
American Rhinologic Society | american-rhinologic.org | PO Box 269, Oak Ridge, NJ 07438 | 973-545-2735
PROGRAM GUIDE
ARS 69th Annual Meeting
September 29-30, 2023 | Omni Nashville Hotel, Nashville, TN

The ARS Welcomes the
AAO-HNS Guest Countries
Canada, Dominican Republic,
India, United Arab Emirates
The ARS will again be featuring the Fall Film Fesstival
- a video seminar featuring the most educational,
unique and impressive videos of cases, complications
and challenges submitted by the membership.
The videos were reviewed by an appointed committee
and rated equally on rarity of pathology, technical
complexity, novelty of procedure, educational value,
and production quality. The top-rated videos (time-
permitting) will be showcased at the meeting with an
opportunity for the video editors to introduce each clip
and respond to questions from the audience.
FALL FILM FESSTIVAL
Friday, September 29, 2023
12:00 - 1:00 pm
Broadway Ballroom GHJK

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
3
WWW.AMERICAN-RHINOLOGIC.ORG
Presidential Welcome
Welcome to the 69th Annual Meeting of the American
Rhinologic Society in Nashville! Pete Batra, ARS
President-Elect and Program Chair, has formulated
a superb educational program that highlights new
rhinologic research, pathophysiology, innovations, patient
care and procedural methods, work-life integration, and
more.
A cornerstone of the ARS Annual Meeting is the David
W. Kennedy Lectureship. This year, Dr. Brent Senior
will be the honored Kennedy Lecturer – discussing his
extraordinary international work. The title of Dr. Senior’s
lecture is “Global Outreach in Rhinology: Lessons
Learned from a Quarter Century in Vietnam.”
The Hwang Family Lectureship was initiated in 2022,
SARAH WISE, MD, FARS
with a focus on mentorship. We are excited to have Dr. Donald Lanza as the second
Hwang Family Lecturer in 2023. Dr. Lanza has a long history of mentorship and teaching
in rhinology – we are excited to hear his perspective on this important topic.
The remainder of the 69th ARS Annual Meeting program is filled with top-rated basic
science and clinical research, as well as papers on chronic rhinosinusitis disease severity
and impact, sinus surgery and postoperative therapies, skull base surgery, and more.
Panels and targeted discussions will cover CRS endotypes and therapeutics, extramural
funding, artificial intelligence in rhinology, pediatric skull base surgery, office based
rhinologic surgery, and several other important topics. This meeting covers an incredible
range of rhinologic areas and should be an excellent educational experience all-around.
Thank you for allowing me to serve as ARS President this year. I look forward to seeing
everyone in Nashville.
Sarah K. Wise, MD, FARS
President, American Rhinologic Society

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
4
Welcome from the President Elect and
Program Chair
I am thrilled to welcome you to the 2023 American Rhinologic Society
Annual Meeting!
As the memories of the pandemic and virtual meetings slowly recede from our
memory, the ARS is thriving after hosting several successful in-person meetings.
We will gather this fall in the beautiful city of Nashville to share exciting educational
content and networking opportunities with our colleagues, trainees, and industry
partners.
PETE S. BATRA, MD, FARS
The meeting will take place on September 29-30,
2023 at the Omni Hotel Nashville. The meeting will
showcase the best in clinical and translational
science in the ARS and highlight the tremendous
expertise on various panels and targeted
conversations. The ARS Annual Meeting promises
not to disappoint!
Original, innovative research is a bedrock of the
foundation of the ARS. The program will highlight 67
abstracts for oral scientic presentation and well over
100 posters. These presentations will cover a myriad
of salient topics including CRS diagnosis and medical
therapies, sinus surgery, rhinosinusitis
pathophysiology, allergy and immunology, and skull
base surgery. Congratulations to the scientic teams
from across the globe for sharing their cutting-edge
research at this meeting. Many thanks to the
Abstract Review Committee for their diligence to
compile this high-quality scientic content.
We are extremely honored to have Professor Brent
Senior present the David W. Kennedy lecture this
year. He will share his vast experience in global
health work titled “Global Outreach in Rhinology:
Lessons Learned from a Quarter Century in Vietnam.”
I am equally honored to share that Dr. Donald Lanza
will deliver the 2nd Hwang Family Lecture titled “The
Meaningfulness of Paying it Forward: My 40-Year
Journey.”
The ARS Annual Meeting has 3 breakout rooms on
Saturday morning, which are designed to grab the
interest of meeting attendees across various aspects
of rhinology. Our ARS Women in Rhinology, Allergy
and Immunology, Skull Base and Orbital Surgery, and
Rhinology in Private Practice Sections have been
instrumental in planning educational sessions in
these breakout rooms. The panels will highlight
several thought-provoking topics across the specialty.
Key panels will discuss Maintaining Balance &
Achieving the Quadripartite Mission, Success in Early
Career Extramural Funding, CRS Endotypes,
Subtypes, and Therapeutics, Pediatric Skull Base
Surgery in the 21st Century, Postoperative Care in
Skull Base Surgery, Setting Up and Maximizing an
ASC for Success, and How to Build a Rhinology
Niche in a Comprehensive ENT Practice. The ARS
and AAOA will hold a joint panel on Saturday
afternoon titled “Oce-Based Procedures Update:
Common Procedures & Dicult Cases.” We will
leverage our strong global partnerships in an
International Collaborative Panel titled “Assessing
Septoplasty Outcomes: An International Perspective.”
Friday’s session will be followed by the President’s
Reception, which oers a great venue for networking
and camaraderie with colleagues. Additional learning
opportunities are available at the Saturday morning
Meet the Authors Poster Viewing and Breakfast, as
well as several industry-sponsored satellite symposia
occurring during breakfast and lunch hours
throughout the meeting. Finally, I am excited to
announce the DEI Luncheon on Saturday titled
“Importance of Diversity and Improving the Pipeline in
Medicine” that will feature Dr. Andre Churchwell, Vice
Chancellor of Outreach, Belonging, and Inclusion at
Vanderbilt University and Dr. James Hildreth,
President of Meharry Medical College. I am grateful
to Dr. Troy Woodard for his leadership in developing
this amazing panel.
I hope it is readily apparent this will be another busy
and informative meeting that is sure to engage
attendees and stimulate conversation not only in the
clinical aspects of rhinology and skull base surgery,
but also the practice of medicine in both the
academic and private practice realms. I want to
extend in advance my sincerest gratitude to our
speakers, planners, and attendees. We truly
appreciate your continued support and engagement
with the American Rhinologic Society. Have a great
meeting, everyone!
Pete S. Batra, MD, FARS
President-Elect/Program Chair
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
5

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
6
American Rhinologic Society Executives - 2023
Sarah Wise, MD, FARS
President
Emory University
550 Peachtree Street
MOT 11th Floor
Atlanta, GA 30308
Tel: 404-778-3381
Fax: 404-686-4540
Email: skmille@emory.edu
Pete Batra, MD, FARS
President Elect
Rush University Medical Center
1611 W. Harrison Street, Suite 550
Chicago, IL 60612
Tel: 312-942-7182
Fax: 312-942-6653
Email: [email protected]
Rakesh Chandra, MD, FARS
Secretary
Vanderbilt University
Suite 7209, Medical Center E, South
Tower
Nashville, TN 37232
Tel: 708-689-0933
Email: [email protected]
Jivianne Lee, MD, FARS
Treasurer
UCLA Medical Center
1131 Wilshire Boulevard
Santa Monica, CA 90401
Tel: 424-259-6559
Email: [email protected]
Kevin Welch, MD, FARS
First Vice President
Northwestern University
675 N. St Clair Street
Suite 15-200
Chicago, IL 60611
Tel: 312-695-3115
Email: [email protected]
Amber Luong, MD, PhD, FARS
Second Vice President
First Vice President
McGovern Medical School
part of UT Health
6431 Fannin, MSB 5.036
Houston, TX 77030
Tel: 713-500-5421
Email: amber[email protected]
Rodney Schlosser, MD, FARS
Immdiate Past President
Medical University of South Carolina
135 Rutledge Ave., MSC 250550
Suite 1130
Charleston, SC 29425
Tel: 843-792-7165
Fax: 843-792-0546
Email: [email protected]
Michael Stewart, MD, FARS
Executive Vice President
Weill Cornell Medical College
575 Lexington Avenue
New York, NY 10022
Tel: 646-962-4777
Fax: 646-962-0388
Email: [email protected]
Brent Senior, MD, FARS
VP Development & Strategic Initiatives
UNC School of Medicine
Physician’s Office Building, G-190
170 Manning Drive, CB#7070
Chapel Hill, NC 27599
Tel: 919-966-3344
Fax: 919-966-7941
Email: [email protected]
Wendi Perez
Executive Administrator
P.O. Box 269
Oak Ridge, NJ 07438
Phone: 973-545-2735
Fax: 973-545-2736 x6
Email: [email protected]
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
7
ARS Board of Directors
ARS Consultants to the Board
Seth Brown,MD,
FARS
Timothy Smith,
MD, FARS,
(Editor in Chief, IFAR)
Stephanie Joe,
MD, FARS
Thomas Higgins,
MD, FARS
Erin O'Brien,
MD, FARS
ARS Staff
Wendi Perez
Executive Administrator
Susan Arias
Development Liaison
Tammy Lorimer
Administrative Assistant/
Office Coordinator
Bradford Woodworth,
MD, FARS
Benjamin Bleier,
MD, FARS
Raj Sindwani,
MD, FARS
Greg Davis, MD,
FARS
David Gudis,
MD, FARS
Zachary Soler, MD,
FARS
Marilene Wang,
MD, FARS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
8
RHINOLOGISTS IN
PRIVATE PRACTICE
SECTION
Greg Davis, MD, FARS
ARS Committee Chairs
AUDIT
Justin Turner, MD,
FARS
BY-LAWS
Bradford Woodworth,
MD, FARS
CME
Kent Lam, MD, FARS
ETHICS
Gretchen Oakley, MD, FARS
INTERNATIONAL
COMMITTEE
Jivianne Lee, MD, FARS
PEDIATRIC
RHINOLOGY
David Gudis, MD, FARS
RESEARCH
Vijay Ramakrishnan, MD,
FARS
MENTORSHIP
Murugappan Ramanathan,
Jr., MD, FARS
EDUCATION
INNOVATION
Abtin Tabaee, MD, FARS
AWARDS
Jean Kim, MD, FARS
HISTORIAN
Michael Benninger, MD,
FARS
INFORMATION
TECHNOLOGY
Chirag Patel, MD, FARS
RESIDENT/FELLOWS
IN TRAINING
Nicholas Rowan, MD
LIVE & ANCILLARY
COURSES
Garret Choby, MD, FARS
ONLINE EDUCATION
Jose Mattos, MD
QUALITY IMPROVEMENT
Zachary Soler, MD, FARS
DIVERSITY & INCLUSION
Troy Woodard, MD, FARS
MEMBERSHIP
Daniel Beswick, MD, FARS
EDUCATION
COORDINATOR
Raj Sindwani, MD, FARS
NEWSLETTER
Jean Anderson Eloy,
MD, FARS
DEVELOPMENT
Brent Senior, MD, FARS
FELLOWSHIP
Stacey Gray, MD, FARS
ALLERGY IN RHINOLOGY
SECTION
Jean Kim, MD, FARS
MARKETING
Sanjeet Rangarajan, MD,
FARS
PATIENT ADVOCACY
J. Peter Manes, MD, FARS
SKULL BASE & ORBITAL
SURGERY SECTION
Kibwei McKinney, MD
WOMEN IN RHINOLOGY
SECTION
Stacey Gray, MD, FARS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
9
Pete Batra, MD, FARS
Program Chair
PROGRAM COMMITTEE
Program Committee
Rakesh Chandra, MD, FARS
Garret Choby, MD, FARS
Devyani Lal, MD, FARS
Kent Lam, MD, FARS
Michael Stewart, MD, FARS
Kevin Welch, MD, FARS
Sarah Wise, MD, FARS
Troy Woodard, MD, FARS
Program Abstract Reviewers
Benjamin Bleier, MD, FARS
Do Yeon Cho, MD
Mindy Rabinowitz, MD, FARS
Adam Deconde, MD
Kara Detwiller, MD, FARS
Angela Donaldson, MD, FARS
Carlos Ebert, MD, FARS
Matthew Geltzeiler, MD, FARS
David Gudis, MD, FARS
Jose Gurrola, MD
Ashleigh Halderman, MD, FARS
Elisa Illing, MD, FARS
Jean Kim, MD, FARS
Michael Kohanski, MD
Edward Kuan, MD, FARS
Stella Lee, MD
Victoria Lee, MD, FARS
Joshua Levy, MD, fARS
Patricia Loftus, MD, FARS
Nyall London, MD, FARS
Amber Luong, MD, PhD, FARS
R. Pete Manes, MD, FARS
Kibwei McKinney, MD
Caitlin McLean, MD
Pete Papagiannopoulos, MD
Zara Patel, MD, FARS
Katie Phillips, MD
Kenneth Rodriguez, MD
Lauren Roland, MD,
Bobby Tajudeen, MD, FARS
Charles Tong, MD, FARS
Elina Toskala, MD, FARS
Troy Woodard, MD, FARS
Carol Yan, MD
William Yao, MD, FARS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
10
ARS Mission Statement
The American Rhinologic Society’s mission is to serve, represent and advance the science and ethical
practice of rhinology. The Society promotes excellence in patient care, research and education in
Rhinology and Skull Base Disorders. The American Rhinologic Society is dedicated to providing
communication and fellowship to the members of the Rhinologic community through on-going medical
education, patient advocacy, and social programs. The ARS continuing medical education activities
serve to improve professional competence, performance, and promote research.
Business/ACCME
Continuing Education
Accreditation Statement
The American Rhinologic Society (ARS) is accredited by the Accreditation Council for Continuing
Medical Education to provide continuing medical education for physicians.
Credit Designation Statement
The ARS designates this live activity for a maximum of 10.50 AMA PRA Category 1 Credits
TM
.
Physicians should claim only the credit commensurate with the extent of their participation in the
activity.
How to Obtain Your CME Certificate
At the conclusion of the meeting, you will be provided with a post-meeting link to claim your CME.
Learning Objectives
Upon completion of this session, participants should be able to:
• Advance the performance of clinical providers in the diagnosis and management of rhinology
diseases, including improving procedural/operative skills and leadership/organizational skills
• Improve healthcare quality through research presentations and panel discussions that incorporate
current health and practice data
• Recognize that the rhinologic health of populations involve factors beyond clinical care, including
economic, social, and environmental factors; healthcare and payer systems; and health disparities

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
11
Download the
Cvent Events App
Now!
Scan this code with a QR
reader to easily download
the app.
QR Code
Goes Here
by
Search for “ARS 69
th
Annual” in the app

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
12
ARS 2023 FRIENDS IN RESEARCH DONORS
DIAMOND
Adam Folbe, MD, FARS
Michael Stewart, MD, FARS
PLATINUM
J. Noble Anderson, Jr. MD
Michael Armstrong, MD
Roy Casiano, MD, FARS
Greg Davis, MD, FARS
John Del Gaudio, MD, FARS
Charles Ebert, Jr., MD, FARS
Jeb Justice, MD, FARS
Robert Kern, MD, FARS
Donald Lanza, MD, FARS
R. Peter Manes, MD, FARS
James Palmer, MD, FARS
Douglas Reh, MD, FARS
Marc Rosen, MD, FARS
Mas Takashima, MD, FARS
Jonathan Ting, MD, FARS
Eugenia Vining, MD
Marilene Wang, MD, FARS
Sarah Wise, MD, FARS
GOLD
Omar G. Ahmed, MD, FARS
Nadeem Akbar, MD
Benjamin Bleier, MD, FARS
Do-Yeon Cho, MD
Noam Cohen, MD, FARS
Michael Cruz, MD, FARS
Subinoy Das, MD, FARS
Steven Davis, MD
Diag-Nose.I0
David Gudis, MD, FARS
Yusuf Gulleth, MD
Corinna Levine, MD, FARS
Raj Sindwani, MD, FARS
Stephanie Smith, MD
Luisam Tarrats, MD, FARS
Elina Toskala, MD, FARS
Rhoda Wynn, MD, FARS
SILVER
John Craig, MD
John Chris Davis, MD
Brennan Dodson, MD
Judd Fastenberg, MD
Yusuf Gulleth, MD
Wayne Hsueh, MD
Aria Jafari, MD
Stephanie Joe, MD, FA
Kent Lam, MD, FARS
Andrew Lane, MD, FARS
Donald Lanza, MD, FARS
Ryan Little, MD
Brian Lobo, MD, FARS
Chadi Makary, MD, FARS
Michael Marino, MD, FARS
Edward McCoul, MD, FARS
Robert Pettis, MD
Hassan Ramadan, MD, FARS
B. Todd Schaeer, MD
John Ulrich, DO
Andrew Victores, MD
BRONZE
Sanford Archer, MD, FARS
Richard Bailey, MD
Jay Chavda, MD
David Conley, MD, FARS
Thomas Edwards, MD
Meha Fox, MD
Rohit Garg, MD, FARS
Thomas Higgins, MD, FARS
Eric Holbrook, MD, FARS
Eyad Khabbaz, MD
Tran Locke, MD
Li-Xing Man, MD, FARS
Sonya Marcus, MD
Michael McGhee, MD
Daniel O’Brien, MD, FARS
Jonathan Overdevest, MD
Katie Phillips, MD
Nicholas Rowan, MD
John Schneider, MD
Kristine Smith, MD
Brian Song, MD
Jason Talmadge, MD
Michael Yim, MD, FARS
FRIEND
Dole Baker, MD
Martin Hopp, MD
Alissa Kanaan, MD
Ramy Mahmoud
Nora Perkins, MD
Katie Phillips, MD
Russell Reitz, MD
David Rosen, MD
Jessica Southwood, MD
Ron Swain, Jr., MD, FARS
Dennis Tang, MD, FARS
As of 9/17/23
Thank you to all donors who have helped get the 2021 Friends in Research Campaign o to a great start!
We thank you for your generosity! With the monies donated over the past few years the ARS has heen
able to continue the Friends in Research sponsored grant which is in addition to our traditional CORE
eorts! New this year the ARS is also oering a three-year, multi-site Con-sortium Grant.
With your support, we can continue to fund the studies that provide clinical insights valuable to the care
of our patients. This work not only advances the care of our patients through scientic innova-tion, but
also generates important data establishing the ecacy and cost eectiveness of our care. In the current
nancial landscape, this is equally important to ensure that our patients have access to the treatment
necessary to address their complaints. We thank you again for your help in this worthy endeavor!
Visit american-rhinologic.org and join us in our 2024 year campaign.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
13
1954 - 1955 Maurice H. Cottle, MD*
1955 - 1956 Ralph H. Riggs, MD*
1956 - 1957 Walter E. E. Loch, MD*
1958 - 1959 Kenneth H. Hinderer, MD*
1959 - 1960 Roland M. Loring, MD*
1960 - 1961 Ivan W. Philpott, MD*
1962 - 1963 Raymond I. Hilsinger, MD*
1963 - 1964 H. Ashton Thomas, MD*
1964 - 1965 Carl B. Sputh, MD
1966 - 1967 Walter J. Aagesen, MD*
1967 - 1968 Richard Hadley, MD*
1968 - 1969 Henry L. Williams, MD*
1970 - 1971 Charles A. Tucker, MD*
1971 - 1972 Pat A. Barelli, MD
1972 - 1973 Gerald F. Joseph, MD
1973 - 1974 Manuel R. Wexler, MD*
1974 - 1975 George H. Drumheiler, MD*
1975 - 1976 Joseph W. West, MD*
1976 - 1977 Albert Steiner, MD*
1977 - 1978 Anthony Failla, MD*
1978 - 1979 Clifford F. Lake, MD*
1979 - 1980 W. K. Locklin, MD
1981 - 1982 Eugene B. Kern, MD
1982 - 1983 Carlos G. Benavides, MD
1983 - 1984 Leon Neiman, MD
1984 - 1985 George C. Facer, MD
1985 - 1986 Larry E. Duberstein, MD
1986 - 1987 Glenn W. Drumheiler, DO
1987 - 1988 Alvin Katz, MD
1988 - 1989 Donald Leopold, MD, FARS
1990 - 1991 Pierre Arbour, MD
1991 - 1992 Fred Stucker, MD, FARS
1992 - 1993 David W. Kennedy, MD, FARS
1993 - 1994 Sanford R. Hoffman, MD
1994 - 1995 Richard J. Trevino, MD
1995 - 1996 Vijay K. Anand, MD
1996 - 1997 Dale H. Rice, MD
1997 - 1998 Michael S. Benninger, MD, FARS
1998 - 1999 William Panje, MD
1999 - 2000 Charles W. Gross, MD
2000 - 2001 Frederick A. Kuhn, MD
2001 - 2002 Paul Toffel, MD, FARS
2002 - 2003 Donald C. Lanza, MD, FARS
2003 - 2004 James A. Hadley, MD, FARS
2004 - 2005 Joseph B. Jacobs, MD, FARS
2005 - 2006 Michael J. Sillers, MD, FARS
2006 - 2007 Howard L. Levine, MD, FARS
2007 - 2008 Marvin P. Fried, MD, FARS
2008 - 2009 James Stankiewicz, MD, FARS
2009 - 2010 Stilianos Kountakis, MD, FARS
2010 - 2011 Brent A. Senior, MD, FARS
2011 - 2012 Michael Setzen, MD, FARS
2012 - 2013 Todd Kingdom, MD, FARS
2013 - 2014 Timothy L. Smith, MD, FARS
2014 - 2015 Roy Casiano, MD, FARS
2015 - 2016 Peter Hwang, MD, FARS
2016 - 2017 John DelGaudio, MD, FARS
2017 - 2018 Richard Orlandi, MD, FARS
2018 - 2019 James Palmer, MD, FARS
2019 - 2020 Robert Kern, MD, FARS
2020 - 2021 Joseph Han, MD, FARS
2021 - 2023 Rodney Schlosser, MD, FARS
*Deceased
Past Presidents
Past Secretaries
2019 - Present Rakesh Chandra, MD, FARS
2015 - 2019 Pete Batra, MD, FARS
2013 - 2015 James Palmer, MD, FARS
2009 - 2012 Peter Hwang, MD, FARS
2005 - 2008 Brent A. Senior, MD, FARS
1999 - 2005 Marvin P. Fried, MD, FARS
1995 - 1999 Frederick Stucker, MD, FARS
1990 - 1995 Frank Lucente, MD
1985 - 1990 George Facer, MD
1980 - 1985 Pat A. Barelli, MD
1975 - 1980 Glenn H. Drumhiller, MD
1970 - 1975 Ralph H. Riggs, MD

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
14
The American Rhinologic Society gratefully acknowledges the following
companies for their support of the 69th Annual Meeting
ARS 69th Annual Meeting Industry Supporters
AstraZeneca
Gold Sponsorship
GlaxoSmithKline
Medtronic
Sano & Regeneron
Silver Sponsorship
Medtronic
Grant Support
Medtronic
19th Annual David W. Kennedy Lectureship
Acclarent
2nd Annual Hwang Family Lectureship
KARL STORZ Endoscopy-America, Inc.
Diversity & Inclusion/Women in Rhinology/Mentorship/Residents & Fellows Combined Program
Stryker
Residents Course
Stryker
Residents Reception
Hemostasis Fiagon
Rhinologists in Private Practice Cocktail Reception
3NT Medical
Acclarent
Advanced RX Compounding
Pharmacy
Aerin Medical
Altus Biologics
AstraZeneca
Brainlab
GlaxoSmithKline
Hemostasis & Fiagon
KARL STORZ Endoscopy-America, Inc.
Lyra Therapeutics
Medical Center Specialty Pharmacy
Medtronic
Nasoneb
NeilMed Pharmaceuticals Inc.
Olympus America Inc.
Prosidio
Sano & Regeneron
Septum Solutions
Stryker
Xoran Technologies
Exhibitors
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
15
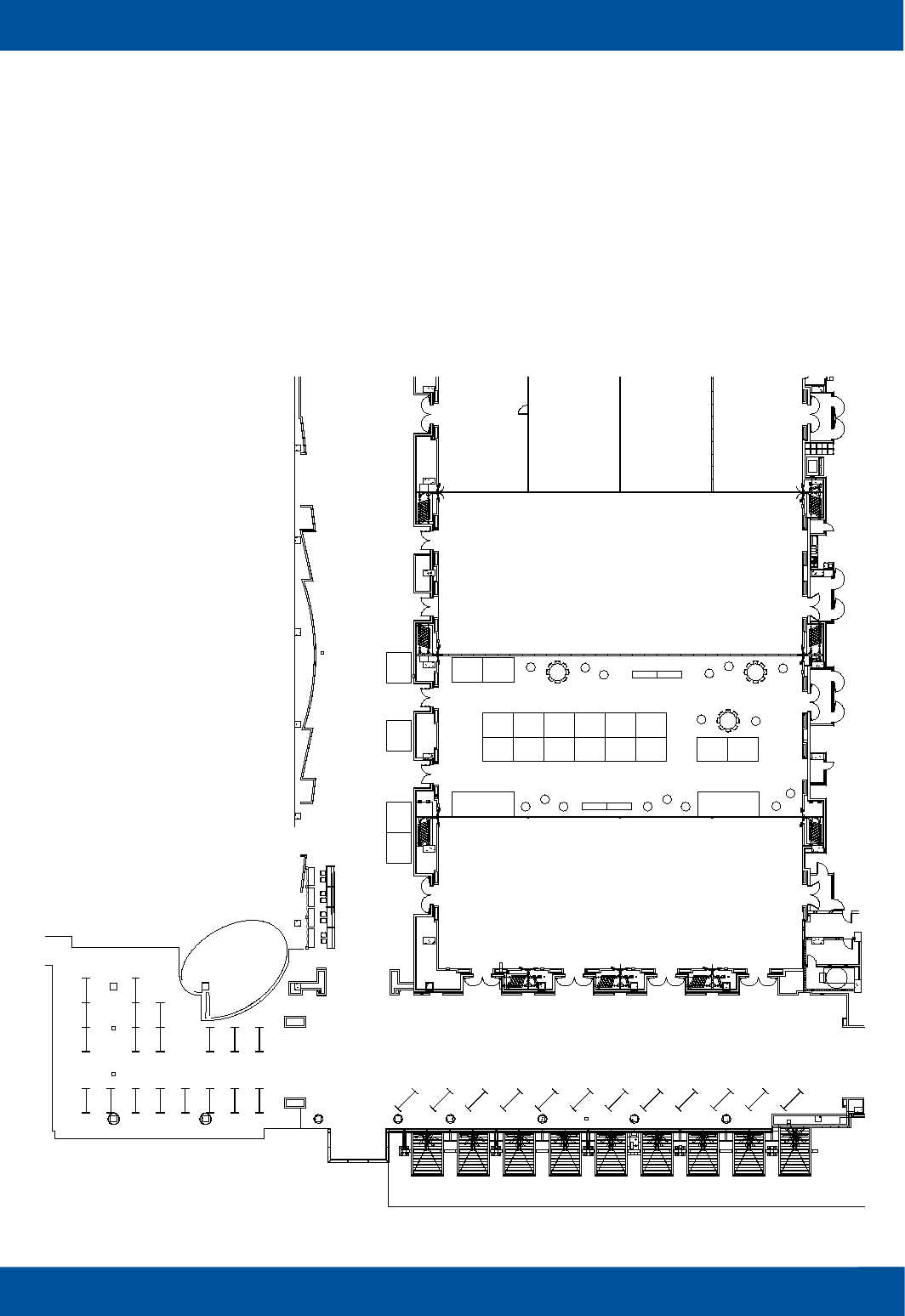
Floor Plan & Exhibit Hall
BROADWAY BALLROOM
A B
C
D
E
G - K
GENERAL SESSION
Broadway
BALLROOM
CIRCULATION
Food & Beverage
36"
36"
Food & Beverage
36"
36"
36" 36"
36"
36"
E
N
T
R
A
N
C
E
R
E
G
I
S
T
R
A
T
I
O
N
POSTER SESSION
101 103 105 107 109 111 115 117
201 203
204 206 208
S1
S2
S3
S4
Advanced RX
Compounding
Pharmacy
Aerin
Medical
100
Hemostasis Fiagon
Medical Center
Specialty
Pharmacy
Sanofi and
Regeneron
Medtronic
Acclarent
KARL STORZ
Endoscopy-
Stryker GSK
Lyra
Therapeutics
NeilMed
Pharmaceuticals
116
Olympus America Inc.
Septum
Solutions
BrainLabNasoneb
Altus
Biologics
3NT
Medical
Xoran
Tech
200 202
AstraZeneca
AIRSUPRA
AstraZeneca
PRECISION
66" / 8
66" / 8
36"
36"
66" / 8
36"
36"
36"
36"
36"
36"
POSTER SESSION
210
Prosidio
2023 ARS 69th Annual Meeting
September 29 - 30, 2023
Omni Nashville Hotel - Broadway Ballroom F - Nashville, TN

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
16
PROGRAM AT A GLANCE
Thursday,
September 28, 2023
Residents Didactic Course
Cumberland 1
12:00 pm – 5:00 pm
By Invitation Only
Residents Dissection Lab
Off Site Location
Details for Shuttle Service
forthcoming
12:00 pm – 5:00 pm
By Invitation Only
Residents Reception
Music Row 5
6:30 pm – 8:00 pm
By Invitation Only
Friday,
September 29, 2023
Residents Didactic Course
Cumberland 2
8:00 am – 12:00 pm
By Invitation Only
Residents Dissection Lab
Off Site Location
Details for Shuttle Service
forthcoming
8:00 am – 12:00 pm
By Invitation Only
Friday,
September 29, 2023
7:00 am – 12:00 pm
Broadway Ballroom ABC
7:00 am - 8:00 am
Board of Directors Breakfast
8:00 am - 12:00 pm
Board of Directors Meeting
Friday,
September 29, 2023
1:00 pm – 5:00 pm
General Session
Broadway Ballroom GHJK
12:00 pm - 1:00 pm
Fall Film FESStival
Broadway Ballroom GHJK
Moderators: Christopher Church, MD,
FARS;
Edward Kuan, MD, FARS
1:00 pm – 1:05 pm
Welcome & Introduction
Pete Batra, MD, FARS
1:05 pm – 1:20 pm
Presidential Address
Sarah Wise, MD, FARS
Top Rated Abstracts –
Clinical Rhinology
Moderators: Kara Detwiller, MD, FARS;
Devyani Lal, MD, FARS; Bobby
Tajudeen, MD, FARS
1:20 pm - 1:27 pm
Topical platelet-rich plasma for post-
COVID olfactory dysfunction – A
randomized controlled trial
Alexander Duffy, MD
1:28 pm – 1:35 pm
Efficacy and safety of EDS-FLU in
chronic rhinosinusitis – Two
randomized controlled trials
James Palmer, MD, FARS
1:36 pm – 1:43 pm
All CRS endotype clusters
demonstrate improvement in patient
reported and objective measures after
endoscopic sinus surgery
Nikita Chapurin, MD, MHS
1:44 pm – 1:51 pm
Peri-operative air quality and post-
operative endoscopic sinus surgery
outcomes
Amarbir Gill, MD
1:52 pm – 1:59 pm
Optimizing topical nasal
corticosteroid irrigations: A
randomized double-blind clinical trial
Zachary Root, BS
1:59 pm – 2:05 PM
Q&A
2:05 pm – 2:15 pm
Awards Ceremony
Jean Kim, MD, FARS
2:15 pm – 3:00 pm
David W. Kennedy Lecture
Introduction: Pete Batra, MD, FARS
Guest Speaker: Brent Senior, MD, FARS
“Global Outreach in Rhinology:
Lessons Learned from a Quarter
Century in Vietnam”
3:00 pm – 3:30 pm
Break with Exhibitors
Top Rated Abstracts – Basic
Science and Translational
Research
Moderators: Benjamin Bleier, MD, FARS:
Do-Yeon Cho, MD; Elina Toskala, MD,
FARS
3:30 pm – 3:37 pm
An eosinophil peroxidase activity
assay accurately predicts eosinophilic
chronic rhinosinusitis
Kristine Smith, MD

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
17
3:38 pm – 3:45 pm
Common cold viruses activate the
unfolded protein response in chronic
rhinosinusitis
Elizabeth Sell, Medical Student
3:46 pm – 3:53 pm
Timing of surgery on tissue IL-13
expression in CRSwNP patients on
dupilumab: A real-world study
Abdul Rahman Alenezi, MD
3:54 pm – 4:01 pm
Glutathione and bicarbonate
nanoparticles improve mucociliary
transport in cystic fibrosis epithelia
Nicholas Rivers, MD
4:02 pm – 4:09 pm
The effects of PM2.5 exposure on the
presentation of acute bacterial
rhinosinusitis
David Grimm, MS
4:09 pm – 4:15 pm
Q&A
4:15 pm – 5:00 pm
Panel: “Maintaining Balance &
Achieving the Quadripartite Mission”
Moderator: Nicholas Rowan, MD
Panelists: Stacey Gray, MD, FARS; Peter
Hwang, MD, FARS; Devyani Lal, MD,
FARS; Rodney Schlosser, MD, FARS;
Sarah Wise, MD, FARS
Sponsored by Residents and Fellows
Committee and Women in Rhinology
Section
5:30 pm – 7:00 pm
President’s Welcome Reception
Broadway Ballroom, 5th Avenue Pre-
Function
Saturday,
September 30, 2023
8:00 am – 12:00 pm
Breakout 1
Basic Science and Clinical
Rhinology
Broadway Ballroom JK
Session Chair: Erin O’Brien, MD,
FARS
7:00 am – 8:00 am
Meet the Authors Poster Viewing &
Breakfast
Room: Grand View Terrace Foyer,
Second Level
8:00 am – 8:35 am
Panel: “Success in Early Career
Extramural Funding”
Moderator: Murugappan Ramanathan,
MD, FARS
Panelists: Andrew Lane, MD, FARS;
Corinna Levine, MD, FARS; Timothy
Smith, MD, FARS; Carol Yan, MD
Sponsored by the Mentorship Committee
Scientific Oral Presentations:
Pathophysiology and
Mechanisms
Moderators: Lauren Roland, MD; Nicholas
Rowan, MD; Kristine Smith, MD
8:35 am – 8:40 am
Acetate and propionate metabolism by
Pseudomonas aeruginosa contributes
to significant sinus inflammation in a
rabbit model of sinusitis
Do-Yeon Cho, MD
8:41 am – 8:46 am
Identifying 5-hydroxymethylcytosine
profiles in cell free DNA from serum in
patients with aspirin exacerbated
respiratory disease
Tiffany Toni
8:47 am – 8:52 am
Increased Staphylococcus abundance
in the sinus microbiome is associated
with chronic rhinosinusitis treatment
resistance
David Hoying, BS
8:53 am – 8:58 am
Long non-coding RNAs related to
extracellular matrix and proteins are
differentially expressed in chronic
rhinosinusitis
Tripti Brar, MBBS, MD
8:59 am – 9:04 am
Comparison between upper and lower
airway microbiome in chronic
rhinosinusitis patients
Juan Carlos Hernaiz-Leonardo, MD, MSc
9:05 am – 9:15 am
Q&A
9:15 am – 9:45 am
Panel: Generative Artificial Intelligence
in Rhinology
Moderator: Chirag Patel, MD, FARS
Panelists: Martin Citardi, MD, FARS; Brian
Lobo, MD, FARS; Martin Desrosiers, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations:
CRS Impact and Disease
Severity
Moderators: Angela Donaldson, MD,
FARS; Amber Luong, MD, PhD, FARS;
Toby Steele, MD
10:15 am – 10:20 am
In vivo nasal micro-optical coherence
tomography imaging reveals
mucociliary dysfunction in chronic
rhinosinusitis
Kadambari Vijaykumar
10:21 am – 10:26 am
Multi-instance learning for eosinophil
quantification of sinonasal
histopathology images
Yi-Tsen Lin, MD, PhD
10:27 am – 10:32 am
Frailty is an independent predictor of
post-operative rescue medication use
after endoscopic sinus surgery
Andrea Lopez, BS
10:33 am – 10:38 am
Cognition and saccadic eye movement
performance are impaired in chronic
rhinosinusitis
David Cvancara, BS
PROGRAM AT A GLANCE

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
18
10:39 am – 10:45 am
Q&A
10:45 am – 10:50 am
Sleep dysfunction is greater in aspirin-
exacerbated respiratory disease than
in other forms of chronic rhinosinusitis
David Cvancara, BS
10:51 am – 10:56 am
Clinical characteristics and
comorbidities associated with non-
eosinophilic chronic rhinosinusitis
Tripti Brar, MBBS, MD
10:57 am – 11:02 am
Impact of chronic rhinosinusitis local
exacerbations on granulomatosis with
polyangiitis disease progression and
systemic exacerbations
Trisha Shang, BA
11:03 am – 11:08 am
Endotype evaluation of Hispanic/
Latinx-American patients with chronic
rhinosinusitis with polyps
Arthur Wu, MD, FARS
11:08 am – 11:15 am
Q&A
11:15 am – 12:00 pm
Panel: “CRS Endotypes, Subtypes,
and Therapeutics: Where are we and
where are we going?”
Moderator: Amber Luong, MD, PhD,
FARS
Panelists: Jeremiah Alt, MD, PhD, FARS;
Robert Kern, MD, FARS; Stella Lee, MD;
Justin Turner, MD, FARS
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Diversity & Inclusion, Women in
Rhinology, Mentorship, Residents &
Fellows Combined Lunch Program
Broadway Ballroom A
“Breaking Barriers: Insights on
Improving Diversity and the Pipeline in
Medicine”
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD;
Kimberly Vinson, MD
Saturday,
September 30, 2023
8:00 am – 12:00 pm
Breakout 2
Skull Base
Broadway Ballroom CD
Session Chair: Bobby Tajudeen,
MD, FARS
7:00 am – 8:00 am
Meet the Authors Poster Viewing &
Breakfast
Room: Grand View Terrace Foyer,
Second Level
8:00 am – 8:30 am
Panel: “Pediatric Skull Base Surgery in
the 21
st
Century: Advances and
Frontiers”
Moderator: David Gudis, MD, FARS
Panelists: Nithin Adappa, MD, FARS;
Garret Choby, MD, FARS; Zara Patel,
MD, FARS
Sponsored by Pediatric Rhinology
Committee
Scientific Oral Presentations:
Skull Base Surgery
Moderators: Mathew Geltzeiler, MD,
FARS; Nyall London, MD, FARS; Peter
Papagiannopoulos, MD
8:30 am – 8:35 am
Mutational landscape and predictors of
survival in head and neck mucosal
melanoma
Brandon Lehrich, BS
8:36 am – 8:41 am
Genomic and clinical analysis of
olfactory neuroblastoma
Theodore Nguyen, BS
8:42 am – 8:47 am
Genomic mutational analysis and
predictors of survival in
nasopharyngeal carcinoma
Benjamin Bitner, MD
8:48 am – 8:53 am
SNOT-22 subdomain outcomes in
sinonasal malignancy: A prospective
multi-center study
David Grimm, MS
8:53 am – 9:00 am
Q&A
9:00 am – 9:05 am
Tranexamic acid in endoscopic sinus
and skull base surgery: A systematic
review and meta-analysis
Sarah Khalife, MD
9:06 am – 9:11 am
The use of aprepitant to reduce
postoperative nausea and vomiting in
endoscopic skull base surgery
Daniel Lee, MD, FRCSC
9:12 am – 9:17 am
Predictors of prolonged length of stay
following intradural endoscopic skull
base surgery
Jonathan Pang, BA
9:18 am – 9:23 am
Quality of life among patients
undergoing endoscopic pituitary gland
resection with and without middle
turbinectomy
Narin N. Carmel Neiderman, MD, MSc
9:23 am – 9:30 am
Q&A
9:30 am – 9:45 am
Targeted Conversations on Important
Topics: Next Generation Sequencing in
Skull Base Surgery
Moderator: Sanjeet Rangarajan, MD,
FARS
Panelists: Corinna Levine, MD, FARS;
Peter Papagiannopoulos, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations:
Rhinology Potpourri
Moderators: Charles Ebert, MD, FARS;
Edward Kuan, MD, FARS; Charles Tong,
MD, FARS
10:15 am – 10:20 am
Stellate ganglion block for post-
COVID-19 parosmia: Does it work?
Bita Naimi, BA
PROGRAM AT A GLANCE

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
19
PROGRAM AT A GLANCE
10:21 am – 10:26 am
Stellate ganglion block for the
treatment of COVID-19-induced
olfactory dysfunction: A prospective
pilot study
Andrew Peterson, MD, MSCI
10:27 am – 10:32 am
Sinonasal pathogenic bacteria in
patients with diabetes mellitus
Trisha Shang, BA
10:33 am – 10:38 am
The role of CCL19 and atypical cytokine
receptor CCRL1 in chronic
rhinosinusitis
Chengetai Mahomva, MD
10:39 am – 10:45 am
Q&A
10:45 am – 10:50 am
Real-world comparison of nasal
obstruction outcome scores between
medial flap turbinoplasty and inferior
turbinate submucous resection during
concurrent septorhinoplasty
Milind Vasudev, BS
10:51 am – 10:56 am
Cadaveric and computed tomography
analysis of the arterial supply and
mucosal dimensions of the anterior
ethmoid artery flap
Lane Donaldson, MD
10:57 am – 11:02 am
Posterior nasal nerve ablation for
management of postnasal drip: A single
center case series
Daniel Gorelik, Research Fellow
11:03 am – 11:08 am
Insurance influence and reimbursement
on common rhinological procedures
Tyler Janz, MD
11:08 am – 11:15 am
Q&A
11:15 am – 12:00 pm
Panel: “Postoperative Care in Skull
Base Surgery: CPAP, Debridement,
Rinses and More!”
Moderator: Mathew Geltzeiler, MD, FARS
Panelists: Nyssa Farrell, MD; Edward
Kuan, MD, FARS; Mindy Rabinowitz, MD,
FARS; Bobby Tajudeen, MD, FARS
Sponsored by the Skull Base and Orbital
Surgery Section
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Diversity & Inclusion, Women in
Rhinology, Mentorship, Residents &
Fellows Combined Lunch Program
Broadway Ballroom A
“Breaking Barriers: Insights on
Improving Diversity and the Pipeline in
Medicine”
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD; Kimberly
Vinson, MD
Saturday,
September 30, 2023
8:00 am – 12:00 pm
Breakout 3
Business of Medicine/Clinical
Rhinology
Broadway Ballroom GH
Session Chair: Greg Davis, MD,
FARS
7:00 am – 8:00 am
Meet the Authors Poster Viewing &
Breakfast
Room: Grand View Terrace Foyer, Second
Level
8:00 am – 8:30 am
Panel: “Setting Up and Maximizing an
ASC for Success”
Moderator: Douglas Reh, MD, FARS
Panelists: Karen Bednarski, MD, FARS;
Leah Hauser, MD; Michael Sillers, MD,
FARS
Sponsored by Rhinologists in Private
Practice Section
Scientific Oral Presentations:
Sinus Surgery and Postop
Therapies
Moderators: Chadi Makary, MD, FARS;
Katie Phillips, MD; William Yao, MD,
FARS
8:30 am – 8:35 am
Outcomes and histopathologic features
for chronic rhinosinusitis macrolide
responders
Madelyn Frank, BA
8:36 am – 8:41 am
Outcomes of “full-house” versus
limited endoscopic sinus surgery for
chronic rhinosinusitis patients
Shreya Ramkumar, BS
8:42 am – 8:47 am
Factors impacting follow-up care in
allergic fungal rhinosinusitis
Jorge Gutierrez, BA
8:48 am – 8:53 am
Efficacy of early postoperative
debridement in sinonasal cavity healing
after functional endoscopic sinus
surgery: A randomized controlled trial
Juan Carlos Hernaiz-Leonardo, MD, MSc
8:53 am – 9:00 am
Q&A
9:00 am – 9:05 am
The effect of low-dose long-term
doxycycline on postoperative outcomes
in patients with eosinophilic chronic
rhinosinusitis
Jin Young Min, MD, PhD
9:05 am – 9:10 am
High dose ciprofloxacin and
azithromycin sinus stent for the
treatment of chronic rhinosinusitis
Do-Yeon Cho, MD
9:10 am – 9:15 am
Quantification of retained budesonide
dose from high-volume saline irrigation
in post-operative chronic rhinosinusitis
Paige Shipman, MS1
9:15 am – 9:20 am
Medication adherence with intranasal
corticosteroid irrigations
Jorge Gutierrez, BA

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
20
9:20 am - 9:25 am
Evaluation of LYR-220 corticosteroid
matrices at week 24 from the BEACON
study in CRS
Brent Senior, MD, FARS
9:25 am – 9:30 am
Q&A
9:30 am – 9:45 am
Targeted Conversations on Important
Topics: Correct Coding for Office-
Based Rhinologic Surgery - Do’s and
Don’ts
Moderator: R. Peter Manes, MD, FARS
Panelists: Seth Brown, MD, FARS; Toby
Steele, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations:
Diagnosis of Rhinosinusitis
and QOL Measures
Moderator: Jean Kim, MD, FARS; Victoria
Lee, MD, FARS;
Mindy Rabinowitz, MD, FARS
10:15 am – 10:20 am
Development and validation of the
sinonasal endoscopic score (SINES)
for chronic rhinosinusitis
Juan Carlos Hernaiz-Leonardo, MD, MSc
10:21 am – 10:26 am
Patient perspectives on recall period
and response options in patient-
reported outcome measures for
chronic rhinosinusitis
symptomatology: An international
multi-centered study
Ahmad Sedaghat, MD, PhD
10:27 am – 10:32 am
The surprising impact of priming on
the SNOT-22
Ibtisam Mohammad, MD
10:33 am – 10:38 am
Nasal symptoms, medication usage,
nasal endoscopy and patient
perspectives as determinants of
physician assessment of chronic
rhinosinusitis control
Ahmad Sedaghat, MD, PhD
10:39 am – 10:45 am
Q&A
10:45 am – 10:50 am
Variation in computed tomography
opacification in sinus disease: A
snapshot in time
Glen D’Souza, MD
10:51 am – 10:56 am
Determining the minimal clinically
important difference for the
questionnaire of olfactory disorders in
people with cystic fibrosis and factors
associated with improvement after
highly effective modulator therapy
Jessa Miller, MD
10:57 am – 11:02 am
Optimization of diagnostic and
procedural codes to identify patients
with acute invasive fungal sinusitis
Marie-Ange Munyemana, BA
11:03 am – 11:08 am
Impact of recurrent acute
rhinosinusitis on quality of life
Zayd Al-Asadi, MD
11:08 am – 11:15 am
Q&A
11:15 am – 12:00 pm
Panel: “How to Build a Rhinology
Clinical Niche in a Comprehensive
ENT Practice”
Moderator: Greg Davis, MD, FARS
Panelists: Mary Ashmead, MD; Michael
Cruz, MD, FARS; Christopher Davis, MD;
Michael Setzen, MD, FARS
Sponsored by Rhinologists in Private
Practice Section
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Diversity & Inclusion, Women in
Rhinology, Mentorship, Residents &
Fellows Combined Lunch Program
Broadway Ballroom A
“Breaking Barriers: Insights on
Improving Diversity and the Pipeline in
Medicine”
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD;
Kimberly Vinson, MD
Saturday,
September 30, 2023
1:00 pm – 5:00 pm
General Session
Broadway Ballroom GHJK
1:00 pm – 1:15 pm
ARS Business Meeting and
Presidential Citations
Sarah Wise, MD, FARS; Michael Stewart,
MD, FARS; Pete Batra, MD, FARS
1:15 pm – 2:00 pm
Hwang Family Lectureship
“The Meaningfulness of Paying It
Forward: My 40-Year Journey”
Introduction: Richard Orlandi, MD,
FARS
Guest Speaker: Donald Lanza, MD,
FARS
Scientific Oral Presentations:
Nasal Polyps and Biologics
Moderators: Elisa Illing, MD, FARS;
Kenneth Rodriguez, MD; Abtin Tabaee,
MD, FARS
2:00 pm – 2:05 pm
Medication use for chronic
rhinosinusitis with nasal polyps
(CRSwNP) pre and post dupilumab
Emily Garvey, BA
2:06 pm – 2:11 pm
Nasal nitric oxide to compare
endoscopic sinus surgery versus
dupilumab for CRSwNP
Daniel Lee, MD, FRCSC
2:12 pm – 2:17 pm
Quantifying patient preferences for
treating nasal polyps: Biologics vs.
surgery
Somtochi Okafor, MD
2:18 pm – 2:23 pm
Sinonasal symptom correlation with
the postoperative polyp scale (POPS)
Arthur Wu, MD, FARS
2:23 pm – 2:30 pm
Q&A
PROGRAM AT A GLANCE

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
21
PROGRAM AT A GLANCE
2:30 pm – 2:35 pm
Blood IgE and eosinophils are not
reliable predictors of nasal
inflammation
Andrew Thamboo, MD, MHSc
2:36 pm – 2:41 pm
Ocular surface adverse events
associated with dupilumab for
treatment of nasal polyps
Austin Swisher, BS
2:42 pm – 2:47 pm
Real world trial for weaning dupilumab
from every 2 to every 4 week
administration
Emily Garvey, BA
2:48 pm – 2:53 pm
Real-world adverse events after type 2
monoclonal antibody use in chronic
rhinosinusitis with nasal polyps
Marisa Dorling, BSc
2:53 pm – 3:00 pm
Q&A
3:00 pm – 3:30 pm
Break with Exhibitors
3:30 pm – 4:15 pm
Combined ARS/AAOA Panel: “Office-
Based Procedures Update: Common
Procedures & Difficult Cases”
Moderator: Jean Kim, MD, FARS
Panelists: Omar Ahmed, MD, FARS;
Charles Ebert, Jr., MD, FARS; Monica
Patadia, MD; Elina Toskala, MD, FARS
4:15 pm – 5:00 pm
International Collaborative Panel:
“Assessing Septoplasty Outcomes:
An International Perspective”
Moderator: Michael Stewart, MD, FARS
Panelists: Sean Carrie, MB, ChB,
FRCS, FRCS(ORL); Chang-Hoon Kim,
MD; Jern-Lin Leong, MD; Ramandeep
Virk, MBBS, MS (ENT)
Sponsored by the International
Committee
5:00 pm
Meeting Adjourns
5:00 pm – 7:00 pm
Rhinologists in Private Practice
Cocktail Reception
Date Night Bar at Assembly Food Hall
5055 Broadway Place
POSTERS
Poster #001
A comparative analysis of nasal
packing with and without bupivacaine
for postoperative pain control after
endoscopic endonasal transsphenoidal
surgery
Karol Avila-Castano
Poster #002
A computational analysis to investigate
anatomical factors associated with
increased likelihood of epistaxis from
intranasal sprays usage
Katherine Gonzalez, BS
Poster #003
WITHDRAWN
Poster #004
A rare case of chronic invasive
curvularia fungal sinusitis
Samuel Hopper, BS
Poster #005
Academic productivity trends of
fellowship-trained U.S. academic
rhinologists
Michael Warn
Poster #006
Acinic cell carcinoma in the nasal
cavity: A case report of a 69-yearold
female complaining of nasal
congestion
Aileen Beatrice Antonio, MD
Poster #007
An assessment of the quality of
artificial intelligence-generated patient
counseling for sinusitis
Gregory Hill, MD
Poster #008
Artificial intelligence based semi-
automatic segmentation for orbital
tumors radiomic measurement
Angela Zhu, BA
Poster #009
WITHDRAWN
Poster #010
Assessing nasal function after
definitive rhinoplasty for unilateral cleft
lip nasal deformity repairs: A pilot
analysis
Elaine Lin, BS
Poster #011
Association of alcohol use with
olfactory function among older adults
Khamis Suleiman
Poster #012
Association of chronic rhinosinusitis
and autoimmune disorders
Chadi Makary, MD, FARS
Poster #013
Association of prior military service
with olfactory function among older
adults
Richard Chiu, BS
Poster #014
Baseline olfactory function and
prospective assessment of patient-
reported outcome measures in
patients with nasal septal perforation
Shreya Ramkumar, BS
Poster #015
Biologic therapies for treating chronic
sinusitis with nasal polyps: What do
patients want to know?
Samuel Razmi, BS
Poster #016
B-LBL presents as sinonasal mass: A
case report
Brandon Vilarello, BA
Poster #017
WITHDRAWN
Poster #018
Case report: Rare angiomyolipoma of
the nasal cavity
Akash Halagur, BA
Poster #019
Cavernous sinus immunoglobulin
G4-related disease - A case report
Erika Bradley, RN, BSN
Poster #020
Characteristics of patients requiring
revision endoscopic sinus surgery- An
11-year single-institution study
Madison Buras, MD
Poster #021
Characterization of chronic
rhinosinusitis by associated medical
comorbidities
Tiffany Toni

