
1100 13th Street NW, Third Floor
Washington, DC 20005
phone 202.955.3500
fax 202.955.3599
www.ncqa.org
Better health care. Better choices. Better health.
October 1, 2018
Dear Colleague:
NCQA is pleased to present the HEDIS
®1
2019 Volume 2: Technical Update. With this release,
NCQA freezes the technical specifications for Volume 2, with the exception of measures that require
pharmacy data and the Risk Adjusted Utilization measures.
Measures that require pharmacy data and the Risk Adjusted Utilization measures will be final when
the Medication List Directory of National Drug Codes (NDC) and the risk-adjustment tables are
posted on November 1, 2018.
This memo contains the following information:
• Random Number (RAND) table for HEDIS 2019.
• Corrections, policy changes and clarifications to HEDIS 2019 Volume 2: Technical
Specifications.
• An announcement and attachments for the following measure specifications:
– Standardized Healthcare-Associated Infection Ratio (HAI).
– Adult Immunization Status (AIS).
– Prenatal Immunization Status (PRS).
– Plan All-Cause Readmissions 2020 Version (PCR2020).
The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, value sets and the Standard Infection Ratio (SIR)
table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.
Following release of the new AIS and PRS measures in the HEDIS 2019 Volume 2: Technical
Specifications, it was determined that additional clarifications were required. The updated versions
of the AIS (Attachment A) and PRS (Attachment B) measure specifications must be used for HEDIS
2019 reporting.
Following release of the draft PCR2020 measure in the HEDIS 2019 Volume 2: Technical
Specifications, it was determined that additional revisions were required for the risk adjustment
weighting for observation stays in the measure. The updated version of the measure specifications
(Attachment C) replaces the version in the HEDIS 2019 Volume 2: Technical Specifications. The
PCR2020 specification is a proposed version of the measure for HEDIS 2020 and will not be
reported in HEDIS 2019.
This memo does not contain changes to medications. Refer to the Medication List Directory
Technical Update document posted with the Medication List Directory (NDC codes) in November
for all medication changes.
1
HEDIS
®
is a registered trademark of the National Committee for Quality Assurance (NCQA).

Better health care. Better choices. Better health.
This memo does not contain coding changes. Organizations must go to the NCQA Download Center
(https://downloads.ncqa.org/customer/Login.aspx) and re-download the Value Set Directory (VSD)
to obtain the October 1 version, which contains all coding changes. The NCQA Download Center
does not list the VSD as “October 1 version” (in the Item Name column) but when organizations re-
download the file, they will see the updated version date. Refer to the Summary of Changes
spreadsheets in the VSD to identify codes and value sets that were added, deleted or revised.
This memo does not contain changes to the HEDIS 2019 Digital Measure Packages or the HEDIS
2019 Rules for Allowable Adjustments. Organizations must go to the NCQA Download Center
(https://downloads.ncqa.org/customer/Login.aspx) and re-download the digital measure packages
and the Rules for Allowable Adjustments to obtain the updated versions, which contain all changes
and adjustments for additional measures in the HEDIS measurement set. Refer to the Summary of
Changes section in the Rules for Allowable Adjustments document to identify revisions. The HEDIS
2019 Rules for Allowable Adjustments updated version will be posted on October 1 and the updated
version of the HEDIS 2019 Digital Measure Packages will be available in the Download Center on
October 2.
Review all items in the table and attachments and incorporate them into your implementation
processes. HEDIS Compliance Auditors will consider these documents to be part of the
specifications. If you have questions about information included in the Technical Update or about
other measure specifications, contact us through our Policy Clarification Support (PCS) system at
http://my.ncqa.org. We wish everyone a successful HEDIS data collection season!
Sincerely,
Cindy Ottone, MHA
Director, Policy-Measures
Enclosure

HEDIS
®
is a registered trademark of the National Committee for Quality Assurance (NCQA). The HEDIS measures and
specifications were developed by and are owned by NCQA. NCQA holds a copyright in the HEDIS measures and
specifications and may rescind or alter these measures and specifications at any time. Users of the HEDIS measures and
specifications shall not have the right to alter, enhance or otherwise modify the HEDIS measures and specifications, and
shall not disassemble, recompile or reverse engineer the HEDIS measures and specifications. Anyone desiring to use or
reproduce the materials, subject to licensed user restrictions, without modifications for an internal, non-commercial
purpose may do so without obtaining any approval from NCQA. Use of the Rules for Allowable Adjustments of HEDIS
to make permitted adjustments of the materials does not constitute a modification. All other uses, including a commercial
use, or any external reproduction, distribution and publication must be approved by NCQA and are subject to a license at
the discretion of NCQA.
No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical,
including photocopy, recording or any information storage and retrieval system, without the written permission of
NCQA.
HEDIS measures and specifications are not clinical guidelines, do not establish a standard of medical care and have not
been tested for all potential applications. The measures and specifications are provided “as is” without warranty of any
kind. NCQA makes no representations, warranties or endorsements about the quality of any product, test or protocol
identified as numerator compliant or otherwise identified as meeting the requirements of a HEDIS measure or
specification. NCQA also makes no representations, warranties or endorsements about the quality of any organization or
clinician who uses or reports performance measures. NCQA has no liability to anyone who relies on HEDIS measures
and specifications or data reflective of performance under such measures and specifications.
Calculated measure results, based on unadjusted HEDIS specifications, may not be termed “Health Plan HEDIS rates”
until they are audited and designated reportable by an NCQA-Certified Auditor. Such results should be referred to as
“Unaudited Health Plan HEDIS Rates.” Additionally, calculated measure results, based on adjusted HEDIS
specifications, may be called only “Uncertified, Unaudited HEDIS rates.” In this publication, “Heath Plan HEDIS rate”
refers to and assumes a result from unadjusted HEDIS specification that has been audited by an NCQA-Certified HEDIS
Auditor.
Limited proprietary coding is contained in the measure specifications for convenience. Users of the proprietary code sets
should obtain all necessary licenses from the owners of these code sets. NCQA disclaims all liability for use or accuracy
of any coding contained in the specifications.
The American Medical Association holds a copyright to the CPT
®
codes contained in the measures specifications.
The American Hospital Association holds a copyright to the Uniform Bill Codes (UB) contained in the measure
specifications. The UB Codes in the HEDIS specifications are included with the permission of the AHA. The UB Codes
contained in the HEDIS specifications may be used by health plans and other health care delivery organizations for the
purpose of calculating and reporting HEDIS measure results or using HEDIS measure results for their internal quality
improvement purposes. All other uses of the UB Codes require a license from the AHA. Anyone desiring to use the UB
Codes in a commercial Product(s) to generate HEDIS results, or for any other commercial use, must obtain a commercial
use license directly from the AHA. To inquire about licensing, contact ub04@healthforum.com
.
Some measure specifications contain coding from LOINC
®
(http://loinc.org). The LOINC table, LOINC codes, LOINC
panels and form file, LOINC linguistic variants file, LOINC/RSNA Radiology Playbook, and LOINC/IEEE Medical
Device Code Mapping Table are copyright © 1995–2018, Regenstrief Institute, Inc. and the Logical Observation
Identifiers Names and Codes (LOINC) Committee and is available at no cost under the license at
http://loinc.org/terms-
of-use.
“SNOMED” and “SNOMED CT” are registered trademarks of the International Health Terminology Standards
Development Organisation (IHTSDO).
“HL7” is the registered trademark of Health Level Seven International.
© 2018 by the National Committee for Quality Assurance, all rights reserved.

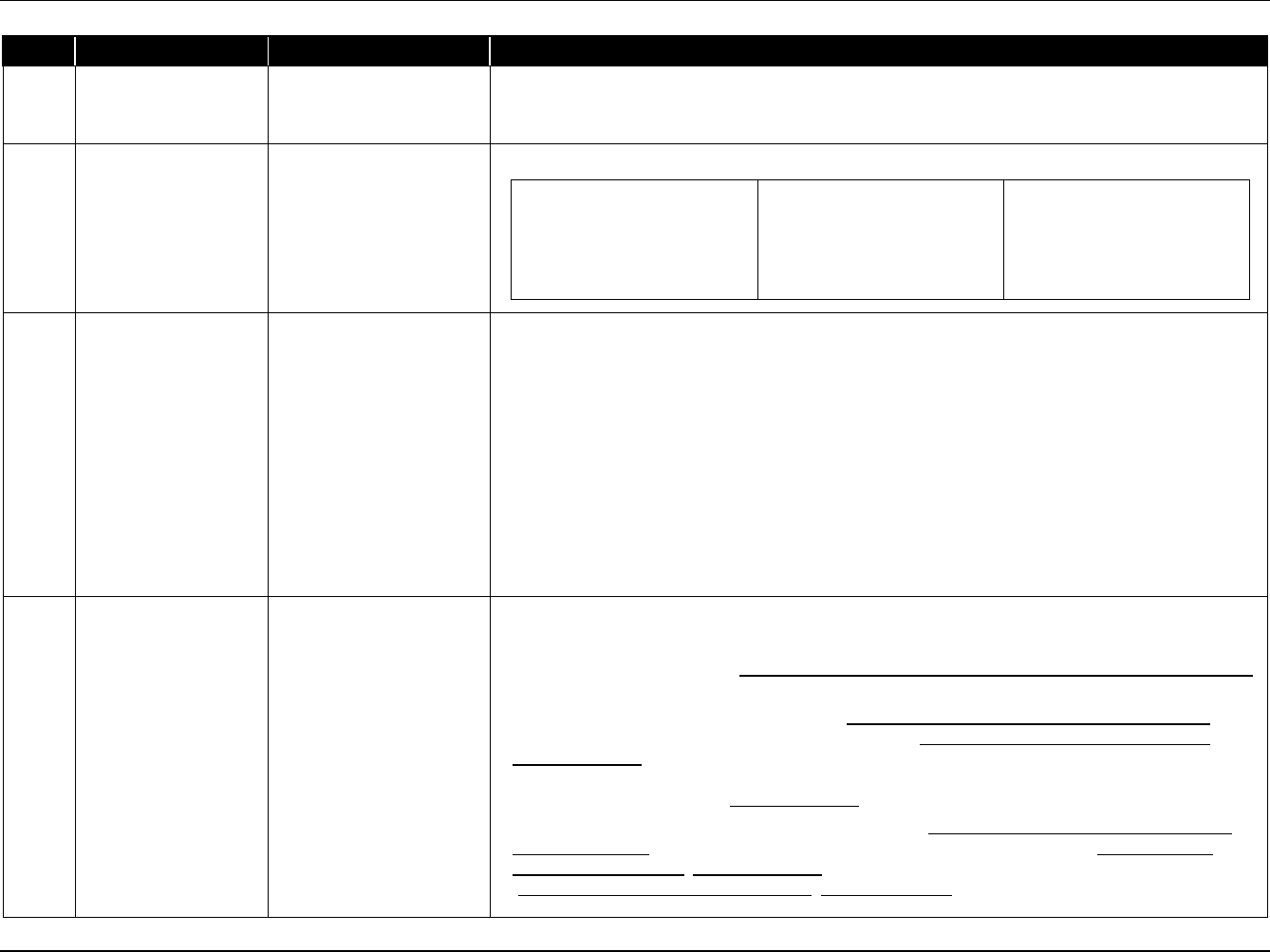
RAND Table for Measures Using the Hybrid Method
HEDIS 2019 Volume 2 Technical Update October 1, 2018
RAND Table for Measures Using the Hybrid Method
Measure RAND
Adult BMI Assessment .48
Weight Assessment and Counseling for Nutrition and Physical Activity
for Children/Adolescents
.35
Childhood Immunization Status and Lead Screening in Children .42*
Immunizations for Adolescents .08
Cervical Cancer Screening .79
Colorectal Cancer Screening .26
Care for Older Adults .23
Controlling High Blood Pressure .20
Comprehensive Diabetes Care .31
Medication Reconciliation Post-Discharge and Transitions of Care .56*
Prenatal and Postpartum Care .03
Well-Child Visits in the First 15 Months of Life (Medicaid only) .75
Well-Child Visits in the Third, Fourth, Fifth and Sixth Years of Life
(Medicaid only)
.85
Adolescent Well-Care Visits (Medicaid only) .82
* The RANDs for these measures are the same. Organizations may choose to use the same sample for the two measures. If
organizations chose to use different samples for these measures a different Minimum Required Sample Size (MRSS) is used
in the sampling protocol.

