
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
2
Table of Contents
About this document .................................................................................................................................... 3
Disclaimer ..................................................................................................................................................... 3
How eating became unhealthy .................................................................................................................... 4
What do fasting and time-restricted eating mean? ..................................................................................... 5
Autophagy and intermittent fasting ............................................................................................................. 6
Healthy eating .............................................................................................................................................. 7
What happens when we eat: all about insulin and insulin resistance ...................................................... 7
The glycemic index ................................................................................................................................... 8
Flattening the glucose curve .................................................................................................................... 9
Why your gut microbiome matters ........................................................................................................ 11
Avoid distracted eating .......................................................................................................................... 12
A brief guide to intermittent fasting/time-restricted eating ...................................................................... 13
How to get started ................................................................................................................................. 14
Remember, (almost) anyone can fast .................................................................................................... 14
Dealing with hunger while fasting .......................................................................................................... 15
What to eat and what not eat ................................................................................................................ 15
Fasting while on medication ................................................................................................................... 18
Women and fasting .................................................................................................................................... 18
Why men and women respond differently to intermittent fasting ........................................................ 19
The menstrual cycle ................................................................................................................................ 19
Fasting and the menstrual cycle ............................................................................................................. 21
Fasting during perimenopause and menopause .................................................................................... 23
Increasing estrogen through diet and lifestyle ....................................................................................... 23
Foods containing phytoestrogens .......................................................................................................... 24
Exercise and menopause ........................................................................................................................ 24
Learn more about intermittent fasting ...................................................................................................... 25
READ ....................................................................................................................................................... 25
WATCH ................................................................................................................................................... 25
References .................................................................................................................................................. 26
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
3
About this document
Many people are concerned about the lingering effects of spike protein, acquired in the body through
either COVID-19 infection or injection, and are wondering how to rid the body of it. The FLCCC
recommends intermittent fasting as one of the most effective ways to induce autophagy, the process by
which the body clears out damaged and misfolded cells. Fasting also has additional health benefits in
that it lowers insulin levels and helps people who have become insulin-resistant to restore sensitivity.
This document should serve as a quick guide to anyone interested in beginning to explore the beneficial
effects of intermittent fasting and time-restricted eating. It is not an exhaustive resource, and we will
continue to evolve and develop it over time. Please read this in conjunction with our prevention,
treatment, and recovery protocols, which contain further details and recommendations specific to
particular health states.
Disclaimer
This guide is meant solely for educational purposes. Never disregard professional medical advice
because of something you have read on our website and releases. This is not intended to be a substitute
for professional medical advice, diagnosis, or treatment regarding any patient. Treatment for an
individual patient is determined by many factors and thus should rely on the judgment of your physician
or qualified healthcare provider. Always seek their advice with any questions you may have regarding
your medical condition or health.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
4
How eating became unhealthy
Humans did not evolve to eat and snack continuously; this is highly maladaptive human behavior. (1, 2)
Data suggests that people in Western cultures spend about 12-14 hours a day eating and snacking. Over
80% of what gets eaten is not even real food — it is highly processed food. (1, 2) Contrast this to our
Paleolithic ancestors, who ate real, unprocessed food once or twice a day and you begin to see the
problem.
To be honest, one does not need to stretch that far back in history to see the contrast. Highly processed
food as a commercial product did not appear until as recently as the 19
th
century. Is it any wonder that
we are now seeing epidemic levels of obesity, metabolic syndrome, type II diabetes, cancer, cardiac
disease, neurodegenerative disease, and autoimmune disease?
One of the most important interventions to reduce these disorders is to eat real, not processed, food in
the right amounts at the right time.
How do you know the difference between real food and processed food? It is quite simple, really. If it
looks like food, it is food. If it comes in a box or has a food label, it’s likely processed.
The more ingredients listed on a product’s label and the more chemicals you see with strange and
unpronounceable names, the more processing the product has undergone.
Figure 1: Real vs Processed food (Source: FLCCC)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
5
The primary focus of this guide is on fasting, which is the time we spend not eating. Still, it is critical to
understand what we should eat, what we should not eat, when and where we should eat, and what
happens inside our bodies when we do eat (as well as what happens when we don’t eat).
What do fasting and time-restricted eating mean?
Fasting, by definition, means abstaining from eating. So technically any time you are not eating a meal,
you are fasting.
Time-restricted eating is a type of fasting where food intake is limited to a short window during the day
(1 to 8 hours), with only fluids such as water, tea, or coffee for the rest of the day. Intermittent fasting
usually involves a longer period of fasting; the most common is alternative day fasting (24-hour fast,
followed by a 24-hour eating window). However, many people fast for several days (3-7 days, or up to
14 days) followed by slow refeeding.
Time-restricted eating and intermittent fasting have many metabolic, cellular, and immunologic
benefits. (3-17) It is important to emphasize that intermittent fasting/time-restricted eating are not
synonymous with starvation; people who fast eat nutrient-dense food. Intermittent fasting does not
activate starvation metabolic pathways.
For example, when the body is starving, it decreases the basal metabolic rate (BMR) and growth
hormone (GH) levels to try to conserve energy and limit growth. Intermittent fasting, on the other hand,
increases BMR and GH. This may explain why diets that advocate the traditional approach of ‘eat fewer
calories and exercise more’ fail most of the time.
While a sporadic 24-hour fast (once a week or less frequently) is an efficient way to lose weight and
potentiate the benefits of time-restricted eating, this is difficult for many individuals to accomplish.
Therefore, we suggest time-restricted feeding as a lasting lifestyle intervention to promote health,
reduce disease burden, slow aging, prevent neurodegenerative disease, prevent cardiovascular disease,
and prevent cancer.
Figure 2: Mark Twain on ‘starvation’ (Source: FLCCC)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
6
Intermittent fasting is the most effective method to achieve sustained weight loss (one should aim for a
healthy weight). In addition, intermittent fasting has a profound effect on promoting immune system
homeostasis, partly by stimulating the clearing of damaged cells (autophagy), damaged mitochondria
(mitophagy), and misfolded and foreign proteins. Fasting improves mitochondrial health and increases
stem cell production. Intermittent fasting is the most effective therapy for the treatment of insulin
resistance, metabolic syndrome, and type II diabetes. In addition, Intermittent fasting has additional
benefits in prolonging health span, curing or alleviating the symptoms of many chronic diseases, as well
as preventing cardiovascular disease, neurodegenerative diseases (Alzheimer’s disease), and cancer. (3-
17)
The metabolic effects of intermittent fasting are numerous and include
decreasing blood glucose levels, increasing insulin sensitivity, decreasing
insulin levels, decreasing insulin-like growth factor, activating the sirtuin
pathway, and activating autophagy. Intermittent fasting is the most
effective means of activating autophagy and accounts for many of its
beneficial effects.