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
22
PROGRAM AT A GLANCE
Poster #022
Choosing wisely in ESS in the era of
biologics (CHESS)
Neil Verma, MDCM, MSc, FRCSC
Poster #023
Clinical outcomes and complications of
endoscopic odondoidectomy: A single
institution experience
Ann Powers, MD
Poster #024
Clinical outcomes of bioabsorbable
nasal implants for nasal valve collapse:
A meta-analysis
Felisha Li, BA
Poster #025
Clinical productivity of fellowship-
trained academic rhinologists: An
analysis of Medicare metrics
Michael Warn
Poster #026
Cohort study: Pluripotent pituitary
adenomas are at higher risk for SIADH
Sabrina Goyal, BS
Poster #027
Combined transnasal, transoral
approach for excision of odontogenic
cysts offers reduced recurrence rates
and favorable sinonasal outcomes
Jennifer Douglas, MD
Poster #028
Comparing physical and virtual “digital
twin” models of endoscopic skull base
disorders for preoperative planning
David Ahmadian, BS
Poster #029
Complications of novel radiofrequency
device use in otolaryngology: A
MAUDE analysis
Sina Torabi, MD
Poster #030
Comprehensive patient-focused
medical illustrations to supplement the
rhinology surgical consent process
Chase Kahn, MD
Poster #031
Contemporary update on the
microbiology of paranasal sinusitis
Alan Workman, MD, MTR
Poster #032
Cranial neuropathies secondary to
allergic fungal rhinosinusitis
Ashleigh Halderman, MD
Poster #033
Craniofacial pain locations and
outcomes after endoscopic sinus
surgery for unilateral sphenoid
sinusitis: A multi-institutional study
Richard Pellizzari, BS
Poster #034
CRSwNP patients using biologicals:
real-world experience in a reference
center
Wilma Anselmo-Lima, PhD
Poster #035
Current otolaryngologic applications of
the novel self-assembling RADA-16
peptide matrix
Arthur Wu, MD
Poster #036
Development of a novel quantitative
PCR assay for diagnosis of
rhinocerebral mucormycosis
Tom Maxim, MD
Poster #037
Differences in patient characteristics
with unilateral versus bilateral allergic
fungal rhinosinusitis
Sei Chung, MD
Poster #038
Dupilumab improved objective and
patient-reported outcomes in patients
with chronic rhinosinusitis with nasal
polyps (CRSwNP) and complete
bilateral nasal obstruction in the sinus-
24 and sinus-52 trials
Prof. Claire Hopkins
Poster #039
Efficacy of olfactory training after
unilateral anterior skull base resection
in patients with olfactory
neuroblastoma: A single-center
prospective study
Teppei Takeda, MD
Poster #040
Epithelial-myoepithelial carcinoma of
the nasal cavity. An interesting case
report and review of the literature
Ariel Waitzman, MD
Poster #041
Eustachian tube recanalization via CO2
guidewire and ureteral stent
Christopher Pool, MD
Poster #042
Evidence for a role of metformin in
preventing olfactory dysfunction
among older adults
Sahar Assi, MD
Poster #043
WITHDRAWN
Poster #044
Extramedullary plasma cell neoplasm
in the nasal cavity: Case presentation
Guillermo Antonio Ramirez, MD
Poster #045
Functional and structural correction of
over-reduced noses by non-rib grafts
Mohsen Naraghi, MD, FARS
Poster #046
Gender differences in quality of life in
patients with skull base pathologies
Parker Tumlin, MD
Poster #047
Granulomatosis with polyangiitis
presenting with skull base
inflammation mimicking petrous
apicitis: A case report and literature
review
Michael Castle, MD
Poster #048
Histopathologic features of patients
with noninvasive fungal rhinosinusitis
Tamara Simpson, BA
Poster #049
WITHDRAWN
Poster #050
Impact of insurance status on CSF leak
presentation
Ali M. Baird, BS
Poster #051
Impact of LYR-210 corticosteroid
matrices on the incidence of acute
exacerbations of chronic rhinosinusitis
in patients from the LANTERN
randomized controlled study
Vineeta Belanger, PhD
Poster #052
Impact of social determinants of health
in chronic rhinosinusitis disease
severity: A scoping review
Avigeet Gupta, MD

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
23
Poster #053
Incident diagnosis of granulomatosis
with polyangiitis in chronic
rhinosinusitis receiving sinus surgery
Trisha Shang, BA
Poster #054
Insight into the mutational landscape
of sinonasal squamous cell carcinoma
Arash Abiri, MS
Poster #055
Interleukin(IL)-4 induces loss of smell
in mice without disrupting olfactory
sensory neuron and epithelial integrity
Dr. Hamid Mattoo
Poster #056
Is it NPC? Endoscopic image
recognition of NPC using narrowing
band imaging versus white light using
deep learning network analysis
Shuhui Xu, MBBS, MRCS (Ireland),
MMed (ORL)
Poster #057
WITHDRAWN
Poster #058
Locally recurrent nasopharyngeal
carcinoma treated with minimally
invasive combined transoral robotic
and transnasal endoscopic resection:
A case report
Abdurrahman Al-Awady
Poster #059
Long term quality of life among
patients undergoing endoscopic
pituitary gland surgery
Narin N. Carmel Neiderman, MD MSc
Poster #060
WITHDRAWN
Poster #061
Metastatic anterior skull base
adenocarcinoma presenting as
hearing loss
Margaret Mitchell, MD, MS-HPEd
Poster #062
Mutational landscape and predictors
of survival in sinonasal
undifferentiated carcinoma
Brandon Lehrich, BS
Poster #063
Nasal septal perforation endoscopy
score correlates with symptom burden
in patients with nasal septal
perforations
Amar Miglani, MD
Poster #064
New techniques of reducing
intraoperative bleeding in endoscopic
sinus surgery for eosinophilic chronic
rhinosinusitis cases with asthma
Yoichiro Narikawa, MD
Poster #065
WITHDRAWN
Poster #066
Novel use of urinalysis dipsticks for
differentiating patients with diverse
sinusitis complaints
Michela Borrelli, BA
Poster #067
Olfaction and neurocognition after
COVID-19: A scoping review
Brandon Vilarello, BA
Poster #068
Open access artificial intelligence and
rhinology patient education
Alice Huang, MD
Poster #069
Optimizing strategy for pre-operative
sinonasal irrigation through 3D
Printing
Kanghyun Kim, BS
Poster #070
Oral corticosteroid (OCS) burden and
healthcare resource utilization (HCRU)
in patients with chronic rhinosinusitis
with nasal polyps (CRSwNP)
undergoing functional endoscopic
sinonasal surgery (FESS): A US real-
world retrospective cohort study
Stella Lee, MD
Poster #071
Paranasal sinus and nasal cavity
squamous cell carcinoma and
adenocarcinoma: A SEER database
analysis
Lacy Brame, DO
Poster #072
Perioperative strategies for improving
quality of life and sinonasal morbidity
after endoscopic skull base surgery: A
systematic review
Satyan Sreenath, MD
Poster #073
Predictors of headache/facial pain
associated with cryotherapy ablation
of the posterior nasal nerve for the
treatment of chronic rhinitia
Samuel Razmi, BS
Poster #074
Predictors of surgical intervention in
children with complicated orbital
cellulitis
Erica McArdle, MD
Poster #075
Proof of Concept: How to use Zoom to
set up a remote telementoring
experience for teaching endoscopic
sinus surgery
Angela Yang
Poster #076
Purasinus, a novel self-assembling
peptide, in a draf-III frontal sinusotomy
Kaitlynne Pak, MD
Poster #077
Radiographic enhancement of the
longus colli muscle in skull base
osteomyelitis
Grant Owen, BA
Poster #078
Rare case of a giant disfiguring frontal
sinus mucocele causing globe
subluxation
Caroline Christmann, MD
Poster #079
Readability and quality analysis of
patient education materials in aspirin
exacerbated respiratory disease
Kush Panara, MD
Poster #080
Real-world effectiveness of
Mepolizumab on upper and lower
airway diseases
Jonathan Bernstein
Poster #081
Reconstruction of sellar defects with
laterally-pedicled native sphenoid
sinus mucosa
Samuel Floren, MD
Poster #082
Referral patterns: Number of providers
and duration of loss before definitive
intervention for olfactory disorders
Bruna Castro, MD
Poster #083
WITHDRAWN
PROGRAM AT A GLANCE

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
24
Poster #084
Report of a novel reconstruction
method using sternocleidomastoid flap
and nasoseptal flap for nasopharyngeal
tumors after nasopharyngectomy
Bita Naimi, BA
Poster #085
WITHDRAWN
Poster #086
Restarting antithrombotic drugs
following functional endoscopic sinus
surgery: A scoping review
Trinithas Boyi, MA
Poster #087
Role of allergic rhinitis in recurrent
acute rhinosinusitis
John Behnke, MD
Poster #088
Safety of proton beam therapy in
patients with sinonasal carcinoma: A
systematic review
Srivatsa Surya Vasudevan, MD, MS
Poster #089
Severe epistaxis after posterior nasal
nerve ablation requiring surgical
intervention: A single center case series
Yuki Yoshiyasu, MD
Poster #090
Severe unilateral refractory epistaxis
arising from the septal branch of the
anterior ethmoid artery
Theodore Nguyen, BS
Poster #091
Severity of chronic sinonasal
symptoms after a major acute
inhalational event: A world trade center
retrospective cohort study
Jerlon Chiu, MD
Poster #092
Sex-based differences in severity of
chronic rhinosinusitis as reported by
SNOT-22 scores
Snehitha Talugula
Poster #093
Shared decision making for patients
with nasal polyposis: Needs
assessment utilizing social media and
clinical cohorts
Isaac Schmale, MD
Poster #094
Sinonasal renal cell-like
adenocarcinoma: Learnings from a
case In pregnancy
Andrew Lee, BS
Poster #095
Stop scrolling: A social media quality
review of sinusitis videos on TikTok
Rose Dimitroyannis, BA
Poster #096
Surgical management of obstructive
nasal polyposis in Cornelia de Lange
syndrome
Trisha Ortiz, Medical Student
Poster #097
Synergistic cytotoxicity of permethrin
and N,N-Diethyl-Meta-Toluamide on
sinonasal epithelia with or without
chronic rhinosinusitis
Hong-Ho Yang, BS
Poster #098
The direct impact of the COVID-19
pandemic on rhinology practice
Sarah Sutton, BS
Poster #099
The effect of acupuncture therapy on
COVID-19 related olfactory loss
Michael Armstrong, MD
Poster #100
The impact of bundled codes on
Medicare volume and reimbursements
for endoscopic sinus surgery
Derek Liu, MD
Poster #101
The impact of Dupilumab treatment on
CRSwNP outcomes in patients with
severe CRSwNP rrom the SINUS-24 and
SINUS-52 studies
Martin Desrosiers, MD
Poster #102
The impact of the lateral crural
reversing on the primary concavity
Mohsen Naraghi, MD, FARS
Poster #103
The influence of facility volume and
type on sinonasal undifferentiated
carcinoma treatment and outcomes
Amy Du, BS
Poster #104
The influence of inhibitors of apoptosis
proteins (IAPs) on chronic
rhinosinusitis with nasal polyps
Wilma Anselmo-Lima, PhD
Poster #105
The role of normal nasal anatomical
variability on intranasal drug particle
transport
Claire Washabaugh
Poster #106
The validation of the readability
enhanced sinonasal sinonasal outcome
test (reSNOT-22) disease-specific
quality of life survey
Adam Kimple, MD, FARS
Poster #107
Three cases of sinonasal organized
hematoma
Sei Kobayashi, MD
Poster #108
Triple-combination Cystic Fibrosis
transmembrane conductance regulator
(CFTR) modulator therapy and
functional endoscopic sinus surgery in
Cystic Fibrosis with chronic
rhinosinusitis
Brian Kinealy, MD
Poster #109
Utilizing 3D navigation to enhance
endoscopic sinus educational
dissection for Otolaryngology trainee
Tadeas Lunga, MD
Poster #110
Voice quality changes follow sinonasal
surgery
Meha Fox, MD
Poster #111
Which intranasal corticosteroids can be
used in patients on PrEP or HAART?
Meghan Nicole Norris, PA-C
Poster #112
Wide resection of extradural skull base
lesions requiring sacrifice of internal
carotid artery: : Preliminary surgical
outcome at a single medical center
Sung-Woo Cho, MD
PROGRAM AT A GLANCE