Specification Updates 1
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Specification Updates
This document contains corrections, policy changes and clarifications to HEDIS
2019 Volume 2, Technical Specifications. NCQA has identified
the appropriate page number, measure/guideline and head/subtitle for each item.
Page
Measure/Guideline
Head/Subtitle
Update
Table of Contents Utilization and Risk
Adjusted Utilization—
Utilization
Add the following text as a Note under the HAI measure:
Note: The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, the value sets and the Standard Infection Ratio
(SIR) table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.
3
What’s New in Volume
2
HAI SIR table Replace the text in this section with the following text:
The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, the value sets and the Standard Infection Ratio
(SIR) table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.
3 What’s New in Volume
2
First-year measure
evaluation
Replace the text in this section with the following text:
The following HEDIS 2018 first-year measures will be publicly reported for HEDIS 2019:
• Transitions of Care.
• Follow-Up After Emergency Department Visit for People With Multiple High-Risk Chronic Conditions.
• Use of Opioids at High Dosage.
• Use of Opioids from Multiple Providers.
The following HEDIS 2018 first-year status measures will be publicly reported for HEDIS 2019:
• Acute Hospital Utilization.
• Hospitalization for Potentially Preventable Complications.
Note
• The Depression Screening and Follow-Up for Adolescents and Adults and Unhealthy Alcohol Use
Screening and Follow-Up measures will not be publicly reported for HEDIS 2019.
17 The NCQA HEDIS
Compliance Audit™
The NCQA HEDIS
Compliance Audit™
Replace the last sentence in the first paragraph with the following text:
Calculated measure results, based on unadjusted HEDIS specifications, may not be termed “Health Plan
HEDIS rates” until they are audited and designated reportable by an NCQA-Certified Auditor. Such
results should be referred to as “Unaudited Health Plan HEDIS Rates.”

Specification Updates 2
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
19 General Guideline 9 Audit Preparation Replace the “By April 17” task in the sixth row in the HEDIS Audit Timeline with the following text:
Organization submits preliminary rates to the auditor for review. Auditors should
review preliminary rates based on the current year’s specifications.
By April 17
20 General Guideline 10
Reporting—Audit Results:
For Performance Measures
In the “NA” row, replace the text in the “Comment” column with the following text:
Small Denominator. The organization followed the specifications, but the denominator was too small
(e.g., <30) to report a valid rate.
a. For EOC and EOC-like measures, when the denominator is fewer than 30.
b. For utilization measures that count member months, when the denominator is fewer than 360
member months.
c. For all risk-adjusted utilization measures, except PCR and HPC, when the denominator is fewer
than 150.*
20 General Guideline 10
Reporting—Audit Results:
For Performance Measures
In the “UN” row replace the third sentence in the “Comment” column with the following text:
This result applies only to a limited set of measures (i.e., Board Certification).
28 General Guideline 30 Supplemental data—
Supplemental data uses—
Supplemental data may
help determine
Remove the bullet that reads:
• Observed Events in the Risk Adjusted Utilization measures.
30 General Guideline 30
Supplemental data—
Supplemental Data
Definitions—Standard
supplemental data
Replace the Note in this section with the following text:
Note: Prior year’s validated historic hybrid medical record result files are reviewed as part of the Data
Preproduction Processing section of the HEDIS Roadmap. These data are loaded as administrative data.
31 General Guideline 30 Supplemental data—
Required Data Elements—
Nonstandard supplemental
data
In the fourth paragraph replace the last sentence, which reads, “NPI or TIN along with date would also be
acceptable,” with “Documentation of NPI/TIN is not required; however, documentation of NPI/TIN along
with date, name and signature is preferred.”
32 General Guideline 30 Supplemental data—
Supplemental Data Timeline
and Systematic Sample
Requirements
In the third paragraph, replace the reference to “General Guideline 30” with “General Guideline 31.”
32 General Guideline 30
Supplemental data—
Identifying and Validating
Supplemental Data
Add the following text as a fourth paragraph after the third paragraph:
For additional information about audit requirements for supplemental data, refer to Volume 5, HEDIS
Compliance Audit: Standards, Policies and Procedures, released each October.*

Specification Updates 3
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
*This edit applies to the printed publication of the Volume 2 Technical Specifications. This language is
included in the e-pub.
33 General Guideline 31
Obtaining Information for
the Systematic Sample
In the second paragraph, remove the following two sentences, “All services must have evidence of
accountability by the practitioner and at a minimum include date, name and signature). NPI or TIN along
with date would also be acceptable.”
34 General Guideline 33 Date Specificity
In the first paragraph, replace the references of “February 5, 2015” with “February 5, 2016“ and replace
the reference to “February 2017” with “February 2018.”
35 General Guideline 35 Collecting Data for
Measures with Multiple
Numerator events
Remove the bullet that reads:
• Adult Immunization Status.
37 General Guideline 40 Coding Systems Included in
HEDIS Value Sets*
Remove the bullet that reads:
•
Medicare Severity Diagnosis-Related Group (MS-DRG).
37 General Guideline 40 Coding Systems Included in
HEDIS Value Sets*
Replace the asterisked language (at the end of the general guideline) with the following text:
* The updates to the International Classification of Diseases diagnosis and procedure codes that go into
effect on October 1, 2018, have been incorporated into the HEDIS 2019 value sets.
39 General Guideline 48 Mapping Proprietary or
Other Codes
Replace the “SNOMED CT” and “RxNorm” bullets with the following text:
• SNOMED CT. Organizations can use the HEDIS Value Set Directory for Allowable Adjustments
(“HEDIS Adjustments VSD”) as a resource.
• RxNorm. Organizations can use the HEDIS Value Set Directory for Allowable Adjustments (“HEDIS
Adjustments VSD”) as a resource.
47 Guidelines for
Calculations and
Sampling
Guidelines for the Hybrid
Method-Table 1: Sample
Size Information for Hybrid
Measures
In the “Controlling High Blood Pressure” row, replace “Y” with “N” in the “Prior Year’s Rate May Be Used
to Reduce MY 2018 Sample Size
1
”
column.
47
Guidelines for
Calculations and
Sampling
Guidelines for the Hybrid
Method-Table 1: Sample
Size Information for Hybrid
Measures
In the “Medication Reconciliation Post-Discharge” row, replace “Y
5”
with “Y” in the “Prior Year’s Rate May
Be Used to Reduce MY 2018 Sample Size
1
”
column.
47 Guidelines for
Calculations and
Sampling
Guidelines for the Hybrid
Method-Table 1: Sample
Size Information for Hybrid
Measures
In the “Transitions of Care” row, replace “N
5
” with “Y
5”
in the “Prior Year’s Rate May Be Used to Reduce
MY 2018 Sample Size
1
”
column.

Specification Updates 4
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
47
Guidelines for
Calculations and
Sampling
Guidelines for the Hybrid
Method-Table 1: Sample
Size Information for Hybrid
Measures
Replace the text in the 5th footnote below the table with the following text:
If a separate sample from the Medication Reconciliation Post-Discharge measure is used for Transitions
of Care, the organization can reduce the sample based only on the prior year’s reported rate for the
lowest rate from all the indicators for Transitions of Care.
52 Guidelines for
Calculations and
Sampling
Example 3 Replace steps 4–6 with the following text:
• Step 4 Because 411 <436 ≤ (411 + 42), skip to step 8.
• Step 5 Skip this step.
• Step 6 Skip this step.
• Step 7 Skip this step.
• Step 8 Sort the list and choose the first 411 as the primary list. The remaining 25 members become the
oversample list*.
*Remember, members in the oversample are used only to replace members excluded from the sample.
58 Guidelines for
Effectiveness of Care
Measures
SES stratification Under the second paragraph, add the following text as a new bullet under the bullet that reads “Other:
Member has ESRD-only status or is assigned “9-none of the above”:
• Unknown: Member’s SES is unknown. May be >0 only for Puerto Rico plans, or if the auditor approved
a small number of unassigned members*.
58 Guidelines for
Effectiveness of Care
Measures
SES stratification Under the second paragraph, add the following text below the last bullet that reads “Total Medicare: Total
of all categories above”:
* Plans must work with auditors to uncover anomalies early (e.g., during preliminary rate review) and
attempt to resolve the cause. NCQA will use the findings from first-year reporting to determine any
necessary changes. Medicare members in Puerto Rico must be counted in the Unknown strata.
58 Guidelines for
Effectiveness of Care
Measures
SES stratification Replace the last three paragraphs with the following text:
Use the SES Stratification Logic table below to determine the member’s stratification using the last three
months of the continuous enrollment period. Use the file run date to determine the member’s stratification
in the last three months of the continuous enrollment period.
59 Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
In the “Strata” column, replace “LIS/DE only” with “LIS/DE.”
59 Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
In the “Strata” column, replace “Disability only” with “Disability.”
Specification Updates 5
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
59
Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
In the “Other” row replace the text in the “Rationale” column with the following text:
Counts ESRD and 9 (None of the above).
59 Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
Add the following row under the “Other” row in the table:
Unknown
Count members with no values
assigned in the Monthly
Membership Detail Data Files.
Subject to auditor review and
approval.
59 Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
Add the following text below the table:
Note:
• Members who enroll in Medicare in the last 2 months of the continuous enrollment period, but are
continuously enrolled for the measure, should be counted in either “Non-LIS/DE, Non-disability,”
“Disability,” “Other” or “Unknown” based on item 48 in the last month of their continuous enrollment
(these members will have less than 3 months of records in the Monthly Membership Detail Data File).
• If item 35:
– Has the same value in the last 3 months of continuous enrollment, use that value.
– Has the same value in 2 of the last 3 months of the continuous enrollment use that value.
– Has different values in each of the last 3 months of continuous enrollment, use the value in the last
month.
71 Childhood Immunization
Status
Administrative
Specification—Numerators,
MMR
Replace the text in this section with the following text:
Any of the following meet criteria:
• At least one MMR vaccination (Measles, Mumps and Rubella (MMR) Vaccine Administered Value Set)
on or between the child’s first and second birthdays.
• At least one measles and rubella vaccination (Measles/Rubella Vaccine Administered Value Set) and
at least one mumps vaccination or history of the illness (Mumps Vaccine Administered Value Set;
Mumps Value Set) on the same date of service or on different dates of service. Only count vaccinations
that are administered on or between the child’s first and second birthdays (e.g., “Vaccine Administered”
value sets). History of illness (Mumps Value Set) can occur on or before the child’s second birthday.
• At least one measles vaccination or history of the illness (Measles Vaccine Administered Value Set;
Measles Value Set) and at least one mumps vaccination or history of the illness (Mumps Vaccine
Administered Value Set; Mumps Value Set) and at least one rubella vaccination or history of the illness
(Rubella Vaccine Administered Value Set; Rubella Value Set) on the same date of service or on
different dates of service. Only count vaccinations that are administered on or between the child’s first

Specification Updates 6
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
and second birthdays (e.g., “Vaccine Administered” value sets). History of illness (Measles Value Set,
Mumps Value Set, Rubella Value Set) can occur on or before the child’s second birthday.
Note: General Guideline 35 (i.e., the 14-day rule) does not apply to MMR.
72 Childhood Immunization
Status
Administrative
Specification—Numerators,
VZV
Replace the text in this section with the following text:
Either of the following meets criteria:
• At least one VZV vaccination (Varicella Zoster (VZV) Vaccine Administered Value Set), with a date
of service on or between the child’s first and second birthdays.
• History of varicella zoster (e.g., chicken pox) illness (Varicella Zoster Value Set) on or before the
child’s second birthday.
72 Childhood Immunization
Status
Administrative
Specification—Numerators,
Hepatitis A
Replace the text in this section with the following text:
Either of the following meets criteria:
• At least one hepatitis A vaccination (Hepatitis A Vaccine Administered Value Set), with a date of
service on or between the child’s first and second birthdays.
• History of hepatitis A illness (Hepatitis A Value Set) on or before the child’s second birthday.
74 Childhood Immunization
Status
Hybrid Specification—
Numerators, Medical
Record
Add the following text as a new paragraph after the fourth paragraph:
Immunizations documented using a generic header (e.g., polio vaccine) or “IPV/OPV” can be counted as
evidence of IPV. The burden on organizations to substantiate the IPV antigen is excessive compared to a
risk associated with data integrity.
83
Breast Cancer
Screening
Eligible Population—
Stratification
Add the following text as a new bullet under the bullet that reads “Other”:
• Unknown.
83 Breast Cancer
Screening
Eligible Population—
Stratification
In the Note, replace the reference to “five” with “six.”
84
Breast Cancer
Screening
Exclusions Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.