Autophagy and intermittent fasting
The 2016 Nobel Prize in Physiology or Medicine was awarded to Yoshinori Ohsumi for his initial
description of the morphological and molecular mechanisms of autophagy in the 1990s. (18, 19)
Let’s get a little scientific for a minute: Autophagy is an evolutionarily conserved lysosomal catabolic
process by which cells degrade and recycle intracellular endogenous (damaged organelles, misfolded or
mutant proteins, and macromolecules) and exogenous (viruses and bacteria) components to maintain
cellular homeostasis. (20-22) Dysfunctional autophagy contributes to many diseases, including cancer
and neurodegenerative diseases.
The specificity of the cargo and the delivery route to lysosomes distinguishes the three major types of
autophagy. Microautophagy involves the direct engulfment of cargo in endosomal/lysosomal membrane
invaginations. Chaperone-mediated autophagy (CMA) recycles soluble proteins with an exposed amino
acid motif that is recognized by the heat shock protein hsc70; these proteins are internalized by binding
to lysosomal receptors. (23)
Macroautophagy (henceforth referred to as autophagy) is the best-characterized process; in this
process, cytoplasmic constituents are engulfed within double-membrane vesicles called
autophagosomes, which subsequently fuse with lysosomes to form autolysosomes, where the cargo are
degraded or recycled. Autophagy occurs at basal levels under physiological conditions and can also be
upregulated in response to stressful stimuli such as hypoxia, nutritional deprivation, DNA damage, and
cytotoxic agents. (6) The molecular machinery that mediates the autophagic process is evolutionarily
conserved in higher eukaryotes and regulated by specific genes (ATG genes), which were initially
characterized in yeast.
To read more about the
metabolic theory of
cancer prevention and
treatment, see
Cancer Care.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
7
Each stage is controlled by different protein complexes regulated by the activation or inactivation of
several stress-responsive pathways, such as those involving mammalian target of rapamycin (mTOR—
nutrient), AMP-activated protein kinase (AMPK—energy) and hypoxia inducible factors (HIFs—stress).
(6)
Intermittent fasting is the most effective means of activating autophagy and accounts for many of its
beneficial effects. Additional activators of autophagy include resveratrol (a naturally occurring
phytochemical found in grapes, berries, wines, pistachio, etc.), spermidine (a naturally occurring
polyamine found in wheat germ, mushrooms, grapefruit, etc.), ivermectin, melatonin, coffee, and red
light/near infra-red radiation.
Healthy eating
What happens when we eat: all about insulin and insulin resistance
Before we get into the details of how to safely and effectively fast, let’s talk about what happens when
we eat.
When we eat or drink foods containing carbohydrates, the body breaks these down into glucose (a type
of sugar) that then enters the bloodstream. As blood sugar rises, the pancreas makes insulin, a hormone
that moves glucose into our cells, which use it for energy. When the body doesn’t have enough
carbohydrates to burn energy it burns fat instead, producing something called ketones, which it then
uses for fuel.
Figure 3: Autophagy pathway (Source: Dr. Mobeen Syed)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
8
As we gain weight, our bodies become less sensitive to insulin. ‘Insulin
resistance’ happens when cells in muscles, fat, and liver don’t respond
well to insulin and cannot use glucose from the blood for energy. The
pancreas then makes more insulin, which causes blood sugar levels to
rise and can lead to type II diabetes.
The glycemic index
The glycemic index is a value assigned to foods based on how quickly those foods increase blood glucose
levels and how high those levels spike. The glycemic index ranks food on a scale from 0 to 100. Pure
glucose is arbitrarily given a value of 100, which represents the relative rise in the blood glucose level
after two hours. The glycemic index of a specific food depends primarily on the quantity and type of
carbohydrate it contains.
Foods that are low on the glycemic index (GI) scale tend to release glucose slowly and steadily. Foods
that are high on the glycemic index release glucose rapidly.
It should be noted that the glycemic index varies from person to person. (24, 25) A continuous glucose
monitor allows for the individual assessment of the glycemic index of various foods.
Figure 4: The blood glucose profile of high and low glycemic index foods (Source: adapted from
Glycemic Index Foundation)
To read more about
insulin resistance and
how to correct it, see
I-CARE: Insulin
Resistance.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
9
Flattening the glucose curve
Time-restricted eating and carbohydrate restriction/ketogenic diet are good ways to reduce spikes in
glucose. But there are many other simple interventions to prevent high glucose spikes. In her book
Glucose Revolution, Jessie Inchauspe (aka “the Glucose Goddess”) describes many of these “hacks.” (26)
Her first recommendation is to eat food in the right order to slow gastric emptying and reduce the
breakdown and absorption of glucose. We often begin a meal with bread, which is exactly the wrong
way around. It is better to begin with greens and fiber, then protein and fat and then if you must eat
starchy foods, make sure they include fiber and make them the last thing you eat. Eat fruit after a meal
and always make sure it is preceded by fiber.
Figure 5: The glycemic index of certain foods (Source: FLCCC)
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
10
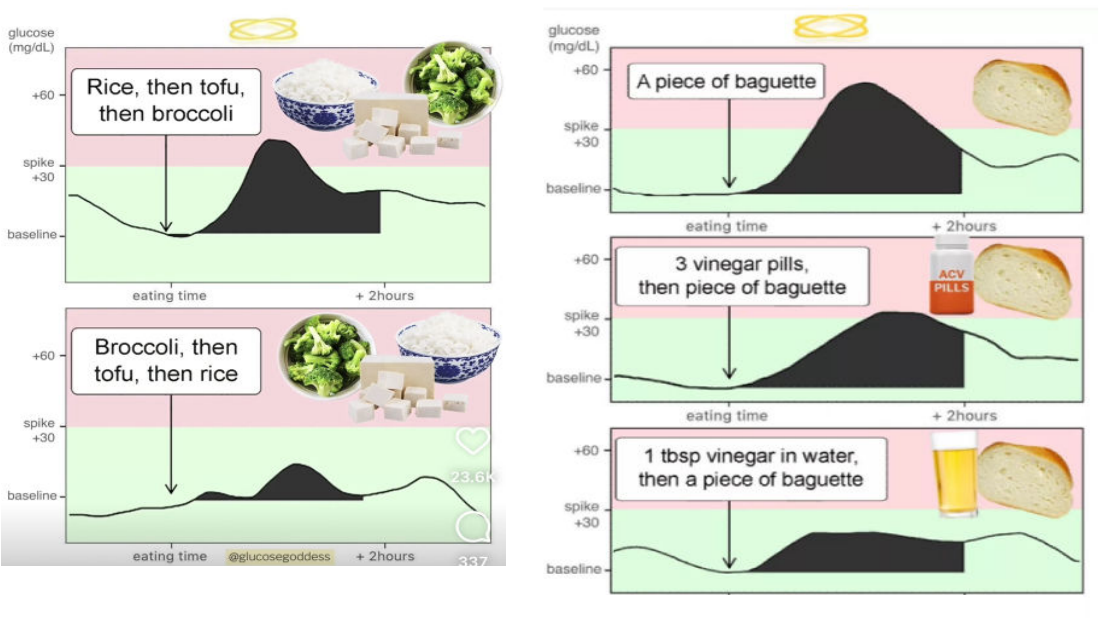
Here’s what that looks like visualized:
Another suggestion is to drink a tablespoon of vinegar (apple cider vinegar, preferably) stirred into a tall
glass of water before eating starch or something sweet. Vinegar, which contains acetic acid, decreases
the glucose spike as well as the release of insulin. Vinegar decreases the enzymatic breakdown of starch,
increases glycogen synthesis (and glucose uptake), and increases fatty acid oxidation. (27-30) Vinegar
may be beneficial even if consumed up to 20 minutes after a starchy food. Note that apple cider vinegar
is usually unpasteurized and should be avoided during pregnancy. If vinegar is not readily available, try
consuming a few fiber tablets (esp. glucomannan tablets) prior to eating a starchy or sweet treat. This
should flatten the curve.
