28 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Healthcare Coordination
Service Definition
Healthcare coordination includes medical coordination provided by a registered nurse (RN) to manage
the healthcare of the individual including physician consults, medication ordering, and development
and nursing oversight of a healthcare support plan. Skilled nursing services are provided within the
scope of the Indiana State Nurse Practice Act. The purpose of healthcare coordination is stabilization,
delay/prevent deterioration of health status, management of chronic conditions, and/or improved health
status. Health Care Coordination is open to any waiver participant whose needs demonstrate the need
for such level of service without duplicating other formal and informal supports.
Because of the different benefits provided under Skilled Nursing and Health Care Coordination,
Medicaid prior authorization for skilled nursing services is not necessary prior to the provision of
healthcare coordination.
The appropriate level of healthcare coordination service should be determined by a healthcare
professional (RN or doctor).
Allowable Activities
• Physician consultations
• Medication ordering
• Development and oversight of a healthcare support plan
Service Standards
• Weekly consultations or reviews
• Face-to-face visits with the individual
• Other activities, as appropriate
• Services must address needs identified in the service plan
• The provider of home healthcare coordination to provide a written report to pertinent parties at least
quarterly
Pertinent parties include the individual, guardian, waiver case manager, all service providers,
and other entities.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Current Indiana RN license for each nurse
• Evidence of a consultation, including complete date and signature; consultation can be with the
individual, other staff, or other professionals, as well as healthcare professionals
• Evidence of a face-to-face visit with the individual, including complete date and signature
Limitations
Healthcare coordination services will not duplicate services provided under the Medicaid State Plan or
any other waiver service.
Healthcare coordination services are:
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-29
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• A minimum of one face-to-face visit per month
• Not to exceed eight hours of healthcare coordination per month
Activities Not Allowed
• Skilled nursing services that are available under the Medicaid State Plan
• Services to participants receiving assisted living waiver service
• Any other service otherwise provided by the waiver
Provider Qualifications
Table 7.10 – Provider Qualifications Table for Health Care Coordination
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1 Home
Health Agency
IC 25-23-1 RN
DA approved
ARCHIVED
Section 7: Service Definitions
I-7-30 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Home-Delivered Meals
Service Definition
A home-delivered meal is a nutritionally balanced meal. This service is essential in preventing
institutionalization because the absence of proper nutrition in individuals with frail and disabling
conditions presents a severe risk to health. No more than two meals per day will be reimbursed under
the waiver.
Allowable Activities
• Provision of meals
• Diet and nutrition counseling provided by a registered dietician
• Nutritional education
• Diet modification according to a physician’s order, as required, meeting the individual’s medical
and nutritional needs
Service Standards
• Home-delivered meals services must follow a written service plan addressing specific needs
determined by the individual’s assessment.
• Home-delivered meals will be provided to persons who are unable to prepare their own meals and
for whom there are no other persons available to do so; or where the provision of a home-delivered
meal is the most cost-effective method of delivering a nutritionally adequate meal, and it is not
otherwise available through other funding sources.
• All home-delivered meals provided must contain at least one-third of the current Recommended
Dietary Allowance (RDA), as established by the Food and Nutrition Board of the National
Academy of Sciences, National Research Council.
• All meals must meet state, local, and federal laws and regulations regarding the safe handling of
food. The provider must also hold adequate and current Servsafe Certification.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Date of service and units of service documented
Activities Not Allowed
• No more than two meals per day to be reimbursed under the waiver
• Services to participants receiving structured family caregiving waiver service
• Services to participants receiving adult family care waiver service
• Services to participants receiving assisted living waiver service
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-31
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.11 – Provider Qualifications Table for Home Delivered Meals
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
Approved
Home
Delivered
Meals Agency
Not required
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: General requirements
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Liability insurance
455 IAC 2 Maintenance of records of services provided
Must comply with all state and local health laws and
ordinances concerning preparation, handling, and serving
of food.
ARCHIVED
Section 7: Service Definitions
I-7-32 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Homemaker Services
Service Definition
Homemaker services offer direct and practical assistance consisting of household tasks and related
activities. Homemaker services assist the individual to remain in a clean, safe, and healthy home
environment. Homemaker services are provided when the individual is unable to meet these needs or
when an informal caregiver is unable to meet these needs for the individual.
Allowable Activities
• Provision of housekeeping tasks, which include:
Dusting and straightening furniture
Cleaning floors and rugs by wet or dry mop and vacuum sweeping
Cleaning the kitchen, including washing dishes, pots, and pans; cleaning the outside of
appliances and counters and cupboards; cleaning ovens and defrosting and cleaning
refrigerators
Maintaining a clean bathroom, including cleaning the tub, shower, sink, toilet bowl, and
medicine cabinet; emptying and cleaning the commode chair or urinal
Laundering clothes in the home or laundromat, including washing, drying, folding, putting
away, ironing, and basic mending and repair
Changing linen and making beds
Washing insides of windows
Removing trash from the home
Choosing appropriate procedures, equipment, and supplies; improvising when there are limited
supplies, keeping equipment clean and in its proper place
Clearing primary walk-ways
• Provision of assistance with meals or nutrition, which includes:
Shopping, including planning and putting food away
Making meals, including special diets under the supervision of a registered dietitian or health
professional
• Running the following essential errands:
Grocery shopping
Household supply shopping
Prescription pickup
• Provision of assistance with correspondence and bill-paying
Service Standards
Homemaker services must follow a written service plan addressing specific needs determined by the
client’s assessment.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-33
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Data record of services provided, including:
Complete date and time of service (in and out).
Specific services and tasks provided.
Signature of employee providing the service (minimally the last name and first initial). If the
person providing the service is required to be a professional, the title of the individual must
also be included.
• Each staff member providing direct care or supervision of care to the individual must make at least
one entry on each day of service. All entries should describe an issue or circumstance concerning
the individual.
• Documentation of service delivery is to be signed by the participant or designated participant
representative.
Activities Not Allowed
• Assistance with hands-on services such as eating, bathing, dressing, personal hygiene, and activities
of daily living.
• Escorting or transporting individuals to community activities or errands.
• Homemaker services provided to household members other than to the participant.
• Cleaning up of the yard, defined as lawn mowing, raking leaves.
• Homemaker services will not be reimbursed when provided as an individual provider by a parent of
a minor child participant, the spouse of a participant, the attorney-in-fact (POA) of a participant, the
healthcare representative (HCR) of a participant, or the legal guardian of the participant, or by any
member of the participant’s household.