Specification Updates 7
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
• Members 66 years of age and older as of December 31 of the measurement year (all product lines)
with frailty and advanced illness. Members must meet BOTH of the following frailty and advanced
illness criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
–
A dispensed dementia medication (Dementia Medications List).
85
Breast Cancer
Screening
Exclusion (optional)
Replace all references of “without a modifier” with “without a right, left or bilateral modifier (Right
Modifier Value Set, Left Modifier Value Set, Bilateral Modifier Value Set).”
86 Breast Cancer
Screening
Table BCS-3: Data
Elements for Breast Cancer
Screening
Replace all references to “Each of the 5 stratifications and total” with “Each of the 6 stratifications and
total.”
91 Colorectal Cancer
Screening
Eligible Population—
Stratification
Add the following text as a new bullet under the bullet that reads “Other”:
• Unknown.
91 Colorectal Cancer
Screening
Eligible Population—
Stratification
In the Note, replace the reference to “five” with “six.”
92
Colorectal Cancer
Screening
Exclusions Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66 years of age and older as of December 31 of the measurement year (all product lines)
with frailty and advanced illness. Members must meet BOTH of the following frailty and advanced
illness criteria to be excluded:

Specification Updates 8
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
–
A dispensed dementia medication (Dementia Medications List).
96
Colorectal Cancer
Screening
Table COL-3: Data
Elements for Colorectal
Cancer Screening
Replace all references to “Each of the 5 stratifications and total” with “Each of the 6 stratifications and
total.”
105 Care for Older Adults Hybrid Specification—
Numerators, Pain
Assessment, Medical
Record
Add the following text as a new paragraph after the dashes:
Do not include pain assessments performed in an acute inpatient setting.
116
Pharmacotherapy
Management of COPD
Exacerbation
Event/diagnosis—step 2
Replace the sentence “An acute inpatient discharge and ED visit on the same date are counted as two
COPD episodes.” with the following:
An acute inpatient discharge and ED visit on the same date are counted as one COPD episode (ED visits
that result in an inpatient stay are excluded in step 1).
126 Asthma Medication
Ratio
Event/diagnosis—Step 1 Remove the bullet in front of the following paragraph (this text is a separate paragraph under the
previous bullet):
Only three of the four visits may be a telehealth visit, a telephone visit or an online assessment. Identify
telehealth visits by the presence of a telehealth modifier (Telehealth Modifier Value Set) or the presence
of a telehealth POS code (Telehealth POS Value Set) associated with the outpatient visit. Use the code
combinations below to identify telephone visits and online assessments:
131 Controlling High Blood
Pressure
Eligible Population—
Exclusions
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
–
Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.

Specification Updates 9
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66–80 years of age as of December 31 of the measurement year (all product lines) with
frailty and advanced illness. Members must meet BOTH of the following frailty and advanced illness
criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
– A dispensed dementia medication (Dementia Medications List).
• Members 81 years of age and older as of December 31 of the measurement year (all product lines)
with frailty (Frailty Value Set) during the measurement year.
138 Persistence of Beta-
Blocker Treatment After
a Heart Attack
Eligible Population—
Exclusions
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66–80 years of age as of December 31 of the measurement year (all product lines) with
frailty and advanced illness. Members must meet BOTH of the following frailty and advanced illness
criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on

Specification Updates 10
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
– A dispensed dementia medication (Dementia Medications List).
• Members 81 years of age and older as of December 31 of the measurement year (all product lines)
with frailty (Frailty Value Set) during the measurement year.
144 Statin Therapy for
Patients With
Cardiovascular
Conditions
Event/diagnosis—
Step 3: Exclusions
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66 years of age and older as of December 31 of the measurement year (all product lines)
with frailty and advanced illness. Members must meet BOTH of the following frailty and advanced
illness criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
–
A dispensed dementia medication (Dementia Medications List).
146 Statin Therapy for
Patients With
Cardiovascular Disease
Eligible Population: Rate
2——Statin Adherence 80%
Replace the Note at the top of the section with the following text:
Note: Members in hospice are excluded from the eligible population. Refer to General Guideline 17:
Members in Hospice.
151
Comprehensive
Diabetes Care
Eligible Population—
Stratification
Add the following bullet under the bullet that reads “Other”:
• Unknown.

Specification Updates 11
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
151 Comprehensive
Diabetes Care
Eligible Population—
Stratification
• In the Note, replace the reference to “five” with “six.”
153 Comprehensive
Diabetes Care
Eligible Population—
Exclusions
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66 years of age and older as of December 31 of the measurement year (all product lines)
with frailty and advanced illness. Members must meet BOTH of the following frailty and advanced
illness criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
– A dispensed dementia medication (Dementia Medications List).
168 Comprehensive
Diabetes Care
Table CDC-3-B: Data
Elements for
Comprehensive Diabetes
Care: Eye Exam (Medicare
SES Stratifications only.
Report the Total Medicare
population in Table CDC-
1/2/3)
Replace all references to “Each of the 5 stratifications” with “Each of the 6 stratifications.”
173
Statin Therapy for
Patients With Diabetes
Eligible Population—Rate
1—Received Statin
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:

Specification Updates 12
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
Therapy—Step 3:
Exclusions
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66 years of age and older as of December 31 of the measurement year (all product lines)
with frailty and advanced illness. Members must meet BOTH of the following frailty and advanced
illness criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
–
A dispensed dementia medication (Dementia Medications List).
174 Statin Therapy for
Patients With Diabetes
Eligible Population—Rate
2—Statin Adherence 80%
Replace the Note at the top of the section with the following text:
Note: Members in hospice are excluded from the eligible population. Refer to General Guideline 17:
Members in Hospice.
179 Disease-Modifying Anti-
Rheumatic Drug
Therapy for Rheumatoid
Arthritis
Eligible Population—
Event/diagnosis
Replace the second paragraph with the following text:
Count a nonacute-to-nonacute direct transfer as two discharges only if both discharges have a diagnosis
of rheumatoid arthritis and different discharge dates.
179 Disease-Modifying Anti-
Rheumatic Drug
Therapy for Rheumatoid
Arthritis
Exclusions Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Medicare members 66 years of age and older as of December 31 of the measurement year who meet
either of the following:
–
Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.

Specification Updates 13
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 66–80 years of age as of December 31 of the measurement year (all product lines) with
frailty and advanced illness. Members must meet BOTH of the following frailty and advanced illness
criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
– A dispensed dementia medication (Dementia Medications List).
• Members 81 years of age and older as of December 31 of the measurement year (all product lines)
with frailty (Frailty Value Set) during the measurement year.
182 Osteoporosis
Management in Women
Who Had a Fracture
Definitions—Negative
Diagnosis History
Replace the fourth paragraph with the following text:
For inpatient stays that were a result of an ED or observation visit, use the date of the ED or observation
visit to determine Negative Diagnosis History.
184 Osteoporosis
Management in Women
Who Had a Fracture
Eligible Population—
Event/diagnosis—Step 5:
Exclusions
Replace the text in this section with the following text:
Exclude members who meet any of the following criteria:
Note: Supplemental and medical record data may not be used for these exclusions.
• Members 67 years of age and older as of December 31 of the measurement year who meet either of
the following:
– Enrolled in an Institutional SNP (I-SNP) any time during the measurement year.
– Living long-term in an institution any time during the measurement year as identified by the LTI flag
in the Monthly Membership Detail Data File. Use the run date of the file to determine if a member
had an LTI flag during the measurement year.
• Members 67–80 years of age as of December 31 of the measurement year (all product lines) with
frailty and advanced illness. Members must meet BOTH of the following frailty and advanced illness
criteria to be excluded:
1. At least one claim/encounter for frailty (Frailty Value Set) during the measurement year.

Specification Updates 14
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
2. Any of the following during the measurement year or the year prior to the measurement year (count
services that occur over both years):
– At least two outpatient visits (Outpatient Value Set), observation visits (Observation Value Set),
ED visits (ED Value Set) or nonacute inpatient encounters (Nonacute Inpatient Value Set) on
different dates of service, with an advanced illness diagnosis (Advanced Illness Value Set). Visit
type need not be the same for the two visits.
– At least one acute inpatient encounter (Acute Inpatient Value Set) with an advanced illness
diagnosis (Advanced Illness Value Set).
– A dispensed dementia medication (Dementia Medications List).
• Members 81 years of age and older as of December 31 of the measurement year (all product lines)
with frailty (Frailty Value Set) during the measurement year.
185 Osteoporosis
Management in Women
Who Had a Fracture
Administrative
Specification—Numerator,
Osteoporosis Medications
Replace the medication “Albandronate“ with “Abaloparatide” in the Other Agents row.
195 Follow-Up Care for
Children Prescribed
ADHD Medication
Eligible Population: Rate
2—C&M Phase
Replace the Note at the top of the section with the following text:
Note: Members in hospice are excluded from the eligible population. Refer to General Guideline 17:
Members in Hospice.
199 Follow-Up After
Hospitalization for
Mental Illness
Event/diagnosis—Acute
readmission or direct
transfer
In the third paragraph, replace the reference to “mental illness” with “mental health disorder.”
215 Diabetes Monitoring for
People With Diabetes
and Schizophrenia
Event/diagnosis—Step 1 Replace the dashed text that reads “electroconvulsive therapy” with the following text:
– Electroconvulsive therapy (Electroconvulsive Therapy Value Set) with any diagnosis of
schizophrenia or schizoaffective disorder (Schizophrenia Value Set).
216 Diabetes Monitoring for
People With Diabetes
and Schizophrenia
Event/diagnosis—Step 2 Remove the bullet in front of the following paragraphs (this text is two separate paragraphs under the
previous bullet):
Only include nonacute inpatient encounters (Nonacute Inpatient Value Set) without telehealth
(Telehealth Modifier Value Set; Telehealth POS Value Set).
Only one of the two visits may be a telehealth visit, a telephone visit or an online assessment. Identify
telehealth visits by the presence of a telehealth modifier (Telehealth Modifier Value Set) or the presence
of a telehealth POS code (Telehealth POS Value Set) associated with the outpatient visit. Use the code
combinations below to identify telephone visits and online assessments:
– A telephone visit (Telephone Visits Value Set) with any diagnosis of diabetes (Diabetes Value Set).
– An online assessment (Online Assessments Value Set) with any diagnosis of diabetes (Diabetes
Value Set).

Specification Updates 15
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
220
Cardiovascular
Monitoring for People
With Cardiovascular
Disease and
Schizophrenia
Event/diagnosis—Step 1
Replace the electroconvulsive therapy dash with the following text:
– Electroconvulsive therapy (Electroconvulsive Therapy Value Set) with any diagnosis of
schizophrenia or schizoaffective disorder (Schizophrenia Value Set).
224 Adherence to
Antipsychotic
Medications for
Individuals With
Schizophrenia
Event/diagnosis—Step 1
Replace the electroconvulsive therapy dash with the following text:
– Electroconvulsive therapy (Electroconvulsive Therapy Value Set) with any diagnosis of
schizophrenia or schizoaffective disorder (Schizophrenia Value Set).
242 Transitions of Care
Hybrid Specification—
Denominator
Replace the third paragraph with the following text:
Organizations that use the Hybrid Method to report the Medication Reconciliation Post Discharge and
Transition of Care measures may use the same sample for both measures. Organizations may reduce
the sample size based only on the prior year’s audited, product line-specific rate for the lowest rate of all
TRC rates and MRP rate.
If a separate sample from the MRP measure is used for TRC, organizations may reduce the sample
based only on the prior year’s audited, product line-specific rate for the lowest TRC indicator.
244 Transitions of Care
Hybrid Specification—
Numerators, Receipt of
Discharge Information,
Medical Record
Replace the fourth bullet with the following text:
• Current medication list.
253
Non-Recommended
Cervical Cancer
Screening in Adolescent
Females
Table NCS-1/2: Data
Elements for Non-
Recommended Cervical
Cancer Screening in
Adolescent Females
Remove the “Numerator events by supplemental data” row.
255 Non-Recommended
PSA-Based Screening
in Older Men
Table PSA-3: Data
Elements for Non-
Recommended PSA-Based
Screening in Older Men
Remove the “Numerator events by supplemental data” row.
259
Appropriate Treatment
for Children With Upper
Respiratory Infection
Table URI-1/2: Data
Elements for Appropriate
Treatment for Children With
Upper Respiratory Infection
Remove the “Numerator events by supplemental data” row.