Finally, make sure you move after you eat. Go for a 20-minute walk within an hour of eating (especially
starchy food). During exercise, muscles take up glucose for energy while increasing mitochondrial
oxidative capacity. (31-33) This is a very effective method to flatten the curve.
Going to the gym or doing resistance exercises is an alternative. If you’re at the office, climb a few stairs.
If you’re largely sedentary, try doing sitting calf raises (look up “soleus pushups”). This simple act of
raising the heel and contracting the calf, which resembles walking, has been demonstrated to reduce
glucose after a meal by about 50%, reduce hyperinsulinemia, and improve lipid metabolism. (34)
When you exercise in a fasting state (exercising when you have not eaten), your liver releases glucose
into the bloodstream to fuel the mitochondria in your muscles; this causes a glucose spike. This is
mediated by increased release of cortisol, epinephrine, and norepinephrine (with decreased glucagon);
i.e., the release of harmful stress hormones. If you exercise prior to eating, we would suggest a shake
Figure 6: Eating food in the right order (Source: Jesse Inchauspe)
Figure 7: Add vinegar before starch (Source: Jesse Inchauspe)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
11
containing powerful superfoods such as plant protein, super green, Omega-3 fatty acids, vitamins and
adaptogenic herbs, probiotics, and fiber, super mushrooms and berries (e.g. Ka’Chava ™
https://www.kachava.com/ and 310 Shakes™ https://310nutrition.com/). This is preferred to a regular
protein shake.
A couple of other things to note:
• Avoid fruit juices and smoothies, which cause a large glucose spike.
• Despite what your mother told you, it is good to skip breakfast. If you do eat breakfast, avoid
sugar, starches, and cereal, which all cause a rapid spike in glucose.
• Avoid snacking throughout the day.
Why your gut microbiome matters
The trillions of bacteria, fungi, and other microscopic organisms that live and work in your intestinal
system are commonly referred to as your “gut microbiome”. These organisms help us digest our food,
control our immune system, and even manage our brain function.
The microbiome affects blood sugar levels and insulin sensitivity too. (35-41) That is why establishing a
healthy microbiome is important for regulating blood glucose levels and ensuring our bodies are
appropriately sensitive to insulin. Some ways to establish a “normal” microbiome include:
Eating a diverse range of foods, including lots of vegetables, legumes, and beans.
Eating fermented foods like yogurt, kefir, apple cider vinegar, kombucha, pickles, sauerkraut,
tempeh, and kimchi.
Eating foods rich in polyphenols, like berries, coffee and tea, nuts and seeds, olives, and beans.
Red wine also has a high polyphenol content, as do resveratrol supplements.
Eating prebiotic fiber foods like chicory root, dandelion greens, asparagus, onions, and garlic.
Supplementation with galactomannan, a product made from the root of the konjac plant and
which contains both soluble and insoluble fiber, is an option.
Eating less sugar and sweeteners.
Reducing stress.
Avoiding unnecessary antibiotics.
Exercising regularly.
Spending time outdoors in the natural world to expose yourself to millions of microbes, many of
which can benefit microbiome diversity.
Getting enough sleep.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
12
Avoid distracted eating
You may not realize it, but where you eat also matters. Studies have shown that eating on the sofa or at
your desk can lead to excess weight gain because we are not as aware of how much we have eaten.
Researchers distinguish between ‘attentive’ and ‘distracted’ eating and have found that attentive eating
aids weight loss without the need for counting calories. (42)
Figure 8: It’s not just what you eat, but where you eat (Source: FLCCC)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
13
A brief guide to intermittent fasting/time-restricted
eating
Fasting is one of the best things you can do for your health. It’s a wonder more people are not doing it.
It’s simple, it’s free, it’s powerful, and it’s flexible. You can still enjoy life’s little pleasures. And it works
with any diet — whether you’re vegan, carnivore, low-carb, or follow a Mediterranean diet.
That said, a low-carbohydrate, high-fat diet is the optimum choice. (Saturated fats and Omega 3-fatty
acids are both healthy fats; don’t be fooled!) Just remember to eat real rather than processed foods,
avoid seemingly healthy foods that may be high in sugar (such as fruit juice), and keep your meals
diverse with lots of leafy greens and cruciferous vegetables (broccoli, cauliflower, cabbage, kale,
arugula, bok choy, etc.) Also, don’t eat (or snack) within 3-4 hours of going to bed. This limits autophagy
while sleeping, which is vital for brain health and glymphatic flow. Cut out snacking and get between 20
and 30 minutes of exercise (aerobic or resistance training) per day.
Benefits of intermittent fasting
Improves
insulin
sensitivity and
lowers blood
glucose
efficiently
Induces
autophagy,
weight loss,
and loss of
body fat
Decreases
inflammation
Increases
growth
hormone
(maintains lean
body mass)
Stabilizes or
increases basal
metabolic rate
Lowers blood
cholesterol
Improves
memory and
mental clarity
Reduces risk of
Alzheimer's
and other
neuro-
degenerative
diseases
Reverses aging
and prolongs
health span
Figure 9: Nine reasons to try intermittent fasting (Source: FLCCC)
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
14
How to get started
Preparing yourself mentally for intermittent fasting or time-restricted eating is half the battle. Don’t
calorie count or obsess about eating and food choices. Remember you will not be starving yourself or
severely restricting caloric intake.
There is pretty much an intermittent fasting plan that can be adapted and modified for any lifestyle.
Check out the 2016 book by Dr. Jason Fung, The Complete Guide to Fasting, for some excellent guidance
on approaches to intermittent fasting. (2)
Time-restricted eating seems to be a particularly effective and practical approach. For timed fasting,
begin slowly: start by allowing yourself a 12-hour eating window 5 days a week. This could mean eating
between 8:00 in the morning and 8:00 in the evening Monday through Friday. After a week or two,
reduce the eating window by an hour or two, and then start doing it 7 days a week. You should aim for
no more than an 8-hour eating window every day. This can be further shortened to 4 hours or less in
time.
The ideal goal is a 1-2 hour eating window, restricted to one meal a day. Timed fasting can be
interspersed with day-long, 36-hour, or 48-hour fasts.
Another approach is called “5:2 fasting”, which means you eat normally for 5 days and fast for 2 days by
restricting caloric intake to about 500 calories on those days. Alternative day fasting is another popular
technique, which entails taking in only liquids for a 24-hour period followed by a 24-hour eating period,
repeating this cycle indefinitely. Other people fast Monday, Tuesday, Wednesday, and Friday and eat
“normally” the other days.