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
25
Thursday, September 28, 2023
Residents Didactic Course
Cumberland 1
12:00 pm – 5:00 pm
By Invitation Only
Residents Dissection Lab
Off Site Location
Details for Shuttle Service forthcoming
12:00 pm – 1:00 pm
By Invitation Only
Residents Reception
Music Row 5
6:30 pm – 8:00 pm
By Invitation Only
Friday, September 29, 2023
Residents Didactic Course
Cumberland 2
8:00 am – 12:00 pm
By Invitation Only
Residents Dissection Lab
Off Site Location
Details for Shuttle Service forthcoming
8:00 pm – 12:00 pm
By Invitation Only
___________________________________________
Friday, September 29, 2023
7:00 am – 12:00 pm
Broadway Ballroom ABC
7:00 am - 8:00 am
Board of Directors Breakfast
8:00 am - 12:00 pm
Board of Directors Meeting
Friday, September 29, 2023
1:00 pm – 5:00 pm
General Session
Broadway Ballroom GHJK
12:00 pm - 1:00 pm
Fall Film FESStival
Broadway Ballroom GHJK
Moderators: Christopher Church, MD, FARS; Edward
Kuan, MD, FARS
1:00 pm – 1:05 pm
Welcome & Introduction
Pete Batra, MD, FARS
1:05 pm – 1:20 pm
Presidential Address
Sarah Wise, MD, FARS
Top Rated Abstracts – Clinical
Rhinology
Moderators: Kara Detwiller, MD, FARS; Devyani Lal,
MD, FARS; Bobby Tajudeen, MD, FARS
1:20 pm - 1:27 pm
Topical platelet-rich plasma for post-COVID
olfactory dysfunction - A randomized controlled
trial
Alexander Duffy, MD
Bita Naimi, BA
Emily Garvey, BA
Ayan Kumar, Resident Physician PGY-4
Chase Kahn, MD
Douglas Farquhar, MD
Mindy Rabinowitz, MD, FARS
Elina Toskala, MD, MBA, PhD, FARS
Marc Rosen, MD, FARS
Gurston Nyquist, MD, FARS
David Rosen, MD
Thomas Jefferson University Hospital
Background:
Patients with post-COVID olfactory dysfunction (OD)
face severe sequelae. Prior studies have demonstrated
the effect of injected platelet-rich plasma (PRP) in
treatment of post-COVID OD; however, topical,
endonasal PRP has yet to be investigated.
Methods:
Randomized controlled trial from July 2022-present.
Patients with OD (Brief Smell Identification Test
(B-SIT)<8/12 on presentation) of 6-24 months’ duration
following suspected or confirmed COVID infection were
included. Patients were excluded if OD predated the
patient’s COVID infection. Patients were treated with
three, once-monthly topical applications of PRP or
placebo (saline) into bilateral olfactory clefts. Patients
completed B-SIT and SCENTinel psychophysical tests
and the Questionnaire of Olfactory Disorders–Negative
Statements (QOD-NS) monthly, from months 1-12.
Results:
Of 104 screened patients, 81 qualified and participated
in the trial. There were no significant differences in
baseline B-SIT, SCENTinel, or QOD-NS scores.
Patients with OD of 12-23 months (n=51) treated with
PRP (n=27) demonstrated a statistically significant
increase in B-SIT scores from baseline to month 4
compared to placebo (+2.3 vs +0.96,p=0.049).
Regardless of OD duration, patients with parosmia
(SCENTinel hedonic score <50) treated with PRP
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
26
(n=14) had an improvement in B-SIT from baseline to
months 4 (+1.8,p=0.01), 5 (+2.3, p=0.007), 6
(+2.8,p=0.006), and 7 (+3.1,p=0.03), whereas those
treated with placebo (n=14) had no improvement in
BSIT at those timepoints.
Conclusion:
Topical PRP may be an efficacious treatment for post-
COVID OD, particularly in those with parosmia. This is
the first study to investigate the use of topical PRP and
demonstrate an improvement in B-SIT scores.
1:28 pm – 1:35 pm
Efficacy and safety of EDS-FLU in chronic
rhinosinusitis – Two randomized controlled trials
James Palmer, MD, FARS
ReOpen Steering Committee Members
Rationale:
The ReOpen program evaluated the efficacy and safety
of the exhalation delivery system with fluticasone (EDS-
FLU, XHANCE®) in chronic rhinosinusitis (CRS).
Methods:
Two 24-week, randomized, controlled trials enrolled
patients with moderate-to-severe CRS with ≥2
symptoms for ≥12 weeks and sinus opacification on CT
scan, with (CRSwNP) or without (CRSsNP) nasal
polyps. Endpoints included combined symptom score
(CSS); average percent ethmoid/maxillary opacified
volume (APOV); frequency of acute exacerbations of
CRS (AECRS); Sinonasal Outcome Test-22 (SNOT-22),
and Pittsburgh Sleep Quality Index (PSQI).
Results:
Patients enrolled in ReOpen1 (CRSwNP and CRSsNP;
n=332) and ReOpen2 (CRSsNP; n=223) received EDS-
FLU one (n=182) or two (n=180) sprays/nostril, or EDS-
placebo (n=185), twice daily. Co-primary symptom and
sinus opacification outcomes improved significantly with
EDS-FLU vs EDS-placebo (CSS LS mean, baseline to
Week 4: -1.62 versus -0.70, P<0.001; APOV LS mean,
baseline to Week 24: -5.54 versus -0.06, P<0.001).
This pattern was observed in both CRSsNP and
CRSwNP subgroups. APOV change associated with
patient-reported improvement was -2.86 points. EDS-
FLU reduced AECRS episodes significantly vs EDS-
placebo (Incidence Rate Ratio=0.389; 95%CI=0.226-
0.669). EDS-FLU also produced significantly greater
improvement in SNOT-22 (Total Score LS mean, -18.02
versus -6.47; P<0.001) and in sleep (PSQI Global
Score LS mean, 1.49 versus -0.78, P=0.006). Reported
adverse events were similar to those reported with
standard-delivery nasal sprays.
Conclusions:
EDS-FLU is the first medication shown in randomized
trials to reduce AECRS and improve symptoms and
quality-of-life in all CRS patients, including CRSsNP.
1:36 pm – 1:43 pm
All CRS endotype clusters demonstrate
improvement in patient reported and objective
measures after endoscopic sinus surgery
Nikita Chapurin, MD, MHS
Jorge Gutierrez, BA
Jess Mace, MPH
Sofia Khan, BS
Timothy Smith, MD, MPH, FARS
Rodney Schlosser, MD, FARS
Zachary Soler, MD, MSc, FARS
Medical University of South Carolina
Background:
It is unclear if chronic rhinosinusitis (CRS) endotypes
show differential response to endoscopic sinus surgery
(ESS). We explored mucus inflammatory cytokine
clusters in a cohort with CRS and associations with
both preoperative and postoperative outcome
measures.
Methods:
Patients with CRS were prospectively recruited
between 2016-2021 into a multi-center observational
study. Mucus was collected from and evaluated for 26
biomarkers preoperatively. Patient reported outcome
measures included the Sino-Nasal Outcome Test
(SNOT-22) and Questionnaire of Olfactory Dysfunction
(QOD). Additional clinical measures of disease severity
included Threshold, Discrimination, and Identification
(TDI) scores using Sniffin’ Stick testing and Lund-
Kennedy endoscopic scores (LKES).
Results:
A total of 128 patients were evaluated and grouped into
type 2 inflammatory, non-type 2 inflammatory, non-
inflammatory and 2 indeterminate clusters based upon
individual protein levels. There was some variability
within individual clusters. Overall, the type 2
inflammatory group was found to report the highest
mean improvement in both SNOT-22 (-28.3 [SD±16.2])
and TDI (6.5 [SD±7.9]) scores after ESS. All endotypes
membership group demonstrated improvement of all
outcome measures after ESS on average, with no
statistically significant between-group differences in
SNOT-22 (p=0.738), QOD (p=0.306), as well as TDI
(p=0.358), LKES (p=0.514) measures.
Conclusions:
All CRS endotype clusters appear to respond favorably
to surgery and show improvement in patient reported
and objective outcome measures. Thus, ESS is a more
generalized therapy, and benefits are not limited to
specific endotypes.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
27
1:44 pm – 1:51 pm
Peri-operative air quality and post-operative
endoscopic sinus surgery outcomes
Amarbir Gill, MD
Benton Tullis, BS
Jess Mace, MPH
Vijay Ramakrishnan, MD, FARS
Daniel Beswick, MD, FARS
Zachary Soler, MD, MSc, FARS
Timothy Smith, MD, MPH, FARS
Jeremiah Alt, MD, PhD, FARS
University of Utah
Objective:
Poor air quality is linked to chronic rhinosinusitis (CRS)
with numerous mechanisms by which airborne irritants
negatively impact mucosal inflammation and wound
healing. It is unknown if peri-operative pollutant
exposure impacts endoscopic sinus surgery (ESS)
outcomes. We assessed the impact of peri-operative
particulate matter (PM) levels on sinonasal-specific and
general quality-of-life (QOL) measures in a multi-
institutional cohort of patients with CRS.
Methods:
Participants with CRS who self-selected ESS were
prospectively enrolled. The 22-item SinoNasal
Outcome Test (SNOT-22) and Medical Outcomes Study
Questionnaire Short-Form 6-D (SF-6D) health utility
values scores were recorded. Using residence zip
codes, patient exposure to PM for the month of surgery
was obtained from Environmental Protection Agency air
quality monitors. Spearman’s correlation coefficients
(R) and 95% confidence intervals (CI) were used to
determine bivariate association.
Results:
389 patients were enrolled with a mean follow-up of 7.2
months (SD +/-2.4). Patients with greater peri-operative
PM2.5 exposure had less improvement in their SNOT-
22 scores after ESS compared to those with less
exposure (p=0.048, R=0.10, 95% CI (-0.002, 0.20). No
similar association was noted with SF-6D scores.
Specifically, the psychological (p=0.014) and sleep
dysfunction (p=0.014) domains of the SNOT-22 were
most significantly impacted by peri-operative PM2.5
concentrations. No correlation was found between
pollutant levels and need for revision ESS (p=0.89).
Conclusion:
Certain types of pollutant exposure may negatively
impact absolute improvement in sinonasal QOL after
ESS. Larger population-based studies are needed to
confirm these findings.
1:52 pm – 1:59 pm
Optimizing topical nasal corticosteroid irrigations:
A randomized double-blind clinical trial
Zachary Root, BS
Veronica Formanek
Thomas Lepley
Joseph Lee
Sarah Sussman
Kathleen Kelly, MD
Bradley Otto, MD
Kai Zhao, MD
The Ohio State University Wexner Medical Center
Background:
The efficacy of topical corticosteroid irrigations in the
management of chronic rhinosinusitis (CRS) can be
variable due to differences in individual anatomy and
ineffective head positioning. We conducted a
randomized double-blinded clinical trial at a tertiary
medical center in Ohio from November 2021 to March
2023 to determine if personalized, 3D-printed nasal
models can optimize head positioning and improve
patient outcomes.
Methods:
31 patients with CRS (22 with no prior sinus surgery)
were randomized into either control (CG, N=10),
backfill (BG, N=10), or model (MG, N=11) groups; daily
2 mg Mometasone irrigations were then performed for
two months with either standard instructions, a head tilt
of 90° to the side with fluid entering the lower nostril, or
in an optimized position as determined by patient-
specific 3D printed irrigation models, respectively.
Results:
Symptom improvements were mild in the CG (NOSE:
47.5±32 to 31.0±34, SNOT-22: 43.9±33 to 32.9±29,
Visual Analog Scale (VAS) of nasal obstruction: 4.00
±2.7 to 2.80±2.4, all p>0.05), moderate in the BG
(NOSE: 54.5±22 to 33.0±20, SNOT-22: 35.8±15 to
26.5±18, VAS: 4.55±2.5 to 3.24±2.7, only NOSE
p<0.05), and significant in the MG (NOSE: 52.3±14 to
16.1±12, SNOT-22: 39.8±17 to 12.4±10, VAS: 4.27±2.0
to 2.22±1.6, all p<0.05). Lund-Mackay scores
significantly improved only in the MG (11.4±4.3 to
7.56±5.9, p<0.05). The MG also had the lowest patient
dropout rate (25.0% vs BG 27.8% vs CG 41.2%).
Conclusion:
3D printing can significantly improve corticosteroid
irrigation outcomes through improved patient education
and optimized head positioning. 3D modelling also
appears to encourage better treatment compliance.
1:59 pm – 2:05 PM
Q&A
2:05 pm – 2:15 pm
Awards Ceremony
Jean Kim, MD, FARS
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
28
2:15 pm – 3:00 pm
David W. Kennedy Lecture
Introduction: Pete Batra, MD, FARS
Guest Speaker: Brent Senior, MD, FARS
“Global Outreach in Rhinology: Lessons Learned
From a Quarter Century in Vietnam”
3:00 pm – 3:30 pm
Break with Exhibitors
Top Rated Abstracts – Basic Science
and Translational Research
Moderators: Benjamin Bleier, MD, FARS; Do-Yeon
Cho, MD; Elina Toskala, MD, FARS
3:30 pm – 3:37 pm
An eosinophil peroxidase activity assay accurately
predicts eosinophilic chronic rhinosinusitis
Kristine Smith, MD
Amarbir Gill, MD
Chelsea Pollard
Shaelene Ashby, PhD
Paige Shipman
Michael Yim, MD, FARS
Joshua Levy, MD, FARS
Gretchen Oakley, MD, FARS
Richard Orlandi, MD, FARS
Jeremiah Alt, MD, PhD, FARS
Abigail Pulsipher, Dr.
University of Utah
Background:
A definitive diagnosis of eosinophilic chronic
rhinosinusitis (eCRS) requires surgical tissue sampling
and histologic enumeration of intact eosinophils.
Eosinophil peroxidase (EPX) is an accurate biomarker
of sinonasal tissue eosinophilia in CRS. A less invasive
and rapid method that accurately identifies tissue
eosinophilia would be of great benefit to patients. The
objective of this investigation was to evaluate a new
clinical tool that utilizes a nasal swab and colorimetric
EPX activity assay to predict a diagnosis of eCRS.
Methods:
A prospective cohort study was conducted using nasal
swabs and sinonasal tissue biopsies obtained from
patients with CRS electing endoscopic sinus surgery.
Patients were classified as non-eCRS (n=19) and
eCRS (n=35) based on pathologically-determined
eosinophil counts of <10 or ≥10 eosinophils/high-power
field, respectively. Swab-deposited EPX activity was
measured and compared to tissue eosinophil counts,
EPX levels, and CRS-specific disease metrics.
Results:
EPX activity was significantly increased in patients with
eCRS compared to in non-eCRS (p<0.0001). With a
relative absorbance unit cut-off value of ≥0.80, the
assay demonstrated high sensitivity (85.7%) and
moderate specificity (79.0%) for confirming eCRS.
Spearman correlations between EPX activity and tissue
eosinophil counts (rs=0.424), EPX levels (rs=0.503),
and Lund-Kennedy endoscopy scores (rs=0.440) in
eCRS were significant (p<0.05).
Conclusions:
This study evaluated a nasal swab sampling method
and EPX activity assay that accurately confirms eCRS.
This method could potentially address the unmet need
to identify sinonasal tissue eosinophilia at the point-of-
care and monitor eosinophil activity and treatment
response.
3:38 pm – 3:45 pm
Common cold viruses activate the unfolded protein
response in chronic rhinosinusitis
Elizabeth Sell, Medical Student
David Renner
Li Hui Tan, PhD
Michael Kohanski, MD, PhD
Susan Weiss, PhD
Noam Cohen, MD, PhD, FARS
University of Pennsylvania
Background:
Viral infections have long been implicated in the
pathogenesis of chronic rhinosinusitis (CRS). Human
coronaviruses (CoV) cause approximately 5-30% of the
common cold. CoV replication causes endoplasmic
reticulum (ER) stress and activates the unfolded protein
response (UPR), a series of pathways that allow cells to
alleviate stress or eliminate chronically stressed cells.
The UPR has been shown to be upregulated in some
patients with CRS; however, it is not known if CoVs can
activate the UPR in the human sinonasal epithelium, or
if pre-existing CRS affects CoV infection.
Methods:
Thus, we aimed to interrogate UPR activation by
human CoV infection. We examined the three branches
of the UPR and their downstream transcription factors
in primary human nasal air-liquid-interface (ALI)
cultures. We infected the ALI cultures with viruses 229E
and NL63 and found that both viruses replicate and
release infectious virions as quantified by plaque assay.
We investigated activation of the UPR at both the
mRNA and protein level using RT-qPCR and western
blot analysis of the UPR sensors and downstream
targets, respectively.
Results:
We found that 229E induces ER stress and triggers
both the IRE1 and PERK branches of the UPR. In
particular, 229E strongly triggers XBP1 splicing, which
may correlate with increased interferon signaling. We
further found that ALI cultures grown from patients with
CRS cleared 229E faster than cultures grown from
patients without CRS, and that viral clearance
correlated with increased interferon production in the
CRS cultures.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
29
Conclusions:
Our data suggest that CoVs activate the UPR stress
response pathway, and that targeting this pathway
could be used to develop novel therapies for patients
with CRS.
3:46 pm – 3:53 pm
Timing of surgery on tissue IL-13 expression in
CRSwNP patients on Dupilumab: A real-world study
Abdul Rahman Alenezi
Andrew P. Lane, MD, FARS
Heather Kulaga
Nicholas Rowan, MD
Johns Hopkins School of Medicine
Background:
Dupilumab is an effective option for CRSwNP
recalcitrant to medical/surgical therapy. In the biologics
era, the role and timing of surgery in CRSwNP is
currently unresolved. On a molecular level, the impact
of surgery relative to initiation of Dupilumab on cytokine
gene expression has not been investigated.
Methods:
Retrospective analysis of prospectively obtained
mucosal samples from 17 recalcitrant eosinophilic
CRSwNP patients, before and after initiating
Dupilumab. Subjects were divided into 2 cohorts,
depending on whether therapy was initiated
immediately after revision endoscopic sinus surgery.
Real-time PCR was used to assess IL-13 mRNA in the
samples. Nasal endoscopy, SNOT-22, and UPSIT
were also performed.
Results:
All subjects had severe CRSwNP s/p multiple
surgeries, and all had good clinical responses to
Dupilumab plus INCS. In the 7 subjects with revision
surgery immediately preceding Dupilumab, IL-13 mRNA
expression underwent a sustained decrease from
baseline over >6 months. In subjects in whom the last
surgery had been performed remote to starting
Dupilumab, IL-13 expression was noted to increase
and be persistently elevated. This difference between
groups was significant (P<0.0004, Mann-Whitney U).
Conclusion:
In recalcitrant CRSwNP patients, revision surgery with
debulking of polyps prior to initiating Dupilumab
appears to prevent long-term elevation of IL-13 mRNA
expression in the sinonasal mucosa. This finding may
suggest that pre-treatment surgery reduces
endogenous drivers of type 2 inflammation that
otherwise persist on Dupilumab. Further studies are
needed to determine whether Dupilumab therapy can
be decreased or withdrawn in such subjects after
mucosal normalization post-surgery.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
30
3:54 pm – 4:01 pm
Glutathione and bicarbonate nanoparticles improve
mucociliary transport in cystic fibrosis epithelia
icholas Rivers, MD
Shaoyan Zhang, PhD
Daniel Lim
Daniel Skinner, BS
Lydia Yang
Marie Ehrhardt
Caitlyn Tomblin
Jessica Grayson, MD
Do-Yeon Cho, MD
Steven M. Rowe, Professor and Director of CF
Research Center
Bradford A. Woodworth, MD, FARS
University of Alabama at Birmingham
Introduction:
Cystic fibrosis (CF) is a respiratory disease
characterized by the overproduction of thick mucus and
ineffective mucus transport. While CFTR modulator
therapy represents a partial solution, novel strategies
are needed to improve its effectiveness, particularly for
non-responders. Lack of functional CFTR decreases
HCO3- secretion causing release of unexpanded, gel-
forming mucins. Replacing HCO3- topically via
irrigation or nebulization is ineffective at alkalizing the
airway surface liquid due to rapid reabsorption and
neutralization by carbonic anhydrase. Furthermore, the
highly oxidative environment of CF airways causes
mucin polymer crosslinking and has been targeted
previously with GSH (cleaves disulfide crosslinking) in
clinical trials although with mixed results. This study
investigates a novel approach using GSH/NaHCO3-
nanoparticles to address mucus obstruction in CF.
Methods:
GSH (1 mM)/NaHCO3- (24 mM) poly(lactic-co-glycolic
acid) nanoparticles were tested on primary CF
sinonasal (F508del/F508del) epithelial cultures,
evaluating dose-release curves, surface pH, toxicity,
and mucociliary transport indices using micro-optical
coherence tomography.
Results:
The nanoparticles showed sustained release with no
cellular toxicity over two weeks. The apical surface pH
gradually increased from 6.63+/-0.21 to 7.11+/-0.39 at
24 hours (p<0.05). MCT (0.059+/-0.023 vs. 0.033+/-
0.006 mm/min) and periciliary liquid depth (5.67+/-0.33
vs. 4.68+/-0.57 µm, p<0.01) were significantly improved
over controls.
Conclusion:
These findings suggest that GSH/NaHCO3-
nanoparticles are a promising treatment option for
viscous mucus in CF and other respiratory diseases of
mucus obstruction such as chronic rhinosinusitis.
4:02 pm – 4:09 pm
The effects of PM2.5 exposure on the presentation
of acute bacterial rhinosinusitis
David Grimm, MS
Michael Yong, Dr.
Z Jason Qian, Dr.
Peter Hwang, MD, FARS
Background:
Exposure to particulate matter 2.5 (PM2.5) is an
established risk factor for poor health outcomes. We
sought to identify associations between PM2.5
exposure and incidence of acute bacterial rhinosinusitis
(ABRS) over the past decade in California.
Methods:
The Merative® MarketScan® Research Databases
were used to identify claims for ABRS in adult
Californians between 2007-2020. Demographic
information, asthma status, allergic rhinitis status, and a
Charlson comorbidity index (CCI) were collected. A
control population without ABRS was generated at a
ratio of 3:1. For each presentation of ABRS a rolling
statistical average of daily PM2.5 from the prior 6
months was mapped based on census-based statistical
area provided by the EPA. Patients’ PM2.5 exposure
was classified as low, medium, or high based on cohort
tertile.
Results:
369,711 ABRS encounters were identified (64.4%
female, 35.6% male, mean age= 41). Mean daily
PM2.5 exposure in the ABRS cohort was 11.90 μg/m3
(IQR 8.82-14.11) vs 10.35 μg/m3 (IQR 7.87-12.26) in
controls (p<0.0001), with a total cohort exposure range
of 1.86-31.63 μg/m3. Compared to patients in the low
PM2.5 exposure tertile, medium exposure patients had
an aOR of 1.40 [1.39-1.41], and high exposure an aOR
of 2.23 [2.21-2.25]. On multivariable logistic regression,
incidence of ABRS increased linearly with PM2.5 levels
(aOR 1.11 [1.10-1.11] per 1 μg/m3 increase in PM2.5).
Female sex (1.57 [1.55-1.58]), asthma (1.39 [1.37-
1.41]), allergic rhinitis (2.02 [2.00-2.04], and CCI (1.05
[1.05-1.06] per point) were also correlated.
Conclusion:
Exposure to PM2.5 is associated with increased
incidence of ABRS in a dose-response fashion,
adjusting for patient demographic and rhinologic
comorbidities.
4:09 pm – 4:15 pm
Q&A
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
31
4:15 pm – 5:00 pm
Panel: “Maintaining Balance & Achieving the
Quadripartite Mission”
Moderator: Nicholas Rowan, MD
Panelists: Stacey Gray, MD, FARS; Peter Hwang, MD,
FARS; Devyani Lal, MD, FARS; Rodney Schlosser,
MD, FARS; Sarah Wise, MD, FARS
Sponsored by Residents and Fellows Committee and
Women in Rhinology Section
5:30 pm – 7:00 pm
President’s Welcome Reception
Broadway Ballroom, 5
th
Avenue Pre-Function Area
Saturday, September 30, 2023
8:00 am – 12:00 pm
Breakout 1
Basic Science and Clinical Rhinology
Broadway Ballroom JK
7:00 am – 8:00 am
Meet the Authors Poster Viewing & Breakfast
Grand View Terrace Foyer, Second Level
Session Chair: Erin O’Brien, MD, FARS
8:00 am – 8:35 am
Panel: “Success in Early Career Extramural
Funding:
Moderator: Murugappan Ramanathan, MD, FARS
Panelists: Andrew Lane, MD, FARS; Corinna Levine,
MD, FARS; Timothy Smith, MD, FARS; Carol Yan, MD
Sponsored by the Mentorship Committee
Scientific Oral Presentations:
Pathophysiology and Mechanisms
Moderators: Lauren Roland, MD; Nicholas Rowan,
MD; Kristine Smith, MD
8:35 am – 8:40 am
Acetate and propionate metabolism by
Pseudomonas aeruginosa contributes to significant
sinus inflammation in a rabbit model of sinusitis
Do-Yeon Cho, MD
Daniel Skinner, BS
Shaoyan Zhang, PhD
Dong Jin Lim, PhD
Natalie Dorin
Jessica Grayson, MD
Bradford A. Woodworth, MD, FARS
University of Alabama at Birmingham
Background:
Understanding how Pseudomonas aeruginosa adapts
to the in vivo nutritional environment has important
implications for treating airway infection. Anaerobe-
derived nutrient (e.g., acetate(AC), propionate(PR))
acquisition by P. aeruginosa may contribute to its
virulence. This study aims to assess the impact of
Pseudomonas AC and PR metabolism on sinusitis
pathogenesis.
Methods:
Rabbit’s sinuses were infected with wild-type (WT) B.
fragilis 638R on Day 0 after blocking the sinus opening
(n=8). On day 4, either WT P. aeruginosa PA14 or
mutantPA14 (ΔacsAΔprpB, cannot metabolize AC and
PR) was inoculated into the same sinus to induce
co-infection (n=4 each). On day 10, blockage was
removed, and rabbits were monitored for 5 more
weeks. Endpoints included colony-forming units,
computerized tomographic (CT) scores, histology, and
chloride (Cl-) transport capability.
Results:
All rabbits developed fulminant sinusitis by blocking the
sinus opening on day 10. A significant weight loss was
noticed in those rabbits infected with both WT bacteria
(638R+PA14) than with 638R+mutantPA14 on Day 10.
Mutant PA14 demonstrated growth defects relative to
WT PA14 (p=0.02) when grown in co-culture with 638R
at day 10. At week 6, subepithelia were significantly
thicker in those infected with both WT bacteria
(638R+PA14) than with 638R+mutantPA14 (p<0.01).
Sinus potential difference revealed greater Cl- transport
in the 638R+mutantPA14 compared to 638R+PA14
(p<0.05).
Conclusions:
Even with the restoration of sinus oxygenation on day
10, those sinuses infected with PA14 (metabolizing AC
and PR) developed significant tissue inflammation and
decreased Cl- secretion, compared to those infected
with mutantPA14, when co-cultured with WT B. fragilis.
8:41 am – 8:46 am
Identifying 5-hydroxymethylcytosine profiles in cell
free DNA from serum in patients with aspirin
exacerbated respiratory disease
Tiffany Toni
Phillip Hsu, Dr.
Emily Papazian, Dr.
Marco Rivas
Diana West-Szymanski
Arpit Panda
Robert Naclerio, MD
Christopher Roxbury, MD, FARS
Nishant Agrawal, Dr.
Chuan He, Dr.
Jayant Pinto, Dr.
Background:
Aspirin exacerbated respiratory disease (AERD) is an
airway disorder characterized by a proinflammatory
state. Although there are genetic and environmental
contributions, the molecular pathogenesis remains
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
32
unknown. We hypothesized that patients with AERD
would exhibit specific epigenetic (5-
hydroxymethylcytosine [5-hmC]) profiles, which could
identify dysregulated systemic pathways, aid in
diagnosis, and predict response to therapy.
Methods:
We compared the 5-hmC profiles in adults with AERD
(n=7) compared to control patients (n=6) without
asthma or polyposis; subjects taking systemic steroids
were excluded. Cell free DNA was isolated from
peripheral blood serum and sequenced. Expression
analysis identified differentially hydroxymethylated
genes (DhMGs) and differentially hydroxymethylated
regions (dhmRs). Metascape analysis of the resultant
DhMGs was used to generate a list of statistically
enriched functions.
Results:
AERD and control groups did not statistically differ by
age (AERD 49.4 ± 13.2 vs. 47.0 ± 12.8, p=0.74), sex
(χ2=0.93, p=0.34), race ( χ2=0.07, p=0.97), or smoking
status (χ2=0.03, p=0.85). According to preset criteria,
275 DhMGs and 246 DhMRs were identified. Principle
component and hierarchical clustering analyses
demonstrated distinct clustering of AERD samples
compared to control samples when both DhMGs and
DhMRs were analyzed. The top 20 statistically enriched
terms from Metascape analysis included differential
expression of immune modulators, cellular development
and differentiation, and response to exogenous
damage.
Conclusions:
In this pilot study, we demonstrate that analysis of
differential 5hmC profiles from cell free serum DNA is a
feasible approach to investigate AERD
8:47 am – 8:52 am
Increased staphylococcus abundance in the sinus
microbiome is associated with chronic
rhinosinusitis treatment resistance
David Hoying, BS
Naseer Sangwan, Director of Microbiome Composition
and Analytics Core
Mohamad Chaaban, MD, FARS
Case Western Reserve University School of Medicine
Introduction:
Chronic rhinosinusitis (CRS) significantly affects
patients’ quality of life. There is emerging evidence that
the sinonasal microbiome plays a role in CRS
phenotypes and treatment response. We performed a
microbial analysis of CRS-involved tissue to correlate
response to sinus surgery with the relative abundance
of distinct microbial populations.
Methods:
Using 16rRNA gene sequencing, we characterized the
microbiome of a cohort of adult patients with CRS with
and without polyps with at least bilateral total ethmoid
sinuses involvement undergoing FESS. DAtest was
used for differential abundance analysis using the
random-forest algorithm, and PERMANOVA was
performed on all principal coordinates. Resistance-to-
treatment (RTT) was defined as a less than 20%
reduction in post-operative SNOT-22 score up to four
months post-operatively compared to the pre-operative
baseline SNOT-22.
Results:
In the cohort of 25 CRS patients, there were four
patients with RTT disease (2 CRSsNP; 2 CRSwNP)
and 21 patients with a successful post-operative
response (5 CRSsNP; 19 CRSwNP). There was no
statistical difference in the mean age between the post-
operative responder and non-responder cohorts (48.4
+/- 15 vs. 45.5 +/- 20.6, p=0.80). At the genera level,
the relative abundance of Staphylococcus was
significantly higher in the non-responder groups
compared to the responder groups (p<0.05).
Additionally, Klebsiella was significantly decreased in
the non-responder group (p<0.05). A receiver operating
curve was able to accurately distinguish between
responders and non-responders based on the sinus
microbiome (AUC=0.92).
Conclusion:
The sinus microbiome could be a helpful predictor of
treatment response with FESS.
8:53 am – 8:58 am
Long non-coding RNAs related to extracellular
matrix and proteins are differentially expressed in
chronic rhinosinusitis
Tripti Brar, MBBS, MD
Chantal McCabe, Bioinformatician
Hirohito Kita
Devyani Lal, MD, FARS
Mayo Clinic in Arizona
Background:
Long non-coding RNAs (lncRNAs) are RNA molecules
greater than >200 nucleotides, without protein-coding
capability. They interact with many molecules, regulate
gene expression, genetic imprinting, histone
modification, DNA methylation, posttranscriptional
silencing etc and play a significant role in epigenetic
regulation. A few studies from China, most using pre-
existing GEO datasets, have investigated lncRNAs in
CRS. We performed an original lncRNA study
comparing CRS versus control tissue.
Methods:
RNA extraction and RNA-sequencing was performed
on ethmoid mucosa of 16 CRS subjects and inferior
turbinate mucosa of 4 control subjects. EdgeR software
was used for bioinformatics analysis; FDR<5%, and
log2 fold change >1.5 or <-1.5 was used to
characterize differentially expressed (DE) lncRNAs.
Pathway analysis was done with Metascape™
software.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
33
Results:
Between CRS and controls, 942 DE lncRNAs were
identified; top pathways were Naba core matrisome
[matrisome: ensemble of ≥1000 genes encoding
extracellular matrix (ECM) and ECM-associated
proteins], hydrogen peroxide catabolic process, ECM
organization, sensory perception of bitter taste, and
Naba proteoglycans. CRSwNP versus controls
identified 2803 DE lncRNAs; top pathways were Naba
core matrisome, ECM organization, response to
wounding/burn healing. CRSsNP versus controls
identified 511 DE lncRNAs; top pathways were Naba
core matrisome, neuron projection development, Naba
proteoglycans and oxygen transport.
Conclusion:
DE of lncRNAs with pathways related to ECM matrix,
ECM glycoproteins, collagens and proteoglycans were
identified between controls and CRS. We identified
epigenetic mechanisms through which structural
integrity disruption associated with CRS may occur.
8:59 am – 9:04 am
Comparison between upper and lower airway
microbiome in chronic rhinosinusitis patients
Juan Carlos Hernaiz-Leonardo, MD, MSc
Changwan Ryu
Athenea Pascual, Research Coordinator
Judy Fan
Rogerio Pezato
Don Sin
Andrew Thamboo, MD
University of British Columbia
Background:
Dysregulation of the airway microbiota is thought to
contribute to airway inflammation in both chronic
rhinosinusitis (CRS) and asthma. However, the
relationship between the upper and lower airway
microbiome remains unclear.
Methods:
Sinus and lung swabs were collected from 29 CRS
participants undergoing sinus surgery. DNA was
extracted and submitted for 16s rRNA microbiome
sequencing. Alpha and beta diversity metrics,
taxonomic composition, and differences between
individual taxa were compared for paired sinus and
bronchial samples.
Results:
24 out of 29 participants had sufficient sample for
analysis. The mean (SD) age was 51.59 (14.57) years,
and 13 (40.6%) patients were female. Eighteen (56.3%)
patients had comorbid asthma. Nasal swabs had
significantly higher alpha diversity indexes (Shannon
and Faith) compared to bronchial swabs (p < 0.001).
Beta diversity metrics were not significantly different
between bronchial and nasal samples. However,
principal coordinate analysis showed no clustering of
paired nasal and bronchial samples. Nasal swabs had
significantly more Lawsonella spp., Corynebacterium
spp., and Staphylococcus spp. compared to bronchia
swabs, while the latter were enriched in Sphingomonas
spp. and Bradyrhizobium spp. (FDR adjusted P <0.01).
Finally, CRS patients with comorbid asthma had
significantly higher Pseudomonas spp. and lower
Staphylococcus spp. in nasal swabs and higher
Bradyrhizobium spp. in bronchial swabs compared to
non-asthmatics (FDR-adjusted P <0.01).
Conclusion:
The nasal and bronchial bacterial microbiomes differ in
important ways, with comorbid asthma being a
significant effect modifier. Nasal swabs alone cannot
predict the lower airway microbiome.
9:05 am – 9:15 am
Q&A
9:15 am – 9:45 am
Panel: “Generative Artificial Intelligence in
Rhinology”
Moderator: Chirag Patel, MD, FARS
Panelists: Martin Citardi, MD, FARS; Brian Logo, MD,
FARS; Martin Desrosiers, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations: CRS
Impact and Disease Severity
Moderators: Angela Donaldson, MD, FARS; Amber
Luong, MD, PhD, FARS; Toby Steele, MD
10:15 am – 10:20 am
In vivo nasal micro-optical coherence tomography
imaging reveals mucociliary dysfunction in chronic
rhinosinusitis
Kadambari Vijaykumar
Do-Yeon Cho, MD
Huimin Leung
Amilcar Barrios
Bo Liu
Heather Hathorne
George M. Solomon, MD
Guillermo J. Tearney
Steven M. Rowe, Professor
Bradford A. Woodworth, MD, FARS
University of Alabama at Birmingham
Background:
Chronic rhinosinusitis (CRS) is known to be associated
with altered mucociliary transport (MCT). Micro-optical
coherence tomography (μOCT) has been used to
determine cellular and functional dynamics of
respiratory epithelia at the 1-μm resolution, enabling
quantification of ciliary motion and mucus transport.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
34
This study aims to compare the mucociliary parameters
between healthy controls (HC) and those with CRS,
with and without nasal polyps (CRSwNP, CRSsNP)
using human µOCT imaging.
Methods:
HC and subjects with CRSwNP and CRSsNP were
enrolled. Clinical histories were obtained, and a nasal
exam was performed prior to intranasal µOCT imaging.
Investigators blinded to the subjects’ conditions
analyzed the in vivo µOCT parameters, including
mucociliary transport (MCT), ciliary beat frequency
(CBF), periciliary liquid depth (PCL), airway surface
liquid depth (ASL), and epithelial thickness (ET).
Results:
Six HC participants (age, 38.7±14.5 years) and 16
subjects with CRS (CRSwNP=6 (age, 42.3±13.7years),
CRSsNP=10 (age, 49±4.1years)) were recruited. Of
those with CRSwNP, 100% had a history of allergic
rhinitis, and 67% had asthma. µOCT analysis showed
that MCT rates were significantly lower in the
cumulative CRS group (MCT (mm/min), 4.32±1.2 CRS
vs 6.98±0.9 HC, P< 0.01), and the decrement was
similar in individual CRS groups (CRSsNP:
4.13±1.7mm/min, P< 0.01; CRSwNP:4.68±1.4mm/min,
P=0.051). No differences in other µOCT parameters
were identified between groups.
Conclusion:
In vivo nasal µOCT imaging demonstrated decreased
MCT in CRS patients with and without NP. This novel
imaging method represents a technologic leap forward
and is feasible for assessing acquired MCT defects
impacting the upper airway epithelium.
10:21 am – 10:26 am
Multi-instance learning for eosinophil quantification
of sinonasal histopathology images
Yi-Tsen Li, MD, PhD
Ming-Sui Lee, Associate Professor
Te-Huei Yeh, Professor
National Taiwan University Hospital
Background:
Identification of eosinophilic chronic rhinosinusitis
(CRS) subtype is critical for treatment decision making
and prognosis prediction. Manual counting of
eosinophils distributed in the sinonasal tissues is time-
consuming and labor-intensive. In this study, we aimed
to develop an automatic system for eosinophil
quantification of sinonasal histopathology images using
a deep learning approach.
Methods:
Pathologic images of sinonasal tissues from 40 patients
with bilateral CRS were obtained and the number of
eosinophils was counted and labeled by medical
researchers. These images were randomly divided into
two groups: training and validation. Candidate images
were selected from each whole slide after filtering the
noise area and background. Each candidate image was
divided into patch images and appraised based on
intensity and colors. Through multi-instance learning,
the training data was used for model construction, and
the model was verified by test data.
Results:
A total of 83 whole slide images were processed, and
there were 15153 training patches and 1894 validation
patches. The validation performance was 86.99% in the
mean of baseline and 88.84% by method of confusion.
We compared the experimental results and pathologic
reports, and the testing performance was 90.90% for
the diagnosis of tissue eosinophilia and 91.67% for that
of non-eosinophilia.
Conclusion:
We established computer-assisted eosinophil
quantification of the sinonasal histopathology images.
This quantification system can aid in determining the
immunotypes of CRS and making treatment strategies
for CRS.
10:27 am – 10:32 am
Frailty is an independent predictor of post-
operative rescue medication use after endoscopic
sinus surgery
Andrea Lopez, BS
Kolin Rubel, MD
Rory Lubner, MD
Kristen Yancey, MD
Rakesh Chandra, MD, FARS
Naweed Chowdhury, MD, MPH
Justin Turner, MD, PhD, FARS
Vanderbilt University School of Medicine
Introduction:
The modified 5-item frailty index (mFI-5) is a validated
risk stratification tool for predicting adverse outcomes
following surgery. In this study, we sought to use mFI-5
to assess the potential relationship between unhealthy
aging and postoperative endoscopic sinus surgery
(ESS) outcomes.
Methods:
A retrospective review identified patients who
underwent sinus surgery at Vanderbilt between 2014
and 2018. Patients were assessed using the mFI-5,
which is calculated based on the presence of five
comorbidities: diabetes mellitus, hypertension requiring
medication, chronic obstructive pulmonary disease
(COPD), congestive heart failure (CHF), and non-
independent functional status. Multivariate analyses
were performed to assess the association of mFI-5
score on need for rescue oral antibiotics, oral
steroids, and antibiotic irrigations within one year
following ESS, adjusting for relevant potential
confounders.
Results: Four hundred and three patients met inclusion
criteria. Within 6 months of surgery, 312 (77%)
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
35
required rescue antibiotics, 243 (60%) required oral
corticosteroids (OCS), and 31 (8%) required
antibiotic rinses. Increasing mFI-5 scores were
significantly associated with higher rates of
postoperative use of rescue antibiotics (p<0.0001),
OCS (p=0.032), and antibiotic irrigation (p<0.0001).
Frailty scores remained as an independent predictor of
these outcomes after adjustment for age, polyp status,
pre-operative sinonasal outcomes test (SNOT-22)
score, and revision surgery status.
Conclusion: Modified frailty scores may be a useful
clinical tool to predict the risk of postoperative rescue
medication use after ESS.
10:33 am – 10:38 am
Cognition and saccadic eye movement
performance are impaired in chronic rhinosinusitis
David Cvancara, BS
Heather Wood
Ashton Lehmann, MD
Waleed Abuzeid, MD, FARS
Ian Humphreys, DO, FARS
Yoshiko Kojima, PhD
Aria Jafari, MD
University of Washington
Introduction:
Patients with chronic rhinosinusitis (CRS) can have
significant cognitive dysfunction. To date, these data
mostly comprise self-reported measurements. The goal
of this study is to utilize objective measures of cognitive
function, including saccadic eye movement
performance, to characterize brain function in patients
with CRS.
Methods:
Subjects were enrolled from rhinology clinic and
underwent sinonasal evaluation and quality-of-life
assessment using Sinonasal Outcome Test-22 (SNOT-
22). Twenty-four subjects met diagnostic criteria for
CRS, and 23 individuals without CRS served as
healthy controls. Cognitive performance was measured
using the Montreal Cognitive Assessment (MoCA) and
established eye movement paradigms (pro-, anti-,
express-, and delayed-saccade tasks) using a video-
based eye tracker.
Results:
Compared to controls, subjects with CRS performed
worse on the MoCA overall and specifically within the
executive functioning, language, and memory domains
(all p<0.05). Forty-two percent of subjects with CRS
demonstrated at least mild cognitive impairment (MoCA
<26). Compared to controls, CRS patients performed
worse on the anti-saccade task with comparatively less
suppression of pro-saccades (62.2% vs. 77.4% correct,
p<0.05), and this performance correlated with SNOT-22
(r=0.32, p<0.05).
Discussion:
This study is the first to utilize objective, researcher-
administered neuropsychiatric assessments to measure
cognitive performance in CRS. CRS significantly
influences cognition across several domains, including
necessary inhibition of reflexive saccades. These
results correlate with sinonasal-specific measures and
suggest impairment in neural pathways that underlie
response to stimuli and inhibitory control.
10:39 am – 10:45 am
Q&A
10:45 am – 10:50 am
Sleep dysfunction is greater in aspirin-exacerbated
respiratory disease than in other forms of chronic
rhinosinusitis
David Cvancara, BS
Ayush Sharma
Dhruv Sharma, MD
Ian Humphreys, DO, FARS
Aria Jafari, MD
Waleed Abuzeid, MD, FARS
University of Washington
Background:
Studies have previously demonstrated that patients
with chronic rhinosinusitis (CRS) experience significant
sleep dysfunction (SD). However, there is a paucity of
literature on SD in aspirin-exacerbated respiratory
disease (AERD). The purpose of this study was to
evaluate the risk and severity of SD in patients with
AERD and to compare this to SD in CRS with
(CRSwNP) and without nasal polyposis (CRSsNP).
Methods:
This cohort study prospectively enrolled adult patients
with CRSsNP (n=223), CRSwNP (n=39), and AERD
(n=32) from an academic tertiary care rhinology clinic.
SD was evaluated using the Neuro-Quality-of-Life
Sleep Function Short Form (Neuro-QOL). Sleep
dysfunction equal to or greater than “moderate” on the
Neuro-QOL is defined as >1.0 standard deviation from
the normalized population mean. Patient demographic
data and additional QOL data were collected using the
SNOT-22, Patient Health Questionnaire-2, and General
Anxiety Disorder-2 tools. Statistical analysis involved
bivariate analysis with the Student’s t-test and
multivariate logistic regression.
Results:
When adjusted for age, sex, SNOT-22 score,
depression, and cognitive function, patients with AERD
had worse Neuro-QOL scores than patients with either
CRSsNP (OR 0.948 95%CI 0.90, 0.99; p=0.02) or
CRSwNP (OR 0.933 95%CI 0.88, 0.98; p=0.016). The
risk of at least moderate SD was significantly greater in
the AERD population than in the CRSsNP (OR 2.9
95%CI 1.2, 6.2;p=0.008) or CRSwNP (OR 2.7 95%CI
1.02, 7.17;p=0.046) groups.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
36
Conclusion:
Compared to patients with CRSsNP and CRSwNP,
patients with AERD reported significantly greater
deficits in sleep. The risk of SD in AERD was
independent of both disease severity and deficits in
mental health or cognition.
10:51 am – 10:56 am
Clinical characteristics and comorbidities
associated with non-eosinophilic chronic
rhinosinusitis
Tripti Brar, MBBS, MD
Shreya Pusapadi Ramkumar
Christopher Dodoo
Claire Yee
Devyani Lal, MD , FARS
Mayo Clinic in Arizona
Background:
Non-eosinophilic CRS (neCRS) is classically believed
to be less recalcitrant than eosinophilic CRS (eCRS).
Studies on neCRS are limited. We compared clinical
characteristics, histopathology, biomarkers and
comorbidities of neCRS versus eCRS.
Methods:
CRS subjects who underwent ESS at a tertiary care
center between 2011-2018 were studied. A cut-off value
of 10 eosinophil counts per high power field (eos/hpf) in
ethmoidal tissue was used to categorize subjects into
neCRS (<10 eos/hpf) or eCRS (≥10 eos/hpf).
Demographics, SNOT-22 and CT scores, tissue
histopathology, blood absolute eosinophil counts
(AEC), serum IgE, urinary LTE4 levels and
performance of subsequent revision ESS was
compared.
Results:
Of 426 CRS subjects, 191 subjects (44.84%) had
neCRS and 235 (55.16%) had eCRS. Patients with
neCRS were significantly older (Mean: 56.3 vs. 50.6
years; p <0.001) with lower pre-operative SNOT-22
score (Median 39.5 vs. 48.0; p <0.001), Lund-Mackay
CT score (Median 9 vs. 13; p <0.001), overall degree of
inflammation (p <0.001), blood AEC (Median 0.1 vs.
0.3; p <0.001) and asthma (39.5% vs. 63.8%; p
<0.0001). Nasal polyps were noted in 27.7% of eCRS
vs. 67.5% of eCRS (p <0.001). Revision ESS rate was
similar in both cohorts. neCRS tissue had significantly
higher lymphocytic predominance (38.2% vs.17%; p
value <0.001) but no differences for fibrosis or
neutrophilia. No significant difference was detected for
gender, depression status, urinary LTE4, serum IgE
and previous ESS history.
Conclusion:
neCRS affects older individuals. Though neCRS
subjects had lower objective and subjective disease
burden, the need for revision ESS was similar to eCRS.
Further characterization of neCRS and recalcitrant
subtypes is warranted.
10:57 am – 11:02 am
Impact of chronic rhinosinusitis local exacerbations
on granulomatosis with polyangiitis disease
progression and systemic exacerbations
Trisha Shang, BA
David Kaelber, Chief Medical Informatics Officer
Mohamad Chaaban, MD, FARS
Case Western Reserve University
Introduction:
Granulomatosis with polyangiitis (GPA) often presents
with chronic rhinosinusitis (CRS), and patients may
receive CRS medication for managing local sinonasal
flares. Our study aimed to determine the impact of CRS
treatment/flares on GPA systemic exacerbations.
Methods:
We used the TriNetX US Collaborative Network
platform to conduct a retrospective study. We searched
for adults with an ICD encounter diagnosis of CRS with
limited GPA (without renal involvement) and with a
RxNorm/HCPCS code for CRS medication (oral
bactrim, mupirocin, or budesonide). Then, we evaluated
outcomes of systemic exacerbation and disease
progression, including ICD encounter diagnoses of GPA
with renal involvement and acute sinusitis, RxNorm/
HCPCS codes of oral corticosteroid and antibiotic
(Augmentin or oral Azithromycin) prescriptions, and
CPT code of sinus surgery, within 1 month-5 years after
patients met all search criteria.
Results:
After a 1:1 propensity match on sex, ethnicity, race,
and age at index, we had 1,417 patients in each cohort.
We found a significantly greater incidence of ICD
encounter diagnosis of GPA with renal involvement
(RR: 2.20, 95% CI [1.61, 3.01]) and of acute sinusitis
(1.33, [1.02, 1.73]), RxNorm/HCPCS code prescriptions
of oral corticosteroids (2.10, [1.66, 2.66]) and antibiotics
(2.40, [1.92, 3.01]), and CPT code of sinus surgery
(2.40, [1.75, 3.29]), in patients prescribed CRS
medication compared to those who were not.
Conclusion:
Sinonasal exacerbations are associated with greater
incidence of GPA systemic exacerbation and disease
progression. Future studies are required to evaluate the
impact of treating local sinonasal flare ups and their
effect on systemic exacerbations and disease
progression.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
37
11:03 am – 11:08 am
Endotype evaluation of Hispanic/Latinx-American
patients with chronic rhinosinusitis with polyps
Arthur Wu, MD, FARS
Dennis Tang, MD, FARS
Kevin Hur, MD
Aria Jafari, MD
Omar Ahmed, MD, FARS
Philip Chen, MD, FARS
Anna Matthew
Benjamin Tam, Medical Student
Haodong Xu
Luv Amin
David Cvancara, MS4
Cedars-Sinai
Background:
Despite being the largest minority group, Hispanic-
Americans are underrepresented in the scientific
literature in the US. Very little has been presented in
terms of their CRS endotype, presentation, and
outcomes. The goal of this study was to evaluate
clinical factors and pathologic features in Hispanic-
American patients with CRSwNP.
Methods:
A retrospective chart review including five academic
centers was performed to review clinical and pathologic
factors in Hispanic-American patients with CRSwNP.
Preoperative SNOT-22, absolute eosinophil count,
absolute neutrophil count, serum IgE, allergy and
asthma status were reviewed when available. All
patients’ pathology was reviewed for overall degree of
inflammation, eosinophils/high powered field (HPF),
neutrophils/HPF, basement membrane thickening,
subepithelial edema, fibrosis, and fungal elements.
Results:
42 Hispanic-American patients were included in the
study. Using >10 eosinophils/HPF as a cutoff for tissue
eosinophilia, 80% of Hispanic-American patients had
tissue eosinophilia. Preoperative mean SNOT-22 score
was 40.2. Mean absolute eosinophil count was 342
cells/µl with 31% of Hispanic patients having peripheral
eosinophilia (>500 cell/µl). Mean serum IgE levels were
448. Comorbid atopic disease was common in Hispanic
patients (69% allergy, 63% asthma).
Conclusion:
Hispanic-American patients with CRSwNP have a
severe TH2 endotype based on more frequent tissue
and peripheral eosinophilia and common atopic
comorbidities of allergy and asthma. Further studies
are required to investigate this population’s treatment
outcomes and further delineate disease endotypes.
11:08 am – 11:15 am
Q&A
11:15 am – 12:00 pm
Panel: “CRS Endotypes, Subtypes, and
Therapeutics: Where are we and Where are we
Going?”
Moderator: Amber Luong, MD, PhD, FARS
Panelists: Jeremiah Alt, MD, PhD, FARS; Robert
Kern, MD, FARS; Stella Lee, MD; Justin Turner, MD,
FARS
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Broadway Ballroom A
Diversity & Inclusion, Women in Rhinology,
Mentorship, Residents & Fellows Combined Lunch
Program
“Breaking Barriers: Insights on Improving Diversity
and the Pipeline in Medicine:
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD; Kimberly Vinson,
MD
Saturday, September 30, 2023
8:00 am – 12:00 pm
Breakout 2
Skull Base
Broadway Ballroom CD
7:00 am – 8:00 am
Meet the Authors Poster Viewing & Breakfast
Grand View Terrace Foyer, Second Level
Session Chair: Bobby Tajudeen, MD, FARS
8:00 am – 8:30 am
Panel: “Pediatric Skull Base Surgery in the 21
st
Century: Advances and Frontiers”
Moderator: David Gudis, MD, FARS
Panelists: Nithin Adappa, MD, FARS; Garret Choby,
MD, FARS; Zara Patel, MD, FARS
Sponsored by the Pediatric Rhinology Committee
Scientific Oral Presentations: Skull
Base Surgery
Moderators: Mathew Geltzeiler, MD, FARS; Nyall
London, MD, FARS; Peter Papagiannopoulos, MD
8:30 am – 8:35 am
Mutational landscape and predictors of survival in
head and neck mucosal melanoma
Brandon Lehrich, BS
Arash Abiri, MS
Theodore Nguyen
Edward Kuan, MD, FARS
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
38
Background:
Head and neck mucosal melanoma (HNMM) is a rare
and aggressive malignancy most commonly affecting
the sinonasal tract and oral cavity. The genetic profile
remains poorly understood.
Methods:
We interrogated the publicly available American
Association for Cancer Research (AACR) Genomics
Evidence Neoplasia Information Exchange (GENIE)
database (v13.0-public) which is a cancer registry
collecting de-identified clinico-genomic information
across 19 cancer centers. Kaplan-Meier log-rank test
was used to evaluate differences in overall survival
(OS).
Results:
Of the 6,802 melanoma patients, 108 (1.6%) had
HNMM. The average age of the cohort was 65.6 +/-
14.7 years. The average tumor mutational burden
(TMB) was 6.1 +/- 5.2. The 1-, 2-, and 5-year OS rates
were 84.2%, 69.6%, and 47.5%, respectively. The most
common mutations were NRAS (n=19; 17.6%), NF1
(n=15; 13.9%), ROS1 (n=14; 13.0%), TERT (n=11;
10.2%), and BRAF (n=11, 10.2%). Of the 19 patients
with NRAS mutation, 7 (47.4%) had Q61R mutation, 5
(26.3%) had Q61K mutation, 3 (15.8%) had G12A, and
2 (10.5%) had G12C. There were no differences in OS
for NRAS (p=0.66), NF1 (p=0.41), TERT (p=0.26), and
BRAF (p=0.47) mutated vs wild-type patients. However,
ROS1 mutated patients had improved OS as compared
to wild-type (5-year OS: 76.6% vs 41.8%; p=0.023)
patients. Lastly, there was improved OS for patients
with high vs low TMB (5-year OS: 66.7% vs 35.8%;
p=0.026).
Conclusions:
We identify ROS1 mutation, an actionable driver
oncogene, as a predictor of HNMM OS. Overall, our
findings improve the understanding of the somatic
mutational landscape of HNMM.
8:36 am – 8:41 am
Genomic and clinical analysis of olfactory
neuroblastoma
Theodore Nguyen, BS
Benjamin Bitner, Dr.
Brandon Lehrich, BS
Jonathan Pang, BA
Arash Abiri, MS
Sina Torabi, MD
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
Olfactory neuroblastoma (ONB) is a rare, malignant
neoplasm arising from the olfactory neuroepithelium
and affecting the sinonasal tract. The goal of this study
is to characterize the genomic pathogenesis of ONB.
Methods:
The American Association for Cancer Research
(AACR) Genomics Evidence Neoplasia Information
Exchange (GENIE) database (v13.0-public) was
queried for genomic and clinical data. Kaplan-Meier
analyses was performed to determine overall survival
(OS). High tumor mutational burden (TMB) was defined
as ≥5 mutations.
Results:
Of the 562 embryonal tumor samples, 31 (5.52%) were
ONB. 12 samples belonged to female patients (38.7%)
and mean age at time of sequencing was
55.97¬¬±2.53 years. Within these samples, 15
(48.39%) were from primary tumors and 13 were from
metastases (41.94%). 1-, 3-, and 5-year OS was
96.2%, 64.9%, and 43.3%, respectively. The average
TMB was 5.0±0.9. When comparing primary tumors vs.
metastases, there was no significant difference in
number of mutations (p=0.491) or fraction of genome
altered (p=0.65). The three most common mutations
were SMARCA4 (n=3, 9.7%), TP53 (n=3, 9.7%), and
mTOR (n=2, 6.5%). There was one patient (3.3%) that
had both SMARCA4 and TP53 mutations. There were
no differences in OS for mTOR (p=0.501) or SMARCA4
(p=0.310) mutated vs. wild-type patients. However,
TP53-mutated patients had worsened OS when
compared to wild-type (5-year OS: 0% vs. 46.2±16.0%;
p=0.021). When comparing high vs. low TMB, there
were no significant differences in OS (p=0.516).
Conclusion:
Understanding the genomic mutational landscape of
ONB may provide insight on potential therapeutic
targets.
8:42 am – 8:47 am
Genomic mutational analysis and predictors of
survival in nasopharyngeal carcinoma
Benjamin Bitner, MD
Theodore Nguyen, BS
Jonathan Pang, BA
Michael Warn, BS
Arash Abiri, MS
Brandon Lehrich, BS
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
Nasopharyngeal carcinoma (NPC) genetics is poorly
understood limiting development of new effective
therapeutic approaches. The objective of this study is
to report common genetic mutations and impact on
survival.
Methods:
We queried the American Association for Cancer
Research (AACR) Genomics Evidence Neoplasia
Information Exchange (GENIE) database (v13.0-public)
for patient clinico-genomic information and determined
differences in overall survival in patients affected by NPC.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
39
Results:
Of the 2,200 head and neck cancer samples, 107
(4.86%) were NPC. Mean age at time of sequencing
was 51.42±1.32 years. Clinical and sequencing data
included tissue from 37 (34.6%) primary tumors and
from 61 (57%) metastases. Collectively, 1-, 3- and
5-year overall survival (OS) was 93.1%, 60.6%, 40.9%,
respectively. Considering sequencing results, the mean
fraction of the genome altered across samples was
0.19±0.03 with an average tumor mutational burden
(TMB) of 3.94±7.47. When comparing sequenced
tissue from primary tumors and metastases, there was
no difference in number of mutations (p=0.64) or
fraction of genome altered (p=0.66). The three most
common mutations were KMT2D (n=24, 22.4%), TP53
(n=20, 18.7%) and CYLD (n=10, 9.3%). There was no
difference in OS for CYLD mutated vs wild-type
patients (p=0.22). TP53 and KMT2D mutations were
associated with worse OS as compared to wild-type
with a 5-year OS of 0% vs 44.7% (p=<0.001) and
20.5% vs 45.9% (p=0.04), respectively. When
comparing high vs low TMB, there was no significant
difference in OS (5-year OS; 27.8% vs 50.4%; p=0.26).
Conclusion:
NPC is often driven by mutation of tumor suppressor
genes indicating potential targets for future therapeutic
strategies in treating NPC.
8:48 am – 8:53 am
SNOT-22 subdomain outcomes in sinonasal
malignancy: A prospective multi-center study
David Grimm, MS
Daniel Beswick, MD, FARS
Eric Wang, MD, FARS
Nithin Adappa, MD, FARS
Garret Choby, MD, FARS
Mathew Geltzeiler, MD, FARS
Anne Getz, MD, FARS
Ian Humphreys, DO, FARS
Edward Kuan, MD, FARS
Christopher Le, MD, FARS
Peter Hwang, MD, FARS
Background:
Sinonasal quality of life (QOL) after treatment for
sinonasal malignancy (SNM) is poorly characterized.
Our previous work indicates that global sinonasal QOL
improves with SNM treatment. This study aims to
characterize SNOT-22 subdomain outcomes in patients
with SNM.
Methods:
Patients with newly diagnosed SNM were prospectively
enrolled in a multi-center observational patient registry.
Demographics, histopathology, and SNOT-22 scores
were recorded over the pre and post treatment period.
Multivariable regression analysis was used to identify
drivers of variation in SNOT-22 subdomains.
Results:
234 SNM patients underwent treatment with curative
intent, with a mean follow up of 22-months. Rhinologic,
Psychological, and Sleep subdomains improved
significantly vs baseline (all P<0.05) while Extra-Nasal,
and Ear/Facial symptoms did not. Multivariable linear
regression showed that adjuvant chemoradiation was
associated with worse outcomes in Rhinologic
(adjusted odds ratio 2.49 [0.27, 4.72]), Extra-Nasal
(1.85 [0.39, 3.3]) and Ear/Facial (2.47 [0.55, 4.38])
subdomains. Pterygopalatine fossa involvement was
associated with worse outcomes in Rhinologic (3.88
[0.93, 6.96]), Extra-Nasal (1.51 [0.23, 2.78]), Ear/Facial
(3.8 [1.89, 5.70]), and Psychological (2.96 [0.07, 5.85])
subdomains. Positive margins were associated with
worse Psychological outcome (3.98, [0.17-7.79]).
Adjuvant radiation alone was associated with worse
Sleep outcome (1.46 [0.12, 2.81]).
Conclusion:
SNOT-22 improvement in SNM patients after treatment
is driven by Rhinologic, Psychological, and Sleep
subdomains. The degree of improvement is influenced
by chemoradiation, pterygopalatine fossa involvement,
and positive margins.
8:53 am – 9:00 am
Q&A
9:00 am – 9:05 am
Tranexamic acid in endoscopic sinus and skull
base surgery: A systematic review and meta-
analysis
Sarah Khalife, MD
Zahra Abdallah, BHsc, Medical Student
Phillip Staibano, Resident Physician
Kelvin Zhou, Resident Physician
Thomas Boi Vu Nguyen, Rhinology Fellow
Doron Sommer, MD
Objective:
Endoscopic sinus surgery (ESS) and endoscopic skull
base surgery (ESBS) approaches have revolutionized
the management of sinonasal and intracranial
pathology. Maintaining surgical hemostasis is essential
as bleeding can obscure visibility of the surgical field,
thus increasing surgical duration, risk of complications
and procedural failure. Tranexamic acid (TXA) acts to
reduce bleeding by inhibiting fibrin degradation. This
review aims to assess whether TXA improves surgical
field quality and reduces intraoperative blood loss
compared to control.
Methods:
We searched PubMed, MEDLINE, Embase, Web of
Science, and Cochrane Library from inception until
September 1, 2022. Two reviewers independently
screened citations, extracted data, and assessed
methodological quality using Cochrane Risk-of-Bias 2.
Data was pooled using a random effect model, with
continuous data presented as mean difference and
dichotomous data presented as Odds Ratio.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
40
Results:
Seventeen ESS RCTS (n = 1377) and one ESBS RCT
(n = 50) were reviewed. Significant improvement in
surgical field quality was achieved with both systemic
TXA (six studies, p < 0.00001) and topical TXA (six
studies, p = 0.01) compared to control. Systemic TXA
(eight studies) and topical TXA (three studies) both
achieved a significant reduction in intraoperative blood
loss compared to control (p< 0.00001). There were
significant differences in operative times (p < 0.001) but
no significant difference in perioperative outcomes (p =
0.30).
Conclusion:
This meta-analysis demonstrated that utilization of TXA
in ESS can improve surgical field quality and reduce
intraoperative blood loss. TXA use did not result in
increased perioperative complications including
thrombotic events.
9:06 am – 9:11 am
The use of aprepitant to reduce postoperative
nausea and vomiting in endoscopic skull base
surgery
Daniel Lee, MD, FRCSC
Jennifer Douglas, MD
Jeremy Chang
Jadyn Wilensky
Christina Jackson
John Lee, MD
M. Sean Grady
Daniel Yoshor
Michael Kohanski, MD, PhD
James Palmer, MD, FARS
Nithin Adappa, MD, FARS
University of Pennsylvania
Introduction:
Postoperative nausea and vomiting (PONV) are
adverse effects following surgery, which may increase
the risk of complications, particularly in endoscopic
skull base surgery. Aprepitant is a neurokinin-1 receptor
blocker, which reduces PONV in other surgical
disciplines. However, its role in endoscopic skull base
surgery remains unclear. The objective of this study
was to investigate the effect of aprepitant in PONV
following endoscopic skull base surgery.
Methods:
A retrospective chart review between July 2021 and
February 2023 of 221 consecutive patients who
underwent endoscopic transsphenoidal surgery (TSA),
extended endonasal approach (EEA), transcribriform
approach or spontaneous CSF leak repair (sCSF).
Primary outcome was the incidence of PONV.
Secondary outcome measures included the number of
anti-emetic use, length of stay and postoperative CSF
leak.
Results:
Out of 221 patients (114 in aprepitant and 107 in non-
aprepitant), there were 162 in TSA, 34 in EEA, 8 in
transcribriform and 17 in sCSF cohorts. There were no
baseline demographic differences across all the groups.
In the overall cohort, the aprepitant group had a
significantly lower incidence of postoperative vomiting
than the non-aprepitant group (1.8% vs. 21.5%,
p<0.001). This trend was shown similarly in both TSA
and EEA groups. Anti-emetic use decreased with
aprepitant use in the TSA group (p<0.05). There was a
trend towards decreased length of stay with aprepitant
in the EEA group (4.8 vs. 9.8 days, p=0.07).
Multivariate analysis demonstrated aprepitant
decreased the incidence of postoperative vomiting with
odds ratio of 0.064.
Conclusion:
Aprepitant may serve as a useful preoperative
treatment to reduce PONV in endoscopic skull base
surgery.
9:12 am – 9:17 am
Predictors of prolonged length of stay following
intradural endoscopic skull base surgery
Jonathan Pang, BA
Madelyn Frank, BA
Kelsey Roman, BS
Jinho Jung, BS
Arash Abiri, MS
Theodore Nguyen
Benjamin Bitner , MD
Frank Hsu, MD, PhD
Edward Kuan, MD, fARS
University of California, Irvine
Background:
Establishing benchmarks for length of stay (LOS) may
inform strategies to reduce nosocomial infections,
improve resource efficiency, and decrease costs. We
explore factors contributing to postoperative LOS in
intradural endoscopic skull base surgery (ESBS).
Methods:
Retrospective chart review was conducted at a tertiary
academic skull base surgery program including
consecutive adult patients who underwent ESBS with
intraoperative cerebrospinal fluid (CSF) leak and
primary repair between July 2018 and February 2023.
LOS comprised the primary outcome and was
calculated as time between end of anesthesia to
discharge from hospital.
Results:
150 patients were included, with mean LOS of 6.7 ± 9.7
days. LOS did not differ significantly between high-flow
(n=86) and low-flow (n=64) CSF leak cohorts (7.0 ± 8.6
vs. 6.4 ± 11.0 days, p=0.697). Defects of the anterior
cranial fossa (n=24, 8.0 ± 12.7 days), suprasellar
region (n=64, 7.6 ± 9.8 days), sella (n=104, 6.3 ± 8.5
days), and posterior cranial fossa (n=13, 5.1 ± 3.0
days) had variable LOS (p=0.657). On multiple linear
regression, after controlling for numerous patient,
surgical, and postoperative factors, extended approach
(B[95%CI]=4.27[0.91, 7.62]), length of bedrest
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
41
(B=1.80[0.32, 3.29]), postoperative stroke
(B=17.09[7.33, 26.85]), postoperative pneumonia/
aspiration (B=5.07[0.06, 10.08]), and postoperative
hypernatremia (B=4.23[0.25, 8.21]) independently
predicted prolonged LOS.
Conclusion:
With healthcare utilization receiving increased attention,
understanding and mitigating factors that extend LOS
is important. The current study identified surgical
approach, bedrest duration, and certain postoperative
complications as key factors prolonging LOS in
intradural ESBS.
9:18 am – 9:23 am
Quality of life among patients undergoing
endoscopic pituitary gland resection with and
without middle turbinectomy
Narin N. Carmel Neiderman, MD, MSc
Orr Raved
Shay Kaufman
Anat Wengier
Avraham Abergel
TASMC
Introduction:
The endoscopic approach to skull base lesions is
considered less aggressive, and associated to
improved tumor related and nasal related quality of life.
However, there is an ongoing literature debate
regarding the necessity to preserve the middle turbine
during the procedure.
Objective:
The aim of the study was to compare tumor and nasal
related quality of life in patients undergoing endoscopic
endonasal resection of pituitary tumors with or without
middle turbine preservation.
Materials and Methods:
Prospective cohort study of all patients with pituitary
adenomas who underwent trans-sphenoidal surgery at Tel
Aviv Sourasky Medical Center between 2014 and 2021.
Recruited patients completed the Anterior Skull Base
Disease-Specific QOL (ASBS-Q) questionnaire and the
Sinonasal Outcome Test 22 (SNOT-22) questionnaire
prior to surgery and 3-6 months post-operatively.
Results:
Our study included 56 patients, 46 patients underwent
middle turbinectomy and 10 did not. The overall score
difference of pre and post ASBS-Q score did not alter
significantly between both groups (0.15±0.64 among
those who underwent middle turbinectomy vs
0.19±0.74 among those who did not; p=0.87). SNOT-22
score difference also did not alter significantly
(1.54±15.29 vs 3.92±16.84, p=0.32) post operatively.
Conclusion:
We found that middle turbinectomy did not cause
significant deterioration in nasal and tumor related QOL
in the post-operative course.
9:23 am – 9:30 am
Q&A
9:30 am – 9:45 am
Targeted Conversations on Important Topics: Next
Generation Sequencing in Skull Base Surgery
Moderator: Sanjeet Rangarajan, MD, FARS
Panelists: Corinna Levine, MD, FARS; Peter
Papagiannopoulos, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations:
Rhinology Potpourri
Moderators: Charles Ebert, MD, FARS; Edward Kuan,
MD, FARS; Charles Tong, MD, FARS
10:15 am – 10:20 am
Stellate ganglion block for post-COVID-19
parosmia: Does it work?
Bita Naimi, BA
Emily Garvey, BA
Megha Chandna, BS
Alexander Duffy, MD
Stephanie Hunter, PhD
Marc Rosen, MD, FARS
Mindy Rabinowitz, MD, FARS
Elina Toskala, MD, MBA, PhD, FARS
Adam Zoga, MD, MBA
Gurston Nyquist, MD, FARS
David Rosen, MD
Thomas Jefferson University Hospital
Aim:
Evaluate stellate ganglion block (SGB) as a treatment
option for post-COVID olfactory dysfunction (OD) and
parosmia.
Methods:
Retrospective study of patients who underwent
unilateral (SGB1) or bilateral (SGB2) SGB for post-
COVID OD. Patients completed Brief Smell
Identification Tests (BSIT) before and after treatments,
and a post-treatment survey investigating subjective
symptom improvement.
Results:
43 patients with post-COVID OD underwent SGB. 30
patients had pre- and post-SGB BSIT scores (mean
OD duration 1.93 ± 0.52 years); 19 patients completed
surveys (mean OD duration 1.91 ± 0.46 years). Mean
BSIT pre-SGB was 8.10 ± 2.40, post-SGB1 8.76 ±
2.41, and post-SGB2 9.00 ± 1.58, with no significant
change in scores (p=0.224). Subjective parosmia
severity on a scale from 1 (not present) to 10 (worst)
improved from preSGB (8.95 ± 1.18) to SGB1 (6.37 ±
2.73) and to SGB2 (5.70 ± 2.45); differences were
significant from preSGB to SGB1 (p<0.001) and
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
42
preSGB to SGB2 (p<0.001). On a scale of 1 (not
present) to 5 (worst), there was a significant decrease
in distorted tastes (median preSGB 4.0 vs. postSGB
3.0, p=0.003), unpleasant odors in the nose (3.0 vs.
2.0, p=0.0042), unpleasantness of smells (3.0 vs. 2.0,
p=0.012), and number of parosmia triggers (4.0 vs. 3.0,
p=0.002) after the procedure (SGB1 or SGB2). After
SGB, patients reported significantly improved ability to
enjoy food (5.0 vs. 2.0, p=0.001), ability to prepare
meals (4.0 vs. 2.0, p=0.002), weight maintenance (4.0
vs. 2.0, p=0.002), and upkeep of personal hygiene (2.0
vs. 1.0, p=0.008).
Conclusion:
SGB may significantly improve subjective parosmia and
QOL for patients with post-COVID OD. Large placebo-
controlled trials are needed to further investigate this
treatment
10:21 am – 10:26 am
Stellate ganglion block for the treatment of COVID-
19-induced olfactory dysfunction: A prospective
pilot study
Andrew Peterson, MD, MSCI
Brevin Miller, Medical Student
Dorina Kallogjeri, MD
Aara Kukuljan, Manager, Division of Clinical Research
Jay Piccirillo, MD
John Schneider, MD, MA
Lauren Roland, MD, MSCI
Lara Crock, MD
Nyssa Farrell, MD
Washington University School of Medicine/Barnes
Jewish Hospital
Background:
There are few effective treatments for COVID-19-
associated olfactory dysfunction (OD), but anecdotal
evidence and case reports describe success with the
use of stellate ganglion blocks (SGBs). The objective of
this study was to explore the effectiveness and safety
of SGBs for the treatment of persistent COVID-19-
induced OD.
Methods:
In this single-arm, prospective pilot trial, adult
participants with a COVID-19 diagnosis ≥ 12 months
prior to enrollment with OD underwent bilateral SGBs.
Subjects were followed for 1 month after completion of
SGB. The primary outcome measure was the change
in 7-point Likert Clinical Global Impression -
Improvement scale for smell loss. Secondary outcome
measures included change in University of
Pennsylvania Smell Identification Test (UPSIT) and
Olfactory Dysfunction Outcomes Rating.
Results:
Twenty participants were enrolled with a mean (SD)
age of 46 (11) years and a mean (SD) duration of OD
of 21 (5) months. At 1-month, 10 (50%) participants
experienced at least slight subjective improvement in
their OD, 11 (55%) attained a clinically meaningful
improvement in smell identification using the UPSIT,
and 7 (35%) achieved a clinically meaningful
improvement in olfactory-specific QOL. The median
difference between UPSIT scores at baseline and
1-month was 6 (95% CI, 3 to 11), exceeding the MCID
of 4. There were no serious adverse events.
Conclusion:
This study found that sequential SGBs for COVID-19-
associated OD were safe and resulted in modest
improvements in subjective olfaction, odor identification,
and olfactory-specific QOL. A larger, placebo-controlled
trial is warranted to determine the efficacy of SGBs for
COVID-19-associated OD
10:27 am – 10:32 am
Sinonasal pathogenic bacteria in patients with
diabetes mellitus
Trisha Shang, BA
David Kaelber, Chief Medical Informatics Officer
Mohamad Chaaban, MD, FARS
Case Western Reserve University
Introduction:
Diabetes mellitus (DM) is known to affect the
microbiome and lower airway inflammation. Our study
aims to examine how DM can impact the development
of chronic rhinosinusitis (CRS) and its microbiome.
Methods:
We conducted a retrospective study using the TriNetX
US Collaborative Network platform. We searched for
adults that had an outpatient visit noted by CPT codes
who had one or more ICD encounter diagnosis of DM
and ever had an HbA1c ≥ 6.5% in their LOINC code.
We compared them to adults who had an outpatient
visit and were never diagnosed with DM and never had
HbA1c ≥ 6.5%. We evaluated an outcome of CRS
encounter diagnosis by ICD code and detection of
Staphylococcus aureus, Haemophilus influenzae, and
Pseudomonas aeruginosa in the nose or cultured
specimens by LOINC code. All outcomes were 1 month
to 5 years after patients met all search criteria.
Results:
After performing a 1:1 propensity match for sex, age at
index, and race, there were 1,770,623 patients in each
cohort. Those with DM were significantly more likely
than those without DM to have a CRS encounter
diagnosis (Risk Ratio: 1.86, 95% CI [1.84, 1.89]). They
were also significantly more likely to have the presence
of S. aureus (3.96, [3.77, 4.16]) detected in nose
samples, and P. aeruginosa (13.32, [10.38, 17.11]), and
H. influenzae (3.58, [3.01, 4.25]) detected in specimen
samples than those without DM.
Conclusion:
Patients with DM have a greater risk of developing
CRS and S. aureus, P. aeruginosa, and H. influenzae
infection than patients without DM. Further studies are
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
43
needed to determine mechanisms behind the
development of a pathogenic sinonasal microbiome in
patients with DM.
10:33 am – 10:38 am
The Role of CCL19 and atypical cytokine receptor
CCRL1 in chronic rhinosinusitis
Chengetai R. Mahomva, MD
Prince A.B. Minkah
Kristine Smith, MD
Gretchen Oakley, MD, FARS
Richard Orlandi, MD, FARS
Jeremiah Alt, MD, PhD, FARS
Abigail Pulsipher, MD
University of Utah
Background:
Chemokine CCL19 has been shown to predict disease
severity in COVID-19 and treatment response in
rheumatoid arthritis. CCL19 exerts both pro- and anti-
inflammatory effects and can be degraded by receptor
CCRL1. CCL19 is elevated in chronic rhinosinusitis
(CRS) but its role in CRS is unknown. This study seeks
to characterize the gene transcriptional changes of
CCL19, its receptors, and associated cytokines and
their correlations with disease severity in CRS.
Methods:
An established database was examined for patients
with CRS and controls. Controls with asthma and
allergy were excluded. mRNA was extracted from
ethmoid tissues and subjected to multiplex gene
expression analysis. Enrollment Lund-Kennedy, Lund-
Mackay, Sinonasal Outcomes Test 22 (SNOT-22), and
Rhinosinusitis Disability Index (RSDI) scores were
collected. Gene transcripts copy numbers were
compared to controls and correlated to disease
severity.
Results:
Thirty-eight subjects (n=7 control; n=31 CRS) were
included. CCL19, CCRL1, and TNFA were significantly
elevated in CRS compared to controls (p<0.05).
CCL19 expression was positively correlated with IL1B
and TNFA expression (p<0.05). TNFA expression was
positively correlated with SNOT-22 and RSDI scores
(p<0.03). CCL19 expression was positively correlated
with SNOT-22 but did not reach significance (p=0.067).
CCRL1 expression was inversely correlated with RSDI
(p=0.027).
Conclusion:
In CRS, CCL19 and CCRL1 may modulate TNF-α
driven pro-inflammatory signaling cascades and may
be predictive markers of disease severity. Further
mechanistic studies are needed to determine the
functional consequences of CCL19 and CCRL1 and
whether they can be identified as potential therapeutic
targets in CRS.
10:39 am – 10:45 am
Q&A
10:45 am – 10:50 am
Real-world comparison of nasal obstruction
outcome scores between medial flap turbinoplasty
and inferior turbinate submucous resection during
concurrent septorhinoplasty
Milinds Vasudev, BS
Amir Hakimi
Ashley Lonergan
Shannen Guarina
Sina Torabi, MD
Allison Hu
Theodore Nguyen, BS
Edward Kuan, MD, FARS
Brian Wong
University of California, Irvine
Objectives:
To compare longitudinal improvement in nasal
obstruction quality-of-life outcomes between medial flap
turbinoplasty (MFT) and inferior turbinate submucous
resection (SMR) concurrently performed with functional
septorhinoplasty.
Methods:
Retrospective review of a prospectively collected cohort
of patients undergoing functional septorhinoplasty
between 2015 to 2022 at a tertiary academic center.
Outcomes were assessed using the Nasal Obstruction
Symptom Evaluation (NOSE) questionnaire
preoperatively and over 12 months postoperatively.
Results:
373 patients were analyzed with longitudinal NOSE
questionnaires. Of these, 298 underwent SMR and 75
underwent MFT. The proportion of intraoperative
techniques including rim graft, spreader graft, auto-
spreader graft, intradomal sutures, interdomal sutures,
and alar spanning sutures were similar between the
two cohorts (p>0.05). Patients in all surgical groups
had a statistically and clinically significant improvement
in NOSE scores between their preoperative and
postoperative follow-up visits (p<0.001). MFT patients
had higher NOSE scores 1 month post-op (40.0 ± 30.5
vs. 31.0 ± 27.97; p=0.017), but lower scores after 10
months (15.2 ± 13.3 vs. 25.4 ± 23.5; p=0.036).
Similarly, patients in the MFT cohort in primary
rhinoplasty procedures reported higher scores initially
but lower after 10 months (p=0.024). Men in the MFT
cohort reported significantly better NOSE outcomes
than the SMR cohort, as early as 4 months post-
surgery and sustained throughout the follow-up period
(10.6 ± 12.3 vs. 22.6 ± 21.4; p=0.012).
Conclusion:
MFT may offer better long-term nasal breathing
outcomes compared to SMR for functional rhinoplasty
patients based on superior long-term NOSE scores.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
44
10:51 am – 10:56 am
Cadaveric and computed tomography analysis of
the arterial supply and mucosal dimensions of the
anterior ethmoid artery flap
Lane Donaldson, MD
John Craig, MD, FARS
Robert Deeb
Background:
The anterior ethmoid artery (AEA) flap has been
successful for repairing anterior septal perforations, and
has been presumed to be axially based from AEA
branches traversing the cribiform plate (CP). However,
limited evidence supports the flap’s axial supply. The
purposes of this cadaveric and computed tomography
(CT) study were to assess the arterial anatomy from
the CP to the septum, and to determine AEA flap length
to predict ideal flap base width should the flap be
random instead of axial.
Methods:
Ten fresh latex-injected cadavers were utilized for
endoscopic dissection to identify arteries traversing the
CPs on each side. First, arterial trajectories along the
septum from the CP were recorded. Measurements
were then made bilaterally along the septum from the
middle turbinate (MT) axilla to the first dominant artery
traversing the CP. Additionally, 100 sinus CTs were
reviewed to measure AEA flap lengths bilaterally.
Results:
From the 10 cadavers, 20 sides were utilized for
measurements. In all cadavers the AEA arterial
branches coursed along the septum diagonally or
horizontally, and never directly vertically from the CP.
The mean distance from the MT axilla to the first artery
traversing the CP was 1.24 ± 1.93 cm (range=1-1.5
cm). Based on CT, mean AEA flap length was 6.39 ±
5.95 cm.
Conclusions:
Based on the non-vertical courses of AEA septal
branches, the AEA flap is more likely a random
transposition flap. Assuming a 3-4:1 length:width ratio,
a flap base width of 1.5-2.5 cm may be necessary to
supply the AEA flap.
10:57 am – 11:02 am
Posterior nasal nerve ablation for management of
postnasal drip: A single center case series
Daniel Gorelik, Research Fellow
Yuki Yoshiyasu, Resident
Samuel Razmi, Medical Student
Masayoshi Takashima, MD, FARS
Omar Ahmed, MD, FARS
Houston Methodist Hospital
Background:
Postnasal drip (PND) is a common concern among
patients with chronic rhinitis and is multifactorial in
nature. Posterior nasal nerve (PNN) ablation is an
option for chronic rhinitis refractory to medical therapy
to typically treat symptoms of nasal congestion,
rhinorrhea, nasal itching and sneezing. The purpose of
this study is to review the efficacy of PNN ablation
among patients that report PND as their primary
symptom.
Methods:
Patients with chronic rhinitis undergoing PNN ablation
at a single institution were reviewed from January 2022
to January 2023. Patients who reported PND as a
primary concern were included in the case series.
Wilcoxon signed-ranks test was used to compare
patients with SNOT-22 pre- and post-procedure
assessments of PND.
Results:
105 chronic rhinitis patients underwent PNN ablation,
with 37 (35.2%) patients treated for a primary concern
of postnasal drip. Follow-up data was available for 31
patients and median follow up was 51 days (IQR,
42-128). 22 (71.0%) patients underwent radiofrequency
neurolysis and 9 (29.0%) patients underwent
cryotherapy ablation. 25/31 (80.6%) patients noted
subjective improvement at follow up. 11 (35.5%)
patients were refractory to reflux treatment. Ten
patients had pre- and post-procedure SNOT-22
assessments of PND. Mean SNOT-22 PND score
significantly improved during follow-up assessment (4.3
vs. 2.1, p=.006).
Conclusion:
Our experience identified that PND is a primary
concern in a substantial portion of chronic rhinitis
patients and PNN ablation may offer an effective
treatment option. This is the first study to look at the
use of PNN ablation for PND as a primary symptom.
Larger studies are needed to further assess the role of
PNN ablation for PND management.
11:03 am – 11:08 am
Insurance influence and reimbursement on
common rhinological procedures
Tyler Janz, MD
Masayoshi Takashima, MD, FARS
Diane Bernahl, MHA
Michael Yim, MD, FARS
Murugappan Ramanathan, MD, FARS
Omar Ahmed, MD, FARS
University of Texas Medical Branch, Galves
Background:
Rhinology procedures are often reimbursed via
healthcare insurance.
However, healthcare insurance’s role in both the
reimbursement and denial of common rhinology
procedures remains unknown. Thus, the goal of this
study is to better understand both initial denials and
final write-offs of procedures and encounters within an
academic rhinological practice.
Methods:
A retrospective chart review was conducted of patients
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
45
who underwent rhinological intervention at a tertiary
medical center from January 1, 2021 to January 1,
2023. Descriptive statistics and frequencies were then
calculated using SPSS 28.0 (IBM Corporation, Armonk,
NY).
Results:
After analysis, 21,767 procedures and encounters were
identified within the study. Of all rhinological procedures
and encounters, 2293 were initially denied (10.53%
denial rate). In-office procedures accounted for 59.4%
of denials. Final denials resulted in an estimated $190,
956.04 revenue lost. The three most costly denied
procedures were: 1. Posterior Nasal Nerve Ablation
(-$47363.20), 2. Nasal Endoscopy with Debridement/
Polypectomy (-$21456.51), and 3. Diagnostic Nasal
Endoscopy (-$17337.87). Blue Cross-Blue Shield,
Medicare, and AETNA had the highest percentage of
denials for the above procedures.
Conclusion:
This study demonstrates the extremely complex nature
of insurance processing and approval for common
rhinological procedures and encounters. A moderate
percentage of rhinological procedures and encounters
were denied even at a high-volume tertiary center
which accounted for a large loss in revenue. Rhinology
practices must continue to remain knowledgeable of
the changes and effects of insurance reimbursement
on their practice.
11:08 am – 11:15 am
Q&A
11:15 am – 12:00 pm
Panel: “Postoperative Care in Skull Base Surgery:
CPAP, Debridement, Rinses and More!”
Moderator: Mathew Geltzeiler, MD, FARS
Panelists: Nyssa Farrell, MD; Edward Kuan, MD,
FARS; Mindy Rabinowitz, MD, FARS; Bobby Tajudeen,
MD, FARS
Sponsored by the Skull Base and Orbital Surgery
Section
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Broadway Ballroom A
Diversity & Inclusion, Women in Rhinology,
Mentorship, Residents & Fellows Combined Lunch
Program
“Breaking Barriers: Insights on Improving Diversity
and the Pipeline in Medicine:
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD; Kimberly Vinson,
MD
Saturday, September 30, 2023
8:00 am – 12:00 pm
Breakout 3
Business of Medicine/Clinical
Rhinology
Broadway Ballroom GH
7:00 am – 8:00 am
Meet the Authors Poster Viewing & Breakfast
Grand View Terrace Foyer, Second Level
Session Chair: Greg Davis, MD, FARS
8:00 am – 8:30 am
Panel: “Setting Up and Maximizing an ASC for
Success”
Moderator: Douglas Reh, MD, FARS
Panelists: Karen Bednarski, MD, FARS; Leah Hauser,
MD; Michael Sillers, MD, FARS
Sponsored by Rhinologists in Private Practice Section
Scientific Oral Presentations: Sinus Surgery and
Postop Therapies
Moderators: Chadi Makary, MD, FARS; Katie Phillips,
MD; William Yao, MD, FARS
8:30 am – 8:35 am
Outcomes and histopathologic features for chronic
rhinosinusitis macrolide responders
Madelyn Frank, BA
Nyein Nyein Htun, Dr
Beverly Wang, Dr
Edward Kuan, MD, FARS
University of California, Irvine
Background:
Macrolides, though classified as antimicrobial drugs,
are known to have anti-inflammatory properties.
Patients with chronic rhinosinusitis (CRS) without
eosinophilic predominance have been proposed as
potential macrolide responders (MR). The aim of this
study is to evaluate outcomes and histopathological
findings of CRS patients who were MR.
Methods:
Patients that received bilateral comprehensive sinus
surgery for CRS followed by steroid irrigations were
retrospectively reviewed. 10 patients were identified as
potential MR and received low-dose azithromycin for
>6 months. 34 patients were included as controls.
Presumed macrolide response was made based on
tissue eosinophil count <10/HPF and persistent mucus
complaints despite steroid irrigations. Resected sinus
tissue was evaluated using structured histopathology.
Results:
MR were older (54.4±16.9 vs 49.1±17.3; p<0.001) and
had a lower rate of asthma (10% vs 62%; p=0.01).
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
46
There was no difference in gender and smoking history
(p>0.05). Histopathological differences between MR
and controls included tissue eosinophil count (5.3± 8.4
vs 24.5±16.0; p<0.001), basement membrane
thickening (40% vs 79%; p=0.04), subepithelial edema
(4% vs 29%; p=0.03), fibrosis (60% vs 12%; p=0.006),
and eosinophilic aggregates (20% vs 70%; p=0.01).
The MR group had lower preoperative SNOT-22 scores
(39.4 vs 46.2; p<0.001), though there was no difference
in subdomains (all p>0.05). At 12 months
postoperatively, both groups had comparable degree of
subjective improvement (-27.2 vs -27.0, p=0.864).
Conclusion:
Despite initial modest improvement with surgery and
steroid irrigations, MR, who have noted histopathologic
features, eventually achieve comparable outcomes to
other CRS subtypes.
8:36 am – 8:41 am
Outcomes of “full-house” versus limited
endoscopic sinus surgery for chronic rhinosinusitis
patients
Shreya Ramkumar, BS
Tripti Brar, Dr
Claire Yee
Michael Marino, MD, FARS
Amar Miglani, MD
Devyani Lal, MD , FARS
Background:
The extent of endoscopic sinus surgery (ESS) for CRS
is often chosen at the surgeon’s discretion. This study
investigates outcomes from full-house (bilateral
maxillary, ethmoid, sphenoid, and frontal sinusotomy)
vs. limited ESS (anything not full-house) performed by
a single surgeon. We study indications and outcomes
of limited vs. full-house ESS.
Methods:
Adult CRS patients who underwent ESS between 2010
to 2018 were retrospectively reviewed. Demographics,
Lund-Mackay CT scores, SNOT-22 scores,
histopathology, and subsequent revision ESS were
analyzed (SAS version 9.04).
Results:
In the study period, 556 patients underwent ESS; 290
underwent full-house and 266 underwent limited ESS.
Median CT score correlated significantly with
performance of full-house vs. limited ESS (13 vs. 8,
p<0.001). Median SNOT-22 score between full-house
(44) and limited ESS (40) was not clinically different.
SNOT-22 improvement at 6 and 12 months was not
significantly different between cohorts (p=0.22) by
repeated measures ANOVA. Significantly more
CRSwNP patients (62.4% vs. 24.4%, p<0.001)
underwent full-house ESS. Overall, 21 patients (7.2%)
underwent revision ESS in full-house vs. 20 (7.5%) in
limited ESS, a non-significant difference (p=0.9).
Limited ESS patients with eosinophil count <10/high-
powered-field were more likely than full-house (11.5%
vs.5.6%) to undergo revision ESS. Rates of revision
ESS were similar for those undergoing limited vs. full-
house for both CRSwNP (6.2% vs.7.2%) and CRSsNP
(8.0% vs.7.3%).
Conclusion:
CT scores appeared to correlate strongly with the
extent of surgery. With this approach, no significant
differences in SNOT-22 scores and revision rates were
found between those undergoing full-house vs. limited
ESS.
8:42 am – 8:47 am
Factors impacting follow-up care in allergic fungal
rhinosinusitis
Jorge Gutierrez, BA
Sofia Khan, BS
Nikita Chapurin
Rodney Schlosser, MD, FARS
Zachary Soler, MD, FARS
Medical University of South Carolina
Introduction:
Allergic fungal rhinosinusitis (AFRS) is associated with
high rates of revision surgery and requires long term
medical management. The purpose of this study was to
analyze barriers to medical care and follow up in
patients with AFRS.
Methods:
Subjects with AFRS and a chronic rhinosinusitis with
nasal polyps (CRSwNP) comparison were
prospectively recruited for completion of the Barriers to
Care Questionnaire (BCQ) and chart review.
Results:
Fifty-nine AFRS and fifty-one CRSwNP patients
participated. AFRS patients were more likely to be lost
to follow up within 6 months of surgery (35.6% vs.
17.7%, p=0.04) and no-show for at least one
appointment (20.3% vs. 5.9%, p=0.03) compared to
CRSwNP patients. Men with AFRS were more likely to
have a single follow-up visit (37.0% vs. 3.1%, p<0.001)
and be lost to follow-up within 6 months (66.7% vs.
9.4%, p<0.001) than women. There were no significant
differences in the BCQ between groups; however, rate
of questionnaire completion was lower in the AFRS
group than the CRS group (62.7% vs 80.4%, p=0.042).
AFRS patients who did not complete the BCQ were
more likely to be male (63.6% vs. 35.1%, p=0.034), lost
to follow-up (77.3% vs. 10.8%, p<0.0001), and have a
single follow up visit (40.9% vs. 5.4%, p<0.0001).
Decreasing age was associated with increased
likelihood of having a single follow-up visit (odds ratio
1.143, 95% CI 1.022-1.276).
Conclusion:
Young, male AFRS patients are more frequently lost to
follow-up after surgery and less likely to complete
questionnaires assessing barriers to care. Further
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
47
investigation is needed to assess barriers to follow-up
and optimize post-surgical treatment in these at-risk
groups.
8:48 am – 8:53 am
Efficacy of early postoperative debridement in
sinonasal cavity healing after functional
endoscopic sinus surgery: A randomized controlled
trial
Juan Carlos Hernaiz-Leonardo, MD, MSc
Bader M. Alim
Marwan Alqunaee, Dr.
Athenea Pascual, Research Coordinator
Judy Fan
Amin R. Javer, MD, FARS
University of British Columbia
Background:
Postoperative debridement (PD) after functional
endoscopic sinus surgery (FESS) is frequently
recommended and performed to improve the healing
process and prevent scar tissue (ST) formation. PD
can be uncomfortable and painful for patients.
Methods:
This open label randomized controlled trial determined
whether PD decreased ST formation compared to
rinsing alone after FESS. We recruited adult patients
with chronic rhinosinusitis (CRS) undergoing primary
FESS. Patients with secondary causes of CRS, primary
immunodeficiencies, or who underwent limited sinus
surgery (i.e., middle meatal antrostomy) were excluded
from the trial. The primary outcome was the presence
of ST at 3 months post FESS. Secondary outcomes
included middle turbinate (MT) lateralization, need for
in-office ST excisions, and revision surgery.
Results:
Ninety-six patients met inclusion criteria for the trial.
The mean age (SD) was 53(16) years, and 64(68%)
were male. Fifty-three patients were randomized to
early (i.e., within six days) PD and 43 received no
debridement. At three months follow-up, 14(33%) non-
debrided patients developed ST compared to 21(40%)
of PD patients (RR 1.21; 95%CI 0.71 - 2.09; p = 0.48).
Six (14%) non debrided patients had MT lateralization
compared to 13(24%) PD patients (RR 1.76; 95%CI
0.73 - 4.23; p = 0.21). Five (12%) non-debrided
patients required an in-office intervention compared to
10(19%) of PD patients (p = 0.35). One patient in the
no-debridement arm required revision FESS compared
to two patients in the PD group (p = 0.74).
Conclusion:
PD does not reduce the incidence of ST formation after
FESS. If PD is necessary, we would advise against
aggressive instrumentation given the high incidence of
ST postoperatively.
8:53 am – 9:00 am
Q&A
9:00 am – 9:05 am
The effect of low-dose long-term doxycycline on
postoperative outcomes in patients with
eosinophilic chronic rhinosinusitis
Jin Young Min, MD, PhD
Hye Kyu Min
Hyun Ji Lee
Suk Ju Ryu
Kyung Hee University School of Medicine
Objective:
Doxycycline (Dc) is a broad-spectrum bacteriostatic
antibiotic of the tetracycline class, which also has anti-
inflammatory action including reduction of ECP and
MMP-9, and antibiotic activity against S.aureus. The
purpose of this study was to investigate the effect of Dc
on postoperative outcomes in CRS patients.
Methods:
Of the CRS patients who underwent ESS from 2020 to
2021 December, 43 adult patients (18 patients taking
Dc after ESS for average 12weeks [200mg loading
dose, then 100mg daily] and 25 patients without Dc)
showing eosinophilic CRS were enrolled in this study.
Subjective symptoms (SNOT-22), postoperative
endoscopic scores (Lund-Kennedy score), and
olfactory outcome were compared between Dc-taking
group and Dc-free group to investigate the effect of Dc
on postoperative outcomes.
Results:
Compared to patients without Dc, there was a
significant improvement in total scores of SNOT-22 in
patients with Dc postoperatively (27.3±5.4 vs 18.7±7.7,
P=0.04). When we assessed 22 individual symptoms,
statistically significant decreases were found in
symptoms including post-nasal discharge and cough
(all, P<0.05). Additionally, patients with Dc had
significantly better outcomes in postoperative
endoscopic scores regarding mucosal edema,
compared to those without Dc (P=0.03). However, no
significant differences were observed in postoperative
olfactory outcomes between the two groups.
Conclusions:
Doxycycline may have a beneficial role for
postoperative disease control status in eosinophilic
CRS.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
48
9:05 am – 9:10 am
High dose ciprofloxacin and azithromycin sinus
stent for the treatment of chronic rhinosinusitis
Do-Yeon Cho, MD
Dong Jin Lim, PhD
Daniel Skinner, BS
Shaoyan Zhang, PhD
Jessica Grayson, MD
Bradford A. Woodworth, MD, FARS
University of Alabama at Birmingham
Background:
Previously, a novel double-coated sinus stent
containing ciprofloxacin (CPF, inner layer) and
azithromycin (AZT, outer layer) (CASS) was developed
but released drug concentrations were found to be
insufficient for clinical usage. This study aims to
improve drug release of CASS by increasing the
concentrations of the two drugs and to assess its safety
in the preclinical rabbit model.
Methods:
To create the CASS with 2mg CPF and 5mg AZT, dip-
coating was used. Scanning electron microscopy
(SEM) confirmed a uniformed double coating and
allowed for visualization of the release patterns of both
drugs, which were assessed over 14 days in saline
solution. The safety of the CASS was addressed using
the preclinical rabbit model through evaluating nasal
endoscopy, histology, and biomarkers before and after
CASS placement.
Results:
SEM confirmed the uniformity of the dual coating of
CPF and AZT and thickness (µm) was found to be
14.7+/-2.4 and 28.1+/-4.6, respectively. The inner
coated ciprofloxacin showed a sustained release over
14 days (release %) when soaked in saline solution
(Day 7, 86.2+/-3.4 vs. Day 14,99.2+/-5.1, n = 3). In vivo
analysis showed that after seven days, 53.1+/-8.2% of
CPF and 44.4+/-3.4% of AZT were released into the
sinus (n = 3). There were no significant differences in
body weight, white blood cell counts, and total protein/
albumin levels before and after CASS placement. Mild
subepithelial edema was noticed in the medial wall of
maxillary sinuses with CASS placement.
Conclusion:
These findings suggest that the CASS stent is an
effective method for delivering therapeutic levels of
antibiotics for CRS. Further studies are needed to
validate the efficacy of the stent in a preclinical model.
9:10 am – 9:15 am
Quantification of retained budesonide dose from
high-volume saline irrigation in post-operative
chronic rhinosinusitis
Paige Shipman, MS1
Kristine Smith, MD
Bhuvanesh Yathavan
Amarbir Gill, MD
Chelsea Pollard
Venkata Yelleppedi
Hamidreza Ghandehari
Abigail Pulsipher, Dr.
Jeremiah Alt, MD, PhD, FARS
University of Utah
Background:
Budesonide high volume saline irrigations (HVSI) are
used ubiquitously to treat chronic rhinosinusitis (CRS)
due to improved sinonasal delivery and efficacy
compared to intranasal corticosteroids sprays. The off-
label use of budesonide is assumed to be safe, with
several studies suggesting the systemically absorbed
dose of budesonide HVSI is low. However, the actual
dose of budesonide to the sinonasal cavity following
HVSI is unknown. The objective of this study was to
further quantify the retained dose of budesonide HVSI.
Methods:
Adult patients with CRS who had undergone
endoscopic sinus surgery (ESS) and had been
prescribed budesonide HVSI were enrolled in a
prospective, observational cohort study. Patients
performed budesonide HVSI (0.5 mg dose) under
supervision in an outpatient clinic and the irrigation
effluent was collected. High-performance liquid
chromatography (HPLC) was used to determine the
dose of budesonide retained after HVSI.
Results:
Twenty-four patients met inclusion criteria. The average
retained dose of budesonide across the cohort was
0.221 mg (SD=0.087, 42%). Increased time from ESS
significantly impacted the retained dose, with those <90
days day post-ESS retaining 56% of administered
budesonide and those >90 days post ESS retaining
32% (p=0.0004).
Conclusion:
The retained dose of budesonide HVSI was found to be
significantly higher than previously estimated and
decreases with time since ESS. Given that budesonide
HVSI is a cornerstone of care in CRS, defining the
retained dose and the potential systemic implications is
critical to understanding the safety of budesonide HVSI.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
49
9:15 am – 9:20 am
Medication adherence with intranasal corticosteroid
irrigations
Jorge Gutierrez, BA
Christian Shannon
Nikita Chapurin, MD
Rodney Schlosser, MD, FARS
Zachary Soler, MD, MSc, FARS
Medical University of South Carolina
Introduction:
The purpose of this study was to investigate real world
adherence to intranasal corticosteroid irrigations using
pharmacy data and assess factors associated with low
adherence.
Methods:
Patients undergoing treatment with corticosteroid
irrigations for any diagnosis during a 2-year period
were prospectively recruited. Subjects completed a
one-time set of questionnaires including the Barriers to
Care Questionnaire (BCQ), 22-item Sino-Nasal
Outcome Test (SNOT-22), and a questionnaire
assessing their experience with corticosteroid
irrigations. Pharmacy data was used to calculate the
Medication Possession Ratio (MPR), a measure of
medication adherence graded from 0 to 1, with 1
indicating the patient possessed the medication 100%
of days in an observed period.
Results:
Seventy-one patients were enrolled. Patients diagnoses
included chronic rhinosinusitis (CRS) without nasal
polyps (n = 37), CRS with nasal polyps (n = 24), or a
non-CRS diagnosis, most commonly chronic rhinitis (n
= 10). The MPR for the overall group was 0.44 ± 0.33.
Just 9.9% of patients had a perfect MPR of 1. Despite
low MPR, only 19.7% of patients reported problems
taking the medication when directly asked. Lower
education resulted in lower MPR (unstandardized B =
0.065, p = 0.046). Increasing BCQ score, indicating
higher barriers to care, was associated with lower MPR
(unstandardized B = –0.010, p = 0.033). The lower the
MPR, the worse patient SNOT-22 scores
(unstandardized B = -15.980, p = 0.036).
Conclusion:
Adherence to corticosteroid irrigations was low and
patients underreported issues with their medication.
Education and barriers to care were associated with
lower adherence which, in turn, was associated with
worse sinonasal quality of life.
9:20 am - 9:25am
Evaluation of LYR-220 corticosteroid matrices at
week 24 from the BEACON study in CRS
Brent Senior, MD, FARS
Vineeta Belanger, PhD
Randall Ow, MD, FARS
M. Scott Major
Stacey Silvers, MD, fARS
Jeffrey Rosenbloom, MD
Lindsay Brayton, Clinical Project Manager
Marina Mihova
Ela Sajjadi, Clinical Research Scientist
Richard Nieman
Robert Kern, MD, FARS
Background:
Endoscopic sinus surgery often fails to directly manage
the underlying inflammation in chronic rhinosinusitis
(CRS), resulting in symptom recurrence within the first
year following surgery in a significant number of
patients. Thus, there is a need for long-acting, local,
anti-inflammatory treatments for these patients. LYR-
220, a corticosteroid matrix being developed to provide
up to 24 weeks of treatment for CRS patients who have
had prior ethmoid surgery, showed promising early
feasibility data in the six patients enrolled in the
uncontrolled Part 1 of the Phase 2 BEACON study.
Here we report the primary analysis of safety and
efficacy of LYR-220 through week 24 from the
randomized, blinded, controlled Part 2 of the BEACON
study.
Methods:
Forty-two symptomatic adult subjects with CRS who
had prior bilateral ethmoidectomy were successfully
enrolled in the multicenter, blinded, randomized,
controlled Part 2 of the two-part BEACON study.
Subjects were randomized 1:1 to receive bilateral
administration of LYR-220 or sham-procedure. Primary
analysis from the 24-week treatment period included
summarization of adverse events and analyses of
change from baseline in SNOT-22 and the composite
score of the 3 cardinal symptoms of CRS (3CS; nasal
blockage, nasal discharge, and facial pain) through
week 24.
Results:
To be presented at the 69th Annual Meeting of the
ARS.
Conclusions:
To be presented at the 69th Annual Meeting of the
ARS.
9:25 am – 9:30 am
Q&A
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
50
9:30 am – 9:45 am
Targeted Conversations on Important Topics:
Correct Coding for Office-Based Rhinology Surgery
– Do’s and Don’ts
Moderator: R. Peter Manes, MD, FARS
Panelists: Seth Brown, MD, FARS; Toby Steele, MD
9:45 am – 10:15 am
Break with Exhibitors
Scientific Oral Presentations:
Diagnosis of Rhinosinusitis and QOL
Measures
Moderators: Jean Kim, MD, FARS; Victoria Lee, MD,
FARS; Mindy Rabinowitz, MD, FARS
10:15 am – 10:20 am
Development and validation of the sinonasal
endoscopic score (SINES) for chronic
rhinosinusitis
Juan Carlos Hernaiz-Leonardo, MD, MSc
Bader M. Alim
Athenea Pascual, Research Coordinator
Khalid Aldossari
Judy Fan
Saada Alsaleh, MBBS
Amin R. Javer, MD, FARS
University of British Columbia
Background:
Although there are several endoscopic grading systems
for chronic rhinosinusitis (CRS), they are limited in their
range and applicability. We aimed to develop and
validate a SiNonasal Endoscopic Score (SiNES)
applicable to all CRS subtypes and investigate its
correlation with patient-reported outcome measures
(PROMs).
Methods:
We recruited 79 CRS patients from two referral centres
from September 2021 to February 2022. Each patient
underwent a sinonasal endoscopy and completed
multiple PROM questionnaires, including SNOT-22 and
symptoms-specific VAS scores. Videos were graded
using the SiNES and modified Lund-Kennedy (MLK)
scores by three independent rhinologists.
Inter-rater and test-retest reliability were assessed via
the Intraclass correlation coefficient (ICC). SiNES and
MLK scores were correlated with PROMs using a
Spearman correlation.
Results:
The mean (SD) age was 54 (15) years, and 41 (51%)
were female. Inter-rater reliability was excellent for the
SiNES (ICC [95% CI]: 0.91 [0.87 to 0.94]) and good for
the MLK score (ICC [95% CI]: 0.82 [0.73 to 0.88]). Test-
retest reliability was excellent for both systems (ICC >
0.9 for all reviewers). No correlation was seen between
endoscopic scores and SNOT-22 or VAS scores.
However, olfactory cleft edema assessed using the
SiNES system was moderately correlated with self-
reported olfactory loss (rho 0.44, p < 0.001).
Conclusions:
The SiNES system is an accurate and reliable grading
framework applicable to any type of CRS. It can be
utilized in clinical and research settings and improves
upon previously published systems.
10:21 am – 10:26 am
Patient perspectives on recall period and response
options in patient-reported outcome measures for
chronic rhinosinusitis symptomatology: An
international multi-centered study
Ahmad Sedaghat, MD, PhD presented by Katie
Phillips, MD
Armo Derbarsegian
Victor Yu
Ahmed Alsayed, MBBS
Benjamin Bitner , MD
David Liu, MD
Sven Schneider
Sarah Adams
Firas Houssein
Zoe Walters
Sidhant Tripathi, Medical Student
University of Cincinnati College of Medicine
Background:
Existing patient-reported outcome measures (PROMs)
for chronic rhinosinusitis (CRS) use a variety of recall
periods and response scales to assess CRS symptom
burden. The global perspectives of CRS patients
regarding recall periods and response scales for CRS
PROMs are unknown.
Methods:
This was a multi-center, cross-sectional study recruiting
461 patients from sites across the United States, Saudi
Arabia, New Zealand, and Austria. Participants chose
which CRS symptom recall period (1 day, 2 weeks, 1
month, >1 month) was most reflective of their current
disease state and upon which to best base treatment
recommendations (including surgery) upon.
Participants also chose which of six response scales
(one visual analogue scale and five Likert scales
ranging from 4–8 items) was easiest to use,
understand, and preferred.
Results:
A plurality of participants (40.0%) felt the current state
of their CRS symptoms was best reflected by a 1
month recall period. However, most patients (56.9%)
preferred treatment recommendations to be determined
by symptoms experienced over a >1 month period.
The four- and five-item Likert scales were the easiest to
use (26.2% and 25.3%, respectively) and understand
(23.6% and 26.6%, respectively). The five-item (26.4%
rating it most preferred and 71.0% rating it preferred)
and four-item Likert (22.5% rating it most preferred and
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
51
56.4% rating it preferred) response scales were also
most preferred.
Conclusion:
Future PROMs for CRS symptoms should consider
assessment of symptoms over a one-month period and
use a four- or five-item Likert response scale to reflect
global patient preferences.
10:27 am – 10:32 am
The surprising impact of priming on the SNOT-22
Ibtisam Mohammad, MD
Stack Taylor, Student
Meghan Nicole Norris
Meredith Alexandria Meyer, Student
Sulgi Kim, Student
Adam Kimple, MD, FARS
Abdullah Zeatoun, Researcher
Cristine N. Klatt-Cromwell, MD
Charles Ebert, Jr., MD, MPH, FARS
Brian D. Thorp, MD, FARS
Brent A. Senior, MD, FARS
UNC
Introduction:
Priming is a well-recognized phenomenon, impacting all
facets of our lives. We are moved to react to situations
based on subconscious cues in the environment. Well
known in the world of marketing, it is less studied in
medicine, and in particular, in how patients perceive
their disease, and how standardized disease-specific
quality of life forms may be impacted.
Methods:
206 consecutive patients with chronic rhinosinusitis
(CRS) and CRS with nasal polyps and chronic rhinitis
were blinded and randomized to be positively primed
(103)or negative primed (103)prior to filling out the
SNOT 22. Positively primed patients were administered
text emphasizing the eminently treatable nature of CRS
and how well people can do. Negatively primed
patients read a description of the marked disability CRS
causes, and possible complications of untreated
disease.
Results:
Groups were matched in age and sex. Median SNOT
22 score in the negatively primed group was 49 and in
the positively primed group 22, a significant difference
of 27 points (p<0.001).
Discussion/Conclusion:
Psychological priming, both negative and positive, has
significant impact on how patient’s fill out the SNOT-22.
Studies utilizing the SNOT-22 as an outcome measure
must take care to minimize this effect.
10:33 am – 10:38 am
Nasal symptoms, medication usage, nasal
endoscopy and patient perspectives as
determinants of physician assessment of chronic
rhinosinusitis control
Ahmad Sedaghat, MD, PhD presented by Katie
Phillips, MD
David Caradonna, MD, FARS
Rakesh Chandra , MD, FARS
Christine Franzese, MD, FARS
Stacey Gray, MD, FARS
Ashleigh Halderman, MD, FARS
Claire Hopkins, MBChB, PhD
Edward Kuan, MD, FARS
Jivianne Lee, MD, FARS
Edward McCoul, MD, FARS
Erin O’Brien, MD, FARS
University of Cincinnati College of Medicine
Background:
Herein, we identify CRS manifestations associated with
how rhinologists assess CRS control, with a focus on
patient perspectives (patient-reported CRS control).
Methods:
Fifteen rhinologists were provided with real-world data
from 200 CRS patients. Rhinologists first classified
patients’ CRS control as “controlled”, “partly controlled”,
and “uncontrolled” using 7 CRS manifestations
reflecting European Position Paper on Rhinosinusitis
and Nasal Polyps (EPOS) CRS control criteria (nasal
obstruction, drainage, impaired smell, facial pain/
pressure, sleep disturbance, use of systemic
antibiotics/corticosteroids in past 6 months, and nasal
endoscopy findings) and patient-reported CRS control.
They then classified patients’ CRS control without
knowledge of patient-reported CRS control.
Results:
CRS control classification was highly consistent across
rhinologists. Rhinologist-assessed CRS control agrees
with patient-reported CRS control significantly better
when rhinologists have knowledge of patient-reported
CRS control than not (kw=0.736 vs. kw=0.554,
p<0.001). Patient-reported CRS control, nasal
obstruction, drainage, and endoscopy findings were
most greatly associated with rhinologist-assessed CRS
control. Rhinologist-assessed control weakly agreed
with EPOS guidelines. Rhinologists classified CRS as
more controlled than EPOS guidelines in almost 50%
of cases.
Conclusions:
This study directly demonstrates the importance of
patient-reported CRS control as a dominant influence
on rhinologists’ CRS control assessment. Knowledge
of patient-reported CRS control may better align
rhinologists’ CRS control assessments and treatment
decisions with patients’ perspectives.
10:39 am – 10:45 am
Q&A
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
52
10:45 am – 10:50 am
Variation in computed tomography opacification in
sinus disease: A snapshot in time
Glen D’Souza, MD
Thomas Jefferson University Hospital
Aim:
To investigate the variability in paranasal sinus
opacification on serial CT scans in patients with chronic
rhinosinusitis (CRS) or recurrent acute rhinosinusitis
(RARS).
Methods:
A retrospective longitudinal study involving adult
patients who underwent functional endoscopic sinus
surgery (ESS) for CRS or RARS and had at least 2
preoperative CT scans of the paranasal sinuses were
included. We excluded patients with prior ESS or
interval ESS between scans. We graded the 1st (CT1)
and 2nd CT (CT2) images using Zinreich modified
Lund-McKay staging system (ZLMS) and assessed the
change in overall and individual sinus scores between
time points.
Results:
Ninety-five patients were included with a median (IQR)
age of 51.9 (31.7) years and 59 (62.1%) females. The
median (IQR) time interval between imaging studies
was 103 (329) days, and the median (IQR) change in
ZLMS was 3.0 (7.5) between time points. Overall, 28
(29.5%) patients showed an interval change in their
overall ZLMS between time points with a median (IQR)
change of 5.0 (7.3). On assessment of individual sinus
scores, 83 (87.4%) patients had a change in score
between time points with 19 (20.0%) patients having a
score change of 2. On comparison of CT 1 and 2, 35
(36.8%) patients showed change from some to no
opacification within a sinus while 30 (31.6%) showed
change from no opacification to some opacification
within a sinus.
Conclusions:
CT scans provide valuable information on the state of
sinuses on the day they were taken, but the pathology,
such as mucosal thickening and opacification change
from day-to-day. While vital for surgical planning, CT
scans should not be the sole indicator for
recommending ESS or determining extent of surgery for
sinonasal disease.
10:51 am – 10:56 am
Determining the minimal clinically important
difference for the questionnaire of olfactory
disorders in people with Cystic Fibrosis and factors
associated with improvement after highly effective
modulator therapy
Jessa Miller, MD
Jennifer Taylor-Cousar, Professor
Jonathan Overdevest, MD
Aastha Khatiwada, Assistant Professor
David Gudis, MD, FARS
Jeremy Tervo, Medical Student
Emily DiMango, Professor
Claire Keating, Associate Professor
Douglas Li, Associate Professor
Jeremiah Alt, MD, PhD, FARS
Daniel Beswick, MD, FARS
University of California, Los Angeles
Introduction:
Olfactory dysfunction (OD) is a common comorbidity in
people with cystic fibrosis (PwCF). The Questionnaire
of Olfactory Disorders-Negative Statements (QOD) is a
validated olfactory outcome measure. The QOD
minimal clinically important difference (MCID) and
factors associated with improvement after highly
effective modulator therapy (elexacaftor/tezacaftor/
ivacaftor (ETI)) have not been determined for PwCF.
Methods:
Prospective observational data was pooled from 7
institutions evaluating PwCF and chronic rhinosinusitis
(CRS). QOD scores and disease characteristics were
assessed. To evaluate internal consistency and
calculate the MCID, Cronbach’s alpha and 4
distribution-based methods were employed,
respectively. For participants who enrolled prior to
starting ETI, QOD scores were also obtained both at
baseline and after ETI initiation. We used multivariable
regression to identify factors associated with QOD
improvement after ETI.
Results:
This study included 123 PwCF, 65 of whom received
ETI. Mean QOD score at baseline for all participants
was 6.5 (standard deviation (SD)=8.0). Mean
Cronbach’s alpha was >/=0.90. The mean MCID
calculated via distribution-based methods was 3.7
points. Of the 65 PwCF who received ETI, the mean
QOD score after ETI was 4.1 for the cohort (SD=5.8).
After ETI, QOD score improvement (decrease)
surpassed the MCID in 22% of participants (14/65).
Worse baseline QOD scores and presence of nasal
polyps were associated with improved QOD scores
after ETI (both p<0.035).
Conclusion:
QOD scores have strong internal consistency among
PwCF. QOD scores are relatively low and have a mean
MCID of 3.7 in PwCF. Worse baseline QOD scores and
nasal polyps were associated with improvement after
ETI.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
53
10:57 am – 11:02 am
Optimization of diagnostic and procedural codes to
identify patients with acute invasive fungal sinusitis
Marie-Ange Munyemana, BA
Omar Ahmed, MD, FARS
Dorina Kallogjeri, MD
Lauren Roland, MD
Washington University in St. Louis
Introduction:
Acute invasive fungal sinusitis (IFS) is a rare disease
with high mortality. Research on IFS has been limited
to small case series and the absence of a designated
international classification of disease code (ICD) has
hindered the use of administrative databases. This
study proposes a novel method to accurately identify
IFS cases using diagnostic and procedural codes
complimented by medications.
Methods:
We identified IFS patients from 2018 to 2022 using
Washington University of St. Louis’s pathology
database. Combinations of diagnostic and procedural
codes were used to query medical records through
EPIC’s data exploration tool, Slicer Dicer. Identified
cases were refined by combination of diagnostic codes
and medications to optimize diagnostic accuracy. Each
iteration of this model was compared to pathology
database. Sensitivity, specificity, and predictive value
were evaluated.
Results:
A total of 44 pathology proven cases were identified.
The highest performing model for detecting IFS was an
algorithm requiring immunocompromised, sinusitis, and
fungal infection ICD codes, presence of sinus surgery
codes and systemic antifungal for 10 days following
sinus surgery, or until time of death. This optimized
model had a positive predictive value of 92%(80%-
98%), classified positive cases with sensitivity of
80%(66%-84%) and negative cases with specificity of
88%(72%-96%).
Conclusion:
Individuals with IFS can be identified with high
sensitivity and specificity by optimizing diagnostic and
procedural codes with duration of antifungal
administration. This model can be applied to large
database studies with high accuracy and is
generalizable for identifying disease states for other
conditions that lack designated ICD codes.
11:03 am – 11:08 am
Impact of recurrent acute rhinosinusitis on quality
of life
Chadi Makary, MD, FARS
Jack Dewey, MD
Zayd Al-Asadi, BS
Dominic Lombardo, BS
Hassan Ramadan, MD, FARS
West Virginia University
Background:
Recurrent sinusitis is a common reason for referral to
otolaryngologists. Differential diagnosis includes
chronic rhinitis (CR), recurrent acute rhinosinusitis
(RARS), and chronic rhinosinusitis (CRS).
Goal:
To study the impact of RARS on the quality-of-life
(QoL) of patients.
Materials and methods:
Cross sectional analysis of patients referred to West
Virginia University from August 2020 to October 2022
for complaints of recurrent/chronic sinusitis was
performed. These patients were divided into RARS,
CRS, or CR according to published guidelines.
Patients’ characteristics, endoscopy scores, and SNOT-
22 scores were collected at their presentation.
Results:
80 patients with RARS were compared to 336 CRS,
and 530 CR patients. Patients with RARS had similar
age to CRS and CR patients (48.8 vs 49.9 vs 46 years
respectively, p=0.237), and were more likely to be
female (72.5% vs 49.4 % vs 64.5% respectively,
p=0.02). Median endoscopy scores in RARS patients
were smaller than CRS but higher than CR (0
[IQR=3,0] vs 4 [IQR=6,3] vs 0 [IQR=0,0]; p<0.0001).
Total SNOT-22 scores in RARS patients were similar to
CRS patients but higher than CR patients (45.9+/-17.8,
vs 41.7+/-20.9, vs 36.9+/-18.5 respectively, p=0.03).
RARS patients had similar rhinological and
extrarhinological domains to CRS patients but worse
than CR patients (p=0.038). Ear/facial domain in RARS
was worse than both CRS and CR patients (p=0.0009).
There were no differences in the sleep and
psychological domains among the three groups.
Conclusion:
QoL in RARS patients is affected similarly to CRS
patients although the objective burden of disease in
these patients is lower.
11:08 am – 11:15 am
Q&A
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
54
11:15 am – 12:00 pm
Panel: “How to Build a Rhinology Clinical Niche in
a Comprehensive ENT Practice”
Moderator: Greg Davis, MD, FARS
Panelists: Mary Ashmead, MD; Michael Cruz, MD,
FARS; Christopher Davis, MD; Michael Setzen, MD,
FARS
Sponsored by Rhinologists in Private Practice Section
12:00 pm – 1:00 pm
Lunch with Exhibitors
12:00 pm – 1:00 pm
Broadway Ballroom A
Diversity & Inclusion, Women in Rhinology,
Mentorship, Residents & Fellows Combined Lunch
Program
“Breaking Barriers: Insights on Improving Diversity
and the Pipeline in Medicine:
Moderator: Troy Woodard, MD, FARS
Panelists: Andre Churchwell, MD; Kimberly Vinson,
MD
Saturday, September 30, 2023
1:00 pm – 5:00 pm
General Session
Broadway Ballroom GHJK
1:00 pm – 1:15 pm
ARS Business Meeting and Presidential Citations
Sarah Wise, MD, FARS; Michael Stewart, MD, FARS;
Pete Batra, MD, FARS
1:15 pm – 2:00 pm
Hwang Family Lectureship
“The Meaningfulness of Paying It Forward: My
40-Year Journey”
Introduction: Richard Orlandi, MD, FARS
Guest Speaker: Donald Lanza, MD, FARS
Scientific Oral Presentations: Nasal
Polyps and Biologics
Moderators: Elisa Illing, MD, FARS; Kenneth
Rodriguez, MD; Abtin Tabaee, MD, FARS
2:00 pm – 2:05 pm
Medication use for chronic rhinosinusitis with
nasal polyps (CRSwNP) pre and post dupilumab
Emily Garvey, BA
Bita Naimi, BA
Alexander Duffy, MD
Chase Kahn, MD
Douglas Farquhar, MD
Marc Rosen, MD
Mindy Rabinowitz, MD
Damaris Pena Evertz, MD
Jessica Most, MD
Elina Toskala, MD, MBA, PhD, FARS
Gurston Nyquist, MD, FARS
Introduction:
This study examines the impact of dupilumab on total
medication use for patients with chronic rhinosinusitis
with nasal polyposis (CRSwNP) and comorbid asthma.
Methods:
Retrospective review of patients with CRSwNP and
asthma at Thomas Jefferson University Hospital
(TJUH). Patients 18 years > and treated at TJUH for at
least one-year pre and post dupilumab initiation were
included. Outcome measures included inhaled
corticosteroid dosage, oral steroid dosage, topical/oral
antibiotics, nasal steroid sprays/rinses, and leukotriene
receptor antagonists (LTRA).
Results:
40 patients met inclusion criteria. The average age at
the time of biologic therapy initiation was 50.81 +/-
16.02 years. 32.5% of the cohort was male. In the year
after dupilumab initiation, patients required significantly
fewer oral steroids for asthma (pre: 800.95 mg +/- 1285
vs. Post: 393.59 mg +/- 932.52, p=0.02) and CRS
exacerbations (pre: 511.67 mg +/- 623.70 vs. Post:
91.03 mg +/- 155.76, p<0.001). Patients also required
fewer antibiotic prescriptions for CRS exacerbations
(3.08 prescriptions +/- 2.45 vs. 0.85 prescriptions
+/-1.29, p<0.001). Fewer patients required leukotriene
receptor antagonists (LTRA) p=0.01 and nasal steroid
sprays (p=0.05). There was no difference in steroid
rinses (p=0.59), or topical antibiotics(p=0.52). There
was also no difference in the number of patients on
high, medium, or low dosed inhaled corticosteroids
(p=0.54).
Conclusion:
Initiation of dupilumab for patients with CRSwNP and
asthma had a significant impact on medication use
including oral antibiotics, LTRA, and oral steroids for
both indications. This is the first study to examine
comprehensive medication use in patients with
CRSwNP and asthma while on dupilumab.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
55
2:06 pm – 2:11 pm
Nasal nitric oxide to compare endoscopic sinus
surgery versus dupilumab for CRSwNP
Daniel Lee, MD, FRCSC
Giovanni Paoletti
Gaia Giuletti
Elysia Grose
Roberto Pinto
Enrico Heffler
John Lee, MD
University of Pennsylvania
Introduction:
There is a need for real-life comparative data between
endoscopic sinus surgery (ESS) and dupilumab for
patients with chronic rhinosinusitis with nasal polyposis
(CRSwNP). The objective of our study was to compare
the outcomes of ESS and dupilumab using nasal nitric
oxide (nNO) as a biomarker of mucosal health, Lund-
Kennedy endoscopy score (LKES), and Sino-nasal
Outcome Test-22 (SNOT-22).
Methods:
A prospective observational cohort of CRSwNP patients
who underwent endoscopic sinus surgery followed by
standard postoperative therapy was compared with
another prospective cohort of CRSwNP patients who
underwent dupilumab therapy. In addition to baseline
characteristics, nNO production levels, LKES and
SNOT-22 levels were compared between the two
cohorts at 1-month and 6-month post-treatment.
Results:
A total of 28 and 37 patients were included in the ESS
cohort and the dupilumab group, respectively. At
1-month and 6-month post-treatment, nNO levels were
comparable between two groups. Compared to
baseline, the ESS cohort showed improvement of nNO
improvement at 1-month post-treatment, while the
dupilumab group did not. At 6-month post-treatment,
both groups exhibited significant improvement of nNO
levels. Similar trend was observed in LKES. SNOT-22
was improved at both 1-month and 6-month post-
treatment compared to baseline.
Conclusion:
ESS and dupilumab confer comparable benefits in
terms of changes in nNO, symptoms and endoscopy
findings at 6-months post-treatment. ESS may result in
more rapid improvement of the outcomes than
dupilumab as evidenced by the 1-month post-treatment
values.
2:12 pm – 2:17 pm
Quantifying Patient Preferences for Treating Nasal
Polyps: Biologics vs. Surgery
Somtochi Okafor, MD
Jessie Sutphin, Ms
Arjita Deb, Dr.
Jonathan Bernstein, Dr
Jui-Chen Yang, Ms
Matthew Wallace, Mr
Ralph Abi Hachem, MD
Shelby Reed, Prof
David Jang, MD, FARS
Duke University
Background:
Biologics are a relatively new treatment alternative to
revision endoscopic sinus surgery (ESS) for patients
with chronic rhinosinusitis with nasal polyps (CRSwNP).
Patient preferences for biologics vs ESS have not been
studied systematically. We conducted a discrete-choice
experiment (DCE) to quantify preferences for treatment
features and outcomes in CRSwNP.
Methods:
Subjects with CRSwNP and at least 1 previous ESS,
completed a DCE survey comprised of 72
experimentally-designed choice sets. In 12 randomly
assigned sets, subjects chose between 2 treatment
options or no additional treatment. 4 features likely to
influence patient decision-making were included:
treatment type (biologic or ESS), oral steroid courses/
year (0,1,2), symptom severity (none, mild, moderate),
and probability of severe symptoms returning within 2
years (10%,30%,40%). Data were analyzed using
mixed-logit (ML) and latent-class analysis (LCA).
Results:
ML (N=195) showed symptom severity had the highest
relative importance weight. LCA revealed 3 unique
classes. Class 1 (53% membership probability)
prioritized outcomes (symptom improvement,
reoccurrence) over treatment type. Class 2 (24%)
preferred ESS and Class 3 (23%) preferred biologics,
irrespective of outcomes. Class 2 & 3 would accept
moderate symptom severity, 2 courses of oral steroids/
year, or 40% chance of reoccurrence to have their
preferred treatment type. Characteristics associated
with class membership (p<0.05) included age,
education, and comorbidities.
Conclusion:
While many patients prioritize outcomes, others have
strong preferences for ESS vs biologics. Quantitative
patient data on treatment preferences offers a new
dimension to decision-making in CRSwNP.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
56
2:18 pm – 2:23 pm
Sinonasal symptom correlation with the
postoperative polyp scale (POPS)
Arthur Wu, MD, FARS
Thomas Higgins, MD, FARS
Dennis Tang, MD, FARS
Elisa Illing, MD, FARS
Taylor Carle, MD
Missael Vasquez
Jonathan Ting, MD, FARS
Satyan Sreenath, MD
Akaber Halawi, MD
Philip Chen, MD, FARS
Cedars-Sinai
Background:
Commonly used endoscopic nasal polyp grading scales
have been shown to correlate poorly with symptom
scores and quality of life metrics. The recently
published Postoperative Polyp Scale (POPS) is a
grading system that more accurately characterizes
polyp recurrence in postoperative sinus cavities,
describing incremental recurrence in relation to the
opened sinus cavities. This study sought to determine if
the POPS correlates with sinus symptoms.
Methods:
CRSwNP patients were prospectively administered
SNOT-22 questionnaires and graded according to the
POPS starting at their 1-month postoperative
appointments. Total POPS scores (sum of each side)
and Max POPS score (larger value of left and right)
were correlated with SNOT-22 total scores and
subdomains using Kendall correlation testing.
Results:
127 patients were enrolled in the study. Both Total
POPS or Max POPS were significantly correlated to the
SNOT-22 total score (p<0.001, p<0.001), Rhinologic
(p<0.001, p<0.001), Extra-Nasal Rhinologic (p<0.001,
p<0.001), Ear/Facial (p<0.001, p<0.001), and
Psychologic (p=0.028, p=0.017) subdomains. Kendall’s
tau indicated strong correlation (>0.3) with Rhinologic
subdomain, moderate correlation (0.21-0.29) with
Extra-Nasal Rhinologic and Ear/Facial subdomains,
and weak correlation (0.1-0.19) with Psychologic
subdomain.
Conclusion:
Previous endoscopic nasal polyp grading scales poorly
correlate with symptoms and patient reported outcome
measures. The new POPS moderately correlates with
the total SNOT-22 score and strongly correlates with
rhinologic symptoms.
2:23 pm – 2:30 pm
Q&A
2:30 pm – 2:35 pm
Blood IgE and eosinophils are not reliable
predictors of nasal inflammation
Andrew Thamboo, MD, MHSc
Judy Fan
Rogerio Pezato, ENT Surgeon
William Daniels
Athenea Pascual, Research Coordinator
Changwan Ryu, ENT Surgeon
Masih Sarafan
Miguel Soares Tepedino
Richard Louis Voegels, Prof
Marco Aurélio Fornazieri, Dr.
Don Sin
St. Paul’s Sinus Centre
Background:
Chronic rhinosinusitis with nasal polyposis (CRSwNP)
is a chronic inflammatory condition of the paranasal
sinuses that is mainly associated with Type 2
inflammation. IgE and eosinophils in blood and nasal
tissue have been suggested as biomarkers for
prognosis and severity of CRSwNP as well as
indications for biological treatment.
Objective:
This study aims to investigate if blood IgE and
eosinophil concentrations can reliably predict nasal
inflammation in CRSwNP by assessing their
relationships with nasal polyp eosinophil concentration.
Methods:
Nasal polyps from CRSwNP patients (N=73) were
collected for hematoxylin and eosin stain and
eosinophil concentration measurement. Blood was
collected to measure IgE and eosinophil
concentrations.
Results:
Weak correlations were found between blood and
tissue eosinophil concentrations (p=0.004, r=0.367)
and blood IgE and eosinophil concentrations (p=0.007,
r=0.372). There is no statistically significant correlation
between blood IgE and tissue eosinophil
concentrations. When dividing patients based on nasal
polyp eosinophil concentration, blood eosinophil level
was higher (p=0.002) in the severely eosinophilic group
(≥100 eos/HPF) than that of the non-eosinophilic group
(<10 eos/HPF).
Conclusion:
Grouping CRSwNP patients based on their tissue
eosinophil level (eosinophilic vs. non-eosinophilic) and
then comparing their blood IgE and eosinophil levels is
not an accurate way to assess the relationships
between tissue and blood biomarkers. Blood IgE and
eosinophils are not reliable biomarkers to predict the
inflammatory condition in CRSwNP and be adopted as
indications for biological treatment. Further research is
needed on the clinical roles of these biomarkers.
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
57
2:36 pm – 2:41 pm
Ocular surface adverse events associated with
dupilumab for treatment of nasal polyps
Austin Swisher, BS
Rijul Kshirsagar, MD
Priscilla Vu, MD
Jonathan Liang, MD, MPH, FARS
Objectives:
Dupilumab was approved to treat chronic rhinosinusitis
with nasal polyps (CRSwNP) in 2019. Ocular surface
reactions (OSR), such as conjunctivitis, have been
associated with dupilumab for atopic dermatitis (AD)
treatment. However, the association of dupilumab-
associated OSR (DA-OSR) for non-AD treatment has
not been adequately studied. We sought to evaluate
DA-OSR for CRSwNP treatment using the FDA Adverse
Event Reporting System (FAERS).
Methods:
FAERS was queried for any general ocular reactions
(DA-GOR) from 2019Q1 to 2022Q4. DA-OSR were
subcategorized from DA-GOR and quantitatively
compared between treatment groups (CRSwNP,
asthma, AD). Simple logistic regression was used to
predict DA-OSR.
Results:
There were 60,198 total observations, of which 5344
were treated for CRSwNP. The prevalence of DA-GOR
and DA-OSR was greatest for AD (15,3%, 7.7%),
followed by CRSwNP (12.2%, 5.0%) and asthma (9.2%,
3.5%). The most commonly reported OSRs were dry
eyes (35.9%), conjunctivitis (15.7%), increased
lacrimation (11.0%), and eye discharge (5.5%). The
reported odds ratio (ROR) of CRSwNP-treated DA-OSR
was 0.84 [0.73-0.97, p=0.015], compared to 1.29 [1.20-
1.40, p<0.001] for AD and 0.66 [0.59-0.73, p<0.001] for
asthma. For CRSwNP treatment, the DA-OSR ROR
was 0.97 [0.90-1.03, p=0.3] for men and 0.78 [0.73-
0.83, p<0.001] for older adults (age >50).
Conclusions:
While there are limitations to FAERS, this database
study confirms the association between dupilumab and
OSR for AD treatment, and does not support a strong
association between dupilumab and OSR for both
CRSwNP and asthma treatment. Younger adults
experience more DA-OSR in CRSwNP treatment
without a specific predilection for gender.
2:42 pm – 2:47 pm
Real world trial for weaning dupilumab from every 2
to every 4 week administration
Emily Garvey, BA
Bita Naimi, BA
Alexander Duffy, MD
Chase Kahn, MD
Paavali Hannikainen, BS
Douglas Farquhar, MD
Marc Rosen, MD, FARS
Elina Toskala, MD, MBA, PhD, FARS
Mindy Rabinowitz, MD, FARS
Jessica Most, MD
Gurston Nyquist, MD, FARS
Introduction:
Initial trials demonstrated that patients receiving
dupilumab for chronic rhinosinusitis with nasal polyps
(CRSwNP) that transitioned to every 4 week
administration after six months experienced continued
improvements. This study is real-world data for weaning
from every 2 to 4 weeks for CRSwNP patients.
Methods:
CRSwNP patients treated with dupilumab for > 6
months with subsequent weaning from every 2 to 4
weeks were included. Outcomes included sinonasal
outcome test (SNOT-22) and polyp scores (Meltzer
Scoring).
Results:
13 patients were included, 12 had comorbid asthma.
Median treatment prior to weaning was 612.5 days.
Weaning rationale included remission (9) coverage/
compliance issues (2), and adverse drug effects (1).
The combined baseline polyp score before dupilumab
was 3.46 +/- 1.55, prior to weaning: 0.15+/-0.36 and at
6 months after weaning: 0.11 +/- 0.33. Baseline SNOT-
22 was: 40.08 +/- 19.12, prior to weaning: 13.78 +/-
14.35 and at 6 months after weaning: 12.33 +/- 10.12.
Remission and 6 month follow up polyp scores
(p<0.001, p=0.003) and SNOT-22 scores (p<0.001 and
p=0.001) were significantly reduced compared to
baseline. 5 patients’ symptoms were adequately
controlled with monthly injections. 1 patient reported
subjective worsening of nasal obstruction, the remaining
6 returned to every 2 weeks due to subjective
worsening of asthma. However, there were no changes
in the asthma control test (ACT) (p=0.49) and FEV1%
(p=0.61) for patients who failed. No patients required
antibiotics or steroids for CRSwNP symptoms during
weaning.
Conclusion:
Every 4-week administration of dupilumab is safe for a
subset of CRSwNP patients to trial. No negative
impacts were noted on objective or subjective measures
of CRSwNP.
PROGRAM ABSTRACTS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
58
2:48 pm – 2:53 pm
Real-world adverse events after type 2 monoclonal
antibody use in chronic rhinosinusitis with nasal
polyps
Marisa Dorling, BSc
Juan Carlos Hernaiz-Leonardo, Clinical Fellow
Athenea Pascual, Research Coordinator
Andrew Thamboo, MD
Amin Javer, MD, FARS
Arif Janjua, MD
University of British Columbia
Purpose:
To investigate the frequency and nature of adverse
events related to type 2 biologic use in patients with
chronic rhinosinusitis with nasal polyps (CRSwNP),
including dupilumab and mepolizumab.
Methods:
This is a single-center retrospective study of real-world
patient data. Patients were included if they have a
diagnosis of CRSwNP, have undergone at least one
endoscopic sinus surgery, and have taken at least two
doses of dupilumab or mepolizumab. Data collected
include demographic information such as age, sex,
past medical and surgical history. The primary
outcomes are the incidence of adverse events and the
types of adverse events observed. Adjusted odds ratio
was calculated to compare the two biologics using
logistic regression modeling.
Results:
42 patients on dupilumab and 29 patients on
mepolizumab were included in this study. 13 (31%) and
5 (17%) patients respectively encountered any adverse
events. The adjusted odds ratio of the adverse event
rates between these two treatment groups was 6.04
(95% confidence interval 1.29-39.15). The most
common adverse events for dupilumab were arthralgia
(12%), injection site reaction (10%), and conjunctivitis
(7%). The most common adverse events for
mepolizumab were headache (7%), arthralgia (3%),
conjunctivitis (3%), cough (3%), and fatigue (3%). Two
patients on dupilumab and one patient on mepolizumab
experienced adverse events leading to discontinuation
of therapy.
Conclusion:
Dupilumab and mepolizumab have significantly different
adverse event profiles. This study contributes to
available data to help guide clinicians’ decision-making
on the use of type 2 biologics in patients with CRSwNP.
2:53 pm – 3:00 pm
Q&A
3:00 pm – 3:30 pm
Break with Exhibitors
3:30 pm – 4:15 pm
Combined ARS/AAOA Panel: Office-Based
Procedures Update: Common Procedures &
Difficult Cases”
Moderator: Jean Kim, MD, FARS
Panelists: Omar Ahmed, MD, FARS; Charles Ebert,
Jr., MD, FARS; Monica Patadia, MD; Elina Toskala,
MD, FARS
4:15 pm – 5:00 pm
International Collaborative Panel: “Assessing
Septoplasty Outcomes: An International
Perspective”
Moderator: Michael Stewart, MD, FARS
Panelists: Sean Carrie, MB, ChB, FRCS,
FRCS(ORL); Chang-Hoon Kim, MD; Jern-Lin Leong,
MD; Ramandeep Virk, MBBS, MS (ENT)
5:00 pm
Meeting Adjourns
5:00 pm – 7:00 pm
Rhinologists in Private Practice Cocktail Reception
Date Night Bar at Assembly Food Hall
5055 Broadway Place
PROGRAM ABSTRACTS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
59
Poster #001
A comparative analysis of nasal packing with and
without bupivacaine for postoperative pain control
after endoscopic endonasal transsphenoidal
surgery
Karol Avila-Castano, Research Fellow
Andrea Otamendi-Lopez
Anyull Dayanna
Bohorquez Caballlero
Angela Donaldson, MD, FARS
Osarenoma Olomu, MD
Introduction:
Postoperative pain control is important after
Endoscopic Endonasal Transsphenoidal Surgery
(EETS). While intravenous and oral methods for pain
control are available, we examined a topical approach
using routine nasal packing for decreasing systemic
medication. Bupivacaine (BP), a long-acting topical
analgesic was applied to the nasal packing used in the
first 24 hours after surgery. We evaluated its effect on
pain control and systemic pain medication use after
EETS.
Method:
A retrospective cohort of 100 patients who underwent
EETS at the Mayo Clinic in Florida between 2019 and
2022 was conducted. Groups were divided based on
whether they received nasal packing soaked with BP
vs no BP. The BP group had an inflatable sponge nasal
packing (Merocel) inflated with BP. The control group
had a non-adherent gauze nasal pack (Telfa). The use
of acetaminophen, use of opiates, and subjective pain
scores (Visual Analogue Scale (VAS)) was compared.
Multiple linear regression models were used to identify
factors influencing VAS postoperatively.
Results:
58% patients were male. The mean age at ETTS was
57 ±16.5 years. 45% received nasal packing with BP.
There was a significant difference in VAS scores
between the two groups at 12 to 24 hours after surgery
with the BP group reporting higher scores for pain
perception (β=0.87, p=0.011). There were no significant
differences in analgesics used between the groups.
Multivariate linear regression identified the length of
surgery, and steroid use as potentially influencing pain
perception after EETS.
Conclusion:
This study is the largest cohort describing the use of
BP in nasal packing after EETS. BP was not found to
reduce pain medications nor improve pain perception
after surgery.
Poster #002
A computational analysis to investigate anatomical
factors associated with increased likelihood of
epistaxis from intranasal sprays usage
Katherine Gonzalez, BS
Amanda Balash
Sarah M. Russel, MD, MPH
Dennis O. Frank-Ito, PhD
Duke University Medical Center
Background:
Intranasal corticosteroids are often recommended as a
first line of treatment for many sinonasal conditions. A
known and potentially serious adverse effect of
intranasal spray therapy usage is epistaxis. Despite
following usage instructions correctly, some patients
may have an increased predisposition of epistasis. This
study uses computational modeling to investigate the
role of nasal morphology on intranasal drug delivery to
the nasal septum.
Methods:
Radiographic images from four adult subjects were
retrospectively selected for three-dimensional
reconstruction of the nasal cavity. Three subjects (N1,
N2, and N3) had a healthy normal nasal anatomy, and
a subject who underwent functional endoscopic sinus
surgery (FESS) for treatment of chronic rhinosinusitis.
Airflow and intranasal spray drug transport were
simulated in each nasal cavity at resting inspiration of
15L/min using computational fluid dynamics modeling.
Intranasal drug delivery was simulated to mimic
recommended usage instructions from manufacturers’
package inserts, with the release of drug particles into
the nasal cavity at 5m/s. Drug particles depositing at
the anterior nasal septal (AS) wall were quantified.
Results:
Subjects NI, N2, and N3 had approximately zero
deposition on the right AS. Left AS depositions were:
N1=63%, N2=45%, and N3=83%. AS depositions in
the subject who underwent FESS were: Left=29% and
Right=87%.
Conclusion:
Preliminary results indicate that anatomical factors
contributing to increased unilateral anterior septal wall
drug depositions even under correct intranasal spray
usage by patient include nasal cycling, septal deviation,
and narrowing of the nasal vestibule.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
60
Poster #003
WITHDRAWN
Poster #004
A rare case of chronic invasive curvularia fungal
sinusitis
Samuel Hopper, BS
Benjamin Stevens, MD
Abdullah Shaheen, MD
Gina D. Jefferson, MD, MS, FACS
Charlotte S. Taylor, MD
Keonho A. Kong, MD
UMMC
Introduction:
Fungal rhinosinusitis (FRS) encompasses a wide
spectrum of diseases that are classified via timeline
and invasiveness. We present a case of a large fungal
mass with osseus erosion without angioinvasion in an
immunocompetent patient.
Case:
A 46 yo immunocompetent AAM presented with a left
nasopharyngeal mass with two-years of left-sided nasal
congestion, epistaxis, hyponasal voice, and ear
fullness. Nasal endoscopy revealed friable tumor in
both nares extending into the left maxillary sinus. MRI
showed a nasopharyngeal mass extending into the
oropharynx and left infratemporal fossa with osseous
destruction of the left pterygoid process. Biopsy
revealed fibroconnective granulation tissue,
multinucleated giant cells, and fungal hyphae, without
evidence of malignancy or angioinvasion. Flow
cytometry was negative. In endoscopic resection the
mass was debulked from the maxillary sinus, posterior
nasopharynx, and the pterygopalatine and
infratemporal fossa. Osseus erosion was noted in the
posterior maxillary wall and pterygoid process. Final
pathology was congruent with original biopsy, and
speciation resulted in Curvularia. Follow up showed
marked clinical improvement with no recurrence after
oral voriconazole for 6 weeks.
Discussion:
Curvularia is generally associated with allergic fungal
sinusitis (AFS). However, the lack of eosinophils
excludes AFS. Chronic granulomatous invasive fungal
sinusitis (CGIFS) due to Curvularia has been reported,
but this case lacked the typically associated
noncaseating granulomas. There has been report of
AFS converting to CGIFS which is a consideration. This
case doesn’t fit into an already defined disease process
highlighting the broad spectrum of FRS and limitations
of current categorization.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
61
Poster #005
Academic productivity trends of fellowship-trained
U.S. academic rhinologists
Michael Warn, Medical Student
Daniella Chan
Theodore Nguyen, BS
Sina Torabi, MD
Benjamin Bitner, MD
Edward Kuan, MD, FARS
Introduction:
Academic productivity is believed to be correlated with
experience and institutional rank, yet there is paucity of
granular academic data between faculty with regard to
institutional rank and industry engagement, and how
these relate to experience.
Methods:
Demographics, academic metrics (publications,
citations, h-index), program rankings, and industry
compensation for academic US rhinologists through
June 2022 were collected and compared between
academic rank and experience.
Results:
A cohort of 278 rhinologists were included. Full
professors had greater academic metrics (all p<0.001)
and industry compensation (all p<0.05) than
associates, assistants, and private practice rhinologists.
Full professors were also more likely to receive NIH-
funding than other groups (p<0.001). Experience and
industry compensation positively correlated with each
other and with academic metrics (all p<0.001) with
significant jumps between the 5-10th and 10-15th year
of practice (p<0.001). However, early career (≤8 years)
rhinologists published more articles per year than late
career (> 8 years) rhinologists (p<0.001). Rhinologists
at Doximity top 10 and 25 programs by reputation and
research output and top 50 USNWR institutions had
significantly greater academic metrics and NIH funding
compared with those who were not (p<0.001). Top 10
and 25 reputation was associated with increased
industry compensation (p=0.024).
Conclusions:
Although early career rhinologists published more
frequently, ascending professorship rank, experience,
and employment at a top-ranked institution were
significantly associated with total academic productivity.
Industry engagement was linked to reputation and
experience.
Poster #006
Acinic cell carcinoma in the nasal cavity: A case
report of a 69-yearold female complaining of nasal
congestion
Aileen Beatrice Antonio, MD
Amando Virgilio Santos, Dr.
Cristina Nieves, Dr.
Ospital Ng Makati
Acinic cell carcinoma (ACC) is a rare, low-grade
primary salivary gland malignancy that represents 2.4
% of all salivary neoplasms. Salivary gland neoplasms
are extremely rare in the nasal cavity. Pleomorphic
adenoma is the most common benign salivary gland
tumor type in the nasal cavity. ACC have been
previously reported in minor salivary glands in the
sinonasal cavity. About 18 cases of acinic cell
carcinoma have been previously described in the
sinonasal cavity. This case of ACC arising from the
nasal cavity presented is the first reported case in this
institution and the Philippines to the best of the
researchers’ knowledge.
The case is as follows: a 69 year old female came in
with a chief complaint of right nasal mass. Two years
prior to admission, the patient now had noticeable
enlargement of fleshy mass with (+) epiphora on the
right which prompted consultation. Biopsy and CT scan
were requested which revealed inverted papilloma and
the patient was advised for surgery. The patient
underwent a medial maxillectomy via lateral rhinotomy
with lip split on the right and excision of infected right
lacrimal sac. Histopathology showed heterogeneous
morphology with epithelial cells resembling ductal cells
or myoepithelial cells arranged as irregular tubules.
This lead to it being reported as acinic cell carcinoma
instead of the initial biopsy result of inverted papilloma.
Results showed that acinic cell carcinoma in the nasal
cavity is extremely rare. Proper interpretation of the
histomorphologic features of this type of tumors should
be done. Acinic cell carcinomas are considered low-
grade neoplasm thus complete surgical resection is
curative but this tumor has shown to have local
recurrence, thus, follow up is essential.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
62
Poster #007
An assessment of the quality of artificial
intelligence-generated patient counseling for
sinusitis
Gregory Hill, MD
Charles Alexander Riley, MD
Jakob Fischer, MD
Anthony Tolisano, Associate Professor
Walter Reed National Military Medical Center
Background:
The quality of online health information is highly
variable and source dependent. Artificial intelligence
language models (AILMs) such as ChatGPT-4
(OpenAI) are likely to become another option for
patients seeking health information.
Methods:
Ten commonly asked questions regarding sinusitis
were derived from Google trends over the past 5
years using the keywords “sinusitis” and “sinus
surgery”. Responses were generated from three
sources: (1) published human expert source, (2)
relevant text from the top 3 links derived from a
Google search, and (3) ChatGPT-4. Three blinded
experts scored the quality of information utilizing the
DISCERN instrument. Fleiss’s kappa was used to
assess interrater reliability. ANOVA one-way testing
evaluated for differences in DISCERN scores by
source type.
Results:
There was no significant difference in response word
count by source type (p>0.05). Interrater reliability
showed moderate correlation (0.59) among the three
blinded reviewers for overall DISCERN scores. The
quality of each source was moderate (human expert
source: 39.9±6.1; Google: 39.2±3.0; ChatGPT-4:
45±9.9). No significant differences in total DISCERN
score was detected among the sources (p>0.05).
The average DISCERN score was higher for
treatment options compared to symptoms or
diagnoses (difference 13.0 points; 95% CI 7.7, 18.3)
for all information sources.
Conclusions:
Similar quality of health information was noted for a
human expert source, Google search, and
ChatGPT-4. All responses were judged to produce
moderate quality information. This has potential
implications for patient education and counseling,
which warrants additional study.
Poster #008
Artificial intelligence based semi-automatic
segmentation for orbital tumors radiomic
measurement
Angela Zhu, BA
Ryan A. Bartholomew
Benjamin Bleier, MD, FARS
Barak Ringel, MD
Massachusetts Eye and Ear; Warren Alpert Medical
School of Brown University
Objectives:
Imaging is essential in the classification and surgical
planning for orbital lesions. New advanced artificial
intelligence (AI) based platforms may allow for
improved tumor assessment, management, and
planning. This study aims to explore the feasibility of
semi-automatic tumor segmentation and to
determine the associations between tumor
morphology, radiomic features, and presenting
symptoms.
Methods:
The open-source 3D-slicer software was used for
MRI-based three-dimensional tumor segmentation
and radiomic features analyses for patients
diagnosed with benign orbital lesions. Sphericity is a
radiomic shape feature that describes how close a
given volume is to a perfect sphere.
Results:
Of the 118 tumors, 94 (79.7%) benign intraconal
tumors were identified. The average patient’s age
was 52.7±17.1 years, with slight female predilection
(57.6%). The mean tumor volume was 336.4mm^3.
Intraconal ORBIT class 2 tumors were larger than
lateral compartment lesions (483.1mm^3 vs.
230.9mm^3, p<0.05). Class 3 tumors’ mean volume
was 262.9mm^3. No significant differences in tumor
volume nor sphericity were identified between tumors
of the remaining ORBIT stages or those located
lateral to the optic nerve. Intraconal tumors
presenting with proptosis (p<0.05) or orbital swelling
(p<0.2) tended to have larger tumor volumes.
Tumors presenting with proptosis (p<0.2), diplopia
(p<0.2), or orbital swelling (p<0.05) tended to be less
“spherical” in shape.
Conclusions:
Orbital tumors’ morphology and volume can
correspond to specific symptom development and
orbital compartment location. The utilization of
3-dimensional semi-automatic segmentation for
treatment planning, outcome measures, and follow-
up warrants further exploration.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
63
Poster #009
WITHDRAWN
Poster #010
Assessing nasal function after definitive
rhinoplasty for unilateral cleft lip nasal deformity
repairs: A pilot analysis
Elaine Lin, BS
Dennis O. Frank-Ito, PhD
Duke University School of Medicine
Background:
Patients with unilateral cleft lip nasal deformity
(uCLND) experience significant nasal obstruction
and olfactory dysfunction, and very little is known of
whether definitive cleft rhinoplasty improves patients’
nasal function. This study aims to assess patient-
reported satisfaction and objective assessments
before and after surgery.
Methods:
Three patients (P1, P2, P3; 18-23 years) with
uCLND were prospectively recruited. Data collected
before and >6 months after definitive cleft rhinoplasty
were: [1] Nasal Obstruction Symptom Evaluation
(NOSE) scores; [2] Standardized Cosmesis and
Health Nasal Outcomes Survey scores to evaluate
nasal obstruction (SCHNOS-O) and nasal cosmesis
(SCHNOS-C); [3] Nasal resistance (NR)
measurement using the NR6 Clinical/Research
Rhinomanometer; and [4] the University of
Pennsylvania Smell Identification Test (SIT).
Results:
NOSE improvement post-surgery were: P1=20, P2=0
and P3=70. P1 was within one standard deviation
(SD) of reported minimal clinically important
difference (MCID; 24.4±15.3), P2 no improvement,
and P3 over 2SD of MCID improvement. SCHNOS-O
post-surgery improvement: P1=25, P2=-5 and
P3=55. P1 and P3 were within 1SD of reported
SCHNOS-O MCID (28.3±17.3) and P2 was worse.
SCHNOS-C post-surgery improvement: P1=3,
P2=17 and P3=80; reported SCHNOS-C MCID was
18.0±12.8. Post-surgery NR decreased by 40% (P1),
2% (P2) and 71% (P3), while SIT improved by 3%
(P2) and 10% (P3) but worsened by 21% (P1).
Conclusions:
Preliminary findings suggest stronger agreement
between patients’ satisfaction and improvement in
their nasal patency compared to their olfactory
improvement. Further, definitive rhinoplasty for
uCLND repairs may not adequately address patients’
olfactory dysfunction.
Poster #011
Association of alcohol use with olfactory
function among older adults
Khamis Suleiman, Medical Student
Richard Chiu, Medical Student
Sharmilee Nyenhuis
Kamal Eldeirawi
Victoria Lee, MD, FARS
University of Illinois College of Medicine
Background:
Olfactory dysfunction (OD) is a common condition
predominantly affecting the elderly population. This
study aims to explore the association between
alcohol consumption and OD. Investigating the
relationship between alcohol consumption and OD is
crucial due to its potential consequences for public
health and to gain insight into the mechanisms
underlying OD.
Methods:
This cross-sectional study was conducted on data for
1,107 adults from Round 3 of the National Social
Life, Health, and Aging Project. Normal olfactory
function was defined as correctly identifying 4–5
odors in the 5-item Sniffin’ Sticks test, and OD was
defined as 0–3 odors correctly identified.
Associations between alcohol use and olfaction were
assessed using logistic regression, and adjusted
odds ratios (OR) were calculated. Analyses were
weighted to account for the sampling design.
Results:
OD was present in 18.9% of adults. The weighted
average age was 76.5 ± 6.7 years among those with
OD and 74.7 ± 5.7 years among those with normal
olfaction. 37.9% of adults with OD reported alcohol
consumption in the last 3 months, compared to
48.0% of adults with normal olfaction. After adjusting
for age, gender, race, education, recent stroke,
dementia, diabetes, and mental health, alcohol
consumption was not associated with OD (OR: 0.77;
95% CI: 0.51–1.17).
Conclusions:
Alcohol consumption was not associated with OD
after controlling for covariates. While this study
provides insight into the relationship between alcohol
consumption and OD, further research is needed
due to conflicting results in previous studies. The
inconsistencies in previous research were likely due
to factors such as study population, study design,
and confounding variables.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
64
Poster #012
Association of chronic rhinosinusitis and
autoimmune disorders
Chadi Makary, MD, FARS
Zayd Al-Asadi, BS
Dominic Lombardo, BS
Sairisheel Gabbi Reddy
Brian Peppers, Assistant Professor
Hassan Ramadan, MD, FARS
West Virginia University
Introduction:
Increasing evidence suggests that autoimmune
disorders and their immunomodulating medications
may increase the risk of rhinosinusitis.
Goal:
To determine if autoimmune disorders are associated
with increased risk of rhinosinusitis.
Methods:
Cross-sectional study of patients referred to West
Virginia University from August 2020 to October 2022
for rhinologic complaints was performed. These
patients were diagnosed either with chronic
rhinosinusitis (CRS) or recurrent acute rhinosinusitis
(RARS) according to published guidelines. Patients’
characteristics, diagnoses, and type and treatment of
autoimmune disorders were reviewed.
Results:
544 rhinosinusitis (463 CRS and 81 RARS patients)
were compared to 595 non-rhinosinusitis (530
chronic rhinitis and 65 facial pain/headache) patients.
Patients with rhinosinusitis were older (50.1 vs 45.8
years old, p=0.0001), more likely to be males (46.7%
vs 35.2%, p<0.0001), more likely to have asthma
(33.6% vs 25.4%, p=0.002), and more likely to have
current and past smoking history (14.3% vs 8.7%,
p=0.003; 28.5% vs 19.7%, p<0.0001 respectively).
Autoimmune disorders were more common in
rhinosinusitis patients (16.4% vs 9.4%, p<0.0001).
Psoriasis and rheumatoid arthritis were the most
common autoimmune disorders in rhinosinusitis
patients (2.9% and 2.5% respectively). Multivariate
logistic regression adjusting for confounders showed
that autoimmune disorders were strongly associated
with rhinosinusitis [OR=2, CI=1.4-2.9]. Subgroup
analysis showed CRS and RARS were equally
associated with autoimmune disorders.
Conclusion:
Autoimmune disorders increase the risk of both CRS
and RARS. Further studies are needed to explore
their role in the treatment outcome of rhinosinusitis.
Poster #013
Association of prior military service with
olfactory function among older adults
Richard Chiu, BS
Khamis Suleiman, Medical Student
Sharmilee Nyenhuis
Kamal Eldeirawi
Victoria Lee, MD, FARS
University of Illinois College of Medicine
Background:
Olfactory dysfunction (OD) is a common condition
primarily affecting the elderly. Several factors have
been implicated in OD, such as age, socioeconomic
status, and neurocognitive disorders; however, the
effect of military service on OD is unclear. It has
been hypothesized that toxins and
neuropsychological changes related to military
deployment may negatively impact olfaction. This
study aims to investigate this association.
Methods:
This cross-sectional study was conducted on data for
992 adults from Round 3 of the National Social Life,
Health, and Aging Project. Normal olfaction was
defined as correctly identifying 4–5 odors in the
5-item Sniffin’ Sticks test, and OD was defined as
0–3 odors correctly identified. Associations between
military service and olfaction were assessed using
logistic regression, and adjusted odds ratios (OR)
were calculated. Analyses were weighted to account
for sampling design.
Results:
OD was present in 18.4% of adults. The weighted
average age was 76.8 ± 6.6 years among those with
OD and 74.6 ± 5.6 years among those with normal
olfaction. About 20% of adults with OD served in the
military, compared to 23.6% of adults with normal
olfaction. After adjusting for age, gender, race,
education, recent stroke, dementia, mental health,
and smoking, participants with prior military service
were less likely to have OD (OR: 0.48; 95% CI:
0.26–0.89).
Conclusions:
Prior military service was unexpectedly protective of
normal olfaction after controlling for covariates. This
may be a result of data limitations, as the military
service variable is self-reported and does not capture
length of service. Further research is needed to
investigate mechanisms or confounders behind this
result.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
65
Poster #014
Baseline olfactory function and prospective
assessment of patient-reported outcome
measures in patients with nasal septal
perforation
Shreya Ramkumar, BS
Bansberg Stephen, Consultant
Michael Marino, MD, FARS
Amar Miglani, MD
Background:
This study evaluated baseline olfactory function and
patient-reported outcome measures (PROMs) of
conservative treatment (saline gel moisturization)
followed by surgical closure in patients with nasal
septal perforation (NSP) of any etiology.
Methods:
Patients who underwent NSP repair at Mayo Clinic
between September 2022 and March 2023 were
prospectively enrolled. Patients with <15 days
between the date of presentation to surgery were
excluded. NOSE-Perf scores, UPSIT scores prior to
surgery, NSP size, and demographics were collected
and analyzed using descriptive statistics.
Results:
Our cohort consisted of 15 patients (10 females, 5
males) with a median of 83 days (IQR: 37.0, 124.5)
between presentation and surgery, during which
patients were treated with saline gel moisturization.
Most patients had normosmia (N=7) or mild
hyposmia (N=5). Patients with normosmia were
younger than patients with any degree of smell loss
(median: 44.0 vs. 55.5 years). Most patients (63%)
with perforation height >1cm had normosmia.
Successful perforation closure was achieved in all
patients using bilateral nasal mucosal flaps
supported with an interposition graft. Median NOSE-
Perf scores at presentation, pre- and post-operatively
were 24 (IQR: 19.0,30.5), 25 (IQR: 13.5,31.5), and 9
(IQR: 7.0,17.0), respectively.
Conclusion:
Although NSP has been postulated to affect
olfaction, most patients in our study had normosmia.
NSP size may not correspond with the degree of
olfactory loss, and further studies are warranted. In a
cohort of NSP patients undergoing surgical repair,
conservative management with saline gel
moisturization provided little symptom benefit. NSP
repair remains a promising option for perforation
closure and improving PROMs.
Poster #015
Biologic therapies for treating chronic sinusitis
with nasal polyps: What do patients want to
know?
Samuel Razmi, BS
Lexi Goehring, Medical Student
Daniel Gorelik, Research Fellow
Kenneth Sims IV, Medical Student
Yuki Yoshiyasu, Resident
Masayoshi Takashima, MD, FARS
Omar Ahmed, MD, FARSTexas A&M School of
Medicine – ENMED
Biologic therapies for chronic rhinosinusitis with
nasal polyps (CRSwNP) are emerging as promising
treatment options for patients with refractory disease.
The objective of this study is to explore the questions
patients are commonly asking online about these
therapies and the quality of the available content.
Most common search terms were identified via
Google Trends. People Also Ask (PAA) questions
were identified and extracted with their associated
website using a freely available program (SEO
Minion). Questions were categorized according to
Rothwell’s criteria by two independent reviewers and
organized into subtopics and categorized. Sources
were evaluated using Flesch Kincaid Grade Level
(FKGL) score for readability and JAMA Benchmark
criteria for quality assessment (0-4, 4 = all criteria
met).
A total of 143 unique questions from 143 unique
websites were collected across 4 search terms.
Questions regarding facts about biologics including
side effects (38.5%) were most common, followed by
facts about CRSwNP (37.8%), and finally treatment
options for CRSwNP (23.7%). FKGL score gave a
mean 12.2 (3.30) grade US reading level - much
higher than the recommended 6-8th grade level.
JAMA benchmark gave a mean of 0.95 (0.85).
Sources answering the PAA questions were mainly
commercial (60.1%) followed by medical practices
(14.0%), academic (13.3%), and government
(12.6%).
Given the novelty of biologic therapies as treatment
for CRSwNP, patients are seeking more information
about biologics. Existing online resources regarding
biologics for CRSwNP should be improved with
material that is easier to read. More academic
sources and scholarly information is needed.
Physicians should be aware of these areas and
counsel accordingly.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
66
Poster #016
B-LBL presents as sinonasal mass: A case report
Brandon Vilarello, BA
Patricia Jacobson, Medical Student
David Gudis, MD, FARS
Jonathan Overdevest, MD, PhD
Columbia University Vagelos College of Physicians
and Surgeons
Introduction:
B-cell lymphoblastic leukemia/lymphoma (B-ALL/
LBL) is primarily a disease of childhood that presents
with lymphadenopathy, fatigue, fever, night sweats,
and weight loss. Initial presentations prompted by
head and neck manifestations are exceedingly rare.
Case Report:
A 5 year-old girl with no significant past medical
history presented with right facial swelling and mild
proptosis on ophthalmologic evaluation. She was
referred to a tertiary care facility by her local
otolaryngologist for further management after CT
imaging revealed right maxillary sinus opacification
and erosion of the anterior maxillary bone. Her
symptoms were initially responsive to prednisone
and amoxicillin-clavulanate, and only right unilateral
nasal discharge persisted with resolution of other
sinonasal/systemic symptoms. Notably, laboratory
values, including complete blood count, were within
limits. Given concern for the etiology of the bony
erosion, the patient presented for a second opinion,
where imaging and recommendation for biopsy
resulted in flow cytometry findings consistent with
B-ALL/LBL. After bone marrow biopsy, the ultimate
diagnosis was Murphy’s stage III B-lymphoblastic
lymphoma.
Conclusions:
Malignant neoplasms of the sinonasal region are rare
in children, where primary sinonasal B-LBL is a
unique occurrence. Clinical features of sinonasal
B-LBL in the paranasal sinuses may masquerade as
pathologies such as acute sinusitis, orbital cellulitis,
and benign tumors or polyps that can lead to a
confounding diagnosis. In this case presentation, an
initial response to steroids and antibiotics should not
provide false reassurance when other features and
signs, such as maxillary bone erosion, may suggest
the presence of malignancy.
Poster #017
WITHDRAWN
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
67
Poster #018
Case report: Rare angiomyolipoma of the nasal
cavity
Akash Halagur, BA
Galit Almosnino, MD
Ryan Little, MD
Geisel School of Medicine at Dartmouth
We report a patient with a rare case of an
angiomyolipoma (AML) arising from the nasal cavity
presenting with nasal obstructive symptoms.
The mass was broadly pedicled to the right lateral
nasal side-wall and excised endoscopically. The
patient’s post-operative course was complicated by
epistaxis requiring Merocel placement but was
without recurrent epistaxis. Immunohistochemical
studies revealed positive SMA, S100, CD61 and
MPO and negative HMB45 and Melan A staining
indicating the presence of spindled smooth muscle
cells, vasculature, lipomatous content, and lack of
melanocytic markers consistent with previous reports
of mucocutaneous AMLs.
Nasal AMLs are exceedingly rare with fewer than 21
cases reported in literature to date. The majority of
the cases have been reported from Asia and the
Middle East with fewer than five cases reported in
the United States. The majority of non-tuberous
sclerosis-related cases are immunophenotypically
distinct from the family of perivascular epithelioid cell
neoplasms (PEComas) typically associated with
renal and extra-renal AML.
Our case of highlights the clinicopathologic features
of AML that are distinct from its broader family of
PEComas, and provides support for their further
classification to ‘angiomyolipomatous hamartoma’ as
suggested by Wang et al. (2021) to distinguish their
lack of epithelioid morphology, lack of melanocytic
immunophenotype, and non-neoplastic nature from
PEComatous AML. Although rare, based on both our
experience and the recent literature, AML should be
included in the differential diagnosis of unilateral
nasal masses.
Poster #019
Cavernous sinus immunoglobulin G4-related
disease- A case report
Erika Bradley, RN, BSN
Mark Arnold, MD
Upstate Medical University
Immunoglobulin G4- related disease (IgG4-RD) is a
rare immune-mediated fibroinflammatory condition.
Symptoms at presentation vary; however, each
organ involved has tumor-like involvement. Diagnosis
relies on biopsy showing histopathological findings
including storiform fibrosis, large amounts of IgG4
plasma cells, and lymphoblastic infiltrates.
We report a rare presentation of IgG4-RD in a
68-year-old Caucasian male who suffered from left-
sided facial pain, superior gaze deficit, left otalgia,
and left-sided visual loss. CT showed left sphenoid
opacification and osteitic changes, and MRI showed
pachymeningeal enhancement of the bilateral
cavernous sinuses, greater on the left side, left
orbital apex, and optic nerve sheath. He underwent
left endoscopic sphenoidotomy, and was treated with
steroids and antibiotics. Tissue biopsies of the left
sphenoid mucosa showed moderate
lymphoplasmocytic inflammation and of the
sphenoid-ethmoid polyp showed prominent IgG4
restricted plasma cell infiltrate. The IgG4/IgG ratio
was greater than 90%, and blood serum IgG4 levels
were elevated at 227 mg/dL, consistent with IgG4-
RD. There was no storiform fibrosis of the biopsied
tissue. Given his complex presentation,
ophthalmology and rheumatology physicians were
involved. His visual acuity improved with IV and later
oral steroids. However, due to persistent
pachymeningeal enhancement on MRI and changes
to color vision, rituximab was given.
This is a unique case of IG4-RD due to a mass in
the nasal cavity outside of the sphenoid sinus
showing IgG4-RD and pachymeningeal
enhancement causing inflammation of the cavernous
sinus due to IgG4-RD. Increased awareness of this
rare presentation of IgG4-RD will improve future
patient outcomes.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
68
Poster #020
Characteristics of patients requiring revision
endoscopic sinus surgery- An 11 year single-
institution study
Madison Buras, MD
Matthew Mitchell
Background:
Chronic rhinosinusitis refers to a sinonasal
inflammatory process which commonly requires
surgical intervention in patients who have failed
medical management, sometimes requiring multiple
revision surgeries to achieve disease control. This
can significantly reduce quality of life and have a
large socioeconomic impact.
Methods:
A retrospective review was performed to identify
patients that underwent endoscopic sinus surgery at
our institution between 2011-2022. The study
included 448 patients who underwent one primary
endoscopic sinus surgery and 307 patients who
underwent multiple surgeries. Data collection
included patient demographics and the presence of
various co-morbidities. The patients who required
only one surgery were compared to those who
required multiple surgeries to determine
characteristics that were predictive of the need for
multiple procedures to achieve disease control.
Results:
In terms of demographics, males were only slightly
more likely to require revision surgery (43% vs 38%).
There was not a statistically significant difference
between patients with diabetes, smoking or asthma.
Patients with allergic fungal rhinosinusitis, polyps,
Samter’s triad, cystic fibrosis, and primary ciliary
dyskinesia were all much more likely to require
revision sinus surgery.
Conclusion:
This study has demonstrated that revision sinus
surgeries were required more often in men and in
patients with allergic fungal rhinosinusitis, polyps,
Samter’s triad, cystic fibrosis, and primary ciliary
dyskinesia. These findings will help us have a more
knowledgeable pre-operative discussion with at-risk
patients, identify controllable characteristics in
patients, and reduce the socioeconomic burden of
this disease process.
Poster #021
Characterization of chronic rhinosinusitis by
associated medical comorbidities
Tiffany Toni
Gengjie Jia, Dr.
Jay Shah, Dr.
Robert Naclerio, MD
Carole Ober, Dr.
Andrey Rzhetsky, Dr.
Jayant Pinto, Dr.
Introduction:
Chronic rhinosinusitis (CRS) is a multifactorial
disease process theorized to arise through the
complex interaction between the host genetic and
inflammatory state induced environmental and
infectious exposures. The relationship between CRS
and other medical comorbidities remains an under
investigated area of CRS research that we
hypothesized would allow for patient disease
stratification.
Methods:
In the following study, we utilized a multi-institutional
database to investigate a total of 5,415,401 patients
aged 18-70 with a diagnosis of CRS. Patients with
respiratory congenital anomaly and cystic fibrosis
were excluded from the study. Supervised machine
learning was used to cluster patients based on
medical comorbidities. These clusters were further
analyzed individually to investigate the percentage of
patients with severe disease, as characterized by
CRS with nasal polyposis (CRSwNP).
Results:
Twenty-three distinct clusters emerged and were
grouped according to similar pathogenesis into the
following nine disease signatures: atopic, cell
epithelial dysfunction, autoimmune, neuropsychiatric,
metabolic syndrome, hormonal, vascular, immune
deficiency, and infectious. Of patients with CRS,
4.0% of patients were also coded as having nasal
polyposis. CRSwNP patients were more likely to be
categorized as having an atopic or infectious disease
signature as compared to chronic rhinosinusitis
without nasal polyposis (CRSsNP) patients.
Conclusions:
Chronic rhinosinusitis can be classified into multiple
subcategories by comorbidity mapping. Furthermore,
CRSwNP is associated with a concomitant diagnosis
of atopic and/or infectious sinonasal disease.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
69
Poster #022
Choosing wisely in ESS in the era of biologics
(CHESS)
Neil Verma, MDCM, MSc FRCSC
Martin Desrosiers, MD
Centre Hospitalier de l’Université de Montréal
Background:
Chronic rhinosinusitis with nasal polyposis
(CRSwNP) is a disease characterized by Th2
inflammation. Approval of biologic therapies has
transformed the landscape of treatment for CRSwNP
with modulation of the immune response to manage
the disease. Endoscopic sinus surgery remains an
important component in the management of
CRSwNP and biologic therapy may influence the
difficulty or complication rates seen in surgery and
post-operatively with respect to surgical recovery.
The goal of this study is to document and
characterize the experiences of Canadian
rhinologists with ESS for CRSwNP performed under
biologic treatment that target Th2 inflammation.
Methods:
An online survey was sent to Canadian fellowship
trained rhinologists to capture their experiences
regarding ESS for patients under biologic therapy
including intra-operative ease, bleeding and
purulence during surgery as well as post-operative
assessment of symptoms and endoscopy compared
to non-biologic therapy standard ESS. We performed
subgroup analysis based on demographic
parameters, primary vs revision surgery and type of
biological agent received.
Results:
We expect that the results of this exploratory
assessment will offer novel and much-needed
information on potential impacts of type-2 targeting
biologics on ESS surgery and identify relevant items
suitable for inclusion in a future clinical registry of
ESS performed in patients under biologic therapy.
Conclusions:
There is a paucity of information on the effect of
biologics on ESS and surgeons would benefit from
recommendations and information when operating
on patients with concomitant biologic therapies.
Improved guidelines would help optimize surgical
interventions and improve surgical outcomes.
Poster #023
Clinical outcomes and complications of
endoscopic odondoidectomy: A single institution
experience
Ann Powers, MD
David Lerner, MD
Janki Shah, MD
Anthony Del Signore, MD
Madeleine Schaberg, MD
Satish Govindaraj, MD, FARS
Raj Shrivastava, MD
Alfred-Marc Iloreta, MD
Introduction:
Odontoidectomy is indicated for anterior
decompression of the cevicomedullary junction to
address a wide variety of pathologies. Endoscopic
approaches reduce perioperative morbidity
associated with the traditional open approaches,
namely gastrostomy and tracheostomy tube
placement.
Methods:
This is a retrospective review of patients undergoing
endoscopic odontoidectomy between 2015-2022.
The electronic medical record was reviewed for
patient factors, operative variables, and post-
operative complications.
Results:
8 patients underwent endoscopic odontoidectomy
with a median age of 55yrs. Indications included
basilar invagination (4), rheumatoid pannus (2),
pathologic fracture with cord compression (1), and
odontoid osteoradionecrosis (1). Endoscopic
odontoidectomy was achieved via transnasal route in
5 patients, while 3 patients required a combined
transnasal-transoral endoscopic approach. All
patients undergoing a combined transnasal-transoral
approach received a temporary tracheostomy at time
of surgery, whereas only 2/5 patients undergoing the
transnasal approach required a tracheostomy
perioperatively. We found all patients undergoing a
combined approach required at least a temporary
gastrostomy tube compared to 2/5 patients
undergoing a purely transnasal approach.
Discussion:
Endoscopic odontoidectomy is associated with
reduced morbidity than the traditional open
approach. Optimally resection is carried out
endoscopically purely via a transnasal route but
sometimes a transoral corridor is necessary to
achieve decompression inferiorly. Our results
suggest a purely transnasal route is preferred with
better post-operative swallowing outcomes. We will
expand on this series with patients from preceding
years.
POSTERS
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
70
Poster #024
Clinical outcomes of bioabsorbable nasal
implants for nasal valve collapse: A meta-
analysis
Felisha Li, BA
Matthew Saleem, BS
Travis Peng
Sarah Van der Els
Carol Wang
Tristan Tham
Donald and Barbara Zucker School of Medicine
Introduction:
While Latera has been shown to improve NOSE
scores long-term in patients, adverse events of the
implant have not been extensively studied. To our
knowledge, this is the first meta-analysis for clinical
outcomes of Latera bioabsorbable implants for nasal
valve collapse.
Methods:
English full-text articles were searched for on
PubMed, Scopus, and Embase databases. Articles
had to report the use of Latera implants; report
adverse events such as complications, inflammation,
and implant retrieval; be from a clinical trial, cohort,
or case-control study. Two reviewers screened
articles and a third settled disagreements. Preferred
Reporting Items for Systematic Reviews and Meta-
Analyses guidelines and the Risk of Bias in Non-
randomized Studies of Interventions tool were used.
After Freeman-Tukey transformation, weighted
proportions were analyzed in a random effects
model.
Results:
Seven studies, three retrospective and four
prospective, representing a total cohort of 513
patients were included in this study. Pooled adverse-
event rate after Latera implant was 13.4% (95% CI:
6.0-23.1%) and implant retrieval rate was 6.8% (95%
CI: 3.8-10.6%). Subgroup analysis found comparable
implant retrieval rates between retrospective (2.5%,
95% CI: 0.1-8.2%) and prospective (8.7%, 95% CI:
6.2-11.6%) studies. There was moderate
heterogeneity in pooled analysis for adverse events
(I2 = 83.8%) and implant retrieval rate (I2 = 42.6%).
Notably, there was no heterogeneity in the
prospective subgroup for implant retrieval rate
(I2=0%).
Discussion:
Implant retrieval is a relatively uncommon
complication of Latera absorbable implant. While the
adverse-event rate was higher, most events in these
studies were mild such foreign body sensation.
Poster #025
Clinical productivity of fellowship-trained
academic rhinologists: An analysis of Medicare
metrics
Michael Warn, Medical Student
Daniella Chan
Theodore Nguyen, BS
Sina Torabi, MD
Benjamin Bitner, Dr.
Edward Kuan, MD, FARS
Introduction:
Current data regarding reimbursement trends in
Medicare services and the types of patients treated
as physicians progress in their academic career is
conflicting, and no such work has been undertaken
for rhinologists.
Methods:
Demographics, professorship rank, and years of
experience of US academic rhinologists were
collected. Those with associated Medicare services,
charges, and patient complexity risk scores (based
on hierarchical condition category coding) were
compared by rank and experience.
Results:
A cohort of 211 rhinologists were included. Private
practice rhinologists performed the most services
(791 [207-1036] vs 404 [182-572]; p =0.016), while
full, associate, and assistant professors billed more
per service ($791.53 [$491.69-1,052.46], $706.85
[$473.48-941.15], $590.34 [$429.91-853.07] vs
$326.08 [$223.37-482.36]; all p<0.001). Full
professors also had higher charges per service
(p<0.001) and total charges (p=0.012) than associate
and assistants, but lower risk scores than assistants
(1.37 [1.26-1.52] vs 1.49 [1.29-1.68]; p =0.013) and
similar risk scores to associates (1.47 [1.25-1.64];
p=0.061). Increasing years of practice was inversely
correlated with risk scores (R=-0.358; p<0.001). As a
cohort, significant declines in risk scores occurred
between the 5-10th and 10th-15th year of practice
(p=0.032) and after the 15th-20th year (p=0.038).
Conclusion:
Academic rhinologists submitted fewer services than
private practice colleagues but had greater total
charges and charges per service. Full professors
charged the most per service and treated patients
with lower risk scores than more junior academic
colleagues. Risk correlates negatively with
experience with significant drops in mid and late
career.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
71
Poster #026
Cohort study: Pluripotent pituitary adenomas are
at higher risk for SIADH
Sabrina Goyal, BS
Jake Lee, MD, MSCI
Kaleigh Roberts, MD, PhD
Sonika Dahiya, MD
Nyssa Farrell, MD
John Schneider, MD, MA
Albert Kim, MD, PhD
Julie Silverstein, MD
Lauren Roland, MD, MSCI
Introduction:
Plurihormonal pituitary adenomas (PPAs), tumors
producing more than one hormone, are exceedingly
rare. The natural history of PPAs, in comparison to
single-secreting pituitary adenomas (PAs), is poorly
understood.
Methods:
Data for 407 resected transsphenoidal PAs was
obtained through a patient repository from a single
tertiary level center. Primary outcomes including
demographics, pre- and post-op endocrinopathies,
tumor morphology, histology, and readmission were
compared between monohormonal and
plurihormonal tumors with bivariate analysis using
Chi-square and unpaired nonparametric Mann-
Whitney tests.
Results:
A total of 383 monohormonal and 24 plurihormonal
tumors were identified between 2015-2023 with an
average age of 51 years. Co-expression patterns
included Prolactin/FSH/LH (n=7), Prolactin/GH (n=3),
ACTH/FSH/LH (n=3), Prolactin/ACTH (n=2),
Prolactin/TSH (n=2), ACTH/FSH/LH/TSH (n=2),
Prolactin/ACTH/FSH/LH (n=2), Prolactin/ACTH/GH
(n=2), Prolactin/ACTH/FSH/LH/TSH (n=1), Prolactin/
GH/FSH/LH/TSH (n=1). Pre- and post-operative
endocrinopathies were present in 16 and 18 cases,
respectively. Ki67 was 2.8 on average with elevated
proliferation in 3 cases. Crooke changes (n=3) and
apoplexy (n=1) were identified. Readmission within
30 days occurred in 6 patients. Compared to
monohormonal tumors, post-operative SIADH
(p=0.024), prolactin (p<0.001), GH (0.0011), FSH/LH
(0.0189), and TSH expression (<0.0001) were higher
in PPAs.
Conclusions:
In this study, we describe our experience with a large
series of PPAs. When determining appropriate post-
operative care of PPAs, higher incidence of SIADH
should be considered.
Poster #027
Combined transnasal, transoral approach for
excision of odontogenic cysts offers reduced
recurrence rates and favorable sinonasal
outcomes
Jennifer Douglas, MD
Kimberly Wei, Medical Student
Kush Panara, MD
Daniel Lee, MD
Michael Kohanski, MD, PhD
Rabie Shanti, Associate Professor
Neeraj Panchal, Assistant Professor
James Palmer, MD, FARS
Nithin Adappa, MD, FARS
University of Pennsylvania
Background:
Odontogenic cysts are fluid-filled, epithelial lined
cavities of dental origin that damage the adjacent
dentition, maxilla, and maxillary sinus, with standard
of care being transoral excision. However, a high
rate of recurrence (14-35%) has been reported. We
present the largest series of odontogenic cysts
managed jointly by rhinologic and oral and
maxillofacial surgeons through a combined
transnasal, transoral endoscopic approach.
Methods:
Retrospective case series of patients undergoing
combined transnasal, transoral endoscopic approach
for excision of odontogenic cysts from 2014-2023.
Records were reviewed for demographics, radiology
and histopathology reports, sinonasal outcomes (via
the 22 item Sinonasal-Outcome Test), and
perioperative course.
Results:
Twenty-three patients met inclusion criteria, 56.5%
male with mean age 44.6 years. Cysts were 3.4 cm
in average maximal diameter with varying pathology
(47.6% odontogenic keratocysts, 28.6% dentigerous
cysts, 14.3% cyst with ameloblastic transformation,
4.8% each ossifying fibroma and chondromyxoid
fibroma). They demonstrated on average no changes
in sinonasal outcomes above the SNOT-22 MCID
and the majority reported improved scores compared
with pre-operative baseline. There were two
episodes of recurrence (9.5%) over a mean follow-up
time of 2.7 years.
Conclusions:
A combined transnasal, transoral endoscopic
approach for excision of odontogenic cysts is a safe
alternative to the transoral approach with a reduced
recurrence rate and favorable sinonasal outcomes.
Herein we report the largest published case series of
a combined approach, with the recommendation it be
considered for improved treatment outcomes for
odontogenic cysts involving the maxillary sinus.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
72
Poster #028
Comparing physical and virtual “digital twin”
models of endoscopic skull base disorders for
preoperative planning
David Ahmadian, BS
Shireen Samargandy, Dr.
Nirushan Narendran, Research Specialist, Senior
Allan Hamilton, Dr.
Minsik Hong
Jerzy Rozenblit, Dr.
Christopher Le, MD, FARS
Michael Avery, Dr.
Eugene Chang, MD, FARS
University of Arizona, College of Medicine – Tucson
Introduction:
A significant challenge in preoperative planning of
endoscopic skull base procedures is visualizing
critical anatomical structures in 3D space.
Wehypothesized that a “digital twin,” or dynamic
personalized 3D image
encapsulating biophysical properties of a patient’s
anatomy might be beneficial in resident surgical
training.
Methods:
Residents in an endoscopic skull base course were
given a traditional
curriculum-based lecture on the hierarchical task
analysis (HTA) steps of an endoscopic approach to
the pituitary gland. They were then exposed to three
different methods of visualizing the patients’
anatomy: 1. DICOM viewer of 3-plane merged CT
and MRI scans, 2. 3D printed model of the patient’s
anatomy, and 3. A virtual reality model created in the
UNITY platform. They were then assessed on their
surgical performance during a cadaveric dissection
of an endoscopic pituitary approach. Residents were
asked to identify critical structures in the dissection,
and their performance was graded using our
published evaluation method by fellowship-trained
attendings. Afterwards, the residents were asked to
complete a Likert-based scale questionnaire on their
opinions regarding the methods of preoperative
planning.
Results:
All trainees completed the three different training
methods. The majority of trainees felt that 3D printed
models and VR simulation were superior in terms of
spatial anatomy localization compared to viewing
traditional 2-dimensional DICOM images. Residents
had significant improvements in cadaveric
dissections after preoperative training.
Conclusions:
3D printed and virtual models of patient-specific
anatomy improves resident awareness of critical
structures in endoscopic skull base surgery.
Poster #029
Complications of novel radiofrequency device
use in otolaryngology: A MAUDE analysis
Sina Torabi, MD
Benjamin Bitner, Dr.
Eric Abello
Theodore Nguyen
Brian Wong
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
With the widespread development and adoption of
intranasal radiofrequency (RF) devices, the objective
herein was to report national adverse events
associated with their use.
Methods:
The Food & Drug Administration’s Manufacturer and
User Facility Device Experience was queried for
adverse events reported after Celon ProBreath
(Olympus), Vivaer (Aerin) and Rhinaer (Aerin) use
since database inception to February 2nd, 2023. The
event descriptions were reviewed and categorized by
three independent reviewers, with any discrepancies
discussed and resolved.
Results:
A total of 22 device-related adverse events were
reported, 11 (50.0%) for Celon, 3 (13.6%) for Vivaer,
and 8 (36.4%) for Rhinaer. 7 (63.6%) of the Celon-
related complications were related to tissue necrosis,
including a palatal perforation, that appeared to be
related to user error. Notably, 1 (9.1%) episode of
pediatric ocular palsy was also reported. Vivaer
complications included synechiae formation that
required excision, a mucosal perforation secondary
to tissue necrosis, and a case of empty nose
syndrome reported directly by the patient. 7 (87.5%)
of the 8 Rhinaer complications were related to
epistaxis. 3 (37.5%) of these epistaxis episodes
required transfusions. Only 1 (14.3%) was
successfully treated with packing, and 6 (85.7%)
required operative intervention.
Conclusion:
Surgeons should exercise vigilance and tissue-
appropriate device settings when utilizing RF
devices. Epistaxis and tissue necrosis may occur, as
well as more rare, but devastating, complications.
POSTERS
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
73
Poster #030
Comprehensive patient-focused medical
illustrations to supplement the rhinology surgical
consent process
Chase Kahn, MD
Bita Naimi, BA
Alexander Duffy, MD
Emily Garvey, BA
Douglas Farquhar, MD
Elina Toskala, MD, MBA, PhD, FARS
Gurston Nyquist, MD, FARS
Marc Rosen, MD, FARS
Mindy Rabinowitz, MD, FARS
Thomas Jefferson University
Introduction: Previous studies have demonstrated
improved patient satisfaction and comprehension
when patients are provided education in a focused
manner. In surgical populations, supplemental media
materials have been used to educate patients on
disease pathophysiology and treatment and have
been deemed of limited usefulness and poor overall
validity for patient information. Anatomically accurate
illustrations can be linked to written or spoken text,
which can markedly increase a patient’s attention,
comprehension, and recall of clinical information.
Currently, there are no studies that have investigated
the practicality of medical illustrations to supplement
the surgical consent process for rhinology surgery.
Objective: This study aims to investigate the benefits
of incorporating specifically designed anatomic
illustrations to improve patient health literacy during
the surgical consent process.
Methods: Detailed anatomically accurate illustrations
were developed in concert with the study PI and a
medical illustrator. Pre-and post-operative images
along with common disease states created to cover
common rhinologic procedures including the surgical
management of epistaxis, dacryocystorhinostomy,
endoscopic sinus surgery, and endonasal pituitary
surgery. Double-sided documents were created with
illustrations on one side and a narrative on the
reverse reiterating the surgical intervention
associated with those images. These were designed
to mimic the pre-operative surgical discussion.
Conclusion: Providers can use these documents
during their surgical discussion to reiterate the
highlights of the discussion and send the patient
home with a visual reminder.
Poster #031
Contemporary update on the microbiology of
paranasal sinusitis
Alan Workman, MD, MTR
Margaret Mitchell, Resident Physician
Richard Lu, Medical Student
Neil Bhattacharyya, MD
Introduction:
Rhinosinusitis, whether acute, recurrent, or chronic,
is thought to be at least in part be characterized by a
disruption of microbiology. Existing studies on the
microbiology of sinusitis, however, are limited by
their sample size.
Methods:
We identified patients within a large health system
that had sinus cultures taken by an otolaryngologist
with a concurrent diagnosis of acute or chronic
rhinosinusitis. These cultures were analyzed based
on their culture type and result.
Results:
A total of 2,302 culture samples were collected,
2,012 (87%) of which were bacterial cultures and
287 (13%) which were fungal cultures. More than
half (1142, 57%) of the bacterial cultures resulted
positively, or with a named genus, while 592 (29%)
were normal sinus flora, 16 (0.8%) resulted as
normal oral flora, and 183 (9%) resulted as no
growth. The most common genus identified was
Staphylococcus (383, 34%), most commonly S.
aureus (311, 81%), 42 of which (14%) showed
methicillin resistance (MRSA). Of the positive
bacterial cultures with named genera, those
represented were Propionibacterium (145, 13%),
Haemophilus (101, 9%), Pseudomonas (94, 8%),
and Streptococcus (83, 7%). Of fungal cultures, 265
(92%) resulted in no growth.
Discussion:
Within a sample of over 2,000 sinus bacterial
cultures, 57% resulted positively with identification of
a named genus, highlighting the utility of this assay.
Alternatively, the vast majority of fungal cultures
showed no growth, suggesting a lack of utility when
treating patients with sinus symptoms. This update
on the microbiology of sinusitis offers both insight
into the baseline nasal microbiology of a broad
population as well as commenting on the potential
utility of sinus culture data.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
74
Poster #032
Cranial neuropathies secondary to allergic fungal
rhinosinusitis
Ashleigh Halderman, MD, FARS
Sei Chung, MD
Kendra Stephen
Nina Stephen
Jenny Kim
University of Texas Southwestern
Background:
Though allergic fungal rhinosinusitis (AFRS) is a
benign, noninvasive process, advanced disease can
result in orbital and skull base erosion resulting in
cranial neuropathies. This review examines the
demographic and clinical characteristics of such
patients.
Methods:
This review describes 55 patients with AFRS, of
which 6 presented with cranial nerve (CN) deficits.
Data on demographics, clinical findings, and patient
anatomy were analyzed using independent t-and
Pearson’s chi-squared tests as appropriate.
Results:
The average age of AFRS patients who presented
with cranial neuropathies was 36 years, which did
not significantly differ from the remaining AFRS
cohort (34 years). Among AFRS patients with CN
deficits, 3 were Black and 3 were White, and there
was an equal distribution by gender. AFRS patients
with CN deficits had significantly higher eosinophil
levels (p=0.01) and absolute eosinophil counts
(p=0.02), compared to AFRS patients without cranial
neuropathies. The total Lund-Mackay scores did not
significantly differ between those with or without
cranial neuropathies. Among AFRS patients with CN
deficits, one patient demonstrated pansinus complete
opacification, and all others had sphenoid-
predominant disease with a posterior pattern of
expansion and erosion. Patients presented with
vision loss (n=6) secondary to optic canal
dehiscence, or CN III or VI palsy (n=2) due to
posteriorly erosive disease at the sphenoclival skull
base.
Conclusions:
AFRS can rarely present with cranial neuropathies
when the disease pattern is sphenoid-predominant
and expansile in a posterior direction towards the
sphenoclival skull base. There may be a propensity
to develop this form of advanced AFRS in those with
greater peripheral.
Poster #033
Craniofacial pain locations and outcomes after
endoscopic sinus surgery for unilateral sphenoid
sinusitis: A multi-institutional study
Richard Pellizzari, BS
John Craig, MD, FARS
Alberto Saibene, MD, MA
Luigi De Donato, MD
Benjamin Bitner , MD
Rijul Kshirsagar, MD
Jennifer Douglas, MD
Edward Kuan, MD, MBA, FARS
Nithin Adappa, MD, FARS
Jacob Eide, MD
Henry Ford Health
Introduction:
Unilateral radiographic sphenoid sinus opacification
is caused by a variety of pathologies including
inflammatory and infectious sinusitis, tumors, and
encephaloceles. The purpose of this study was to
report craniofacial pain locations and outcomes in
unilateral sphenoid sinusitis (USS) patients who
underwent endoscopic sinus surgery (ESS).
Methods:
A multi-institutional retrospective cohort study was
conducted on all adult patients who had ESS for
USS from 2015-2022. Patient demographics,
presenting symptoms and nasal endoscopy findings,
surgical extent, and craniofacial pain outcomes were
recorded. Exclusion criteria included age <18 years,
immunodeficiency, invasive fungal sinusitis, and
neoplasia. Descriptive statistics were calculated.
Results:
Of the 52 study patients, mean age was 61 +/- 15
years, and 71.2% were female. Craniofacial pain
was present in 65.4% of patients in the following
locations: retrobulbar (47.1%), frontal/forehead
(47.1%), whole head/face (17.6%), maxillary/cheek
(17.6%), occipital (14.7%), and vertex (8.8%). Most
patients had normal nasal endoscopies, while 26.9%
had mucopurulence, 11.5% edema, and 7.7% polyps
in the sphenoethmoid recess. The most common
pathologies were fungal ball (36.5%) and chronic
rhinosinusitis without nasal polyps (23.1%). Of the
34 patients with craniofacial pain, 76.5% resolved by
their first postoperative visits (mean 10.6 days) and
88.2% resolved by their second postoperative visits
(mean 38.9 days).
Conclusion:
In USS patients, the most common craniofacial pain
locations were retrobulbar and frontal/forehead, with
a minority having occipital and vertex pain. ESS
resolved the craniofacial pain in nearly 90% of
patients.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
75
Poster #034
CRSwNP patients using biologicals: real-world
experience in a reference center
Wilma Anselmo-Lima, MD, PhD
Vanessa Dinarti, PhD
Gabriela Silveira, MD
Otavio Mieli, MD
José Lemos, MD
Marcio Nakanishi, PhD
Denny Garcia, PhD
Luisa Arruda, PhD
Fabiana Valera, PhD
Edwin Tamashiro, PhD
Ribeirão Preto Medical School of University of São
Paulo
Background:
CRSwNP is predominantly a type 2 inflammatory
disease in Western populations. In difficult-to-control
patients, anti-type 2 biologicals have been shown to
be an effective rescue treatment. However, there are
limited data on CRSwNP patients undergoing
biologicals outside Europe and the US. Aim: To
evaluate outcomes in difficult-to-control CRSwNP
patients undergoing dupilumab treatment in a
reference center.
Methods:
24 patients from São Paulo, Brazil, unresponsive to
conventional treatments who received dupilumab for
at least 3 months were evaluated by blood eosinophil
counts, Lund–Kennedy (LK) endoscopic score,
SNOT-22, and olfactometry. Pre and post-treatment
parameters were compared.
Results:
Patients presented a mean age of 49.4 years, 69%
had AERD and 23.1% had asthma associated only.
Median blood eosinophilia was 600 cells/uL (P25-
75= 350-1000) Median time of Dupilumab use was 9
months (P25-75= 5.3-16 months). Dupilumab
promoted a significant improvement in SNOT-22
scores (Δ=-34.5, p<0.0001), LK score (Δ=-4.5,
p<0.0001), and olfactory test (p<0.0001). Length
time of use was associated with better outcomes in
LK and olfactory test, but not for SNOT-22. Three
patients discontinued the use of dupilumab (despite
sinonasal symptoms were controlled) due to adverse
events.
Conclusions:
In our center, most of patients experienced a
significant improvement in symptoms and objective
measures in patients with CRSwNP treated with with
Dupilumab. Prospective follow-up is necessary to
better elucidate long-term efficacy and incidence of
side effects.
Poster #035
Current otolaryngologic applications of the novel
self-assembling RADA-16 peptide matrix
Arthur Wu, MD, FARS
Kaitlynne Pak
Dennis Tang MD, FARS
Satyan Sreenath, MD
Christopher Ito, MD, FARS
Brent Senior, MD, ARS
Kent Lam, MD, FARS
Thomas Higgins, MD, FARS
Kevin Hur, MD
Benjamin Tam
Cedars-Sinai
Background:
PuraGel® is a novel RADA-16 based self-
assembling peptide matrix gel intended to prevent
adhesions between mucosal surfaces, control
minimal bleeding following surgery or nasal trauma,
and act as an adjunct to aid in the natural healing
process. Current literature is sparse but includes use
in nasopharyngeal stenosis, turbinate reduction, and
sinus surgery. The goal of this study is to determine
current use patterns and possible complications
among US otolaryngologists.
Methods:
A list of current US academic institutions who have
used RADA16 was obtained and a brief survey was
distributed. Number and type of cases as well as
complications were queried.
Results:
7 of the 13 current academic sites using the product
responded, including seven academic rhinologists.
The product was used in 174 cases including 84
FESS, 41 septoplasty/turbinate reduction, 11
nasoseptal flap donor sites, 4 Draf III, 14 medial
maxillectomies, 6 sinonasal tumor resections (non-
inverted papilloma), 8 tonsillectomies, and 5 nasal
stenosis. There were 13 complications encountered.
Complications mostly were related to stensosis and
bleeding. There were 6 instances of sinonasal
scarring/stenosis, 4 of which required reoperation.
There were 2 tonsil bleeds and 3 episodes of
epistaxis.
Conclusion:
As with any novel technology, there is a learning
curve with the usage of this product. The RADA-16
gel appears to have novel uses for promoting
mucosal healing, providing a matrix for migrating
cells to repopulate and heal denuded tissue.
However, when used in tight areas where it might fill
potential space, there is a possibility for creating
stenosis. Further studies will be helpful to determine
appropriate use and applications of this novel
product.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
76
Poster #036
Development of a novel quantitative PCR assay
for diagnosis of rhinocerebral mucormycosis
Tom Maxim, MD
Jivianne Lee, MD, FARS
Eri Srivatsan
Albert Ko
Ashraf Ibrahim
Yiyou Gu
David Beenhouwer
Nicholas Jackson
Daniel Manzoor
David Geffen School of Medicine at UCLA
Introduction:
Rhinocerebral mucormycosis (RCM) is an
angioinvasive disease targeting the paranasal
sinuses and surrounding soft tissues, typically in
immune-compromised hosts. Frozen tissue analysis
is relied upon for expedited diagnosis but suffers
from reduced sensitivity (83-87.5%) in comparison to
permanent pathology, risking false negative results
and treatment delays. The Mucorales CotH3 protein
is a key mediator of host cell invasion, representing
a promising target for PCR development as an
alternative diagnostic method.
Methods:
Four custom primers/probes were developed
targeting highly conserved sequences of the CotH3
gene. Purified DNA from four of the most common
invasive Mucorales strains (Rhizopus delemar,
Mucor circinelloides, Lichtheimia, Rhizomucor) were
used to test primer performance in quantitative PCR.
Aspergillus fumigatus DNA served as negative
control. Cycle threshold (Ct) values were
established.
Results:
Average Ct values demonstrate primers 1, 2 and 4
amplified the target sequence of Rhizopus delemar
DNA at cycle 26 and dilute Rhizopus DNA at cycle
30-32. Primers 1 and 4 are most sensitive to
Rhizopus delemar, with Ct values 9-12 cycles lower
compared to the other Mucorales strains. Primer 4
showed highest sensitivity to Lichtheimia and Mucor
circinelloides. Rhizomucor was not amplified.
Aspergillus DNA showed no amplification of the
target sequence using primer 1, and non-specific
low-level amplification in 1 of 3 wells using primers 2
and 4.
Conclusions:
A novel quantitative PCR targeting the CotH3 gene
detects Mucorales DNA with high specificity and
sensitivity. Primer 4 showed the best overall
performance across multiple Mucorales strains and
merits further testing in human subjects.
Poster #037
Differences in patient characteristics with
unilateral versus bilateral allergic fungal
rhinosinusitis
Sei Chung, MD
Kendra Stephen
Nina Stephen
Jenny Kim
Ashleigh Halderman, MD, FARS
University of Texas Southwestern
Background:
Allergic fungal rhinosinusitis (AFRS) is a noninvasive
form of fungal sinusitis and is a subtype of chronic
sinusitis with nasal polyps (CRSwNP). Unlike other
forms of CRSwNP, AFRS can be unilateral or
bilateral. While various demographic factors as they
relate to disease severity and recalcitrance have
been previously evaluated, little work has looked at
potential differences between patients who present
with unilateral versus bilateral AFRS.
Methods:
A retrospective review identified 55 patients with
AFRS. Data on demographics, insurance status,
comorbidities, anatomic features, and CT findings
were analyzed using independent t-and Pearson’s
chi-squared tests.
Results:
32.7% had unilateral AFRS and 67.3% had bilateral
AFRS. Those with bilateral disease were older (38 vs
28 years, respectively; p=0.02), more likely to be
Black (p=0.04), and had active or prior tobacco use
(p=0.025). There was no significant difference in
insurance status. Neither septal deviation nor the
presence of concha bullosa were associated with
unilateral versus bilateral disease. There were no
significant differences in the presence of asthma or
self-reported allergic rhinitis. There was a trend
towards greater peripheral eosinophilia in those with
bilateral AFRS. Patients with bilateral AFRS were
significantly more likely to present with cranial nerve
deficits (p=0.02) secondary to expansile and erosive
disease at the sphenoid, petrous, and clival skull
base.
Conclusions:
Compared to patients with unilateral AFRS, those
with bilateral AFRS were older, more likely to be of
Black race, and have positive smoking history. To our
knowledge, this is the first study to describe
differences in patients with unilateral versus bilateral
disease.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
77
Poster #038
Dupilumab improved objective and patient-
reported outcomes in patients with chronic
rhinosinusitis with nasal polyps (CRSwNP) and
complete bilateral nasal obstruction in the sinus-
24 and sinus-52 trials
Prof. Claire Hopkins
Martin Wagenmann, MD, PhD
Asif Khan, Dr.
Claus Bachert, Dr.
Jerome Msihid, Dr.
Scott Nash, Dr.
Yamo Deniz, Dr.
Paul Rowe, Dr.
Harry Sacks, Dr.
Juby Jacob-Nara, Dr.
Düsseldorf University Hospital
Background:
In CRSwNP, a nasal polyp score (NPS) of 8/8
signifies complete bilateral nasal obstruction.
Dupilumab is efficacious in severe CRSwNP; here
we report outcomes in patients (pts) with NPS=8.
Methods:
Post-hoc analysis of pts with NPS=8 at
randomization (after 28 days’ intranasal
corticosteroids [CS]) in SINUS-24/52 (NCT02912468/
NCT02898454), receiving dupilumab 300 mg/
placebo every 2 weeks.
Objective assessments:
NPS (0−8), peak nasal inspiratory flow (PNIF),
Lund‒Mackay computed tomography (LMK-CT;
0−24); pt-reported assessments: nasal congestion,
loss of smell (NC, LoS; 0−3), 22 item Sino-Nasal
Outcome Test (SNOT-22; 0−110).
Results:
98/724 (13.5%) pts had baseline NPS=8 (placebo/
dupilumab, 30/68). Mean (SD) baseline PNIF (L/
min), LMK-CT, NC, LoS, SNOT-22 were 33.8 (45.1),
18.9 (3.9), 2.7 (0.4), 2.9 (0.3), 56.9 (21.6),
respectively. All assessments improved with
dupilumab vs placebo at Week 24 (least squares
mean difference [95% CI]): NPS −2.04 [−2.67,
−1.40], PNIF 65.9 [39.4, 92.4], LMK-CT −4.97
[−6.50, −3.44], NC −1.30 [−1.72, −0.89], LoS −0.96
[−1.39, −0.54], SNOT-22 −25.3 [−34.1, −16.4], with
similar results at Week 52. At Week 24,
69.1%/10.0% pts (dupilumab/placebo) achieved NPS
improvement ≥1; 51.5%/0% LMK-CT improvement
≥5; 73.5%/16.7% NC improvement ≥1; 60.3%/20.0%
LoS improvement ≥1; all P<0.0001; 73.5%/40.0%
SNOT-22 improvement ≥8.9 (P=0.001). Fewer pts
required systemic CS or sinonasal surgery through
Week 24 with dupilumab than placebo
(11.8%/36.7%, P=0.0005).
Conclusions:
In pts with CRSwNP and NPS=8, dupilumab
demonstrated significant, clinically relevant reduction
in NPS, improved nasal inspiratory flow, symptoms,
and health-related quality of life, and reduced need
for systemic CS/surgery vs placebo.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
78
Poster #039
Efficacy of olfactory training after unilateral
anterior skull base resection in patients with
olfactory neuroblastoma: A single-center
prospective study
Teppei Takeda, MD
Omura Kazuhiro
The Jikei University School of Medicine
Introduction:
Unilateral skull base resection for selected patients
with olfactory neuroblastoma is useful in controlling
the tumor while ensuring a minimally invasive
approach to the patient. Furthermore, unilateral skull
base resection has been reported to be useful in
preserving the sense of smell. However, not all cases
preserve the sense of smell. In the present study, we
investigated whether postoperative olfactory training
is useful in preserving the sense of smell after
unilateral anterior skull base resection.
Methods:
This study is a single-center case-control study. At
our institution, postoperative olfactory training has
been offered to patients who have undergone
unilateral anterior skull base resection since 2022.
Patients who underwent unilateral anterior skull base
resection only for ONB patients from 2018 to
December 2021 were defined as the control group,
while patients who underwent unilateral anterior skull
base resection and postoperative olfactory training
after January 2022 were defined as the case group,
and the olfactory preservation rate in each group was
examined. The same surgeon and anterior skull base
resection reconstruction method were used. Olfactory
function tests were conducted using Open Essence
to evaluate olfactory identification ability.
Results:
Six patients in the control group and seven patients
in the case group were analyzed. In an Open
Essence olfactory function test, 2 out of 6 (33%) in
the control group and 5 out of 7 (71%) in the case
group had a preserved sense of smell.
Conclusion:
Although the number of cases in this study is limited,
we believe that olfactory training intervention may
improve the
postoperative olfactory preservation rate.
Poster #040
Epithelial-myoepithelial carcinoma of the nasal
cavity. An interesting case report and review of
the literature
Ariel Waitzman, MD
Jacob Waitzman, Medical Student
Jeremy Powers Chief, Dept of Pathology
Rohan Deraniyagala, Assistant Professor
Epithelial-Myoepithelial carcinoma is an extremely
rare malignancy. We present a case study of a
patient with Epithelial-Myoepithelial carcinoma of the
nasal cavity, with presentation of clinical, radiologic
and pathologic images. The case report involves a
67 year old female presenting with nasal obstruction
and recurrent mild unilateral epistaxis. CT and
endoscopy demonstrated a friable polypoid mass
involving the septum and middle turbinate on the
right side. Endoscopic biopsy was consistent with an
Epithelial-Myoepithelial carcinoma, intermediate
grade. The case was presented at our Head and
Neck Tumor Board with a recommendation for
surgery, reserving radiation therapy for positive
margins or recurrent disease. The patient underwent
endoscopic resection with clear clinical margins.
Final pathology (the pathologist did not feel frozen
sections would be reliable with this tumor type)
revealed microscopic positive margins in 2 areas. A
second endoscopic resection was performed
removing tissue up to the skull base, again with no
clinically detectable tumor. Final pathology, however,
again revealed a microscopic positive margin at the
skull base. The patient subsequently underwent full
course radiation therapy to the right nasal cavity
including the skull base. The patient remains
disease free at this time and is closely followed.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
79
Poster #041
Eustachian tube recanalization via CO2 guidewire
and ureteral stent
Christopher Pool, MD
David Keschner
Kaiser Permanente Orange County
Patulous eustachian tube dysfunction is a rare
disorder that can be treated with different
medications and procedures aimed at improving
quality of life by decreasing or eliminating the
diameter of the eustachian tube orifice. Complete
obliteration of the eustachian orifice risks chronic
serous otitis media which can itself create substantial
morbidity. We describe a case of eustachian tube
recanalization after prior obliteration using a CO2
laser guidewire and a ureteral stent. The patient
underwent myringotomy with endoscopic placement
of the guidewire through the hypotympanic
eustachian tube orifice, combined with transnasal
endoscopic balloon dilation of the eustachian tube,
and subsequent retrieval in the nasal cavity. A
ureteral stent was then placed via Seldinger
technique. The stent was removed after three
months and with long term patency and resolution of
symptoms. This is the first case report to describe
recanalization using both balloon dilation and
ureteral stenting.
Poster #042
Evidence for a role of metformin in preventing
olfactory dysfunction among older adults
Sahar Assi, MD
Wuyang Zhang
Nicholas Reed
Andrew P. Lane, MD, FARS
Murray Ramanathan, MD, FARS
Nicholas Rowan, MD
Johns Hopkins Bloomberg School of Public Health
Background:
Olfactory dysfunction (OD) is increasingly recognized
as a hallmark of unhealthy aging and mortality, but
therapies remain elusive. Recognizing the increased
prevalence of OD in individuals with diabetes, and
the potential anti-aging effects of metformin, we
examined the association of metformin use with OD.
Methods:
Asynchronous cross-sectional study of participants
with diabetes from the National Social Life, Health,
and Aging Project (NSHAP), Waves 2 (2010-11) and
3 (2015-16). Olfactory sensitivity (OS), the ability to
detect the presence of an odorant, and olfactory
identification (OI), the ability to identify the odorant,
were tested. Weighted multivariable logistic
regression was used to examine the association
between metformin use at Wave 2 and odds of OS/
OI dysfunction at Wave 3, adjusted for age, sex,
race/ethnicity, education, BMI, HbA1c, and years
since diabetes diagnosis at Wave 2.
Results:
In a sample of 228 participants with diabetes (mean
age=69 years, 53% female, 21% Black), 112 (49%)
were metformin users. In the adjusted model, relative
to nonusers, metformin users had 63% lower odds of
OS dysfunction at Wave 3 (Odds Ratio [OR]=0.37,
[95% Confidence Interval=0.15-0.90] p=0.030). A
more pronounced association was observed in a
subgroup of 61 participants with normal OS function
at Wave 2, where metformin users had 96% lower
odds of OS dysfunction at Wave 3 (OR=0.04 [0.01-
0.16] p<0.001). While not statistically significant,
metformin use was associated with lower odds of OI
dysfunction (OR=0.56 [0.28-1.14]).
Conclusion:
Metformin use is associated with lower odds of OS
dysfunction among individuals with diabetes,
suggesting a potential protective effect mediated
through peripheral mechanisms of olfac
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
80
Poster #043
WITHDRAWN
Poster #044
Extramedullary plasma cell neoplasm in the
nasal cavity: Case presentation
Guillermo Antonio Ramirez, MD
Cesar Alfonso Gutierrez Espinoza, Dr.
Extramedullary plasmacytoma is a rare neoplasm,
however when it occurs, the ENT area is the most
frequently affected site. The few series of patients
reported in the literature, and especially in our
environment, mean that current management is not
very widespread. Diagnosis is somewhat difficult to
perform only with clinical elements, which makes the
laboratory and histopathological study with specific
techniques of vital importance. It is known that its
transformation into multiple myeloma constitutes the
main prognostic factor, hence the patient must
undergo to rigorous monitoring.
The case of a 78-year-old woman is presented, who
is registered as a secondary to a chest wall tumor
corresponding to a plasma cell neoplasm, which is
later evaluated due to presenting symptoms of nasal
obstruction predominantly left with outlet of mucous
discharge of months of evolution, which was
diagnosed as an extramedullary plasma cell
neoplasm
Clinically, they can manifest as a nasal mass,
increased volume and facial pain, airway obstruction,
epistaxis, rhinorrhea, proptosis, dysphagia or
dysphonia. In relation to its extension, 3 stages are
distinguished. The diagnosis of extramedullary
plasmacytoma is based on histological evidence of a
plasma cell tumor in an extramedullary location (not
bone) and without clinical, histological or radiological
evidence of multiple myeloma.
In the following work we address the presentation of
a clinical case and follow-up of a patient with plasma
cell neoplasia.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
81
Poster #045
Functional and structural correction of over-
reduced noses by non-rib grafts
Mohsen Naraghi, MD, FARS
Orphans World Wide
Introduction:
The selection of the ideal graft has been an issue of
concern for its donor site morbidity and other
possible problems such as graft visibility and
irregularities, infection, and inflammatory reactions.
This retrospective result describes the author’s
experience with non-rib diced cartilage fascia graft in
over-reduced Noses.
Methods:
Thirty-seven secondary rhinoplasty cases underwent
non-rib diced cartilage grafts with facia temporalis
augmentation from 2015 to 2022. Combining open
and endoscopic approaches provided good material
for structural support and camouflage purposes
exclusively from the non-rib sources, including
septum and concha cartilage.
Results:
Functional and aesthetic results revealed significant
improvement in all patients. Three cases with more
resorption in the supra-tip area were managed non-
surgically. Four cases underwent postoperative
massage to refine the molding of cartilages up to two
weeks after surgery. Improvement of over-resected
dorsum on profile and restoration of parallel aesthetic
lines were our cases’ most common improvement
items.
Conclusion:
Advantages of non-rib graft include: Avoiding any
incision in the chest to harvest rib cartilage; Using
minimal cartilage from dierent sources; Less
visibility over time; Decreased risk of torsion and
warping of the graft; Complete attachment of the
graft to the recipient bed, ensuring more stability;
More compatibility with an asymmetric bed with bony
and cartilaginous irregularities and more eectively
camouflaging such asymmetries; Flexibility and
compliance of the soft cartilage fascia graft to be
massaged and modified meticulously even in
postoperative visits.
Poster #046
Gender differences in quality of life in patients
with skull base pathologies
Parker Tumlin, MD
Meghan Turner, MD
Hassan Ramadan, MD, FARS
Chadi Makary, MD, FARS
Background: Recent studies showed that female
patients with chronic rhinosinusitis (CRS) suffer a
worse disease-specific quality of life (QoL).
Goal: To investigate gender differences in QoL in
non-rhinosinusitis patients with sinonasal and skull
base pathologies.
Methods:
Cross-sectional analysis of patients presenting to
West Virginia University Otolaryngology clinic from
August 2020 to November 2022 with inverted
papilloma (IP), spontaneous CSF rhinorrhea, Grave’s
orbitopathy (referred for orbital decompression), and
skull base tumors was performed. Baseline QoL was
measured using the sinonasal outcome test-22
(SNOT-22). Patients’ demographics and
comorbidities were reviewed. Patients with
concomitant CRS were excluded.
Results:
98 patients were included (50 with skull base tumors,
19 Grave’s orbitopathy, 15 CSF rhinorrhea, and 14
IP). Mean age was 53.6 years (12-4-81.5), 52% were
female. There was no age difference between
females and males. Smoking history, asthma, and
allergic rhinitis were also similar between the two
groups. Males were more likely to have nasal septal
deviation (38.2% vs 17.8%, p=0.04). Overall SNOT-
22 was similar between females and males (30.3 vs
22.7, p=0.06). However, females had significantly
worse scores in the ear/facial, psychological, and
sleep subdomains (5.2 vs 3.2, p=0.019; 12 vs 6.9,
p=0.004; 10.1 vs 6.9, p=0.035 respectively). Similar
results were obtained in patients with skull base
tumors.
Conclusion:
Female patients with non-rhinosinusitis sinonasal
and skull base pathologies show higher non-
rhinological subjective disease burden. Further
studies with larger sample sizes are needed to
confirm these findings.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
82
Poster #047
Granulomatosis with polyangiitis presenting with
skull base inflammation mimicking petrous
apicitis: A case report and literature review
Michael Castle, MD
Matthew Carter, Medical Student
Alexander Poulakis, Medical Student
Li-Xing Man, MD, FARS
Isaac Schmale, MD
University of Rochester Medical Center
Background:
Granulomatosis with polyangiitis (GPA) is an
autoimmune granulomatous disease. Non-classic
clinical presentations of GPA can provide diagnostic
challenges and lead to delays in diagnosis. We
present a unique case highlighting rare
manifestations of GPA including primarily skull base
inflammatory findings.
Case Description:
A 29-year-old male presented with headache, right
otorrhea, cranial neuropathies, and hearing loss.
Labs showed an elevated ESR and CRP. Initial CT
and MRI demonstrated enhancement of the petrous
apex. Flexible laryngoscopy showed nasal crusting
and a large septal perforation. Despite normal vital
signs and normal white count, his initial management
was for an infectious etiology. Further workup
revealed proteinuria and c-ANCA positivity, and a
kidney biopsy established a diagnosis of GPA. Later
nasal endoscopy confirmed extensive nasal crusting
and large septal perforation consistent with GPA.
Discussion and Review:
There are approximately 20 studies that describe
GPA presentations involving the skull base. In the
largest retrospective review of 29 patients, no
patients had otorrhea. To date, otorrhea has been
reported in 2 patients with GPA. In one report,
otorrhea and skull base findings on imaging led to
infectious treatment, thus highlighting the confusion
seen in this rare pattern of GPA presentation.
Conclusion:
Autoimmune workup should be considered in
patients with skull base enhancement on imaging
that is not consistent with neoplasia or severe
infection. Likely to be consulted in such cases, the
otolaryngologist should keep a high index of
suspicion for GPA in the setting of unexplained skull
base inflammation, coexistent septal perforations,
and nasal crusting.
Poster #048
Histopathologic features of patients with
noninvasive fungal rhinosinusitis
Tamara Simpson, BA
Ali M. Baird, Medical Student
Pete Batra, MD, FARS
Peter Filip, MD
Hannah J. Brown, MD
Sarah Khalife, MD
Paolo Gattuso, MD
Bobby A. Tajudeen, MD, FARS
Peter Papagiannopoulos, MD
Rush Medical College
Introduction:
Noninvasive fungal rhinosinusitis (FRS) can be
subclassified into allergic fungal rhinosinusitis
(AFRS) or fungal ball (FB). This study investigates
the histopathologic features of noninvasive FRS to
further understand its distinct pathogenesis from
other types of chronic rhinosinusitis (CRS). Currently
there are no studies that examine histopathologic
features of noninvasive fungal disease.
Methods:
A retrospective review of 468 patients undergoing
functional endoscopic sinus surgery (FESS) was
performed. Data was collected on patient
demographics, medical comorbidities, and structured
histopathology reports consisting of 13 variables.
Results:
Of 36 patients with noninvasive FRS, 21 (58.3%) had
FB and 15 (41.7%) had AFRS. Patients with AFRS
had increased tissue eosinophilia (>5 per HPF)
compared to FB (86.7% vs 19.0%, p<0.001). 432
patients comprised the CRS control group. The
mean age for the noninvasive FRS group was 54.1
years compared to 50.1 years for the CRS group.
The noninvasive FRS group had higher rates of
severe overall inflammation compared to the CRS
controls (33.3% vs. 3.9%, p<0.001). The noninvasive
FRS group showed increased fungal elements
(27.8% vs. 4.4%, p<0.001), subepithelial edema
(63.9% vs. 43.8%, p=0.02), and Charcot-Leyden
crystals (17.1% vs. 4.6%, p=0.002).
Conclusion:
Histopathologic analysis of noninvasive FRS showed
increased extra mucosal fungal elements, moderate
to severe overall degree of inflammation,
subepithelial edema, fibrosis, and Charcot-Leyden
crystals compared to non-fungal CRS. These
variables represent unique differences in the
pathogenesis of noninvasive fungal disease;
therefore, possible targets in diagnosis and treatment
could benefit disease progression.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
83
Poster #049
WITHDRAWN
Poster #050
Impact of insurance status on CSF leak
presentation
Ali M. Baird, BS
Jamie Masliah, Resident
Peter Filip, MD
Sarah Khalife, MD
Peter Papagiannopoulos, MD
Pete Batra, MD, FARS
Bobby Tajudeen, MD, FARS
Rush Medical College
Introduction:
Spontaneous cerebrospinal fluid (CSF) leaks are
known complications of idiopathic intracranial
hypertension (IIH), a disease that disproportionally
affects Black and Hispanic women. Prior studies
demonstrated that patients with IIH had lower
median household incomes and lived in food
swamps. The aim of this study is to identify
relationships between health disparities, measured
by insurance status, and the clinical presentation of
CSF leaks in patients with IIH.
Methods:
A retrospective chart review was conducted of
patients with IIH who underwent surgical
management for spontaneous CSF leaks from 2009
to 2022. Data was collected on patient
demographics, health insurance status (Medicaid,
Medicare or private), zip codes, and CSF leak
presentation.
Results:
50 patients undergoing treatment for spontaneous
CSF leaks were analyzed with a mean age of 56.1
+/- 12.6 years and a mean BMI of 38.9 +/- 7.38. 13
patients had Medicaid insurance, 7 had Medicare
insurance, and 30 had private insurance. Black (n=8,
61.5%) and Hispanic patients (n=3, 23.1%) made up
the majority of the Medicaid group. Although not
statistically significant, patients with Medicaid
compared to patients with Medicare or private
insurance were more likely to present with
preoperative meningitis (38.5% vs 14.3% and 16.7%,
p= 0.247) and have a higher number of skull base
dehiscences (2.38 vs 1.86 and 1.87, p=0.441).
Conclusion:
Insurance status acts as one marker for the social
determinants of health and may predict severity at
presentation in patients with spontaneous CSF leaks.
Patients with Medicaid coverage were more likely to
present with preoperative meningitis or multiple skull
base dehiscences, indicating a prolonged
presentation.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
84
Poster #051
Impact of LYR-210 corticosteroid matrices on the
incidence of acute exacerbations of chronic
rhinosinusitis in patients from the LANTERN
randomized controlled study
Vineeta Belanger, PhD
Brent Senior, MD, FARS
Agnieszka Wrobel
Anders Cervin, MD, PhD
Lindsay Brayton, Clinical Project Manager
Allison Gartung
Lyra Therapeutics, Inc.
Background:
LYR-210 is an implantable corticosteroid matrix
designed to provide up to 24 weeks of localized
sinonasal treatment for surgically naïve chronic
rhinosinusitis (CRS) patients. LYR-210 (7500µg)
demonstrated safety and significant efficacy
improvements compared to control at week 24 in the
LANTERN study. This presentation reports the
impact of LYR-210 on the incidence of acute
exacerbations of CRS (AECS) in patients from the
LANTERN study.
Methods:
Symptomatic adult CRS patients who failed previous
medical management were enrolled in a multicenter,
blinded, randomized, controlled Phase 2 LANTERN
study, and received bilateral administration of LYR-
210 (7500µg) (N=21) or LYR-210 (2500µg) (N=23) or
sham-procedure control (N=23). Percentages of
patients experiencing AECS, defined as a sudden
worsening of symptoms resulting in the treating
physician reporting an escalation of treatment, was
prespecified as an exploratory endpoint and
assessed at weeks 4, 8, 12, 16, 20, and 24. The
number and proportion of patients experiencing
AECS, along with two-sided 90% confidence
intervals (CIs) vs. control were determined.
Results:
Two LYR-210 (7500µg)-treated patients (9.5%) [CI:
-0.4, -0.019], five LYR-210 (2500µg)-treated patients
(21.7%) [CI: -0.3, 0.13], and seven control patients
(30.4%) experienced an AECS by week 24. The first
incidence of AECS in the control group occurred by
week 4, compared to week 20 for the LYR-210
(7500µg) group.
Conclusion:
There was a reduction in the occurrence of AECS in
the LYR-210 (7500µg) group compared to control
during the 24-week treatment period in the
LANTERN study. This important clinical effect is
being studied further in the pivotal Phase 3 trials of
LYR-210 (ENLIGHTEN I & ENLIGHTEN II).
Poster #052
Impact of social determinants of health in
chronic rhinosinusitis disease severity: A
scoping review
Avigeet Gupta, MD
Julian Purrinos, Medical Student
Kibwei McKinney, MD
Renata Grozovksy, Clinical Research Scientist
Corinna Levine, MD, FARS
The University of Oklahoma Health Sciences Center
Background:
While social determinants of health (SDoH) are
known to influence chronic rhinosinusitis (CRS), little
is known regarding the specific impact of SDoH on
CRS disease severity. This comprehensive scoping
review summarizes the existing body of literature to
assess the size and scope of the current literature
examining the impact of SDOH on objective markers
of CRS severity.
Methods:
We performed a scoping review of the PubMed,
Ovid, and EMBASE databases with assistance of
senior librarian in accordance with the Preferred
Reporting Items for Systematic Reviews and Meta-
Analysis extension for Scoping Reviews (PRISMA-
Scr) checklist.
Results:
A total of 1516 references were identified, of which
1285 underwent title and abstract screening. 215 full-
text articles were reviewed, and 21 articles met
inclusion criteria for analysis of outcomes data.
Several SDoH themes with regards to outcome
measures for CRS were ascertained from the
literature search including sex, race, ethnicity,
socioeconomic status, behavioral and lifestyle
outcomes, and environmental exposures. The
majority of articles contained heterogenous
outcomes without statistically significant differences
for Lund-McKay and Lund-Kennedy Scores among
the identified SDoH themes. Several articles found
worse radiographic or endoscopic CRS disease
severity associated with SDoH categories of male
sex, African-American race, smoking, and lower
socioeconomic status.
Conclusions:
This scoping review highlights the paucity of
rhinology literature regarding the influence of SDoH
on objective CRS disease severity. Further research
efforts should be directed towards understanding
these differences in various populations with CRS.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
85
Poster #053
Incident diagnosis of granulomatosis with
polyangiitis in chronic rhinosinusitis receiving
sinus surgery
Trisha Shang, BA
David Kaelber, Chief Medical Informatics Officer
Mohamad Chaaban, MD, FARS
Case Western Reserve University
Purpose:
Granulomatosis with polyangiitis (GPA) is a disease
that can first present with chronic rhinosinusitis
(CRS). Patients are sometimes diagnosed with GPA
after sinus surgery. Our study aimed to determine
GPA incident diagnosis in CRS patients with and
without sinus surgery.
Methods:
We conducted a retrospective study using the
TriNetX US Collaborative Network platform. We used
encounter diagnosis ICD codes and surgery CPT
codes. We included adults with a CRS encounter
diagnosis who had sinus surgery after a CRS
encounter diagnosis versus those without sinus
surgery. Our outcome was a GPA encounter
diagnosis 1 month-5 years after CRS diagnosis and
sinus surgery (if received). We analyzed time to GPA
diagnosis by the proportion of patients with GPA in
each group diagnosed annually for 5 years after their
first CRS diagnosis. For GPA patients in each group,
we also compared nasal septal perforation (NSP)
incidence.
Results:
After a 1:1 propensity match on sex, ethnicity, and
race, n=246,525 in each cohort. CRS patients with
sinus surgery had higher incidence of a GPA
encounter diagnosis versus those without sinus
surgery (RR: 3.44, 95% CI [2.83, 4.17]). A
significantly greater proportion of patients with sinus
surgery had a GPA encounter diagnosis in years 1-3
post-CRS encounter diagnosis than those without
sinus surgery. GPA patients with sinus surgery had
significantly higher (4.88, [2.04, 11.66]) NSP
incidence than those without sinus surgery.
Conclusion:
Incident GPA encounter diagnosis is higher and
earlier in patients with at least one CRS encounter
diagnosis and sinus surgery. With higher risk for
complications like NSPs, more awareness and
research are needed to help identify these patients
preoperatively.
Poster #054
Insight into the mutational landscape of
sinonasal squamous cell carcinoma
Arash Abiri, MS
Brandon Lehrich, BS
Theodore Nguyen, MD
Benjamin Bitner, MD
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
Genetic mutations play a crucial role in the
development and progression of sinonasal
squamous cell carcinoma (SNSCC). Understanding
how these mutations drive disease progression and
impact patient survival can help guide cancer
management and patient counseling.
Methods:
We queried the American Association for Cancer
Research (AACR) Genomics Evidence Neoplasia
Information Exchange (GENIE) database (v13.0-
public), which is a publicly available cancer registry
collecting de-identified clinic-genomic data across 19
cancer centers. Cox Proportional Hazards and
Kaplan-Meier analyses were used to evaluate
differences in all-cause mortality and overall survival
(OS), respectively.
Results:
Of 59 SNSCC patients, 34 presented with primary
malignancies, 10 (29.4%) of whom were female. The
average age of this cohort was 58.4 ± 14.9 years,
and the median tumor mutational burden (TMB) was
6 (range: 1-59). The 1-, 2-, and 5-year OS of the
cohort was 88.2%, 56.1%, and 35.6%, respectively.
The most common gene mutations were TP53
(38.2%), FANCA (17.6%), PIK3CA (17.6%), KMT2D
(17.6%), and FBXW7 (14.7%). Higher TMB was
associated with increased all-cause mortality (HR
1.077; 95% CI, 1.008-1.151; p=0.029). Tumors with
TP53 mutations were associated with lower OS
(p=0.046).
Conclusions:
Higher tumor mutational burden and TP53 mutation
were found to be predictors of lower OS in patients
with primary SNSCC.
POSTERS
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
86
Poster #055
Interleukin(IL)-4 induces loss of smell in mice
without disrupting olfactory sensory neuron and
epithelial integrity
Hamid Mattoo, Dr.
Yannis Hara, PhD
Mithilesh Kumar Jha, Dr.
Scott Nash, Dr.
Asif Khan, Dr.
Jamie Orengo, Dr.
Alexandra Hicks, Dr.
Sanofi
Background:
Recent studies in mice showed that administration of
IL-4, but not IL-13, induces loss of smell, and IL-4
has a dominant effect on transcriptome, including
activation of immune pathways and impairment of
olfactory neuronal signaling. Here, we conducted
histological analysis of the effects of IL-4 and IL-13 in
the olfactory epithelium to further explore the
mechanism of IL-4-evoked loss of smell.
Methods:
BALB/cJ mice received intranasal administration of
IL-4 and/or IL-13 daily for 5 days and the olfactory
epithelium subjected to histological analysis.
Immunofluorescence was used to detect immune cell
infiltration (anti-CD45, anti-CD68, and anti-tryptase
for total immune cells, macrophages, and mast cells,
respectively), apoptosis (anti-cleaved caspase-3),
proliferation (anti-Ki67), immature olfactory neurons
(anti-GAP43), mature olfactory neurons (anti-OMP),
and horizontal basal cells (anti-Krt5).
Results:
IL-4, but not IL-13, induced significant infiltration of
immune cells, including mast cells and macrophages.
Neither cytokine induced apoptosis, affected
immature or mature olfactory neuronal integrity, or
altered basal cell proliferation.
Conclusions:
IL-4 administration elicits loss of smell in mice
without inducing structural modification of the
olfactory mucosa, suggesting that a direct effect of
IL-4 on olfactory neuronal signaling may underlie this
pathophysiology. Furthermore, inflammatory cell
mechanisms may play an additional role in IL-4
evoked loss of smell.
Poster #056
Is it NPC? Endoscopic image recognition of NPC
using narrowing band imaging versus white light
using deep learning network analysis
Shuhui Xu, MBBS,MRCS(Ireland),MMed(ORL)
Chwee Ming Lim, Senior Consultant
Neville Teo, MBBS
Singapore General Hospital
Purpose:
Develop an AI model that assists in cancer detection
in the post-nasal space during nasoendoscopic using
narrow band imaging versus white light.
Method:
Nasoendoscopy of patients with and without NPC
were recorded in both white light and narrow band
imaging. From each video, image frames were
sampled at 5 images per second and subdivided into
sub-directories based on the light source and nasal
region with malignant/normal annotations. Of the 82
videos, image frames from 63 videos (44 normal and
19 with malignant lesions) were used to train the AI
model and images from 17 videos (12 normal and 5
with malignant lesions) to test the model
performance. Convolutional Neural Networks (CNN)
(ResNet18 and ResNet50), and a transformer model
(ViT) were used in the experiments. As the dataset is
severely long-tailed for both “all region” and “Post-
nasal space” only region experiments, a class-
balanced sampling approach was adopted during the
training regimeIn all experiments, all models were
trained based on binary cross-entropy loss and using
adam optimizer. All experiments followed a batch
size = 64, a learning rate = 1x10^(-6) and trained for
41 epochs. The model performances were evaluated
based on accuracy, recall, precision and F1 score.
Results:
ResNet50 model trained using class-balanced
sampling was observed to perform better than the
model models. It was observed that the model
trained on a white-light source image performed
better than models trained on blue-light source
images. When we consider the class-specific
accuracy, the malignant lesion detection accuracy
was 83.7%.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
87
Poster #057
WITHDRAWN
Poster #058
Locally recurrent nasopharyngeal carcinoma
treated with minimally invasive combined
transoral robotic and transnasal endoscopic
resection: A case report
Abdurrahman Al-Awady, Mr.
David Lerner, MD
Michael Berger, MD
Alfred-Marc Iloreta, MD
Scott Roof, Dr.
Background:
Recurrent nasopharyngeal carcinoma (NPC) after
treatment with radiation represents a surgical
challenge due to the close proximity to skull base
structures and difficult access. Traditionally, open
approaches were employed, but are associated with
significant morbidity. We present a case of locally
recurrent NPC involving the clivus which was
resected using a combined transoral robotic and
endoscopic transnasal approach.
Case:
Patient is 73 year old male with history of cT3N2M0
EBV-related nasopharyngeal squamous cell
carcinoma treated with chemoradiation, which
recurred locally in the left nasopharynx and clivus 7
months after completion of treatment. Resection was
performed using a combined transoral robotic and
endoscopic approach, achieving negative margins.
The transoral robotic approach allowed excellent
visualization of the inferior and lateral margins (torus
tubarii). The transanasal endoscopic portion was
used to accomplish the superior extent of the
nasopharyngectomy and drilling of the clival bone.
Reconstruction was performed with anterolateral
thigh free fascial flap (ATL) combined endonasal and
transoral corridor. Microvascular anastomosis
employed facial vessels at the facial notch, avoiding
a standard neck incision. Patient is currently with no
evidence of disease, velopharyngeal insufficiency or
aspiration.
Discussion:
We present a case in which a combined transoral
robotic and transnasal endoscopic approach was
used to accomplish a salvage nasopharyngectomy.
Reconstruction was performed using an ATL free
fascial flap, with minimal invasive microvascular
anastomosis. This combined approach allowed for
superior visualization of the salvage resection as well
as a minimally invasive reconstruction.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
88
Poster #059
Long term quality of life among patients
undergoing endoscopic pituitary gland surgery
Narin N. Carmel Neiderman, MD, MSc
TASMC
Introduction:
The endoscopic approach to Pituitary adenoma
resection is less aggressive associated with
decreased morbidity, yet to date it was not evaluated
for long term nasal and tumor related quality of life
(QOL).
Objective:
To evaluate long term quality of life in patients after
endoscopic endonasal resection of pituitary tumors
and detect predictors for poor quality of life.
Materials and Methods:
Prospective cohort study of all patients with pituitary
adenomas who underwent transsphenoidal surgery
at Tel Aviv Sourasky Medical Center between 2014
and 2021. Recruited patients completed the Anterior
Skull Base Disease-Specific QOL (ASBS-Q)
questionnaire and the Sinonasal Outcome Test 22
(SNOT-22) questionnaire prior to surgery, and 1,2
and 3 to 5 years after surgery. Demographic and
clinical data was collected.
Results:
Our study included 43 patients. The overall ASBS-Q
and SNOT-22 scores did not decrease throughout
the duration of the study. SNOT-22 Score difference
between baseline and the year 1,3,5 was found to be
0.81[-4.84-6.58], 3.35[-4.32-11.02], 3.73[-2.22-9.68]
accordingly, and were not found statistically
significant. ASBS-Q score difference also did not
alter significantly (0.24[0.02-0.45], 0.18[-0.05-0.404],
0.101[-0.12-0.32] accordingly). Factors such as
secreting and non-secreting tumors, tumor size,
intraoperative cerebrospinal fluid leak, gross tumor
resection,
endocrine remission, and the use of nasoseptal flap
reconstruction did not have a significant effect on
QOL.
Conclusion:
Patients undergoing extended endoscopic approach
for pituitary lesions maintained high nasal and and
tumor related QOL in the 5 post-operative years.
Poster #060
WITHDRAWN
POSTERS
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
89
Poster #061
Metastatic anterior skull base adenocarcinoma
presenting as hearing loss
Margaret Mitchell, MD, MS-HPEd
Lillian Dattilo, Dr.
Obinna Nwosu, Dr.
Bradley Welling, Dr.
Eric Holbrook, MD, FARS
Harvard Medical School/Mass Eye and Ear
Objective:
To describe a case of metastatic adenocarcinoma to
the cribriform plate region and leptomeninges
presenting as bilateral hearing loss.
Methods:
Retrospective chart and histopathological review
were utilized.
Results:
A 62 year-old man presented to the emergency
department with two months of progressive bilateral
hearing loss, otalgia, and imbalance. His otologic
exam was normal with audiogram demonstrating
bilateral profound sensorineural hearing loss. He
underwent CT imaging which showed no
abnormalities of temporal bones but abnormal
demineralization of the right fovea ethmoidalis and
cribiform plate; MRI then demonstrated an enhancing
lesion in this region extending intracranially as well
as multiple nodularities of his anterior skull base and
along cranial nerves III, V, VIII, IV and X. CSF fluid
analysis was without diagnostic results.
He was thus taken to the operating room for
endoscopy and biopsy of his right olfactory cleft
region which was notable for polypoid edema. Final
pathology returned as mucinous adenocarcinoma
with signet ring features concerning for metastatic
spread of a gastrointestinal primary malignancy.
Subsequent imaging with PET CT revealed moderate
update in the sigmoid colon. Given the
leptomeningeal spread of the metastatic lesion, the
patient underwent whole brain palliative radiation
with plan for subsequent systemic chemotherapy
pending further workup findings of the GI primary.
Conclusions:
This case demonstrates a metastatic skull base
lesion presenting with an unusual symptom of
bilateral hearing loss requiring endoscopic biopsy for
diagnosis.
Poster #062
Mutational landscape and predictors of survival
in sinonasal undifferentiated carcinoma
Brandon Lehrich, BS
Arash Abiri, MS
Theodore Nguyen, BS
Edward Kuan, MD, FARS
Background:
Sinonasal undifferentiated carcinoma (SNUC) is a
rare primary neuroendocrine tumor of the nasal
cavity and paranasal sinuses with limited data
available on the mutational landscape and genetic
drivers of disease.
Methods:
We interrogated the publicly available American
Association for Cancer Research (AACR) Genomics
Evidence Neoplasia Information Exchange (GENIE)
database (v13.0-public) which is a cancer registry
collecting de-identified clinic-genomic data across 19
cancer centers. Kaplan-Meier log-rank test was used
to evaluate differences in overall survival (OS).
Results:
Of the 2,200 head and neck cancer patients, 25
(1.1%) had SNUC. The average age of the cohort
was 52.4 +/- 17.9 years. The average tumor
mutational burden (TMB) was 6.7 +/- 3.7. The 1-, 2-,
and 5-year OS rates were 67.3%, 35%, and 29.1%,
respectively. The most commonly mutated genes
were TP53 (n=10; 40%), IDH2 (n=8; 32%), ARID2
(n=4; 16%), and PIK3CA (n=3; 12%). Only 1 (4%)
patient had a mutation in SMARCA2, and 1 (4%)
patient had a mutation in SMARCB1. Of the 8
patients with IDH2 mutations, 6 (75%) had R172S
mutation, 1 (12.5%) had R172T, and 1 (12.5%) had
R172M mutation. There were no differences in OS
for TP53 mutated vs wild-type (p=0.34) and ARID2
mutated vs wild-type (p=0.22) patients; however,
there was a trend towards increased OS in IDH2
mutated vs wild-type (p=0.056) patients. There was
improved OS for patients with high vs low TMB
(p=0.0019).
Conclusions:
SNUC diagnosis and classification of disease
remains challenging, but high mutational burden may
impact survival through higher likelihood of
actionable mutations.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
90
Poster #063
Nasal septal perforation endoscopy score
correlates with symptom burden in patients with
nasal septal perforations
Amar Miglani, MD
India Rangel
Cody Smith, MD
Bansberg Stephen, Consultant
Michael Marino, MD, FARS
Mayo Clinic Hospital, Phoenix, AZ
Background:
Nasal septal perforations (NSP) are a heterogenous
group of disorders that may present with varying
degrees of inflammatory changes observed during
endoscopic examination. Recently, a validated NSP
endoscopic scoring system was developed
demonstrating fair-to moderate interrater agreement
and substantial intrarater agreement. The objective of
this study was to determine correlation of NSP
endoscopy scores with patient reported symptoms.
Methods:
Video nasal endoscopy recordings were obtained for
patients with NSP. Nasal endoscopies were
independently reviewed using previously validated NSP
endoscopy scoring system for the following physical
exam findings: edema, crusting, scarring, granulation
tissue, and septal deviation. Scoring for each exam
finding was reported on a 3-point scale. Endoscopy
scores were correlated with the NOSE-perf scores – a
validated patient reported outcome measure assessing
NSP symptom burden.
Results:
Video nasal endoscopies for 33 patients with NSP were
reviewed. The mean (+ SD) NOSE-perf score and
mean (+ SD) NSP endoscopy score were 20.5 (+ 9.1)
and 5.6 (+ 2.7), respectively. The NSP endoscopy
scores were moderately correlated with NOSE-perf
scores (r=0.44)(p=0.008).
Conclusion:
NSP endoscopy score is a validated endoscopic
scoring system to assess NSP inflammatory changes.
NSP endoscopy correlates moderately well with patient
reported symptoms. The NOSE-perf score and NSP
endoscopy score may be useful tools for standardized
assessment of NSP outcomes.
Poster #064
New techniques of reducing intraoperative bleeding
in endoscopic sinus surgery for eosinophilic
chronic rhinosinusitis cases with asthma
Yoichiro Narikawa, MD
Yasuyuki Hinohira, Professor
Naruo Shoji
Takatoshi Tokudome
Sei Kobayashi, Associate Professor
Introduction:
Eosinophilic chronic rhinosinusitis (eCRS) is known as
refractory sinusitis with nasal polyps showing
remarkable eosinophil infiltration. Nasal polyps
frequently recur in eCRS cases with bronchial asthma
even if endoscopic sinus surgery (ESS) was performed
on. eCRS cases with asthma are classified into severe
type by Japanese epidemiological study. Intraoperative
bleeding disturbing surgical field is a significant factor
to cause recurrence in surgical treatment of eCRS. Our
new techniques of reducing intraoperative bleeding in
ESS are shown, and the outcome is compared with
previous method.
Cases & methods:
ESS was performed on 39 eCRS cases with asthma,
under general anesthesia and image-guided system.
Prior to ESS procedure, 1% lidocaine with 1: 100000
epinephrine was injected around sphenopalatine artery
(SPA) and Ager nasi. In 20 cases (new group),
hydrophilic urethane sponge (HUS) dipped in 0.1%
epinephrine was put on the region injected for 3 to 5
minutes. After removing HUS, the contracted blood
vessels in the mucosa were cauterized. SPA was also
cauterized after dissected and identified. HUS was
used for reducing bleeding instead of tampon gauzes
on demand during surgery. In the remaining 19 cases
(previous group), only regional injection and tampon
gauze hemostasis were done during surgery.
Outcomes and conclusion:
No complication was found during and after surgery in
all cases. Intraoperative bleeding was statistically
reduced in the new group from 194.8 to 97.5 ml,
compared with the previous group. Our new
techniques of reducing intraoperative bleeding in ESS
for severe ECR cases is considered as acceptable.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
91
Poster #065
WITHDRAWN
Poster #066
Novel use of urinalysis dipsticks for
differentiating patients with diverse sinusitis
complaints
Michela Borrelli, BA
Martin Hopp, MD, PhD
Sarah Ustrell
Jonathin Raskin
Tasha Nasrollahi
Cedars Sinai Medical Center
Introduction:
Various clinical diagnoses present themselves to
ENT clinics with nonspecific “sinus” symptoms that
require an in-depth history and physical exam for
proper diagnosis. To make an accurate diagnosis,
most physicians use costly diagnostic testing such as
nasal endoscopy and computed tomography to
differentiate between various clinical diagnoses. The
objective of our study was to determine if using a
urine dipstick provides a cost-effective tool that could
help differentiate between the multitude of “sinus”
disorders in otolaryngology clinics.
Methods:
Patients presenting with “sinus” complaints were
prospectively enrolled in this IRB-approved study
with a goal of 100 patients in total. Nasal mucus was
sampled using a nasal culture swab from each
patient that presented to the otolaryngology clinic.
These cultured swabs were subsequently placed on
a urinalysis dipstick to assess for leukocytes, nitrites,
protein, and pH. Results were converted to a
numerical score. Lund-Kennedy nasal endoscopy
scores and Lund-McKay CT scores were
documented when available. The final clinical
diagnoses were recorded after the standard testing
was completed.
Results:
Significant findings include reporting that ARS vs.
normal using the whole dipstick score was
significant. ARS vs. normal using the leukocyte value
was close to significant with a p-value = 0.055.
Further stat analysis may be valuable if a higher
dipstick score correlates to a higher Lund-McKay
score for all comers.
Conclusions:
Urinalysis dipsticks may be an incredibly valuable
and cost-effective tool not only in the otolaryngology
specialty but in many other specialties as well.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
92
Poster #067
Olfaction and neurocognition after COVID-19: A
scoping review
Brandon Vilarello, BA
Patricia Jacobson, Medical Student
Jeremy Tervo, Medical Student
Nicholas Waring, Medical Student
David Gudis, MD, FARS
Terry Goldberg, Professor
D. P. Devanand, Professor
Jonathan Overdevest, MD
Columbia University Vagelos College of Physicians
and Surgeons
Introduction:
COVID-19 can include symptoms reflective of acute
and chronic neurological changes. Prior research
has identified that chemosensory changes,
particularly olfactory loss, may reflect greater, central
neurological dysfunction in neurodegenerative
diseases like Alzheimer’s. This review examines
current literature to look at the relationship between
neurocognition and olfaction in otherwise healthy,
young to middle-aged adults following COVID-19.
Methods:
A systematic literature search of PubMed, Ovid
Embase, Web of Science, and Cochrane Library was
conducted with bibliographic review, per PRISMA-
ScR guidelines. Published studies underwent title/
abstract and full-text screening to identify those
evaluating the coincident outcomes of cognition and
olfactory deficits.
Results:
Seventeen studies were eligible for data extraction
after the review process. Eleven studies found
statistically significant poorer cognition in those
suffering from olfactory dysfunction. Three studies
showed no association, and one study reported
lower anosmia prevalence in patients with cognitive
impairment.
Conclusion:
To date, the majority of studies suggest that olfactory
dysfunction is associated with poorer cognition.
Higher level of evidence studies are needed to
further elucidate the relationship between olfaction
and cognition following COVID-19 illness.
Poster #068
Open access artificial intelligence and rhinology
patient education
Alice Huang, MD
Michael Chang, MD
Jayakar Nayak, MD, PhD
Peter Hwang, MD, FARS
Zara Patel, MD, FARS
Background:
ChatGPT is a language processing tool launched by
OpenAI, with more than 100 million users as of
January 2023. This powerful artificial intelligence (AI)
tool has unknown accuracy or reliability in medical
settings. This study sought to analyze the accuracy
of ChatGPT-generated responses to common
rhinologic patient questions.
Methods:
Four rhinologists developed consensus a priori on
responses to a list of 10 common questions from
rhinology patients. The questions were posed to
ChatGPT, with responses individually graded by the
surgeons on a scale of 0 to 3: 0=incorrect
information that could lead a patient to miss or
misunderstand a potential diagnosis, or imply a
treatment option that is not correct or possible;
1=incorrect information that would not significantly
change a patient’s understanding, OR correct but
incomplete information; 2=complete and correct
information; 3=correct information beyond the
“expert” response.
Results:
Mean grade for ChatGPT responses was 1.65. For 3
questions, raters agreed that ChatGPT responses
were equal to or better than expert responses. For 6
questions, ChatGPT provided responses that were
incorrect or incomplete based on at least 2
rhinologists’ scores, with 4 rated this way by mean
rater grades. Interclass correlation coefficient (ICC)
was 0.602, indicating only moderate reliability among
raters.
Conclusion:
Open access AI tools will be resources for patients
seeking health information. This preliminary study of
ChatGPT responses to rhinologic questions
demonstrates mixed accuracy and completeness as
well as provision of incorrect information in some
cases. Patient education and further study is needed
to understand the limitations, role, and impact of this
technology.
POSTERS
AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
93
Poster #069
Optimizing strategy for pre-operative sinonasal
irrigation through 3D Printing
Kanghyun Kim, BS
Raymond Wen
Kai Zhao, Associate Professor
The Ohio State University
Background:
While topical sinus irrigation remains a key strategy
in management of sinonasal disease, the variability
in nasal structure among patients often demands an
individualized strategy. We investigate different
permutations of irrigation strategy to optimize
outcomes through 3D printing.
Methods:
Eleven pre-operative models were 3D printed with a
FormLabs Form 3 SLA printer based on individual
CT scans. Irrigations were performed by squeeze
bottle through a silicon putty water tight seal. The
four head positions of 45° to-the-side, 90° to-the-
side, 45° forward and 45° to-the-side and 45°
forward were filmed, with varying fluid entry through
the upper (conventional) or lower (backfill) nostril.
Results:
Due to restrictive ostia, all models showed filling of
the maxillary sinus only. Among the different head
positions, optimal penetration was recorded for 90°
to-the-side backfill (n=6), 90° to-the-side conventional
(n=4), 45° to-the-side backfill (n=2), 45° to-the-side
conventional (n=2), 45° forward and 45° to-the-side
backfill (n=3), and 45° forward (n=1). The average
penetration score for the optimal position across all
models was significantly higher (p<0.05) for all head
position permutations with the exception of 90°
to-the-side backfill, which saw a notable but not
significant increase.
Conclusions:
Nasal anatomy variation among patients is not
conducive to a one-size-fits-all irrigation strategy.
Even though 90° to-the-side backfill showed the
highest average score among the standard positions,
optimal individualized head positions demonstrated a
higher average score. Therefore, 3D printing can
serve as a method to identify an individual optimal
strategy and improve irrigation outcomes.
Poster #070
Oral corticosteroid (OCS) burden and healthcare
resource utilization (HCRU) in patients with
chronic rhinosinusitis with nasal polyps
(CRSwNP) undergoing functional endoscopic
sinonasal surgery (FESS): A US real-world
retrospective cohort study
Stella Lee, MD
Danielle Isaman , Ms.
Asif Khan, Dr.
Anju Peters, MD
Peter Hwang, MD, FARS
Sietze Reitsma, MD
Natalia Petruski-Ivleva, Dr.
Scott Nash, Dr.
Juby Jacob-Nara, Dr.
Sanofi
Background:
The impact of FESS on OCS burden and HCRU for
patients (pts) with CRSwNP is understudied.
Methods:
Retrospective cohort study of adult CRSwNP pts
undergoing vs not undergoing FESS, using US
claims data (Optum; 2011−2021). Pts were
propensity score matched to adjust for confounding.
OCS burden (cumulative dose in mg prednisone
equivalents), other medications, procedures/
diagnostic tests, HCRU, and costs were compared
among FESS vs non FESS pts in the 1 year post
index date. Intervention/follow-up periods were
defined as Day 0−44/45−365, respectively.
Results:
Each group included 8,909 pts. During follow-up,
OCS cumulative dose was 18% lower in FESS vs
non-FESS pts (mean difference in mg prednisone
equivalent dose: −40 mg [95% CI −64 to −16] per
pt). In pts who filled an OCS prescription (34.6%
[FESS] vs 36.0% [non-FESS]), OCS burden
remained high in both groups (mean [SD] cumulative
dose: 521 [786] vs 612 [906] mg). Mean total
healthcare costs in FESS vs non-FESS pts were
$28,832 vs $2,537 per pt during the intervention
period, but similar during follow-up ($15,659 vs
$15,926, respectively). During follow-up, HCRU was
similar between FESS and non-FESS pts, except
that FESS pts had higher odds of visiting an
otolaryngologist (odds ratio [OR] 2.9 [95% CI 2.7,
3.1]). FESS pts had higher odds than non-FESS pts
of polypectomy (OR [95% CI] 5.7 [4.9, 6.7]) and
airway endoscopy (3.6 [3.4, 3.9]) during follow-up.
Overall, 20.7%, 22.5% and 29.2% of all pts filled a
prescription for leukotriene antagonists, NSAIDs, and
oral antibiotics during follow-up, respectively.
Conclusion:
In real-world US practice, pts with CRSwNP who
underwent FESS had similar OCS and HCRU
burden to those who did not, and similar costs during
follow-up.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
94
Poster #071
Paranasal sinus and nasal cavity squamous cell
carcinoma and adenocarcinoma: A SEER
database analysis
Lacy Brame, DO
Spencer Hall, MPH
Daniel Zhao, PhD
Aniruddha Parikh, MD
Kibwei McKinney, MD
Lurdes Queimado, MD, PhD
Oklahoma State Center for Health Sciences
Background:
Paranasal sinus malignancies are rare and make up
3% to 5% of head and neck cancers in the United
States. They are aggressive malignancies with poor
prognosis. Previous studies have reported poorer
survival with advanced age, stage, and other social
factors. In our study, we sought to identify factors
associated with worse survival for squamous cell
carcinoma (SCC) and adenocarcinoma (AC)
specifically.
Methods:
Data was collected from the Surveillance,
Epidemiology, and End Results (SEER) database
from 2000-2019. SCC and AC of the paranasal
sinuses and nasal cavity were included in the study.
Variables such as gender, age, marital status,
income, race, and stage were collected. Kaplan-
Meier curves were generated and log-rank tests
were performed to analyze variables associated with
survival.
Results:
A total of 5,810 individuals with SCC and 84
individuals with AC of the nasal cavity and paranasal
sinuses were identified. Sixty-six percent of patients
were male and 87% were older than 50 years.
Median overall survival was 53 and 133 months for
SCC and AC patients, respectively. Among SCC,
survival was significantly different by age (p
<0.0001), race (p <0.0001), marital status (p
<0.0001), and stage (p <0.0001). No significant
differences in survival were identified by income or
gender.
Conclusions:
Consistent with the literature, overall survival was
higher for AC than for SCC patients. Of importance,
this analysis demonstrated that several individual
factors such as age, race, marital status, and stage
impact survival. Understanding the factors
associated with poor survival from these tumors will
aid in guiding treatment and understanding
disparities that exist among this patient population.
Poster #072
Perioperative strategies for improving quality of
life and sinonasal morbidity after endoscopic
skull base surgery: A systematic review
Satyan Sreenath, MD
Walter Fitschen, Medical Student
Elisa Illing, MD, FARS
Vijay Ramakrishnan, MD, FARS
Jonathon Ting, MD, FARS
Indiana University School of Medicine
Background:
Though the endonasal corridor in endoscopic skull
base surgery (ESBS) avoids invasive approaches,
significant postoperative morbidity exists. Several
studies have explored surgical techniques, nasal
dressings, and perioperative management for
optimizing quality of life (QOL) following ESBS. This
systematic review provides a global understanding of
strategies for optimizing sinonasal healing and
morbidity following ESBS.
Methods:
Using PRISMA guidelines, PubMed, Ovid, and
Cochrane databases were searched for articles
reporting QOL measures and/or endoscopic grading
of sinonasal healing after ESBS. Articles were
stratified based on intervention including operative
technique, donor site grafting after nasoseptal flap
(NSF) harvest, nasal dressings, and use of topical
irrigations.
Results:
27 studies comprising 1775 patients were included.
QOL measures included the ASK-12, SNOT-22, and
olfactory testing. Endoscopic grading of healing was
scored on Likert and visual analog scales.
Modifications to the EEA with preservation of
sinonasal structures decreased morbidity with
improved QOL. Reconstructive techniques and
grafting of the NSF donor site improved
mucosalization rates and decreased crusting. Few
studies exist on the impacts of nasal dressings and
nasal irrigation on healing and QOL.
Conclusions:
This systematic review provides a landscape of
current techniques for improving QOL and morbidity
after ESBS. Modifications to the EEA and grafting
approaches allow for preservation of sinonasal
structures with the intent of decreasing crusting and
preserving mucociliary function. Further study is
required to understand the impact of intranasal
dressings and nasal irrigations on postoperative QOL
following ESBS.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
95
Poster #073
Predictors of headache/facial pain associated
with cryotherapy ablation of the posterior nasal
nerve for the treatment of chronic rhinitia
Samuel Razmi, BS
Daniel Gorelik, Research Fellow
Yuki Yoshiyasum, Resident
Masayoshi Takashima, MD, FARS
Omar Ahmed, MD, FARS
Texas A&M School of Medicine
Cryotherapy ablation of the posterior nasal nerve is
an effective treatment for patients with chronic rhinitis
but is associated with postoperative headache/facial
pain in some patients. The purpose of this study is to
understand factors that may be associated with this
complication.
Patients who underwent cryotherapy ablation at a
single institution from January 2021 to January 2023
were included. Demographics and information
regarding clinical characteristics were collected and
reviewed. Mann-Whitney U and Chi-square tests
were used to assess significance in quantitative and
categorical data, respectively (alpha = 0.05).
29 patients underwent cryotherapy ablation. None of
these patients received preoperative pain
medication. Thirteen (44.8%) patients reported
having a severe headache/facial pain occurring
immediately after the procedure, with a mean
duration of 57.1 minutes (SD=50.5). The average
age of patients experiencing this adverse event was
53.4 years (SD=21.5) which was significantly lower
(p=0.03) than patients who did not experience
headache/facial pain (69.9 years, SD=9.4).
Headaches/facial pain occurred most in Caucasians
(84.6%) and females (65.1%), but neither association
was statistically significant (p>0.05). There was no
association of previous medication use or sinus
surgery, nor smoking status with headaches/facial
pain.
Postoperative headaches/facial pain are more
common in our cohort compared to previously
reported rates in the literature. In our sample,
younger age appears to play a significant role in
likelihood of headache/facial pain. Physicians should
consider this factor when counseling patients, though
larger studies are needed to confirm these findings.
Poster #074
Predictors of surgical intervention in children
with complicated orbital cellulitis
Erica McArdle, MD
John Behnke, Resident
Amani Kais, Post Graduate Research Fellow
Chadi Makary, MD, FARS
Hassan Ramadan, MD, FARS
West Virginia University
Background:
Orbital cellulitis in children, while rare, can lead to
serious complications, sometimes requiring surgical
intervention.
Objective:
To evaluate specific variables at presentation that
can predict when surgical intervention will be
required for pediatric orbital cellulitis.
Methods:
Retrospective case-control study of children referred
to West Virginia University children’s hospital from
January 2012 to July 2022 was performed. Children
who were diagnosed with preseptal cellulitis, orbital
cellulitis, and orbital abscess were included.
Diagnosis was based on clinical presenting
symptoms, physical exam findings and CT imaging.
Patients’ characteristics, CT imaging, inflammatory
markers and associated acute bacterial rhinosinusitis
were reviewed. Orbital cellulitis secondary to trauma,
tumor, cutaneous infection were excluded.
Results:
118 children were identified. Mean age was 7.3 years
and 65 (58.1%) were males. Mean Lund-McKay (LM)
CT score was 5.3. 53 (44.9%) children had orbital
cellulitis/abscess with the remaining having pre-
septal cellulitis. 18 (15.3%) children required surgery;
17 (94.4%) were for orbital abscess and 1 (5.6%) for
pre-septal cellulitis (p<0.0001). Univariate analysis
showed a high CRP, large abscess volume, female
gender, high LM CT score, older age were predictors
of surgery. Multivariate logistic regression analysis
showed age older than 10 years, LM CT score
higher than 5, female gender, large abscess volume
were predictors of surgery.
Discussion:
Females older than 10 years, large abscess, high LM
CT score had higher rates of surgery for complicated
orbital cellulitis. This may be valuable for clinical
decision making in attempt to provide timely care
and reduce length of stay.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
96
Poster #075
Proof of concept: How to use Zoom to set up a
remote telementoring experience for teaching
endoscopic sinus surgery
Angela Yang
Rachel Daum
Michael Yong, Dr.
Michael Chang, Dr.
Peter Hwang, MD, FARS
Background:
Remote surgical training remains an unmet need in
the field of rhinology. This is especially valuable for
learners who are geographically distant from highly-
skilled instructors. Our study aimed to validate a
telementoring model for endoscopic sinus surgery
(ESS), and develop an accurate description of the
technical setup.
Methods:
Surgical trainees at Stanford University (SU)
underwent live-virtual teaching sessions of ESS
taught by a remote mentor. An endoscopic view of
the surgery was live-streamed through Zoom, a
secure cloud-based video platform. Interviews were
conducted and surveys were administered to
trainees and mentors after each session.
Results:
2 post-graduate senior surgical resident trainees and
2 remote mentors were included, and a total of 4
live-virtual sessions were conducted. Surgical trainee
and mentor satisfaction for the in-progress model
were moderate. Participants indicated that the
experience approximated in-person mentorship
moderately well, with all participants indicating that
they would use the system again for remote
mentoring. Highlights from interviews included the
good audio quality and the ability for remote 2-way
feedback through both still-image capture and
telestration. Live annotation was noted to be better
than still-image capture, and occasionally better than
in-person verbal guidance. Areas for improvement
included ergonomics of screen placement, video lag,
and video resolution.
Conclusion:
ESS lends itself well to live-telementoring, with the
operative field being projected remotely through a
high-definition endoscope with 2-way audio and
video feedback. Establishment of a reliable
telementoring model will aid future surgical training
as the set-up improves over time.
Poster #076
Purasinus, a novel self-assembling peptide, in a
draf-III frontal sinusotomy
Kaitlynne Pak, MD
Arthur Wu, MD, FARS
Dennis Tang, MD, FARS
Cedars Sinai Medical Center
Introduction:
Stenosis and adhesions are known complications in
a Draf-III frontal sinusotomy. Various techniques
have been proposed to maintain patency but no
technique has been proven as more superior.
RADA16 hydrogel is a self-assembling synthetic
peptide shown to promote wound healing and
prevent adhesion formation. RADA16 has been
studied in animal models, which shows wound
healing and tissue regeneration properties through
creation of an extracellular matrix; however, there’s a
paucity of described application in patients.
Presently, there are no reports of RADA16 use in a
Draf-III frontal sinusotomy. We report two successful
cases of a patient with history of chronic
rhinosinusitis who underwent sinus surgeries with
Draf-III frontal sinusotomies.
Cases:
A 59F with aspirin-exacerbated respiratory disease
presented with recurrent polyps. A revision sinus
surgery was performed with a Draf-III using RADA16
and a steroid eluting stent in the Draf-III cavity. At 3
week postop, there was no exposed bone and the
cavity remained widely open with minimal
debridement. Cavity was patent at 2 months postop.
A 62M with recurrent nasal polyps with prior sinus
surgery presented with recurrent polyps. He
underwent a Draf-III and RADA16 and silastic stents
were placed. The silastic stent was removed at 2
weeks postop. No exposed bone was seen and the
cavity remained widely open. At 5 months, the cavity
remained open, but polyps had recurred and were
managed with biologic injections.
Conclusion:
We present the first described cases of using
RADA16 after a Draf-III in combination with both
dissolvable and nondissolvable stents. This
technique can help in accelerating mucosalization of
denuded bone during sinus surgery.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
97
Poster #077
Radiographic enhancement of the longus colli
muscle in skull base osteomyelitis
Grant Owen, BA
Peter Filip, MD
Alana Ravasio, Medical Student
Jamie Masliah, Resident
Peter Papagiannopoulos, MD
Bobby Tajudeen, MD, FARS
Rush Medical College, Rush University Medical
Center
Introduction:
Several radiographic findings have been reported in
skull base osteomyelitis (SBO). However, the role of
longus colli muscle enhancement has not been
reported. This study aimed to determine the
frequency of longus colli muscle enhancement on
imaging in SBO.
Methods:
A retrospective institutional chart review examined
patients with SBO between January 2017 and
February 2023. Along with demographic information,
computerized tomography (CT) and magnetic
resonance imaging (MRI) reports were reviewed for
infection location (rhinologic origin, otologic origin,
other origin) and longus colli enhancement. Scans
reporting enhancement of the longus colli,
prevertebral musculature, or prevertebral space were
considered positive. Fisher’s exact test was used to
compare rates of enhancement by infection location.
Results:
22 patients with confirmed SBO were included,
average age was 69.1 years (range 23-89 years).
Otologic origin was the most common site of
infection (n=9, 40.9%), followed by rhinologic (n=8,
36.4%) and other origin (n=5, 22.7%). Longus colli
enhancement was observed in 11 patients (50.0%),
with most being rhinologic origin (n=8) followed by
otologic (n=2) and other origin (n=1). The rate of
longus colli enhancement was significantly higher in
rhinologic origin compared to otologic and other
origins (100.0% vs 22.2% vs 20.0%, p=0.001). CT
was positive in 4 of 9 cases, while MRI was positive
in 9 of 11 cases.
Conclusion:
This case series suggests a potential link between
longus colli muscle enhancement on radiographic
imaging and SBO, particularly in cases of rhinologic
origin. Further research is needed to determine
biostatistical significance and overall clinical utility of
this finding.
Poster #078
Rare case of a giant disfiguring frontal sinus
mucocele causing globe subluxation
Caroline Christmann, MD
James Eng, Dr.
Sunthosh Sivam, Dr.
Baylor College of Medicine
Background:
Mucoceles are expansile lesions of the paranasal
sinuses that may cause compression and remodeling
of surrounding structures. Giant mucoceles are rare
but may cause vision impairment, erosion of the
anterior and posterior tables, and disfigurement.
Learning Objectives:
Understand the natural history of mucoceles, discuss
multidisciplinary approaches to repair, and identify
open approaches that best preserve future cosmesis.
Methods:
The case of a 28-year-old male with a frontal sinus
mucocele was reviewed. A literature review was
performed to find similar cases of frontal mucoceles
with orbital complications.
Results:
The patient presented with a 7-year history of an
enlarging forehead mass causing compression of the
nasal bones and subluxation of the right globe with
exposure keratopathy, microbial keratitis, and corneal
perforation. CT scan revealed a 15.8x11.8x10.0cm
frontal mucocele with foci of posterior table erosion
and an eggshell remnant of the anterior table. The
patient underwent emergent open resection,
including frontal sinus obliteration and reconstruction
with titanium mesh by Facial Plastics and
Reconstructive Surgery. Neurosurgery assisted with
posterior table repair, and Oculoplastic Surgery
performed a temporary tarsorrhaphy.
Conclusion:
Giant frontal sinus mucoceles are rare, with only one
other case report of a frontal mucocele causing
globe subluxation. Multidisciplinary management in
an open approach to the frontal sinuses was critical
in providing a safe outcome and creating the
foundation for a cosmetic result in subsequent
stages.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
98
Poster #079
Readability and quality analysis of patient
education materials in aspirin exacerbated
respiratory disease
Kush Panara, MD
Daniel Lee, Fellow Physician
Elysia Grose
Jenelle Safadi
Jennifer Douglas, Fellow Physician
Michael Kohanski, MD, PhD
James Palmer, MD, FARS
John Lee, MD
Nithin Adappa, MD, FARS
John Bosso, MD
Background:
Aspirin exacerbated respiratory disease (AERD) is a
complex disease that requires patients to strictly
adhere to treatment regimens for successful
outcomes. Therefore, patient education is integral in
the successful management of AERD. We aim to
evaluate the readability and quality of online patient
education material (PEMs) on AERD.
Methods:
An online search for PEMs on AERD was conducted.
PEMs were categorized based on origin from either
academic medical institutions/hospitals or
government, private, or professional organizations.
Readability was evaluated with the Flesch-Kincaid
Grade level (FKGL), Flesch Reading Ease (FRE),
Coleman Liau Index (CLI), and SMOG Index. The
DISCERN tool with two raters was used to calculate
quality. Summary statistics were calculated and
unpaired two-tailed t-tests was used to evaluate
continuous variables.
Results:
Out of 99 initial results, a total of 34 PEMs were
included after excluding non-education materials.
The average FRE score was 39.6 equivalent to a
“difficult” interpretation. The average grade level of
the PEMs was above the twelfth grade with FKGL,
CLI and SMOG index. Most of the studies (26/34,
76.4%) had DISCERN scores indicative of good or
excellent quality. There were no significant
differences between PEMs originating from medical
institutions and PEMs originating from other sources
in terms of quality or readability.
Conclusion:
PEMs on AERD are good or excellent quality.
However, the interpretation of the educational
material may be difficult to comprehend for an
average individual. We highlight the need for quality
improvement and optimization of readability of
PEMs.
Poster #080
Real-world effectiveness of Mepolizumab on
upper and lower airway diseases
Jonathan Bernstein, Dr.
Elizabeth Packnett, Ms.
Carolyn Lew, Dr.
Yvonne Robles, Ms.
Arjita Deb, Dr.
University of Cincinnati
Background:
Asthma and nasal polyps (NP) frequently co-occur,
share similar pathophysiology, and incur
considerable airway disease burden, including OCS
exposure. In this study we evaluated the
effectiveness of mepolizumab in a real-world
population of patients with comorbid asthma and NP.
Methods:
MarketScan Commercial and Medicare Databases
were used to study 189 patients with comorbid
asthma and NP who initiated mepolizumab between
November 2015 and September 2020, ≥18 years of
age at mepolizumab initiation (index date), and 12
months continuous enrollment before and after the
index date. NP and asthma outcomes, adherence
and persistence following mepolizumab initiation,
were compared in the 1-year baseline and variable
follow-up period with a post-hoc analysis comparing
outcomes in the first year of follow-up to the 1-year
baseline.
Results:
On mepolizumab, patients experienced fewer
asthma-related exacerbations compared to baseline
(first year of follow-up: 54.7% relative reduction,
p<.001; variable follow-up: 61.6% relative reduction,
p<.001). Sinus surgeries per patient per year (PPPY)
decreased by 14.7% in the first year of follow-up and
by 51.6% during the variable follow-up (p<.001) from
baseline. The OCS mean daily-dose decreased by
76.9% in the first year of follow-up and by 81.1%
during the variable follow-up (p<.001). OCS bursts
PPPY decreased by 58.8% in the first year of follow-
up and by 61.7% during the variable follow-up
(p<0.001). Nearly ¾ of patients were persistent
(74.1%) and 67.2% were adherent to mepolizumab
in the first year following initiation.
Conclusion:
Mepolizumab treatment in comorbid patients
correlated with clinically impactful outcomes for
upper and lower airway disease.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
99
Poster #081
Reconstruction of sellar defects with laterally-
pedicled native sphenoid sinus mucosa
Samuel Floren, MD
Merica Xiong
Timothy McCulloch
Azam Ahmed
Ian Koszewski, MD, FARS
University of Wisconsin
Background:
While purely endoscopic endonasal approaches to
the sella turcica have emerged as a favorable option
for resection of most pituitary tumors, optimal
reconstruction after transsphenoidal pituitary surgery
remains poorly established. Goals of reconstruction
include avoiding complications such as postoperative
CSF leak, minimizing short- and long-term morbidity,
and optimizing sinonasal functional outcomes. Here
we describe a single-institution experience of a novel
reconstructive technique using laterally-pedicled
native sphenoid mucosal flaps.
Methods:
A retrospective single armed chart review was
performed of all patients who underwent primary
transsphenoidal pituitary resection with
reconstruction using the described pedicled septal
mucosal flaps between the dates of 01/01/2018 and
02/02/2023.
Results:
44 patients underwent the above-described
reconstruction with an average age of 53 (range:
25-77) and an average tumor size of 2.0 cm (range:
0.4-4.5cm). No patients developed postoperative
CSF leak. There was one complication of
postoperative pneumocephalus after aggressive
nasal blowing. 9 patients (20%) used topical
corticosteroids in the postoperative setting,
compared to 6 patients (14%) pre-operatively. For
patients who completed a postoperative Sino-Nasal
Outcome Test-22, the average score 2 months
postoperatively was 18.
Conclusions:
In appropriately selected patients, the use of
laterally-pedicled native sphenoid mucosal flaps is a
safe, effective, and intuitive reconstructive adjunct for
small to medium sized sellar lesions.
Poster #082
Referral patterns: Number of providers and
duration of loss before definitive intervention for
olfactory disorders
Bruna Castro, MD
David Grimm, BS
Lei Shi
Farideh Hosseinzadeh, MD
Zara Patel, MD, FARS
Stanford University School of Medicine
Background:
Patients with olfactory disorders (OD) often first
present to primary or urgent care settings. However,
knowledge about recommended treatment options in
this setting may vary. This study sought to evaluate
the referral pattern and management of patients with
OD before being seen by a smell expert.
Methods:
Retrospective cohort study in a tertiary care center.
Adult patients seen between 2016-2022 with
anosmia, hyposmia, parosmia or phantosmia with a
documented psychophysical smell test were
identified by diagnosis codes. Demographic and
other patient factors, well as etiology, treatment
options tried at each provider, and University of
Pennsylvania Smell Identification (UPSIT) scores
were collected.
Results:
A total of 100 patients were included, with 53 female,
47 male and 1 unknown gender. The mean age was
57 years old (range: 24-90). UPSIT mean score was
19.58 (range: 4-39). Post viral infection was the
principal cause of smell loss corresponding to 43%,
idiopathic 34%, head trauma 8%, post-surgery 6%,
CRS 5%, chemical exposure 2%, and
neurodegenerative disease 1%. The mean total
number of providers seen prior to seeing a smell
expert was two. The average time of smell loss until
the first provider visit was 31 months (range 1 - 480
months). The average time from first provider visit to
visit with a smell expert was an additional 9.8 months
(range 1-120 months). As most patients were not
started on a definitive treatment option for smell loss
until seeing a smell expert, this equalled an average
of 3.4 years before definitive intervention.
Conclusion:
Knowledge of treatment options for smell loss is
lacking amongst primary and urgent care providers
and the timeline to see a smell expert remains too
long.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
100
Poster #083
WITHDRAWN
Poster #084
Report of a novel reconstruction method using
sternocleidomastoid flap and nasoseptal flap for
nasopharyngeal tumors after
nasopharyngectomy
Bita Naimi, BA
Alexander Duffy, MD
Jay Trivedi
Emily Garvey, BA
Chase Kahn, MD
Marc Rosen, MD, FARS
Elina Toskala, MD, MBA, PhD, FARS
Mindy Rabinowitz, MD, FARS
James Evans, MD
Gurston Nyquist, MD, FARS
Adam Luginbuhl, MD
Thomas Jefferson University Hospital
Introduction:
The sternocleidomastoid (SCM) flap has been widely
utilized in head and neck reconstruction. We
describe two cases utilizing a novel reconstruction
method after expanded endonasal and transcervical
resections of nasopharyngeal (NP) tumors using a
combined pedicled SCM flap with a nasoseptal flap
(NSF) onlay.
Technique:
Combined endoscopic, endonasal and transcervical
approach to NP tumors allows for expanded
resection and proximal control of the internal carotid
artery. Adjuvant therapy including cesium seeds may
be placed. SCM flap is superiorly pedicled and
rotated into the defect to provide bulk and coverage
of neurovascular structures. NSF is raised and laid
endonasally along the lateral pharyngeal defect.
Cases:
1: A 39-year-old male with a history of EBV+
nasopharyngeal carcinoma presented two years after
chemoradiation with rT1N0 EBV+ disease. He
underwent a combined endonasal and transcervical
approach to a right nasopharyngectomy with cesium
seed brachytherapy placement and closure with a
right SCM flap and left NSF. There were no
complications or fistula at 5-months follow-up.
2: A 77-year-old female with T2N1 nasopharyngeal
adenoid cystic carcinoma underwent a combined
approach to left nasopharyngectomy, left neck
dissection, right NSF, and left pedicled SCM flap.
The flap remained patent with no evidence of fistula
at follow-up and through adjuvant radiation.
Conclusion:
We describe the novel use of the SCM-NSF
combination for reconstruction of lateral pharyngeal
defects after nasopharyngectomy. A pedicled SCM
flap with NSF onlay can limit scarring, prevent
infection and fistula formation, and protect critical
neurovascular structures through adjuvant treatment
for primary and recurrent NP tumors.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
101
Poster #085
WITHDRAWN
Poster #086
Restarting antithrombotic drugs following
functional endoscopic sinus surgery: A scoping
review
Trinithas Boyi, MA
Rhys Richmond, BS
R. Peter Manes, MD, FARS
Ryan Rimmer, MD, FARS
Yale School of Medicine
Background:
Anticoagulant and antiplatelet agents are routinely
discontinued preoperatively to reduce the risk of
hemorrhage. There are no clear guidelines on when
to resume these agents in otolaryngologic patients
following functional endoscopic sinus surgery
(FESS). Our goal was to identify and systematically
review existing literature related to this topic.
Methods:
We systematically queried PubMed, Embase, Ovid,
Web of Science, Cochrane, and CINAHL databases,
following the Preferred Reporting Items for
Systematic Reviews and Meta-Analyses (PRISMA)
guidelines, to identify publications reporting
antithrombotic use in endoscopic sinus surgery. The
primary outcomes were recommendations on the
timing of resuming antithrombotic use.
Results:
We identified 104 unique articles, which underwent
independent title and abstract review by two
reviewers, with 20 undergoing full-text review and 7
meeting eligibility for analysis. Only 3 publications
were case-control studies, 1 was a cohort study, and
3 were literature reviews. All publications discussed
when to stop antithrombotic agents; however, only 3
articles discussed when to restart agents, with mixed
recommendations.
Conclusions:
A paucity of literature exists related to resuming
anticoagulant or antiplatelet agents following
functional endoscopic sinus surgery. Additional
research is needed to establish consensus
guidelines.
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
102
Poster #087
Role of allergic rhinitis in recurrent acute
rhinosinusitis
John Behnke, MD
Zayd Al-Asadi, BS
Dominic Lombardo, BS
Hassan Ramadan, MD, FARS
Chadi Makary, MD, FARS
West Virginia University
Background:
While recurrent acute rhinosinusitis (RARS) is a
relatively common diagnosis with significant
healthcare burden, few reports have evaluated its
association with other comorbidities.
Goal: To evaluate the association between allergic
rhinitis (AR) and RARS.
Methods:
A retrospective case-control study was conducted
using patients presenting to the West Virginia
University rhinology clinic from August 2020 to
October 2022. Cases included patients diagnosed
with RARS, and controls were patients diagnosed
with headache and/or facial pain syndrome. Patients’
characteristics and comorbidities were reviewed.
RARS was diagnosed based on the International
Consensus Statement on Allergy and Rhinology
criteria of four or more independent episodes of
acute rhinosinusitis per year with at least one
episode documented by objective findings, and
complete resolution of the infection between
episodes. Patients with concomitant chronic
rhinosinusitis (CRS) or recurrent exacerbations of
CRS were excluded.
Results:
The study cohort contained 143 patients, 82 patients
with RARS and 61 control patients. Patients with
RARS were older (49 vs 43.5, p=0.05). There was
no difference in gender, smoking history, obstructive
sleep apnea (OSA), or nasal septal deviation
between the RARS patients and controls. AR and
asthma were significantly associated with RARS
(OR=11.1, p<0.0001; OR=2.75, p=0.013
respectively). RARS patients had similar proportions
of seasonal and perennial allergies (21.9%), with
14.1% affected by both.
Conclusion:
Allergic rhinitis is strongly associated with RARS;
therefore, evaluation for AR should be considered
when treating these patients. Future studies with
larger sample sizes are needed to confirm these
results.
Poster #088
Safety of proton beam therapy in patients with
sinonasal carcinoma: A systematic review
Srivatsa Surya Vasudevan, MD, MS
Estephania Candelo, Research Fellow
Alireza Sharifi, Research Fellow
Angela Donaldson, MD, FARS
Mayo Clinic
Introduction:
In sinonasal carcinomas (SNC), treatment with
proton therapy (PT) is noted to provide excellent
local control, especially after gross total resection.
However, depending on dose and duration, PT can
be associated with both acute toxicity (AT) and late
toxicity (LT). We reviewed published studies on PT
toxicity after treatment for SNC.
Methods:
PubMed, Embase, EBSCO, Scopus, Science Direct,
Web of Science, and Cochrane library were
searched for articles discussing PT toxicity in the
SNC population. Full-text screening was performed
to extract data on AT (within 3 months) and LT (more
than 3 months). The data comparing toxicity groups
as well as controls were analyzed using STATA.
Results:
We identified 13 studies that met inclusion criteria.
Pooled data from these studies included 684 patients
who underwent PT for SNC. 272/684 (39.7%)
patients with a mean age of 58.6 (SD ± 8.85)
developed PT-mediated toxicity. 107/684 (15.6%) of
the patients developed AT and 165/684 (24.1%)
developed LT. Among all toxicity patients: dermatitis,
oral mucositis, and facial pain were the most
common toxicities noted in 48.5%, 29.7% and 20.2%
of the patients, respectively. 41.9% of AT and 70.2%
of LT were grade 2 toxicities based on the Common
Terminology Criteria for Adverse Events. There was
no statistically significant difference in the incidence
of AT compared to LT (P=0.345). There appears to
be a correlation between higher grades of AT and
presence of LT (P <0.121).
Conclusion:
More studies are needed to confirm the correlation
between AT and LT as well as risk of developing AT
versus LT. The outcomes of this study can help
physicians infer toxicity in different stages of PT and
educate the patients regarding such occurences.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
103
Poster #089
Severe epistaxis after posterior nasal nerve
ablation requiring surgical intervention: A single
center case series
Yuki Yoshiyasu, MD
Brian Wang, Physician/Surgeon
Daniel Gorelik, Research Fellow
Masayoshi Takashima, MD, FARS
Omar Ahmed, MD, FARS
University of Texas Medical Branch
Background:
Posterior nasal nerve (PNN) ablation is an emerging
treatment option for refractory chronic rhinitis. These
cryoablation (Clarifix) and radiofrequency heat
ablation (Rhinaer, Neuromark) procedures are well-
tolerated and can generally be safely performed in
an office setting under local anesthesia. Given the
novelty of PNN ablation, there is limited literature on
procedure related complications. This objective of
this case series is to report rare but severe epistaxis
requiring surgical intervention following PNN
ablation.
Methods:
Medical records were reviewed for patients who
underwent PNN ablation between August 2018 and
January 2023 at a tertiary care medical center.
Results:
192 patients were included in our case series, of
which 5 patients (2.6%) had significant epistaxis
requiring further intervention. All 5 patients had
in-clinic PNN ablation. Devices used for ablation
were the following: 2 Clarifix, 2 Rhinaer, 1
Neuromark. The complications occurred at mean 22
days (range 18 -24 days) post-operatively. 4 patients
were treated with endoscopic sphenopalatine artery
ligation (3 unilateral, 1 bilateral); 1 patient required
unilateral endoscopic cauterization. No further
epistaxis events were reported after interventions. 4
patients had history of hypertension on
antihypertensives. Only 1 patient was on blood
thinners (ASA 325mg).
Conclusion:
Our experience indicates that PNN ablation can be
associated with major complications such as
significant posterior epistaxis. While overall reported
complication rates are low and most adverse events
are minor complications (headache, dry eye, minor
bleeding not requiring intervention etc.), PNN
ablation should be performed with appropriate
caution.
Poster #090
Severe unilateral refractory epistaxis arising from
the septal branch of the anterior ethmoid artery
Theodore Nguyen, BS
Benjamin Bitner , MD
Jonathan Pang, BA
Li Tang Meller, BS
Katelyn Dilley, BS
Sina Torabi, MD
Arash Abiri, MS
Milind Vasudev, BS
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
The septal branch of the anterior ethmoidal artery
(sbAEA) may manifest as an arterial vascular pedicle
in the superior mid-nasal septum, has become
increasingly linked to severe refractory epistaxis.
Here we describe the presentation, predisposing
factors, treatment, and outcomes of severe refractory
epistaxis originating from the sbAEA.
Methods:
Patients presenting with severe refractory epistaxis
from July 2020 through July 2022 were
retrospectively identified. Those with intraoperative
confirmation of sbAEA-associated epistaxis were
included. Patient demographics, presentation,
imaging and laboratory studies, treatments, and
treatment outcomes were recorded.
Results:
Seven patients (5 males) with unilateral (n=6) and
bilateral (n=1) sbAEA epistaxis were identified. The
mean age was 63.7±4.5 years and mean BMI was
29.4±0.9. The most common comorbidity was
hypertension (n=5), with none having a history of
bleeding disorders. Five patients had undergone
previous treatment attempts without epistaxis
resolution. One patient had previously undergone
SPA ligation and one with contralateral packing
placement prior to hospitalization. Preoperatively,
imaging was unremarkable in all patients and
hemoglobin was 8.86±0.89 g/dL, with 2 patients
requiring one and three units of blood transfusion,
respectively. All patients underwent directed
cauterization with complete resolution of symptoms,
no complications, and uneventful follow-up visits
(8.0±3.5 months).
Conclusions:
sbAEA-associated severe refractory epistaxis may
be challenging to recognize, but is associated with
high treatment success through directed cautery.
Increased awareness of this source of severe
bleeding may increase epistaxis treatment success
POSTERS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
104
Poster #091
Severity of chronic sinonasal symptoms after a
major acute inhalational event: A world trade
center retrospective cohort study
Jerlon Chiu, MD
Hannah Sfreddo
David Lehmann
Sonya Marcus, MD
Stony Brook Medicine
Background:
Chronic air pollution exposure is a known risk factor
for the development of upper airway disease. Less is
known about the effect of acute occupational
exposure. The purpose of this study was to
determine the relationship between intensity of acute
air pollutant exposure and chronic sinonasal
symptoms in World Trade Center (WTC) Health
Program patients.
Methods:
WTC patients who were referred to the
otolaryngology clinic at a tertiary-care medical center
for sinonasal symptoms (2010-2020) and had sinus
imaging available were included in this retrospective
cohort study. Pollutant exposure was categorized as
“low,” “intermediate,” “high,” and “very high,” based
on location and duration of exposure to WTC
pollutants, which is consistent with previous
literature. Lund-Mackay (LMK) and Sinonasal
Outcome Test (SNOT-22) scores were used to
evaluate severity of disease. Statistical analysis was
performed to determine the relationship, if any,
between pollutant exposure and LMK/SNOT-22
scores.
Results:
141 patients were included in this study. Average age
at presentation was 44.7 years (SD 8.6) and was
normally distributed. 13.5% were female. Most
patients had “high” exposure (47.5%). Median LMK
score was 2 (IQR: 0 – 5). Mean SNOT-22 score was
42.8 (n=30). “Very high” exposure was associated
with a higher LMK score than “low” exposure (U =
177, p = 0.016). Number of days worked at WTC-
sites was associated with a higher SNOT-22 score (r
= 0.43, p = 0.019, 95% CI [0.07, 0.69]). All other
results were not significant.
Conclusions:
This study found that there is a significant positive
association between the number of days worked at
WTC-sites and a higher SNOT-22 score.
Poster #092
Sex-based differences in severity of chronic
rhinosinusitis as reported by SNOT-22 scores
Snehitha Talugula
Richard Chiu, Medical Student
Sharmilee Nyenhuis
Kamal Eldeirawi
Victoria Lee, MD, FARS
University of Illinois College of Medicine
Background:
Chronic rhinosinusitis (CRS) is a widely prevalent
condition, however its degree of severity according
to sex requires further study. The literature shows
that sex-based differences exist in the severity of
asthma and allergic airway disease in the population.
These findings point to a potential hormonal cause
for this difference, but there is no study suggesting
the role of sex in CRS. The purpose of this study
was to determine the association of sex and CRS
severity in the United States.
Methods:
This study was conducted on data gathered from
181 participants documented in the NAVIGATE 1 and
NAVIGATE II randomized control trials within the
OPTINOSE database. US participants were
analyzed based on sex controlling for airway related
comorbidities, including history of asthma, race, and
ethnicity. SNOT-22 scores were assessed as a
measure of CRS severity. The association between
sex and SNOT-22 scores were determined using
multiple linear regression.
Results:
There were 81 female and 100 male patients. SNOT-
22 scores were significantly higher in females.
Average reported SNOT-22 scores in females were
53.8 ± 16.5 and 46.8± 18.8 in males. On adjusted
regression, the association of sex and SNOT-22
scores approached but did not reach significance (β:
-4.97; 95% CI: -10.68 - 0.73; p = 0.09).
Conclusions:
On average, females had more severe
manifestations of CRS in comparison to men, with
the adjusted association approaching significance.
Further studies, potentially looking at hormones as a
cause of pathogenesis, are needed to better
elucidate the role of sex in CRS.
POSTERS