• Services to participants receiving adult family care waiver service, structured family caregiving
waiver service, or assisted living waiver service.
Provider Qualifications
Table 7.12 – Provider Qualifications Table for Homemaker Services
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed
Personal
Services Agency
IC 16-27-4
DA approved
A&D,
TBI
FSSA/DA-
Approved
Homemaker
Individual
Not required
DA approved
455 IAC 2 Provider qualifications: becoming an
approved provider; maintaining approval
455 IAC 2 Provider qualifications: general
requirements
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements
455 IAC 2 Personnel records
Compliance with IC 16-27-4, if applicable.
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1
IC 16-27-4
DA approved
ARCHIVED

Section 7: Service Definitions
I-7-34 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Nutritional Supplements
Service Definition
Nutritional (dietary) supplements include liquid supplements, such as Boost
®
or Ensure
®
to maintain
an individual’s health in order to remain in the community.
Supplements should be ordered by a physician based on specific life stage, gender, or lifestyle.
Reimbursement for approved nutritional supplement expenditures is reimbursed through the local
AAA that maintains all applicable receipts and verifies the delivery of services. Providers can directly
relate to the State Medicaid Agency at their election.
Allowable Activities
Enteral Formulae, category 1, such as Boost or Ensure.
Service Standards
Nutritional supplement services must follow a written service plan addressing specific needs
determined by the individual’s assessment.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Documentation to support services rendered
Limitations
An annual cap of $1,200 is available for nutritional supplement services.
Activities Not Allowed
• Services available through the Medicaid State Plan (a Medicaid State Plan prior authorization
denial is required before reimbursement is available through the Medicaid waiver for this service)
• Services to participants receiving adult family care waiver service
• Services to participants receiving assisted living waiver service
Provider Qualifications
Table 7.13 – Provider Qualifications Table for Nutritional Supplements
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
Approved
Nutritional
Supplements
Agency
Not required
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Transfer of individual’s record upon change
of provider
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-35
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Waiver
Provider
Licensure/
Certification
Other Standard
455 IAC 2 Maintenance of records of services
provided
455 IAC 2 Liability insurance
455 IAC 2 Individual’s personal file; site of service
delivery
ARCHIVED
Section 7: Service Definitions
I-7-36 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Personal Emergency Response System
Service Definition
Personal emergency response system (PERS) is an electronic device that enables certain individuals at
high risk of institutionalization to secure help in an emergency. The individual may also wear a
portable help button to allow for mobility. The system is connected to the person’s telephone and
programmed to signal a response center once a “help” button is activated. The response center is
staffed 24 hours a day, seven days per week by trained professionals.
Allowable Activities
• PERS limited to those individuals who live alone or who are alone for significant parts of the day,
and have no regular caregiver for extended periods of time; and who would otherwise require
extensive supervision
• Device installation service
• Ongoing monthly maintenance of device
Service Standards
Personal emergency response services must follow a written service plan addressing specific needs
determined by the individual’s assessment.
Documentation Standards
• Identified needs in the service plan
• Services outlined in the service plan
• Documentation of expense for installation
• Documentation of monthly rental fee
Activities Not Allowed
• The replacement cost of lost or damaged equipment.
• Reimbursement is not available for PERS supports when the individual requires constant
supervision to maintain health and safety.
• Services to participants receiving adult family care waiver service, structured family care waiver
service, or assisted living waiver service.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-37
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.14 – Provider Qualifications Table for Personal Emergency Response System
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
Approved
Personal
Emergency
Response
System
Agency
Not required
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: General requirements
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements;
documentation of qualifications
455 IAC 2 Warranty required
Compliance with applicable building codes and permits
ARCHIVED
Section 7: Service Definitions
I-7-38 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Pest Control
Service Definition
Pest control services are designed to prevent, suppress, or eradicate anything that competes with
humans for food and water, injures humans, spreads disease to humans, or annoys humans, and is
causing or is expected to cause more harm than is reasonable to accept. Pests include insects such as
roaches, mosquitoes, and fleas; insect-like organisms, such as mites and ticks; and vertebrates, such as
rats and mice.
Services to control pests are services that prevent, suppress, or eradicate pest infestation.
Reimbursement for approved pest control expenditures is reimbursed through the local AAA who
maintains all applicable receipts and verifies the delivery of services. Providers can directly relate to
the State Medicaid agency at their election.
Allowable Activities
Pest control services are added to the service plan when the case manager determines through direct
observation or client report that a pest is present that is causing or is expected to cause more harm than
is reasonable to accept. Services to control pests are services that suppress or eradicate pest infestation.
Service Standards
Pest control services must follow a written service plan addressing specific needs determined by the
individual’s assessment.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Receipts of specific service, date of service, and cost of service completed
Limitations
An annual cap of $600 is available for pest control services.
Activities Not Allowed
• Pest control services may not be used solely as a preventative measure; there must be
documentation of a need for this service either through a care manager’s direct observation or
individual report that a pest is causing or is expected to cause more harm than is reasonable to
accept.
• Services to participants receiving adult family care waiver service.
• Services to participants receiving assisted living waiver service.
ARCHIVED
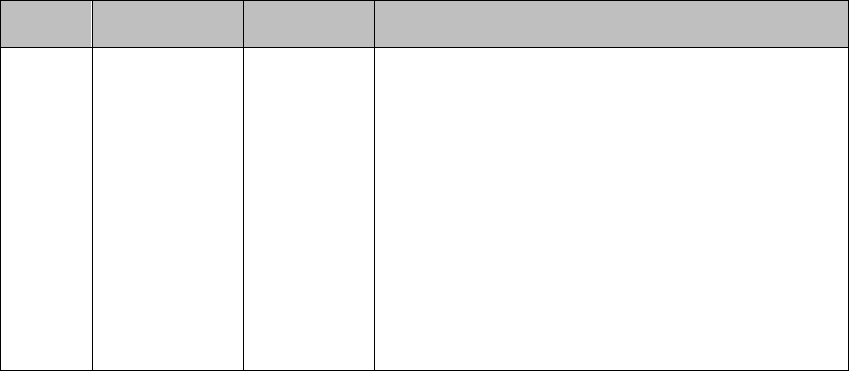
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-39
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.15 – Provider Qualifications Table for Pest Control
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA-
Approved Pest
Control Agency
IC 15-3-3.6
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: General
requirements
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements;
documentation of qualifications
455 IAC 2 Warranty required
Pesticide applicators must be certified or licensed
through the Purdue University Extension Service and
the Office of the Indiana State Chemist.