Whatever approach you do, remember that the goal is to adopt this as a healthy, sustainable lifestyle so
think of it as a marathon, not a sprint. Set achievable goals and listen to your body. Avoid pills and
potions.
A continuous glucose monitor provides instant metabolic feedback and is strongly recommended when
first initiating time-restricted feeding and until metabolic stability is achieved (e.g., Abbott Freestyle
Libre 3). The glucose response to various foods is highly variable; a CGM allows an individual to
determine their glucose response to a particular food group (see section on glycemic index and
flattening the curve).
Remember, (almost) anyone can fast
Some people ask what they should do if they are unable to fast. In truth, there are only a few groups of
people who should avoid intermittent fasting. These include children under age 18, as it can impair their
growth, and people who are malnourished or underweight (BMI < 20). Women who are pregnant or
breastfeeding should also not try intermittent fasting. Some premenopausal women seem to be less
tolerant of time-restricted eating and should therefore restrict the eating window slowly (see section
below). Other approaches to intermittent fasting should probably be avoided in women.
If you have diabetes, gout, or serious underlying medical conditions, you should consult your primary
care physician before trying to fast, as changes in your medications and close monitoring may be
required.
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
15
Otherwise, humans have evolved over millions of years to be well-adapted to fasting. All humans can
fast; indeed, it is an integral component of many religious lifestyles. (43-45) People who have tried and
failed are likely severely insulin resistant and may be addicted to carbohydrates and sugar. Ironically,
fasting is the best remedy for these people. We suggest a slow and progressive approach to time-
restricted feeding; start by skipping breakfast and then slowly increase the time of your fasting window.
Dealing with hunger while fasting
First, remember that — like with everything — fasting becomes easier the more you do it. As you fast,
you will improve your insulin sensitivity and do away with the insulin spike that increases the feeling of
hunger. Ketosis, the state that occurs when the body starts burning fat instead of sugar, also reduces the
feeling of hunger; with prolonged fasting, you will stop feeling hungry.
Until you reach that state, try doing things like removing yourself from all food stimuli. Break the habit
of eating at specific times of the day. It is important to stay well-hydrated during fasting periods; drink
lots of water and/or an electrolyte solution. When you do eat, try to follow a ketogenic diet; ketones
suppress the appetite.
If you do feel hungry, try having a cup of protein-rich bone broth, tea, or coffee. Don’t add sugar though.
Instead try Stevia, which in itself has important metabolic benefits. (46) Make sure your stevia product
does not contain erythritol, which has been shown to increase cardiovascular complications. (47)
In his book Dr. Jason Fung recommends drinking coffee with added coconut oil (medium chain
triglycerides) or heavy cream and to avoid all carbohydrates and protein during fasting. (2) Remarkably,
caffeine stimulates autophagy, (48-50) while coconut oil has numerous health benefits. (51-53)
What to eat and what not eat
Healthy foods include (but are not limited to):
• All vegetables (especially avocado, cruciferous, and leafy vegetables)
• Nuts (almonds, brazil nuts, cashews, and pistachios)
• Peanut butter (but avoid the white bread and grape jelly!) and chia seeds.
• Fish (especially Alaskan salmon and sardines)
• Chicken breast (free range, no hormones, no antibiotics)
• Eggs (they’ve been giving a bad rap!)
• Meat (grass-fed, no hormones, avoid processed meats)
• Blueberries (limit volume if highly insulin resistant)
• Grapefruit (limit volume if highly insulin resistant). Note: Grapefruit juice decreases the activity
of the cytochrome P450 3A4 (CYP3A4) enzymes that are responsible for breaking down many
drugs and toxins. When grapefruit juice is consumed, the enzyme’s ability to break down the
drug for elimination is decreased. Blood levels of the drug may rise, resulting in a risk for new or
worsened side effects. Therefore, check interactions between grapefruit and the drugs you are
taking.
• Coffee with heavy cream or coconut oil; choose Stevia (without erythritol) over sugar or artificial
sweeteners.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
16
Say goodbye to:
• Donuts
• Bagels, bread, pretzels, tortillas
• Sweetened low-fat yogurt.
• Cereal bars
• Cookies, muffins, baked products
• Chips
• French fries
• Rice and pasta
• Potatoes
• Canned fruits/fruit juices
• Watermelon and bananas
• “Fake health foods”
Figure 10: Top 10 best foods (Source: FLCCC)

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
17
Healthy and unhealthy oils
Figure 11: Top 10 worst foods (Source: FLCCC)
Figure 12: Healthy and unhealthy cooking oils (Source: FLCCC)
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
18
When cooking, avoid seed oils high in linoleic acid. Linoleic acid is an essential Omega-6 fatty acid that
our bodies require in small amounts. Unfortunately, many people eat up to 10 times the desired amount
of linoleic acid, because of excess consumption of foods made with seed oils. Too much linoleic acid is
associated with inflammation, obesity, heart disease and other unfavorable conditions. Therefore,
avoid:
• Soybean oil
• Corn oil
• Cottonseed oil
• Sunflower oil
• Sesame oil
• Grapeseed oil
• Safflower oil
• Rice bran oil
• Margarine
Instead, opt for healthy oils and fats such as the ones listed below. Use only high-quality products and
check production and expiration dates.
• Olive oil (oleic acid, Omega-9 monounsaturated fatty acids); never heat olive oil to the point
where it produces smoke
• Avocado oil (oleic acid, Omega-9 monounsaturated fatty acids)
• Coconut oil (medium chain fatty acid)
• Flaxseed oil (alpha-linolenic acid, ALA Omega-3)
• Walnut and Pecan oils; these oils should be refrigerated to avoid spoilage
• Butter (saturated fat)
Fasting while on medication
Some medications are contraindicated with intermittent fasting. For example, proton pump inhibitors
(PPI), which reduce stomach acid, should be avoided as they block autophagy. Suddenly discontinuing a
PPI can cause rebound esophagitis, so an H2-blocker like famotidine or ranitidine may be an alternative.
An aloe vera stomach formula or diluted apple cider vinegar have been suggested as alternatives to a
PPI; however, there is limited data to support these interventions.
Hydroxychloroquine (HCQ), which is recommended in some COVID-19 protocols, can interfere with the
autophagy process and therefore may limit the benefits of intermittent fasting. Generally, it is fine to
continue taking vitamins and supplements while fasting and these do not break your fast.
Women and fasting
Several studies have suggested that intermittent fasting may not be as beneficial for pre-menopausal
women as it is for men. This is likely because calorie restriction in females is associated with changes in
the release of hypothalamic hormones, which may impact the menstrual cycle.
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
19
Why men and women respond differently to intermittent fasting
Women have different hormone profiles than men, and their hormones are constantly in flux.(54) While
men have a hormone profile that is relatively similar from day to day, women's hormones (at least until
after menopause) shift cyclically. The response to fasting differs depending on the day of their cycle.