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
105
POSTERS
Poster #093
Shared decision making for patients with nasal
polyposis: Needs assessment utilizing social
media and clinical cohorts
Isaac Schmale, MD
Minjoo Jo, Medical Student
Li-Xing Man, MD, FARS
University of Rochester Medical Center
Background:
The management of chronic rhinosinusitis with nasal
polyps (CRSwNP) has become increasingly complex
with no single best treatment option. As such,
CRSwNP treatment involves shared decision making
(SDM). However, little is known regarding patient
treatment and counseling preferences. This study
investigates patient and provider needs relating to
CRSwNP treatment and SDM.
Methods:
We conducted REDCap surveys among CRSwNP
patients from CRSwNP Facebook groups. Surveys
assessed patient understanding, concerns, and
preferences regarding treatment. Additionally,
providers who work with CRSwNP patients at our
institution were surveyed. Responses were
categorized and analyzed for emergent themes.
Results:
44 patients and 6 providers completed surveys.
Physician counseling (21) and the internet (17) were
considered to have the biggest influence on patient
treatment decisions while lack of information was the
top factor that made treatment decisions difficult (24).
The top two patient goals for therapy were nasal/
breathing improvement (49) and improved quality of
life (26). From provider surveys, all six providers
stated that improved delivery of credible treatment
information would help patients and improve SDM.
Conclusion:
Both patients and providers believed that reliable
information and SDM were important for improving
CRSwNP care. Although most patients felt that their
providers supported their decisions, many patients
considered lack of information from physicians as the
number one reason their treatment decision was
difficult. A patient decision aid incorporating accurate
treatment options, costs, and risks/benefits could
help CRSwNP patients and allow for future well-
designed trials looking at SDM outcomes.
Poster #094
Sinonasal renal cell-like adenocarcinoma:
Learnings from a case In pregnancy
Andrew Lee, BS
Ryan Little, MD
Linton Evans, MD
Maggie Mouzourakis, MD
Geisel School of Medicine at Dartmouth
Sinonasal Renal Cell-Like Adenocarcinoma
(SNRCLA) is an extremely rare sinonasal tract
malignancy with a characteristic clear cell histology
reminiscent of clear cell renal cell carcinoma. There
have been at least 16 confirmed cases of SNRCLA.
We report the case of a 42-year-old Ukrainian
refugee female presenting to our clinic at 32 weeks
gestation with a recurrent right nasal cavity mass
measuring 8.1 x 4.1 x 4.4 cm. Associated symptoms
included bilateral nasal obstruction, anosmia,
epistaxis, diplopia and right proptosis. To our
knowledge, this is the first case of SNRCLA in a
pregnant patient. Cesarean section was performed
15 days prior to primary resection. A combined
endoscopic endonasal resection and bifrontal
craniotomy was required to achieve gross total
resection of this vascular tumor with negative
surgical margins. The tumor involved a large portion
of the bilateral nasal septum as well as the cribriform
plate. Anterior cranial fossa reconstruction was
performed using a pericranial flap. Interventional
radiology (IR) performed diagnostic angiography with
embolization of the bilateral sphenopalatine arteries.
There was significant vascular supply from the
bilateral anterior and posterior ethmoid arteries as
well as a large contribution from the right vidian
artery. This unique case underscores the challenges
from the accentuated hypervascularity of SNRCLA
malignancies in setting of unknown contributions
from pregnancy as well as the unclear role of IR
embolization.