ARCHIVED
Section 7: Service Definitions
I-7-40 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Residential-Based Habilitation
Service Definition
Residential-based habilitation service provides training to regain skills that were lost secondary to the
traumatic brain injury (TBI).
Allowable Activities
Goal-oriented training and demonstration with:
• Skills related to activities of daily living:
Personal grooming
Bed making and household chores
Planning meals, the preparation of food
• Skills related to living in the community:
Using the telephone
Learning to prepare lists and maintaining calendars of essential activities and dates, and other
organizational activities to improve memory
Handling money and paying bills
Shopping and errands
Accessing public transportation
Service Standards
Residential-based habilitation services must follow a written service plan addressing specific
measurable goals and objectives to help with the acquisition, retention, or improvement of skills that
were lost secondary to the TBI.
Residential-based habilitation services must be monitored monthly.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• A data record of services provided, including:
Complete date and time of service (in and out)
Specific services/tasks provided
• Monthly documentation of progress toward identified goals
• Signature of employee providing the service (minimally the last name and first initial). If the person
providing the service is required to be a professional, the title of the individual must also be
included.
• Each staff member providing direct care or supervision of care to the individual must make at least
one entry on each day of service. All entries should describe an issue or circumstance concerning
the individual.
• Documentation of service delivery is to be signed by the participant or designated participant
representative.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-41
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Limitations
Services provided through residential-based habilitation service will not duplicate services provided
under the Medicaid State Plan or any other waiver service.
Activities Not Allowed
• Payments for residential-based habilitation are not made for room and board.
• Payment for residential-based habilitation does not include payments made directly or indirectly
when provided as an individual provider by a parent of a minor child participant, the spouse of a
participant, the attorney-in-fact (POA) of a participant, the healthcare representative (HCR) of a
participant, or the legal guardian of a participant.
• Payments will not be made for routine care and supervision.
• Residential-based habilitation services to participants receiving adult family care waiver service.
Provider Qualifications
Table 7.16 – Provider Qualifications Table for Residential Based Habilitation
Waiver
Provider
Licensure/
Certification
Other Standard
TBI
FSSA/DA-
Approved
Residential
Based
Habilitation
Agency
Not required
DA approved
455 IAC 2 Provider qualifications; general
requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements
455 IAC 2 Personnel records
Habilitation services must be performed by persons
who are supervised by a CBIS or Qualified Intellectual
Disability Professional; or a physical, occupational, or
speech therapist licensed by the state of Indiana who
have successfully completed training or have
experience in conducting habilitation programs.
ARCHIVED
Section 7: Service Definitions
I-7-42 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Respite Services
Service Definition
Respite services are services that are provided temporarily or periodically in the absence of the usual
caregiver. Service may be provided in the following locations:
• In an individual’s home
• In the private home of the caregiver
The level of professional care provided under respite services depends on the needs of the individual.
• An individual requiring assistance with the following:
Bathing
Meal preparation and planning
• Specialized feeding, such as an individual who:
Has difficulty swallowing
Refuses to eat
Does not eat enough
• Dressing or undressing
• Hair and oral care
• Weight-bearing transfer assistance should be considered for a respite home health aide under the
supervision of a registered nurse
• Individuals requiring infusion therapy; venipuncture; injection; wound care for surgical, decubitus;
incision; ostomy care; or tube feedings should be considered for respite nursing services
Allowable Activities
• Home health aide services
• Skilled nursing services
Service Standards
• Respite services must follow a written service plan addressing specific needs determined by the
individual’s assessment
• The level of care and type of respite will not exceed the requirements of the service plan; therefore,
skilled nursing services will only be provided when the needs of the individual warrant skilled care
• If an individual’s needs can be met with an LPN, but an RN provides the service, the service may
only be billed at the LPN rate.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Documentation must include the following elements:
Reason for the respite
Location where the service was rendered
Type of respite rendered
• Data record of staff to individual service, documenting the complete date and time in and time out,
and the number of units of service delivered that day. Each staff member providing direct care or
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-43
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
supervision of care to the individual makes at least one entry on each day of service describing an
issue or circumstance concerning the individual
• Documentation should include date and time, and at least the last name and first initial of the staff
person making the entry. If the person providing the service is required to be a professional, the title
of the individual must also be included. (Example: If a nurse is required to perform the service, the
RN title would be included with the name.) Any significant issues involving the individual
requiring intervention by a healthcare professional or case manager that involve the individual also
need to be documented
Activities Not Allowed
• Respite shall not be used as day/child care to allow the persons normally providing care to go to
work
• Respite shall not be used as day/child care to allow the persons normally providing care to attend
school
• Respite shall not be used to provide service to a participant while participant is attending school
• Respite may not be used to replace services that should be provided under the Medicaid State Plan
• Respite will not be reimbursed when provided as an individual provider by a parent of a minor child
participant, the spouse of a participant, the attorney-in-fact (POA) of a participant, the healthcare
representative (HCR) of a participant, or the legal guardian of a participant
• Respite must not duplicate any other service being provided under the participant’s POC
• Services to participants receiving adult family care waiver service
• Services to participants receiving assisted living waiver service
• Services to participants receiving structured family caregiving service
Provider Qualifications
Table 7.17 – Provider Qualifications Table for Respite
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1
DA approved
ARCHIVED
Section 7: Service Definitions
I-7-44 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Specialized Medical Equipment and Supplies
Service Definition
Specialized medical equipment and supplies are medically prescribed items required by the
individual’s service plan, which are necessary to assure the health, welfare, and safety of the
individual, which enable the individual to function with greater independence in the home, and without
which the individual would require institutionalization.
All specialized medical equipment and supplies must be approved by the waiver program prior to the
service being rendered.
• Individuals requesting authorization for this service through HCBS waivers must first exhaust
eligibility of the desired equipment or supplies through the Medicaid State Plan, which may require
prior authorization (PA).
There should be no duplication of services between HCBS waiver and Medicaid State Plan.
The refusal of a Medicaid vendor to accept the Medicaid reimbursement through the Medicaid
State Plan is not a justification for waiver purchase.
Preference for a specific brand name is not a medically necessary justification for waiver
purchase. The Medicaid State Plan often covers like equipment but may not cover the specific
brand requested. When this occurs, the individual is limited to the Medicaid State Plan covered
service or brand.