Women may be more sensitive to changes in nutrient balance than men due to a molecule called
kisspeptin.(55) Kisspeptin controls an integral part of the reproductive pathway and is sensitive to
hormones like insulin and leptin, which regulate hunger and satiety. As women have higher levels of
kisspeptin, this may affect their ability to fast.
Women may respond differently to decreases in specific macronutrients, such as protein or
carbohydrates. If women do not eat adequate protein for their body weight and activity levels, the body
will sense that amino acids (the building blocks of protein) are low, which can negatively impact
estrogen binding and a hormone called insulin-like growth factor 1. Both are important for thickening
the lining of the uterus during the menstrual cycle.
For women to develop a fasting strategy, they need to understand the hormonal changes that occur
with the menstrual cycle.
The menstrual cycle
A menstrual cycle is determined by the number of days from the first day of one period to the first day
of the next. Day one of the menstrual cycle is the first full bleeding day of the period. A typical cycle is
approximately 24 to 35 days (on average, 28 days for most women). It is not abnormal for a woman’s
cycle to occasionally be shorter or longer.
The menstrual cycle occurs in three phases: follicular, ovulatory, and luteal. The first half of the cycle is
known as the follicular phase and the second half of the cycle is considered the luteal phase. Midway
through the cycle — between days 12 and 16 — ovulation occurs, and this is known as the ovulatory
phase.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
20
On Day 1 of the menstrual cycle, estrogen and progesterone levels are low. Low levels of estrogen and
progesterone signal the pituitary gland to produce Follicle Stimulating Hormone (FSH). FSH begins the
process of maturing a follicle (fluid-filled sac in the ovary containing an egg). The follicle produces more
estrogen to prepare the uterus for pregnancy. At ovulation, usually around day 12-14, increased
estrogen levels trigger a sharp rise in Luteinizing Hormone (LH) from the pituitary gland, causing the
release of the egg from the follicle. The ruptured follicle (corpus luteum) now secretes progesterone and
estrogen to continue to prepare the uterus for pregnancy. If the egg is not fertilized, estrogen and
progesterone levels drop and, on day 28, the menses begin.
Days 1-10 of the menstrual cycle are great days for fasting and eating a more keto or lower
carbohydrate diet. This is a hormonally resilient time. During days 1-7, there is a subsequent rise in
testosterone, which supports body mass. This is a great time for fat-burning and resistance training.
Right after ovulation, which varies around day 14, the body becomes less insulin-sensitive, and it is
therefore important to reduce complex carbohydrate intake as insulin sensitivity is at its lowest during
this phase. Consider intermittent fasting and following a lower complex carbohydrate diet while
increasing fiber, healthy fats, and protein.
The third and fourth weeks of the menstrual cycle are the luteal phase; post-ovulation. Here
progesterone levels are highest and metabolism changes yet again. Progesterone is a potent appetite
stimulant but slows digestion. This a great time to add green juicing, bone broths, increasing hydration,
and increasing fiber to keep bowel movements regular.
Week 4 is the final week of the luteal phase, when the body begins to build hormones to prepare for
menstruation. This is a great time to bring in healthy carbohydrates with a wide variety of vegetables
and grains to support menstruation.
Figure 13: Hormone levels and phases of the menstrual cycle (Source: Human Biology)
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
21
Fasting and the menstrual cycle
Although there are no comparable human studies, experiments in rats have shown that three to six
months of alternate-day fasting caused a reduction in ovary size and irregular reproductive cycles in
female rats. (56) Similarly, in a murine model, Kumar and Kaur demonstrated that intermittent fasting
negatively influences reproduction in young animals due to its adverse effects on the complete
hypothalamus-hypophysial-gonadal axis. (57) However, it should be noted that, in this study, the female
rats were very young (3 months old), which corresponds to a human aged 9 years old. (54) In addition,
rats have a much higher high basal metabolic rate than humans and are metabolically very different
from humans.
There is limited data on the changes in sex hormone levels and gonadotropins during fasting in humans.
In patients doing intermittent fasting during the Muslim observance of Ramadan (no eating from sunrise
to sunset for one month), Caglayan et al., measured the levels of FSH, LH, estradiol (E2), testosterone,
and prolactin (PRL) during and after the menstrual period. (43) In this study, the levels of these
hormones were not statistically different before and during fasting.
Chennaoui et al., did not observe any difference in testosterone and PRL levels before, during, and one
week after Ramadan in eight middle-distance athletes. (45) Similarly, Li et al., measured LH and FSH in
young women with obesity and polycystic ovarian syndrome (PCOS) followed by an 8-hour time-
restricted eating regimen for 5 weeks. (58) At the conclusion of the study, LH and FSH remained
unchanged. However, Heilbronn et al., reported that alternate-day fasting adversely affected glucose
tolerance in nonobese women but not in nonobese men. (59)
It is possible that alternate-day fasting results in greater disruption of the hypothalamus-hypophysial-
gonadal axis than does 8- to 12-hour time-restricted eating. In addition, the timing of time-restricted
eating may be important. Jakubowicz et al., demonstrated that a large meal later in the day (at dinner)
augmented estrogen levels in women with PCOS, as compared to eating earlier in the day. (14)
There are many anecdotal stories of women who have experienced changes to their menstrual cycles
after starting intermittent fasting (likely alternate-day or fasting for more than 24 hours). For this
reason, pre-menopausal women may need to follow a modified approach. (60)
The first step is to adopt healthy eating habits and reduce the intake of processed foods and high
carbohydrates; saturated fats, cholesterol-rich foods, and Omega-3 fatty acids are healthy fats. To
reduce any adverse effects, women should take a mild approach to fasting: shorter fasts and fewer
fasting days. We would suggest beginning a program of time-restricted eating consisting of fasting for 12
hours for two to three days a week and increasing from there. Furthermore, the fasting window should
begin at least 4 hours before going to sleep.
Fasting days should be nonconsecutive and spaced evenly across the week (for example, Monday,
Wednesday, and Friday).

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
22
With time, the fasting window can slowly (over weeks) be increased to 16 hours and the number of
fasting days per week increased; the increase in the duration and frequency of fasting should be based
on the individual woman’s response to fasting. It has been suggested that the cycle of intermittent
fasting be linked to the phases of the menstrual cycle (see table below). (60)
In women who follow a more conservative intermittent fasting regimen, the addition of resveratrol and
spermidine may augment autophagy. (61-65)
Table 1. An approach to fasting linked to phases of the menstrual cycle
Day Phase Type of Fast Type of Food Comment
1 – 10 Follicular 12-72 hours Keto Insulin sensitive;(66) Aerobic exercise
11-15 Ovulation 12-15 hours Keto Testosterone peaks; weight training
16-19 Early Luteal 12-72 hours Keto Declining hormones; less intense
exercise
20-bleed Late luteal No fasting Complex CHO Insulin resistant; less exercise-
walking, yoga
Source: Adapted from Fast Like a Girl (60)
Figure 14: A modified approach to fasting for pre-menopausal women (Source: Dr. Mobeen Syed)
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
23
Fasting during perimenopause and menopause
During perimenopause, hormone levels fluctuate because of fewer ovulations, which means less
progesterone is produced in the second half of the menstrual cycle. Periods can be erratic, skipped, or
heavy. Symptoms result from the change in the ratio of estrogen to progesterone, and the imbalance
creates the symptoms.