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
106
POSTERS
Poster #095
Stop scrolling: A social media quality review of
sinusitis videos on TikTok
Rose Dimitroyannis, BA
David Fenton, Medical Student
Stella Cho, Medical Student
Christopher Roxbury, MD, FARS
Social media has emerged as a way to inform
healthcare decisions. TikTok is a social media
platform that allows users to post short-form videos.
The study aimed to assess the quality of sinusitis-
related videos on TikTok.
A TikTok search was done on 1/29/2023 using
sinusitis-related hashtags: #sinusitis, #sinus,
#sinusinfection. Number of views/shares per day,
poster type (influencer [>10000 followers], lay
individual [<10000 followers], and medical
professional), content categories (medical advice,
marketing, comedy, and lifestyle/acceptability), and
content type (educational vs. factual) were collected.
The Patient Education Materials Assessment Tool for
AudioVisual Material (PEMAT-AV) and Journal of the
American Medical Association (JAMA) Benchmark
Criteria were used to measure understandability,
actionability, and reliability. Descriptive statistics were
performed using Welch’s t-test (α=0.05).
Of the 140 videos analyzed, 54.2% (76) of posters
were influencers and 17.1% (24) were medical
providers. Influencer videos were shared significantly
more than medical providers’ (p<0.05). Medical
advice was the most common influencer (48.6%,
37/76) and medical professional (87.5%, 21/24)
content. Influencer understandability and actionability
scores were significantly lower than medical
providers’ (p<0.05), but there was no significant
difference in reliability. While 63% (48/76) of
influencer videos claimed to be educational, only
37.5% (18/48) of educational influencer videos were
considered factual.
Most influencer-posted TikTok videos on sinusitis,
categorized as medical advice claiming to be
educational, are non-factual. Medical providers must
find ways to address misinformation and disseminate
factual, educational content.
Poster #096
Surgical management of obstructive nasal
polyposis in Cornelia de Lange syndrome
Trisha Ortiz, Medical Student
Michelle Yu
Aaron Pearlman, MD, FARS
Weill Cornell Medicine
Cornelia de Lange syndrome (CdLS) is a rare
genetic developmental disorder identified by distinct
multi-system malformations, including facial
dysmorphism, growth restriction, hirsutism, limb
abnormalities, and intellectual disability. About a third
of patients with CdLS experience recurrent and or
chronic sinus infections, often with nasal polyposis.
This report describes a case of nasal polyposis in an
8-year-old boy with Cornelia de Lange Syndrome.
The patient presented to his pediatric
otolaryngologist with nasal obstruction and snoring.
Exam was notable for bilateral obstructive nasal
lesions, concerning for nasal polyps. His sinonasal
disease was refractory to multiple systemic and
topical therapies. He was referred to a rhinologist for
surgical management. His CT scan was consistent
with the exam findings and showed bilateral nasal
polyposis with pansinus mucosal disease.
He underwent endoscopic sinus surgery and
postoperatively had improved nasal breathing on
follow up. The patient continues to improve
postoperatively on topical steroid therapy.
Given the rarity of the disorder, there is limited
literature discussing the features or management of
sinus disease associated with CdLS. Endoscopic
sinus surgery may be considered in pediatric patients
with CdLS with nasal polyposis refractory to systemic
and topical therapies in order to relieve and manage
nasal obstruction.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
107
POSTERS
Poster #097
Synergistic cytotoxicity of permethrin and N,N-
Diethyl-Meta-Toluamide on sinonasal epithelia
with or without chronic rhinosinusitis
Hong-Ho Yang, BS
Saroj Basak, PhD
Tom Maxim, MD
Daniel Shin, MD, PhD
Christine Wells, PhD
Eri Srivatsan
Jivianne Lee, MD, FARS
Objective:
Permethrin and N,N-Diethyl-Meta-Toluamide (DEET)
have been shown to be cytotoxic to healthy
sinonasal epithelial cells (SNEC). In this study, we
investigate whether their concurrent exposure elicits
synergistic cytotoxicity, and whether this synergy
differs between SNEC with and SNEC without
Chronic Rhinosinusitis (CRS).
Methods:
Ethmoid sinus mucosal specimens were obtained
from 1 non-CRS patient (Tissue A) and 3 CRS
patients (Tissue B, C, D). Specimens were expanded
on culture plates and exposed to 0-5μm Permethrin
and DEET for 7 days. Each experiment was
replicated in triplet and cell viability was recorded
every 2 hours using IncuCyte. Zero interaction
potency score (ZIP) was computed every 12 hours
between 24h and 144h using SynergyFinder.
Results:
When given alone, dose-response cytotoxicity of
Permethrin and DEET was seen up to 2.5μm, and
resistance was seen at 5μm for all tissues. For tissue
A, significant synergy was seen up to 2.5, 1.25μm
(CP, CD) throughout the entire exposure period, with
peak synergy seen at 84h at 1.25, 0.625μm (ZIP
20.2, 95% C.I. 17.1-23.7). For all 3 CRS tissues, no
significant synergy was seen during the first 4 days.
For tissue B, synergy was first seen at 144h at 2.5,
1.25μm (ZIP 4.2, 95% C.I. 1.8-7.3). For tissue C,
synergy was first seen at 108h at 0.625, 0.625μm
(ZIP 12.7, 95% C.I. 2.8-23.8). For tissue D, no
significant synergy was seen at all timepoints.
Conclusion:
This is the first study to investigate the combined
effect of pesticides on SNEC. Results substantiated
the synergistic cytotoxicity of permethrin and DEET
on SNEC. Moreover, CRS tissues appear to be more
resistant to this synergy, as more prolonged
exposure was needed to elicit synergistic cytotoxicity.
Poster #098
The direct impact of the COVID-19 pandemic on
rhinology practice
Sarah Sutton, BS
April Taniguchi
Shaun A. Nguyen, Dr.
Zachary Soler, MD, MSc, FARS
Rodney Schlosser, MD, FARS
Medical University of South Carolina
The coronavirus of 2019 (COVID) pandemic
triggered numerous concerns regarding the risks of
in person clinic visits and endoscopy procedures.
While this has been assessed through survey data,
the direct effect of COVID on a rhinology practice
has not been studied quantitatively. To assess the
impact of COVID and subsequent recovery, a
retrospective chart review (MUSC IRB
Pro00125626), of all patients seen at a tertiary
rhinology clinic during the spring (March through
June) of 2019, 2020, and 2022 was performed. Visit
type (new vs established), location (in person vs
virtual), diagnosis, imaging, treatment plans, and
follow-up visit type were collected. Total COVID
(2020) encounters were 30% of pre-COVID (2019)
volumes. In 2020, 27% of encounters were virtual,
and established patient visits decreased from 60% to
46% (all p<0.008). The proportion of sinusitis
patients seen in clinic who underwent endoscopy
decreased from 98% in 2019 to 87% in 2020
(p=0.02), while computed tomography scans (CTs)
increased from 10% (2019) to 23% (2020) and 30%
(2022) (p=0.03). In contrast, there was little change
in management of patients diagnosed with tumor,
orbital pathology, or cerebrospinal fluid leak. In 2022,
total encounters were 132% of 2019 encounters with
the greatest increases in new patients with
inflammatory and non-surgical diagnoses. The
proportion of endoscopies was similar to 2019 levels,
but CTs remained elevated. The COVID-19
pandemic significantly affected the total number of
patients seen, virtual visit encounters, nasal
endoscopies, and imaging utilization. Further
research is needed to determine if patient outcomes
were impacted and if these changes in practice will
persist as we transition away from COVID
regulations.