Reimbursement is limited to the Medicaid State Plan fee schedule, if the requested item is
covered under Medicaid State Plan.
All requests for items to be purchased through a Medicaid waiver must be accompanied by
documentation of Medicaid State Plan PA request and decision, if the requested item is
covered under the Medicaid State Plan.
• Specialized medical equipment and supplies shall be authorized only when it is determined to be
medically necessary and shall have direct medical or remedial benefit for the waiver individual.
This determination includes the following considerations:
The request is the most cost-effective or conservative means to meet the individual’s specific
needs.
The request is individualized, specific, and consistent with, but not in excess of, the
individual’s needs.
• Requests will be denied if the DA director or designee determines the documentation does not
support the service requested.
Allowable Activities
Justification and documentation is required to demonstrate that the request is necessary to meet the
individual’s identified needs:
• Communication devices − Computer adaptations for keyboard, picture boards, and so forth. The
Request for Approval (RFA) must be accompanied by documentation of a Medicaid State Plan PA
request and the decision rendered under the Medicaid State Plan.
• Generators (portable) − When ventilator, daily use of oxygen via a concentrator, continuous
infusion of nutrition (tube feeding), or medication through an electric pump are medical
requirements of the individual. The generator is limited to the kilo-wattage necessary to provide
power to the essential life-sustaining equipment, and is limited to one generator per individual per
ten-year period.
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-45
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Interpreter service − Provided in circumstances where the interpreter assists the individual in
communication during specified scheduled meetings for service planning (for example, waiver case
conferences and team meetings) and is not available to facilitate communication for other service
provision.
• Self-help devices − Including over-the-bed tables, reachers, adaptive plates, bowls, cups, drinking
glasses, and eating utensils that are prescribed by a physical therapist or occupational therapist.
• Strollers − When needed because the individual’s primary mobility device does not fit into the
individual’s vehicle/mode of transportation, or when the individual does not require the full-time
use of a mobility device, but a stroller is needed to meet the mobility needs of the individual outside
of the home setting. The RFA must be accompanied by documentation of a Medicaid State Plan PA
request and the decision rendered under the Medicaid State Plan.
• Manual wheelchairs − When required to facilitate safe mobility. The RFA must be accompanied by
documentation of a Medicaid State Plan PA request and the decision rendered under the Medicaid
State Plan.
• Maintenance − Limited to $500 annually for the repair and service of items that have been
provided through an HCBS waiver. Items that were previously purchased through the waiver, but
not listed in allowable activities, will continue to be maintained according to the definition.
Requests for service must detail parts and labor costs
If the need for maintenance exceeds $500, the case manager will work with other available
funding streams and community agencies to fulfill the need. If service costs exceed the annual
limit, those parts and labor costs funded through the waiver must be itemized clearly to
differentiate the waiver service provision from those parts and labor provided through a non-
waiver funding source.
• Posture chairs and feeding chairs − As prescribed by a physician, occupational therapist, or
physical therapist. The RFA must be accompanied by documentation of a Medicaid State Plan PA
request and the decision rendered under the Medicaid State Plan.
Service Standards
• Specialized medical equipment and supplies must be of direct medical or remedial benefit to the
individual.
• All items shall meet applicable standards of manufacture, design, and service specifications.
Documentation Standards
Documentation standards include the following:
• The identified direct benefit or need must be documented within:
Service plan
Physician prescription and clinical evaluation, as deemed appropriate
• Medicaid State Plan prior authorization request and the decision rendered, if applicable
• Signed and approved RFA to Authorize Services
• Signed and approved service plan
• Provider of services must maintain receipts for all incurred expenses related to this service
• Must be in compliance with FSSA- and division-specific guidelines and policies.
Limitations
Maintenance is limited to $500 annually for the repair and service of items that have been provided
through an HCBS waiver:
• Requests for service must detail parts and labor costs.
ARCHIVED
Section 7: Service Definitions
I-7-46 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• If the need for maintenance exceeds $500, the case manager works with other available funding
streams and community agencies to fulfill the need. If service costs exceed the annual limit, parts
and labor costs funded through the waiver must be itemized clearly to differentiate waiver service
from parts and labor provided through a non-waiver funding source.
Activities Not Allowed
The following items and equipment are not allowed under specialized medical equipment and supplies:
• Hospital beds
• Air fluidized suspension mattresses and beds
• Therapy mats
• Parallel bars
• Scales
• Activity streamers
• Paraffin machines or baths
• Therapy balls
• Books
• Games
• Toys
• Electronics such as CD players, radios, cassette players, tape recorders, television, VCR/DVDs,
cameras or film, videotapes, and other similar items
• Computers and software
• Adaptive switches and buttons
• Exercise equipment, such as treadmills or exercise bikes
• Furniture
• Appliances such as refrigerator, stove, hot-water heater
• Indoor and outdoor play equipment, such as swing sets, swings, slides, bicycles adaptive tricycles,
trampolines, playhouses, merry-go-rounds
• Swimming pools, spas, hot tubs, or portable whirlpool pumps
• Tempur-Pedic-type mattresses, positioning devices, pillows
• Bathtub lifts
• Motorized scooters
• Barrier creams, lotions, or personal cleaning cloths
• Totally enclosed cribs and barred enclosures for restraint purposes
• Vehicle modifications
• Any equipment or items that can be authorized through the Medicaid State Plan
Any equipment or items purchased or obtained by the individual, his or her family members, or
other non-waiver providers
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-47
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.18 – Provider Qualifications Table for Specialized Medical Equipment and Supplies
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1
DA approved
455 IAC 2 Warranty required
A&D,
TBI
FSSA/DA-
Approved
Specialized
Medical
Equipment and
Supplies Agency
IC 25-26-21
Certification
IC 6-2.5-8-1
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: general
requirements
455 IAC 2 Maintenance of records of services
provided
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements; documentation of qualifications
455 IAC 2 Warranty required
ARCHIVED

Section 7: Service Definitions
I-7-48 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Structured Day Program
Service Definition
Assistance with acquisition; retention; or improvement in self-help, socialization, and adaptive skills
that takes place in a nonresidential setting, separate from the home in which the individual resides.
Services shall normally be furnished four or more hours per day on a regularly scheduled basis, for one
or more days per week, unless provided as an adjunct to other day activities included in an individual’s
service plan.