During menopause, estrogen is no longer produced by the ovaries and is made in smaller amounts by
the adrenal glands and in fat tissue. Estrogen is still produced in the body, but in lower amounts than in
younger, menstruating women.
The most significant hormone change of menopause is the lack of progesterone, creating a period of
estrogen dominance and low progesterone. Menopause is associated with low estrogen levels, insulin
resistance, and features of the “metabolic syndrome”; (66-69) therefore, intermittent fasting/time
restricted eating combined with a ketogenic diet may increase estrogen levels and “rebalance”
hormonal levels.
In addition, berberine (600 mg once or twice a day) is suggested, as this natural herb increases insulin
sensitivity, improves the lipid profile, and has beneficial effects on the microbiome. (70-73) Taking
melatonin (0.75-5 mg at night; extended-release tablets) is another promising strategy to manage
postmenopausal patients via restoring the osteoporosis-impaired osteogenic potential of bone marrow
mesenchymal stem cells. (74)
Increasing estrogen through diet and lifestyle
Certain behaviors and lifestyle adjustments can help address low estrogen levels:
• Aim for a healthy body weight: Being underweight is a risk factor for low hormone levels.
• Moderate exercise: Overexercising can contribute to low estrogen levels. Exercise in
moderation.
• Reduce stress: Too many stress hormones can cause the hormones that regulate your
reproductive system to become imbalanced. Incorporating stress-reduction techniques into
your daily routine is good for your overall well-being and your hormones, too. Engage in
pleasurable activities (intimacy, hugging, kissing, sex, etc.) to induce the release of oxytocin,
which decreases cortisol release and rebalances the hormonal profile.
• Get enough sleep: Sleep recharges your body so your hormones can function properly. On
average, adults need between seven and nine hours of sleep each night.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
24
Foods containing phytoestrogens
Phytoestrogens are plant-based estrogens. Some studies suggest that eating foods containing
phytoestrogens helps with menopause symptoms like hot flashes. Some phytoestrogens may help
promote heart health, bone health, and skin elasticity. More research is needed to know for sure.
Some foods that contain phytoestrogens include:
• Legumes (soybeans, lentils, chickpeas, peanuts). Consider soy isoflavones!(60 mg daily) (73) but
avoid in patients with a history of breast or ovarian cancer.
• Seeds (flaxseed, sunflower seed).
• Berries (strawberries, raspberries, blueberries).
• Fruits (plums, pears, apples, grapes, and berries).
Exercise and menopause
During menopause, when the body's estrogen levels decrease, bone loss can increase and calcium
absorption decreases. However, regular exercise can help support calcium absorption and reduce the
risk of osteoporosis. Here are some exercises that can help:
• Weight-bearing exercises: Weight-bearing exercises involve bearing your body weight through your
feet and legs, and they can help to build bone density and support calcium absorption. Examples
include walking, jogging, dancing, and weightlifting.
• Resistance training: Resistance training, such as weightlifting, can help to stimulate bone growth and
improve bone density. It can also help to increase muscle mass, which can support the bones and
reduce the risk of falls.
• Yoga and Pilates: Yoga and Pilates can help to improve balance, flexibility, and posture, which can
reduce the risk of falls and fractures.
• Outdoor activities: Getting outside and engaging in activities such as gardening, hiking, and cycling
can help to increase vitamin D levels, which is important for calcium absorption and bone health.
In addition to exercise, it's also important in menopause to maintain a healthy diet that includes
calcium-rich foods such as leafy green vegetables, nuts and seeds, and fortified foods. It's also important
to get enough Vitamin D, either through sun exposure or supplementation, as this helps the body absorb
calcium. Overall, regular exercise can have a positive impact on hormones, cortisol, and glucose levels,
leading to improved health and well-being.

A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
25
Learn more about intermittent fasting
READ
•
I-CARE Insulin Resistance: A Guide to Managing Insulin Resistance, Metabolic Syndrome, and Type II
Diabetes
• ‘The Complete Guide to Fasting’ by Dr. Jason Fung
• ‘The Real Meal Revolution’ by Dr. Tim Noakes
• How I Reversed Type II Diabetes by Dr. Paul Marik
WATCH
FLCCC videos
• Webinar:
Intermittent Fasting for Health
• Webinar: Intermittent Fasting for Women
• Long Story Short: How to Maximize Autophagy
• Long Story Short: Coffee Induces Autophagy
• Guide: How to Make Bulletproof Coffee
• Guide: Let’s Talk About Resveratrol
YouTube videos
• Amazing fasting benefits by Pradip Jamnadas, MD.
https://www.youtube.com/watch?v=RuOvn4UqznU
• Fasting for health and longevity with Dr. Jason Fung, MD.
https://www.youtube.com/watch?v=rQsMRjAwcFo
• Reversing Type 2 Diabetes by Jason Fung, MD. https://www.youtube.com/watch?v=6KS7M0s2fJM
• The 7 Important Intermittent Fasting Rules, Eric Berg, DC.
https://www.youtube.com/watch?v=l7s8K_CLOrs
• The MOST Important Intermittent Fasting Basics for Beginners, Eric Berg, DC.
https://www.youtube.com/watch?v=1rfzjRoalWM
• The COMPLETE GUIDE To Intermittent Fasting for WOMEN (How To Do It Correctly!) by Mindy Pelz,
DC.
https://www.youtube.com/watch?v=uIToWSXziWI
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
26
References
1. Lustig RH. Metabolical. The lure and lies of processed food, Nutrition and Modern Medicine:
Harper; 2021.
2. Fung J, Moore J. The complete guide to fasting: Victory Belt Publishing; 2016.
3. Akasheh RT, Kroeger CM, Trepanowski JF, Gabel K, Hoddy KK. Weight loss efficacy of alternative
day fasting versus daily calorie restriction in subjects with subclinical hypothyroidism: a
secondary analysis. Applied Physiology, Nutrition, & Metabolism. 2020;45.
4. Albosta M, Bakke J. Intermittent fasting: is there a role in the treatment of diabetes? A review of
the literature and guide for primary care physicians. Clinical Diabetes and Endocrinology.
2021;7:3.
5. Anson RM, Guo Z, de Cabo R, Lyun T, Rios M, Hagepanos A, et al. Intermittent fasting dissociates
beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury
from calorie intake. PNAS. 2003;100:6216-20.
6. Antures F, Erustes AG, Costa AJ, Nascimento AC, Bincoletto C, Ureshino RP, et al. Autophagy and
intermittent fasting: the connection for cancer therapy? Clinics. 2018;73 (Suppl 1):e814S.
7. Bhutani S, Klempel MC, Berger RA, Varady KA. Improvements in coronary heart disease risk
indicators by alternate-day fasting involve adipose tissue modulators. Obesity. 2010;18:2152-9.