Specification Updates 16
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
264 Avoidance of Antibiotic
Treatment in Adults
With Acute Bronchitis
Table AAB-1/2: Data
Elements for Avoidance of
Antibiotic Treatment in
Adults With Acute Bronchitis
Remove the “Numerator events by supplemental data” row.
268
Use of Imaging Studies
for Low Back Pain
Table LBP-1/2: Data
Elements for Use of
Imaging Studies for Low
Back Pain
Remove the “Numerator events by supplemental data” row.
278 Potentially Harmful
Drug-Disease
Interactions in the
Elderly
Table DDE-3: Data
Elements for Potentially
Harmful Drug-Disease
Interactions in the Elderly
Remove the “Numerator events by supplemental data” row.
283 Use of High-Risk
Medications in the
Elderly
Table DAE-3: Data
Elements for Use of High-
Risk Medications in the
Elderly
Remove the “Numerator events by supplemental data” row.
284 Use of Opioids at High
Dosage
Measure Description—Note Remove the second sentence, which reads:
The proportion will be calculated and displayed as a permillage (multiplied by 1,000) instead of a
percentage in reports.
287 Use of Opioids at High
Dosage
Table UOD-A: Opioid
Morphine Milligram
Equivalent Conversion
Factors
1
Remove the second footnote under the table, which reads:
MME conversion factor for buprenorphine patches is 12.6 based on the assumption that one milligram of
parenteral buprenorphine is equivalent to 75 milligrams of oral morphine and that one patch delivers the
dispensed micrograms per hour over a 24 hour day and remains in place for 7 days. Using the formula,
Strength per Unit * (Number of Units/ Days Supply) * MME conversion factor = MME/Day: 5 µg/hr.
buprenorphine patch * (4 patches/28 days) * 12.6 = 9 MME/day.
288
Use of Opioids at High
Dosage
Table UOD-1/2: Data
Elements for Use of Opioids
at High Dosage
Remove the “Numerator events by supplemental data” row.
289
Use of Opioids From
Multiple Providers
Measure Description—Note Remove the second sentence, which reads:
The proportion will be calculated and displayed as a permillage (multiplied by 1,000) instead of a
percentage in reports.

Specification Updates 17
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
292 Use of Opioids From
Multiple Providers
Table UOP-1/2: Data
Elements for Use of Opioids
From Multiple Providers
Remove the “Number events by supplemental data” row.
293 Risk of Continued
Opioid Use
Measure Definitions—IPSD Replace the second sentence of the definition with the following text:
The earliest prescription dispensing date for an opioid medication during the Intake Period.
295 Risk of Continued
Opioid Use
Table COU-1/2: Data
Elements for Risk of
Continued Opioid Use
Remove the “Number events by supplemental data” row.
295 Risk of Continued
Opioid Use
Data Elements for
Reporting
Replace the table name with the following text:
• Table COU-1/2/3: Data Elements for Risk of Continued Opioid Use
321 Initiation and
Engagement of AOD
Abuse or Dependence
Treatment
Initiation of AOD Treatment Replace the second paragraph with the following:
If the Index Episode was an inpatient discharge (or an ED/observation visit that resulted in an inpatient
stay), the inpatient stay is considered initiation of treatment and the member is compliant.
351
Well-Child Visits in the
First 15 Months of Life
Note Add the following as the third bullet under Mental Developmental History:
• Notation of “well-developed.”
355 Well-Child Visits in the
Third, Fourth, Fifth and
Sixth Years of Life
Note Add the following as the third bullet under Mental Developmental History:
• Notation of “well-developed.”
359 Adolescent Well-Care
Visits
Note Add the following as the third bullet under Mental Developmental History:
• Notation of “well-developed.”
384
Identification of Alcohol
and Other Drug
Services
Table IAD-1/2/3:
Identification of Alcohol and
other Drug Services
Replace all “MAT” references with “medication treatment.”
404
Standardized
Healthcare-Associated
Infection Ratio
Entire Measure
Specification
Remove the Definitions, Eligible Population, Calculations of Hospital Discharge Weight, Calculation of
Weighted Standardized Infection Ratios (SIR), and data elements sections in their entirety from the
measure specification. Replace the text in the Summary of Changes to HEDIS 2019 section with the
following text:
The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, value sets and the Standard Infection Ratio (SIR)
table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.

Specification Updates 18
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
410 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 1 In the first sentence replace the reference to “IHU” with “AHU.”
411 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5 Add the following text as a new bullet under the bullet that reads “Other”:
• Unknown: Member’s SES is unknown. May be >0 only for Puerto Rico plans, or if the auditor approved
a small number of unassigned members*.
411 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5 Add the following text below the last bullet:
*Plans must work with auditors to uncover anomalies early (e.g., during preliminary rate review) and
attempt to resolve the cause. NCQA will use the findings from first-year reporting to determine any
necessary changes. Medicare members in Puerto Rico must be counted in the Unknown strata.
411
Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5 Add the following text below the last bullet that reads “Total Medicare: Total of all categories above”:
Use the following SES Stratification Logic table below to determine the member’s stratification using the
last three months of the continuous enrollment period. Use the file run date to determine the member’s
stratification in the last three months of the continuous enrollment period.
412 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5—SES
Stratifications Logic
In the “Strata” column, replace “LIS/DE only” with “LIS/DE.”
412 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5—SES
Stratifications Logic
In the “Strata” column, replace “Disability only” with “Disability.”
412 Guidelines for
Effectiveness of Care
Measures
SES stratification—SES
Stratifications Logic
In the “Other” row, replace the text in the “Rationale” column with the following text:
Counts ESRD and 9 (None of the above).
412
Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5—SES
Stratifications Logic
Add the following row under the “Other” row in the table:
Unknown
Count members with no values
assigned in the Monthly
Membership Detail Data Files.
Subject to auditor review and
approval.
412 Guidelines for Risk
Adjusted Utilization
Measures
Guideline 5—SES
Stratifications Logic
Add the following text below the table:
Note:

Specification Updates 19
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
• Members who enroll in Medicare in the last 2 months of the continuous enrollment period, but are
continuously enrolled for the measure, should be counted in either “Non-LIS/DE, Non-disability,”
“Disability,” “Other” or “Unknown” based on item 48 in the last month of their continuous enrollment
(these members will have less than 3 months of records in the Monthly Membership Detail Data File).
• If item 35:
– Has the same value in the last 3 months of continuous enrollment, use that value.
– Has the same value in 2 of the last 3 months of the continuous enrollment, use that value.
– Has different values in each of the last 3 months of continuous enrollment, use the value in the last
month.
412 Guidelines for Risk
Adjusted Utilization
Measures
Utilization Risk Adjustment
Determination—Step 1
Add the following text as the last sentence in the third paragraph:
For the HFS measure, exclude the primary discharge diagnosis on the skilled nursing facility discharge
(SND) to the community.
417 Plan All-Cause
Readmissions
Eligible Population—
Stratification
Add the following text as a new bullet under the bullet that reads “Other”:
• Unknown.
417
Plan All-Cause
Readmissions
Eligible Population—
Stratification
In the Note, replace the reference to “five” with “six.”
422 Plan All-Cause
Readmissions
Administrative
Specification—Reporting:
SES Stratification (Medicare
only)
Add the following text as a new bullet under the bullet that reads “Other: Member has ESRD-only status
or is assigned ‘9-none of the above’”:
• Unknown: Member’s SES is unknown.
425 Plan All-Cause
Readmissions
Table PCR-B-3: Plan All-
Cause Readmissions Rates
by SES Stratification
(Medicare, 18-64)
Add the following row under the “Other” row:
Unknown
425
Plan All-Cause
Readmissions
Table PCR-D-3: Plan All-
Cause Readmissions Rates
by SES Stratification
(Medicare, 65+)
Add the following row under the “Other” row:
Unknown
425 Plan All-Cause
Readmissions
Table PCR-D-3: Plan All-
Cause Readmissions Rates
by SES Stratification
(Medicare, 65+)
In the asterisked text below the table, replace the reference to “Table PCR-B-3” with “Table PCR-C-3.”
Specification Updates 20
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
430
Hospitalization
Following Discharge
From a Skilled Nursing
Facility
Numerator—Step 1 Add the following text at the end of Step 1:
Note: Count each unique acute inpatient admission or observation stay hospitalization only once toward
the numerator, for the last denominator event.
If a single numerator event meets criteria for multiple denominator events, only count the last
denominator event. For example, consider the following events:
• SNF Stay 1: May 1–10.
• SNF Stay 2: May 15–25.
• Acute Inpatient Stay: May 30–June 5.
The SND of May 10 and May 25 are included as denominator events. The acute inpatient stay counts as
a numerator event only towards the last denominator event (Stay 2, May 15–25).
430 Hospitalization
Following Discharge
From a Skilled Nursing
Facility
Reporting: Count of
Expected Hospitalizations
Replace the text in this section with the following text:
Step 1 Calculate the number of expected inpatient admission or observation stay hospitalizations for
each age and total, for each category (30-day hospitalization, 60-day hospitalization).
Step 2 Round to four decimal places using the .5 rule and enter the Count of Expected Hospitalizations
into the reporting tables.
431 Hospitalization
Following Discharge
From a Skilled Nursing
Facility
Reporting: Variance
Replace the text in this section with the following text:
Step 1 Calculate the variance (from Risk Adjustment Weighting, step 8) for each age and overall total,
for each category (30-day hospitalization, 60-day hospitalization).
Step 2 Round to four decimal places using the .5 rule and enter the variance into the reporting tables.
439 Acute Hospital
Utilization
Expected count of
hospitalization—Step 5
Replace “Truncate the variance for reporting to 4 decimal places” to “Round the variance for reporting to
4 decimal places using the .5 rule” in the second paragraph.
439
Acute Hospital
Utilization
Expected count of
hospitalization—Step 5
Remove the Note.
441,
442,
443,
444
Acute Hospital
Utilization
Table AHU-A-2/3, Table
AHU-B-2/3, Table AHU-C-
2/3 and Table AHU-D-2/3
Replace the white shading with grey shading in the following rows for each cell in these rows:
• 18-64 Total Male
• 18-64 Total Female
• 65+ Total Male
• 65+ Total Female
447 Emergency Department
Utilization
Expected count of
hospitalization
Replace the section head that reads “Expected count of hospitalization” with “Expected Count of ED
Visits.”

Specification Updates 21
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
448
Emergency Department
Utilization
Risk Adjustment Weighting
and Calculation of Expected
Events—Step 5 and Step 6
Replace all references to “PPD” with “PPV” and all references to “PUCD” with “PUCV.”
448 Emergency Department
Utilization
Risk Adjustment Weighting
and Calculation of Expected
Events—Step 6
Replace the sentence that reads “Truncate the variance for reporting to 4 decimal places” with “Round
the variance for reporting to 4 decimal places using the .5 rule” in the second paragraph.
448 Emergency Department
Utilization
Risk Adjustment Weighting
and Calculation of Expected
Events—Step 6
Remove the Note.
449 Emergency Department
Utilization
Reporting: Variance Replace the reference to “PUCD” with “PUCV.”
458 Hospitalization for
Potentially Preventable
Complications
Risk Adjustment Weighting
and Calculation of Expected
Events—Step 5
Remove the Note.
492
Depression Screening
and Follow-Up for
Adolescents and Adults
Characteristics—
Stratification
Replace the second bullet with the following text:
• Product line: Commercial, Medicare, Medicaid.
493
Depression Screening
and Follow-Up for
Adolescents and Adults
Definitions–Depression
screening instruments,
Instruments for Adults (18+
years)
Remove the following rows:
Depression Scale (DEPS)** Total Score ≥9
Duke Anxiety-Depression Scale (DADS)
®
** Total Score ≥30
493 Depression Screening
and Follow-Up for
Adolescents and Adults
Definitions–Depression
screening instruments,
Instruments for Adults (18+
years)
Replace the last row with the following text:
Clinically Useful Depression Outcome Scale (CUDOS) Total Score ≥11
493 Depression Screening
and Follow-Up for
Adolescents and Adults
Definitions–Depression
screening instruments
Remove the following asterisked text below the table:
** The LOINC codes were not available at the time of the publication release. They will be included in the
release of the HEDIS 2019 Volume 2 Technical Update memo.
495 Depression Screening
and Follow-Up for
Adolescents and Adults
Follow-Up on Positive
Screen—Numerator 2
Replace the bullet and sub-bullet at the top of the page with the following text:
– Documentation of additional depression screening indicating either no depression or no symptoms
that require follow-up. For example, if the initial positive screen resulted from a PHQ-2 score,
documentation of a negative finding from a subsequent PHQ-9 qualifies as evidence of follow-up.
Specification Updates 22
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
495
Depression Screening
and Follow-Up for
Adolescents and Adults
Data Criteria (Element
Level)
Under “Value Sets:” replace the 7th and 8th bullets with the following text:
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”
495
Depression Screening
and Follow-Up for
Adolescents and Adults
Data Criteria (Element
Level)
Add the following bullets to the end of the “Value Sets:” list:
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”
• “Participation: Medicare (2.16.840.1.113883.3.464.1004.1516)”
495 Depression Screening
and Follow-Up for
Adolescents and Adults
Data Criteria (Element
Level)
Under “Direct Reference Codes:” replace the 4th bullet with the following text:
• “Assessment, Performed: Clinically Useful Depression Outcome Scale [CUDOS] (LOINC Code 90221-
3)”
495
Depression Screening
and Follow-Up for
Adolescents and Adults
Data Criteria (Element
Level)
Remove the following bullets from the “Direct Reference Codes:” list:
• “Assessment, Performed: Depression scale [DEPS] (LOINC Code Requested)”
•
“Assessment, Performed: Duke Anxiety Depression Scale [DADS] (LOINC Code Requested)”
498
Utilization of the PHQ—
9 To Monitor
Depression Symptoms
for Adolescents and
Adults
Characteristics—
Stratification
Replace the second bullet with the following text:
• Product line: Commercial, Medicare, Medicaid.
498 Utilization of the PHQ—
9 To Monitor
Depression Symptoms
for Adolescents and
Adults
Characteristics—Guidance Under Requirement #2, replace the second bullet with the following:
• PHQ-9 Modified for Teens: 12-17 years of age.
499 Utilization of the PHQ—
9 To Monitor
Depression Symptoms
for Adolescents and
Adults
Exclusions Replace “Autism spectrum disorder” with “Pervasive developmental disorder.”
500
Utilization of the PHQ—
9 To Monitor
Depression Symptoms
for Adolescents and
Adults
Data Criteria (Element
Level)
Under “Value Sets:” replace the 7
th
and 8
th
bullet with the following text:
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”