Service Standards
• Structured day program services must follow a written service plan addressing specific needs
determined by the individual’s assessment.
• Structured day services shall focus on enabling the individual to attain or maintain his or her
functional level.
• Structured day program services may serve to reinforce skills or lessons taught in school, therapy,
or other settings.
Documentation Standards
• Identified need in the service plan
• Services outlined in the service plan
• Data record of services provided, including:
Complete date and time of service (in and out)
Specific services/tasks provided
Signature of the employee providing the service (minimally the last name and first initial). If
the person providing the service is required to be a professional, the title of the individual must
also be included.
• Each staff member providing direct care or supervision of care to the individual must make at least
one entry on each day of service. All entries should describe an issue or circumstance concerning
the individual.
Limitations
Note: Services provided through structured day program should not duplicate any
service provided under the Medicaid State Plan or other waiver service.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-49
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Provider Qualifications
Table 7.19 – Provider Qualifications Table for Structured Day Program
Waiver
Provider
Licensure/
Certification
Other Standard
TBI
FSSA/DA-
Approved
Structured Day
Program
Agency
Not required
DA approved
455 IAC 2 Provider Qualifications; General
requirements
455 IAC 2 General requirements for direct care
staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements
455 IAC 2 Personnel Records
Habilitation services must be performed by
persons who are supervised by a CBIS or
Qualified Intellectual Disability Professional or a
physical, occupational, or speech therapist
licensed by the state of Indiana and have
successfully completed training or have
experience in conducting habilitation programs.
ARCHIVED
Section 7: Service Definitions
I-7-50 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Structured Family Caregiving
Service Definition
Structured family caregiving (SFC) means a living arrangement in which a participant lives in their
private home or the private home of a principal caregiver who may be a nonfamily member or a family
member who is not the participant’s spouse, the parent of the participant who is a minor, or the legal
guardian of the participant.
Necessary support services are provided by the principal caregiver (family caregiver) as part of
structured family caregiving. Only agencies may be structured family caregiving providers, with the
structured family caregiving settings being approved, supervised, trained, and paid by the approved
agency provider. The provider agency must conduct two visits per month to the home – one by a
registered nurse and one by a structured family caregiving home manager. The provider agency must
keep electronic daily notes.
The goal of this service is to provide necessary care while emphasizing the participant’s independence.
The goal is reached through a cooperative relationship between the participant (or the participant’s
legal guardian), the participant’s HCBS Medicaid waiver case manager, and the structured family
caregiving provider. The participant’s needs shall be addressed in a manner that supports and enables
the individual to maximize abilities function at the highest level of independence possible. The service
is designed to provide options for alternative long-term care to persons who meet nursing facility level
of care and whose needs can be met in a SFC setting.
Another goal is to preserve the dignity, self-respect, and privacy of the participant by ensuring high-
quality care in a noninstitutional setting. Care is to be furnished in a way that fosters the independence
of each participant to facilitate aging in place in a home environment that provides the participant with
a range of care options as the needs of the participant change.
Allowable Activities
• Personal care and services.
• Homemaker or chore services.
• Attendant care and companion care services.
• Medication oversight (to the extent permitted under State law).
• Transportation for community activities that are therapeutic in nature or assist with maintaining
natural supports. (Medicaid State Plan transportation should be requested for medical
transportation.)
• Respite for the family caregiver. (Funding for this respite is included in the per diem paid to the
service provider; the actual service of respite care may not be billed in addition to the per diem.)
• Assistance with correspondence and bill paying, if requested by the participant.
• Other appropriate supports, as described in the individual’s service plan.
Service Standards
• Structured family caregiving must be reflected in the participant’s service plan
• Services must address the participant’s level of service needs
Documentation Standards
• Identified need in the service plan
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-51
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Services outlined in the service plan
• Requires completed Adult Family Care Level of Service Evaluation form. (The case manager must
give the completed Adult Family Care Level of Service Evaluation form to the provider.)
Activities Not Allowed
• Structured family caregiving service will not be reimbursed when provided as an individual
provider by a parent of a minor child participant, the spouse of a participant, the attorney-in-fact
(POA) of a participant, the healthcare representative (HCR) of a participant, or the legal guardian of
a participant.
• Personal care services provided to medically unstable or medically complex participants as a
substitute for care provided by a registered nurse, licensed practical nurse, licensed nurse, or other
health professional.
• Separate payment will not be made for homemaker, respite, transportation, personal emergency
response system, attendant care, assisted living, home-delivered meals, healthcare coordination, or
adult family care, as these activities are integral to and inherent in the provision of structured family
caregiving services.
Provider Qualifications
Table 7.20 – Provider Qualifications Table for Structured Family Caregiving
Waiver
Provider
Licensure/
Certification
Other Standard
A&D
FSSA/DA-
Approved
Structured
Family
Caregiving
Agency
Not required
Provider and home must meet the requirements of the Indiana
Adult Foster Care Service Provision and Certification
Standards.
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: general requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
455 IAC 2 Transfer of individual’s record upon change of
provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality improvement system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Transportation of an individual
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Individual’s personal file; site of service delivery
ARCHIVED
Section 7: Service Definitions
I-7-52 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-53
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Supported Employment
Service Definition
Supported employment services consist of paid employment for persons for whom competitive
employment at or above the minimum wage is unlikely, and who, because of their disabilities, need
intensive ongoing support to perform in a work setting. Supported employment is conducted in a
variety of settings, particularly worksites where persons without disabilities are employed. Supported
employment includes activities needed to sustain paid work by individuals receiving waiver services,
including supervision and training.
Service Standards
• Supported Employment services must follow a written service plan addressing specific needs
determined by the individual’s assessment.
• When Supported Employment services are provided at a worksite where persons without
disabilities are employed, payment will only be made for the adaptation, supervision and training
required by individuals receiving waiver services as a result of their disabilities and will not include
payment for supervisory activities rendered as a normal part of the business setting.
• Supported Employment services furnished under the waiver must be services which are not
available under a program funded by either the Rehabilitation Act of 1973 or P.L. 94-142.
Documentation will be maintained in the file of each individual receiving this service, showing that
the service is not otherwise available under a program funded under the Rehabilitation Act of 1973
or P.L. 94-142.
Documentation Standards
• Identified need in the service plan.
• Services outlined in the service plan.
• Data record of services provided, including:
Complete date and time of service (in and out).
Specific services /tasks provided.