8. Cho Y, Hong N, Kim KW, Cho SJ, Lee M, Lee YH, et al. The effectiveness of intermittent fasting to
reduce body mass index and glucose metabolism: A systematic review and meta-analysis. J. Clin.
Med. 2019;8:1645.
9. Clifton KK, Ma CX, Fontana L, Peterson LL. Intermittent fasting in the prevention and treatment
of cancer. CA Cancer J. Clin. 2021;71:527-46.
10. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N. Engl. J.
Med. 2019;381:2541-51.
11. de Toledo FW, Grundler F, Bergouigan A, Drinda S, Michalsen A. Safety, health improvement and
well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects.
PloS ONE. 2019;14:e0209353.
12. Harvie MN, Pegington M, Mattson MP, Dillon B, Evans G, Jebb SA. The effects of intermittent or
continuous energy restriction on weight loss and metabolic disease risk markers: a randomised
trial of young overweight women. Int. J. Obes. 2011;35:714-27.
13. Heilbronn LK, Smith SR, Martin CK, Anton SD. Alternate-day fasting in nonobese subjects: effects
on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 2006;81:69-73.
14. Jakubowicz D, Barnea M, Wainstein J, Froy O. Effects of caloric intake timing on insulin
resistance and hyperandrogenism in lean women with polycystic ovary syndrome. Clinical
Science. 2013;125:423-32.
15. Liu H, Javaheri A, Godar RJ, Murphy J, Ma X, Rohagi N, et al. Intermittent fasting preserves beta-
cell mass in obesity-induced diabetes via the autophagy-lysosome pathway. Autophagy.
2017;13:1952-68.
16. Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease
processes. Ageing Res. Rev. 2017;39:46-58.
17. Vasim I, Majeed CN, DeBoer MD. Intermittent fasting and metabolic health. Nutrients.
2022;14:631.
18. Takeshige K, Baba M, Tsuboi S, Noda T, Ohsumi Y. Autophagy in yeast demonstrated with
proteinase-deficient mutants and conditions for its induction. J. Cell. Biol. 1992;119:301-11.
19. Tsukada M, Ohsumi Y. Isolation and characterization of autophagy-defective mutants of
Saccharomyces cerevisiae. FEBS. 1993;333:169-74.
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
27
20. Mizushima N, Komatsu M. Autophagy: Renovation of cells and tissues. Cell. 2011;147:728-41.
21. Levine B, Klionsky DJ. Development by self-digestion: Molecular mechanisms and biological
function of autophagy. Developmental Cell. 2004;6:463-77.
22. Galluzzi L, Baehrecke EH, Ballabio A, Boya P, Cecconi F, Choi AM, et al. Molecular definitions of
autophagy and related processes. The EMBO Journal. 2017;36:1811-36.
23. Kaushik S, Cuervo AM. Chaperone-mediated autophagy: a unique way to enter the lysosome
world. Trends in Cell Biology. 2012;22:407-17.
24. Barclay AW, Augustin LS, Brighenti F, Delport E, Henry CJ, Sievenpiper JL, et al. Dietary glycaemic
index labelling: A global perspective. Nutrients. 2021;13:3244.
25. Matthan NR, Ausman LM, Meng H, Tighiouart H, Lichtenstein AH. Estimating the reliability of
glycemic index values and potential sources of methodological and biological variability. Am. J.
Clin. Nutr. 2016;104:1004-13.
26. Inchauspe J. Glucose Revolution. New York: Simon & Schuster; 2022.
27. Santos HO, de Moraes WM, da Silva GA, restes J, Schoenfeld BJ. Vinegar (acetic acid) intake on
glucose metabolism: A narrative review. Clinical Nutrition ESPEN. 2019;32:1-7.
28. Shishehbor F, Mansoori A, Shirani F. Vinegar consumption can attenuate postproandial glucose
and insulin responses: a systematic review and meta-analysis of clinical trials. Diabetes Research
and Clinical Practice. 2017;127:1-9.
29. Siddiqui FJ, Assam PN, de Souza NN, Sultana R, Dalan r, Chan ES. Diabetes control: Is vinegar a
promising candidate to help achieve targets?? Journal of Evidence-Based Integrative Medicine.
2018;23:1-12.
30. Petsiou EI, Mitrou PI, Raptis SA, Dimitriadis GD. Effect and mechanisms of action of vinegar on
glucose metabolism,lipid profile, and body weight. Nutrition Reviews. 2014;72:651-61.
31. Little JP, Gillen JB, Percival ME, Safdar A, Tarnopolsky MA, Punthakee Z, et al. Low-volume high-
intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in
patients with type 2 diabetes. Journal of Applied Physiology. 2011;111(6):1554-60.
32. Praet SF, Manders RJ, Lieverse AG, Kuipers H, Stehouwer CD, Keizer HA. Influence of acute
excercise on hyperglycemia in insulin-treated type-2 diabets. Medicine & Science in Sports &
Exercise. 2006(2037):2044.
33. Dipla K, Zafeiridis A, Mintziori G, Boutou AK, Goulis DG, Hackney AC. Exercise as a therapeutic
intervention in gestational diabetes mellitus. Endocrines. 2021;2:65-78.
34. Halilton MT, Hamilton D, Zderic TW. A potent physiological method to magnify and sustain
soleus oxidative metabolism improves glucose and lipid regulation. iScience. 2022;25:104869.
35. Yu EW, Gao L, Stastka P, Cheney MC, Soto MT, Ford CB, et al. Fecal microbiota transplantation
for the improvement of metabolism in obesity: The FMT-TRIM double-blind placebo-controlled
pilot trial. PloS ONE. 2020;17:e1003051.
36. Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BA, et al. Human
gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535:376-81.
37. Sung MM, Kim TT, Denou E, Soltys CL, Hamza SM, Byrne NJ, et al. Improved glucose homeostasis
in obese mice treated with resveratrol is associated with alterations in the gut microbiome.
Diabetes. 2017;66:418-25.
38. Nieuwdorp M, Gilijamse PW, Pai N, Kaplan LM. Role of the microbiome in energy regulation and
metabolism. Gastroenterology. 2014;146:1525-33.
39. Rebello CJ, Burton J, Heiman M, Greenway FL. Gastrointestinal microbiome modulator improves
glucose tolerance in overweight and obese subjects: A randomized controlled pilto trial. J.
Diabetes Complications. 2015;29:1272-6.
40. Maruvada P, Leone V, Kaplan LM, Chang EB. The human microbiome and obesity: Moving
beyond associations. Cell Host & Microbe. 2017;22:589-99.
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
28
41. Vallianou NG, Stratigou T, Tsagarakis S. Microbiome and diabetes: Where are we now? Diabetes
Research and Clinical Practice. 2018;146:111-8.
42. Robinson E, Aveyard P, Daley A, Jolly K, Lewis A, Lycett D, et al. Eating attentively: a systematic
review and meta-analysis of the effect of food intake memoery and awareness on eating. Am. J.
Clin. Nutr. 2013;97:728-42.
43. Caglayan EK, Goemen AY, Delibas N. Effects of long-term fasting on female hormone levels:
Ramadan model. Clin. Exp. Obst. & Gyn. 2014:17-9.