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
108
POSTERS
Poster #099
The effect of acupuncture therapy on COVID-19
related olfactory loss
Michael Armstrong, MD
Thomas O. Byrne
Jason Calva
Carlos Pinheiro-Neto, MD
Garret Choby, MD, FARS
Erin O’Brien, MD, FARS
Brent Bauer
Janalee Stokken, MD, FARS
Mayo Clinic
Olfactory loss is a common symptom in patients with
COVID-19 infection. While budesonide irrigation and
olfactory training are effective, many patients fail to
recover olfaction. The objective of this study was to
examine the effect of acupuncture therapy on
COVID-19 related olfactory loss.
Thirty patients were randomized into two groups. The
standard group was treated with twice daily
budesonide irrigation and olfactory training. The
acupuncture group was treated with ten sessions of
acupuncture therapy in addition to the standard
group treatment. University of Pennsylvania Smell
Identification Test (UPSIT), 10-point visual analog
scale (VAS), and Sino-Nasal Outcome Test (SNOT-
22) scores were obtained at baseline and after three
months of treatment. Differences between study
arms were compared using Fisher’s exact and
Wilcoxon rank sum tests.
A total of 18 patients completed the study. Twenty-
seven percent of patients in the standard (3/11) and
43% of patients in the acupuncture group (3/7) had
an increase in UPSIT score by at least 5 points
(p=0.63). Mean UPSIT score improvement was 3.2
in the standard and 2.6 in the acupuncture group
(p=0.78). Mean VAS score improvement was 1.7 in
the standard and 1.9 in the acupuncture group
(p=1.00). Mean SNOT-22 score improvement was
3.5 in the standard and 7.1 in the acupuncture group
(p=0.89). There were no significant differences in
score improvement on subgroup analysis of patients
with olfactory loss > 12 months.
The effect of acupuncture on COVID-19 related
olfactory loss is uncertain. Further research into the
treatment of olfactory loss is warranted.
Poster #100
The impact of bundled codes on Medicare
volume and reimbursements for endoscopic
sinus surgery
Derek Liu, MD
Sina Torabi, MD
Benjamin Bitner, MD
Edward Kuan, MD, FARS
University of California, Irvine
Introduction:
In 2018, Medicare introduced changes to the
Endoscopic Sinus Surgery (FESS) family of Current
Procedural Terminology (CPT) codes. Three new
codes were introduced which bundled
ethmoidectomy with either frontal sinusotomy or
sphenoidotomy, with or without removal of tissue.
This study evaluates the volume and
reimbursements for FESS before and after the
introduction of bundled codes in 2018.
Methods:
Trends were analyzed using the Part B National
Summary Data File from years 2010 to 2021.
Volume was examined as the total number of
sinuses treated per year, with bundled codes
equated to two sinuses treated. An interrupted time
series analysis was conducted on volume and
reimbursements before and after the introduction of
bundled codes in 2018.
Results:
Prior to 2018, volume and reimbursements for FESS
grew at a mean rate of 2.5% ± 2.2% per year and
6.9% ± 6.6% per year, respectively. In 2020, likely
due to the COVID-19 pandemic, volume and
reimbursement decreased by 23.8% and 13.8%,
respectively. Excluding 2020 and 2021 from
interrupted time series analysis, the year 2018 was
associated with significantly decreased total
reimbursement (-13.9%, p=0.014) but stable
procedural volume (+0.72%, p=0.602). From 2018
to 2019, the rates of change of volume (+3.1%,
p=0.750) and reimbursements (4.9%, p=0.878)
remained similar to annual trends prior to 2018.
Conclusion:
Medicare-based FESS volume and reimbursements
steadily increased from 2010 to 2017. In 2018,
payments decreased significantly despite no change
in volume, which may be correlated to the
introduction of bundled CPT codes. Another
significant decrease in both volume and payments
occurred in 2020, likely due to the COVID-19
pandemic.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
109
POSTERS
Poster #101
The impact of Dupilumab treatment on CRSwNP
outcomes in patients with severe CRSwNP rrom
the SINUS-24 and SINUS-52 studies
Martin Desrosiers, MD
Scott Nash, Dr.
Andrew P. Lane, MD, FARS
Stella Lee, MD
Eugenio De Corso, Dr.
Changming Xia, Dr.
Asif Khan, Dr.
Juby Jacob-Nara, Dr.
Harry Sacks, MD, FAAP
Paul Rowe, Dr.
Yamo Deniz, Dr.
University of Montreal
Background:
Impaired nasal airflow is recognized as a high
burden of disease for patients with chronic
rhinosinusitis with nasal polyps (CRSwNP). This post
hoc analysis evaluated the effect of dupilumab on
key clinical outcomes for patients with CRSwNP and
baseline peak nasal inspiratory flow (PNIF) that is
abnormal (< 120 L/min) or normal (≥ 120 L/min) in
the SINUS-24 and SINUS-52 trials (NCT02912468/
NCT02898454).
Methods:
PNIF was recorded in patients treated with
dupilumab 300 mg every 2 weeks or placebo in the
pooled SINUS-24/SINUS-52 population. Changes in
CRSwNP outcome measures were analyzed to
Week 24 in patients with normal and abnormal
baseline PNIF.
Results:
Of 724 patients in the pooled intention-to-treat
population, 76% had PNIF < 120 L/min at baseline.
At Week 24, dupilumab significantly improved
CRSwNP outcomes for patients with a normal or
abnormal baseline PNIF. These included (least
squares mean difference [95% CI] vs placebo for
baseline PNIF < 120 or ≥ 120 L/min, respectively):
PNIF (41.2 [33.8, 48.5] and 29.5 [15.9, 43.1]), nasal
polyp score (–1.86 [–2.12, –1.59] and –2.01 [–2.47,
–1.54]), loss of smell score (–1.03 [–1.18, –0.89] and
–1.02 [–1.30, –0.75]), nasal congestion/obstruction
(–0.81 [–0.96, –0.67] and 1.10 [–1.32, –0.89]),
SNOT-22 (–18.86 [–21.97, –15.75] and –18.03
[–23.18, –12.88]), UPSIT (10.03 [8.71, 11.35] and
11.41 [8.91, 13.91]), and LMK-CT (–5.99 [–6.63,
–5.36] and –6.33 [–7.43, –5.23]) vs placebo. All
analyses P < 0.0001 vs placebo.
Conclusion:
Most patients had impaired nasal airflow at baseline.
However, dupilumab improved clinical outcome
measures in patients with severe CRSwNP
irrespective of baseline PNIF.
Poster #102
The impact of the lateral crural reversing on the
primary concavity
Mohsen Naraghi, MD, FARS
Orphans World Wide
Introduction:
Extreme concavities of the lower lateral crura can
cause severe aesthetic and functional problems.
Lateral crural reversing can contour the shape,
reconstruct lateral crus completely, and correct
concavity and valve collapse by a simple but delicate
technique. It could be done with or without
reinforcing grafts.
Methods:
This retrospective study was directed at thirty-four
primary rhinoplasty patients with the follow-up from
one to eight years. After transcolumellar and
marginal incisions, the skin flap was elevated in a
supraperichondrial plane, exposing the lower lateral
cartilages and cartilaginous dorsum. Then the
mucosa was detached from the posterior surface of
the lower lateral crura. The cartilages were released,
excised, reversed, and fixed in place. Different lateral
crural grafts were used in some of the patients.
Results:
All patients were improved in form and function with
different degrees of improvement according to the
Nasal Obstruction Symptom Evaluation (NOSE)
Scale. There was no significant difference between
the patient with or without the use of grafts.
Postoperative swelling was longer in patients with
grafts. However, there was no long-term complication
and all patients were satisfied with the long-term
aesthetic and functional results.
Conclusion:
With the lower lateral crural reverse plasty, severe
concavities of the lower lateral crura can be
corrected. This technique is a useful and
reproducible procedure, performed without additional
tissue to achieve functionally and aesthetically
satisfying and enduring results.