Signature of employee providing the service (minimally the last name and first initial). If the
person providing the service is required to be a professional, the title of the individual must
also be included.
• Each staff member providing direct care or supervision of care to the individual must make at least
one entry on each day of service. All entries should describe an issue or circumstance concerning
the individual.
Limitations
When supported employment services are provided at a worksite where persons without disabilities are
employed, payment will only be made for the adaptation, supervision, and training required by
individuals receiving waiver services as a result of their disabilities.
Activities Not Allowed
• Services funded under the Rehabilitation Act of 1973 or P.L. 94-142
• Reimbursement for supervisory activities rendered as a normal part of standard business procedures
in a business setting where persons without disabilities are also employed
ARCHIVED

Section 7: Service Definitions
I-7-54 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Reimbursement for incentive payments, subsidies, or unrelated vocational training expenses for the
following:
Incentive payments made to an employer to encourage or subsidize the employer’s
participation in a supported employment program
Payments that are passed through to users of supported employment programs or
Payments for vocational training that are not directly related to an individual’s employment
program
Provider Qualifications
Table 7.21 – Provider Qualifications Table for Supported Employment
Waiver
Provider
Licensure/
Certification
Other Standard
TBI
FSSA/DA-
Approved
Supported
Employment
Agency
Certification
CARF
DA approved
455 IAC 2 Provider qualifications; general
requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements
455 IAC 2 Personnel records
TBI
Community
Mental
Health Center
Not required
DA approved
455 IAC 2 Provider qualifications; general
requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and
requirements
455 IAC 2 Personnel records
IC 12-7-2-38(1) Community Mental Health Center
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-55
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Transportation
Service Definition
Transportation services are services offered in order to enable individuals served under the waiver to
gain access to waiver and other community services, activities, and resources, specified by the service
plan.
Service Standards
• Transportation services must follow a written service plan addressing specific needs determined by
the individual’s assessment.
• This service is offered in addition to medical transportation required under 42 CFR 431.53 and
transportation services under the Medicaid State Plan, defined at 42 CFR 440.170(a) (if applicable),
and should not replace them.
• Whenever possible, family, neighbors, friends, or community agencies that can provide this service
without charge will be utilized.
Transportation services are reimbursed at three types of service:
• Level 1 transportation – The individual does not require mechanical assistance to transfer in and out
of the vehicle.
• Level 2 transportation – The individual requires mechanical assistance to transfer into and out of
the vehicle.
• Adult day service transportation – The individual requires round-trip transportation to access adult
day services.
Documentation Standards
• Identified need in the service plan.
• Services outlined in the service plan.
• A provider or its agent shall maintain documentation that the provider meets and maintains the
requirements for providing services under 460 IAC 1.2.
Limitations
Services provided under transportation service will not duplicate services provided under the Medicaid
State Plan or any other waiver service.
Activities Not Allowed
• May not be used to meet medical transportation needs already available under the Medicaid State
Plan.
• Separate waiver transportation services are not available to participants receiving adult family care
services.
• Services to participants receiving assisted living waiver service.
ARCHIVED

Section 7: Service Definitions
I-7-56 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Provider Qualifications
Table 7.22 – Provider Qualifications Table for Transportation
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
Licensed Home
Health Agency
IC 16-27-1
DA approved
Compliance with applicable vehicle/driver licensure
for vehicle being utilized
A&D,
TBI
FSSA/DA-
Approved
Transportation
Agency
Not required
DA approved
455 IAC 2 Becoming an approved provider;
maintaining approval
455 IAC 2 Provider qualifications: general
requirements
455 IAC 2 General requirements for direct care staff
455 IAC 2 Procedures for protecting individuals
455 IAC 2 Unusual occurrence; reporting
455 IAC 2 Transfer of individual’s record upon
change of provider
455 IAC 2 Notice of termination of services
455 IAC 2 Provider organizational chart
455 IAC 2 Collaboration and quality control
455 IAC 2 Data collection and reporting standards
455 IAC 2 Quality assurance and quality
improvement system
455 IAC 2 Financial information
455 IAC 2 Liability insurance
455 IAC 2 Transportation of an individual
455 IAC 2 Documentation of qualifications
455 IAC 2 Maintenance of personnel records
455 IAC 2 Adoption of personnel policies
455 IAC 2 Operations manual
455 IAC 2 Maintenance of records of services
provided
455 IAC 2 Individual’s personal file; site of service
delivery
Compliance with applicable vehicle/driver licensure
for vehicle being utilized
ARCHIVED
DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-57
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Vehicle Modifications
Service Definition
Vehicle modifications (VMOD) are the addition of adaptive equipment or structural changes to a
motor vehicle that permit an individual with a disability to safely transport in a motor vehicle. Vehicle
modifications, as specified in the service plan, may be authorized when necessary to increase an
individual’s ability to function in a home and community based setting and to ensure accessibility of
the individual with mobility impairments. These services must be necessary to prevent or delay
institutionalization. The necessity of such items must be documented in the service plan by a
physician’s order. Vehicles necessary for an individual to attend post-secondary education or job
related services should be referred to Vocational Rehabilitation Services.
The vehicle to be modified must meet all the following:
• The individual or primary caregiver is the titled owner.
• The vehicle is registered and/or licensed under state law.
• The vehicle has appropriate insurance as required by state law.
• The vehicle is the individual’s sole or primary means of transportation.
• The vehicle is not registered to or titled by a FSSA approved provider.
All vehicle modifications must be approved by the waiver program prior to services being rendered.
• Vehicle modification requests must meet and abide by the following:
The vehicle modification is based on, and designed to meet, the individual’s specific needs.
Only one vehicle per an individual’s household may be modified.
The vehicle is less than 10 years old and has less than 100,000 miles on the odometer.
If the vehicle is more than five years old, the individual must provide a signed statement from a
qualified mechanic verifying that the vehicle is in sound condition.
• All vehicle modification shall be authorized only when it is determined to be medically necessary
and/or shall have direct medical or remedial benefit for the waiver individual. This determination
includes the following considerations:
The modification is the most cost effective or conservative means to meet the individual’s
specific needs.
The modification is individualized, specific, and consistent with, but not in excess of, the
individual’s needs.
All bids must be itemized.
• Many automobile manufacturers offer a rebate of up to $1,000 for individuals purchasing a new
vehicle requiring modifications for accessibility. To obtain the rebate, the individual is required to
submit to the manufacturer documented expenditures of modifications. If the rebate is available, it
must be applied to the cost of the modifications.