Specification Updates 23
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
500 Utilization of the PHQ—
9 To Monitor
Depression Symptoms
for Adolescents and
Adults
Data Criteria (Element
Level)
Add the following bullets to the end of the “Value Sets:” list:
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”
• “Participation: Medicare (2.16.840.1.113883.3.464.1004.1516)”
502 Depression Remission
or Response for
Adolescents and Adults
Characteristics—
Stratification
Replace the second bullet with the following text:
• Product line: Commercial, Medicare, Medicaid.
502 Depression Remission
or Response for
Adolescents and Adults
Characteristics—Guidance Under Requirement #1, replace the second bullet with the following:
• PHQ-9 Modified for Teens: 12-17 years of age.
503
Depression Remission
or Response for
Adolescents and Adults
Initial Population Add the following text as a separate row under “Ages”:
Event/Diagnosis Members with a diagnosis of major depression or dysthymia that starts before and
overlaps with the intake period or starts during the intake period, and a PHQ-9 score >9 during the intake
period (IESD).
503 Depression Remission
or Response for
Adolescents and Adults
Exclusions Replace “Autism spectrum disorder” with “Pervasive developmental disorder.”
503 Depression Remission
or Response for
Adolescents and Adults
Depression Follow-Up Replace the text in Denominator 1 with the following text:
The initial population, minus exclusions.
504
Depression Remission
or Response for
Adolescents and Adults
Data Criteria (Element
Level)
Under “Value Sets:” replace the 6th and 7th bullets with the following text:
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”
504 Depression Remission
or Response for
Adolescents and Adults
Data Criteria (Element
Level)
Add the following bullets to the end of the “Value Sets:” list:
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”
• “Participation: Medicare (2.16.840.1.113883.3.464.1004.1516)”
504 Depression Remission
or Response for
Adolescents and Adults
Data Elements for
Reporting—Table DRR-B-
1/2: Data Elements for
Depression Remission or
Response for Adolescents
In the “Data Element” column remove “Denominator.”

Specification Updates 24
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
and Adults (Medicaid and
Commercial)
504
Depression Remission
or Response for
Adolescents and Adults
Data Elements for
Reporting—Table DRR-B-3:
Data Elements for
Depression Remission or
Response for Adolescents
and Adults (Medicare)
In the “Data Element” column remove “Denominator.”
506
Unhealthy Alcohol Use
Screening and Follow-
Up
Characteristics—
Stratification
Replace the 2nd bullet with the following text:
• Product line: Commercial, Medicare, Medicaid.
507 Unhealthy Alcohol Use
Screening and Follow-
Up
Data Criteria (Element
Level)
Under “Value Sets:” replace the 2nd bullet with the following text:
• “Diagnosis: Dementia (2.16.840.1.113883.3.464.1004.1507)”
507 Unhealthy Alcohol Use
Screening and Follow-
Up
Data Criteria (Element
Level)
Under “Value Sets:” replace the last four bullets with the following text:
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Patient Characteristic Sex: Female AdministrativeGender (2.16.840.1.113883.3.464.1004.1457)”
•
“Patient Characteristic Sex: Male AdministrativeGender (2.16.840.1.113883.3.464.1004.1458)”
507 Unhealthy Alcohol Use
Screening and Follow-
Up
Data Criteria (Element
Level)
Add the following bullets to the end of the “Value Sets:” list:
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”
•
“Participation: Medicare (2.16.840.1.113883.3.464.1004.1516)”
509 Adult Immunization
Status
Entire Measure
Specification
Remove this measure and its specification in its entirety from Volume 2 and replace it with the measure
specification in Attachment A.
514 Prenatal Immunization
Status
Entire Measure
Specification
Remove this measure and its specification in its entirety from Volume 2 and replace it with the measure
specification in Attachment B.
1-18 Appendix 1 Standardized Healthcare-
Associated Infection Ratio
(HAI)
In the Standardized Healthcare-Associated Infection Ratio (HAI) row, replace the text in the “Changes for
HEDIS 2019” column with the following text:
The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, value sets and the Standard Infection Ratio (SIR)
table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.

Specification Updates 25
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Page
Measure/Guideline
Head/Subtitle
Update
7-3 Appendix 7 Effectiveness of Care
Measures
Replace measure acronym “AABV” with “AAB.”
7-5 Appendix 7 Effectiveness of Care
Measures
Replace measure acronym “HSF” with “HFS.”
7-5 Appendix 7 Access/Availability of Care,
Utilization and Risk
Adjusted Utilization
Measures
Add the following text as a Note under the table:
Note: The HAI measure is suspended and will not be collected for HEDIS 2019 reporting. Due to the
suspended status of the measure, the specifications, value sets and the Standard Infection Ratio (SIR)
table are being removed from the HEDIS 2019 Volume 2: Technical Specifications.
8-1 Appendix 8 Plan All-Cause
Readmissions 2020 Version
Remove this measure and its specification in its entirety from Volume 2 and replace it with the measure
specification in Attachment C.

Specifications Updates—Attachment A 26
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Adult Immunization Status (AIS)
*Developed with support from the Department of Health and Human Services (DHHS), Office of the
Assistant Secretary for Health (OASH), National Vaccine Program Office (NVPO).
SUMMARY OF CHANGES FOR HEDIS 2019
• First-year measure.
SUMMARY OF CHANGES FOR HEDIS 2019 TECHNICAL UPDATE
• Clarified how to calculate the composite rate in the Requirements section.
• Revised the member ages for commercial/Medicaid plans in Figure 1.
• Added direct reference codes for numerators 1-4 for history of anaphylactic reaction to specific
vaccines and removed the generic history of anaphylactic reaction to vaccine denominator exclusion
and value set.
• Added direct reference codes for numerator 2 for history of encephalopathy due to Tdap or Td vaccine
and removed the generic encephalopathy denominator exclusion and value set.
• Clarified in numerator 3 that the two doses of herpes zoster recombinant vaccine must be at least 28
days apart.
• Renamed the “Immunization, Administered: Pneumococcal Conjugate Vaccine 23” value set in the
Data Criteria (Element Level) section to “Immunization, Administered: Pneumococcal Polysaccharide
Vaccine 23” value set.
• Replaced the “Medication, Active: Chemotherapy” value set in the Data Criteria (Element Level)
section with the “Procedure, Performed: Chemotherapy Grouper” and “Encounter, Performed:
Chemotherapy Grouper” value set.
• Added a value set in the Data Criteria (Element Level) section for “Device, Applied: Cochlear Implant.”
Description
The percentage of members 19 years of age and older who are up-to-date on recommended routine
vaccines for influenza, tetanus and diphtheria (Td) or tetanus, diphtheria and acellular pertussis (Tdap),
zoster and pneumococcal.
Measurement Period
Measurement
period
January 1–December 31.
Clinical Recommendation Statement
The Advisory Committee on Immunization Practices recommends annual influenza vaccination; and
tetanus, diphtheria and acellular pertussis (Tdap) and/or tetanus and diphtheria (Td) vaccine; herpes
zoster vaccine; and the 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent
pneumococcal polysaccharide vaccine (PPSV23) for adults at various ages.

Specifications Updates—Attachment A 27
HEDIS 2019 Volume 2 Technical Update October 1, 2018
References
Kim, D.K., L.E. Riley, K.H. Harriman, P. Hunter, C.B. Bridges. 2017. “Advisory Committee on
Immunization Practices Recommended Immunization Schedule for Adults Aged 19 Years or Older —
United States, 2017.” MMWR Morb Mortal Wkly Rep 66:136–8. DOI:
http://dx.doi.org/10.15585/mmwr.mm6605e2
Characteristics
Scoring
Proportion.
Type
Process.
Item count
Members.
Stratification Report each of the following age strata by product line:
• Age (years): 19–65 (commercial and Medicaid only), 66+ (Medicare only).
• Product line: Commercial, Medicare, Medicaid.
Risk adjustment
None.
Improvement
notation
A higher score indicates better performance.
Guidance Allocation
The member was continuously enrolled with a medical benefit throughout the
participation period. Refer to ECDS General Guideline 5: Member Allocation to
HEDIS ECDS Measures.
Requirements
1. For HEDIS, separate files are submitted by product line.
2. The composite is based on a model that looks at the number of
immunizations that were administered or contraindicated due to history of
anaphylactic reaction or encephalopathy following vaccination (numerator) out
of the possible number of immunizations needed to be administered to
members per clinical guideline recommendations for that age group
(denominator).
3. For commercial and Medicaid plan members 19–65
years of age,
Denominator 5 is determined by summing Denominators 1–3. Numerator 5 is
determined by summing Numerators 1–3.
4. For Medicare plan members 66 years of age and older, Denominator 5 is
determined by summing Denominators 1–4. Numerator 5 is determined by
summing Numerators 1–4.

Specifications Updates—Attachment A 28
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Figure 1: Example of calculation for composite rate
Note: The tables provide an example of how a commercial, Medicaid and Medicare plan with three members
at different ages would calculate the composite rate.
Shaded boxes indicate the number of recommended vaccinations for the member based on their age and the
checkmarks indicate whether the immunization was administered.
MEDICARE PLANS
Composite Rate:
7 immunizations
provided;
12 immunizations
needed
=
58%
Vaccines
Member A
Age 70
Member B
Age 68
Member C
Age 66
Influenza
Td or Tdap
Zoster
Pneumococcal
COMMERCIAL/MEDICAID PLANS
Composite Rate:
4 immunizations
provided;
8 immunizations
needed
=
50%
Vaccines
Member A
Age 64
Member B
Age 50
Member C
Age 19
Influenza
Td or Tdap
Zoster
NA
Pneumococcal NA NA NA
Definitions
Participation The identifiers and descriptors for each organization’s coverage used to define
members’ eligibility for measure reporting.
Allocation for reporting is based on eligibility during the participation period.
Initial Population
Participation
period
Measurement period.
Ages
19 years of age and older at the start of the measurement period.
Exclusions
Exclusions Exclude members with any of the following:
• Active chemotherapy during the measurement period.
• Bone marrow transplant during the measurement period.
• History of immunocompromising conditions, cochlear implants, anatomic or
functional asplenia, sickle cell anemia & HB-S disease or cerebrospinal

Specifications Updates—Attachment A 29
HEDIS 2019 Volume 2 Technical Update October 1, 2018
fluid leaks any time during the member’s history through the end of the
measurement period.
• In hospice or using hospice services during the measurement period.
Immunization Status: Influenza
Denominator 1
The initial population, minus exclusions.
Numerator 1 Members in Denominator 1 who received an influenza vaccine on or between
July 1 of the year prior to the measurement period and June 30 of the
measurement period; or prior anaphylaxis due to Haemophilus influenzae type b
vaccine or its components any time during or before the measurement period.
Immunization Status: Td/Tdap
Denominator 2
Same as Denominator 1.
Numerator 2 Members in Denominator 2 who received at least one Td vaccine or one Tdap
vaccine between nine years prior to the start of the measurement period and the
end of the measurement period; or
Members in Denominator 2 with history of at least one of the following
contraindications any time during or before the measurement period:
• Anaphylaxis due to Tdap vaccine, anaphylaxis due to Td vaccine or its
components.
• Encephalopathy due to Tdap or Td vaccination (post tetanus vaccination
encephalitis, post diphtheria vaccination encephalitis or post pertussis
vaccination encephalitis).
Immunization Status: Zoster
Denominator 3 Members in Denominator 1, 50 years of age and older at the start of the
measurement period.
Numerator 3 Members in Denominator 3 who received at least one dose of the herpes zoster
live vaccine or two doses of the herpes zoster recombinant vaccine (at least 28
days apart) anytime on or after the member’s 50th birthday; or prior adverse
reaction caused by zoster vaccine or its components any time during or before
the measurement period.
Immunization Status: Pneumococcal
Denominator 4 Members in Denominator 1, 66 years of age and older as of the start of the
measurement period.
Numerator 4 Members in Denominator 4 who were administered both the 13-valent
pneumococcal conjugate vaccine and the 23-valent pneumococcal
polysaccharide vaccine at least 12 months apart, with the first occurrence after
the age of 60; or prior pneumococcal vaccine adverse reaction any time during or
before the measurement period.