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
110
POSTERS
Poster #103
The influence of facility volume and type on
sinonasal undifferentiated carcinoma treatment
and outcomes
Amy Du , BS
Sina Torabi, MD
Arash Abiri, MS
Khodayar Goshtasbi, MD
Edward Kuan, MD, FARS
Background:
Sinonasal undifferentiated carcinoma (SNUC) is a
rare and highly aggressive primary malignancy of the
sinonasal tract, with multimodal strategies being the
cornerstone of treatment. This study evaluates the
influence of facility volume and type on SNUC
treatment and overall survival (OS).
Methods:
The 2004-2016 National Cancer Database was
queried for SNUC patients receiving definitive
treatment. Facilities were categorized by volume by
calculating the mean number of patients treated per
facility during the study time span and using cutoff
volumes that were 0.5 standard deviations above
and below the mean. Low-volume facilities (LVFs)
were defined as treating 1 patient, high-volume
facilities (HVFs) as treating ≥4 patients, and mid-
volume facilities (facilities treating 2-3 patients) were
excluded. Differences in treatment course, outcomes,
and OS by facility volume and type were assessed
using multivariable regression.
Results:
731 patients (34.3% female, 83.3% white) were
included. Facilities were categorized into 165 LVFs
and 58 HVFs. Compared to LVFs, HVFs treated
more patients >65 years of age (79.3% vs 60.6%,
p=0.010), more patients with private insurance
(65.5% vs 49.1%, p=0.008), and patients were more
likely to receive chemotherapy (77.6% vs 59.4%,
p=0.038). On Cox proportional-hazard multivariate
regression, no significant association was found
between OS and facility volume or type (p=0.458 and
p=0.677, respectively).
Conclusion:
Higher facility volume and academic facility type do
not appear to be a significant predictor of improved
survival outcomes in the treatment of SNUC, which
may be attributed to its highly aggressive course.
Poster #104
The influence of inhibitors of apoptosis proteins
(IAPs) on chronic rhinosinusitis with nasal
polyps
Wilma Anselmo-Lima, MD, PhD
Fabiana Valera, PhD
Ivna Passos, MD, PhD
Marina Fantucci, MD
Adriana Murashima, MD
Lilian Silva, MD
Denny Garcia, PhD
Francesca Faria, MD
Ronaldo Martins, MD, PhD
Eurico Arruda Neto, MD, PhD
Edwin Tamashiro, PhD
Ribeirão Preto Medical School of University of São
Paulo
Introduction:
Inhibitors of apoptosis proteins (IAPs) could have a
role in the CRSwNP or interfere with the
susceptibility of NP with topical nasal corticosteroids.
Objectives:
To compare the expression of IAPs between patients
with CRSwNP and controls, to associate the
expression of IAPs with the response to nasal
corticosteroids, and to correlate the expression of
IAPs to inflammatory markers.
Methods:
We obtained nasal biopsies from patients with
CRSwNP (n=27) and controls (n=16). The gene
expression of IAPs (XIAP, BIRC2/IAP1 and BIRC3/
IAP2) and caspases (CASP3, CASP7, CASP9 and
BCL2) were measured by qRT-PCR. The dosages
IFN-α, IL-5, IL-33, IL-10, IL-17, and TGF-β were
measured by the Luminex. Principal Component
Analysis (PCA) was used to correlate the expression
of the markers with the response to nasal
corticosteroids in the patients.
Results:
We found lower expression of the three IAP genes
and significantly higher expression of the cytokines
INF-α, IL-5, and TGF-β in patients compared to
controls.BIRC2/IAP1 expression was significantly
associated with poor response to topical
corticosteroids. PCA analysis identified that BIRC2/
IAP1, XIAP, BCL2, CASP9, IL-17 and IL-33 were
increased in patients with better clinical response,
while CASP7 and TGF- β were related to worse
response to treatment.
Conclusions:
Our data suggest that the decrease in IAPs
expression is significant in the CRSwNP
pathophysiology and may predict worse outcome to
clinical treatment.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
111
POSTERS
Poster #105
The role of normal nasal anatomical variability on
intranasal drug particle transport
Claire Washabaugh, BS
Ryan M. Sicard, BS
Sarah M. Russel, MD, MPH
Dennis O. Frank-Ito, PhD
Background:
This study investigates the role of two normal nasal
anatomical variations – nasal vestibule notched
indentation size (permanent variation) and nasal
cycle (temporal variation) – on intranasal spray drug
particle transport in the cavity of three healthy adult
subjects (S1, S2, and S3) with normal nasal
anatomy.
Methods:
The Nasal Obstruction Symptom Evaluation (NOSE)
scores and cone beam computed tomography
(CBCT) images were obtained from all subjects.
Unilateral notched indentation size and nasal cycling
state at time of CBCT were assessed. CBCT images
were used to create subject-specific nasal cavity
models for performing computational fluid dynamics
airflow and intranasal spray particle transport
simulations.
Results:
NOSE scores were: S1=15, S2=25, and S3=0.
Unilateral notched assessment showed the right side
had larger indentation (narrower nasal vestibule) in
all three subjects. Nasal cycling states: S1 left side
was less patent, S2 left side was less patent, and S3
right side was less patent. Drug particle depositions
showed 91-94% anterior deposition on the side with
greater notched indentation versus 58-87% anterior
deposition on the smaller notched indentation side.
Posterior depositions on lateral and septal mucosa
were: less patent nasal cycle side had 0-8% and
0-23% lateral and septal depositions, respectively;
more patent nasal cycle side had 0.03-7% and
0-0.17% lateral and septal depositions, respectively.
Conclusion:
Findings from pilot data suggest that larger nasal
vestibule notched indentation may lead to increased
anterior deposition. More patent nasal cycling side
had greater posterior lateral mucosa deposition, and
less patent nasal cycling side had greater posterior
septal mucosa deposition.
Poster #106
The validation of the readability enhanced
sinonasal sinonasal outcome test (reSNOT-22)
disease-specific quality of life survey
Abdullah Zeatoun, MD, Presented by Adam Kimple,
MD, FARS
University of North Carolina-Chapel Hill
Introduction:
The readability of the Sinonasal Outcome Test
(SNOT-22) QOL survey is above the recommended
6th-grade level for patient-centered documents.
Previous studies have demonstrated that patients
with limited health literacy have worse sinonasal
disease-specific Quality of Life (QOL) than patients
with adequate health literacy. This study aimed to
validate the proposed improved alternative
Readability Enhanced Sinonasal Outcome Test
(reSNOT-22).
Methods:
Three validated readability metrics were used to
analyze the readability of the SNOT-22 questions.
For questions that were outside of the 6th-grade
level, alternative texts were devised by a panel of
Rhinologists (n=5). Second, the alternative text was
presented to patients, and they were asked to
choose the text that made the most sense to them,
while the Brief health literacy screening tool (BRIEF)
was collected at the same visit. Finally, the
reSNOT-22 was validated in a clinical population and
compared to the original SNOT-22 in Chronic
Rhinosinusitis (CRS) patients.
Results:
The three readability measure scores were 5th,7th,
and 11th grade for the SNOT-22. 7 of the 22
questions were above the recommended 6th-grade
reading level.
The proposed alternative text reSNOT-22 improved
the SNOT-22 grade-level readability. To date, 49
patients have been enrolled. The mean age was 52,
and 22 females.
Conclusion:
The SNOT-22 readability is above the recommended
level. However, with simple alterations, the new
reSNOT-22 is easier, simpler, and preferred by
patients.