• Requests for modifications may be denied if the DA director or designee determines the
documentation does not support the service requested.
Allowable Activities
Justification and documentation is required to demonstrate that the modification is necessary in order
to meet the individual’s identified needs. The following are allowed under vehicle modifications:
• Wheelchair lifts;
ARCHIVED
Section 7: Service Definitions
I-7-58 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
• Wheelchair tie-downs (if not included with lift);
• Wheelchair/scooter hoist;
• Wheelchair/scooter carrier for roof or back of vehicle;
• Raised roof and raised door openings;
• Power transfer seat base (excludes mobility base);
• Maintenance is limited to $500 annually for repair and service of items that have been funded
through an HCBS waiver:
Requests for service must differentiate between parts and labor costs.
If the need for maintenance exceeds $500, the case manager will work with other available
funding streams and community agencies to fulfill the need. If service costs exceed the annual
limit, those parts and labor costs funded through the waiver must be itemized clearly to
differentiate the waiver service provision from those parts and labor provided through a non-
waiver funding source.
• Items requested that are not previously listed must be reviewed and decision rendered by the State
division director or State agency designee.
Service Standards
• Vehicle modification must be of direct medical or remedial benefit to the individual
• All items must meet applicable manufacturer, design, and service standards
Documentation Standards
• The identified direct benefit or need must be documented within:
Service plan
Physician prescription and/or clinical evaluation as deemed appropriate
• Documentation/explanation of service within the RFA to authorize services must include:
Ownership of vehicle to be modified
Vehicle owner's relationship to the individual
Make, model, mileage, and year of vehicle to be modified
• Signed and approved RFA
• Signed and approved service plan
• Provider of services must maintain receipts for all incurred expenses related to the modification
• Must be in compliance with FSSA- and division-specific guidelines and/or policies
Limitations
A lifetime cap of $15,000 is available for vehicle modifications. In addition to the applicable lifetime
cap, $5,000 will be allowable annually for repair, replacement, or an adjustment to an existing
modification that was funded by an HCBS waiver.
Activities Not Allowed
Examples or descriptions of modifications/items not covered include, but are not limited to, the
following:
• Lowered-floor van conversions
• Purchase, installation, or maintenance of CB radios, cellular phones, global positioning and tracking
devices, or other mobile communication devices
• Repair or replacement of modified equipment damaged or destroyed in an accident
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 7: Service Definitions
Library Reference Number: PRPR10013 7-59
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
• Alarm systems
• Auto loan payments
• Insurance coverage
• Driver’s license, title registration, or license plates
• Emergency road service
• Routine maintenance and repairs related to the vehicle itself
• Services to participants receiving adult family care waiver service
• Services to participants receiving assisted living waiver service
Provider Qualifications
Table 7.23 – Provider Qualifications Table for Vehicle Modifications
Waiver
Provider
Licensure/
Certification
Other Standard
A&D,
TBI
FSSA/DA
approved
Vehicle
Modification
Agency
Not required
DA approval based upon provider compliance with
455 IAC 2
DA approved
455 IAC 2 Becoming an approved provider; maintaining
approval
455 IAC 2 Provider qualifications: general requirements
455 IAC 2 Liability insurance
455 IAC 2 Professional qualifications and requirements;
documentation of qualifications
455 IAC 2 Maintenance of records of services provided
455 IAC 2 Warranty required
ARCHIVED
ARCHIVED
DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 I-8-1
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Section 8: Provider Help
INsite Communication Instructions
The following are the steps for the case manager to obtain communications from INsite:
1. From the main screen in INsite, click Release Notes.
2. Click Manuals > Bulletins > Procedures.
3. Choose the manual to view, look at the entire table of contents (double-click on the manual title),
index, or perform a search.
4. Contact the INsite Helpdesk at [email protected].gov if additional assistance is needed.
Helpful Websites
Consult the following websites for more information:
• www.in.gov/fssa – Find information by type of person in need: children, seniors, families,
developmentally disabled (DD), and so forth. All programs and services available are listed on this
site.
• www.in.gov/fssa/2329.htm – Find information and resources about the Division of Aging (DA)
programs and services.
• www.in.gov/fssa/da/4743.htm – Find information about how to become a provider of DA services.
• https://ddrsprovider.fssa.in.gov/IFUR – Submit initial incident reports and case manager follow-up
reports for waiver and Money Follows the Person (MFP) services.
• www.indianamedicaid.com – Find IHCP provider bulletins and the IHCP Provider Manual.
Telephone contact information for providers is also available on this website.
Helpful Contact Numbers
Contact the Division of Aging at 1-888-673-0002. See Figure 8.1 for information on local Area
Agency on Aging offices.
ARCHIVED

Section 8: Provider Help HCBS Waiver Program Provider Manual
I-8-2 Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
Figure 8.1: Location and contact information for local AAA offices
AREA 1
Northwest Indiana Community Action
Corporation
5240 Fountain Drive
Crown Point, IN 46307
219.794.1829 OR 800.826.7871
TTY: 888.814.7597
FAX: 219.794.1860
www.nwi-ca.com
AREA 2
REAL Services, Inc.
1151 S. Michigan Street
South Bend, IN 46601-3427
574.284.2644 OR 800.552.7928
FAX: 574.284.2642
www.realservicesinc.org
AREA 3
Aging & In-Home Services of
Northeast Indiana, Inc.
2927 Lake Avenue
Fort Wayne, IN 46805-5414
260.745.1200 OR 800.552.3662
FAX: 260.422.4916
www.agingihs.org
AREA 4
Area IV Agency on Aging &
Community Action Programs, Inc.
660 N. 36th Street
Lafayette, IN 47903-4727
765.447.7683 OR 800.382.7556
TDD: 765.447.3307
FAX: 765.447.6862
www.areaivagency.org
AREA 5
Area Five Agency on Aging &
Community Services, Inc.
1801 Smith Street, Suite 300
Logansport, IN 46947-1577
574.722.4451 OR 800.654.9421
FAX: 574.722.3447
www.areafive.com
AREA 6
LifeStream Services, Inc.
1701 Pilgrim Boulevard
Yorktown, IN 47396-0308
765.759.1121 OR 800.589.1121
TDD: 800.801.6606
FAX: 765.759.0060
www.lifestreaminc.org
AREA 7
Area 7 Agency on Aging and Disabled
West Central Indiana
Economic Development District, Inc.