Specifications Updates—Attachment A 30
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Immunization Status: Composite
Denominator 5
The sum of denominators 1–4.
Numerator 5
The sum of numerators 1–4.
Data Criteria (Element Level)
Value Sets:
• “Diagnosis: Anatomic or Functional Asplenia (2.16.840.1.113883.3.464.1004.1477)”
• “Diagnosis: Cerebrospinal Fluid Leak (2.16.840.1.113883.3.464.1004.1448)”
• “Diagnosis: Cochlear Implant (2.16.840.1.113883.3.464.1004.1520)”
• “Procedure, Performed: Cochlear Implant (2.16.840.1.113883.3.464.1004.1447)”
• “Device, Applied: Cochlear Implant (2.16.840.1.113883.3.464.1004.1521)”
• “Diagnosis: Immunocompromising Conditions (2.16.840.1.113883.3.464.1004.1502)”
• “Diagnosis: Sickle Cell Anemia and HB-S Disease (2.16.840.1.113883.3.464.1004.1505)”
• “Immunization, Administered: Adult Influenza Vaccine (2.16.840.1.113883.3.464.1004.1476)”
• “Immunization, Administered: Td Vaccine (2.16.840.1.113883.3.464.1004.1244)”
• “Immunization, Administered: Tdap Vaccine (2.16.840.1.113883.3.464.1004.1506)”
• “Immunization, Administered: Herpes Zoster Live Vaccine (2.16.840.1.113883.3.464.1004.1478)”
• “Immunization, Administered: Herpes Zoster Recombinant Vaccine
(2.16.840.1.113883.3.464.1004.1494)”
• “Immunization, Administered: Pneumococcal Conjugate Vaccine 13
(2.16.840.1.113883.3.464.1004.1439)”
• “Immunization, Administered: Pneumococcal Polysaccharide Vaccine 23
(2.16.840.1.113883.3.464.1004.1440)”
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”
• “Participation: Medicare (2.16.840.1.113883.3.464.1004.1516)”
• “Procedure, Performed: Chemotherapy Grouper (2.16.840.1.113883.3.464.1004.1500)”
• “Encounter, Performed: Chemotherapy Grouper (2.16.840.1.113883.3.464.1004.1519)”
• “Procedure, Performed: Bone Marrow Transplant (2.16.840.1.113883.3.464.1004.1499)”
Direct Reference Codes:
• “Diagnosis: Anaphylaxis due to Haemophilus influenzae type b vaccine (SNOMEDCT Code
433621000124101)”
• “Diagnosis: Anaphylaxis Due to Td Vaccine (SNOMEDCT Code 428281000124107)”
• “Diagnosis: Anaphylaxis Due to Tdap Vaccine (SNOMEDCT Code 428291000124105)”
• “Diagnosis: Adverse Reaction Caused by Zoster Vaccine (SNOMEDCT Code 451291000124104)”
• “Diagnosis: Pneumococcal Vaccine Adverse Reaction (SNOMEDCT Code 293116002)”
• “Diagnosis: Post Tetanus Vaccination Encephalitis (SNOMEDCT Code 192710009)”

Specifications Updates—Attachment A 31
HEDIS 2019 Volume 2 Technical Update October 1, 2018
• “Diagnosis: Post Diphtheria Vaccination Encephalitis (SNOMEDCT Code 192711008)”
• “Diagnosis: Post Pertussis Vaccination Encephalitis (SNOMEDCT Code 192712001)”
Data Elements for IDSS Reporting
Organizations that submit data to NCQA must provide the following data elements in a specified file.
Table AIS-A: 1/2/3 Metadata Elements for Adult Immunizations Status
Metadata ID
Metadata Specification
MeasurementYear Measurement year
CollectionMethod Data collection methodology (electronic clinical data)
Table AIS-B:1/2 Data Elements for Adult Immunizations Status (Medicaid and Commercial)
Indicator
Data Element
Data Source
Immunization Status: Influenza Initial population EHR
Immunization Status: Td/Tdap Exclusions HIE/Clinical Registry
Immunization Status: Zoster Denominator Case Management Registry
Numerator Administrative
Table AIS-B:3 Data Elements for Adult Immunizations Status (Medicare)
Indicator
Data Element
Data Source
Immunization Status: Influenza Initial population EHR
Immunization Status: Td/Tdap Exclusions HIE/Clinical Registry
Immunization Status: Zoster Denominator Case Management Registry
Immunization Status: Pneumococcal Numerator Administrative

Specifications Updates—Attachment B 32
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Prenatal Immunization Status (PRS)
*Developed with support from the Department of Health and Human Services (DHHS), Office of the
Assistant Secretary for Health (OASH), National Vaccine Program Office (NVPO).
SUMMARY OF CHANGES FOR HEDIS 2019
• First-year measure.
SUMMARY OF CHANGES FOR HEDIS 2019 TECHNICAL UPDATE
• Added a requirements section to guidance to clarify how to calculate the start of pregnancy for
numerator 2.
• Added direct reference codes to numerators 1 and 2 for history of anaphylactic reaction to influenza or
Tdap vaccines and removed the history of anaphylactic reaction to vaccine denominator exclusion and
value set.
• Added direct reference codes to numerator 2 for history of encephalopathy due to Td or Tdap vaccine
and removed the encephalopathy denominator exclusion and value set.
Description
The percentage of deliveries in the measurement period in which women received influenza and
tetanus, diphtheria toxoids and acellular pertussis (Tdap) vaccinations.
Measurement Period
Measurement
period
January 1–December 31.
Clinical Recommendation Statement
Advisory Committee on Immunization Practices (ACIP) clinical guidelines recommend that all women
who are pregnant or who might be pregnant in the upcoming influenza season receive inactivated
influenza vaccines. ACIP also recommends that pregnant women should receive one dose of Tdap
during each pregnancy, preferably during the early part of gestational weeks 27–36, regardless of prior
history of receiving Tdap.
References
Kim, D.K., L.E. Riley, K.H. Harriman, P. Hunter, C.B. Bridges. 2017. “Advisory Committee on
Immunization Practices Recommended Immunization Schedule for Adults Aged 19 Years or Older —
United States, 2017.” MMWR Morb Mortal Wkly Rep 66:136–8. DOI:
http://dx.doi.org/10.15585/mmwr.mm6605e2
.

Specifications Updates—Attachment B 33
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Characteristics
Scoring
Proportion.
Type
Process.
Item count
Deliveries.
Stratification Report deliveries by the following:
Product line: Commercial, Medicaid.
Risk adjustment
None.
Improvement
notation
A higher score indicates better performance.
Guidance Allocation
The member was continuously enrolled with a medical benefit from the 28 days
prior to the delivery through the delivery date.
Requirements
1. Numerator 2: Use gestational age at time of delivery and the delivery date to
calculate the start of the pregnancy. Note: If weeks of gestation at time of
delivery is not available, the delivery is not compliant for the numerator.
Definitions
Pregnancy
episode
1. Delivery date occurs during the measurement period.
2. Excludes pregnancy <37 gestational weeks at time of delivery.
Participation The identifiers and descriptors for each organization’s coverage used to define
members’ eligibility for measure reporting.
Allocation for reporting is based on eligibility during the participation period.
Initial Population
Participation
period
28 days prior to delivery date through the delivery date.
Initial population
Deliveries during the measurement period.
Exclusions
Exclusions Exclude deliveries where members have any of the following:
• Weeks of gestation less than 37 at time of delivery.
• In hospice or using hospice services during the measurement period.

Specifications Updates—Attachment B 34
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Immunization Status: Influenza
Denominator 1
The initial population minus exclusions.
Numerator 1 Deliveries where members received an adult influenza vaccine on or between
July 1 of the year prior to the measurement period and the delivery date; or
deliveries where members had a prior anaphylactic reaction to influenza vaccine
or its components any time during or before the measurement period.
Immunization Status: Tdap
Denominator 2
Same as Denominator 1.
Numerator 2 Deliveries where members received at least one Tdap vaccine during the
pregnancy (including on the delivery date); or
Deliveries where member has a history of at least one of the following
contraindications any time before or during measurement period:
• Anaphylactic reaction to Tdap or Td vaccine or its components;
• Encephalopathy due to Td or Tdap vaccination (post tetanus vaccination
encephalitis, post diphtheria vaccination encephalitis or post pertussis
vaccination encephalitis).
Immunization Status: Combination
Denominator 3
Same as Denominator 1
Numerator 3
Deliveries that met criteria for both Numerator 1 and Numerator 2
Data Criteria (Element Level)
Value Sets:
• “Diagnosis: Weeks of Gestation Less than 37 (2.16.840.1.113883.3.464.1004.1479)”
• “Diagnosis: 37 Weeks Gestation (2.16.840.1.113883.3.464.1004.1509)”
• “Diagnosis: 38 Weeks Gestation (2.16.840.1.113883.3.464.1004.1510)”
• “Diagnosis: 39 Weeks Gestation (2.16.840.1.113883.3.464.1004.1511)”
• “Diagnosis: 40 Weeks Gestation (2.16.840.1.113883.3.464.1004.1512)”
• “Diagnosis: 41 Weeks Gestation (2.16.840.1.113883.3.464.1004.1513)”
• “Diagnosis: 42 Weeks Gestation (2.16.840.1.113883.3.464.1004.1514)”
• “Diagnosis: 43 Weeks Gestation (2.16.840.1.113883.3.464.1004.1515)”
• “Intervention, Performed: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Intervention, Order: Hospice (2.16.840.1.113883.3.464.1004.1504)”
• “Immunization, Administered: Tdap Vaccine (2.16.840.1.113883.3.464.1004.1506)”
• “Immunization, Administered: Adult Influenza Vaccine (2.16.840.1.113883.3.464.1004.1476)”
• “Participation: Commercial (2.16.840.1.113883.3.464.1004.1518)”
• “Participation: Medicaid (2.16.840.1.113883.3.464.1004.1517)”

Specifications Updates—Attachment B 35
HEDIS 2019 Volume 2 Technical Update October 1, 2018
• “Procedure, Performed: Deliveries (2.16.840.1.113883.3.464.1004.1508)”
Direct Reference Codes:
• “Diagnosis: Length of gestation at birth (observable entity) (SNOMEDCT Code 412726003)”
• “Diagnosis: Influenza Virus Vaccine Adverse Reaction (SNOMEDCT Code 420113004)”
• “Diagnosis: Anaphylactic Reaction Due to Td Vaccine (SNOMEDCT Code 428281000124107)”
• “Diagnosis: Anaphylactic Reaction Due to Tdap Vaccine (SNOMEDCT Code 428291000124105)”
• “Diagnosis: Post Tetanus Vaccination Encephalitis (SNOMEDCT Code 192710009)”
• “Diagnosis: Post Diphtheria Vaccination Encephalitis (SNOMEDCT Code 192711008)”
• “Diagnosis: Post Pertussis Vaccination Encephalitis (SNOMEDCT Code 192712001)”
Data Elements for IDSS Reporting
Organizations that submit data to NCQA must provide the following data elements.
Table PRS-A: 1/2 Metadata Elements for Prenatal Immunization Status
Metadata ID
Metadata Specification
MeasurementYear Measurement year
CollectionMethod Data collection methodology (electronic clinical data)
Table PRS-B: 1/2 Data Elements for Prenatal Immunization Status
Indicator
Data Element
Specification Data Source
Immunization Status:
Influenza
Initial population EHR
Immunization Status:
Tdap
Exclusions HIE/Clinical Registry
Immunization Status:
Combination
Denominator Case Management Registry
Numerator Administrative

Specifications Updates—Attachment C 36
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Plan All-Cause Readmissions 2020 Version (PCR2020)
This specification should not be used for HEDIS 2019 reporting. This is the proposed version of the
measure for HEDIS 2020. Additional changes may be included when released for reporting.
SUMMARY OF CHANGES TO HEDIS 2020
• Added definitions of “outlier,” “nonoutlier” and “plan population.”
• Added observation stays to inpatient admissions.
• Revised direct transfers to include observation discharges.
• Added steps to remove hospitalizations for outlier members and report a count of outlier members.
• Removed the high-frequency hospitalization stratification for Medicaid.
• Added a step in the Risk Adjustment Weighting section for observation stay IHS.
• Removed the base weight variable from the risk adjustment weighting.
• Added instructions and data element tables to report plan population and outlier rate.
• Added instructions and data element tables to report the rate among index stays discharged or
transferred to skilled nursing care.
Description
For members 18 years of age and older, the number of acute inpatient and observation stays during the
measurement year that were followed by an unplanned acute readmission for any diagnosis within 30
days and the predicted probability of an acute readmission. Data are reported in the following
categories:
1. Count of Index Hospital Stays (IHS) (denominator).
2. Count of Observed 30-Day Readmissions (numerator).
3. Count of Expected 30-Day Readmissions.
Note: For commercial and Medicaid, report only members 18–64 years of age.
Definitions
IHS Index hospital stay. An acute inpatient or observation stay with a discharge on
or between January 1 and December 1 of the measurement year. Exclude
stays that meet the exclusion criteria in the denominator section.
Index Admission
Date
The IHS admission date.
Index Discharge
Date
The IHS discharge date. The index discharge date must occur on or between
January 1 and December 1 of the measurement year.
Index
Readmission
Stay
An acute inpatient or observation stay for any diagnosis with an admission date
within 30 days of a previous Index Discharge Date.