44. Chaouachi A, Leiper JB, Souissi N, Coutts AJ, Chamari K. Effects of Ramadan intermittent fasting
on sports performace and training: A review. International Journal of Sports Physiology and
Performance. 2009;4:419-34.
45. Chennaoui M, Desgorces F, Drogou C, Boudjemaa B, Tomaszewski A, Burnat P, et al. Effects of
Ramadan fasting on physical performance and metabolic, hormonal, and inflammatory
parameters in middle-distance runners. Appl. Physiol. Nutr. Metab. 2009;34:587-94.
46. Carrera-Lanestosa A, Moguel-Ordonez Y, Segura-Campos M. Stevia rebaudiana Bertoni: A
natural alternative for treating disease associated with metabolic syndrome. Journal of
Medicinal Food. 2017;20:933-43.
47. Witkowski M, Nemet I, Alamri H, Wilcox J, Gupta N, Nimer N, et al. The artificial sweetner
erythritol and cardiovascular event risk. Nature Medicine. 2023.
48. Pietrocola F, Malik SA, Marino G, Vacchelli E, Senovilla L, Chaba K, et al. Coffee induces
autophagy in vivo. Cell Cycle. 2014;13:1987-94.
49. Ray K. Caffeine is a potent stimulator of autophagy to reduce hepatic lipid content - a coffee for
NAFLD? Nature Reviews Gastroenterology & Hepatology. 2013;10:563.
50. Sinha RA, Farah BL, Singh BK, Siddique MM, Li Y, Wu Y, et al. Caffeine stimulates hepatic lipid
metabolism by the autophagy-lysosomal pathway in mice. Hepatology. 2014;59:1366-80.
51. Dacasin AB, Diagono DM, So PK, Bautista VR, Bucu ML, Bueno PR. The potential use of virgin
coconut oil as an adjunctive treatment for COVID-19: A review. Journal of Pharmacognosy and
Phytochemistry. 2021;10:37-49.
52. Teng M, Zhao YJ, Khoo AL, Yeo TC, Yong QW, Lim BP. Impact of coconut oil consumption on
cardiovascular health: a systematic review and meta-analysis. Nutrition Reviews. 2019;78:249-
59.
53. Santos HO, Howell S, Earnest CP, Teixeira FJ. Coconut oil intake and its effects on the
cardiometabolic profile - A structured literature review. Progress in Cardiovascular Diseases.
2019;62:436-43.
54. Cienfuegos S, Corapi S, Gabel K, Ezpeleta M, Kalam F, Lin S. Effects of intermittent fasting on
reproductive hormone levels in females and males: A review of human trials. Nutrients.
2022;14:2343.
55. Tng EL. Kisspeptin signalling and its roles in humans. Singapore Med J. 2015;56(12):649-56.
56. Martin B, Pearson M, Kebejian L, Golden E, Keselman A, Bender M. Sex-dependent metabolic,
neuroendocrine, and cognitive responses to dietary energy restriction and excess.
Endocrinology. 2007;148:4318-33.
57. Kumar S, Kaur G. Intermittent fasting dietary restriction regimen negatively influences
reproduction in young rats: A study of hypothalamo-hypophysial-gonadal axis. PloS ONE.
2013;8:e52416.
58. Li C, Xing C, Zhang J, Zhao H, Shi W, He B. Eight-hour time restricted feeding improves endocrine
and metabolic profiles in women with anovulatory polycystic ovary syndrome. J. Transl. Med.
2021;19:148.
A guide to intermittent fasting, time-restricted eating, and healthy habits (2023/12/11)
29
59. Heilbronn LK, Civitarese AE, Bogacka I, Smith SR, Hulver M, Ravussin E. Glucose tolerance and
skeletal muscle gene expression in response to alternate day fasting. Obesity Research.
2005;13:574-81.
60. Pelz M. Fast like a girl. Carlsbad, CA: Hay House; 2022.
61. Kou X, Chen N. Resveratrol and natural autophagy regulator for prevention and treatment of
Alzheimers disease. Nutrients. 2017;9:927.
62. Morselli E, Galluzzi L, Kepp O, Criollo A, Maiuri MC, Madeo F. Autophagy mediates
pharmacological lifespan extension by spermidine and resveratrol. Aging. 2009;1:961-70.
63. Morselli E, Marino G, Bennetzen MV, Eisenberg T, Megalou E, Schroeder S, et al. Spermidine and
resveratrol induce autophagy by distinct pathways converging on the acetylproteome. J. Cell.
Biol. 2022;192:615-29.
64. Park D, Jeong H, Lee MN, Koh A, Kwon O, Yang YR, et al. Resveratrol induces autophagy by
directly inhibiting mTOR through ATP competition. Scientific Reports. 2016;6:21772.
65. Tian Y, Song W, Li D, Cai L, Zhao Y. Resveratrol as a natural regulator of autophagy for
prevention and treatment of cancer. OncoTargets and Therapy. 2019;12:8601-9.
66. De Paoli M, Zakharia A, Werstuck GH. The role of estrogen in insulin resistance. A review of
clinical and preclinical data. Am. J. Pathol. 2021;191:1490-8.
67. Pu D, Tan R, Yu O, Wu J. Metabolic syndrome in menopause and associated factors: a meta-
analysis. Climacteric. 2017;20:583-91.
68. Christakis MK, Hasan H, De Souza LR, Lindsay S. The effect of menopause on metabolic
syndrome: cross-sectional results from the Canadian Longitudinal Study on aging. Menopause.
2020;27:999-1009.
69. Oya J, Nakagami T, Yamamoto Y, Fukushima S, Takeda M, Endo Y, et al. Effects of age on insulin
resistance and secretion in subjects without diabetes. Internal Medicine. 2014;53:941-7.
70. Yao Y, Chen H, Yan L, Wang W, Wang D. Berberine alleviates type 2 diabetic symptoms by
altering gut microbiota and reducing aromatic amino acids. Biomedicine & Pharmacotherapy.
2020;131:110669.
71. Fang Y, Zhang J, Zhu S, He M, Ma S, Jia Q, et al. Berberine ameliorates ovariectomy-induced
anxiety-like behaviors by enrichment in equol generating gut microbiota. Pharmacological
Research. 2021;163:105439.
72. Caliceti C, Rizzo P, Cicero AF. Potential benefits of berberine in the management of
perimenopausal syndrome. Oxidative Medicine and Cellular Longevity. 2015;2015:723093.
73. Cicero AF, Tartagni E, Ferroni A, De Sando V, Grandi E, Borghi C. Combined nutraceutical
approach to postmenopausal syndrome and vascular remodeling biomarkers. Journal of
Alternative & Complementary Medicine. 2013;19:582-7.
74. Zhou Y, Wang C, Si J, Wang B, Zhang D, Ding D, et al. Melatonin up-regulates bone marrow
mesenchymal stem cells osteogenic action but suppresses their mediated osteoclastogenesis via
MT(2) -inactivated NF-kB pathway. Br. J Pharmacol. 2020;177(9):2106-22.