1718 Wabash Avenue
Terre Haute, IN 47807
812.238.1561 OR 800.489.1561
TDD: 800.489.1561
FAX: 812.238.1564
www.westcentralin.com
16 Area Agencies
AREA 8
CICOA Aging & In-Home Solutions
4755 Kingsway Drive, Suite 200
Indianapolis, IN 46205-1560
317.254.5465 OR 800.432.2422
TDD: 317.254.5497
FAX: 317.254.5494
www.cicoa.org
AREA 9
Area 9 In-Home & Community Service Agency
520 South 9th Street
Richmond, IN 47374
765.966.1795 OR 800.458.9345
FAX: 765.962.1190
www.iue.edu/area9
AREA 10
Area 10 Agency on Aging
631 W. Edgewood Drive
Ellettsville, IN 47429
812.876.3383 OR 800.844.1010
FAX: 812.876.9922
www.area10agency.org
AREA 11
Thrive Alliance
1531 13th Street, Suite G900
Columbus, IN 47201
812.372.6918 OR 866.644.6407
FAX: 812.372.7864
www.thrive-alliance.org
AREA 12
LifeTime Resources, Inc.
13091 Benedict Drive
Dillsboro, IN 47018
812.432.6200 OR 800.742.5001
FAX: 812.432.3822
www.lifetime-resources.org
AREA 13
Generations
Vincennes University Statewide
Services
1019 N. 4th Street
Vincennes, IN 47591
812.888.5880 OR 800.742.9002
FAX: 812.888.4566
www.generationsnetwork.org
AREA 14
LifeSpan Resources, Inc.
33 State Street, Third Floor
New Albany, IN 47151-0995
812.948.8330 OR 888.948.8330
TTY: 812.542.6895
FAX: 812.948.0147
www.lsr14.org
AREA 15
Hoosier Uplands / Area 15 Agency
on Aging and Disability Services
521 West Main Street
Mitchell, IN 47446
812.849.4457 OR 800.333.2451
TDD: 800.743.3333
FAX: 812.849.4467
www.hoosieruplands.org
AREA 16
SWIRCA & More
16 W. Virginia Street
Evansville, IN 47737-3938
812.464.7800 OR 800.253.2188
FAX: 812.464.7843
www.swirca.org
To contact your local Area Agency toll-free, call 1-800-986-3505.
ARCHIVED

DA HCBS Waiver Program Provider Manual Section 8: Provider Help
Library Reference Number: PRPR10013 8-3
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Communications
General Information
The Indiana Health Coverage Programs (IHCP) publishes the following communications to providers
at indianamedicaid.com:
• IHCP provider bulletins
• IHCP banner pages (published each week)
Providers may also subscribe to the Email Notification Service at indianamedicaid.com. This service
sends emails to subscribers when new communications are posted on indianamedicaid.com.
ARCHIVED
ARCHIVED

DA HCBS Waiver Program Provider Manual
Library Reference Number: PRPR10013 I-8-i
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version: 3.0
Index
A
address and telephone changes .................. 1-2
adult day services ........................................ 7-1
adult family care .......................................... 7-4
Aged and Disabled waiver ........................... 5-1
Area Agencies on Aging ........................ 5-1, 8-2
assisted living .............................................. 7-8
attendant care ........................................... 7-10
B
banner pages ............................................... 8-3
behavior management .............................. 7-13
bulletins ....................................................... 8-3
C
case management .............................. 6-1, 7-15
certification ................................................. 1-3
claim voids and replacements ..................... 2-2
claims billing instructions ............................ 2-1
community transition ................................ 7-19
D
dietary supplements .................. See nutritional
supplements
E
eligibility ...................................................... 2-1
E-mail Notification Service .......................... 8-3
environmental modification assessment .. 7-26
environmental modifications .................... 7-21
H
healthcare coordination ............................ 7-28
Home and Community-Based Services waivers
................................................................. 1-1
home-delivered meals ............................... 7-30
homemaker services ................................. 7-32
I
IndianaAIM .................................................. 1-2
INsite ............................................. 1-2, 2-1, 8-1
L
level of care .......................................... 1-2, 5-1
LOC ......................................... See level of care
M
Medicaid Fraud Control Unit ....................... 4-1
Medicaid Management Information System 1-
2
MFCU.............. See Medical Fraud Control Unit
MMIS See Medicaid Management Information
System
N
NOA .................................. See Notice of Action
Notice of Action .......................................... 1-2
nutritional supplements ............................ 7-34
P
personal emergency response system ...... 7-36
pest control services ................................. 7-38
provider application process ....................... 1-3
provider database ....................................... 1-2
Provider Enrollment Application ................. 1-4
Provider Enrollment Update Form .............. 1-5
provider enrollment updates ...................... 1-5
Provider Licensure and Certification
Adult Day Service .................................... 7-3
Adult Family Care ........................... 7-6, 7-51
Assisted Living ......................................... 7-9
Attendant Care ...................................... 7-11
Behavior Management/Behavior Program
and Counseling .................................. 7-14
Case Management ................................ 7-16
Community Transition ........................... 7-20
Environmental Modification Assessor .. 7-27
Environmental Modifications ................ 7-25
Health Care Coordination...................... 7-29
Home Delivered Meals .......................... 7-31
Homemaker Services ............................ 7-33
Nutritional Supplements ....................... 7-34
Personal Emergency Response System . 7-37
Pest Control ........................................... 7-39
Residential Based Habilitation .............. 7-41
Respite .................................................. 7-43
Specialized Medical Equipment and
Supplies ............................................. 7-47
Structured Day Program ....................... 7-49
Supported Employment ........................ 7-54
Transportation ...................................... 7-56
Vehicle Modifications ............................ 7-59
provider selection profiles .......................... 1-2
ARCHIVED
HCBS Waiver Program Provider Manual Index
I-8-ii Library Reference Number: PRPR10013
Published: July 16, 2015
Policies and Procedures as of May 1, 2015
Version:3.0
R
residential-based habilitation ................... 7-40
respite services .......................................... 7-42
S
Section 1915(c) of the Social Security Act ... 1-1
specialized medical equipment and supplies 7-
44
structured family caregiving ...................... 7-50
supported employment............................. 7-53
T
telephone and address changes ................. 1-2
transportation services ............................. 7-55
Traumatic Brain Injury waiver ..................... 5-2
V
vehicle modifications ................................ 7-57
W
waiver audits ............................................... 4-1
ARCHIVED