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
112
POSTERS
Poster #107
Three cases of sinonasal organized hematoma
Sei Kobayashi, MD
Yasuyuki Hinohira, Professor
Masakazu Murayama
Yoichiro Narikawa
Takatoshi Tokudome
Naruo Shoji
Tomotaka Shimura
Taketoshi Nogaki
Introduction:
Organized hematoma of the sinonasal tract is a rare
clinical disease, which requires differential diagnosis
from malignant tumor. We report three cases of
organized hematoma.
Case:
66 year-old female visited us with oral bleeding. The
easily bleeding tumor-like lesion was found in the left
gingivabuccal sulcus. Computed tomography (CT)
showed well-defined expansive soft tissue shadows
with bone erosion. The lesion showed high intensity
in T1 and low intensity in T2-weighted magnetic
resonance imaging (MRI). Caldwell-Luc operation for
total removal of the tumor was performed.
28 year-old female visited us with the right nasal
bleeding from polyps in the middle nasal meatus. CT
and MRI showed the mass lesion existing from the
right nasal cavity to the maxillary sinus with bone
erosion. Caldwell-Luc operation for total removal of
the tumor was performed.
70 year-old male visited us with the frequent
epistaxis. Rhinoscopy revealed easily bleeding mass
lesion in the middle nasal meatus. CT showed the
mass lesion located in frontal sinus and ethmoid
sinus with bone erosion. The lesion showed low
intensity in T1 and high intensity in T2-weighted MRI.
Extranasal approach combined with endonasal
endoscopic surgery was performed.
No recurrent lesion has been seen in the three
cases.
Discussion:
Organized hematoma of the sinonasal tract is very
rare. The progressive expansion of the tumor causes
the demineralization of adjacent structures. In many
patients with organized hematoma, the findings of
CT and MRI are similar to neoplastic diseases.
Therefore, surgical intervention is required in order to
distinguish from malignant tumors.
Poster #108
Triple-combination Cystic Fibrosis
transmembrane conductance regulator (CFTR)
modulator therapy and functional endoscopic
sinus surgery in Cystic Fibrosis with chronic
rhinosinusitis
Brian Kinealy, MD
Tony Mangino, PhD
Amina Anwar, Medical Student
Michael Anstead, MD, FCCP
Brett Comer, MD, FARS
Cystic fibrosis (CF) causes dysfunction of the CF
transmembrane conductance regulator (CFTR),
leading to manifestations that include bronchiectasis,
pancreatic insufficiency, and chronic rhinosinusitis
(CRS). Computed tomography demonstrates CRS in
90-100% of patients with CF. The rate of functional
endoscopic sinus surgery (FESS) in CF is greater
than 20%. Prior to the advent of targeted therapies,
the rate of revision FESS was shown to be
significantly higher in adult CF patients with CRS
compared to adults without CF, on the order of
18.7% compared to 13.4%. These patients also
underwent revision FESS sooner than the general
population, with a mean of 3.52 years as opposed to
4.23 years. Elexacaftor/tezacaftor/ivacaftor (ELX/
TEZ/IVA) treatment has been associated with
decreased Lund-Mackay scores and decreased
sinus opacification, but little is known regarding the
effect of CFTR modulators on FESS or revision
FESS. With the advent of ELX/TEZ/IVA treatment in
2019, CF patients would be expected to return for
revision FESS by late 2022, unless there were a
substantial effect of ELX/TEZ/IVA on sinonasal
symptomatology and need for revision surgery. This
study is a retrospective review of adult patients with
CF and CRS who underwent FESS at the University
of Kentucky between the years of 2006 and 2022.
We hypothesized that treatment with CFTR
modulator therapy decreases the likelihood of
revision FESS and increases the duration between
index operation and subsequent FESS. Preliminary
data suggests that both revision FESS rate is
decreased with the use of ELX/TEZ/IVA and that
duration between FESS surgeries is positively
impacted by the use of ELX/TEZ/IVA.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
113
POSTERS
Poster #109
Utilizing 3D navigation to enhance endoscopic
sinus educational dissection for Otolaryngology
trainees
Tadeas Lunga, MD
Aviv Spillinger
Sandra Lin, MD, FARS
Background:
Functional endoscopic sinus surgery (FESS) carries
intraoperative risks, requiring CT scans for proper
patient anatomical mapping. Use of a 3D Navigation
System (TruDi) may reduce these risks and enhance
training through image-guided navigation. This study
evaluated how TruDi may enhance anatomical
understanding, thoroughness, and outcomes for
sinus surgeries among otolaryngology trainees.
Methods:
Eleven otolaryngology residents participated in
cadaveric endoscopic sinus dissection with
increasing difficulty on a cadaver head based on
their PGY year. TruDi technology was visible on the
right side and hidden on the left side dissection. Fast
Anatomical Mapping was used to evaluate the
completeness of dissection with and without the
technology. A one-way repeated ANOVA was
conducted on five residents to examine the
completeness of dissection. After dissection, Likert
scale questionnaires were completed by trainees
assessing their overall experience with the TruDi
system.
Results:
Eight residents found the technology helpful, six felt
safer using it, seven felt it aided the completeness of
surgery, nine felt it improved understanding of
anatomy, and ten said they would use it again. Of
the five residents evaluated for completeness of
dissection, there was no statistically significant
difference between dissections performed with and
without TruDi.
Conclusion:
3D navigation system shows promise in improving
the learning experience for trainees. It may aid in the
completeness of surgery and understanding of
anatomy while providing additional safety. Although
the completeness of surgery was not significantly
different with or without the TruDi system, further
evaluation is needed to draw definitive conclusions.
Poster #110
Voice quality changes follow sinonasal surgery
Meha Fox, MD
Tran Locke, MD
Sylvia Adu-Gyamfi, Training Associate
Sarah Blumhardt, Speech Pathologist
Lauren Brewster, Medical Student
Julina Ongkasuwan, Professor
Baylor College of Medicine
Introduction:
Voice affects social function. Prior studies
demonstrate variable impact of sinonasal surgery on
voice quality measures, and none assess formant
changes. The purpose of this study was to delineate
any objective and clinician-perceived subjective
changes in voice quality following sinonasal surgery.
Methods:
From November 2021 to August 2022, six adults
were recruited. Pre- and post-operative voice
recordings were analyzed using KayPentax
computerized speech lab software. Consensus
Auditory-Perceptual Evaluation of Voice (CAPE-V)
assessment was completed by two independent
reviewers. Wilcoxon signed-rank test was used to
analyze the pre- and post-operative formant and
CAPE-V scores.
Results:
Four males underwent endoscopic sinus surgery,
and two females underwent septoplasty with inferior
turbinate reduction. There was a statistically
significant difference between pre- and post-
operative formants 2 (F2) and 3 (F3) for the nasal
consonant /n/. There was no statistically significant
difference in pre- and post-operative formants 1-4
(F1-F4) for the nasal sounds /m/, /a/, and /i/, or in F1
and F4 for the sound /n/. However, the change in
mean for F2-4 /m/, F4 /a/, F1-4 /n/, and F2-4 /i/ was
greater than 50 Hz, which is clinically significant.
There was no statistically significant difference in
pre- and post-operative CAPE-V scores.
Conclusion:
Prior studies demonstrate variable changes in voice
following sinonasal surgery. Our study revealed a
clinically significant difference in formants. Lack of
statistical significance is likely due to small study
population. Larger scale studies assessing objective
and subjective measures of voice are needed to
better define voice changes following sinonasal
surgery.

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
114
POSTERS
Poster #111
Which intranasal corticosteroids can be used in
patients on PrEP or HAART?
Meghan Nicole Norris, PA-C
Erin Lopez
Daniel Alicea Delgado, MD
Brian D. Thorp, MD, FARS
Cristine N. Klatt-Cromwell, MD
Charles S. Ebert, Jr., MD, MPH, FARS
Brent Senior, MD, FARS
Adam Kimple, MD, FARS
UNC
Background:
Approximately 1.3 million Americans live with HIV.
Pre-exposure prophylactic (PrEP) has increased by 8
fold in the last 5 years. Intranasal corticosteroids
(INCS) are typically avoided in patients on
antiretroviral therapy regimens that include protease
inhibitors as they decrease the metabolism of
iatrogenic steroids. This can result in Cushing’s
syndrome and adrenal suppression even from use of
topical nasal steroids. We are interested to know
which INCS are contraindicated in patients on PrEP
and highly active antiretroviral therapy (HAART)
regimens.
Methods:
University of Liverpool HIV Medication Interaction
Checker was used to assess antiretroviral therapy
and PrEP medication interactions with fluticasone,
mometasone, budesonide, beclomethasone,
triamcinolone, and flunisolide nasal sprays.
Results:
The PrEP medications are emtricitabine / tenofovir
(Truvada), emtricitabine / tenofovir (Descovy) and
cabotegravir (Apretude). There were no reported
interactions with INCS and any of the PrEP
medications. INCS should be avoided in patients on
HAART regimens that include ritonavir, cobicistat,
darunavir, atazanavir, efavirenz, etravirine,
lenacapavir, or nevirapine. The exception to this rule
is that beclomethasone can generally be used safely;
however, clinicians should monitor for symptoms of
Cushing’s syndrome, such as fatigue, muscle
weakness and weight gain in any patient on HAART
and INCS.
Conclusion:
INCS may be safely utilized in patients on PrEP.
Patients on HAART regimens that do not include
ritonavir, cobicistat, darunavir, atazanavir, efavirenz,
etravirine, lenacapavir, or nevirapine can be treated
with INCS with reasonable oversight and monitoring
for symptoms of Cushing’s syndrome.
Poster #112
Wide resection of extradural skull base lesions
requiring sacrifice of internal carotid artery:
Preliminary surgical outcome at a single medical
center
Sung-Woo Cho, MD
Tae-Bin Won, MD, PhD
Kihwan Hwang, MD
Seoul National University Bundang Hospital
Introduction:
Skull base lesions invading internal carotid artery
(ICA) are challenging as these pathologies can
progress and eventually lead to death. In this study,
we tried to evaluate our preliminary surgical outcome
of extradural skull base lesions requiring sacrifice of
ICA.
Methods:
Retrospective review of patients was performed for
those who underwent endoscopic radical resection of
extradural skull base lesion invading the ICA. In all
cases, invaded ICAs were occluded either
spontaneously or intentionally. Pathologies,
management of ICA, and surgical outcomes were
evaluated.
Results:
Eleven cases (mean age 61.7 years) were collected.
Pathologies were osteoradionecrosis (ORN) (N=7),
ORN combined with malignancy (N=3), and
malignancy without ORN(N=1). ICAs were managed
as follows; spontaneous ICA occlusion (N=5).
occluded intentionally (pre-operative embolization or
intra-op planned ligation) (N=5), and extracranial to
intracranial bypass surgery (N=3). Mean duration of
follow up was 20 months (range 3-56 months). After
radical resection, severe headache decreased from
72.7% to 17.2%. However, cranial nerve palsy was
increased from 72.7% to 81.8%. There were 3 cases
of disease progression and eventual death. Among
them 2 had uncontrolled cancer regrowth and the
other developed brain stem necrosis after adjuvant
radiotherapy. The 2-year progression free survival
was 71.6%. All the patients without disease
progression (N=8) were alive and showed acceptable
functional outcome with ECOG performance below 1.
Conclusion:
Radical resection of the skull base lesion invading
ICA can be performed with no peri-operative
mortality. Depending on the disease pathology, good
post operative performance can be expected.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
115
Fellows of the American Rhinologic Society
Waleed Abuzeid, MD, FARS
Nithin Adappa, MD, FARS
Omar Ahmed, MD, FARS
Abdullah Al Bader, MBBS, FARS
Ford Albritton IV, MD, FARS
Gustavo Almodovar-Mercado, MD, FARS
Ghassan Alokby, MD, FARS
Jeremiah Alt, MD, PhD, FARS
Kenneth Altman, MD, FARS
Jastin Antisdel, MD, FARS
Sanford Archer, MD, FARS
Henry Barham, MD, FARS
Fuad Baroody, MD, FARS
Emily Barrow, MD, FARS
Pete Batra, MD, FARS
Richard Beck, MD, FARS
Adam M. Becker, MD, FARS
Karen Bednarski, MD, FARS
Jeffrey Bedrosian, MD, FARS
Thomas Benda, MD, FARS
Michael Benninger, MD, FARS
Regan Bergmark, MD, FARS
Daniel Beswick, MD, FARS
Naveen Bhandarkar, MD, FARS
Benjamin S. Bleier, MD, FARS
Robert Bridge, MD, FARS
Seth Brown, MD, FARS
Nicolas Busaba, MD, FARS
Jose Busquets Ferriol, MD, FARS
Adam Campbell, MD, FARS
Raewyn Campbell, MD, FARS
David Caradonna, MD, FARS
Roy Casiano, MD, FARS
Peter Joseph Catalano MD, FARS
Mohamad Chaaban, MD, FARS
Yvonne Chan, MD, FARS
Rakesh Chandra, MD, FARS
Dennis F. Chang, MD, FARS
Eugene Chang, MD, FARS
Philip Chen, MD, FARS
Nipun Chhabra, MD, FARS
Alexander Chiu, MD, FARS
Garret Choby, MD, FARS
Andy Chua, MD, FARS
Christopher Church, MD, FARS
Martin J. Citardi, MD, FARS
David Clark, MD, FARS
Perrin Clark, MD, FARS
Alen Cohen, MD, FARS
Noam Cohen, MD, FARS
Brett Comer, MD, FARS
David Conley, MD, FARS
John Craig, MD, FARS
Dana Crosby, MD, FARS
Michael Cruz, MD, FARS
Opeyemi Daramola, MD, FARS
Subinoy Das, MD, FARS
Greg Davis, MD, FARS
Nathan Deckard, MD, FARS
Robert DeDio, MD, FARS
John Del Gaudio, MD, FARS
Kara Detwiller, MD, FARS
H. Peter Doble, MD, FARS
Brennan Dodson, MD, FARS
Angela Donaldson, MD, FARS
Marc Dubin, MD, FARS
Jay Dutton, MD, FARS
Charles Ebert, Jr., MD, FARS
David Edelstein, MD, FARS
Jean Anderson Eloy, MD, FARS
Alexander Farag, MD, FARS
Elisabeth Ference, MD, FARS
Adam Folbe, MD, FARS
Karen Fong, MD, FARS
Christine Franzese, MD, FARS
Marvin P. Fried, MD, FARS
Richard Gall, MD, FARS
Rohit Garg, MD, FARS
Mathew Geltzeiler, MD, FARS
Ross Germani, MD, FARS
Andrew Goldberg, MD, FARS
James D. Gould, MD, FARS
Satish Govindaraj, MD, FARS
Parul Goyal, MD, FARS
Scott Graham, MD, FARS
Stacey Gray, MD, FARS
David Greene, MD, FARS
David Gudis, MD, FARS
James Hadley, MD, FARS
Ashleigh Halderman, MD, FARS
Joseph Han, MD, FARS
Wade Han, MD, FARS
Gady Har-El, MD, FARS
Richard Harvey, MD, FARS
Samuel Helman, MD, FARS
Thomas Higgins, MD, FARS
Eric Holbrook, MD, FARS
Christian Hull, MD, FARS
Ian Humphreys, DO, FARS
Peter Hwang, MD, FARS
Elisa Illing, MD, FARS
Christopher Ito, MD, FARS
David Jang, MD, FARS
Amin Javer, MD, FARS
Stephanie Joe, MD, FARS
Deya Jourdy, MD, FARS
Jeb Justice, MD, FARS
Seth Kanowitz, MD, FARS
Boris Karanlov, MD, FARS
David Kennedy, MD, FARS
Robert Kern, MD, FARS
David Keschner, MD, FARS
Esther Kim, MD, FARS
Jean Kim, MD, FARS
Adam Kimple, MD, FARS
Todd Kingdom, MD, FARS
Anna Knisely, MD, FARS
Ian Koszewski, MD, FARS
Stilianos Kountakis, MD, FARS
Jeffrey S. Krivit, MD, FARS
John Krouse, MD, FARS
Edward Kuan, MD, FARS
Devyani Lal, MD, FARS
Kent Lam, MD, FARS
Andrew Lane, MD, FARS
Donald Lanza, MD, FARS
Christopher Le, MD, FARS
Richard A. Lebowitz, MD, FARS
Annie Lee, MD, FARS
Jivianne Lee, MD, FARS
Victoria Lee, MD, FARS
William Leight, MD, FARS
Randy Leung, MD, FARS
Corinna Levine, MD, FARS
Howard Levine, MD, FARS
Joshua Levy, MD, FARS
Jonathan Liang, MD, FARS
Sandra Y. Lin, MD, FARS
Brian Lobo, MD, FARS
Todd Loehrl, MD, FARS
Neal Lofchy, MD, FARS
Patricia Loftus, MD, FARS
Nyall London, MD, FARS
Mark C. Loury, MD, FARS
Lauren Luk, MD, FARS
Amber Luong, MD, PhD, FARS
Luis Fernando Macias-Valle, MD, FARS
Chadi Makary, MD, FARS
Li-Xing Man, MD, FARS
Lee Mandel, MD, FARS
R. Peter Manes, MD, FARS
Michael Marino, MD, FARS
Steven Marks, MD, FARS
Alice Maxeld, MD, FARS
Stanley McClurg, MD, FARS
Edward McCoul, MD, FARS
K. Chris McMains, MD, FARS
Bradford Mechor, MD, FARS
Josh Meier, MD, FARS
Christopher Melroy, MD, FARS
Ralph B. Metson, MD, FARS
Suzette Mikula, MD, FARS

ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
116
Fellows of the American Rhinologic Society
Joseph Mirante, MD, FARS
Jeffrey Myhill, MD, FARS
Mohsen Naraghi, MD, FARS
Ryan Neilan, MD, FARS
Gurston G. Nyquist, MD, FARS
Gretchen M. Oakley, MD, FARS
Daniel O'Brient, MD, FARS
Erin O'Brien, MD, FARS
Richard Orlandi, MD, FARS
Randall Ow, MD, FARS
James Palmer, MD, FARS
Ankit Patel, MD, FARS
Chirag Patel, MD, FARS
Zara Patel, MD, FARS
Spencer Payne, MD, FARS
Aaron Pearlman, MD, FARS
Robert Pincus, MD, FARS
David M. Poetker, MD, FARS
Alan Pokorny, MD, FARS
Juan Portela, MD, FARS
Jordan Pritikin, MD, FARS
Melissa A. Pynnonen, MD, FARS
Mindy Rabinowitz, MD, FARS
Roheen Raithatha, MD, FARS
Hassan Ramadan, MD, FARS
Jeevan Ramakrishnan, MD, FARS
Vijay Ramakrishnan, MD, FARS
Murugappan Ramanathan, Jr, MD, FARS
Sanjeet Rangarajan, MD, FARS
Douglas D. Reh, MD, FARS
Camilo Reyes, MD, FARS
Ryan Rimmer, MD, FARS
Rachel Roditi, MD, FARS
John Romanow, MD, FARS
Austin Rose, MD FARS
Marc Rosen, MD, FARS
Allan Rosenbaum, MD, FARS
Arthur Rosner, MD, FARS
Brian Rotenberg, MD, FARS
Christopher Roxbury, MD, FARS
Paul Russell, III, MD, FARS
Matthew Ryan, MD, FARS
Alok Saini, MD, FARS
Zoukaa Sargi, MD, FARS
Rodney J. Schlosser, MD, FARS
Jerry Schreibstein, MD, FARS
Theodore Schuman, MD, FARS
Kirby Scott, DO, FARS
Brent A. Senior, MD, FARS
Gavin Setzen, MD, FARS
Michael Setzen, MD, FARS
Adam M. Shapiro, MD, FARS
David A. Sherris, MD, FARS
Alan Shikani, MD, FARS
Timothy Siglock, MD, FARS
Michael J. Sillers, MD, FARS
Stacey Silvers, MD, FARS
Raj Sindwani, MD, FARS
Ameet Singh, MD, FARS
Douglas Skurada, MD, FARS
Timothy Smith, MD, FARS
Zachary Soler, BA, FARS
Alla Y. Solyar, MD, FARS
James A. Stankiewicz, MD, FARS
Michael Stewart, MD, FARS
Janalee K. Stokken, MD, FARS
J. Pablo Stolovitzky, MD, FARS
Scott Stringer, MD, FARS
Jeffrey Suh, MD, FARS
Krishnamurthi Sundaram, MBBS, FARS
Ronnie Swain, Jr., MD, FARS
Abtin Tabaee, MD, FARS
Mas Takashima, MD, FARS
Bobby Tajudeen, MD, FARS
Thomas Tami, MD, FARS
Dennis Tang, MD, FARS
Luisam Tarrats, MD, FARS
Jordan Teitelbaum, MD, FARS
Erica Thaler, MD, FARS
Brian Thorp, MD, FARS
Jonathan Ting, MD, FARS
Charles Tong, MD, FARS
Elina Toskala, MD, FARS
Justin Turner, MD, FARS
Winston Vaughan, MD, FARS
Darshni Vira, MD, FARS
Frank Virgin, MD, FARS
Jarrett Walsh, MD, FARS
Eric Wang, MD, FARS
Marilene Wang, MD, FARS
Danielle Warner, MD, FARS
Robert Weiss, MD, FARS
Kevin Welch, MD, FARS
Sarah Wise, MD, FARS
Ian James Witterick, MD, FARS
Troy D. Woodard, MD, FARS
Bradford A. Woodworth, MD, FARS
Erin Wright, MD, FARS
Bozena Wrobel, MD, FARS
Arthur W. Wu, MD, FARS
Rhoda Wynn, MD, FARS
William Yao, MD, FARS
Michael Yim, MD, FARS
Mark A. Zacharek, MD, FARS
Become a Fellow of the American Rhinologic Society:
https://www.american-rhinologic.org/fellow-of-the-ars
ARS Fellow Membership: A physician who has met the criteria for Regular membership and has
the following additional qualifications: must be out of residency for at least 3 years, 50 surgical
rhinologic cases in two years, Publications or other evidence of scholarly activity in rhinology,
attendance at two American Rhinologic Society meetings or ARS-sponsored courses over a
three-year period may apply to become a Fellow of the Society. Fellows shall have the same
rights and privileges of Regular members and shall be eligible to vote, serve on one or more
committees, and in addition may hold office. A complimentary on-line and hard copy subscrip-
tion to the International Forum of Allergy & Rhinology will be provided with your paid annual
membership.

AMERICAN-RHINOLOGIC.ORG
ARS 69TH ANNUAL MEETING • SEPTEMBER 29-30, 2023 • NASHVILLE, TN
117
Keep up to date with current research regarding the
management of otolaryngic allergy, rhinologic, and skull
base diseases. IFAR is indexed in PubMed and ISI, and
achieved a first year impact factor of 1.00. With its app you
will experience:
• Readable, print-like experience enhanced with dynamic
figures, tables, and references
• Rapid access to breaking research — Early View articles
updated as they publish
• Adjustable text and table sizing with “pinch and zoom”
• Ability to browse content before downloading an issue,
and to download issues to read offline
• Email and social media sharing tools
• Links to supplemental material online
• Convenient alerts when new issues are available
Your invitation to experience
the International Forum of Allergy & Rhinology app
International Forum of Allergy & Rhinology. To Go.
Introducing International Forum of Allergy & Rhinology for the iPad
®
, iPhone
®
, and iPod
®
.
Apple, iPad, iPhone, and iPod are trademarks of Apple Inc., registered in the U. S. and other. App Store is a service mark of Apple Inc.
Can’t Access International Forum of Allergy & Rhinology? Recommend this title to your institutional library.
ARS and AAOA Members! Your subscription includes the new app!
Log in with your regular Wiley Online Library log-in to access journal content with the app
Submit your next paper to:
http://mc.manuscriptcentral.com/alr
If your institution subscribes to IFAR , follow the
steps below to get access:
Register to create an account on Wiley Online Library
or, if you already have one, log in
Access Wiley Online Library from your institution’s
network and log in. If you are off-site and need
help getting access to licensed content, contact your
librarian
Visit the roaming access section of “My Profile” and
click “Activate Roaming Access”
Download the International Forum of Allergy &
Rhinology app from iTunes
Launch app from the Newsstand, and follow the steps
in the access wizard
1
2
3
4
5
Enter your Wiley Online Library account information.
For more detailed instructions, visit Journal iPad
®
App
Frequently Asked Questions
SCAN AND
DOWNLOAD
Submit your next paper to:
http://www.american-rhinologic.org/journal
International Forum of Allergy and Rhinology
Top 20 Reviewers
Ryan Rimmer, MD, FARS
Mathew Geltzeiler, MD, FARS
Daniel Beswick, MD, FARS
Nyall London, MD, FARS
Do-Yeon Cho, MD
Nicholas Rowan, MD
Christopher Brook, MD
Chadi Makary, MD, FARS
Edward Kuan, MD, FARS
Naweed Chowdhury, MD
Jerey Suh, MD, FARS
Lauren Roland, MD
Victoria Lee, MD, FARS
Justin Turner, MD, FARS
Devyani Lal, MD, FARS
Benjamin Bleier, MD, FARS
Kara Detwiller, MD, FARS
Garret Choby, MD, FARS
Rodney Schlosser, MD, FARS
David Gudis, MD, FARS

Contact: Wendi Perez, ARS Executive Administrator
Tel: 973-545-2735, Ext. 4105 Email: [email protected]
american-rhinologic.org
Twitter / Facebook / Instagram: @amrhinosociety
ARS 13th Annual
Summer Sinus
Symposium
Best Sinus Course in the World:
Improving Rhinology from Office to OR
July 12-14, 2024
Hyatt Regency New Orleans
New Orleans, LA
13
TH
Annual
ARS 70th
Annual Meeting
September 26-28, 2024
Miami, FL
COSM 2024
May 15-16, 2024
Hyatt Regency Chicago
Chicago, IL
2024
SAVE THE DATE