Specifications Updates—Attachment C 37
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Index
Readmission
Date
The admission date associated with the Index Readmission Stay.
Planned hospital
stay
A hospital stay is considered planned if it meets criteria as described in step 3
(required exclusions) of the numerator.
Plan population Members who meet all of the following criteria:
• 18 and older as of January 1 of the measurement year.
• Enrolled on January 1 of the measurement year.
• Continuously enrolled for at least 365 days at any point between January
1 of the year prior to the measurement year and December 1 of the
measurement year with no more than one gap in enrollment of up to 45
days during the 365-day period.
Outlier Medicaid and Medicare members with four or more index hospital stays during
the measurement year.
Commercial members with three or more index hospital stays during the
measurement year.
Nonoutlier Members in the plan population who are not considered outliers.
Classification
period
365 days prior to and including an Index Discharge Date.
Risk Adjustment Tables
Table
Table Description
HCC-Surg Surgery codes for Risk Adjustment Determination
PCR-DischCC Discharge Clinical Condition category codes for Risk Adjustment Determination
CC-Comorbid Comorbid Clinical Condition category codes for Risk Adjustment Determination step 2
HCC–Rank HCC rankings for Risk Adjustment Determination step 3
HCC-Comb Combination HCCs for Risk Adjustment Determination step 5
PCR-MA-DischCC-
WeightUnder65
MA and SNP primary discharge weights for Risk Adjustment Weighting step 3 for ages
under 65
PCR-MA-DischCC-Weight-65plus
MA and SNP primary discharge weights for Risk Adjustment Weighting step 3 for ages
65 and older
PCR-MA-SDischCC-Weight-
Under65
MA and SNP primary discharge weights for Risk Adjustment Weighting step 3 for index
stays discharged to skilled nursing among ages under 65
PCR-MA-SDischCC-Weight-
65plus
MA and SNP primary discharge weights for Risk Adjustment Weighting step 3 for index
stays discharged to skilled nursing among ages 65 and older
PCR-Comm-DischCC-Weight Commercial primary discharge weights for Risk Adjustment Weighting step 3
PCR-MD-DischCC-Weight Medicaid primary discharge weights for Risk Adjustment Weighting step 3
PCR-MA-ComorbHCC-Weight-
Under65
MA and SNP comorbidity weights for Risk Adjustment Weighting step 4 for ages under
65

Specifications Updates—Attachment C 38
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Table
Table Description
PCR-MA-ComorbHCC-Weight-
65plus
MA and SNP comorbidity weights for Risk Adjustment Weighting step 4 for ages 65 and
older
PCR-MA-SComorbHCC-
WeightUnder65
MA and SNP comorbidity weights for Risk Adjustment Weighting step 4 for index stays
discharged to skilled nursing among ages under 65
PCR-MA-SComorbHCC-Weight-
65plus
MA and SNP comorbidity weights for Risk Adjustment Weighting step 4 for index stays
discharged to skilled nursing among ages 65 and older
PCR-Comm-ComorbHCC-Weight Commercial comorbidity weights for Risk Adjustment Weighting step 4
PCR-MD-ComorbHCC-Weight Medicaid comorbidity weights for Risk Adjustment Weighting step 4
PCR-MA-OtherWeights-Under65 MA and SNP observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5 for ages under 65
PCR-MA-OtherWeights-65plus MA and SNP observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5 for ages 65 and older
PCR-MA-SOtherWeights-
Under65
MA and SNP observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5 for index stays discharged to skilled nursing among ages under
65
PCR-MA-SOtherWeights-65plus
MA and SNP observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5 for index stays discharged to skilled nursing among ages 65 and
older
PCR-Comm-OtherWeights
Commercial observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5
PCR-MD-OtherWeights Medicaid observation stay, surgery, age and gender weights for Risk Adjustment
Weighting steps 1, 2, 5
Note: The risk adjustment tables will be released on November 1, 2018, and posted to www.ncqa.org.
Eligible Population
Note: Members in hospice are excluded from the eligible population. Refer to General Guideline 17: Members
in Hospice.
Refer to General Guideline 10: Reporting for small denominator limits.
Product line
Stratification
Commercial, Medicare, Medicaid (report each product line separately).
For only Medicare IHS’, report the following SES stratifications and total:
• Non-LIS/DE, Nondisability.
• LIS/DE.
• Disability.
• LIS/DE and Disability.
• Other.
• Unknown.
• Total Medicare.
Note: The stratifications are mutually exclusive, and the sum of all six stratifications is
the Total population.
Specifications Updates—Attachment C 39
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Ages
For commercial, ages 18–64 as of the Index Discharge Date.
For Medicare, ages 18 and older as of the Index Discharge Date.
For Medicaid, ages 18–64 as of the Index Discharge Date.
Continuous
enrollment
365 days prior to the Index Discharge Date through 30 days after the Index
Discharge Date.
Allowable gap No more than one gap in enrollment of up to 45 days during the 365 days prior to
the Index Discharge Date and no gap during the 30 days following the Index
Discharge Date.
Anchor date
Index Discharge Date.
Benefit
Medical.
Event/
diagnosis
An acute inpatient or observation stay discharge on or between January 1 and
December 1 of the measurement year.
The denominator for this measure is based on discharges, not members. Include
all acute inpatient or observation stay discharges for nonoutlier members who had
one or more discharges on or between January 1 and December 1 of the
measurement year.
Follow the steps below to identify acute inpatient and observation stays.
Administrative Specification
Denominator
The eligible population.
Step 1 Identify all acute inpatient and observation stay discharges on or between January
1 and December 1 of the measurement year. To identify acute inpatient and
observation stay discharges:
1. Identify all acute and nonacute inpatient stays (Inpatient Stay Value Set)
and observation stays (Observation Stay Value Set).
2. Exclude nonacute inpatient stays (Nonacute Inpatient Stay Value Set).
3. Identify the discharge date for the stay.
Inpatient and observation stays where the discharge date from the first setting and
the admission date to the second setting are two or more calendar days apart
must be considered distinct stays.
The measure includes acute discharges from any type of facility (including
behavioral healthcare facilities).
Step 2 Direct transfers: For discharges with one or more direct transfers, use the last
discharge.
Using the discharges identified in step 1, identify direct transfers between acute
inpatient and observation or between observation and acute inpatient using the
definition below.
A direct transfer is when the discharge date from the first stay precedes the
admission date to a subsequent stay by one calendar day or less. For example:
Specifications Updates—Attachment C 40
HEDIS 2019 Volume 2 Technical Update October 1, 2018
• A discharge on June 1, followed by a subsequent admission on June 1, is a
direct transfer.
• A discharge on June 1, followed by a subsequent admission on June 2, is a
direct transfer.
• A discharge on June 1, followed by a subsequent admission on June 3, is
not a direct transfer; these are two distinct stays.
• A discharge on June 1, followed by a subsequent admission on June 2 (with
discharge on June 3), followed by a subsequent admission on June 4, is a
direct transfer.
Exclude the hospital stay if the direct transfer’s discharge date occurs after
December 1 of the measurement year.
Step 3
Exclude hospital stays where the Index Admission Date is the same as the Index
Discharge Date.
Step 4:
Required
exclusions
Exclude hospital stays for the following reasons:
• The member died during the stay.
• Female members with a principal diagnosis of pregnancy (Pregnancy Value
Set) on the stay.
• A principal diagnosis of a condition originating in the perinatal period
(Perinatal Conditions Value Set) on the discharge claim.
Note: For hospital stays where there was a direct transfer (identified in step 2), use the
original stay and any direct transfer stays to identify exclusions in this step.
Step 5
Calculate continuous enrollment.
Step 6 Remove hospital stays for outlier members and report these members as outliers
in Tables PCR-1/2/3 and PCR-D-3.
Note: Count discharges with one or more direct transfers (identified in step 2) as one
discharge when identifying outlier members.
Step 7 Assign each remaining acute inpatient or observation stay to an age and
stratification category using the reporting instructions below.
Risk Adjustment Determination
For each IHS among nonoutlier members, use the following steps to identify risk adjustment categories
based on presence of observation stay status at discharge, surgeries, discharge condition, comorbidity,
age and gender.
Observation
Stay
Determine if the IHS at discharge was an observation stay (Observation Stay Value
Set). For direct transfers, determine the hospitalization status using the last discharge.
Surgeries Determine if the member underwent surgery during the stay. Download the list of
codes from the NCQA website (Table HCC-Surg) and use it to identify surgeries.
Consider an IHS to include a surgery if at least one procedure code in Table HCC-
Surg is present from any provider between the admission and discharge dates.
Discharge
Condition
Assign a discharge Clinical Condition (CC) category code or codes to the IHS
based on its primary discharge diagnosis, using Table PCR-DischCC. For direct
transfers, use the primary discharge diagnosis from the last discharge.

Specifications Updates—Attachment C 41
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Exclude diagnoses that cannot be mapped to Table PCR-DischCC.
Comorbidities Refer to the Utilization Risk Adjustment Determination in the Guidelines for Risk
Adjusted Utilization Measures.
Risk Adjustment Weighting
For each IHS among nonoutliers, use the following steps to identify risk adjustment weights based on
observation stays status at discharge, surgeries, discharge condition, comorbidity, age and gender.
Note: The final weights table will be released on November 1, 2018.
Step 1 For each IHS discharge that is an observation stay, link the observation stay IHS weight.
• For Medicare product lines ages 18–64:
– Use Table PCR-MA-OtherWeights-Under65.
– Use Table PCR-MA-SOtherWeights-Under65.
•
For Medicare product lines ages 65 and older:
– Use Table PCR-MA-OtherWeights-65plus.
– Use Table PCR-MA-SOtherWeights-65plus.
•
For commercial product lines: Use Table PCR-Comm-OtherWeights.
•
For Medicaid product lines: Use Table PCR-MD-OtherWeights.
Step 2 For each IHS with a surgery, link the surgery weight.
• For Medicare product lines ages 18–64:
– Use Table PCR-MA-OtherWeights-Under65.
– Use Table PCR-MA-SOtherWeights-Under65.
•
For Medicare product lines ages 65 and older:
– Use Table PCR-MA-OtherWeights-65plus.
– Use Table PCR-MA-SOtherWeights-65plus.
•
For commercial product lines: Use Table PCR-Comm-OtherWeights.
• For Medicaid product lines: Use Table PCR-MD-OtherWeights.
Step 3 For each IHS with a discharge CC Category, link the primary discharge weights.
• For Medicare product lines ages 18–64:
– Use Table PCR-MA-DischCC-Weight-Under65.
– Use Table PCR-MA-SDischCC-Weight-Under65.
•
For Medicare product lines ages 65 and older:
– Use Table PCR-MA-DischCC-Weight-65plus.
– Use Table PCR-MA-SDischCC-Weight-65plus.
•
For commercial product lines: Use Table PCR-Comm-DischCC-Weight.
• For Medicaid product lines: Use Table PCR-MD-DischCC-Weight.
Step 4 For each IHS with a comorbidity HCC Category, link the weights.
• For Medicare product lines ages 18–64:
– Use Table PCR-MA-ComorbHCC-Weight-Under65.
– Use Table PCR-MA-SComorbHCC-Weight-Under65.
• For Medicare product lines ages 65 and older:

Specifications Updates—Attachment C 42
HEDIS 2019 Volume 2 Technical Update October 1, 2018
–
Use Table PCR-MA-ComorbHCC-Weight-65plus.
– Use Table PCR-MA-SComorbHCC-Weight-65plus.
•
For commercial product lines: Use Table PCR-Comm-ComorbHCC-Weight.
• For Medicaid product lines: Use Table PCR-MD-ComorbHCC-Weight.
Step 5 Link the age and gender weights for each IHS.
• For Medicare product lines ages 18–64:
– Use Table PCR-MA-OtherWeights-Under65.
– Use Table PCR-MA-SOtherWeights-Under65.
•
For Medicare product lines ages 65 and older:
– Use Table PCR-MA-OtherWeights-65plus.
– Use Table PCR-MA-SOtherWeights-65plus.
•
For commercial product lines:
– Use Table PCR-Comm-OtherWeights.
•
For Medicaid product lines:
– Use Table PCR-MD-OtherWeights.
Step 6 Sum all weights associated with the IHS (i.e., observation stay, presence of surgery, primary
discharge diagnosis, comorbidities, age and gender) and use the formula below to calculate
the Estimated Readmission Risk for each IHS
Estimated Readmission Risk =
(
∑
WeightsForIHS)
1+
(
∑
WeightsForIHS)
OR
Estimated Readmission Risk = [exp (sum of weights for IHS)] / [ 1 + exp (sum of weights for
IHS)]
Note: “Exp” refers to the exponential or antilog function.
Step 7 Calculate the Count of Expected Readmissions for each age and stratification category. The
Count of Expected Readmissions is the sum of the Estimated Readmission Risk calculated
in step 6 for each IHS in each age and stratification category.
= �(Estimated Readmission Risk)
Step 8 Use the formula below and the Estimated Readmission Risk calculated in step 6 to calculate
the variance for each IHS.
Variance = Estimated Readmission Risk x (1 – Estimated Readmission Risk)
Example: If the Estimated Readmission Risk is 0.1518450741 for an IHS, then the variance
for this IHS is 0.1518450741 x 0.8481549259 = 0.1287881476.
Note: This variance is calculated at the IHS level. Organizations must sum the variances for
each stratification and age when populating the Variance cells in the reporting tables.

Specifications Updates—Attachment C 43
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Sample Table: PCR—Risk Adjustment Weighting
Member
ID*
Admiss.
Counter Age Gender
Age and
Gender
Weight
Surgical
Weight
ICD-10
Diagnosis
Code
Discharge CC
HCC-PCR
Sum of
Weights
Estimated
Readmissions
Risk Variance
Category Weight Category Weight
1250 1 67 Female -2.619 -0.2753 T44992S 58 0.2990
18 0.1961
-2.1783 0.1017 0.0914
55 0.2209
4010 1 50 Male -2.4722 NA J439 111 0.4221 NA NA -2.0501 0.1140 0.1010
4010 2 50 Male -2.4722 NA B180 29 0.6090 87 0.141 -1.7222 0.1516 0.1286
*Each Member ID field with a value represents a unique IHS.
Numerator
At least one acute readmission for any diagnosis within 30 days of the Index Discharge Date.
Step 1 Identify all acute inpatient and observation stays with an admission date on or between January 3 and December 31 of the
measurement year. To identify acute inpatient and observation admissions:
1. Identify all acute and nonacute inpatient stays (Inpatient Stay Value Set) and observation stays (Observation Stay
Value Set).
2. Exclude nonacute inpatient stays (Nonacute Inpatient Stay Value Set).
3. Identify the admission date for the stay.
Inpatient stays and observation stays where the discharge date from the first setting and the admission date to the second
setting are two or more calendar days apart must be considered distinct stays. If an organization consolidates these stays
into a single event (for any reason), the original distinct inpatient or observation stay must be used.

Specifications Updates—Attachment C 44
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Step 2
Direct transfers: For discharges with one or more direct transfers, use the last discharge.
Using the discharges identified in step 1, identify direct transfers between acute inpatient and
observation or between observation and acute inpatient using the definition below.
A direct transfer is when the discharge date from the first stay precedes the admission date
to a subsequent stay by one calendar day or less. For example:
• A discharge on June 1, followed by a subsequent admission on June 1, is a direct
transfer.
• A discharge on June 1, followed by a subsequent admission on June 2, is a direct
transfer.
• A discharge on June 1, followed by a subsequent admission on June 3, is not a direct
transfer; these are two distinct stays.
• A discharge on June 1, followed by a subsequent admission on June 2 (with discharge
on June 3), followed by a subsequent admission on June 4, is a direct transfer.
Step 3 Exclude acute hospitalizations with any of the following criteria on the discharge claim:
• Female members with a principal diagnosis of pregnancy (Pregnancy Value Set).
• A principal diagnosis for a condition originating in the perinatal period (Perinatal
Conditions Value Set).
• Planned admissions using any of the following:
– A principal diagnosis of maintenance chemotherapy (Chemotherapy Value Set).
– A principal diagnosis of rehabilitation (Rehabilitation Value Set).
– An organ transplant (Kidney Transplant Value Set, Bone Marrow Transplant Value
Set, Organ Transplant Other Than Kidney Value Set, Introduction of Autologous
Pancreatic Cells Value Set).
– A potentially planned procedure (Potentially Planned Procedures Value Set) without
a principal acute diagnosis (Acute Condition Value Set).
Note: For hospital stays where there was a direct transfer (identified in step 2), use the
original stay and any direct transfer stays to identify exclusions in this step.
Step 4
Remove hospital stays for outlier members.
Step 5 For each remaining IHS, determine if any of the acute inpatient and observation stays have
an admission date within 30 days after the Index Discharge Date.
Reporting: Number of Members in Plan Population
Step 1
Determine member age as of January 1 of the measurement year.
Step 2 Report the count of members in the plan population for each age and gender group and the
overall total. Enter these values in reporting Tables PCR-1/2/3 and PCR-D-3.
Reporting: Number of Outliers
Step 1
Determine member age as of January 1 of the measurement year.
Step 2 Report the count of outlier members for each age and gender group and the overall total.
Enter these values in reporting Tables PCR-1/2/3 and PCR-D-3.

Specifications Updates—Attachment C 45
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Calculated: Number of Nonoutliers
The number of members in the plan population minus the number of outliers for each age and gender
group and the overall total calculated by IDSS.
Calculated: Outlier Rate
The number of outlier members divided by the number of members in the plan population, multiplied by
1,000, for each age and gender group and the overall total. Calculated by IDSS.
Reporting: Denominator
Count the number of IHS among nonoutlier members for each age group and enter these values into the
reporting table under Count of Index Stays.
Reporting: SES Stratification (Medicare only)
Step 1 Determine the member’s SES stratifications as of the end of the continuous enrollment
period for each Medicare discharge:
• Non-LIS/DE, Nondisability: Member is eligible for Medicare due to age only (i.e., does
not receive LIS, is not DE for Medicaid, does not have disability status).
• LIS/DE: Member is eligible for Medicare due to age and receives LIS (includes
members eligible for Medicare due to DE), does not have disability status.
• Disability: Member is eligible for Medicare due to disability status only.
• LIS/DE and Disability: Member is eligible for Medicare, receives LIS and has disability
status.
• Other: Member has ESRD-only status or is assigned “9—none of the above.”
• Unknown: Member’s SES is unknown.
• Total Medicare: Total of all categories.
Step 2 Report Medicare discharges based on the SES stratification assigned for each Medicare
index stay in Table PCR-B-3 and Table PCR-F-3.
Reporting: Skilled Nursing Care Stratification (Medicare only)
Step 1 For Medicare nonoutlier members, determine if the IHS was discharged or transferred to
skilled nursing care (Skilled Nursing Stay Value Set).
An index stay is discharged or transferred to skilled nursing care when the discharge date
from the acute inpatient or observation stay precedes the admission date for skilled nursing
care by one calendar day or less. For example:
• An index stay discharge on June 1, followed by an admission to a skilled nursing
setting on June 1, is an IHS discharged or transferred to skilled nursing care.
• An index stay discharge on June 1, followed by an admission to a skilled nursing
setting on June 2, is an IHS discharged or transferred to skilled nursing care.
• An index stay discharge on June 1, followed by an admission to a skilled nursing
setting on June 3, is not an IHS discharged or transferred to skilled nursing care.
Step 2 Report Medicare discharges for each IHS discharged or transferred to skilled nursing care to
an age group in Table PCR-C-3 and Table PCR-G-3.

Specifications Updates—Attachment C 46
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Reporting: Numerator
Count the number of observed IHS among nonoutlier members with a readmission within 30 days of
discharge for each age group and enter these values into the reporting tables under Count of Observed
30-Day Readmissions.
Calculated: Observed Readmission Rate
The Count of Observed 30-Day Readmissions divided by the Count of Index Stays calculated by IDSS.
Reporting: Count of Expected 30-Day Readmissions
Step 1 Calculate the Count of Expected Readmissions among nonoutlier members for each age
group and overall total.
Step 2 Round to four decimal places using the .5 rule and enter the Count of Expected
Readmissions into the reporting tables.
Calculated: Expected Readmission Rate
The Count of Expected 30-Day Readmissions divided by the Count of Index Stays calculated by IDSS.
Reporting: Variance
Step 1 Calculate the total (sum) variance for each SES stratification (Medicare only), skilled nursing
stratification (Medicare only) and age group.
Step 2 Round to four decimal places using the .5 rule and enter the variance into the reporting
tables.
Calculated: O/E Ratio
The Count of Observed 30-Day Readmissions divided by the Count of Expected 30-Day Readmissions
calculated by IDSS.
Note
• Supplemental data may not be used for this measure.

Specifications Updates—Attachment C 47
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Table PCR-1/2/3: Plan Population and Outlier Rate (Medicaid, Commercial and Medicare, 18–64)
Age Sex
Members in Plan
Population
Outlier Members Nonoutlier Members Outlier Rate
18-44
Male
Female
Total
45-54
Male
Female
Total
55-64
Male
Female
Total
Total
Male
Female
Total
Table PCR-A-1/2/3: Plan All-Cause Readmissions Rates Among Nonoutlier Members by Age (Medicaid,
Commercial and Medicare, 18–64)
Age
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate Variance O/E Ratio
18-44
45-54
55-64
Total*
*The Total for Medicare for the data elements in this table must match the Total Medicare data elements in Table
PCR-B-3.
Table PCR-B-3: Plan All-Cause Readmissions Rates Among Nonoutlier Members by SES Stratification
(Medicare, 18–64)
SES Stratification
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate Variance O/E Ratio
Non-LIS/ DE,
Non-disability
LIS/DE
Disability
LIS/DE and
Disability
Other
Unknown
Total Medicare*
*The Total Medicare for the data elements in this table must match the Total for Medicare for the data elements in Table
PCR A-1/2/3.

Specifications Updates—Attachment C 48
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Table PCR-C-3: Plan All-Cause Readmissions Rates Among Nonoutlier Members Discharged or Transferred to
Skilled Nursing Care by Age (Medicare, 18–64)
Age
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate Variance O/E Ratio
18-44
45-54
55-64
Total
Table PCR-D-3: Plan Population and Outlier Rate (Medicare, 65+)
Age Sex
Members in Plan
Population
Outlier Members
Nonoutlier
Members
Outlier Rate
65-74
Male
Female
Total
75-84
Male
Female
Total
85+
Male
Female
Total
Total
Male
Female
Total
Table PCR-E-3: Plan All-Cause Readmissions Rates Among Nonoutlier Members by Age (Medicare, 65+)
Age
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate Variance O/E Ratio
65-74
75-84
85+
Total*
*The Total for Medicare for the data elements in this table must match the Total Medicare data elements in Table
PCR-F-3.

Specifications Updates—Attachment C 49
HEDIS 2019 Volume 2 Technical Update October 1, 2018
Table PCR-F-3: Plan All-Cause Readmissions Rates Among Nonoutlier Members by SES Stratification
(Medicare, 65+)
SES Stratification
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate Variance O/E Ratio
Non-LIS/ DE,
Non-disability
LIS/DE
Disability
LIS/DE and
Disability
Other
Unknown
Total Medicare*
* The Total Medicare for the data elements in this table must match the Total for Medicare for the data elements in Table
PCR-E-3.
Table PCR-G-3: Plan All-Cause Readmissions Rates Among Nonoutlier Members Discharged or Transferred to
Skilled Nursing Care by Age (Medicare, 65+)
Age
Count of
Index Stays
Count of
Observed
30-Day
Readmissions
Observed
Readmission
Rate
Count of
Expected
30-Day
Readmissions
Expected
Readmission
Rate
Variance
O/E Ratio
18-44
45-54
55-64
Total
